Page 1
operating manual
&
user’s guide
v2.10z6BJ24/03/2004EN
Page 2

BTL – 07p operating manual & user's guide
I. DIRECTIONS FOR USE................................................................................................................................... 4
Outer appearance 4
Controls and dipslays 4
Connection to the mains 5
Choosing the ultrasound frequency 5
Choosing and connecting emitter head 5
Choosing PPR (pulse-to-period ratio) 5
Choosing pulse frequency 5
Choosing intensity of acoustic output 5
Time setting 6
Ultrasound generation 6
Indication of stationary waves 6
Interrupting the therapy 6
Selecting the program 6
Saving personalised programs 6
Combined ultrasound/electrotherapy 6
Connecting the units 6
Starting the combined therapy 7
Ending the combined therapy 7
Summary of directions for use 7
Safety instructions 7
Useful addresses ...................................................................................................................................8
Warranty..................................................................................................................................................8
Maintenance and transport 8
Troubleshooting: 8
Technical specifications of probe 9
Technical specifications of unit 9
Pulse width 10
II. USER'S GUIDE .......................................................................................................................................... 11
Mechanism of action 11
Methods of application 12
Ultrasound frequency 13
Modes of operation 13
Emitter head size 13
Application time 13
Intensity 13
Procedure frequency 13
Total number of treatments 13
Specific contraindications of ultrasonic therapy 14
Procedure 15
A therapeutic example 15
Combined therapy 16
Ultrasound and low frequency currents 16
Mechanism of action 16
Application time 16
Intensity 16
Total number of procedures 16
Frequency of procedures 16
Procedure Prescription 16
A therapeutic example 17
Ultrasound + amplitude modulated mid-frequency currents 17
Mechanism of action 17
Application time 17
Number of procedures 17
Procedure frequency 17
Procedure prescription 17
A therapeutic example 17
page 2
Page 3

BTL – 07p operating manual & user's guide
Ultrasound + TENS (transcutaneous electrostimulation) 18
Mechanism of action 18
Application time 18
Intensity 18
Total number of treatments 18
Frequency of treatment 18
Procedure prescription 18
A therapeutic example 18
III. LIST OF PROGRAM NUMBERS FOR ULTRASOUND THERAPY ........................................................... 19
IV. LIST OF PROGRAM NUMBERS FOR COMBINED ULTRASOUND THERAPY/ELECTROTHERAPY.... 25
page 3
Page 4
BTL – 07p operating manual & user's guide
I. DIRECTIONS FOR USE
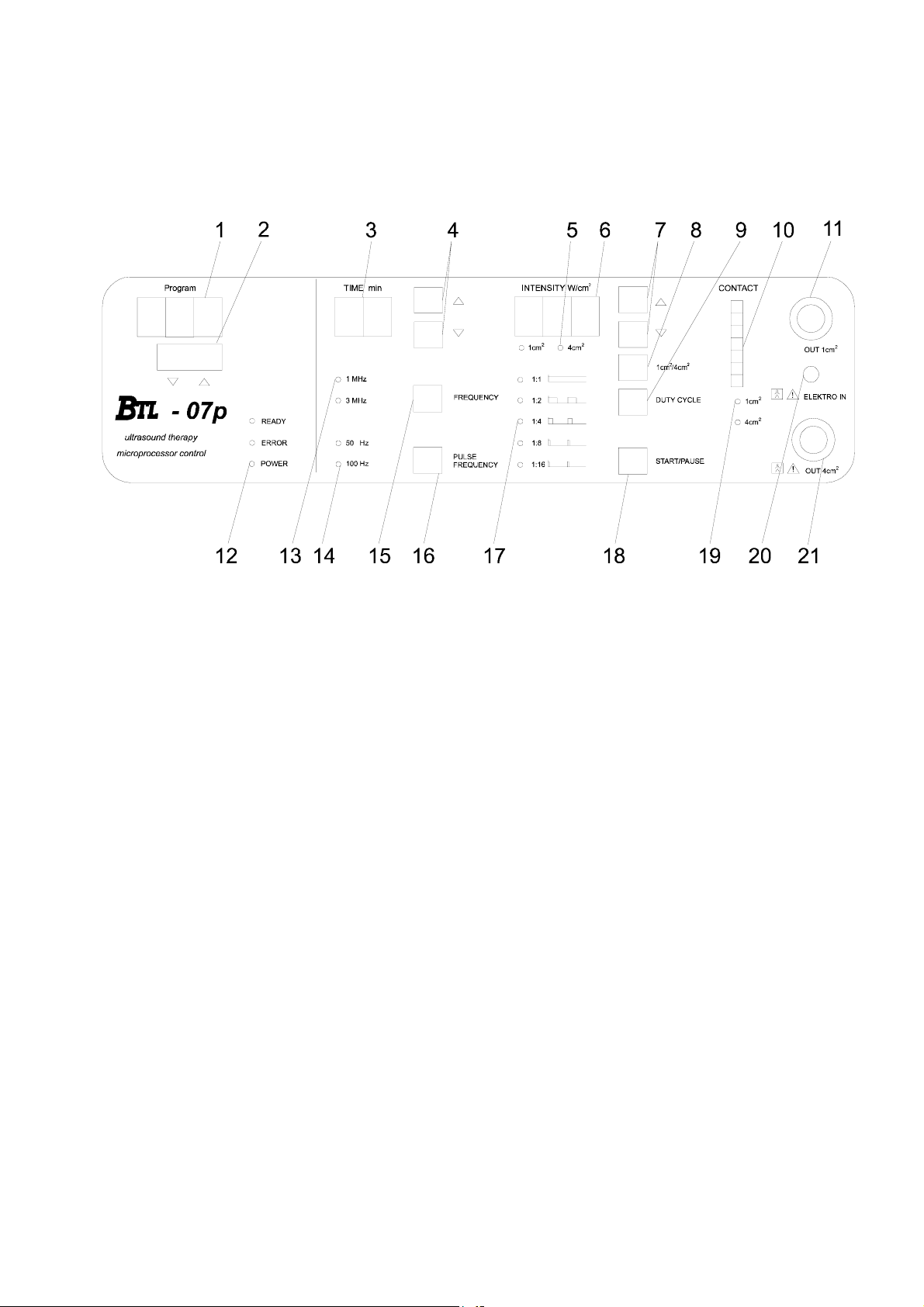
FRONT PANEL OF BTL-07p
Outer appearance
Front panel features: pilot-lights, displays, push-buttons, input for emitter head, input for BTL-06, input for
electrical cable, mains switch, fuses, serial and model number are located on the rear panel.
Controls and dipslays
1) Display indicating power absorbed by patient (in kilojoules).
2) Select button
3) Time display to show pre-set and remaining therapy time (in minutes).
4) Push-button to set therapy time (in minutes).
5) LED diode indicating use of set parameters.
6) Display of pre-set acoustic output (indicated by two pilot lights).
7) Push-button to set acoustic output.
8) Push-button to change indication of acoustic output.
9) Duty Cycle push-button.
10) Column lights indicating contact of emitter head with skin.
11) Small ultrasound emitter head connector.
12) Signal lights:
• Ready - Emitter heads connected; intensity/therapy time is set.
• Error - Light signal a hardware defect indicating.
• Power - Light signal indicating the unit is on.
13) LED diodes. Indicate pre-set frequency.
14) LED diodes. Indicate pre-set pulse frequency.
15) Push-button to set 1 MHz/3 MHz frequency.
16) Push-button to set 50 Hz/100 Hz pulse frequency.
17) LED diode. Indicates PPR.
18) START/PAUSE push-button. Starts, ends and interrupts therapy.
19) LED diodes. Indicate 1 cm
2
or 4 cm
2
emitter head sizes.
20) Ultrasound emitter head connector.
21) Electrotherapy unit connector.
page 4
Page 5
BTL – 07p operating manual & user's guide
Connection to the mains
Read the "Safety Instructions" before using instrument!
Make sure that the mains switch is at "0". Connect mains cable to the connector on the rear panel with mains 230
V/50 Hz. Switch the main switch to "1". The program number, the preset treatment time, and the ultrasound
frequency are lit up on the display.
Choose the irradiation surface area and the emitter head (1 cm
2
or 4 cm
2
). Connect the emitter head with emitter
head connector on the front panel. Never change emitter heads during ultrasound generation. Change emitter
heads only if the instrument is switched off with the START/PAUSE button (17). Use RESET button if you begin
therapy with another patient.
Choosing the ultrasound frequency
Use the FREQUENCY push-button (15) to choose the 1 MHz or 3 MHz frequency. The green diodes (13),
situated to the left of the FREQUENCY button, indicate which of the two frequencies is activated. Both
frequencies can be applied with either emitter head sizes. Choose a 1 MHz frequency if you wish to
therapeutically affect deep tissues and a 3 MHz frequency for superficial tissues.
Choosing and connecting emitter head
2
Two emitter heads of either 1 cm
Connect the emitter head to the Connector (11, 21). Connect the 1 cm
2
4 cm
head to Connector (21). The LED diode (19) indicates which emitter head is in use. Both emitter heads can
or 4 cm
2
can be used with the BTL-07p.
2
emitter head to Connector (11) and the
be used for either continuous or pulse modes and for both frequencies. The emitter head must be connected
before intensity of acoustic output is set. The therapy cannot start without connecting and identifying the emitter
head.
The red diode on the emitter head indicates insufficient contact between the emitter head and the tissue.
If contact is insufficient, the control light lights up red.
The countdown on the TIME display (3) stops. Power absorption (indicated by the light blinking) stops. Therapy is
interrupted until contact is restored.
If there is proper contact, the control signal on the emitter head will light up green.
Choosing PPR (pulse-to-period ratio)
Different pulse-to-period ratios are related to different ultrasound thermic effects. Continuous ultrasound deeply
heats tissues. A 1:2 or 1:4 PPR ultrasound only has a moderate thermic effect and 1:8 or 1:16 PPR ultrasound
has an athermic.
Use the DUTY CYCLE push-button (9) to set the PPR. The activated PPR is indicated by the green diode (17).
Choosing pulse frequency
The pulse ultrasound (1:2 - 1:16 PPR) allows the user to choose one of the pulse frequencies and the time
duration.
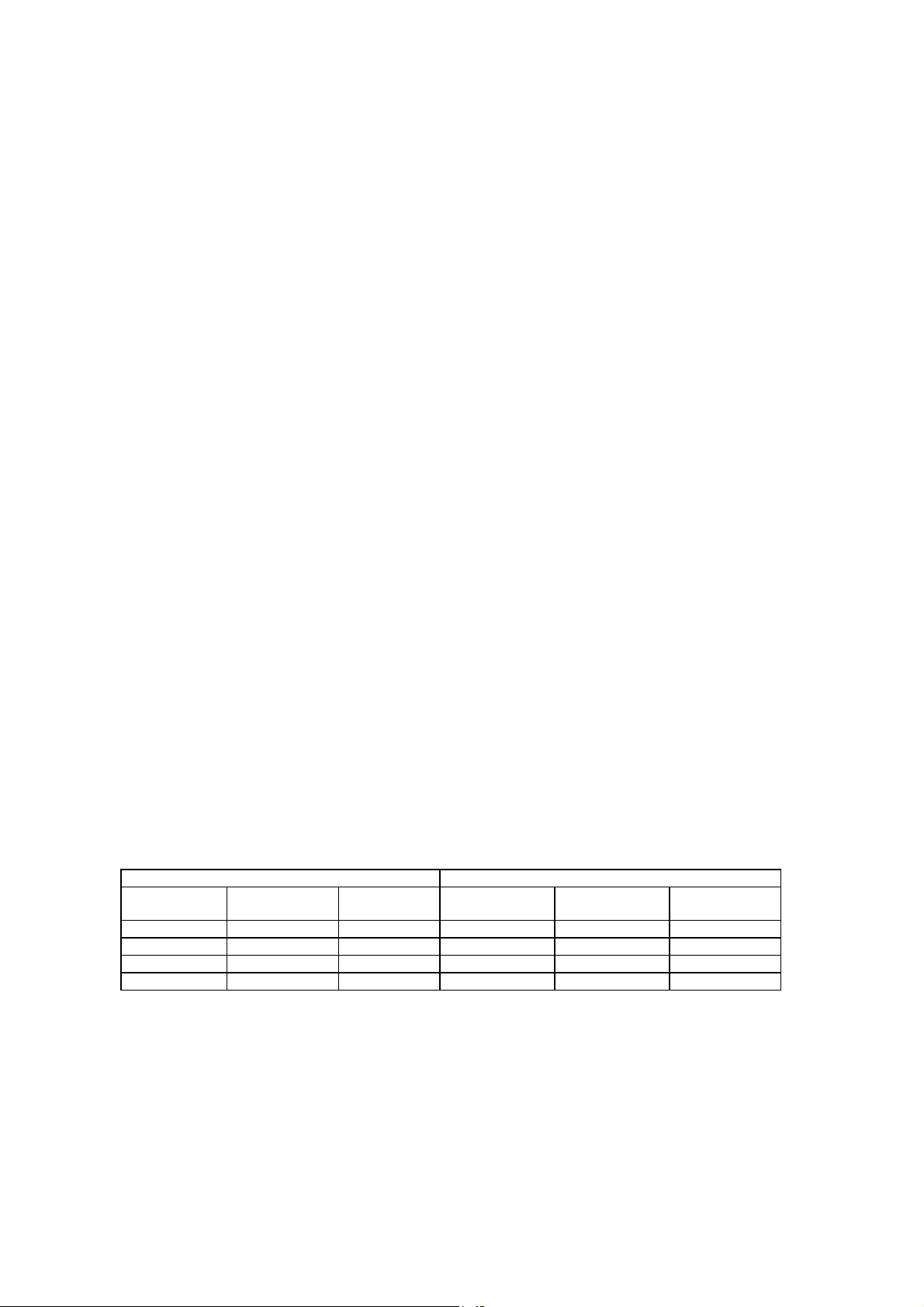
The BTL-07p uses 50 Hz and 100 Hz pulse frequencies. Press the PULSE FREQUENCY button (16) to switch
between the two frequencies. The activated pulse frequency is indicated by the diode next to the PULSE
FREQUENCY button (14). Impulse and pause duration of both frequencies are specified in the following tables.
Frequency 50 Hz, period duration 20ms Frequency 100 Hz, period duration 10ms
Duty cycle Impulse
duration
Pause
duration
Duty cycle Impulse
duration
Pause
duration
1: 2 10 ms 10 ms 1: 2 5 ms 5 ms
1: 4 5 ms 15 ms 1: 4 2.5 ms 7.5 ms
1: 8 2.5 ms 17.5 ms 1: 8 1.25 ms 8.75 ms
1: 16 1.25 ms 18.75 ms 1: 16 0.625 ms 9.375 ms
Choosing intensity of acoustic output
2
Press up/down arrow push-buttons (7) to set intensity. Continuous mode employs intensities up to 2 W/cm
mode up to 3 W/cm
2
(in steps of 0.1 W/cm
2
). Pressing down the up/down push-button will increase or decrease
, pulse
intensity.
page 5
Page 6

BTL – 07p operating manual & user's guide
Time setting
The therapy time is shown on the TIME display (3). Press the up/down arrow push-buttons to increase or
decrease time (4). The time is adjustable in steps of 0.5 minute up to 5 minutes and in steps of 1 minute up to 25
minutes. The maximum application time is 25 minutes. Hold the up/down push-button pressed to increase or
decrease time.
Ultrasound generation
Generation of ultrasound begins after the following operations have taken place:
Connect an emitter head to the instrument.
Set intensity and time. READY control light should light up. If it does not, check the emitter head (19) connection
and the head type (5). Try the other emitter head (8).
Press START/PAUSE push-button (18). The set time must not be 0. The time display starts to count/down the
pre-set time.
If there is sufficient contact between the emitter head and the skin, the “Program” display will stop showing the
program number and will start to count the amount of absorbed energy. The lowest green light in the CONTACT
row will light up (10) and the light in the TIME and INTENSITY decimal boxes will start to blink. The columnar
graph (10) and the emitter head control light both monitor the quality of contact during application. If contact is
insufficient, diodes light up red. If this happens, moisten the skin with more ultrasound gel.
A cold emitter head can also cause insufficient contact. In this case set the intensity to 0.1 W/cm
2
and generate
ultrasound for approximately 1 minute to warm up the head. Then set the intensity. If there is insufficient contact
between the head and the patient, the unit stops. If there is proper contact, the therapy continued. All parameters
can be changed at any time.
Indication of stationary waves
Any ultrasound application to a bone or bony area situated just under the skin (condyles, epicondyles, ankles)
may, if the emitter head is not moved sufficiently, result in interference between a reflected wave and an arising
wave arising (stationary wave). Consequently, there are "peaks of intensity". A peak of intensity is an area, which
is exposed to intensity higher than the preset intensity level. There is an increased local temperature in these
areas.
BTL-07p emitter heads have a very low BNR. Further more, the BTL-07p features an optic indicator to signal
stationary waves, placed on the Bar-graph (10) (the orange LED diode). Respond to this signal by immediately
removing the emitter head from the application site in order to eliminate any risk of soft tissue damage.
Interrupting the therapy
Pressing the START/PAUSE push-button (18) immediately interrupts the therapy. The time countdown stops and
the pre-set intensity level, as well as the amount of absorbed energy, do not change. To continue therapy, press
the START/PAUSE push-button again. To start a new treatment, set the time and start the ultrasound generation.
Selecting the program
The unit has pre-set programs for ultrasound and combined ultrasound/electrotherapy. The list of programs and
procedures can be found in the user’s guide. Press button (2) to select the program or diagnosis. Any parameters
can be changed before starting the application. Press the START/PAUSE button (18) to start the therapy.
Saving personalised programs
The BTL-07p enables you to save your own programs, which can be stored under codes 80-99. Set all
the parameters. Press and hold the START/PAUSE button. After 2 seconds the bar-graph (10) blinks and there is
an acoustic signal. Programs are stored when the unit is turned off.
Combined ultrasound/electrotherapy
The BTL-07p allows the user to apply ultrasound and electrotherapy at the same time. The ultrasound instrument
can be connected to the BTL-06 electrotherapy unit. Do not connect the BTL-07p to electrotherapy units
manufactured by other companies.
Connecting the units
Place the BTL-06 on the ultrasound BTL-07p. For combined therapy, the units are connected with a special cable.
Plug the cable connector of an ultrasound emitter head into the outlet on the front panel (21). Insert the cable for
combined therapy into the electrotherapy unit outlet (channel B for voltage mode). Insert the red banana plug into
the BTL-07p outlet (20). Connect the electrode to the green banana plug. The ultrasound emitter head then
serves as the anode (+) and the electrode as the cathode (-).
page 6
Page 7
BTL – 07p operating manual & user's guide
Starting the combined therapy
Set the instruments after they are connected. Set all needed parameters on the BTL 07p and press the
START/PAUSE button (17). Press the STOP button (V/mA) (18) to set the voltage (the V control light is on).
Choose the program and set the therapy time. Apply the electrode and the emitter head to the treatment area.
The moment the emitter head touches the skin, the ultrasound will start and the time will begin to count down.
Press the button (19) on the electrotherapy unit to set the voltage and start the combined therapy. Caution: Keep
the ultrasound emitter head on the treated area during the therapy!
Ending the combined therapy
After the pre-set time has elapsed and the START/PAUSE button (17) on the BTL-07p has been pressed, the
combined therapy stops. If there is a need to stop or interrupt the application before the pre-set time elapses,
press the button (18) on the BTL-06 before removing the emitter head or the electrode from the skin.
Summary of directions for use
1. Connect the instrument to the mains.
2. Switch the instrument to "1".
3. Connect an emitter head to the instrument.
4. Choose the required program.
5. Check if the READY control light is flashing. If it is not, the emitter head is probably not connected.
6. Press the START/PAUSE push-button (17) to start application.
7. Press the START/PAUSE push-button (17) to interrupt therapy.
8. Therapy ends automatically when the pre-set time has elapsed.
Safety instructions
The BTL-07p ultrasonic therapy instrument is constructed with maximum regard for the safety of the patient and
therapist. However, it is absolutely essential to strictly follow the safety instructions below:
1. Read the operation manual carefully before you use the instrument for the first time.
2. Make sure that the parameters of the mains correspond to those of the instrument.
3. The mains must be installed and correspond to valid norms. Call a qualified electrician if in doubt.
4. If the instrument is exposed to a sudden temperature charge, allow at least 1 hour for the temperature of the
instrument to equalize before turning it on.
5. Stop the therapy immediately if the instrument shows any signs of malfunction. If the instrument does not
turn on when activated, call or fax BTL’s Service Department. Do not attempt to repair the instrument!
Removing the instrument housing will invalidate the service warranty.
6. Do not touch the metallic parts of the emitter head during therapy.
7. Make sure that all set parameters correspond to the desired parameters.
8. Do not cover the vents. Do not place the instrument on a soft surface that would prevent air from circulating
beneath it.
9. Never use the connectors for anything else but the electrotherapeutic instrument and the emitter head.
The user should not use the instrument, if it does not work as described in this manual. Contact your BTL service
technician. The user is responsible for all damages resulting from using such an instrument.
All materials that come in contact with the patient (gel, emitter head cleaners, etc.) comply with ISO 10993-1,
ISO 10993-3 and ISO 10993-5 standards on hypersensitivity, toxicity and carcinogenicity.
The user is responsible for use of all materials and parts not supplied by BTL.
WARNING!
!
These symbols mean that the electric voltage and current flowing through the input may exceed safe
levels. BTL-07p has a BF safety level and floating attached parts. Never use the instrument in a manner other
than that described in this operation manual!
page 7
Page 8
BTL – 07p operating manual & user's guide
Useful addresses
The product is manufactured in accordance with the EU Medical Devices Directive by :
BTL Industries Ltd.
Suite 401 Albany House
324-326 Regents Street
London, W1B 3BL United Kingdom
E-mail: sales@btlnet.com
http://www.btlnet.com
For service, please contact service department at service@btlnet.com
Warranty
The Manufacturer of this product warrants the product to be free from defects in workmanship and material for a
period of twelve months after the date of shipment from the factory. This warranty excludes any disposable items
and accessories, including, but not limited to cables or leads, power cords and electrodes. The manufacturer
agrees to correct such defects without charge, or at its option to replace the item with a comparable model. To
register and be eligible for warranty service, you must send or fax the fully completed warranty registration form
within 30 days of installation. All costs of shipment are the responsibility of the purchaser. Damage to any part
such as by accident or misuse or improper installation or by use of any accessories or abrasive material not
produced by the Manufacturer is not covered by this warranty. Because of varying climatic conditions, this
warranty does not cover any changes in finish, including rusting, pitting, corrosion, tarnishing or peeling. Servicing
performed by unauthorized persons render this warranty invalid. There is no other express warranty. The
Manufacturer hereby disclaims any and all warranties, including but not limited to, those of merchantability and
fitness for a particular purpose to the extent permitted by law. The duration of any implied warranty which cannot
be disclaimed is limited to the time period as specified in the express warranty. The Manufacturer shall not be
liable for incidental, consequential, or special damages arising out of, or in connection with product use or
performance except as may be otherwise accorded by law.
This warranty may differ from the warranty terms and conditions provided by your supplier and by applicable laws
in your country.
.
Maintenance and transport
The unit can be cleaned with a damp cloth. Do not use alcohol-based solutions. Transport the instrument in its
original packaging. Remove the power cable and emitter heads. Avoid rough handling.
Fuses are located on the rear panel in black round cases. Make sure that the power switch is in position “0”.
Unplug the mains cable from the instrument and from the mains plug. Use an appropriate screwdriver to rotate the
inner segment of the fuse case counter-clockwise to remove and replace the fuse. Use only those fuses specified
on the label below the fuse cases. Only qualified persons should replace fuses.
If the unit no longer works and you plan to throw it out, please return it to the manufacturer so it can disposed of
safely, or take it to a specialized disposal company.
Troubleshooting:
Problem
No power or light displayed Check if the mains cable is plugged to the mains and the unit. Check
Therapy does not begin Check if the READY control light is blinking and set the therapy time.
The emitter head is plugged in but the
LED diode does not flash Check if the connector is properly connected. Plug the small emitter
Signal lights are non-functional,
Er is displayed Contact your service technician.
CONTACT signal lights up red Skin is too dry.
during application Insufficient body contact.
Solution
the fuse.
Make sure that you are using the emitter head shown on the display.
head in the upper and the large emitter head in the lower connector.
If the heads are connected and the control light does not flash
contact your service technician.
Wrong emitter head size. Remember to use the larger emitter head
for small, uneven surfaces.
page 8
Page 9

BTL – 07p operating manual & user's guide
If this signal persists, try to calibrate the emitter head. The 07p
calibration procedure should be done as follows:
• Prepare yourself some water container for app. 0.5 liter (water
temperature should be around 30 °C) with a sponge (or some
swab or cotton wool) at the bottom.
• Connect your emitter head to proper connector.
• Turn on the device and choose the emitter heads type, by
pressing appropriately button, you are going to calibrate.
• Start generating ultrasound for app. 2 min. at a 2 W intensity,
PIP=1:1. Use both frequencies one after another.
• Stop the therapy (if it is running).
• Put emitter head into the water – app. 1cm under the water level
(1cm from the metal top of the head).
• Press the “Pulse frequency” button down and hold it there. The
bar graph LEDs will be running up and down. After certain time
you will hear a sound. Release the “Pulse frequency” button
and remain the emitter head under the water until the bar graph
LEDs will stop running.
• Take the emitter head out of the water and dry it with some
cloth.
• Leave the emitter in the air.
• Press the “Frequency” button down and hold it there. The bar
graph LEDs will be running up and down. After certain time you
will hear a sound. Release the “Frequency” button and wait
until the bar graph LEDs will stop running.
- the calibration is done.
You might control it after:
- begin generating and leave the emitter head in the air (the red LED
should be on), put the emitter head into the water (the green LED
should be on immediately).
READY signal does not light up Set application time and/or acoustic output.
Emitter head is not connected.
Technical specifications of probe
Effective radiation area (ERA): 1 cm
Accuracy of radiation area:
2
or 4 cm2 (depends on size of head)
± 20 %
Radiation frequency: 1 MHz or 3 MHz
Accuracy of radiation area:
± 10 kHz
Insulation: IP 67
Weight: 0,3 kg approx.
BNR: < 5.0
Contact indication: green/red indicator on probe
Technical specifications of unit
Maximum acoustic power:
continual operation:
pulse operation:
2 W/cm
3 W/cm
2
± 20 %
2
± 20 %
duty cycle: 1:1, 1:2, 1:4, 1:8, 1:16 for frequency 50 Hz or 100 Hz
accuracy of duty cycle:
accuracy of frequency:
Therapy time adjustment:
± 20 %
± 20 %
in the range of 0 - 25 min. (in steps of 0.5 min. up to 10 min.,
and 1 steps from 10 min. up )
Mains voltage: 198 V to 252 V (complies with EN)
50 Hz ± 10 %
Energy input: 50 VA Max
Working conditions:
room temperature
+ 15 °C to + 40 °C
relative humidity: 0 % to 80 %
atmospheric pressure: 700 hPa to 1060 hPa
Storage conditions:
room temperature:
- 10 °C to + 55 °C
relative humidity: 0 % to 85 %
page 9
Page 10

BTL – 07p operating manual & user's guide
atmospheric pressure: 650 hPa to 1100 hPa
Dimensions: 375 x 110 x 225 mm
Weight: 3.5 kg approx.
The unit is designed to comply with
standards
EN 60601-1:1990
EN 55 011
Equipment class: class I
Type B applied part:
BF (symbol
)
Protection: IP 20
Mains transformer fuses used:
primary side (external): 2 x T 250 mA
secondary side (internal): 1 x F 100 mA, 2 x T 250 mA, 2 x T 630 mA
End of therapy indicator: acoustic signal
ON indication: POWER green control light
Proportional contact indication : CONTACT green bar-graph
Error or bad skin contact indication: ERROR and CONTACT red controls
ON/OFF switch marking: 0/1
Standard accessories: 1 ultrasound probe with area 1 cm2
1 ultrasound probe with area 4 cm2
1 bottle ultrasound gel
2 spare fuses (external)
Pulse width
-t
[ms] tp [ms] T [ms] f [Hz] Duty factor
i
10 10 20 50 1:2
5 15 20 50 1:4
2.5 17.5 20 50 1:8
1.25 18.75 20 50 1:16
5 5 10 100 1:2
2.5 7.5 10 100 1:4
1.25 8.75 10 100 1:8
0.625 9.375 10 100 1:16
Important!
Each BTL-07p instrument has its own specific ultrasonic emitter heads that are produced and set only for that
particular unit. Do not use emitter heads from a different BTL-07p unit or an ultrasound unit made by another
producer. Protect the emitter heads from shock or intense cold. Do not bend the cable. Be especially careful
with the emitter head connection area. Regularly disinfect emitter heads with a commonly used disinfectant.
page 10
Page 11

BTL – 07p operating manual & user's guide
II. USER'S GUIDE
Mechanical waves with a frequency higher than 20,000 Hz are called ultrasound. Ultrasound is not generated
electronically for the application of therapy and is classified as mechano-therapy.
Mechanism of action
If a minimal air gap between emitter head and body surface is eliminated, the emitter head vibration will be more
easily transferred deeply into the tissues in the form of longitudinal waves. Every cell in the path of the ultrasonic
"beam" will begin to oscillate: a micro-massage is followed by a transformation from gel to sol (jelly structures
becoming liquefied) and transformation from mechanical to thermal power, with deep warming of tissues.
The amount of heat generated is dependent on the amount of energy that is absorbed. Other effects of ultrasound
(solution degassing, cavitation arising of cavities in humour, and local alkalization) are negligible with the small
intensities and ultrasound doses that are used for physical therapy.
The prophylaxis of ultrasound side-effects must include the knowledge that molecular oscillation occurs not only in
the course of the ultrasonic beam but, as a result of humour transportation to areas that are distant from the
application site, may possibly result in the restoration of former epistaxis or the acceleration of menstruation.
The quality of an ultrasonic beam and its distance from the emitter head determine its characterization as a close
or distant ultrasonic field. Great variation in ultrasound intensity caused by interferential effects and low beam
divergence is typical characteristics of a close ultrasonic field. The length of the close field is directly proportional
to the effective emitting surface of the emitter heads (ERA) and indirectly proportional to the frequency. For
example, the length of a close field with a 4 cm
cm; the length of a close field with a 1 cm
2
2
ERA emitter head and a 1 MHz frequency is 2 cm.
ERA emitter head and a 1 MHz frequency is approximately 10
The characteristics of a distant ultrasonic field are increasing beam divergence, gradual decrease in intensity and
almost no interferential processes.
Therapeutic effects take place mostly in a close field. Since the ultrasonic beam in a close field shows marked
interferential effects (interference of applied and reflected waves, both constructive and destructive), the result is
an uniform ultrasonic beam. The beam’s peaks of intensity (local increase in intensity caused by constructive
interference) may reach values many times higher than the preset value (the rise of stationary waves).
The Beam Non-uniformity Ratio (BNR) illustrates how often peaks of intensity exceed preset values. This value is
characteristic for an ultrasonic head when the frequency is fixed. A good quality head should not exceed 6. With a
preset intensity of 1 W/cm
2
, the intensity should not exceed 6 W/cm2 in any part of the ultrasonic beam.
The BNR of older ultrasonic heads, as well as many of the newer ones (where the producer does not mention
the BNR), is often 20 or more!
The Effective Radiating Area (ERA) is always smaller than the actual surface area of the emitter head (the ERA is
determined by the size of the piezoelectric crystal or ceramic table that generates ultrasound by oscillating). The
dose of ultrasound (amount of power emitted to surface area) is therefore related to the ERA, not to the actual
surface area of the emitter head.
Refraction and reflection of ultrasound follow the laws of wave physics. They originate from ultrasonic wave
transmission between tissues and the differences in vibration flow speed in these tissues. Therapeutic application
must include elimination of the air gap between the emitter head and skin (a 10
ultrasonic wave reflection because of the marked difference in the air and skin flow speed. With a pre-set intensity
of 1.0 W/cm
2
, the tissue receives only 10 mW/cm
2
- energy without any biological effect). Therefore, modern
-9
m thick air gap causes 99 %
ultrasonic heads have a built-in optic and/or acoustic unit that gives a signal and stops the time counter when
contact is insufficient.
Ultrasonic beam power increases (constructive interference) and decreases (destructive interference) occur as a
result of interference in the close field, which reaches its peak (up to 35 %) at the soft tissue-bone boundary.
It is necessary to move the emitter head continuously (see below) to prevent tissue lesions at peaks of intensity.
The BTL-07p signals when there are stationary waves and stops ultrasonic power generation until stationary
waves are eliminated through more rapid movement of the emitter head.
As a result of reflection and constructive interference increases in local intensity and temperature may occur,
particularly in the periosteum-bone boundary. This increase can cause periosteum pain during treatment. When
this occurs, the intensity must be lowered immediately.
Ultrasound is primarily absorbed in deep tissues. Since these tissues contain virtually no thermoreceptors, it is
impossible to perceive a rise in local temperature. Nociceptive receptors are irritated and the patient feels pain
only if the local temperature exceeds 45
ο
C. Most experts agree that a short-lasting local temperature of 45οC
is not dangerous.
As far as classic inflammation (edema, erythema, local temperature increase, pain, and non-function) is
concerned, additional heat production is contraindicated. In certain cases, only a pulse ultrasound (athermic) can
be applied.
In the peracute period of post-traumatic states (up to 24 - 36 hours), even pulse ultrasound application is
contraindicated (resulting vibrations obstruct capillary proliferation and may cause laggard bleeding).
page 11
Page 12

BTL – 07p operating manual & user's guide
Increases in local temperature and micromassage have several physiological effects:
1. Improvement in local circulation resulting in metabolic improvement. Vasodilatation increase follows the
increasing temperature (more evident in continuous ultrasound).
2. Increased permeability of capillaries resulting in quick extravasation humour absorption.
3. Improvement in local circulation and decreased orthosympathic activity, leading to marked muscle relaxation.
4. Local ischemia pain improvement.
5. Transformation from gel to sol occurs as a result of fibrinogen to fibrin transformation, and haematoma and
edema transform to gel. Ultrasound dissolves this gel and hastens reabsorption. Since fibrinogen to fibrin
transformation is a fundamental feature of the healing process (scar formation), we do not recommend the
application of ultrasound during the peracute post-traumatic period.
6. Tissue regeneration improves as a result of the above-mentioned effects.
Ultrasound can also have several negative effects:
1. Tissue lesion - a mechanic and/or thermic tissue lesion can occur when intensity is too strong. Particularly
sensitive is the nervous system (peripheral nerve), which is situated just on the bone (interference) and just
below the surface (close field). If intensity is too strong, flow speed can decelerate in the corresponding nerve,
followed by a total (reversible) impulse flow block and irreversible disintegration of the neuron (myelin coats
are preserved). Bone projections just under the skin (ankles, epicondyles, spondyle spines, etc.) are also
sensitive.
2. Leukocyte mobility impairment is minimized by sufficiently moving of the emitter head.
3. Other negative effects, largely caused by overdoses, are possible: glycemia decline, increased fatigue,
nervousness, changes in appetite, constipation, increased tendency to catch colds (common and severe).
Methods of application
A) Application site and movement of the emitter head
1. Static application: A special holder fixes the emitter head at the application site and emitter head is not
moved. This is the least suitable method because of the possibility of the above-mentioned adverse effects.
2. Semistatic application: Employed when the application site corresponds with the ERA of the emitter head.
The therapist moves the emitter head continuously in a circular pattern.
3. Dynamic application: Employed when the application site is larger than the ERA of the emitter head. The
therapist moves the emitter head in a circular pattern. The application time is prolonged proportionally to the
ERA and the size of the application site.
B) Application site
1. Local application: The ultrasound is applied to the affected site. This is the most common type of application,
and is particularly suitable for the management of muscle spasm, chronic post-traumatic edemas, etc.
2. Segmental application: The ultrasound is applied to the nerve radix outflow of the affected site (e.g., Sudeck
syndrome, morbus Raynaud). This method of application is paravertebral and homolateral, making it suitable
for the management of limb diseases (arms C5 - Th1, legs L3 - S1).
3. Neural application: Based on the effect of flow speed decrease in the peripheral nerve to which ultrasound
has been applied. The boundary between the lowering of conductivity and irreversible nerve damage
(asymptomatic) is very narrow. Neural application is considered risky and indicated infrequently as phantom
pain.
4. Radicular application: Ultrasound is applied to the corresponding spinal cord radix and then to the
manifested Head zone.
C) Contact between emitter head and body surface
1. Direct contact: Provided by a contact medium (a special gel for ultrasound therapy). This method is
considered customary, and it is therefore not necessary to mention it in an ultrasound therapy prescription.
However, because paraffin oil does not conduct electricity, it is useful to use a "conductive gel" for an
ultrasound therapy when giving combined therapy (ultrasound + electrotherapy).
2. Subaqual emission:
Advantages: Subaqual emission employs most of the distant ultrasonic field so that risk of interference is
almost eliminated. In addition, there is no need to apply emitter head pressure against the skin in order to
maintain sufficient contact (the pressure is unpleasant or even painful for a post-trauma patient). Ultrasound
can be applied to interphalangeal joints as well with this method, because treatment is not limited by uneven
surfaces.
Disadvantages: Cumbersome and difficult handling of the special porcelain tanks. Ultrasound application is
limited to acral the body parts. The therapist also risks lesions to the hands if precautions against dipping them
into the water tank during therapy are not followed (due to reflection and interference of the ultrasonic waves).
Some emitter heads (newer ones included) are advertised as water resistant, but neither feature a holder nor
provide a safe subaqual ultrasound treatment. Ultrasound application through a thin-walled rubber bag
(surgical gloves, condom) full of previously boiled water may be a solution. However, this method makes it
page 12
Page 13

BTL – 07p operating manual & user's guide
necessary to eliminate even a minimal air gap between the skin, the bag and the emitter head by using
vaseline or paraffin oil, often considered unnecessarily time-consuming.
Ultrasound frequency
Older instruments operate at a fixed frequency, usually 0.8 - 1 MHz. Newer ones have a choice of frequencies.
The level of frequency is determined by the affected tissue’s location (see above). A frequency of 1 MHz for deep
tissues and 3 MHz for superficial tissues is recommended.
Modes of operation
A/ continuous ultrasound - predominantly deep heat generation in tissues. This form of ultrasound is
contraindicated in inflamed areas and in cases where local warming of the tissue is undesirable.
B/ pulse ultrasound - the shortened impulse time is followed by a decreased pulse-to-period ratio - PPR. As
a result, the thermic effect is suppressed. With a PPR smaller than 1:8, an athermic effect can be expected.
The BTL-07p’s impulse time is shown by a proportional number. This number actually represents a fraction, which
expresses a certain part of the ultrasonic emission period. With a pulse frequency of 100 Hz, the period time is 10
ms. A 1:4 PPR means that the impulse lasts 1/4 of the period (2.5 ms). A pause lasts the rest of the period (7.5
ms).
1:8 PPR - the impulse lasts 1.25 ms (1/8 of 10 ms) and the pause 8.75 ms.
With a pulse frequency of 50 Hz, the period is 20 ms long. 1:4 PPR - the impulse time is 5 ms (1/4 of 20 ms),
pause 15 ms. 1:16 PPR - the impulse time is 1.25 ms (1/16 of 20 ms), pause 18.75 ms.
Emitter head size
The emitter head size determines the effective radiating area - ERA 1 cm
2
(small) and 4 cm
2
(medium - although
some producers consider it large). The choice of emitter head size is determined by the size of the application
site. Ultrasound emission to large areas is difficult for the therapist, lasts too long, and the dose is not applied
consistently.
Small ERA 1 cm
2
emitter heads are used either to manage trigger points and scars or to manage small, uneven
surfaces which have to be treated by the subaqual method if the emitter head size is large.
Application time
Individual application times vary. They largely depend on the stage of the disease or condition. In acute states, an
application lasts 3 minutes; in chronic states, 5 minutes. Application time is then extended using a positive step
method. Application time usually must not exceed 10 minutes. When the application site area is x-times larger
than the emitter head ERA, application time must be prolonged x-times. The dynamic method should be used.
Intensity
An intensity of 0.5 W/cm
0.2 W/cm
2
on the spasmodic fibres of m. temporalis. This muscle is situated just below the surface, on the bone.
Since work is usually performed in a close ultrasonic field, a very low intensity is chosen.
In chronic states, a 0.8 - 1.0 W/cm
Using a positive step method and paying close attention to the patient’s reactions, the intensity is increased.
Continuous ultrasound intensity must not exceed 2.0 W/cm
2
is used initially in acute states. In certain cases it is even lower - e.g. in trismus
2
intensity is initially used.
2
or a pulse ultrasound intensity of 3.0 W/cm2.
It is not recommended to increase two parameters at the same time. If application time is extended, do not
increase intensity. If intensity is increased, do not extend application time.
Procedure frequency
For acute cases: 5 times a week. For chronic cases: 3 times a week. In some cases it is suitable to change the
procedure frequency during the treatment process (e.g. 3 times a day, 3 times every second day).
Total number of treatments
The total number of treatments varies according to individual circumstances, and can range from a single
application prior to myosceletal surgery to 9 applications over a 3-week period for chronic states.
page 13
Page 14

BTL – 07p operating manual & user's guide
Specific contraindications of ultrasonic therapy
A) Absolute
Epiphysis of growing bones
Ultrasound patients risk irreversible growth zone damage, deformity and/or permanent disablement. Since older
types of ultrasound instruments operate at low intensities (displayed data does not correspond with the actual
amount of the energy applied), their use does not lead, in most cases, to growth zone damage. For this reason,
many physicians disagree with this contraindication. Modern stronger and more effective instruments can, in
contrast with the older ones, cause actual growth zone damage, especially when the emitter is not moved
sufficiently. Prevention of this contraindication is the absolute responsibility of the prescribing physician and the
ultrasound therapist.
Gonads
Small doses result in transient and high doses in permanent spermio- or ovogenesis impairment.
Eyes
The use of opthalmic ultrasound instruments is restricted to specialized centers. Physiotherapy must follow the
above-mentioned contraindication.
St. P. laminectomy
Since the spinal cord is not completely covered by an osseous cover after laminectomy, ultrasound application to
the medulla may result in transient or permanent paraparesis DK (when the axons of the spinal cord paths are
disorganized). This is one of the most serious negative effects of physiotherapy.
New bleeding (anywhere)
Since ultrasound waves spread considerably via humours during ultrasound therapy, various side-effects may
occur in spite of the lowered wave energy. For example, by applying ultrasound to a knee, refractory epistaxis can
re-occur.
B) Relative
Brain, Heart, Parenchymatous Organs
There is no reason to apply ultrasound to these organs. In addition, the brain is covered by the cranium. However,
an article was published about a person who irradiated his sinuses while applying ultrasound to his own knee. This
patient died because of massive bleeding in the forehead lobe, as the calcified atheroma plate was disturbed. It is
widely believed that this was not an accident. This information is included only as a strong reminder to the
therapist that ultrasound is not to be used in these areas. A patient must never apply ultrasound to himself or
herself, even if the application site can be reached easily.
Peripheral Nerves (situated just below the surface, on the bone)
This group includes: n. ulnaris in the elbow area, volar areas of the wrist, inguines, the areas under the external
and internal ankles, etc.
As a result of constructive interference (stationary waves), local intensity peaks occur in all of the abovementioned areas. Intensity peaks lead to impulse flow speed prolongation and irreversible destruction of nerve
fibres. Muscular fibres and myelin covers of the damaged nerves are usually preserved.
Bone projections just under the skin: - spinous projections of the spondyles, ankles, condyles, and
epicondyles.
This is again a commonly ignored contraindication. Many experts consider ultrasonic therapy to be an
epicondylitis treatment. This is only true insofar as ultrasound application to a corresponding muscular group
(extensoric if lateral, flexoric if there is ulnar epicondylitis) is also taking place. Direct ultrasound application to a
painful attachment often leads to increased pain, but more often leads to the process of chronification (the same
effect as that of numerous massive local corticosteroid applications).
Similarly, the application of ultrasound directly to the spine often results in refractory periosteum pain around
spinal projections.
Emphysema, Bronchiectasis (via ultrasound therapy on the chest)
Menses
This contraindication is considered absolute as far as the hypogastrium area is concerned. Before ultrasound is
applied to a different area, the patient should be told that intensity of menstruation might increase (more often in
menstruation acceleration than in the form of metrorrhagia). If the anamnesis shows that an ultrasound application
may adversely affect menstruation, the therapist should refuse to carry out the procedure and suggest that the
patient consult her physician.
page 14
Page 15

BTL – 07p operating manual & user's guide
Procedure Prescription
Name, surname, date of birth, insurance company
Name and number of diagnosis and stage of disease
Name of procedure - ultrasound + the form. PPR (if pulse ultrasound is used)
Form of application: Dynamic, Local
Emitter head size (ERA)
Intensity and changes of intensity during treatment (step); highest tolerable level
Application time and application changes during treatment (step); longest time tolerated
Frequency of procedure and its changes during treatment
Total number of procedures
Date of next appointment
Date of prescription, name and signature of prescribing physician
Facultative features of the prescription
Patient's position, contact medium, additional information for the physiotherapist.
Instructions for a patient
Ultrasound therapy is mostly asymptomatic, but a sensation of moderate heat or warmth may be felt in the treated
area. A burning sensation on the skin during therapy indicates insufficient contact. Pain during application
indicates either an overdose or insufficient movement of the emitter head. In the case of an overdose, stop the
procedure immediately and inform prescribing physician. Therapy can be resumed at a lower intensity, usually
after a one-day break.
After the first treatment, a transient deterioration of the disease may occur. A marked improvement should occur
not later than the third application. If there is no improvement (in acute and subacute states), ultrasound therapy
should not be continued.
If ultrasound therapy is applied to chronic processes (which rarely happens) or to change the mechanical qualities
of tissues (e.g., Dupuytren's contracture or plantar aponeurosis related to calcar calcanei), impressive results
cannot be expected by the third application. If ultrasound therapy is not immediately followed by a manual therapy,
results should not be expected, even after the tenth application.
Procedure
1. Inform the patient about the procedure. NEVER LET PATIENTS APPLY THE ULTRASOUND
TO THEMSELVES!
2. It is unnecessary to inform patients about rare contraindications unless such information is specifically
requested. However, be sure to ask if epistaxis is present or if patient is menstruating.
3. Place the patient in the proper position for the therapy.
4. Use a sufficient amount of the appropriate contact medium.
5. Set the prescribed intensity and time, apply the emitter head, and switch on the ultrasound.
6. Move the emitter head continuously in accordance with the prescribed application.
7. Repeatedly ask the patient about his or her sensations. If he or she feels a burning sensation, add more
contact medium. If pain occurs, lower the intensity. If necessary, interrupt the procedure and inform the
prescribing physician.
8. After the prescribed time has elapsed, lower the intensity and switch the instrument off. Most instruments
switch off automatically.
9. Clean the contact medium off the patient and dry the skin.
A therapeutic example
Large edema in outer ankle region; two days after distortion; high palpatory soreness (tenderness), X-ray
negative.
Dg.: Distorsio art. talocruralis l.dx. Hematoma gravis reg. condyl.
fibul. l.dx. S 90.0 sub-acute
Pulse ultrasound, PPR 1:8 (heat generation would exasperate both the condition and the healing process).
Frequency 3 MHz (superficial process).
Subaqual, semistatic application. Emitter head distance: 10 cm (for local soreness, sufficient contact can not be
made. In addition, a close ultrasonic field must not be applied to a bony projection situated just under the skin.)
Emitter head size (ERA): 4 cm
Water temperature: 20οC. (Simultaneous negative thermotherapy for subacute states)
Intensity: 2.0 - 3.0 W/cm
2
2
, step 0.2 W/cm
2
(A subacute process usually calls for a lower intensity. However, in this
case, the use of pulse ultrasound is most important with a distant ultrasonic field where intensity is at least two
times lower).
Application time: 6 minutes. Irradiated area is approximately twice larger than the emitter head ERA. The shortest
time for acute states is twice 3 minutes. Since intensity increases in increments, length of time should not.
Frequency of procedures: At first, three procedures daily, after that every second day. As the condition changes
from subacute to subchronic, pauses between procedures are lengthened in order to give the organism a better
opportunity to heal itself.
Total number of procedures: 5
page 15
Page 16

BTL – 07p operating manual & user's guide
Combined therapy
Combined therapy is the application of two or more kinds of energy. Classic diadynamic currents comprised of
simultaneous low frequency galvanic and pulse currents are also considered a form of combined therapy.The
procedure generally includes the following combinations:
ultrasound + low frequency currents
ultrasound + amplitude modulated mid-frequency currents
ultrasound + TENS
Ultrasound and low frequency currents
Can be used with one unit or by connecting two separate units (BTL-06 + BTL-07p). The desired current with
an adjustable intensity should be brought to the emitter head. The other electrode is placed opposite the emitter
head so that the ultrasound field and the low frequency current are both located in the treatment area.
Mechanism of action
The myorelaxation is effective, if the proper frequency (100 - 200 Hz) is used. The combined therapy with a 3 MHz
ultrasound frequency is suitable especially for treating the located myospasm, uncoordinated muscle fibres and
the trigger points.
The risk of galvanic effect is heightened. It can be seen on the emitter head rather than on the skin. To guarantee
the patient’s safety it is necessary to be aware of this, especially if higher frequencies are used.
Application time
Usually 3 - 6 minutes. The application time can be extended with the positive step method. In acute states or in
cases when the treatment area is small, the length of the therapy should be reduced.
Intensity
Set the ultrasound intensity at 0.5 - 0.7 W/cm
2
for continuous ultrasound and at a max. 1.0 W/cm2 for a pulse
ultrasound with 1:2 PPR or greater. Set the low frequency component intensity according to the object.
When searching for the trigger points, set the threshold sensitive intensity outside the area where reflex changes
are expected and with this intensity try to get as close as possible to the area. The intensity will be above
threshold sensitive in a hyperalgeic zone, and the patient may even feel pain. The threshold motor and above
threshold motor pre-set intensity evokes a motor response. If the pain threshold is not reached, use the same
intensity for the therapy. Otherwise adjust the low frequency component intensity according to the current used
and effect desired.
The size of the indifferent desk electrode should be 2x - 10x larger so that the sensitivities are located on
the ultrasound margin.
Total number of procedures
A total of 2 - 3 treatments is recommended, based on the indication + effect. Five or more treatments are
recommended only in special cases.
Frequency of procedures
Daily or as a pre-medication (postisometric relaxation-PPR).
Procedure Prescription
Name, surname, date of birth, insurance company.
Name and number of diagnosis and stage of disease.
Name of procedure, type of the unit (BTL-06 + BTL-07p).
Emitter head size, frequency, characteristic and intensity of the ultrasound component, mode of application.
Characteristics of the low frequency component, therapeutic intensity.
Treatment location. Placement and indifferent electrode size.
Application time and application changes during treatment (step).
Frequency of procedure and changes during treatment.
Total number of procedures.
Date of next appointment.
Date of prescription, name and signature of prescribing physician.
page 16
Page 17

BTL – 07p operating manual & user's guide
A therapeutic example
Epicondilitis radialis subchronica of a typist. There is a trigger point in the middle of m. extensor carpi radialis
brevis.
Epicondilitis radialis humeri l.dx., M 77.1, subchronica (Sch)
Combined therapy (BTL-06 + BTL-07p)
BTL-07p: f = 3MHz, 1:4 PPR, 0.8 W/cm
2
- 1.2 W/cm2, emitter head ERA = 4 cm2, semistatic application
BTL-06: faradic surge, 150 Hz, 3/3 (program 0254), threshold motor
Location: right forearm extensors, trigger point in the middle of m.extensor carpi radialis brevis.
Indifferent electrode at least 6 x 6 cm on the right forearm flexors
Application time: 4 minutes
Number of treatments: 3, daily application
Ultrasound + amplitude modulated mid-frequency currents
The mid-frequency currents have no galvanic effects,and better tolerance. They have a deeper effect hence can
be used for changing reflexes in deep muscles. Use a 1 MHz ultrasound frequency when treating deeply
underlying muscles.
The combination of the BTL-06 and BTL-07p offers a selection of ultrasound parameters and amplitude
modulations Hence these currents can be used for surface muscles (at a 3 MHz frequency) as well as deep
muscles (at a 1 MHz frequency)
Mechanism of action
Same as the ultrasound/electrotherapy combination (see above). Optimal myorelaxation is attained at
150 - 180 Hz frequencies (The effectiveness of myorelaxation, unlike that of diadynamic current, is not lowered by
a 50 Hz frequency. (MF - DD current).
Use the continuous ultrasound if improving the myorelaxation by increasing the temperature. If you want to point
out the micro-massage or if hyperthermia is not indicated, use the pulse ultrasound.
Application time
3 - 10 minutes. Using the positive step method after 1 minute is recommended. The application time for
the semistatic method refers to the affected area, whose surface is equal to the emitter head ERA. The application
time for dynamic method should be x times longer because the affected area is x times larger than the emitter
head ERA.
An initial intensity of 0.4 - 0.6 W/cm
intensity 0.5 - 1.0 W/cm
2
and for 1:8 - 1:16 PPR use the initial intensity 1.0 - 1.3 W/cm2.
2
is used for continuous ultrasound (1:1 PPR). For 1:2 - 1:4 PPR use the
The AMP intensity is chosen according to the effect. The above threshold sensitive intensity principally has an 100
Hz amplitude modulation analgetic effect. Use the threshold motor intensity for an optimum myorelaxation
modulation 150 - 180 Hz effect. The patient should not feel any pain or burning in hyperallergenic zones or at
trigger points during the application. If the application becomes painful, set the lower ultrasound intensity (include
this in the patient‘s medical record and make sure the patient‘s doctor does an immediate check-up on the
patient). If a burning sensation is felt on the trigger point, set the lower mid-frequency component intensity, add
the desired contact medium (it is not necessary to inform the patient‘s doctor).
Number of procedures
Usually 3 - 6 treatments. Written justification must be given in the patient‘s medical record for a greater number of
treatments. Three applications are recommended for a status acutus in deeply lying muscles. More applications
for usual status subacutus or subchronicus. Therapy may be continued if the effect is good and no causal therapy
is available.
Procedure frequency
Apply daily for status acutus. For status subchronicus the frequency may be changed within one cure period
(3 times a day, later 3 times every second day).
Procedure prescription
Same as the ultrasound/electrotherapy combination (see above).
A therapeutic example
Inner incoordination in m.piriformis with persistent entezopathy of the right iliac joint
Inner incoordination of m.piriformis l.dx. with entezopathy in the iliac area, M76.7, subchronica (Sch)
Combined therapy ultrasound + AMP with the BTL-06 + BTL-07p
Ultrasound: 1MHz, emitter head 4 cm
2
, 1:4 PPR, 0.5 - 1.0 W/cm2, semistatic application
page 17
Page 18

BTL – 07p operating manual & user's guide
AMP: FM 90 - 140 Hz, fluently 3/3/3 - program 0945, threshold motor sensitive intensity
M.piriformis l.dx.;indifferent electrode minimum 6 x 6 cm, lateral on the right thigh (tr.iliotibialis)
Application time: 6 minutes (for ultrasound frequency use the step method; if the ultrasound intensity is fixed
the application time can be 5 - 10 minutes, step 1 minute)
Frequency: First, 3 procedures daily, later every second day
Total number of treatments: 6
Ultrasound + TENS (transcutaneous electrostimulation)
While emphasis was placed on myorelaxation, therapy of hyperalgetic zones and trigger points in the
aforementioned types of combined therapy, a combined US and TENS treatment is applied as a general
analgesic, not only for the above mentioned reflex changes but also for other kinds of pains. In these cases, we
recommend that you review the list of pains that ultrasound can treat because not every pain can be treated with
an ultrasound. The combined US and TENS treatment can be used for myalgia (post-injury, reflexive, etc.), posttraumatic pain (after 24 - 36 hours), lege artis during the whole therapy (relaxation, decompression, etc.) The
preferred TENS impulses are symmetric biphasal or alternating biphasal impulses - program numbers 10, 11, 13,
14, 16, and 17 (the galvanic effect is omitted). When the degree of pain is small, use continual (conventional) or
random TENS; when the degree of pain is greater, use a basic TENS 100 Hz frequency and 2-8 Hz burst
frequency. The intensity should always be as high as the patient can stand it. This combination will have a faster
effect than other sequential procedures. However, it is important to keep in mind all the contraindications for
ultrasound (see Operator’s Manual - Ultrasound).
Mechanism of action
Reducing the perception of pain positively affects the trophic in the injured area. The simultaneous ultrasound
application followed by increased capillary permeability, improved extravasal liquid absorbtion,
increased vasoactive amines secretion and the influence on the pre-capillar spfincters are considered the most
effective prevention against the algodystrophic syndrom. Physical therapy in the porouses area is contraindicated.
Use the segmental method only for trophicus.
Application time
Status acutus : 3 - 5 minutes.
Status subacutus : 3 - 10 minutes (you may use the positive step method).
Intensity
The ultrasound intensity - see above. The continuous TENS intensity abovethreshold sensitive - at the highest
tolerable level, TENS burst at highest tolerable level. Use the TENS surge with the above threshold motor
intensity for the trigger points or application to spastic muscles.
Total number of treatments
Individual, usually 1 - 6 treatments in one therapy.
Frequency of treatment
Usually daily application. In selected cases, every second day as the sessions come to an end. In segemental
long term treatments(sy. Sudeck, for example)., we recommend ending the therapy by slowly decreasing the
frequency of treatments (three times a week, twice a week, once a week and then ending the therapy
Procedure prescription
Same as the ultrasound + low frequency therapy combination (see above).
A therapeutic example
Large haematoma in m.quadriceps femoris after contusion, more than 24 hours after injury, very painful.
Haematoma gravis reg.m.quadricipitis fem. l. sin.,S 70.1, acutus
Combined therapy ultrasound + TENS burst (BTL-06 + BTL-07p)
Ultrasound: 1MHz, 1:16 PPR, 1 W/cm
TENS: burst, symetric biphase impulse, f = 100 Hz, f
2
, emitter head 4 cm2, semistatic application
= 5 Hz = program 1332, intensity at the highest tolerable
burst
level
Location: Haematoma on the anterior surface of the left thigh, indifferent electrode minimum 6x6 cm on
the posterior surface of the thigh opposite the haematoma
Application time: 2-10 minutes, step 2 minutes
Freqency: First, 3 procedures daily, later every second day
Total number of procedures: 5
page 18
Page 19

BTL – 07p operating manual & user's guide
III. LIST OF PROGRAM NUMBERS FOR ULTRASOUND THERAPY
List of diagnoses
1 Arthritis rheumatoides
2 Arthritis rheumatoides (subaqualis)
3 Arthrosis chronica
4 Arthrosis chronica (inactiva)
5 Arthrosis subchronica
6 Bursitis acuta
7 Bursitis chronica
8 Bursitis subacuta
9 Cicatrix acuta
10 Cicatrix cheloidum
11 Cicatrix subacuta
12 Decubitus
13 Distensio muscularis acuta
14 Distensio muscularis profundus
15 Distorsio acuta
16 Distorsio acuta (subaqualis)
17 Distorsio chronica
18 Distorsio subacuta
19 Epicondylitis acuta
20 Epicondylitis chronica
21 Epicondylitis subacuta
22 Haematoma chronica
23 Haematoma subacuta
24 Haematoma subchronica
25 Myalgia
26 Myorelaxatio
27 Myospasmus
28 Oedema chronica
29 Oedema subacuta
30 Oedema subchronica
31 Spondylarthrosis ancylopoetica (M. Bechterevi)
32 Sy. algodystrophicus (Sy. Sudeck)
33 Tendinitis acuta
34 Tendinitis acuta (subaqualis)
35 Tendinitis chronica
36 Tendinitis subacuta
37 Tendinitis subacuta (subaqualis)
38 Tendovaginitis acuta
39 Tendovaginitis acuta (subaqualis)
40 Tendovaginitis chronica
41 Tendovaginitis subacuta
42 Tendovaginitis subacuta (subaqualis)
43 Trigger points profundus
44 Trigger points superficialis
45 Ulcus cruris
46 Vasoneurosis universalis (M. Raynaud)
page 19
Page 20

BTL – 07p operating manual & user's guide
1. Arthritis rheumatoides
2
Emitter head: 1 cm
. Frequency: 3 MHz, 1:4 PPR. Intensity: 0.8 - 1.2 W/cm2, step 0.1 W/cm2. Semistatic
application.
Application time: 5 minutes, 2 - 3x a week. Total number of treatments: 6 - 10.
2. Arthritis rheumatoides (subaqualis)
Emitter head: 4 cm2. Frequency: 1 MHz, 1:2 PPR. Intensity: 1.0 - 2.0 W/cm2, step 0.1 W/cm2.
Application time: 5 minutes, 2 - 3x a week. Total number of treatments: 6 - 10.
Subaqual application: Emitter head distance 10 - 12 cm. Water temperature 36
o
C.
3. Arthrosis chronica
2
Emitter head: 4 cm
. Frequency: 3 MHz, 1:2 PPR. Intensity: 1.2 W/cm2. Semistatic application.
Application time: 5 - 8 minutes, 0.5 minute steps, 3x a week. Total number of treatments: 6 - 9.
Apply to edema. Patient must feel no pain during application.
4. Arthrosis chronica (inactiva)
Emitter head: 4 cm2. Frequency: 1 MHz, 1:2 PPR. Intensity: 1.0 - 2.0 W/cm2, step 0.2 W/cm2. Dynamic
application.
Application time: 10 minutes, 3x a week. Total number of treatments: 6 - 9.
Apply to the whole affected joint. For joints situated just under the surface, the 3 MHz frequency is recommended.
5. Arthrosis subchronica
Emitter head: 4 cm
2
. Frequency: 3 MHz, 1:4 PPR. Intensity: 0.8 - 1.5 W/cm2, step 0.1 W/cm2. Semistatic
application.
Application time: 4 minutes daily, 5x a week. Total number of treatments: 5 - 6.
Apply to edema. Patient must feel no pain during application.
6. Bursitis acuta
Emitter head: 4 cm
2
. Frequency: 1 MHz, 1:8 PPR. Intensity: 1.2 W/cm2. Semistatic application.
Application time: 1 - 3 minutes, 0.5 minute steps, daily, 5x a week. Total number of treatments: 3 - 5.
Apply to edema. Pain must not be aggravated.
7. Bursitis chronica
Emitter head: 4 cm2. Frequency: 1 MHz, 1:1 PPR. Intensity: 1.0 W/cm2. Semistatic application.
Application time: 5 minutes, 1 minute steps, 3x a week. Total number of treatments: 6 - 9.
Lower intensity if pain is aggravated.
8. Bursitis subacuta
2
Emitter head: 4 cm
. Frequency: 1 MHz, 1:4 PPR. Intensity: 1.2 W/cm2. Semistatic application.
Application time: 3 - 6 minutes, 1 minute steps, 3 - 5x a week. Total number of treatments: 3 - 5.
Apply to edema. Pain must not be aggravated during the application.
9. Cicatrix acuta
Emitter head: 1 cm
2
. Frequency: 3 MHz, 1:4 PPR. Intensity: 0.5 - 1.0 W/cm2, step 0.1 W/cm2. Semistatic
application.
Application time: 4 minutes, 2x a day, 5x a week. Total number of treatments: 2 - 5.
It is necessary to obey the principles of asepsis.
10. Cicatrix cheloidum
Emitter head: 1 cm
2
. Frequency: 3 MHz, 1:2 PPR. Intensity: 1.5 - 2.5 W/cm2, step 0.2 W/cm2. Semistatic
application.
Application time: 3 minutes, 2 - 3x a week. Total number of treatments: 3 - 6 (more, if effect is positive).
This procedure should be followed with manual techniques (compressive massage, fascia techniques, etc.).
page 20
Page 21

BTL – 07p operating manual & user's guide
11. Cicatrix subacuta
2
Emitter head: 1 cm
. Frequency: 3 MHz, 1:2 PPR. Intensity: 0.5 - 1.0 W/cm2, step 0.1 W/cm2
Application time: 4 minutes, 3 - 5x a week. Total number of treatments: 3 - 5.
It is necessary to obey the principles of asepsis.
12. Decubitus
Emitter head: 4 cm
2
. Frequency: 3 MHz, 1:4 PPR. Intensity: 0.8 W/cm2. Semistatic application.
Application time: 5 minutes, 3 - 5x a week.
Apply only to the edge of the decubitus. Lower intensity if pain is aggravated.
13. Distensio muscularis acuta
Emitter head: 4 cm
Application time: 5 - 7 minutes, 1 minute steps, daily. Total number of treatments: 3.
Emitter head distance 10 - 12 cm. Water temperature 20
2
. Frequency: 1 MHz, 1:8 PPR. Intensity: 2.0 W/cm2. Subaqual application.
o
C.
14. Distensio muscularis profundus
2
Emitter head: 4 cm
. Frequency: 3 MHz, 1:1 PPR. Intensity: 1.0 - 2.0 W/cm2, step 0.2 W/cm2. Semistatic
application.
Application time: 5 minutes, 3x a week.
Use 1 MHz frequency for deeper sites.
15. Distorsio acuta
Emitter head: 4 cm
2
. Frequency: 3 MHz, 1:4 PPR. Intensity: 0.8 W/cm2. Semistatic application.
Application time: 3 minutes, daily, 5x a week. Total number of treatments: 3 - 5.
Apply to edema.
16. Distorsio acuta (subaqualis)
Emitter head: 4 cm
Application time: 5 - 7 minutes, 1 minute steps, daily. Total number of treatments: 3.
Subaqual application: Emitter head distance 10 - 12 cm. Water temperature 20
2
. Frequency: 1 MHz, 1:8 PPR. Intensity: 2.0 W/cm2.
o
C.
17. Distorsio chronica
2
Emitter head: 4 cm
. Frequency: 3 MHz, 1:1 PPR. Intensity: 1.0 - 1.5 W/cm2. Semistatic application.
Application time: 5 minutes, 3x a week. Total number of treatments: 6 - 9.
Apply to chronic edema.
18. Distorsio subacuta
Emitter head: 4 cm
2
. Frequency: 3 MHz, 1:1 PPR. Intensity: 1.0 W/cm2. Semistatic application.
Application time: 5 minutes, 3x a week. Total number of treatments: 3 - 5.
Apply to edema.
19. Epicondylitis acuta
Emitter head: 4 cm
2
. Frequency: 3 MHz, 1:8 PPR. Intensity: 1.2 W/cm2. Semistatic application.
Application time: 3 minutes, 5x a week. Total number of treatments: 3 - 5.
Localize irradiation to the muscular group of the affected epicondyle.
Direct application of ultrasound to the epicondyle is contraindicated!
20. Epicondylitis chronica
Emitter head: 1 cm. Frequency: 3 MHz, 1:2 PPR. Intensity: 1.0 - 2.0 W/cm2, step 0.2 W/cm2. Semistatic
application.
Application time: 5 minutes, 3x a week. Total number of treatments: 5 - 15 (must be followed by post-isometric
relaxation of the corresponding muscular group).
Apply to fibres with inner incoordination or to previously diagnosed trigger points.
Direct application of ultrasound to the epicondyle is contraindicated!
21. Epicondylitis subacuta
Emitter head: 1 cm
2
. Frequency: 3 MHz, 1:2 PPR. Intensity: 1.5 W/cm2. Semistatic application.
page 21
Page 22

BTL – 07p operating manual & user's guide
Application time: 3 - 5 minutes, 1 minute steps, 3 - 5x a week. Total number of treatments: 6 - 9.
Apply to fibres with inner incoordination or to previously diagnosed trigger points.
Direct application of ultrasound to the epicondyle is contraindicated!
22. Haematoma chronica
2
Emitter head: 4 cm
. Frequency: 3 MHz, 1:1 PPR. Intensity: 1.0 - 1.2 W/cm2, step 0.1 W/cm2. Dynamic
application.
Application time: 4 minutes, 3x a week. Total number of treatments: 3 - 6.
23. Haematoma subacuta
Emitter head: 4 cm
2
. Frequency: 3 MHz, 1:4 PPR. Intensity: 1.0 - 2.0 W/cm2, step 0.1 W/cm2. Dynamic
application.
Application time: 4 minutes, 3 - 5x a week. Total number of treatments: 3 - 5.
24. Haematoma subchronica
Emitter head: 4 cm
2
. Frequency: 3 MHz, 1:2 PPR. Intensity: 1.0 - 2.0 W/cm2, step 0.1 W/cm2. Dynamic
application.
Application time: 4 minutes, 3 - 5x a week. Total number of treatments: 3 - 5.
25. Myalgia
Emitter head: 4 cm
step 0.2 W/cm
2
. Frequency: 1 MHz (for superficial muscles 3 MHz), 1:1 PPR. Intensity: 1.5 - 2.0 W/cm2,
2
. Dynamic application.
Application time: 5 minutes, 3 - 5x a day. Total number of treatments: 5 - 8.
In order to have long-term effect physiotherapy must immediately follow irradiation.
26. Myorelaxatio
Emitter head: 4 cm
0.2 W/cm
2
. Dynamic application.
2
. Frequency: 1 MHz (for superficial muscles: 3 MHz), 1:1 PPR. Intensity: 1.5 - 2.0 W/cm2, step
Application time: 5 minutes, 3 - 5x a day. Total number of treatments: 5 - 8.
In order to have long-term effect physiotherapy must immediately follow irradiation.
27. Myospasmus
Emitter head: 4 cm
0.2 W/cm
2
. Dynamic application.
2
. Frequency: 1 MHz (for superficial muscles: 3 MHz), 1:1 PPR. Intensity: 1.5 - 2.0 W/cm2, step
Application time: 5 minutes, 3 - 5x a day. Total number of treatments: 5 - 8.
In order to have long-term effect physiotherapy must immediately follow irradiation.
28. Oedema chronica
Emitter head: 4 cm
2
. Frequency: 3 MHz, 1:1 PPR. Intensity: 1.0 - 1.2 W/cm2, step 0.1 W/cm2. Dynamic
application.
Application time: 4 minutes, 3x a week. Total number of treatments: 3 - 6.
29. Oedema subacuta
Emitter head: 4 cm
2
. Frequency: 3 MHz, 1:4 PPR. Intensity: 1.0 - 1.2 W/cm2, step 0.1 W/cm2. Dynamic
application.
Application time: 4 minutes, 3 - 5x a week. Total number of treatments: 3 - 5.
30. Oedema subchronica
Emitter head: 4 cm
2
. Frequency: 3 MHz, 1:2 PPR. Intensity: 1.0 - 1.2 W/cm2, step 0.1 W/cm2. Dynamic
application.
Application time: 4 minutes, 3 - 5x a week. Total number of treatments: 3 - 5.
page 22
Page 23

BTL – 07p operating manual & user's guide
31. Spondylarthrosis ancylopoetica (M. Bechterevi)
2
Emitter head: 4 cm
. Frequency: 1 MHz, 1:1 PPR. Intensity: 1.0 - 2.0 W/cm2, step 0.1 W/cm2. Dynamic
application.
Application time: 15 minutes, 3x a week. Total number of treatments: 9 - 12.
Apply to paravertebral fornix to the most stiff or painful region. In order to have a long-term effect, physiotherapy
must immediately follow irradiation.
Irradiation of the vertebral spine is contraindicated!
32. Sy. algodystrophicus (Sy. Sudeck)
Emitter head: 4 cm
2
. Frequency: 3 MHz, 1:2 PPR. Intensity: 1.0 W/cm2. Dynamic application.
Application time: 15 minutes, 5x a week for clinically diagnosed algodystrophy, 2x a week for incipient
algodystrophy.
For treatment of arms, use ultrasound on C5 - Th1 region homolaterally (segmental application), for treatment of
legs, L2 - L5 region.
Direct (local) irradiation of the affected area is absolutely contraindicated!
The vertebral spine must not be irradiated when employing segmental application!
33. Tendinitis acuta
Emitter head: 1 cm
2
. Frequency: 3 MHz, 1:16 PPR. Intensity: 1.0 - 2.0 W/cm2, step 0.2 W/cm2. Semistatic
application.
Application time: 3 minutes, 5x a week. Total number of treatments: 2 - 5.
Treatment must include immobilization.
34. Tendinitis acuta (subaqualis)
Emitter head: 4 cm
Application time: 4 minutes, 5x a week. Total number of treatments: 2 - 5.
Subaqual application: Emitter head distance 10 - 12 cm. Water temperature 18 - 25
2
. Frequency: 1 MHz, 1:8 PPR. Intensity: 1.0 - 2.0 W/cm2, step 0.2 W/cm2.
o
C.
Treatment must include immobilization.
35. Tendinitis chronica
Emitter head: 4 cm2. Frequency: 3 MHz, 1:1 PPR. Intensity: 1.0 - 1.5 W/cm2, step 0.1 W/cm2. Semistatic
application.
Application time: 5 minutes, 2 - 3x a week. Total number of treatments: 5 - 10.
Treatment must include physiotherapy.
36. Tendinitis subacuta
Emitter head: 4 cm
2
. Frequency: 3 MHz, 1:4 PPR. Intensity: 1.0 - 2.0 W/cm2, step 0.2 W/cm2. Semistatic
application.
Application time: 5 minutes, 3 - 5x a week. Total number of treatments: 3 - 5.
37. Tendinitis subacuta (subaqualis)
Emitter head: 4 cm
Application time: 5 minutes, 3 - 5x a week. Total number of treatments: 3 - 5.
Subaqual application: Emitter head distance 10 - 12 cm. Water temperature: 35
2
. Frequency: 1 MHz, 1:2 PPR. Intensity: 1.5 - 2.5 W/cm2, step 0.2 W/cm2.
o
C.
38. Tendovaginitis acuta
2
Emitter head: 1 cm
. Frequency: 3 MHz, 1:16 PPR. Intensity: 2.0 - 2.5 W/cm2, step 0.1 W/cm2. Semistatic
application.
Application time: 2 minutes, 2x a day, 5x a week. Total number of treatments: 3 - 5.
39. Tendovaginitis acuta (subaqualis )
Emitter head: 4 cm
2
. Frequency: 1 MHz, 1:4 PPR. Intensity: 1.5 - 2.5 W/cm2, step 0.2 W/cm2.
Application time: 4 minutes, 2x a day - 5x a week. Total number of treatments: 3 - 5.
Subaqual application: Emitter head distance: 10 - 12 cm. Water temperature: 18 - 25
40. Tendovaginitis chronica
2
Emitter head: 4 cm
. Frequency: 3 MHz, 1:1 PPR. Intensity: 1.5 - 2.5 W/cm2, step 0.2 W/cm2. Semistatic
application.
page 23
o
C.
Page 24

BTL – 07p operating manual & user's guide
Application time: 5 minutes, 2 - 3x a week. Total number of treatments: 5 - 15.
Physiotherapy must follow.
41. Tendovaginitis subacuta
Emitter head: 4 cm2. Frequency: 3 MHz, 1:4 PPR. Intensity: 1.0 - 1.5 W/cm2, step 0.1 W/cm2. Semistatic
application.
Application time: 5 minutes, 3 - 5x a week. Total number of treatments: 3 - 5.
42. Tendovaginitis subacuta (subaqualis)
Emitter head: 4 cm
Application time: 5 minutes, 3 - 5x a week. Total number of treatments: 3 - 5.
Subaqual application: Emitter head distance 10 - 12 cm. Water temperature: 18 - 25
2
, Frequency: 1 MHz, 1:4 PPR. Intensity: 2.0 - 2.5 W/cm2, step 0.1 W/cm2.
o
C.
43. Trigger points profundus
2
Emitter head: 1 cm
. Frequency: 1 MHz, 1:4 PPR. Intensity: 2.0 - 3.0 W/cm2, step 0.2 W/cm2. Semistatic
application.
Application time: 2 - 3 minutes per trigger, 2x a day - 5x a week.
Corresponding myoskeletal technique should immediately follow irradiation.
Apply to the triggers that feature typical radiation when detected by either palpation or combined therapy.
44. Trigger points superficialis
Emitter head: 1 cm
2
. Frequency: 3 MHz, 1:4 PPR. Intensity: 0.5 - 1.0 W/cm2, step 0.1 W/cm2. Semistatic
application.
Application time: 2 minutes per trigger, 2x a day - 5x a week.
Trigger points are severely sore points, usually situated in the affected area.
Myoskeletal technique should immediately follow irradiation.
45. Ulcus cruris
Emitter head: 1 or 4 cm
2
(considering the size of the ulcer). Frequency: 3 MHz, 1:4 PPR. Intensity: 0.8 W/cm2.
Dynamic application.
Application time: 4 - 7 minutes, 0.5 minute steps, daily, 5x a week.
Apply only to the edges of the ulcer. If pain is aggravated during application, lower the dose.
46. Vasoneurosis universalis (M. Raynaud)
Emitter head: 4 cm
2
. Frequency: 3 MHz, 1:2 PPR. Intensity: 1.0 W/cm2. Segmental application (C5 - Th1 region
homolaterally, HK or DK in L3 - L5 region bilaterally).
Application time: 15 minutes, 3x a week the first week, then 2x a week. Total number of treatments: 5 - 15.
page 24
Page 25

BTL – 07p operating manual & user's guide
IV. LIST OF PROGRAM NUMBERS FOR COMBINED ULTRASOUND THERAPY/ELECTROTHERAPY
51 Lumbalgie
52 Myalgia mm. superficiales
53 Myalgia mm. profundi
54 Relaxatio mm. superficiales
55 Relaxatio mm. profundi
56 Trigger points mm. superficiales
57 Trigger points mm. profundi
58 Zona hyperalgesica
page 25
Page 26

BTL – 07p operating manual & user's guide
List of program numbers for combined ultrasound therapy/electrotherapy
51. Lumbalgie
Emitter head: 4 cm2. Frequency: 3 MHz, 1:4 PPR. Intensity: 0.5 W/cm2.
Electrotherapy: TENS cont., f = 100 Hz constant (program 1625).
Contralateral electrode placement.
Intensity above threshold sensitive.
Application time: 1 - 5 minutes, step 1 minute, daily. Total number of treatments: 3 - 5.
52. Myalgia mm. superficiales
Emitter head: 1 cm
2
. Frequency = 3 MHz, 1:2, 1:4 PPR. Intensity: 0.5 W/cm2.
Electrotherapy: DF, base 1 mA (program 0113).
Contralateral electrode placement.
Intensity above threshold sensitive.
Application time: 1 - 2 minutes, max. 6 minutes, daily. Total number of treatments: 2 - 3.
53. Myalgia mm. profundi
Emitter head: 1 cm
2
. Frequency = 1 MHz, 1:2, 1:4 PPR. Intensity: 1.5 - 1.7 W/cm2, step 0.1 W/cm2.
Electrotherapy: DF, base 1 mA (program 0113).
Contralateral electrode placement.
Intensity above threshold sensitive.
Application time: 1 - 2 minutes, max. 6 minutes, daily. Total number of treatments: 3 - 5.
54. Relaxatio mm. superficiales
Emitter head: 1 cm
2
. Frequency = 3 MHz, 1:1, 1:2, 1:4 PPR. Intensity: 0.5 - 1.0 W/cm2, step 0.1 W/cm2.
Electrotherapy: TENS cont., f = 100Hz (program 1725)
Contralateral electrode placement.
Intensity above threshold sensitive.
Application time: 1 - 10 minutes, step 1 minute, daily. Total number of treatments: 1 - 6.
55. Relaxatio mm. profundi
Emitter head: 4 cm
2
. Frequency = 1 MHz, continual PPR. Intensity: 0.5 - 1.0 W/cm2, step 0.1 W/cm2.
Electrotherapy: AMP, FM 100 - 200 Hz, steps 3/3 (program 0947)
Contralateral electrode placement.
Intensity at threshold motor.
Application time: 1 - 10 minutes, step 1 minute, daily. Total number of treatments: 1 - 6.
56. Trigger points superficialis
Emitter head: 1 cm
2
. Frequency = 3 MHz, 1:2 PPR. Intensity: 0.5 W/cm2.
Electrotherapy: TENS cont., f = 100 Hz const. (program 1625)
Contralateral electrode placement.
Intensity at threshold motor.
Application time: 1 minute, daily. Total number of treatments: 1 - 5.
57. Trigger points profundi
A/ Trigger point finding
Emitter head: 1 cm
lowered). Frequency = 1 MHz, 1:4 PPR. Intensity: 2.0 W/cm
2
(a 4 cm2 head can also be used, but proper aim is difficult and degree of accuracy is
2
.
Electrotherapy: TENS continuous, imp. 0.05 ms, asymmetrically biphase, f = 100 Hz, (program 1525)
Procedure:
First apply contact gel (electrically conductive) to the examined area. Set the ultrasound parameters.
Outside the hyper-allergic zone (HAZ) or the assumed trigger (TP) set the intensity of the electrical to threshold
sensitive and through a fluent head movement we move to the assumed and reflective changed area. HAZ is
announced by the patient as a increased intensity of a feeling by electric current bypass. TP localisation can be
found in two ways:
1. The patient reports a typical radiating pain.
2. Asymptotic motor effect (muscle contraction) in the affected muscle.
page 26
Page 27

BTL – 07p operating manual & user's guide
Note the current intensity in mA, causing the reaction.
B/ TP treatment
Without moving the head, change the PPR to 1:2, maintaining the original intensity and using either a semistationary or a stationary method to apply the combined therapy directly to the TP for 1 - 3 minutes. There must
be no standing waving - acoustic and optical indication.
All parameters of the electric component, only if there is a lowered intensity (the patient stops perceiving the
current), increase it and maintain it at a threshold sensitive.
C/ Therapy effect control
Set identical parameters as in A including the current intensity and move the head as in A. If the therapy is
successful the original TP will no longer exist.
Otherwise, repeat the B procedure.
If a palpably or clinically diagnosed trigger cannot be detected by the method described in A, repeat the whole
procedure with the ultrasound intensity increasing by 0.1 W/cm
2
, ceteris paribus.
58. Zona hypelgesica
2
Emitter head: 1 cm
. Frequency = 3 MHz, 1:2 PPR. Intensity: 0.5 W/cm2.
Electrotherapy: TENS cont., f = 100 Hz const. (program 1625).
Contralateral electrode placement.
Intensity above threshold motor.
Application time: 1 - 3 minutes, daily. Total number of treatments: 1 - 6.
page 27
Page 28

BTL – 07p operating manual & user's guide
This product is manufactured in accordance with the EU Medical Devices Directive by:
BTL Industries Ltd.
Suite 401 Albany House
324-326 Regents Street
London, W1B 3BL United Kingdom
E-mail: sales@btlnet.com
http://www.btlnet.com
For service, please contact service department at service@btlnet.com
.
© All rights reserved. No part of this manual may be reproduced, saved in a research centre or transferred by any means incl.
electronic, mechanic, photographic or other records without previous approval from BTL Industries Limited
BTL Industries Limited operates a policy of continuous development. Therefore, it reserves the right to make changes and
improvements to the Product described in this manual without prior notice.
The contents of this document is provided "as is". Except as required by applicable law, no warranties of any kind, either
expressed or implied, are made in relation to the accuracy, reliability or contents of this document. BTL Industries Limited
reserves the right to revise this document or withdraw it at any time without prior notice.
page 28
 Loading...
Loading...