Page 1

Obstetrical Care
SERVICE GUIDE
Avalon Fetal Monitor
FM20
FM30
FETAL MONITORING
Page 2

Printed in Germany 07/05
*M2703-9000A*
Part Number M2703-9000A
4512 610 10021
S
Page 3
1Table of Contents
1 Introduction 1
Who Should Read This Guide 1
What to Do Next 1
Repair Strategy 2
Manufacturer’s Information 2
Passwords 3
Warnings and Cautions 3
2 Site Preparation 5
Introduction 5
Site Planning 5
Roles and Responsibilities 5
Site Preparation Responsibilities 5
Procedures for Local Staff 6
Procedures for Philips Personnel 7
Site Requirements 7
Space Requirements 7
Environmental Requirements 7
Safety Requirements (Customer or Philips) 8
Electrical Requirements (Customer or Philips) 8
Connecting Non-Medical Devices 8
Cabling Options and Requirements for Connection to OB TraceVue 9
Mounting Options 9
Input Devices 10
3 Installation Instructions 11
Initial Inspection 11
Mechanical Inspection 11
Electrical Inspection 11
Claims for Damage 11
Repackaging for Shipment or Storage 12
Mounting Instructions 12
Line Voltage Selection 12
Connecting the Monitor to AC Mains 12
Connecting the Monitor to Non-Medical Devices 13
Checking and Setting Line Frequency 13
Checking/Setting Paper Scale 13
Checking/Setting Paper Speed 13
PS/2 Keyboard/Mouse 14
i
Page 4
4 Theory of Operation 15
Monitor Hardware Overview 15
Power Supply 16
Connector Block 16
Bus Master Board 16
Main CPU Board 16
Fetal Recorder (Thermal Printer Unit) 16
Recorder Adapter Board 17
Thermal Line Printhead (TLPH) 17
Paper Sensor 17
Stepper Motor 17
LCD Display and Touchscreen 17
Noninvasive Blood Pressure Assembly 17
SpO2 Assembly 17
Input/Output Interface Boards 18
Transducer Hardware Overview 18
Tr a n s d u c e r Ty p e s 19
Functional Description of the Transducer CPU 19
CPU (Micro Controller) 19
Analog-to-Digital Converter 19
Communication Transceiver (CAN Bus Driver) 19
EEPROM 19
Toco Transducer Frontend 19
Ultrasound Transducer Frontend 20
Toco+ Transducer Frontends 20
To co Fr o n te n d 20
IUP Frontend 20
ECG Frontend 20
5 Interfaces 21
LAN / RS232 Interface 21
Dual PS/2 Interface 21
6 Testing and Maintenance 23
Recommended Frequency 23
When to Perform Test Blocks 24
Test Reporting 25
How to Carry Out the Test Blocks 25
Preventive Maintenance Procedures 26
Other Regular Tests 26
Visual Check 26
Fetal Recorder Maintenance 26
Testing Transducers and Patient Modules 26
Ultrasound Transducer Electrical Check 26
Toco Transducer Electrical Check 28
ii
Page 5
Testing the Patient Module (M2738A)/Toco+ Transducer (M2735A): DECG Mode 28
Testing the Patient Module (M2738A)/Toco+ Transducer (M2735A): MECG Mode 29
Testing the Patient Module (M2738A)/Toco+ Transducer (M2735A): IUP Mode 30
Performance Assurance Tests 31
Noninvasive Blood Pressure Performance Tests 31
Accuracy Test 31
Leakage Test 32
Linearity Test 32
Valve Test 32
SpO2 Performance Test 32
Safety Tests 33
Warnings, Cautions, and Safety Precautions 33
Electrical Isolation Diagram 34
Safety Test Procedures 34
S(1): Sum of Functional Earth and Enclosure Leakage Current Test 34
S(2): Patient Leakage Current - Single Fault Condition (SFC), Mains on Applied Part 35
System Test 36
What is a Medical Electrical System? 36
General Requirements for a System 36
System Example 36
Touchscreen Calibration 37
Disabling/Enabling Touch Operation 38
Checking the Fetal Recorder Offset 39
Setting the Fetal Recorder Offset 39
Fetal Recorder Selftest Report 40
7 Troubleshooting 41
Who Should Perform Repairs 41
Replacement Level Supported 41
Hardware Revision Check 41
Software Revision Check 42
Obtaining Replacement Parts 42
Troubleshooting Guide 42
Checks for Obvious Problems 42
Checks Before Opening the Instrument 42
Checks with the Instrument Switched On, AC connected 43
Individual Parameter INOPs 43
Initial Instrument Boot Phase 44
Troubleshooting Tables 44
How to Use the Troubleshooting Tables 44
Boot Phase Failures 45
Screen is Blank 46
Touchscreen Not Functioning 46
General Monitor INOP Messages 47
Keyboard/Mouse Not Functioning 48
Alarm Tones 48
iii
Page 6
Alarm Behavior 48
Fetal Recorder 48
LAN / RS232 51
Tr a n s du c e r s 5 2
Status Log 53
Troubleshooting with the Support Tool 54
Troubleshooting the Individual Measurements or Applications 54
8 Disassembly and Reassembly 55
Introduction 55
Serial Numbers 56
Removing the Top Cover Assembly 57
Removing the Display Assembly 59
Replacing the Display Assembly 62
Recorder Disassembly 64
Removing the Drawer Assembly 64
Replacing the Drawer Assembly 66
Removing the Recorder Chassis 68
Removing the Thermal Line Printhead (TLPH) 72
Replacing the TLPH 73
Replacing the Recorder Chassis 74
Removing the Paper Sensor Assembly 75
Replacing the Paper Sensor Assembly 75
Removing the Recorder Adapter Board 75
Replacing the Recorder Adapter Board 77
Removing the Stepper Motor 78
Replacing the Stepper Motor 79
Replacing the Top Cover Assembly 80
Removing the Power Supply Assembly 81
Replacing the Power Supply Assembly 82
Removing the Noninvasive Blood Pressure Assembly 82
Replacing the Noninvasive Blood Pressure Assembly 84
Removing the SpO2 Assembly 85
Replacing the SpO2 Assembly 86
Removing the Interface Boards 87
Removing the Main CPU Board 88
Replacing the Main CPU Board 89
Exchanging the Loudspeaker 89
Exchanging the Transducer Cable 90
Exchanging the Transducer Belt Button 92
9 Parts 95
Monitor 95
Tr a n s d u c e r s 96
Patient Modules 97
Mounting Hardware 97
iv
Page 7
Assembly and Kit Contents 98
Bottom Housing Assembly (M2703-64101) 98
Power Supply Assembly (M2703-60001) 99
Top Cover Assembly (M2703-60052) 99
Top Cover Housing (M2703-64102) 100
Stepper Motor Assembly (M2703-60004) 100
Paper Sensor Assembly (M2703-60003) 100
Drawer Assembly (M2703-64651) 100
Display Assembly (M2703-64503) 101
Transducer Cable Assembly (M2735-64201) 101
Small Parts Kit - Top (M2735-64202) 102
Small Parts Kit - Bottom (M2703-64203) 102
Belt Button Kit (M2703-64204) 102
10 Upgrades 105
11 Understanding Configuration 107
What is Configuration Mode? 107
Understanding Settings 108
Entering and Leaving Configuration Mode 108
Storing Changes in the User Defaults 109
Loading the Factory Default 109
Loading the User Defaults 110
Loading Configurations Using the Support Tool 110
About Configuration Files (.cfg) 111
Selecting the Correct Configuration 111
12 Configuration Settings Appendix 113
Documenting Monitor Configurations 113
Using the Configuration Tables 113
Configuration Table Example 114
Understanding Configuration Implications 114
Measurement-Related Settings 115
Color Configuration 115
Configuring FHR (Ultrasound) 115
FHR Configuration Implications 115
Configuring Toco 116
Configuring IUP 116
Configuring DFHR (DECG) 116
DFHR Configuration Implications 116
Configuring MHR (ECG) 117
ECG Configuration Implications 117
Configuring Pulse 118
Configuring SpO
Configuration Implications 119
SpO
2
Configuring Noninvasive Blood Pressure (NBP) 119
2
119
v
Page 8

NBP Configuration Implications 120
Monitor-Related Settings 121
Configuring Alarms 121
Alarm Settings Configuration Implications 121
Configuring the NST Timer 122
NST Timer Configuration Implications 122
Configuring Fetal Recorder Settings 122
Recorder Configuration Implications 123
Configuring User Interface Settings 123
User Interface Configuration Implications 124
Hardware Settings 124
Global Settings 125
Global Settings Configuration Implications 125
vi
Page 9

1
1Introduction
This Service Guide contains technical details for the Avalon FM20 and FM30 Fetal/Maternal
Monitors. It provides a technical foundation to support effective troubleshooting and repair. It is not a
comprehensive, in-depth explanation of the product architecture or technical implementation. It offers
enough information on the functions and operations of the monitoring systems so that engineers who
repair them are better able to understand how they work. It covers the physiological measurements and
the monitor hardware that acquires and displays them.
The Avalon FM20/FM30 Fetal Monitor Service Guide supplements the maintenance and
troubleshooting procedures, carried out by the operator, that are described in the Instructions for Use.
Refer to the Instructions for Use for maintenance and troubleshooting procedures that may be
performed during normal operation.
Only qualified service personnel should attempt to install the system, disassemble the monitor, remove
or replace any internal assemblies, or replace the transducer cable or belt buttons.
Who Should Read This Guide
This guide is for biomedical engineers or technicians responsible for troubleshooting, repairing, and
maintaining Philips’ Avalon fetal monitors.
You must:
•understand English
• be familiar with standard medical equipment installation procedures
• be familiar with current conventional technical terms as used throughout this guide
What to Do Next
Familiarize yourself with the contents of this guide and the Instructions for Use before attempting to
service or repair the system.
1
Page 10

1 Introduction Repair Strategy
Repair Strategy
The Service Support Tool software helps you to determine whether a fault is a hardware or software
problem. The main replaceable parts are:
• unit exchange for the transducers
•replacement of
– the top cover assembly
– the bottom housing
– the power supply assembly
– the display assembly
– the recorder adapter board
– the paper drawer assembly
– the paper sensor assembly
– the stepper motor assembly
–the SpO
– the noninvasive blood pressure assembly
–the main CPU board
– the bus master board
– the socket connector block
–the transducer cable
– the transducer belt button
See Chapter 9, “Parts” for part numbers, and Chapter 8, “Disassembly and Reassembly” for repair
details.
assembly
2
Repair or replacement of individual components on the boards is not supported, and should never be
attempted.
For tests that you are required to perform after repairs, refer to “When to Perform Test Blocks” on
page 24.
Manufacturer’s Information
© Copyright 2003 - 2005. Koninklijke Philips Electronics N.V.
All Rights Reserved.
Philips Medizin Systeme Böblingen GmbH
Hewlett-Packard-Str. 2
71034 Böblingen, Germany
2
Page 11

Passwords 1 Introduction
Passwords
In order to access different modes within the monitor a password may be required. The passwords are
listed below.
Monitoring Mode: No password required
Configuration Mode: 71034
Demo Mode: 14432
Service Mode: 1345
Refer to Chapter 11, “Understanding Configuration” before making any changes to the monitor
configuration.
Warnings and Cautions
In this guide:
•A warning alerts you to a potential serious outcome, adverse event or safety hazard. Failure to
observe a warning may result in death or serious injury to the user or patient.
•A caution alerts you where special care is necessary for the safe and effective use of the product.
Failure to observe a caution may result in minor or moderate personal injury or damage to the
product or other property, and possibly in a remote risk of more serious injury.
3
Page 12

1 Introduction Warnings and Cautions
4
Page 13

Introduction
This section describes the procedures you should follow to plan and prepare a site for an Avalon
FM20/FM30 fetal monitor installation.
• Site planning.
• Roles and responsibilities for local and Philips personnel.
Site Planning
The careful planning of the site for the FM20/FM30 monitor is essential for its safe and efficient
operation. A consulting schedule should be established between the Customer and Philips Sales and
Support Representatives, to ensure that all preparations are completed when the system is delivered.
2
2Site Preparation
The site planning phases prior to equipment installation are:
Location: Planning the location of the various system components.
Environment: Confirming and correcting, as necessary, the environment of the proposed installation
site(s).
System Capabilities: Explaining the possibilities for system expansion.
Mounting: Referencing the mounting hardware information website for the listing of suitable
mounting hardware recommended for use with the various system components, and all details on the
available mounts and accessories.
Cabling: Identifying the requirements for the cabling, conduiting and faceplates for connecting the
various system components.
Roles and Responsibilities
This section describes the procedures necessary to prepare a site for a system installation. The
procedures are grouped into two parts: procedures that local staff or contractors are responsible for, and
procedures that Philips personnel are responsible for.
Site Preparation Responsibilities
Local Staff
• Ensure that all safety, environmental and power requirements are met.
• Provide power outlets.
• Prepare mounts, and consult Philips for detailed mounting requirements.
5
Page 14
2 Site Preparation Introduction
• Pull cables, install conduit, install wallboxes.
Philips Personnel
• Provide the customer with the safety, environmental and power requirements.
•Assemble mounts, as necessary.
• Provide requirements for cabling.
Procedures for Local Staff
The following tasks must be completed before the procedures for Philips personnel may be started.
• Providing Power Outlets
Provide a power outlet in the vicinity (1 m or 3 ft) or any peripheral equipment.
WARNING Only the power cables provided with the system may be used. For reasons of safety, power (mains)
extension cables or adapters shall not be used.
• Preparing Mounts
Where ceiling, wall, or shelf mounts are required for mounting the equipment, the customer is
responsible for the following:
– Providing and installing all hardware which is required to install the mounting hardware supplied
by Philips as detailed in the installation notes.
– Making sure that all ceilings, walls, and mounting rails that supports mounting hardware are
suitable for their proposed load.
WARNING It is the customer's responsibility to have the attachment of the mounting hardware to the ceiling, wall,
or mounting rail and the construction of the ceiling, wall, or mounting rail evaluated for structural
integrity and compliance with all local, state and any other required codes by a registered, professional,
structural and/or mechanical engineer.
Although considerable effort has been made to ensure the safety of the ceiling mount installation and
or mounting guidelines, it is to be understood that the installation itself is beyond the control of Philips
Medical Systems. Accordingly, Philips Medical Systems will not be responsible for the failure of any
such installation.
• Providing Conduit
– Providing conduit and/or trunking of a sufficient cross-sectional area for the planned cables and
possible future expansion (for additional components or systems).
– Providing and/or installing suitable wall boxes to accommodate the faceplates.
•Pulling Cables
WARNING NEVER run power cables through the same conduit or trunking used for system cables.
•Installing Wall Boxes
6
Page 15
Site Requirements 2 Site Preparation
It is the customer's responsibility to provide and install wallboxes to house faceplates. The customer
must notify the Philips installation coordinator of which size is to be used.
Procedures for Philips Personnel
Before you begin the procedures in the installation sections, ensure that the customer has completed all
necessary preparations outlined in the previous section, “Procedures for Local Staff.”
Site Requirements
The site requirements are listed in this section.
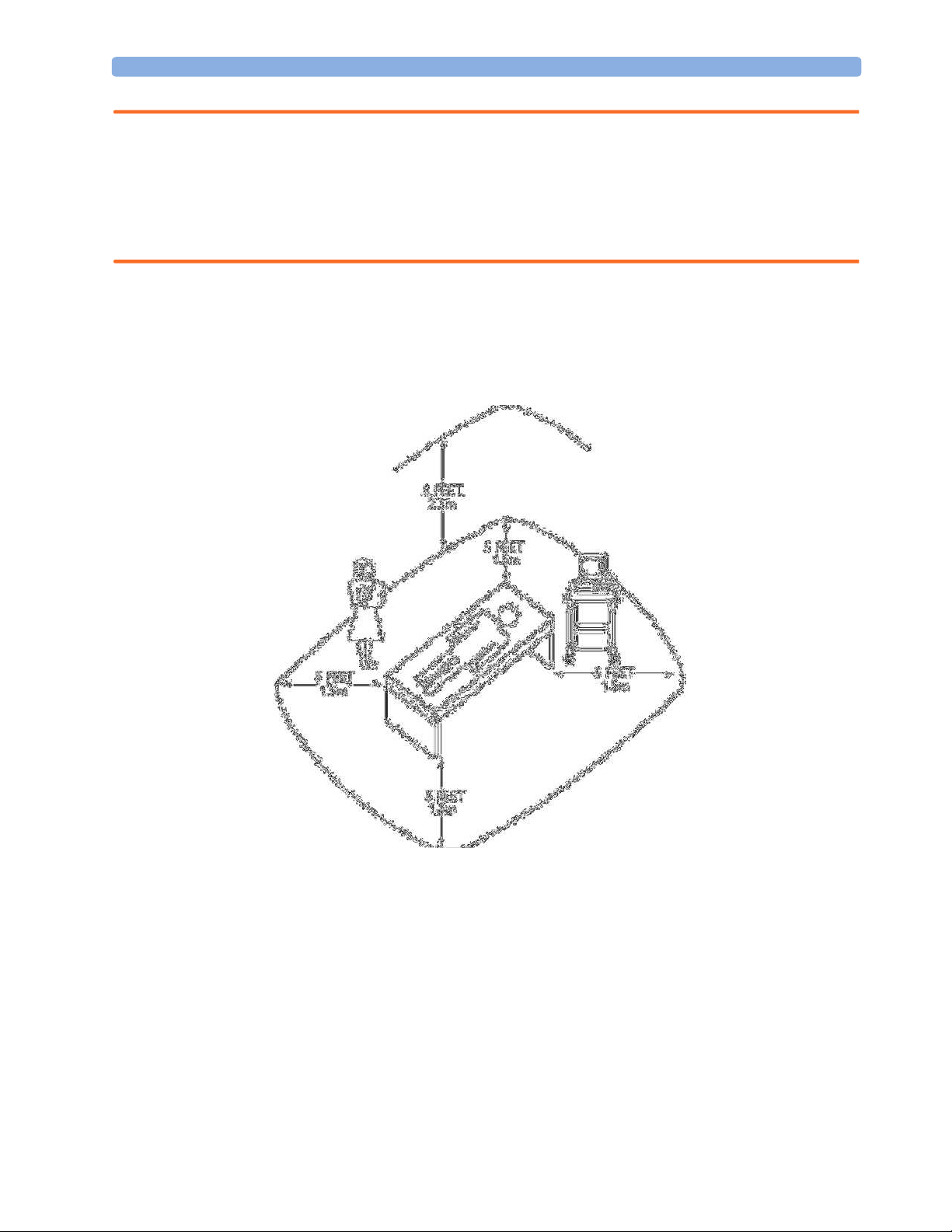
Space Requirements
The situating of the monitor should be planned such that the nursing staff are able to monitor the
patient with relative ease, with all patient connectors and controls readily available and the displays
clearly visible. The location should also allow access to service personnel without excessive disruption
and should have sufficient clearance all round to allow air circulation.
Dimensions and weight:
Monitor:
Size (W x H x D): 335 x 286 x 133 mm (13.2 x 11.3 x 5.2 in)
Weight; 5.1 kg (11.2 lb)
Transducer:
Size (diameter): 83 mm (3.27 in)
Weight (without cable): 190g (6.7 oz.)
Environmental Requirements
The environment where the FM20/FM30 monitor will be used should be reasonably free from
vibration, dust and corrosive or explosive gases. The ambient operating and storage conditions for the
FM20/FM30 monitor must be observed. If these conditions are not met, the accuracy of the system
will be affected and damage can occur.
.
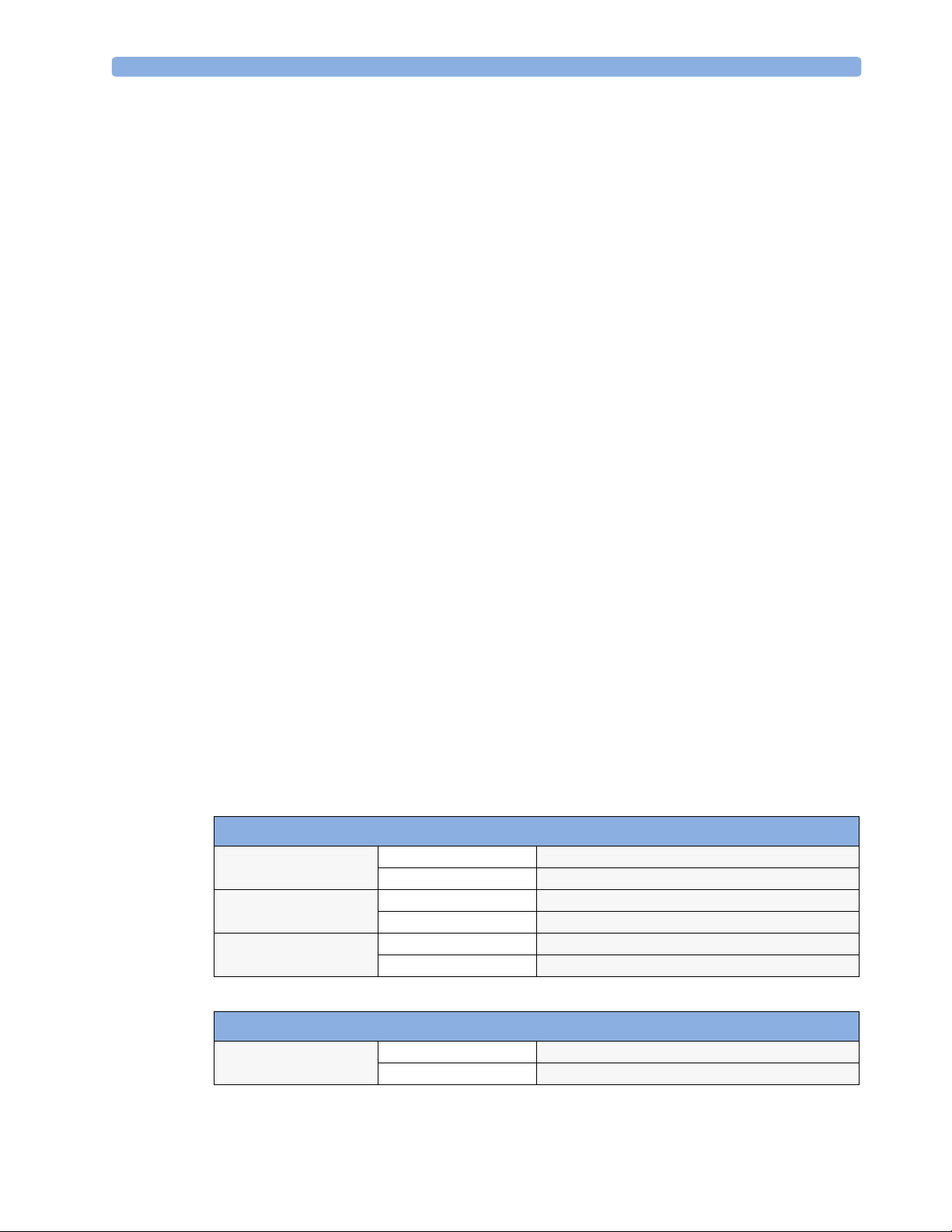
Monitor (M2702A/M2703A)
Temperature Range Operating 0°C to 45°C (32°F to 113°F)
Storage
Humidity Range Operating <95% relative humidity @ 40°C/104°F
Storage
Altitude Range Operating -500 to 3000 m/-1640 to 9840 ft.
Storage
-20°C to 60°C (-4°F to 140°F)
<90% relative humidity @ 60°C/140°F
-500 to 3000 m/-1640 to 9840 ft.
Transducers (M2734A/M2735A/M2736A)
Temperature Range Operating 0°C to 40°C (32°F to 104°F)
Storage
-40°C to 60°C (-40°F to 140°F)
7
Page 16
2 Site Preparation Site Requirements
Transducers (M2734A/M2735A/M2736A)
Humidity Range Operating <95% relative humidity @ 40°C/104°F
Storage
Altitude Range Operating -500 to 3000 m/-1640 to 9840 ft.
Storage
SpO2 Sensors
Operating Temperature Range 0°C to 37°C (32°F to 98.6°F)
<90% relative humidity @ 60°C/140°F
-500 to 3000 m/-1640 to 9840 ft.
Safety Requirements (Customer or Philips)
The monitor is an electrical Class II device in which the protection against electric shock does not rely
on basic insulation and a protective earth conductor but on double and/or reinforced insulation.
WARNING • Always use the supplied power cord with the earthed mains plug to connect the monitor to an
earthed AC mains socket. Never adapt the mains plug from the power supply to fit an unearthed AC
mains socket.
• The protective earth conductor is required for EMC purposes. It has no protective function against
electric shock! The protection against electric shock in this device is provided by double and/or
reinforced insulation.
• Do not use additional AC mains extension cords or multiple portable socket-outlets. If a multiple
portable socket-outlet without an approved isolation transformer is used, the interruption of its
protective earthing may result in enclosure leakage currents equal to the sum of the individual earth
leakage currents, so exceeding allowable limits.
Electrical Requirements (Customer or Philips)
Line Voltage Connection
The FM20/FM30 monitor uses < 60 W.
Line Voltage: the FM20/FM30 monitor may be operated on ac line voltage ranges of
100 to 240V (50/60 Hz).
Connecting Non-Medical Devices
The standard IEC-60601-1-1 applies to any combination of devices, where at least one is a medical
device. Therefore IEC-60601-1-1 must still be met after all devices are connected.
8
Page 17
Site Requirements 2 Site Preparation
WARNING • Do not use a device in the patient vicinity if it does not comply with IEC-60601-1. The whole
installation, including devices outside of the patient vicinity, must comply with IEC-60601-1-1.
Any non-medical device, including a PC running an OB TraceVue system, placed and operated in
the patient’s vicinity must be powered via an approved isolation transformer that ensures mechanical
fixing of the power cords and covering of any unused power outlets.
• Do not connect any devices that are not supported as part of a system.
Whenever you combine equipment to form a system, for example, connecting the monitor to an OB
TraceVue system, perform a system test according to IEC 60601-1-1 (see “System Test” on page
36).
Figure 1 Equipment Location in the Patient Vicinity
Cabling Options and Requirements for Connection to OB TraceVue
For cabling options and requirements for connection to an OB TraceVue system, refer to the OB
TraceVue Site Preparation Guide and the OB TraceVue Service Guide.
Mounting Options
See “Mounting Hardware” on page 97 for a list of mounting options. Refer to “Mounting
Instructions” on page 12, or contact your local Philips representative for advice on mounting the
monitor.
9
Page 18
2 Site Preparation Site Requirements
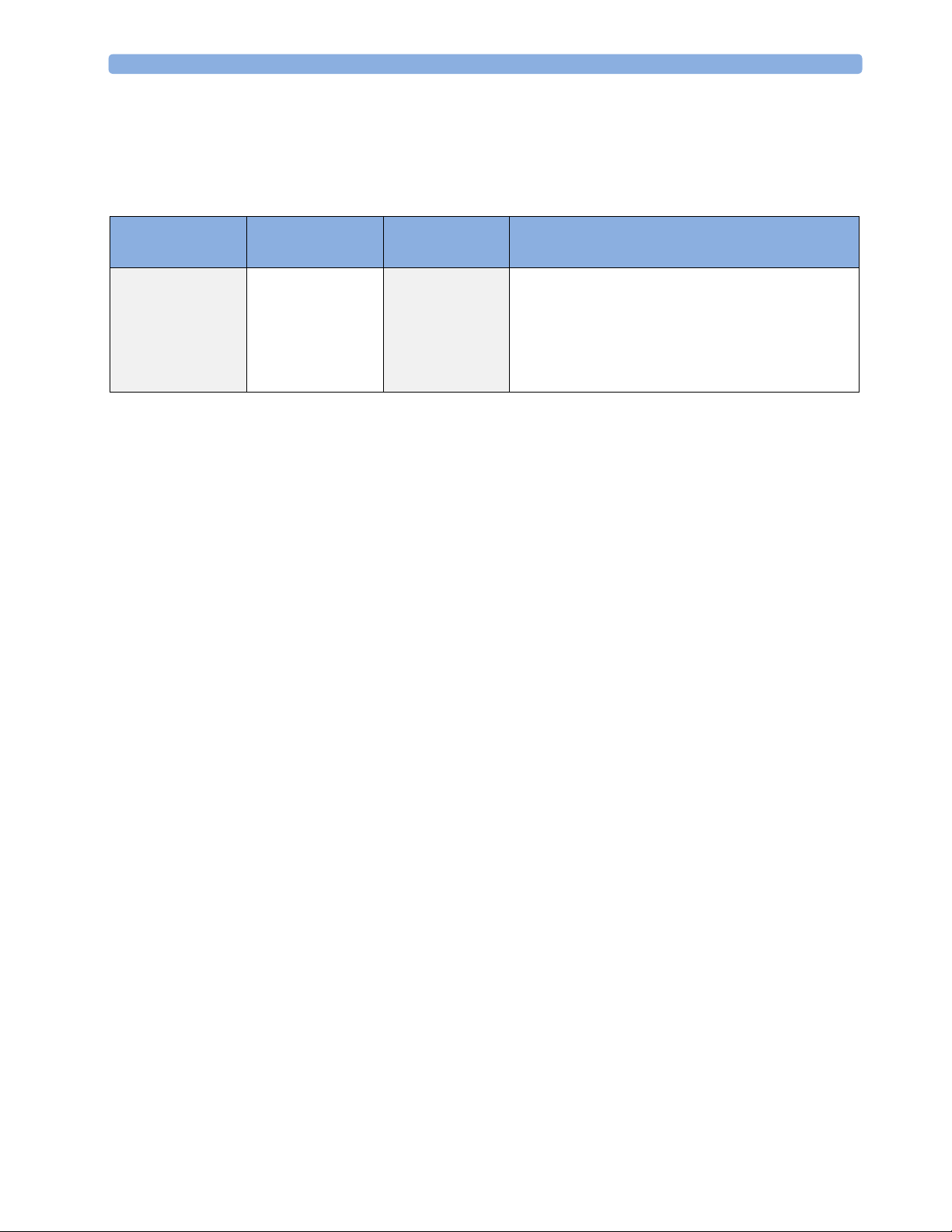
Input Devices
The following tables describes the input devices which can be connected to the monitor via the
optional PS/2 interface.
Product Option
Number
M8024A #A01 862454 9898 031 24741 Slimline Keyboard with integrated Trackball
M8024A #B01 M4046-60104 4512 610 00661 Optical Mouse USB / PS/2
M8024A #C01 M4046-60103 4512 610 00651 Wired Track Ball USB / PS2
M8024A #C02 M4046-60105 4512 610 00671 Wireless Track Ball
M8024A #C03 M4046-60106 4512 610 00681 Wired off table Track Mouse
Part Number 12NC Part
Number
Description
10
Page 19

3Installation Instructions
The information contained in this chapter, in addition to that given in the Instructions for Use, should
enable the monitor to be installed ready for use (the preparation and planning should be adhered to as
specified in the “Site Preparation” chapter). Safety checks and inspection procedures for mounts are
explained in the “Testing and Maintenance” chapter, and configuration of the system is explained in
the “Configuration” chapter.
Please keep the packing materials until you have completed the initial inspection, in case there is a
defect on arrival.
Initial Inspection
Inspect the delivery on arrival.
3
Mechanical Inspection
Open the shipping container(s) and examine each part of the instrument for visible damage, such as
broken connectors or controls, or scratches on the equipment surfaces. If the shipping carton/container
is undamaged, check the cushioning material and note any signs of severe stress as an indication of
rough handling in transit. This may be necessary to support claims for hidden damage that may only
become apparent during subsequent testing.
Electrical Inspection
The instrument has undergone extensive testing prior to shipment. Safety testing at installation is not
required (except in situations where devices are interconnected forming a system, see “Connecting
Non-Medical Devices” on page 143). An extensive self check may be performed. This
recommendation does not supersede local requirements.
All tests are described in the “Testing and Maintenance” chapter of this manual.
Claims for Damage
When the equipment is received, if physical damage is evident or if the monitor does not meet the
specified operational requirements of the patient safety checks or the extended self check, notify the
carrier and the nearest Philips Sales/Support Office at once. Philips will arrange for immediate repair or
replacement of the instrument without waiting for the claim settlement by the carrier.
11
Page 20
3 Installation Instructions Repackaging for Shipment or Storage
Repackaging for Shipment or Storage
If the instrument is to be shipped to a Philips Sales/Support Office, securely attach a label showing the
name and address of the owner, the instrument model and serial numbers, and the repair required (or
symptoms of the fault). If available and reusable, the original Philips packaging should be used to
provide adequate protection during transit. If the original Philips packaging is not available or reusable
please contact the Philips Sales/Support Office who will provide information about adequate
packaging materials and methods.
Mounting Instructions
Every type of compatible mounting solution is delivered with a complete set of mounting hardware
and instructions. Refer to the Site prep chapter for a list of mounting options. Refer to the
documentation delivered with the mounting hardware for instructions on assembling mounts.
WARNING It is the customer's responsibility to have the attachment of the mounting hardware to the ceiling, wall,
or mounting rail and the construction of the ceiling, wall, or mounting rail evaluated for structural
integrity and compliance with all local, state and any other required codes by a registered, professional,
structural and/or mechanical engineer.
Ensure that this commitment has been met before assembling mounts.
Line Voltage Selection
You do not need to set the line voltage, as this is done automatically by the power supply. The monitor
has a wide-range power supply that allows you to operate the monitor from an AC (alternating current)
power source of 100 V to 240 V (± 10%) and 50 to 60 Hz (± 5%).
Connecting the Monitor to AC Mains
The monitor is an electrical Class II device in which the protection against electric shock does not rely
on basic insulation and a protective earth conductor but on double and/or reinforced insulation.
WARNING • Always use the supplied power cord with the earthed mains plug to connect the monitor to an
earthed AC mains socket. Never adapt the mains plug from the power supply to fit an unearthed AC
mains socket.
• The protective earth conductor is required for EMC purposes. It has no protective function against
electric shock! The protection against electric shock in this device is provided by double and/or
reinforced insulation.
12
• Do not use AC mains extension cords or multiple portable socket-outlets.
Page 21
Connecting the Monitor to Non-Medical Devices 3 Installation Instructions
Connecting the Monitor to Non-Medical Devices
Connect the monitor to an obstetrical surveillance system, such as OB TraceVue, via the optional
system interface. For cabling requirements, refer to “Cabling Options and Requirements for
Connection to OB TraceVue” on page 9. For safety-related information, refer to “Connecting NonMedical Devices” on page 8, and “System Test” on page 36.
Checking and Setting Line Frequency
Before using the monitor, check that the line frequency setting is correct for your location, and change
the setting if necessary in Configuration Mode.
WARNING An incorrect line frequency setting can affect the ECG filter, and disturb the ECG measurement.
Ensure the line frequency setting is correct.
To set the line frequency:
1 Enter the Main Setup menu.
2 Select Global Setting s.
3 Select Line Frequency and select 50Hz or 60Hz from the pop-up list.
Checking/Setting Paper Scale
You can check the paper Scale Type (US for paper with a scale of 30-240, or Europe for paper with a
scale of 50-210) in the Fetal Recorder menu. In Monitoring Mode, you can see this setting (grayed
out), but you cannot change it. It can be changed in Configuration Mode.
1 Enter the Main Setup menu by selecting the SmartKey .
2 Select Fetal Recorde r.
3 Check the current setting for Scale Type. If it is not appropriate, change it in the Fetal Recorder
menu in Configuration Mode:
Select Scale Type to toggle between US and Europe.
Checking/Setting Paper Speed
You can choose a paper speed of 1, 2, or 3 centimeters per minute (cm/min). The default setting is 3
cm/min.
As a change in paper speed results in a change in the appearance of a FHR trace, you are advised to
ensure ALL monitors in your institution are set to the same speed.
To set the paper speed:
1 Enter the Main Setup menu using the SmartKey .
2 Select Fetal Recorder.
3 In the Recorder menu, you can see the current speed setting. Select Recorder Speed.
4 Select the desired speed from the given choices: 1, 2 or 3 cm/min.
13
Page 22

3 Installation Instructions Checking and Setting Line Frequency
PS/2 Keyboard/Mouse
Switch off the monitor before connecting any PS/2 compatible device.
Connect the PS/2 connector to the PS/2 Interface board in the monitor at the slot indicated by the
appropriate symbol.
The default keyboard language setting for all initial configurations is “US”. However, the monitor will
not automatically select the best matching language for the keyboard depending on the language of its
software. This means that there is no such choice as “Automatic” for the keyboard language.
To configure the keyboard language manually, go to Service Mode, select Main Setup ->
Hardware -> Keyboard and then select the proper language. Please note that this setting does not
clone.
14
Page 23
4Theory of Operation
This chapter describes the functional operation of the monitor and the transducers. It incorporates features of
the mechanical design, indicating the physical relationship of the assemblies and components.
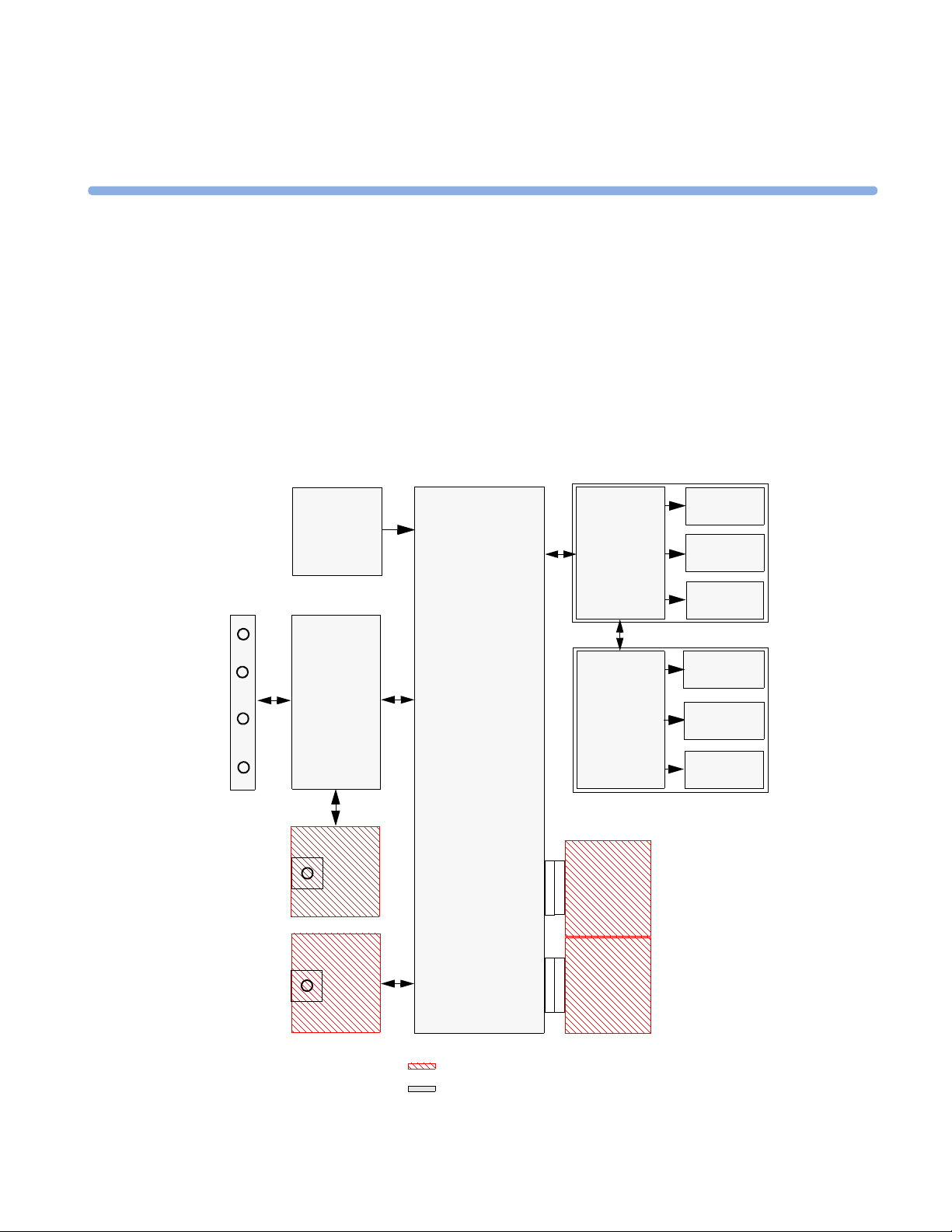
Monitor Hardware Overview
4
Power
Supply
Bus Master
Connector Block
SpO
2
Main CPU
Recorder
Adapter
Display
Adapter
IF Board 1
Thermal
Printhead
Paper
Sensor
Stepper
Motor
Touch
Screen
Display
Panel
Backlight
Converter
Fetal Recorder
Display Assembly
NIBP
IF Board 2
optional boards
standard boards
15
Page 24

4 Theory of Operation Power Supply
The monitor consists of nine main functional components:
• Power supply M2703-60001
• Connector Block (1253-8415)
• Bus Master Board (M2703-66460)
• Main CPU Board (M2703-66450)
• Fetal Recorder (Thermal Printer Unit)
• Display Assembly (M2703-64503)
• Noninvasive Blood Pressure Board (optional, M2703-64502)
•SpO
• Input /Output Interface Boards (optional):
Board (optional, M2703-66453)
2
– LAN / RS232 (M2703-67501)
– Dual PS/2 (M8086-67501)
Power Supply
The power supply is a wide-range input switching unit, with an output of 24V. It is located in the bottom
housing assembly.
Connector Block
Any compatible fetal transducer, patient module or remote event marker can be connected in any order to
the monitor via the sockets on the Connector Block. The Connector Block is located on the Bus Master
Board, and is exchangeable.
Bus Master Board
The signals from the transducers or sensors are conveyed from the sensor sockets on the Connector
Carrier Board (M2703-66421) to the Bus Master Board (M2703-66420).
The Bus Master Board is responsible for transducer detection, communicates with the connected
transducers via a CAN bus, and communicates parameter data to the Main CPU Board via a serial link for
further processing and display.
Main CPU Board
The Main CPU Board controls the monitor’s human interface, and is responsible for the final processing
of data from the Bus Master Board. It sends this data to the TFT display, and to the thermal printer unit
for recording traces and other patient data. It also controls the optional LAN/RS232 and PS/2 interface
boards.
Fetal Recorder (Thermal Printer Unit)
The fetal recorder is located in the Top Cover Assembly. The recorder consists of the following major
parts:
16
Page 25
LCD Display and Touchscreen 4 Theory of Operation
•Recorder Adapter Board
•Thermal Line Printhead (TLPH)
•Paper Sensor
•Stepper Motor
Recorder Adapter Board
Recorder signals are handled by the Recorder Adapter Board (M2703-66430), connected to the Main CPU
Board. Video signals to the display are also wired through this board, and connection to the Display
Adapter Board is made via a silver-colored 50-pin ribbon cable.
The recorder unit, including the TLPH, is connected to the Recorder Adapter Board via a white 50-pin,
ribbon cable. The stepper motor and the paper sensor are also connected to the Recorder Adapter Board.
The Recorder Adapter Board is connected to the Main CPU Board via a 154-pin connector.
Thermal Line Printhead (TLPH)
The TLPH is located on its own holder in the recorder chassis.
Paper Sensor
The paper sensor hardware consists of a reflective light sensor that detects the black marks on the trace
paper, and paper-out. It is attached to the RFI Bracket, and connected to the Recorder Adapter Board via a
removable cable connector.
Stepper Motor
The stepper motor is a bipolar motor controlled by a micro-stepping motor driver on the Recorder Adapter
Board. The motor is located on the recorder chassis and is connected to the Recorder Adapter Board via a
removable cable connector.
LCD Display and Touchscreen
The LCD Display Assembly consists of a four-wire resistive touchscreen, a 6.5” TFT panel, and a backlight
inverter, all connected to the Display Adapter Board (M2703-66440) and fitted into the display housing.
The board is connected to the Recorder Adapter Board (M2703-66430) via a 50-pin ribbon cable. The
green power LED is incorporated into the Display Adapter Board.
Noninvasive Blood Pressure Assembly
The optional Noninvasive Blood Pressure Assembly (M2703-64602) is located in the front lefthand corner
of the bottom housing assembly. It is connected via a serial link to the Main CPU Board.
SpO2 Assembly
The optional SpO2 Assembly (M2703-64603) is physically located on the Bus Master Board, but sends
data directly to the Main CPU Board via a serial link.
17
Page 26
4 Theory of Operation Input/Output Interface Boards
Input/Output Interface Boards
There are two optional interface boards available:
• LAN/RS232 Interface Board, used for connecting to a PC running the Support Tool and to a
surveillance and documentation system such OB TraceVue.
• PS/2 Interface Board, used for connecting an external keyboard or mouse.
The interface boards plug into the two interface slots on the underside of the device, and are controlled by
the Main CPU Board.
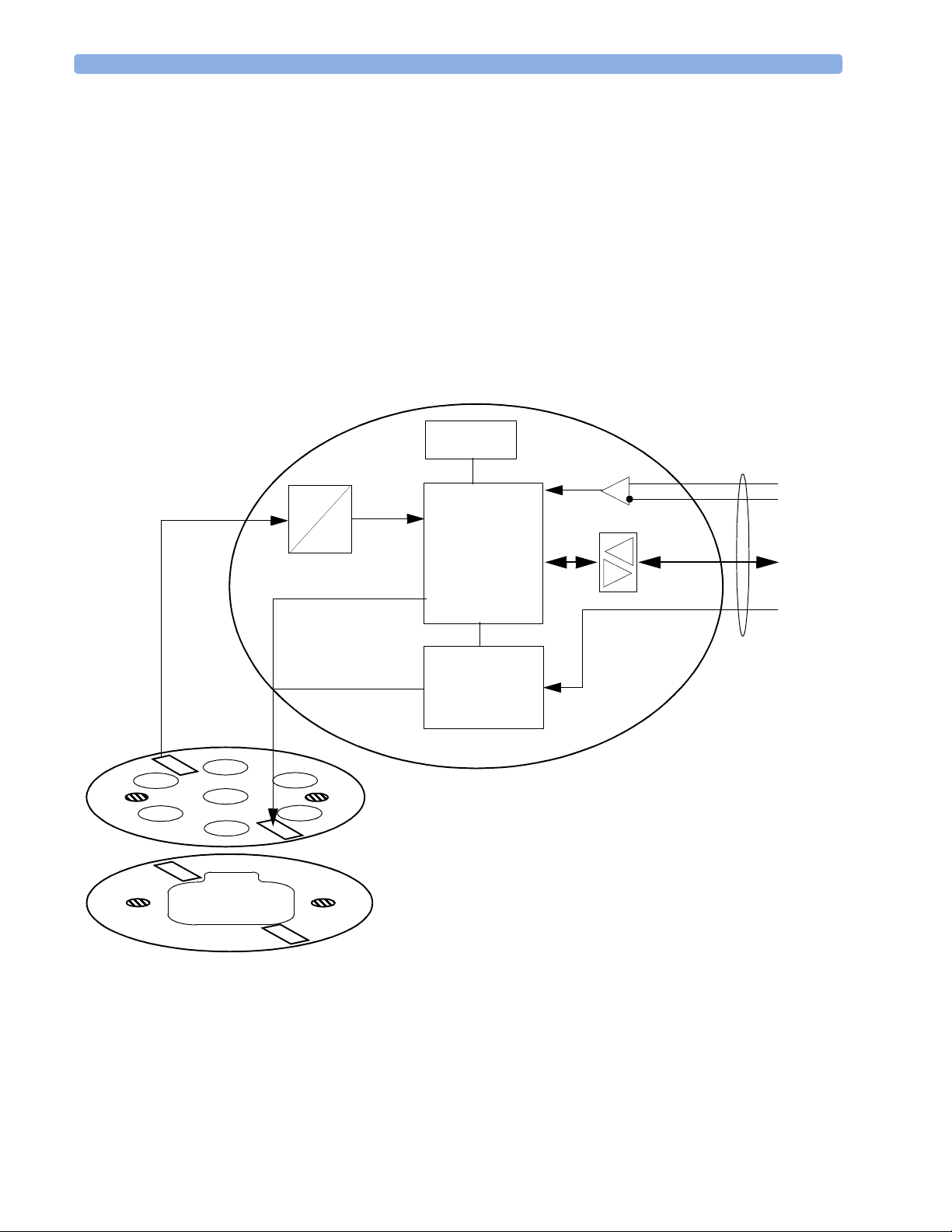
Transducer Hardware Overview
Analog Signal
Analog/ Digital conversion
A
D
Timing and Mode Control
EEPROM
Master Clock recovery
Signal
processor
Power supply
and reset
Ultrasound frontend board
or alternatively
Transducer
cable
Communication Transceiver
Power and
Identification
Transducer CPU board
18
TOCO/ECG frontend board
1
Page 27
Transducer Types 4 Theory of Operation
Transducer Types
Transducers consist of the following types:
•US
•Toco
+
•Toco
They all share the same power supply, and analog-to-digital conversion circuitries. The processor software
is also the same for all transducers. The frontends, however, are specific to each transducer type.
(includes DECG/MECG and IUP capability)
Functional Description of the Transducer CPU
The CPU section of the transducers is made up of the following main functional blocks:
• CPU (micro controller)
• Analog-to-Digital Converter
• Communication Transceiver (CAN bus driver)
• EEPROM
CPU (Micro Controller)
A single-chip processor is used to control the transducer, generate the frontend control signals, control the
analog-to-digital signal conversion, and to perform the signal processing.
Analog-to-Digital Converter
Analog-to-digital (A/D) signal conversion is carried out by the 16-bit AD converter. Digital signals are
directly communicated from the A/D converter to the CPU.
Communication Transceiver (CAN Bus Driver)
The communications transceiver (CAN bus driver) communicates directly with the transducer CPU, and
allows the transducer to communicate with the Bus Master Board via the CAN bus.
EEPROM
The serial EEPROM stores all non-volatile data required to operate the transducer (for example, calibration
and correction factors for frontend gains and offsets, country-specific information, serial numbers and error
logs).
Toco Transducer Frontend
Uterine activity is measured by evaluating the hardness of the mother’s abdomen with a pressure sensitive
resistor bridge (strain gauge sensor element). The strain gauge sensor element requires an excitation voltage
and its differential output signal is proportional to the pressure applied to it. A DC excitation voltage is
used, and the resulting output signal is fed directly to an A/D signal converter before being sent to the
processor.
19
Page 28

4 Theory of Operation Ultrasound Transducer Frontend
Ultrasound Transducer Frontend
The ultrasound frontend is a pulsed Doppler system with a 1.0 MHz ultrasound frequency, and a pulse
repetition rate of 3 kHz. Seven ultrasound crystals are used as transmitter and receiver.
Toco+ Transducer Frontends
Several parameter frontends are combined on one board. In addition to the Toco frontend, additional
supported parameters are DECG, MECG and IUP.
A seven-pin ‘D-type’ socket carries all parameter related inputs and outputs. An external mode resistor,
connected to one of the pins, automatically detects which mode to set when an adapter cable is plugged in
(whether it is DECG, MECG, or IUP).
Toco Frontend
See “Toco Transducer Frontend” on page 19.
IUP Frontend
Intrauterine pressure (IUP) is measured via a piezo resistive bridge with AC excitation connected to the
RA / LA input pins of the ECG amplifier. A/D conversion of the IUP signal is done by the 16-bit A/D
converter.
ECG Frontend
The ECG frontend measures both DECG and MECG, using a 3-lead system (RA, LA and reference
electrode). The ECG mode is automatically detected when an adapter cable is attached. Input lines are
ESD protected.
20
Page 29

5Interfaces
There are two interface boards available as options for the Avalon fetal monitors:
• LAN / RS232 system interface
•Dual PS/2 interface
LAN / RS232 system
interface
5
Dual PS/2 system
interface
The interfaces are “plug-and-play” boards, and fit into dedicated slots on the underside of the monitor. See
“Removing the Interface Boards” on page 87 for details of how to remove and fit the boards.
LAN / RS232 Interface
The LAN / RS232 system interface has two fully isolated ports:
• The LAN connection can be used for connecting the monitor to PC for configuration or upgrade using the
Support Tool, and for future system expansion.
• The RS232 connection can be used for connecting the monitor to an obstetrical information and
surveillance system, such as OB TraceVue.
Dual PS/2 Interface
This interface provides two PS/2 ports to enable the monitor to be connected to off-the-shelf, “plug-andplay” input devices:
• Mouse: any specified PS/2 mouse or trackball may be used for navigation and data entry.
• Computer keyboard: a PS/2 computer keyboard can be used for data entry instead of the on-screen pop-up
keyboard.
21
Page 30

5Interfaces Dual PS/2 Interface
22
Page 31

6Testing and Maintenance
This chapter contains the testing and maintenance procedures to ensure the proper functioning of the
monitor and accessories, covering preventive maintenance, performance assurance and safety.
Carry out the procedures as specified in the following sections.
For detailed instructions on how to clean the monitor, transducers and accessories, see the monitor’s
Instructions for Use.
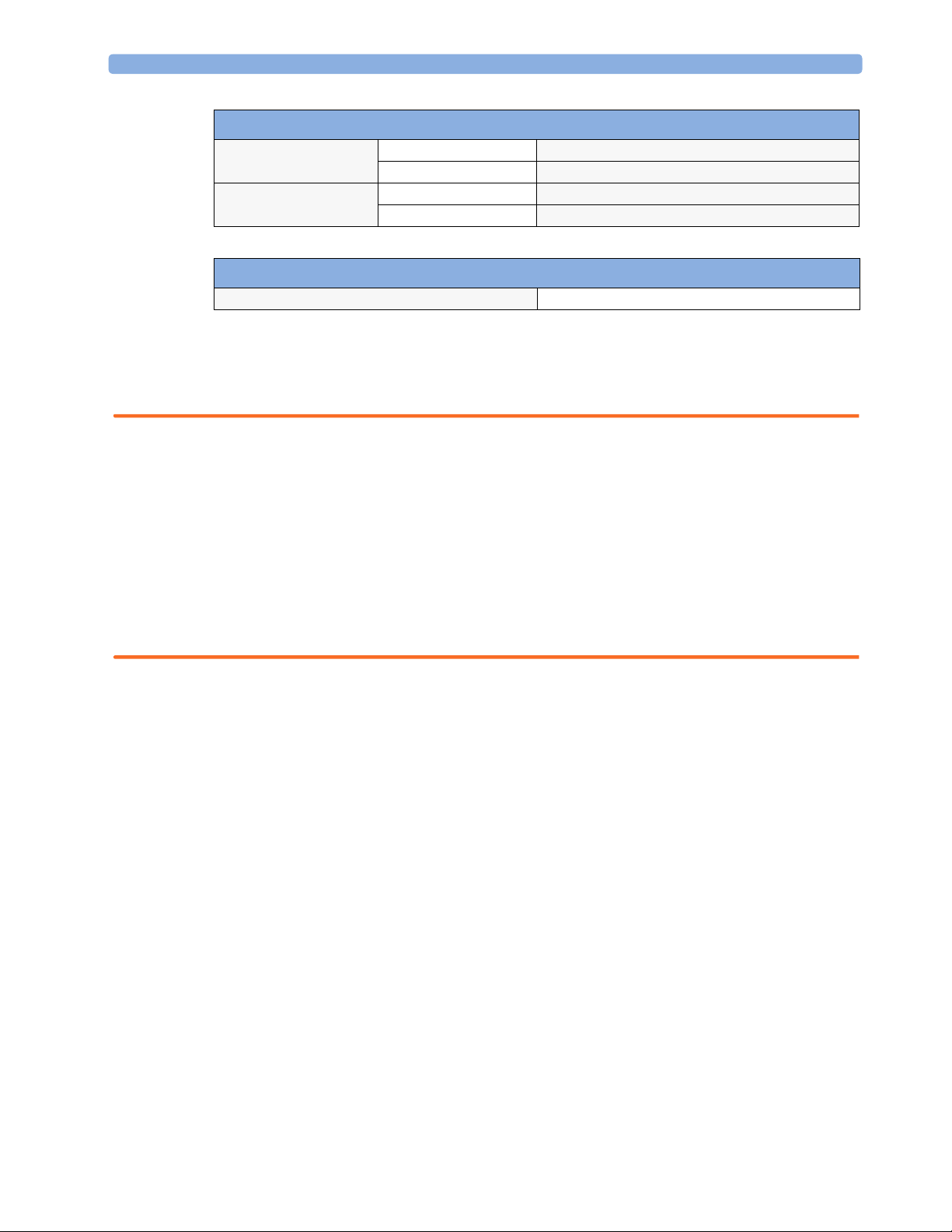
Recommended Frequency
Perform the procedures as indicated in the suggested testing timetable. These timetable
recommendations do not supersede local requirements.
Table 1: Suggested Testing Timetable
6
Te s ts Frequency
Preventive Maintenance
Other Regular Tests
Performance Assurance
Te s ts
Safety Tests
Noninvasive Blood Pressure Calibration Once every two years, or as specified by
local laws (whichever comes first).
Visual Inspection Before each use.
Recorder Maintenance Once a year, or if the printout is
degraded.
Testing Transducers and Patient Modules Once a year, or if you suspect the
measurement is incorrect.
Noninvasive Blood Pressure Performance Tests Once every two years, or if you suspect
SpO
Performance
2
Enclosure Leakage Current
Patient Leakage Current
the measurement is incorrect.
Once every two years and after repairs
where the power supply is removed or
replaced, or the monitor has been
damaged by impact.
23
Page 32

6 Testing and Maintenance When to Perform Test Blocks
When to Perform Test Blocks
This table tells you when to perform specific test blocks. See page 25 for test details.
Table 2: When to perform test blocks
Service Event Test Block(s) Required - Complete these tests
Installation Perform Visual, Power On, Performance test blocks (see Table 3).
Preventive Maintenance Perform Noninvasive Blood Pressure Performance tests blocks (see Table 3).
Other Regular Tests and Tasks
• Visual Inspection Perform Visual test block (see Table 3).
• Transducer and Patient Module
Te s ti n g
• Recorder Maintenance Regular cleaning and maintenance (see “Fetal Recorder Maintenance” on
Repairs
• Repairs when the monitor has been
damaged by impact.
• Repairs where the power supply has
been removed or replaced.
• All other repair events. Perform Visual, Power On and Performance test blocks (Table 3).
Upgrades
See “Testing Transducers and Patient Modules” on page 26.
page 26
Perform the recorder selftest (see “Fetal Recorder Selftest Report” on page 40).
Perform Visual, Power On and Performance test blocks, and when the
monitor has been damaged by impact, or where the power supply has been
removed or replaced, perform safety test blocks (see Table 3).
For upgrade information refer to
“Upgrades” on page 105.
Combining or Exchanging System
Components
All other service events Perform Visual, Power On and Performance test blocks
Perform Visual, Power On, Performance test blocks
(see Table 3).
Perform the System Test (see Table 3 and “System Test” on page 36).
(see Table 3).
24
Page 33

Test Reporting 6 Testing and Maintenance
Test Reporting
Authorized Philips personnel report test result back to Philips to add to the product development
database. Hospital personnel, however, do not need to report results.
How to Carry Out the Test Blocks
Key to Table 3 P = Pass, F = Fail, X = test result value to be recorded
Table 3: Test and Inspection Matrix
What to Record
Tes t B l oc k Test or Inspection to be Performed Expected Test Results
Visual Inspect the monitor, transducers, patient
modules and cables for any damage.
Are they free of damage? If Yes, Visual test is passed. V:P or V:F
on Service Record
(Philips
Personnel o nly)
Power On Power on the unit.
Does the self-test complete successfully? If Yes, Power On test is passed. PO:P or PO:F
Noninvasive
Blood Pressure
Per forman ce
Te s t s
SpO
2
Per forman ce
Te s t
Safety (1) Perform Safety Test: Sum of Functional
Safety (2) Perform Safety Test: Patient Leakage Current
Perform the Accuracy Test (see page 31) X1 = value displayed by monitor
Performance Leakage Test (see page 32) X2 = leakage test value
Performance Linearity Test (see page 32) X3 = value displayed by monitor
Performance Valve Test (see page 32) X4 = value < 10 mmHg PN:P/X4 or
Perform the SpO2 Performance Test (see
page 32)
Earth and Enclosure Leakage Current Normal and Single Fault Conditions.
- Single Fault Condition, mains on applied
part.
Difference ≤ 3mmHg
X2 < 6 mmHg
Difference ≤ 3mmHg
Value should be between 95% and
100%
With mains cable:
Maximum leakage current (X1)
≤ 100µA
Maximum leakage current (X2)
≤ 50µA @ 264V
PN:P/X1 or
PN:F/X1
PN:P/X2 or
PN:F/X2
PN:P/X3 or
PN:F/X3
PN:F/X4
No reporting
necessary
S(1):P/X1 or
S(1):F/X1
S(2):P/X2 or
S(2):F/X2
System Perform the system test according to sub
clause 19.201 of IEC 60601-1-1, if
applicable, after forming a system.
Enclosure Leakage Current:
≤ 100µA (Normal Condition)
≤ 300µA (Single Fault Condition)
Protective Earth Leakage Current of
Multiple Portable Socket-Outlets:
≤ 500µA
Patient Leakage Current: ≤ 10µA
System test:P or
System test: F
25
Page 34

6 Testing and Maintenance Preventive Maintenance Procedures
Preventive Maintenance Procedures
The preventive maintenance tasks are restricted to the noninvasive blood pressure measurement
calibration. Carry out the noninvasive blood pressure measurement performance tests at least every two
years, or as specified by local laws (whichever comes first).
Other Regular Tests
The care and cleaning requirements that apply to the monitor and its accessories are described in the
Instructions for Use. This section details the periodic maintenance recommended for the monitor,
transducers and accessories.
Visual Check
Check all exterior housings for cracks and damage. Check the condition of all external cables, especially
for splits or cracks and signs of twisting. If serious damage is evident, the cable should be replaced
immediately. On the Toco
not damaged. Check that all mountings are correctly installed and secure. Refer to the instructions that
accompany the relevant mounting solution.
+
transducer and the patient module, ensure that the adapter cable socket is
Fetal Recorder Maintenance
The recorder platen, thermal printhead and paper sensor should be cleaned at least once a year, or
when needed (when traces become faint).
Clean the assemblies as follows:
• Clean the recorder platen with a lint-free cloth using a soap/water solution.
• Wipe the printhead using a cotton swab moistened with 70% Isopropyl alcohol based solution.
• Check the paper sensing mechanism is dust free.
Testing Transducers and Patient Modules
If any of the following tests fail, repeat the test using another transducer. If the second transducer
passes the tests, confirming that the first transducer is defective, contact your service personnel.
If the second transducer also fails the tests, contact your Philips Service Engineer or Response Center.
Ultrasound Transducer Electrical Check
CAUTION Use of ultrasound gel that is not approved by Philips may reduce signal quality and may damage the
transducer. This type of damage is not covered by warranty.
To test an ultrasound transducer:
26
1 Switch on the monitor and the recorder.
2 Connect the transducer to the fetal monitor.
3 Select the fetal heart sound for this channel.
4 Increase the loudspeaker volume to an audible level.
Page 35

Other Regular Tests 6 Testing and Maintenance
The ultrasound transducer contains seven piezoelectric crystals. Basic functioning of each can be
5
verified by holding a flat bottomed pencil or similar above each crystal and moving it up and down
as shown.
6 A sound should be heard for each crystal tested. The pencil should be held two to three centimeters
from the transducer surface when the test is carried out.
Crystals
7 A sound should also be heard when the transducer is moved back and forth over a solid surface, or
the hand as shown.
27
Page 36

6 Testing and Maintenance Other Regular Tests
Toco Transducer Electrical Check
To test a Toco transducer:
1 Switch on the monitor and the recorder.
2 Connect the transducer to the fetal monitor.
3 Gently apply pressure to the Toco sensor.
4 Check that the value on the display and paper shows this change in pressure.
5 Lay the transducer face up on a hard, flat surface for a few seconds.
6 Press the Toco Baseline Key to re-adjust the Toco display to 20.
7 Turn the transducer over so that the Toco sensor is resting on the flat surface. You should see a
marked increase in the value of the Toco reading in the Toco display.
Toco display = 20
Toco display = 35 - 45
Testing the Patient Module (M2738A)/Toco+ Transducer (M2735A): DECG Mode
1 Switch on the monitor and the recorder.
2 Connect the patient module or Toco
3 Attach the DECG adapter cable M1362B to the socket on the patient module or Toco
+
transducer to the fetal monitor.
+
transducer.
28
4 Ensure that the DFHR channel display on the fetal monitor shows the DECG LEADS OFF
INOP with the DECG adapter cable attached.
5 Take a Fetal Scalp Electrode, and connect it to the DECG adapter cable.
Page 37

Other Regular Tests 6 Testing and Maintenance
6 EITHER
Make a short between the spiral electrode and the reference electrode with your fingers (it is best to
wet your fingers first). Use a sterile Fetal Scalp Electrode.
CAUTION The tip of the spiral electrode is sharp. Take care not to injure your fingers.
Spiral
Electrode
Reference
Electrode
OR
Cut off the plastic tip of the fetal scalp electrode (containing the spiral and reference electrodes)
from the end of the wires. Strip the insulation from the end of the wires, and connect them to a
patient simulator.
Note—We do not recommend the use of a specific patient simulator. The use of a patient simulator does
not allow checking the specification of the ECG-functionality; it allows only a check of general
function.
Result: the DECG LEADS OF F INOP should disappear.
If the test results are not as outlined above, repeat the test with another ECG transducer. If this does
not solve the problem, try the following:
• Check tall connections.
•If the DECG LEADS OFF INOP is still displayed, the DECG adapter cable may be defective.
Replace the adapter cable.
If the problem persists, replace the transducer.
Testing the Patient Module (M2738A)/Toco+ Transducer (M2735A): MECG Mode
1 Switch on the monitor and the recorder.
2 Connect the patient module or Toco
3 Attach the MECG adapter cable M1363A to the red color-coded socket on the patient module or
+
transducer
To c o
4 EITHER
Attach electrodes to the M1363A adapter cable, and apply the electrodes to the skin (for example on
the wrists).
OR
Attach the M1363A adapter cable to a patient simulator.
Note—We do not recommend the use of a specific patient simulator. The use of a patient simulator does
not allow checking the specification of the ECG-Functionality; it allows only a check of general function.
+
transducer to the fetal monitor.
29
Page 38

6 Testing and Maintenance Other Regular Tests
Result: You should see MECG values displayed on the maternal display or annotated on the recorder
trace.
If the test results are not as outlined above, repeat the test with another ECG transducer. If this does
not solve the problem:
• The MECG adapter cable may be defective. Replace the adapter cable, and repeat the test.
• Check all connections.
Testing the Patient Module (M2738A)/Toco+ Transducer (M2735A): IUP Mode
To test the IUP functionality of the patient module or the Toco+ transducer, you need the following:
Expansion
chamber
Toco+ transducer
(shown) or patient
module
IUP cable
(9898 031 43931)
‘T’ adapter
Cut end of
catheter
Manometer
IUP catheter
(M1333A)
•Manometer.
• Expansion chamber.
• Three lengths of silicone tubing with a ‘T’ adapter.
1 Switch on the monitor and the recorder.
2 Connect the patient module or Toco
3 Attach the IUP adapter cable (9898 031 43931) to the socket on the patient module or Toco
+
transducer to the fetal monitor.
transducer.
+
30
4 Cut the sensor tip off an IUP catheter (M1333A).
5 Connect the catheter to the IUP adapter cable.
6 Connect the silicone tubing to the test volume chamber and the manometer as shown in the picture.
7 Connect the cut end of the catheter to the silicone tubing.
8 Apply a pressure of 80 mmHg ± 5 mmHg with the manometer. Check that the value on the display
and on trace corresponds to this pressure. Slowly release the pressure, and check that the value on the
display and on trace shows this change in pressure.
Page 39

Performance Assurance Tests 6 Testing and Maintenance
Performance Assurance Tests
Some of the following test procedures must be performed in service mode. To enter service mode select
Operating Modes in the main menu. Then select Service Mode and enter the password.
Noninvasive Blood Pressure Performance Tests
This section describes noninvasive blood pressure test procedures. The monitor must be in service
mode.
Table 3 gives the expected test results for each of the tests.
Accuracy Test
This test checks the performance of the noninvasive blood pressure measurement. Connect the
equipment as shown:
Expansion Chamber
Tubing
Connect to Noninvasive Blood
Pressure socket
Manometer
Tools required:
• Reference manometer (includes hand pump and valve), accuracy 0.2% of reading.
• Expansion chamber (volume 250 ml +/- 10%)
• Appropriate tubing.
In service mode, the systolic and diastolic readings indicate the noise of noninvasive blood pressure
channels 1 and 2 respectively. When static pressure is applied, the reading in noninvasive blood
pressure channel 1 should be below 50. The value in parentheses indicates the actual pressure applied
to the system.
1 Connect the manometer and the pump with tubing to the noninvasive blood pressure connector
on the monitor and to the expansion chamber.
2 In service mode, select the Setup NBP menu.
3 Select Close Valves: On
4 Raise the pressure to 280 mmHg with the manometer pump.
5 Wait 10 seconds for the measurement to stabilize.
6 Compare the manometer values with the displayed values.
7 Document the value displayed by the monitor (X1).
8 If the difference between the manometer and displayed values is greater than 3 mmHg, calibrate
the noninvasive blood pressure measurement. If not, proceed to the leakage test.
31
Page 40

6 Testing and Maintenance Performance Assurance Tests
To calibrate the noninvasive blood pressure measurement, select Close Valves off then
9
Calibrate NBP and wait for the instrument to pump up the expansion chamber.Wait a few
seconds after pumping stops until EnterPrVal is highlighted and then move the cursor to the
value shown on the manometer. If one of the following prompt messages appears during this step,
check whether there is leakage in the setup:
– NBP unable to calibrate–cannot adjust pressure
– NBP unable to calibrate–unstable signal
10 Press Confirm.
If the INOP NBP Equipment Malfunction message occurs in monitoring mode, go back to service
mode and repeat the calibration procedure.
Leakage Test
The noninvasive blood pressure leakage test checks the integrity of the system and of the valve. It is
required once every two years and when you repair the monitor or replace parts.
1 If you have calibrated, repeat steps 2 to 6 from the accuracy test procedure so that you have 280
mmHg pressure on the expansion chamber.
2 Watch the pressure value for 60 seconds.
3 Calculate and document the leakage test value (X2).
Linearity Test
1 Reduce the manometer pressure to 150 mmHg.
2 Wait 10 seconds for the measurement to stabilize.
3 After these 10 seconds, compare the manometer value with the displayed value.
4 Document the value displayed by the monitor (X3)
5 If the difference is greater than 3 mmHg, calibrate the noninvasive blood pressure measurement
Valve Test
1 Raise the pressure again to 280 mmHg.
2 Select Close valves: Off.
3 Wait five seconds and then document the value displayed. The value should be less than 10
X2 = P1 - P2
where P1 is the pressure at the beginning of the leakage test and P2 is the pressure displayed after
60 seconds.
The leakage test value should be less than 6 mmHg.
(see steps 9 to 10 in the accuracy test procedure).
mmHg.
4 Document the value displayed by the monitor (X4).
SpO2 Performance Test
This test checks the performance of the SpO2 measurement.
Tools required: none
32
Page 41

Safety Tests 6 Testing and Maintenance
Connect an adult SpO2 transducer to the SpO2 connector.
1
2 Measure the SpO
3 The value should be between 95% and 100%.
value on your finger (this assumes that you are healthy).
2
Safety Tests
You are recommended to file the results of safety tests. This may help to identify a problem early
particularly if the test results deteriorate over a period of time.
Warnings, Cautions, and Safety Precautions
• These tests are a proven means of detecting abnormalities that, if undetected, could prove dangerous
to either the patient or the operator.
• You can perform all tests using commercially available Safety Analyzer test equipment. You can
perform basic measurements with widely available multifunction instruments such as the HP 3469A
multimeter or equivalent.
• The consistent use of a Safety Analyzer as a routine step in closing a repair or upgrade is emphasized
as a mandatory step to maintain approval agency status. You can also use the Safety Analyzer as a
troubleshooting tool to detect abnormalities of line voltage and grounding plus total current loads.
• For Europe and Asia/Pacific, the monitor complies with:
IEC60601-1:1988 + A1:1991 + A2:1995 = EN60601-1:1990 +A1:1993 + A2:1995
For USA, the monitor complies with:
UL60601-1
• Additional tests may be required according to local regulations.
•Normally, a Safety Analyzer is used to perform these procedures. Popular testers include the
DEMPSEY 232D, or for use in Europe, testers like the Rigel, Metron or Gerb. Follow the
instructions of the Instrument manufacturer.
• Any device that is connected to the medical device must comply with IEC60601-1, and UL606011:2003 for the USA, if within the patient vicinity and be separately tested at the same intervals as the
monitor. Devices forming a system must comply with IEC60601-1-1.
• Any device that is connected to the medical device must comply with IEC60601-1-1 if outside the
patient vicinity and be tested accordingly.
• Perform safety tests as described on the following pages.
33
Page 42

6 Testing and Maintenance Safety Tests
Electrical Isolation Diagram
This diagram gives an overview of the electrical isolation of the monitor. Accessible metal parts are
identified (see arrows).
Switch
Line
Protective
Earth
Neutral
100V.240V
ac
Fuses
Safety Test Procedures
Use the test procedures outlined here only for verifying safe installation or service of the product. The
setups used for these tests and the acceptable ranges of values are derived from local and international
standards but may not be equivalent. These tests are not a substitute for local safety testing where it is
required for an installation or a service event. If using the Metron Safety tester, perform the tests in
accordance with your local regulations, for example IEC60601-1, UL60601-1 (US), CD IEC62353,
and IEC60601-1-1. The Metron Report should print results as detailed in this chapter, together with
other data.
C
Y
C
Y
primary
side
C
Y1
C2
C
Y1
Housing sheet metal
secondary
side
24 V
dc
5
V
dc
3
V
dc
C
Y1
C1
C
Y1
Accessible metal parts
in the top cover (accessed by
opening the paper drawer)
5 V
24 V
I/O boards
30 V
dc
C
22pF
Y2
5 V
dc
dc
dc
(RS232)
Keyboard and
Mouse
patient modules
12 V
dc
(US,TOCO,ECG,SpO2)
Accessible metal
parts (interface slot)
S(1): Sum of Functional Earth and Enclosure Leakage Current Test
Test to perform:
This test measures leakage current of exposed metal parts of the FM20/FM30 monitor and the
functional earth leakage current. It tests normal and reversed polarity. Perform the test with S1 closed
(Normal Condition) and with S1 open (Single Fault Condition).
34
Page 43

Safety Tests 6 Testing and Maintenance
NOTE
The protective earth conductor is required for EMC purposes. It has no protective function against
electric shock. The protection against electric shock is provided by double and/or reinforced insulation.
This safety test is based on IEC 60601-1 and CD IEC62353 (date of circulation:2004-04-09)
For measurement limits, refer to test block Safety (1), “Test and Inspection Matrix” on page 25.
Report the highest value.
You can find metal parts of the device:
• In the top cover (accessed by opening the paper drawer).
• In an interface slot located in the bottom housing (you need to remove the interfaces if they are
fitted).
Location of metal parts
S(2): Patient Leakage Current - Single Fault Condition (SFC), Mains on Applied Part
Test to perform:
MECG Electrodes
This test measures patient leakage current from applied part to earth caused by external main voltage
on the applied part of 264V. Each polarity combination possible shall be tested. This test is applicable
for ECG measurement inputs.
This safety test is based on IEC 60601-1 and CD IEC62353 (date of circulation:2004-04-09)
For measurement limits and test voltage, refer to test block Safety (2), “Test and Inspection Matrix” on
page 25.
Report the highest value.
35
Page 44

6 Testing and Maintenance System Test
System Test
After mounting and setting up a system, perform system safety tests according to IEC60601-1-1.
What is a Medical Electrical System?
A medical electrical system is a combination of at least one medical electrical device and other electrical
equipment, interconnected by functional connection or use of a multiple portable socket-outlet.
General Requirements for a System
After installation or subsequent modification, a system must comply with the requirements of the
system standard IEC/EN60601-1-1. Compliance is checked by inspection, testing or analysis, as
specified in the IEC60601-1-1 or in this book.
Medical electrical equipment must comply with the requirements of the general standard IEC/
EN60601-1, its relevant particular standards and specific national deviations. Non-medical electrical
equipment shall comply with IEC and ISO safety standards that are relevant to that equipment.
Relevant standards for some non-medical electrical equipment may have limits for enclosure leakage
currents higher than required by the standard IEC60601-1-1. These higher limits are acceptable only
outside the patient environment. It is essential to reduce enclosure leakage currents when non-medical
electrical equipment is to be used within the patient environment.
System Example
This illustration shows a system where both the medical electrical equipment and the non-medical
electrical equipment are situated at the patient’s bedside.
Key:
Non-Medical Devices
Distance to patient
must be >= 1.5m
Power cables:
Data cables:
Personal
Computer
Isolation
Transformer
Medical Devices
Fetal Monitor
36
Page 45

Touchscreen Calibration 6 Testing and Maintenance
WARNING • Do not use additional AC mains extension cords or multiple portable socket-outlets. If a multiple
portable socket-outlet without an approved isolation transformer is used, the interruption of its
protective earthing may result in enclosure leakage currents equal to the sum of the individual earth
leakage currents, so exceeding allowable limits.
• Do not connect any devices that are not supported as part of a system.
• Any non-medical device placed and operated in the patient’s vicinity must be powered via an
approved isolation transformer that ensures mechanical fixing of the power cords and covering of
any unused power outlets.
Touchscreen Calibration
To access the touchscreen calibration screen:
1 Enter service mode
2 Select Main Setup
3 Select Hardware
4 Select Calibrate Touch
Please touch slow ly each target as it appea rs on screen.
Do not power off the mo ni tor until this calib ration has
completed.
Make sure you complete the calibration procedure without powering off the monitor mid-way. If the
monitor is powered off after the first point is touched, the touch panel will be deactivated until the
touch calibration is performed again.
37
Page 46

6 Testing and Maintenance Disabling/Enabling Touch Operation
If the touchscreen is accidentally mis-calibrated by selecting the wrong spot, you must use another
input device to re-enter calibration mode. If you have the support tool, you can select Reset Touch
Calibration to Default and it will create a rough calibration which will allow you to access
the calibration menu again via the touchscreen.
Disabling/Enabling Touch Operation
To disable touchscreen operation of the monitor, press and hold the Main Screen key for about
three seconds. A red padlock will blink on the key. Press and hold the Main Screen key again for
about three seconds to re-enable touchscreen operation.
38
Page 47

Checking the Fetal Recorder Offset 6 Testing and Maintenance
Checking the Fetal Recorder Offset
The easiest way to check the recorder offset is to connect a resting Toco transducer (one that is not
under any load) to the monitor and then change the offset setting until the trace is recording 20 units
on the paper. Due to the delay between changing the offset setting and seeing the change on the paper,
you may have to repeat this procedure to set the offset.
When viewed from the front of the monitor, 0 is the setting that prints the trace the furthest to the
right, and 10 is the setting that prints the trace furthest to the left. If the trace from the resting Toco
transducer is printed below the 20 unit gridline, you need to increase the offset setting. If the trace is
printed above the 20 unit gridline, you need to decrease the offset setting. When the trace is recording
20 units, the offset is correctly set.
Setting the Fetal Recorder Offset
To set the fetal recorder offset, you first need to run the fetal recorder calibration:
1 In Main Setup, select Fetal Recorder to enter the Fetal Recorder menu.
The current setting for the recorder offset is shown (but it is still grayed out, and you cannot select
it yet).
2 Select Calibration to start the recorder calibration printout.
3 The recorder stops, and the Cal. Offset becomes selectable. Select Cal. Offset, and
select the offset value from 0 to 10 from the list, as appropriate. The recorder then finishes the
calibration printout.
4 Repeat if necessary until the trace is recording 20 units on the paper in Monitoring Mode,
matching the value displayed on the screen.
39
Page 48

6 Testing and Maintenance Fetal Recorder Selftest Report
Fetal Recorder Selftest Report
To verify your printer configuration, or if you doubt the performance of the recorder, you may want to
print a test report.
To print a selftest report, in Service Mode, select M ain Setup -> Fetal Recorder->
Selftest.
Here is an excerpt from a sample test report to give you an idea what it looks like (the exact appearance
may vary slightly):
40
This line should print exactly on the 20
unit gridline (Toco baseline) if the
recorder is correctly calibrated
Example of selftest report
Check the test pattern to ensure all the heating elements on the printer head are operational. Ensure
that:
• No more than 20 dots are missing over the entire printhead.
• No more than 2 adjacent dots are inoperative.
• No dots in the mode annotation (for example, FHR1) are inoperative.
If the any of the above conditions are not met, replace the printhead (see “Removing the Thermal Line
Printhead (TLPH)” on page 72).
Ensure that all printed lines are straight. If the lines are not straight, there may be a problem with the
paper recorder speed.
Page 49

7Troubleshooting
A list of system error messages and troubleshooting information for common problems you may encounter
while using the monitor and its accessories is given in the Instructions for Use. This chapter provides a guide for
qualified service personnel for troubleshooting problems that cannot be resolved by the user.
CAUTION If the troubleshooting procedure requires you to disassemble the monitor or transducers, be certain to follow
the disassembly and reassembly procedures given in Chapter 8, “Disassembly and Reassembly”.
Who Should Perform Repairs
Only qualified service personnel should open the monitor housing, remove and replace components, or make
adjustments. If your medical facility does not have qualified service personnel, contact Philips’ Response
Center or your local Philips representative.
7
WARNING High Voltage - Voltages dangerous to life are present in the instrument when it is connected to the mains
power supply. Do not perform any disassembly procedures with power applied to the instrument. Failure to
adhere to this warning could cause serious injury or death.
Replacement Level Supported
The replacement level supported for this product is to the printed circuit board (PCB) and major subassembly
level. Once you isolate a suspected PCB, follow the procedures in Chapter 8, “Disassembly and Reassembly”
to exchange the PCB with a known good replacement. Check to see if the symptom disappears and that the
monitor passes all performance tests. If the symptom persists, swap back the replacement PCB with the
suspected malfunctioning PCB (the original PCB that was installed when you started troubleshooting) and
continue troubleshooting as directed in this chapter.
Hardware Revision Check
Some troubleshooting tasks may require that you identify the hardware revision of your monitor’s main
board. To check your hardware revision:
1 Enter the Main Setup menu and select Revision.
41
Page 50

7 Troubleshooting Software Revision Check
2
Select Product.
You see the hardware revision in the pop-up window, along with the serial number, part number, and
the software revision.
The following table shows which part number corresponds to which hardware revision:
Hardware Revision Board Number Description
A.00.05 M2703-66510 Main CPU Board
Software Revision Check
Some troubleshooting tasks may require that you identify the software revision of your monitor. You can
find the software revision along with other information, such as the system serial number, in the monitor
revision screen.To access the monitor revision screen:
1 Enter the Main Setup menu and select Revision.
2 Select Product.
You see the software revision in the pop-up window, along with the serial number, part number, and the
hardware revision.
NOTE The part numbers listed in the monitor revision screen do not necessarily reflect the part numbers
required for ordering parts. Please refer to Chapter 9, “Parts” for the ordering numbers.
NOTE The system serial number can also be found on the lower right corner on the front of the monitor.
Obtaining Replacement Parts
See Chapter 9, “Parts” section for details on replacement parts.
Troubleshooting Guide
Problems with the monitor are separated into the categories indicated in the following sections and tables.
Check for obvious problems first. If further troubleshooting instructions are required refer to the
Troubleshooting Tables.
Taking the recommended actions discussed in this section will correct the majority of problems you may
encounter. However, problems not covered here can be resolved by calling Philips Response Center or
your local representative.
Checks for Obvious Problems
When first troubleshooting the instrument, check for obvious problems by answering basic questions such
as the following:
1 Is the power switch turned on?
2 Is the AC power cord connected to the instrument and plugged into an AC outlet?
Checks Before Opening the Instrument
You can isolate many problems by observing indicators on the instrument before it is necessary to open
the instrument.
42
Page 51

Troubleshooting Guide 7Troubleshooting
Checks with the Instrument Switched On, AC connected
The green power LED lights for about 1.5 seconds after switching on, and then goes out, and remains unlit
doing normal operation. The location of the green LED is shown in the following photograph:
Green Power LED
Individual Parameter INOPs
If you see any of the following parameter INOPs:
DECG EQUIP MALF IUP EQUIP MALF
ECG EQUIP MALF NBP EQUIP MALF
Fetrec EQUIP MALF OB EQUIP MALF
FHR1 EQUIP MALF SpO
FHR2 EQUIP MALF SpO
FHR3 EQUIP MALF TOCO EQUIP MALF
try exchanging the relevant component (transducer, sensor, patient module or board) with a known good
replacement, following the procedures in Chapter 8, “Disassembly and Reassembly”. Check to see if the
INOP disappears, and that you can measure the parameter in question normally. If the INOP persists,
swap back the original component and continue troubleshooting as directed in this chapter.
In the case of the INOPs
are two or more ultrasound transducers attached to the monitor,
INOP was issued, using the blue transducer Finder LED. Touching a numeric on the screen makes the
Finder LED light on the transducer providing the measurement. If you cannot identify the suspected
transducer directly because the transducer Finder LED does not light due to the defect, identify the other,
functioning transducers by activating their Finder LEDs, thus finding the defective one by a process of
elimination.
EQUIP MALF
2
SENSOR MALF
2
FHR1 EQUIP MALF, FHR2 EQUIP MALF, and FHR3 EQUIP MALF, when there
identify the transducer for which the
43
Page 52

7 Troubleshooting Troubleshooting Guide
Initial Instrument Boot Phase
The following table describe the regular initial boot phase of the monitor. If the boot phase does not
proceed as described below go to Boot Phase Failures for Troubleshooting information.
Time (sec.)
after Power
On
0 Switch the monitor on using the On/Off switch.
2 The green AC Power LED lights for about 1.5 seconds.
3.5 Green AC Power LED is turned off, and remains off.
5 You hear a ‘pop’ from the loudspeaker
6-8 Boot Screen with the Philips Logo appears on the display. Test Sound is issued.
8-10 Boot Screen with the Philips Logo disappears
Fixed screen elements (for example smart keys, alarm fields) appear on the screen.
10-15 First measurement information appears on the screen, touchscreen is functional.
Troubleshooting Tables
The following tables list troubleshooting activities sorted according to symptoms.
How to Use the Troubleshooting Tables
The possible causes of failure and the remedies listed in the troubleshooting tables should be checked and
performed in the order they appear in the tables. Always move on to the next symptom until the problem
is solved.
Boot Phase Event
Boot Phase Failures
Screen is Blank
Touchscreen Not Functioning
General Monitor INOP Messages
Alarm Tones
Fetal Recorder
LAN / RS232
44
Page 53

Troubleshooting Guide 7Troubleshooting
Boot Phase Failures
Symptoms Possible Ca u ses of
Failure
Green LED does not
light up, and no test tone
is heard
Green LED does not
light up, but you hear a
test tone
Green LED stays on
continuously
Green LED blinks
(indicating cyclic
reboots)
No AC mains connection Check that the power cord is not damaged and is
Power supply defective
Power On/Off switch
defective
Aborted/interrupted or
inconsistent software
configuration
Main CPU Board defective
Display Assembly not
connected to the Main
CPU Board
Touch controller defective
Display Adapter Board
defective
LED defective
Main CPU Board defective Try loading new software. If this does not solve the
Hardware failure Connect Support Tool directly to monitor with
Software fault
Hardware failure
Failure Isolation and Remedy
properly connected to the monitor. Check that the
power cord is correctly connected to a powered AC
mains socket.
Remove power supply and check if output voltage is
within the specifications (24V). Measure on multicolored wired connection between red and black wires
Exchange power supply if defective
Replace power supply
Perform a software upgrade using the Support Tool.
Replace Main CPU Board. Add boards in reverse
order and try again with each board.
Check if Display Assembly is connected correctly to
the Recorder Adapter Board.
Check that the multi-pin connector between the
Recorder Adapter Board and the Main CPU Board
Replace the Display Assembly.
Disconnect and reconnect the flat cable of the Display
Adapter Board and check again
Try to switch on the monitor. If it operates normally,
the LED is defective. Repair is effected by replacing
the Display Assembly.
problem, replace Main CPU Board.
crossover cable and start “search for defective devices”
If no device is detected, proceed as described above in
the section “Green LED stays on continuously”
If the Support Tool can detect the device and it
indicates the Operating Mode is ‘Boot’, download
and store the status log. Reload software and re-clone
the monitor. If this fixes the problem e-mail the status
log to your local response center
If this does not rectify the problem, follow the
instructions under “Green LED stays on
continuously”.
45
Page 54

7 Troubleshooting Troubleshooting Guide
Symptoms Possible Cau ses of
No Test Sound issued
or
INOP
Malfunct.
Screen is Blank
The information listed in this table is only valid if the boot phase has completed without error. See Boot Phase
Failures table for a description of the boot phase.
Symptoms Possible Cau ses of
Display is blank or
brightness is reduced
Speaker
issued
Failure Isolation and Remedy
Failure
Speaker cable disconnected
Speaker defective
Main CPU Board defective
Check speaker connections.
Check for INOPs and follow instructions
Exchange speaker
Exchange Main CPU Board
Failure Isolation and Remedy
Failure
Display Adapter Board
cable not connected
Backlight tubes defective Replace Display Assembly.
Backlight inverter defective
Display adapter board
defective
LCD flat panel defective
Main CPU Board defective Replace Main CPU Board.
Check cable connection of Display Assembly to the
Recorder Adapter Board.
Touchscreen Not Functioning
Symptoms Possible Causes of
Touchscreen not
functioning
Touch Position invalid Touch not calibrated Perform touch calibration:
Failure
Touchscreen functionality
has been temporarily
disabled
Touch screen cable not
connected
Touch controller defective
To u c h S e n so r d e f e c t iv e
Main CPU Board defective
Failure Isolation and Remedy
Check if touchscreen functionality has been
temporarily disabled (padlock symbol on Main
Screen key). If yes, press and hold the Main Screen
key to re-enable touchscreen operation.
Check connection from the Display Assembly to the
Recorder Adapter Board.
If the problem is not resolved, check that the multipin connector between the Recorder Adapter Board
and the main CPU Board.
Replace Display Assembly
Replace Main CPU Board
1. Enter the Main Setup Menu
2. Select Hardware
3. Select Calibrate Touch
See “Touchscreen Calibration” on page 37
46
Page 55

Troubleshooting Guide 7Troubleshooting
General Monitor INOP Messages
INOP Message Possible Causes of
Failure Isolation and Remedy
Failure
CheckInternVoltage Problem with the voltages
(5V) in the monitor
Check Monitor Temp The temperature inside the
monitor is too high
Main Board defective
Check Settings
Internal.Comm.Malf. Main CPU Board defective Replace Main CPU Board.
Settings Malfunc. Problem during cloning
INOP occurs during
normal operation,
indicating a possible
monitor software problem
INOP occurs after a
software upgrade,
indicating a possible
incomplete or unsuccessful
upgrade
process.
Memory space in which the
settings are stored has been
corrupted
Main CPU Board defective
Remove all I/O boards and put them back in one
at a time to isolate any defective board. If this does
not resolve the problem, replace the main board.
Check the environment for possible causes.
Replace Main Board.
Check the monitor and patient settings before you
resume monitoring. If the settings are unexpected,
there may be a problem with the monitor software.
1 Silence the INOP.
2 Load the User Defaults (see “Loading the User
Defaults” on page 110).
3 If this is unsuccessful, try loading the Factory
Default (see “Loading the Factory Default” on
page 109), and reconfigure the monitor in
Configuration Mode, and save the new settings
in the User Defaults.
If the INOP persists, there is an unresolved
software problem. Report the problem to factory
support.
Clone the correct settings via the Support Tool.
Reclone configuration file.
Reclone configuration file. This will reload the
memory space.
Replace Main CPU Board.
47
Page 56

7 Troubleshooting Troubleshooting Guide
Keyboard/Mouse Not Functioning
Alarm Tones
Symptoms Possible Causes of
Failure
Keyboard/Mouse attached
directly to the monitor not
functioning
Keyboard/Mouse not
connected properly
Keyboard/Mouse defective
PS/2 I/O board is not
properly plugged in
PS/2 I/O board defective
Symptoms Possible Causes of
Failure
INOP Message Speaker
Malfunct.
Alarm occurs but no alarm
sound is issued
is displayed
Speaker cable disconnected
Speaker defective
Sound amplifier on Main
CPU Board defective
Vol u me s et t o 0 Increase volume
Speaker defective
Sound amplifier on Main
CPU Board defective
Failure Isolation and Remedy
Check cabling
Replace Keyboard/Mouse
Ensure the PS/2 I/O board is properly plugged in. If
necessary, remove the board and plug it in again.
Replace I/O board
Failure Isolation and Remedy
Reconnect speaker cable
Replace speaker
Main CPU Board
Replace speaker
Main CPU Board
Alarm Behavior
If your monitor did not alarm in the way in which the end user expected, please consult the Instructions for
Use for possible setup issues or configuration settings which could affect alarm behavior.
Fetal Recorder
Symptom Possible Cause Corrective Action
Paper empty warning is
issued in the status line at
the bottom of the screen,
but paper is not out.
Drawer is open.
Paper jam.
Paper sensor dirty.
Paper sensor defective.
Close the drawer.
Open the drawer, remove paper, tear off scrumpled
paper and re-load, or load a new pack of paper.
Close the drawer.
Clean paper sensor (see Chapter 6, “Testing and
Maintenance”).
Exchange paper sensor (see
Chapter 8, “Disassembly and Reassembly” and
Chapter 9, “Parts”.
48
Page 57

Troubleshooting Guide 7Troubleshooting
Symptom Pos sible Cause Corrective Action
No paper transport. Poor connection. Check all internal connectors.
Paper jam.
Open the drawer, remove paper, tear off scrumpled
section of paper and re-load, or load a new pack of
paper. Close the drawer.
Motor cable is disconnected.
Check that the motor cable is properly connected
to the Recorder Adapter Board.
Motor is defective.
To test the functioning of the motor, open the
drawer and press the recorder
Start/Stop key
to start the recorder. A good motor should rotate
for between one and three minutes (depending on
the paper speed).
If the motor does not rotate, replace the motor (see
“Removing the Stepper Motor” on page 78).
The recorder appears to be
running normally, but the
paper remains blank
Drawer is open.
Thermal Printhead is
disconnected.
Thermal Printhead is
defective.
Close the drawer.
Check the connection. Then run the recorder
Selftest to verify correct printing (see “Fetal
Recorder Selftest Report” on page 40).
Replace the Thermal Printhead. Then calibrate the
recorder (see “Setting the Fetal Recorder Offset”
on page 39).
The wrong side of the paper
Load the paper correctly, the right way up.
is facing up.
No recorder key is available
on the screen, and the
INOP
FetRec MALF is
issued.
The recorder has not been
calibrated.
EEPROM on the Recorder
Adapter Board is defective
Calibrate the recorder (see “Setting the Fetal
Recorder Offset” on page 39).
Exchange the Recorder Adapter Board and
calibrate the recorder (see “Setting the Fetal
Recorder Offset” on page 39).
Recorder Controller on the
Main CPU Board is
defective.
Exchange the Main CPU Board and calibrate the
recorder (see “Setting the Fetal Recorder Offset”
on page 39).
49
Page 58

7 Troubleshooting Troubleshooting Guide
Symptom Possible Cause Corrective Action
The INOP Check Paper
is issued.
The INOP WRONG PAPER
SCALE
is issued.
Bad or distorted printout
within the first 1 cm of the
trace.
Poor print quality. Heat setting needs adjusting. Adjust the Thermal Printhead heat setting.
Paper not feeding properly. Paper incorrectly loaded. Load paper correctly.
Tr a ce i s no t p ri n te d
correctly with reference to
the paper gridlines.
The drawer is open and
there is paper on the paper
sensor.
Paper jam.
Paper sensor dirty.
Paper sensor defective.
The platen is dirty.
Paper is not approved by
Philips.
Inadequate contrast of paper
marks.
Paper with the wrong scale
has been loaded (for
example, European paper
has been loaded instead of
US paper).
Paper drawer was not fully
closed.
Thermal Printhead dirty.
Thermal Printhead failure.
The platen is dirty. Clean the platen (see Chapter 6, “Testing and
Offset needs adjusting. Calibrate the recorder and change the offset (see
Ensure the paper is loaded correctly, and close the
drawer.
Open the drawer, remove paper, tear off scrumpled
section of paper and re-load, or load a new pack of
paper. Close the drawer.
Clean paper sensor (see Chapter 6, “Testing and
Maintenance”).
Exchange paper sensor
(see Chapter 8, “Disassembly and Reassembly”
and Chapter 9, “Parts”.
Clean the platen (see Chapter 6, “Testing and
Maintenance”).
Use only paper approved by Philips.
Use only Philips approved paper.
Calibrate the recorder.
Check, and if necessary, replace the paper pack
with one with the correct scale. Check, and if
necessary, change the paper scale setting to the
correct setting for the paper used.
Always ensure the paper drawer is fully closed
before starting recording.
Then run the recorder Selftest to verify correct
printing (see “Fetal Recorder Selftest Report” on
page 40).
Clean the Thermal Printhead
(see Chapter 6, “Testing and Maintenance”).
Then run the recorder Selftest to verify correct
printing (see “Fetal Recorder Selftest Report” on
page 40).
Exchange the Thermal Printhead (see “Removing
the Thermal Line Printhead (TLPH)” on page 72
and “Replacing the TLPH” on page 73).
Then run the recorder Selftest to verify correct
printing (see “Fetal Recorder Selftest Report” on
page 40).
Maintenance”).
“Setting the Fetal Recorder Offset” on page 39).
50
Page 59

Troubleshooting Guide 7Troubleshooting
LAN / RS232
Symptoms Cause of Failure Failure Isolation and Remedy
External device (such as a
surveillance system like OB
TraceVue) not receiving
data
The LAN/RS232 port is
not configured for data
export
The cable between the
external device and the
monitor is not connected
correctly or defective
The external device does
not support the version of
the data export protocol
used in the monitor
A terminal concentrator is
used in between the device
and the monitor and a
protocol with dynamic
speed negotiation is used
The LAN/RS232 board is
in a wrong slot (slot has
been changed after software
configuration or an
additional board has been
plugged in)
The LAN/RS232 board is
defective
Check configuration of the LAN/RS232 ports in
configuration mode
Check cable and replace if necessary
Check if the device supports the version of the data
export protocol. Upgrade device or monitor if
necessary (if matching versions exist).
Some terminal concentrators do not support
changing the transmission speed (baud rate)
dynamically. Check if the connection works
without the concentrator
Verify correct placement of the I/O boards
Check board and replace if necessary
51
Page 60

7 Troubleshooting Troubleshooting Guide
Transducers
Symptoms Possible Cause Failure Isolation and Remedy
Transducer appears not to
work, and the transducer
Finder LED does not light
when you touch the
parameter field on the
screen.
INOP
OB EQUIP MALF
is displayed.
Transducer appears not to
work, but the transducer
Finder LED lights when
you touch the parameter
field on the screen.
Defective transducer cable.
Defective connector block.
Transducer or connector
block is defective.
Bus Master Board is
defective.
No power to Bus Master
Board.
Visually inspect the transducer cable and the cable
connector for damage. If there are obvious signs of
damage, replace the cable.
Visually inspect the connector block and the sensor
sockets for damage. If there are obvious signs of
damage, replace the connector block.
Try plugging the transducer into a different sensor
socket.
• If the Finder LED works, then the original
socket is defective. Replace the connector block.
• If the Finder LED still does not light in any of
the other sockets, try using a known good
transducer. If the Finder LED lights, the original
transducer is defective: replace it.
Try using a known good transducer. If the Finder
LED does not light in any of the sockets using a
known good transducer, then the Bus Master
Board is defective. Replace the Bus Master Board.
If both the SpO2 board and the Bus Master Board
are not working, exchange the power supply.
52
INOP
OB EQUIP MALF
is displayed.
All transducers (US, Toco,
IUP and ECG) do not
work.
INOP
OB EQUIP MALF
is displayed.
Bus Master Board is
defective.
Replace Bus Master Board.
Page 61

Troubleshooting Guide 7Troubleshooting
Symptoms Pos sible Cause Failure Isolation and Remedy
Status Log
Many events that occur during start-up or regular monitoring are logged in the Status Log. The Status Log
can be cleared. Not all entries in the Status Log are errors. You can print the Status Log only via the
Support Tool.
Transducer is connected,
INOP
OB EQUIP MALF
is displayed.
Transducer belt button is
broken or damaged.
Main CPU board is
defective.
Transducer defective.
Interrupted transducer
upgrade, or software based
malfunction of the
transducer, including
communication problems
between the Bus Master
Board and the transducer.
Mechanical damage. Replace the belt button.
Replace Main CPU Board.
Replace transducer.
Perform soft ware upgr ade of the transducer with
the Support Tool.
Handle transducers with care.
Never use a transducer with a broken or damaged
knob.
Monitor Id. Code No. Date
Time
H 18202 20100 1 4 Apr 05 16:37
C 1721 21050 1 4 Apr 05 15:37
The Status Log window shows logged events which caused a reboot of the monitor.
To enter the Status Log Window, select Main Setup -> Revision. The following list opens up:
• Status Log
• Product
• Appl. SW
• Config
•Boot
• Language
•OB
• FetRec
Select Status Log.
53
Page 62

7 Troubleshooting Troubleshooting Guide
The first column in the log identifies the event class (“C”: caused a cold start, “H”: caused a hot start, “N”:
no restart, for information only). Column 3 and 4 identify the event source and event code. Column 4
counts the number of occurrences of the event. The last column shows the time and date of the last
occurrence of the event.
The following pop-up keys overlay the SmartKeys:
Clear
StatLog
Clear StatLog
This key clears the currently displayed Status Log
M2703A
This key switches to the Monitor Revision Window
If an event occurs repeatedly, contact your Philips Service Representative.
NOTE It is possible, using the support tool, to download the status log and send it to your Philips Service
Representative as a file (for example via e-mail).
M2703A
Troubleshooting with the Support Tool
Using the support tool you can:
• access the full status log which can be saved as a file
•reload software
• identify defective devices
• reset touch screen calibration
For details on how to perform these tasks see the Support Tool User Manual.
Troubleshooting the Individual Measurements or Applications
For problems isolated to an individual parameter or application, please consult the Instructions for Use and
configuration information.
If the Instructions for Use did not resolve an individual parameter problem, then another transducer or
patient module should be tried.
If you are getting questionable readings for individual measurements you may want to do the performance
assurance tests in Chapter 6, “Testing and Maintenance”.
The performance of the individual applications are affected by the configuration of the monitor. When
contacting Philips support you may be asked about the configuration of the monitor to aid in
troubleshooting.
54
Page 63

8Disassembly and Reassembly
WARNING • Before attempting to open or disassemble the monitor, disconnect it from the AC mains supply.
• Energized circuits are accessible with the covers open. Do not work on the monitor with the covers open
and AC power connected. Only qualified service personnel should open or disassemble the monitor.
• Performance verification: do not place the system into operation after repair or maintenance has been
performed, until all performance tests and safety tests listed in Chapter 6, “Testing and Maintenance” have
been performed. Failure to perform all tests could result in erroneous parameter readings, or patient/
operator injury.
CAUTION Observe ESD (electrostatic discharge) precautions when working within the unit.
8
Introduction
Remember to store all screws and parts in a safe place for later refitting.
How to Use this Chapter
The disassembly sections detail the step-by-step procedures you use to access replaceable parts of the monitor
and the transducers.
The monitor consists of two major assemblies:
•The top cover assembly
• The bottom housing assembly
The top cover assembly consists of the top cover housing, the display assembly, the recorder assembly, and the
recorder adapter board.
The bottom housing assembly consists of the bottom housing, the power supply assembly, the main CPU
board, the bus master board, and depending on the options ordered, the noninvasive blood pressure assembly,
the SpO
All part numbers of spare parts are listed in Chapter 9.
assembly, the input device interfaces, and the RS232/LAN interface.
2
55
Page 64

8 Disassembly and Reassembly Serial Numbers
Tools Required
CAUTION When replacing the front cover, do not over-torque the screws. Excessive torque may damage the plastic
screw mountings.
You need the following tools:
• Flat-head screwdriver, head thickness 0.5 mm to fit
transducer screw
• Torx-head screwdriver, size T-10, minimum shaft length
80mm
• Small flat-head screwdriver, 2.0-3.0 mm
•Long-nosed pliers
Serial Numbers
The serial number of the monitor appears on the device nameplate at the rear of the bottom housing. It is
also stored electronically in the power supply.
• If you change the bottom housing, remove the nameplate from the old housing and fit it to the new
housing.
• If you exchange the power supply of the monitor, you may have to re-enter the monitor serial number
afterwards. Check the serial number of the monitor in the Support Tool device view to see whether this
is necessary: if the sixth digit of a monitor serial number is an “X”, you must re-enter the serial number,
which you will find on the nameplate. Refer to the Support Tool Instructions for Use for details of how to
change or re-enter a serial number.
56
Page 65

Removing the Top Cover Assembly 8 Disassembly and Reassembly
Removing the Top Cover Assembly
1 First fold the display completely flat.
1 Carefully place the monitor upside down. To avoid scratches, place the unit on some cloth or other soft
surface.
57
Page 66

8 Disassembly and Reassembly Removing the Top Cover Assembly
2
Remove the four screws securing the top cover assembly to the bottom housing, using a T-10 Torx
driver.
Screws
3 To gain access to the screw in the rear right hand corner, release the cable guide aside as illustrated.
58
4 Holding both top cover and bottom housing assemblies together, place the monitor upright again.
Page 67

Removing the Display Assembly 8 Disassembly and Reassembly
5
Separate the top cover from the bottom housing from the front of the monitor as illustrated.
6 The top cover assembly is now separated from the bottom housing assembly.
Top cover
assembly
Removing the Display Assembly
1 Remove the top cover assembly (see page 57).
2 Place the top cover assembly top down on a cloth or other soft surface.
Bottom
housing
assembly
59
Page 68

8 Disassembly and Reassembly Removing the Display Assembly
Recorder
cable
Recorder adapter board
First release the cable lock by moving it in the direction of the arrows, then disconnect the white
3
recorder ribbon cable from the recorder adapter board.
Cable lock
4 Next, disconnect the silver display ribbon cable from the recorder adapter board after releasing the cable
lock.
60
Page 69

Removing the Display Assembly 8 Disassembly and Reassembly
5
Turn over the top cover assembly.
6 Remove the two plastic hinge pins on either side of the display housing. Release them by turning the
slotted head anti-clockwise with a small flat-bladed screwdriver.
7 Squeeze the arms of the ratchet clip to remove it from the slots on the rear of the display housing and the
top cover as illustrated.
8 Gently pull the display ribbon cable through the cable guide, and remove the display assembly.
61
Page 70

8 Disassembly and Reassembly Replacing the Display Assembly
Cable guide
Replacing the Display Assembly
Replacing the display assembly is the reverse of the removal procedure.
1 With the top cover assembly facing upwards, feed the display ribbon cable through the cable guide in
the top cover assembly.
62
2 Carefully turn over the top cover assembly together with the display assembly.
3 Gently pull the display ribbon cable fully through the cable guide.
Recorder ribbon
cable
Display ribbon
cable
4 Reconnect the display ribbon cable to the recorder adapter board, ensuring that the cable lock is secure
after fitting.
Page 71

Replacing the Display Assembly 8 Disassembly and Reassembly
Reconnect the white recorder ribbon cable to the recorder adapter board, ensuring the cable lock is
5
secure after fitting.
Cable lock
6 Refit the plastic hinge pins. Do not apply excessive force when refitting the hinge pins. Turn the head of
the hinge pin gently with a small screwdriver. You will feel when the pin is seated correctly, the head
should be flush with the surface, and the slot in the head of the pin should be pointing in the same plane
as the side of the display assembly housing.
Correct final position
63
Page 72

8 Disassembly and Reassembly Recorder Disassembly
7
Refit the ratchet clip into the slots on the rear of the display housing and the top cover, as a reversal of
the removal procedure.
Recorder Disassembly
The recorder consists of the following major sub-assemblies:
• Drawer Assembly
•Recorder Chassis
•Thermal Line Printhead (TLPH) Holder
• Recorder Adapter Board
• Stepper Motor
Removing the Drawer Assembly
1 Press the paper table release to unlock the paper drawer and then pull the table forward to open it fully.
64
2 Squeeze the two plastic lugs on the underside of the drawer to release the drawer, and then pull to
remove the drawer. (Here shown with the top cover removed.)
Page 73

Recorder Disassembly 8 Disassembly and Reassembly
.
Detail showing plastic
hooks open
65
Page 74

8 Disassembly and Reassembly Recorder Disassembly
Replacing the Drawer Assembly
Before replacing the drawer assembly, refer to the previous photographs, and study the detail showing the
position of the plastic hooks when the drawer is fixed in position.
Detail showing plastic
hooks latched onto
metal guide. This is
how the hooks should
be when the drawer
is fixed in position.
1 Slide the drawer into the drawer recess on the top cover, and check that it is located correctly on the
runners.
2 Latch the two plastic hooks onto the metal guides to secure the drawer in place. You will find it easier to
use a long-nosed pair of pliers to move the hook into position, as shown in the following photographs.
66
Page 75

Recorder Disassembly 8 Disassembly and Reassembly
Final position (hook
latched onto metal
guide)
67
Page 76

8 Disassembly and Reassembly Recorder Disassembly
Removing the Recorder Chassis
1 Remove the top cover assembly (see page 57).
2 Slide open the paper drawer, to gain access to the two countersunk screws (in the following
photographs, we have removed the drawer assembly).
3 Remove the two countersunk screws.
4 Turn over the top cover assembly and place it top down on a cloth or other soft surface.
RFI bracket
Recorder chassis
Recorder
cable
Stepper motor
Paper sensor
Display cable
Recorder adapter board
under recorder
cable
68
Page 77

Recorder Disassembly 8 Disassembly and Reassembly
5
First release the cable lock by moving it in the direction of the arrows, then disconnect the white recorder
ribbon cable from the recorder adapter board.
Cable lock
6 Next, disconnect the silver display ribbon cable from the recorder adapter board after releasing the cable
lock.
7 Disconnect the stepper motor the paper sensor cable connectors from the recorder adapter board.
Paper sensor
cable connector
connector
Stepper motor
cable connector
69
Page 78

8 Disassembly and Reassembly Recorder Disassembly
8
Remove the two screws (one on each side) fastening the RFI bracket to the recorder chassis.
9 Partially unscrew the screw nearest the recorder adapter board holding the stepper motor to the recorder
chassis, until the thread no longer protrudes. This allows the necessary clearance for removing the RFI
bracket.
70
10Remove the four screws holding the recorder chassis.
Page 79

Recorder Disassembly 8 Disassembly and Reassembly
Free the RFI bracket on the stepper motor side by applying a little sideways pressure to the recorder
11
chassis, while at the same time pulling the RFI bracket forwards.
.
12Remove the RFI bracket.
71
Page 80

8 Disassembly and Reassembly Recorder Disassembly
13
Lift out the recorder chassis.
Removing the Thermal Line Printhead (TLPH)
1 Remove the recorder chassis as described in the section “Replacing the Recorder Chassis” on page 74”.
.
TLPH in holder
2 Turn the recorder chassis over.
Screws holding TLPH
to TLPH holder
72
Page 81

Recorder Disassembly 8 Disassembly and Reassembly
3
Remove the two screws holding the TLPH to the TLPH holder.
4 Turn the chassis assembly over again, and carefully remove the TLPH from the holder as shown.
Replacing the TLPH
The procedure for replacing the TLPH is a reversal of the removal procedure.
73
Page 82

8 Disassembly and Reassembly Recorder Disassembly
Replacing the Recorder Chassis
The procedure for replacing the recorder chassis is a reversal of the removal procedure (see “Replacing the
Recorder Chassis” on page 74 for the sequence).
1 Ensure that the TLPH holder has been fitted to the recorder chassis, as described in the previous
section.
2 Place the recorder chassis into position, and drive the four fixing screws in lightly. Do not tighten yet!
3 Turn over the top cover housing, then secure the two countersunk screws. This centers the recorder
chassis correctly.
4 Turn over the top cover again, and replace the RFI bracket, reversing the removal procedure. Secure the
RFI bracket to the recorder chassis with the two screws.
5 Tighten the stepper motor screw that you loosened to allow removal of the RFI bracket.
74
Page 83

Recorder Disassembly 8 Disassembly and Reassembly
6
Now tighten the four screws to secure the recorder chassis.
7 Ensure that you reconnect the paper sensor cable and the stepper motor cable to the recorder adapter
board.
Removing the Paper Sensor Assembly
1 Remove the top cover assembly (see “Removing the Top Cover Assembly” on page 57).
2 Place the top cover assembly top down on a cloth or other soft surface.
3 Disconnect the paper sense cable connector from the recorder adapter board.
Paper sensor
cable connector
4 Turn over the top cover and remove the screw holding the paper sensor to the RFI bracket.
Replacing the Paper Sensor Assembly
The procedure for replacing the paper sensor is a reversal of the removal procedure. Ensure that the paper
sensor cable is properly connected to the recorder adapter board.
Removing the Recorder Adapter Board
1 Remove the top cover assembly (see “Removing the Top Cover Assembly” on page 57).
2 Place the top cover assembly top down on a cloth or other soft surface.
75
Page 84

8 Disassembly and Reassembly Recorder Disassembly
Recorder
cable
Recorder adapter board
First release the cable lock by moving it in the direction of the arrows, then disconnect the white
3
recorder ribbon cable from the recorder adapter board.
Cable lock
4 Next, disconnect the silver display ribbon cable from the recorder adapter board after releasing the cable
lock.
76
Page 85

Recorder Disassembly 8 Disassembly and Reassembly
Disconnect the stepper motor the record-sense cable connectors from the recorder adapter board.
5
Paper sensor
cable connector
6 With all cables disconnected, remove the recorder adapter board.
Replacing the Recorder Adapter Board
The procedure to replace the recorder adapter board is a reversal of the removal procedure. Ensure that all
cables are firmly reconnected.
connector
Stepper motor
cable connector
77
Page 86

8 Disassembly and Reassembly Recorder Disassembly
Removing the Stepper Motor
1 Remove the top cover assembly (see “Removing the Top Cover Assembly” on page 57).
2 Place the top cover assembly top down on a cloth or other soft surface.
Stepper motor
3 Disconnect the stepper motor cable connector from the recorder adapter board.
Stepper motor
cable connector
4 Remove the two screws holding the stepper motor to the recorder chassis. Note that the upper screw is
secured with a small nut.
78
Page 87

Replacing the Stepper Motor 8 Disassembly and Reassembly
5 Remove the stepper motor.
Replacing the Stepper Motor
1 Refit the stepper motor to the recorder chassis, but do NOT tighten the screws yet! The upper slot on
the stepper motor allows fine adjustment when meshing the gears together.
2 Close the drawer assembly.
3 Gently mesh the stepper motor gear with that of the paper roller.
CAUTION Do NOT press the gears together or exert any pressure on the stepper motor spindle.
79
Page 88

8 Disassembly and Reassembly Replacing the Top Cover Assembly
4
When in place, tighten the screws, remembering that the upper screw is secured with a small nut.
Replacing the Top Cover Assembly
1 Ensure all items are replaced in the top cover assembly. Check that all the cables are reconnected.
2 Carefully align the front edge of the top cover assembly with the front edge of the bottom housing
assembly.
3 With the front edge of the top cover still located in the front edge of the bottom housing, gently lower
the top cover, making sure the multi-pin connector on the recorder adapter board aligns with the socket
on the main CPU board.
4 Place the top cover back to its normal position. Apply a little pressure to seat the multi-pin connector.
80
Page 89

Removing the Power Supply Assembly 8 Disassembly and Reassembly
5 Holding both assemblies together, carefully place the unit upside down on a soft surface to prevent
scratching or other damage.
6 Refit the four screws securing the top cover assembly to the bottom housing, using a T-10 Torx driver, as
a reversal of the procedure in “Removing the Top Cover Assembly” on page 57. Turn the monitor the
right way up.
CAUTION When replacing the top cover, do not over-torque the screws. Excessive torque may damage the screw
mountings.
Removing the Power Supply Assembly
1 Remove the top cover assembly (see page 57).
2 Disconnect the power supply cable connector from the main CPU board. While removing the
connector, support the end of the main CPU board to prevent excessive flexing.
Remove power
supply cable
3 Remove the three screws securing the power supply
81
Page 90

8 Disassembly and Reassembly Replacing the Power Supply Assembly
Lift the cable end of the power supply assembly with one hand, while guiding the power socket/on/off
4
switch free of the aperture in the bottom housing, then lift out the power supply
Replacing the Power Supply Assembly
The procedure to replace the power supply assembly is a reversal of the removal procedure. Remember to
reconnect the power supply cable connector.
Removing the Noninvasive Blood Pressure Assembly
1 Remove the top cover assembly (see page 57).
The NiBP assembly is identified in the next picture.
Noninvasive Blood
Pressure Assembly
Noninvasive Blood Pressure
cable
Noninvasive Blood Pressure
tubing
82
Page 91

Removing the Noninvasive Blood Pressure Assembly 8 Disassembly and Reassembly
2
Disconnect the tubing from the noninvasive blood pressure connector, and the ribbon cable from the
main CPU board.
3 Disconnect the grounding cable’s spade connector.
4 Remove the two screws holding the noninvasive blood pressure assembly to the bottom housing, then
remove the noninvasive blood pressure assembly.
83
Page 92

8 Disassembly and Reassembly Replacing the Noninvasive Blood Pressure Assembly
5
To separate the noninvasive blood pressure assembly from the noninvasive blood pressure assembly
holder, remove the three screws.
Replacing the Noninvasive Blood Pressure Assembly
The procedure to replace the noninvasive blood pressure assembly is a reversal of the removal procedure.
84
Page 93

Removing the SpO2 Assembly 8 Disassembly and Reassembly
Removing the SpO2 Assembly
1 Remove the top cover assembly (see page 57).
The SpO
assembly is identified in the next picture.
2
SpO
assembly
2
(Power supply
shown removed)
2 Remove the two screws holding the SpO
assembly.
2
Screw locations
3 Remove the flat brown cable from the rear of the SpO
sensor socket.
2
85
Page 94

8 Disassembly and Reassembly Replacing the SpO2 Assembly
4
Lift the side of the SpO2 assembly nearest the SpO2 socket, carefully disconnecting the multi-pin
connector shown.
Multi-pin
connector
5 Remove the SpO
assembly.
2
Replacing the SpO2 Assembly
The procedure to replace the SpO2 assembly is a reversal of the removal procedure.
86
Page 95

Removing the Interface Boards 8 Disassembly and Reassembly
Removing the Interface Boards
The interface boards can be accessed from the underside of the monitor’s housing.
1 Turn the monitor upside down on a non-scratch surface.
2 Release the board by pressing the clip that keeps the board in place, as shown. Use a small flat-headed
screwdriver to gently prise the board out if it is too tight to pull out with your fingers.
3 Pull the board out.
87
Page 96

8 Disassembly and Reassembly Removing the Main CPU Board
Removing the Main CPU Board
To remove the main CPU board, proceed as follows:
1 Remove the top cover assembly (see page 57).
2 Remove the screws holding the metal shield.
Screws
3 Remove the shield.
4 Disconnect the loudspeaker cable (1), the power supply cable (2), the bus master board cable (3), and
the noninvasive blood pressure cable (4) from the main CPU board.
88
12 34
Page 97

Replacing the Main CPU Board 8 Disassembly and Reassembly
5
Remove the main CPU board by lifting it straight up.
Replacing the Main CPU Board
The procedure to replace the main CPU board is a reversal of the removal procedure. Ensure all the cables
are properly reconnected.
Exchanging the Loudspeaker
1 Remove the top cover assembly (see page 57).
2 Disconnect the loudspeaker cable connector from the main CPU board.
3 Remove the three screws holding the loudspeaker, and remove the loudspeaker.
4 Refit the loudspeaker, making sure to refit the o-ring gasket. If a new gasket is required, it is available as
part of the bottom housing small parts kit. (See “Small Parts Kit - Bottom (M2703-64203)” on
page 102.)
Loudspeaker
cable connector
Loudspeaker
89
Page 98

8 Disassembly and Reassembly Exchanging the Transducer Cable
Exchanging the Transducer Cable
See the “Transducer Cable Assembly (M2735-64201)” on page 101 for items that come with the cable.
Important when fitting the screw covers! Do NOT remove the screw covers from the frame to which
they are attached. Leave them in place, as it is the only way to align the screw covers correctly. They
detach from the frame when you press them into position.
To exchange a transducer cable:
1 Pierce a screw cover with a small, flat-bladed screwdriver. Important! Do NOT try to prise out a screw
cover from the side, without piercing it, as this will damage the transducer top cover.
1 Gently rock the screwdriver back and forth until the screw cover comes out. Repeat to remove all three
screw covers
2 Remove the three screws, and remove the transducer top cover.
90
Page 99

Exchanging the Transducer Cable 8 Disassembly and Reassembly
Disconnect the small cable connector, remove the old cable, and fit the new cable (as a reversal of the
removal procedure).
3 Remove the sealing gasket from the top cover, and replace it with the new one supplied with the cable.
+
While handling a Toco/Toco
transducer, take care not to displace the strain gauge. Fit a new gasket to
the top cover, ensuring the gasket is properly seated, replace the top cover and secure it with the three
screws.
4 Leaving the screw covers attached to the frame, carefully align the screw covers with the screw recesses in
the top cover. Next, partially press in two of the covers at the same time, then press in the third one (they
detach from the frame as you push them in). Then make sure all three covers are pushed completely into
the recesses.
91
Page 100

8 Disassembly and Reassembly Exchanging the Transducer Belt Button
Exchanging the Transducer Belt Button
CAUTION NEVER immerse a transducer in liquid if the belt button has been removed, or is loose, broken or
damaged.
M2703-64204
Replacement Belt Button Kit
Contents:
1 Remove the belt button using the tool provided with the belt button kit.
x5
x1
2 Dispose of the old belt button. Take a new belt button and fit it to the transducer. Initially, screw the
button in by hand about four turns, then complete the job with the supplied tool. Stop applying force
when the head of the tool makes contact with the body of the tool at the point indicated by the arrows.
4x
92
 Loading...
Loading...