Page 1

M1026A Anesthetic Gas Module
Service Guide
Anesthetic Gas Module
M1026A
Patient Monitoring
Page 2

Part Number M1026-9101A
*M1026-9101A*
S PHI
Page 3

1Table of Contents
Introduction 5
Description 5
Product Structure 5
Physical Specifications 5
Environmental Specifications 6
Performance Specifications 6
CO2 Measurement 7
AWRR derived from CO2 Waveform 7
N2O Measurement 7
O2 Measurement 7
Anesthetic Agent Measurement 7
Alarm Ranges 8
Alarm Delay 8
Apnea Alarm 8
INOP Alarms 8
General Measurement Principles 9
Theory of Operation 9
Main PC Board 10
Power Supply 11
Pneumatic System 11
Pump 12
Water t r ap 12
Sample Flow Through the Pneumatic Path 13
Agent Identification Assembly 13
Measurement Principle 14
O2 Sensor 14
Specifications 14
Measurement Principle 14
Infrared Measurement Assembly 15
Installation and Patient Safety 16
Physical Installation 16
Environment 17
Label Sheet 17
Making Connections to the AGM 17
Sample Gas Connections to the Gas Exhaust 18
Returning the Gas Sample 18
Setting Up the Gas Return 19
Removing the Gas Sample 20
Setup and Configuration Procedures 20
Altitude Configuration 20
3
Page 4

Connect Sample Input Tubing 20
Preventive Maintenance (PM) Tasks 20
Post-Installation Checks 21
Safety Requirements Compliance and Considerations 21
Explanation of Symbols Used 21
Power Supply Requirements 22
Grounding the System 22
Equipotential Grounding 23
Combining Equipment 23
Checking and Calibrating the Anesthetic Gas Module 23
Access Service Functions of the M1026A Anesthetic Gas Module 23
When and how to check the Philips M1026A Anesthetic Gas Module 25
Equipment required for checking 25
Checks and adjustments 26
Performance Leakage Check 26
Performance Diagnostic Check 27
Performance Flowrate Check 27
Total Flowrate Check and Adjustment in Purge Mode 27
Measurement Path Flowrate Check and Adjustment 28
Total Flowrate Check in Normal Mode 30
Zero Calibration 30
Barometric Pressure Check and Calibration 31
Span Calibration Check 32
Disposal of Empty Calibration Gas Cylinder 34
Maintaining the Anesthetic Gas Module 35
Preventive Maintenance (PM) Tasks 35
Cleaning 36
Replace PM Parts 36
Internal Nafion Tubing with Bacterial Filters and manifold Seals 36
Room-Air Filter 38
Pump Filter 39
Performance Checks 40
Other factors to maximize uptime or reduce cost of ownership: 40
Troubleshooting the Anesthetic Gas Module 40
Compatibility Criteria for the AGM and the IntelliVue Monitors 40
Flow Charts for Communication and Measurement Type Problems 40
Hardware Related Troubleshooting Strategy 45
INOPs 46
Calibration Checks 48
Calibration Checks Troubleshooting Table 49
Diagnostic Checks 50
Problem Solving Hierarchy 51
Pneumatic System Diagnostic Checks 52
O2 Assembly Diagnostic Checks 52
Optical Path Disgnostic Checks 55
4
Page 5

IR Measurement Assembly Diagnostic Checks 56
Agent ID Assmebly Diagnostic Checks 57
Power Supply Diagnostic Checks 58
Operating Temperature Diagnostic Checks 59
Test Points, Connectors and Jumpers 59
Tes t P o i n t s 5 9
Connectors 60
Jumpers 60
Repairing the Anesthetic Gas Module 62
Introduction 62
The Top Cover 64
Removal 64
Replacement 64
Lifting the IR Measurement Mounting Bracket 66
Removal 67
Replacement 67
Infrared Measurement Assembly Head 69
Transferring NVRAM Data to a Replacement Head 69
Sample Cell 73
Removal 73
Replacement 73
Solenoid Valve #1 77
Removal 77
Replacement 77
Power Supply Unit 79
Removal 79
Replacement 79
Main PC Board 80
Removal 80
Replacement 81
O2 Sensor 82
Removal 82
Replacement 83
Agent Identification Head 85
Removal 85
Replacement 86
Pump 87
Removal 87
Replacement 87
Fan 88
Removal 88
Replacement 88
Solenoid Valve #2 90
Removal 90
Replacement 90
5
Page 6

To p C o v e r P C B o a r d 91
Removal 91
Replacement 91
Watertrap Manifold and Protector 93
Removal 93
Replacement 93
Power Fuses 94
Removal 94
Replacement 94
Test and Inspection Matrix 94
When to Perform Test Blocks 98
Safety Test Appendix 99
Parts List 101
Calibration Equipment 106
6
Page 7
Introduction
This chapter contains the following information on the M1026A Anesthesia Gas Module:
• A description of the Module, including its physical, environmental and performance specifications
• A general explanation of the measurement principles that the Module uses to measure gas
concentrations
• The theory of operation of the Module: the layout of its components and how they work.
Description
The Philips M1026A Anesthetic Gas Module works together with the IntelliVue MP90 patient
monitors through an RS232 serial interface. It measures the airway gases of ventilated patients who are
under general gas anesthesia, or emerging from it.
1
1Anesthetic Gas Module
The module produces graphical wave data, and inspired and end-tidal numeric data for the following
gases:
•CO
•N
• One volatile anesthetic agent
•O
It also generates numerics for the patient’s airway respiration rate (AWRR).
The Agent Identification feature identifies which anesthetic agent is being used.
2
O
2
(optional)
2
Product Structure
The only version of the M1026A Anesthetic Gas Module compatible with the IntelliVue Monitoring
System is:
M1026A #A05: M1026A Watertrap with 5-Agent-ID (Hal, Iso, Enf, Des, Sev)
• #C03 (MUST-Option): adds fast O
Physical Specifications
Size (H x W x D)
90mm x 370mm x 467mm (3.54 x 14.6 x 18.4 in).
measurement
2
5
Page 8

1 Anesthetic Gas Module Introduction
Weight
8.2 kg (18 lb).
Environmental Specifications
Operating Temperature
15 to 40°C (59 to 104°F).
Storage Temperature
-40 to 65°C (-40 to 149°F).
Humidity Limit (Operating)
up to 95% RH max @ 40 °C (104 °F).
non-condensing
Humidity Limit (Storage)
up to 95% RH max @ 65 °C (149 °F).
non-condensing
Altitude Range (Operating)
-305 to 3048m (-1,000 to 10,000 ft).
Altitude Range (Storage)
-305 to 5,486m (-1,000 to 18,000 ft).
Warm-up Time
After switching on: 2 minutes to measure, 8 minutes for full specification accuracy.
Performance Specifications
All Performance and accuracy specifications are valid based on gas sample tubing M1658A, including
watertrap M1657B, and airway adapter 13902A.
Humidity Correction: For CO
Wet: p [mmHg] = c [Vol%] * (p_abs - p_H
Dry: p [mmHg] = c [Vol%] * p_abs /100
Where p = partial pressure, c = gas concentration, p_abs = pressure in breathing circuit, p_H
mmHg, partial pressure of water vapor of exhaled gas (37
For all other gases the readings are always given as dry values.
Sample Flow Rate: 150 ml/min.
Sample Delay Time: All measurements and alarms are subject to a delay of 3 seconds.
Total System Response Time = the sum of the delay time and the rise time.
the humidity correction can be set to “wet” or “dry”.
2
O)/100
2
o
C, 100% rh).
O = 47
2
6
Page 9
Introduction 1 Anesthetic Gas Module
CO2 Measurement
Range: 0 to 76 mmHg
Accuracy: 1.5 mmHg (0 - 40 mmHg)
2.5 mmHg (40 - 60 mmHg)
4.0 mmHg (60 - 76 mmHg)
Resolution: 1 mmHg
Rise-time: 410 msec typical
The total system response time is the sum of the sample delay time (3 seconds) and the rise time (410
msec typical)
AWRR derived from CO2 Waveform
Range: 0 to 60 rpm
Accuracy: ± 2 rpm
Resolution: 1 rpm
Detection Criteria: 6 mmHg variation in CO
N2O Measurement
Range: 0 to 85 vol%
Accuracy: 1.5 vol% + 5% relative
Resolution: 1 vol%
Rise-time: 510 msec typical
Measurement
O
2
Range: 0 to 100vol%
Accuracy: ± 2.5 vol% or 5% relative, whichever is the greater.
Resolution: 1 vol%
Rise-time: 450 msec typical
2
Anesthetic Agent Measurement
Agent Range (vol%) Accuracy Resolution Rise Time
Halothane 0 - 7.5 0.2 vol% + 4.0% relative 0.05 < 740
Enflurane 0 - 7.5 0.1 vol% + 4.0% relative 0.05 < 620
7
Page 10
1 Anesthetic Gas Module Introduction
Agent Range (vol%) Accuracy Resolution Rise Time
Isoflurane 0 - 7.5 0.1 vol% + 4.0% relative 0.05 < 610
Sevoflurane 0 - 9.0 0.1 vol% + 4.0% relative 0.05 < 570
Desflurane 0 - 20.0 0 . 1 v o l % + 6 . 0 % r e l a t i v e 0 . 0 5 ( 0 - 1 0 )
0.1 (10.1-20)
< 540
Alarm Ranges
Agent High Range Low Range
AWRR 10 - 60 rpm 0 - 59 rpm
ETCO
2
IMCO
2
inN2O 0 - 82 vol% none
inO
2
et SEV 0.1 - 9.0 vol% 0.0 - 8.9 vol%
in SEV 0.1 - 9.0 vol% 0.0 - 8.9 vol%
et DES 0.2 - 20.0 vol% 0.0 - 19.8 vol%
in DES 0.2 - 20.0 vol% 0.0 - 19.8 vol%
Halothane, Enflurane, Isoflurane
et 0.1 - 7.5 vol% 0.0 - 7.4 vol%
in 0.1 - 7.5 vol% 0.0 - 7.4 vol%
20 - 76 mmHg 10 - 75 mmHg
2 - 20 mmHg none
19-100 vol% 18 - 99 vol%
Alarm Delay
10 seconds if no automatic zero calibration occurs within that time.
Apnea Alarm
INOP Alarms
INOP alarms are triggered if:
• The Philips M1026A Anesthetic Gas Module is disconnected or switched off.
• The equipment malfunctions.
• The Agent-ID malfunctions.
• Zero calibration has failed.
8
Delay Range: 10 - 40 seconds
Criterion No detected breath within the adjusted delay time
Alarm: Within 2 seconds after this criterion is met, if no automatic zero
occurs
Page 11

Introduction 1 Anesthetic Gas Module
• Zero calibration is in progress.
• The gas sample tube is occluded, or the water trap is full.
• The Philips M1026A Anesthetic Gas Module is unable to measure.
• Gas contaminant is detected.
• Agent mixture detected.
• Anesthetic agent detected but not selected.
• The module is in warm-up mode.
• No breath detected.
• The Anesthetic Gas Module is incompatible with the monitor
General Measurement Principles
The Philips M1026A Anesthetic Gas Module uses a technique called Non-Dispersive Infrared Gas
Concentration Measurement (NDIR) to measure the concentration of gases.
This works as follows:
• The gases that the Philips M1026A Anesthetic Gas Module can measure absorb infrared (IR) light.
• Each gas has its own absorption characteristic. The gas mixture is transported into a sample cell, and
an IR filter selects a specific band of IR light to pass through the gas. For multiple gas measurements,
multiple IR filters are used.
• The higher the concentration of gas in the mixture the more IR light it absorbs. This means that
higher concentrations of IR absorbing gas results in lower transmission of IR light.
• The amount of IR light transmitted through an IR absorbing gas is measured.
• From the amount of IR light transmitted, the concentration of gas can be calculated. This
calculation provides the gas concentration value.
gas cannot be measured with this technique as it does not absorb IR light. Hence O2 gas is
O
2
measured with a sensor that makes use of the paramagnetic properties of O
technique.
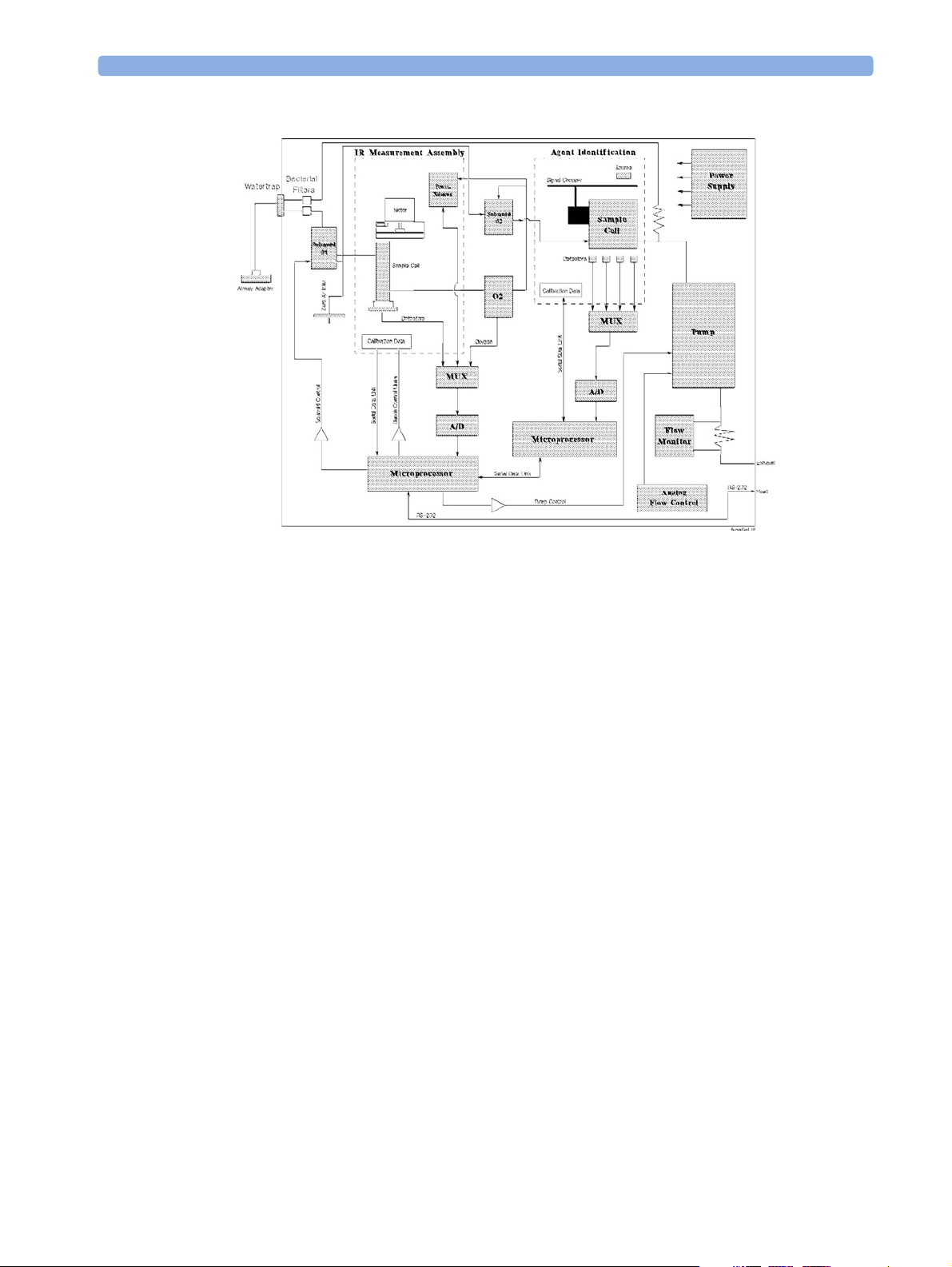
Theory of Operation
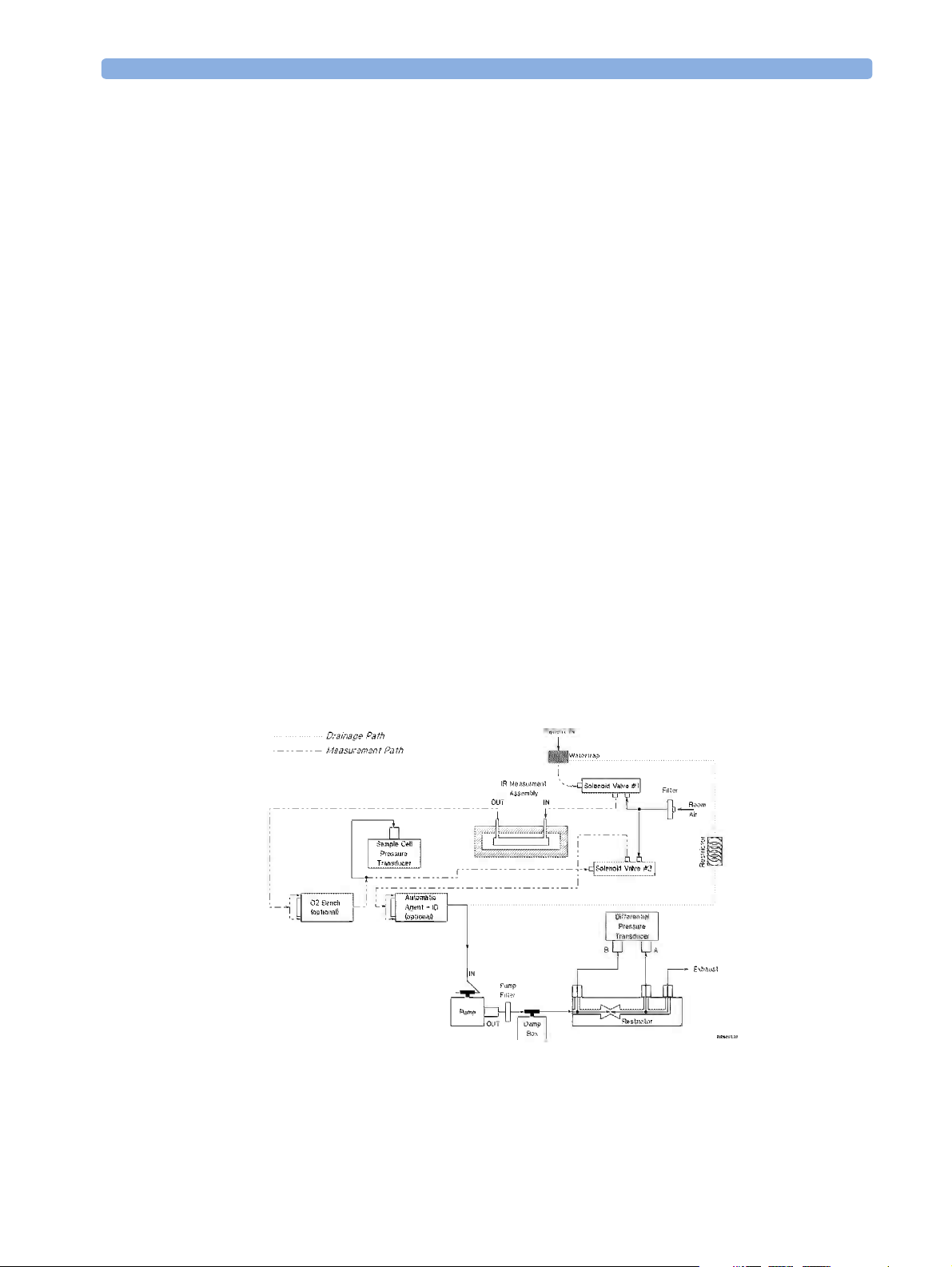
Figure 1 shows the functional blocks within the Philips M1026A Anesthetic Gas Module.
for its fast measurement
2
9
Page 12
1 Anesthetic Gas Module Introduction
The main components of the Philips M1026A Anesthetic Gas Module are:
• Main PC Board.
• Switching Power Supply.
• Pneumatic System.
• Agent Identification.
•O
• Infrared Measurement Assembly.
Main PC Board
This digital board:
• Controls the pneumatic system and the IR measurement assembly.
• Converts the preamplified analog output signal from the IR detector into a digital value. Under
software-controlled processing, this is then converted to a fully compensated gas concentration
value.
• Converts analog signals from the sample cell pressure sensor, transducer, sample cell temperature
thermistor, and the ambient temperature thermistor, into digital environmental data for gas
compensation and data reporting.
Figure 1 Anesthetic Gas Module Functional Block Diagram
Sensor.
2
10
• Converts an analog O
for CO
compensation and O2 data reporting.
2
signal, supplied by the O2 measurement system, into O2 concentration data
2
Page 13
Introduction 1 Anesthetic Gas Module
• Converts analog signals from the flow-control servo system and power supply into digital data for
status reporting.
• Processes the algorithm for end-tidal, inspired and respiration rate values.
• Controls the communication between the monitor and the Philips M1026A Anesthetic Gas Module
through an RS232 interface that uses a standard communications protocol.
• Contains the software program that controls the Philips M1026A Anesthetic Gas Module in a 128K
EPROM.
Power Supply
The input voltage is 100V - 240V. The output voltages are ±12V and +5V and the maximum output is
55W.
Pneumatic System
The main parts of the pneumatic system are:
•Watertrap.
• Pump assembly, including pump outlet filter.
• Two solenoid valves.
• Tubing system including:
– Differential pressure transducer and restrictor for control of the total flow.
–Measurement path.
– Drainage path parallel to measurement path.
• Ambient air reference filter.
Figure 2 Pneumatic System
11
Page 14

1 Anesthetic Gas Module Introduction
The pneumatic system works in the following way:
1 Eliminates residual water and fluids from patient sample gas using the watertrap and eliminates
water vapor using Nafion Tubing.
2 Splits the patient’s sample gas flow (150ml/min) into the measurement path (120ml/min) and
drainage path (30ml/min).
3 Passes the patient’s sample gas in the measurement path at 120ml/min through the measurement
benches.
4 Delivers zero calibration gas to the sample cells for the periodic zeroing.
5 Exhausts the patient’s sample gas, the zero calibration gas, and the span calibration gas.
6 Monitors for an occlusion in the sampling pneumatics.
Pump
The servo-controlled pump is attached to the exhaust of the Anesthetic Gas Module. It generates the
flow through the system and pulls the gas from the airway adapter through the measurement
subsystems to the exhaust outlet. It also delivers the zero calibration gas to the sample cells of the
measurement subsystems for the periodic zero procedures and it exhausts the patient’s sample gas, the
zero calibration and field calibration gases.
Watertrap
The flow-rate control logic drives the pump as hard as necessary to maintain the selected flow rate. A
partial occlusion or an inefficient pump results in the pump being driven harder. A serious occlusion
results in the pump being driven at or near its maximum load. This triggers a sensing circuit, which
then reports an occlusion.
Water Separation Filters
Wate r Fuse s
Patient Sample Inlet
Wate r Res e rvo i r
12
Figure 3 Watertrap
Page 15

Introduction 1 Anesthetic Gas Module
The watertrap consists of two water separation filters, two water fuses and a water reservoir. The gas
sample coming from the patient may contain fluids which are separated from the gas at the first water
separation filter. The gas is then split into two paths, the “measurement” path with the main part of the
total gas flow (including water vapor) continuing on the “dry” side of the separation filter and the
“drainage” path (containing any liquid droplets) with the smaller amount of the total flow continuing
on the “wet” side of this filter. At the pump both gas paths are recombined.
The watertrap proper includes “water fuses” in both the “measurement” and the “drainage” paths,
consisting of a material that swells when getting wet (when the reservoir is full or when fluid penetrates
the separation filter and enters the “measurement” path) and blocks the respective path at the inlet of
the unit. Once the “water fuses” are blown, any passage of fluid is blocked and the gas flow resistance
increases so that an occlusion is detected.
Sample Flow Through the Pneumatic Path
• The drainage path serves to withdraw fluid separated from the gas sample into the watertrap
reservoir, so that the AGM interior is protected from fluid that might cause an occlusion in the
measurement path.The drainage path leads into the large watertrap reservoir where all liquid water
and other fluids are collected. When the drainage path leaves the watertrap through a water
separation filter and a through a water fuse it leads through internal Nafion tubing then through a
bacterial protection filter and flow restrictor directly to the pump. This flow restrictor determines
the percentage distribution between drainage and measurement path flow.
• The measurement path leads through a water separation filter and through a water fuse on into the
measurement system. The patient sample gas (on the measurement path) then flows through
internal Nafion tubing and through a bacterial protection filter to the first solenoid valve. Room air
for the zero calibration is alternatively input (via a dust filter) to this solenoid valve. The solenoid
valve switches between the two gases depending on the current mode of operation - normal
measurement or zero calibration.
The patient sample gas or zero calibration gas then flows through the measurement subassemblies:
• the IR Measurement Assembly (for measurement of anesthetic agent, CO
•the O
cell (if present)
2
and N2O)
2
• the Agent Identification assembly.
A second solenoid valve between the O
cell and the Agent Identification Assembly routes room air
2
directly to the Agent Identification Assembly for optimal purging of the assembly during zero
calibration.
From the Agent Identification Assembly the patient sample gas or zero calibration gas flows to the
pump. Before reaching the pump, it joins the drainage path again.
From here it is passed through a filter and damper to the flow sensor which consists of a differential
pressure transducer and a flow restrictor. The flow sensor determines, stabilizes and limits the flow rate
of the sampled gas.
After the gas has passed through the flow sensor it is routed through a second damper to the Sample
Gas output.
Agent Identification Assembly
The agent ID analyzer identifies which anesthetic agents are present in a gas sample drawn from the
patients’s airway. The anesthetic agents are identified from a set of known anesthetic gases.
13
Page 16

1 Anesthetic Gas Module Introduction
Isoflurane
Enflurane
Halothane
Sevoflurane
Desflurane
Measurement Principle
Sample gas passes through the agent identification head where the absorption characteristics of the gas
are measured. This is done using NDIR technology as described in General Measurement Principles.
The head outputs analog signals and sends them for processing to identify the anesthetic agent.
Data averaging is used to ensure accurate measurements when agent concentrations are low. The
information used to calculate the concentrations of the three agents includes:
• The preamplified outputs from the IR detector.
• The thermistor output from the agent identification head.
• Zero calibration constants.
O2 Sensor
Specifications
Weight 335 g (0.75 lbs)
Size (HxWxD) 54 x 54 x 56 mm
Calibration Zero: Room Air
Measurement Principle
The O2 sensor uses a fast O2 measurement technique that utilizes O2 paramagnetic properties.
Two sealed spheres forming a dumb-bell assembly are filled with N
suspended in a symmetrical non-uniform magnetic field. The spheres take up a position away from the
most intense part of the field, due to the diamagnetic force on the dumbbells. The dumb-bell assembly
is then surrounded by the sample gas.
When the surrounding sample gas contains O
the magnetic field by the relatively stronger paramagnetic O
is proportional to the paramagnetism of the surrounding gases, and can therefore be taken as a measure
of the oxygen concentration.
Span: Suitable calibrated mixture
, the dumb-bell spheres are forced even further out of
2
. The dumb-bell assembly is
2
gas. The torque acting on the dumb-bell
2
14
This torque is measured by monitoring the current required in a servo system that attempts to return
the dumb-bells to their normal position.
Page 17
Introduction 1 Anesthetic Gas Module
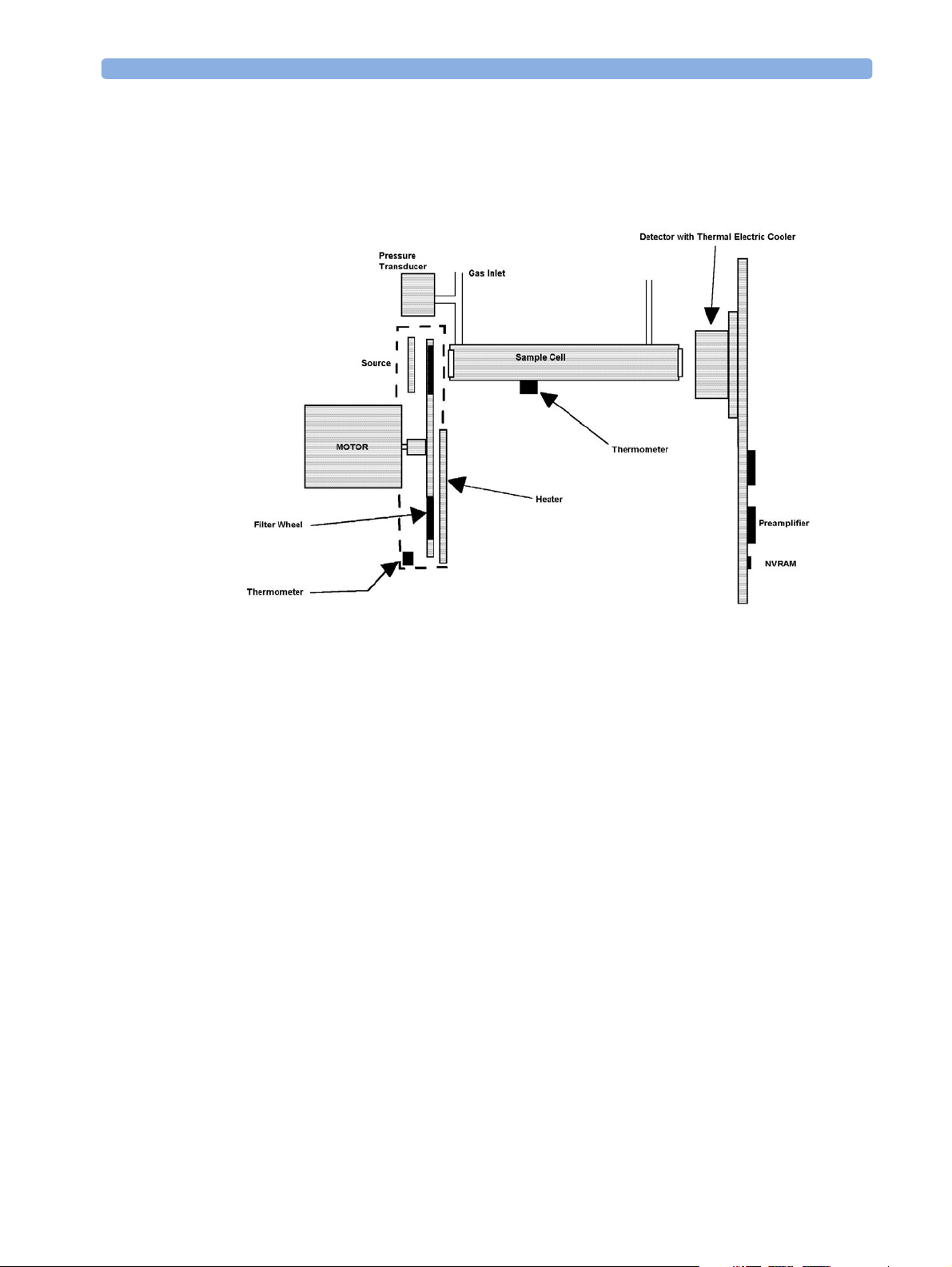
Infrared Measurement Assembly
The measurement assembly measures the IR light absorption of the gases in its sample cell (see Figure
4).
Figure 4 Anesthetic Gas Module Measurement Assembly
The measurement assembly contains the following subassemblies:
IR Source: The ceramic IR source is heated to 600°C by applyin g a constant
drive voltage across it.
Filter Wheel Assembly: The filter wheel assembly includes IR filters for the anesthetic agent,
CO
, N2O and a reference channel. A blank segment (dark period)
2
marks the beginning and end of the filter series.
Sample Cell: The sample cell is a stainless steel tube. It has non-IR absorbing
sapphire windows at both ends, and barbed inlet and outlet ports.
The inlet and outlet ports are placed as close as possible to the
windows so that the gas flows effectively through the cell.
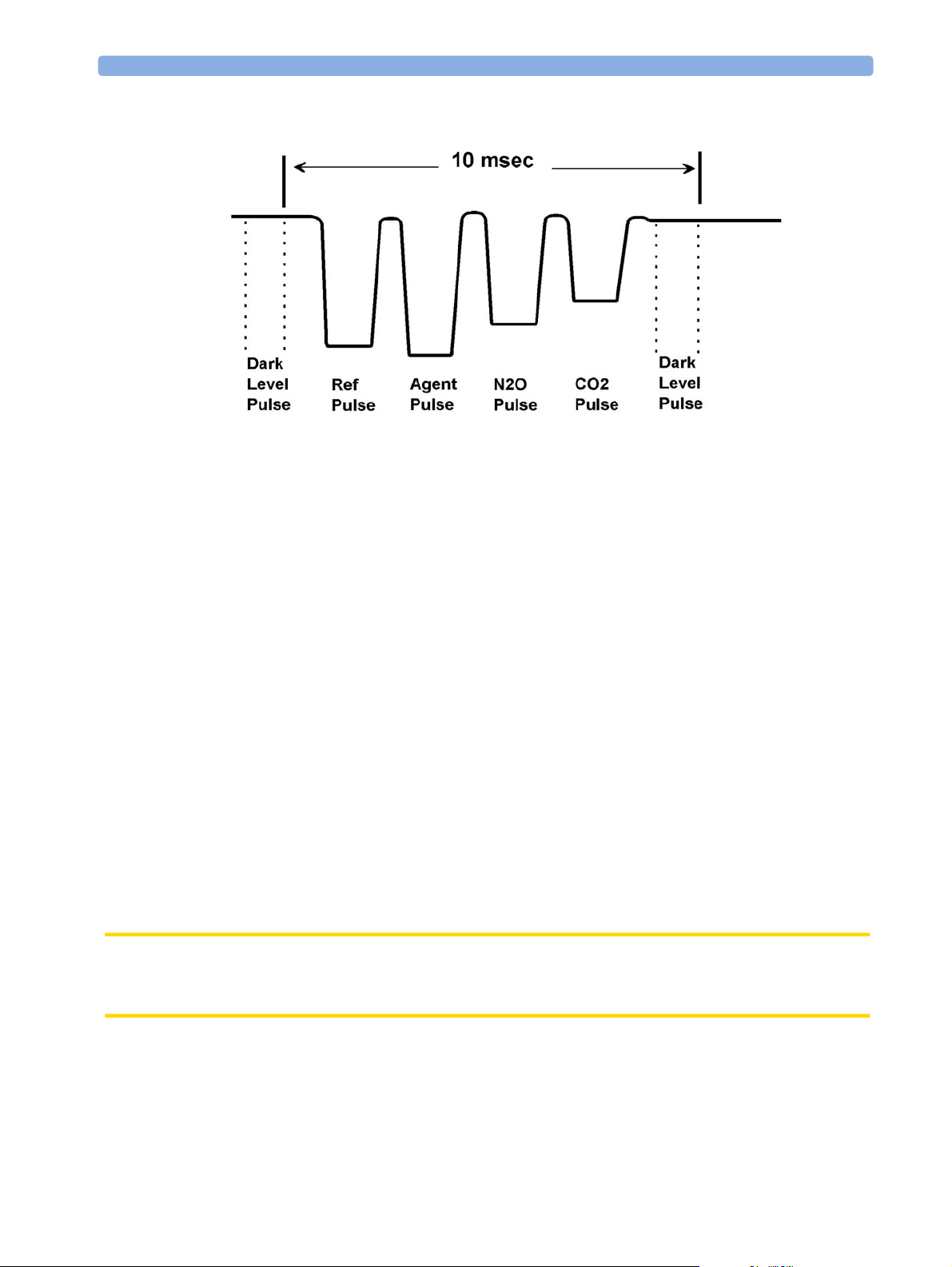
Preamp Assembly The preamplifier board assembly includes an IR detector, an IR-
detector thermistor, a TE cooler, and a pre-amplification circuit. The
output from the preamplifier is a stream of pulses; this pulse train has
one pulse for each IR filter, and is terminated by a blank period (dark
level phase) (see Figure 5).
15
Page 18
1 Anesthetic Gas Module Installation and Patient Safety
Figure 5 IR Detector Output Signal
Installation and Patient Safety
This chapter describes how to install the Philips M1026A Anesthetic Gas Module. It details the
operating environment required by the Philips M1026A Anesthetic Gas Module as well as instructions
on how to affix the local language labels and physically connect it to the monitor. Next, the patient
safety information is detailed. Finally, this chapter describes the software setup required and any postinstallation checks that have to be performed before using the Philips M1026A Anesthetic Gas Module
together with a reminder of the preventive maintenance (PM) checks and their frequencies.
Where post-installation procedures are specific to installation, they are described in full in this chapter.
For procedures which are also used in other situations (for example calibration, preventative
maintenance, etc.), a reference to the description will be given.
Physical Installation
This section describes the operating and storage environment for the Philips M1026A Anesthetic Gas
Module, affixing the local-language labels, connecting to the monitor, and fitting the gas exhaust
return system.
CAUTION The Philips M1026A Anesthetic Gas Module must be positioned horizontally on a level surface. To
avoid condensed water collecting in the patient sample tube, it is recommended that the Philips
M1026A Anesthetic Gas Module is positioned at or above patient level, wherever possible.
16
Page 19
Installation and Patient Safety 1 Anesthetic Gas Module
Environment
WARNING Possible explosion hazard if used in the presence of flammable anesthetics.
The environment where the Philips M1026A Anesthetic Gas Module is used should be free from
vibration, dust, corrosive or explosive gases, and extremes of temperature and humidity.
For a cabinet mounted installation with the monitor, allow sufficient room at the front for operation
and sufficient room at the rear for servicing with the cabinet access door open.
The Philips M1026A Anesthetic Gas Module operates within specifications at ambient temperatures
between 15°C and 40°C, 8 minutes after switching it on.
Ambient temperatures that exceed these limits could affect the accuracy of this instrument and cause
damage to the components and circuits. Allow at least 2 inches (5cm) clearance around the instruments
for proper air circulation.
CAUTION If the Philips M1026A Anesthetic Gas Module has been stored at temperatures below freezing, it needs
a minimum of 4 hours at room temperature to warm up before any connections are made to it.
Make sure that the Philips M1026A Anesthetic Gas Module is free of condensation before operation.
Condensation can form when equipment is moved from one building to another, thus being exposed
to moisture and differences in temperature.
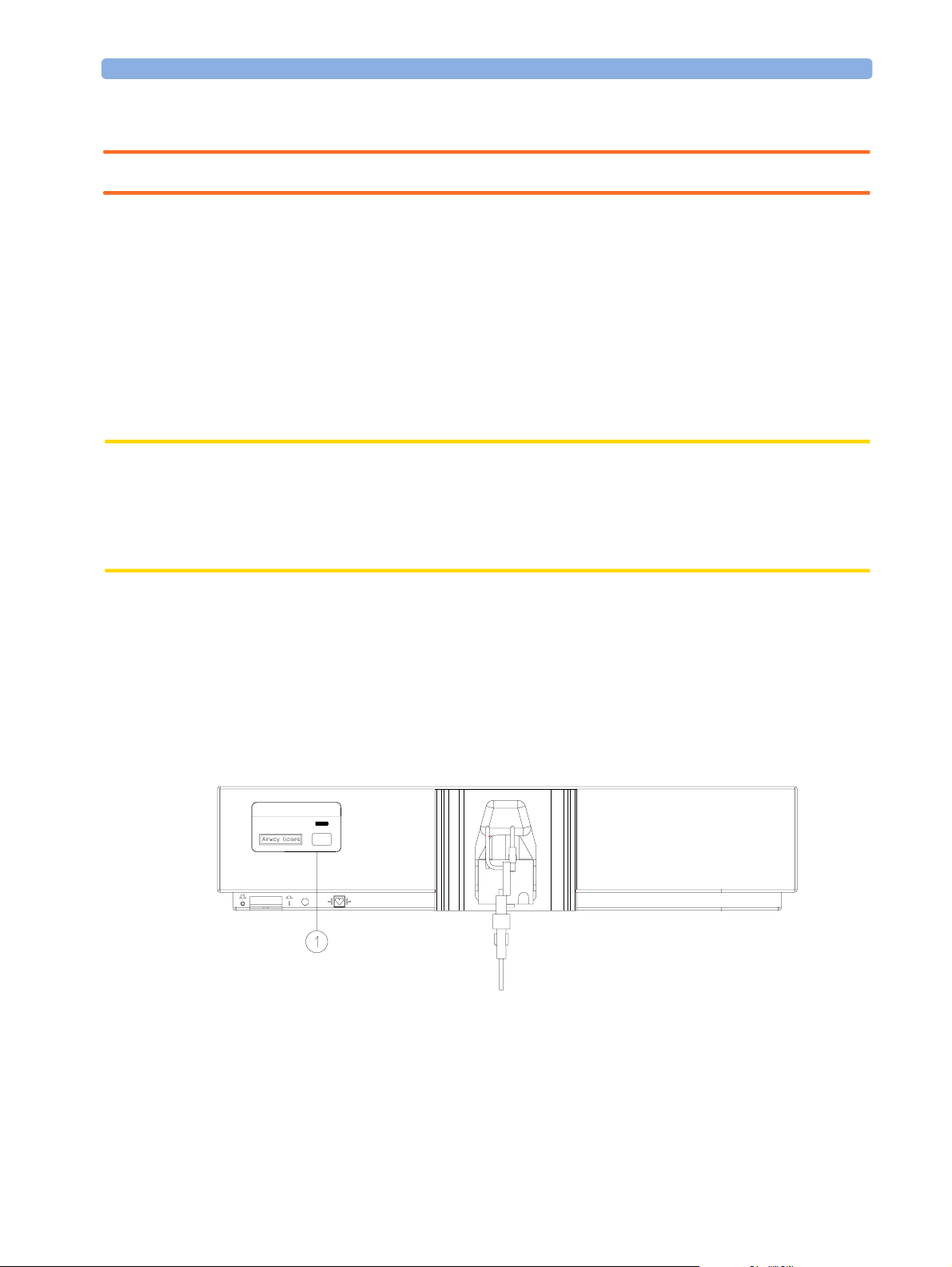
Label Sheet
There is a label sheet included with the Philips M1026A Anesthetic Gas Module which has the
translated versions for “Airway Gases”. You can stick a translated version over “Airway Gases” on the
left of the front panel. See (1) in Figure 6.
PAD M1026A
Figure 6 Label for the Philips M1026A Anesthetic Gas Module
Making Connections to the AGM
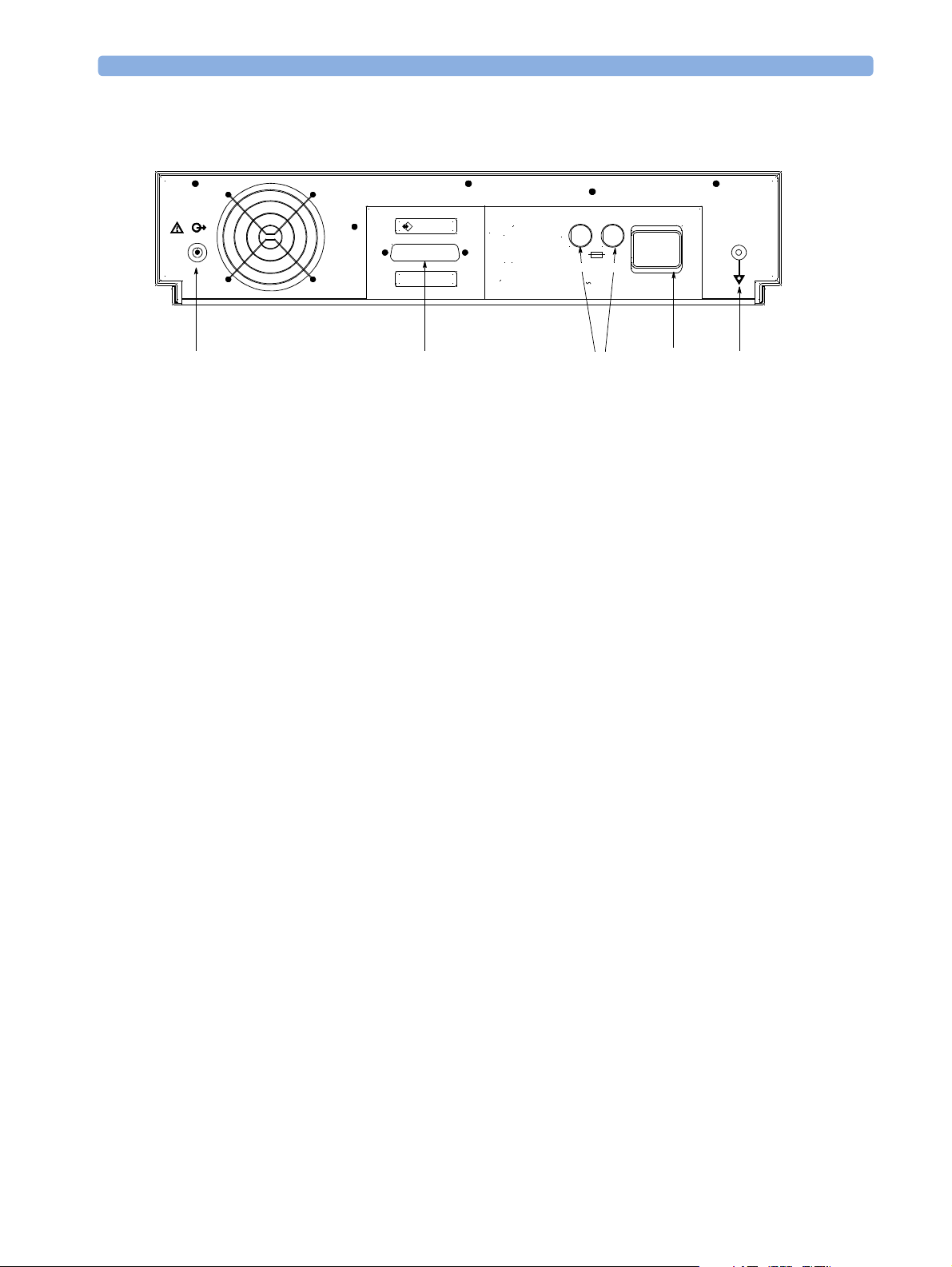
All connections to the AGM are made on its rear panel. Refer to Figure 7.
17
Page 20
1 Anesthetic Gas Module Installation and Patient Safety
600VA max.
100-240V
50-60 Hz
brear2d.tif
MONITOR
RS 232
T1.6 H 250V
60/140
(6)
Gas
Outlet
(2)
RS232
Connector
(5)
Fuses
Figure 7 The Rear Panel
1 Local power connector; this is a 3-pin connector, used to connect the AGM to the local line voltage
supply.
The module can be operated from an ac power source of 100 - 240 V ± 10%, 50/60 Hz. The
adjustment is made automatically by the power supply inside the module.
2 RS232 Connector (RS232 Interface); this is a 25-pin “D” type connector, used to connect the
AGM to the RJ45 connector of the monitor (Slot 08a, 07a, 04a, 03a, or 02a, - MIB I/O port - see
Connection of Devices via the MIB/RS232 Interface in the Installation Instructions section).
The connection can be made with the following cables:
– M1026A#K11 1 m (M1026-61001)
– M1026A#K12 3 m (M1026-61002)
– M1026A#K13 10 m (M1026-61003)
(1)
Local
Power
Connector
(4)
Equipotential
Grounding
Terminal
3 Equipotential Grounding Terminal; this is used to connect the AGM to the hospital’s grounding
system.
4 Line protection fuses, T1.6 H 250V.
5 Anesthetic gas exhaust. If N
O and/or other inhalation anesthetics are used during anesthesia,
2
pollution of the operating room should be prevented. Once the gas sample has passed through the
AGM, it should either be returned to or removed from the anesthesia circuit.
Sample Gas Connections to the Gas Exhaust
Returning the Gas Sample
You will need the following equipment to return the gas sample to the anesthesia circuit:
18
Page 21
Installation and Patient Safety 1 Anesthetic Gas Module
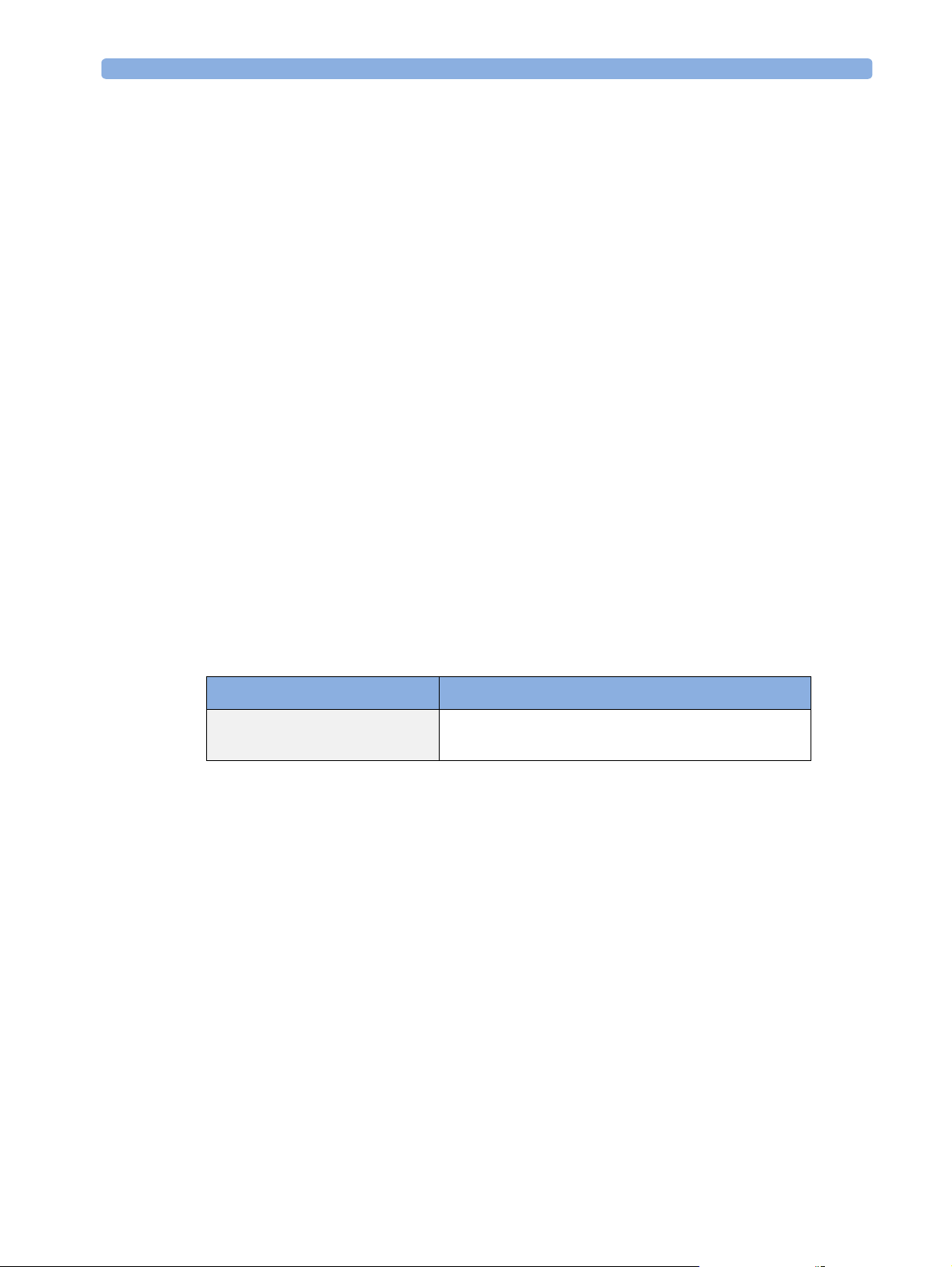
Equipment Part Number Comments
Gas Exhaust Return Line M1655A Tu b i ng i n cl u d e s t wo p ar t s :
Tube A = 50cm long
Tube B = 3m long
Gas Exhaust Return Filter M1656A Single patient use only
NOTE
The M1655A may not be available in all countries.
Setting Up the Gas Return
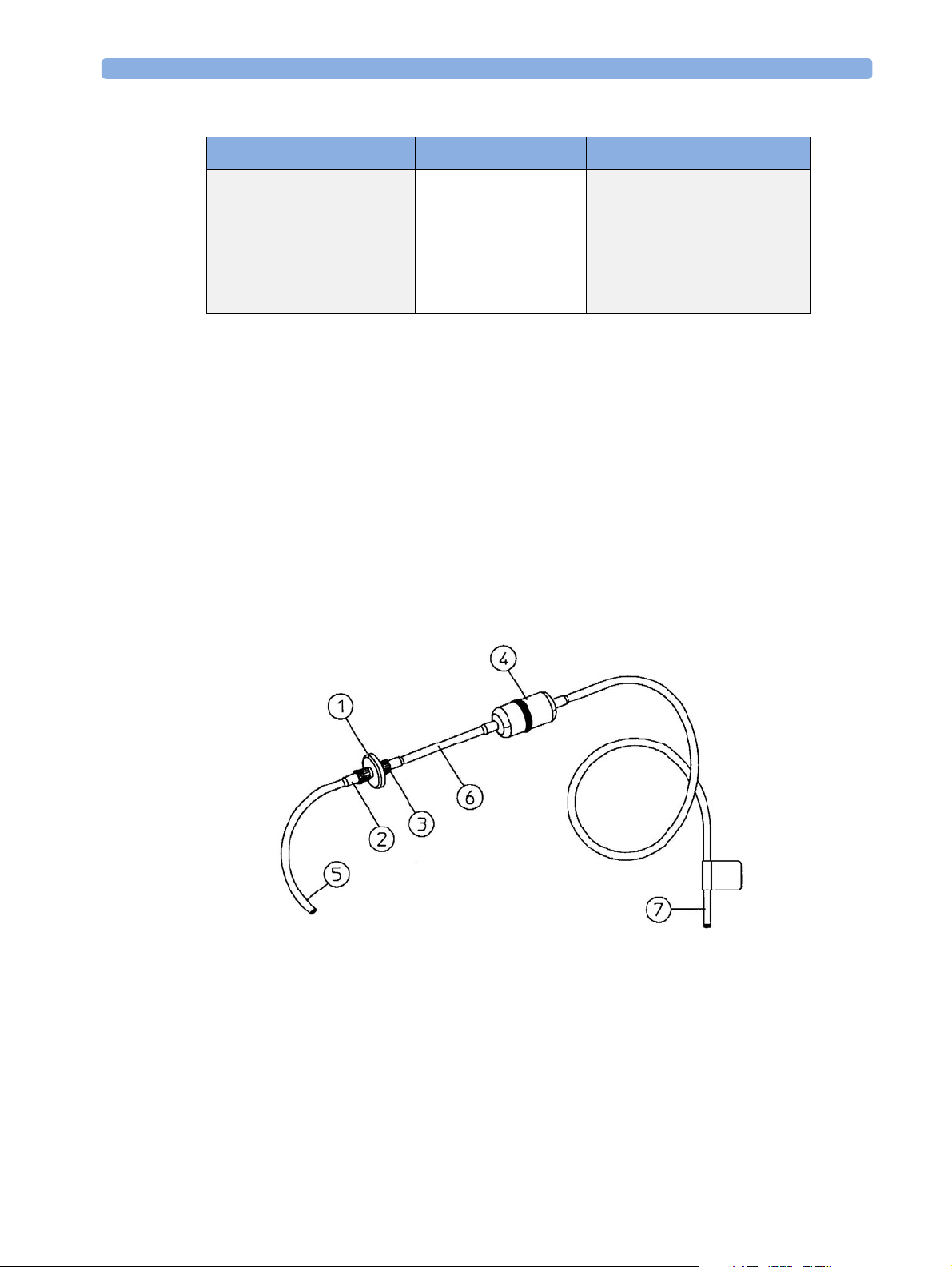
(see diagram Figure 8)
1 Fit the male luer lock connection (2) of the shorter tube, to the female side of the M1656A Gas
Exhaust Return Filter.
2 Fit the female luer lock connection (3) of the longer tube, to the male side of the M1656A Gas
Exhaust Return Filter.
3 Fit the open end (7) of the longer tube to the AGM’s Anesthetic Gas Exhaust.
4 Fit the open end (5) of the shorter tube to the ventilation circuit.
Figure 8 Setting Up the Gas Return
1 M1656A Gas Exhaust Return Filter
M1655A Gas Exhaust Return Line comprising:
2 Female luer lock
3 Male luer lock
19
Page 22

1 Anesthetic Gas Module Installation and Patient Safety
Dampener
4
5 Shorter tube
6 Connecting tube
7 Longer tube - connected to AGM exhaust port
Removing the Gas Sample
To remove the gas sample from the anesthesia circuit, a scavenging system needs to be connected to the
AGM’s Anesthetic Gas Exhaust. If you intend to use a scavenging system with the AGM, one of the
following parts must also be connected to protect it against malfunction:
1 A ventilator reservoir where the suction pressure does not exceed 0.3-0.4 mmHg or
2 A scavenging interface, properly set and maintained (see scavenging interface manufacturer’s
instructions).
Setup and Configuration Procedures
This section describes final setting up and configuration procedures that must be completed after the
AGM is connected to the monitor and switched on but before the AGM is used for monitoring.
Altitude Configuration
The altitude setting for the monitor is important as it is used as a reference to check the AGM ambient
pressure measurement.
See the Installation Instructions section for details.
Connect Sample Input Tubing
Connect the sample input tubing to the watertrap at the patient sample inlet on the water separation
filter. For details, refer to the Instructions for Use.
Preventive Maintenance (PM) Tasks
The preventive maintenance (PM) tasks are described in detail in chapter 5 of this guide. Here is a
short list of the PM tasks and how often they must be performed.
To ensure operation of the Philips M1026A Anesthetic Gas Module within specified limits:
1 Check the ventilator fan in the AGM for proper operation and build-up of dust and lint every 6
months.
2 Check the AGM’s calibration at least once every 12 months, or whenever the validity of the
readings is in doubt.
3 Replace the internal Nafion; tubing, room air filter, and pump filter, internal bacterial filters and
watertrap manifold seals, using the PM kit, every 12 months.
20
4 Test the pump using the test procedure provided in the PM Kit every 12 months. The square-
shaped pump should be cleaned before testing; the round-shaped pump may not be cleaned.
5 Check electrical safety (ground impedance test and enclosure leakage current test) at least every 12
months.
All safety and maintenance checks must be made by qualified service personnel.
Page 23
Installation and Patient Safety 1 Anesthetic Gas Module
WARNING Failure to implement a satisfactory maintenance schedule by the individual, hospital or institution
responsible for the operation of this equipment may cause equipment failure and possible health
hazards.
Post-Installation Checks
See Test and Inspection Matrix for details.
WARNING Do not use the instrument for any monitoring procedure on a patient if you identify anything which
indicates impaired functioning of the instrument.
Safety Requirements Compliance and Considerations
The Philips M1026A Anesthetic Gas Module complies with the following international safety
requirements for medical electrical equipment:
• UL 2601-1
• IEC-60601-1
• CSA C22.2 No. 601.1-M90
• EN 60601-1
• EN 60601-1-2
Explanation of Symbols Used
Attention, consult accompanying documents.
Indicates that the instrument is type CF and is designed to have special
protection against electric shocks (particularly regarding allowable leakage
currents, having an F-Type isolated (Floating) applied part), and is
defibrillator proof.
A gas output (this symbol is also used to indicate an electrical output on the
monitor).
21
Page 24
1 Anesthetic Gas Module Installation and Patient Safety
A gas input (on the monitor this symbol can also stand for a video or 60V dc
input).
Equipotential grounding terminal.
RS232 communication port.
Fuse.
Protective earth ground.
Electrical shock hazard.
The Anesthetic Gas Module is protected against the effects of defibrillation and electrosurgery.
Power Supply Requirements
The system and the Anesthetic Gas Module can both be operated from an AC supply of 100 - 240V
±10%, 50 - 60Hz.
Grounding the System
To protect the patient and hospital personnel, the cabinet of the installed equipment has to be
grounded. The equipment is supplied with a detachable 3-wire cable which grounds the instrument to
the power line ground (protective earth) when plugged into an appropriate 3-wire receptacle. If a 3wire receptacle is not available, consult the hospital electrician.
22
Page 25
Checking and Calibrating the Anesthetic Gas Module 1 Anesthetic Gas Module
WARNING Do not use a 3-wire to 2-wire adapter.
Equipotential Grounding
Protection class 1 instruments are already included in the protective grounding (protective earth)
system of the room by way of grounding contacts in the power plug. For internal examinations on the
heart or the brain, Computer Module and Display Module of the System and the Philips M1026A
Anesthetic Gas Module must have separate connections to the equipotential grounding system.
One end of the equipotential grounding cable (potential equalization conductor) is connected to the
equipotential grounding terminal on the instrument’s rear panel and the other end to one point of the
equipotential grounding system. The equipotential grounding system assumes the safety function of
the protective grounding conductor if ever there is a break in the protective grounding system.
Examinations in or on the heart (or brain) should only be carried out in rooms designed for medical
use incorporating an equipotential grounding system.
Combining Equipment
If it is not evident from the instrument specifications whether a particular instrument combination is
hazardous or not, for example, due to summation of leakage currents, the user should consult the
manufacturers concerned or an expert in the field, to ensure that the necessary safety of all instruments
concerned will not be impaired by the proposed combination.
Checking and Calibrating the Anesthetic Gas Module
This chapter explains how to check the Anesthetic Gas Module to ensure that it is operating within its
specified limits. A list of the equipment required to carry out the checks is included, as well as step-by
step instructions for the calibrations.
If you receive fail indications while testing, refer to the troubleshooting section of this chapter for
guidance. If you are instructed to remove or replace parts of the Anesthetic Gas Module refer to the
respective section.
Access Service Functions of the M1026A Anesthetic Gas Module
Enter service mode and select the service screen (see Testing and Maintenance for instructions on
entering service mode). In the
Analyzer Diagnostic
displayed. In this window you can as well start the flow calibration, the barometric pressure calibration
and the gas span calibration.
Setup Gas Analyzer menu can be accessed by either going to the Main Setup menu and
The
selecting
Gas Analyzer, or by pressing the setup key on the Anesthetic Gas Module.
Setup Gas Analyzer menu you can choose whether the Gas
window or the Gas Analyzer Calibration window should be
23
Page 26
1 Anesthetic Gas Module Checking and Calibrating the Anesthetic Gas Module
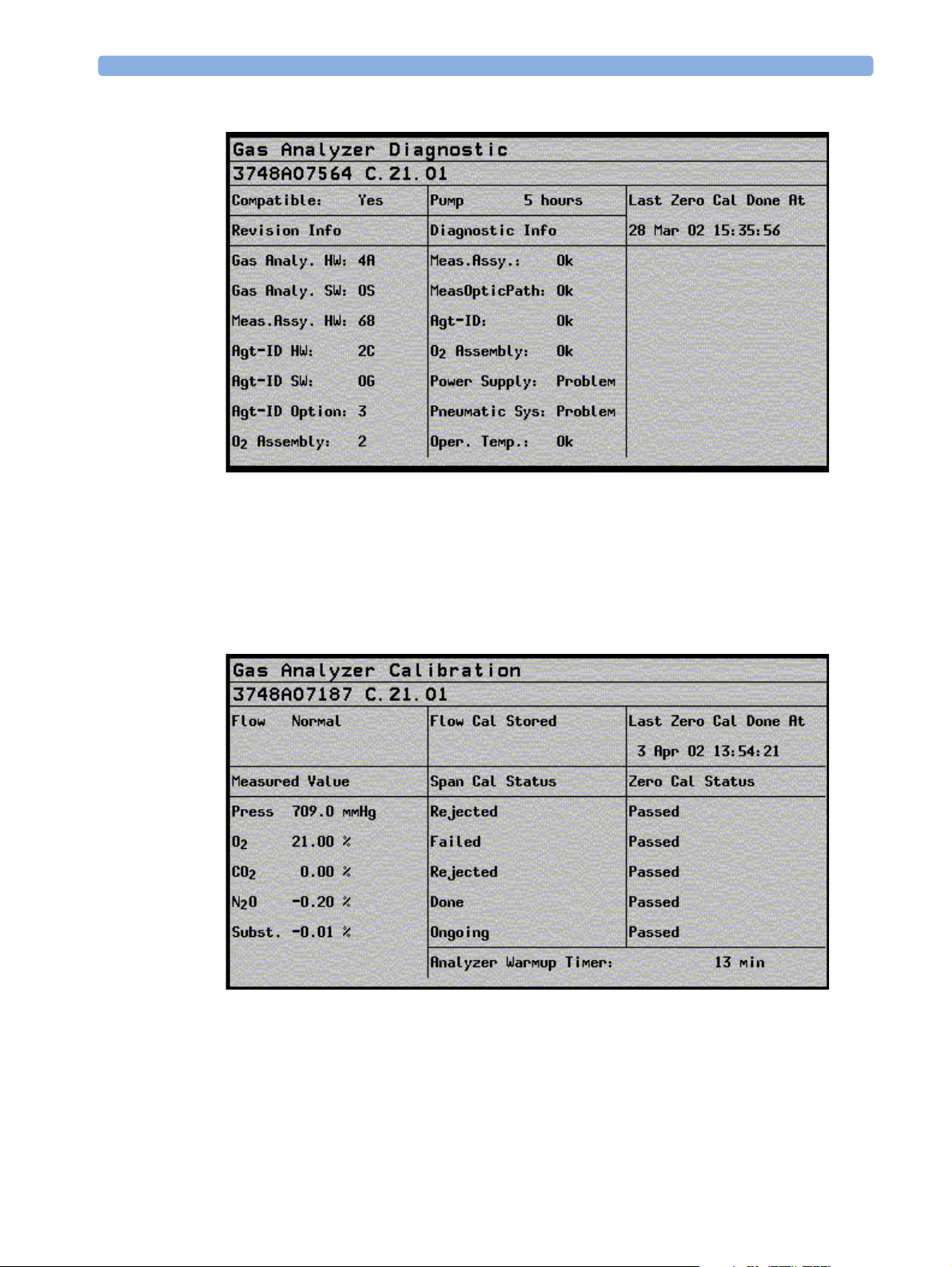
Figure 9 Gas Analyzer Diagnostic Window
This window provides you with diagnostic information about the AGM. In the
Analyzer
menu select Service Window then select Calibration to access this window.
Setup Gas
24
Figure 10 Gas Analyzer Calibration window
Page 27
Checking and Calibrating the Anesthetic Gas Module 1 Anesthetic Gas Module
This window provides you with information about all calibrations that can be performed on the
Anesthetic Gas Module. In the
Diagnostic to access this window.
Setup Gas Analyzer menu select Service Window then select
When and how to check the Philips M1026A Anesthetic Gas Module
To ensure that the Philips M1026A Anesthetic Gas Module operates with the specified limits, it must
be checked:
1 After installation
2 Every 12 months or if the measurements are in doubt.
3 After repairing the AGM
If you find values outside the tolerance limits while checking, the Philips M1026A Anesthetic Gas
Module must be recalibrated. Tolerance values are given at the end of each section.
The basic steps to check the Philips M1026A Anesthetic Gas Module are:
1 Enter Service Mode at the monitor and wait for first automatic zero calibration after the warm-up
period.
2 Perform:
a. a leakage check
b. a flowrate check
to ensure that there are no leaks in the gas system and that the flowrates are set correctly.
3 Perform Zero calibration.
4 Check that there are no reported errors.
5 Check the Barometric Pressure calibration; perform it if necessary.
6 Check the Span calibration of gases; perform it if necessary.
7 If Barometric Pressure or Span calibrations were performed, re-perform Zero calibration.
WARNING Only perform Zero, Barometric Pressure and gas Span calibration checks when the top cover is closed.
Light and electro-magnetic interference can affect the measurements.
Equipment required for checking
The following equipment is required for checking the AGM. Part numbers are given in the Parts List
section.
1 Electronic Flowmeter M1026-60144 (Instructions are provided with the flowmeter. See also
Service Note M1026A-034).
2 Span Calibration Equipment.
–Calibration Gas.
–Calibration Tubing
25
Page 28
1 Anesthetic Gas Module Checking and Calibrating the Anesthetic Gas Module
WARNING Philips Calibration Gas contains Halocarbon 22. Halocarbon 22 is represented in the Calibration
menu by “Substitute”, which is the default. If you are using another calibration gas, this must be
selected in the menu.
Checks and adjustments
The following sections explain the steps needed to carry out the checks and adjustments. A complete
check and calibration procedure requires approximately 45 minutes, including waiting time.
NOTE Make sure that the watertrap is attached.
Performance Leakage Check
Complete the following steps to do a performance leakage check:
NOTE Do not perform the leakage check while a Zero calibration is running.
1 Switch on the Philips M1026A Anesthetic Gas Module and the monitor.
2 Wait until the Anesthetic Gas Module enters the warm up phase.
3 Connect a flowmeter to the exhaust outlet of the Philips M1026A Anesthetic Gas Module.
4 Connect the watertrap to the watertrap manifold.
5 Note the flowrate.
6 Block the gas inlet at the watertrap inlet connector (use your fingertip).
The reading at the flowmeter should decrease to Zero (see table below). If it does not, systematically
block the pneumatic path at various points before the pump to isolate the leakage point. (See Figure
2, "Pneumatic System" for tubing connections.) When the fault has been corrected, repeat the
leakage check.
7 Connect the flowmeter to the inlet.
8 Note the flowrate.
9 Block the Anesthetic Gas Module exhaust (using your finger tip).
10 Check the effect of blocking the exhaust.
The reading at the flowmeter should decrease to Zero (see Table 4-1). If it does not, systematically
block the pneumatic path at various points after the pump to isolate the leakage point. (See Figure 2,
"Pneumatic System" for tubing connections.) When the fault has been corrected, repeat the leakage
check.
26
Items Value / Tolerance
Leakage Range: 0 → 4 ml/min
Page 29
Checking and Calibrating the Anesthetic Gas Module 1 Anesthetic Gas Module
Performance Diagnostic Check
Complete the following to do a performance diagnostic check:
1 Enter the service mode of the monitor and let the Philips M1026A Anesthetic Gas Module
complete the warm-up phase (the
2 Make sure that the watertrap is attached.
3 In the Setup Gas Analyzer menu select Service Window then select Diagnostic to
access the
4 Check that no permanent problems are reported for the Philips M1026A Anesthetic Gas Module
in the
Gas Analyzer Diagnostic window.
Gas Analyzer Diagnostic window.
GA WARMUP INOP disapears).
Performance Flowrate Check
Always perform a leakage check before the flowrate check. Three flowrates need to be checked in the
following order:
1 To t a l f lo w i n Purge mode.
2 Flow in Measurement Path in Normal mode.
3 To t a l f lo w i n Normal mode.
These flowrate checks are described in the following three procedures.
The total flow is measured by connecting the flowmeter to the exhaust, the measurement path flow is
measured by connecting the flowmeter to the gas inlet with a special test fixture.
The Flowrate values are summarized in the following table:
Total Flowrate Va lu e
Purge 310 ml/min
Normal 150 ml/min
NOTE Do not perform the flowrate check while a Zero calibration is running.
Total Flowrate Check and Adjustment in Purge Mode
To make the flowrate measurements and any necessary adjustment:
1 Enter the service mode of the monitor and let the Philips M1026A Anesthetic Gas Module
complete the warm-up phase (the
2 In the Setup Gas Analyzer menu select Service Window then select Calibration to
access the
3 Enter the Setup Gas Analyzer menu and select Start Flow Cal.
Gas Analyzer Calibration window.
GA WARMUP INOP disapears).
4 Select Flow Rate.
5 Select Purge for purge flow (310 ml/min).
6 Connect a flowmeter to the exhaust port of the Philips M1026A Anesthetic Gas Module.
27
Page 30
1 Anesthetic Gas Module Checking and Calibrating the Anesthetic Gas Module
7 Note the actual flowrate by following the instructions accompanying the flowmeter. If the actual
flowrate is outside the tolerance, it must be adjusted. If no adjustments are required, select Stop
Flow Cal.
Total Flowrate in Purge Mode To l er a nc e
310 ml/min +/- 15 ml/min
Flowrate Adjustment:
8 Remove the Philips M1026A Anesthetic Gas Module top cover (see “The Top Cover” on page 64)
9 Correct the flowrate by adjusting potentiometer R125 on the Main PC board until the required
value is achieved.
Flowrate Calibration:
10 If you have made adjustments you must save the settings. Therefore select Store Flow Cal and
confirm when prompted.
The system then runs through various flowrates and switches the pump off before it saves the
values internally.
The flow display in the Calibration window reflects these changes and the status “Flow Cal
Stored” appears.
11 Disconnect the flowmeter from the exhaust port.
Measurement Path Flowrate Check and Adjustment
The flowrate of the measurement path is checked using a test fixture in the form of a modified
watertrap. In order to perform the flow rate check, the following equipment is required:
• Flow Split Test Tool M1026-60136
• Electronic Flowmeter M1026-60144
NOTE 1 Check that the test fixture is still valid for use. It must be less than two years old. The test fixture is
labelled with a “Received” date that needs to be filled in when the test fixture is received.
2 The flow value that is labelled on the test fixture is to be used to perform the measurement path
flowrate check. It is only valid for this test fixture.
3 Check the test fixture visually for leaks. Regularly perform a leakage check with the test fixture
attached instead of the watertrap. Block both lines (drainage and measurement) at the same time
while performing the leakage check. Block the measurement line with a luer cap or a similar device
and the drainage line with your fingertip. If a leak exists, replace the test fixture.
WARNING Always handle the test fixture carefully and avoid contact with dust. Do not change or modify the test
line/loops as this can change the flow resistance.
28
Make sure that there are no sharp bends or kinks in the tubing that leads to the test fixture. If a kink is
visible, replace the fixture and use the new one.
Page 31

Checking and Calibrating the Anesthetic Gas Module 1 Anesthetic Gas Module
xxx
To make the flowrate measurements and any necessary adjustment:
1 Enter the service mode of the monitor and let the Philips M1026A Anesthetic Gas Module
complete the warm-up phase (the
GA WARMUP INOP disapears).
2 In the Setup Gas Analyzer menu select Service Window then select Calibration to
access the
Gas Analyzer Calibration window.
3 Enter the Setup Gas Analyzer menu and select Start Flow Cal.
4 Select Flow Rate.
5 Select Normalfor normal flow (150 ml/min).
6 Remove the watertrap from its manifold and connect the flow split test fixture to the Philips
M1026A Anesthetic Gas Module.
7 Connect the measurement line of the test fixture to the flowmeter using the mal Luer Lock.
Check:
8 Note the actual flowrate by following the instructions accompanying the flowmeter. If the actual
flowrate is outside the tolerance, it must be adjusted. The target value for the flow is labelled on the
test-fixture. If no adjustments are required, select Stop Flow Cal.
Measurement Path Flowrate To l e ra n c e
Value labelled on Test Fixture +/- 3 ml/min
Flowrate Adjustment:
29
Page 32

1 Anesthetic Gas Module Checking and Calibrating the Anesthetic Gas Module
Remove the Philips M1026A Anesthetic Gas Module top cover (see the respective section in this
9
manual)
10 Correct the flowrate by adjusting potentiometer R126 on the Main PC board until the required
value is achieved.
Flowrate Calibration:
11 If you have made adjustments you must save the settings. Therefore select Store Flow Cal and
confirm when prompted.
The system then runs through various flowrates and switches the pump off before it saves the
values internally.
12 Disconnect the flowmeter from the test-fixture.
13 Replace test-fixture with watertrap
Total Flowrate Check in Normal Mode
To make the flowrate measurements and any necessary adjustment:
1 Enter the service mode of the monitor and let the Philips M1026A Anesthetic Gas Module
complete the warm-up phase (the
GA WARMUP INOP disapears).
2 Enter the Setup Gas Analyzer menu and select Start Flow Cal.
3 Select Flow Rate.
4 Select Normal for normal flow (150 ml/min).
5 Connect a flowmeter to the exhaust port of the Philips M1026A Anesthetic Gas Module.
Check:
6 Note the actual flowrate by following the instructions accompanying the flowmeter. If the actual
flowrate is outside the tolerance, check all tubing for occlusions (for example kinks, dirt) and
replace if necessary. Repeat flowrate check. If the flowrate is still no within tolerance, exchange the
Nafion tubing, bacterial filters and restrictor in the drainage path (provided with the Internal
Tubing Kit and the Preventive Maintenance Kit) before repeating flowrate check.
If no adjustments are required, select Stop Flow Cal.
Total Flowrate in Normal Mode To l er a nc e
has to be between 132 ml/min
170 ml/min
7 Disconnect the flowmeter from the exhaust port.
Zero Calibration
NOTE Only perform a zero calibration with the top cover closed. Light and electro-magnetic interference may
affect the measurements. Zero calibration is not possible during warm-up.
Complete the following to perform a zero calibration in service mode:
1 In the Setup Gas Analyzer menu select Service Window.
2 Select Calibration to access the Gas Analyzer Calibration window.
30
Page 33

Checking and Calibrating the Anesthetic Gas Module 1 Anesthetic Gas Module
In the Setup Gas Analyzer menu select Zero Cal and press Confirm when prompted to.
3
4 Wait until zero calibration is complete. In the Gas Analyzer Calibration window a OK /
Failed indication is displayed against each channel. If a Failed indication cannot be cleared by
another zero calibration refer to the appropriate section of this manual and correct the fault. Then
repeat this procedure.
Barometric Pressure Check and Calibration
For this calibration you need the absolute barometric pressure at your hospital location. Normally this
value can be provided by the hospital as it is needed in the laboratory.
If the hospital cannot provide an accurate value for the barometric pressure, call the local airport or
weatherstation. Since airports and weatherstations normally provide you with a pressure that has been
corrected to sea level, ensure that the value you are given is an uncorrected absolute barometric pressure
reading! The following table shows you typical barometric pressures at various altitudes.
Altitude Typ ic al
Barometric
Pressure
Altitude Typi ca l
Barometric
Pressure
Altitude Typi ca l
Barometric
Pressure
0 m 760 mmHg 1100 m 664 mmHg 2200 m 577 mmHg
100 m 751 mmHg 1200 m 656 mmHg 2300 m 570 mmHg
200 m 742 mmHg 1300 m 648 mmHg 2400 m 562 mmHg
300 m 733 mmHg 1400 m 639 mmHg 2500 m 555 mmHg
400 m 724 mmHg 1500 m 631 mmHg 2600 m 548 mmHg
500 m 715 mmHg 1600 m 623 mmHg 2700 m 540 mmHg
600 m 707 mmHg 1700 m 616 mmHg 2800 m 533 mmHg
700 m 698 mmHg 1800 m 608 mmHg 2900 m 526 mmHg
800 m 689 mmHg 1900 m 600 mmHg 3000 m 519 mmHg
900 m 681 mmHg 2000 m 592 mmHg
1000 m 672 mmHg 2100 m 585 mmHg
If only a corrected (to sea-level or 0 meters) reading is available, uncorrect the reading for the altitude
you are on using the following equation:
p
typical
p
barometricpcorrected
where:
=
------------------------- -
×
760mmHg
p
corrected
p
typical
ambient air pressure corrected to sea-level
=
typical atmospheric pressure at a given altitude
=
Conversion: 1 mmHg = 1.33 hPa = 0.03937 inHg
31
Page 34

1 Anesthetic Gas Module Checking and Calibrating the Anesthetic Gas Module
NOTE
Only perform a Barometric Pressure check and calibration with the top cover closed. Light and electromagnetic interference may affect the measurements. Pressure calibration is not possible during warmup.
Complete the following to steps to perform a barometric pressure check and calibration:
1 Get the absolute barometric pressure at your hospital location.
2 Enter the service mode of the monitor and let the Philips M1026A Anesthetic Gas Module
complete the warm-up phase (the
3 In the Setup Gas Analyzer menu, select Service Window.
4 Select Calibration to access the Gas Analyzer Calibration window.
GA WARMUP INOP disapears).
Check:
5 Check if the barometric pressure displayed next to the Press label. in the calibration window is
within the tolerance limits. A zero calibration is automatically started in order to display the
calibrated pressure value. This value is updated with each following zero calibration.
Measured Value To l er a nc e
Barometric Pressure +/- 5 mmHg
Calibration:
6 Enter the Setup Gas Analyzer menu and select Start Press. Cal.
7 Select the value representing the current absolute barometric pressure and confirm when prompted
8 After calibration has been completed, check if the barometric pressure displayed next to Press. in
the calibration window is within the tolerance limits.
Span Calibration Check
NOTE The Philips M1026A Anesthetic Gas Module should run for at least 30 minutes before continuing
with the following calibration procedures. This is to allow the module to reach a stable measurement
condition. The Analyzer Warmup timer in the Calibration window indicates the time span since the
last power on.
Only perform Span calibration checks when the top cover is closed. Light and electro-magnetic
interference can affect the measurements.
Before performing a Span calibration check, you must first perform:
• Performance Leakage Check.
• Performance Diagnostic Check.
• Performance Flowrate Check .
•Zero Calibration Check .
32
• Barometric Pressure Calibration Check .
• Ensure that there is enough gas in the calibration gas bottle.
• Check tubing assembly.
Page 35

Checking and Calibrating the Anesthetic Gas Module 1 Anesthetic Gas Module
Figure 11 Span Calibration Equipment including Gas Canister and Spray Valve
CAUTION Ensure that the room you are working in is well-ventilated, and that the Philips M1026A Anesthetic
Gas Module exhaust is properly connected to the gas scavenging system.
1 In the Setup Gas Analyzer menu select Service Window.
2 Select Calibration to access the Gas Analyzer Calibration window.
3 Select the Select Cal Agent item from the Setup Gas Analyzer menu.
4 Pre-select the agent that is being used during calibration. If Halocarbon 22 is in use, select
Subst..
5 Connect the calibration gas bottle, the reservoir bag and the sample line as shown in Figure 11,
"Span Calibration Equipment including Gas Canister and Spray Valve".
6 Wait u nt i l th e GA OCCLUSION INOP appears on the monitor. Now wait for another 10 seconds
to let the Anesthetic Gas Module completely evacuate the reservoir bag.
7 Now fill the reservoir bag with gas.
CAUTION Do not pressurize the reservoir bag.
Do not attempt the calibration process if tere are any visible leaks in the bag or tubing.
Prevent the bag from emtying before the calibration procedure is complete.
33
Page 36

1 Anesthetic Gas Module Checking and Calibrating the Anesthetic Gas Module
Check
8 Check if the readings for the different gases in the Gas Analyzer Calibration window are
within the specified tolerance limits.
Gas M1660A value Tol e r a n c e L i mi t s
O
2
CO
2
N2O40%+/- 2.0%
Anesthetic Agent
or Halocarbon 22 as substitute
52% +/- 1.0%
5% +/- 0.1%
3% +/- 0.1%
9 Perform a span calibration for each gas that you find out of its tolerance limits.
Calibration
10 In the Setup Gas Analyzer menu select the calibration item for each gas that you want to
calibrate. You must have completed the flow adjusment in order to perform these calibrations. The
different items are:
Start O2 Cal
Start CO
Start N
Start Agent
Cal
2
O Cal
2
Cal
11 .Select the concentration of the appropriate gas in your test gas and confirm when prompted to.
12 Wait for the calibration to finish. Check that in the Gas Analyzer Calibration window a
Done indication is displayed against the gas that you wanted to calibrate. If not, repeat the span
calibration for this gas.
If you still get a failure refer to the troubleshooting section of this chapter and correct the fault.
Then repeat span calibration.
13 Repeat steps 10 to 12 until all the gases that were out of tolerance are calibrated.
14 If any calibration was necessary, perform a zero calibration and repeat the Span Calibration Check.
15 Remove the calibration gas from the system and purge with room air for 10 seconds. Then check
that the values in the
Gas Analyzer Calibration window reflect the concentrations present
in room air inside the tolerance limits:
at 20.9% +/- 0.2%
O
2
at 0% +/- 0.1%
CO
2
N
O at 0% +/- 0.3%
2
Agent at 0% +/- 0.1%
If this is not the case, repeat all calibration checks and procedures.
These values are valid for the Philips M1660A Calibration Gas Mixture.
For other calibration gas mixtures use the values specified for the mixture, applying the same tolerance
limits as given in this table for the Philips mixture (for example Japanese users should calibrate the
Anesthetic GAs Module using the DOT29M1060 gas mixture of Schott Medical Products).
Disposal of Empty Calibration Gas Cylinder
1 Empty cylinder completely by pushing in the pin of the valve.
34
Page 37

Maintaining the Anesthetic Gas Module 1 Anesthetic Gas Module
2 Once the cylinder is empty, drill a hole in the cylinder
CAUTION Be careful to assure that the cylinder is completely empty before you try to drill the cylinder.
3 Write "Empty" on the cylinder and place it with your scrap metal or, if you do not collect scrap
metal for recycling, dispose of the cylinder.
Maintaining the Anesthetic Gas Module
WARNING Failure to implement a satisfactory maintenance schedule by the individual, hospital or institution
responsible for the operation of this equipment may cause equipment failure and possible health
hazards.
This chapter describes the Preventive Maintenance tasks (PMs) required to keep the Philips M1026A
Anesthetic Gas Module in good working order. PMs are performed to a timetable before problems
arise as a means to reduce failures.
Where a PM requires either a calibration or replacement procedure, you will be referred to the relevant
chapter of this guide. The PMs are listed, within a table, in ascending order of the frequency they are
performed.
All checks that require the instrument to be opened must be made by qualified service personnel.
CAUTION Take precautions when dealing with potentially contaminated parts, such as tubing and other
components of the patient circuit. Wear gloves, mask and gown while handling components that come
into contact with the patient’s exhalant gas or fluids.
Preventive Maintenance (PM) Tasks
Here is a list of the PM tasks required to ensure satisfactory operation of the Philips M1026A
Anesthetic Gas Module within its specified limits and how often they must be performed.
• Check the ventilator fan in the AGM for proper operation every 6months.
• Check the AGM’s calibration at least once every 12 months, or whenever the validity of the readings
is in doubt. Refer to Checking and Calibrating the Anesthetic Gas Module for details.
• Replace the internal Nafion tubing, room air filter, and pump filter, two internal bacterial filters,
and two watertrap manifold seals using the PM kit, every 12 months.
• Test the pump using the test procedure provided in the PM Kit every 12 months. If the test fails,
replace the pump.
• Check electrical safety (ground impedance and enclosure leakage current test) at least every 12
months.
35
Page 38

1 Anesthetic Gas Module Maintaining the Anesthetic Gas Module
Cleaning
Each time the top cover is removed from the AGM for repair or calibration, you should take the
opportunity to clean the inside of the module, as the fan may draw debris such as dust and lint into the
enclosure.
WARNING Switch off the instrument and disconnect it from the mains power supply. Take standard electrostatic
precautions. For example, wrist strap connected to electrical ground.
The user should be encouraged to periodically clean the exterior casing of the AGM. The outside of the
gas sample tubing should be cleaned before connecting to the next patient.
Replace PM Parts
Every 12 months the PM parts should be replaced for new with the PM kit (Philips Part Number
M1026-60132). The PM kit comprises an internal Nafion tubing with two internal bacterial filters,
pump filter, room-air filter, and two internal bacterial filters, and two seals for the watertrap manifold.
Internal Nafion Tubing with Bacterial Filters and manifold Seals
36
Figure 12 Removing the Nafion Tubing, Bacterial Filters and Watertrap Manifold Seals
Removal
Page 39

Maintaining the Anesthetic Gas Module 1 Anesthetic Gas Module
To remove the Nafion tubing, filters and manifold seals (refer to Figure 12):
1 Ensure that the module is switched off and isolated from the mains power supply. Remove the top
cover of the module. Check if the module needs cleaning (because of dust, lint, etc.).
2 Unscrew the cable clamps (1) holding the Nafion tubing in place on the main PC board.
3 Unscrew the bacterial filters (2) at the metal bracket.
4 Remove the Nafion tubing connections (3) from the watertrap manifold.
5 Remove the two screws (4) holding the watertrap manifold on the protector. The screws are
accessible from the rear side of the front cover through two holes provided for this purpose.
6 Pull out the two seals from the tubing connectors of the manifold using pointed tweezers; slide one
side of the tweezers between the seal and the connector, then grasp and pull.
Replacement
To replace the Nafion tubing, filters and manifold seals (refer to Figure 12):
1 Take a new seal in the tweezers and press it onto the fitting in the tubing connector. Push down on
the seal using the handle of the tweezers (or another blunt instrument), taking care not to damage
the seal, until it sits properly. Repeat with the second seal.
2 Screw the watertrap manifold onto the protector through the holes in the front cover.
3 Replace the Nafion tubing connection to the watertrap manifold. Take care to attach the tubing
with the red mark at the end to the connector with the red marking (this indicates the “drainage”
path). The gap between the end of the nafion tubing and the manifold connectors (visible through
the purple connector tubing) must be less than 1mm.
4 Replace the Nafion tubing connection to the metal bracket. Screw on the bacterial filters, again
matching the red markings.
5 Attach the cable clamps to the Nafion tubing (if not already attached) and screw the cable clamps
onto the main PC board.
37
Page 40

1 Anesthetic Gas Module Maintaining the Anesthetic Gas Module
Room-Air Filter
Figure 13 Removing and Replacing the Room-Air Filter
Removal
To remove the room-air filter (refer to Figure 13):
1 Using a cross-tipped screwdriver, remove the screw and washer (1) securing the room-air filter’s
mounting bracket.
2 Remove the pneumatic tubing (2) from the underside of the room-air filter.
3 Using a flat-tipped screwdriver, pry off the short section of tubing (4) that secures the room-air
filter to its bracket (3).
4 Remove the room-air filter from its bracket.
Replacement
To replace the room-air filter (refer to Figure 13):
1 Push the room-air filter into the locating hole provided in its bracket (3).
2 Push on the short section of tubing (4) that secures the room-air filter to its bracket.
3 Replace the pneumatic tubing (2) to the underside of the room-air filter.
4 Using a cross-tipped screwdriver, replace the screw and washer (1) securing the room-air filter’s
mounting bracket.
38
Page 41

Maintaining the Anesthetic Gas Module 1 Anesthetic Gas Module
Pump Filter
Figure 14 Removing and Replacing the Pump Filter
Removal
To remove the pump filter (refer to Figure 14):
1 Using a cross-tipped screwdriver, remove the screw securing the pump filter(1).
2 Lift the pump filter and remove the pneumatic tubing from the pump exhaust (2).
3 Press the filter out of its plastic clip and remove the tubing from the underside of the pump filter
(3).
Replacement
To replace the pump filter (refer to Figure 14):
1 Connect the open tubing end that comes with the filter to the pump exhaust (2). Ensure that the
elbow connector on the pump filter is connected to the pump exhaust.
2 Replace the pump filter and secure with the screw (1).
3 Pass the tubing through the clip and connect it to the underside of the filter and slide the pump
filter into its plastic clip (3).
4 Replace the top cover of the module.
39
Page 42

1 Anesthetic Gas Module Troubleshooting the Anesthetic Gas Module
Performance Checks
See Test and Inspection Matrix.
Other factors to maximize uptime or reduce cost of ownership:
Electromechanical devices in general have limited life expectancies and failure rates higher than devices
with only electronic components. Thus, lower cost electromechanical devices such as pumps and
solenoids should be pro-actively considered for replacement.
We recommend exchanging the pump M1026-60330 after 6000 hours.
Changing the solenoids after 3000 hours will also maximize AGM uptime.
Any change in recommended exchange intervals will be communicated via Service Notes.
Troubleshooting the Anesthetic Gas Module
This chapter provides a recommended procedure for locating and identifying faults on the Philips
M1026A Anesthetic Gas Module.
It details how to proceed when hardware or measurement related INOPs occur.
It details how to proceed when errors are flagged for:
• Failed calibration checks and procedures
• Failed diagnostic checks.
In addition, it provides flow charts for communication and measurement type problems.
Equipment needed for troubleshooting:
•Flowmeter
• Flow Split Test Kit
•PM Kit
• Multimeter
• Calibration equipment
•Tubing kit
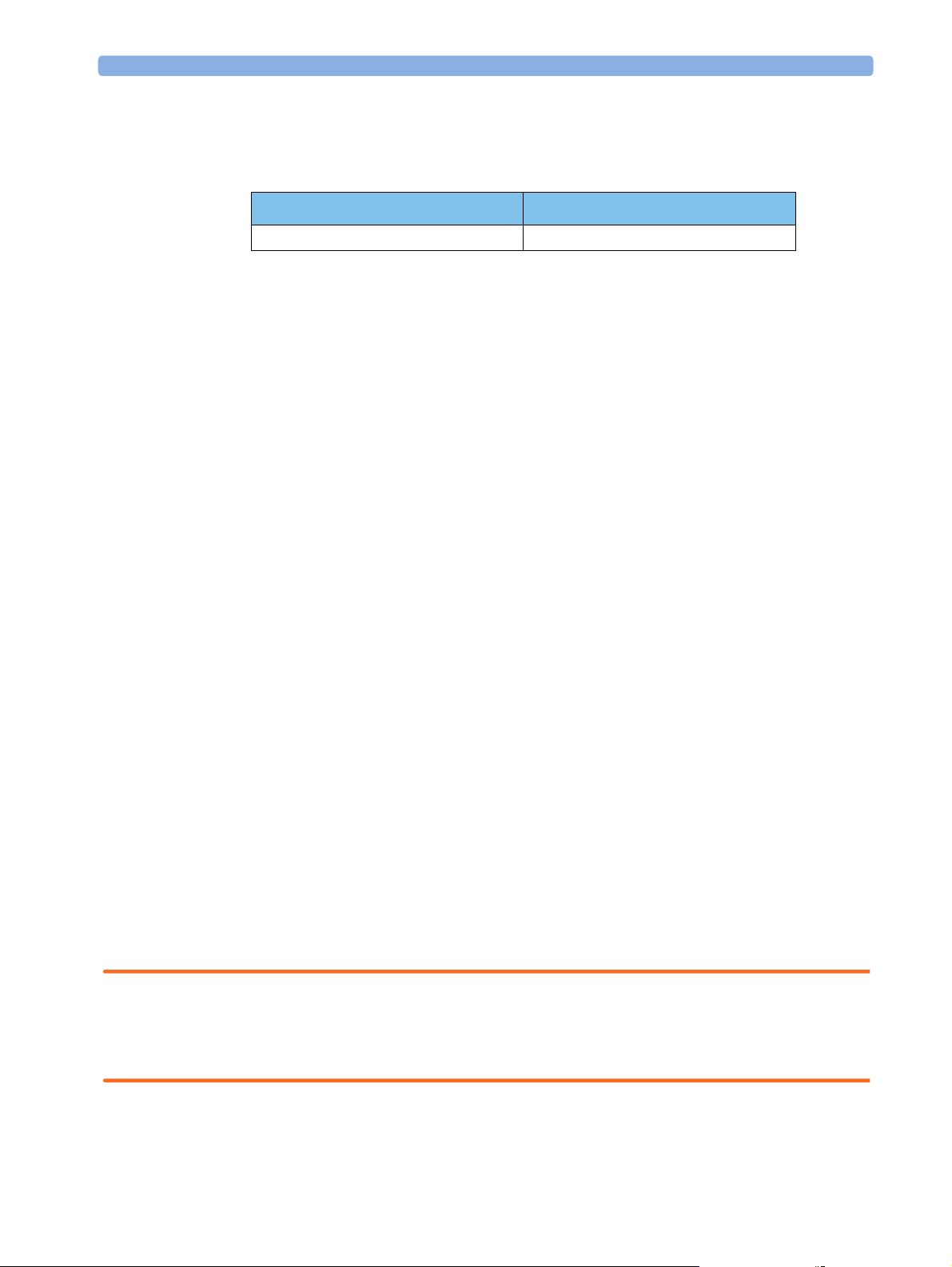
Compatibility Criteria for the AGM and the IntelliVue Monitors
Compatibility criteria can be checked in the Gas Analyzer Diagnostic Window. For compatibility with
the IntelliVue patient monitors the AGM must fulfill the follwoing requirements:
Protocol Revision: C.21.xx or greater
Agt_ID Option: 3
Assembly: 2
O
2
Flow Charts for Communication and Measurement Type Problems
The first flow chart shows three common types of problems and the identification information needed
about the AGM.
40
Page 43

Troubleshooting the Anesthetic Gas Module 1 Anesthetic Gas Module
Obtain:
–AGM Serial No.
–AGM SW Revision
Problem Call
–Options
(see lables on rearpanel and Gas
Analyzer Diagnostic
window)
AGM/IntelliVue Communication type problem
Measurement type problem
- No INOP available
A
Figure 15 Troubleshooting - Problem Identification
To access the identification information, refer to the
Diagnostic
window
Hardware related INOPs/ solid
or intermittent problems
B
See INOPs
Check Gas Analyzer
Calibration and Diagostic
window and follow the troubleshooting tables if problems are
reported.
Revision Info column of the Gas Analyzer
Figure 16 Gas Analyzer Diagnostic Window
41
Page 44

1 Anesthetic Gas Module Troubleshooting the Anesthetic Gas Module
This window gives such information as serial number, software revision and options configured:
The second flow chart continues from the first at the point A “Communication Problem”.
A
Communication
problem from the
beginning. (LED steadily
on)
Checks to perform.
Check that the Anesthesia
SW bundle #H30 is
installed on the monitor.
(Set monitor into Standby
mode and check for
“IntelliVue Anesthesia
#H30”).
If not order upgrade to
Anesthesia SW.
Check for correct RS232
config and correct MIB
port. Correct the settings if
necessary.
Check for proper physical
connections/cables (see
chapter 2).
Problem
Done
fixed
Problem
not fixed
Communication problem occurs
during operation, indicated by
flashing LED and INOP GA
EQUIP MALFUNCT.
Still communication
problem
Connect and run AGM on
other IntelliVue monitor.
Communication
problem fixed
Troubleshoot original
IntelliVue monitor
• follow troubleshooting table
Power Supply
Diagnostic
Checks
•check all internal
cables for damage /
loose fit
42
if that does not help,
replace the motherboard
Figure 17 Troubleshooting - Communication Problems
Page 45

Troubleshooting the Anesthetic Gas Module 1 Anesthetic Gas Module
The third flow chart continues from the first, from the point B “Measurement-type Problem - No
INOP”.
B
Gas measurement
accuracy problems,
Check accessories for
leaks, kinks and other
damages. Replace if
necessary.
Check connections for
blockages. If any,
remove them.
Problem
not fixed
Problem fixed
Use Calibration gas
(M1660A) in SERVICE
MODE (not in
Monitoring mode) and
perform a complete
calibration check of
suspect channels(s).
(incl. leakage and
flowrate checks)
Calibration
check failed
Calibration
check passed
Perform a full
calibration
Calibration
failed
Calibration
passed
Follow troubleshooting
table Calibration
Checks for failed
calibrations.
Automatic
O2 is not measured
agent
identification
problems.
Check if sample line is
connected. If not,
connect it.
Check on IntelliVue if
C
parameter O2 is on.
If not, turn it on.
Problem
DONE
not fixed
Follow
troubleshooting table
O2 Assembly
Diagnostic Checks.
DONE, AGM
measures correctly.
DONE, AGM measures
correctly.
Problem
fixed
DONE
Agent is not measured
Check if sample line is
connected. If not,
connect it.
Check on IntelliVue if
parameter Agent is on.
If not, turn it on.
Problem
Problem fixed
not fixed
DONE
Follow
troubleshooting table
Agent ID Assembly
Diagnostic Checks.
Disappearing
waves
D
Figure 18 Troubleshooting - Measurement Problems with No INOPS
Flow charts illustrated in Figure 19 and Figure 20 follow on from here.
43
Page 46

1 Anesthetic Gas Module Troubleshooting the Anesthetic Gas Module
The fourth flow chart continues from the third, from point C “Agent ID Problems”:
C
Check Agent-ID in Gas
Analyzer
Diagnostic window.
Agent-ID
reported
Check for correct agent
configuration (auto/
manual mode). Correct
setting is necessary.
Problem
not fixed
Problem fixed
Check if there is a
change from one agent
to another.
Agent-ID not reported
DONE
Explain that the transit time
in the anesthesia circuit is up
to 10-15 min. before the new
Check the cable
connections of the AgentID. Reconnect cables if
necessary.
Problem
Problem fixed
not fixed
Follow troubleshooting
table Agent ID
Assembly
Diagnostic Checks
DONE
agent can be detected (time
No agent
exchange
Problem fixed
Check if an agent is
administered while the
problem is observed.
Agent is
present
No agent present
Use Cal. gas in
monitoring mode.
until the old agent is washed
out, operating with low flow).
The INOP “Agent Mixture”
identifies an agent exchange
(two agents present at one
time).
DONE
Correct identification
DONE, agent-ID works properly
Halocarbon 22 must be
identified as Halothane
(they are very similar).
No correct
Follow troubleshooting table Agent
ID Assembly Diagnostic
Checks
44
Figure 19 Troubleshooting - Agent ID Problems
The fifth flow chart also continues from the third, from point D “Disappearing Waves”:
Page 47

Troubleshooting the Anesthetic Gas Module 1 Anesthetic Gas Module
D
Disappearing waves in
warmup mode.
Wait if it also occurs in
normal mode.
Yes No
Disconnect exhaust tubing
if available.
Problem
not fixed
Perform flowrate check and
pump test which is
provided in the PM kit. I f
pump test failes, replace
pump, if flow check fails
read just and calibrate
flowrates.
Problem
fixed
Problem
fixed
DONE
DONE
Problem not
fixed
Keep unit running for >90 min.
Take care that the Gas Analyzer
is not configured to go into
standby during that time. If
standby configuration has to be
altered, switch it back again
Check Gas Analyzer
Calibration and
Diagnostic window and follow
troubleshooting tables for reported
errors.
DONE
Figure 20 Troubleshooting - Disappearing Waves
Hardware Related Troubleshooting Strategy
Overall troubleshooting strategy for hardware related problems/hardware and measurement related
AGM INOPs:
1 Always perform a leak and flowrate check before continuing any other troubleshooting. If any
check fails, first fix leak and/or flowrate problem and repeat a zero calibration. Then check whether
problems still exist.
There are only two device conditions that make it impossible to perform a leak/flowrate check:
– Pump is not running:
Check for proper electrical connection and check that AGM is not in Standby Mode. If OK,
replace pump.
– INOP "GAS AN. EQUIP MALF": see “INOPs” on page 46.
2 After the first zero calibration, always check which AGM INOP’s are displayed in Monitoring
Mode. Refer to “INOPs” on page 46 where you can find a listing of possible root causes and their
45
Page 48

1 Anesthetic Gas Module Troubleshooting the Anesthetic Gas Module
corrective actions to the most common hardware and measurement related AGM INOP’s. Check
out the possible problems in the order given in the table!
3 After the first zero calibration, always check which problems are flagged in the Gas Analyzer
Diagnostic window. Troubleshoot flagged problems in the Gas Analyzer Diagnostic window
following the hierarchy given in “Problem Solving Hierarchy” on page 51 and the related
troubleshooting tables and/or troubleshoot zero calibration failures.
INOPs
Check out the possible problems in the order given in the following table.
INOP Possible Problem/Cause Corrective action
GA. NOT
AVAILABLE
GA
INCOMPATIBLE
GAEQUIP MALF Either AGM - monitor connection
GAS OCCLUSION External occlusion (inlet or exhaust
AGM not switched on. Switch on AGM
AGM not properly connected.
This version of the AGM is
incompatible with the monitor
problem, serious problem with a
subassembly or Main PC Board
problem.
Serious IR measurement head
problem.
accessories).
Internal occlusion
Weak/defective pump
Leakage between pump and flow
restrictor
Flow transducer incorrectly
connected to flow restrictor
Check physical connections.
Disconnect AGM.
Check RS232 connection, RS232
cable and MIB board of monitor. If
ok, check whether status (“OK” or
“PROBLEM”) is shown in AG Diag
Window. If yes, troubleshoot
subassemblies according hierarchy. If
status “UNKNOWN” is shown for
all assemblies for more than 4 min.
after Power On, replace main pcb.
Check IR head and replace it if
necessary, check whether Service Note
M1026A-035/038 applies.
Disconnect all external tubing/filters
and check whether occlusion
disappears.
Troubleshoot internal occlusion and
remove it
Perform pump test (provided in PM
Kit M1026-60132), replace it if
necessary.
Check pneumatic path between
pump and flow restrictor tubing for
leakages
Check that the transducer ports A
and B on the Main PC board are
connected to the correct side of the
flow restrictor.
46
Page 49

Troubleshooting the Anesthetic Gas Module 1 Anesthetic Gas Module
INOP Possible Problem/Cause Corrective action
GA ZERO FAILED Purge Flow out of tolerance. Adjust purge flow and calibrate flow.
Repeat zero calibration.
No flow calibration after flow
Perform flow calibration
adjustment.
Occlusion during zero calibration.
Solenoid 1 defective.
Measured ambient pressure does not
match with configured altitude in
ACMS Service Mode (tolerance is +/-
Remove occlusion.
Replace solenoid 1.
Verify correct altitude setting /
pressure Cal value.
If necessary, adjust it.
60 mmHg).
IR measurement head problem.
Check IR head and replace it if
necessary.
O2 ZERO FAILED O2 new zero constants out of range. Troubleshoot O2 sensor and replace it
if necessary.
AGENT IDENT
ZERO FAILED
Solenoid 2 defective Replace solenoid 2.
Agent-ID problem.
Troubleshoot Agent-ID and replace it
if necessary.
O2 EQUIP MALF O2 span failed. Check O2 span calibration. If it fails,
troubleshoot span calibration/ O
2
sensor and replace it if necessary.
O
is built in, but set to digital 45%. If O2 value is set to digital “45%” in
AGENT IDENT
MALF
XXX MEAS
DISTURBED
(XXX: N
agent or O
O, CO2,
2
)
2
2
Serious Agent-ID problem. Check Agent-ID and replace it if
Minor transient IR head problem
(Minor transient O
if XXX = O
2
2
)
sensor problem
Service Mode, replace the O
sensor.
2
necessary.
If it lasts only for a few seconds and
clears itself, NO ACTION
REQUIRED.
If it doesn't clear itself, troubleshoot
IR head/ O
sensor and replace it if
2
necessary.
GAS AN
ACCURACY ?
Flow rate error. Check flow (purge and normal),
adjust and calibrate if necessary.
No flow calibration after flow
Perform flow calibration
adjustment
Partial occlusion.
IR head problem.
Troubleshoot for occlusion.
Troubleshoot IR head and replace it if
necessary.
If it lasts only for a few seconds and
clears itself, NO ACTION
REQUIRED
O2 UNABLE TO
MEASURE
Flow rate error. Check flow (purge and normal),
adjust and calibrate if necessary
No flow calibration after flow
Perform flow calibration
adjustment
47
Page 50

1 Anesthetic Gas Module Troubleshooting the Anesthetic Gas Module
INOP Possible Problem/Cause Corrective action
O2 data not valid. Troubleshoot O2 sensor and replace it
if necessary.
CO2 UNABLE TO
MEASURE
AGT UNABLE TO
MEASURE
N2O UNABLE TO
MEASURE
CO2 span failed / CO2 data not valid. Check CO2 span calibration. If it
fails, troubleshoot span calibration/
IR head and replace it if necessary.
Agent span failed / Agent data not
valid.
N2O span failed / N2O data not
valid.
Check agent span calibration. If it
fails, troubleshoot span calibration/
IR head and replace it if necessary.
Check N2O span calibration. If it
fails, troubleshoot span calibration/
IR head and replace it if necessary.
Calibration Checks
To access the Gas Analyzer Calibration window select Gas Analyzer Calibration in the
Setup Gas Analyzer menu.
A Passed/Failed indication is displayed for the Zero and the Span calibrations. Refer
to the table below for possible causes of Failed indications, and their recommended
corrective actions.
48
Page 51

Troubleshooting the Anesthetic Gas Module 1 Anesthetic Gas Module
Calibration Checks Troubleshooting Table
Symptom Possible Cau se Corrective Action
Zero calibration
shows Failed/
Agent-ID Zero
Calibration failed.
(Agent-ID Zero
failed is only seen as
INOP in monitoring
mode)
O2 Zero calibration
shows Failed.
Solenoid or air reference
filter problem.
Check the solenoid while running a Zero
calibration, by feeling whether air is being
pulled in at the room air filter. If not, first
replace the room air filter. If the problem still
persists, replace the solenoid. If Agent-ID zero
calibration failed, check solenoid #2.
Occluded pneumatics
Check for an occlusion, such as bent or
collapsed tubing. Listen for a louder or higher
frequency pump noise. This can indicate that
the pump is working to compensate for an
internal occlusion. Replace watertrap/tubing/
filter, if necessary.
Flowrate problem.
Perform leakage check. If problem still persists,
perform flowrate check.
Flow transducer
incorrectly connected to
flow restrictor
Pump problem
Check that the transducer ports A and B on the
Main PC board are connected to the correct side
of the flow restrictor.
Block the gas inlet port and verify that the
pump is driven harder to compensate for the
reduction in flow. Perform pump test provided
in the Preventative Maintenance kit. Caution:
The instructions on cleaning apply only to the
“old-type” square shaped pump; do not clean
the “new type” round pump. If the pump fails
the test, replace it.
IR measurement head
problem
Agent-ID problem
Check out IR measurement head . Replace if
necessary.
Check out Agent-ID. Replace if necessary.
Flowrate problem. Perform leakage check. If problem still persists,
perform flowrate check.
Span problem Perform a Zero calibration followed by a Span
O
2
calibration. Check that the Span calibration is
within the accepted tolerance. If not, repeat the
Zero and Span calibration one more time.
O
sensor problem. If calibration still fails, perform the O2 check for
2
a defective sensor as described above. If the O
check fails, replace the O
sensor.
2
2
49
Page 52

1 Anesthetic Gas Module Troubleshooting the Anesthetic Gas Module
Symptom Possible Cau se Corrective Action
Span calibration
shows Failed (for
O
, N2O, CO2,
2
agent).
O2 Span calibration
shows Failed.
Zero calibration failed
for the indicated
channel.
Agent selection or
calibration values
(CalValue) incorrect
Flowrate problem.
Leakage problem.
Wrong gas applied.
Calibration reservoir bag
empty or calibration gas
canister empty.
Measurement assembly
problem.
O2 sensor problem. Check O2 sensor problem as described above.
Follow corrective actions for failed Zero
calibration described above.
Check for proper selection of Agent and
calibration values .
Check the flowrate.
Perform leakage check. Check integrity of
tubing and replace if necessary.
Check the label on the gas canister.
Check that there is enough gas available.
Check the Gas Analyzer Diagnosticwindow for
a Measurement assembly problem. If a problem
is flagged, follow corrective actions as described
in the troubleshooting tables. After that, or if no
problem was flagged, return to the Gas Analyzer
Calibration window. If the failed status is still
shown against Span Calibration, repeat the Span
calibration. After that, perform a Zero
calibration.
Diagnostic Checks
WARNING If you carry out checks with replacement parts, be aware of the high-voltage locations. Never remove
cables or sub-assemblies while the Module is powered on.
To access the Gas Analyzer Diagnostic window select Gas Analyzer Diagnostic in the Setup
Gas Analyzer
50
menu.
Page 53

Troubleshooting the Anesthetic Gas Module 1 Anesthetic Gas Module
Figure 21 Gas Analyzer Diagnostic Window
Problem Solving Hierarchy
To help identify a problem, a OK/Problem message is displayed for major subassemblies. If a
problem is displayed use the following pages to isolate the problem according to the following
hierarchy (this hierarchy overrides the sequence shown on the display):
1 Pneumatic System
2 IR Measurement Assembly (Meas. Assy)
3 Optical Path (Meas. Optic. Path)
4 O
Assembly (O2 Assy)
2
5 Agent ID Assembly (Agt-Id Assy)
6 Power Supply
7 Operating Temperature
Gas Analyzer Diagnostic window also displays the number of pump operation hours.
The
NOTE To remove the top cover, refer to the section The Top Cover.
Refer to the following tables for possible causes of
Problem indications, and their recommended
corrective actions.
51
Page 54

1 Anesthetic Gas Module Troubleshooting the Anesthetic Gas Module
Pneumatic System Diagnostic Checks
Symptom Possible Cause Corrective Action
Pneumatic Sys. shows
Problem
Weak pu m p If this Problem is flagged temporarily during
a zero calibration or purge mode this could
indicate a weak pump. Replace the pump if
problem persists
Occluded pneumatics Check for an occlusion, such as bent or
collapsed tubing, or dirty room air filter.
Listen for a louder or higher frequency pump
noise. This can indicate that the pump is
working to compensate for an internal
occlusion. Replace watertrap/tubing/filter, if
necessary.
Defective cables Check the cables for signs of damage or wear.
Check the connectors for damaged or loose
connections. If any defects are apparent,
replace the cable.
Solenoid or air reference
filter problem
Flowrate problem Perform leakage check. If problem still
Flow transducer
incorrectly connected to
flow restrictor
Pump problem Block the gas inlet port and verify that the
Defective power supply Carry out the checks for the power supply.
Defective main PC
board.
Check the solenoid while running a Zero
calibration, by feeling whether air is being
pulled in at the room air filter. If not, first
replace the room air filter. If the problem still
persists, replace the solenoid.
persists, perform flowrate check.
Check that the transducer ports A and B on
the Main PC board are connected to the
correct side of the flow restrictor
pump is driven harder to compensate for the
reduction in flow. Perform pump test
provided in the Preventative Maintenance
kit. Caution: The instructions on cleaning
apply only to the “old-type” square shaped
pump; do not clean the “new type” round
pump. If the pump fails the test, replace it.
If the checks above do not solve the problem,
replace the main PC board.
O2 Assembly Diagnostic Checks
Symptom Possible Cause Corrective Action
O2 Assy shows
Problem
52
O2 jumpers incorrectly
set
O2 sensor failed Zero/
Span calibration
Check if the O2 jumpers are correctly set.
See calibration checks.
Page 55

Troubleshooting the Anesthetic Gas Module 1 Anesthetic Gas Module
Symptom Possible Cause Corrective Action
Defective O2 sensor If two solenoids are installed, disconnect
cable of solenoid #2 (near O
sensor).
2
Go into Gas Analyzer Calibration window
Start a zero calibration to get the actual
barometric pressure reading.
Note the measured barometric pressure in
mmHg displayed in the Calibration window
Using a voltmeter, check the O
sensor
2
voltage as follows:
Connect voltmeter ground to TP1.
Measure TP8 voltage. 1% O
is
2
approximately equal to 10mV.
As the O
measurement is influenced by the
2
barometric pressure, the correct voltage must
be calculated as follows:
O
concentration of gas in mV multiplied by
2
the measured barometric pressure in mmHg
and divided by 760 mmHg.
For example, correct calculated voltage for
room air (20.9% O
) and barometric
2
pressure of 720 mmHg is: 209 mV x 720
mmHg / 760 mmHg = 198mV.
If the voltage is not within ±10% of
calculated value, proceed to adjust O
Zero
2
and Span potentiometers in the following
order:
Table continued on next page.
53
Page 56

1 Anesthetic Gas Module Troubleshooting the Anesthetic Gas Module
Symptom Possible Cause Corrective Action
Zero Adjust:
Calculate the correct voltage as described
above using the actual room air O
2
concentration and measured barometric
pressure. Adjust RV2 potentiometer on the
PC Board until the voltmeter reads the
calculated voltage ±1mV. You can also use a
gas which does not contain O
and adjust
2
RV2 potentiometer on the PC Board until
the voltmeter reading is 0 mV ±1mV. The
gas must be applied at the room air filter.
Span Adjust:
Apply Philips Calibration Gas M1660A
(containing 52% O
) to the room air filter
2
(connect the calibration tubing to the open
end of the room air filter). Calculate the
correct voltage as described above using the
specific O
concentration and measured
2
barometric pressure. Adjust RV1 until the
voltmeter reads the calculated voltage ±10
mV. Disconnect the calibration tubing from
the room air filter.
Reconnect cable of solenoid #2 if it was
disconnected.
If these adjustments are not successful, check
the pneumatic system for leakages If the
problem still persists, replace the O
sensor.
2
If any adjustment was necessary, perform a
Zero calibration followed by an O
Span
2
calibration.
Defective cables. Check the cables connecting the O2
assembly and the main PC board for signs of
damage or wear. Check the connectors for
damaged or loose connections. If any defects
are apparent, replace the cable.
Defective power supply Carry out the checks for the power supply .
Defective main PC
board.
If the checks above do not solve the problem,
replace the main PC board.
54
Page 57

Troubleshooting the Anesthetic Gas Module 1 Anesthetic Gas Module
Optical Path Disgnostic Checks
Symptom Possible Cause Corrective Action
MeasOpticPath shows
Problem
Defective or
contaminated sample
cell
Defective IR
measurement assembly
head
Defective power supply
Defective main PC
board
Remove the sample cell and visually check it
to see if it is contaminated. The inside of the
cell should be smooth and shiny. If not,
replace the sample cell. Wait after the first
Zero Calibration to see whether the problem
disappears.
If problems are cleared after warm-up, but
were present during warm-up, let the AGM
run for at least 90 minutes after Power On to
allow the unit to reach the 90 minutes zero.
This is a special zero calibration where "new"
zero constants for the next warm-up phase
are stored. This prevents that problems are
flagged during the next warm-up phase
Carry out the checks for the IR measurement
assembly head . With the replacement head
connected, check that Optical Path problem
is no longer flagged. If the problem is gone,
use a new head. If not, continue checks as
described below.
Carry out the checks for the power supply .
If the checks above do not solve the problem,
replace the main PC board.
55
Page 58

1 Anesthetic Gas Module Troubleshooting the Anesthetic Gas Module
IR Measurement Assembly Diagnostic Checks
Symptom Possible Cause Corrective Action
Meas. Assy shows
Problem
Defective IR
measurement assembly
head
Defective power supply
Defective cables
Defective main PC
board
Do the following IR measurement assembly
head checks:
Check whether Service Note
M1026A-035/038 applies
Remove the sample cell (see Repairing the
Anesthetic Gas Module) and visually check it
to see if it is contaminated. The inside of the
cell should be smooth and shiny.
Perform flow and Span gas calibration (in
order to store new reference values)
Using a voltmeter, check the IR source
voltage as follows:
Connect the voltmeter ground to TP1.
Measure TP6 voltage. It should be 7.87V
±20mV.
If this voltage is within limits, proceed to the
next check. If not, adjust the potentiometer
R178 to the required value. If the
adjustment is not possible, replace the
measurement assembly head.
Power off. Connect a replacement head with
the ribbon cable and reconnect the tubing.
Turn power back on and see if the Meas.
Assy still shows Problem. If the message is
gone, replace the head. If the problem
persists, continue checking.
Carry out the checks for the power supply .
Check the cables connecting the
measurement head and the main PC board
for signs of damage or wear. Check the
connectors for damaged or loose
connections. If any defects are apparent,
replace the cable.
If the checks above do not solve the problem,
replace the main PC board.
56
Page 59

Troubleshooting the Anesthetic Gas Module 1 Anesthetic Gas Module
Agent ID Assmebly Diagnostic Checks
Symptom Possible Cause Corrective Action
Agt-ID. Assy shows
Problem
Wrong Ag e n t-ID
software revision
Defective agent ID
head.
Defective power supply
Defective cables
Defective main PC
board
Check for correct Agent-ID revision in AG
Revision window, item:
Agt-ID SW
If necessary, replace Agent-ID EPROM.
Do the following agent ID head checks:
Using a voltmeter, check the IR source
voltage at the main PC board as follows:
Connect the voltmeter ground to TP1.
Measure TP11 voltage. It should be 7.92V
±20mV.
If this voltage is within limits, proceed to the
next check. If not, adjust the potentiometer
R180 to the required value. If adjustment is
not possible, replace the Agent-ID head.
Power off. Connect a replacement head with
the ribbon cable and reconnect tubing. Turn
power back on and see if the Agt.-Id still
shows Problem. If the message is gone,
replace the head. If the problem persists,
continue checking. Power Supply Diagnostic
Checks
Carry out the checks for the power supply .
Check the cables connecting the
measurement head and the main PC board
for signs of damage or wear. Check the
connectors for damaged or loose
connections. If any defects are apparent,
replace the cable.
If the checks above do not solve the problem,
replace the main PC board.
57
Page 60

1 Anesthetic Gas Module Troubleshooting the Anesthetic Gas Module
Power Supply Diagnostic Checks
Symptom Possible Cause Corrective Action
Power Supply shows
Problem
Weak pu m p If this Problem is flagged temporarily during
a zero calibration or purge mode this could
indicate a weak pump. Replace the pump if
problem persists
Defective power supply
Defective cables
Defective main PC
board
Using a voltmeter, check the power supply
voltages at the main PC board. The power
supply connectors should carry the following
voltages:
TP14: +12V ±600 mV
TP15: +5V ±250 mV
TP16: -12V ±600 mV
TP17: +12V ±600 mV
TP18: Analog Ground
If any of the above voltages are out of limits,
carry out the checks again while
systematically disconnecting the
subassemblies (remember to power off the
Module before removing cables and
subassemblies). If the voltage(s) are still out
of limits, replace the power supply.
Check the cables connecting the
measurement head and the main PC board
for signs of damage or wear. Check the
connectors for damaged or loose
connections. If any defects are apparent,
replace the cable.
If the checks above do not solve the problem,
replace the main PC board.
58
Page 61

Troubleshooting the Anesthetic Gas Module 1 Anesthetic Gas Module
Operating Temperature Diagnostic Checks
Symptom Possible Cause Corrective Action
Oper. Temp. shows
Problem
Defective fan Check that the fan runs smoothly and check
Insufficient air
circulation due to fan
working inefficiently
Operating environment
for the module falls
outside of specified
limits
Defective IR
measurement assembly
head
Defective agent ID
head
Defective power supply
Defective main PC
board.
Test Points, Connectors and Jumpers
its cable. If necessary, replace fan or cable.
Check the fan aperture for blockages or dust
on the fan blade or guard. If necessary,
unblock or clean the fan aperture.
Do not operate the module in such an
environment.
Follow its corrective action.
Follow its corrective action
Follow its corrective action
If the checks above do not solve the problem,
replace the main PC board.
Test Points
The following table lists the test points; also refer to Figure 22.
Tes t Po in t Description Tol e r an c e Va lu e ( ± )
TP1 Analog Gnd 1 (AGND1)
TP2 Analog Dark Level Clamp (10DLCL)
TP3 M1026A Preamp Signal 400mVpp ±30mv
TP4 M1026A A/D Converter Input
TP5 AC Pump Motor Reference (not used)
TP6 IR source voltage for IR measurement assembly head
(R178)
TP7 Thermal Electric Cooler Drive Voltage to M1026A
Head (TE+)
TP8 Oxygen Transducer Signal Output (O2SIG). Signal
varies with O
TP9 Analog Ground 2 (AGND2)
TP10 M1026A A/D Converter Input
concentration.
2
7.87 V ±20mv
250mV ±100mV (after at
least 15 min. warm-up)
Examples: 20.8% O2 is
approx. 208mV, 50.0%
O
is approx. 500mV
2
1
59
Page 62

1 Anesthetic Gas Module Troubleshooting the Anesthetic Gas Module
Tes t Po in t Description Tol e r an c e Va lu e ( ± )
TP11 IR source voltage for agent ID head (R180) 7.92 V ±20mV
TP13 Isolated Ground for isolated RS-232
communications with the Host Computer via J14
TP14 +12VHP +12V ±600mV
TP15 +5V +5V ±250mV
TP16 -12V -12V ±600mV
TP17 +12V +12V ±600mV
TP18 Analog Ground 3 (AGND3)
1. Measurement requires an oscilloscope.
Connectors
The following table lists the connectors on the main PCB.
Connector Description
J1 IR Measurement Assembly Head
J2 Agent ID Head
J3 Factory use only
J4 Factory use only
J5 DC Power: pins 1&2: +12VHP, pins 3&4: +5V GND (DGND), pin 6:
AGND, pin 7: AGND, pin 8: -12V, pin 9: +12V
J6 PC Board connector (also for NVRAM data transfer)
JP7 Top cover jumper
J8 Pump driver for DC pump and AC pump (DC PUMP/AC PUMP)
J10 Oxygen Transducer Connection
J13 Factory use only
J14 Connection to Host Computer for communications, RS-232
J15 Fan power (FAN1)
J16 Not used
J17 Power LED
J19 Factory use only
J20 Factory use only
J21 O2 Solenoid (SOL2)
J22 Optional Front Panel I/O
1. Use DC pump only.
1
Jumpers
60
The following table shows the correct jumper settings for the O2 sensor (if installed).
Page 63

Troubleshooting the Anesthetic Gas Module 1 Anesthetic Gas Module
Jumper Paramagnetic O2 Sensor No O2 Sensor
10IRQ1 OPEN OPEN
10IRQ2 OPEN OPEN
10IRQ3 CLOSED OPEN
The top cover Jumper, JP7, must always be closed, whether or not the top cover is connected.
Main EPROM
Agt-ID EPROM
U11
Figure 22 Potentiometers, Jumpers, and Test Points
Legend:
1 Flowrate potentiometers (R125, Purge flow and R126, Normal flow)
2 IR Source potentiometers (R178, R180)
3O
jumper (10IRQ)
2
4 Top cover jumper (JP7)
5EPROMs
6 Microprocessors
7Test pins
61
Page 64

1 Anesthetic Gas Module Repairing the Anesthetic Gas Module
8Flow transducer
9 Top-cover PC board connector / NVRAM transfer
Repairing the Anesthetic Gas Module
Introduction
This section contains detailed removal and replacement procedures for all field-replaceable units in the
Philips M1026A Anesthetic Gas Module.
CAUTION Use caution when handling tubing and other components of the patient circuit. Wear gloves, mask and
gown while handling components that come into contact with the patient’s exhalant gas or fluids.
Before you can remove any of these field replaceable units, you first need to remove the top cover of the
Anesthetic Gas Module. The procedure for this is described in “The Top Cover” on page 64.
WARNING Switch off the instrument and disconnect it from the mains power supply. Take standard electrostatic
precautions. For example, a wrist strap connected to electrical ground.
Figure 23 shows the field-replaceable units for the Anesthetic Gas Module. These are:
•Top Cover
• Infrared (IR) Measurement Assembly (2)
•Sample Cell
•Solenoid Valve #1 (7)
•Power Supply Unit (1)
• Main PC Board (13)
•O
Paramagnetic Assembly (11)
2
• Agent Identification Head (9)
•Pump (3)
•Fan (5)
• Solenoid Valve #2 (10)
•Top Cover PC Board (15)
•PM Kit comprising:
–Room Air Filter (6)
– Nafion Tubing and internal bacterial filters(12)
– Watertrap manifold seals
– Pump Filter (4)
62
• Watertrap Manifold and Protector
Page 65

Repairing the Anesthetic Gas Module 1 Anesthetic Gas Module
•Power fuses
Figure 23 Main Subassemblies (showing O
of the Anesthetic Gas Module
paramagnetic sensor with integrated pc board)
2
63
Page 66

1 Anesthetic Gas Module Repairing the Anesthetic Gas Module
The Top Cover
Removal
To remove the top cover (refer to Figure 24 and Figure 25):
1 Make sure that the module is switched off and isolated from the mains power supply.
2 Remove the watertrap from the front of the cover (to avoid fluids in the watertrap reaching the
water fuses when the cover is tipped).
3 Using a cross-tipped screwdriver, remove the 7 screws (1) securing the top cover to the body. These
screws are located at the rear of the module and on the sides.
4 Slide the top cover (2) forward approximately 4cm.
NOTE At this stage, the top cover is still connected to the main PC board by a flat cable and the internal
Nafion tubing.
5 Carefully lift the top cover until the flat cable connector (3) leading to the main PC board is
accessible.
6 Remove the flat cable connector (3) from the top cover.
7 If necessary, remove the internal Nafion tubing.
8 Remove the top cover from the module.
Replacement
To replace the top cover (refer to Figure 26 and Figure 27):
1 Ensure that the module is switched off and isolated from the mains power supply.
2 Reconnect the flat cable connector (3).
3 If necessary, reconnect the internal Nafion tubing, following the given markings.
4 Carefully lower the top cover (4) onto the chassis (5).
5 Slide the top cover towards the rear of the module until the locating holes on the top cover are
6 Using a cross-tipped screwdriver, replace the 7 screws (1) securing the top cover to the module. The
aligned with the threaded bores in the module.
locating holes are under the top cover at the rear and sides of the module.
64
Page 67

Repairing the Anesthetic Gas Module 1 Anesthetic Gas Module
1
600VA max.
100-240V
50-60 Hz
brear2d.tif
MONITOR
RS 232
T1.6 H 250V
60/140
Figure 24 Top Cover Securing Screws for the Anesthetic Gas Module
Figure 25 Sliding Off the Top Cover of the Anesthetic Gas Module
65
Page 68

1 Anesthetic Gas Module Repairing the Anesthetic Gas Module
Figure 26 Sliding On the Top Cover of the Anesthetic Gas Module
3
Figure 27 Main PC Board Connector to the Top Cover of the Anesthetic Gas Module
Lifting the IR Measurement Mounting Bracket
Several of the field replaceable subassemblies are mounted on the IR measurement mounting bracket,
which is a subassembly of the Anesthetic Gas Module, as shown in Figure 28.
66
Page 69

Repairing the Anesthetic Gas Module 1 Anesthetic Gas Module
The IR assembly mounting bracket must first be lifted and stood on end before any of the following
units can be removed or replaced:
• IR measurement assembly and sample cell.
•Solenoid valve #1.
Removal
To lift the IR Measurement mounting bracket (refer to Figure 28 and Figure 29):
1 Ensure that the module is switched off and isolated from the mains power supply. Remove the top
cover of the module.
2 Remove the cables from the cable clip.
3 Remove the connection from the gas exhaust (1).
4 Using a cross-tipped screwdriver, remove the four screws and lock washers (2) securing the IR
Measurement mounting bracket to the module.
5 Lift the IR Measurement mounting bracket and stand it carefully on its end, so that the ribbon
cables are at the bottom. The securing screws on the underside are now accessible, as shown in
Figure 29.
Replacement
To replace the IR Measurement mounting bracket (refer to Figure 28 and Figure 29):
1 Ensure that the module is switched off and isolated from the mains power supply.
2 Lay the IR Measurement mounting bracket carefully onto its 4 spacers so that the locating holes
are aligned with the threaded bores.
3 Make sure that the dampener (3), cable clamp (4) and bracket with flow restrictor (5) are in place.
Using a cross-tipped screwdriver, fit the four screws and lock washers (2) securing the IR
Measurement mounting bracket to the module.
4 Reconnect the pneumatic tubing to the gas exhaust (1).
5 Replace the power connection to the pump (where applicable) and secure the cables with the clip.
6 Replace the top cover of the module.
NOTE After replacing the IR Measurement mounting bracket, check that all flat-cable connectors are firmly
seated and show no signs of damage.
67
Page 70

1 Anesthetic Gas Module Repairing the Anesthetic Gas Module
Figure 28 Lifting the IR Measurement Mounting Bracket
68
Page 71

Repairing the Anesthetic Gas Module 1 Anesthetic Gas Module
Figure 29 Underside of the IR Measurement Mounting Bracket
Infrared Measurement Assembly Head
Transferring NVRAM Data to a Replacement Head
When you replace an IR measurement head, you need to transfer its data to the replacement head. The
data is stored in non-volatile RAM (NVRAM) on the head and includes:
• System serial number
• Pump hours
• Flow rate limits
• User span constant for all channels
•User O
•O
•IR source voltage
The NVRAM transfer board (NTB) reads data from the old head and transfers it to the replacement
head. The NTB is included with each replacement head.
Procedure for Transferring Data
1 Disconnect the Anesthetic Gas Module from the monitor.
calibration values
2
delay cycles
2
2 Turn off power to the Anesthetic Gas Module.
69
Page 72

1 Anesthetic Gas Module Repairing the Anesthetic Gas Module
Remove the Anesthetic Gas Module top cover and disconnect it from the Main PC board.
3
4 Connect the 40-pin cable of the NTB to the 40-pin connector of the new replacement IR
Measurement head.
5 Connect the 10-pin cable of the NTB to the top cover connector (J6) on the Main PC board.
6 Power up the Anesthetic Gas Module and observe the LED on the NTB.
7 For about the first 5 seconds the LED on the NTB will be amber. Whenever the LED is amber, the
NTB is processing information and you must stand by until the LED changes color again. During
these first 5 seconds, the NVRAMs of both the old and the new measurement heads are being read
and checked. If the LED changes to a solid green color, the NVRAM transfer process can begin.
Please skip to step 8 if the LED is green.
When either NVRAM cannot be read, it may take up to one minute before the LED changes color
and you will observe one of two error conditions:
– If the LED changes to a solid red color, a problem reading the old measurement head has
occurred. Turn off the power and check all connections. Make sure the ribbon cables are not
broken and correctly seated. Repeat the procedure staring with step 6.
If the LED is still on red, proceed with the installation of the new analyzer head regardless. The
NVRAM transfer will not be possible, but the replacement head has default information for
pump hours and no serial number. However, before installing the new measurement head, you
need to verify that the head is functional:
a. Replace the old measurement head with the new one.
b. Repeat the NVRAM transfer procedure from step 6.
If the LED blinks alternately red and green, the head is functional and you can continue with the
installation of the new head. If the LED is solid red, either the new head and/or the cable from
the head to the main PC board is defective. In this case you must replace the head or the cable or
both.
NOTE When installing a new measurement head and using the default NVRAM data, a flow rate calibration
must be performed because no flow rates will be transferred. If no flow rate calibration is performed, a
problem with the pneumatic system will be flagged during Anesthetic Gas Module operation.
– If the LED blinks alternately red and green, a problem occurred reading the new analyzer head.
Turn off the power and check all connections. Make sure the ribbon cables are not broken and
correctly seated. Repeat the procedure staring with step 6.
If the LED is still blinking red and green you need to check whether the failed NVRAM transfer is
due to a defective NTB and/or cable connection:
a. Replace the old measurement head with the new one.
b. Repeat the NVRAM transfer procedure from step 6.
If the LED is solid red, the new measurement head is defective. In this case you must use a new
replacement measurement head and return to step 4. If the LED blinks alternately green and red,
the NTB and/or the attached cables are defective. In this case you need to use a new NTB, or
you can install the new measurement head with the default NVRAM data.
70
Page 73

Repairing the Anesthetic Gas Module 1 Anesthetic Gas Module
Once the LED is on green, you can begin the NVRAM transfer process by pressing the momentary
8
push button switch on the NTB. The LED will change to amber for about 5 seconds, followed by
solid green indicating a good transfer of NVRAM data.
If you observe a blinking red LED, no transfer or a bad transfer of NVRAM data occurred. Proceed
with the installation of the new measurement head regardless. The NVRAM transfer will not be
possible, but the replacement head has default information for pump hours and no serial number.
However, a flow rate calibration must be performed because no flow rates will be transferred. If no
flow rate calibration is performed, a problem with the pneumatic system will be flagged during
Anesthetic Gas Module operation.
9 If step 8 was successful, the Anesthetic Gas Module can now be powered off. The NTB can be
disconnected and the old measurement head removed and replaced with the new head (see removal
and replacement procedure below).
10 Reconnect the Anesthetic Gas Module to the monitor.
NOTE When returning the defective measurement head for repair, make sure to return the NVRAM transfer
board with the head.
Instructions for the transfer procedure are also included with the NTB.
Removal
To remove the IR measurement assembly head (refer to Figure 30 and Figure 31):
1 Remove the flat-cable (1) connector from the main PC board.
2 Remove the pneumatic connections (2) from the sample cell, which are located on top of the IR
measurement assembly head.
3 Remove the pressure transducer connection (3) located on the side of the IR measurement
assembly head.
4 Stand the IR measurement mounting bracket on end (refer to “Lifting the IR Measurement
Mounting Bracket” on page 66).
5 Using a cross-tipped screwdriver, remove the 3 screws (4) securing the IR measurement assembly
head to the IR measurement mounting bracket.
6 Remove the IR measurement assembly head carefully from the IR measurement mounting bracket.
Replacement
To replace the IR measurement assembly head (refer to Figure 30 and Figure 31):
1 Place the IR measurement assembly head in the IR measurement mounting bracket so that the
threaded bores on the head align with their corresponding locating holes on the IR measurement
mounting bracket.
2 Using a cross-tipped screwdriver, replace the three screws (4) securing the IR measurement
assembly head to the IR measurement mounting bracket.
3 Replace the IR measurement mounting bracket (refer to “Lifting the IR Measurement Mounting
Bracket” on page 66).
4 Replace the transducer reference connection (3) located on the side of the IR measurement
assembly head.
71
Page 74

1 Anesthetic Gas Module Repairing the Anesthetic Gas Module
Replace the pneumatic connections (2) to the sample cell (located on top of the IR measurement
5
assembly head).
NOTE Check that all tubing is tightly connected and show no signs of damage.
6 Replace the flat-cable (1) connector to the main PC board.
NOTE After replacing the IR measurement assembly head, check that all flat-cable connectors are firmly
seated and show no signs of damage.
Now perform the performance checks described in the “Test and Inspection Matrix” on page 94.
72
Figure 30 Removing the IR Measurement Assembly Head
Page 75

Repairing the Anesthetic Gas Module 1 Anesthetic Gas Module
Sample Cell
Removal
To remove the sample cell (refer to Figure 32, Figure 33, Figure 34 and Figure 35):
1 Stand the IR measurement mounting bracket on end, towards the main PC board (refer to “Lifting
2 Remove the pneumatic connections (1) from the sample cell, which are located on top of the IR
3 Using a cross-tipped screwdriver, remove the four screws (2) securing the sample cell cover plate
4 Lay the IR measurement assembly head flat and, using a flat-tipped screwdriver, apply pressure
5 Carefully withdraw the sample cover and bracket (5) from the IR measurement head.
6 Using a cross-tipped screwdriver, remove the screw (6) securing the clamping plate (7) to the
7 Remove the sample cell (9).
Figure 31 Locating Screws for the IR Measurement Assembly Head
the IR Measurement Mounting Bracket” on page 66).
measurement assembly head.
and bracket (3) from the IR measurement assembly head. Retain these parts for later replacement.
from above to the overlapping part (4) of the sample cell cover, and pry it off.
sample cell bracket (8).
Replacement
To replace the sample cell (refer to Figure 32, Figure 33, Figure 34 and Figure 35):
73
Page 76

1 Anesthetic Gas Module Repairing the Anesthetic Gas Module
Position the sample cell (9) onto its bracket (8) and hold it in place with the clamping plate (7).
1
2 Using a cross-tipped screwdriver, replace the screw (6) securing the clamping plate to the bracket.
Before tightening the screw, ensure that the pipes to the sample cell are aligned parallel with the
sides of the bracket.
NOTE Make sure the temperature sensor has not slipped out of its hole. This can prevent the bracket from
being pushed home.
3 Insert the sample cell bracket and cover (5) into the base of the IR measurement assembly head.
Push the bracket home so that the surface of the cover plate is flush with the base of the IR
measurement head. The two gas tubes should now protrude from the holes (1) on top of the IR
measurement head.
4 Using a cross-tipped screwdriver, replace the four screws (2) securing the sample cell cover plate
and bracket (3) to the IR measurement assembly head.
5 Replace the pneumatic connections (1) to the sample cell, which are located on top of the IR
measurement head.
NOTE Check that all tubing is tightly connected and show no signs of damage.
6 Replace the IR measurement mounting bracket (refer to “Lifting the IR Measurement Mounting
Bracket” on page 66).
NOTE After replacing the sample cell, check that all flat-cable connectors are firmly seated and show no signs
of damage.
Now perform the performance checks described in the “Test and Inspection Matrix” on page 94.
74
Page 77

Repairing the Anesthetic Gas Module 1 Anesthetic Gas Module
Figure 32 Removing the Sample Cell Pneumatic Connections
75
Page 78

1 Anesthetic Gas Module Repairing the Anesthetic Gas Module
Figure 33 Removing the Sample Cell Cover
76
Figure 34 Extracting the Sample Cell Bracket
Page 79

Repairing the Anesthetic Gas Module 1 Anesthetic Gas Module
Figure 35 Replacing the Sample Cell
Solenoid Valve #1
Removal
To remove solenoid valve #1 (refer to Figure 36 and Figure 37):
1 Remove the pneumatic tubing (1) from solenoid valve #1.
2 Remove the power connector (2) from the main PC board.
3 Pry the twisted pair supplying power from the solenoid valve out of the cable clip (3).
4 Using a cross-tipped screwdriver, remove the three screws (4) securing the IR measurement
assembly head.
5 Lift the IR measurement head slightly so that the screws (5) securing the solenoid valve are
accessible.
6 Using a cross-tipped screwdriver, remove the two screws securing solenoid valve #1 to the IR
measurement mounting bracket.
7 Carefully remove solenoid valve #1 and its cable from the IR measurement mounting bracket.
Replacement
To replace solenoid valve #1 (refer to Figure 36 and Figure 37):
77
Page 80

1 Anesthetic Gas Module Repairing the Anesthetic Gas Module
Lift the IR measurement assembly head slightly so that the threaded bores (5) on the mounting
1
bracket for the solenoid valve are accessible.
2 Carefully position Solenoid Valve #1 so that its locating holes align with the threaded bores on the
mounting bracket.
3 Using a cross-tipped screwdriver, replace the two screws (5) securing Solenoid Valve #1 to the IR
measurement mounting bracket.
4 Snap the twisted pair from the solenoid valve into the cable clip (3) securing the twisted pairs that
connect the IR measurement assembly head to the main PC board.
5 Replace the connection (2) to the main PC board.
6 Replace the pneumatic tubing (1) to Solenoid Valve #1.
NOTE Check that all tubing is tightly connected and show no signs of damage.
After replacing Solenoid Valve #1, check that all flat-cable connectors are firmly seated and show no
signs of damage.
7 Using a cross-tipped screwdriver, replace the three screws (4) securing the IR measurement
assembly head.
8 Replace the IR measurement assembly mounting bracket (refer to “Lifting the IR Measurement
Mounting Bracket” on page 66).
Now perform the performance checks described in the “Test and Inspection Matrix” on page 94.
78
Figure 36 Removing the Solenoid Valve #1
Page 81

Repairing the Anesthetic Gas Module 1 Anesthetic Gas Module
Figure 37 Replacing the Solenoid Valve #1
Power Supply Unit
Removal
To remove the power supply unit (refer to Figure 38):
1 Ensure that the module is switched off and isolated from the mains power supply. Remove the top
cover of the module.
2 Remove the ac power connector (1) from the power supply unit.
3 Remove the power connector (2) from the main PC board.
4 Using a cross-tipped screwdriver, remove the four screws (3) securing the power supply unit to its
mounting.
5 Remove the power supply unit.
Replacement
To replace the power supply unit (refer to Figure 38):
1 Ensure that the module is switched off and isolated from the mains power supply.
2 Carefully place the power supply unit so that its locating holes are aligned with the threaded bores
in the mounting on the module.
3 Using a cross-tipped screwdriver, replace the four screws (3) securing the power supply unit to its
mounting.
4 Connect the power connector (2) to the main PC board.
79
Page 82

1 Anesthetic Gas Module Repairing the Anesthetic Gas Module
Connect the ac power connector (1) to the power supply unit.
5
6 Replace the top cover of the module.
Now perform the performance checks described in the “Test and Inspection Matrix” on page 94.
Figure 38 Removing and Replacing the Power Supply Unit
Main PC Board
Removal
To remove the main PC board (refer to Figure 39):
1 Ensure that the Module is switched off and isolated from the mains power supply. Remove the top
cover of the module.
2 Remove the pneumatics tubing from the pressure transducer (1).
3 Remove the main PC board connector (2) from the power supply unit.
4 Remove the power connectors (3) that connect the main PC board to the fan, solenoid valve #1,
pump and solenoid valve #2.
5 Remove the flat-cable connector (4) from the IR measurement head.
6 Remove the flat-cable connector (5) from the RS232 connector.
7 Remove the flat-cable connector (6) from the agent identification head.
80
Page 83

Repairing the Anesthetic Gas Module 1 Anesthetic Gas Module
If O2 sensor is present, remove the flat-cable connector (7) from the small O2 sensor PC board (or
8
directly from the O
9 Remove the connector (9) from the power LED.
10 Using a cross-tipped screwdriver, remove the cable clamps (12).
11 Using a cross-tipped screwdriver, remove the 6 screws (10) securing the main PC board to its
sensor, for sensors with integrated PC board).
2
mounting on the module.
12 Carefully remove the main PC board.
Replacement
To replace the main PC board (refer to Figure 39):
1 Ensure that the module is switched off and isolated from the mains power supply.
2 Carefully place the main PC board on its mounting in the Anesthetic Gas Module so that the 6
locating holes are aligned with the threaded bores.
3 Using a cross-tipped screwdriver, replace the 6 screws and washers (10) securing the main PC
board to its mounting, and replace the cable clamps.
4 Replace the connector (9) to the power LED.
5 If the O
directly to the O
6 Replace the flat-cable connector (6) to the agent ID head.
7 Replace the flat-cable connector (5) to the RS232 connector.
8 Replace the flat-cable connector (4) to the IR measurement head.
9 Replace the power connectors (3) that connect the main PC board to the fan, pump, solenoid #1
sensor is present, replace the flat-cable connector (7) to the O2 sensor PC board (or
2
sensor). Verify the O2 jumper settings.
2
and solenoid #2.
10 Replace the main PC board connector (2) to the power supply unit.
11 Refit the pneumatic tubing to the pressure transducer (1). Check that all tubing is tightly
connected and show no signs of damage.
12 Replace the top-cover cable (8) to the PC board.
NOTE After replacing the main PC board, check that all flat-cable connectors are firmly seated and show no
signs of damage.
Verify the O
jumper settings as described in “Jumpers” on page 60.
2
Make a flowrate check.
13 Replace the top cover of the module. Ensure that the top cover jumper (JP7) is set to “closed”.
14 Do a configuration check in service mode (Agent-ID, O
sensor).
2
Now perform the performance checks described in the “Test and Inspection Matrix” on page 94.
81
Page 84

1 Anesthetic Gas Module Repairing the Anesthetic Gas Module
O2 Sensor
Removal
Figure 39 Removing the Main PC Board
The O2 sensor is always replaced together with the small PC board that controls it. The newer O2
sensors have the board integrated inside the sensor housing.
To remove the O2 sensor and its PC board follow the steps marked (a) and to remove the O2 sensor
with integrated PC board follow the steps marked (b) (refer to Figure 40 and Figure 41):
1 Ensure that the module is switched off and isolated from the mains power supply. Remove the top
cover of the module.
2 Remove the 3 pneumatic connections (1) from the O
3 Remove the flat cable connector (2) from the PC board that controls the O
4 Remove the flat cable connector (2) from the connector on the top of the O
5 Release the clips (3) securing the PC board to its mounting.
6 Using a cross-tipped screwdriver, remove the two screws and washers (4) securing the O
sensor.
2
sensor.
2
sensor housing.
2
2
sensor to
its mounting brackets.
7 Carefully remove the O
sensor [(b) along with its PC board.]
2
82
Page 85

Repairing the Anesthetic Gas Module 1 Anesthetic Gas Module
NOTE
If you are not operating O2, remove the appropriate jumper.
Replacement
To replace the O2 sensor and its PC board follow the steps marked (a) and to replace the O2 sensor
with integrated PC board follow the steps marked (b) (refer to Figure 40 and Figure 41):
1 Ensure that the module is switched off and isolated from the mains power supply.
2 Carefully place the O
threaded bores.
3 Press the PC board onto its mounting until it clicks into place, and is firmly secured by the clips
(3).
NOTE Make sure that the PC board is inserted so that the smaller connector points toward the main PC
board.
1 Place the bracket with the internal bacterial filters (5) onto the mounting bracket, aligning the
locating holes.
2 Using a cross-tipped screwdriver, replace the two screws and washers (4) securing the O
its mounting.
3 Replace the flat cable connector (2) that connects the main PC board to the PC board that controls
sensor.
the O
2
4 Replace the flat cable connection (2) to the top of the O
sensor on its mounting so that the locating holes are aligned with the
2
sensor housing.
2
sensor to
2
NOTE Verify the O
jumper settings.
2
5 Replace the 3 pneumatic connections (1) to the O
sensor inlets (upper and lower connections). Connect the single tubing to the outlet
the O
2
(middle connection). Check that all tubing is tightly connected and show no signs of damage.
NOTE After replacing the O
connectors are firmly seated and show no signs of damage.
6 Replace the top cover of the module.
Now perform the performance checks described in the “Test and Inspection Matrix” on page 94.
sensor. Connect the tubing with the T-piece to
2
sensor and, where applicable, its controlling PC board, check that all flat-cable
2
83
Page 86

1 Anesthetic Gas Module Repairing the Anesthetic Gas Module
Figure 40 Removing the Connections of the O2 Sensor
84
Figure 41 Removing the O
Sensor with its PC Board
2
Page 87

Repairing the Anesthetic Gas Module 1 Anesthetic Gas Module
Figure 42 Layout showing O2 sensor with Integrated PC Board
Figure 43 Location of Adjustment Potentiometers on O
Agent Identification Head
Removal
To remove the agent ID head (refer to Figure 44):
Sensor with Integrated PC Board
2
1 Ensure that the module is switched off and isolated from the mains power supply. Remove the top
cover of the module.
2 Remove the flat cable connection (1) from the Agent-ID.
3 Remove the 3 pneumatic connections (2) from the side of the agent ID head.
85
Page 88

1 Anesthetic Gas Module Repairing the Anesthetic Gas Module
Using a cross-tipped screwdriver, remove the 4 screws (3) securing the agent ID head to the IR
4
measurement mounting bracket.
5 Carefully remove the agent ID head from the module.
Replacement
To replace the agent ID head (refer to Figure 44):
1 Place the agent ID head onto the IR measurement unit so that its threaded bores align with the
locating holes provided.
2 Replace the 3 pneumatic connections (2) to the side of the agent ID head. The top and bottom
connections are the inlets, and the middle connection is the outlet to the pump. Check that all
tubing is tightly connected and show no signs of damage.
3 Using a cross-tipped screwdriver, replace the 4 screws (3) securing the agent ID head to the IR
measurement mounting bracket.
4 Replace the flat cable connection (1) to the Agent-ID.
NOTE After replacing the agent ID head, check that all flat-cable connectors are firmly seated and show no
signs of damage.
5 Replace the top cover of the module.
Now perform the performance checks described in the “Test and Inspection Matrix” on page 94.
86
Figure 44 Removing and Replacing the Agent ID Head
Page 89

Repairing the Anesthetic Gas Module 1 Anesthetic Gas Module
Pump
Removal
To remove the pump (refer to Figure 45):
1 Ensure that the module is switched off and isolated from the mains power supply. Remove the
cover of the module.
2 Remove the pneumatic connections (1) and/or (4) from the pump.
3 Remove the power connection from the main PC board (2).
4 Using a cross-tipped screwdriver, remove the two screws and washers (3) securing the pump to the
IR measurement mounting bracket.
5 Carefully slide out the pump from the IR measurement mounting bracket.
Replacement
To replace the pump (refer to Figure 45):
1 Carefully position the pump so that the threaded bores in the pump align with the locating holes
on the IR measurement mounting bracket.
2 Using a cross-tipped screwdriver, replace the two screws and washers (3) securing the pump to the
IR measurement mounting bracket.
3 Replace the connection (2) to the main PC board (to the dc pump connector).
4 Replace the pneumatic connections (1) and/or (4) to the pump. Check that all tubing is tightly
connected and show no signs of damage.
NOTE After replacing the pump, check that all flat-cable connectors are firmly seated and show no signs of
damage.
5 Replace the top cover of the module.
Now perform the performance checks described in the “Test and Inspection Matrix” on page 94 and
reset the pump hours.
To reset pump hours, select
monitor’s service mode. Confirm when prompted.
Reset Pump Hours from the Setup Gas Analyzer menu in the
87
Page 90

1 Anesthetic Gas Module Repairing the Anesthetic Gas Module
Fan
Removal
To remove the fan (refer to Figure 46 and Figure 47):
1 Ensure that the Anesthetic Gas Module is switched off and isolated from the mains power supply.
2 Remove the power connector (1) from the main PC board.
3 Pry the twisted pair supplying power from the fan out of the cable clip (2).
4 Using a cross-tipped screwdriver, remove the four screws and washers (3) securing the fan and the
5 Remove the fan and connecting cable from the module.
Replacement
To replace the fan (refer to Figure 46 and Figure 47):
1 Ensure that the Module is switched off and isolated from the mains power supply.
2
Figure 45 Replacing the Pump
Remove the top cover of the module.
grill to the back panel of the module.
Replace the fan and connecting cable.
Replace the four screws and washers (3) that secure the fan into the back panel of the module.
88
Page 91

Repairing the Anesthetic Gas Module 1 Anesthetic Gas Module
Snap the twisted pair from the fan into the cable clip (2) securing the twisted pairs that connect the
3
IR measurement head with the main PC board.
4 Replace the connector (1) to the main PC board.
5 Replace the top cover of the module.
Now perform the performance checks described in the “Test and Inspection Matrix” on page 94.
Figure 46 Removing the Fan Cabling
89
Page 92

1 Anesthetic Gas Module Repairing the Anesthetic Gas Module
Figure 47 Removing the Fan
Solenoid Valve #2
Removal
To remove solenoid valve #2 (refer to Figure 48):
1 Ensure that the Module is switched off and isolated from the mains power supply. Remove the top
cover of the module.
2 Remove the pneumatic tubing (1) from solenoid valve #2.
3 Remove the connection (2) from the main PC board.
4 Using a cross-tipped screwdriver, remove the two screws (3) securing the solenoid valve to its
bracket.
5 Remove solenoid valve #2.
Replacement
To replace solenoid valve #2 (refer to Figure 48):
1 Ensure that the Module is switched off and isolated from the mains power supply.
2 Position the solenoid valve on its bracket so that the locating holes on the valve align with threaded
bores in the bracket.
90
3 Using a cross-tipped screwdriver, replace the two screws (3) securing the solenoid valve to its
bracket.
4 Replace the connection (2) to the main PC board.
5 Replace the pneumatic tubing (1) to solenoid valve #2. Check that all tubing is tightly connected
and show no signs of damage.
Page 93

Repairing the Anesthetic Gas Module 1 Anesthetic Gas Module
NOTE
After replacing solenoid valve #2, check that all flat-cable connectors are firmly seated and show no
signs of damage.
6 Replace the top cover of the module.
Now perform the performance checks described “Test and Inspection Matrix” on page 94.
Figure 48 Removing the Solenoid Valve #2
Top Cover PC Board
Removal
To remove the top cover PC board (refer to Figure 49 and Figure 50):
1 Ensure that the Module is switched off and isolated from the mains power supply. Remove the top
cover of the module.
2 Remove the connector (1) from the top cover PC board.
3 Using a hex-socket screwdriver, remove the three nuts, washers and spacers (2) securing the PC
board to the top cover of the module.
4 Remove the PC board.
Replacement
To replace the top cover PC board (refer to Figure 49 and Figure 50):
1 Ensure that the Module is switched off and isolated from the mains power.
91
Page 94

1 Anesthetic Gas Module Repairing the Anesthetic Gas Module
Carefully fit the PC board over the three locating screws on the top cover of the module.
2
3 Using a hex-socket screwdriver, replace the three nuts, washers and spacers (2) securing the PC
board to the top cover.
4 Replace the connector (1) to the top cover PC board.
5 Replace the top cover of the module.
Now perform the performance checks described “Test and Inspection Matrix” on page 94.
Figure 49 Removing the Top Cover PC Board Connection
Figure 50 Removing the Top Cover PC Board
92
Page 95

Repairing the Anesthetic Gas Module 1 Anesthetic Gas Module
Watertrap Manifold and Protector
Removal
To remove the manifold and protector (refer to Figure 51):
1 Remove the top cover of the module.
2 Remove the Nafion tubing and purple connector tubing from the manifold connectors (1) on the
inside of the front cover.
3 Using a cross-tipped screwdriver, unscrew the 4 screws (2) securing the protector to the front cover
and remove the protector.
4 Using a cross-tipped screwdriver, unscrew the 2 screws (3) securing the manifold to the protector.
Replacement
To replace the manifold and protector (refer to Figure 51):
1 Using a cross-tipped screwdriver, replace the 2 screws securing the manifold to the protector.
2 Using a cross-tipped screwdriver, replace the 4 screws securing the protector to the front cover.
3 Replace the Nafion tubing and purple connector tubing onto the manifold connectors on the
inside of the front cover. Take care to attach the tubing with the red mark at the end to the
connector with the red marking (this indicates the “drainage” path). The gap between the end of
the nafion tubing and the manifold connectors (visible through the purple connector tubing) must
be less than 1mm.
Now perform the performance checks described “Test and Inspection Matrix” on page 94.
Figure 51 Removing the Watertrap Manifold and Protector
93
Page 96

1 Anesthetic Gas Module Repairing the Anesthetic Gas Module
Power Fuses
Removal
To remove the power fuses (refer to Figure 52):
1 Using a flat-tipped screwdriver, unscrew the fuse counter-clockwise (1).
2 Pull the fuse cap and fuse clear of the display.
3 Pull the fuse out of the fuse cap and note the fuse rating.
4 Repeat the steps for the other fuse.
Replacement
To replace the power fuses (refer to Figure 52):
1 Put one end of the fuse into the fuse cap.
2 Put the fuse and fuse cap into the receptacle in the rear of the display.
3 Using a flat-tipped screwdriver, screw the fuse clockwise into the receptacle.
4 Repeat the steps for the other fuse.
Figure 52 The Power Fuses
Test and Inspection Matrix
The Test and Inspection Matrix describes:
• which tests need to be performed
• the expected test results
• what should be written by Philips service personnel on the Philips Installation Report or Customer
Service Order (CSO).
The second section When to Perform Test Blocks describes when the tests should be performed.
94
Page 97

Repairing the Anesthetic Gas Module 1 Anesthetic Gas Module
These tables should be followed for all installations and repairs.
NOTE The test procedures outlined for this test block are to be used only for verifying safe installation or
service of the product in question. The setups for these tests and the acceptable ranges or values are
derived from local and international standards but may not be equivalent. These are not a substitute for
local safety testing where it is required for an installation or service event.
Tes t B lo c k Na me Test or Inspection to be performed Expected Test Result What to Record
on Service
Record
Visual Check for any mechanical damage and all
external leads and accessories. Is the device
free of damage and are all accessories properly
set up?
Power On Switch on the module. A built-in selftest and
communication test are running for two
minutes after "Power On". The green setup
LED near the power button indicates by
flashing if one of the tests failed. When tests
are successfully completed after 2 minutes the
LED is off and the AGM will enter warmup
mode (indicated by INOP
"GA.WARMUP").
Does AGM boot up successfully without
displaying any error or malfunction messages?
Performance
Leakage Check
Perform Leakage Check Measured flow value:
Expected answer is "yes".
If so, visual test is passed.
Expected answer is "yes". If so,
PowerOn test is passed .
0-4 ml/min
V: P or
V: F
where P=Pass and
F=Fail
PO: P or
PO: F
where P=Pass and
F=Fail
PL: P or
PL: F
where P=Pass and
F=Fail
Performance
Flowrate Check
Perform Flowrate Check. Document the
actual flowrates.
Flowrates M1026A #A02/#A05:
Purge =
x1 (310 +/- 15 ml/min)
Measurement Path =
x2 (labelled value +/- 3 ml/min)
Normal =
x3 (132 - 170 ml/min)
PF: P/x1/x2/x3 or
PF: F/x1/x2/x3
where P=Pass and
F=Fail
95
Page 98

1 Anesthetic Gas Module Repairing the Anesthetic Gas Module
Tes t B lo c k Na me Test or Inspection to be performed Expected Test Result What to Record
on Service
Record
Performance
Diagnostic Check
Performance Zero
Calibration Check
Perform the Diagnostic/Error Check.
Does the status of each subassembly display
as "OK" in
window?
The subassemblies are:
- Meas. Assembly
- Meas. Opt. Path
- Agent-ID
- O2 Assembly
- Main PCB
- Power Supply
- Pneumatic System
- Operat. Temperature
Does the status of each channel display as
"OK" in the
Calibration
calibration?
The channels are:
- Press
Gas Analyzer Diagnostic
Gas Analyzer
window after zero
Expected answer is "yes".
If so, Error/Diagnostic check is
passed.
Expected answer is "yes".
If so, zero calibration check is
passed.
PD:P or
PD:F
where P=Pass and
F=Fail
PZC:P or
PZC:F
where P=Pass and
F=Fail
Performance
Barometric
Pressure Check
96
- O2
- CO2
- N2O
- Subst.
Perform Barometric Pressure Check . Difference between actual
measured pressure value and
actual ambient pressure value =
x (<= 5 mmHg)
PBP:P/x or
PBP:F/x
where P=Pass and
F=Fail
Page 99

Repairing the Anesthetic Gas Module 1 Anesthetic Gas Module
Tes t B lo c k Na me Test or Inspection to be performed Expected Test Result What to Record
on Service
Record
Performance Span
Calibration Check
Performance
Normal Operation
Check
Perform the Span Calibration Check.
Document the actual measured values for
each gas channel.
If failed (out of specified tolerances) perform a span calibration for specific gas
channel.
Enter Monitoring mode and check that all
AGM related waves and numerics are present
and correspond to the user’s configuration.
O2 value = x1 (+- 1.0% to O2
calibration value )
CO2 value = x2 (+- 0.1% to
CO2 calibration value)
N2O value = x3 (+- 2.0% to
N2O calibration value))
Agent value = x4 (+- 0.1% to
Agent value)
When calibration of EACH gas
channel was necessary, status of
each channel shows "Done".
Result to report in this case is
PSH:P (without individual gas
value results)
Expected answer is "yes". If so,
performance normal operation
check is passed.
PSH:P/x1/x2/x3/
x4 or
PSH:F/x1/x2/x3/
x4
where P=Pass and
F=Fail
alternatively
PSH:P or
PSH:F
where P=Pass and
F=Fail
PNO: P or
PNO: F
Performance Pump
Te s t
Performance Fan
Check
Are all AGM waves and numerics present
according to the user’s configuration?
Using the pump test kit provided in the PM
kit, clean and test the pump according to the
included instructions. Did the pump pass the
test?
Check that the cooling fan runs smoothly.
Did the fan pass the test?
Expected answer is "yes".
If so, test is passed.
Expected answer is "yes".
If so, fan check is passed.
where P=Pass and
F=Fail
PPU: P or
PPU: F
where P=Pass and
F=Fail
PFA: P or
PFA: F
where P=Pass and
F=Fail
97
Page 100

1 Anesthetic Gas Module Repairing the Anesthetic Gas Module
Tes t B lo c k Na me Test or Inspection to be performed Expected Test Result What to Record
on Service
Record
Safety Step 1
Protective Earth.
See Safety Test Appendix for details / S (2).
Step 2
Enclosure Leakage Current - Normal
Condition.
See Safety Test Appendix for details / S (4).
Step 3
En cl o su re Le ak ag e C ur re nt - S . F. C. Op en
Supply.
See Safety Test Appendix for details / S (5).
Step 4
Enclosure Leakage Current - S.F.C. Open
Earth.
See Safety Test Appendix for details / S (6).
With mains cable:
Maximum impedance = x1 (<=
100 mOhms)
Maximum leakage current = x2
(<= 100 uA)
Maximum leakage current = x3
(<=500uA)
(<= 300 uA, for US and/or UL
devices)
Maximum leakage current = x4
(<=500uA)
(<= 300 uA, for US and/or UL
devices)
S:P/x1/x2/x3/x4
or
S:F/x1/x2/x3/x4
where P=Pass and
F=Fail
When to Perform Test Blocks
Service Event
(When performing.....
Installation Visual, Power On
Test Block(s) Required
....... Complete these tests)
Performance Leakage Check, Diagnostic Check, Zero Calibration Check,
Barometric Pressure Check,
Span Calibration Check and Normal Operation Check
98
 Loading...
Loading...