Page 1
GE Healthcare
Quick Guide
GE EK-Pro
Arrhythmia Algorithm
Multi-lead arrhythmia monitoring
Arrhythmia means any disturbance or irregularity of the
cardiac rhythm. Stability of the cardiac rhythm is essential
for sufficient pumping function of the heart and adequate
cardiac output. Maintaining adequate cardiac output is vital
for organ perfusion and survival. Therefore, fast and accurate
detection of arrhythmia is critical.
Each ECG lead views the heart at a unique angle. Multi-lead
monitoring provides continuous viewing of the heart rhythm
from multiple sites. The more leads that are used, in general,
the more reliable the information is for arrhythmia analysis.
A multi-lead arrhythmia algorithm uses more than one ECG
lead for detection and analysis of cardiac arrhythmias. The
performance of a multi-lead algorithm, in general, may
exceed that of a single-lead algorithm. In noisy situations,
there might be noise present on some leads, while the signal
in other leads might be good enough for reliable detection
of cardiac rhythm. Sometimes ventricular beats can be
more obvious in some of the leads than in others where the
changes in morphology are minor. It is also possible that
QRS amplitude can be low in one lead and normal in others.
Therefore, the sensitivity of the algorithm may increase when
more than one lead is used.
The recognition of ventricular beats may be improved by
multi-lead monitoring, and the same applies to QRS detection.
The decision between normal and ventricular beats may be
more reliable when information from more than one lead is
available. The GE EK-Pro arrhythmia algorithm uses I, II, III,
and the V/VA lead for arrhythmia detection. The American
Heart Association (AHA) has recommended that two or
preferably three or more leads should be displayed and
monitored simultaneously. Exceeding the AHA’s minimum
recommendation, the distinctive GE EK-Pro algorithm utilizes
four simultaneous leads for analysis.
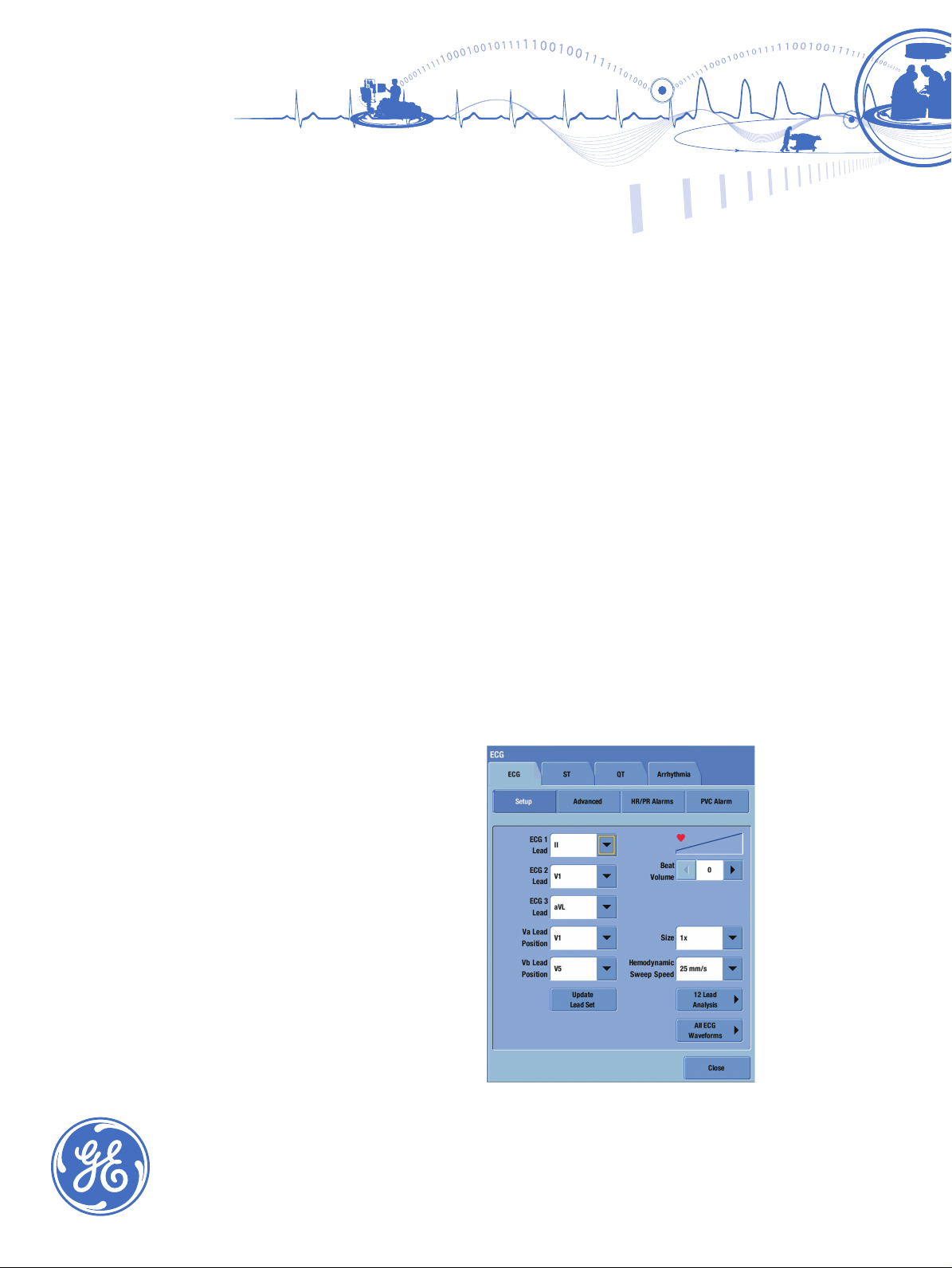
Window in CARESCAPE modular monitors to select
the ECG leads to be analysed.
Page 2

How are arrhythmias monitored?
The GE EK-Pro algorithm processing can be represented by
three major phases: 1) Event Detection and Correlation,
2) Event Measurement and Classification, and 3) Arrhythmia
Detection. Continuous correlation, incremental template
updating and contextual analysis are processing techniques
used by the GE EK-Pro algorithm. Continuous correlation
attempts to find the best match between each incoming
complex and the set of stored (learned) templates. Incremental
template updating allows information from each beat,
which correlates over time, to be reflected in the associated
template. Contextual analysis uses information from
neighboring QRS complexes along with existing template
measurements to make the best possible decision regarding
the beat’s origin (e.g., early, wide). Additionally, the GE EK-Pro
algorithm also monitors ST changes of up to 12 leads.
For ST monitoring details, please consult the appropriate
user manual.
Event Detection and Correlation filters the incoming signal
before detecting the incoming events. As the events are
detected, incremental template updating is applied on the
signal. Here also the noise analysis is done in order to decide
whether if any of the incoming channels are too noisy to
be analyzed. Each detected QRS complex is compared to
previously detected QRS complexes and the templates are
updated accordingly, or a new template is created and the
beat is added on the beat list.
Practical aspects in bedside
arrhythmia monitoring
Signal quality
Careful skin preparation and the use of high-quality electrodes
are key to ensuring a good signal in ECG and especially
arrhythmia monitoring. A good signal helps ensure accurate
arrhythmia detection and helps decrease the number of false
alarms. In case there is an artifact in one of the analyzed
leads, the GE EK-Pro algorithm gives a message on noisy ECG
and, if the condition continues, the algorithm finally goes into
suspend mode. This is communicated by “Arrhyhtmia paused”
or “Arrhy suspend” message, depending on the GE monitor in
use. Artifacts can be a result of motion or poor skin-electrode
contact.
Relearning
When the morphology of the patient’s ECG changes
considerably (e.g. due to change of electrodes/electode
locations), relearning should be started manually. This can be
done in the ECG menu by selecting Relearn QRS.
Patients with pacemakers
Pacemaker detection needs to be activated when patients
with pacemakers are monitored. Pacemaker detection
is always on with the E-PSM or E-PRESTN module family.
Pacemaker detection needs to be activated when the
CARESCAPE™ Patient Data Module or Tram™ is used.
Event Measurement and Classification task uses the beat
list to define the timing, for example, the temporal information
of the patient rhythm. The algorithm can classify the beat in
question by using the information from the preceding and
following beats. A beat is classified as normal, ventricular or
artifact and, in combination of the decision of the past beat
template, the final label is given and the heart rate is also
updated accordingly.
Arrhythmia Detection uses the beat list to get information in
run lengths of normal and ventricular beats. Based on this, R-R
interval information and heart rate, the algorithm concludes
whether there are any arrhythmias present. The criteria for
calling an arrhythmia are listed in the table at the end of this
document. There is a separate analysis to detect the presence
of ventricular fibrillation.
The Advanced ECG tab provides the user with
options to adjust the ECG settings. Examples of
options include Pacemaker Detection, Relearning
QRS, and switching between multi-lead and single
lead analysis.
Page 3

Bedside arrhythmia alarms
In GE monitors there are two arrhythmia analysis modes:
Lethal and Full. The Lethal mode is the standard and Full is an
optional choice. The Lethal mode detects asystole, ventricular
fibrillation/ventricular tachycardia and ventricular tachycardia.
In the neonatal mode bradycardia is also considered a lethal
arrhythmia. The details of arrhythmia alarms criteria are
described in the following table.
A Fib, Irregular (Tram) Absence of P-waves and irregular R-R intervals
Accel. Ventric. Run of PVCs with a run length of at least six beats and the rate requirements have not met
Asystole HR decreased to zero
Bigeminy Every other beat is a PVC (N-V-N-V-N)
Couplet Two consecutive PVCs are detected between normal beats N-V-V-N. The coupling interval
HR High/Tachy, PSM: HR High only The displayed 4/8-beat average ECG heart rate exceeds the user-selected common HR high
HR Low/Brady The displayed 4/8-beat average ECG heart rate falls below the user-selected common HR
Missing Beat* Actual R-R interval more than 1.8 times the average R-R interval
Multifocal PVCs* Over the last 15 beats two or more premature ventricular beats with dierent morphologies
Pause Actual R-R interval exceeds 3s (Tram) or a congured value 1-5s
CARESCAPE Patient Data Module,
Tram: V Fib/V Tach
R on T Isolated PVC is detected within 100 ms of the peak of the T-wave of the patient’s
Rapid VT* A run on PVCs is detected with a run length of six beats or more. In addition, an eective
Single PVC An isolated PVC is detected
Trigeminy Every third beat is a PVC (N-N-V-N-N-V-N)
V Brady Run of PVCs with a run length of at least three beats; additionally, at least two consecutive
V Tach A run of PVCs, with run length six beats or more; in addition, an eective HR that exceeds
VT > 2 A run of PVCs, with run length more than two beats, but less than six, and less than required
V Tach or V Brady
between the PVCs must be less than 600ms
limit or ECG HR high limit
low limit or ECG HR low limit
are detected
(CARESCAPE Patient Data Module)
ECG waveform indicates a chaotic ventricular rhythm
predominant normal beat
heart rate that exceeds 160 bpm
R-R intervals in the run must have an eective HR less than the age specic limits (60 or 50)
100 - 160 beats per minute (age-specic limits)
for V Tach; additionally, at least two concecutive R-R intervals must have an eective HR
that exceeds 100-160 beats per minute (age specic limits)
The GE EK-Pro algorithm is used with the CARESCAPE Patient Data Module, CARESCAPE Monitor B850, CARESCAPE Monitor B650,
Tram module, Solar
* Missing beat, Multifocal PVC and Rapid VT alarm labels are only available with version 12 of the GE EK-Pro arrhythmia algorithm.
Version 12 is only available with the CARESCAPE Monitor B650 when used with the Patient Side Module (E-PSM). In case of these
alarms CARESCAPE Monitor B650 sends mapped alarms to the CARESCAPE Network. This is due to limitations in the CARESCAPE
Network. Alarms are mapped as follows: Missing beat sent as Pause, Multifocal PVC sent as PVC, Rapid VT sent as V Tach.
For the most current arrhythmia calls, please consult the user manual specic to your current monitor for the details.
®
monitors, Dash® monitors, ApexPro® telemetry, and CARESCAPE Telemetry.
Additional resources
For white papers, guides and other instructive materials about our clinical measurements, technologies
and applications, please visit http://clinicalview.gehealthcare.com/
Page 4

© 2010 General Electric Company – All rights reserved.
GE, GE Monogram, CARESCAPE and ApexPro are
trademarks of General Electric Company.
Solar, Dash and Tram are trademarks of GE Medical
Systems Information Technologies, Inc.
GE Healthcare reserves the right to make changes in
specications and features shown herein, or discontinue
the product described at any time without notice or
obligation. Contact your GE Healthcare representative for
the most current information.
GE Healthcare Finland Oy, a General Electric company,
doing business as GE Healthcare.
GE Healthcare, a division of General Electric Company.
CAUTION: U.S. Federal law restricts this device to sale by or
on the order of a licensed medical practitioner.
Consult the monitor User’s Guide for detailed instructions.
About GE Healthcare
GE Healthcare provides transformational medical technologies and services that
are shaping a new age of patient care. Our broad expertise in medical imaging and
information technologies, medical diagnostics, patient monitoring systems, drug
discovery, biopharmaceutical manufacturing technologies, performance improvement
and performance solutions services help our customers to deliver better care to more
people around the world at a lower cost. In addition, we partner with healthcare leaders,
striving to leverage the global policy change necessary to implement a successful shift
to sustainable healthcare systems.
Our “healthymagination” vision for the future invites the world to join us on our
journey as we continuously develop innovations focused on reducing costs, increasing
access and improving quality around the world. Headquartered in the United Kingdom,
GE Healthcare is a unit of General Electric Company (NYSE: GE). Worldwide, GE Healthcare
employees are committed to serving healthcare professionals and their patients in more
than 100 countries. For more information about GE Healthcare, visit our website at
www.gehealthcare.com.
GE Healthcare
8200 West Tower Avenue
Milwaukee, WI 53223
U.S.A.
GE Healthcare Finland Oy
Kuortaneenkatu 2
00510 Helsinki
Finland
GE Healthcare
3/F Building # 1,
GE Technology Park
1 Hua Tuo Road
Shanghai 201203
www.gehealthcare.com
China
imagination at work
DOC0783131 10/10
 Loading...
Loading...