Page 1

SOMATOM
Spirit
Application Guide
Protocols
Principles
Helpful Hints
syngo 3D
syngo Fly Through
syngo Dental CT
syngo Osteo CT
syngo Volume Evaluation
syngo Dynamic Evaluation
Software Version syngo CT 2005C
Page 2

The information presented in this Application Guide is
for illustration only and is not intended to be relied
upon by the reader for instruction as to the practice of
medicine. Any health care practitioner reading this
information is reminded that they must use their own
learning, training and expertise in dealing with their
individual patients.
This material does not substitute for that duty and is
not intended by Siemens Medical Solutions Inc., to be
used for any purpose in that regard. The drugs and
doses mentioned are consistent with the approval
labeling for uses and/or indications of the drug. The
treating physician bears the sole responsibility for the
diagnosis and treatment of patients, including drugs
and doses prescribed in connection with such use.
The Operating Instructions must always be strictly
followed when operating the CT System. The source
for the technical data is the corresponding data sheets.
The pertaining operating instructions must always be
strictly followed when operating the SOMATOM Spirit.
The statutory source for the technical data are the
corresponding data sheets.
We express our sincere gratitude to the many
customers who contributed valuable input.
Special thanks to Heike Theessen, Christiane
Bredenhöller, Kristin Pacheco, Karin Ladenburger, and
Chen Mahao for their valuable assistance.
To improve future versions of this Application Guide,
we would greatly appreciate your questions,
suggestions and comments.
Please contact us:
USC-Hotline:
Tel. no.+49-1803-112244
email ct-application.hotline@med.siemens.de
Editor: Ute Feuerlein
2
Page 3
Overview
User Documentation 14
Scan and Reconstruction 16
Dose Information 28
Workflow Information 36
Application Information 54
Head 70
Neck 88
Shoulder 94
Thorax 98
Abdomen 110
Pelvis 124
Spine 132
Upper Extremities 146
3
Page 4
Lower Extremities 154
Vascular 162
Specials 176
Children 184
syngo 3D 240
syngo Fly Through 258
syngo Dental CT 268
syngo Osteo CT 274
syngo Volume Evaluation 288
syngo Dynamic Evaluation 306
4
Page 5
5
Page 6
Contents
User Documentation 14
Scan and Reconstruction 16
• Concept of Scan Protocols 16
• Scan Set Up 17
• Scan Modes 18
- Sequential Scanning 18
- Spiral Scanning 18
- Dynamic Serioscan 18
• Slice Collimation and Slice Width 19
- Slice Collimation and Slice Width for
Spiral Mode and HR Spiral Mode 20
- Slice Collimation and Slice Width for
Sequence Mode and HR Sequence Mode 20
• Increment 21
• Pitch 22
• Window values 23
• Kernels 24
• Image Filters 25
• Improved Head Imaging 27
Dose Information 28
• CTDI
and CTDI
W
• Effective mAs 30
• CARE Dose 32
Vol
- How does CARE Dose work? 32
Workflow Information 36
• Recon Jobs 36
• Examination Job Status 37
• Auto Load in 3D and Post-processing
Presets 38
• How to Create your own
Scan Protocols 39
- Edit/Save Scan Protocol 39
- Scan Protocol Manager 40
6
28
Page 7

Contents
• Contrast Medium 45
- The Basics 45
-IV Injection 47
-Bolus Tracking 48
- Test Bolus using CARE Bolus 50
- Test Bolus 51
Application Information 54
• SOMATOM life 54
-General Information 54
-Key Features 55
- Description 56
- Access to Computer Based Training or
Manuals on CD ROM 57
- SRS Based Services 58
- Download of Files 59
- Contact incl. DICOM Images 60
- Trial Order and Installation 62
• Image Converter 64
• File Browser 66
• Patient Protocol 68
Head 70
• Overview 70
• Hints in General 71
- Head Kernels 71
• HeadRoutine 72
• HeadSeq 74
• InnerEarHR 76
• InnerEarHRSeq 78
• Sinus 80
• SinusSeq 82
• Orbita 84
• Dental 86
7
Page 8
Contents
Neck 88
• Overview 88
• Hints in General 89
-Body Kernels 90
• Neck 92
Shoulder 94
• Overview 94
• Hints in General 95
-Body Kernels 95
• Shoulder 96
Thorax 98
• Overview 98
• Hints in General 99
- Body Kernels 101
• ThoraxRoutine/ThoraxRoutine08s 102
• ThoraxFast 104
• ThoraxHRSeq 106
• LungLowDose 108
Abdomen 110
• Overview 110
• Hints in General 111
- Body Kernels 113
• AbdomenRoutine/AbdomenRoutine08s 114
• AbdomenFast 116
• AbdMultiPhase/AbdMultiPhase08s 118
• AbdomenSeq 122
8
Page 9
Contents
Pelvis 124
• Overview 124
• Hints in General 125
- Body Kernels 125
• Pelvis 126
• Hip 128
• SI_Joints 130
Spine 132
• Overview 132
• Hints in General 133
- Body Kernels 135
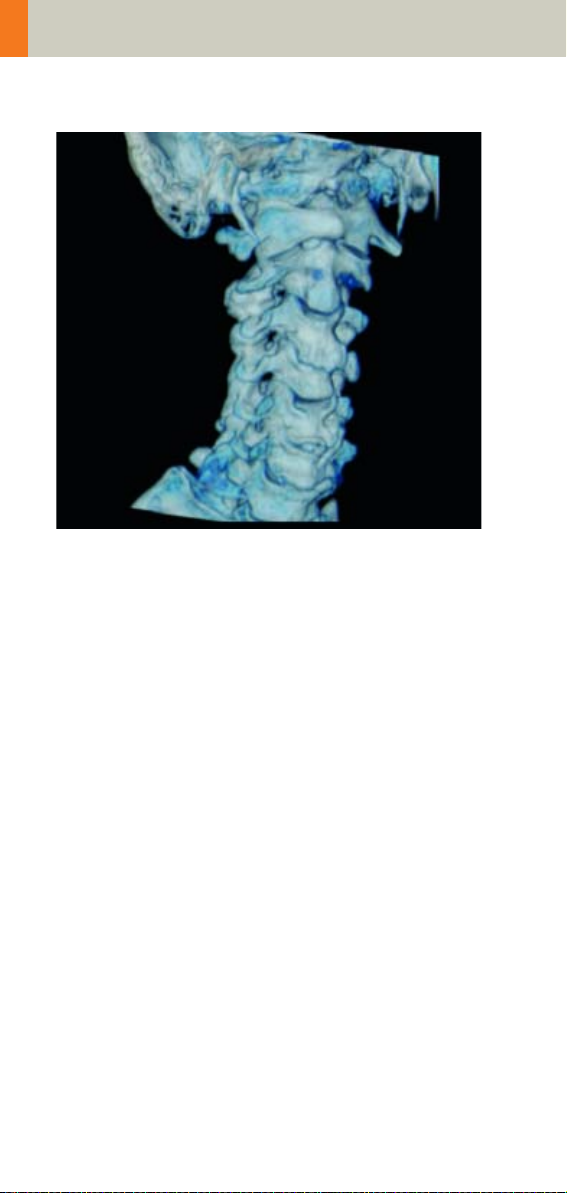
• C-Spine 136
• C-SpineSeq 138
• Spine 140
• SpineSeq 142
• Osteo 144
Upper Extremities 146
• Overview 146
• Hints in General 147
- Body Kernels 148
• WristHR 150
• ExtrRoutineHR 152
Lower Extremities 154
• Overview 154
• Hints in General 155
- Body Kernels 156
• KneeHR 158
• FootHR 160
• ExtrRoutineHR 161
9
Page 10
Contents
Vascular 162
• Overview 162
• Hints in General 163
- Head Kernels 163
- Body Kernels 163
• HeadAngio/HeadAngio08s 164
• CarotidAngio/CarotidAngio08s 166
• ThorAngio/ThorAngio08s 168
• Embolism 170
• BodyAngioRoutine/BodyAngioRoutine08s 172
• BodyAngioFast 174
Specials 176
• Overview 176
- Trauma 176
- Interventional CT 176
- Test Bolus 176
• Trauma 177
- The Basics 177
• PolyTrauma 178
• HeadTrauma 180
• Interventional CT 181
• Biopsy 182
• TestBolus 183
Children 184
• Overview 184
• Hints in General 187
- Head Kernels 190
- Body Kernels 191
• HeadRoutine_Baby 192
• HeadRoutine_Child 194
• HeadSeq_Baby 196
• HeadSeq_Child 198
• InnerEar 200
• SinusOrbi 202
• Neck 204
10
Page 11
Contents
• ThoraxRoutine_Baby 206
• ThoraxRoutine_Child 208
• ThoraxHRSeq_Baby 210
• ThoraxHRSeq_Child 212
• Abdomen_Baby 214
• Abdomen_Child 216
• Spine_Baby 218
• Spine_Child 220
• ExtrHR_Baby 222
• ExtrHR_Child 224
• HeadAngio 226
• HeadAngio08s 228
• CarotidAngio 230
• CarotidAngio08s 232
• BodyAngio 234
• BodyAngio08s 236
• NeonateBody 238
syngo 3D 240
- Multi Planar Reconstruction (MPR) 240
- Maximum Intensity Projection (MIP) 240
- Shaded Surface Display (SSD) 241
- Volume Rendering Technique (VRT) 241
- Prerequisites 242
• Workflow 242
- Loading the Images 242
- Creating Series 244
- Editing 246
- Documentation of Results 249
• Workflow for a CT Extremity Examination 250
- Using MPR/MPR Thick 250
- Using SSD 251
- Using VRT 251
• Workflow for a CT Angiography 252
- Using MIP/MIP Thin 252
- Using VRT/VRT Thin/Clip 253
• Hints in General 254
- Setting Views in the Volume Data Set 254
- Changing /Creating VRT Presets 255
11
Page 12
Contents
- Auto Load in 3D and Post-processing
Presets 257
- Blow-up Mode 257
syngo Fly Through 258
• Key Features 258
• Prerequisites 259
• The Basics for CT Virtual Endoscopy 259
- SSD and VRT Presets for Endoscopic
Renderings 259
- Endoscopic Viewing Parameters/
Fly Cone Settings 260
- Patient Preparation 262
• Workflow 263
- Navigation of the Endoscopic Volume 265
- Fly Path Planning 266
syngo Dental CT 268
• The Basics 268
• Scan Protocols 269
• Additional Important Information 271
syngo Osteo CT 274
• The Basics 274
• Scanning Procedure 275
• Configuration 278
• Evaluation Workflow 282
• Additional Important Information 287
syngo Volume Evaluation 288
• Prerequisites 290
• Workflow 291
• General Hints 300
• Configuration 303
12
Page 13

Contents
syngo Dynamic Evaluation 306
• Prerequisites 308
• Workflow 309
- 1. Loading the Images 309
- 2. Inspecting the Input Images 310
- 3. Generation of Parameter Images 310
- 4. Creating a Baseline Image 313
- 5. Evaluation of Region of Interests 314
- 6. Enhancement Curve 315
- 7. Documentation of Results 316
• General Hints 317
13
Page 14

User Documentation
For further information about the basic operation,
please refer to the corresponding syngo CT Operator
Manual:
syngo CT Operator Manual
Volume 1:
Security Package
Basics
Preparations
Examination
CARE Bolus CT
syngo CT Operator Manual
Volume 2:
syngo Patient Browser
syngo Viewing
syngo Filming
syngo 3D
syngo CT Operator Manual
Volume 3:
syngo Data Set Conversion
syngo Dental CT
syngo Dynamic Evaluation
syngo Osteo CT
syngo Volume
14
Page 15

User Documentation
15
Page 16

Scan and Reconstruction
Concept of Scan Protocols
The scan protocols for adult and children are defined
according to body regions – Head, Neck, Shoulder,
Thorax, Abdomen, Pelvis, Spine, Upper Extremities,
Lower Extremities, Specials, and Vascular.
The general concept is as follows: All protocols without
suffix are standard spiral modes. E.g., “Shoulder”
means the spiral mode for the shoulder.
The suffixes of the protocol name are follows:
“Routine“: for routine studies
“Seq”: for sequence studies
“Fast“: use a higher pitch for fast acquisition
“HR“: use a thinner slice width (1.0 mm) for High Resolution studies and a thicker slice width for soft tissue
studies
The availability of scan protocols depends on the system configuration.
16
Page 17

Scan and Reconstruction
Scan Set Up
Scans can be simply set up by selecting a predefined
examination protocol. To repeat any mode, just click
the chronicle with the right mouse button for “repeat”.
To delete it, select “cut“. Each range name in the chron
icle can be easily changed before “load“.
Multiple ranges can be run either automatically with
“auto range“, which is denoted by a bracket connecting
the two ranges, or separately with a “pause” in
between.
-
17
Page 18

Scan and Reconstruction
Scan Modes
Sequential Scanning
This is an incremental, slice-by-slice imaging mode in
which there is no table movement during data acquisi
tion. A minimum interscan delay in between each
acquisition is required to move the table to the next
slice position.
Spiral Scanning
Spiral scanning is a continuous volume imaging mode.
The data acquisition and table movements are performed simultaneously for the entire scan duration.
There is no interscan delay and a typical range can be
acquired in a single breath hold.
Each acquisition provides a complete volume data set,
from which images with overlapping can be reconstructed at any arbitrary slice position. Unlike the
sequence mode, spiral scanning does not require additional radiation to obtain overlapping slices.
-
Dynamic Serioscan
Dynamic serial scanning mode without table feed.
Dynamic serio can still be used for dynamic evaluation,
such as Test Bolus.
18
Page 19

Scan and Reconstruction
Slice Collimation and Slice Width
Slice collimation is the slice thickness resulting from
the effect of the tube-side collimator and the adaptive
detector array design. In Multislice CT, the Z-coverage
per rotation is given by the product of the number of
active detector slices and the collimation (e.g., 2 x
mm).
1.0
Slice width is the FWHM (full width at half maximum)
of the reconstructed image.
With the SOMATOM Spirit, you select the slice collimation together with the slice width desired. The slice
width is independent of pitch, i.e. what you select is
always what you get. Actually, you do not need to be
concerned about the algorithm any more; the software
does it for you.
The Recon icon on the chronicle will be labeled with
“RT”. After the scan, the Real Time displayed image
series has to be reconstructed.
The following tables show the possibilities of image
reconstruction in spiral and sequential scanning.
19
Page 20

Scan and Reconstruction
Slice Collimation and Slice Width for Spiral Mode and HR Spiral Mode
1 mm: 1, 1.25, 2, 3, 5 mm
1.5 mm: 2, 3, 5, 6 mm
2.5 mm: 3, 5, 6, 8, 10 mm
4 mm: 5, 6, 8, 10 mm
5 mm: 6, 8, 10 mm
Slice Collimation and Slice Width for Sequence Mode and HR Sequence Mode
1.0 mm: 1, 2 mm
1.5 mm: 1.5, 3 mm
2.5 mm: 2.5, 5 mm
4.0 mm: 4, 8 mm
5.0 mm 5, 10 mm
20
Page 21
Scan and Reconstruction
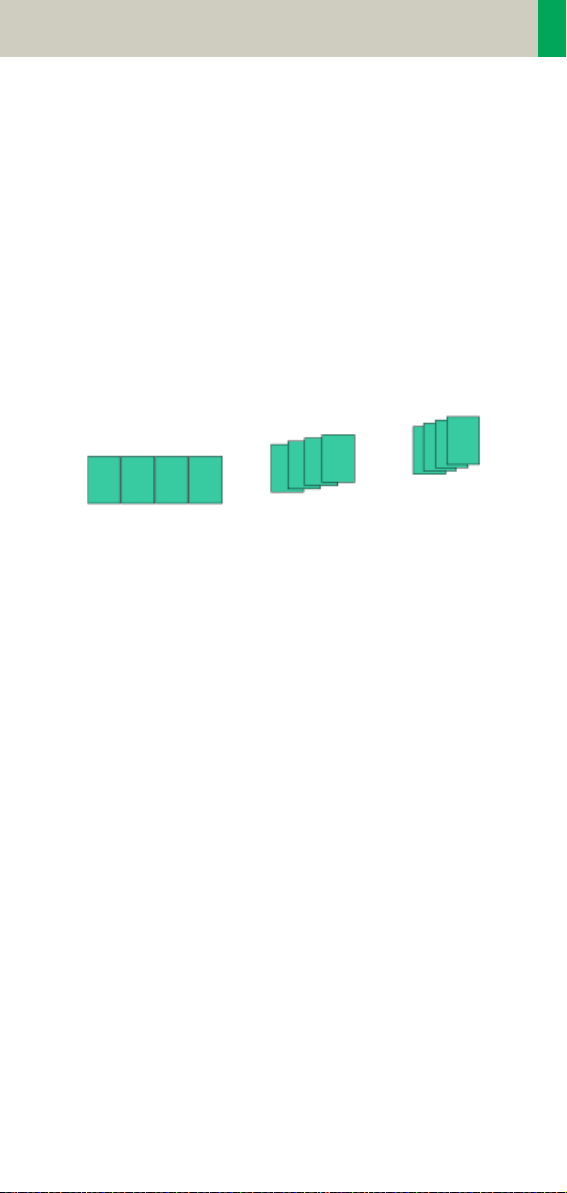
Increment
The increment is the distance between the reconstructed images in the Z direction. When the increment
chosen is smaller than the slice thickness, the images
are created with an overlap. This technique is useful to
reduce partial volume effect, giving you better detail of
the anatomy and high quality 2D and 3D post-process
ing.
Slice Thickness = 10 mm
-
Increment = 10 mm
Reconstruction Increment
Increment = 5 mm
Increment = 3 mm
21
Page 22
Scan and Reconstruction
Pitch
In single slice CT:
Pitch = table movement per rotation/slice collimation
E.g.,: slice collimation = 5 mm,
table moves 5 mm per rotation, then pitch = 1.
With the Siemens Multislice CT, we differentiate
between:
Feed/Rotation, the table movement per rotation
Volume Pitch, table movement per rotation/single
slice collimation.
Pitch Factor, table movement per rotation/complete
slice collimation.
E.g., slice collimation = 2 x 5 mm,
table moves 10 mm per rotation,
then Volume Pitch = 2, Pitch Factor = 1.
With the SOMATOM Spirit, the pitch, slice, collimation,
rotation time, and scan range can be adjusted. The
pitch factor can be selected from 0.5-2.
Pitch 1
Pitch Models
22
Pitch 1.5
Pitch 2
Page 23
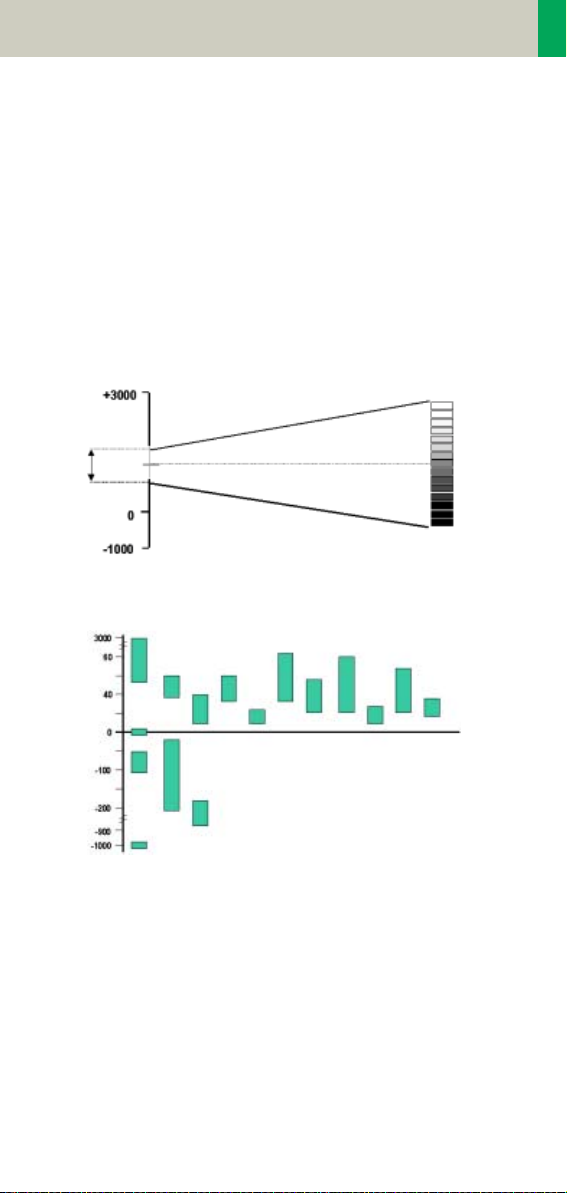
Scan and Reconstruction
Window values
The Scale of the CT Hounsfield Units is from -1024 to
+3071.
The displayed window values have to correspond to
the anatomical structure.
Windowing is used to optimize contrast and brightness
of images.
Hounsfield Units
Spleen
Fat
Window
center C
Kidneys
Pancreas
Lung
Adrenal
Glands
Blood
Heart
Window
width W
Bones
Water
Breast
Air
Organ specific window values
Gray scale
white
CT-window values
Liver
Tumo r
Bladder
Colon
black
23
Page 24

Scan and Reconstruction
Kernels
There are 3 different types of kernels: “H“ stands for
Head, “B“ stands for Body, “C“ stands for ChildHead.
The image sharpness is defined by the numbers – the
higher the number, the sharper the image; the lower
the number, the smoother the image.
A set of 18 kernels is supplied, consisting of:
• 6 body kernels: smooth (B20s), medium smooth
(B31s), medium (B41s), medium sharp (B50s), sharp
(B60s), high res (B70s)
• 7 head kernels: smooth (H21s), medium smooth
(H31s), medium (H41s), medium sharp (H50s),
sharp (H60s), high res (H70s), ultra high res (H80s)
• 3 child head kernels: smooth (C20s), medium
(C30s), sharp (C60s)
• 2 special kernels: S80s, U90s
Note: Do not use different kernels for body parts other
than what they are designed for.
For further information regarding the kernels, please
refer to the “Hints in General” of the corresponding
body region.
24
Page 25
Scan and Reconstruction
Image Filters
There are 3 different filters available:
LCE: The Low-contrast enhancement (LCE) filter
enhances low-contrast detectability. It reduces the
image noise.
• Similar to reconstruction with a smoother kernel
• Reduces noise
• Enhances low-contrast detectability
• Adjustable in four steps
• Automatic post-processing
25
Page 26
Scan and Reconstruction
HCE: The High-contrast enhancement (HCE) filter
enhances high-contrast detectability. It increases the
image sharpness, similar to reconstruction with a
sharper kernel.
• Increases sharpness
• Faster than raw-data reconstruction
• Enhances high-contrast detectability
• Automatic post-processing
ASA: The Advanced Smoothing Algorithm (ASA) filter reduces noise in soft tissue, while edges with high
contrast are preserved.
• Reduces noise without blurring of edges
• Enhances low-contrast detectability
• Individually adaptable
• Automatic post-processing
26
Page 27
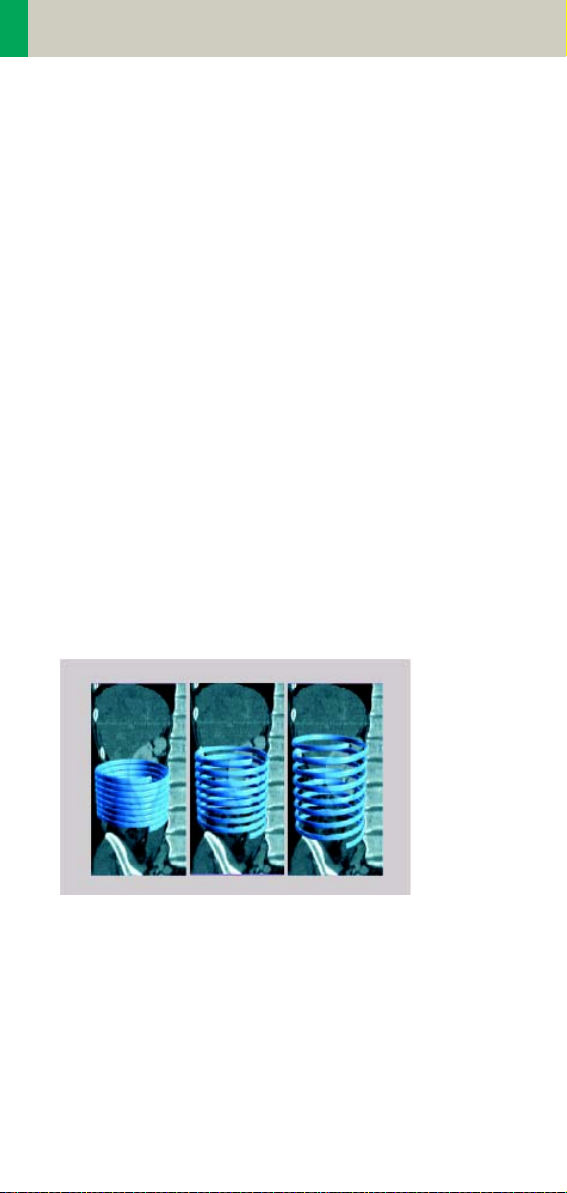
Scan and Reconstruction
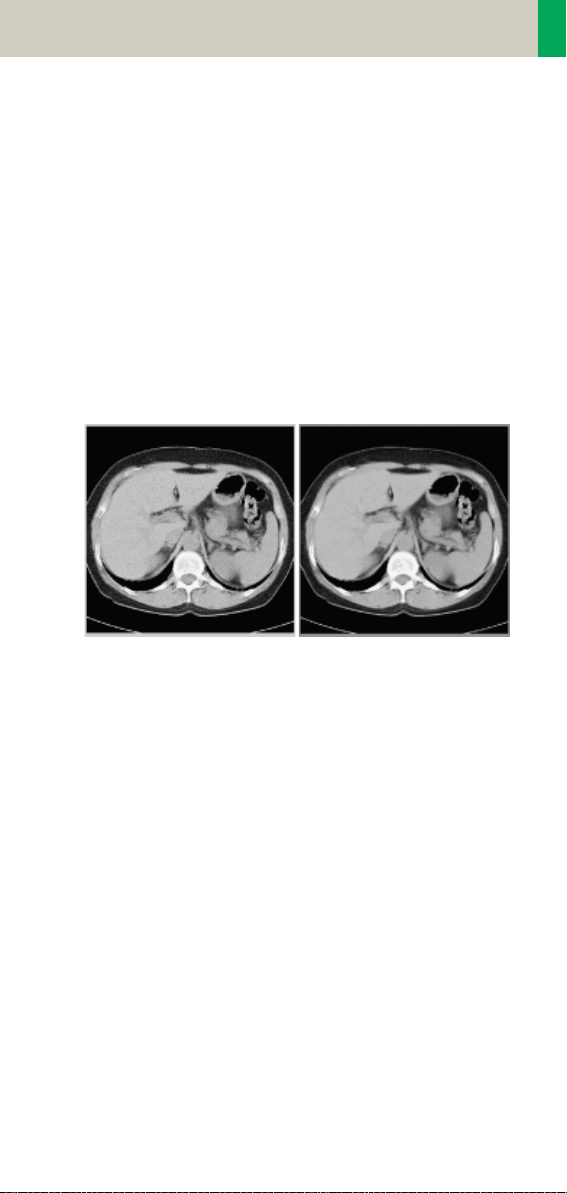
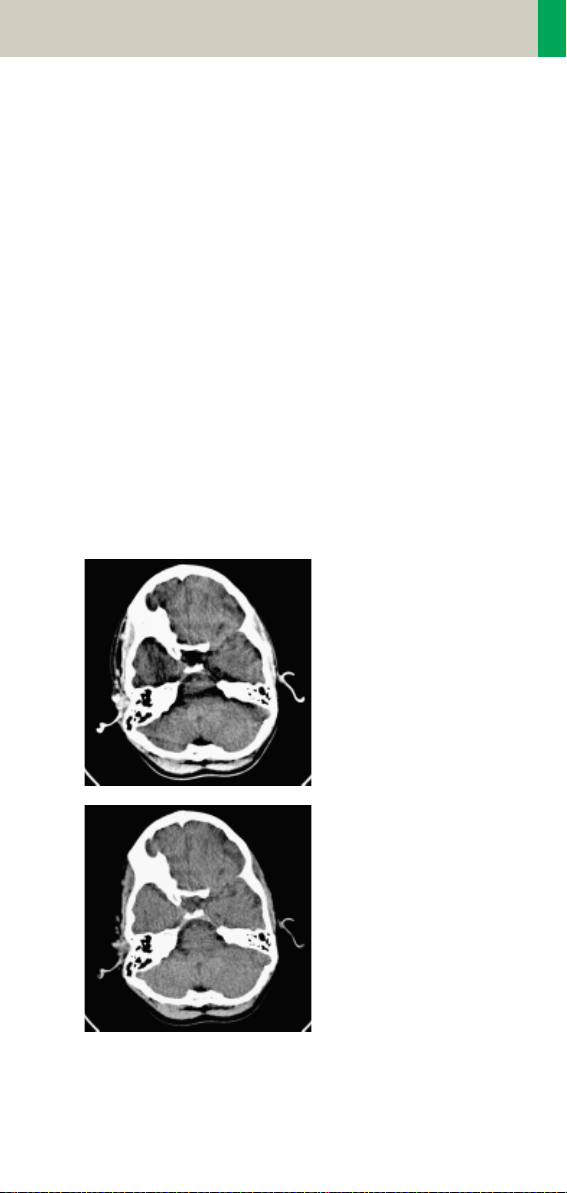
Improved Head Imaging
An automatic bone correction algorithm has been
included in the standard image reconstruction. Using a
new iterative technique, typical artifacts arising from
the beam-hardening effect, e.g., Hounsfield bar, are
minimized without any additional post-processing.
This advanced algorithm allows for excellent images of
the posterior fossa, but also improves head image
quality in general. Bone correction is activated auto
matically for body region “Head”.
In order to optimize image quality versus radiation
dose, scans in the body region “Head” are provided
within a maximum scan field of 300 mm with respect
to the iso-center. No recon job with a field of view
exceeding those limits will be possible. Therefore,
patient positioning has to be performed accurately to
ensure a centered location of the skull.
Head image without
correction.
-
Head image with corrections.
27
Page 28

Dose Information
CTDIW and CTDI
Vol
The average dose in the scan plane is best described by
the CTDIW for the selected scan parameters. The CTDI
is measured in the dedicated plastic phantoms – 16 cm
diameter for head and 32 cm diameter for body (as
defined in IEC 60601 –2 – 44). This dose number gives
a good estimate for the average dose applied in the
scanned volume as long as the patient size is similar to
the size of the respective dose phantoms.
Since the body size can be smaller or larger than
32 cm, the CTDIW value displayed can deviate from the
dose in the scanned volume.
The CTDIW definition and measurement is based on single axial scan modes. For clinical scanning, i.e. scanning of entire volumes in patients, the average dose
will also depend on the table feed in between axial
scans or the feed per rotation in spiral scanning. The
dose, expressed as the CTDI
, must therefore be cor-
W
rected by the Pitch Factor of the spiral scan or an axial
scan series to describe the average dose in the scanned
volume.
For this purpose the IEC defined the term “CTDIVol“ in
September 2002:
W
CTDI
= CTDIW/Pitch Factor
Vol
This dose number is displayed on the user interface for
the selected scan parameters.
28
Page 29

Dose Information
The CTDI
tion of the radiation risk associated with CT examination. For the purpose, the concept of the “Effective
Dose“ was introduced by ICRP (International Commis
sion on Radiation Protection). The effective dose is
expressed as a weighted sum of the dose applied not
only to the organs in the scanned range, but also to the
rest of the body. It could be measured in whole body
phantoms (Alderson phantom) or simulated with
Monte Carlo techniques.
The calculation of the effective dose is rather complicated and has to be done by sophisticated programs.
These have to take into account the scan parameters,
the system design of individual scanner, such as x-ray
filtration and gantry geometry, the scan range, the
organs involved in the scanned range and the organs
affected by scattered radiation. For each organ, the
respective dose delivered during the CT scanning has
to be calculated and then multiplied by its radiation
risk factor. Finally, the weighted organ dose numbers
are added up to get the effective dose.
The concept of effective dose allows the comparison of
radiation risk associated with different CT or x-ray
exams, i.e. different exams associated with the same
effective dose would have the same radiation risk for
the patient. It also allows comparing the applied x-ray
exposure to the natural background radiation,
e.g., 2 – 3 mSv per year in Germany.
value does not provide the entire informa-
vol
-
29
Page 30

Dose Information
Effective mAs
In sequential scanning, the dose (Dseq) applied to the
patient is the product of the tube current-time (mAs)
and the CTDI
D
= D
seq
In spiral scanning, however, the applied dose (Dspiral)
is influenced by the “classical“ mAs (mA x Rot Time)
and in addition by the Pitch Factor. For example, if a
Multislice CT scanner is used, the actual dose applied
to the patient in spiral scanning will be decreased
when the Pitch Factor is larger than 1, and increased
when the Pitch Factor is smaller than 1. Therefore, the
dose in spiral scanning has to be corrected by the Pitch
Factor:
D
= (D
spiral
To make it easier for the users, the concept of the
“effective“ mAs was introduced with the SOMATOM
Multislice scanners.
The effective mAs takes into account the influence of
pitch on both the image quality and dose:
Effective mAs = mAs/Pitch Factor
per mAs:
w
x mAs
CTDIw
x mA x Rot Time)/Pitch Factor
CTDIw
To calculate the dose you simply have to multiply the
CTDIw per mAs with the effective mAs of the scan:
D
spiral
= D
x effective mAs
CTDIw
30
Page 31

Dose Information
For spiral scan protocols, the indicated mAs is the
effective mAs per image. The correlation between tube
current mA and effective mAs of spiral scans on a Multislice CT scanner is given by the following formula:
Effective mAs = mA x RotTime/Pitch Factor
Pitch Factor =
mA =
where Slice collimation refers to the collimation of one
detector row, and nrow is the number of used detector
rows.
effective mAs
R o t T i m e
Feed/Rot
nrow x Slice collimation
x Pitch Factor
31
Page 32

Dose Information
CARE Dose
CARE Dose is a clinical application package that provides real-time tube current modulation for Spiral and
Sequential Scanning.
CARE Dose reduces patient dose significantly, especially in the regions of shoulder and pelvis. It decreases
tube load, which extends the capacity for volume scanning with thinner slices, larger volumes or Multi-phase
studies.
It can also improve image quality by increasing mA,
thus reducing image noise on the lateral views.
How does CARE Dose work?
It reduces the mA for low attenuation views up to 90%
and keeps the nominal higher mA for high attenuation
views, e. g. in the lateral projection. This is done “onthe-fly”, i.e. the scanner adapts the mA in real-time,
according to the patient’s attenuation profile.
32
Page 33

Dose Information
,
Low attenuation,
low mA
Example of scanning the shoulder region.
High
attenuation
high mA
rel. units
lateral
TOP
Object attenuation
Modulated tube current
time
Principle of CARE Dose tube current adaption.
• CARE Dose is pre-selected by default for most standard protocols. It can be switched on/off in the Scan
subtask card.
33
Page 34

Dose Information
• For the average patients examination, CARE Dose
does not require any manual changes to the scan
protocol. However, the mAs must be adapted manually for obese and pediatric patients.
• The mean value of the mAs applied will be lower
than what you have selected. Although the average
mA for the entire scan will be lower than selected,
we allow the scanner to apply increased mA levels
for the high attenuation views. This may cause dif
ferent results of the tube load controller when
switching on and off CARE Dose.
• The mean value of the effective mAs applied is
shown in the image text.
-
34
Page 35

Dose Information
35
Page 36

Workflow Information
Recon Jobs
In the Recon card, you can define up to 3 reconstruction jobs for each range with different parameters,
either before or after you acquire the data. When you
deselect all chronicle entries, all open recon jobs will
be automatically reconstructed after you click on
“Recon“. In case you want to add more than 3 recon
jobs, simply click the icon on the chronicle with the
right mouse button and select “delete recon job“ to
delete the one which has been completed, and then
one more recon job will be available in the Recon card.
Note: What you delete is just the job from the display,
not the images that have been reconstructed. Once
reconstructed, these completed recon jobs stay in the
browser, until deleted from the hard drive.
36
Page 37

Workflow Information
Examination Job Status
You can get an overview of all recon jobs by clicking on
the recon task symbol in the status bar or selecting
Transfer – Examination Job Status in the main menu of
the Patient Browser.
The Examination Job Status dialog will appear where
all recon jobs (completed, queued and in work) are
listed. You can stop, restart and delete each job by
clicking the according button. To give a selected job a
higher priority click “urgent”.
The column “Type“ shows you which kind of reconstruction is queued.
Two types are displayed:
–Recon
all recon jobs from the Recon card
–Auto 3D
all 3D reconstructions which you have sent via “Auto
post-processing” automatically into the 3D card.
These jobs will be deleted from the job list as soon as
the patient is closed in the 3D card.
37
Page 38

Workflow Information
Auto Load in 3D and Postprocessing Presets
You can activate the Auto load in 3D function on the
Examination card/Auto Tasking and link it to a recon
job. For example, the 2
width in some of the examination protocols.
On the 3D card you have the ability to create Range
Parallel and Radial protocols for Multi-Planar-Reconstruction (MPR) and Thin Maximum-Intensity-Projection (MIP Thin) which can be linked to a special series.
For example, if you always do sagittal MPRs for a Spine
examination, once you load a Spine examination into
the 3D card, select the image type (MPR, MIP Thin),
select the orientation and open the Range Parallel
function. Adapt the range settings (Image thickness,
Distance between the images etc.) and hit the link but
ton. From that point on, you have a predefined postprocessing protocol, linked to the series description of
a Spine examination.
The same can be done for VRT presets. In the main
menu, under Type/VRT Definition, you can link VRT presets with a series description.
nd
recon job with thinner slice
-
38
Page 39

Workflow Information
How to Create your own
Scan Protocols
There are two different ways to modify and create your
scan protocols:
Edit/Save Scan Protocol
If you want to modify an existing protocol or create a
new one, e.g., you want to have two “AbdomenRoutine-Protocols” with different slice width, we recommend to do this directly on the Examination card.
User-specific scan protocols can be saved with the following basic procedure:
• Register a patient, you can choose any patient position in the “Patient Model Dialog“.
• Select an existing scan protocol in the “Patient Model
Dialog”.
• Modify the scan protocol, change parameters, add
new ranges etc., so that the new protocols fit your
needs.
• Scan your patient as usual.
• Check if all parameters are as you desire.
•Select Edit/Save Scan Protocol in the main menu.
• Select the folder where you want the new protocol to
appear and the scan protocol name in the pop-up
dialog.
• You can either use the same name to overwrite the
existing scan protocol, or enter a new name, which
will create a new protocol name and will not alter
any of the existing protocols already stored.
39
Page 40

Workflow Information
Hints
• You can save your scan protocol at any time of the
examination.
• It is recommended that you save your own scan protocol with a new name in order to avoid overwriting
the default scan protocol.
• Do not use special characters. In addition, do not
even use any blank spaces. Allowed are all numbers
from 0 to 9, all characters from A to Z and a to z and
explicitly the _ (underscore).
• Do not rename scan protocol files on Windows level.
This will lead to inconsistencies.
• You can now save your own scan protocols in any
predefined folder. The organ characteristics will
belong to the scan protocol not to the region.
• In the Patient Model Dialog, the modified scan protocols are marked with a dot in front of the protocol.
Scan Protocol Manager
If you want to modify special parameters for all existing scan protocols or you want to modify the folder
structure, we recommend doing this in the “Scan Pro-
tocol Manager”. The “Scan Protocol Manager” is
opened and all protocols are loaded.
User-specific scan protocols can be saved with the following basic procedure:
Open “Options, on the “Scan Protocol Manager” icon.
• Rename a protocol:
Select a scan protocol with the right mouse button.
Select “Rename” and enter a new name for the protocol.
40
Page 41

Workflow Information
• Change one (or more) parameters for all Customer
protocols:
Select “Edit – Find/Replace”. Open the “Column“ list
box and choose the desired parameter. Select a new
function of this parameter in the “Function“ list box.
Under the button next to the Function entry you can
choose special selections, e.g., you can in-/decrease
all mAs values by a certain percentage, e.g., 5%.
Select “Replace All”.
41
Page 42

Workflow Information
• Define a protocol as Emergency protocol.
Select the desired scan protocol with the right
mouse button. Select entry “Set as new emergency
protocol”. The selected protocol is marked with a red
cross.
• Change the structure of the protocol tree. You can
sort all Customers protocols as needed. Select the
desired protocols, press right mouse button.
You will find the entries:
– Cut/copy
– Paste
to change the sorting of your protocol tree. You can
also do this easily by dragging and dropping the protocols under the desired position.
42
Page 43

Workflow Information
Hints
• With the Find/Replace function you can easily insert
an API command for all protocols as needed.
• Also all Auto Tasking actions, e.g., the transfer to
configured network nodes can be set within one
action. Within the “Function” button you can set your
transfer actions depending on the slice width.
• By sorting the scan protocols, all organ characteristics will belong to the protocol, so it does not matter
which folder you choose.
• The entry “Set to defaults” in the main menu/ context
sensitive menu will reset all your changes to the Siemens default values.
• Display of actions:
– Invalid protocols or parameters are marked in yel-
low.
– Changed, but not yet saved protocols and/or
parameters are marked in green.
• With the entries Save/Save as/Save all, you can save
your changes.
• For security purposes it is not possible to do any
changes in the Siemens protocols, although you can
copy or drag&drop these protocols into a Customer
folder.
• Scan protocols can be deleted if they belong to the
USER category. Only complete scan protocols can be
deleted. It isn’t possible to delete scan protocol
entries or scan protocol recon jobs.
• If there are unsaved scan protocols when closing the
Scan Protocol Manager you will be informed by a
message.
• You can configure the displayed columns and their
position with “View configure columns”.
43
Page 44

Workflow Information
Additional Information:
1.System/Run offers the tool “Restore Default Scan Protocols“ which allows you to remove user specific
scan protocols and to restore the Siemens default
settings.
2.The main menu entry “Edit” offers save/delete Scan
Protocols.
3.System/Run or the main menu entry “View” in the
Scan Protocol Manager offer the tool “List Scan Protocols” which generates an HTML table of all available scan protocols. This list can be printed or saved
on Floppy (Right-click in the table, click View Source/
File/Save As…).
44
Page 45

Workflow Information
Contrast Medium
The Basics
The administration of intravenous (IV) contrast material during spiral scanning improves the tissue characterization and characterization of lesions, as well as the
opacity of vessels. The contrast scan will yield good
results only if the acquisition occurs during the optimal
phase of enhancement in the region of interest. There
fore, it is essential to initiate the acquisition with the
correct start delay. Since multislice spiral CT can pro
vide much faster speed and shorter acquisition time, it
is even more critical to get the right timing to achieve
optimal results.
-
-
40 s scan
Longer scan time Shorter scan time
The dynamics of the contrast enhancement is determined by:
• Patient cardiac output
•Injection rate
• Total volume of contrast medium injected
• Concentration of the contrast medium
• Type of injection – uni-phasic or bi-phasic
• Patient pathology
10 s scan
45
Page 46

Workflow Information
Aortic time-enhancement curves after i.v. contrast
injection (computer simulation*).
All curves are based on the same patient parameters
(male, 60-year-old, 75 kg).
Relative Enhancemen t [HU]
Time [s]
Relative Enhancement [HU]
Time [s]
2 ml/s, 120 ml, 300 mg I/ml 4 ml/s, 120 ml, 300 mg I/ml
Relative Enhancement [HU]
Time [s]
Relative Enhancement [HU]
Time [s]
80 ml, 4 ml/s, 300 mg I/ml 120 ml, 4 ml/s, 300 mg I/ml
Relative Enhancement [HU]
Time [s]
Relative Enhancement [HU]
Time [s]
Uni-phase 140 ml, 4 ml/s,
370 mg I/ml
Bi-phase 70 ml, 4 ml/s,
plus 70 ml,
2 ml/s, 370 mg I/ml
*Radiology 1998; 207:647 – 655
46
Page 47

Workflow Information
IV Injection*
The administration of a contrast medium depends on
the indication and on the delay times to be used during
the examination. The patients weight and circulatory
situation also play a role. In general, no more than 3 ml
per kg of body weight for adults and 2 ml per kg of
body weight for children should be applied.
For CTA studies (arterial phase), the principle is to keep
contrast injection throughout the duration of the scan.
Thus, the total amount of contrast medium needed
should be calculated with the following formula:
CM = (start delay time + scan time) x flow rate.
CARE Bolus or Test Bolus may be used for optimal contrast bolus timing. Please refer to the special protocols.
To achieve optimal results in contrast studies, the use
of CARE Bolus is recommended. In case it is not available, use Test Bolus. Once completed, load images into
Dynamic Evaluation for calculation of Time to Peak
enhancement.
*For more information regarding the general use of
drugs and doses mentioned in this guide, please
refer to page 2.
47
Page 48

Workflow Information
Bolus Tracking
This is an automatic Bolus Tracking program, which
enables triggering of the spiral scanning at the optimal
phase of the contrast enhancement.
General Hints
• This mode can be applied in combination with any
spiral scanning protocol. Simply insert “Bolus Tracking” by clicking the right mouse button in the chronicle. This inserts the entire set up including pre-monitoring, i.v. bolus and monitoring scan protocol. You
can also save the entire set up as your own scan protocol.
• The pre-monitoring scan is used to determine the
position of the monitoring scans. It can be performed at any position of interest. You can also
increase the mAs setting to reduce the image noise
when necessary.
• To achieve the shortest possible spiral start delay
(2 s), the position of the monitoring scans relative to
the beginning of spiral scan must be optimized.
A “snapping” function is provided:
– After the Topogram is performed, the predefined spi-
ral scanning range and the optimal monitoring position will be shown.
– If you need to redefine the spiral scanning range,
you should also reposition the monitoring scan in
order to keep the shortest start delay time (2 s). (The
distance between the beginning of the spiral scan
ning range and the monitoring scan will be the
same).
-
48
Page 49

Workflow Information
– Move the monitoring scan line towards the optimal
position and release the mouse button, it will be
snapped automatically. (Trick: if you move the monitoring scan line away from the optimal position the
“snapping” mechanism will be inactive).
• Place a ROI in the premonitoring scan on the target
area or vessel used for triggering with one left
mouse click. (The ROI is defined with double circles
– the outer circle is used for easy positioning, and
the inner circle is used for the actual evaluation). You
can also zoom the reference image for easier posi
tioning of the ROI.
• Set the appropriate trigger threshold, and start contrast injection and monitoring scans at the same
time.
During the monitoring scans, there will be simultaneous display of the relative enhancement of the target ROI. When the predefined density is reached, the
spiral acquisition will be triggered automatically.
• You can also initiate the spiral any time during the
monitoring phase manually – either by pressing the
START button or by left mouse clicking the START
radio button. If you do not want to use automatic
triggering, you can set your trigger threshold num
ber extremely high so that it will not trigger automatically, and you can start the spiral when you
desire.
-
-
49
Page 50

Workflow Information
Test Bolus using CARE Bolus
You can use the CARE Bolus option as a “Test Bolus“.
How to do it
1.Insert a Bolus tracking via the right mouse button
submenu prior to the spiral.
2.Insert “contrast“ from the right mouse button context menu prior to the monitoring scans.
Hint: By inserting “contrast“ you are interrupting the
Auto range function, and therefore an automatic
start of the spiral is not possible!
3.Start with the Topogram.
4.Position the premonitoring scan and the spiral
range.
5.Perform the premonitoring scan, position and
accept the ROI.
6.Start monitoring scans and a short amount of con-
trast (20 ml/2.5 ml/sec.).
Hint: With starting the spiral the system is switching
to the Trigger subtask card. The trigger line is not
shown at this stage.
7.Now you can read the proper delay from the Trigger
subtask card.
8. Insert the delay in the Routine subtask card and load
the spiral.
9.Start spiral and injector with the full amount of contrast.
50
Page 51

Workflow Information
Test Bolus
This is a low dose sequential protocol without table
feed used to calculate the start delay of a spiral scan to
ensure optimal enhancement after the contrast
medium injection. The Dynamic Evaluation function
may be used to generate the time density curve.
You can find the “Test Bolus“ scan protocol in the chapter “Specials“.
How to do it
1.Select the spiral mode that you want to perform, and
then “Append” the Test Bolus mode under Special
protocols.
2.Insert the Test Bolus mode above the spiral mode for
contrast scan by “cut/paste” (with right mouse but
ton).
3. Perform the Topogram, and define the slice position
for Test Bolus.
4.Check the start delay, number of scans and cycle
time before loading the mode.
5.A Test Bolus with 10 – 20 ml is then administered
with the same flow rate as during the subsequent
spiral scan. Start the contrast media injection and
the scan at the same time.
-
51
Page 52

Workflow Information
6. Load the images into the Dynamic Evaluation function and determine the time to the peak enhancement. Alternatively, on the image segment, click
“select series” with the right mouse button and posi
tion an ROI on the first image. This ROI will appear
on all images in the Test Bolus series. Find the image
with the peak HU value, and calculate the time “delta
t” taken to reach the peak HU value (do not forget to
add the preset start delay time). This time can then
be used as the optimal start delay time for the spiral
scan.
-
52
Page 53

Workflow Information
53
Page 54

Application Information
SOMATOM life
General Information
SOMATOM life @ Your Scanner provides actual news
around your scanner, shows you helpful configuration
information of your system and enables you to access
the Siemens Extranet where you will find further
opportunities to enhance your possibilities to use the
CT system.
To benefit from the Siemens Extranet, a Siemens
Remote Service connection is required. The Siemens
Extranet allows you to order Trial Licenses, download
the necessary Application Guide or find interesting
information related to your CT system.
Note: Siemens Remote Service is an optional part of
your service contract that also covers remote service
capabilities for your CT system to optimize the system
availability and is also prerequisite for other services.
54
Page 55

Application Information
Key Features
All users:
• General Information
• Access to Web Based E-Training or Manuals on CD
ROM
In combination with a Siemens Remote Service connection:
• News-Ticker archive and FAQ (frequently asked questions) section
• Free trial software order and installation
• Download of information, manuals and scan protocols
• A contact function for an easy and fast interface to
Siemens including the ability to attach up to two
DICOM images
Note: In regard to legal issues, not all services may be
available in every country.
55
Page 56

Application Information
Description
All users:
Start SOMATOM life @ Your Scanner by selecting
SOMATOM life under "options" in your syngo menu bar
and you will find a browser window that allows you to
access different information about your hard- and soft
ware environment.
Under e.g., "System Information" you have information
such as software version or scan second counter.
Under Customer Information you can enter your
demographic data.
Note: The institution data and at least one contact person have to be entered to be able to access the Siemens Extranet. The link to the Siemens Extranet will be
visible only after you have entered this data.
-
56
Page 57

Application Information
Access to Computer Based Training or Manuals on CD ROM
Start the Computer Based Training to learn more about
your software and enhance your clinical knowledge.
Note: The syngo Basics Training is pre-installed on your
system and can directly be used by selecting SOMA
TOM Educate. The syngo Advanced Application Training can be downloaded in the Siemens Extranet or is
sent to you automatically on CD if you request a trial
software via the Siemens Extranet.
In case a document (e.g., Application Guide) is not visible after being opened:
• Minimize or move the Browser window of the SOMATOM life platform.
-
Under the navigation path "World" you can also start
your manual CD ROM.
57
Page 58

Application Information
SRS Based Services
During the start up of your system you will receive
actual information in the "Newsticker" and see the
expiration date of installed trial software.
Note: Siemens will send you a Newsticker whenever
there is helpful information for CT users. The trial
licenses are valid for 90 days and can only be ordered
once.
Access the Siemens Extranet by clicking on "Extranet".
After entering your CT system serial number you will
be forwarded to the workspace. You can find the serial
number in the system information in the offline part of
SOMATOM life @ Your Scanner.
Now you have the ability to view information and use
the different services.
58
Page 59

Application Information
Download of Files
Each download will be performed in the background. If
you disconnect your Siemens Extranet session and
start to work with the CT scanner, the download will
continue until it is completed. Due to bandwidth rea
sons it is only possible to perform one download at a
time.
Note: Depending on your connection speed, the
download of larger files like e.g., the Advanced Application Training may take a long time.
Downloaded files can be found in the "Offline" folder
which can be accessed under menu: Options/ File
Browser/ Offline.
-
After the download, the WBT will install itself and can
be started within the SOMATOM life offline part under
SOMATOM Educate.
59
Page 60

Application Information
Downloaded Scan Protocols are stored in the update
folder until installation. To install all downloaded protocols, choose the Scan Protocol Manager via Options/
Configuration and select "Import Scan Protocols" in the
menu tab "Scan Protocol". After successful import, all
downloaded protocols can be found under the name
that is stated in the Extranet in the "Siemens Folder".
Also, see the chapter Scan Protocol Manager for more
information.
Contact incl. DICOM Images
You are able to send emails to Siemens directly from
your scanner. For further explanation, even DICOM
images can be attached. To add an image, select the
images you want to send on your Viewing card and
export these images to H:\Offline as a DICOM image.
Also, see chapter "Export Function" for more information.
After exporting the image, open the Siemens Extranet
and choose "Contact". After entering your message
you can easily attach the image by selecting the
images from the File Browser with the shortcut "CTRL"
and "C" and paste it with the shortcut "CTRL" and "P"
into the Extranet.
60
Page 61

Application Information
Note: Every patient image will be made anonymous
before sending. Because the SOMATOM life window is
always in front, we recommend to restore/ minimize it
to be able to switch between both screens, the File
Browser and the SOMATOM life window.
61
Page 62

Application Information
Trial Order and Installation
As a SOMATOM CT user you can request trial clinical
software directly from the scanner. The requested soft
ware will be provided and installed automatically
through our Siemens Remote Services connection.
After you have accessed the SOMATOM life Extranet,
you can choose system specific trial software under
SOMATOM Expand. After clicking on "Order Trial" and
confirming a License Agreement for Trial-Use Soft
ware, you need to enter your contact data. You can
then submit the license request.
-
-
62
Page 63

Application Information
At the same time, you are informed that you can
expect the trial option to be installed within 8 working
days and you will then be informed about the successful installation via the SOMATOM life message window
that appears during system start-up.
63
Page 64

Application Information
Image Converter
The CT Application Common DICOM Adapter provides
conversion between different DICOM data sets as they
may be provided by other CT vendors.
– You will find the converter in the Application menu
of the Patient Browser.
In the pop-up window you can select the application
for which you want to convert the images.
64
Page 65

Application Information
After conversion you can load these data sets into the
application of your choice.
65
Page 66

Application Information
File Browser
The File Browser provides the ability to access and to
manage your created files:
• Copy images and files to the CD Burn folder.
• Access to all created reports and movies (AVI files).
• Access to the offline folder.
• Access to downloaded files.
Open the File Browser via the main menu entry
"Options – File Browser".
The File Browser provides special folders for our Applications. Therein the created reports and movies are
saved.
With an external PC connected you can access your
offline data on the external PC for post-processing.
Transfer files to floppy:
– Select the desired files and send them via the right
mouse button menu on a floppy disk.
Burn on CD:
– Select the desired files and drag & drop them into the
folder “Burn on CD” (or send them via the right
mouse button menu to the folder “Burn on CD“).
– Open the “LocalJobStatus” in the Patient Browser and
clear all entries.
– Select “Record to Offline“ in the Transfer menu of the
Patient Browser.
–CD burning starts.
– Hint: CD burning of offline files is only possible in a
single session.
66
Page 67

Application Information
Review reports and movies:
– Select the desired files and double-click on them.
– The corresponding program, e.g., Movie Media
Player will be opened and you can review what you
have saved.
– Now you can send these files to floppy or burn it on
CD.
Hint
• Files with the following extensions cannot be
started/ opened from the File Browser
“bat“, “cmd“, “com“, “exe“, “reg“, “dot“, “htm“,
“html“, “pl“, “vbs“, “js“, “wsf“, “wsh“, “xml“.
67
Page 68

Application Information
Patient Protocol
Scan: number of scan range
kV: kilo Volt
mAs: averaged applied mAs of the range
ref. mAs: quality ref. mAs of the range
TI: Rotation Time
cSL: collimated Slice
CTDI
: CTDIw
vol
DLP: Dose Length Product
Pitch Factor
For further information please refer to
the chapter “Dose Information“.
CTDIvol x (length + collimated slice)
10
68
Page 69

Application Information
69
Page 70

Head
Overview
– HeadRoutine
Spiral mode for base of the skull and cerebrum routine studies
– HeadSeq
Sequential mode for base of the skull and cerebrum
routine studies
– InnerEarHR
Spiral mode for inner ear studies with a high resolution kernel
– InnerEarSeqHR
Sequence mode for inner ear studies with a high resolution kernel
– Sinus
Spiral mode for sinus studies
– SinusSeq
Sequence mode for sinus studies
– Orbita
Spiral mode for orbital studies
– Dental
Spiral mode for dental studies
70
Page 71

Head
Hints in General
• Topogram: Lateral, 256 mm.
• Patient positioning:
Patient lying in supine position, arms resting against
body, secure head well in the head holder, support
lower legs.
• Gantry tilt is available for both, sequence and spiral
scanning.
However, image artifacts may occur if spirals are
acquired with a tilt angle greater than 8°.
• For all head studies, it is very important for image
quality to position the patient in the center of the
scan field. Use the lateral laser beam to make sure
that the patient is positioned in the center.
• In order to optimize image quality versus radiation
dose, scans are provided within a maximum scan
field of 300 mm with respect to the iso-center. No
recon job with a field of view exceeding those limits
will be possible. Therefore, patient positioning has to
be performed accurately to ensure a centered loca
tion of the skull.
-
Head Kernels
• For soft tissue head studies, the standard kernel is
H41s; softer images are obtained with H31s or H21s
sharper images with H50s.
• High resolution head studies should be performed
with H60s, H70s (e.g., for dental and sinuses) and
H80s (e.g., inner ear).
71
Page 72

Head
HeadRoutine
Indications:
Spiral mode for routine head studies, e.g., stroke, brain
tumors, cranial trauma, cerebral atrophy, hydrocephalus, and inflammation, etc.
Two ranges are predefined for the base of the skull and
cerebrum.
A range for the base of 4 cm will be covered in 23 sec.,
a range for the cerebrum of 8
27 sec.
cm will be covered in
72
Page 73

Head
Base Cerebrum
kV 130 130
Effective mAs 110 110
Rotation time 1.5 sec 1.5 sec
Slice collimation 1.5 mm 2.5 mm
Slice width 3.0 mm 8.0 mm
Feed/Rotation 3.0 mm 5.0 mm
Pitch Factor 1.0 1.0
Increment 3.0 mm 8.0 mm
Kernel H31s H31s
CTDIVol
Effective dose Male:
Contrast medium IV injection
Volume 50 – 60 ml
Flow rate 2 ml/sec.
Start delay 50 – 60 sec.
25.05 mGy 25.05 mGy
Male:
0.37
mSv
Female:
0.38
mSv
0.70
Female:
0.77
mSv
mSv
Hints
• An automatic bone correction allows for improved
head image quality, without any additional post-pro
cessing.
• In order to optimize image quality versus radiation
dose, scans are provided within a maximum scan
field of 300 mm with respect to the iso-center. No
recon job with a field of view exceeding those limits
will be possible. Therefore, patient positioning has to
be performed accurately to ensure a centered loca
tion of the skull.
-
-
73
Page 74

Head
HeadSeq
Indications:
Sequence mode for routine head studies, e.g., stroke,
brain tumors, cranial trauma, cerebral atrophy, hydrocephalus, and inflammation, etc.
Two ranges are predefined. One for the base of the
skull and one for the cerebrum, the scan length for the
entire head is 12.4
For both ranges a typical gantry tilt of -20° is predefined.
mm.
74
Page 75

Head
BaseSeq CerebrumSeq
kV 130 130
Effective mAs 240 240
Rotation time 1.5 sec 1.5 sec
Slice collimation 1.5 mm 4.0 mm
Slice width 3.0 mm 8.0 mm
Feed/Scan 3.0 mm 8.5 mm
Kernel H31s H31s
CTDIVol
Effective dose Male:
Contrast medium IV injection
Start delay 60 sec.
Flow rate 2 ml/sec.
Volume 50 – 60 ml
54.65 mGy 51.43 mGy
Male: 1.52 mSv
0.77
mSv
Female:
Female:
0.80
mSv
1.68
mSv
Hints
• An automatic bone correction allows for improved
head image quality, without any additional post-pro
cessing.
• In order to optimize image quality versus radiation
dose, scans are provided within a maximum scan
field of 300 mm with respect to the iso-center. No
recon job with a field of view exceeding those limits
will be possible. Therefore, patient positioning has to
be performed accurately to ensure a centered loca
tion of the skull.
-
-
75
Page 76

Head
InnerEarHR
Indications:
Spiral mode for inner ear High Resolution studies, e.g.,
inflammatory changes, tumorous processes of pyramids, cerebellopontine angle tumors, post-traumatic
changes, etc.
A range of 2.5 cm will be covered in 22 sec.
InnerEar 2
kV 130
Effective mAs 70
Rotation time 1.5 sec
Slice collimation 1.0 mm
Slice width 2.0 mm 1.25 mm
Feed/Rotation 2.0 mm
Pitch Factor 1.0
Increment 2.0 mm 0.8 mm
Kernel H80s H80s
CTDIVol
Effective dose Male: 0.17 mSv
15.94 mGy
Female: 0.20 mSv
nd
reconstr.
76
Page 77

Head
Hints
• For image reconstruction of soft tissue, use kernel
H31s.
• An automatic bone correction allows for improved
head image quality, without any additional post-processing.
• In order to optimize image quality versus radiation
dose, scans are provided within a maximum scan
field of 300 mm with respect to the iso-center. No
recon job with a field of view exceeding those limits
will be possible. Therefore, patient positioning has to
be performed accurately to ensure a centered loca
tion of the skull.
-
77
Page 78

Head
InnerEarHRSeq
Indications:
Sequential mode for inner ear studies, e.g., inflammatory changes, tumorous processes of pyramids, cerebellopontine angle tumors, post-traumatic changes,
etc.
A typical gantry tilt of -20 degree is predefined. A
range of 2.5
cm will be covered.
InnerEarSeq
kV 130
Effective mAs 140
Rotation time 1.5 sec
Slice collimation 1.0 mm
Slice width 1.0 mm
Feed/Scan 2.0 mm
Kernel H80s
CTDIVol
Effective dose Male: 0.32 mSv
Contrast medium IV injection
Start delay 60 sec.
Flow rate 2 ml/sec.
Total amount 50 – 60 ml
78
31.88 mGy
Female: 0.38 mSv
Page 79

Head
Hints
• For image reconstruction of soft tissue, use kernel
H31s.
• An automatic bone correction allows for improved
head image quality, without any additional post-processing.
• In order to optimize image quality versus radiation
dose, scans are provided within a maximum scan
field of 300 mm with respect to the iso-center. No
recon job with a field of view exceeding those limits
will be possible. Therefore, patient positioning has to
be performed accurately to ensure a centered loca
tion of the skull.
-
79
Page 80

Head
Sinus
Indications:
Spiral mode for paranasal sinuses studies, e.g., sinusitis, mucocele, pneumatization, polyposis, tumor, corrections etc.
A range of 7 cm will be covered in 37 sec.
Sinus 2
kV 130
Effective mAs 60
Rotation time 1.0 sec
Slice collimation 1.0 mm
Slice width 3.0 mm 1.25 mm
Feed/Rotation 2.0 mm
Pitch Factor 1.0
Increment 3.0 mm 0.8 mm
Kernel H70s H70s
CTDIVol
Effective dose Male: 0.21 mSv
Contrast medium IV injection
Start delay 60 sec
Flow rate 2 ml/sec
Total amount 50 – 60 ml
80
13.66 mGy
Female: 0.22 mSv
nd
reconstr.
Page 81

Head
Hints
• An automatic bone correction and an advanced algorithm allows for improved head image quality, without any additional post-processing.
• In order to optimize image quality versus radiation
dose, scans are provided within a maximum scan
field of 300 mm with respect to the iso-center. No
recon job with a field of view exceeding those limits
will be possible. Therefore, patient positioning has to
be performed accurately to ensure a centered location of the skull.
• For image reconstruction of soft tissue, use kernel
H31s.
81
Page 82

Head
SinusSeq
Indications:
Sequential mode for paranasal sinuses studies, e.g.,
sinusitis, mucocele, pneumatization, polyposis, tumor,
corrections etc.
A range of 4.2 cm will be covered.
SinusSeq
kV 130
Effective mAs 120
Rotation time 1.0 sec
Slice collimation 1.5 mm
Slice width 3.0 mm
Feed/Scan 3.0 mm
Kernel H70s
CTDIVol
Effective dose Male: 0.22 mSv
27.32 mGy
Female: 0.24 mSv
Contrast medium IV injection
Start delay 60 sec
Flow rate 2 ml/sec
Total amount 50 – 60 ml
82
Page 83

Head
Hints
• An automatic bone correction and an advanced algorithm allows for improved head image quality, without any additional post-processing.
• In order to optimize image quality versus radiation
dose, scans are provided within a maximum scan
field of 300 mm with respect to the iso-center. No
recon job with a field of view exceeding those limits
will be possible. Therefore, patient positioning has to
be performed accurately to ensure a centered location.
• For image reconstruction of soft tissue, use kernel
H31s.
83
Page 84

Head
Orbita
Indications:
Spiral mode for orbital studies, e.g., fracture.
A range of 2 cm will be covered in 12 sec.
Orbita 2
kV 130
Effective mAs 100
Rotation time 1.0 sec
Slice collimation 1.0 mm
Slice width 3.0 mm 1.25 mm
Feed/Rotation 2.0 mm
Pitch Factor 1.0
Increment 3.0 mm 0.8 mm
Kernel H70s H70s
CTDIVol
Effective dose Male:
Contrast medium IV injection
Start delay 60 sec
Flow rate 2 ml/sec
Volume 50 – 60 ml
22.77 mGy
0.10
mSv
Female:
0.11
mSv
nd
reconstr.
84
Page 85

Head
Hints
• An automatic bone correction and an advanced algorithm allows for improved head image quality, without any additional post-processing.
• In order to optimize image quality versus radiation
dose, scans are provided within a maximum scan
field of 300 mm with respect to the iso-center. No
recon job with a field of view exceeding those limits
will be possible. Therefore, patient positioning has to
be performed accurately to ensure a centered location of the skull.
• For image reconstruction of soft tissue, use kernel
H31s.
85
Page 86

Head
Dental
This is the scan protocol for the syngo Dental CT application package. It is used for evaluation and reformatting of the upper and lower jaws.
It enables the display and measurement of the bone
structures of the upper and lower jaw as the basis for
planning in oral surgery.
Indications:
Spiral mode for dental studies.
A range of 5 cm will be covered in 27 sec.
Dental
kV 130
Effective mAs 45
Rotation time 1.0 sec
Slice collimation 1.0 mm
Slice width 1.25 mm
Feed/Rotation 2.0 mm
Pitch Factor 1.0
Increment 0.5 mm
Kernel H60s
CTDIVol
Effective dose Male: 0.13 mSv
10.25 mGy
Female: 0.16 mSv
Load the study into the application “syngo Dental CT”.
For further information, please refer to the chapter
"syngo Dental CT".
86
Page 87

Head
88
87
Page 88
Neck
Overview
– Neck
Spiral mode for soft tissue routine neck studies
Page 89

Neck
Hints in General
• Topogram: Lateral, 256 mm
• Patient positioning
Patient lying in supine position, hyperextend neck
slightly, secure head well in head holder.
• Patient respiratory instruction:
do not breathe, do not swallow.
• For contrast studies, CARE Bolus may be used to optimize the bolus timing.
• For image reconstruction of bone structures, use kernel B60.
89
Page 90

Neck
Body Kernels
• As standard kernels for body tissue studies B31s or
B41s are recommended; softer images are obtained
with B20s.
• For higher sharpness, as is required e.g., in patient
protocols for cervical spine, shoulder, extremities,
thorax, the kernels B50s, B60s, B70s are available.
• In case of 3D study only, use kernel B20s and at least
50% overlapping for image reconstruction.
Patient positioning is very important for artifact-free
images. The thoracic girdle should be positioned as far
as possible in the caudal direction. This can be done
using a strap with a permanent loop or Velcro fastener
at its end. The ends of the strap must be attached to
the patients wrists. Then the strap must be wrapped
around the patients feet with his legs extended and
under tension. The entire thoracic girdle is thus pulled
toward the patients feet.
90
Page 91

Neck
92
91
Page 92

Neck
Neck
Indications:
For soft tissue spiral studies in the cervical region, e.g.,
tumors, lymphoma, abscesses etc.
A typical range of 20 cm will be covered in 42 sec.
Neck
kV 130
Effective mAs 70
Rotation time 1.0 sec
Slice collimation 2.5 mm
Slice width 5.0 mm
Feed/Rotation 5.0 mm
Pitch Factor 1.0
Increment 5.0 mm
Kernel B50s
CTDIVol
Effective dose Male: 1.79 mSv
7.55 mGy
Female: 1.87 mSv
Contrast medium IV injection
Start delay 45 sec.
Flow rate 2.0 ml/sec.
Total amount 120 ml
Page 93

Neck
Hints
• Due to its iodine content, the thyroid gland is hyperdense in relation to the neighboring muscles both
before and after an IV CM injection. For displays of
the parotid, thyroid or the floor of the mouth, the
slice thickness should be < 5 mm and the length of
the range should be adapted to match the anatomic
region.
• Target the FoV to ensure adequate coverage of the
region of interest in the upper neck & middle neck
levels as well as to include the axilla in the lower
neck level if required.
93
Page 94

Shoulder
Overview
– Shoulder
Spiral mode for bone shoulder routine studies
94
Page 95

Shoulder
Hints in General
• Topogram: TOP, 256 mm.
• Patient positioning:
Patient lying in supine position, the uninjured arm
placed above the head, the injured arm placed flat
against his body. Position side under examination in
the center and support the other side with a Bocollo
pillow.
• If only one side is examined, it is advisable to enter
the side examined in the comment line.
• Contrast medium is required for soft tissue mass
evaluation.
• To further optimize MPR image quality, we recommend that you reduce one or more of the following
parameters: collimation, reconstruction increment,
and slice width for image reconstruction.
Body Kernels
• As standard kernels for body tissue studies B31s or
B41s are recommended; softer images are obtained
with B20s.
• For higher sharpness, as is required e.g., in patient
protocols for cervical spine, shoulder, extremities,
thorax, lung, the kernels B50s, B60s, B70s are avail
able.
-
95
Page 96

Shoulder
Shoulder
Indications:
Spiral mode for bone studies and soft tissue, e.g., evaluation of joint cavities, masses, trauma, dislocations,
orthopedic indications etc.
A scan range of 10 cm will be covered in 35 sec.
96
Page 97

Shoulder
Shoulder 2nd reconstruction
kV 130
Effective mAs 70
Rotation time 1.0 sec
Slice
collimation
Slice width 3.0 mm 2.0 mm
Feed/Rotation 3.0 mm
Pitch Factor 1.0
Increment 3.0 mm 1.5 mm
Kernel B60s
CTDIVol
Effective dose Male:
Hints
• Use raw data to review a target region if necessary.
• For image reconstruction of soft tissue, use kernel
B31s and a slice width of 5.0 mm.
• Coronal and sagittal 2D planar reconstructions are
important for evaluation of the joint space & bursa
sacs in CT arthograms.
• 3D renderings are helpful for complex fractures &
dislocations.
1.5 mm
7.55 mGy
0.94
mSv
Female:
1.13
mSv
97
Page 98

Thorax
Overview
– ThoraxRoutine/ThoraxRoutine08s
Spiral mode for routine chest studies
– ThoraxFast
Spiral mode for fast chest studies
– ThoraxHRSeq
Sequential mode for high resolution lung studies
– LungLowDose
Spiral mode with very low dose for early visualization of pathologies
98
Page 99

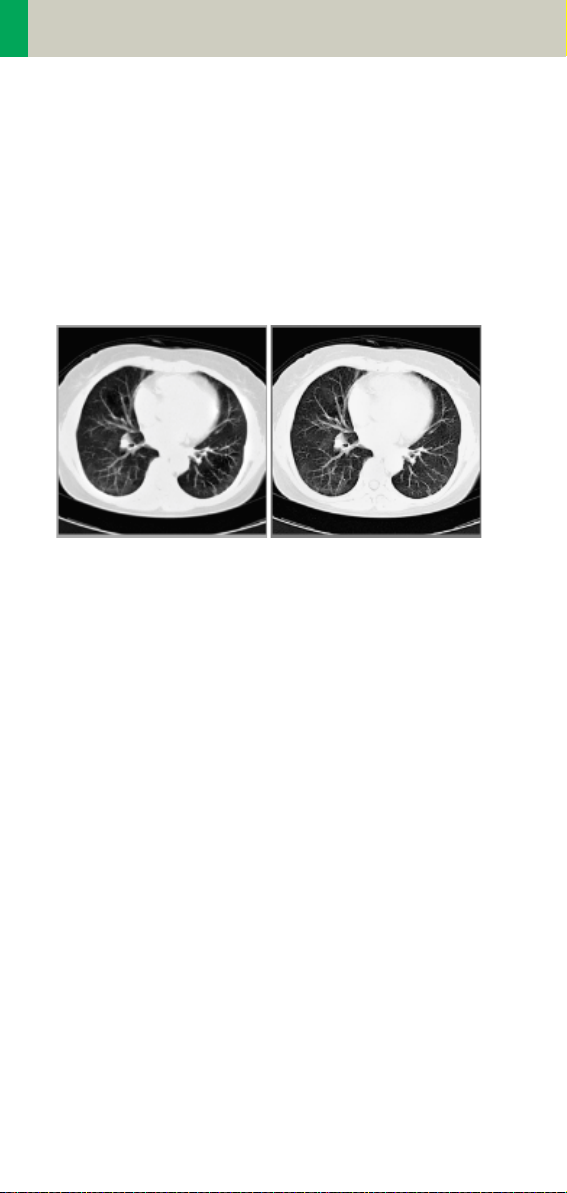
Thorax
Hints in General
• Topogram: TOP, 512 mm.
• Patient positioning: Patient lying in supine position,
arms positioned comfortably above the head in the
head-arm rest, lower legs supported.
• Contrast medium administration: in general, IV
injections are employed in all mediastinal examinations, but not in routine high resolution studies of
diffuse interstitial lung diseases. An IV contrast
medium injection improves the vascular opacifica
tion and facilitates the visualization of the lesions,
lymph nodes and the vessels.
• Stasis of contrast medium in the arm & superior vena
cava often result in high density streak artifacts
either in the region of the aortic arch or in the region
of the subclavian vein. A caudo-cranial (bottom to
top) scanning direction should be used to reduce this
artifact – by simply acquiring the data in this region
at the later phase of the spiral scan. In addition, if the
patient cannot hold his/her breath for the duration of
the entire scan, breathing motion will be less appar
ent in the apex than in the lower lobes.
• CARE Bolus may be used to optimize the bolus timing. Set the ROI for monitoring scan in the aorta at
the level of the diaphragm with triggering threshold
of 120 HU, or use manual triggering.
-
-
99
Page 100

Thorax
• Lung images should be documented in both soft tissue window and lung window.
• It is also possible to interleave the soft tissue & lung
setting images in one film sheet. This can be set up
in the configuration for filming.
• To further optimize MPR image quality, we recommend that you reduce one or more of the following
parameters: collimation, reconstruction increment,
and slice width for image reconstruction.
100
 Loading...
Loading...