Page 1

SOMATOM Sensation Cardiac
Application Guide
Software Version A60
Page 2

2
The information presented in this application guide
is for illustration only and is not intended to be relied
upon by the reader for instruction as to the practice
of medicine. Any health care practitioner reading this
information is reminded that they must use their own
learning, training and expertise in dealing with their
individual patients.
This material does not substitute for that duty and is
not intended by Siemens Medical Solutions Inc., to
be used for any purpose in that regard. The drugs and
doses mentioned herein were specified to the best of
our knowledge. We assume no responsibility what is
over for the correctness of this information. Variations
may prove necessary for individual patients.
The treating physician bears the sole responsibility
for all of the parameters selected. The pertaining operating instructions must always be strictly followed
when operating the SOMATOM Sensation Cardiac.
The statutory source for the technical data are the
corresponding data sheets. To improve future versions
of this application guide, we would highly appreciate
your questions, suggestions and comments.
Please contact us:
CT Application Hotline:
Tel. no. +49-9191-18 80 88 (outside Germany)
0130-18 53 91 (in Germany)
Fax no. +49-9191-18 99 98
email: somatom.examinationprotocol@siemens.com
We express our sincere gratitude to the many customers
who contributed valuable input.
In addition I would like to stress at this point that the
SOMATOM Sensation Cardiac Application Guide is
based very much on the other SOMATOM Application
Guides which have been written by Dr. Xiao-Yan Chen,
Loke-Gie Haw and Bettina Klingemann.
Special thanks to Dr. med. Martin Heuschmid,
Universitätsklinikum Tübingen.
Editor: Ute Feuerlein
Page 3
3
3
Overview
General 8
HeartView CT 22
Bolus Tracking 54
WholeBodyAngio 62
LungCARE 64
CT Colonography 66
Children 68
Head 88
Neck 98
Thorax 102
Abdomen 112
Extremities 124
Page 4
4
Content
General 8
· Concept 8
· Scan Set Up 8
· Scan and Reconstruction 9
– Slice Collimation and Slice Width 9
– Pitch 10
– Recon Job 11
– Kernels 11
– Image Filter 11
· Effective mAs 12
· Dose Information 13
· CARE Dose 16
· How does it work 16
· Workflow 18
· Contrast Medium IV Injection 19
· How to Create your own Scan Protocols 20
Page 5
5
Content
HeartView CT 22
· The Basics 22
– Important Anatomical Structures
of the Heart 22
– Cardiac Cycle and ECG 25
– Temporal Resolution 25
– Technical Principles 26
– Preview Series Reconstruction 27
– ECG Trace Editor 28
– ECG Pulsing 28
– CardioCARE 29
– CardioSharp 29
· How to do it 30
– Calcium Scoring 30
– Hints in General 30
– Placement of ECG Electrodes 31
· CaScoreSpiStd 32
· CaScoreSpiStd0.5s 33
· CaScoreSeqStd 34
– Coronary CTA 35
– General Hints 36
· CoronaryStd 37
· CoronaryStd0.5s 38
· CorStd_LowHeartRate 39
· CoronaryCARE 40
· CoronaryCARE0.5s 41
· CoronarySharp 42
· CoronarySharp0.5s 44
· ECGTrigCTA 46
– Aortic and Pulmonary Studies 48
– General Hints 48
· PulmonaryECG 49
· Additional Important Information 50
Page 6
6
Content
Bolus Tracking 54
· The Basics 54
· How to do it 56
· CARE Bolus 56
– General Hints 56
· Test Bolus 58
– Application Procedures 59
· Additional Important Information 60
WholeBodyAngio 62
LungCARE 64
CT Colonography 66
Children 68
· Hints in General 69
· HeadSpi05s 72
· HeadSeq0.5s 74
· HeadAngio 76
· CarotidCTA 78
· NeonateBody 80
· ChestRoutine 82
· AbdPelRoutine 84
· AbdCTA 86
Head 88
· Overview 88
· Hints in General 89
· Angio Head 90
· AngioThinSlice 92
· HeadSeq0.5s 94
· HeadSpi0.5s 96
Neck 98
· Overview 98
· Hints in General 99
· AngioCarotid 100
Page 7
7
Content
Thorax 102
· Overview 102
· Hints in General 103
· LungLowDose 104
· PulmonaryEmboli 106
· ThoraxCombi 108
· ThoraxRoutine 110
Abdomen 112
· Overview 112
· Hints in General 113
· AbdRoutine 116
· AngioFast 118
· AngioRoutine 120
· AbdomenSeq 122
Extremities 124
· Overview 124
· Hints in General 125
· AngioRunOff 126
Page 8

8
General
Concept
The scan protocols for adult are defined according
to body regions – Head, Neck,Thorax, Abdomen,
Extremities.
The pediatric scan protocols are defined under the
folder “Children”.
The protocols for special applications are defined
under “Special”.
The general concept is as follows:
“Fast”: uses 1.5 mm slice collimation and a higher
pitch for fast acquisition for CT Angios or trauma cases.
“Routine”: uses either 0.75 mm or 1.5 mm slice
collimation depending on the region of interest for
routine studies.
“ThinSlice”: uses 0.75 mm slice collimation for
thin slice studies.
“Combi”: uses 0.75 mm as slice collimation and
reconstruct images as both thinner slice width for
HiRes or CTA and thicker slice width for soft tissue
studies.
“Seq”: stands for Sequence. E. g. “HeadSeq” means
the sequence mode for the head;
“Spi” stands for “Spiral”. E. g. “HeadSpi” means the
spiral mode for the head.
Scan Set Up
Scans can be simply set up by selecting a predefined
examination protocol. To repeat any mode, just click
the chronicle with the right mouse button for “repeat”.
To delete it, select “cut”. Each chronicle is rewriteable
before “load”.
Multiple ranges can be run either automatically with
“auto range”, or separately with a “pause” in between.
Page 9

9
General
Scan and Reconstruction
Slice Collimation and Slice Width
Slice collimation is the slice thickness collimated by
the tube collimator, which determines the Z-coverage
per rotation. In Multislice CT, this is divided by the
number of active detector channels (e.g. 16 x 0.75 mm).
Slice width is the true thickness of the reconstructed
image.
With the SOMATOM Sensation Cardiac, you select the
slice collimation together with the slice width desired,
the slice width is independent of pitch and algorithm,
i. e. what you select is always what you get. Actually,
you do not need to care about the algorithm any more;
the software does it for you.
On the SOMATOM Sensation Cardiac some slice widths
are marked as “fast” (blue background). These images
will be reconstructed with highest performance (up
to 6-10 images per second). All others will be reconstructed with up to 3 images per second.
The reconstruction time depends on slice collimation
and the reconstructed slice width. To get the fast
performance, slice width has to be at least 3 times the
slice collimation.
During scanning the user normally will get “real time”
reconstructed images in full image quality, if the “fast”
slice has been selected.
In some cases – this depends also on Scan range, Feed/
Rotation and Reconstruction increment – the Recon
icon on the chronicle will be labeled with “RT”. This indicates the real time display of images during scanning.
The real time displayed image series has to be reconstructed afterwards.
Page 10

10
General
The following tables show you the possibilities of image
reconstruction in spiral and sequential scanning.
Slice Collimation and Slice Width for Spiral Mode
0.75 mm 0.75, 1, 1.5, 2, 3, 4, 5, 6, 7, 8, 10 mm
1.5 mm 2, 3, 4, 5, 6, 7, 8, 10 mm
Cardio Spiral Modes
0.75 mm 0.75, 1.0, 1.5, 2,3 mm
1.5 mm 2, 3, 4, 5 mm
Slice Collimation and Slice Width for Sequence Mode
0.75 mm 0.75, 1.5, 3, 4.5, 9 mm
1.5 mm 1.5, 3, 4.5, 6, 9 mm
5 mm 5, 10 mm
ECG triggered Modes
0.75 mm 0.75, 1.5, 3 mm
1.5 mm 1.5, 3, 6 mm
Pitch
In single slice CT:
Pitch = table movement per rotation/slice collimation
E. g.: slice collimation = 5 mm,
table moves 5 mm per rotation, then pitch = 1.
With the SOMATOM Sensation Cardiac, in Siemens
Multislice CT, we differentiate between:
Feed/Rotation, the table movement per rotation
Volume Pitch, the table movement per rotation/single
slice collimation
E. g.: single slice collimation = 1.5 mm, table moves
24 mm per rotation, then the Volume Pitch = 16
Pitch Factor, the table movement per rotation/
collimation
E. g.: slice collimation = 16 x 1.5 mm, table moves
24 mm per rotation, then the Pitch Factor = 1
With the SOMATOM Sensation Cardiac, you do not
need to select pitch. Once the scan range, scan time,
slice collimation, and rotation time is defined, the
software will adapt the table feed per rotation accordingly. The Pitch Factor can be freely adapted from
0.5 to 1.5.
Page 11

11
General
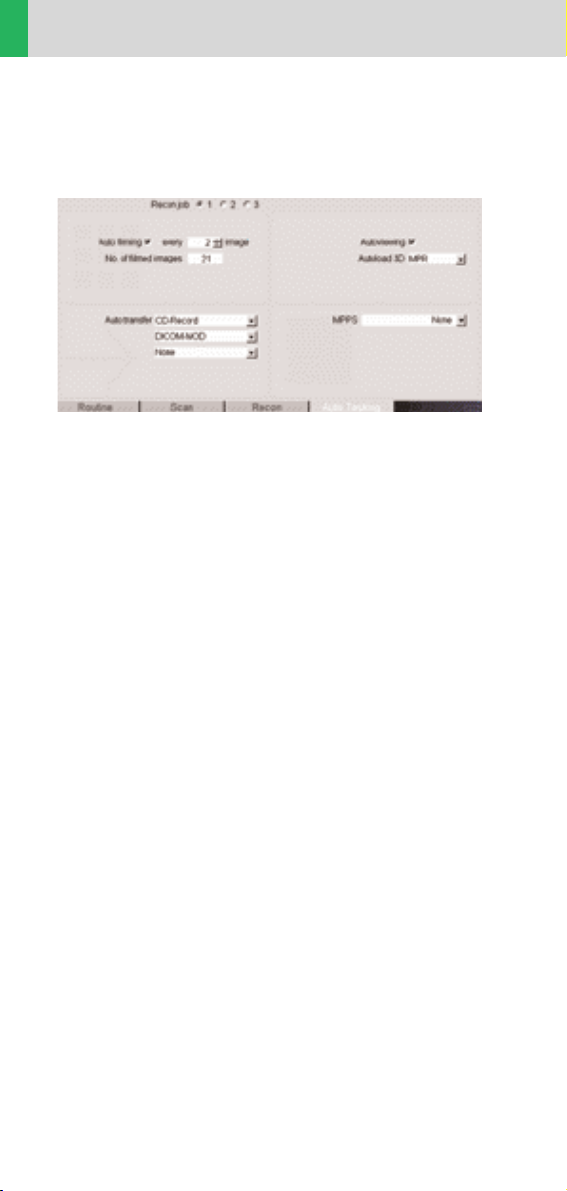
Recon Job
In the Recon card, you can define up to 3 reconstruction jobs with different parameters either before or
after you acquire the data. When you click on “Recon”,
they will all be done automatically. In case you want
to add another recon job, simply click the little icon on
the chronicle with the right mouse button and select
“delete recon job” to delete the one which has been
completed, and then one more recon job will be available in the Recon card (Note: what you delete is just
the job from the display, not the images that have
been reconstructed).
You can also reconstruct images for all scan modes
completed at once – do not select any chronicle before
you click “Recon”.
Kernels
There are 5 different types of kernels: “H” stands for
Head, “B” stands for Body and “C” stands for ChildHead.
The image sharpness are defined by the numbers –
the higher the number, the sharper the image; the
lower the number, the smoother the image.
Note: Do not use different kernels for other body parts
than designed for.
Image Filter
There are 4 different filters available:
PFO: To reduce beam-hardening artifacts in head
images, particularly in the base of the skull,
use the Posterior Fossa Optimization (PFO) filter.
ASA: The Advanced Smoothing Algorithm (ASA)
filter reduces noise in soft tissue while edges with high
contrast are preserved.
LCE: The Low-contrast enhancement (LCE) filter
enhances low-contrast detectability. It reduces the
image noise.
HCE: The High-contrast enhancement (HCE) filter
enhances high-contrast detectability. It increases the
image sharpness.
Page 12

12
General
Effective mAs
In sequential scanning, the dose (D
seq
) applied to the
patient is the product of the tube current-time (mAs)
and the CTDI
w
per mAs:
D
seq
= D
CTDI
w
x mAs
In spiral scanning, however, the applied dose (D
spiral
)
is influenced by the mAs (mA x Rot Time) and in addition by the Pitch Factor. For example, if a Multislice CT
scanner is used, the actual dose applied to the patient
in spiral scanning will be decreased when the Pitch
Factor is larger than 1, and increased when the Pitch
Factor is smaller than 1. Therefore, the dose in spiral
scanning has to be corrected by the Pitch Factor:
D
spiral
= (D
CTDI
w
x mA x Rot Time)/Pitch Factor
To make it easier for the users, the concept of the
effective mAs was introduced with the SOMATOM
Multislice scanners.
The effective mAs takes into account the influence of
pitch on both the image quality and dose:
Effective mAs = mAs/Pitch Factor
To calculate the dose on the SOMATOM Sensation
Cardiac, you simply have to multiply the CTDI
w
per mAs
with the effective mAs of the scan:
D
spiral
= D
CTDI
w
x effective mAs
For spiral scan protocols, the indicated mAs is the
effective mAs per image. The correlation between tube
current mA and effective mAs of spiral scans on a Multislice CT scanner is given by the following formula:
Effective mAs = mA x RotTime/Pitch Factor
Pitch Factor =
Feed/Rot
nrow x Slice collimation
mA =
effective mAs
x Pitch Factor
RotTime
where collimated Slice refers to the collimation of one
detector row, and nrow is the number of used detector
rows.
Page 13

13
General
Dose Information
The dose as described by CTDIwis displayed on the
user interface for the selected scan parameters. The
CTDI
w
is measured in the dedicated plastic phantoms –
16 cm diameter for head and 32 cm diameter for
body (as defined in IEC 60601-2-44). This dose number
gives a good estimate for the average dose applied
in the scanned volume as long as the patient size is
similar to the size of the respective dose phantoms.
Since the body size can be smaller or larger than 32 cm,
the CTDI value displayed can deviate from the dose in
the scanned volume.
The CTDI
w
value does not provide the entire information
of the radiation risk associated with CT examination.
For the purpose, the concept of the “Effective Dose“ was
introduced by ICRP (International Commission on
Radiation Protection). The effective dose is expressed
as a weighted sum of the dose applied not only to the
organs in the scanned range, but also to the rest of the
body. It could be measured in whole body phantoms
(Alderson phantom) or simulated with Monte Carlo
techniques.
The calculation of the effective dose is rather complicated and has to be done by sophisticated programs.
These have to take into account the scan parameters,
the system design of individual scanner, such as x-ray
filtration and gantry geometry, the scan range, the
organs involved in the scanned range and the organs
affected by scattered radiation. For each organ, the
respective dose delivered during the CT scanning has
to be calculated and then multiplied by its radiation
risk factor. Finally the weighted organ dose numbers
are added up to get the effective dose.
Page 14

14
General
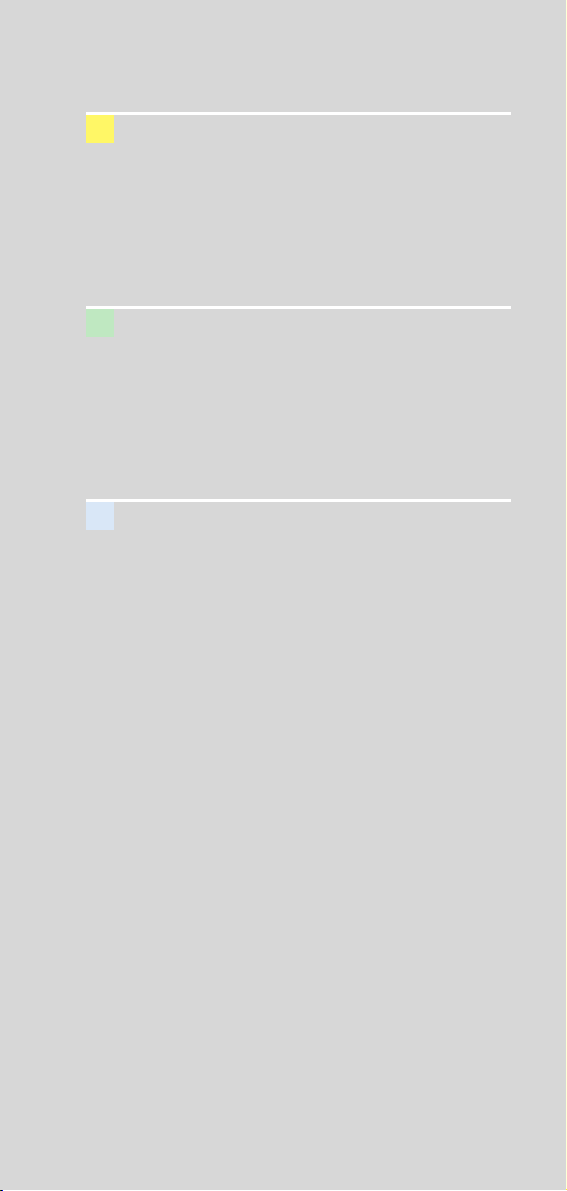
Fig. 1: User interface of the PC program WinDose.
All parameters necessary for the effective dose calculation have to be specified.
** The Calculation of Dose from External Photon Expo-
sures Using Reference Human Phantoms and Monte
Carlo Methods. M. Zankl et al. GSF report 30/91
** Radiation Exposure in Computed Topography, edited
by Hans Dieter Nagel, published by COCIR c/o ZVEI,
Stresemannallee 19, D-60596, Frankfurt, Germany.
The concept of effective dose would allow the comparison of radiation risk associated with different CT or
x-ray exams, i. e. different exams associated with the
same effective dose would have the same radiation risk
for the patient. It also allows comparing the applied
x-ray exposure to the natural background radiation,
e. g. 2 – 3 mSv per year in Germany.
For most of our scan protocols, we calculated the
effective dose numbers for standard male* and female*
and listed the result in the description of each scan
protocol.
The calculation was done by the commercially available program “WinDose“ (Wellhoefer Dosimetry) – as
shown in figure 1-3. For pediatric protocols, we used
the WinDose calculation and the correction factors
published in “Radiation Exposure in Computed Topography“**, in which there only the conversion factors
for the age of 8 weeks and 7 years old are available.
Page 15
15
General
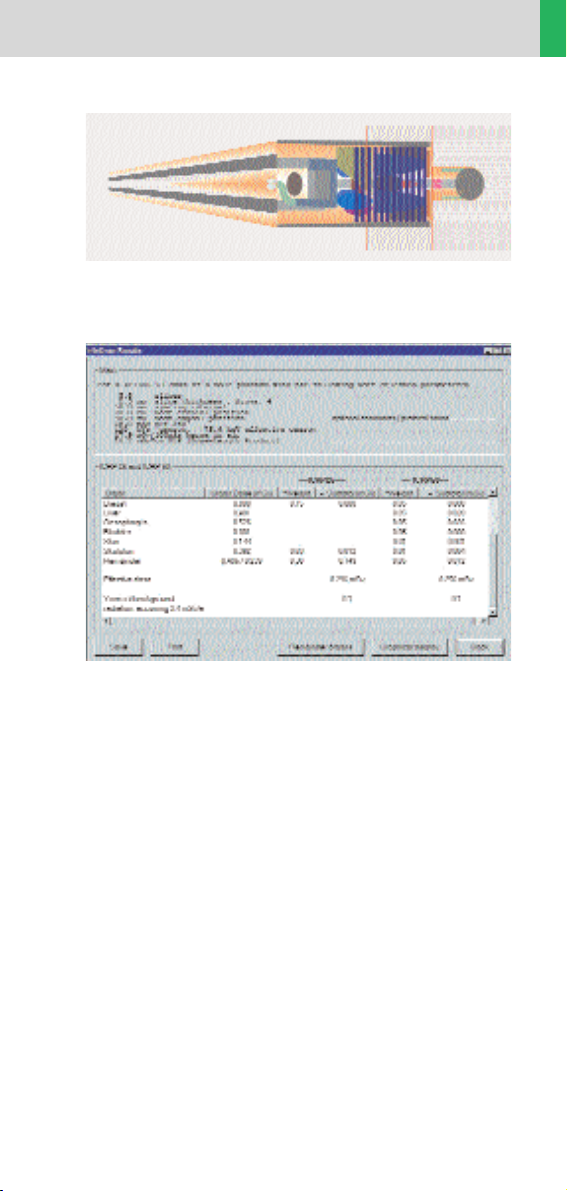
Fig. 2: A graphic interface of WinDose allows to
specify the anatomical scan range.
Fig.3: Results as output of WinDose with the organ
dose readings and the effective dose according
to ICRP26 (previous version) and ICRP60 (currently
valid).
Please note:
Effective dose values were calculated with the
WinDose™ Software Version 2.1, which was optimized
for SOMATOM Volume Zoom scanners.
SOMATOM Sensation Cardiac has modified shaped
filters which might cause slightly different effective
dose numbers ( difference not expected to be more
than 5%). An update of WinDose™ for the SOMATOM
Sensation Cardiac is currently developed.
Page 16
16
General
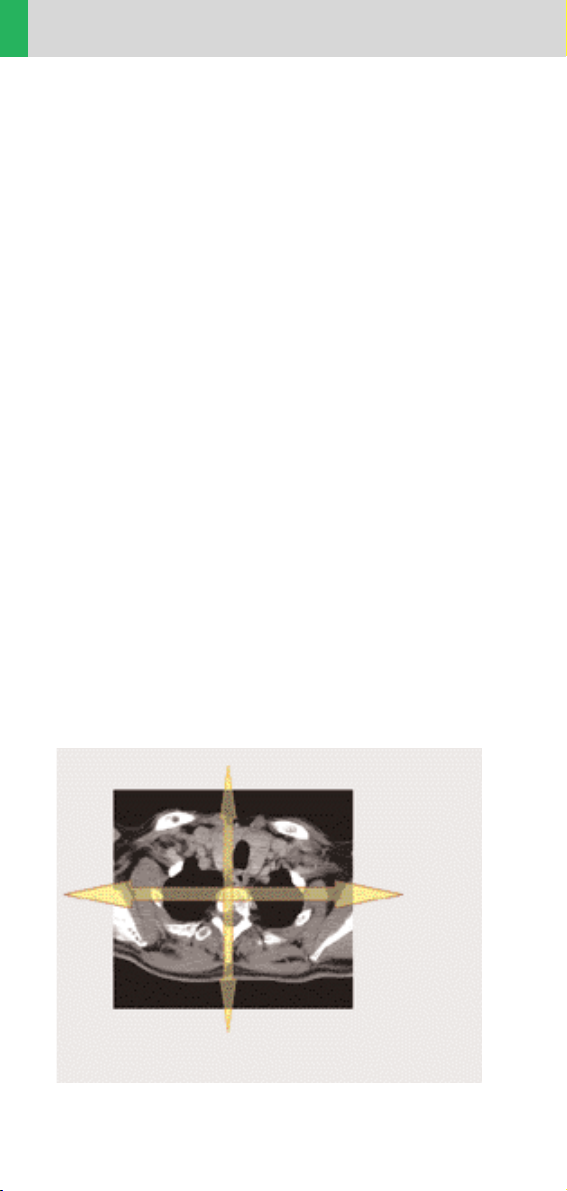
Fig. 1: Example of scanning in the region of shoulder.
CARE Dose
CARE Dose is a clinical application package that provides real-time tube current modulation for Spiral and
Sequential Scanning.
CARE Dose reduces patient dose significantly, especially in the regions of shoulder and pelvis. It decreases
tube load, which extends the capacity for volume
scanning with thinner slices, larger volumes or Multiphase studies.
It can also improve image quality by increasing mA
and thus reducing image noise on the lateral views.
How does it work
It reduces the mA for low attenuation views up to 90%
and keeps the nominal higher mA for high attenuation
views, e.g. in the lateral projection (Fig. 1). This is done
“on-the-fly”, i.e. the scanner adapts the mA in real-time,
according to the patient’s attenuation profile (Fig. 2).
High
attenuation,
high mA
Low attenuation,
low mA
Page 17
17
General
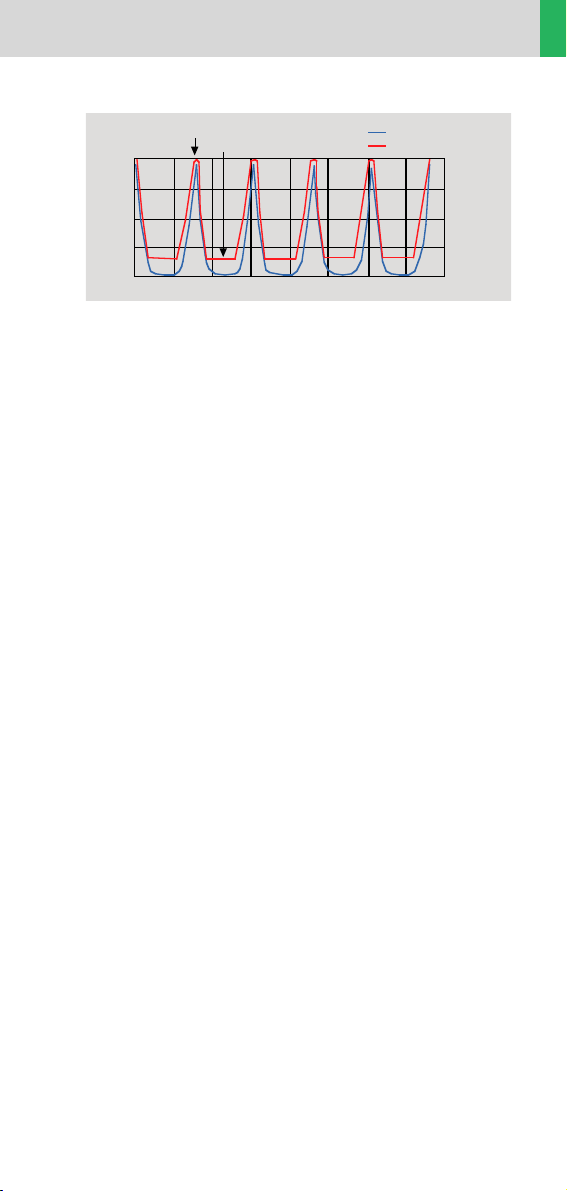
Fig. 2: Principle of CARE Dose tube current adaptation.
• CARE Dose is pre-selected by default for all standard
protocols, except head and cardiac protocols. It can
be switched on/off in the scan card.
• The application of CARE Dose does not require any
changes in the scan parameters. The mean value
of the mAs applied will be lower than what you have
selected.
• The mean value of the effective mAs applied is shown
in the image text.
lateral
1.00
0.75
0.50
0.25
rel. units
a.p.
time
Object attenuation
Modulated tube current
Page 18
18
General
Workflow
Auto Load in 3D and Postprocessing Presets
You can activate the “Auto load in 3D” function on the
Examination Card/Auto Tasking and link it to a recon
job. For example, the 2
nd
recon job with thinner slice
width in some of the examination protocols. If the postprocessing type is chosen from the pull down menu,
the reconstructed images will be loaded automatically
into the 3D Card on the Navigator with the corresponding postprocessing type.
On the 3D Card you have the possibility to create for
MPR and MIPthin Range Parallel and Radial protocols
which can be linked to a special series.
For example, if you always do some sagittal Multiplanar Reconstructions for a Spine examination, you load
once a Spine examination into the 3D Card. Select the
image type (MPR, MIPthin), select the orientation
and open the Range Parallel function. Adapt the range
settings (Image thickness, Distance between the
images etc.) and hit the link button. From now on, you
have a predefined postprocessing protocol, linked to
the series description of a Spine examination.
Exactly the same can be done for VRT presets. In the
main menu, under Type/VRT Definition, you can link
VRT presets with a series description.
Page 19
19
General
Some of the Scan protocols, mainly for Angio examinations, are already delivered with Auto load in 3D.
If you do not like, please deselect the Auto load in 3D
and save your scan protocol.
Some of the Scan protocols are delivered with links
to a postprocessing protocol. If you do not like our
suggestions, please delete the Range Parallel preset or
overwrite them with your own settings.
Contrast Medium IV Injection*
The administration of a contrast medium depends on
the indication and on the delay times to be used during
the examination. The patients weight and circulatory
situation also play a role. In general, no more than 3 ml
per kg of body weight for adults and 2 ml per kg of body
weight for children should be applied.
As a rule of thumb, the contrast medium injection
should be stopped when the scan (or acquisition)
is finished. Keep this in mind, you may save contrast
medium in your routine study since the Multislice
spiral scan can be up to 32 times faster than a 1 second,
single slice spiral scan.
For CTA study (arterial phase), the principle is to keep
contrast injection for the whole scan. Thus, the total
amount of contrast medium needed should be calculated with the following formula:
CM = (start delay time + scan time) x flow rate.
CARE Bolus or Test Bolus may be used for optimal
contrast bolus timing. Please refer to the Application
Guide for special protocols.
* For more information regarding the general use
of drugs and doses mentioned in this guide, please
refer to page 2.
Page 20

20
General
How to Create your own
Scan Protocols
User-specific scan protocols can be saved with the
following basic procedure:
– Register a test patient, patient position must be
head-supine.
– Select a scan protocol.
– Set the table position to 0 (either at the gantry panel,
or on the topogram routine card).
– Modify the scan protocol, change parameters,
add new ranges etc.
– Do not load the scan protocol.
– Select Edit/Save Scan Protocol in the main menu.
– Select the organ region and the scan protocol name
in the pop-up dialog. You can either use the same
name to modify the existing scan protocol, or enter
a new name.
Page 21
21
General
Tips:
– It is recommended that you save your own scan
protocol with a new name in order to avoid overwriting the default scan protocol.
– You may use preceding numbers (e.g. 1_Abdomen)
for user specific scan protocols to make them appear
on top of the list and to distinguish them from the
Siemens defaults.
– Do not use special characters like “/“, “.“ or “\“ within
scan protocol names.
– Don’t rename scan protocol files on Windows NT
level – this will lead to inconsistencies.
– Do not mix head and body scan protocols: e. g. do
not save a head mode in the abdomen directory.
– System/Run offers the tool “Restore Default Scan
Protocols“ which allows one to remove user specific
scan protocols and to restore the Siemens default
settings.
– System/Edit offers save/delete Scan Protocols.
– System/Run also offers the tool “List Scan Protocols”
which generates an HTML table of all available scan
protocols. This list can be printed or saved on Floppy
(“File/Save As…”).
Page 22

22
HeartView CT
HeartView CT
HeartView CT is a clinical application package
specifically tailored to cardiovascular CT studies.
The Basics
Important Anatomical Structures of the Heart
Four chambers:
• Right atrium – receives the deoxygenated blood
back from the body circulation through the superior
and inferior vena cava, and pumps it into the right
ventricle
• Right ventricle – receives the deoxygenated blood
from the right atrium, and pumps it into the pulmonary circulation through the pulmonary arteries
• Left atrium – receives the oxygenated blood back
from the pulmonary circulation through the pulmonary veins, and pumps it into the left ventricle
• Left ventricle – receives the oxygenated blood from
the left atrium, and pumps it into the body circulation
through the aorta.
Page 23
23
HeartView CT
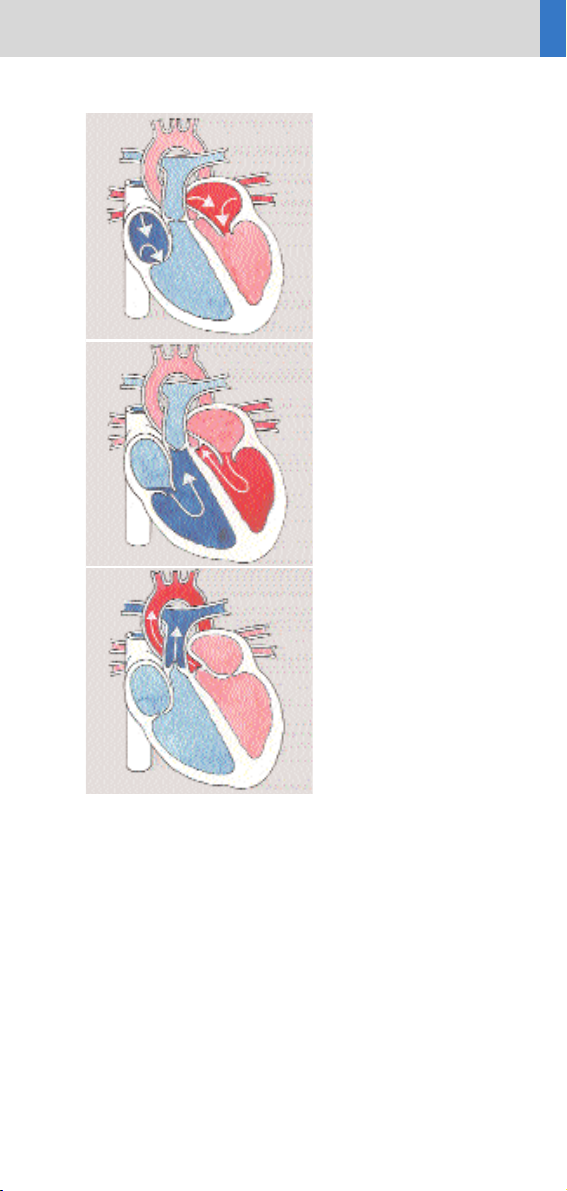
Fig. 1:
Blood fills both atria
Fig. 2:
Atria contract, blood
enters ventricles
A: Aorta
P: Pulmonary Artery
RV: Right Ventricle
LV: Left Ventricle
RA: Right Atrium
LA: Left Atrium
Fig. 3:
Ventricles contract,
blood enters into
aorta and pulmonary
arteries
RA
LA
A
P
RV
LV
Page 24
24
HeartView CT
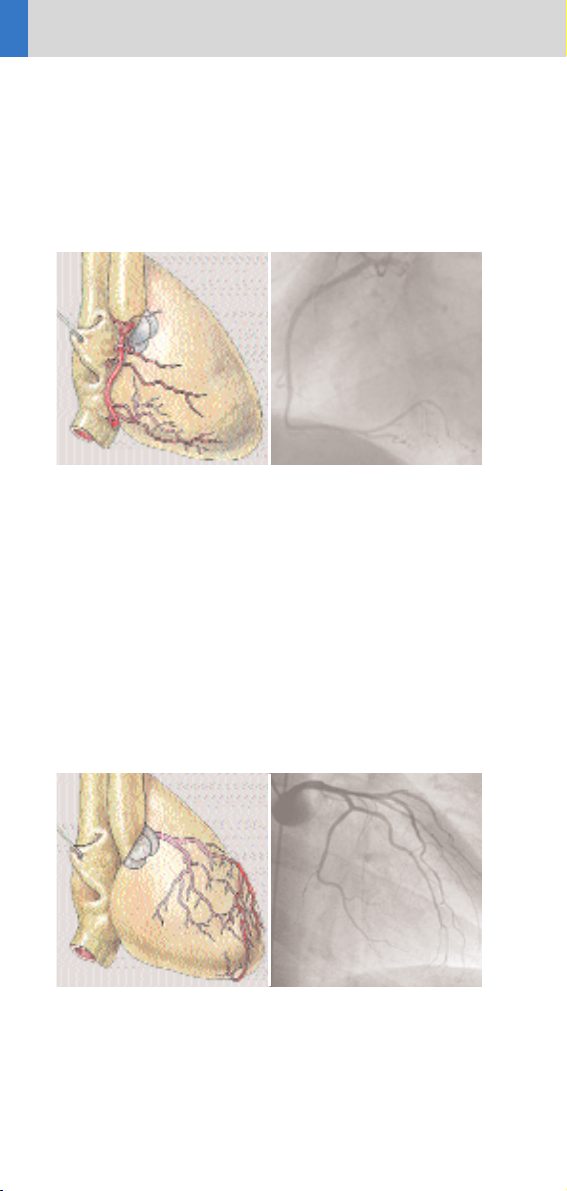
Coronary arteries:
• Right coronary artery (RCA)
Right coronary artery supplies blood to the right
atrium, right ventricle, a small part of the ventricular
septum.
• Left coronary artery (LCA)
Left coronary artery supplies blood to the left atrium,
left ventricle and a large part of the ventricular septum.
SVC:Superior Vena Cava
IVC: Inferior Vena Cava
RA: Right Atrium
RV: Right Ventricle
A: Aorta
PA: Pulmonary Artery
Fig. 4: Front view Fig. 5: Conventional
Angiography
LM: Left Main Artery
LAD: Left Anterior Descending Artery
Cx: Circumflex Artery
Fig. 6: Front view Fig. 7: Conventional
Angiography
RV
PA
RA
A
IVC
SVC
LM
Cx
LAD
➝
➝
➝
Page 25
25
HeartView CT
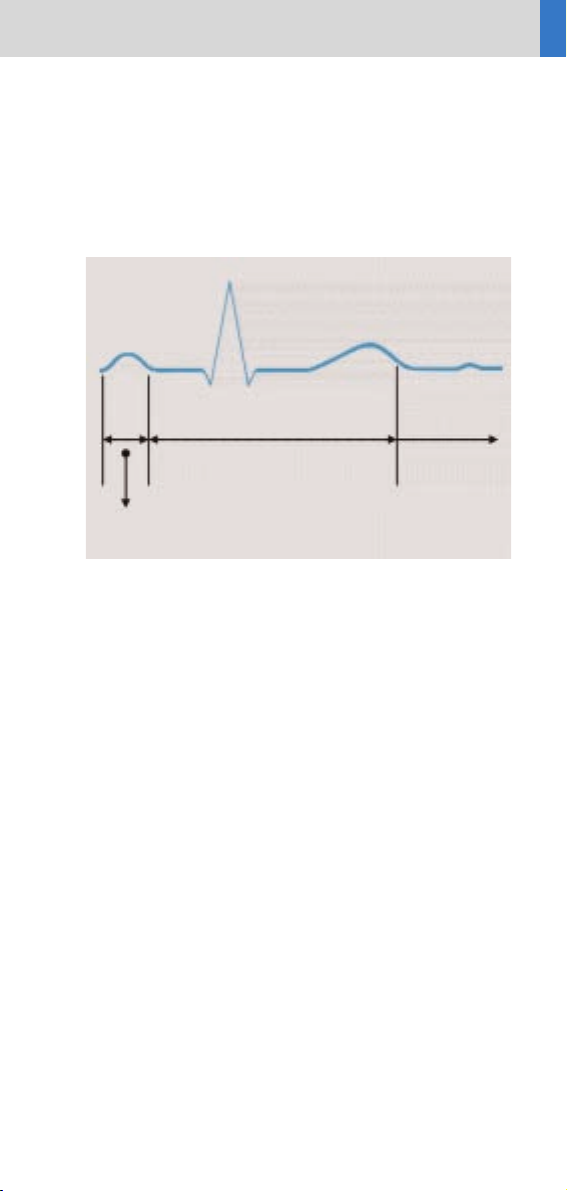
Cardiac Cycle and ECG
The heart contracts when pumping blood and rests
when receiving blood. This activity and lack of activity
form a cardiac cycle, which can be illustrated by an
Electrocardiograph (ECG) (Fig. 8).
To minimize motion artifacts in cardiac images, the
following two requirements are mandatory for a CT
system:
• Fast gantry rotation time in order to achieve fast
image acquisition time
• Prospective synchronization of image acquisition
or retrospective reconstruction based on the ECG
recording in order to produce the image during the
diastolic phase when the least motion happens.
Temporal Resolution
Temporal resolution, also called time resolution,
represents the time window of the data that is used for
image reconstruction. It is essential for cardiac CT
imaging – the higher the temporal resolution, the fewer
the motion artifacts. With the SOMATOM Sensation
Cardiac, temporal resolution for cardiac imaging can
be achieved at down to 105 ms.
Fig. 8
R
T
U
S
Q
P
Ventricular contraction
Systolic phase
Atrial contraction
Diastolic phase
Relaxation
Diastolic
phase
Page 26
26
HeartView CT
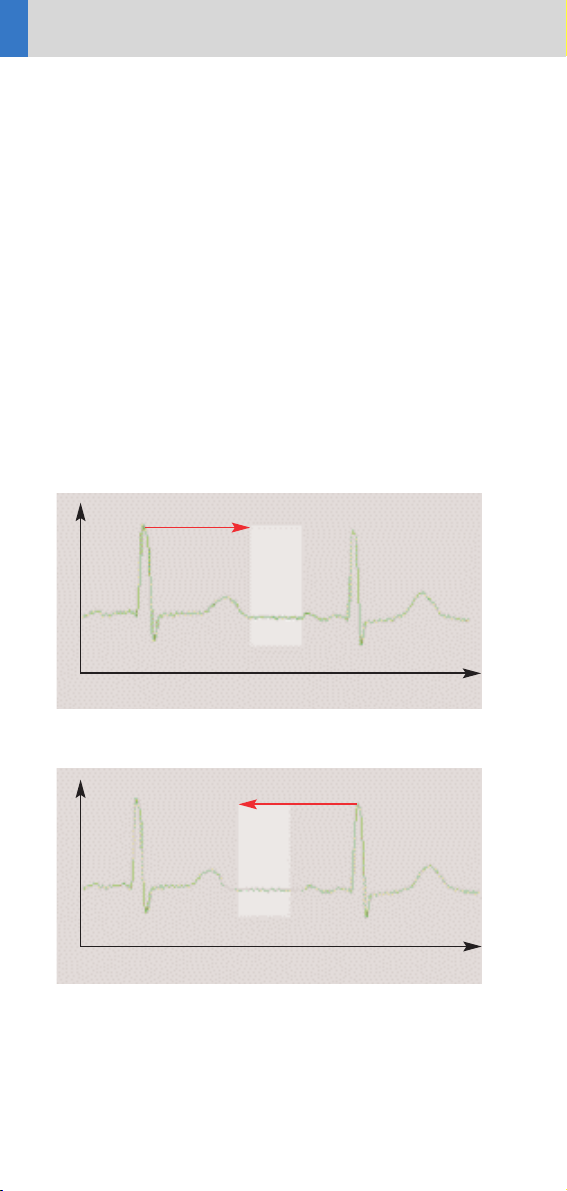
Technical Principles
Basically, there are two different technical approaches
for cardiac CT acquisition:
• Prospectively ECG triggered sequential scanning.
• Retrospectively ECG gated spiral scanning.
In both cases, an ECG is recorded and used to either
initiate prospective image acquisition (ECG triggering),
or to perform retrospective image reconstruction
(ECG gating). A given temporal relation relative to the
R-waves is predefined and can be applied with the
following possibilities:
Relative – delay: a given percentage of R-R interval (_RR)
relative to the onset of the previous or the next R-wave
(Fig. 9, 10).
Time
Time
ECG (t)
ECG (t)
50 % of R-R
-50 % R-R
Scan/
Recon
Scan/
Recon
Fig. 9
Fig. 10
Page 27
27
HeartView CT
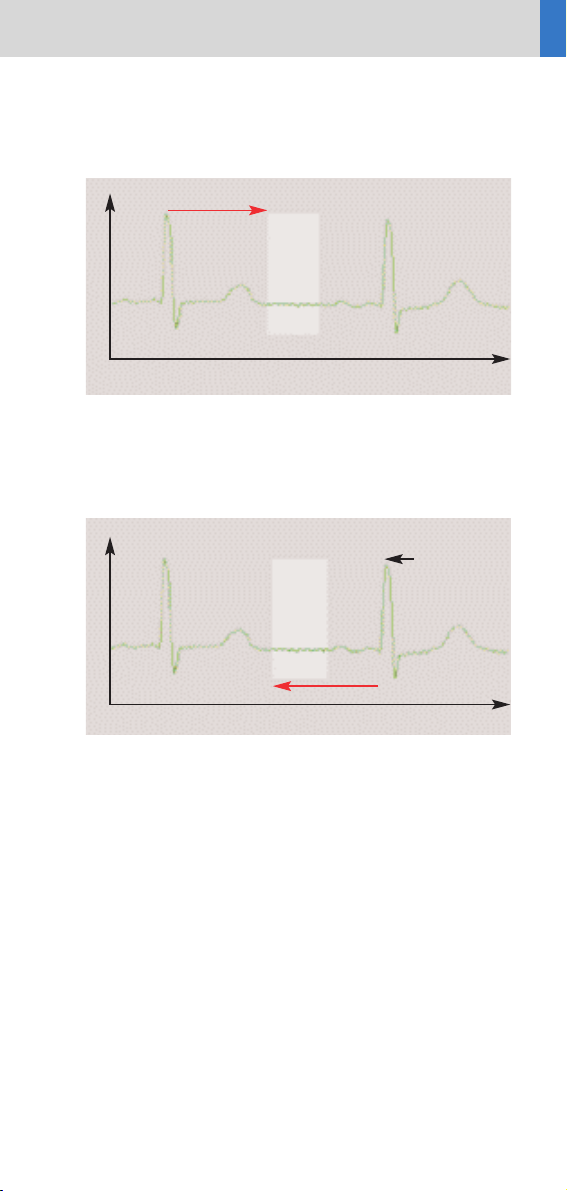
Absolute – delay: a fixed time delay after the onset of
the R-wave (Fig. 11).
Absolute – reverse: a fixed time delay prior to the onset
of the next R-wave (Fig. 12).
Preview Series Reconstruction
Preview series can be used to define the optimal time
window before the full series is reconstructed.
Click on the preview series button in the Trigger card.
The slice position of the preview series is based on the
currently displayed image in the tomogram segment,
which has to be chosen by the user.
Fig. 11
Time
Estimated
R-Peak
ECG (t)
-400 msec
Scan/
Recon
Fig. 12
Time
ECG (t)
400 msec
Scan/
Recon
Page 28
28
HeartView CT
ECG Trace Editor
The ECG trace editor is used for adaptation of image
reconstruction to irregular heart rates. This editing
tool can be used after the scan is acquired. By using
the right mouse menu on the Trigger card you can use
several modification tools for the ECG Sync, such as
Delete, Disable, Insert. To reset the ECG curve select
the check box Original ECG.
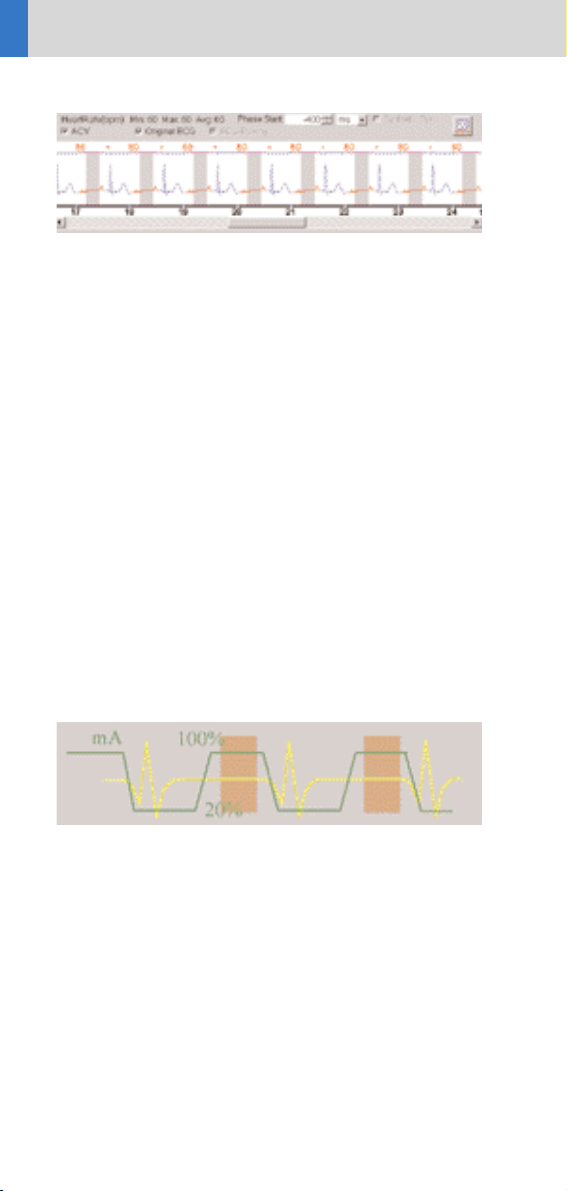
ECG Pulsing
ECG Pulsing is a dedicated technique used for online
dose modulation for Cardiac imaging. The tube current
is ECG-controlled and reduced during systolic phases
of the cardiac cycle while maintained normal during
diastolic phases when best image quality is required.
As shown in figure 13, essential dose reduction up to
50% can be achieved. It can be switched on/off by the
user (Fig. 14).
Fig. 13: Dose modulation with ECG pulsing.
Page 29
29
HeartView CT
Fig. 14
CardioCARE
This is a dedicated cardiac filter which can reduce
image noise thus provides the possibility of dose reduction. It is applied in a pre-defined scan protocol called
“CoronaryCARE.”
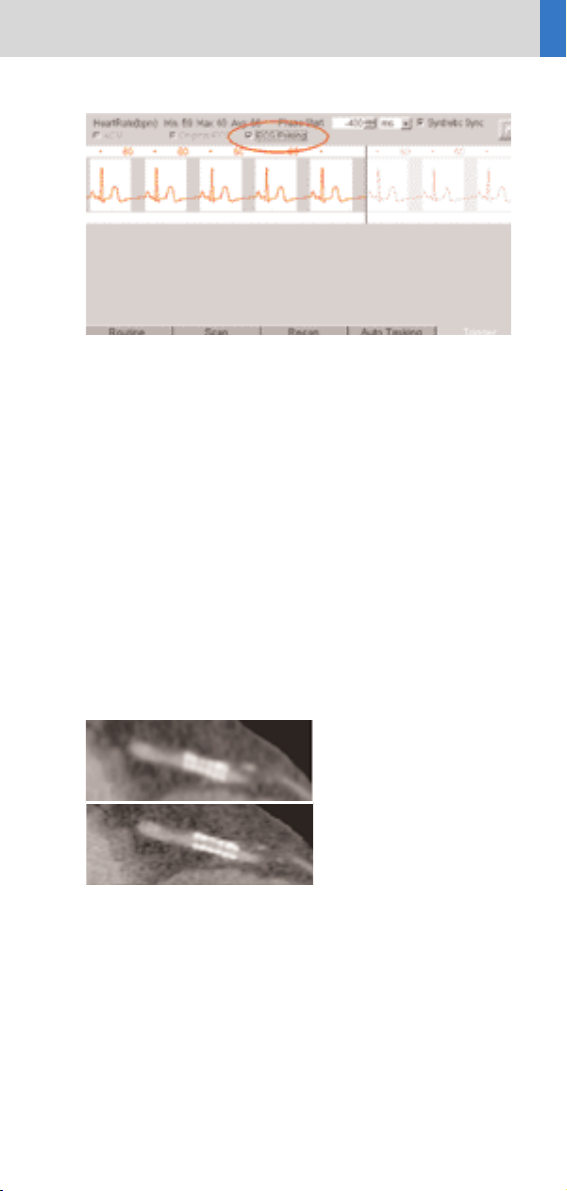
CardioSharp
This is a dedicated reconstruction kernel used for
better edge definition in coronary artery imaging. It is
applied in a pre-defined cardiac scan protocol called
“CoronarySharp.”
Image examples are shown in figure 15.
Fig. 15:
Image reconstruction
with (15b)
and without (15a)
Cardio Sharp kernel.
15a
15b
Page 30

30
HeartView CT
How to do it
Calcium Scoring
This application is used for identification and quantification of calcified lesions in the coronary arteries. It
can be performed with both ECG triggering (sequential scanning) and gating (spiral scanning) techniques.
The following scan protocols are predefined:
• CaScoreSpiStd
– Standard spiral scanning protocol with ECG gating
and a 0.42 s Rotation Time
• CaScoreSpiStd0.5s
– Standard spiral scanning protocol with ECG gating
and a 0.5 s Rotation Time
• CaScoreSeqStd
– Sequential scanning protocol with ECG triggering
Hints in General:
• Kernel B35f is dedicated to calcium scoring studies.
To ensure the best image quality and correlation to
known reference data, other kernels are not recommended.
• Use the ECG triggered protocol generally except for
patients with arrhythmia. Use the ECG gated protocol
when accuracy and/or reproducibility are essential,
e.g. follow-up studies of calcium scoring or comparison studies with conventional angiography.
• The protocol with 0.42 s Rotation Time can be
applied to all examinations for HeartView CT.
Temporal resolution for cardiac imaging can be
achieved at down to 105 ms.
The temporal resolution for the protocol with 0.5 s
Rotation Time can be achieved at down to 125 ms.
• We recommend a tube voltage of 120 kV. If the tube
voltage is lowered to 80 kV please use at least effective mAs 250. The use of 80 kV is not advised for large
patients.
Page 31

31
HeartView CT
Placement of ECG Electrodes:
US Version (AHA standard)
White Electrode
on the right mid-clavicular line, directly below the
clavicle
Black Electrode:
on the left mid-clavicular line, 6 or 7 intercostal space
Red Electrode:
right mid-clavicular line, 6 or 7 intercostal space
Placement of ECG Electrodes:
Europe Version (IEC standard)
Red Electrode:
on the right mid-clavicular line, directly below the
clavicle
Yellow Electrode:
on the left mid-clavicular line, 6 or 7 intercostal space
Black Electrode:
right mid-clavicular line, 6 or 7 intercostal space
Page 32

32
HeartView CT
CaScoreSpiStd
Indications:
This is a standard spiral scanning protocol, using
an ECG gating technique for coronary calcium scoring
studies, with a rotation time of 0.42 seconds.
Topogram:
AP, 512 mm.
From the carina until
the apex of the heart.
A typical range of
15 cm covering the
entire heart can
be done in 11.6 s.
CaScoreSpiStd
kV 120
Effective mAs 133
Slice collimation 1.5 mm
Slice width 3 mm
Feed/Rotation 5.7 mm
Rotation time 0.42 sec.
Temporal Resolution Up to105 ms*
Kernel B35f
Increment 1.5 mm
Image order cr-ca
CTDI
w
9.6 mGy
Effective Dose Male: 2.1 mSv
Female: 3.1 mSv
* Depends on heart rate.
Page 33

33
HeartView CT
* Depends on heart rate.
CaScoreSpiStd0.5s
Indications:
This is a spiral scanning protocol, using an ECG gating
technique for coronary calcium scoring studies, with
a rotation time of 0.5 seconds.
Topogram:
AP, 512 mm.
From the carina until
the apex of the heart.
A typical range of
15 cm covering the
entire heart can
be done in 11.7 s.
CaScoreSpiStd0.5s
kV 120
Effective mAs 133
Slice collimation 1.5 mm
Slice width 3 mm
Feed/Rotation 6.8 mm
Rotation time 0.5 sec.
Temporal Resolution Up to125 ms*
Kernel B35f
Increment 1.5 mm
Image order cr-ca
CTDI
w
9.6 mGy
Effective Dose Male: 2.1 mSv
Female: 3.1 mSv
Page 34

34
HeartView CT
CaScoreSeqStd
Indications:
This is a sequential scanning protocol using an ECG
triggering technique for coronary calcium scoring
studies.
Topogram:
AP, 512 mm.
From the carina until
the apex of the heart.
CaScoreSeqStd
kV 120
Effective mAs 30
Slice collimation 1.5 mm
Slice width 3 mm
Feed/Rotation 18 mm
Rotation time 0.42 sec.
Temporal resolution 210 ms
Kernel B35f
Image order cr-ca
CTDI
w
2.2 mGy
Effective Dose Male: 0.5 mSv
Female: 0.7 mSv
If you apply API for image acquisition, please make
sure that the breathhold interval in the Patient Model
Dialog is longer than the total scan time, e.g. 50 s,
otherwise the image acquisition will be interrupted by
the default breathhold interval. This does not apply
when API is not activated.
Page 35

35
HeartView CT
Coronary CTA
This is an application for imaging of the coronary
arteries with contrast medium. It can be performed
with both ECG triggering and gating techniques. The
following scan protocols are predefined:
• CoronaryStd
– Standard spiral scanning protocol with ECG gating,
using a rotation time of 0.42 seconds.
• CoronaryStd0.5s
– Standard spiral scanning protocol with ECG gating,
using a rotation time of 0.5 seconds.
• CorStd_LowHeartRate
– Special spiral scanning protocol with ECG gating,
using a 0.42 second rotation time, for patients with
a heart rate below 50 bpm.
• CoronaryCARE
– Spiral scanning protocol with rotation time
0.42 s and dedicated cardiac filter (Cardio CARE)
which reduces image noise thus makes dose
reduction possible.
• CoronaryCARE0.5s
– Spiral scanning protocol with rotation time
0.5 s, and dedicated cardiac filter (Cardio CARE)
which reduces image noise thus makes dose
reduction possible.
• CoronarySharp
– Spiral scanning protocol with rotation time
0.42 s and dedicated reconstruction kernel for better
edge definition in coronary artery imaging.
• CoronarySharp0.5s
– Spiral scanning protocol with rotation time
0.5 s and dedicated reconstruction kernel for better
edge definition in coronary artery imaging.
• ECGTrigCTA
– Sequential scanning protocol with ECG triggering,
using a rotation time of 0.42 s.
Page 36

36
HeartView CT
General Hints:
• Generally speaking, the ECG gated protocol is recommended for premium image quality of the coronary
arteries, and whenever 3D postprocessing, such as
MPR, MIP, VRT or Fly Through, is required.
• Always use the ECG gated protocol for patients with
arrhythmia.
Page 37

37
HeartView CT
CoronaryStd
Indications:
This is a standard spiral scanning protocol, using a
Rotation Time of 0.42 s, with an ECG gating technique
for coronary CTA studies.
Topogram:
AP, 512 mm.
Approximately, from
the carina until the
apex of the heart.
A typical range of
12 cm covering the
entire heart can
be done in 18.7 s.
CoronaryStd
kV 120
Effective mAs 500
Slice collimation 0.75 mm
Slice width 1 mm
Feed/Rotation 2.8 mm
Rotation time 0.42 sec.
Temporal resolution Up to 105 ms*
Kernel B30f
Increment 0.5 mm
Image order cr-ca
CTDI
w
42.0 mGy
Effective dose Male: 7.0 mSv
Female: 10.2 mSv
* Depends on heart rate.
Page 38

38
HeartView CT
CoronaryStd0.5s
Indications:
This is a standard spiral scanning protocol, using a
Rotation Time of 0.5 s, with an ECG gating technique
for coronary CTA studies.
Topogram:
AP, 512 mm.
Approximately, from
the carina until the
apex of the heart.
A typical range of
12 cm covering the
entire heart can
be done in 18.4 s.
CoronaryStd0.5s
kV 120
Effective mAs 500
Slice collimation 0.75 mm
Slice width 1 mm
Feed/Rotation 3.4 mm
Rotation time 0.5 sec.
Temporal resolution Up to 125 ms*
Kernel B30f
Increment 0.5 mm
Image order cr-ca
CTDI
w
42.0 mGy
Effective dose Male: 7.0 mSv
Female: 10.2 mSv
* Depends on heart rate.
Page 39

39
HeartView CT
CorStd_LowHeartRate
Indications:
This is a special spiral scanning protocol for coronary
CTA studies. It uses ECG gating technique and a 0.42 s
rotation time, and should be used for patients with
heart rate below 50 bpm.
Topogram:
AP, 512 mm.
Approximately, from
the carina until the
apex of the heart.
A typical range of
12 cm covering the
entire heart can
be done in 23.7 s.
CoronaryStdLow
kV 120
Effective mAs 500
Slice collimation 0.75 mm
Slice width 1.0 mm
Feed/Rotation 2.2 mm
Rotation time 0.42 sec.
Temporal resolution Up to 105 ms*
Kernel B30f
Increment 0.5 mm
Image order cr-ca
CTDI
w
42.0 mGy
Effective dose Male: 7.0 mSv
Female: 10.2 mSv
* Depends on heart rate.
Page 40

40
HeartView CT
CoronaryCARE
Indications:
This is a spiral scanning protocol, using a rotation
time of 0.42 s, ECG gating technique and a dedicated
cardiac filter which can reduce images noise thus
makes the dose reduction possible for coronary CTA
studies.
Topogram:
AP, 512 mm.
Approximately, from
the carina until the
apex of the heart.
A typical range of
12 cm covering the
entire heart can
be done in 18.7 s.
CoronaryCARE
kV 120
Effective mAs 267
Slice collimation 0.75 mm
Slice width 1 mm
Feed/Rotation 2.8 mm
Rotation time 0.42 sec.
Temporal resolution Up to 105 ms*
Kernel B30f
Increment 0.5 mm
Image order cr-ca
CTDI
w
22.4 mGy
Effective dose Male: 3.8 mSv
Female: 5.5 mSv
* Depends on heart rate.
Page 41

41
HeartView CT
CoronaryCARE0.5s
Indications:
This is a spiral scanning protocol, using a Rotation
Time of 0.5 s, ECG gating technique and a dedicated
cardiac filter which can reduce images noise thus
makes the dose reduction possible for coronary CTA
studies.
Topogram:
AP, 512 mm.
Approximately, from
the carina until the
apex of the heart.
A typical range of
12 cm covering the
entire heart can
be done in 18.4 s.
CoronaryCARE0.5s
kV 120
Effective mAs 267
Slice collimation 0.75 mm
Slice width 1 mm
Feed/Rotation 3.4 mm
Rotation time 0.5 sec.
Temporal resolution Up to 125 ms*
Kernel B30f
Increment 0.5 mm
Image order cr-ca
CTDI
w
22.4 mGy
Effective dose Male: 3.8 mSv
Female: 5.5 mSv
* Depends on heart rate.
Page 42

42
HeartView CT
CoronarySharp
Indications:
This is a spiral scanning protocol, using a Rotation
Time of 0.42 s, ECG gating technique and a dedicated
cardiac reconstruction kernel for better edge definition in coronary artery imaging.
Topogram:
AP, 512 mm.
Approximately, from
the carina until the
apex of the heart.
A typical range of
12 cm covering the
entire heart can
be done in 18.7 s.
CoronarySharp
kV 120
Effective mAs 500
Slice collimation 0.75 mm
Slice width 1 mm
Feed/Rotation 2.8 mm
Rotation time 0.42 sec.
Temporal resolution Up to 105 ms*
Kernel B46f
Increment 0.5 mm
Image order cr-ca
CTDI
w
42.0 mGy
Effective dose Male: 7.0 mSv
Female: 10.2 mSv
* Depends on heart rate.
Page 43

43
HeartView CT
Page 44

44
HeartView CT
CoronarySharp0.5s
Indications:
This is a spiral scanning protocol, using a Rotation
Time of 0.5 s, ECG gating technique and a dedicated
cardiac reconstruction kernel for better edge definition in coronary artery imaging.
Topogram:
AP, 512 mm.
Approximately, from
the carina until the
apex of the heart.
A typical range of
12 cm covering the
entire heart can
be done in 18.4 s.
* Depends on heart rate.
CoronarySharp0.5s
kV 120
Effective mAs 500
Slice collimation 0.75 mm
Slice width 1 mm
Feed/Rotation 3.4 mm
Rotation time 0.5 sec.
Temporal resolution Up to 125 ms*
Kernel B46f
Increment 0.5 mm
Image order cr-ca
CTDI
w
42.0 mGy
Effective dose Male: 7.0 mSv
Female: 10.2 mSv
Page 45

45
HeartView CT
Fig. 1:
Image reconstruction
with (a)
and without (b)
Cardio Sharp kernel.
a
b
Page 46

46
HeartView CT
ECGTrigCTA
Indications:
This is a sequential scanning protocol with an ECG
triggering technique for coronary CTA studies. It could
also be applied for aortic CTA studies, e.g. aortic
dissection.
Topogram:
AP, 512 mm.
From the aortic arch
until the apex of the
heart.
If you apply API for a single breathhold acquisition,
please make sure that the breathhold interval in the
Patient Model Dialog is longer than the total scan
time, e.g. 50 s, otherwise the image acquisition will be
interrupted by the default breathhold interval. This
does not apply when API is not activated.
For longer ranges, e.g. the entire thoracic aorta,
that can not be acquired within a single breathhold,
please ensure that the breathhold interval in the
Patient Model Dialog is set up correctly, according to
the patient’s level of cooperation.
Page 47

47
HeartView CT
ECGTrigCTA
kV 120
Effective mAs 120
Slice collimation 1.5 mm
Slice width 1.5 mm
Feed/Scan 18 mm
Rotation time 0.42 sec.
Temporal resolution 210 ms
Kernel B30f
Image order cr-ca
CTDI
w
8.64 mGy
Effective dose Male: 1.5 mSv
Female: 2.2 mSv
Page 48

48
HeartView CT
Aortic and Pulmonary Studies
The following scan protocol is predefined:
• PulmonaryECG
– Spiral scanning protocol with ECG gating
General Hints:
• The PulmonaryECG protocol is recommended for
aortic or pulmonary studies, e. g. aorta dissection or
pulmonary emboli.
Page 49

49
HeartView CT
PulmonaryECG
Indications:
This is a spiral scanning protocol with an ECG gating
technique for aortic and pulmonary studies, e.g. aortic
dissection or pulmonary emboli.
PulmonaryECG
kV 120
Effective mAs 200
Slice collimation 1.5 mm
Slice width 3.0 mm
Feed/Rotation 5.6 mm
Rotation time 0.42 sec.
Temporal resolution Up to 105 ms*
Kernel B30f
Increment 2.0 mm
Image order cr-ca
CTDI
w
14.4 mGy
Effective dose Male: 5.7 mSv
Female: 7.3 mSv
Topogram:
AP, 512 mm.
From the aorta arch
until the tip of the
sternum.
A typical range of
30 cm can be covered
in 23 s.
* Depends on heart rate.
Page 50

50
HeartView CT
Additional Important
Information
By default, the “Synthetic Trigger” (ECG triggered
scanning) or “Synthetic Sync” (ECG gated scanning) is
activated for all predefined cardiac scan protocols
(Fig. 1 and 2). And it is recommended to keep it always
activated for examinations with contrast medium.
In case of ECG signal loss during the acquisition, this
will ensure the continuation of the triggered scans or
allows an ECG to be simulated for retrospective gating.
If it is deactivated, the scanning will be aborted in case
of ECG signal loss during the acquisition.
Fig. 2
Fig. 1
Page 51

51
HeartView CT
ACV (Adaptive Cardio Volume) (Fig. 3) is a dedicated
algorithm for bi-phase image reconstruction. The image
temporal resolution of 105 ms can be achieved with
ACV. By default, it is switched on for all coronary CTA
scan protocols, and switched off for all calcium scoring
scan protocols. And it is not recommend to change this
default setting.
Fig. 3
Page 52

52
HeartView CT
You can activate the “Auto load in 3D” function on the
Examination Card/Auto Tasking and link it to a recon
job. If the postprocessing type is chosen from the pull
down menu, the reconstructed images will be loaded
automatically into the 3D Card on the Navigator with
the corresponding postprocessing type.
On the 3D Card you have the possibility to create for
MPR, MIPthin Range Parallel and Radial protocols which
can be linked to a special series.
For example, if you always do MIP Reconstructions for
a Coronary CTA examination, you load once the images
into the 3D Card. Select the image type (e.g. MIPthin)
and the orientation, and then open the Range Parallel
function. Adapt the range settings (Image thickness,
Distance between the images etc.), hit the link button
and save. From now on, you have a predefined postprocessing protocol, linked to the series description of
a coronary CTA examination.
Exactly the same can be done for VRT presets. In the
main menu, under Type/VRT Definition, you can link
and save VRT presets with a series description.
Some of the Scan protocols are delivered with links
to a postprocessing protocol. If you do not like our
suggestions, please delete the Range Parallel preset or
overwrite them with your own settings.
Page 53

53
HeartView CT
Calcium Scoring evaluation is performed on a separate
syngo task card:
1. The threshold of 130 HU is applied for score
calculation by default, however, you can modify it
accordingly.
2. In addition to the seeding method, you can use
freehand ROI for the definition of lesions.
3. The separation and modification of lesions within
a defined volume (depth in mm) can be performed
not only on 2D slices, but also with 3D editing.
4. For easier identification of small lesions, you can
blowup the display.
5. You can customize hospital/office information on
the final report using Report Configuration.
6. You can generate HTML report including site specific information, free text and clinical images. This
then can be saved on floppy disc and/or printed.
7. The results are displayed online in a separate
segment including the following information:
– Area (in mm
3
)
– Peak density (in HU)
– Volume (in mm
3
)
– Calcium mass (mg calcium Hydroxyapatite)
– Score (Agatston method)
8. The results can be printed on laser film, paper
printer or saved into data base.
User interface of syngo Calcium Scoring
Page 54

54
Bolus Tracking
The Basics
The administration of intravenous (IV) contrast
material during spiral scanning improves the detection
and characterization of lesions, as well as the opacity
of vessels. The contrast scan will yield good results
only if the acquisition occurs during the optimal phase
of enhancement in the region of interest. Therefore,
it is essential to initiate the acquisition with the correct
start delay. Since Multislice spiral CT can provide much
faster speed and shorter acquisition time, it is even
more critical to get the right timing to achieve optimal
results (Fig. 1a,1b).
The dynamics of the contrast enhancement is
determined by:
• Patient cardiac output
• Injection rate (Fig. 2a, 2b)
• Total volume of contrast medium injected
(Fig. 3a, 3b)
• Concentration of the contrast medium (Fig. 3b, 4a)
• Type of injection – uni-phasic or bi-phasic
(Fig. 4a, 4b)
• Patient pathology
Fig. 1a: Longer scan time Fig. 1b: Shorter scan time
40 s scan 10 s scan
Page 55

55
Bolus Tracking
Aortic time-enhancement curves after i.v. contrast
injection (computer simulation*).
All curves are based on the same patient parameters
(male, 60-year-old, 75 kg).
Fig. 2a: 2 ml/s,
120 ml, 300 mg I/ml
Fig. 2b: 4 ml/s,
120 ml, 300 mg I/ml
Fig. 3a: 80 ml,
4 ml/s, 300 mg I/ml
Fig. 3b:120 ml,
4 ml/s, 300 mg I/ml
Fig. 4a: Uni-phase
140 ml, 4 ml/s,
370 mg I/ml
Fig. 4b: Bi-phase
70 ml, 4 ml/s, plus 70 ml,
2 ml/s, 370 mg I/ml
*Radiology 1998; 207:647-655
Relative Enhancement [HU]
Time [s]
0 20406080100 120
300
250
200
150
100
50
0
Relative Enhancement [HU]
Time [s]
0 20406080100 120
300
250
200
150
100
50
0
Relative Enhancement [HU]
Time [s]
020406080100120
400
350
300
250
200
150
100
50
0
Relative Enhancement [HU]
Time [s]
0 20 40 60 80 100 120
300
250
200
150
100
50
0
Relative Enhancement [HU]
Time [s]
0 20406080100 120
300
250
200
150
100
50
0
Relative Enhancement [HU]
Time [s]
0 20406080100 120
300
250
200
150
100
50
0
Page 56

56
Bolus Tracking
How to do it
To achieve optimal results in contrast studies, use of
CARE Bolus is recommended. In case it is not available,
use Test Bolus.
CARE Bolus
This is an automatic bolus tracking program, which
enables triggering of the spiral scanning at the optimal
phase of the contrast enhancement.
General Hints:
1. This mode can be applied in combination with
any spiral scanning protocol. Simply insert “Bolus
tracking” by clicking the right mouse button in
the chronicle. This inserts the entire set up including
pre-monitoring, i. v. bolus and monitoring scan
protocol. You can also save the entire set up as your
own scan protocols (please refer to page 20 “How
to Create your own Scan Protocols”).
2. The pre-monitoring scan is used to determine the
level of monitoring scans. It can be performed at
any level of interest. You can also increase the mAs
setting to reduce the image noise when necessary.
3. To achieve the shortest possible spiral start delay
(2 s), the position of the monitoring scans relative
to the beginning of spiral scan must be optimized.
A “snapping” function is provided:
Page 57

57
Bolus Tracking
• After the Topogram is performed, the predefined
spiral scanning range and the optimal monitoring
position will be shown.
• If you need to redefine the spiral scanning range,
you should also reposition the monitoring scan in
order to keep the shortest start delay time (2 s).
(The distance between the beginning of the spiral
scanning range and the monitoring scan will be
the same).
• Move the monitoring scan line towards the opti-
mal position and release the mouse button, it will
be snapped automatically. (Trick: if you move the
monitoring scan line away from the optimal position the “snapping” mechanism will be inactive).
4. Place an ROI in the premonitoring scan on the
target area or vessel used for triggering. (The ROI
is defined with double circles – the outer circle is
used for easy positioning, and the inner circle is
used for the actual evaluation). You can also zoom
the reference image for easier positioning of the
ROI.
5. Set the appropriate trigger threshold, and initiate
the contrast injection and monitoring scans at the
same time.
During the monitoring scans, there will be simultaneous display of the relative enhancement of the
target ROI. When the predefined density is reached,
the spiral acquisition will be triggered automatically.
6. You can also initiate the spiral any time during the
monitoring phase manually – either by pressing the
START button or by clicking the START key. If you
do not want to use automatic triggering, you can
deselect it.
Page 58

58
Bolus Tracking
TestBolus
Indications:
This mode can be used to test the start delay of an
optimal enhancement after the contrast medium
injection.
TestBolus
kV 120
Effective mAs 30
Slice collimation 5.0 mm
Slice width 10 mm
Feed/Scan 0 mm
Rotation time 0.5 sec.
Kernel B40f
Cycle time 2 s
Page 59

59
Bolus Tracking
Application Procedures:
1. Select the spiral mode that you want to perform,
and then “Append” the TestBolus mode under Special
protocols.
2. Insert the Test Bolus mode above the spiral mode
for contrast scan by “cut/paste” (with right mouse
button).
3. Perform the Topogram, and define the slice position
for TestBolus.
4. Check the start delay, number of scans and cycle
time before loading the mode.
5. A test bolus with 10-20 ml is then administered
with the same flow rate as during the following spiral
scan. Start the contrast media injection and the
scan at the same time.
6. Load the images into the Dynamic Evaluation
function and determine the time to the peak enhancement.
Alternatively, on the image segment, click “select series”
with the right mouse button and position an ROI on
the first image. This ROI will appear on all images in
the test bolus series. Find the image with the peak HU
value, and calculate the time “delta t” taken to reach
the peak HU value (do not forget to add the preset
start delay time). This time can then be used as the
optimal start delay time for the spiral scan.
Page 60

60
Bolus Tracking
Additional Important
Information
1. The preset start delay time for monitoring scans
depends on whether the subsequent spiral scan will
be acquired during the arterial phase or venous
phase. The default value is 10 s. You can modify it
accordingly.
2. It should be pointed out that when using “Test
Bolus”, there may be residual contrast in the liver
and kidneys prior to scanning. This may result in
an inaccurate arterial and equilibrium phase.
3. The trigger threshold is not an absolute value but
a relative value compared to the non-contrast scan.
E.g. if the CT value is 50 HU in the non-contrast
image, and your trigger level is 100 MU, then the
absolute CT value in the contrast image will be
150 HU.
4. If you change slice collimation, rotation time or kV
in the spiral scanning protocol after CARE Bolus
is inserted, a longer spiral start delay time will be
the result, e.g. 14 s. This is due to the necessary
mechanical adjustments, e.g. moving the slice
collimators. Therefore, it is recommended that you
modify the parameters of the spiral scanning
before inserting the CARE Bolus.
Page 61

61
Bolus Tracking
5. If API is used in conjunction with CARE Bolus, the
actual start delay time for the spiral will be as long
as the length of API including the predefined start
delay time. E. g. if the predefined the start delay is
2 s, and the API lasts 5 s, the spiral will start 5 s after
the threshold is reached.
6. In case you have to interrupt the monitoring
scanning due to injection problem, you can repeat it
afterwards by inserting CARE Bolus again with a
right mouse click. The same Topogram can still be
used.
Page 62

62
WholeBodyAngio
This scan protocol can be used for a whole Body Angio.
A range of 100 cm can be covered in 21.4 s.
WholeBodyAngio 2ndReconstr.
kV 120
Effective mAs 130
Slice collimation 1.5 mm
Slice width 6 mm 2 mm
Feed/Rotation 24.0 mm
Rotation time 0.5 sec.
Kernel B30f B20f
Increment 6 mm 1.5 mm
Image order cr-ca
The reconstruction can be loaded in the 3D Card,
MPR. Select the Range function and a predefined range,
linked to the series, will pop up.
Please notice, if you are not satisfied with the Range
preset adapt the parameters to your needs and link them
to the series.
MPRthick: WholeBodyAngio coronal
Image thickness 3
Distance between images 3
Number of images 60
Page 63

63
WholeBodyAngio
Page 64

64
LungCare
LungCare
kV 120
Effective mAs 20
Slice collimation 0.75 mm
Slice width 1.0 mm
Feed/Rotation 18.0 mm
Rotation time 0.5 sec.
Kernel B50f
Increment 0.5 mm
Image order cr-ca
CTDI
w
1.7 mGy
Effective dose Male: 0.6 mSv
Female: 0.7 mSv
A dedicated low dose Spiral mode for the syngoLung
CARE evaluation.
Indications:
Lung studies with low dose setting, e. g. early visualization of pulmonary nodules.
A typical thorax study in a range of 30 cm will be
covered in 8.9 s.
We recommend using a tube voltage of at least
120 kV.
For further information on the syngo Lung CARE
Application, please refer to the Application Guide
“Clinical Options”.
Page 65

65
LungCare
Page 66

66
CT Colonography
For Colonography studies.
A typically range of 40 cm can be covered in 13.9 s.
CT Colonography 2ndReconstr.
kV 120
Effective mAs 100
Slice collimation 0.75 mm
Slice width 5.0 mm 1.0 mm
Feed/Rotation 15.0 mm
Rotation time 0.5 sec.
Kernel B30f B30f
Increment 5.0 mm 0.7 mm
Image order cr-ca
CTDI
w
7.8 mGy
Effective dose Male: 4.5 mSv
Female: 6.9 mSv
Page 67

67
CT Colonography
We recommend using a tube voltage of at least 120 kV.
A comprehensive study consists of four sections:
Preparation, examination in supine & prone positioning
and post processing.
• Patient preparation
In the case of CT Colonography, adequate preparation in bowel cleansing must be done prior to the
CT examination.
Important for good results in a CT Colonography
examination is the optimal preparation of the
patient.
The patient has to start with a diet and bowel
cleaning two days prior to the examination like for
a conventional Colonoscopy.
• Patient examination
The bowels can be delineated with air. Or, if desired,
with carbon dioxide, water or iodine/barium suspension.
Have patient inflate colon with air to maximum
tolerance.
To decrease colon spasm, e. g. Buscopan
™
or
Glucagon
™
can be given IV.
Usually a prone and supine examination are done
to differentiate between polyps and fecal matter
within the colon.
• Postprocessing
For further information on the syngo Fly Through
Application, please refer to the Application Guide
“Clinical Options”.
Page 68

68
Children
Overview
This folder contains 8 organ specific pediatric protocols with 2 to 5 age or weight dependant subgroups.
For your convenience, the protocols are numbered
according to the body regions, i.e. from head to
abdomen.
The scan protocols for Head and Neck regions are
defined according to age, and the scan protocols for
the other body regions are defined according to body
weight.
As a default, the effective mAs is set to the lowest
category, e. g. less than 6 months in head modes, and
the suggested effective mAs values for the other categories are written in additional lines in the chronicle.
For a few protocols, 80 kV is used instead of 120 kV,
either to exploit the significantly higher image contrast
of iodine contrast media at 80 kV or to reach a lower
dose level than possible with 120 kV.
• HeadSpi0.5s
For routine head spiral studies
• HeadSeq0.5s
For routine head sequential studies
• Head Angio
For head CT Angio studies
• CarotidCTA
For carotid CT Angio studies
• NeonateBody
Spiral mode for neonate studies
• ChestRoutine
For routine chest spiral studies
• AbdPelRoutine
For routine abdominal studies
• AbdCTA
For abdominal CT Angio studies
Page 69

69
Children
Hints in General
1. Topograms: 256 mm lateral topograms are defined
for the head modes, and 512 mm AP topograms are
defined for the body modes. Please keep in mind that
the children’s size can be dramatically different. You
should press the “Hold Measurement“ button whenever the range shown on the real time growing topogram is long enough, in order to avoid unnecessary
radiation.
In a consistent effort to reduce the total dose of an
examination, all topograms of the pediatric protocols
are defined at 80 kV with minimum current (50 mA).
2. Gantry tilt is available for sequence scanning, not
for spiral scanning.
3. For all head studies, it is very important for image
quality to position the patient in the center of the scan
field. Use the lateral laser beam to make sure that the
patient is positioned in the center.
4. Warm surroundings and dimmed lighting are helpful
to make children more cooperative.
5. Sedation: Although the advent of the Multislice
scanner has enabled the user to scan through an area
of interest much faster than ever, sometimes, patient
motion can still lead to severe motion artifacts seen on
the resultant images. This becomes a factor especially
with infants and younger children who are unable to
hold still for the exam. Sedating this population may
be a viable option for your institution. Of course, appropriate protocols need to be established at your specific
institution. For instance, the drug of choice for specific
ages/weights of these patients (taking into consideration the total time of the exam), the form of administration, patient preps, adequate monitoring of the
patient (pre-scan, during the exam and post-scan) etc.
should all be taken into consideration.
Page 70

70
The proper personnel and equipment must also
be readily available at your disposal in the event of
a problem.
6. Oral and rectal contrast administration: Depending
on the reason for the exam/status of the patient, oral
contrast may or may not be given to these patients.
In general, oral contrast is recommended to opacify
the intestinal tract, as unopacified bowel can have
the appearance of abdominal fluid or mass effect. Oral,
as well as rectal contrast may be required. Usually, a
diluted mixture of iodine and water is used as an oral
agent. Different substances can be added to this mixture to help reduce the bitter taste and make it more
pleasing to the child (apple juice, fruit drink mixes are
just a few of these). Barium may of course be used
in some cases as well. Negative contrast agents such
as water are becoming more popular for delineation
of stomach or bowel wall borders, or when 3D reconstructions are needed. The user needs to be aware of
all the contraindications of any of the contrast agents
they are using. It is recommended to refer to the specific vendors recommendations regarding this.
7. I.V. contrast administration: In general, 1-2 ml per
kg of body weight should be applied, however, since
the scanning can be completed in just a few seconds,
please keep in mind that the total injection time should
not be longer than the sum of start delay time and the
scan time – do not inject contrast after the scanning is
finished.
It is recommended to use CARE Bolus in order to
achieve optimal contrast enhancement.
Both start delay time and injection rate are exam-/
patient-dependent. I.V. injection with a power injector
is recommended for all scans whenever possible.
Some guidelines to follow with respect to flow rate are
noted in the chart below.
Children
Page 71

71
Note: these are injector guidelines based on an
antecubital injection site. These guidelines may need
to be adjusted if the site is more peripheral.
Needle Size (gauge) Flow Rate (ml/sec)
22 1.5
20 2.0 – 3.0
18 3.0 – 5.0
Central lines and ports may need to be hand injected
or power injected at a very low flow rate (1 ml/sec).
PIC lines and 24 gauge (or smaller) lines are usually
hand injected. All of these protocols should be decided
on by your institution’s appropriate personnel.
8. Applications with 80 kV: For CTA protocols, the tube
voltage was set to 80 kV and the mAs values were
raised by a factor of 1.5 over the reduced 120 kV values.
This measure roughly reduces the dose by another
factor of 2. At a lower kV, substances with a high atomic
number (such as iodine) have a significantly higher CT
value (= vascular contrast). Iodine CT values at 80 kV
are about 50% higher than at 120 kV.
80 kV was also used for applications when the lowest
achievable mAs at 120 kV was still higher than necessary for sufficient noise level (for technical reasons,
generators need to operate at a certain minimum
current for stable operation). For applications such
as neonate or airway scanning, the low tube output at
80 kV can be used to further reduce the dose to the
patient.
9. Please observe the recommended mAs settings in
the chronicle.
Note, that these recommendations are valid for the
default tube voltage of the specific protocol.
If the voltage is lowered from 120 kV to 80 kV sub-
stantially higher mAs values have to be used (at least
by a factor of 2).
Children
Page 72

72
HeadSpi0.5s
Indications:
Spiral mode for routine head studies, e. g. tumors,
hydrocephalus, hemorrhaging, abnormalities, etc.
HeadSpi0.5s
kV 120
Effective mAs *
Slice collimation 1.5 mm
Slice width 4.0 mm
Feed/Rotation 12.2 mm
Rotation time 0.5 sec.
Kernel C30f
Increment 4.0 mm
Image order ca-cr
Contrast medium IV injection
Start delay exam dependent
Flow rate dependent upon needle size/Access site
Total amount 1– 2 ml per kg of body weight
* The mAs should be adjusted to the age of the child.
* The conversion factor for an 8-week-old, and a scan
range of 90 mm was used.
** The conversion factor for a 7-year-old, 260 mAs and
a scan range of 110 mm was used.
Body Weight kV mAs CTDI
w
Effective dose
(mGy) (mSv)
< 6 months 120 90 17.1 Male: 1.7*
Female: 1.7*
6 months – 120 150 28.5
3 years
3 years – 120 220 41.8 Male: 4.4**
6 years Female: 4.3**
Children
Page 73

73
Tips
• Children, who are more than 6 years old, should
be scanned with an adult protocol as the skull by this
time is fully grown.
• When bone structure is of interest, use kernel C60s
for image reconstruction.
• Posterior Fossa Optimization Filter
PFO: To reduce beam-hardening artifacts in head
images, particularly in the base of the skull, use the
Posterior Fossa Optimization (PFO) filter.
Children
Page 74

74
HeadSeq0.5s
Indications:
Sequential mode for routine head studies for
children, e.g. tumors, hydrocephalus, hemorrhaging,
abnormalities, etc.
HeadSeq0.5s
kV 120
Effective mAs *
Slice collimation 1.5 mm
Slice width 4.5 mm
Feed/Scan 18.0 mm
Rotation time 0.5 sec.
Kernel C30f
Image order ca-cr
Contrast medium IV injection
Start delay exam dependent
Flow rate dependent upon needle size/Access site
Total amount 1– 2 ml per kg of body weight
* The mAs should be adjusted to the age of the child.
* The conversion factor for an 8-week-old, and a scan
range of 90 mm was used.
** The conversion factor for a 7-year-old, 260 mAs and
a scan range of 117.5 mm was used.
Age kV mAs CTDI
w
Effective dose
(mGy) (mSv)
< 6 months 120 90 20.8 Male: 2.1*
Female: 2.1*
6 months – 120 150 34.8
3 years
3 years – 120 220 51.0 Male: 4.1**
6 years Female: 3.9**
Children
Page 75

75
Tips
• Children, who are more than 6 years old, should
be scanned with an adult protocol as the skull by this
time is fully grown.
• When bone structure is of interest, use kernel C60s
for image reconstruction.
• Posterior Fossa Optimization Filter
PFO: To reduce beam-hardening artifacts in head
images, particularly in the base of the skull, use the
Posterior Fossa Optimization (PFO) filter.
Children
Page 76

76
HeadAngio
Indications:
Spiral mode for head CT angiography, e.g. cerebral
vascular abnormalities, tumors etc.
HeadAngio 2ndReconstr.
kV 80
Effective mAs *
Slice collimation 0.75 mm
Slice width 2.0 mm 1.0 mm
Feed/Rotation 6.8 mm
Rotation time 0.5 sec.
Kernel H20f H10f
Increment 2.0 mm 0.7 mm
Image order ca-cr
* The mAs should be adjusted to the age of the child.
* The conversion factor for an 8-week-old, and a scan
range of 40 mm was used.
** The conversion factor for a 7-year-old and a scan
range of 60 mm was used.
Age kV mAs CTDI
w
Effective dose
(mGy) (mSv)
< 6 years 80 100 8.4 Male: 0.4*
Female: 0.4*
6 years – 80 150 12.6 Male: 0.3**
12 years Female: 0.4**
Children
Page 77

77
Tips
• Children, who are more than 12 years old should be
scanned with an adult protocol.
• The first recon job is defined for soft tissue visualization.
Contrast medium IV injection
Start delay 18 –20 sec.
Flow rate dependent upon needle size/Access site
Total amount 1– 2 ml per kg of body weight
MIPthin: HeadAngio coronal
Image thickness 3
Distance between images 3
Number of images 35
For the 2ndreconstruction the Autoload into MIPthin
Range on the 3D Card is activated. The images will be
automatically loaded into 3D, MIPthin, and a coronal
MIPthin Range will pop up.
Please notice, if you are not satisfied with the Range
preset adapt the parameters to your needs and link them
to the series.
Children
Page 78

78
Children
CarotidCTA
Indications:
CT angiography of the carotid arteries, e. g. carotid
stenosis or occlusion, vascular abnormalities of the
carotids or vertebral arteries, etc.
CarotidCTA 2ndReconstr.
kV 80
Effective mAs *
Slice collimation 0.75 mm
Slice width 5.0 mm 1.0 mm
Feed/Rotation 12 mm
Rotation time 0.5 sec.
Kernel B30f B20f
Increment 5.0 mm 0.7 mm
Image order cr-ca
* The mAs should be adjusted to the age of the child.
* The conversion factor for an 8-week-old, and a scan
range of 80 mm was used.
** The conversion factor for a 7-year-old and a scan
range of 120 mm was used.
Age kV mAs CTDI
w
Effective dose
(mGy) (mSv)
< 6 years 80 100 2.6 Male: 0.6*
Female: 0.7*
6 years – 80 150 3.9 Male: 0.4**
12 years Female: 0.4**
Page 79

79
Children
Tips
• Children, who are more than 12 years old should be
scanned with an adult protocol.
• The first recon job is defined for soft tissue visualization.
Contrast medium IV injection
Start delay exam dependent
Flow rate dependent upon needle size/Access site
Total amount 1– 2 ml per kg of body weight
MIPthin: CarotidCTA coronal
Image thickness 3
Distance between images 3
Number of images 20
For the 2ndreconstruction the Autoload into MIPthin
Range on the 3D Card is activated. The images will be
automatically loaded into 3D, MIPthin, and a coronal
MIPthin Range will pop up.
Please notice, if you are not satisfied with the Range
preset adapt the parameters to your needs and link them
to the series.
Page 80

80
Children
NeonateBody
Indications:
Spiral mode for routine neonate body studies, e. g.
tumors, abnormalities, malformations, abscesses, etc.
NeonateBody
kV 80
Effective mAs 25
Slice collimation 1.5 mm
Slice width 6.0 mm
Feed/Rotation 24 mm
Rotation time 0.5 sec.
Kernel B30f
Increment 6.0 mm
Image order cr-ca
CTDI
w
0.55 mGy
Effective mAs* Male: 0.5 mSv
Female: 0.7 mSv
* The conversion factor for an 8-week-old, and a scan
range of 150 mm was used.
Page 81

81
Children
Tips
• You can modify the slice width for image reconstruction according to the clinical indications.
Contrast medium IV injection
Start delay exam dependent
Flow rate dependent upon needle size/Access site
Total amount 1– 2 ml per kg of body weight
Page 82

82
Children
ChestRoutine
Indications:
Spiral mode for routine thorax studies, e. g.
pneumonia, tumors, metastases, lymphoma, vascular
abnormalities etc.
ChestRoutine 2ndReconstr.
kV 120
Effective mAs *
Slice collimation 1.5 mm
Slice width 6.0 mm 6.0 mm
Feed/Rotation 24.0 mm
Rotation time 0.5 sec.
Kernel B30f B60f
Increment 6.0 mm 6.0 mm
Image order cr-ca
* The mAs should be adjusted to the body weight
of the child.
Page 83

83
Children
Tips
• Children with a body weight of more than 54 kg
should be examined with an adult protocol.
• The first and second recon jobs are defined for
visualization of the mediastinum and the lungs,
respectively.
Contrast medium IV injection
Start delay exam dependent
Flow rate dependent upon needle size/Access site
Total amount 1– 2 ml per kg of body weight
* The conversion factor for an 8-week-old, and a scan
range of 100 mm was used.
** The conversion factor for a 7-year-old and a scan
range of 150 mm was used.
Body weight kV mAs CTDI
w
Effective dose
(mGy) (mSv)
< 15 kg 120 17 1.2 Male: 0.6*
Female: 0.8*
15 – 24 kg 120 20 1.4
25 – 34 kg 120 30 2.1 Male: 0.9**
Female: 1.1**
35 – 44 kg 120 50 3.5
45 – 54 kg 120 70 4.9
Page 84

84
AbdPelRoutine
Indications:
Spiral mode for routine studies in the region
of abdomen and pelvis, e. g. tumors, lymphoma,
abscesses, post-traumatic changes, etc.
AbdPelRoutine 2ndReconstr.
kV 120
Effective mAs *
Slice collimation 1.5 mm
Slice width 5.0 mm 5.0 mm
Feed/Rotation 24.0 mm
Rotation time 0.5 sec.
Kernel B30f B60f
Increment 5.0 mm 5.0 mm
Image order cr-ca
* The mAs should be adjusted to the body weight
of the child.
* The conversion factor for an 8-week-old, and a scan
range of 100 mm was used.
** The conversion factor for a 7-year-old and a scan
range of 150 mm was used.
Body weight kV mAs CTDI
w
Effective dose
(mGy) (mSv)
< 15 kg 120 20 1.4 Male: 0.9*
Female: 1.2*
15 – 24 kg 120 35 2.5
25 – 34 kg 120 55 3.8 Male: 2.3**
Female: 3.1**
35 – 44 kg 120 85 6.0
45 – 54 kg 120 120 8.4
Children
Page 85

85
Contrast medium IV injection
Start delay exam dependent
Flow rate dependent upon needle size/Access site
Total amount 1 – 2 ml per kg of body weight
Tips
• Children with a body weight of more than 54 kg
should be examined with an adult protocol.
• There are two recon jobs predefined. The second
one is for the reconstruction of the lungs in the upper
range.
Children
Page 86

86
Children
AbdCTA
Indications:
For abdominal CT Angio studies, e. g. vascular
abnormalities, aneurysms, etc.
AbdCTA 2ndReconstr.
kV 80
Effective mAs *
Slice collimation 0.75 mm
Slice width 3.0 mm 1.0 mm
Feed/Rotation 12 mm
Rotation time 0.5 sec.
Kernel B30f B20f
Increment 3.0 mm 0.7 mm
Image order cr-ca
* The mAs should be adjusted to the body weight
of the child.
* The conversion factor for an 8-week-old, and a scan
range of 100 mm was used.
** The conversion factor for a 7-year-old and a scan
range of 200 mm was used.
Body weight kV mAs CTDI
w
Effective dose
(mGy) (mSv)
< 15 kg 80 30 0.8 Male: 0.4*
Female: 0.6*
15 – 24 kg 80 50 1.3
25 – 34 kg 80 75 1.9 Male: 0.9**
Female: 1.4**
35 – 44 kg 80 110 2.9
45 – 54 kg 80 150 3.9
Page 87

87
Children
Contrast medium IV injection
Start delay exam dependent
Flow rate dependent upon needle size/Access site
Total amount 1 – 2 ml per kg of body weight
Tips
• Children with a body weight of more than 54 kg
should be examined with an adult protocol.
• The first recon job is defined for image viewing and
filming.
MIPthin: AbdCTA sagittal
Image thickness 3
Distance between images 3
Number of images 60
For the 2ndreconstruction the Autoload into MIPthin
Range on the 3D Card is activated. The images will be
automatically loaded into 3D, MIPthin, and a sagittal
MIPthin Range will pop up.
Please notice, if you are not satisfied with the Range
preset adapt the parameters to your needs and link them
to the series.
Page 88

88
Head
Overview
• AngioHead
For CT Angio studies using 0.75 mm slice collimation
and a 1.0 mm slice thickness
• AngioThinSlice
For CT Angio studies using 0.75 mm slice collimation
and 0.75 mm slice thickness
• HeadSeq0.5s
Sequence mode for base of the skull and cerebrum
routine studies and a 0.5 s rotation time
• HeadSpi0.5s
Spiral mode for base of skull and cerebrum routine
studies and a 0.5 s rotation time
Page 89

89
Head
Hints in General
1. Topogram: Lateral, 256 mm.
2. Patient positioning:
Patient lying in supine position, arms resting against
body, secure head well in the head holder, support
lower legs.
3. Gantry tilt is available for sequence scanning, not
for spiral scanning.
4. For all head studies, it is very important for image
quality to position the patient in the center of the
scan field. Use the lateral laser beam to make sure
that the patient is positioned in the center.
5. For image reconstruction of bone structure, use
kernel H60.
6. In general, cerebrum studies with contrast medium,
except CTA and nasopharynx, can be performed
by hand injection. Start the scan after the injection
is completed.
Page 90

90
Head
AngioHead
Indications:
Spiral mode for cerebral CT Angios, e. g. cerebral
vascular abnormalities, tumors and follow up studies
etc.
A range of 80 mm will be covered in 3.3 s.
Page 91

91
Head
AngioHead 2ndReconstr.
kV 120
Effective mAs 100
Slice collimation 0.75 mm
Slice width 4.0 mm 1.0 mm
Feed/Rotation 15.0 mm
Rotation time 0.5 sec.
Kernel H20f H10f
Increment 4.0 mm 0.7 mm
Image order ca-cr
CTDI
w
21.1 mGy
Effective dose Male: 0.4 mSv
Female: 0.5 mSv
Use of CARE Bolus with monitoring scans positioned at
the level of the basilar artery or carotid artery. Set the
trigger threshold at 120 HU, or use manual triggering.
MIPthin: AngioHead coronal
Image thickness 3
Distance between images 3
Number of images 35
For the 2ndreconstruction the Autoload into MIPthin
Range on the 3D Card is activated. The images will be
automatically loaded into 3D, MIPthin, and a coronal
MIPthin Range will pop up.
Please notice, if you are not satisfied with the Range
preset adapt the parameters to your needs and link them
to the series.
Contrast medium IV injection
Start delay 18 sec.
Flow rate 3.5 ml/s
Total amount 75 ml
Page 92

92
Head
AngioThinSlice
Indications:
For cerebral CT Angio studies, with one reconstruction
job for a 0.75mm slice thickness.
E.g. cerebral vascular abnormalities, tumor, and follow
up studies etc.
A range of 80 mm will be covered in 6.5 s.
Page 93

93
Head
AngioThinSlice 2ndReconstr.
kV 120
Effective mAs 130
Slice collimation 0.75 mm
Slice width 4.0 mm 0.75 mm
Feed/Rotation 6.8 mm
Rotation time 0.5 sec.
Kernel H20f H10f
Increment 4.0 mm 0.5 mm
Image order ca-cr
CTDI
w
27.4 mGy
Effective dose Male: 0.6 mSv
Female: 0.7 mSv
Use of CARE Bolus with monitoring scans positioned at
the level of the basilar artery or carotid artery. Set the
trigger threshold at 120 HU, or use manual triggering.
MPRthick: AngioThinSlice coronal
Image thickness 3
Distance between images 3
Number of images 35
For the 2ndreconstruction the Autoload into MPRthick
Range on the 3D Card is activated. The images will be
automatically loaded into 3D, MPRthick, and a coronal
MPRthick Range will pop up.
Please notice, if you are not satisfied with the Range
preset adapt the parameters to your needs and link them
to the series.
Contrast medium IV injection
Start delay 18 sec.
Flow rate 3.5 ml/sec.
Total amount 75 ml
Page 94

94
Head
HeadSeq0.5s
Indications:
Sequence mode for routine head studies, e. g.
stroke, brain tumors, cranial trauma, cerebral atrophy,
hydrocephalus, and inflammation, etc.
Two ranges are predefined. One for the base of the
skull and one for the cerebrum.
Page 95

95
Head
ThinSliceSeq RoutineSeq
kV 120 120
Effective mAs 250 250
Slice collimation 0.75 mm 1.5 mm
Slice width 4.5 mm 9.0 mm
Feed/Scan 9.0 mm 18.0 mm
Rotation time 0.5 sec. 0.5 sec.
Kernel H31f H31f
Image order ca-cr ca-cr
CTDI
w
58.2 mGy 60.3 mGy
Effective dose Male: 0.7 mSv Male: 1.6 mSv
Female: 0.8 mSv Female: 1.8 mSv
PosteriorFossaOptimization Filter
PFO: To reduce beam-hardening artifacts in head
images, particularly in the base of the skull, use the
Posterior Fossa Optimization (PFO) filter.
If you want to set up the scan with only one range,
i. e. either 12 x 0.75 mm or 12 x 1.5 mm, you can
easily delete one mode by clicking the chronicle with
the right mouse button, and select cut.
Contrast medium IV injection
Start delay 60 sec.
Flow rate 2 ml/sec.
Total amount 50 – 60 ml
Page 96

96
Head
HeadSpi0.5s
Indications:
Spiral mode for routine head studies, e. g. stroke,
brain tumors, cranial trauma, cerebral atrophy, hydrocephalus, and inflammation, etc.
Two ranges are predefined for the base of the skull
and cerebrum.
Page 97

97
Head
ThinSliceSpi RoutineSpi
kV 120 120
Effective mAs 320 320
Slice collimation 0.75 mm 1.5 mm
Slice width 4.0 mm 8.0 mm
Feed/Rotation 6.8 mm 13.7 mm
Rotation time 0.5 sec. 0.5 sec.
Kernel H31f H31f
Increment 4.0 mm 8.0 mm
Image order ca-cr ca-cr
CTDI
w
50.6 mGy 45.6 mGy
Effective dose Male: 0.7 mSv Male: 1.1 mSv
Female: 0.8 mSv Female: 1.2 mSv
PosteriorFossaOptimization Filter
PFO: To reduce beam-hardening artifacts in head
images, particularly in the base of the skull, use the
Posterior Fossa Optimization (PFO) filter.
If you want to set up the scan with only one range,
i.e. either 16 x 0.75 mm or 16 x 1.5 mm, you can
easily delete one mode by clicking the chronicle with
the right mouse button, and select cut.
Contrast medium IV injection
Start delay 60 sec.
Flow rate 2 ml/sec.
Total amount 50 – 60 ml
Page 98

98
Neck
Overview
• AngioCarotid
For CTA studies
Page 99

99
Neck
Hints in General
1. Topogram: Lateral, 256 mm.
2. Patient positioning:
Patient lying in supine position, hyperextend neck
slightly, secure head well in head cradle.
3. Patient respiratory instruction:
do not breathe, do not swallow.
4. For image reconstruction of bone structure, use
kernel B60.
5. In case of 3D study only, the mAs value can be
reduced by 50%. Use kernel B10 and 50% overlapping for image reconstruction.
6. For examinations in the Neck/Shoulder region at
least 120 kV is recommendable for optimized image
quality. For large patients 140 kV is advisable.
Page 100

100
Neck
AngioCarotid
Indications:
Noninvasive CT angiography of carotid stenosis
or occlusions, plaques course abnormalities of the
carotids and vertebral arteries, etc.
A range of 20 cm including the aortic arch will be
covered in 8.9 s.
 Loading...
Loading...