Erbe Erbosonat Ultrasound User manual

ERBE
erbosonat Ultrasound Therapy Unit
User Manual
Type Nr. 10205-010 / V 1.3
10.98.


erbosonat Ultrasound Therapy Unit
User Manual
Type Nr. 10205-010 / V 1.3
Manual part number 80122-001
All rights reserved. No part of this document may be translated, stored in information retrieval systems, or
transmitted in any form or by any means - electronic or mechanical, including photocopying, recording or
otherwise - without the written permission of ERBE Elektromedizin.
Printed by ERBE Elektromedizin, Tübingen
Printed in Germany
Copyright ERBE Elektromedizin GmbH, Tübingen 1998

Chapter Title Page
1 Important Foreword..........................................................1-1
2 Physical Principles of Ultrasonic Therapy......................2-1
2.1 What is Ultrasound? ............................................................2-2
2.2 Ultrasound Generation.........................................................2-2
2.3 Physical Principles of Therapeutically Relevant Effects
of Ultrasound.......................................................................2-2
2.4 Concerted Utilization of Non-Thermal and/or Thermal
Effects..................................................................................2-4
3 Therapeutic Effects of Ultrasound,
Undesirable Side Effects....................................................3-1
3.1 General.................................................................................3-2
3.2 Non-Thermal Effects...........................................................3-2
3.3 Thermal Effects....................................................................3-2
3.4 Undesirable Side Effects......................................................3-3
4 Ultrasonic Radiation Methods..........................................4-1
4.1 Continuous Ultrasound........................................................4-2
4.2 Pulsed Ultrasound................................................................4-2
5 Treatment Technique........................................................5-1
5.1 Coupling using Ultrasonic Gel, Liquid Paraffin, etc...........5-2
5.2 Subaqueous Coupling..........................................................5-2
6 Dosage, Indications, Additional Treatment
Information ........................................................................6-1
6.1 Indications............................................................................6-2
6.2 Contraindications ................................................................6-2
6.3 Additional Treatment Information.......................................6-3
7 Description and Operation................................................7-1
7.1 General Description ............................................................7-2
7.2 Description of the Control Elements ...................................7-3
7.3 Ultrasound Operation...........................................................7-6
7.4 Operation in Combination with the erbogalvan..................7-6
7.5 Technical Specifications......................................................7-8
8 Installation and Initial Operation ....................................8-1
9 Cleaning and Disinfection.................................................9-1
9.1 Unit......................................................................................9-2
9.2 Ultrasound Applicators........................................................9-2
10 Maintenance, Care, Disposal..........................................10-1
10.1 Maintenance of the unit accessories..................................10-2
10.2 Modifications and repairs..................................................10-2

Care of the Ultrasound Applicators................................................10-2
Disposal of the unit.........................................................................10-2
11 Functional Testing...........................................................11-1
12 Safety Inspections ............................................................12-1
12.1 Equipment..........................................................................12-2
12.2 Ultrasound Applicators......................................................12-2
13 Accessories........................................................................13-1
14 Warranty..........................................................................14-1
15 Literature, Regulations, Standards, Legislation...........15-1
Addresses
Important Foreword
1

1. Important Foreword
The
erbosonat
in order to detect any damage that may have occurred in shipment and to verify the equipment
has been correctly installed, the equipment should be rechecked for proper and safe operation
after installation, prior to initial operation, and before each subsequent use.
The
erbosonat
familiar with the features and operation of the equipment.
In order to prevent accidental injuries due to faults occurring in, or to failures of the equi p-
ment or of any of its accessories, the equipment and all of its accessories should be regularly
checked for proper and safe operation. These checks should be performed exclusively by personnel whose knowledge, training and practical experience qualifies them to perform such
checks.
Please see page 12-2
has been checked for proper and safe operation prior to shipment. However,
ultrasonic therapy unit should be used on patients exclusively by personnel
1 - 2
Physical Principles of Ultrasonic Therapy
2

2. Physical Principles of Ultrasonic Therapy
A prerequisite for the efficient and, for the patient, safe application of ultrasonic therapy is an
understanding of the physical principles of ultrasound as well as the effects which ultrasound
can cause in biological tissues.
2.1 What is Ultrasound?
Ultrasound refers to mechanical oscillations, or vibrations, at frequencies above the audible
range of the human ear, that is, above about 20 kHz. Ultrasonic therapy uses frequencies from
about 800 kHz to about 3000 kHz. The vibration amplitude depends, among other things, on
the power density (watts/cm2) and is about 0.00003 mm. This very small vibration amplitude
hardly gives the impression that it can achieve a therapeutic effect in biological tissue.
At 1000 000 vibrations per second and a vibration amplitude of 0.00003 mm, however, the
constituent particles travel the remarkable distance of 4 x 1000 000 x 0.00003 mm = 12 cm.
Even more remarkable is the fact that the generation of these vibrations requires an acceleration of approx. 1000 000 m/s2. This acceleration is 100 000 times greater than the acceleration
due to the earth’s gravity.
2.2 Ultrasound Generation
Ultrasound generation today utilizes mainly the piezoelectric effect of piezoceramics.
Piezoceramics are special electrically polarized ceramics. Their density, or volume, can be
influenced by an electric field. The change in volume of the ceramic is directly proportional to
the electrical charge introduced into it.
If a time-varying electrical voltage is applied to a piezoceramic, the volume of the ceramic
changes proportionally to the electrical voltage. The change in volume results in a change in
length. This occurs in a preferred direction prescribed by the shape and polarization direction
of the piezoceramic.
Such a component can be called an electromechanical transducer. An ultrasonic therapy
device consists basically of an electromechanical transducer and a high-frequency generator.
2.3 Physical Principles of Therapeutically Relevant Effects of
Ultrasound
Ultrasound can cause non-thermal as well as thermal effects.
2.3.1 Non-Thermal Effects
Non-thermal effects of ultrasound in biological tissue result from the high accelerative forces.
Even at a power density of 1 W/cm2, these are about 100 000 times the acceleration due to the
earth’s gravity.
Unfortunately, little has been learned up to now about the relationships between physical,
physiological, and/or biochemical effects. The corresponding statements are mainly empirical
and hypothetical.
Probably the most well-known effect of ultrasound is the cavitation of water-containing
tissue. Cavitation is characterized by the formation of microscopic bubbles in intra- and
extracellular fluids when a critical acceleration is exceeded. These bubbles can cause tissue
fractionation. The cavitation effect is used in ultrasonic surgery for tissue dissection and must
2 - 2
be avoided in ultrasonic therapy at all costs. Producing the cavitation effect requires very high
power densities. These cannot be achieved when the erbosonat is properly used.
2.3.2 Thermal Effects
The ultrasonic energy radiated into tissue is absorbed by the tissue and transformed endogenously into heat. The heat produces thermal effects such as hyperemia, which in turn
influences the metabolic processes in the ultrasonically irradiated tissue.
The thermal effects of ultrasound are similar to the thermal effects of shortwave, decimetricwave, or microwave therapy. The differentiation from these HF therapies lies solely in the application technique.
Ultrasonic therapy is characterized by the fact that a more directed application is possible
than with the HF-therapeutic procedures. This is especially true in the treatment of diseased
joints. Moreover, ultrasound has a further advantage in the treatment of joints: due to the
reflection of the ultrasound by hard tissue (cartilage, bones), there is increased warming in the
interface between the hard and soft tissue.
NOTE!
Excessive local application of ultrasonic energy can cause thermal tissue damage. For this reason, at high ultrasonic power levels, an ultrasound applicator must not be applied too long to
one location.
2 - 3
2.4 Concerted Utilization of Non-Thermal and/or Thermal Effects
In general, ultrasound simultaneously produces non-thermal as well as thermal effects. The
non-thermal effects depend chiefly on the level of acceleration, or the power density.
The endogenous heat generation is proportional to the ultrasonic energy radiated into the tissue. The ultrasonic energy radiated into tissue is proportional to the effective ultrasonic power
and the duration.
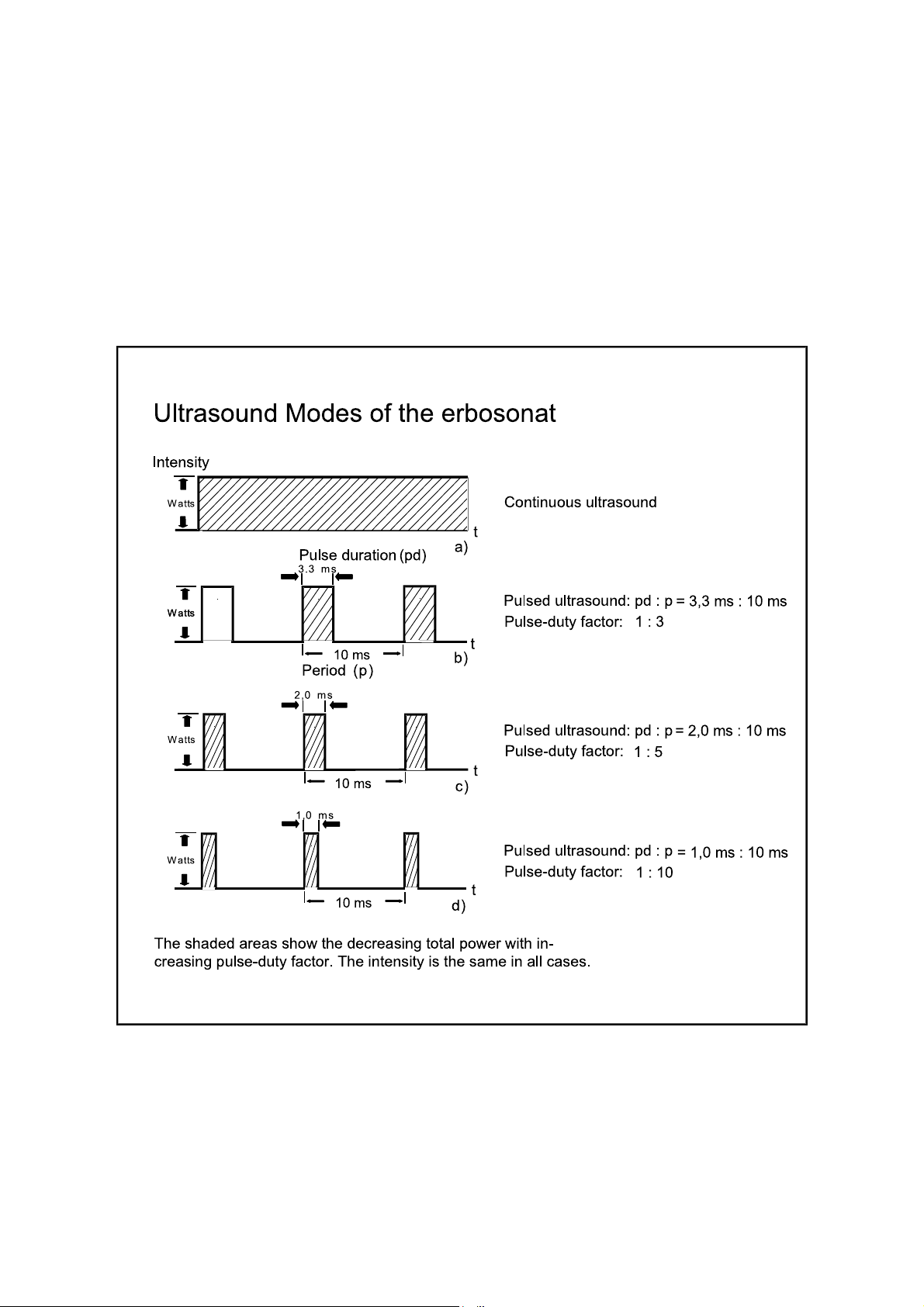
By modulating the amplitude of the ultrasound, the non-thermal effects can be emphasized
and at the same time the thermal effects reduced. Pulse modulation is advantageous in this
case.
2 - 4
3
Therapeutic Effects of Ultrasound, Undesirable
Side Effects

3. Therapeutic Effects of Ultrasound, Undesirable Side
Effects
3.1 General
Whether ultrasound generates therapeutic and/or undesirable side effects depends mainly on
the dosage and the application technique. According to the current state of knowledge, it can
be assumed that tissue damage cannot occur when ultrasound is properly used.
Since ultrasound applied in therapeutic doses shows no persistent effects, endangerment of the
patient as a result of cumulative effects can be ruled out, even in t he case of repeated applications. With respect to therapeutic effects, the distinction is made between primary and secondary effects.
Primary effects are the accelerative forces generated by ultrasound and the transformation of
ultrasonic energy into heat. The primary effects in turn cause secondary effects: these can be
categorized as non-thermal and thermal effects.
3.2 Non-Thermal Effects
Unfortunately, no scientific information concerning non-thermal effects is available, rather
only hypotheses. Our knowledge is based on comprehensive empirical experience. The
following are hypothetical causes for non-thermal effects of ultrasound:
l Piezoelectric effects, especially in bone. The pressure waves deform fibrils and fibers and
induce electrical potentials.
Result: Increased cell activity. Influence on membrane permeability, including that for
ions.
l Deformation of fibrils and fibers with induction of electrical potentials.
Result: Increased activity of fibroblasts and osteoblasts.
The non-thermal effects are proportional to the intensity of the ultrasound or the accelerative
forces caused by the ultrasound.
3.3 Thermal Effects
In principle, the thermal effects of ultrasound do not differ from the thermal effects of highfrequency diathermy. The two procedures differ only in the application technique and the
selectivity of the heat generation.
In high-frequency diathermy, endogenous heat generation depends in particular on the electri-
cal properties of the various tissues. With ultrasonic diathermy, on the other hand, endogenous heat generation depends in particular on the mechanical properties of the various tis-
sues.
Ultrasonic diathermy is preferable to high-frequency diathermy when directed to certain regions such as joints. In both diathermy procedures, the heat or temperature serves as a
stimulus for triggering secondary effects such as hyperemia and analgesia.
The thermal effects are proportional to the ultrasonic energy introduced into the tissue.
3 - 2

3.4 Undesirable Side Effects
3.4.1 Cavitation
Cavities containing gas or vapor can form during the negative-pressure phase of the ultrasonic
wave. The microscopic bubbles can implode and trigger intensive mechanical effects and temperature jumps. Cavitation is not possible when the currently-employed low-dosage recommendations are followed, when dynamic ultrasonic radiation (moving ultrasound applicator)
is used, and when the equipment is functioning properly.
3.4.2 Pain Sensations
Intensive heat generation at the muscle-bone interface is desirable for many therapeutic applications, but it can lead to pain sensations at the sensitive periosteum. Remedy: Use low dosage; do not use the applicator too long in one location; and question the patient concerning
pain.
3.4.3 Impaired Thermal Sensitivity Due to Medication
Ensure that the patient has not taken medication affecting thermal sensitivity.
3 - 3

3 - 4
Ultrasonic Radiation Methods
4
 Loading...
Loading...