Page 1

PHYSICIAN'S
MANUAL
2011
Page 2

Page 3

TABLE OF CONTENTS
PREAMBLE ............................................................................................................................................. 1
GENERAL CONSI DERATIONS ....................................................................................................... 1
TERMS AND DEFINITIONS ............................................................................................................. 2
SERVICES INSURED BY MSI ......................................................................................................... 6
SERVICES NOT INSURED BY MSI ................................................................................................ 7
PRINCIPLES OF ETHICAL BILLING ............................................................................................... 9
TARIFF ........................................................................................................................................... 10
ASSESSMENT RULES FOR VISITS AND RELATED SERVICES ............................................... 11
ASSESSMENT RULES FOR SPECIALIZED SERVICES ............................................................. 21
ASSESSMENT RULES FOR PROCEDURES ............................................................................... 30
PROCEDURES FOR AMENDMENTS TO THE PREAMBLE AND FEE SCHEDULE .................. 42
EXPLANATORY CODES ........................................................................................................................ 1
MISCELLANEOUS .................................................................................................................................. 1
UNIT VALUES .................................................................................................................................. 1
HEALTH SERVICE CODES ............................................................................................................. 1
Additional Services..................................................................................................................... 1
Community Services .................................................................................................................. 1
Other Dental Operations NEC ................................................................................................... 1
Workers' Compensation Board .................................................................................................. 1
PROLONGED CONSULTATIONS ................................................................................................... 3
MULTIPLES ...................................................................................................................................... 3
DETENTION ..................................................................................................................................... 3
PREMIUM FEES .............................................................................................................................. 3
OUTDATED SERVICE ENCOUNTERS ........................................................................................... 3
OUTDATED RECIPROCAL SERVICE ENCOUNTERS .................................................................. 3
TERMINATION DATE ...................................................................................................................... 3
SPECIALTY ABBREVIATIONS ....................................................................................................... 4
CATEGORY ABBREVIATIONS ....................................................................................................... 4
MODIFIER DESCRIPTIONS ............................................................................................................ 5
PREAUTHORIZATION SERVICE ENCOUNTERS ........................................................................ 12
RADIOLOGY .................................................................................................................................... 1
NON-PATIENT-SPECIFIC BULK BILLING FEES ............................................................................ 1
PATHOLOGY ................................................................................................................................. 19
INTERNAL MEDICINE ................................................................................................................... 23
ANAESTHESIA ................................................................................................................................ 1
DERMATOLOGY ............................................................................................................................ 11
DIAGNOSTIC & THERAPEUTIC ................................................................................................... 19
FAMILY PRACT ICE ....................................................................................................................... 40
INTENSIVE CARE UNIT ................................................................................................................ 54
MEDICINE ...................................................................................................................................... 56
NEUROLOGY ................................................................................................................................. 65
NEUROSURGERY ......................................................................................................................... 74
OBSTETRICS & GYNAECOLOGY ................................................................................................ 90
OPHTHALMOLOGY ..................................................................................................................... 108
ORTHOPAEDICS ......................................................................................................................... 124
OTOLARYNGOLOGY .................................................................................................................. 155
PAEDIATRICS .............................................................................................................................. 169
PATHOLOGY ............................................................................................................................... 179
PHYSICAL MEDICI N E ................................................................................................................. 181
PLASTIC SURGERY .................................................................................................................... 189
PSYCHIATRY ............................................................................................................................... 207
RADIOLOGY ................................................................................................................................ 217
SURGERY .................................................................................................................................... 219
UROLOGY .................................................................................................................................... 259
NUMERIC INDEX ............................................................................................................................. 1
ALPHABETICAL INDEX ................................................................................................................ 30
Page 4

Page 5

PREAMBLE
The Preamble is the authority for the proper interpretation of the Fee Schedule. Fees will not be correctly interpreted
without reference to the Preamble. This Fee Schedule is maintained through mutual agreement by the Department of
Health and Doctors Nova Scotia.
1. GENERAL CONSIDERATIONS
Physicians may be paid by the Nova Scotia Department of Health using various remuneration methods. The MSI
Physician’s Manual details Fee-For-Service remuneration. Remuneration methods, other than Fee-For-Service,
follow the conditions of the contracts or agreements as agreed to by the physician(s), the Nova Scotia Department
of Health and Doctors Nova Scotia with respect to the specific arrangement.
1.1 Each physician who participates in the care of a patient is entitled to fair and appropriate compensation for the
services rendered to the patient.
1.2 The Fee Schedule identifies the amounts prescribed as claimable for insured services rendered by physicians.
Insured services means all services that are medically necessary and are not specifically excluded by
legislation or regulation. The listing of any service or procedure in the Fee Schedule does not ensure payment
by Nova Scotia Medical Services Insurance (MSI) if the service is provided when it is not medically necessary.
1.3 Unless otherwise indicated, fees listed are for professional services only.
1.4 Professional services provided to a patient may be claimed by a physician only when he or she
renders the visit or procedure or when he or she supervises the procedure.
1.4.1 All insured services include, where appropriate, any necessary discussion or advice to the patient or
their agent, completion of a medical record, prescribing of medication or therapy, requisitioning of
diagnostic services, arranging referrals, including a letter of referral where required, and similar
activities normally associated with providing insured services to patients.
1.4.2 Where provision of a service generates charges for long-distance telephone calls, unusual postal or
other expenses, the physician may deem them to exceed the normal allowance made in the tariff and
bill the patient directly, subject to the conditions for billing non-insured services.
1.5 Physicians are required to submit service encounters for insured services provided to eligible patients in the
format prescribed by MSI. Non-participating physicians are required by Regulation under the
and Insurance Act to give reasonable notice of this fact to a patient or someone acting on his or her behalf,
before providing a service.
1.6 Service encounters submitted beyond 90 days from date of service shall not be payable and will be
adjudicated to pay “zero” unless MSI is of the opinion the delay is justified. Resubmission of refused service
encounters must be within 185 days of the date of service. The only exception to this policy will be through
special consideration in exceptional extenuating circumstances.
Claims for registered hospital in-patients must also be submitted within the 90 day time limitation whether or
not the patient has been discharged or continues as an inpatient. In situations where the physician knows that
the claims will not be submitted within the prescribed time period, loss of revenue can potentially be avoided
by contacting MSI to request an extension.
1.7 Service encounters for services to patients from other provinces that are covered under the reciprocal billing
agreement must be submitted within 1 year of date of service. See the Billing Instructions Manual for further
details on reciprocal billing.
personally
Health Services
May 2011 PREAMBLE - 1
Page 6
1.8 PHYSICIAN RECORD REQUIREMENTS TO SUPPORT CLAIMS
1.8.1 An appropriate medical record must be maintained for all insured services claimed. The minimum
record must contain, for MSI purposes, the following:
(A) Patient’s name;
(B) Patient’s Nova Scotia Health Card Number;
(C) Date of the service for which the claim is being made;
(D) Reason for the visit/presenting complaint(s);
(E) Any clinical findings appropriate to the presenting complaint(s) and reflective of the service
code(s) claimed;
(F) Working diagnosis;
(G) Treatment prescribed;
(H) Time and duration of visit in the case of time-based fees;
(I) Name of referring physician, where appropriate;
(J) Name of consultant and rationale of referral, where appropriate; and whether referred for
diagnosis or treatment; and
(K) A Consultant will send a report to the referring physician where appropriate and retain same on
file.
1.8.2 Where a procedural code is claimed, the patient record of that procedure must contain information
which is sufficient to verify the type and extent of the procedure according to the fees claimed.
1.8.3 All claims submitted to MSI must be verifiable from the patient records associated with the services
claimed and be billed in accordance with the Preamble. If the record does not substantiate the claim
for the service, then the service is not paid for or a lesser benefit is given.
1.8.4 Where a differential fee is claimed based upon time, location, etc., the information on the patient
record must substantiate the claim.
1.8.5 Where the fee claimed is calculated on a time basis, start and finish times must be part of the patient
record of that service.
1.8.6 Documentation of services which are being claimed to MSI must be completed before claims for
those services are submitted to MSI.
1.8.7 For MSI purposes, it is required that physicians maintain records supporting services claimed to MSI
for a period of five years in order to substantiate claims submitted. For medicolegal purposes adult
patients’ records should be retained for a minimum of ten years from the date of the last entry in the
record. For patients who are children, physicians should keep the record until ten years after the day
on which the patient reached or would have reached the age of 19 years (the age of majority in Nova
Scotia).
1.8.8 All service items claimed to MSI are the sole responsibility of the physician rendering the service with
respect to appropriate documentation and claim submission.
2. TERMS AND DEFINITIONS
2.1 MEDICAL NECESSITY
Medically necessary services may be defined as those services provided by a physician to a patient with the
intent to diagnose or treat physical or mental disease or dysfunction, as well as those services generally
accepted as promoting health through prevention of disease or dysfunction.
The provision of a service listed in the Schedule of Benefits does not ensure payment by Medical Services
Insurance. Services provided in circumstances where they were not medically necessary are not insured. For
the purpose of this Preamble, Medical services, which are explicitly deemed to be non-insured under the
Health Services and Insurance Act or its Regulations, remain uninsured regardless of individual judgments
regarding their medical necessity.
May 2011 PREAMBLE - 2
Page 7
2.2 SCHEDULE OF BENEFITS
The Schedule lists all insured procedures, their descriptions and codes, any special conditions, and the value
in units. When the term schedule is used in this Preamble, it means the Schedule of Benefits. (This refers to
the electronic document).
2.3 PHYSICIAN
“Physician” means a legally qualified medical practitioner whose name is entered in the register kept by the
College of Physicians and Surgeons of Nova Scotia as being qualified and licensed to practice medicine.
He/She must be in good standing and not under suspension pursuant to any of the provisions of the Medical
Act.
2.4 GENERAL PRACTITIONER
“General Practitioner” means a physician who engages in the general practice of medicine or a physician who
is not a specialist as defined by the
2.5 SPECIALIST / SPECIALTY
A “specialist” is defined as one whose name appears in the Specialist Register of the College of Physicians
and Surgeons of Nova Scotia. However, when the term "specialty" is used, it means any or all specialties,
including General or Family Practice. For the purpose of this Preamble, the terms General and Family
Practice are used interchangeably.
2.6 STATUTORY HOLIDAYS
Holidays are defined for the purpose of claiming special rates as New Year's Day, Good Friday, Easter
Monday, Victoria Day, Canada Day, Civic Holiday, Labour Day, Thanksgiving, Remembrance Day, Christmas
2.7 TERMS USED FOR REPORTING OR DESCRIBING SERVICES TO MSI
Day and Boxing Day. The list of dates designated as statutory holidays will be issued annually by MSI.
Note: If a physician chooses to provide routine, scheduled services during a statutory holiday, he/she is not
entitled to payment at the holiday rate.
(See Section 6 and the Billing Instructions Manual)
2.7.1
2.7.2
2.7.3
2.7.4
2.7.5
2.7.6
Service
When the term “service” is used in this manual, it is in the context of an insured visit or procedure that
is identified by a specific service code in the MSI Schedule of Benefits.
Modifier
Modifiers are special codes added to the record of a service that identify the generic context within
which the service was provided (specialty, time, place, etc.). Some modifiers are for the purpose of
clarification; others affect the tariff applied to the service. A detailed list of modifiers may be found in
the miscellaneous section of this manual.
Qualifier
A qualifier is an Alpha character appended to some service codes to subdivide the code and thereby
distinguish differences specific to that procedure. e.g. 03.26A, 98.12B.
Units / Unit Value
The MSI Schedule of Benefits uses units to represent the value of a service. The value of a unit
varies according to the applicable Tariff. Two unit values exist, an Anaesthetic Unit Value used
specifically for claiming anaesthetic services, and a Medical Service Unit Value specifying the dollar
value of all other services.
Tariff
The MSI Tariff is the actual monetary value of a service. It is derived from the number of units
applicable to a service (which may vary according to relevant modifiers), the Medical Service Unit
Value, and any individual billing factors based on practice location or billing thresholds, or other
factors that may exist from time to time.
Rate
When the tariff for a service is modified by specialty, time, or some other factor, the applicable tariff
may vary according to the specific circumstances.
Medical Act.
May 2011 PREAMBLE - 3
Page 8
2.7.7 Add-On
An “add-on” is a procedure which is always performed in association with another procedure and
never by itself. An “add-on” procedure is paid at full fee.
2.8 AGE
Where age is a factor in determining eligibility for payment, or modifies the service, the following age ranges
are defined:
• Premature - 2500 grams or less at birth
• Neonate/Newborn - the 10 days following delivery
• Infant - up to and including 23 months
• Child - up to and including 15 years of age
• Adult - 16 years of age and over
See the Billing Instructions Manual for how to claim services that use age modifiers.
2.9 HOME/RESIDENCE
“Home” includes patient's home, group homes, seniors lodges, personal care homes and provincial
correctional centres. It does not include institutions as defined in Section 2.12.
2.10 GROUP PRACTICE/CLINIC
A group practice is defined as the arrangement whereby two or more physicians are in practice, and each
physician maintains and has access to medical records and histories of the patients.
2.11 HOSPITAL
For the purposes of this Preamble, hospital means a facility for the observation, care, and treatment of
persons suffering from a psychiatric disorder; a hospital for treatment of persons with sickness, disease or
injury, including maternity care, as approved under the
2.12 INSTITUTION
Licensed and approved chronic care hospitals, residential centres, nursing homes and homes for special care.
2.13 OFFICE
An "office" is defined as the location where a physician is practicing his or her profession. An office may be
located in the physician's home, in a hospital, in an institution, or in other facilities or buildings.
2.14 HOME CARE NOVA SCOTIA PROGRAMS
2.14.1
2.14.2
2.15 PARTICIPATING PHYSICIAN
A physician who is registered with MSI to receive compensation for insured medical services.
2.16 NON-PARTICIPATING PHYSICIAN
A physician who has elected not to receive compensation for insured medical services from MSI. Patient
reimbursement is described in the Billing Instructions Manual.
2.17 TECHNICAL COMPONENT
Some diagnostic procedures have separately listed technical and interpretive components. When a physician
must perform the technical component of a procedure that is normally carried out by a technician, the
physician may claim a fee for the technical component. If a technician carries out the technical component the
physician may claim for the interpretive component only.
Acute Home Care
The Acute Home Care program is a provincial program designed to provide to patients in their
homes, with acute episodic illnesses, short term acute care involving nursing and other services
available normally only in hospital, thereby preventing or shortening a hospital admission.
Chronic Home Care
Chronic Home Care is a provincial program which provides home support services, personal care
services, nursing services and home oxygen services to persons with assessed unmet needs who
are convalescing, chronically ill, disabled, or experiencing debilities of old age. Services provided
have the objectives of maintaining or improving the individual’s level of functioning; addressing the
individuals’ needs during rehabilitation or convalescence; delaying or preventing admission into
institutions; and/or providing family relief services to the individual’s informal caregivers.
Health Services and Insurance Act.
May 2011 PREAMBLE - 4
Page 9

2.18 INTERPRETIVE COMPONENT
This is the interpretation of the results of a diagnostic procedure for which a fee may be claimed separately
from performing the procedure itself.
2.19 FUNCTIONAL CENTRE
A standard area or site within a hospital or institution; e.g. outpatient department, intensive care unit, etc.
Assigned functional centre modifier will be required as part of a service encounter for services provided in
such areas.
2.20 INTENSIVE CARE UNIT
Intensive care units are special areas recognized and funded by the Department of Health to provide high
intensity care. These units would include Neonatal, Paediatric, Coronary, and such other units as are
recognized by the Department. Generally, special fees apply to patients in such areas unless the patients no
longer need the care of such a unit, but remain in the intensive care area (e.g., due to lack of beds on general
ward or recovery room).
2.21 PREMIUM FEES
Premium Fees are additional amounts paid above normal or customary rates on eligible services provided on
an emergency basis during designated times. An emergency basis is defined as services, which must be
performed without delay because of the medical condition of the patient. (See Item 7.4)
2.22 INDEPENDENT CONSIDERATION
Independent consideration is a process for assessing services where a unit value is not listed. Refer to Billing
Instructions Manual. (See Item 6.3.1)
2.23 INTERIM FEE
The tariff temporarily assigned to a new procedure during the process of adding it to the schedule of benefits.
(See Item 6.3.2)
2.24 EXCEPTIONAL CLINICAL CIRCUMSTANCES
Allowance is sometimes made for alteration of the tariff associated with individual service encounters when a
physician can demonstrate significantly increased difficulty, time, or other factors involved in providing care.
(See Item 6.3.3)
2.25 THIRD PARTY
A person or organization other than the patient, his/her agent, or MSI that is requesting and/or assuming
financial responsibility for a medical or medically related service.
2.26 EMERGENCY CARE CENTRES
An Emergency care centre is a special designation provided by the Department of Health to Emergency
departments meeting certain standards including 24-hour on-site on-call.
2.27 ANTENATAL (PRENATAL)
The term antenatal (prenatal) applies to pregnancy related visits from the time of confirmation of pregnancy to
delivery.
2.28 POST PARTUM
The term Post Partum describes in-hospital-limited visits to the mother following delivery.
2.29 POST NATAL
The term Post Natal describes a single limited visit performed approximately 6 weeks following delivery for the
purpose of assessment and advice to the mother.
2.30 OTHER LOCATIONS
This modifier applies to locations of service not defined elsewhere, such as recreational facilities, watercraft,
or roadside.
2.31 TRAVEL
Travel means movement from one geographic location to another. Interpretations specific for travel to certain
locations:
2.31.1 Within an apartment building, movement from one unit to another is considered travel.
May 2011 PREAMBLE - 5
Page 10
2.31.2 Movement within a hospital, even between separate buildings on one contiguous site, is not
considered travel. If a hospital has several geographically separate sites, movement between sites is
considered travel.
2.31.3 Movement between rooms or units of a licensed nursing home or special care institution is not
considered travel.
2.31.4 If a physician maintains a medical office within or adjoining his or her place of residence, entering the
office for the purpose of rendering emergency treatment is considered travel during certain time
periods.
2.31.5 If a physician has arranged to have an office in a hospital or in an attached building, going from the
office to the hospital to attend a patient is not considered travel.
2.32 DETENTION AND OFFICE VISITS
Medical detention occurs when a practitioner’s time is given exclusively to one patient for active treatment
and/or monitoring of that patient at the sacrifice of all other work. Detention time may only be claimed for
emergency care and/or treatment provided outside of the office. (See Section 7.3)
2.33 TRANSFER OF CARE
Transfer of care occurs when the responsibility for the care of a patient is completely transferred, either
temporarily or permanently, from one physician to another. (See Section 7.8.1)
2.34 MOST RESPONSIBLE PHYSICIAN
The most responsible physician is the attending physician who is primarily responsible for the day to day care
of the patient in hospital.
2.35 LOCUM TENENS
A physician who temporarily replaces another physician who is absent from the practice.
(See Billing Instructions Manual)
Note: The locum physician may not claim under the billing number of the physician being replaced.
2.36 SESSIONAL FEES
Sessional fees apply to pre-approved services of a physician engaged on a time basis; e.g., approved group
immunization and Well Women's Clinics, public health medicine or other professional services to a
government department, agency or public body. For proper submission of service encounters refer to the
Billing Instructions Manual.
3. SERVICES INSURED BY MSI
3.1 Physicians' services rendered to persons registered with MSI in a recognized clinical setting; e.g., the patient's
home, the doctor's office, at a hospital, clinic or institution, or scene of an emergency. This includes all
diagnostic, medical, psychiatric, surgical, or therapeutic procedures, including the services of anaesthetists
and assistants as per the definition of medical necessity in Item 2.1. Some services may require prior
approval.
3.2 Family planning or contraceptive advice, insertion of intrauterine devices and similar appliances, and
sterilization procedures. Therapeutic abortion is an insured service.
3.3 Completion of a medical certificate for observation for the purpose of a patient's admission for psychiatric
evaluation.
3.4 Services that are insured, but with restrictions:
routine
3.4.1 Coverage for
10 years of age and for those 65 years of age and over. For all others, routine refractive vision
analysis is an uninsured service.
3.4.2 Age specific preventive services where indicated as determined by current guidelines for well baby
care, vaccinations, inoculations, etc. This would include examinations offered to individuals who
refractive vision analysis is limited to once every 24 months for persons under
May 2011 PREAMBLE - 6
Page 11

have a family history, symptoms or signs or other diseases that put them at risk for preventable target
conditions.
3.4.3 Group sessional clinics, e.g., immunization or “well person”, when pre-approved by MSI. (See Billing
Instructions Manual for details)
3.4.4 Complete history and physical examinations, but only when medically necessary to establish a
diagnosis (See “Services Not Insured by MSI”).
3.4.5 The services of an anaesthetist when required in conjunction with specified dental surgical
procedures listed in Schedule A of the Regulations of the Health Services and Insurance Act and only
when medical necessity requires these services to be performed in a hospital.
3.5 When complications occur following a non-insured procedure, treatment which is medically necessary is an
insured service.
4. SERVICES NOT INSURED BY MSI
Fees for the following services are not insured by MSI. The physician must determine who has responsibility for
payment, if any. When complications arise following an uninsured procedure see Section 3.5.
4.1 Services available to residents of Nova Scotia under the
of Veterans' Affairs, Canadian Forces, RCMP, the
Canada or under any statute or law of any other jurisdiction either within or without Canada.
4.2 When a prescription or a requisition for a diagnostic or therapeutic service is provided to a patient without a
clinical evaluation of the patient, the requirements of an insured visit service have not been met and no service
encounter should be submitted.
4.3 Diagnostic, preventive or other physician's services available through the Nova Scotia Hospital Insurance
Program, the Department of Health, or other government agencies.
4.4 Autopsy services, except by alternate service encounter submission mechanisms.
(See Billing Instructions Manual)
4.5 Services at the request of Third Parties
Health examinations or provision of health information required in connection with employment, insurance,
admission, legal proceedings, etc., or any similar request by a third party are not insured. Responsibility for
payment may lie either with the patient or the third party requesting the examination or information. This
excludes Third Party as defined in Section 18 of the
The following are examples only, and do not represent a complete list:
4.5.1 Insurance company examinations and requests for medical information
4.5.2 Examinations requested by educational institutions, youth groups, summer camps
4.5.3 Employer requested examinations, sick certificates
4.5.4 Examinations required to support legal claim
4.5.5 Services required by a legal proceeding including preparation of records, reports, letters or
certificates, or appearance and/or testimony in a court or other tribunal
4.5.6 Department of Immigration - Passport or Visa
4.5.7 Any diagnostic services associated with the above
4.6 Services, supplies, and other materials provided through the physician's office when such supplies are not
normally considered part of office overhead.
4.6.1 Photocopying or other costs associated with transfer of records
Workers' Compensation Act, through the Department
Hospital Insurance Act, any Act of the Parliament of
Health Services and Insurance Act.
May 2011 PREAMBLE - 7
Page 12

4.6.2 Long distance telephone charges incurred specifically on the patient's behalf
4.6.3 Items such as drugs, injectable materials, biological sera, dressings, strapping, tray fees, etc. used in
rendering medical care, except for pap smear tray fees and Provincial Immunization tray fees
4.6.4 Medical/Heal th devic es (e.g., eye glasses, contact lenses, hearing aids, surgical appliances, trusses,
wheelchairs, crutches and prosthetic appliances)
4.6.5 Physician's advice by telephone, letter, fax or e-mail is an uninsured service.
However, telephone, fax or e-mail advice for Home Dialysis, Acute Home Care, Chronic Home Care,
Anticoagulant Supervision and Palliative Care are insured services under certain circumstances
4.6.6 Mileage or travelling time except as defined in Item 7.3 relating to Detention Time or blended
mileage/travel detention for Acute Home Care home visits
4.7 Physicians’ services provided to their own families
4.8 Gender Reversal (Trans-sexual surgery)
4.9. Services which, in the opinion of the Department of Health, have been performed for cosmetic purposes only.
4.9.1 Cosmetic Surgery is defined as a service done solely for the purpose of altering the appearance of
the patient and not medically necessary
4.9.2 When there is doubt as to whether the proposed surgery is medically required or cosmetic, the
operating surgeon should obtain prior approval from MSI. Anaesthetic and other fees associated with
non-insured services are non-insured as well. MSI will pay for a visit or consultation to determine if a
treatment method is insured, even though the proposed procedure is non-insured.
4.10 Group immunizations performed without receiving pre-approval by MSI
4.11 Acupuncture
4.12 Electrolysis
4.13 Reversal of Sterilization
4.14 In-vitro fertilization
4.15 Comprehensive visits when there are no signs, symptoms, or (family) history of disease or disability, which
would make such an examination medically necessary. This excludes those examinations performed in
accordance with guidelines in 3.4.2 relating to preventive health exams.
4.16 Services provided by other health care workers, with certain exceptions, which are not insured under MSI.
This would include services of chiropractors, podiatrists, physiotherapists, psychologists, nurses or other
paramedical personnel.
4.16.1 Dental services, except those which are described as benefits under the MSI Dental Program.
Information can be obtained by contacting MSI office.
4.16.2 Ancillary services, such as charges for an ambulance, etc.
4.16.3 Optometric services, exc ept those, which are described as benefits under the MSI Optometric
Program. Information can be obtained by contacting MSI office.
4.17 Costs of medical services, which are primarily related to research or experimentation, are not the responsibility
of the patient or MSI.
4.18 There are alternate submission methods for Holter, ECG, Pathology, Diagnostic Radiology and other services
performed and billed to MSI. See non-patient specific bulk billing sections of the Physician’s Manual.
4.19 Blood Alcohol Sampling and Documentation at the request of the Department of Justice
May 2011 PREAMBLE - 8
Page 13

4.19.1 Claims for Blood Alcohol Sampling on impaired drivers will be processed by Medavie Blue Cross
Accounting Department, for reimbursement by the Department of Justice. The total fee should
include:
(a) venipuncture, if performed by the physician, at the rate listed in the Schedule of Benefits
(b) kilometers to be paid at the current government rate. Information on the current rate may be
obtained from the Department of Health or any other Provincial Department
(c) if travel time is involved, the rate will be paid based on the fee for detention as listed in the
Schedule of Benefits
(d) where appropriate documents are completed, a fee of 45 units may be claimed
4.19.2 Where insured medical services are provided to the impaired driver, the physician should cl aim under
the appropriate MSI code in the usual manner. Where insured medical services are not provided to
the impaired driver, the appropriate visit fee may be added to the above and billed to the Department
of Justice. Under no circumstances should a visit be claimed to both the Department of Justice and
MSI.
4.19.3 Service encounters based on the rates above should be submitted on the physician's letterhead to:
Accounting Department
Medavie Blue Cross
P. O. Box 2200
Halifax, NS B3J 3C6
4.20 Sexual Assault Examination
4.20.1 This is an assessment of a patient in which the physician follows the protocol prescribed by the
Department of Justice for the investigation of alleged sexual assault.
4.20.2 The forensic examination portion of the treatment of a sexual assault victim is not insured under MSI,
but can be billed to the Medavie Blue Cross Accounting Department for reimbursement by the
Department of Justice in the same manner as for Blood Alcohol sampling above. The police agency
requesting the forensic examination must be indicated. (See Billing Instructions Manual re: fees)
Where insured medical services are provided to the sexual as sault victim, the physician should cl aim
under the appropriate MSI code in the usual manner.
5. PRINCIPLES OF ETHICAL BILLING
5.1 A physician who provides professional services to a patient is entitled to compensation commensurate with
the services provided to the patient. These services are des ignated as ei ther insured or non-insured. Insured
services are those listed in the MSI Physician's Manual.
5.2 Ethical principles of billing for non-insured services are outlined in the publication “Guide to Billing Non-Insured
Services,” Doctors Nova Scotia. Information can be obtained by contacting Doctors Nova Scotia.
5.3 The following principles apply to service encounters for insured services:
5.3.1 All insured services claimed must reflect services rendered personally by the physician in an
appropriate clinical setting. Certain delegated medical acts done under supervision of the physician
present on the premises may also be claimed.
5.3.2 A physician will not claim for services rendered to members of his or her family.
5.3.3 As part of the provision of an insured service, patients may be charged directly for the provision of
consumable items not covered by MSI, completing forms, photocopying, long distance telephone,
and similar charges. These charges must be explained and agreed to by the patient before the
insured service is provided. (See Item 4.6)
5.4 Billing for insured and non-insured services at the same visit.
May 2011 PREAMBLE - 9
Page 14
5.4.1 A physician must exercise caution whenever billing MSI and the patient or a third party during the
same visit. In principle, under no circumstances should any service, or any component of a service,
be claimed for twice.
5.4.2 Whenever possible, the attending physician must acquaint the patient, or person responsible for the
patient, with the financial obligation involved in the patient's care.
5.4.3 If the insured service is the primary reason for the visit, any additional charges for non-insured
services must be explained to, and accepted by, the patient before provision of these services.
Charges for non-insured services will reflect only those services over and above those provided on
an insured basis. It is not appropriate to bill both MSI and WCB for the same service.
5.4.4 At no time should provision of insured services be contingent upon the patient agreeing to accept
additional non-insured services.
5.4.5 When physicians are providing non-insured services, they are required to advise the patient of
insured alternatives, if any exist.
5.4.6 Incidental findings
(a) If an inconsequential health matter or finding is discovered or discussed during the provision of a
non-insured service, it is not appropriate to claim for an insured service.
(b) If a significant health matter or finding becomes evident, necessitating additional insured
examination(s) or treatment(s), then these subsequent medically necessary services may be
claimed to MSI.
5.4.7 When a non-insured service is the primary reason for the visit, any service encounter for insured
services provided, as a medical necessity will reflect only services over and above those provided on
a non-insured basis.
6. TARIFF
The MSI tariff is negotiated between the Department of Health and Doctors Nova Scotia.
6.1 The Canadian Classification of Diagnostic Therapeutic and Surgical Procedures (CCP) forms the basis for
descriptions of services in the Schedule of Benefits insured by MSI.
6.2 The MSI adaptation of CCP does not include all possible CCP codes and MSI uses two additional levels of
detail as follows:
6.2.1 Qualifiers are appended to a CCP code to distinguish between related procedures applied to the
same anatomic area or condition, or to accommodate procedures that are a composite of two or
more services.
6.2.2 Modifiers describe the context of a service according to who performed the service, who received the
service and when, where, and sometimes how the service was provided.
6.3 Units per service are determined through the Fee Schedule Advisory Committee, a standing committee of the
Master Agreement Steering Committee with representation from Doctors Nova Scotia, Department of Health
and the District Health Authorities. An attempt is made to set the number of units for a service relative to other
services in the schedule, reflecting factors such as duration, complexity, overhead, specialty status, and time
of day or week. Practitioners are expected to use the published units for insured services except in the
following instances:
6.3.1 Independent consideration is applied to certain services recognized to have wide variation in case to
case complexity and time. Refer to Billing Instructions Manual. Independent consideration services
must be accompanied by complete details, including duration of service, adequate to explain and
justify the number of units requested. (See Item 2.22)
May 2011 PREAMBLE - 10
Page 15

Note: Independent consideration no longer refers to situations where an interim tariff has been
established or for exceptional clinical circumstances as explained below.
6.3.2 Interim Fees may be established in certain circumstances with approval by Department of Health. A
CCP Code will be activated to describe the new service and an Interim Fee assigned. Interim Fees
will be published in the MSI Physicians’ Bulletin.
6.3.3 Exceptional Clinical Circumstances may warrant a fee other than that listed. In the event a
practitioner performs a service he or she believes should be insured, but is unable to find an
appropriate service code, or finds an appropriate service code but feels the listed tariff does not
adequately compensate the service, a request for an exceptional fee may be submitted. The request
must be accompanied by complete details, including the duration of the service, adequate to explain
6.3.4. If a physician feels a particular fee is under or overvalued in relation to similar services, he or she
and justify the number of units requested.
Note: The exceptional fee process is not intended for use on a routine basis when a physician
disagrees with the listed tariff for a service.
should request Doctors Nova Scotia consider renegotiating the fee with the Department of Health.
7. ASSESSMENT RULES FOR VISITS AND RELATED SERVICES
7.1 “Visit” is a generic term used for service encounters where there is an evaluation of a patient either as the sole
service, or in association with one or more procedural services. A visit may not be claimed where the
procedural service includes a visit component or where claiming a visit is otherwise prohibited. Visits are
governed by a common set of rules, and more specific rules apply to diff erent categories of visits. Visits may
occur in all locations; and include consultations; counseling; and care, as in directive, continuing, or supportive
care.
There are several different CCP codes that apply to visits and multiple factors that modify these codes. Care
must be taken to identify the appropriate code for the visit service provided, and any modifying factors. Not all
combinations of codes and modifiers are valid.
7.2 VISIT TYPES
7.2.1
7.2.2
7.2.3
(a) When the sole reason for the visit is to provide a procedure to a patient, only the listed
(b) Only one visit may be claime d from a single service encounter.
(c) A Comprehensive or Initial Limited Visit may not be claimed within 30 days of a Comprehensive
A Limited Visit or an Initial Limited Visit may be claimed when the physician provides a limited
assessment for diagnosis and treatment of a patient's condition. It includes a history of the
presenting problem and an evaluation of relevant body systems.
A Comprehensive Visit or a subsequent comprehensive visit is an in-depth evaluation of a patient
necessitated by the seriousness, complexity, or obscurity of the patient’s complaint(s) or medical
condition. This service includes ensuring a complete history is recorded in the medical record and
performing a physical examination appropriate to the physician’s specialty and the working diagnosis.
General Visit Rules
procedure fee will apply.
Consultation on the same patient for the same condition.
(d) A Comprehensive Visit may not be claimed within 30 days of a previous Limited or
Comprehensive Visit. However, a Subsequent Comprehensive Visit service may be claimed by
the specialties of Internal Medicine, Neurology, and Paediatrics. These restrictions do not apply
to General Practice.
(e) An Initial Limited Visit service used by certain specialties may not be claimed within 30 days of
any visit or procedure. A Limited Visit only will apply.
May 2011 PREAMBLE - 11
Page 16

(f) Visits requested in one time period and performed in another time period must always be
(g) When follow-up visits are made at the convenience of the physician, the 0800 to 1700, Monday
(h) If more than one visit is provided by the same physician to the same patient on the same day in
(i) A Pap Smear may not be claimed in addition to a visit, consultation or procedure for a
(j) When a visit was made solely for an injection, then only an injection may be claimed. The
(k) A visit is not claimable with Psychotherapy or Counseling codes at the same service encounter.
7.2.4
(a)
(b)
(c)
(d)
(e)
Limited Visits by Location (See Section 7.2.6)
claimed using the lesser of the two rates.
to Friday visit rate will apply.
separate service encounters, documentation of the necessity for the extra visit(s) must be
recorded on the chart. Time of service occurrence must be provided on second and subsequent
visits.
gynecological or obstetrical diagnosis, nor is it payable in addition to a complete physical exam.
injection must be provided under the direct supervision of a physician physically present on the
premises.
Office - A Limited Visit may be claimed when the physician sees the patient and performs a
limited assessment for a new condition or when monitoring or providing treatment of an
established condition.
OPD - Emergency Department - A Limited Visit may be claimed when the physician provides
medical treatment to a patient presenting to an OPD - Emergency Department. It is payable at
the appropriate fee for the time at which the service is provided.
Hospital - A Limited Visit may be claimed when the physician provides dail y care to the patient.
Daily limited visits may be claimed by more than one physician when different conditions are
being treated. A weekly maximum applies to routine hospital visits to patients after 56 days
hospitalization except for paediatricians. Multiple unscheduled visits on the same day are
excluded from the weekly maximum.
Discharge Fee - A hospital Discharge Fee may be claimed by the physician (either a general
practitioner or a specialist when a patient is admitted for non-surgical hospitalization) who
performs the activities involved in discharging a hospital in-patient. These activities include, as
necessary, the completion of the patient’s chart, discharge summary, writing prescriptions for
the patient, providing discharge instructions to the patient and arranging for follow up care for
the patient.
The fee is not payable where major surgery, minor surgery, major fracture and/or minor fracture
care is provided in a hospital setting unless a patient is transferred to a general practitioner for
follow-up care after surgery/fracture care. In this case, the general practitioner may claim the
discharge fee if the general practitioner performs the discharge duties. This fee cannot be
claimed by the operating surgeon in association with any surgical code being billed.
A hospital visit fee may be claimed in addition to the discharge fee where a hospital visit is
provided on the same day.
Acute Home Care - A Limited Visit may be claimed when the physician provides daily care to the
patient and may occur at the patient’s home or OPD. Acute care services may be provided for
up to 15 days but are to be discontinued when no longer required. The patient’s requirement for
Acute Home Care is reviewed regularly. An average length of stay of 5 to 7 days in Acute Home
Care is anticipated. If appropriate, patients may be transferred to Chronic Home Care if they
require ongoing home care services for convalescence or continuing care following the period of
acute illness.
In exceptional circumstances, extended admissions for up to a total of 30 days may be
authorized by the Care Co-ordinator in consultation with the attending physician.
May 2011 PREAMBLE - 12
Page 17
(f)
(g)
7.2.5
(a)
(b)
(c)
(v) Acute Home Care - A Comprehensi ve Visit may be claimed for the direct admission to the
(d)
(e)
7.2.6
(i) First Patient Seen: The rate for the first patient seen is only applicable for those cases
(b)
Home or Other Locations - A Limited Visit may be claimed when the physician provides a limited
examination for diagnosis and treatment of a patient's condition or provides ongoing treatment of
an established condition.
Institutions (See Section 7.2.6(d))
Comprehensive Visits by Location
Office - Comprehensive Visits in the office may not be claimed more than once every 30 days
when diagnosing and treating a new condition or further complications of an existing condition.
Visits provided within a 30-day period for the same condition or complication should be claimed
as a Limited Visit. (See Item 7.2.3)
OPD or Emergency Department - A Comprehensive Visi t may be claimed, when appropriate, in
the OPD or Emergency when a patient is seen for the first time that day by that physician.
Follow-up visits for the same condition on the same or subsequent day should be claimed as a
Limited Visit.
Hospital - A Comprehensive Visit may be claimed for the first examination in hospital for
diagnosis and treatment once per patient per admission for each specialty involved in the care
of the patient. If a patient has a comprehensive visit in the Emergency Department by the family
doctor covering the ED and is then admitted and has a second comprehensive visit by a
different (admitting) family doctor, the ED physician may claim the Complete Examination code
and the admitting physician may claim the First Examination code.
(i) If a specialist readmits a referred patient within 30 days for the same or related condition,
only a Limited Visit may be claimed.
(ii) There are no restrictions on Paediatricians readmitting referred patients.
(iii) If a specialist readmits an un-referred patient within 10 days for the same or related
condition, only a Limited Visit may be claimed.
(iv) If a General Practitioner readmits any patient within 10 days for the same or related
condition, only A Limited Visit may be claimed.
Acute Home Care Program from the office, home, OPD and unscheduled emergency
locations. This must follow notification to the appropriate Home Care Nova Scotia
Coordinators. The service will include the first examination for diagnosis and treatment once
per patient, per admission.
Home or Other Locations - A Comprehensive Visit may be claimed when diagnosing and
treating a new condition or further complication of an existing condition, but may not be claimed
more than once every 30 days. Comprehensive Visits provided within a 30-day period will be
approved at the appropriate Limited Visit fee.
Institutions (See Section 7.2.6(d))
Rules Specific to Location
(a)
OPD and Emergency Department - If the patient is kept in OPD or Emergency under
observation for more than 4 hours, an additional Limited Visit may be claimed when the need
can be supported by the patient's condition and documentation on the chart.
requiring the physician to make a separate trip to the OPD or Emergency Department.
(ii) Additional Patients: An Extra Patient Limited Visit is applicable for additional patients seen
following the first patient. The rate for extra patients is applicable for additional patients seen
following each separate trip to the hospital. An Extra Patient Limited Visit applies in those
situations where a physician is in the hospital for any purpose and is asked to see a patient
in the OPD or Emergency Room.
The Emergency Care Centre visit rates may only be claimed in designated Emergency Care
Centres approved by the Department of Health.
May 2011 PREAMBLE - 13
Page 18
(c) A Home Visit is a service rendered by a physician to a patient or patients following travel to the
patient's home. The patient or patient's representative must request the physician to visit. A
Home Visit may only be claimed when the patient's condition or situation justifies the service. If
the nature of the patient's condition requires periodic scheduled home visits, a daily home visit
can be claimed. (See Items 7.2.3(f), 7.2.3(g))
(i) Additional patients seen in the same apartment or private dwelling: The first person seen is
claimed at the Appropriate Home Visit. Other patients seen are claimed as additional
patients. However, a visit to another apartment in the same building is regarded as a
separate home visit and the appropriate fee should be claimed for the first person seen
therein.
(d)
7.2.7
7.2.8
7.2.9
Definitions:
An Institutional First Visit arises when, at the specific request of an appropriate institutional
authority, patient or patient's family or guardian, the physician visits and renders services to the
patient in an institution.
(i) Additional patients seen at the same visit should be claimed at the appropriate Limited Visit
fee.
(ii) When prearranged routine trips are made to an institution, Limited Visit Fees shall be
claimed only for those patients where medical necessity exists.
(iii) If the physician believes his or her services are inadequately compensated under the
institutional visit rules, he or she may enter into a contractual agreement with the institution
for a form of “retainer” or other remuneration method to supplement his or her income from
visit fees. This supplemental remuneration would be a non-insured service.
Urgent Visits (All locations)
The underlying principle is that the demands of the patient’s condition and/or the physician
interpretation of that condition, is such that the physician must respond immediately. Immediate
attendance because of personal choice or availability does not constitute an Urgent Visit. (See the
definition of travel in Item 2.31)
Urgent Visit - Hospital Inpatient - Request by hospital staff. An Urgent Visit applies when a
(a)
physician travels to see a registered inpatient at the request of hospital staff.
Urgent Care in Office - Request by Patient. An urgent care visit applies when the physician is
(b)
called to see the patient and must travel to his or her office outside the hours of 0800 to 1700
Monday to Friday or during other scheduled office hours. An Urgent Care Visit does not apply to
a patient attending the office during scheduled office hours regardless of the patient’s condition.
If additional patients are seen at the same time, a limited visit applies.
Urgent Visit - Sacrifice of Office Hours - All other locations. An Urgent Visit may be applied
(c)
when the physician is called to see a patient and interrupts his or her regular office hours and
travels from one location to another to attend the patient.
Management of Closed Head Injury - Initial examination and recommendation re further treatment.
This service may be claimed only by a Paediatrician or Neurosurgeon.
General Practice Complex Care Visit
A complex care visit code may be billed a maximum of 4 times per patient per year by the f amily
physician and/or the practice (not by walk-in clinics) providing on-going comprehensive care to the
patient who is under active management for 3 or more of the following chronic diseases: asthma,
COPD, diabetes, chronic liver disease, hypertension, chronic renal failure, congestive heart failure,
ischaemic heart disease, dementia, chronic neurological disorders, cancer. The physician must
spend at least 15 minutes in direct patient intervention and the visit must address at least one of the
chronic diseases either directly or indirectly. Start and finish times are to be recorded on the patient’s
chart.
The term active management is intended to mean that the patient requires on-going monitoring,
maintenance or intervention ro control, limit progression, or palliate a chronic disease.
The term chronic neurological disorders is intended to include progressive degenerative disorders
(such as Multiple Sclerosis, Amyotropic Lateral Sclerosis, Parkinson’s disease, Alzheimer’s disease),
May 2011 PREAMBLE - 14
Page 19

stroke or other brain injury with a permanent neurological deficit, paraplegia, or quadriplegia and
epilepsy.
7.2.10
7.3 DETENTION TIME (See Definition Item 2.32)
Detention commences 30 minutes after the practitioner is first in attendance and may be claimed in 15-minute
increments thereafter. This may include travel time spent with the patient travelling from one location to
another. However, travel time to transport donor organs from a donor site to the recipient site for
transplantation, begins at the time the retrieving surgeon accompanied by the donor organs leave the donor
site. Where any service is performed during the time spent with the patient, either the service, or the
Detention Time, but not both, should be claimed. The circumstances in each case, and the time involved,
should be documented with the service encounter. When claimed with a Comprehensive or Limited
Consultation, Detention Time commences after one hour.
7.3.1 Detention Time Does Not Apply To:
7.3.2 Detention Time Is Not Payable In Conjunction with Fees Paid for the Following on the Same Day:
(a) Intensive Care or Critical Care (See Items 7.9.2 and 7.9.3 )
7.4 PREMIUM FEES (See Definition Item 2.21)
Premium fees may be claimed for certain services provided on an emergency bas is during designated time
periods. An emergency basis is defined as services, which must be performed without delay because of the
medical condition of the patient.
7.4.1 Premium Fees May Be Claimed For:
(a) Consultations, except where a consult is part of the composite fee
(b) Surgical procedures except those performed under local or no anaesthetic
(c) Fractures regardless of whether an anaesthetic is administered
(d) Obstetrical deliveries
(e) Newborn Resuscitation
(f) Selected Diagnostic Imaging Services
(g) Pathology Services
Case Management Conference Fee
A case management conference is a formal, scheduled, multi-disci plinary health team meeting. It is
initiated by an employee of the DHA/IWK , or a Director of Nursing or Director of Care of an eligible
Long Term Care facility to discuss the provision of health care to a specific patient. Neither the
patient not the family need to be present.
It may be claimed by more than one physician simultaneously as necessary for case management.
The case conference must be documented in the health record with a list of all physician participants.
To claim the case conference fee, the physician must participate in the conference for a minimum of
15 minutes and remuneration will be calculated in 15 minute time increments based o n the sessional
rate. Start and finish times are to be recorded on the patient’s chart.
(a) Waiting time for an operating room, x-rays, laboratory results or administrative duties
(b) Counseling or Psychotherapy
(c) Advice given to the patient or patient's family or representative(s)
(d) Waiting time for a patient's arrival for assessment or treatment
(e) Waiting time for attendance by another medical practitioner or consultant
(f) Return trip if the physician is not in attendance with a patient
(g) Time spent in completing or reviewing patient charts
(h) More than one patient at a time
(i) Office visits
(b) Diagnostic and therapeutic procedures
(c) Obstetrical Delivery
May 2011 PREAMBLE - 15
Page 20
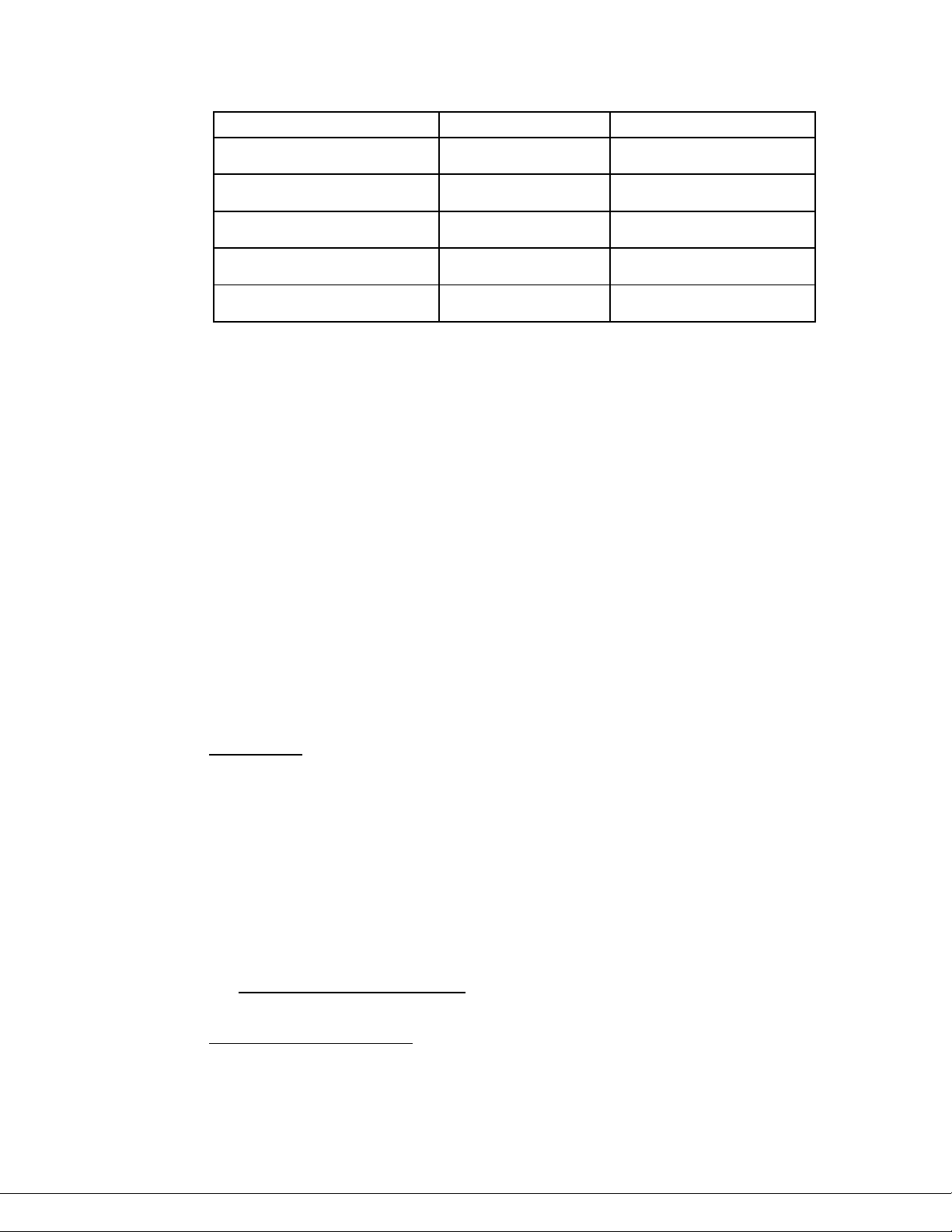
Time Period
Time
Payment Rate
Monday to Friday
17:00 - 23:59
US=PREM (35%)
Tuesday to Saturday
00:00 - 07:59
US=PR50 (50%)
Saturday
08:00 - 16:59
US=PREM (35%)
Saturday to Monday
17:00 - 07:59
US=PR50 (50%)
Recognized Holidays
08:00 - 23:59
US=PR50 (50%)
7.4.2 The designated times where premium fees may be claimed and the payment rates are:
Premium fees also apply to emergency anaesthesia for a surgical procedure (not a diagnostic or
therapeutic) provided by a non-certified anaesthetist at the interruption of his or her regularly
scheduled office hours.
Premium fees are paid at 35% or 50% of the appropriate service code but at not less than 18 units for
patient-specific services and at not less than 9 units for non-patient-specific diagnostic imaging and
pathology services paid through the hospital by special arrangement with MSI (See Section 9.7)
7.4.3 If a service requires use of an anaesthetic, the anaesthetic start time determines if a premium fee
may be claimed.
7.4.4 Premium fees may not be claimed with:
(a) Detention
(b) Critical Care/Intensive Care
(c) Diagnostic and Therapeutic Procedures other than Selected Diagnostic Imaging Services (See
Section 7.4.1)
(d) Surgeons and assistants fees for liver transplants
7.5 REFERRED SERVICES
Referred services include all types of Consultations and any Visits subsequent to the original referral. In the
absence of a proper referral, specialty rates may not apply.
7.5.1
7.5.2
A consultation is a service resulting from a formal request by the patient's physician, nurse
practitioner, midwife, optometrist or dentist, after appropriate evaluation of the patient, for an opinion
from a physician qualified to furnish advice. This may arise when the complexity, obscurity or
seriousness of the patient's condition demands a further opinion, when the patient requires access to
specialized diagnostic or therapeutic services, or when the patient, or an authorized person acting on
the patient's behalf, requests another opinion.
A consultation requires a written report to the referring physician, nurse practitioner, midwife,
optometrist or dentist; an evaluation of relevant body systems; an appropriate record; and, advice to
the patient. It may include the ordering of appropriate diagnostic tests and procedures as well as
discussion with the patient, other persons relevant to the case, and the referring physician, nurse
practitioner, midwife, optometrist or dentist. The composition of a consultation will vary with a
particular specialty.
Health Services and Insurance Act, Item 33, provides that Nova Scotia Medical Services
The
Insurance has the authority to require a copy of the consultation report for administrative purposes.
A Comprehensive Consultation is a Comprehensive Visit as per Section 7.2.2 with a written report to
the referring physician, nurse practitioner, midwife, optometrist or dentist. This service includes
performing and recording of a complete history and a complete physical examination appropriate to
the physician's specialty.
May 2011 PREAMBLE - 16
Page 21
7.5.3 A Limited Consultation is performed when the nature of the patient's problem does not warrant a
comprehensive consultation. A limited consultation includes a history limited to and related to the
presenting problem, and an examination, which is limited to relevant body systems.
7.5.4
7.5.5
7.5.6 Consultations for Non-Specialist Physicians will usually be paid at the general practitioner
7.5.7 A consultation may not be claimed in the circumstances listed below:
7.5.8 Some services may not be claimed in addition to a consultation. (See Section 9.2.9(b))
7.6 CARE BY MORE THAN ONE PHYSICIAN
Care by more than one physician refers to ongoing visit services provided to a patient where some form of
coordination of the responsibility for the patient's care between a referring physician and the consultant(s) is
implied. All care visits are coded as Limited Visits, and the nature of the responsibility of the physicians
involved determines the role claimed. (See Definition for Transfer of Care in Item 2.33)
7.6.1
A Repeat Consultation applies only where there has been a re-referral of the patient by the same
physician, nurse practitioner, midwife, optometrist or dentist to the same consultant for the same
condition, or complication thereof within 30 days of the initial consultation. A repeat consultation
requires all the elements of a limited consultation and implies interval care by another physician.
The situation where the
repeat consultation.
A Prolonged Consultation
for comprehensive consultations and a half-hour for repeat consultations. A prolonged consultation
cannot be claimed with a limited consultation. Prolonged consultations are paid in 15-minute time
blocks or portion thereof. Prolonged consultations are not to be confused with active treatment
associated with detention.
A prolonged consultation may be claimed only by the following specialties:
(a) Anaesthesia
(b) Internal Medicine
(c) Neurology
(d) Physical Medicine
(e) Paediatrics
(f) Psychiatry
consultation rate except where alternative arrangements have been made with the Department of
Health.
(a) Where ongoing care is provided without an original referral the appropriate non-referred visit is
payable.
(b) The patient's regular attending physician cannot claim a consultation and must claim the
appropriate visit.
(c) A consult may not be claimed for referrals from other health care professionals; e.g., nurses,
podiatrists. However consults may be claimed for referrals from nurse practitioners, midwives,
optometrists and dentists.
Supportive Care is defined as a Limited Visit provided by the family physician or referring physician in
a situation where the responsibility for the medical and surgical care of a registered hospital in-patient
has temporarily been transferred to a consultant.
(a) Service encounters are limited to only once every three days from the date of hospital admission
up to and including the ninth day, and twice weekly thereafter for the remainder of the patient's
hospital stay.
(b) If medical complications develop or are present which require active management by the
referring physician, regular Hospital Visits, not Supportive Care, should be claimed.
consultant requests the patient to return for a later examination is not a
may be applied to cases where the consultation extends beyond one hour
May 2011 PREAMBLE - 17
Page 22
7.6.2 Directive Care is defined as a Limited Visit following a consultation that can be claimed for services
provided in the office, home or to registered in-patients by specialist consultants. It is intended that
the referring physician is responsible for the general condition of the patient and that the consultant is
directing only the care relevant to his/her specialty. In such cases the consultant may claim Directive
Care and the referring physician may claim the appropriate home, office or in-patient visit. More than
one specialist at a time may claim directive care on a patient.
7.6.3
7.7 SUPERVISION
Supervision of treatment by a physician, without actually having a “face-to-face” interaction with the patient, is
a service that may be claimed in the following special cases.
7.7.1 Supervision of Home Dialysis refers to supervision by a nephrologist of patients registered in a Home
(a) Home Dialysis P rogram registration is initiated when a patient begins training or is accepted into
(b) No in-patient chronic dialysis supervision fees may be charged on the registered patients.
(c) The supervisory fee is for comprehensive management of all aspects of home dialysis care for
(d) Supervisory fee is claimed monthly by the supervising nephrologist for each home dialysis
7.7.2 Supervision of a patient on long term anticoagulant therapy may be claimed once monthly if the
7.7.3 Payment for supervision of a registered Acute Home Care patient can include medical chart review,
7.8 OTHER CARE OR VISITS
7.8.1
(a)
Continuing Care is defined as a Limited visit following a consultation that can be claimed for services
provided in the office, home or to registered in-patients by specialist consultants. It is intended that
the consultants assume responsibility for the care of the patient's medical condition. When the
patient remains in the hospital and the consultant is providing Continuing Care the general
practitioner or paediatrician may claim Supportive care. Only one consultant per specialty may claim
Continuing Care for a patient at a time. When a specialist is providing continuing care in the home or
office, the General Practitioner may claim the appropriate visit code.
Dialysis Program.
a program, and terminates with successful transplantation, change to in-centre dialysis, loss of
resident status, or death.
However if a registered patient is admitted to a centre without an attending nephrologist and the
patient is incapable of performing their own dialysis the attending physician may claim the
treatment of chronic renal failure by any dialytic method. Other in-patient visits and procedures
may be claimed during hospital admission.
registered patients, including all scheduled or emergent out patient visits, direction of care by
phone or other means, and liaison with other treating physicians.
program patient registered as of the first day of that month. For newly registered patients,
service encounters commence the following month.
patient's treatment is managed by telephone, fax or e-mail advice. If the date of service falls within a
complete month of hospitalization, this service may not be claimed.
telephone calls, fax or e-mail advice and blended mileage/travel detention. (See Billing Instructions
Manual)
Transfer of Care
A transferal, as distinguished from a referral, takes place when there is formal transfer of
responsibility for the patient’s care from one physician to another. (See Item 2.33)
Temporary transfer would include situations where the first physician must be absent (e.g.,
holiday or illness) and arranges patient coverage by the second physician with the intention of
resuming care of the patient upon return.
Permanent transfer would involve any situation where the physician has no intention of
resuming care of the patient.
May 2011 PREAMBLE - 18
Page 23
(b) Regardless of specialty, the physician to whom the patient is transferred is not entitled to a
consultation or comprehensive visit fee. When transfers occur from one specialty to another, or
from one hospital to another occur, the receiving physician may be entitled to a consultation or
comprehensive visit fee.
(c) However, if the patient has a medical problem necessitating referral to another physician, and
responsibility for the patient’s care is transferred with, or subsequent to the referral, it is
appropriate for the receiving physician to claim a consultation.
7.9 INTENSIVE CARE UNIT
7.9.1 Intensive Care Unit (ICU) services refers to services rendered in intensive care units (ICUs) approved
by the Department of Health by physicians who have been assigned by a hospital to the ICU staff by
reason of special training or experience.
7.9.2
(a) The 24-hour time period for claiming ICU services is from 8 a.m. to 8 a.m. of the following day.
7.9.3
General Rules
(b) There should only be one Day 1 (First Day) claimed during the same ICU admission even if the
patient’s status changes. Day 1 is normally the date of admission to the ICU. However if the
physician does not actually see the patient until the next day (e.g., because a resident is
covering), then Day 1 can be the date when the patient is first seen by the physician. Day 1 can
only be claimed again if the patient is re-admitted to the ICU at least 24 hours after discharge.
This does not preclude Ventilatory Care Day 1 and Critical Care Day 1 being claimed on the
same day.
(c) Two physicians may claim ICU fees for the same patient on the same day but not the same fee
code; e.g., one can claim Critical Care and the other can claim Ventilatory Care. However, no
other ICU fee code may be claimed in addition to Comprehensive Care. Also, the Intensive
Care daily rate may not be claimed in addition to Critical Care.
(d) If a patient is transferred from one ICU to another in the
ICU fees on the same day. However, this precludes billing another Day 1.
(e) When a transfer to a
can claim in a 24-hour period.
(f) ICU fees can be claimed up to and including the day that the patient is medically suitable for
transfer from the ICU or off ICU care. Then the Intensive Care daily rate or continuing care,
depending on the condition of the patient, should be claimed if the patient remains in the ICU
after the transfer order is written.
(g) To claim ICU fees under ordinary circumstances, intensivists should be immediately available to
the ICU.
(h) A surgeon can claim ICU fees, except for ICU Day 1 codes immediately following surgery, for
his/her own post-operative patient if he/she is the sole providing physician to the patient in the
ICU. Surgeons do not ordinarily claim ICU fees during the postoperative period because other
physicians provide care in the ICU. However, some facilities do not have enough staff available
for separate coverage of the ICU and, under these circumstances, a surgeon can claim ICU
fees. This does not prevent a surgeon from claiming ICU fees for non-operative patients.
Critical Care Codes (Critical Care, Ventilatory Care and Comprehensive Care)
These codes may only be claimed for daily care of critically ill patients admitted to intensive care units
approved by the Department of Health. The Critical Care, Ventilatory Care and Comprehensive Care
services listed below include initial consultation and assessment and daily management of the
patient. Use of these codes precludes claiming for detention on any patient on the same day.
different hospital occurs, more than one physician (in different hospitals)
same institution, both sites can claim
May 2011 PREAMBLE - 19
Page 24
(a) Critical Care - Critical Care comprises all aspects of care of a critically ill patient in a designated
intensive care area. Critical Care excludes ventilatory support except as designated below.
These fees do not apply when patients who are not
area; or when patients who were critically ill recover but remain in the intensive care area (e.g.,
lack of beds on general ward or recovery room).
Ventilatory Care - This includes provision of all types of ventilatory care including face mask
(b)
ventilation; e.g., bipap ventilation; management of the intubated airway, including tracheal toilet
by suction catheter with or without instillation; and use of mechanical ventilation of the critically ill
patient; as well as the supervision and obtaining of blood for blood gas assessment.
Comprehensive Care - When a physician provides both critical care and ventilatory support
(c)
services to a patient, a service encounter claim should be submitted for Comprehensive Care.
(d) The following specific procedures are included within the critical care tariff:
• Arterial puncture
• Blood gases
• Cardiac arrest
• Cardioversion and non-invasive transthoracic pacing
• Defibrillation
• Emergency resuscitation
• Haematology and biochemistry
• Insertion of arterial lines percutaneously or by cut down
• Insertion of chest tube
• Insertion of CVP catheters percutaneously or by cut down
• Insertion of intravenous lines
• Insertion of urinary catheters and nasogastric tubes
• Interpretation of laboratory tests
• Interpretation of rhythm strips
• Intracranial pressure monitoring interpretation
• Lumbar puncture
• Management of cardiac arrhythmias
• Paracentesis
• Stress test
• Thoracentesis
• Venipuncture of peripheral and central veins
(e) The following procedures are excluded from critical care and may be claimed separately:
• Bronchoscopy
• Insertion of temporary pacemakers
• Intra aortic balloon catheters
• Left heart catheterization with angiograms and coronary arteriograms
• Esophago-gastroscopy
• Peritoneal dialysis for acute renal failure
• Radionuclide scans
• Selective coronary graft angiography
• Selective pulmonary angiogram
• Swan Ganz Catheterization
• Ultrasonography
7.9.4
Intensive Care
The Intensive Care daily rate may be claimed by one physician per patient per twenty-four hours.
Should a procedure be performed on the patient during this time, then the physician has the option of
claiming for the procedure or for the intensive care but not for both.
Intensive Care Detention may be claimed on an hourly basis, if needed, when a patient de-stabilizes.
If codes for detention are claimed for a patient, then the Intensive Care daily rate cannot be claimed
for that patient. The daily rate may be charged for other patients. A duration of service must be
provided on these service encounters. An hourly sessional fee may be claimed in certain
circumstances.
critically ill are admitted to an intensive care
May 2011 PREAMBLE - 20
Page 25
7.9.5 Beating Heart Donor
If the support of a beating donor (03.05A) does not require continuous attendance by an ICU
physician and the physician can attend to other patients, then the regular Intensive Care Unit Codes
are to be claimed for the support of the beating donor.
7.10 PALLIATIVE CARE
7.10.1
7.10.2
7.10.3
Consultation
The Palliative Care Consultation can only be claimed by designated physicians (general practitioners
or specialists) with recognized expertise in palliative care. The service provided must fulfill the normal
requirements for a consultation as specified in the Preamble. The consultation includes a
psychosocial assessment, comprehensive review of pharmacotherapy, appropriate counselling, and
consideration of appropriate community resources where indicated. A prolonged consultation cannot
be claimed. Specialists can claim the palliative care consultation fee or the consultation fee
appropriate to their specialty. It is payable once per patient per physician. Physicians billing the
Palliative Care Consult must forward a letter to MSI indicating his/her credentials.
Physicians providing palliative care must have completed a minimum of six days of intensive didactic
or small group training in palliative care, and a one-week clinical practicum in palliative care with a
qualified physician supervisor.
Support Visit
The Palliative Care Support Visit is a time-based all-inclusive visit for the purpose of providing pain
and symptom management, emotional support and counselling to patients with terminal disease.
The physician must spend at least 80% of the time claimed with the patient and cannot claim for
any other visits with the patient on the same day. Palliative care support can be claimed for the
last 90 days before the patient’s death and is billed retroactively. The physician must keep records to
support the claims, as well please be advised to include text on any outdated claims.
As physicians billing Palliative Care Support visits will be unable to determine the 90 day previous to
death he/she must initially submit the appropriate visit fee when seeing the patient. Once date of
death is indicated the physician must delete the previously billed appropriate visit and then bill the
Palliative Care Support Visit for any visit service provided in the previous 90 days.
Chart Review and/or Telephone Call
The Palliative Care Medical Chart Review and/or Telephone call, fax or e-mail advice eligible for
payment are those initiated by health care professionals involved with the care of the palliative care
patient. Telephone calls, fax or e-mails initiated by the palliative patient or his/her family members
are not eligible. Physicians and health care professionals involved should keep a detailed record of
telephone calls, fax or e-mails. Palliative care medical chart review and/or telephone calls, fax or emails can be claimed for the last 90 days before the patient’s death and are billed retroactively.
8. ASSESSMENT RULES FOR SPECIALIZED SERVICES
8.1 GENERAL RULES REGARDING SPECIALIZED SERVICES:
8.1.1
Payment of Specialist Fees
Under MSI, insured services provided by specialists would only be payable at the rate listed for visits
under that particular specialty when the service provided is within the field of the specialty concerned.
If such services are not considered to be within the specialty field, payment will be made at
appropriate Family Practice rates. Physicians who are not specialists but do specialist work will not
be paid specialist rates. Specialist visit rates are payable only to those physicians whose names
appear on the Specialist Register of the College of Physicians and Surgeons of Nova Scotia and
where there has been a referral of the patient to the specialist by the attending physician, nurse
practitioner, midwife, optometrist or dentist. Patients seen at the initiative of the specialist without a
referral will not entail payment of specialist rates.
The MSI physician number of the referring doctor, the MSI midwfe number of the referring midwife,
optometrist provider number, dentist provider number or the MSI nurse practitioner number of the
referring nurse practitioner, who is subject to a Collaborative Practice Agreement with a physician as
approved by the Diagnostics and Therapeutics Committee of the College of Registered Nurses of
(See referred services Item 7.5)
May 2011 PREAMBLE - 21
Page 26
Nova Scotia (“the Nurse Practitioner” ) and who has the agreement of the physician to refer patients
to specialists, must appear on the service encounter. If the number of the referring doctor, the nurse
practitioner, midwife, optometrist or dentist is not indicated, then the service encounter will be
returned for resubmission. Where no prior service by the referring doctor, nurse practitioner,
optometrist, dentist or midwife can be identified, a confirmation of referral may be requested.
8.1.2
8.2 ANAESTHETIC SERVICES
8.2.1 An Anaesthetic Consultation applies if a registered anaesthetist is requested by another physician to
8.2.2
Clinical Supervision
A teaching physician is entitled to receive payment for the services he or she provides in a teaching
setting with the assistance of a resident or medical student. He or she shall be present at, and assist
in, the performance of such services or shall be immediately available to render assistance when
necessary.
No fees shall be payable to a medical specialist for seeing a patient within the framework of his or her
teaching and research functions.
A physician may claim either for the resident's procedure or for his or her own services, but not both,
when they are performed at the same time.
No visit or procedural fee may be claimed if the patient is not seen by the teaching physician at the
time that the visit or procedure is rendered except under the following circumstances:
(a) In psychotherapy, where the presence of the attending physician would distort the
psychotherapy milieu, it is appropriate for the attending physician to claim for psychotherapy
when a record of the interview is carefully reviewed with the resident and the procedure thus
supervised. However, the time charged by the attending physician may not exceed the total
time spent by him or her in both such interview and direct supervision and should not exceed the
total time spent by a physician with the patient.
(b) In other departments or services , the attending physician should only cl aim for visits on the days
when actual supervision of that patient's care takes place through the presence of that attending
physician in the clinical teaching unit on that day. This, of course, involves a physical visit to the
patient and/or a chart review with detailed discussion with the other member(s) of the health
team.
(c) In those situations where on a regular basis an attending physician might supervise concurrently
multiple procedures or services through the use of other members of the team, the total service
encounters made by the attending physician shall not exceed the amount that the attending
physician might claim in the absence of the other members of the team.
Any service encounter rendered should be in the name of the responsible attending physician.
see a patient in consultation because of the complexity, obscurity, or significance of pre-existing
medical problems prior to the administration of an anaesthetic. In these circumstances, the
anaesthetist may claim a consultation fee as well as the anaesthetic fee.
An Anaesthetic Consultation may also apply in situations where the anaesthetist has been referred a
patient for the purpose of pain control, or other anaesthesia specialty related services.
The routine pre-anaesthetic evaluation does not qualify as a consultation, regardless of where and
when this evaluation is performed, as this evaluation is included in the fee for the anaesthesia. Preanaesthetic clinic assessments for same day surgery shall not be deemed to form part of the fee for
anaesthesia services.
General Rules for Anaesthetic Services
The fees listed are for all types of anaesthetic services required for the performance of an insured
procedure by another physician.
May 2011 PREAMBLE - 22
Page 27
(a) A physician cannot claim for both the anaesthesia and the procedure(s) performed under that
anaesthesia, except where the procedure is an anaesthesia-related procedure; e.g., fibreoptic
bronchoscopy for airway management, pulmonary toilet, etc.
(b) All anaesthetic services are time-based composite fees which normally include a preoperative
evaluation, administration of anaesthetic substances, injections, transfusions, IV's, procedures
such as intubation, laryngoscopy, use of anaesthesia monitoring equipment, other procedures
related to the anaesthetic technique used and post operative attendance.
(c) Post operative attendance is interpreted as terminating at that time when the anaesthetist is no
longer in personal attendance, having determined that the patient can safely be placed under
the customary post-operative supervision. Additional time for repeat visits to the patient in the
recovery room, as the need occurs, may be added to the anaesthesia time.
(d) Approved preanaesthetic clinics for same day surgery are paid as sessional fees.
(e) Anaesthetic services must be provided in a hospital or facility approved by the Department of
Health.
8.2.3
(b)
Calculation of Anaesthetic Fees
Anaesthetic fees are determined by adding the Basic Units and Anaesthesia Time Units.
A Basic Unit is listed for most procedures. It is the value assigned to each procedure to cover
(a)
all anaesthetic services except the time actually spent either in administering the anaesthesia or
in unusual detention with the patient. Additional procedures, not routine components of an
anaesthetic procedure, will be billed either as additional anaesthesia procedures, or as
replacements for, or additions to, the basic units. These procedures include the following items,
for which the basic rate will be increased or replaced by a unit value specific to the factors listed
below (See Billing Instructions Manual):
(i) Controlled Hypotension - when using a specific technique to produce hypotension in
association with an anaesthetic, the units will be increased.
(ii) Resuscitation of Newborn - When providing anaesthesia for a delivery, it becomes
necessary to provide active resuscitation of the newborn, an additional fee may be added to
the mother's service encounter for anaesthetic. If the anaesthetist was not involved in the
mother's care, service encounters for resuscitation should be claimed under resuscitation in
the normal manner.
(iii) Anaesthesia for infants under 5000 grams - the units are increased.
(iv) Anaesthetic for pacemakers - When monitoring of pacemaker function with pacemaker
monitoring programming equipment is performed in addition to the anaesthesia for
pacemaker insertion, an additional fee may be claimed.
(v) Cardiac Bypass - When a pump with or without an oxygenator and with or without
hypothermia is employed in conjunction with an anaesthetic, the anaesthetic Basic Units will
be replaced.
Note: Arterial catheterization, right cardiac catheterization (Swan Ganz) and central venous
pressure monitoring may not be claimed in addition to the basic units for cardiac
bypass.
(vi) Hypothermia - When employed in conjunction with anaesthesia, the Basic Unit will be
replaced.
(vii) Epidural Anaesthesia - The basic units for obstetrical or non-obstetrical pain management
for the introduction of catheter and maintenance care are different and will be distinguished
by an appropriate modifier.
Anaesthetic Time Units, except where otherwise specified, are computed by allowing one unit
for each fifteen minutes, or part thereof, of anaesthesia time. Double time units apply when
anaesthetic time extends beyond one hour for procedures with basic anaesthetic values of 4 or
5 units and after two hours when the basic is 6 units or greater. Anaesthesia time begins when
the anaesthetist is first in attendance with the patient for the purpose of creating the anaesthetic
state and ends when the patient has been placed under customary post operative supervision
and the anaesthetist is no longer in personal attendance.
If resuscitation is necessary during the anaesthetic time, add the time for resuscitation to the
anaesthetic time. Resuscitation and anaesthesia time cannot be claimed simultaneously.
May 2011 PREAMBLE - 23
Page 28
8.2.10
8.2.11
8.2.4
8.2.5
8.2.6
8.2.7
8.2.8
8.2.9
Claiming for Procedures in Addition to Anaesthetic Fees
When an approved add-on procedure is performed for the purpose of monitoring a patient intra
operatively or post operatively; e.g., insertion of an arterial line, pulmonary artery catheter (SwanGanz) or central venous pressure catheter, nerve block or insertion of epidural catheter for
postoperative pain management, the appropriate CCP codes may be claimed in addition to the usual
anaesthetic fee according to rules for payment of multiple diagnostic and therapeutic procedures.
Anaesthetist's Presence Required
Where a physician requests an anaesthetist to be available to provide monitored anaesthesia care at
any period during which the physician is carrying out a procedure without general or regional
anaesthesia, he or she shall be paid the usual anaesthetic fee for basic and time value for the
complete period, whether or not anaesthesia is administered for any or all of that period.
The anaesthetist should be in the operating room area. During this time no other procedures may be
claimed.
More than One Anaesthetist Present at the Same Time
When special circumstances require the services of more than one anaesthetist in the interest of the
patient, the second anaesthetist will be entitled to claim 50% of the applicable anaesthetic fee, except
in the case where specific second anaesthetist fee schedules exist; e.g., liver transplantation.
Consecutive Anaesthetist
Where one anaesthetist starts a procedure and is replaced by another during an anaesthetic
procedure, the first anaesthetist should claim the appropriate basic fee plus time units for the time he
or she is present and the second anaesthetist should claim the time units for which he or she is
present. The start time of the first anaesthetist shall dictate when double time units begin, for either
and both anaesthetists. The second anaesthetist will start to claim double time units when the double
time unit point is reached, based on the case start time (if not already beyond this point, in which
case double time units would be claimed at the time of takeover). Accordingly the consecutive
anaesthetist must indicate the case start time as well as the consecutive start time. The end time for
the first anaesthetist and the start time for the consecutive anaesthetist should coincide.
Anaesthetic Stand-By Fee
This fee applies only when a scheduled anaesthesia is not given or is delayed for more than one
hour. The stand-by fee is claimed using the Medical Service Unit Value rather than the Anaesthetic
Unit Value and is calculated in half hour intervals or portion thereof. The specific Anaesthetic
standby fee code is to be used.
Cancelled Surgery
(a) If an anaesthetist examines a patient prior to surgery and
(i) determines the patient is not a candidate for surgery and the operation is cancelled prior to
the induction of anaesthesia, the anaesthetist may claim a Limited Consult; or
(ii) if the surgery is cancelled for some other (non-anaesthetic) reason prior to the induction of
anaesthesia, he or she may claim a Limited Visit (formerly hospital subsequent visit) for this
service.
(b) If the operation is cancelled after induction, regardless of whether the Surgeon has started, the
procedural basic units plus time units shall apply, except in the case where a higher basic fee
would apply, as might occur for example, in the case of a cardiac arrest resuscitation.
Bilateral/Multiple Procedures
When bilateral or multiple surgical, diagnostic, or therapeutic procedures are performed during the
same anaesthetic, the anaesthetist shall claim the Basic Units corresponding to the procedure having
the highest Basic, plus Time Units. When procedures are performed at separate times with separate
anaesthetics, the anaesthetist is entitled to claim full anaesthetic units for each procedure.
Anaesthetic Detention
When the safety and welfare of the patient necessitates the presence of an anaesthetist immediately
before or after anaesthesia for services not considered usual pre or post operative care, it is
appropriate to claim this time as anaesthetic time and add it to the total time claimed.
May 2011 PREAMBLE - 24
Page 29
8.2.12 If an epidural has not been inserted for labour or for the surgical delivery (C/S) but is inserted post
delivery for pain control, an anaesthetist may claim for maintenance of post op epidural pain control
using time units only.
8.2.13 An anaesthetist may claim a new basic for post op pain control following an initial anaesthetic service
if there has been a time lapse from the time that he/she released the patient to the recovery room
staff.
8.2.14
8.3 OBSTETRICAL SERVICES
8.3.1
(a) Routine prenatal care includes care for less serious obstetrical complications incidental to the
(b) Only one prenatal Comprehensive Visit may be claimed per pregnancy.
(c) No more than 12 limited (routine) Prenatal Visits may be claimed for one patient's pregnancy
(d) All prenatal visits include pregnancy related counselling or advice to the patient or patient's
(e) Any prenatal visit, limited or comprehensive, includes a pap smear. The Prenatal
(f) Complicated pregnancies may require additional visits. (See Billing Instructions Manual )
8.3.2
8.3.3
Anaesthetic Independent Consideration
For procedures indicated that have no listed value, the basic portion of the calculated value will be
the same as that listed for a comparable procedure. Consideration for region and modifying
conditions or techniques may be requested. Documentation of the modifying factors is required by
MSI. (See Billing Instructions Manual)
Routine Prenatal Care
pregnancy; e.g., cystitis and simple anaemia, false labour, mild hypertension, leucorrhea,
vaginal discharge and obesity.
regardless of the number of physicians involved.
representative(s).
Comprehensive Assessment includes venipuncture, as well.
Prenatal care does not include services rendered for major complications related to pregnancy
requiring hospital care, visits or services for conditions unrelated to pregnancy, nor care of the
newborn.
Attendance at Labour and Delivery
This is a service involving constant or periodic attendance on a patient during the period of labour to
provide all aspects of care. This includes the initial assessment, and such subsequent assessments
as may be indicated, including ongoing monitoring of the patient's condition.
Obstetrical Delivery covers services rendered during delivery, including medical or surgical inductions
by the attending physician, suturing of minor lacerations, hypnosis, detention time during labour, local
or regional anaesthesia and manual removal of placenta by the attending physician, and all
obstetrical maneuvers that may be required (e.g., use of forceps).
Obstetrical Delivery - Specific Rules
(a) All deliveries performed between 1700 to 0800 hrs; all day Saturdays, Sundays and holidays (as
defined in 2.6) qualify for the appropriate premium fee. (See Section 7.4.2)
(b) Multiple Deliveries
(i) Multiple vaginal births are paid additional fees.
(ii) In the c ase of multiple births, when both a vaginal delivery and a Caesarian Section must be
performed, the C-section is claimed at full fee and the vaginal delivery at 65%.
(ii) When multiple babies are delivered by Caesarian Section, only one service encounter may
be made.
May 2011 PREAMBLE - 25
Page 30
(c) Obstetrical Surgeries do not follow the usual surgical rules as stated in Section 9.3. Pre and
post operative visits with a pregnancy-related diagnosis are paid in addition to the surgical
procedure.
(d) Obstetrical Non Surgical Deliveries
Pre-delivery consultations may be claimed only in exceptional clinical circumstances.
(e) (i) When the term of pregnancy has been 20 weeks or more, the delivery fee is paid in full.
(ii) When the gestation period is less than 20 weeks, the appropriate procedural or visit code is
payable.
8.3.4
8.3.5
8.3.6
8.3.7
8.3.8
8.4 PAEDIATRIC SERVICES
8.4.1
Postpartum Care
In hospital postpartum care is the routine care of a well mother in the postpartum period. Visits may
be billed starting on the first calendar day following birth. Although not normally claimed by more
than one physician, general practitioners and delivering specialists may charge postpartum visits
concurrently.
Post Natal Care Visit
A Post Natal Care Visit usually occurs about 6 weeks following delivery. The service may include a
pelvic examination with pap smear. It may be billed only once following delivery by one physician. It
is not considered a post-operative visit in the context of surgical/procedural rules. A diaphragm fitting
or insertion of an IUD can be claimed with a postnatal visit.
Specialist Obstetrical Care
Specialist rates may be claimed only when there is both a referral
referral. The fact that the patient has been referred does not in itself indicate the presence of
obstetrical difficulties necessitating referral. The indications for the medical necessity must be stated
on the service encounter. Where there is no medical necessity, transfer of a patient to an
obstetrician by a doctor who does not practice obstetrics is not a referral.
Obstetrician (or GP) Present to Assist at Delivery
The following services may be claimed in addition to the service encounter for delivery by the
physician receiving assistance.
(a) When an obstetrician’s presence is requested at a delivery performed by another physician,
he/she should claim an Obstetrical Delivery using the assistant modifier.
(b) When an obstetrician is present at a delivery to assist a General Practitioner, he/she may claim
a Specialist Obstetrical Delivery.
(c) MSI recognizes and pre-authorizes certain non-obstetricians in areas without specialist
obstetrical services as being allowed to claim obstetrical assistance to another physician during
labour and delivery. The rate claimed is equivalent to the Specialist Obstetrical Delivery.
Obstetrical Patients Transferred During Labour
A transfer fee may be claimed for situations where a general practitioner admits and provides care for
an obstetrical patient and then transfers that patient to another facility for delivery because of
complications of the mother and/or fetus requiring specialist intervention.
general practitioners only.
Detention may be claimed with this fee if the general practitioner accompanies the patient by
ambulance to the second facility, but is only payable for the time the physician spends on route to the
second facility.
The transfer fee, with or without detention, is not payable if the referring general practitioner attends
the delivery at the second facility and is paid the delivery fee.
Newborn Care
Newborn Care is the routine in-hospital care of a healthy infant on a daily basis up to the first five
days after birth. It includes a Comprehensive Assessment, Limited Visits as appropriate and
and medical necessity for the
This fee is billable by
May 2011 PREAMBLE - 26
Page 31

necessary parental advice. Care of unhealthy infants who are born with an existing medical condition,
or whose condition deteriorates after birth, should be claimed as any other hospitalized patient.
Newborn Care includes treatment of minor conditions.
Newborn Care may not normally be claimed for the same patient by more than one physician per
day. When a well baby is transferred to another hospital, service encounters for newborn care by a
physician at each hospital may be appropriate.
The fee for a circumcision or a release of tongue tie is payable in addition to a newborn care visit,
when medically necessary, and should be submitted as EC (Exceptional Circumstance) with text.
8.4.2
8.4.3
8.4.4
8.4.5
Well Baby Care
Well Baby Care refers to periodic office visits of a well baby for routine measurement of growth and
development, necessary parental instructions and necessary immunizations. Well Baby Care visits
are payable as one per month during the first six months; one visit during each three-month period up
to one year of age; and one visit at eighteen months of age. The visit fee at twelve months of age
have a four week buffer on either side of the first birthday for billing. The visit fee at eighteen months
of age have a two week buffer on either side of the date of eighteen months of age for billing.
Paediatric Care by a Paediatrician
(a) If newborn and premature care is provided by a paediatrician (care of a healthy newborn in
hospital), the paediatrician must claim at the same rate as Newborn Care for a General
Practitioner. No consultation is payable to the paediatrician if the infant is referred for the care
of a healthy newborn.
(b) If newborn and premature care is provided by a paediatrician to an infant who appears initially
well but becomes ill after a number of days with a condition that would normally require a
consultation, a Consultation may be claimed.
(c) Routine care is considered to include minor conditions; e.g., mild jaundice, cradle cap and mild
skin conditions.
Attendance at High Risk Delivery
(a) Paediatrician
Attendance by a paediatrician at a high-risk delivery is payable as a Comprehensive
Consultation and if it is extended beyond 1 hour, it is payable as a Prolonged Consultation.
(b) Non-Paediatrician
Attendance by a non-paediatrician at a high-risk delivery is payable as a Limited Visit in hospital
modified with the role of resuscitation.
Paediatric Care of Over-age Patients Age 16 up to and Including 18 Years of Age
(a) Services associated with the care of over-age patients in hospital by a paediatrician are to be
paid at paediatric rates.
(b) Paediatric consultations, whether comprehensive or limited, at any location for over-age patients
are to be paid at paediatric rates.
(c) Visits, excluding paediatric consultations, outside hospital for over-age patients are not to be
paid at paediatric rates except for:
(i) Behavioral management.
(ii) Follow-up visits in a paediatrician’s office for approved over-age patients with complex multi-
system medical problems. Application must be made in writing to the MSI Medical
Consultant and prior approval obtained for each patient.
May 2011 PREAMBLE - 27
Page 32

8.5 PSYCHIATRIC SERVICES
8.5.1
8.5.2
8.5.3
8.5.4
8.6 PSYCHOTHERAPY
The following services apply to General Practitioners (See Definition in Section 2.4) and Psychiatrists.
Restrictions apply to General Practitioners only.
The provision of psychotherapeutic services by General Practitioners is limited to 20 hours per patient or
family or group per physician per year. To exceed this limit for individual patients or families or groups, the
General Practitioner must either: document on the chart and notify MSI, through the text field on the service
encounter, that a Psychiatrist concurs that extended psychotherapeutic services are needed; or, if the General
Practitioner is unable to access a Psychiatric Consultant directly, then the option will be available to obtain an
exemption in a timely manner through MSI from a Psychiatric Consultant(s) skilled in psychotherapy and its
applications.
8.6.1
Psychiatric Care
Psychiatric Care is any form of assessment or treatment by a psychiatrist on the Register of
Specialists of the Province of Nova Scotia, in which there is consideration and attempted alteration of
the patient's bio-psychosocial functioning.
Psychiatric Assessment
Psychiatric Assessment of an accused person when requested by the court requires the name of the
judge involved in the case.
Therapeutic/Diagnostic Interview
This service relates to a specific child and may take place with allied health professionals, education,
correction, or other community resources. This applies to interviews by psychiatrists but does not
preclude resident involvement.
Salaried/Contract (Facility-based) Psychiatry
This refers to non-Fee for Service psychiatric care provided in the context of public mental health
services.
(a) Physicians providing these services are remunerated on a salaried or contract basis.
(b) No physician providing Salaried/Contract Psychiatric services may claim on a Fee for Service
basis for any services to a patient registered as a public mental health services client except by
special arrangement between the director of the facility at which the patient is registered, MSI,
and the psychiatrist involved.
Individual Psychotherapy
Individual Psychotherapy is any form of treatment for mental illness, behavioral maladaptions and/or
other problems that are assumed to be of an emotional nature in which a physician deliberately
establishes a professional relationship with a patient for the purposes of removing, modifying or
retarding existing symptoms, of attenuating or reversing disturbed patterns of behavior and of
promoting positive personality growth and development.
(a) Individual Psychotherapy is claimed in 15-minute intervals. The therapist must spend at least
80% of the time claimed in therapeutic intervention with the patient.
Restrictions (Apply to General Practitioners only)
(b)
(i) A minimum of 2 intervals must be claimed per visit.
(ii) Treatment for medical complaints, acute adjustment reactions or bereavement reactions do
(iii) Unless unusual clinical circumstances can be demonstrated to the Medical Consultant at
• More than 90 continuous minutes (or 6 continuous fifteen minute intervals) per patient per
• A patient younger than 4 years old
• More than one General Practitioner treating the same illness for a particular patient
not qualify as psychotherapy. They should more appropriately be claimed as counselling.
MSI, individual psychotherapy may not be claimed for the following:
day
May 2011 PREAMBLE - 28
Page 33

8.6.2
8.6.3.
8.7 HYPNOTHERAPY
The following services apply to General Practitioners and Psychiatrists.
Practitioners only.
Hypnotherapy is therapy undertaken with a patient who has been placed in an altered state of consciousness.
(a) Hypnotherapy is claimed in 15-minute intervals. The hypnotherapist must spend at least 80% of
(b) Physicians practising hypnotherapy should have appropriate training equivalent to that provided
(c)
(i) A minimum of two intervals must be claimed per session.
(ii) Unless unusual clinical circumstances can be demonstrated to the Medical Consultant at
Group Psychotherapy
Group Psychotherapy differs from individual psychotherapy in that it is provided to a group of 4 to 8
individuals per session.
(a) Group Psychotherapy is claimed in 15 minute intervals. The therapist must spend at least 80%
of the time claimed in therapeutic intervention with the group of patients.
Restrictions (Apply to General Practitioners only)
(b)
(i) A minimum of 2 intervals must be claimed per group session.
(ii) Unless unusual clinical circumstances can be demonstrated to the Medical Consultant at
MSI, Group Psychotherapy may not be claimed for the following:
• More than 2 continuous hours (or 8 continuous fifteen minute intervals) per group per day
• A group member younger than 4 years old
• More than one General Practitioner treating the same illness for a particular group of
patients
Family Therapy
Family Therapy is defined as psychotherapy in which the therapist regards the patients as a
subsystem of a “family” and in which the therapeutic responsibility is not only to the patients but to
other family members as well.
(a) The assessment rules are the same as for Group Psychotherapy, but 2 or more members of the
family must be present for the session to qualify as Family Therapy.
(b) Family Therapy is claimed in 15 minute intervals. The therapist must spend at least 80% of the
time claimed in therapeutic intervention with the family.
Restrictions (Apply to General Practitioners only)
(c)
(i) A minimum of 2 intervals must be claimed per family session.
(ii) Unless unusual clinical circumstances can be demonstrated to the Medical Consultant at
MSI, Family Therapy may not be claimed for the following:
• More than 2 continuous hours (or 8 continuous fifteen minute intervals) per family per day
• A patient younger than 4 years old
• More than one General Practitioner treating the same family group
Restrictions apply to General
the time claimed in direct therapeutic intervention with the patient.
by the Nova Scotia Society of Clinical Hypnosis workshops.
Restrictions (Apply to General Practitioners only):
MSI, hypnotherapy may not be claimed for the following:
• More than 10 hours per patient per physician per year
• More than 90 continuous minutes (or 6 continuous intervals) per patient per day
• A patient younger than 4 years old
• More than one General Practitioner treating the same illness for a particular patient
May 2011 PREAMBLE - 29
Page 34

8.8 COUNSELLING
The following services and restrictions apply to General Practitioners only.
(a) Counselling is a prolonged discussion directed at addressing problems associated with
adjustment reactions or bereavement reactions.
(b) Counselling may be claimed in 15-minute intervals. At least 80% of the time claimed must be
spent in direct patient intervention.
(c)
8.9 LIFESTYLE COUNSELLING
The following services and restrictions apply to General Practitioners only.
Lifestyle Counselling is a prolonged discussion where the physician attempts to direct the patient in the proper
management of health related concern; e.g., lipid or dietary counselling, AIDS advice, smoking cessation,
healthy heart advice, etc.
(a) Lifestyle Counselling may be claimed in 15-minute intervals. At least 80% of the time claimed
(b)
at the same service encounter
Restrictions
Unless unusual clinical circumstances can be demonstrated to the Medical Consultant at MSI,
counselling may not be claimed for the following:
• More than 5 hours per patient per physician per year
• More than 1 hour per patient per day
• A patient younger than 4 years old
• More than one General Practitioner providing counselling to a particular patient
must be spent in direct patient intervention.
Restrictions
Unless unusual clinical circumstances can be demonstrated to the Medical Consultant at MSI,
lifestyle counselling may not be claimed for the following:
• More than 2 hours per patient per physician per year
• More than 30 minutes per patient per day
• A patient younger than 4 years old
• More than one General Practitioner providing lifestyle counselling to a particular patient
9. ASSESSMENT RULES FOR PROCEDURES
9.1 Procedures are a type of patient service distinguished from visits by several features. They generally have a
specifically defined technique involving either a physical therapeutic intervention with the patient; the obtaining
of some diagnostic sample, image or biophysiological measurement; or the interpretation of a sample,
measurement, or image. A procedure may include elements of a visit, evaluation, or care depending on the
specific procedure and the clinical setting.
9.1.1 Procedures fall into three categories for assessment purposes: Diagnostic and Therapeutic
procedures, Surgical procedures, and Fractures. Subject to the rules in this section, procedures may
be claimed in association with visit services, or with other procedures.
9.1.2 Procedures may be claimed only when they are carried out by, or under the supervision of, a
physician.
9.2 DIAGNOSTIC AND THERAPEUTIC PROCEDURES
9.2.1 No premium fees may be claimed for Diagnostic and Therapeutic procedures other than selected
Diagnostic Imaging Services (See Section 7.4.1)
9.2.2 Diagnostic and Therapeutic procedures can be performed in any location, with the exception of the
following procedures which have location-specific restrictions and may be claimed only when
performed by a physician in the appropriate (sub) specialty:
acute
May 2011 PREAMBLE - 30
Page 35

(a) When performed outside of a hospital
(i) Electrocardiogram - Internist and Paediatrician.
(ii) Electromyogram - Neurologist (including Paediatric Neurologist), Physiatrist and
Neurosurgeon
(iii) Electroencephalogram - Neurologist (including Paediatric Neurologist) and Neurosurgeon.
(b) When performed in hospital
(i) Stress Test - Internist and Physiatrist in approved centres (See Billing Instructions Manual)
(ii) Procedures performed in a catheterization lab - Cardiologist (including Paediatric
Cardiologist) and Radiologist
(iii) Intensive care associated with Respiratory Insufficiency - Anaesthetist.
9.2.3 Submaximal Exercise Testing
(a) This service may only be claimed in approved centres as noted in Item 9.2.2 (b)(i) above.
(b) If the patient has been seen in consultation by the specialist performing the test within the
previous 14 days, no visit service or consultation may be claimed.
(c) If the patient has not been seen by the specialist within the previous 14 days, a Comprehensive
Initial Visit or consultation service may be claimed.
However, it should be noted that there must be a medical necessity for the comprehensive visit
and components of this visit (as outlined in section 7.2.2 of the Preamble) must be performed
and documented in the patient’s chart. Similarly, if a consultation is claimed with an exercise
test, the rules governing referred services (section 7.5 of the Preamble) must be followed.
(d) If the patient has been examined by another specialist within the previous 14 days for a problem
related to the condition for which the exercise test is being performed, a Comprehensive Initial
Visit service, but not a consultation, may be claimed.
9.2.4 Interpretation of Holter Monitoring may be claimed only when abnormalities are present. (Billed
through Facilities - not to MSI)
9.2.5 Where multiple diagnostic and therapeutic procedures are performed at the same service encounter,
the procedure with the greater value is claimed at 100% and subsequent procedures at 50%.
Procedures defined as “Add-Ons” in the schedule text may be claimed at 100%.
9.2.6 Service encounters by assistants are not normally applicable to Diagnostic and Therapeutic
procedures with the following exceptions. Assistant fees should be claimed at the current surgical
assistant rate (See Section 9.5.1).
(a) Excisional breast biopsy after localization of a mammographic abnormality.
(b) Mediastinoscopy: when assisting with a mediastinoscopy, regardless of whether a flexible or
rigid bronchoscopy is also performed, claim the assistant fee for mediastinoscopy alone.
(c) Fetal procedures under ultrasound guidance.
(d) Catheter ablation of cardiac arrhythmias.
(e) Percutaneous Endoscopic Gastrostomy.
(f) Percutaneous Endoscopic Gastro-jejunostomy.
9.2.7 Venipuncture for the purpose of blood collection is not an insured service when performed by a
physician with the following exceptions:
(a) The physician's office is greater than 24 km (15 miles) from the closest laboratory blood
collection service.
(b) When the physical condition of the patient makes it medically necessary for the physician to
personally take the sample.
9.2.8 Nasogastric (Levine) tube insertion is considered part of the appropriate visit service encounter.
May 2011 PREAMBLE - 31
Page 36

9.2.9 Diagnostic and therapeutic procedures are divided into two groups, procedures that cannot be
claimed with a visit code, and those where a visit service may be claimed if one is provided.
(a) Procedures designated as “visit excluded” cannot have a service encounter for any visit service
from the same service encounter.
(i) When a visit excluded procedure is the sole reason for the service encounter, the procedure
alone should be claimed.
(ii) If a visit service and a visit excluded procedure are provided at the same service encounter,
only the service of greater value should be claimed.
(b) Procedures designated as “visit allowed” may have a service encounter for any visit-related
service from the same service encounter with the exception that the following procedures may
not be claimed in association with a consult:
(i) Cerumen - removal of - unilateral or bilateral
(ii) Tonometry
(iii) Gonioscopy
(iv) Visual fields (tangent, screen and/or perimetry)
(v) Flexible fibre - optic endoscopy of the nose, nasopharynx, and larynx
(vi) Pap smear
(vii) Venipuncture of a person 7 years or older
(viii) Medical certificate for observation for psychiatric evaluation 1st doctor
(ix) Medical certificate for observation for psychiatric evaluation 2nd doctor
9.2.10
9.2.11
Provincial Immunizations
Physicians may claim for the administration of immunizations covered by the Provincial Immunization
Program. These services may be claimed by any registered physician.
If one vaccine is administered but there is no associated office visit billable, i.e. the sole purpose of
the visit is the immunization, one injection can be claimed at a full fee.
If one or more vaccines are administered in conjunction with an office visit, the office visit and the first
injection can be claimed at full fee. All subsequent injections will be paid at 50% of the specified
MSU.
If two vaccines are administered at the same visit but there is no associated office visit, a claim for
each specific immunization can be submitted at full fee. All subsequent injections will be paid at 50%
of the specified MSU.
For children eighteen months of age and under, if a vaccine is administered in conjunction with a well
baby care visit, the well baby care visit and the immunization may be claimed.
Tray Fees
Provincial Immunization Tray Fee - When a physician has incurred the cost of supplies when
(a)
administering an immunization covered by the Provincial Program, a tray fee can be claimed for
each injection. There is to be no charge to the patient/family for the supplies and/or disposables
associated with any of these immunizations. Maximum of four tray fees can be claimed per
service encounter.
Pap Smear Tray Fee - When a physician has incurred the cost of supplies when performing a
(b)
pap smear, a tray fee can be claimed. There will be no charge to the patient for any supplies,
equipment or disposables associated with the performance of a pap smear.
The following billing guidelines should be used:
(i) A pap smear tray fee can be claimed when a pap smear is performed alone or as part of a
comprehensive examination, an office visit, or a gynecological procedure.
(ii) An office visit may be claimed in conjunction with a pap smear only if the visi t is for a
nongynecological complaint.
(iii) A visit for a pap smear and an unrelated medical condition can include a claim for the office
visit, pap smear, and pap smear tray fee.
May 2011 PREAMBLE - 32
Page 37

9.2.12
(a) When referring to electromyography with muscles of more than one region, or
(b) When referring to nerve condition studies, per nerve studied: “per nerve studied” is
branch are required.
9.3 SURGICAL SERVICES
9.3.1 Surgical procedures are described as Major if they have a value in excess of 50 units:
9.3.2 Surgical procedures are described as Minor if they are less than or equal to 50 units:
(a) When a visit service is provided during the same service encounter as a minor surgical
(b) A consultation prior to surgery may be claimed, even if the surgery is on the same day, except
Electromyography
examination of a specific region, “region” is intended to mean one or more of the four following
anatomical areas: head and neck, both upper limbs, both lower limbs; trunk (anterior and
posterior).
intended to mean both the motor and sensory never conduction examination of a single nerve
(mixed, motor or sensory). Multiples may be claimed when another nerve (mixed, motor
or sensory) is examined and when separate nerve conduction studies of a major nerve
(a) The procedure fee is intended to cover the operation and customary pre-operative, operative
and post-operative care by the surgeon or a designated covering physician.
(i) A consultation at any time prior to surgery may be claimed, even if the surgery is on the
same day. A visit other than a consultation is not payable the same day as a major surgical
procedure.
(ii) Preoperative care includes:
• Comprehensives visit (the admission history and physical exam).
• Hospital visits for up to two calendar days immediately prior to and including the day of
surgery.
• Hospital visits in a preoperative period that extends beyond two days should be claimed
using the appropriate visit codes.
(iii) Postoperative care includes care during the postoperative hospital stay up to 14 days.
(iv) Urgent Visits or Emergency Hospital Visits (See Item 7.2.7) to attend the patient for an
unrelated condition are not included in the surgical benefit and may be claimed accordingly.
(v) Hospital Visits may be claimed starting on the 15th postoperative day for visits if the
postoperative in hospital stay exceeds 14 consecutive calendar days. For the purpose of
calculation, the day of the last operative procedure is considered day 0. Weekly routine visit
maximums beyond 56 days apply starting from the date of admission.
(vi) When a patient is readmitted to hospital during the first 14 days of the post surgical period
because of post-operative complications which do not require a surgical procedure, the
surgeon or other physician attending this readmitted patient should claim hospital visits as
for a new admission.
Note: There will be no reduction in the surgical payment when a service related to the
surgery is claimed by another physician in the post-op period.
procedure for a reason other than the condition for the minor surgery, the greater of either the
visit or the minor surgery may be claimed, otherwise only the minor surgery service encounter
applies. However, in the case of a service encounter for suture of a laceration with a value less
than or equal to 50 units, the appropriate visit may also be claimed.
where the consultation is explicitly included as part of the procedure.
May 2011 PREAMBLE - 33
Page 38

(c) Post-operative care following minor surgery may be claimed, except for those minor surgical
procedures which specify “complete care” and include all post-operative visits by the same
physician in the 14 days following the procedure.
(d) The services of an assistant at minor surgery are not usually required.
9.3.3 Special restrictions or interpretations applicable to Major or Minor Surgery:
(a) Procedural codes and their associated tariff are intended to remunerate the physician for all
parts of the procedure that would normally be considered the defined technique for that
procedure. It is not appropriate to de-construct (unbundle) the procedure into constituent parts
and bill MSI for these codes in addition to the procedural codes.
(b) Local anaesthesia is not payable in addition to the surgical fee.
(c) Endoscopic procedures performed on a patient on the same day as major urological surgery by
the same physician may be claimed at 50% in addition to the major surgical fee except where
the surgery is done in a separate operating room. Other diagnostic and therapeutic procedures
may be claimed at 100% with other major urology surgery.
(d) When one physician performs a definitive procedure on an organ or within a body cavity, only
that service should be claimed. The procedure used to provide surgical exposure should not be
claimed; e.g., a laparotomy is not to be claimed to provide access to the abdominal cavity
except when no definitive procedure is performed within the abdomen. When one physician
provides surgical exposure for a procedure performed by a physician in another specialty, the
exposure and definitive procedures may be claimed separately by the respective physicians.
(e) Fees for the application of casts, splints and dressings at the time of surgery may not be
claimed.
(f) Fees for the application or removal, by the operating surgeon, of casts, splints and dressings
during the 30 days following surgery may not be claimed.
(g) Vascular Procedure Service encounters
(i) Repair/bypass/graft includes thromboendarterectomy and/or anastomosis and/or
thrombectomy of the peripheral artery being repaired, and harvesting of vein unless
otherwise specified in the procedure description.
(ii) Common femo ral arter y repair includes repair to the profunda artery before the second
major branch of the profunda artery.
(iii) If the profunda artery repair extends beyond the second major branch of the profunda
artery, an extended profundoplasty fee may be claimed in addition as the second
procedure.
(iv) When resection of an abdominal aneurysm is combined with an aortic graft plus femoral
artery repair (unilateral or bilateral) only one procedure, which ever has the higher unit
value, should be claimed.
(h) Arthroscopy
(i) Composite arthroscopy fees include the procedure and arthroscopy.
(ii) When other or multiple surgical procedures are performed through the arthroscope, only the
major fee applies.
(i) Injections of medication into a bursa, ganglion, joint, or tendon may not be claimed with surgery
performed in the same location. This applies whether the medication is delivered via
arthroscope or directly into the location.
(j) Compression Sclerotherapy (Feganization)
Codes for compression sclerotherapy for varicose veins are designed to cover all services for
that diagnosis, for the same leg, for a period of one year.
(k) Bilateral Procedures
(i) Unless otherwise specified, bilateral procedures are claimed at an additional 50% of the
unilateral procedure.
May 2011 PREAMBLE - 34
Page 39

9.3.4 Cancelled Surgery
9.4 FRACTURES
9.4.1
9.4.2
9.4.3
(ii) When bilateral procedures are performed subsequent to a major procedure through the
same incision they should be claimed at 50% and 25%.
(iii) When bilateral procedures are performed subsequent to a major procedure through a
separate incision, they should be claimed at 65% and 32.5%.
(iv) When performed under separate anaesthetics at an interval, the full fee will be charged for
each procedure.
(l) Multiple Procedures - Same Physician
(i) When multiple operative procedures are performed through a single incision in the course of
an abdominal operation or on any one organ or cavity, the principal procedure will be
claimed plus 50% for the secondary procedures (secondary incidental procedures, such as
appendectomy, which are not indicated by pathology, shall not be claimed).
(ii) A physician who performs multiple operative procedures simultaneously in different areas
and through different incisions shall claim for the major procedure plus an additional 65% for
each of the lesser procedures. Laparoscopic operations are considered to utilize a single
incision regardless of the number of incisions.
(m) The full procedural fee will apply when subsequent, related operative procedures are performed
during the postoperative period.
(n) Combinations of Multiple and Bilateral procedures should be claimed based on the rules
applicable to the highest valued procedure.
(o) Unrelated Surgical Procedures - Different Physicians
When two or more unrelated procedures are performed through separate incisions or in
unrelated areas, but utilizing the same anaesthetic, by two different physicians in different fields
of practice and with different skills, the fee provided in the Schedule under each procedure will
be paid at 100% to each physician.
(p) An arthrodesis procedure includes bone grafting.
(q) Debridement
All claims for debridement, HSC 98.11, must indicate in electronic text the area debrided, the
start and finish time, and whether performed under a local or general anaesthetic. Only the time
from the start to the finish of the debridement may be claimed.
In the event of cancellation of surgical procedure, regular visit rules apply for surgeons.
Surgical Rules (See Item 9.3) apply to treatment of fractures except:
(a) A fracture procedure (not dislocation) includes necessary after care up to 42 days. The
application and removal of casts or traction devices is included in the fee, even if removal takes
place after the 42 day period.
(b) Regardless of the type of anaesthesia employed, all fracture service encounters are eligible for
premium fees during the designated times.
Major Fractures
Major fractures are defined as those requiring procedures in excess of 50 units. Rules for major
surgery apply and an appropriate consult may be claimed pre-operatively. A comprehensive
consultation is appropriate only for those patients who are referred with significant systemic illness or
requiring general anaesthesia. A limited consultation is appropriate only for those patients who are
referred and where the diagnosis is unclear or management alternatives require prolonged
discussion or assessment.
Minor Fractures
Minor Fractures are defined as those procedures less than or equal to 50 units. Minor surgical rules
apply to minor fractures including preoperative consultation. (See consult guidelines in 7.5) Rules
regarding non-bilateral multiple fractures may be claimed at fee + 65%. However, the 42-day
aftercare rule does apply.
May 2011 PREAMBLE - 35
Page 40

9.4.4
9.4.5
9.4.6
9.4.7
9.4.8
9.4.9
9.4.10
9.4.11
9.4.12
9.4.13
9.4.14
Fracture and Non Fracture Procedures Performed at the Same Service Encounter
(a) When fracture procedures and non fracture procedures are performed at different sites, claim
100% for the greater and 65% for the lesser procedure.
(b) When performed at the same site, claim 100% for the greater procedure and 50% for the
lesser procedure.
Treatment of Fracture with No Reduction
When a fracture is treated by any method other than an open or closed reduction, visit fees apply.
This shall include the application, changing and removal of casts and/or splints.
Closed Reduction
Closed reduction is the reduction of a fracture by manipulation or traction.
Multiple Closed Reductions
Where multiple closed reductions are carried out for the same fracture, at different service
encounters, the following rules apply:
(a) When performed by the same physician, claim 50% for each reduction.
(b) When performed by different physicians the first physician’s payment will be reduced to 50% of
the listed fee and the second physician's payment will be valued at 100%.
Open Reduction
Open reduction is the reduction of a fracture by an operative procedure and includes exposure of the
fracture site with fixation as indicated. If an open reduction with extensive debridement is necessary,
the appropriate open reduction should be claimed plus a service encounter for independent
consideration or exceptional clinical circumstances covering the debridement portion of the service.
The supporting text should indicate the total duration of service.
Multiple Open Reductions
Multiple open reductions performed at different service encounters may each be claimed at 100%.
Closed followed by Open Reduction
Where a closed reduction is followed by an open reduction, whether performed by the same or
different physician, the service encounter will be reduced to 50% for the closed reduction and the
service encounter for the open reduction will be valued at 100%.
Compound Fractures or Dislocations
The following should be applied when claiming for treatment of a compound fracture or dislocation:
(a) The service encounter for
service encounter for the appropriate (non-compound) fracture or dislocation.
(b) If an
Multiple Fractures
Where multiple major fractures are treated by the same surgeon the greater procedure is claimed at
100% and 50% is claimed for each additional fracture.
Re-Fracture
Where a re-fracture procedure has been performed, a service encounter for exceptional clinical
circumstances may be made.
Bone Grafting for Fractures
(a) For a primary bone graft in a fresh fracture, claim 50% of the appropriate bone graft code in
(b) Treatment of a non-union fracture with bone grafting is claimed under the appropriate bone graft
(c) Reaming is not considered a “bone graft” for assessment purposes and should not be claimed.
open reduction is performed, only a service encounter for the open reduction will apply.
addition to the primary fracture procedure.
procedure code except when there is a new displacement where both the open reduction and
the bone graft are claimed.
closed treatment of a compound fracture or dislocation is 150 % of the
May 2011 PREAMBLE - 36
Page 41

9.5 SURGICAL ASSISTANTS
A surgical assistant is defined as a physician who assists the operating surgeon throughout a substantial
portion of the operation.
9.5.1
9.6 RADIATION ONCOLOGY
Treatment planning may not be claimed with a consultation on the same day by the same physician.
However, it may be claimed as an additional fee following gold seed and caesium needle implants. Gold seed
and caesium needle implants should be classified as major surgical procedures.
9.7 PATHOLOGY AND DIAGNOSTIC IMAGING SERVICES
Most service encounters for services in the schedule of benefits for these specialties are processed by a
special arrangement with MSI. These service encounters are limited to hospital based physicians in the
appropriate specialties. Procedures not covered by these special arrangements should be claimed on a fee
for service basis as listed in the Schedule of Benefits.
Diagnostic Imaging service encounters should conform to the requirements set out in the Preamble.
Surgical Assistant's Service Encounter
An assistant should render a separate service encounter for services provided. A surgical assistant's
service encounter is 33.8% of the surgical fee regardless of whether the assistant is certified as a
specialist. The service encounter should be calculated to the nearest unit with a minimum of 21
units. However, when a general practitioner that has participated in the prenatal care assists at a
vaginal delivery or a Caesarean Section, he/she will be paid a full general practitioner delivery fee.
The delivery fee would apply to another general practitioner covering the practice.
(a) Surgical assists are not payable for minor procedures or diagnostic and therapeutic services,
except as defined in 9.2.6. When ADON (add on) procedures are done during a major surgical
procedure for which a surgical assistant is payable, the assistant’s service encounter is 33.8% of
the total surgical fee. In unusual circumstances where an assistant fee is not normally paid, the
assistant should submit a service encounter with an accompanying letter from the surgeon
explaining the necessity. In cases of fracture procedures, no visits may be claimed pertaining to
the post fracture care up to 42 days following the fracture procedure. (See Item 9.4)
(b) A surgical assist is not payable for some major surgical procedures. A list of codes is provided in
the Billing Instructions Manual.
(c) Service encounters for routine hospital visits, in the 14 days post-op, are not allowed in addition
to an assist fee. However, service encounters for the following services are allowed:
(i) A home, office or OPD visit on the same day if medical necessity is established
(ii) Comprehensive visit same day as trauma or emergency surgery
(iii) Procedures with visits allowed.
(iv) Supportive Care
(v) Visits in postoperative period for diagnosis unrelated to the surgery
(vi) If transfer of care from the surgeon to the assistant occurs because the surgeon is
unavailable (e.g., out of town) the assistant may claim daily visits for in-hospital post-op
care.
(d) Second Assistant
When a second assistant is necessary, his or her claim is 50% of the stated service encounter
for the first assistant with a minimum of 10.5 units. The need for a second assistant is to be
supported by a letter from the surgeon explaining the necessity.
(e) Cancelled Surgery
(i) When an anaesthetic has begun and the operation is cancelled prior to commencement of
surgery, if the assistant has scrubbed but is not required to do more, only a Hospital Visit
may be claimed.
(ii) If the operation is cancelled after surgery has commenced, the procedural units for the
intended principal procedure will apply.
May 2011 PREAMBLE - 37
Page 42

9.8 FACILITY NON-PATIENT SPECIFIC BULK BILLING
An agreement between Doctors Nova Scotia and the Department of Health regarding the introduction of a Fee
Schedule for Radiology/Non-Patient specific fees became effective June 1, 1995.
Bulk billing refers to non-patient specific services billed through MSI on approved programs (e.g., radiology,
pathology, internal medicine). The following section provides information on the programs that are approved
and paid through MSI. The appropriate forms outlining the MSI billing codes are available upon request from
the Alternate Funding Department, MSI.
9.8.1
A. Radiographs
Radiology
Interpretation Fee
This represents the benefit for consultation between the radiologist and the referring service provider,
fluoroscopy, interpretation of diagnostic images, fluoroscopic findings and supervision of diagnostic
imaging services by a radiologist. If a formal written report is not generated on a separate document,
the interpretation fee is incomplete and may not be billed. In addition, an immediate oral report may
be given if indicated and/or requested.
Fee Schedule Interpretation
Self referral is not ethical and a consultation with the referring service provider should be held before
performing any further examination. However, where the referring service provider is not immediately
available, in exceptional cases further examination may be provided if considered necessary by the
radiologist.
Although there is no provision for “additional views”, the Fee Schedule recognizes that added views
are sometimes necessary; therefore, this has been taken into consideration for fees where additional
views may be performed.
When a requisition for one extremity is received, no additional charge shall be made for
comparison x-rays of the opposite site.
IVP includes an abdominal survey film. No separate claim shall be made for the abdomen. If
tomography is routinely performed there shall be no extra fee.
The fluoroscopy claim shall not be submitted for an examination performed by the radiologist
where fluoroscopy is an integral part of the examination; e.g., examination of GI Tract, Urinary
Tract, Special Procedures.
The Fluoroscopy Only charge is for use when no other procedure is claimed.
Abdomen and chest studies shall not be claimed in gastrointestinal (G.I.) and genitourinary
(G.U.) examinations.
Sacrum/coccyx, abdomen, S.I. joints and pelvis shall not be claimed in lumbar spine
examinations. Thoracic spine shall not be claimed in chest examinations.
Chest studies shall not be claimed in mammography cases.
Nasal bones or sinuses shall not be claimed in skull examinations.
An Upper G.I. series includes a study of the swallowing mechanism and esophagus. An
esophagus can only be billed if additional special views including video, food bolus, etc., are
made.
Submitted films are films deemed to be those from another institution whose reinterpretation has
been requested by a service provider.
May 2011 PREAMBLE - 38
Page 43

The necessity of having plain film studies available prior to special procedures (e.g.,
myelography) is obvious. It is not essential that they be done at the same institution. If they
have been done at an outside institution, then it is the responsibility of the referring service
provider and the radiologist to have these films available. If, however, they cannot be made
available to the radiologist, it is acceptable practice to repeat the appropriate examination and
claim for it.
Reasonable effort should be made to review original examinations f rom another centre. No
current outside examination of acceptable quality should be repeated.
When using the paediatric codes, Upper G.I., Colon and Cystography, it is recognized the added
time these examinations take; however, the age limit for these fee codes is twelve (12) years not
sixteen (16) years as in the workload measurement system.
When a CT examination is performed with and without contrast, the combined code shall be
used.
B. Ultrasound
An abdominal general ultrasound includes a study of all appropriate areas and organs. No
restricted or special fees may be added to this examination. Specific fees shall be used as
appropriate; e.g., Pylorus, Appendix, Aorta, Kidneys and Bladder; these fees are not
cumulative.
An ultrasound examination of the pelvis in the first trimester of pregnancy is to be billed as a
Pelvic Ultrasound.
Biophysical profile, shall only be charged when films are made and a written report
generated by a radiologist.
The fee for a radiologist performing a portable examination is an add-on fee to be charged
for studies performed outside the department which require the radiologist to be in
attendance for the entire examination.
When both pelvic and endovaginal examinations are performed, they shall be as
endovaginal with pelvic.
The intraoperative code is to be used when the radiologist is present in the operating room
and no other code may be claimed for that examination.
C. Vascular Studies
Unilateral and Bilateral Venogram studies of the extremities should include a central film. No
additional claim may be made for that film.
Only one claim should be made for angiography, irrespective of the number of modalities
used; e.g., cut film, DSA, cine.
No claim may be made for an arch or abdominal aortic angiogram unless a proper flush
study has been performed. An angiographic interpretation fee may only be charged when
the vessel has been specifically selected and films taken.
The DSA interpretation fees apply to venous injections only.
D. Drainage or biopsy procedures
Drainage or biopsy procedures charged through MSI billing include imaging and no separate
claim may be made for the imaging or interpretation. Abscess cavity films are part of the
drainage fee.
E. Nuclear Medicine
A Thyroid Uptake Special includes stimulation and/or suppression studies.
May 2011 PREAMBLE - 39
Page 44

9.8.2
9.8.3
(a) Surgicals, gross and microscopic
Bill both Plasma Volume and Red Cell Volume only if they are measured separately.
A.C.E. Inhibitor Renogram should be billed when the A.C.E. Inhibitor is administered by and
directly supervised by the service provider. If not, a Renal Scan and Renogram should be
billed.
Renal static imaging is to be billed instead of a renal scan and renogram when only static
(e.g., - DMSA) images are obtained.
Residual Urine Volume is an add-on fee.
Tomography will be an add-on fee, every time it is used.
Hepatobiliary with a pharmacologi cal stimulation includes either morphine stimulation or
C.C.K. Stimulation.
“One area” for Bone, Bone Marrow and Gallium Scans i ndicates one body area; e.g., skull,
foot, pelvis.
Flow Studies, when appropriate, will be an add-on fee.
Computer manipulation is included in the interpretation fee and is no longer recognized as a
separate item.
Myocardial rest quantitative, myocardial stress and rest quantitative, are add-on fees.
one
Tumour imaging includes
imaging studies e.g., - labeled antibody studies for the specific detection of tumours. It does
not include other studies with specific codes. It is not an add-on fee.
Internal Medicine
Electrocardiogram, electroencephalogram and holter monitoring are for interpretation only when
performed in hospital.
Pulmonary functions: simple spirometry, flow/volume loops, helium dilution, carbon monoxide
single breath, pulmonary stress test, bedside spirometry, body plethysmography are insured
when performed in hospital.
Echocardiography: M-mode, two di mensional, doppler-quantitative, doppler-qualitative are
insured when performed in hospital.
Pathologists
Effective October 1, 1993, the responsibility for payments to Pathologists for fee-for-service
payments (Pathology Units) was transferred to Medical Services Insurance (MSI). Salary payments,
management fees and sessional payments will continue to be paid by hospitals. All billings are
forwarded to MSI directly by the service providers performing the services.
Pathologists may claim Pathology Units from MSI by submitting the list of services on the claim
forms. Service providers may assign payments to group practices. Each pathologist must submit a
separate form for his/her services.
Third party request for services should continue to be billed directly to the third party (e.g., medical
examiners autopsies or requests from WCB, etc.)
When more than one surgical specimen is received from a patient, the following rules apply:
P2325 - may be claimed for each specimen taken from anatomically distinct surgical sites.
whole body imaging for thyroid cancer or specialized tumour
May 2011 PREAMBLE - 40
Page 45

P2345 - may be claimed when 3 or more separate surgical s pecimens are taken from the
same anatomic site.
P2346 - may be claimed when a single large complex cancer specimen, which includes
lymph nodes, is examined for the purposes of providing a pathologic cancer staging.
Definitions:
Anatomically distinct site: For the purposes of correctly interpreting anatomic pathology fee code
P2325, the body is considered to be divided into the following distinct anatomical areas: head
and neck; upper limbs; trunk (anterior and posterior). The following organ systems are also
considered to be distinct surgical sites: upper GI tract; female reproductive system; male
reproductive system; separate organs within the abdominal or thoracic cavities may be claimed
as distinct sites. For example, 2 separate skin specimens from the right and left arms are
considered as one site; specimens from uterus and ovary are one site; specimens from colon
and liver are two sites.
Clarifications:
Frozen Sections (intraoperative consult with tissue): For the purposes of correctly interpreting
anatomic pathology fee code P2326, all frozen sections taken from one surgical specimen are
considered to be one frozen section. When separate organs or anatomic areas are sent for
frozen section, then it is appropriate to bill for 2 frozen sections; separate sentinel nodes may
also be considered as separate specimens. For example, examination of several margins from
one skin cancer is one frozen section; examination of multiple margins from two separate skin
cancers (even though they may be within the same anatomically distinct surgical site as defined
above) can be considered as two frozen sections.
9.9 OPHTHALMOLOGICAL SERVICES
9.9.1
(a) An eye examination is payable under MSI when it is medically required. The service encounter
(b) Coverage for
(c) Visual Fields, Tonometry and Gonioscopy are included in the fee for a complete eye exam and
9.9.2
Complete Eye Examination
should show an indication of presenting symptoms or diagnoses.
under 10 years of age and for those 65 years of age and over. For all others, routine refractive
vision analysis is an uninsured service.
ophthalmological consultation.
Contact Lens Fitting
Fitting of medically indicated contact lenses by a physician is an insured service under Nova Scotia
Medical Services Insurance. In view of continuing developments and improvements in contact lens
materials and therapy, it is recognized that they may prove to be of benefit in conditions not as yet
listed.
(a) There are two types of lenses recognized:
(i) Bandage contact lens/lenses should be claimed for Zero prescription lens/lenses applied to
immobilize the eye to enable recovery for certain conditions. Follow-up visits may be
claimed in addition.
(ii) Corrective lenses may be fitted to restore monocular or binocular vision where this cannot
be achieved by other methods and to improve visual fields where this is compromised by
high refractive error.
(b) Conditions for which contact lens fitting is an insured service on the basis of medical necessity:
Albinism, aniridia, anterior membrane corneal dystrophies, aphakia, astigmatism requiring over
5 dioptres of cylindrical correction, bullous keratopathy, chronic corneal edema, corneal
abrasion, corneal burn, corneal lacerations, corneal ulcer, descemetocele, dry eye syndromes,
entropion, high refractive errors (6 dioptres spherical equivalent or over in children under age
16, 10 dioptres spherical equivalent or over in adults), keratoconus, neuroparalytic keratopathy,
nystagmus, old trachoma, paralysis of superior rectus muscle, pemphigus, post penetrating
keratoplasty, postoperative discomfort or lacerations or perforations, prevention of
routine refractive vision analysis is limited to once every 24 months for persons
May 2011 PREAMBLE - 41
Page 46

symblepharon, recurrent cornea erosion, Stevens-Johnson disease, stromal herpes simplex,
thermal burns, trichiasis, vernal conjunctivitis, anisometropia, corneal degeneration, epithelial
defect, pathological myopia, Marfan's Syndrome and pseudophakia.
(c) Conditions for which contact lens fitting may not be claimed:
Macular degeneration, open angle glaucoma, diabetic retinopathy, strabismus, borderline
glaucoma and amblyopia.
(d) Contact lens fitting includes follow up for 90 days by the same physician.
9.9.3 A complete ophthalmological exam including refraction may be claimed before and after cataract
surgery.
9.9.4 When as the result of an error or omission by the patient, an insured service is provided within the
two-year limit, the provider will be notified by MSI that an uninsured service has been rendered. The
provider may then bill the patient the usual and customary fee. If the provider is unable to collect, a
reduced fee will be paid by MSI. This service applies only to patients in the insured age group.
9.10 PRONOUNCEMENT OF DEATH
For attendance on the patient for the purpose of pronouncement of death, a Limited Visit may be claimed.
9.11 DENTAL SERVICES
9.11.1 Referrals from dentists to physician specialists are acceptable provided that the dentist discuss the
patient with the family physician before seeking such consultation and that the physician specialist
send a copy of his or her report to the family physician as well as to the referring dentist.
9.11.2 Other Physicians' services provided at the request of a dentist are regarded as non-referred services;
consultation or referred visit service codes shall not be used when submitting service encounters.
10. PROCEDURES FOR AMENDMENTS TO THE PRE AMBLE AND FEE S CHE DULE
10.1 When it is necessary, in the course of normal program administration, to make interim interpretations of the
Preamble or Schedule of Benefits, MSI will utilize the following process.
10.1.1 Interim interpretations and interim fees will be published in a Physician’s Bulletin.
10.1.2 If permanent fees are negotiated between the Department of Health and Doctors Nova Scotia, the
appropriate section(s) of the fee schedule will be updated.
10.2 Fee Codes will be reviewed every two years. If there is no utilization of a fee code for two years, MSI will
consult with Doctors NS who will inform the appropriate sections. If there is no valid reason for maintaining
the code, MSI will remove the code and communicate this change in a Physician’s Bulletin.
May 2011 PREAMBLE - 42
Page 47

EXPLANATORY CODES - 1
May 2011
E
C
AD002
Service encounter has been refused as a duplicate billing exists.
AD003
Service encounter has been refused as electronic text is required.
AD004
Service encounter has been refused as this service has previously been approved.
AD005
Service encounter has been refused. A previous service encounter for 13.59L, RO=INPN has been
approved at this same encounter.
AD006
Service encounter has been refused as a previous service encounter has been approved and
includes this service.
RO=INTD.
new service encounter using the appropriate combination modifier value.
encounter for the combination of this immunization and the one from the deleted service encounter.
AD011
Service encounter has been refused. Previous payment has been made this day for a portion of this
combination injection.
AD012
Service encounter has been refused. Previous payment has been made this date for a portion of
this combination injection.
AD013
Service encounter has been refused as electronic text is required for this service to be approved at
location indicated.
AD014
Service encounter has been disallowed as surgery has been performed during this hospitalization.
AD015
Service encounter has been disallowed as a previous service encounter has been approved for the
discharge fee at this hospitalization.
AD016
Service encounter has been disallowed as surgery has been performed by you during this
hospitalization.
AD017
Service encounter has been disallowed as patient history indicates conflicting hospital admit dates.
verified the date.
code.
approved to you.
service.
AD021
Service encounter has been refused. Previous approval has occurred to you under MMRV.
AD022
Service encounter has been refused. Previous approval has occurred to you under PENV.
AD023
Service encounter has been refused. Previous approval has occurred to you under MMQU.
EXPLANATORY CODES
XPLANATORY
ODE
AD001 Service encounter has been refused. When a procedure and the daily rate for intensive care are
both claimed, only one, the procedure or intensive care is approved.
AD007 Service encounter has been refused as previous payment has been approved under 13.59L,
AD008 Service encounter has been refused. Delete original immunization approved this day and submit a
AD009 Service encounter has been refused. Delete one of the original submissions and submit a service
DESCRIPTION
AD010 Service encounter has been refused as previous payment has been made this day for a portion of
this combination.
Check your records to confirm admit date and submit a reassess (action code R) once you have
AD018 Service encounter has been refused as you have been approved this service under a combination
AD019 Service encounter has been refused. A portion of this combination service has previously been
AD020 Service encounter has been refused. Previous payment has been made to you for a portion of this
Page 48

EXPLANATORY CODES - 2
May 2011
E
CODE
AD024
Service encounter has been refused. Previous approval has occurred under MMR2 and/or QUAD.
AD025
Service encounter has been refused as previous approval has occurred to you under MMQU.
AD026
Service encounter has been refused as you have previously been approved an injection covered in
this service.
AD027
Service encounter has been refused as a portion of this service has been previously approved.
AD028
Service encounter has been reduced to 50%. Only one 13.59L at full fee is payable when a visit is
claimed
AD029
Service encounter has been reduced to 50% as two previous immunizations were paid at full fee on
this date.
AD030
Service encounter has been refused. Two immunizations have been paid at full fee this date. Delete
one immunization and resubmit at LV50 along with your visit/consult claim.
AD031
Service encounter has been refused as the patient's birthdate is inappropriate for this service
AD032
Service encounter has been refused as the maximum number of PENT injections has been reached.
AD033
Service encounter has been refused as patient must be one year of age.
AD034
Service encounter has been reduced to 50% as a visit and previous injection have been billed.
AD035
Service encounter has been refused as the maximum number of PNEC injections have been
approved.
AD036
Service encounter has been refused as the patient has not reached the appropriate age for this type
of injection.
AD037
Service encounter has been refused as the diagnostic code indicated and age of patient does not
warrant payment of the influenza vaccine.
AD038
Service encounter has been refused as a maximum of two 13.59L RO=PNEU immunizations have
been previously paid.
AJ001
Service encounter has been adjusted according to information provided by you.
AJ002
Service encounter has been adjusted according to information provided on another service
encounter.
AN001
Service encounter has been refused. When multiple procedures are performed during the same
time, only one anaesthetic fee applies.
AN002
Service encounter has been refused. When a procedure and the daily rate for intensive care are
both claimed, only one, the procedure or intensive care is approved.
primary fracture procedure.
only one is approved at 100%.
both claimed, only one, the procedure or intensive care is approved.
this same service encounter.
time only one is approved at 100%.
both claimed, only one, the procedure or intensive care is approved.
100% at this same encounter.
XPLANATORY
DESCRIPTION
BG001 Service encounter has been approved at 50% of the appropriate bone graft code in addition to the
BG002 Service encounter has been reduced. When multiple procedures are performed at the same time,
BG003 Service encounter has been refused. When a procedure and the daily rate for intensive care are
BG004 Service encounter has been approved at 50% as another procedure has been approved at 100% for
BG005 Service encounter has been approved at 50%. When multiple procedures are performed at the same
CC001 Service encounter has been refused. When a procedure and the daily rate for intensive care are
CC002 Service encounter has been approved at 50% as another procedure has previously been approved at
Page 49

EXPLANATORY CODES - 3
May 2011
E
CODE
CN001
Service encounter has been refused. When billing a stress test and a consultation and the patient
has been examined by a different cardiologist in the previous 14 days, a visit fee only applies.
CN002
Service encounter has been refused as a repeat consultation is not payable unless a consultation for
a related diagnosis with the same referring physician has been approved in the previous 30 days.
CN003
Service encounter has been refused as a complete care code includes related visits for the following
14 days.
CN004
Service encounter has been refused as you have previously been paid a visit or consultation this day
under the same service occurrence number.
CN005
Service encounter for a consultation with detention has been refused as you have previously been
approved a visit allowed procedure at the same service encounter.
CN006
Service encounter has been refused as a consultation and psychotherapy or counselling are not
payable at the same service encounter.
CN007
Service encounter has been disallowed as this service is included in the postoperative care.
CN008
Service encounter has been disallowed as this service is included in the postoperative care of
fractures.
CN009
Service encounter has been disallowed as contact lens fitting includes follow up for three months.
claimed, but will be approved at 0 units during the 90 days following major surgery.
care.
year.
CN013
Service encounter has been refused as detention is not payable in the office.
CN014
Service encounter has been disallowed as it is included as postoperative care of a fracture.
CN015
Service encounter has been disallowed. Contact lens fitting includes follow up for three months.
CN016
Service encounter has been disallowed as a consultation is considered included in the procedural
removal of retained placenta.
CN017
Service encounter has been disallowed as this service is payable once per patient per physician.
PACS consultation is disallowed.
obstetrical trauma repair.
CN020
Service encounter has been refused as a 03.09B has previously been approved for this day.
you or another physician on this day.
another physician this day.
CR003
Service encounter has been refused as modifier type {in} value, date of service and admit to intensive
care date do not agree.
CR004
Service encounter has been disallowed. When a procedure and the daily rate for intensive care are
both claimed, only one, the procedure or intensive care is approved.
CR005
Service encounter has been refused as date of service indicated is prior to intensive care admit date
given.
XPLANATORY
CN010 Service encounter has been disallowed. The first postoperative clinic or office recheck should be
DESCRIPTION
CN011 Service encounter has been disallowed as a consultation is not approved the same day as critical
CN012 Service encounter has been disallowed as compression sclerotherapy includes after care for one
code for induction of labor by artificial rupture of membranes as well as the procedural code for
CN018 When a comprehensive or limited consultation is billed within 30 days of a PACS consultation the
CN019 Service encounter has been disallowed as a consultation is considered included in the fee for an
CR001 Service encounter has been disallowed as a comprehensive critical care visit has been approved to
CR002 Service encounter has been refused as another intensive care visit has been approved to you or
Page 50

EXPLANATORY CODES - 4
May 2011
E
CODE
CR006
Service encounter has been refused as you have previously been approved a consultation or visit
this day.
CR007
Service encounter has been disallowed. Critical care and ventilatory support are included in
comprehensive care.
CR008
Service encounter has been refused as your specialty is not valid for providing intensive care
associated with respiratory insufficiency.
CR009
Service encounter has been refused as modifier type {in} value, admit to intensive care date and date
of service do not agree.
CR010
Service encounter has been refused as modifier type {in} value, date of service and admit to intensive
care date do not agree.
CS001
Service encounter has been disallowed as application of casts and/or splints is not approved
following a fracture procedure.
CS002
Service encounter has been disallowed as application of casts and/or splints is included in the
fracture procedure.
CS003
Service encounter has been disallowed as it is included in the surgery performed.
only one is approved at 100%.
both claimed, only one, the procedure or intensive care is approved.
service encounter, only one is approved.
fracture procedure.
DE001
Service encounter has been refused as payment responsibility is invalid for service provided.
DE002
Service encounter has been refused as payment responsibility is not valid for service indicated.
DE003
Service encounter has been refused. Payment responsibility indicated is not valid for this service.
DE004
Service encounter has been refused as payment responsibility and service indicated do not agree.
DE005
Service encounter has been disallowed as electronic text is required for this service.
the previous 30 days.
DE007
Service encountered has been disallowed as this service is restricted to individuals aged 18-64 years.
DE008
Service encounter has been disallowed as the recipient is 65 years of age or older.
DE009
Service encounter has been refused as this service has already been approved for this year.
this year.
this year.
claim on history.
previously been paid this year.
only one is approved at 100%.
XPLANATORY
CS004 Service encounter has been reduced. When multiple procedures are performed at the same time
DESCRIPTION
CS006 Service encounter has been refused. When a procedure and the daily rate for intensive care are
CS007 Service encounter has been disallowed. When a visit and minor surgery are performed at the same
CS008 Service encounter has been disallowed as application of casts and/or splints is included in the
DE006 Service encounter has been disallowed as C9999 has been approved to you or another provider in
DE010 Service encounter has been refused as two medication reviews have previously been approved for
DE011 Service encounter has been refused as the second condition amount has already been approved for
DE012 Service encounter has been refused as there is already one Unattached Patient Bonus payment
DE013 Service encounter has been refused as two Long-Term Care Clinical Geriatric Assessments have
DL001 Service encounter has been reduced. When multiple procedures are performed at the same time,
Page 51

EXPLANATORY CODES - 5
May 2011
E
CODE
DL002
Service encounter has been disallowed. When a visit and dislocation are performed at the same
service encounter, only one is approved.
DL003
Service encounter has been refused. When a procedure and the daily rate for intensive care are
both claimed, only one, the procedure or intensive care is approved.
DL004
Service encounter has been approved at 50 % as another procedure has previously been approved
at 100%.
DL005
Service encounter has been reduced to 50% as another procedure has previously been approved at
100% at this same encounter.
DL006
When multiple procedures are performed at the same time, only one is approved at 100%.
DL007
Service encounter has been disallowed as a visit and major surgery are not both payable the same
day.
ED001
Invalid or omitted record type.
ED002
Omitted action code or invalid action code and record sub-type combination.
ED003
Invalid service encounter number. (invalid or omitted submitter ID, year, sequence number, and/or
check digit.)
ED004
Invalid or omitted txn. type.
ED005
Omitted record sub-type or invalid txn. type and record sub-type combination.
ED006
Invalid payment responsibility.
ED007
Invalid or omitted service encounter type.
ED008
Invalid or omitted service start date.
ED009
Invalid or omitted service occurrence number.
ED010
Invalid or omitted diagnostic code 1.
ED011
Invalid or omitted diagnostic code 2 or 3.
ED012
Invalid multiples indicated.
ED013
Invalid modifier type, modifier value or invalid combination of type and value.
ED014
Invalid claimed unit value.
ED015
Claimed unit value must be numeric if unit value indicator contains a value of Y or health service code
contains a value of EC, IC, or IF.
ED016
Invalid claimed amount.
ED017
Invalid unit value indicator.
ED018
Unit value indicator must be blank if claimed unit value is blank.
ED019
Invalid paper support document indicator.
ED020
Invalid or omitted hospital admit date or hospital admit date inappropriate for the location
ED021
Hospital admit date cannot be subsequent to service date.
ED022
Hospital admit date must be present if service is for a registered inpatient.
ED023
Invalid intensive care admit date.
ED024
Intensive care admit date cannot be prior to hospital admit date.
ED025
Intensive care admit date is required when functional centre contains a value of NICU or INCU.
ED026
Invalid start time.
XPLANATORY
DESCRIPTION
Page 52

EXPLANATORY CODES - 6
May 2011
E
CODE
ED027
Invalid pre-authorization number.
ED028
Invalid injury diagnostic code.
ED029
Omitted or invalid service provider number or number not valid for date of service.
ED030
Invalid or omitted provider type.
ED031
Provider type is not valid for service provider number and/or date of service indicated.
ED032
Invalid referral provider number
ED033
Referral provider number must be present and must be valid.
ED034
Referral provider number and referral provider type must be blank if OOP referral indicator contains a
value of Y.
ED035
Referral provider number must be blank if referral provider type is blank.
ED036
Referral provider number must be present if referral provider type is present.
ED037
Invalid referral provider type.
ED038
Referral provider type must be blank if referral provider number is blank.
ED039
Invalid business arrangement for provider number or provider type; or, ineffective for the service start
date on the service encounter.
ED040
Business arrangement is not valid for service provider number and/or date of service.
ED041
Invalid or omitted specialty code.
ED042
Specialty code not valid for service provider number and/or date of service.
ED043
Specialty code present on service encounter is invalid for business arrangement indicated.
ED044
Invalid or omitted facility number or functional centre
ED048
Invalid or omitted service recipient health card number.
ED049
Invalid service recipient health card number for date of service or recipient is ineligible for the
program
ED050
Duplicate service encounter number previously submitted.
ED051
Service encounter number match not found.
indicated.
ED053
Invalid or omitted referral provider type.
ED054
Referral provider type not valid for date of service for referral provider number indicated.
ED055
Facility number invalid for location code indicated.
ED056
Facility number present on service encounter is invalid for business arrangement indicated.
ED057
Invalid or omitted location code.
ED058
Invalid or omitted program.
ED060
Service recipient birth date is omitted or service start date is prior to birth date.
ED062
Health service code is invalid, omitted or invalid for the business arrangement indicated.
ED063
Invalid or omitted pay to code.
ED064
Invalid pay to health card number.
XPLANATORY
DESCRIPTION
ED052 Referral provider type must be present and valid for service date if referral provider number is
Page 53

EXPLANATORY CODES - 7
May 2011
E
CODE
ED065
Service encounter has been refused as the service encounter that shares the same text cannot be
found.
ED066
Invalid record sequence.
ED067
Invalid or omitted surname on person data record.
ED068
Invalid or omitted given name on person data record.
ED069
Invalid date of birth on person data record.
ED070
Birth date in person data record must be blank if pay to code is OTHR and birth date must be present
on person data record if pay to code is RECP.
ED071
Invalid gender code on person data record.
ED072
Omitted address on person data record.
ED073
Invalid or omitted city name on person data record.
ED074
Invalid or omitted province/state code on person data record.
ED075
Invalid country on person data record.
ED076
Service encounter has been refused as the person data record is absent.
ED077
Only one CPD1, CBE1, or CTX1 permitted for each service encounter transaction
ED078
Recipient health card number and pay to health card number are the same
ED079
Remuneration method not fee for service or shadow billing.
ED080
Health service code must contain supporting text and claimed unit value.
ED081
Invalid health card number check digit.
ED082
Invalid record length.
ED083
CPD1 record sub-type present when it is not required.
ED084
Out of province referral indicator is not blank or it contains a value other than Y.
ED085
Non-printable characters in chart number field.
ED086
Non-printable characters in unused field.
ED087
Invalid postal code format.
ED088
Guardian/parent HCN is not alphanumeric.
ED089
Supporting text contains unprintable characters.
ED090
Invalid submitter ID.
ED091
Invalid year in the service encounter number on the CTX1 record sub type.
ED092
Invalid sequence number in the service encounter number on the CTX1 record sub type.
ED093
Invalid check digit on the service encounter number on the CTX1 record sub type.
ED094
Unsupported transaction type.
ED095
Transaction badly formed.
ED096
Parent or guardian must contact MSI to validate health card number for preregistered newborn.
ED097
Date of service is subsequent to expiry date for health card number.
ED098
Hospital admit date and intensive care admit date must be blank for action code of P.
ED099
Birth date is blank on base service encounter record and person data record.
XPLANATORY
DESCRIPTION
Page 54

EXPLANATORY CODES - 8
May 2011
E
CODE
ED100
Duplicate service encounter number previously submitted, currently in held status, waiting for manual
review.
ED101
Provider type not allowed to bill.
ED102
Provider type not allowed to refer.
ED103
Service recipient birth date does not match birth date on health card.
ED104
Service encounter accepted at zero as it is outdated.
GN001
Service encounter has been refused as a similar service has been approved on the same day.
GN002
Service encounter has been refused as hospital admit date is required for services performed on
registered inpatients.
GN003
Service encounter has been refused as this is an excluded service under the reciprocal billing
agreement.
GN004
Service encounter has been refused as self referral is not acceptable.
GN005
Service encounter has been refused as payment responsibility WCB is not valid for patient under
sixteen.
GN006
Service encounter has been refused as hospital admit date is necessary for processing this service.
GN007
Service encounter has been refused as modifier AG value does not agree with age of patient.
GN008
Service encounter has been disallowed as this procedure is included in critical care.
GN009
Service encounter has been refused as patient's sex is invalid for service provided.
GN010
Service encounter has been refused. Please resubmit with text indicating specific areas involved.
GN011
Service encounter has been disallowed as a consultation has been approved to you in the previous
14 days.
GN012
Service encounter has been refused as no preauthorization number was indicated or number
indicated is invalid.
GN013
Service encounter has been refused as it is a duplicate submission.
GN014
Service encounter has been refused as a previously reduced matching service encounter is not
present.
GN015
Service encounter has been reassessed.
GN016
Invalid or omitted health service code.
GN017
Service encounter has been refused as your specialty is not approved for performing this service.
GN018
Service encounter has been refused as first and consecutive anaesthetic start times cannot be the
same.
GN019
Service encounter has been refused as it is an exact duplicate to a previously submitted service
encounter.
GN020
Service encounter has been adjudicated according to information provided.
GN021
Service encounter has been adjudicated according to a decision by the medical claims evaluation
committee.
GN022
Service encounter has been refused as it is an uninsured service under MSI.
GN023
Service encounter has been refused as it is outdated.
GN024
Service encounter has been disallowed as it is an uninsured service under MSI.
GN025
Service encounter has been refused as this service is included in the composite fee.
XPLANATORY
DESCRIPTION
Page 55

EXPLANATORY CODES - 9
May 2011
E
CODE
GN026
Service encounter has been adjudicated based on duration of service.
GN027
Service encounter has been refused as it requires multiples. Resubmit using the correct number of
multiples.
GN028
Service encounter has been refused. Resubmit indicating duration of service.
GN029
Service encounter has been refused as an assistant is not approved for this service.
GN030
Service encounter has been refused. If resubmitting, provide all details that will assist in determining
payment.
GN031
Service recipient birth date does not match birth date on health card. Birth date from health card
should be used. This does not affect payment.
GN032
Service encounter has been refused. Resubmit using the appropriate health service code(s) as listed
in your Physician’s Manual.
GN033
Service encounter has been refused. Resubmit, indicating in the claimed unit value field, the number
of units required for the procedure performed.
GN034
Service encounter has been refused as the pay to code indicated is not appropriate.
GN035
Service encounter has been refused as pay to code indicated is not valid for payment responsibility
indicated.
GN036
Service encounter has been refused as a previous service under this same service code has been
approved.
GN037
Service encounter has been refused as a previous service has been approved under this same
service code at this service encounter.
GN038
Service encounter has been refused as a previous service encounter has been accepted for this
same service code.
code has been approved.
GN040
Service encounter has been disallowed as a visit and surgery are not both payable.
GN041
Service encounter has been refused as a previous service encounter was approved for this same
health service code.
indicated.
performed.
explanatory text.
encounter number.
GN047
Service encounter has been refused. Submit a reassess (action code R) for the original submission
to aid in the assessment of your claim.
GN049
Service encounter has been disallowed as text provided does not provide sufficient details. If
resubmitting please provide more details to aid in the assessment of your claim.
XPLANATORY
DESCRIPTION
GN039 Service encounter has been refused as a previous service encounter for this same health service
GN042 Service encounter has been refused as payment responsibility is not valid for date of service
GN043 Service encounter has been refused. Resubmit indicating start and finish time for procedure
GN044 Service encounter has been disallowed as a service occurrence other than 1 has been used without
GN045 Service encounter has been disallowed as text provided does not include the original service
GN046 Service encounter had been disallowed as text provided does not include the time of the encounter
GN048 Service encounter has been disallowed. Submit a reassess (action code R) for the original
submission to aid in the assessment of your claim.
Page 56

EXPLANATORY CODES - 10
May 2011
E
CODE
GN050
Service encounter has been refused. Resubmit under the same health service code using the
appropriate lesser value modifier for the service provided.
GN052
Service encounter has been disallowed. Resubmit with a copy of the time sheet for the surgery
MA001
Service encounter has been approved at 50%. When multiple closed or no reductions are performed
should be claimed.
fracture.
followed by an open reduction.
only one is approved at 100%.
both claimed, only one, the procedure or intensive care is approved.
encounter only one is approved at 100%.
procedures are performed at the same time.
MA008
Service encounter has been refused. Interim service code has expired. Application must be
submitted to Doctors Nova Scotia for establishing a permanent health service code.
MI001
Service encounter has been approved at 50%. When multiple closed or no reductions are performed
should be claimed.
MI002
Service encounter has been refused. 50% of the listed fee for the initial closed or no reduction is
fracture.
MI003
Service encounter for no or closed reduction has been approved at 50% of the listed fee as it has
been followed by an open reduction.
MI004
Service encounter has been reduced. When multiple procedures are performed at the same time,
only one is approved at 100%.
MI005
Service encounter has been refused. When a procedure and the daily rate for intensive care are
both claimed, only one, the procedure or intensive care is approved.
MI006
Service encounter has been reduced. When multiple procedures are performed at the same
encounter, only one is approved at 100%.
MJ001
Service encounter has been reduced to 50%. When multiple surgical procedures are performed at
the same time, only one is approved at 100%.
MJ002
Service encounter has been refused. When a procedure and the daily rate for intensive care are
both claimed, only one, the procedure or intensive care is approved.
MJ003
Service encounter has been refused as this once per lifetime procedure has previously been
approved.
pacemaker insertion.
XPLANATORY
GN051 Service encounter has been refused as a service encounter one (1) has not been claimed for this
day.
performed to aid in the adjudication of your claim.
on the same fracture, at different service encounters, by the same provider 50% for each reduction
MA002 Service encounter has been reduced. 50% of the listed fee for the initial closed or no reduction is
approved when a different physician performs a subsequent closed or no reduction on the same
MA003 Service encounter for closed reduction has been approved at 50% of the listed fee as it has been
MA004 Service encounter has been reduced. When multiple procedures are performed at the same time,
MA005 Service encounter has been refused. When a procedure and the daily rate for intensive care are
DESCRIPTION
MA006 Service encounter has been reduced. When multiple procedures are performed at the same
MA007 Service encounter has been reduced. Only one procedure is approved at 100% when multiple
on the same fracture, at different service encounters, by the same provider 50% for each reduction
approved when a different provider performs a subsequent closed or no reduction on the same
MJ004 Service encounter has been refus ed as this adjustment of leads occurred within 30 days of
Page 57

EXPLANATORY CODES - 11
May 2011
E
CODE
MJ005
Service encounter has been refused as initial cauterization of the rectum has been approved in the
previous 30 days.
MJ006
Service encounter has been refused as initial photo coagulation has been approved for eye(s)
indicated in the previous 30 days.
MJ007
Service encounter has been refused as this is not the appropriate health service code for post-op
haemorrhage when claimed by the surgeon who performed the tonsillectomy.
MJ008
Service encounter has been refused as a preauthorization number was not indicated.
MJ009
Service encounter has been adjudicated based on the surgeons submission.
MJ010
Service encounter has been refused. Resubmit with a copy of the operative report to aid in the
adjudication of your service encounter.
MJ011
Service encounter has been refused based on the age of the recipient.
MJ012
Service encounter has been refused as this health service is not appropriate for persons 16 years or
older.
MJ013
Service encounter has been refused as this health service is not appropriate for persons under 16
years of age.
MJ014
Service encounter has been reduced to 50%. Only one procedure is approved at 100% when
multiple surgical procedures are performed at the same time.
service.
MJ016
Service encounter has been disallowed as this service is included in a previously approved
procedure.
MJ017
Service encounter has been refused as no preauthorization number was indicated.
number.
been approved.
approved.
adjudication of your service encounter.
has already been claimed by you for this date.
anal sphincter on this date.
this date.
MJ025
Service encounter has been refused as a claim for donor has already been received for this patient.
A patient cannot be both a donor and recipient of a liver.
MJ026
Service encounter has been refused as a claim for recipient has already been received for this
patient. A patient cannot be both a donor and recipient of a liver.
MJ027
Service encounter has been disallowed as the injected substance has not been indicated.
MJ028
Service encounter has been refused as a claim for the ICD insertion team fee has already been made
for this patient.
XPLANATORY
DESCRIPTION
MJ015 Service encounter has been disallowed as thi s procedure is included in a previously approved
MJ018 Service encounter has been refus ed as this service requires electronic text or a prior approval
MJ019 Service encounter has been refus ed as a previous service encounter for a second physician has
MJ020 Service encounter has been refus ed as a previous service encounter for an assist fee has been
MJ021 Service encounter has been refus ed. Resubmit with a copy of the outpatient report to aid in the
MJ022 Service encounter has been refus ed as a total abdominal hysterectomy or repair of inverted uterus
MJ023 Service encounter has been refus ed as you have already claimed a repair of obstetrical trauma or
MJ024 Service encounter has been refus ed as you have already claimed a repair of obstetrical trauma on
Page 58

EXPLANATORY CODES - 12
May 2011
E
CODE
MJ029
Service encounter has been refused as a claim for the ICD insertion composite fee has already been
made for this patient.
MN001
Service encounter has been disallowed as it is included in the delivery.
MN002
Service encounter has been disallowed as compression sclerotherapy includes after care for one
year.
MN003
Service encounter has been disallowed. When a visit and a surgical procedure are claimed together,
only one is approved.
MN004
Service encounter has been disallowed. When a visit and minor surgery are performed at the same
service encounter, only one is approved.
MN005
Service encounter has been refused as this procedure has been performed within the previous 7
days.
MN006
Service encounter has been refused. When a procedure and the daily rate for intensive care are
both claimed, only one, the procedure or intensive care is approved.
MN007
Service encounter has been reduced. When multiple procedures are performed at the same time,
only one is approved at 100%.
MN008
Service encounter has been refused as it is a deinsured service for patients under one year of age.
encounter, only one is approved at 100%.
MN010
Service encounter has been disallowed as it is included in the fee for the adenoidectomy.
MN011
Service encounter has been disallowed as procedure claimed and a consultation are not both
payable.
MS001
Service encounter has been refused. Complete details are necessary when billing this service.
NR001
Service encounter has been adjudicated based on a decision by the medical consultant.
NR002
Service encounter has been approved under the appropriate code.
NR003
Service encounter has been refused as a second assistant is not approved for this service.
NR004
Service encounter has been adjudicated based on the fee payable for the assistant.
NR005
Service encounter has been adjudicated based on the fee payable to the second assistant.
NR006
Service encounter has been refused. Indicate actual procedure performed when resubmitting.
NR007
Service encounter has been approved at the general practice rate re age of patient.
NR008
Service encounter has been refused. Submit a new service encounter once approval has been
received from the psychotherapy waiver review committee.
NR009
Please delete original submission and submit a new service encounter for a partial eye exam.
NR010
Service encounter has been refused as this visit is not payable during intensive care.
NR011
Service encounter has been refused as date of service appears incorrect according to our records.
NR012
Service encounter has been adjusted based on information provided by MSI audit.
NR013
Service encounter has been refused. Delete original submission and resubmit using the appropriate
modifier of region both.
NR014
Service encounter has been refused. Resubmit with a copy of the pathology report to aid in the
adjudication of your service encounter.
NR015
Service encounter has been approved at the internal medicine rate re age of patient.
NR016
Service encounter has been disallowed as all the requirements for billing this service have not been
met.
XPLANATORY
MN009 Service encounter has been reduced. When multiple procedures are performed at the same
DESCRIPTION
Page 59

EXPLANATORY CODES - 13
May 2011
E
CODE
NR017
Service encounter has been refused as a previous payment covers all or a portion of this
combination.
NR018
Service encounter has been refused as previous payment covers this submission.
NR019
Service encounter has been refused as this same service has been approved for another provider.
NR020
Service encounter has been refused. Resubmit using the appropriate service occurrence number.
NR021
Service encounter has been adjudicated based on the time indicated for the consecutive
anaesthetist.
NR022
Service encounter has been adjudicated according to the weekly maximum payable after 56 days of
hospitalization.
NR023
Service encounter has been disallowed as a pap smear is not payable with a visit for a
gynaecological or obstetrical diagnosis.
NR024
Service encounter has been adjusted in accordance with the surgical rules described in the
Preamble.
NR025
Service encounter has been adjudicated based on the preamble ruling for outdated submissions.
NR026
Service encounter has been refused as the hospital admit date indicated is incorrect.
NR027
Service encounter has been adjudicated based on preamble rules.
NR028
Service encounter has been adjudicated based on payment for a bilateral procedure.
NR029
Resubmit under the appropriate health service code for this bilateral procedure.
NR030
Service encounter has been disallowed as medical necessity was not indicated.
NR031
Service encounter has been disallowed as the appropriate documentation has not been received.
NR032
Service encounter has been disallowed as copies of the referral letter and consult report are required.
NR033
Service encounter has been disallowed as the required WCB form was not received within the
appropriate time.
NR034
Service encounter has been adjudicated according to the rate set by workers' compensation board.
NR035
Service encounter has been refused as region (right, left, both) was not indicated.
NR036
Service encounter may be readjudicated according to the submission by the surgeon.
NR037
Service encounter has been disallowed as the injection indicated is not on the provincial
immunization list.
NR038
Service encounter has been disallowed as the tray fee is not applicable for service provided.
NR039
Service encounter has been accepted at zero as it is outdated.
NR040
Service encounter has been refused as prior approval number indicated is not valid.
NR041
Service encounter has been disallowed as the maximum number of this type of visit allowed without a
prior approval number have been approved for this episode.
NR042
Service encounter has been disallowed as the maximum number of preauthorized visits for this
episode have been approved.
NR043
Service encounter has been disallowed as the maximum number of encounters for this service per
year has been reached.
NR044
Service encounter has been disallowed as the maximum number of well baby visits allowed have
been approved for payment.
NR045
Service encounter has been refused. Resubmit using the appropriate health service code(s) as listed
in the Physician’s Manual and/or Physicians' Bulletin.
XPLANATORY
DESCRIPTION
Page 60

EXPLANATORY CODES - 14
May 2011
E
CODE
NR046
Service encounter payment has been calculated based on the percentage payable on the total major
surgical procedural fee(s) excluding the premium fee portion.
NR047
Service encounter has been refused. Resubmit using the appropriate health service code based on
information provided.
NR048
Service encounter has been refused. Resubmit indicating the base units used for the procedure
performed.
NR049
Service encounter has been refused. Resubmit indicating the correct region.
NR050
Service encounter has been disallowed as text provided does not warrant approval.
NR051
Patient history transfer has occurred due to duplicate registration of individual. Patient history will
now appear under the active registration number.
NR052
Service encounter has been refused as previous payment has occurred under an incorrect HCN.
Internal adjustment will be made to correct our records.
NR053
Service encounter has been refused as the business arrangement indicated is incorrect according to
our records.
NR054
Service encounter has been disallowed. Delete the original submission and submit a new service
encounter under the appropriate business arrangement.
verified the date you have indicated is correct.
NR056
Service encounter has been adjudicated based on information published in a Physicians’ Bulletin.
Manual.
NR058
Service encounter has been adjudicated based on information contained in the Physician’s Manual.
modifier used in relation to intensive care admit date indicated.
based on the information you have provided.
NR061
Service encounter has been refused re diagnosis indicated.
medication. An over the counter drug or product is not insured.
comprehensive visit.
NR064
Service encounter has been refused. Referring provider indicated is invalid for referral.
NR065
Service encounter has been adjudicated based on telephone conversation.
NR066
Service encounter has been refused as hospital admit date is incorrect.
NR067
Service encounter has been refused as intensive care admit date is incorrect.
NR068
Service encounter has been adjudicated based on the operative and/or pathology report.
published in the Physicians' Bulletin.
anaesthetist.
NR071
Indicate type of anaesthesia (general or local) for procedure performed.
XPLANATORY
NR055 Service encounter has been disallowed as patient history indicates conflicting intensive care admit
dates. Confirm intensive care admit date and submit a reassess (action code R) once you have
DESCRIPTION
NR057 Service encounter has been adjudicated based on information contained in the Billing Instructions
NR059 Service encounter has been refused as electronic text was not present explaining date of service and
NR060 Service encounter has been refused. Delete the original submission and submit a new encounter
NR062 Service encounter has been refused as this service is only insured in conjunction with prescribed
NR063 Service encounter has been refused as diagnosis indicated does not warrant approval of a
NR069 Service encounter has been refused. Resubmit a new service encounter based on information
NR070 Service encounter has been adjudicated based on the time indicated for the simultaneous
Page 61

EXPLANATORY CODES - 15
May 2011
E
CODE
NR072
Service encounter has been disallowed. Submit a reassess (action code R) along with a copy of the
operative report to aid in the assessment of your service encounter.
NR073
Service encounter has been disallowed as a pap smear is not payable in addition to a visit,
NR074
Service encounter has been refused. A maximum of one hour only for a Palliative Care Support Visit
is payable per patient per day.
NR075
Service encounter for tray fee has been adjusted to agree with number of injections approved.
NR076
Service encounter has been adjudicated based on diagnosis indicated.
NR077
Service encounter has been adjudicated based on correspondence from MSI.
NR078
Service encounter has been disallowed. Submit a reassess (action code R) along with a copy of the
outpatient report to aid in the assessment of your service encounter.
NR079
Service encounter payment has been calculated based on the percentage payable on the total major
surgical procedure(s).
NR080
Service encounter has been refused as the pay to code is not BAPY.
NR081
Service encounter has been adjudicated according to the weekly maximum of 80 units per week after
56 days from admission.
NR082
Please contact MSI regarding this claim
NR083
Service encounter has been refused as a substance other than air was injected.
both claimed, only one, the procedure or intensive care is approved.
labour.
OP001
Service encounter has been disallowed as routine vision care is uninsured re age of patient.
Payment has been approved to you or another provider in the previous year.
older.
another provider in the previous year.
another provider in the previous year.
OP006
Service encounter has been disallowed as a previous optometric vision analysis has been approved
to you or another provider during the previous year.
OP007
Service encounter has been disallowed as a previous continuing care visit has been approved to you
or another provider during the previous year.
OP008
Service encounter has been refused as this service is not payable for your specialty.
OP009
Service encounter has been disallowed as only one routine optometric vision analysis is payable
during a two year period.
OP010
Service encounter has been disallowed as only one routine optometric vision analysis is payable
during a two year period.
OP011
Service encounter has been refused as electronic text is required with reference to the specific drug
involved.
XPLANATORY
DESCRIPTION
consultation or procedure for a gynecological or obstetrical diagnosis.
OB001 Service encounter has been refused. When a procedure and the daily rate for intensive care are
OB002 Service encounter has been disallowed as you have previously been approved for transfer during
OP002 Service encounter has been disallowed. Only one exam for medical necessity is payable per year.
OP003 Service encounter has been disallowed as this service is not payable for persons 19 years of age and
OP004 Service encounter has been disallowed as an optometric vision analysis has been approved to you or
OP005 Service encounter has been disallowed as a continuing care visit has been approved to you or
Page 62

EXPLANATORY CODES - 16
May 2011
E
CODE
OP012
Service encounter has been disallowed as this once per lifetime procedure has previously been
approved for either region right, left or both.
OP013
Service encounter has been disallowed as this once per lifetime procedure has previously been
approved for either region left or both.
OP014
Service encounter has been disallowed as this once per lifetime procedure has previously been
approved for either region right or both.
OP015
Service encounter has been disallowed as a routine vision analysis is not an insured service re age of
patient.
OP016
Service encounter has been disallowed as it is routine in nature.
OP017
Service encounter has been disallowed as this service is only payable for a non-routine diagnosis.
OP018
Service encounter has been disallowed re routine diagnosis indicated.
OP019
Service encounter has been disallowed as an optometric vision analysis has been approved in the
past year.
OP020
Service encounter has been disallowed as a continuing care visit is payable only once per year.
OP021
Service encounter has been disallowed as a previous optometric vision analysis was approved during
the previous year.
OP022
Service encounter has been disallowed as continuing care visits are payable once per year only.
OP023
Service encounter has been disallowed as a routine diagnosis has been indicated.
OP024
Service encounter has been disallowed due to routine diagnosis indicated.
OP025
Service encounter has been disallowed as another non-routine vision analysis has been approved
during the previous year.
OP026
Service encounter has been disallowed as a previous continuing care visit has been approved during
the last year.
OP027
Service encounter has been disallowed as diagnosis does not warrant payment of this service.
OP028
Service encounter has been approved at the non referred rate for this service as the referring
provider type is not PH.
OP029
Service encounter has been disallowed as the maximum 6 visits allowed per year for this type of
service have been approved.
OP030
Service encounter has been refused as text is required indicating the name of the prescribed drug or
that no prescription was required.
receiving the referral.
OP032
Service encounter has been refused as your specialty is not valid for service claimed.
included on the service encounter.
indicated.
OP035
Service encounter has been refused as you have previously been paid a visit this day.
this day.
payable at the same service encounter.
XPLANATORY
DESCRIPTION
OP031 Service encounter has been refused as text is required indicating the name of the ophthalmologist
OP033 Service encounter has been refused as the required keratoconus diagnostic code (37160) was not
OP034 Service encounter has been refused as no diagnostic code warranting payment of premium fee was
OP036 Service encounter has been refused as you have previously been paid an Optometric Vision Analysis
PC001 Service encounter has been refused as psychotherapy or counselling and a consultation are not
Page 63

EXPLANATORY CODES - 17
May 2011
E
CODE
PC002
Service encounter has been refused as psychotherapy or counselling and a visit are not payable at
the same service encounter.
PC003
Service encounter has been refused. A maximum of 90 continuous minutes of individual
psychotherapy only is allowed per patient per day.
PC004
Service encounter has been refused as a minimum of one half hour must be spent per visit for
psychotherapy to be payable.
PC005
Service encounter has been refused as patient is under four years of age.
PC006
Service encounter has been adjudicated according to total hours approved in the previous 365 days.
PC007
Service encounter has been refused as another physician is providing psychotherapy to this patient.
PC008
Service encounter has been refused. A maximum of 2 hours of group psychotherapy only is allowed
per patient per day.
PC009
Service encounter has been refused. A maximum of 2 hours of family therapy only is allowed per
patient per day.
PC010
Service encounter has been refused as you have previously been approved the intensive care daily
rate this day.
PC011
Service encounter has been refused. A maximum of 90 minutes of hypnotherapy only is allowed per
patient per day.
hypnotherapy to be payable.
PC013
Service encounter has been refused. A maximum of one hour of counselling only is allowable per
patient per day.
allowable per patient per day.
approved.
approved.
previously been approved.
PC018
Service encounter has been refused. Maximum limit of 10 hours of hypnotherapy per year has
previously been approved.
PC019
Service encounter has been refused. Maximum limit of 5 hours of counselling per year has
previously been approved.
PC020
Service encounter has been refused. Maximum limit of 2 hours of lifestyle counselling per year has
previously been approved.
PC021
Service encounter has been approved at the maximum allowed per day for this service.
PC022
Service encounter has been disallowed as patient is 19 years of age or greater.
PC023
Service encounter has been disallowed as location and/or provider specialty is not appropriate for
service claimed.
PC024
Service encounter has been refused as you have not indicated that prior approval has been issued.
Maximum limit of 20 hours per year for individual psychotherapy has previously been approved.
PC025
Service encounter has been refused as you have not indicated that prior approval has been issued.
Maximum limit of 20 hours per year for group psychotherapy has previously been approved.
XPLANATORY
DESCRIPTION
PC012 Service encounter has been refused. A minimum of one half hour must be spent per visit for
PC014 Service encounter has been refused. A maximum of 30 minutes of lifestyle counselling only is
PC015 Service encounter has been refused as you have not indicated that a waiver or prior approval has
been issued. Maximum limit of 15 hours per year for individual psychotherapy has previously been
PC016 Service encounter has been refused as you have not indicated that a waiver or prior approval has
been issued. Maximum limit of 15 hours per year of group psychotherapy has previously been
PC017 Service encounter has been refused. Maximum limit of 15 hours of family therapy per year has
Page 64

EXPLANATORY CODES - 18
May 2011
E
CODE
PC026
Service encounter has been refused. Maximum limit of 20 hours of family therapy per year has
previously been approved.
PC027
Service encounter has been refused as you have not indicated that prior approval has been issued.
Maximum limit of 20 hours per year for family therapy has previously been approved.
PC028
Service encounter has been refused as you have not indicated that prior approval has been issued.
Maximum limit of 20 hours per year for group therapy has previously been approved.
PC029
Service encounter has been refused as you have not indicated that prior approval has been issued.
Maximum limit of 20 hours per year for individual therapy has previously been approved.
PC030
Service encounter has been refused as you have not indicated that prior approval has been issued.
Maximum limit of 10 hours per year for hypnotherapy has previously been approved.
PC031
Service encounter has been refused as you have not indicated that prior approval has been issued.
Maximum limit of 2 hours per year for lifestyle counselling has previously been approved.
PC032
Service encounter has been refused as you have not indicated that prior approval has been issued.
Maximum limit of 5 hours per year for counselling has previously been approved.
PP001
Hospital out-patient and/or emergency room charges incurred outside Canada are not insured.
PP002
Radiology and/or laboratory costs incurred outside Canada are not insured.
PP003
Private facility costs are not insured.
PP004
Services received outside Canada for non-urgent/pre-existing medical conditions are not insured.
PP005
Medical services known to be required prior to departure from your home province are not insured.
PP006
Medical services such as monitoring, stabilizing or continuing treatment of existing medical conditions
are not insured.
PP007
Routine/annual physical examinations or those requested by a third party are not insured.
PP008
Routine eye exams performed outside Nova Scotia are not insured.
PP009
Prescription drugs purchased outside Nova Scotia are not insured.
PP010
Services provided by non-medical personnel are not insured.(examples-chiropractor, physiotherapist,
pac-physician's assistant certified, podiatrist)
PP011
Ambulance services, medical supplies, mileage costs, telephone advice or charges for preparation of
reports, records, certificates are not insured.
PP012
Eye glasses, hearing aids or other prosthetic appliances are not insured.
PP013
This service encounter was submitted by active claims management. Please refer to electronic text.
PP014
This claim is not payable as our records show this patient is registered for MSI on a student visa/work
Scotia.
allowable based on the payment policy of the province where you received treatment.
allowable based on Nova Scotia rates.
allowable based on Nova Scotia rates.
business arrangement is cheque.
review.
XPLANATORY
DESCRIPTION
permit/nato exchange and therefore is eligible for health coverage only in the province of Nova
PP015 Your claim for medical services outside Nova Scotia has been paid at the maximum amount
PP016 Your claim for medical services received outside Canada has been pai d at the maximum amount
PP017 Your claim for medical services received in Nova Scotia has been paid at the maximum amount
PP018 Service encounter has refused as a pay to code of BAPY is not appropriate. Payment method for this
PP019 The remainder of your claims have been forwarded to the Nova Scotia Department of Health for their
Page 65

EXPLANATORY CODES - 19
May 2011
E
CODE
PP020
Services received outside Canada for non-urgent medical conditions are not insured.
PP021
Services received outside Canada for pre-existing medical conditions are not insured.
PP022
Your claim for medical services outside Nova Scotia has been paid at the maximum amount
allowable based on Nova Scotia rates.
PP023
Your claim for dental services has been forwarded to Quickcard Solutions Inc. for review.
PR001
This claim is not payable as replacement costs have been approved in the previous two years.
PR002
This claim for early replacement has been approved for payment.
PR003
This claim is not payable as replacement costs have been approved in the previous 7 years.
PR004
This claim is not payable as replacement costs have been approved in the previous 2 years.
PR005
This claim for prosthetic services has been approved at the maximum amount allowable, based on
Nova Scotia rates.
PR006
This claim is not payable as replacement costs have been approved in the previous 5 years.
PR007
This claim is not payable as replacement costs have been approved in the previous 2 years.
PR008
This claim has not been approved as your client is over 19 years of age and under 65 years of age,
and is not registered with cnib.
PR009
This claim has been refused as it requires multiples. Resubmit indicating the appropriate number of
multiples.
PR010
Service encounter has refused as pay to code should be BAPY.
PR011
This claim is not payable as replacement costs have been approved in the previous 4 years.
RF001
Service encounter has been refused. No adjustment is warranted.
RF002
Service encounter has been refused. Delete original submission(s) and submit new action code A
transaction based on correct information or information provided by you.
RF003
Request for readjudication has been refused. Approval for this request has been previously
processed.
RF004
Request for readjudication has been refused. Denial of this request has been previously processed.
RF005
Payment under this visit service cannot be approved. Delete the original service encounter and
submit under the appropriate subsequent visit service.
VA001
Service encounter has been disallowed as a pap smear is not payable with a comprehensive
evaluation.
VA002
Service encounter has been refused as this service is included in the consultation.
VA003
Service encounter has been reduced. When multiple diagnostic and therapeutic procedures are
performed, only the fee for one is approved at 100%.
VA004
Service encounter has been disallowed as this procedure cannot be claimed in addition to the basic
units for cardiac bypass.
VA005
Service encounter has been disallowed as it is included in limited prenatal and postnatal visits.
VA006
Service encounter has been disallowed as it is included in the delivery.
VA007
Service encounter has been disallowed as venipuncture is not payable in hospital unless medical
necessity exists.
VA008
Service encounter has been refused as service is not approved in location indicated.
XPLANATORY
DESCRIPTION
Page 66

EXPLANATORY CODES - 20
May 2011
E
CODE
VA009
Service encounter has been disallowed as the maximum limit per week has previously been
approved.
VA010
Service encounter has been disallowed as local anaesthetic is not approved when performed in
conjunction with minor surgery.
VA011
Service encounter has been refused as you have previously been approved a consultation with
detention at the same service encounter.
VA012
Service encounter has been refused as venipuncture is included in the comprehensive prenatal
exam.
VA013
Service encounter has been refused as modifier value indicated and patients age do not agree.
VA014
Service encounter has been refused. When a procedure and the daily rate for intensive care are
both claimed, only one, the procedure or intensive care is approved.
VA015
Service encounter has been disallowed as this service is included in a visit or consultation.
VA016
Service encounter has been refused as this service is included in the fee for a complete eye exam.
VA017
Service encounter has been refused as your specialty is not approved for performing this procedure.
VA018
Service encounter has been reduced. When multiple diagnostic and therapeutic procedures are
performed, only one is approved at 100%.
VA019
Service encounter has been refused as it is a stand alone procedure and another service has been
approved.
VA020
Service encounter has been refused as a previous stand alone procedure has been approved.
VA021
Service encounter has been refused as you have previously been approved a visit with detention at
the same service encounter.
VA022
Service encounter has been refused as this service is included in the comprehensive visit.
VA023
Service encounter has been refused. This service is included in the comprehensive visit.
VA024
Service encounter has been refused as this procedure is included in the comprehensive visit.
VA025
Service encounter has been disallowed as this service is included in the surgery.
VA026
Service encounter has been refused as the provider must be a qualified allergist.
VA027
Service encounter has been refused as this service is only approved at hospital locations.
VA028
Service encounter has been disallowed as this service is included in the visit previously approved at
this same service encounter.
VA029
Service encounter has been disallowed as this procedure is included in the previously approved visit.
VA030
Service encounter has been disallowed as local anaesthesia is not payable in addition to the surgical
fee.
VA031
Service encounter has been refused as a comprehensive examination for the same or similar
the medical necessity of this complete examination.
the last year.
days for invasive EEG video telemetry.
days for non-invasive EEG video telemetry.
as the insertion of CRT pacemaker/defibrillator device.
XPLANATORY
DESCRIPTION
diagnosis has been approved to you within the past year. Please provide further details regarding
VA032 Service encounter has been refused as a comprehensive examination has been paid to you within
VA033 Service encounter has been refused as you have already claimed the maximum of four subsequent
VA034 Service encounter has been refused as you have already claimed the maximum of four subsequent
VA035 Service encounter has been refused as you cannot claim electrophysiology studies on the same day
Page 67

EXPLANATORY CODES - 21
May 2011
E
CODE
VE001
Service encounter has been disallowed as visit excluded procedures are included in the consultation.
VE002
Service encounter has been reduced. When multiple diagnostic and therapeutic procedures are
performed, only the fee for one is approved at 100%.
VE003
Service encounter has been disallowed. When a procedure and the daily rate for intensive care are
both claimed, only one, the procedure or intensive care is approved.
VE004
Service encounter has been disallowed as visit excluded procedures and a visit are not payable at
the same service encounter.
VE005
Service encounter has been refused. When a procedure and the daily rate for intensive care are
both claimed, only one, the procedure or intensive care is approved.
VE006
Service encounter has been disallowed as this service applies only to patients in the insured age
group.
VT001
Service encounter has been disallowed as this service is included in the postoperative care of
fractures.
VT002
Service encounter for comprehensive evaluation has been refused as a comprehensive evaluation
has been approved in the previous 30 days.
admission.
been approved and the patient has been readmitted within 30 days for the same or related condition.
or similar diagnosis.
the previous 9 months to you or another physician.
another physician.
VT008
Service encounter has been disallowed as a complete care code includes a visit the same day and
related visits for the following 14 days.
VT009
Service encounter has been disallowed as a fracture procedure has been approved to you on the
same day or in the previous 42 days.
VT010
Service encounter has been disallowed as a well baby visit is not payable after one year of age.
VT011
Service encounter has been disallowed as a well baby visit has been approved to you or another
physician during this age interval.
VT012
Service encounter has been disallowed as after six months of age well baby visits are approved on
the basis of once every three months up to one year of age.
VT013
Service encounter for comprehensive visit has been refused as you have been approved a
consultation in the previous 30 days.
VT014
Service encounter has been disallowed as the maximum number of prenatal visits have been
approved.
VT015
Service encounter has been disallowed as a post partum visit cannot be approved on the same day
as a delivery.
VT016
Service encounter has been refused as you or another physician have previously been approved for
first exam of healthy newborn.
VT017
Service encounter has been refused as newborn care of a healthy infant is only approved for the first
five days after birth.
XPLANATORY
VT003 Service encounter for in-patient comprehensive evaluation has been refused as another in-patient
comprehensive evaluation has been approved to you or another physician in your specialty for this
DESCRIPTION
VT004 Service encounter been has disallowed as an in-patient comprehensive evaluation has previously
VT005 Service encounter has been refused as the patient has been readmitted within 10 days for the same
VT006 Service encounter has been refused as a comprehensive pregnancy exam has been approved during
VT007 Service encounter has been refused as a previous post natal care visit has been approved to you or
Page 68

EXPLANATORY CODES - 22
May 2011
E
CODE
VT018
Service encounter has been disallowed as visit excluded procedures and a visit are not payable at
the same service encounter.
VT019
Service encounter has been disallowed as another physician has been approved an inpatient hospital
visit on this date.
VT020
Service encounter has been disallowed as this is included in the assist fee.
VT021
Service encounter has been refused as continuing or directive care must be preceded by a
consultation
VT022
Service encounter has been refused as a visit and psychotherapy or counselling are not payable at
the same service encounter.
VT023
Service encounter has been refused as you have previously been approved a visit or consultation
this day under the same service occurrence number.
VT024
Service encounter has been disallowed as this service is included in the preoperative care.
VT025
Service encounter has been disallowed as this service is included in the postoperative care.
VT026
Service encounter has been refused as you or another physician have previously been approved
anticoagulant supervision for this same month.
VT027
Service encounter has been disallowed as contact lens fitting includes follow up for three months.
VT028
Service encounter for a visit on the same day as a stress test has been disallowed as the patient was
seen in consultation in the previous 14 days.
VT029
Service encounter has been disallowed as a visit is not approved the same day as critical care.
VT030
Service encounter has been disallowed as compression sclerotherapy includes after care for one
year.
VT031
Service encounter has been refused as detention is not payable in the office.
VT032
Service encounter for a visit with detention has been refused as you have previously been approved
a visit allowed procedure at the same service encounter.
VT033
Service encounter has been adjudicated according to the weekly maximum of 44 units allowed per
week after 56 days from admission.
VT034
Service encounter has been disallowed as an inpatient comprehensive evaluation has previously
been approved and the patient has been readmitted within 10 days for the same or related condition.
you this day or subsequent day for the same or related condition.
previous 30 days.
days.
days for the same or related diagnosis.
previous 30 days.
VT040
Service encounter has been disallowed as supportive care is approved once every three days up to
and including the ninth day from admission and twice weekly thereafter.
VT041
Service encounter has been accepted at zero. The first postoperative clinic or office recheck should
be claimed, but will be approved at 0 units during the 90 days following major surgery.
VT042
Service encounter has been disallowed. When a visit and surgery are performed at the same service
encounter, only one is approved.
XPLANATORY
DESCRIPTION
VT035 Service encounter has been disallowed as a comprehensive visit has been previously approved to
VT036 Service encounter has been refused as a comprehensive visit has been approved to you in the
VT037 Service encounter has been refused as a previous visit has been claimed by you in the previous 30
VT038 Service encounter has been refused as you have been approved a consultation in the previous 30
VT039 Service encounter for initial limited visit has been refused as you have attended this patient in the
Page 69

EXPLANATORY CODES - 23
May 2011
E
CODE
VT043
Service encounter has been refused as a newborn care visit has previously been approved for this
day.
VT044
Service encounter has been refused as modifier DA value is inappropriate after 56 days from
admission.
VT045
Service encounter has been refused as this is an invalid service for age of patient.
VT046
Service encounter has been refused as health service code and modifier combination indicated is
invalid for your specialty.
VT047
Service encounter has been refused as the maximum of three services per patient per day has been
approved.
VT048
Service encounter has been disallowed as it is not payable in addition to the assistant fee.
VT049
Service encounter has been disallowed as it is included in the postoperative care of fractures.
VT050
Service encounter has been refused. Resubmit under the visit code using modifier for role of
detention in conjunction with all other required modifiers.
VT051
Service encounter has been refused. You have previously been approved a comprehensive
evaluation during this hospitalization.
VT052
Service encounter has been disallowed as a previous well baby visit has been approved for this three
month period.
encounter.
VT054
Service encounter has been disallowed as it is included in the fracture procedure performed this
same day.
VT055
Service encounter has been disallowed. Contact lens fitting includes follow up care for three months.
physician.
delivery.
VT058
Service encounter has been refused as the patient has not yet reached the age of 65.
immunizations at this same encounter.
surgery.
previously approved at this same service encounter.
VT062
Service encounter has been disallowed as you have previously been approved a delivery fee.
VT063
Service encounter has been disallowed as delivery did occur at the same facility.
VT064
Service encounter has been disallowed as a visit is included in the previously approved procedure.
this provider.
a previous visit by the same provider.
VT067
Service encounter has been disallowed. This service is only approved for general practitioners.
explaining the medical necessity of a comprehensive visit within 30 days of a previous visit.
XPLANATORY
DESCRIPTION
VT053 Service encounter has been disallowed as it is included in the surgery performed at this same
VT056 Service encounter has been disallowed as this service has been approved to you or another
VT057 Service encounter has been disallowed as attendance with patient during labour is included in the
VT059 Service encounter has been refused. Two previous service encounters have been approved for
VT060 Service encounter has been disallowed as a visit the same day as major surgery is included in the
VT061 Service encounter has been disallowed as it is included in a diagnostic and therapeutic procedure
VT065 Service encounter has been disallowed as 30 days has not elapsed since recipient was last seen by
VT066 Service encounter has been disallowed. Comprehensive visits cannot be approved within 30 days of
VT068 Service encounter has been refused. Resubmit as a limited visit or resubmit providing electronic text
Page 70

EXPLANATORY CODES - 24
May 2011
E
CODE
VT069
Service encounter has been disallowed based on the limitations applied to supportive care visits.
VT070
Service encounter has been disallowed as you have been approved a visit during the previous two
days.
VT071
Service encounter for supportive care has been disallowed as you have been approved two visits
within the previous two days.
VT072
Service encounter for supportive care has been disallowed as you have been approved two visits
within the previous three days.
VT073
Service encounter for supportive care has been disallowed as you have been approved two visits
within the previous four days.
VT074
Service encounter for supportive care has been disallowed as you have been approved two visits
within the previous five days.
VT075
Service encounter for supportive care has been disallowed as you have been approved two visits
within the previous six days.
VT076
Service encounter has been refused as modifier value OV65 does not agree with age of patient.
VT077
Service encounter has been refused. Resubmit under the same health service code using the
appropriate modifiers for the service provided.
VT078
Service encounter has been refused as patient’s age is inappropriate for this service.
previously been approved.
VT080
Service encounter has been refused as modifier DA value is inappropriate after 56 days from hospital
admission.
of life has been approved.
of life has been approved.
VT083
Service encounter has been refused as the patient is not insured for this service at this time.
VT084
Service encounter has been refused as the patient is not insured for this service at this time.
approved.
18 months.
diagnosis.
service for this diagnosis.
VT089
Service encounter has been refused as functional center is not indicated.
duration of the current treatment cycle.
VT091
Service encounter has been disallowed as this service is included in the CGA1 service that has
previously been approved.
WB001
Service encounter has been disallowed according to information provided by workers compensation
board.
approved.
XPLANATORY
DESCRIPTION
VT079 Service encounter has been refused as the maximum number of complex care visits for the year has
VT081 Service encounter has been refused as the maximum of 8 well baby care visits in the first 13 months
VT082 Service encounter has been refused as the maximum of 8 well baby care visits in the first 13 months
VT085 Service encounter has been refused as the maximum of 9 well baby care visits has previously been
VT086 Service encounter has been refused as only one well baby care visit is insured when patient age is
VT087 Service encounter has been refused as you have previously been approved this service for this
VT088 Service encounter has been refused as you or another provider have previously been approved this
VT090 Service encounter has been disallowed as electronic text is required to indicate the start date and
WB002 Service encounter has been disallowed as previous payment under WCB7 or WCB8 has been
Page 71

EXPLANATORY CODES - 25
May 2011
E
CODE
WB003
Service encounter has been approved at the WCB6 rate.
WB004
Service encounter has been adjusted based on a decision by workers' compensation board.
WB005
Service encounter has been disallowed as payment under WCB7 has been approved.
WB006
Service encounter has been disallowed as payment under WCB8 has been approved.
WB007
Service encounter has been refused as this form code has not been approved for implementation.
WB008
Service encounter has been refused re payment responsibility indicated.
WB009
Service encounter has been disallowed as previous payment under WCB9 or WCB10 has been
WB010
Service encounter has been refused as a consultation service has not been claimed for this date.
WB011
Service encounter has been refused as this type of visit is no longer payable under WCB. Please
resubmit using the appropriate physician assessment health service code.
WB012
Service encounter has been refused as you have previously claimed a physician assessment service
this day.
WB013
Service encounter has been refused as you have previously claimed a physician assessment service
this day.
WB014
Service encounter has been refused as you have previously been paid a special assessment service
for this date.
WB015
Service encounter has been refused as you have previously been paid an assessment service with
completion of form 8/10 this date.
WB016
Service encounter has been refused as a previous assessment has been claimed by you for this
date.
date.
date.
date.
date.
date.
WB022
Service encounter has been disallowed as a previous service for WCB has been claimed this day.
WB023
Service encounter has been disallowed as a previous visit fee for WCB has been claimed this day.
disability and form 8/10 is not applicable.
approved.
WB026
Service encounter has been refused as a previous payment under WCB9 has been approved.
XPLANATORY
DESCRIPTION
approved.
WB017 Service encounter has been refused as a previous assessment has been claimed by you for this
WB018 Service encounter has been refused as a previous chart summary has been claimed by you for this
WB019 Service encounter has been refused as a previous chart summary has been claimed by you for this
WB020 Service encounter has been refused as a previous case conference has been claimed by you for this
WB021 Service encounter has been refused as a previous case conference has been claimed by you for this
WB024 WCB has advised the adjustment of this claim to the appropriate visit fee as the client is on long term
WB025 Service encounter has been refused as previous payment under WCB11 or WCB12 has been
Page 72

May 2011
MISCELLANEOUS - 1
A
2008
M
31, 2009
A
2009
M
31, 2010
A
2010
M
31, 2011
A
2011
M
31, 2012
A
2012
M
31, 2013
A
2013
M
31, 2014
A
2014
M
31, 2015
MSU
(MSI)
AU
(MSI)
MSU
(WCB)
AU
(WCB)
MISCELLANEOUS
UNIT VALUES
Two unit values exist, an Anaesthetic Unit (AU) value used specifically for claiming anaesthetic services and a Medical
Service Unit (MSU) specifying the unit value of all other services. The chart below reflects the MSU and AU rate
increases scheduled for both MSI and WCB.
PRIL 1,
TO
ARCH
$2.23 $2.26 $2.28 $2.30 $2.32 $2.37 $2.42
$15.91 $16.15 $16.31 $16.47 $16.63 $16.96 $17.30
PRIL 1,
ARCH
TO
PRIL 1,
ARCH
TO
PRIL 1,
ARCH
TO
PRIL 1,
ARCH
TO
PRIL 1,
ARCH
TO
PRIL 1,
TO
ARCH
$2.48 $2.51 $2.53 $2.56 *
$17.68 $17.94 $18.12 $18.30 *
* *
* *
*Values have yet to be determined
For further information refer to th e Physician’s Manual Preamble and/or the Billing Instructions Manual.
HEALTH SERVICE CODES
03.08 - Consultation, described as Comprehensive
03.07 - Consultation, described as Limited
03.05 - Other Diagnostic Interview and Evaluation (includes critical care, ventilatory care, comprehensive care,
intensive care, neonatal intensive care).
03.04 - Diagnostic Interview and Evaluation, described as Comprehensive - In depth evaluation with complete history
and physical examination.
03.03 - Diagnostic Interview and Evaluation, described as Limited - Limited assessment with history of the presenting
problem.
Additional Services
MAAS EC Exceptional Circumstances ....................................................................................... EC
MAAS IC Independent Consideration ....................................................................................... IC
MAAS IF Interim Fee ................................................................................................................ IF
Community Services
DEFT C9999 Community Services Medical Assessment Form ...................................................... $25.00
Other Dental Operations NEC
MAAS 36.99A Assistant for dental surgery performed by a dentist
(RO=DTAS) ............................................................................................................... IC
Workers' Compensation Board
DEFT WCB2 W CB Office Visit Examination for Pneumoconiosis .................................................. 20.5 units
DEFT WCB11 Physician assessment service. Combined office visit and
completion of Form 8/10 .......................................................................................... $123.40
Page 73

May 2011
MISCELLANEOUS - 2
DEFT WCB12 EPS physician assessment Service.
Combined office visit and completion of Form 8/10 .................................................. $153.55
DEFT WCB13 Chart Summaries / Written Reports. Detailed reports billed in 15 minute intervals
- plus multiples, if applicable ..................................................................................... $37.50 per 15 min
DEFT WCB14 Chart Summaries / Written Reports. Detailed reports billed for the
total number of pages - plus multiples, if applicable .................................................. $125 per page
DEFT WCB15 Case Conferencing and Teleconferencing (Treating Physician)
Conferencing billed by the Treating Physician
- plus multiples, if applicable ..................................................................................... $37.50 per 15 min
DEFT WCB16 Case Conferencing and Teleconferencing (EPS Physician)
Conferencing billed by an EPS physician - plus multiples, if applicable .................... $50 per 15 min
DEFT WCB17 Photocopying of charts. Photocopying of chart notes ............................................. $25.00 *
* Note: $25.00 will be paid through MSI; if the physician negotiates a different
amount then they must invoice the entire service directly to WCB.
DEFT WCB18 Special Assessment Service (WCB Authorization Only).
Special assessment service requiring WCB approval prior to use ............................ $61.70
DEFT WCB19 Special Reporting Service (WCB Authorization Only).
Special reporting service requiring WCB approval prior to use ................................. $61.70
DEFT WCB98 Second opinion consultation specifically requested by WCB regarding
back surgery .............................................................................................................. 64.2 units
The following are applicable to the specialty of Orthopaedics only:
DEFT WCB9 W CB completion of Form 9 in conjunction with an expedited non-emergency
Orthopaedic Consultation
RF=REFD, SP=ORTH ............................................................................................... 30.43 units
DEFT WCB10 WCB completion of Form 10 in conjunction with an expedited non-emergency
Orthopaedic Major Surgical Procedure
SP=ORTH ................................................................................................................. IC
Page 74

May 2011
MISCELLANEOUS - 3
PROLONGED CONSULTATIONS
A Prolonged Consultation may be applied to cases where the consultation extends beyond one hour for Comprehensive
Consultations and a half-hour for Repeat Consultations. A Prolonged Consultation cannot be claimed with a Limited
Consultation and is not to be confused with active treatment associated with detention. Prolonged Consultations are paid
in 15-minute time intervals or portions thereof. This information is entered on your service encounter using the Multiples
indicator. For further details refer to the Billing Instructions Manual Chapter 5.
A Prolonged Consultation may be claimed by the following specialities only:
Anaesthesia .....................15 units per 15 minutes
Internal Medicine .............13.5 units per 15 minutes
Neurology ........................13.5 units per 15 minutes
Physical Medicine ............13.5 units per 15 minutes
Paediatrics .......................16.3 units per 15 minutes
Psychiatry ........................18.22 units per 15 minutes
MULTIPLES
The Multiples indicator (MU) indicates the number of services performed (e.g., number of lesions), the length of time
(e.g., 15 minute time intervals, detention, counselling, etc.) or the percentage of body (burns) or surface area (e.g.,
square inches). For further details refer to the Billing Instructions Manual Chapter 4.
DETENTION
Medical detention occurs when a service provider’s time is given exclusively to one patient for active treatment and/or
monitoring of that patient at the sacrifice of all other work. Detention time is not payable when provided in the office.
Detention commences 30 minutes after the provider is first in attendance and may be claimed in 15 minute increments
thereafter. The first 30 minutes is the appropriate visit fee. When claimed with a Comprehensive or a Limited
Consultation, detention time commences after 1 hour. The fee for detention is 12.5 units per 15 minutes. The detention
modifier RO=DETE must be indicated on the service encounter. For further details refer to the Preamble.
PREMIUM FEES
Premium fees may be claimed for certain services provided on an emergency basis during designated time periods. An
emergency basis is defined as a service which must be performed without delay because of the medical
condition of the patient.
Premium Fees are paid at 35% (US=PREM) or 50% (US=PR50) of the appropriate service code but at not less than 18
units for patient specific services and not less than 9 units for non-patient specific services. For further details refer to the
Preamble.
OUTDATED SERVICE ENCOUNTERS
Service encounters submitted beyond 90 days from date of service shall not be payable unless MSI is of the opinion the
delay is justified. Resubmission of refused service encounters must be within 185 days of the date of service. The only
exception to this policy will be through special consideration in extenuating circumstances by writing to the Manager of
MSI Programs.
Note: WCB and facility based non patient specific service encounters follow the same ruling.
OUTDATED RECIPROCAL SERVICE ENCOUNTERS
Service encounters submitted beyond one year from date of service shall not be payable.
TERMINATION DATE
The expiry date of a Health Service Code tariff temporarily assigned to a new procedure during the process of adding it
to the Schedule of Benefits. For further details refer to the Preamble under item Interim Fees.
Page 75

May 2011
MISCELLANEOUS - 4
SPECIALTY ABBREVIATIONS
ANAE - Anaesthesia
ANPA - Anatomical Pathology
CARD - Cardiology
CASG - Cardiovascular/Thoracic Surgery
CLIA - Clinical Immunology & Allergy
COMD - Community Medicine
DENT - Dental Practitioner
DERM - Dermatology
DIRD - Diagnostic Radiology
EMMD - Emergency Medicine
ENDO - Endodontics
ENME - Endocrinology & Metabolism
GAST - Gastroenterology
GEMD - Geriatric Medicine
GENP - General Practitioner
GNSG - General Surgery
HAGY - Haematology
HAPA - Haematological Pathology
HUGE - Human Genetics
INDI - Infectious Diseases
INMD - Internal Medicine
MDON - Medical Oncology
MEBI - Medical Biochemistry
MEGE - Medical Genetics
MEMI - Medical Microbiology
NCMD - Nuclear Medicine
NEPA - Neuropathology
CATEGORY ABBREVIATIONS
ADON - Add On
ALPM - Alternate Payments
ANAE - Anaesthesia
BOGR - Bone Graft
CASP - Casts and Splints
COCR - Complete Care
CONS - Consultation
CRCR - Intensive Care / Critical Care
DEFT - Default
DISL - Dislocation
MAAS - Manual Assess
NEPE - Neurology Paediatric
NEPH - Nephrology
NEUR - Neurology
NUSG - Neurosurgery
OBGY - Obstetrics & Gynaecology
ODON - Orthodontics
OPHT - Ophthalmology
OPTO - Optometry
ORAL - Oral Surgery
ORTH - Orthopaedic Surgery
OTOL - Otolaryngology
PATH - General Pathology
PEDI - Paediatrics
PEDO - Pedodontics
PERI - Periodontics
PHMD - Physical Medicine & Rehabiltation
PLAS - Plastic Surgery
PROS - Prosthodontics
PSYC - Psychiatry
RADI - Diagnosti c & Therapeutic Radiology
RDON - Radiation Oncology
RHEU - Rheumatology
RSMD - Respiratory Medicine
THSG - Thoracic Surgery
UROL - Urology
VASG - Vascular Surgery
MAFR - Major Fracture
MASG - Major Surg ery
MIFR - Minor Fracture
MISG - Minor Surgery
OBST - Obstetrical
OPTO - Optometry
PMNO - Pain Management (non obstetrical)
PSYC - Psychiatric Care
VADT - Visit Allowed Diagnostic & Therapeutic Procedure
VEDT - Visit Excluded Diagnostic & Therapeutic Procedure
VIST - Visit
Page 76

MISCELLANEOUS -5
TYPE
VALUE
DESCRIPTION
AG
ADUT
Person 16 years and older
AG
CH04
Child up to four years
AG
CH07
Child up to seven years
AG
CH12
Child up to twelve years
AG
CH16
Child up to sixteen years
AG
NWBN
Newborn (infant up to and including ten days)
AG
OV65
Person 65 years and older
AG
PR07
Person 7 years and older
AN
DFED
Delivery following epidural introduction
AN
EPID
Epidural anaesthetic
AN
GENL
General anaesthetic
AN
LABR
Labor
AN
LOCL
Local anaesthetic
AN
PNCT
Pain control
AN
REGL
Regional
AP
ABDO
Abdominal
AP
ANTE
Anterior
AP
CERV
Cervical
AP
CLSD
Closed procedure
AP
DRSL
Dorsal
AP
EXTR
External
AP
INPR
Intra peritoneal
AP
LMBR
Lumbar
AP
OPEN
Open procedure
AP
PERC
Percutaneous approach
AP
PERI
Perineal
AP
POST
Posterior
AP
SUBC
Subcutaneous
AP
THOR
Thoracic
AP
TRUR
Transurethral
AP
VAGN
Vaginal
AP
WPLO
With pleura open
CO
BPU5
By-pass pump - patient under 5000 grams
CO
CHYO
Controlled hypotension
MODIFIER DESCRIPTIONS
The following is a list of all available modifiers. In order to be paid the correct value for the service rendered, the
appropriate modifiers and/or modifier combinations must be submitted. This Physician’s Manual provides a list of the
base unit values for the Health Service Codes. The complete list of all unit values and modifiers or modifier combinations
is also available on your computer system.
AP WPLC With pleura closed
May 2011
Page 77

MISCELLANEOUS -6
T
V
D
CO
CRBY
Cardiac by-pass with pump
CO
HPTH
Hypothermia
CO
INFE
Infant resuscitation after delivery
CO
PACM
Pacemaker monitoring
CO
UN5K
Patient under 5000 grams
CT
PROF
Professional component
CT
TECH
Technical component
DA
DALY
Daily rate applies
DA
RGE1
Date range defining Saturday, Sunday and Holidays
DA
RGE2
Sundays and Holidays
DA
WKLY
Weekly rate applies
FN
DTOX
Detox Centre
FN
EMCC
Emergency Care Centre
FN
INCU
Intensive care
FN
INPT
Inpatient
FN
NICU
Neonatal Intensive Care
FN
OTPT
Outpatient
IN
CC01
Critical care first day
IN
CC10
Critical care day 2 to 10 inclusive
IN
CC11
Critical care 11th day onward
IN
CP01
Comprehensive care 1st day
IN
CP10
Comprehensive care day 2 to 10 inclusive
IN
CP11
Comprehensive care 11th day onward
IN
INCR
Intensive care per day
IN
INHD
Intensive care per half day
IN
INPH
Intensive care per hour
IN
NIC1
Neonatal intensive care day 1
IN
NIC4
Neonatal intensive care day 2 to 4 inclusive
IN
NIC5
Neonatal intensive care day 5 onward
IN
VC01
Ventilatory care first day
IN
VC10
Ventilatory care day 2 to 10 inclusive
IN
VC11
Ventilatory care 11th day onward
LO
CCNT
Correctional Centre
LO
HMHC
Acute Home Care
LO
HOME
Home
LO
HOSP
Hospital
LO
NRHM
Nursing Home
LO
OFFC
Office
LO
OTHR
Other
YPE
ALUE
ESCRIPTION
May 2011
Page 78

MISCELLANEOUS -7
T
V
D
LV
LV50
The second or subsequent procedure done through the same approach
LV
LV65
Indicates a procedure done through separate approach
ME
ABDM
Abdominal
ME
CMST
Composite procedure
ME
COMP
Complicated procedure
ME
CRYO
Cryotherapy treatment by freezing
ME
CURT
Curettage scraping
ME
ELEC
Electrocautery removal by burning
ME
EXRM
Removal by excision
ME
EXTN
External
ME
FTSG
First stage
ME
INTN
Internal
ME
INTR
Intrauterine
ME
LAPA
Procedure performed by laparotomy
ME
LASR
Procedure performed using laser technique
ME
MAJO
Extensive complication
ME
MINO
Complexity minor or limited
ME
RADI
Radical extensive procedure
ME
SCOP
Procedure performed through scope
ME
SDSG
Second stage
ME
SIMP
Simple procedure
ME
TELE
Telemedicine Conference
ME
VAGN
Vaginal
OL
HMHC
OPD visit from Acute Home Care
OL
HOME
Admission from home to Acute Home Care
OL
INPT
Admission from inpatient to Acute Home Care
OL
OFFC
Admission from office to Acute Home Care
OL
OTPT
Admission from OPD to Acute Home Care
OL
USEM
Admission from unscheduled emergency call to Acute Home Care
PO
COML
Entire procedure performed
PO
ONTW
One to twenty percent of body
PO
PART
Partial procedure performed
PO
RADI
Procedure to the fullest extent
PO
SBTL
Subtotal (less than complete)
PO
SEGM
Segmental part of the body
PO
TOTF
Twenty-one to thirty-five percent of body
PO
TSOV
Thirty-six percent of body and over
PO
WEGE
Wedge part of the segment
PT
CDDR
Cadaver donor
PT
DONR
Donor
YPE
ALUE
ESCRIPTION
May 2011
Page 79

MISCELLANEOUS -8
T
V
D
PT
EXPT
Additional patient seen at same location
PT
FTPT
First patient seen
PT
LIDR
Live donor
PT
PRBK
Patient referred back
PT
PRTO
Patient referred to Ophthalmologist
PT
RECP
Recipient
RF
REFD
Referring doctor
RG
BOTH
Bilateral procedure
RG
FEMR
Femur head and neck
RG
LEFT
Procedure performed on the left side of the body
RG
RIGT
Procedure performed on the right side of the body
RO
ABAS
Abdominal assistant
RO
ABDM
Abdominal surgeon two team approach
RO
ABDO
Abdominal surgeon
RO
ADAC
Adacel (diphtheria, pertussis and tetanus)
RO
ANAE
Anaesthetist
RO
ANCO
Anticoagulant supervision per month
RO
ANTL
Antenatal
RO
BOTR
Boostrix (diphtheria, pertussis and tetanus)
RO
CAPT
Comprehensive reassessment of a cancer patient
RO
CCDT
Continuing care and detention
RO
CCDX
Continuing care in conjunction with attending and describing a differential diagnosis
RO
CHDT
Closed head injury with detention
RO
CLHD
Closed head injury
RO
CNTC
Continuing care
RO
CRTC
Palliative care medicine chart review (and/or telephone call, fax or email initiated by a
health care professional)
RO
DBSU
Double set up
RO
DETE
Detention
RO
DIRC
Directive care
RO
DRDT
Directive care and detention
RO
DTAS
Dental assistant
RO
DUTY
Duty doctor
RO
DYDT
Duty doctor and detention
RO
EXEM
Injection when potential for allergic reaction to ingredient exists
RO
FPHN
First physician
RO
HMDY
Home dialysis
RO
HMTE
Acute or chronic home care, medical chart review, telephone calls, fax or email
RO
HPVV
HPV Vaccine
RO
INCH
Physician in hyperbaric chamber
YPE
ALUE
ESCRIPTION
May 2011
Page 80

MISCELLANEOUS -9
T
V
D
RO
INFL
Injection for various strains of influenza
RO
INPR
Interpretation and procedure
RO
INTP
Interpretation
RO
MENC
Meningococcal type C conjugate vaccine
RO
MMAR
Injection for measles, mumps and rubella
RO
NBCR
Newborn care
RO
OBDA
Obstetrical delivery assist
RO
OTCH
Physician out of hyperbaric chamber
RO
PAMO
Pathology materials only
RO
PAND
Injection for pandemic vaccination
RO
PCSV
Palliative care support visit
RO
PEAS
Perineal assistant
RO
PENT
Injection for diphtheria, pertussis, tetanus, poliomyelitis and haemophilus influenza type B
RO
PNEC
Pneumococcal conjugate vaccine (Prevnar)
RO
PNEU
Injection for pneumococcal pneumonia, bacteraemia and meningitis
RO
PRIN
Perineal surgeon two team approach
RO
PROC
Procedure
RO
PTNT
Post natal
RO
PTPP
Post partum
RO
QUAD
Injection for diphtheria, pertussis, tetanus and poliomyelitis
RO
RESC
Resuscitation
RO
RNDT
Resuscitation of newborn with detention
RO
SNAS
Second assistant
RO
SPCR
Supportive care
RO
SPHN
Second physician
RO
SPIN
Supervision and interpretation
RO
SRAS
Surgical assistant
RO
SSAN
Second simultaneous anaesthetist
RO
STBY
Standby
RO
SUPV
Supervision
RO
TALR
Telephone advice and medical chart review of liver transplant recipient
RO
TCCP
Telephone advice and medical chart review of a cancer patient by the Oncologist
RO
TEDI
Injection for tetanus and diphtheria (adults)
RO
TRPL
Treatment planning
RO
TRTL
Trauma team leader
RO
UPCK
Visit pacemaker check
RO
VARI
Injection for varicella
RO
VGSG
Vaginal surgeon
RO
WBCR
Well baby care
YPE
ALUE
ESCRIPTION
May 2011
Page 81

MISCELLANEOUS -10
T
V
D
RP
CON2
Second chronic disease managed
RP
INTL
Initial
RP
REPT
A repeat of a service
RP
REVS
Revision
RP
SUBS
Subsequent similar service
SE
FEML
Female
SE
MALE
Male
SP
ANAE
Anaesthetist
SP
ANPA
Anatomical Pathology
SP
CARD
Cardiology
SP
CASG
Cardiovascular/Thoracic surgery
SP
CLIA
Clinical Immunology and Allergy
SP
COMD
Community Medicine
SP
DENT
Dental General Practitioner
SP
DERM
Dermatology
SP
DIRD
Diagnostic Radiology
SP
EMMD
Emergency Medicine
SP
ENDO
Endodontics
SP
ENME
Endocrinology and Metabolism
SP
GAST
Gastroenterology
SP
GEMD
Geriatric Medicine
SP
GENP
General Practitioner
SP
GNSG
General Surgery
SP
HAGY
Haematology
SP
HAPA
Haematological Pathology
SP
HUGE
Human Genetics
SP
INDI
Infectious Diseases
SP
INMD
Internal Medicine
SP
MDON
Medical Oncology
SP
MEBI
Medical Biochemistry
SP
MEGE
Medical Genetics
SP
MEMI
Medical Microbiology
SP
NCMD
Nuclear Medicine
SP
NEPA
Neuropathology
SP
NEPE
Neurology Paediatric
SP
NEPH
Nephrology
SP
NEUR
Neurology
SP
NUSG
Neurosurgery
SP
OBGY
Obstetrics and Gynaecology
YPE
ALUE
ESCRIPTION
May 2011
Page 82

MISCELLANEOUS -11
T
V
D
SP
ODON
Orthodontics
SP
OPHT
Ophthalmology
SP
OPTO
Optometry
SP
ORAL
Oral Surgery
SP
ORTH
Orthopaedic Surgery
SP
OTOL
Otolaryngology
SP
PATH
General Pathology
SP
PEDI
Paediatrics
SP
PEDO
Pedodontics
SP
PERI
Periodontics
SP
PHMD
Physical Medicine and Rehabilitation
SP
PLAS
Plastic Surgery
SP
PROS
Prosthodontics
SP
PRPR
Prosthetic Provider
SP
PSYC
Psychiatry
SP
RADI
Diagnostic and Therapeutic Radiology
SP
RDON
Radiation Oncology
SP
RHEU
Rheumatology
SP
RSMD
Respiratory Medicine
SP
THSG
Thoracic Surgery
SP
UROL
Urology
SP
VASG
Vascular Surgery
TI
AMNN
0801-1200
TI
ETMD
2001-2359
TI
EVNT
1701-2000
TI
GPEW
GP Evening & Weekend Office Visit Incentive (M-F 1800-2200 or S/S 0900-1700)
TI
MDNT
0000-0800
TI
NNEV
1201-1700
US
PREM
Premium fee of 35 percent
US
PR50
Premiu m fee of 50 percent
US
SCHD
Planned / Scheduled outpatient visit (0800-2000)
US
UCHH
Urgent call back by acute home care staff
US
UIOH
Urgent visit interrupting normal office hours
US
UNOF
Urgent visit not interrupting office hours
YPE
ALUE
ESCRIPTION
May 2011
Page 83

MISCELLANEOUS -12
SERVICE CODE
DESCRIPTION
22.5C
Plastic repair (without skin graft) eyelid - no prior appro val required if condition is
trauma related
30.4
Surgical correction of prominent ear - congenital (18 years and older)
30.61A
External ear otoplasty, exclusive of simple lacerations (minor)
30.61A
External ear otoplasty, exclusive of simple lacerations (major)
30.61B
Total reconstruction of ear (Pinna) (18 years and older)
33.74
Rhinoplasty with bone or cartilage graft (entire)
33.74
Rhinoplasty with bone or cartilage graft (partial)
33.76B
Complete rhinoplasty with submucous resection without skin grafting
33.76D
Rhinoplasty - removal of hump
33.76E
Scalping rhinoplasty - two stages
33.79B
Reconstruction of nasal tip, ala and columella
56.93
Gastroplasty or gastric bypass for morbid obesity
97.31A*
Unilateral mammoplasty with nipple transplantation
97.31C
Unilateral functional pedicled breast reduction (unilateral)
97.32*
Bilateral reduction mammoplasty
97.32B
Bilateral functional pedicled breast reduction
97.43*
Unilateral augmentation mammoplasty by implant or graft
97.44*
Bilateral augmentation mammoplasty by implant or graft
97.6B*
Breast reconstruction by myocutaneous flap and breast prosthesis
97.6C*
Breast reconstruction using rectus abdominis flap, including reconstruction of the
rectus sheath as required.
97.6D*
Deep inferior epigastric perforator (DIEP) free flap breast reconstruction
97.75A*
Breast reconstruction by myocutaneous flap and prosthesis
97.77*
Other repair or reconstruction of nipple
97.94A*
Removal of breast prosthesis
97.94B*
Removal of breast prosthesis with capsulectomy
98.93A
Dermabrasion - full face
98.93B
Dermabrasion - less than 1/4 of face
98.93C
Dermabrasion of single area face (e.g., trauma scar)
98.93D
Dermabrasion between 1/4 and 1/2 of face
EC
Lipectomy (single reduction - plastic operation)
PREAUTHORIZATION SERVICE ENCOUNTE RS
Service encounters submitted for the following procedures must have prior approval and a valid referral in order to be
paid. Refer to the Billing Instructions Manual, Chapter 5 for information on submitting prior approval codes.
* prior approval unless procedure is post-mastectomy for malignant or pre-malignant condition
HEALTH
May 2011
Page 84

CODE
GROUP
DESCRIPTION
VALUE
1
Other
Interpretation of submitted films
6.25
2
Other
Fluoroscopy in O.R.
3.13
3
Other
Conventional tomography
9.38
5
H&N
Skull - routine views
4.40
6
H&N
Temporomandibular joints
4.34
7
H&N
Internal auditory meati
4.34
8
H&N
Sella turcica
4.34
9
H&N
Optic foramina
4.34
11
H&N
Mastoids - added view
4.34
12
H&N
Eye for foreign body
4.34
15
H&N
Facial bones
4.40
20
H&N
Mandible
3.31
25
H&N
Nasal bones
3.31
30
H&N
Sinuses - paranasal
3.88
35
H&N
Salivary gland region
3.31
45
H&N
Panorex (teeth - full set)
4.97
50
H&N
Arthrogram
20.76
55
H&N
Dacrocystogram
5.53
60
H&N
Sialogram
9.38
70
H&N
Speech study
44.24
105
Bone
Cervical spine
5.19
110
Bone
Thoracic spine
3.31
115
Bone
Lumbar spine
5.19
120
Bone
Sacrum / coccyx
3.31
125
Bone
Scoliosis series
8.85
126
Bone
Scoliosis with stress
11.07
129
Bone
Metastatic series (5)
9.12
130
Bone
Metabolic bone survey
9.12
131
Bone
All long bones added to 129
2.28
140
Mylo
Discogram
11.07
150
Mylo
Lumbar myelogram
18.75
151
Mylo
Complete myelogram
28.14
152
Mylo
Cervical injection myelogram
18.75
185
Other
Fetal Study
3.31
205
Bone
Shoulder
3.41
210
Bone
Scapula
3.41
215
Bone
A.C. joints with and without weights
3.41
RADIOLOGY NON-PATIENT - SPECIFIC BULK BILLING FEES
UNIT
May 2011 RADIOLOGY NON-PATIENT-SPECIFIC BULK BIL LING FEES Page 1
Page 85

CODE
GROUP
DESCRIPTION
UNIT
VALUE
220
Bone
Clavicle
3.41
221
Bone
Bone age determination
4.53
223
Bone
Scaphoid
3.41
224
Bone
Humerus
3.41
225
Bone
Elbow
3.41
226
Bone
Wrist
3.41
227
Bone
Forearm
3.41
228
Bone
Hand
3.41
229
Bone
Finger
1.71
230
Bone
Arthrogram shoulder
20.76
305
Bone
Hip
3.41
310
Bone
Pelvis
3.31
315
Bone
Pelvis and hips
3.99
320
Bone
Sacroiliac joints
3.31
321
Bone
Patella
3.41
322
Bone
Foot
3.41
323
Bone
Ankle
3.41
324
Bone
Knee
3.41
325
Bone
Calcaneus
3.41
326
Bone
Tibia and fibula
3.41
327
Bone
Toe
1.71
328
Bone
Feet - weight bearing
6.64
335
Bone
Femur
3.41
340
Bone
Orthoroentgenogram (leg length measurement)
2.58
350
Bone
Arthrogram hip
20.76
351
Bone
Arthrogram knee
20.76
403
Other
Fluoroscopy 10 minutes
12.50
404
Chest
Single view
3.13
405
Chest
Multiple views
5.13
425
Chest
Ribs - each side
2.90
435
Chest
Sternum
3.31
439
Bone
Dual photon densitometry
11.73
440
Bone
Sternoclavicular joints
3.41
445
H&N
Neck - for soft tissue
3.31
470
Chest
Bronchogram unilateral
11.07
484
Mammo
Mammography screening bilateral
5.09
485
Mammo
Mammography unilateral
7.19
486
Mammo
Breast cystography
6.63
May 2011 RADIOLOGY NON-PATIENT-SPECIFIC BULK BIL LING FEES Page 2
Page 86

CODE
GROUP
DESCRIPTION
UNIT
VALUE
490
Mammo
Mammography diagnostic bilateral
14.07
495
Mammo
Needle localization
34.39
500
Mammo
Galactography
6.63
505
Mammo
Stereotactic localization
19.29
510
Mammo
Surgical specimen radiography
3.82
605
Abdomen
Survey film
3.13
610
Abdomen
Multiple films
3.88
620
G.I.
Esophagus
14.62
625
G.I.
Upper G.I. series
18.69
630
G.I.
Upper G.I. paediatric
28.05
635
G.I.
Small bowel study
9.67
640
G.I.
Enteroclysis
26.57
650
G.I.
Colon - barium only
14.91
655
G.I.
Colon paediatric - single
22.37
660
G.I.
Colon - double contrast
19.92
666
G.I.
Defaecography
26.57
670
G.I.
Cholecystogram
4.97
690
G.I.
T-tube cholangiogram
6.63
691
G.I.
Operative cholangiogram
4.66
695
G.I.
ERCP
6.63
709
G.I.
Herniography
9.38
710
G.I.
Fistula/sinus with contrast
4.40
745
G.I.
Percutaneous transhepatic cholangiogram
6.63
815
G.I.
Intravenous urogram (IVP)
14.53
823
G.U.
Retrograde pyelogram
4.53
830
G.U.
Voiding cystourethrogram
11.07
835
G.U.
Cystogram paediatric
18.75
840
G.U.
Loopogram
4.40
845
G.U.
Retrograde urethrogram
4.53
846
G.U.
Cavernosogram
4.40
850
G.U.
Antegrade (t-tube) pyelogram
4.53
865
G.U.
Renal cystogram
6.63
885
G.U.
Vasogram
4.40
895
G.U.
Hysterosalpingogram
5.53
910
G.U.
Pelvimetry
6.63
1001
Vascular
Venous DSA - abnormal or renal
35.52
1002
Vascular
Venous DSA - aortic arch
39.58
1003
Vascular
Pulmonary angiogram bilateral
93.79
May 2011 RADIOLOGY NON-PATIENT-SPECIFIC BULK BIL LING FEES Page 3
Page 87

CODE
GROUP
DESCRIPTION
UNIT
VALUE
1004
Vascular
Pulmonary angiogram unilateral
62.53
1006
Vascular
Unilateral peripheral arteriogram
22.14
1007
Vascular
Bilateral peripheral arteriogram
33.21
1008
Vascular
Aortography (abdominal)
44.21
1009
Vascular
Visceral selective arteriogram
44.21
1010
Vascular
Venogram extremity
25.01
1011
Vascular
Venocavogram selective
22.14
1012
Vascular
Visceral venogram
22.14
1013
Vascular
Spinal artery selective
22.14
1014
Vascular
Bronchial artery selective
44.21
1015
Vascular
Lymphangiogram
44.21
1016
Vascular
Arch aortogram
44.21
1017
Vascular
Spleenoportogram
53.90
1018
Vascular
Intraoperative angiogram
43.77
1021
Vascular
Common carotid bilateral
55.83
1022
Vascular
Internal carotid bilateral
55.83
1023
Vascular
External carotid bilateral
55.83
1024
Vascular
Vertebral bilateral
55.83
1026
Vascular
Common carotid unilateral
30.45
1027
Vascular
Internal carotid unilateral
30.45
1028
Vascular
External carotid unilateral
30.45
1029
Vascular
Vertebral unilateral
30.45
1056
Cardiac
Coronary arteries
50.75
1057
Cardiac
Coronary arteries with ergot
25.38
1058
Cardiac
Coronary artery grafts
50.75
1059
Cardiac
P.T.C.A.
50.75
1061
Cardiac
Right ventriculogram
25.38
1062
Cardiac
Left ventriculogram
25.38
1063
Cardiac
Cardiac panning < 45 min.
60.90
1064
Cardiac
Cardiac panning > 45min.
121.81
1071
Cardiac
Aortic root (cardiac)
25.38
1105
C.T.
CT head without contrast
42.33
1111
C.T.
CT head with contrast
42.33
1115
C.T.
CT head without and with contrast
53.27
1121
C.T.
CT neck without contrast
42.33
1125
C.T.
CT neck with contrast
42.33
1130
C.T.
CT neck without and with contrast
53.27
1135
C.T.
CT thorax without contrast
42.33
May 2011 RADIOLOGY NON-PATIENT-SPECIFIC BULK BIL LING FEES Page 4
Page 88

CODE
GROUP
DESCRIPTION
UNIT
VALUE
1141
C.T.
CT thorax with contrast
42.33
1145
C.T.
CT thorax without and with contrast
53.27
1150
C.T.
CT abdomen without contrast
42.33
1155
C.T.
CT abdomen with contrast
42.33
1160
C.T.
CT abdomen without and with contrast
53.27
1162
C.T.
CT extremities without contrast
42.33
1163
C.T.
CT extremities with contrast
42.33
1164
C.T.
CT extremities without and with contrast
53.27
1165
C.T.
CT pelvis without contrast
42.33
1166
C.T.
CT pelvis with contrast
42.33
1167
C.T.
CT pelvis without and with contrast
53.27
1169
C.T.
CT spine without contrast
42.33
1170
C.T.
CT spine with contrast
42.33
1172
C.T.
CT spine without and with contrast
53.27
1173
C.T.
Densitometry CT
9.07
1180
C.T.
3D reconstruction
12.16
1186
C.T.
CT head special without contrast
42.33
1187
C.T.
CT head special with contrast
42.33
1188
C.T.
CT head special without and with contrast
53.27
1205
Ultrasound
Abdomen general
25.39
1206
Ultrasound
Spine
25.39
1211
Ultrasound
Aorta
12.50
1212
Ultrasound
Appendix
18.75
1213
Ultrasound
Kidneys
18.75
1214
Ultrasound
Pylorus
18.75
1220
Ultrasound
Pelvis, male or female (GYN)
18.75
1225
Ultrasound
Endovaginal
26.95
1226
Ultrasound
Endovaginal with pelvic
38.70
1231
Ultrasound
Endorectal
25.39
1245
Ultrasound
Obstetrical
27.51
1246
Ultrasound
Obstetrical, recheck
12.50
1250
Ultrasound
Biophysical profile
4.84
1255
Ultrasound
Obs. Multiple - (add on)
20.04
1256
Ultrasound
Obs. Multiple - recheck (add on)
6.25
1264
Ultrasound
Cerebral
33.49
1265
Ultrasound
Thyroid/parathyroid (neck)
18.75
1270
Ultrasound
Real time (eye)
38.70
1271
Ultrasound
Axial length measurement
25.44
May 2011 RADIOLOGY NON-PATIENT-SPECIFIC BULK BIL LING FEES Page 5
Page 89

CODE
GROUP
DESCRIPTION
UNIT
VALUE
1275
Ultrasound
Scrotum
25.45
1280
Ultrasound
Shoulder
18.75
1285
Ultrasound
Hip
18.75
1295
Ultrasound
Breast, single
12.50
1296
Ultrasound
Chest
18.75
1297
Ultrasound
Popliteal fossa
12.50
1298
Ultrasound
Subcutaneous mass
12.50
1306
Ultrasound
Intraoperative U/S
47.56
1307
Ultrasound
Portable - M.D. in attendance
18.75
1309
Ultrasound
Fetal echo
78.16
1310
Ultrasound
Two dimensional cardiac
47.56
1311
Ultrasound
M-Mode cardiac
25.44
1312
Ultrasound
Doppler - quantitative, cardiac
30.45
1313
Ultrasound
Doppler - qualitative, cardiac
15.23
1335
Ultrasound
Doppler abdominal blood vessels
33.49
1340
Ultrasound
Carotid doppler
33.49
1345
Ultrasound
Doppler - extremities
18.75
1405
M.R.I.
Cranial multisection SE
40.97
1406
M.R.I.
Cranial multisection IR
25.76
1407
M.R.I.
Cranial repeat, sequence
19.91
1409
M.R.I.
Ent multisection SE
40.97
1411
M.R.I.
Ent multisection IR
25.76
1412
M.R.I.
Ent repeat, sequence
19.91
1415
M.R.I.
Thorax multisection SE
46.83
1416
M.R.I.
Thorax multisection IR
40.97
1417
M.R.I.
Thorax repeat, sequence
23.42
1420
M.R.I.
Abdomen multisection SE
46.83
1421
M.R.I.
Abdomen multisection IR
40.97
1422
M.R.I.
Abdomen repeat, sequence
23.42
1425
M.R.I.
Pelvis multisection SE
46.83
1426
M.R.I.
Pelvis multisection IR
40.97
1427
M.R.I.
Pelvis repeat sequence
23.42
1430
M.R.I.
Extremities multisection SE
40.97
1431
M.R.I.
Extremities multisection IR
25.76
1432
M.R.I.
Extremities repeat, sequence
19.91
1440
M.R.I.
Spine (one seq.) multisection SE
37.47
1441
M.R.I.
Spine (one seq.) multisection IR
24.58
1442
M.R.I.
Spine (one seq.) repeat, sequence
18.73
May 2011 RADIOLOGY NON-PATIENT-SPECIFIC BULK BIL LING FEES Page 6
Page 90

CODE
GROUP
DESCRIPTION
UNIT
VALUE
1445
M.R.I.
Spine (two adjoining) multisection SE
44.50
1446
M.R.I.
Spine (two adjoining) multisection IR
37.47
1447
M.R.I.
Spine (two adjoining) repeat sequence
22.25
1450
M.R.I.
Spine (two not add.) multisection SE
66.74
1451
M.R.I.
Spine (two not add.) multisection IR
37.47
1452
M.R.I.
Spine (two not add.) repeat sequence
32.78
1453
M.R.I.
Add 30% for gating
14.05
1776
Nuc. Med.
Labelled WBC
41.04
1777
Nuc. Med.
Gallium (one area)
28.14
1778
Nuc. Med.
Gallium (multiple areas)
35.08
1790
Nuc. Med.
Vascular study (flow) add on
11.73
1810
Nuc. Med.
Brain scan
11.73
1811
Nuc. Med.
Brain perfusion
46.89
1812
Nuc. Med.
CSF study (cisternogram)
35.18
1813
Nuc. Med.
Shunt function study
46.89
1814
Nuc. Med.
Radionuclide arthrogram
35.18
1816
Nuc. Med.
Bone scan - one area
23.45
1817
Nuc. Med.
Bone scan - multiple areas
28.14
1818
Nuc. Med.
Bone marrow - one area
23.45
1819
Nuc. Med.
Marrow scan - multiple areas
28.14
1820
Nuc. Med.
Bone density
11.73
1830
Nuc. Med.
Lung ventilation scan
23.45
1835
Nuc. Med.
Lung scan perfusion
23.45
1840
Nuc. Med.
Liver and spleen
18.75
1843
Nuc. Med.
Haemangioma (RBC)
28.14
1845
Nuc. Med.
Spleen scan (RBC)
18.75
1850
Nuc. Med.
Hepatobiliary
23.45
1853
Nuc. Med.
Bile salt study
23.45
1855
Nuc. Med.
Gastric emptying
23.45
1860
Nuc. Med.
Ectopic gastric mucosa
23.45
1865
Nuc. Med.
G.I bleed
46.89
1870
Nuc. Med.
G.E. reflux
18.75
1871
Nuc. Med.
Esophageal motility
46.89
1872
Nuc. Med.
Ciliary motion study
31.27
1873
Nuc. Med.
Peritoneal/venous shunt
23.45
1875
Nuc. Med.
Renal static imaging
11.73
1880
Nuc. Med.
Renal scan and renogram
35.18
1881
Nuc. Med.
A.C.E. renal scan
46.89
May 2011 RADIOLOGY NON-PATIENT-SPECIFIC BULK BIL LING FEES Page 7
Page 91

CODE
GROUP
DESCRIPTION
UNIT
VALUE
1885
Nuc. Med.
Diuretic stimulation (add on)
11.73
1890
Nuc. Med.
Testicular scan
23.45
1899
Nuc. Med.
Residual urine (add on)
11.73
1904
Nuc. Med.
Myocardial rest
23.45
1905
Nuc. Med.
Mycardial stress and rest
37.52
1906
Nuc. Med.
Myocardial rest quantitative (add on)
7.04
1907
Nuc. Med.
Myocardial stress and rest quantitative - add on
11.73
1910
Nuc. Med.
MUGA with quantitative
23.45
1911
Nuc. Med.
Exercise MUGA
58.62
1912
Nuc. Med.
Myocardial Infarction
23.45
1913
Nuc. Med.
Cardiac first pass
28.14
1914
Nuc. Med.
Cardiac shunt
23.45
1915
Nuc. Med.
Venoscintigram
23.45
1920
Nuc. Med.
Thyroid uptake
18.75
1921
Nuc. Med.
Thyroid scan
18.75
1922
Nuc. Med.
Thyroid uptake special
23.45
1925
Nuc. Med.
Adrenal scan
70.34
1930
Nuc. Med.
Parathryoid scan
35.18
1935
Nuc. Med.
Tumor imaging
28.14
1940
Nuc. Med.
Salivary gland scintigraphy
23.45
1945
Nuc. Med.
Dacroscintigraphy
30.48
1946
Nuc. Med.
Lymphoscintigram
23.45
1947
Nuc. Med.
Isolated limb perfusion
11.73
1950
Nuc. Med.
Tomography (add on)
12.50
1951
Nuc. Med.
Hepatobiliary with pharmacologic stimulation
35.18
1955
Nuc. Med.
Hyperthyroidism (therapy)
42.21
1960
Nuc. Med.
Carcinoma of thyroid (therapy)
58.62
1961
Nuc. Med.
Metastatic carcinoma (therapy)
42.21
1962
Nuc. Med.
Ascites or pleural effusion (therapy)
42.21
1963
Nuc. Med.
Synovectomy (therapy)
42.21
1964
Nuc. Med.
Polycythemia (therapy)
42.21
1970
Nuc. Med.
Red cell volume
11.73
1971
Nuc. Med.
Plasma volume
11.73
1972
Nuc. Med.
Red cell survival
23.45
1973
Nuc. Med.
Sequestration study
46.89
1974
Nuc. Med.
Ferrokinetics
23.45
1976
Nuc. Med.
Stool for blood loss
11.73
1977
Nuc. Med.
I-131 Gastrointestinal protein loss study
11.73
May 2011 RADIOLOGY NON-PATIENT-SPECIFIC BULK BIL LING FEES Page 8
Page 92

CODE
GROUP
DESCRIPTION
UNIT
VALUE
1978
Nuc. Med.
C-14 Breath test
11.73
1979
Nuc. Med.
Glomerular filtration rate (with blood samples)
11.73
1981
Nuc. Med.
Schilling test with or without intrinsic factor
11.73
1995
Nuc. Med.
Retrograde nuclide cystogram
18.75
May 2011 RADIOLOGY NON-PATIENT-SPECIFIC BULK BIL LING FEES Page 9
Page 93

May 2011 RADIOLOGY NON-PATIENT-SPECIFIC BULK BIL LING FEES Page 10
Page 94

CODE
GROUP
DESCRIPTION
PREMIUM
VALUE
UNIT
VALUE
3001
Other
Interpretation of submitted films
35%
15.25
5001
Other
Interpretation of submitted films
50%
15.25
3005
H&N
Skull - routine views
35%
13.40
5005
H&N
Skull - routine views
50%
13.40
3012
H&N
Eye for foreign body
35%
13.34
5012
H&N
Eye for foreign body
50%
13.34
3015
H&N
Facial bones
35%
13.40
5015
H&N
Facial bones
50%
13.40
3020
H&N
Mandible
35%
12.31
5020
H&N
Mandible
50%
12.31
3030
H&N
Sinuses - paranasal
35%
12.88
5030
H&N
Sinuses - paranasal
50%
12.88
3105
Bone
Cervical spine
35%
14.19
5105
Bone
Cervical spine
50%
14.19
3110
Bone
Thoracic spine
35%
12.31
5110
Bone
Thoracic spine
50%
12.31
3115
Bone
Lumbar spine
35%
14.19
5115
Bone
Lumbar spine
50%
14.19
3120
Bone
Sacrum / coccyx
35%
12.31
5120
Bone
Sacrum / coccyx
50%
12.31
3150
Mylo
Lumbar myelogram
35%
27.75
5150
Mylo
Lumbar myelogram
50%
28.13
3151
Mylo
Complete myelogram
35%
37.99
5151
Mylo
Complete myelogram
50%
42.21
3205
Bone
Shoulder
35%
12.41
5205
Bone
Shoulder
50%
12.41
3223
Bone
Scaphoid
35%
12.41
5223
Bone
Scaphoid
50%
12.41
3224
Bone
Humerus
35%
12.41
5224
Bone
Humerus
50%
12.41
3225
Bone
Elbow
35%
12.41
5225
Bone
Elbow
50%
12.41
3226
Bone
Wrist
35%
12.41
5226
Bone
Wrist
50%
12.41
3227
Bone
Forearm
35%
12.41
5227
Bone
Forearm
50%
12.41
RADIOLOGY NON-PATIENT SPECIFIC BULK BILLING
– PREMIUM FEES
May 2011 RADIOLOGY NON-PATIENT-SPECIFIC BULK BIL LI N G FEES - PREMIUM FEES Page 11
Page 95

CODE
GROUP
DESCRIPTION
PREMIUM
VALUE
UNIT
VALUE
3228
Bone
Hand
35%
12.41
5228
Bone
Hand
50%
12.41
3305
Bone
Hip
35%
12.41
5305
Bone
Hip
50%
12.41
3310
Bone
Pelvis
35%
12.31
5310
Bone
Pelvis
50%
12.31
3321
Bone
Patella
35%
12.41
5321
Bone
Patella
50%
12.41
3322
Bone
Foot
35%
12.41
5322
Bone
Foot
50%
12.41
3323
Bone
Ankle
35%
12.41
5323
Bone
Ankle
50%
12.41
3324
Bone
Knee
35%
12.41
5324
Bone
Knee
50%
12.41
3325
Bone
Calcaneus
35%
12.41
5325
Bone
Calcaneus
50%
12.41
3326
Bone
Tibia and fibula
35%
12.41
5326
Bone
Tibia and fibula
50%
12.41
3335
Bone
Femur
35%
12.41
5335
Bone
Femur
50%
12.41
3403
Other
Fluoroscopy 10 min.
35%
21.50
5403
Other
Fluoroscopy 10 min.
50%
21.50
3404
Chest
Single view
35%
12.13
5404
Chest
Single view
50%
12.13
3405
Chest
Multiple views
35%
14.13
5405
Chest
Multiple views
50%
14.13
3425
Chest
Ribs - each side
35%
11.90
5425
Chest
Ribs - each side
50%
11.90
3435
Chest
Sternum
35%
12.31
5435
Chest
Sternum
50%
12.31
3445
H&N
Neck - for soft tissue
35%
12.31
5445
H&N
Neck - for soft tissue
50%
12.31
3605
Abdomen
Survey film
35%
12.13
5605
Abdomen
Survey film
50%
12.13
3610
Abdomen
Multiple films
35%
12.88
3625
G.I.
Upper G.I. series
35%
27.69
5625
G.I.
Upper G.I. series
50%
28.04
3650
G.I.
Colon - barium only
35%
23.91
5610 Abdomen Multiple films 50% 12.88
May 2011 RADIOLOGY NON-PATIENT-SPECIFIC BULK BIL LI N G FEES - PREMIUM FEES Page 12
Page 96

CODE
GROUP
DESCRIPTION
PREMIUM
VALUE
UNIT
VALUE
5650
G.I.
Colon - barium only
50%
23.91
3655
G.I.
Colon Paediatric - single contrast
35%
31.37
5655
G.I.
Colon Paediatric - single contrast
50%
33.56
3710
G.I.
Fistula/sinus with contrast
35%
13.40
5710
G.I.
Fistula/sinus with contrast
50%
13.40
3745
G.I.
Percutaneous transhepatic cholangiogram
35%
15.63
5745
G.I.
Percutaneous transhepatic cholangiogram
50%
15.63
3815
G.U.
Intravenous urogram (IVP)
35%
23.53
5815
G.U.
Intravenous urogram (IVP)
50%
23.53
3845
G.U.
Retrograde urethrogram
35%
13.53
5845
G.U.
Retrograde urethrogram
50%
13.53
3850
G.U.
Antegrade (T-tube) Pyelogram
35%
13.53
5850
G.U.
Antegrade (T-tube) Pyelogram
50%
13.53
4001
Vascular
Venous DSA-abdominal or renal
35%
47.95
6001
Vascular
Venous DSA-abdominal or renal
50%
53.28
3002
Vascular
Venous DSA-aortic arch
35%
53.43
5002
Vascular
Venous DSA-aortic arch
50%
59.37
3003
Vascular
Pulmonary angiogram bilateral
35%
126.62
5003
Vascular
Pulmonary angiogram bilateral
50%
140.69
3006
Vascular
Unilateral peripheral arteriogram
35%
31.14
5006
Vascular
Unilateral peripheral arteriogram
50%
33.21
3007
Vascular
Bilateral peripheral arteriogram
35%
44.83
5007
Vascular
Bilateral peripheral arteriogram
50%
49.82
3008
Vascular
Aortography (abdominal)
35%
59.68
5008
Vascular
Aortography (abdominal)
50%
66.32
3009
Vascular
Visceral selective arteriogram
35%
59.68
5009
Vascular
Visceral selective arteriogram
50%
66.32
3010
Vascular
Venogram extremity
35%
34.01
5010
Vascular
Venogram extremity
50%
37.52
3013
Vascular
Spinal artery selective
35%
31.14
5013
Vascular
Spinal artery selective
50%
33.21
3016
Vascular
Arch aortogram
35%
59.68
5016
Vascular
Arch aortogram
50%
66.32
3021
Vascular
Common carotid bilateral
35%
75.37
5021
Vascular
Common carotid bilateral
50%
83.75
3022
Vascular
Internal carotid bilateral
35%
75.37
5022
Vascular
Internal carotid bilateral
50%
83.75
3023
Vascular
External carotid bilateral
35%
75.37
5023
Vascular
External carotid bilateral
50%
83.75
May 2011 RADIOLOGY NON-PATIENT-SPECIFIC BULK BIL LI N G FEES - PREMIUM FEES Page 13
Page 97

CODE
GROUP
DESCRIPTION
PREMIUM
VALUE
UNIT
VALUE
3024
Vascular
Vertebral bilateral
35%
75.37
5024
Vascular
Vertebral bilateral
50%
83.75
3026
Vascular
Common carotid unilateral
35%
41.11
5026
Vascular
Common carotid unilateral
50%
45.68
3027
Vascular
Internal carotid unilateral
35%
41.11
5027
Vascular
Internal carotid unilateral
50%
45.68
3028
Vascular
External carotid unilateral
35%
41.11
5028
Vascular
External carotid unilateral
50%
45.68
3029
Vascular
Vertebral unilateral
35%
41.11
5029
Vascular
Vertebral unilateral
50%
45.68
3056
Cardiac
Coronary arteries
35%
68.51
5056
Cardiac
Coronary arteries
50%
76.13
3058
Cardiac
Coronary artery grafts
35%
68.51
5058
Cardiac
Coronary artery grafts
50%
76.13
3059
Cardiac
P.T.C.A.
35%
68.51
5059
Cardiac
P.T.C.A.
50%
76.13
3061
Cardiac
Right ventriculogram
35%
34.38
5061
Cardiac
Right ventriculogram
50%
38.07
3062
Cardiac
Left ventriculogram
35%
34.38
5062
Cardiac
Left ventriculogram
50%
38.07
3071
Cardiac
Aortic root (cardiac)
35%
34.38
5071
Cardiac
Aortic root (cardiac)
50%
38.07
4105
C.T.
CT head without contrast
35%
57.15
6105
C.T.
CT head without contrast
50%
63.50
3111
C.T.
CT head with contrast
35%
57.15
5111
C.T.
CT head with contrast
50%
63.50
4115
C.T.
CT head without and with contrast
35%
71.91
6115
C.T.
CT head without and with contrast
50%
79.91
3125
C.T.
CT neck with contrast
35%
57.15
5125
C.T.
CT neck with contrast
50%
63.50
3135
C.T.
CT thorax without contrast
35%
57.15
5135
C.T.
CT thorax without contrast
50%
63.50
3141
C.T.
CT thorax with contrast
35%
57.15
5141
C.T.
CT thorax with contrast
50%
63.50
3145
C.T.
CT thorax without and with contrast
35%
71.91
5145
C.T.
CT thorax without and with contrast
50%
79.91
4150
C.T.
CT abdomen without contrast
35%
57.15
6150
C.T.
CT abdomen without contrast
50%
63.50
3155
C.T.
CT abdomen with contrast
35%
57.15
May 2011 RADIOLOGY NON-PATIENT-SPECIFIC BULK BIL LI N G FEES - PREMIUM FEES Page 14
Page 98

CODE
GROUP
DESCRIPTION
PREMIUM
VALUE
UNIT
VALUE
5155
C.T.
CT abdomen with contrast
50%
63.50
3160
C.T.
CT abdomen without and with contrast
35%
71.91
5160
C.T.
CT abdomen without and with contrast
50%
79.91
3162
C.T.
CT extremities without contrast
35%
57.15
5162
C.T.
CT extremities without contrast
50%
63.50
3165
C.T.
CT pelvis without contrast
35%
57.15
5165
C.T.
CT pelvis without contrast
50%
63.50
3166
C.T.
CT pelvis with contrast
35%
57.15
5166
C.T.
CT pelvis with contrast
50%
63.50
3167
C.T.
CT pelvis without and with contrast
35%
71.91
5167
C.T.
CT pelvis without and with contrast
50%
79.91
3169
C.T.
CT spine without contrast
35%
57.15
5169
C.T.
CT spine without contrast
50%
63.50
3180
C.T.
3D reconstruction
35%
21.16
5180
C.T.
3D reconstruction
50%
21.16
3186
C.T.
CT head special without contrast
35%
57.15
5186
C.T.
CT head special without contrast
50%
63.50
3187
C.T.
CT head special with contrast
35%
57.15
5187
C.T.
CT head special with contrast
50%
63.50
3188
C.T.
CT head special without and with contrast
35%
71.91
5188
C.T.
CT head special without and with contrast
50%
79.91
4205
Ultrasound
Abdomen general
35%
34.39
6205
Ultrasound
Abdomen general
50%
38.09
3211
Ultrasound
Aorta
35%
21.50
5211
Ultrasound
Aorta
50%
21.50
3212
Ultrasound
Appendix
35%
27.75
5212
Ultrasound
Appendix
50%
28.13
3213
Ultrasound
Kidneys
35%
27.75
5213
Ultrasound
Kidneys
50%
28.13
3214
Ultrasound
Pylorus
35%
27.75
5214
Ultrasound
Pylorus
50%
28.13
3220
Ultrasound
Pelvis, male or female (GYN)
35%
27.75
5220
Ultrasound
Pelvis, male or female (GYN)
50%
28.13
4225
Ultrasound
Endovaginal
35%
36.38
6225
Ultrasound
Endovaginal
50%
40.43
4226
Ultrasound
Endovaginal with pelvic
35%
52.25
6226
Ultrasound
Endovaginal with pelvic
50%
58.05
3245
Ultrasound
Obstetrical
35%
37.14
5245
Ultrasound
Obstetrical
50%
41.27
May 2011 RADIOLOGY NON-PATIENT-SPECIFIC BULK BIL LI N G FEES - PREMIUM FEES Page 15
Page 99

CODE
GROUP
DESCRIPTION
PREMIUM
VALUE
UNIT
VALUE
3246
Ultrasound
Obstetrical, recheck
35%
21.50
5246
Ultrasound
Obstetrical, recheck
50%
21.50
3250
Ultrasound
Biophysical profile
35%
13.84
5250
Ultrasound
Biophysical profile
50%
13.84
3255
Ultrasound
Obs. multiple - (add on)
35%
29.04
5255
Ultrasound
Obs. multiple - (add on)
50%
30.06
3275
Ultrasound
Scrotum
35%
34.45
5275
Ultrasound
Scrotum
50%
38.18
3285
Ultrasound
Hip
35%
27.75
5285
Ultrasound
Hip
50%
28.13
3298
Ultrasound
Subcutaneous mass
35%
21.50
5298
Ultrasound
Subcutaneous mass
50%
21.50
3307
Ultrasound
Portable - M.D. in attendance
35%
27.75
5307
Ultrasound
Portable - M.D. in attendance
50%
28.13
4335
Ultrasound
Doppler abdominal blood vessels
35%
45.21
6335
Ultrasound
Doppler abdominal blood vessels
50%
50.24
3345
Ultrasound
Doppler - extremities
35%
27.75
5345
Ultrasound
Doppler - extremities
50%
28.13
4405
M.R.I.
Cranial multisection SE
35%
55.31
6405
M.R.I.
Cranial multisection SE
50%
61.46
3407
M.R.I.
Cranial repeat, sequence
35%
28.91
5407
M.R.I
Cranial repeat, sequence
50%
29.87
3409
M.R.I.
Ent multisection SE
35%
55.31
5409
M.R.I.
Ent multisection SE
50%
61.46
3412
M.R.I.
Ent repeat, sequence
35%
28.91
5412
M.R.I.
Ent repeat, sequence
50%
29.87
3415
M.R.I.
Thorax multisection SE
35%
63.22
5415
M.R.I.
Thorax multisection SE
50%
70.25
3416
M.R.I.
Thorax multisection IR
35%
55.31
5416
M.R.I.
Thorax multisection IR
50%
61.46
3417
M.R.I.
Thorax repeat, sequence
35%
32.42
5417
M.R.I.
Thorax repeat, sequence
50%
35.13
3420
M.R.I.
Abdomen multisection SE
35%
63.22
5420
M.R.I.
Abdomen multisection SE
50%
70.25
3421
M.R.I.
Abdomen multisection IR
35%
55.31
5421
M.R.I.
Abdomen multisection IR
50%
61.46
3422
M.R.I.
Abdomen repeat, sequence
35%
32.42
5422
M.R.I.
Abdomen repeat, sequence
50%
35.13
4425
M.R.I.
Pelvis multisection SE
35%
63.22
May 2011 RADIOLOGY NON-PATIENT-SPECIFIC BULK BIL LI N G FEES - PREMIUM FEES Page 16
Page 100

CODE
GROUP
DESCRIPTION
PREMIUM
VALUE
UNIT
VALUE
6425
M.R.I.
Pelvis multisection SE
50%
70.25
3426
M.R.I.
Pelvis multisection IR
35%
55.31
5426
M.R.I.
Pelvis multisection IR
50%
61.46
3427
M.R.I.
Pelvis repeat sequence
35%
32.42
5427
M.R.I.
Pelvis repeat sequence
50%
35.13
3430
M.R.I.
Extremities multisection SE
35%
55.31
5430
M.R.I.
Extremities multisection SE
50%
61.46
3432
M.R.I.
Extremities repeat, sequence
35%
28.91
5432
M.R.I.
Extremities repeat, sequence
50%
29.87
3440
M.R.I.
Spine (one seg.) multisection SE
35%
50.58
5440
M.R.I.
Spine (one seg.) multisection SE
50%
56.21
3442
M.R.I.
Spine (one seg.) repeat, sequence
35%
27.73
5442
M.R.I.
Spine (one seg.) repeat, sequence
50%
28.10
4445
M.R.I.
Spine (two adjoining) multisection SE
35%
60.08
6445
M.R.I.
Spine (two adjoining) multisection SE
50%
66.75
3447
M.R.I.
Spine (two adjoining) repeat sequence
35%
31.25
5447
M.R.I.
Spine (two adjoining) repeat sequence
50%
33.28
3453
M.R.I.
Add 30% for gating
35%
23.05
5453
M.R.I.
Add 30% for gating
50%
23.05
3776
Nuc. Med.
Labelled WBC
35%
55.40
5776
Nuc. Med.
Labelled WBC
50%
61.56
3790
Nuc. Med.
Vascular study (flow) (add on)
35%
20.73
5790
Nuc. Med.
Vascular study (flow) (add on)
50%
20.73
3810
Nuc. Med.
Brain scan
35%
20.73
5810
Nuc. Med.
Brain scan
50%
20.73
3811
Nuc. Med.
Brain perfusion
35%
63.30
5811
Nuc. Med.
Brain perfusion
50%
70.34
3816
Nuc. Med.
Bone scan (one area)
35%
32.45
5816
Nuc. Med.
Bone scan (one area)
50%
35.18
3817
Nuc. Med.
Bone scan (multiple areas)
35%
37.99
5817
Nuc. Med.
Bone scan (multiple areas)
50%
42.21
3830
Nuc. Med.
Lung ventilation scan
35%
32.45
5830
Nuc. Med.
Lung ventilation scan
50%
35.18
3835
Nuc. Med.
Lung scan perfusion
35%
32.45
5835
Nuc. Med.
Lung scan perfusion
50%
35.18
4850
Nuc. Med.
Hepatobiliary
35%
32.45
6850
Nuc. Med.
Hepatobiliary
50%
35.18
3865
Nuc. Med.
G.I. bleed
35%
63.30
5865
Nuc. Med.
G.I. bleed
50%
70.34
May 2011 RADIOLOGY NON-PATIENT-SPECIFIC BULK BIL LI N G FEES - PREMIUM FEES Page 17
 Loading...
Loading...