Laerdal SimMan 3G Trauma User Manual

SimMan 3G
Trauma
User Guide
EN
www.laerdal.com


CONTENTS
INTRODUCTION 4
SimMan 3G Trauma Patient Simulator 4
CAUTIONS AND WARNINGS 5
General Simulator Handling 5
Antivirus and Firewalls 5
File Security and Backup of Data 5
FEATURES 6
SimMan 3G Trauma Overview 6
General 7
Laerdal Simulation Software 7
Airway Features 8
Breathing Features 9
Circulation 10
Bleeding 10
Sounds 11
Eyes Settings and Configurations 11
Drugs and IV 11
SimMan 3G Trauma Clothing 12
SETUP 13
Inserting and Connecting the Batteries 13
The Power Panel 14
Charging the Batteries 14
Battery Use 15
Battery Warnings 16
Using the Internal Compressor 16
Turning the Internal Compressor OFF Using LLEAP 16
Changing Default Compressor Settings Using LLEAP 16
Air/CO
Panel 17
2
Blood and Fluid System 17
Adjusting Fluid Flow 19
Connecting Wounds Kit 20
Removing Wounds 20
Simulate Severe Bleeding Using LLEAP 20
Administering IV Fluids 21
Cleaning the IV Arm 21
Connecting Defibrillation Adapter Plates 22
Connecting the Blood Pressure Cuff 23
Calibrating the IV Arm Flowmeter Using LLEAP 23
Connecting the SpO
Changing Genitalia Modules 24
Probe 23
2
Inserting Urine Catheter 24
Changing the Upper Dentures 24
Bleeding Modules 25
Replacing and Filling IO Units with Blood 29
Transporting SimMan 3G Trauma 32
Unpacking the Patient Simulator 32
MAINTENANCE 33
Daily Maintenance 33
Before Storage or Shipping 33
Regular Cleaning of Fluid and Blood System 33
Installing and Upgrading LLEAP 35
Removing/Changing Router 35
Opening the Torso 36
Attaching the Left Leg 36
Attaching the Right Leg 37
Attaching the Left Arm 37
Attaching the Right Arm 38
Replacing Crico Tape/Neck Skin 38
Replacing Chest Drain Pleura 39
Replacing Pneumothorax Bladders 39
Replacing Chest Rise Bladder 40
Replacing Lung Bladders 40
Replacing Simulator Skins 41
Replacing Blood System Filter 41
Servicing the Patient Simulator 41
TROUBLESHOOTING 42
SPARE PARTS AND ACCESSORIES 45
3
3

INTRODUCTION
SimMan 3G Trauma Patient
Simulator
For Advanced Clinical Simulation
SimMan 3G Trauma is an advanced patient simulation system that
facilitates training of Basic and Advanced Life Support. The system
allows the instructor to effectively assess the learner’s individual and
team skills based on a realistic clinical situation.
SimMan 3G Trauma allows observation and recognition of most
vital signs. This is achieved through direct interaction with the Patient
Simulator and observation of the Patient Simulator’s status as viewed
on the Patient Monitor.
The SimMan 3G Trauma Simulation System
Features Include:
– An advanced configurable airway, comprised of adjustable lung
compliance and resistance - allowing simulation of difficult airway
management cases.
– Eyes that respond to light and react according to the clinical
state of the Patient Simulator.
– Bleeding and Wound Modules are fed from an internal blood
reservoir. An external Blood Fill Unit may be connected for
extended bleeding cases.
– Simulated Secretions: sweat, tears, froth, urine and ear fluids are
fed from an internal fluid reservoir. An external Fluid Fill Unit
may be connected for extended use.
– Focus on Quality CPR (QCPR): measurement and feedback
according to the 2005 and 2010 Guidelines.
– Vascular Access (intra osseous) via the tibia and sternum.
– Automatic Simulation Control based on preprogrammed and
validated Patient Cases.
WLAN Communication
Communication between the Patient Simulator and the PCs is based
on WLAN communication. The Patient Simulator and PCs can also
be connected to a LAN cable network, and WLAN disabled.
The Main Components of the SimMan 3G
Trauma System:
SimMan 3G Trauma is an adult life-size wireless Patient Simulator,
with internal battery power, internal air compressor and fluid
reservoirs. Interventions by learners are registered by the system in
the session log, and used for later debriefing.
The Instructor PC controls the simulation. The headset allows the
instructor to simulate interactive voice communication between the
patient and the learner.
Software available for use with the simulator includes LLEAP for
controlling scenarios, SimDesigner for creating and editing scenarios,
SimView server or SessionViewer for debriefing simulation sessions
with video capture and a Patient Monitor application.
4
CAUTIONS AND WARNINGS
General Simulator Handling
The Patient Simulator should be operated by trained personnel only.
Treat the Patient Simulator as you would treat a real patient.
Warning: Do not ventilate the Patient Simulator with oxygen
enriched air or flammable gases.
− Do not introduce fluids into or onto the Patient Simulator
(except as directed in the User Guide), as this may damage the
Patient Simulator and it’s components.
− Do not introduce humidified air into the system during
ventilation.
− Never perform mouth-to-mouth or mouth-to-nose rescue
breathing on the Patient Simulator. The simulator’s airways are
not designed for cleaning or disinfection.
− Do not use the Patient Simulator if the internal tubing and
cabling is disconnected.
− Never use the Patient Simulator outdoors in wet conditions, as
this may pose a shock hazard or damage the simulator.
− Never use the Patient Simulator in temperatures exceeding 40°
C (104°F), as this may cause overheating and shut down.
− Never use the Patient Simulator in temperatures below 4 °C (39
°F), as this may damage the fluid system.
− The Patient Simulator should never be stored in temperatures
below -15° C (5° F).
− The Patient Simulator will automatically shut down if the battery
temperature exceeds 60°C (140°F).
− Using a defibrillator in temperatures over 35° C (95° F) may
cause overheating and shut down.
Warning: Avoid pinch hazards - Do not remove protective bushings
from the Patient Simulator’s joints or use it without the external skins.
Warning: Avoid all sharp edges on the Patient Simulator to prevent
personal injury.
Do not use the Patient Simulator if:
− Limbs are not attached to the torso
− Skins are torn or not properly fastened
− Internal or external cables, tubes or connectors are damaged
− There is fluid leakage inside the Patient Simulator torso
− There are unusual sounds indicating air leakage or mechanical
damage
− There are signs of electrical malfunction, such as an unresponsive
Patient Simulator or unusual smell or smoke
Hygiene
– To maintain Patient Simulator skins, wash hands before use and
place the Patient Simulator on a clean surface.
– Wear gloves as required during simulation scenarios.
– After using the Fluid and Blood System, follow the cleaning
instructions (see Maintenance section).
– After using the SimMan 3G Trauma Wound Kit, remove glue
residue from the Patient Simulator skin with Laerdal Medical
Wipes.
– Use only Laerdal Airway Lubricant in the Patient Simulator’s
airway. Do not spray airway lubricant into the Patient Simulator.
Lubricate tools only.
Prevent Stains on Patient Simulator Skins
Avoid using colored plastic gloves, as they may cause discoloration of
the Patient Simulator skin.
Do not use felt-tipped markers, ink pens, acetone, iodine or other
staining medications near the Patient Simulator. Take care not to
place the Patient Simulator on newsprint or colored paper. All
staining may be permanent.
Transportation and Storage
SimMan 3G Trauma is heavy; ensure that the Patient Simulator is
properly secured during transportation to prevent personal injury or
damage to the product.
Antivirus and Firewalls
The Patient Simulator and PCs are not supplied with Antivirus
programs. Windows firewall is activated by default. It is the
customer’s responsibility to protect the simulation system
components from unauthorized access.
The Patient Simulator will revert to factory settings each time the
power is switched off.
The customer should install all recommended Windows updates
from Microsoft. General security measures should be taken before
browsing the internet.
It is recommended that the SimMan 3G Trauma PCs are used
only as Patient Simulator controllers. Downloading other software
programs onto these machines may introduce unexpected errors.
File Security and Backup of Data
The customer is responsible for file security and backup routines for
all simulation session data. All use and storage of simulation session
data should be in accordance with local rules, regulations or laws,
and is the sole responsibility of the customer.
Cautions and WarningsFeaturesSetupMaintenanceSpare Parts Troubleshooting
5
DC Input 9-24V X, XA
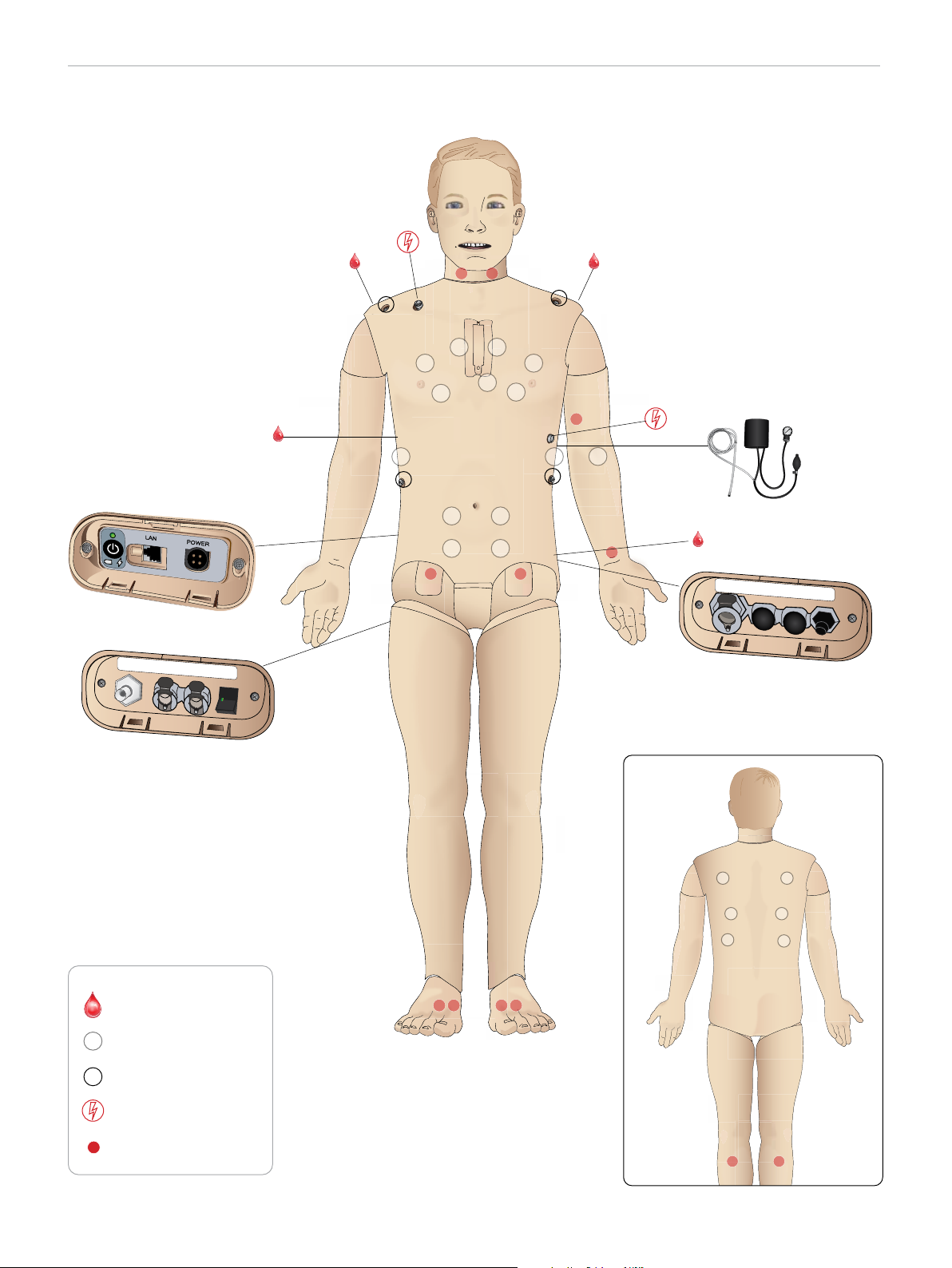
FEATURES
SimMan 3G Trauma Overview
Power Panel
Air Out
Fluid Fill Panel
Bleeding ports
Speakers
Air / CO
2
Inlet
Blood
Fluid
Inlet
Activate
Inlet
Filling
Air/CO2 Panel
Blood
Outlet
ECG Connectors
Defib Connectors
Pulses
6
FEATURES
General
Main Anatomical Features
Dimensions (Patient Simulator only):
1800mm (l) x 550mm (w) chest (5. 90 ft x 1.80 ft)
Weight (Patient Simulator only): 38.5kg (85 lbs)
Weight (with clothes): 40 Kg (88 lbs)
Default male body with interchangeable genitalia pads.
Configurable Anatomical Features
Genitalia
The Patient Simulator comes with a neutral genitalia pad as default.
The pad can be changed for a male or female module, both included
with the SimMan 3G Trauma System. See Changing Genitalia Modules
section.
Teeth
Patient Simulator comes with a set of soft teeth as default. These can
be exchanged for a hard set of teeth, included with the SimMan 3G
Trauma System. See Changing Upper Dentures section.
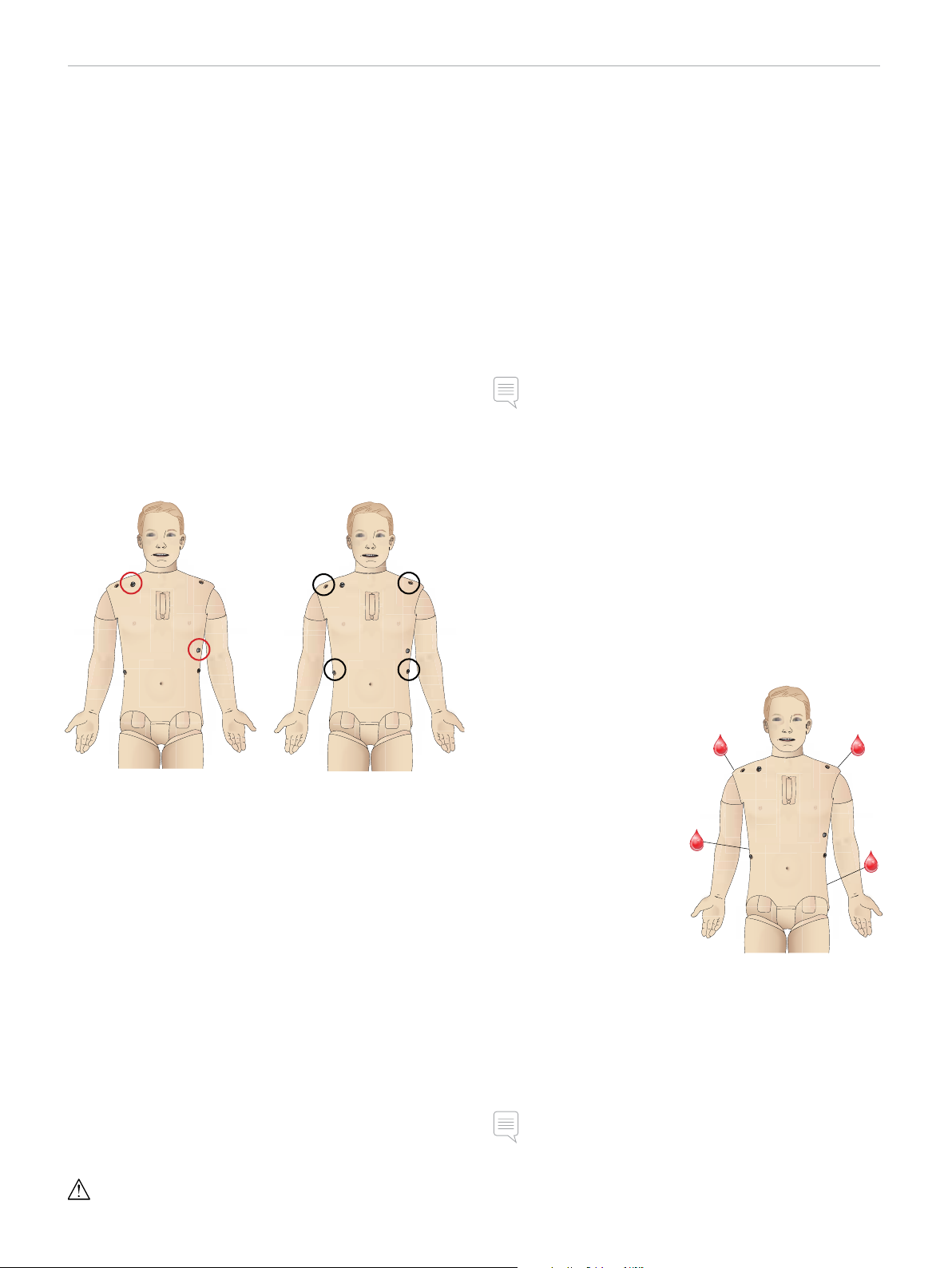
Trauma Modules/Limbs
Left Leg - amputation and bleeding module
Right Arm - amputation and bleeding module
The SimMan 3G Trauma arm adaptor kit is used to connect the
trauma arm modules.
Contact your local Laerdal representative to enquire about other
trauma modules compatible with SimMan 3G Trauma.
Laerdal Simulation Software
To run a simulation, LLEAP (Laerdal Learning Application) must be
started from Laerdal Simulation Home on the Instructor PC.
Cautions and WarningsFeaturesSetupMaintenanceSpare Parts Troubleshooting
Laerdal Simulation Home
Laerdal Simulation Home is an application from where LLEAP and
other Laerdal programs related to patient simulation can be found
and started. The help files can also be opened from here. Laerdal
Simulation Home is located in the Laerdal Medical folder under the
Windows start menu (Windows 7).
Software used in a simulation session comprises the following main
applications:
− LLEAP (Laerdal Learning Application)
− Voice Conference Application
− Patient Monitor
− SimView Ser ver or Session Viewer
In addition SimDesigner and other applications are also used for
designing or preparing a simulation.
LLEAP
LLEAP is the instructor’s application from where the simulation
session is run, controlled and monitored. LLEAP can be operated
in Automatic or Manual mode. Automatic mode is used for
preprogrammed scenarios while Manual mode allows the instructor
full manual control of the simulation session. Running simulations in
Manual Mode requires some medical expertise to create clinically
sound simulations.
Mobility of joints
Neck: Movement can be on a 3-axis movement of head.
Range of movement can be restricted. See Airway
Features section.
Shoulders: 3-axis rotation
Lumbar: 1-axis
Elbows: Fixed, no mobility
Wrists: 3-axis rotation
Thumbs: Free mobility
Hip joints: 3-axis rotation
Knees: 1-axis rotation
Ankles: 1-axis rotation
Note: Do not remove protective bushings at shoulder or lower back.
These are present to protect users from pinch points.
Voice Conference Application (VCA)
The VCA software allows the instructor to communicate through
the simulator during the session. VCA can also be used to
communicate with other instructors on a network, and create
separate channels where only members can communicate.
Patient Monitor
The Patient Monitor application emulates a typical hospital patient
monitor. It is the learner’s console and can be set up and controlled
by the instructor, as well as by the learner through on-screen touch
menus.
Session Viewer and SimView Server
Session Viewer and SimView Server are applications that record
video and patient monitor screen captures during simulation, in
addition to providing an interface to debrief your session. After a
session is ended, log files generated in LLEAP are transferred and
merged with the video files in Session Viewer or SimView Server for
the debrief.
Session Viewer typically runs locally on the same computer as used
for LLEAP, SimView Server runs on a dedicated ser ver in the local
network. During the first startup of LLEAP, you are prompted to
select a debriefing system available on your computer or on a local
network. This can be changed later.
7

FEATURES
Other Applications
There are also other programs that are used in conjunction with
the simulation sessions, for example License Manager for handling
program licenses and Simulator Firmware & Network Wizard for
updating the firmware of the simulators or troubleshooting network
problems.
SimDesigner
The SimDesigner application allows you to configure your own
preprogrammed scenarios. It can also be used to analyze and print
out a graphical representation of a scenario.
SimDesigner must be installed to allow conversion of legacy
instructor application files to LLEAP compatible file formats.
For a full overview of all applications and their help files, start LLEAP
Simulation Home.
Web Downloads
Visit www.laerdal.com/download to download the latest User Guide
and Software.
Airway Features
The airway is anatomically modeled as far as the bronchia.
The airways can be manipulated by a learner:
− Head tilt/Chin lift
− Jaw thrust with articulated jaw
− Cricoid pressure and manipulation
− Suctioning (oral & nasopharyngeal)
If the tongue fallback feature is enabled, head tilt is required to open
the airways for mask ventilations. The Patient Simulator may be
ventilated by normal and emergency methods:
Use of a malleable stylet is recommended - make sure it does not
extend beyond the ET tube.
Recommended styles:
− i-Gel
− Fiberoptic intubation
− Combitube (size small adult is suitable)
− Retrograde intubation
− Needle cricothyrotomy
− Surgical cricothyrotomy
The following Patient Simulator features indicate incorrect
tube placement:
− Right main stem intubation – unilateral chest rise
− Stomach distention
− Lack of chest sounds, CO
section)
exhalation (see Breathing Features
2
Configurable Airway Features
Patient Simulator features may be configured to present various
airway scenarios:
− The airway may be closed automatically or manually. There are
four levels of resistance and compliance within the airway.
− Tongue edema - multiple levels
− Phar yngeal swelling
− Lar yngospasm
− Decreased cer vical range of motion
− Trismus
− Teeth - soft upper dentures may be replaced with a hard set of
teeth for enhanced realism while practicing intubations.
− Bag-mask ventilation
− Orotracheal intubation
− Nasotracheal intubation
− Transtracheal intubation
Prior to using airway adjuncts, apply a small amount of Laerdal
Airway Lubricant to the equipment. Do not spray lubricant directly
into the airway,
The following equipment or methods are suitable to secure
the Patient Simulator’s airway:
− Lar yngeal mask airways: The airways are designed for use with
size #4, but size #5 may also seal correctly.
− Endotracheal tube intubation, Size ID 7.5 - 8.5 is suitable, but
using the smaller size reduces wear of the Patient Simulator’s
airways.
During simulation, the following conditions can be set:
− Can’t intubate/can ventilate
− Can’t intubate/can’t ventilate
The following information is automatically registered in the
SimMan 3G Trauma simulation session:
− Detection of proper head position.
− Jaw Thr ust
− Pneumothorax decompression
− Ventilations
− Stomach distension
Note: In LLEAP the airway and breathing status for the current
simulator is shown in a window. Settings for lung resistance,
compliance, and other parameters can be made. See LLEAP Help
for further information.
8
FEATURES
Breathing Features
The SimMan 3G Trauma can simulate spontaneous breathing:
− Bilateral and unilateral chest rise and fall
− There are 4 compliance settings, from normal to extremely stiff
− There are 4 settings for airway resistance, from normal to
extremely tight.
− Normal and abnormal breath sounds
− 5 anterior auscultation sites and 6 posterior auscultation sites
− Unilateral, bilateral and lobar breath sounds
− Oxygen saturation and phlethysmogram
− CO
Patient Monitor features - Breathing
− SpO
− Airway respiration rate (awRR)
− End-tidal CO
− End-tidal O
− inO
− pH
exhalation for use with third-party End-tidal CO2 detectors
2
(Requires connection to an external CO
Warning: Do not ventilate the Patient Simulator with oxygen
enriched air or flammable gass.
Caution: Do not ventilate Patient Simulator lungs using humidified
air.
2
(etCO2)
2
(etO2)
2
2
reservoir)
2
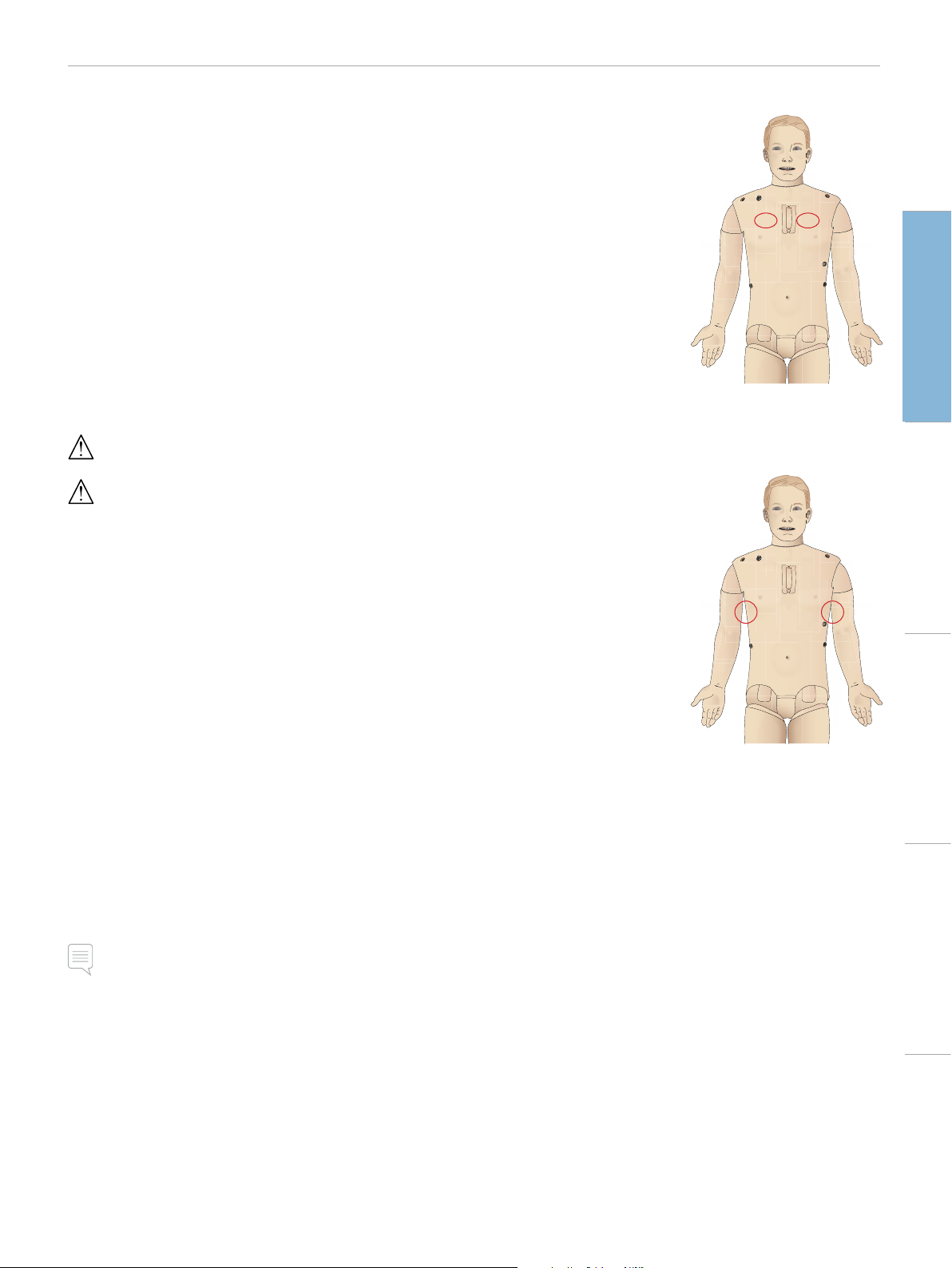
Pneumothorax
Tension pneumothorax with
needle decompression can be
performed at bilateral mid
clavicle line, 2nd intercostal
space. The pneumothorax
bladders may be pierced +/-10
times, the pressure inside the
bladder will drop after repeated
puncturing.
A 22 (or smaller) gauge
needle is recommended for
decompression of the chest.
Using a smaller gauge needle
increases the longevity of the
chest skin and bladders.
However, a too small gauge prevents automatic detection of the
decompression event in the simulation model.
Chest Tube Inser tion
Chest tube insertion can be
simulated. Exploration and cut
can be made at left or right
mid-axillary line in the 4th and
5th intercostal space.
Cautions and WarningsFeaturesSetupMaintenanceSpare Parts Troubleshooting
Lung specifications
− Max tidal volume: 1.2 liters
− Max tidal volume registered in the LLEAP is 900ml. All volumes
higher than 900ml will register as 900ml
− Max airway pressure: 80 cm H
− Simulated stomach inflation star ts from approximately 40cmH
airway pressure.
Note: Lungs are not intended for use with PEEP-valves.
O
2
O
2
9
FEATURES
Circulation
Cardiac features
− Extensive ECG library, pulses from 0-220.
− Hear t sounds - for every anterior location
− ECG rhythm monitoring (4-connector, 3-lead ECG)
− 12-lead ECG display
− Pacing
− Defibrillation and cardio version using live defibrillators
Defibrillation
− With live defibrillators; energy level and waveform model is
registered by the Patient Simulator.
− The energy levels and number of shocks required for automatic
conversion are set in each simulation Patient Case.
Defibrillation Studs 3-Lead ECG Studs
Patient Monitor features - Circulation
− ECG (12-lead) and hear t rate (HR)
− Pulse
− NBP
− ABP
− PA P
− C .O.
Patient Monitor features - Temperatures
− TPeri
− Tblood
Note: A variety of settings in the Circulation and Fluids window can
be made in LLEAP. See LLEAP Help for further information.
Bleeding
To allow the Patient Simulator to bleed realistically, it has internal
reservoirs for simulated blood. See Blood and Fluid System section.
The four bleeding ports and blood flow can be adjusted
independently from LLEAP:
− Upper and lower bleeding ports
− Venous and arterial
− Works with various wound modules and moulage kits
Circulation features
− BP measured manually by auscultation of Korotkoff sounds
− Carotid, brachial, radial, femoral, popliteal, dorsalis pedis, and
posterior tibialis pulses synchronized with ECG
− Pulse strength variable with BP
− Pulses are synchronized with ECG when the instructor sets the
pulse strength manually
− Pulse palpation is detected and logged
CPR
− Compliant with 2005 and 2010 Guidelines
− Compressions generate palpable pulses, blood pressure wave
form, and ECG artifacts
− Realistic compression depth and resistance
− Detection of depth, release and frequency of compressions
− Real-time view of Quality of CPR on the Instructor’s PC
Warning: Do not use automated chest compression machines on
the Patient Simulator.
Bleeding Treatment:
− Bandage
− Pressure point
− Tourniquet
− Surgical Clamps
Vascular Access:
− IV access (right arm)
− Intraosseous access (tibia
and sternum)
Consumables and
Spare Parts:
− Laerdal Ar tificial Blood
− Fill Units
− Wound modules
− Replacement trauma arm/leg.
Note: A variety of settings in the Circulation and fluids window can
be made in LLEAP. See LLEAP Help for further information.
10
FEATURES
Sounds
Two types of sounds can be used in a scenario:
– Body sounds
– Vocal sounds
The sounds can be triggered by the scenario or controlled by the
instructor.
Body Sounds
The body sounds are simulated sounds from a human body, like
heart, lungs, and bowel sounds. The sounds are integrated and
generated in the Patient Simulator and transferred through the
integrated speakers.
Vocal Sounds
The vocal sounds are sounds from the throat like coughing, moaning,
and crying as well as spoken words. The sounds are integrated in
LLEAP and transferred to the Patient Simulator.
In addition, the instructor can communicate through a microphone
and the voice is then transferred to the Patient Simulator through
the VCA.
Note: A variety of settings in the Sounds window can be made in
LLEAP. See LLEAP Help for further information
Drugs and IV
Drugs and drug concentrations can be registered manually by the
instructor in LLEAP.
Patient Monitor features – Drugs
– Train-of-Four (TOF)
– in N
O, et N2O
2
– Anesthesia agents
– Lab reports
User-replaceable items, spare par ts
– Intra-muscular Pad x 3
– Sternal IO Pad
– Tibial IO Pad
Vascular Access (IV and IO) Locations
Intraosseous access with needle insertion is possible through the
left tibia and the Sternal IO pad. The IO pads may be punctured
numerous times before being replaced.
To replace the IO modules, see Replacing and Filling IO Units with
Blood section.
Cautions and WarningsFeaturesSetupMaintenanceSpare Parts Troubleshooting
Eyes Settings and Configurations
The calculated Glasgow Coma Scale score for the Patient Case is
displayed in LLEAP. The following sources of information help the
learner to judge the state of disability:
Eyes
– Blinking eyelids
– Eyelids: open, closed or partially open
– Eyelids can be opened for examination by the learner
– Pupil dilation: constricted, dilated or in between
– Pupillary accommodation
– Synchrony/asynchrony
– Normal and sluggish speed of response
Note: A variety of settings in the Circulation and Fluids window can
be made in LLEAP. See LLEAP Help for further information.
Caution: Do not inject fluids into these pads unless approved IO
modules with fluid outlets are in place.
Intra-muscular (IM) Injection
Use the pad placed under the Torso Skin on the right buttock for
intramuscular injection training. Use the tigh pads (left and right) for
IM injection.
11

FEATURES
SimMan 3G Trauma Clothing
Included with the Patient Simulator:
− Shir t, with side zippers
− Trousers, with full-length side zippers
− Boxer shorts underwear
− Belt
Note: For washing instructions see care labels.
Simulated Removal of the Clothes
To simulate cutting with scissors: unzip the zippers placed alongside
the seams on both sides.
12
SETUP
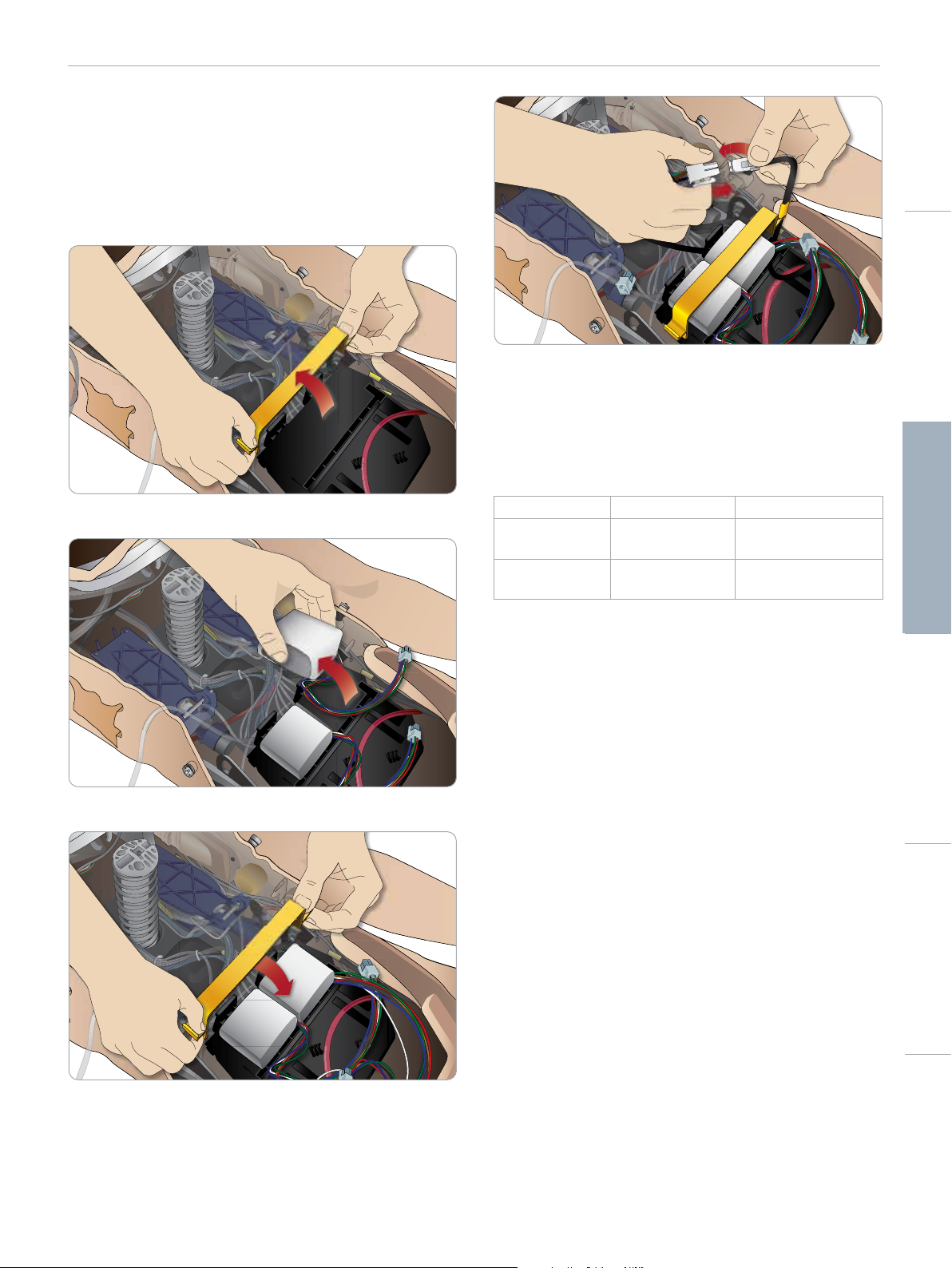
Inserting and Connecting the
Batteries
Open the torso as described in steps 1 - 4, Opening the Torso.
To remove the batteries, follow the same procedure in reverse.
1 Release the battery clamp by unhooking the clips on either side.
2 Insert both batteries into the battery tray.
Cautions and WarningsFeaturesSetupMaintenanceSpare Parts Troubleshooting
After connecting the batteries, connect the Patient Simulator to the
external power supply (12V to 24V) while turned OFF.
The batteries will charge if the Patient Simulator is ON and
connected to an external power supply in the range of (20V - 24V).
Battery - Cable and Tube Descriptions
Name/Label Tube/Cable Color Connector Description
Battery 1 Black harness cable Black rectangular
connector, 6 lead
Battery 2 Black harness cable Black rectangular
connector, 6 lead
3 Snap the battery clamp back into place over the batteries.
4 Connect the corresponding battery cables from the batteries to
the torso.
13
DC Input 9-24V X, XA
POWER
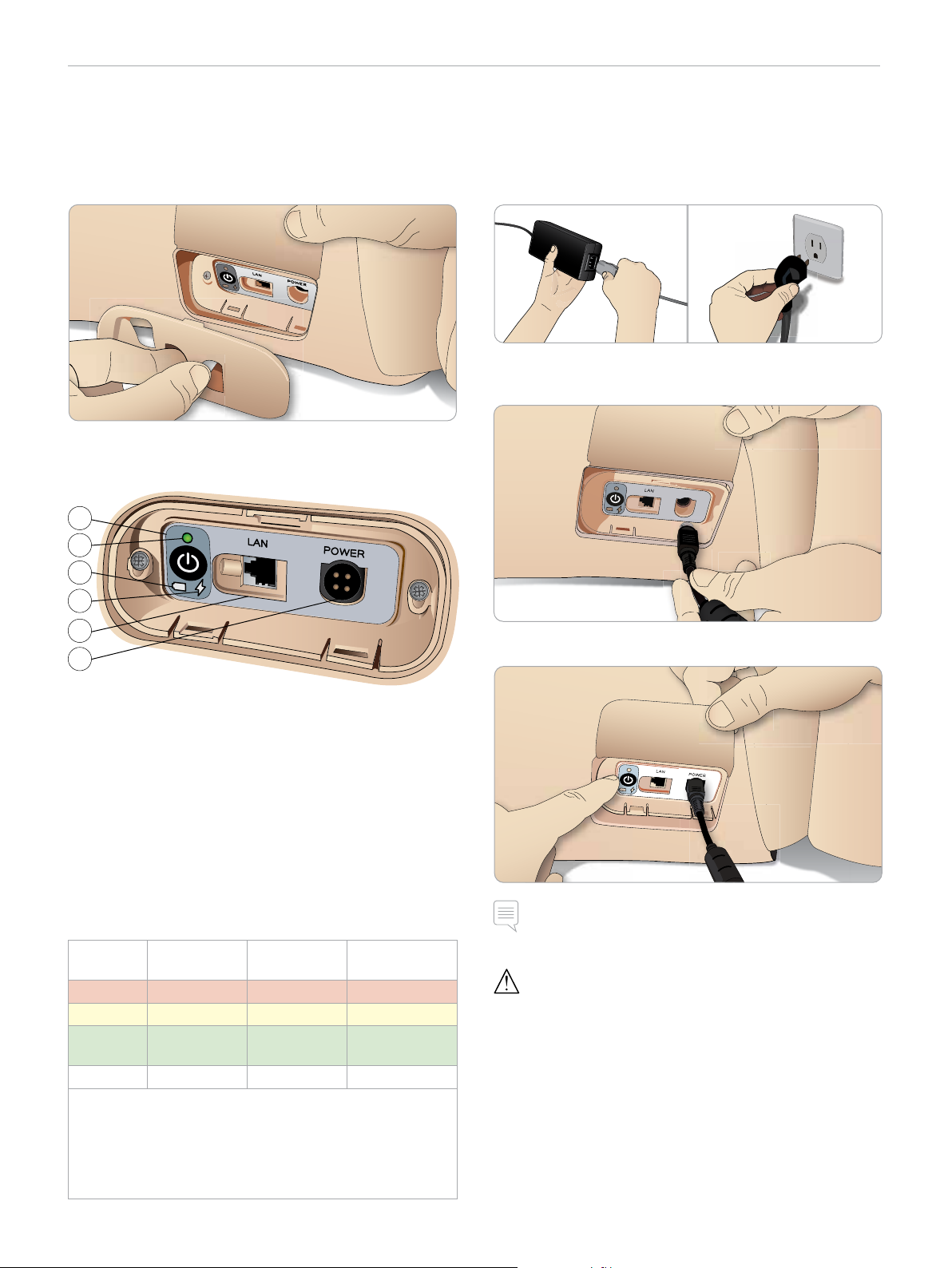
SETUP
The Power Panel
The power panel is found on the right side of the Patient Simulator,
under a loose skin flap. Lift the skin flap and pull out the protective
cover.
To ensure easy access, use the zippered clothing provided with the
Patient Simulator.
1
2
Charging the Batteries
Inside the Patient Simulator
1 Connect the Patient Simulator to the external power supply
with a power cord and plug that meets local specifications.
2 Plug the power supply into a wall outlet and connect the power
cable to the power inlet on the Patient Simulator’s power panel.
3
4
5
6
Power panel overview
1 Power ON / OFF button
2 Power status indicator
3 Battery status indicator
4 Charging status indicator
5 LAN network cable connector
6 External power supply connector
Power Status Indicator Description
Indicator
Light Color
Red Power save* 0% - 20% Not charging**
Yellow Star t up 20% - 70% Charging
Green Running 70% - 100% Charge almost
No light Off Off No charge****
* Blinking light
** One or both batteries missing, overheated, damaged or
otherwise not able to charge
*** Not recommended to charge the batteries too long
**** No power input, batteries are charged.
Power Save is activated whenever Patient Simulator is paused.
Power Status Battery Status Charge Status
complete***
3 Press the ON button to power on the Patient Simulator.
Note: During start up, the Patient Simulator’s eyes will blink and
the power status indicator light will be yellow.
Caution: After Patient Simulator is turned off, wait 20 seconds
before restarting. If not, Patient Simulator may not function properly.
14
 Loading...
Loading...