Page 1

840
Ventilator System
Part No. 4-070088-00
Rev. F
October 2006
Technical Reference Manual
Operator’s and
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s & Technical Reference Manual
Page 2

Page 3

Copyright information
Copyright 1997, 1998, 2003, 2005, 2006 Puritan-Bennett Corporation. All rights
reserved. The 840
Puritan Bennett proprietary information, covered by one or more of the following
U.S. Patents and foreign equivalents: 4,954,799; 5,161,525; 5,271,389; 5,301,921;
5,319,540; 5,339,807; 5,368,019; and 5,390,666. 840, 800 Series, DualView,
SandBox, SmartAlert, Flow-by, and PTS 2000 are trademarks of Puritan-Bennett
Corporation.
The information contained in this manual is the sole property of Puritan-Bennett
Corporation and may not be duplicated without permission. This manual may be
revised or replaced by Puritan-Bennett Corporation at any time and without
notice. You should ensure that you have the most current applicable version of
this manual; if in doubt, contact Puritan-Bennett Corporation or visit the Puritan
Bennett product manual web page at:
http://www.mallinckrodt.com/respiratory/resp/Serv_Supp/
While the information set forth herein is believed to be accurate, it is not a
substitute for the exercise of professional judgment.
The ventilator should be operated and serviced only by trained professionals.
Puritan Bennett’s sole responsibility with respect to the ventilator, and its use, is as
stated in the limited warranty provided.
Nothing in this manual shall limit or restrict in any way Puritan Bennett’s right to
revise or otherwise change or modify the equipment (including its software)
described herein, without notice. In the absence of an express, written agreement
to the contrary, Puritan Bennett has no obligation to furnish any such revisions,
changes, or modifications to the owner or user of the equipment (including its
software) described herein.
TM
Ventilator System is manufactured in accordance with
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s & Technical Reference Manual
i
Page 4

Applicability
The information in this manual applies to
ventilator versions
840
manufactured or updated after August 2005. Some of this
information may not apply to earlier versions. Contact your
Puritan Bennett representative if in doubt.
Definitions
This manual uses three special indicators to convey information
of a specific nature. They include:
Warning
Indicates a condition that can endanger the patient or the
ventilator operator.
Caution
Indicates a condition that can damage the equipment.
NOTE:
Indicates points of particular emphasis that make
operation of the ventilator more efficient or
convenient.
840 Ventilator System Operator’s & Technical Reference Manual 4-070088-00 Rev. F (10/06)
ii
Page 5

Warnings, cautions, and notes
Please take the time to familiarize yourself with the following
safety considerations, special handling requirements, and
regulations that govern the use of the
• To ensure proper servicing and avoid the possibility of physical
injury, only qualified personnel should attempt to service or
make authorized modifications to the ventilator.
The user of this product shall have sole responsibility for any
ventilator malfunction due to operation or maintenance
performed by anyone not trained by Puritan Bennett.
• To avoid an electrical shock hazard while servicing the
ventilator, be sure to remove all power to the ventilator by
disconnecting the power source and turning off all ventilator
power switches.
• To avoid a fire hazard, keep matches, lighted cigarettes, and all
other sources of ignition (e.g., flammable anesthetics and/or
heaters) away from the
Ventilator System and oxygen
840
hoses.
Do not use oxygen hoses that are worn, frayed, or
contaminated by combustible materials such as grease or oils.
Textiles, oils, and other combustibles are easily ignited and
burn with great intensity in air enriched with oxygen.
Ventilator System.
840
In case of fire or a burning smell, immediately disconnect the
ventilator from the oxygen supply, facility power, and backup
power source.
• When handling any part of the
Ventilator System, always
840
follow your hospital infection control guidelines for handling
infectious material.
Puritan Bennett recognizes that cleaning, sterilization,
sanitation, and disinfection practices vary widely among
health care institutions. It is not possible for Puritan Bennett
to specify or require specific practices that will meet all needs,
or to be responsible for the effectiveness of cleaning,
sterilization, and other practices carried out in the patient care
setting.
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s & Technical Reference Manual
iii
Page 6

• Patients on life-support equipment should be appropriately
monitored by competent medical personnel and suitable
monitoring devices.
The
Ventilator System is not intended to be a
840
comprehensive monitoring device and does not activate
alarms for all types of dangerous conditions for patients on
life-support equipment.
• For a thorough understanding of ventilator operations, be sure
to thoroughly read this manual before attempting to use the
system.
• Before activating any part of the ventilator, be sure to check
the equipment for proper operation and, if appropriate, run
SST as described in this manual.
• Do not use sharp objects to make selections on the graphic
user interface (GUI) display or keyboard.
• US federal law restricts this device to sale by or on the order of
a physician.
• Check the ventilator periodically as outlined in the
840 Ventilator System Service Manual
; do not use if defective.
Immediately replace parts that are broken, missing, obviously
worn, distorted, or contaminated.
• An alternative source of ventilation should always be available
when using the
Ventilator System.
840
Warranty
The
and workmanship in accordance with the Puritan Bennett
Medical Equipment Warranty supplied with your ventilator. Keep
a maintenance record to ensure the validity of the warranty.
Ventilator System is warranted against defects in material
840
Year of manufacture
The graphic user interface (GUI), breath delivery unit (BDU),
backup power source (BPS), and compressor contain a specific
year of manufacture applicable only for that assembly. The year of
manufacture is indicated by the fifth and sixth digits of the serial
number which is located at the back panel of the GUI, BDU, and
BPS, and the side panel of the compressor.
840 Ventilator System Operator’s & Technical Reference Manual 4-070088-00 Rev. F (10/06)
iv
Page 7
Manufacturer
Puritan-Bennett Corporation
4280 Hacienda Drive
Pleasanton, CA 94588 USA
Authorized representative
Tyco Healthcare UK LTD
154 Fareham Road
Gosport PO13 0AS, U.K.
Electromagnetic susceptibility
The
IEC 60601-1-2:2004 (EMC Collateral Standard), including the Efield susceptibility requirements at a level of 10 volts per meter, at
frequencies from 80 MHz to 2.5 GHz, and the ESD requirements
of this standard.
However, even at this level of device immunity, certain
transmitting devices (cellular phones, walkie-talkies, cordless
phones, paging transmitters, etc.) emit radio frequencies that
could interrupt ventilator operation if operated in a range too
close to the ventilator. It is difficult to determine when the field
strength of these devices becomes excessive.
Practitioners should be aware that radio frequency emissions are
additive, and that the ventilator must be located a sufficient
distance from transmitting devices to avoid interruption. Do not
operate the ventilator in a magnetic resonance imaging (MRI)
environment.
Ventilator System complies with the requirements of
840
Warning
Accessory equipment connected to the power receptacle,
analog, and digital interfaces must be certified according
to IEC 60601-1. Furthermore, all configurations shall
comply with the system standard IEC 60601-1-1. Any
person who connects additional equipment to the power
receptacle, signal input part, or signal output part of the
840 ventilator configures a medical system, and is
therefore responsible for ensuring that the system
complies with the requirements of the system standard IEC
60601-1-1. If in doubt, consult Puritan Bennett Technical
Services at 1.800.255.6774 or your local representative.
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s & Technical Reference Manual
v
Page 8

This manual describes possible ventilator alarms and what to do if
they occur. Consult with your institution’s biomedical
engineering department in case of interrupted ventilator
operation, and before relocating any life support equipment.
Customer assistance
For further assistance contact your local Puritan Bennett
representative.
Preface
This manual is divided into two parts: the operator’s manual and
the technical reference. The operator’s manual describes how to
operate the Puritan Bennett
provides product specifications and accessory order numbers. The
technical reference includes background information about how
the ventilator functions, including details on its operating modes,
self-tests, and other features. In the table of contents and index,
the prefix OP- identifies page numbers in the operator’s manual,
and the prefix TR- identifies page numbers in the technical
reference.
Any references to the software options
Plus
®
(VV+)
which includes VC+ and VS breath types
Proportional Assist Ventilation
that are made in this manual assume that the option has been
installed on the ventilator. If these options aren’t installed, then
references to their functions do not apply.
Ventilator System. It also
840
®
, Volume Ventilation
Tube Compensation (TC)
®
(PAV+),
BiLevel
and
, NeoMode®,
While this manual covers the ventilator configurations currently
supported by Puritan Bennett, it may not be all-inclusive and may
not be applicable to your ventilator. Contact Puritan Bennett for
questions about the applicability of the information.
840 Ventilator System Operator’s & Technical Reference Manual 4-070088-00 Rev. F (10/06)
vi
Page 9

Contents
Operator’s Manual
1 Introduction OP 1-1
1.1 Technical description. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 1-3
1.1.1 General background . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 1-3
1.1.2 Pressure and flow triggering . . . . . . . . . . . . . . . . . . . . . . . . . OP 1-5
1.1.3 Breathing gas mixture . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 1-5
1.1.4 Inspiratory pneumatics . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 1-6
1.1.5 Patient circuit . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 1-6
1.1.6 AC mains and backup power system . . . . . . . . . . . . . . . . . . . OP 1-7
1.1.7 Ventilator emergency states. . . . . . . . . . . . . . . . . . . . . . . . . . OP 1-8
1.2 Graphic user interface . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 1-9
1.3 User interface controls and indicators . . . . . . . . . . . . . . . . . . . . . . OP 1-11
1.3.1 Onscreen symbols and abbreviations . . . . . . . . . . . . . . . . . . . OP 1-18
1.4 Ventilator system labeling symbols. . . . . . . . . . . . . . . . . . . . . . . . . OP 1-24
2 How to set up the 840 ventilator OP 2-1
2.1 How to connect the electrical supply . . . . . . . . . . . . . . . . . . . . . . OP 2-3
2.2 How to connect the air and oxygen supplies . . . . . . . . . . . . . . . . . OP 2-8
2.3 How to connect the patient circuit components . . . . . . . . . . . . . . OP 2-11
2.3.1 How to select and connect a patient circuit . . . . . . . . . . . . . . OP 2-12
2.3.2 How to install the expiratory filter and collector vial. . . . . . . . OP 2-15
2.3.3 How to install the flex arm. . . . . . . . . . . . . . . . . . . . . . . . . . . OP 2-18
2.3.4 How to install the humidifier . . . . . . . . . . . . . . . . . . . . . . . . . OP 2-19
2.3.5 How to use the ventilator cart . . . . . . . . . . . . . . . . . . . . . . . . OP 2-22
3 How to run Short Self Test (SST) OP 3-1
3.1 Introduction to SST . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 3-1
3.2 When to run SST . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 3-2
3.3 SST components and requirements . . . . . . . . . . . . . . . . . . . . . . . . OP 3-3
3.4 SST Procedure . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 3-4
3.5 SST Results. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 3-12
3.5.1 How to interpret individual SST test results . . . . . . . . . . . . . . OP 3-14
3.5.2 SST outcomes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 3-15
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s and Technical Reference Manual
vii
Page 10

Contents
4 How to use the 840 ventilator OP 4-1
4.1 Structure of user interface . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 4-2
4.2 Patient setup. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 4-3
4.2.1 How to ventilate with most recent control parameters . . . . . OP 4-4
4.2.2 How to ventilate with new control parameters . . . . . . . . . . . OP 4-4
4.2.3 Patient data and current settings. . . . . . . . . . . . . . . . . . . . . . OP 4-7
4.2.4 Ideal Body Weight (IBW). . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 4-10
4.3 How to change the main ventilator control parameters. . . . . . . . . OP 4-15
4.4 Mode, breath type, and other changes . . . . . . . . . . . . . . . . . . . . . OP 4-16
4.5 How to select a constant timing variable during
respiratory rate changes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 4-17
4.6 How to change apnea ventilation settings. . . . . . . . . . . . . . . . . . . OP 4-19
4.7 How to set alarms . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 4-20
4.8 How to change other settings . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 4-22
4.9 Expiratory pause maneuvers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 4-23
4.10 Inspiratory pause maneuvers. . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 4-24
4.11 How to interpret inspiratory pause maneuver results
for static compliance and resistance . . . . . . . . . . . . . . . . . . . . . . OP 4-26
4.12 How to use NIV. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 4-27
4.12.1 NIV intended use . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 4-27
4.12.2 NIV breathing interfaces . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 4-27
4.12.3 NIV setup . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 4-28
4.12.4 High spontaneous inspiratory time limit setting. . . . . . . . . . OP 4-32
4.12.5 Apnea setup . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 4-32
4.12.6 Alarm setup. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 4-32
4.12.7 Changing patient from INVASIVE to NIV Vent Type. . . . . . . OP 4-34
4.12.8 Changing patient from NIV to INVASIVE Vent Type. . . . . . . OP 4-35
4.12.9 NIV patient data . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 4-35
840 Ventilator System Operator’s and Technical Reference Manual 4-070088-00 Rev. F (10/06)
viii
Page 11

Contents
5 How to handle alarms OP 5-1
5.1 Ventilator alarm classifications . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 5-1
5.2 Alarm silence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 5-2
5.3 Alarm reset . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 5-4
5.4 Alarm log. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 5-5
5.5 Alarm volume . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 5-6
5.6 Alarm messages. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 5-7
6 How to view graphics OP 6-1
6.1 Graphics display function. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 6-1
6.2 How to set up a graphics display . . . . . . . . . . . . . . . . . . . . . . . . . . OP 6-2
6.3 Graphics display details and calculations . . . . . . . . . . . . . . . . . . . . OP 6-3
6.4 How to adjust displayed graphics. . . . . . . . . . . . . . . . . . . . . . . . . . OP 6-4
6.5 The graphics display FREEZE function . . . . . . . . . . . . . . . . . . . . . . OP 6-5
6.6 How to print patient data graphics . . . . . . . . . . . . . . . . . . . . . . . . OP 6-6
6.7 Automatic display of graphics . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 6-6
6.8 When graphics are not accessible . . . . . . . . . . . . . . . . . . . . . . . . . OP 6-7
7 Preventive maintenance OP 7-1
7.1 How to dispose of used parts. . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 7-1
7.2 How to clean, disinfect and sterilize parts. . . . . . . . . . . . . . . . . . . . OP 7-2
7.2.1 How to clean components. . . . . . . . . . . . . . . . . . . . . . . . . . . OP 7-6
7.3 Disinfection and sterilization . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 7-6
7.4 Preventive maintenance procedures for the operator . . . . . . . . . . . OP 7-8
7.4.1 Total operational hours . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 7-9
7.4.2 Inspiratory and expiratory bacteria filters . . . . . . . . . . . . . . . . OP 7-12
7.4.3 Daily or as required: collector vial and drain bag . . . . . . . . . . OP 7-14
7.4.3.1 How to remove the collector vial . . . . . . . . . . . . . . . . . . OP 7-14
7.4.3.2 How to remove the drain bag . . . . . . . . . . . . . . . . . . . . OP 7-14
7.4.4 Daily or as required: in-line water traps . . . . . . . . . . . . . . . . . OP 7-15
7.4.5 Every 250 hours: compressor inlet filter . . . . . . . . . . . . . . . . . OP 7-15
7.4.6 Every year: ventilator inspection. . . . . . . . . . . . . . . . . . . . . . . OP 7-16
7.4.7 Every 2 years or as necessary: oxygen sensor . . . . . . . . . . . . . OP 7-17
7.4.7.1 Oxygen sensor replacement procedure . . . . . . . . . . . . . OP 7-17
7.5 Additional preventive maintenance procedures . . . . . . . . . . . . . . . OP 7-23
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s and Technical Reference Manual
ix
Page 12

Contents
7.6 Storage . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 7-25
7.7 Repacking and shipping . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 7-25
A Specifications OP A-1
A.1 Physical characteristics . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP A-2
A.2 Environmental requirements . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP A-3
A.3 Pneumatic specifications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP A-4
A.4 Electrical specifications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP A-5
A.5 Compliance and approvals . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP A-7
A.5.1 Manufacturer’s Declaration . . . . . . . . . . . . . . . . . . . . . . . . . . OP A-9
A.6 Technical specifications. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP A-18
A.7 Ranges, resolutions, and accuracies . . . . . . . . . . . . . . . . . . . . . . . . OP A-23
A.7.1 Recommended limits . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP A-23
A.7.2 Software options. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP A-24
B Part numbers OP B-1
C Pneumatic schematic OP C-1
D Alarm and oxygen sensor calibration testing OP D-1
D.1 Alarm test. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP D-1
D.2 Oxygen sensor calibration test . . . . . . . . . . . . . . . . . . . . . . . . . . . OP D-6
E Remote alarm and RS-232 ports OP E-1
E.1 Remote alarm port . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP E-2
E.2 RS-232 port. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP E-3
E.3 How to configure the RS-232 ports . . . . . . . . . . . . . . . . . . . . . . . . OP E-4
E.4 Printers and cables . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP E-5
E.5 RS-232 port commands. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP E-6
840 Ventilator System Operator’s and Technical Reference Manual 4-070088-00 Rev. F (10/06)
x
Page 13

Contents
Technical Reference
1 Introduction to breath delivery TR 1-1
2 Detecting and initiating inspiration TR 2-1
2.1 Internally triggered inspiration. . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 2-2
2.1.1 Pressure sensitivity . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 2-2
2.1.2 Flow sensitivity . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 2-4
2.1.3 Time-cycled inspiration . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 2-6
2.2 Operator-triggered inspiration . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 2-6
3 Detecting and initiating exhalation TR 3-1
3.1 Internally initiated exhalation. . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 3-1
3.1.1 Time-cycled exhalation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 3-1
3.1.2 End-inspiratory flow method . . . . . . . . . . . . . . . . . . . . . . . . . TR 3-2
3.1.3 Airway pressure method . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 3-3
3.2 Backup limits . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 3-4
3.2.1 Time limit . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 3-4
3.2.2 High circuit pressure limit . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 3-4
3.2.3 High ventilator pressure limit. . . . . . . . . . . . . . . . . . . . . . . . . TR 3-4
4 Mandatory breath delivery TR 4-1
4.1 Comparison of pressure- and volume-based mandatory breaths . . TR 4-1
4.2 Compliance compensation for volume-based mandatory breaths . TR 4-3
4.3 BTPS compensation for volume-based mandatory breaths. . . . . . . TR 4-5
4.4 Manual inspiration. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 4-5
5 Spontaneous breath delivery TR 5-1
6 Assist/control (A/C) mode TR 6-1
6.1 Breath delivery in A/C . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 6-1
6.2 Rate change during A/C . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 6-3
6.3 Changing to A/C mode . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 6-3
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s and Technical Reference Manual
xi
Page 14

Contents
7 Synchronous intermittent mandatory
ventilation (SIMV) TR 7-1
7.1 Breath delivery in SIMV . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 7-3
7.2 Apnea ventilation in SIMV . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 7-4
7.3 Changing to SIMV mode. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 7-5
7.4 Rate change during SIMV . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 7-7
8 Spontaneous (SPONT) mode TR 8-1
8.1 Breath delivery in SPONT . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 8-1
8.2 Changing to SPONT mode . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 8-1
9 Apnea ventilation TR 9-1
9.1 Apnea detection . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 9-1
9.2 Transition to apnea ventilation . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 9-3
9.3 Key entries during apnea ventilation . . . . . . . . . . . . . . . . . . . . . . . TR 9-3
9.4 Resetting apnea ventilation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 9-3
9.4.1 Resetting to A/C . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 9-4
9.4.2 Resetting to SIMV . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 9-4
9.4.3 Resetting to SPONT . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 9-4
9.5 Phasing in new apnea intervals . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 9-5
10 Detecting occlusion and disconnect TR 10-1
10.1 Occlusion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 10-1
10.2 Disconnect . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 10-3
10.3 Occlusions and disconnect annunciation. . . . . . . . . . . . . . . . . . . TR 10-5
11 Phasing in setting changes TR 11-1
12 Ventilator settings TR 12-1
12.1 Apnea ventilation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-1
12.2 Circuit type and Ideal Body Weight (IBW) . . . . . . . . . . . . . . . . . TR 12-2
12.3 Disconnect sensitivity (D
12.4 Expiratory sensitivity (E
12.5 Expiratory time (T
840 Ventilator System Operator’s and Technical Reference Manual 4-070088-00 Rev. F (10/06)
xii
). . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-4
E
) . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-3
SENS
) . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-4
SENS
Page 15

Contents
12.6 Flow pattern . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-4
12.7 Flow sensitivity (V
12.8 High spontaneous inspiratory time limit (2T
12.9 Humidification type . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-7
12.10 I:E ratio . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-7
12.11 Ideal body weight (IBW) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-7
12.12 Inspiratory pressure (P
12.13 Inspiratory time (T
12.14 Mode and mandatory breath type. . . . . . . . . . . . . . . . . . . . . . . TR 12-9
12.15 O
% . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-12
2
12.16 Peak inspiratory flow (V
12.17 PEEP . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-13
12.17.1 PEEP restoration. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-14
12.18 Plateau time (T
12.19 Pressure sensitivity (P
12.20 Pressure support (P
12.21 Respiratory rate (f) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-16
12.22 Rise time % . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-16
12.23 Safety ventilation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-17
12.24 Spontaneous breath type. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-18
12.25 Tidal volume (V
12.26 Vent type. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-19
). . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-5
SENS
I SPONT
) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-8
I
) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-8
I
) . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-13
MAX
) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-14
PL
) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-15
SENS
) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-15
SUPP
). . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 12-19
T
). . . . . . . . . . . TR 12-6
13 Alarms TR 13-1
13.1 Alarm handling . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 13-1
13.1.1 Alarm messages. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 13-3
13.1.2 Alarm summary . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 13-5
13.2 AC POWER LOSS alarm . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 13-22
13.3 APNEA alarm . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 13-22
13.4 CIRCUIT DISCONNECT alarm . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 13-23
13.5 DEVICE ALERT alarm . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 13-23
13.6 High circuit pressure (
13.7 High delivered O
13.8 High exhaled minute volume (
13.9 High exhaled tidal volume (
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s and Technical Reference Manual
↑P
) alarm. . . . . . . . . . . . . . . . . . . . . . . TR 13-24
PEAK
% (↑O2%) alarm . . . . . . . . . . . . . . . . . . . . . . . TR 13-25
2
↑V
↑
TE
) alarm . . . . . . . . . . . . . . . TR 13-25
V
ETOT
) alarm. . . . . . . . . . . . . . . . . . . . TR 13-26
xiii
Page 16

Contents
13.10 High inspired tidal volume alarm (↑VTI, ↑V
↑V
TI SPONT
13.11 High respiratory rate (
) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 13-26
↑f
) alarm . . . . . . . . . . . . . . . . . . . . . . TR 13-27
TOT
TI MAND
,
13.12 INSPIRATION TOO LONG alarm . . . . . . . . . . . . . . . . . . . . . . . . TR 13-27
13.13 Low circuit pressure alarm (
13.14 Low delivered O
% (↓O2%) alarm . . . . . . . . . . . . . . . . . . . . . . TR 13-28
2
↓P
) . . . . . . . . . . . . . . . . . . . . . . TR 13-28
PEAK
13.15 Low exhaled mandatory tidal volume
(
↓V
TE MAND
) alarm . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 13-29
13.16 Low exhaled spontaneous tidal volume
(
↓V
TE SPONT
13.17 Low exhaled total minute volume (
) alarm . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 13-30
↓
) alarm . . . . . . . . . . TR 13-30
V
E TOT
13.18 PROCEDURE ERROR alarm. . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 13-31
14 Patient data TR 14-1
14.1 Delivered O2% . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 14-1
14.2 End expiratory pressure (PEEP) . . . . . . . . . . . . . . . . . . . . . . . . . . TR 14-2
14.3 End inspiratory pressure (P
14.4 Exhaled minute volume (V
14.5 Exhaled tidal volume (V
TE
14.6 I:E ratio (I:E) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 14-4
14.7 Intrinsic (auto) PEEP (PEEP
14.8 Mean circuit pressure (P
14.9 Peak circuit pressure (P
14.10 Plateau pressure (P
MEAN
PEAK
) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 14-6
PL
14.11 Spontaneous minute volume (V
14.12 Static compliance and resistance (C
14.13 Total respiratory rate (f
TOT
) . . . . . . . . . . . . . . . . . . . . . . . . . TR 14-2
I END
) . . . . . . . . . . . . . . . . . . . . . . . . . TR 14-3
E TOT
) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 14-4
) and total PEEP (PEEP
I
) . . . . . . . . . TR 14-5
TOT
). . . . . . . . . . . . . . . . . . . . . . . . . . . TR 14-5
) . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 14-5
E SPONT
) . . . . . . . . . . . . . . . . . . TR 14-6
STAT
and R
) . . . . . . . . . . TR 14-7
STAT
) . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 14-13
15 Safety net TR 15-1
15.1 Patient problems. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 15-1
15.2 System faults. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 15-2
15.3 Ongoing background checks . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 15-3
15.4 Hardware monitoring circuitry . . . . . . . . . . . . . . . . . . . . . . . . . . TR 15-4
15.5 Power on self test (POST) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 15-5
15.6 Short self test (SST) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 15-5
840 Ventilator System Operator’s and Technical Reference Manual 4-070088-00 Rev. F (10/06)
xiv
Page 17

Contents
15.7 Extended self test (EST) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 15-5
15.8 Oxygen sensor calibration . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 15-6
15.9 Exhalation valve calibration . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 15-6
15.10 Ventilator inoperative test . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 15-6
15.11 Flow sensor offset calibration . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 15-6
15.12 Atmospheric pressure transducer calibration . . . . . . . . . . . . . . . TR 15-6
16 Power on self test (POST) TR 16-1
16.1 Safety . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 16-1
16.2 POST characteristics. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 16-2
16.3 POST following power interruptions . . . . . . . . . . . . . . . . . . . . . . TR 16-3
16.4 POST fault handling. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 16-4
16.5 POST system interface . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 16-4
16.6 POST user interface . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 16-5
17 Short self test (SST) TR 17-1
18 Extended self test (EST) TR 18-1
18.1 EST results . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 18-2
18.2 EST failure handling. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 18-3
18.3 EST safety considerations . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 18-3
19 RS-232 commands TR 19-1
19.1 RSET command . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 19-1
19.2 SNDA command . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 19-1
Glossary
Index
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s and Technical Reference Manual
xv
Page 18

Contents
This page is intentionally blank.
840 Ventilator System Operator’s and Technical Reference Manual 4-070088-00 Rev. F (10/06)
xvi
Page 19

Figures
Operator’s manual
Figure 1-1. 840 Ventilator System block diagram . . . . . . . . . . . . . . . OP 1-4
Figure 1-2. 840 Ventilator System graphic user interface (GUI) . . . . . OP 1-10
Figure 2-1. How to lift the ventilator components . . . . . . . . . . . . . . . OP 2-2
Figure 2-2. How to connect the ventilator power cord . . . . . . . . . . . OP 2-5
Figure 2-3. Ventilator power switch, AC indicator, and AC panel. . . . OP 2-6
Figure 2-4. Power cord storage on the cart . . . . . . . . . . . . . . . . . . . . OP 2-7
Figure 2-5. How to connect the air and oxygen supplies. . . . . . . . . . OP 2-10
Figure 2-6. How to connect the patient circuit . . . . . . . . . . . . . . . . . OP 2-14
Figure 2-7. How to install the expiratory filter and collector vial . . . . OP 2-16
Figure 2-8. How to use the collector vial with or
without the drain bag . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 2-17
Figure 2-9. How to install the flex arm. . . . . . . . . . . . . . . . . . . . . . . . OP 2-18
Figure 2-10. How to install the humidifier
(Fisher & Paykel version shown) . . . . . . . . . . . . . . . . . . . OP 2-21
Figure 2-11. How to lock and unlock the cart’s front wheels . . . . . . . . OP 2-22
Figure 3-1. Test button location . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 3-5
Figure 4-1. Touch screen user interface . . . . . . . . . . . . . . . . . . . . . . . OP 4-2
Figure 4-2. Ventilator Startup screen . . . . . . . . . . . . . . . . . . . . . . . . . OP 4-3
Figure 4-3. Touch screen appearance during normal ventilation
(shown with alarm silence and
100% O
Figure 4-4.
(or TH) selected as the constant during rate change. . . OP 4-18
T
I
Figure 4-5. Alarm setup. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 4-21
Figure 4-6. New patient setup screen — NIV. . . . . . . . . . . . . . . . . . . OP 4-29
Figure 4-7. NIV ventilator settings screen . . . . . . . . . . . . . . . . . . . . . OP 4-31
Figure 4-8. New patient default alarm settings . . . . . . . . . . . . . . . . . OP 4-33
Figure 4-9. More patient data screen — NIV . . . . . . . . . . . . . . . . . . . OP 4-36
Figure 5-1. Alarm indicators . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 5-2
Figure 5-2. Alarm Silence in Progress indicator (lower screen) . . . . . . OP 5-3
Figure 5-3. Alarm log . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 5-5
Figure 5-4. Alarm message format. . . . . . . . . . . . . . . . . . . . . . . . . . . OP 5-8
Figure 6-1. Pressure-volume loop . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 6-2
Figure 7-1. How to empty the collector vial and seal the drain bag . . OP 7-15
Figure 7-2. 806 compressor with inlet filter. . . . . . . . . . . . . . . . . . . . OP 7-16
/CAL in progress) . . . . . . . . . . . . . . . . . . . . . . . OP 4-9
2
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s and Technical Reference Manual
xvii
Page 20

Figures
Figure 7-3. Dislodge the O2 sensor access cover . . . . . . . . . . . . . . . . OP 7-19
Figure 7-4. Open O
Figure 7-5. Locate O
Figure A-1. Recommended patient circuit configurations . . . . . . . . . OP A-22
Figure B-1. Ventilator accessories . . . . . . . . . . . . . . . . . . . . . . . . . . . OP B-2
Figure C-1. Pneumatic schematic . . . . . . . . . . . . . . . . . . . . . . . . . . . OP C-1
Figure E-1. Remote alarm and RS-232 ports . . . . . . . . . . . . . . . . . . . OP E-1
Figure E-2. Remote alarm port pinout (view from back of GUI). . . . . OP E-2
Figure E-3. RS-232 serial port pinout . . . . . . . . . . . . . . . . . . . . . . . . OP E-3
Technical Reference
Figure 2-1. Declaring inspiration using pressure sensitivity . . . . . . . . TR 2-3
Figure 2-2. Declaring inspiration using flow sensitivity . . . . . . . . . . . TR 2-4
Figure 2-3. Time-cycled inspiration. . . . . . . . . . . . . . . . . . . . . . . . . . TR 2-6
Figure 3-1. Initiating exhalation using the
end-inspiratory flow method. . . . . . . . . . . . . . . . . . . . . . TR 3-2
Figure 3-2. Initiating exhalation using the airway pressure method. . TR 3-3
Figure 6-1. A/C mode, no patient effort detected. . . . . . . . . . . . . . . TR 6-2
Figure 6-2. A/C mode, patient effort detected . . . . . . . . . . . . . . . . . TR 6-2
Figure 6-3. A/C mode, VIM and PIM breaths . . . . . . . . . . . . . . . . . . TR 6-2
Figure 7-1. SIMV breath cycle
(mandatory and spontaneous intervals) . . . . . . . . . . . . . TR 7-1
Figure 7-2. SIMV breath cycle, PIM delivered within
mandatory interval . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 7-2
Figure 7-3. SIMV breath cycle, PIM not delivered within
mandatory interval . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 7-2
Figure 7-4. Apnea ventilation in SIMV. . . . . . . . . . . . . . . . . . . . . . . . TR 7-5
Figure 9-1. Apnea interval equals breath period . . . . . . . . . . . . . . . . TR 9-2
Figure 9-2. Apnea interval greater than breath period. . . . . . . . . . . . TR 9-2
Figure 9-3. Apnea interval less than breath period . . . . . . . . . . . . . . TR 9-2
Figure 12-1. 840 ventilator modes and breath types. . . . . . . . . . . . . . TR 12-11
Figure 13-1. Alarm message format (upper GUI screen) . . . . . . . . . . . TR 13-3
sensor access port . . . . . . . . . . . . . . . . . . . . . . OP 7-20
2
sensor . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 7-21
2
840 Ventilator System Operator’s and Technical Reference Manual 4-070088-00 Rev. F (10/06)
xviii
Page 21
Tables
Operator’s manual
Table 1-1. 840 Ventilator System controls and indicators . . . . . . . . . OP 1-11
Table 1-2. BDU indicators . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 1-17
Table 1-3. 840 Ventilator System symbols and abbreviations . . . . . . OP 1-18
Table 2-1. Patient circuit and IBW values . . . . . . . . . . . . . . . . . . . . . OP 2-13
Table 3-1. SST test sequence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 3-8
Table 3-2. Individual SST test results . . . . . . . . . . . . . . . . . . . . . . . . OP 3-14
Table 3-3. Overall SST outcomes . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 3-15
Table 4-1. Determining IBW based
on patient height (cm to kg) OP 4-10
Table 4-2. Determining IBW based
on patient height (ft, in. to lb) OP 4-13
Table 4-3. Patient circuit and IBW values . . . . . . . . . . . . . . . . . . . . . OP 4-15
Table 4-4. Monitored ventilator control parameters . . . . . . . . . . . . . OP 4-16
Table 4-5. Automatic settings changes—INVASIVE to NIV . . . . . . . . OP 4-34
Table 4-6. Automatic settings changes—NIV to INVASIVE . . . . . . . . OP 4-35
Table 5-1. Alarm messages. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP 5-9
Table 7-1. Procedures to clean, disinfect, and sterilize parts . . . . . . . OP 7-3
Table 7-2. Disinfection and sterilization procedures . . . . . . . . . . . . . OP 7-7
Table 7-3. Operator preventive maintenance procedures
and frequency OP 7-10
Table 7-4. Service preventive maintenance procedures and intervals OP 7-24
Table A-1. Physical characteristics. . . . . . . . . . . . . . . . . . . . . . . . . . . OP A-2
Table A-2. Environmental requirements . . . . . . . . . . . . . . . . . . . . . . OP A-3
Table A-3. Pneumatic specifications . . . . . . . . . . . . . . . . . . . . . . . . . OP A-4
Table A-4. Electrical specifications . . . . . . . . . . . . . . . . . . . . . . . . . . OP A-5
Table A-5. Compliance and approvals . . . . . . . . . . . . . . . . . . . . . . . OP A-8
Table A-6. Electromagnetic Emissions. . . . . . . . . . . . . . . . . . . . . . . . OP A-10
Table A-7. Electromagnetic Immunity . . . . . . . . . . . . . . . . . . . . . . . OP A-11
Table A-8. Electromagnetic Immunity – conducted and radiated RF . OP A-13
Table A-9. Recommended separation distances between portable
and mobile RF communications equipment
and the 840 Ventilator System . . . . . . . . . . . . . . . . . . . . OP A-15
Table A-10. Compliant cables. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP A-16
Table A-11. Technical specifications . . . . . . . . . . . . . . . . . . . . . . . . . . OP A-18
4-070088-00 Rev F (10/06) 840 Ventilator System Operator’s and Technical Reference Manual
xix
Page 22

Tables
Table A-12. Ventilator settings. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP A-24
Table A-13. Alarm settings. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP A-40
Table A-14. Patient data . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . OP A-45
Table A-15. Other Screens — displayed data . . . . . . . . . . . . . . . . . . . OP A-52
Table B-1. Ventilator parts and accessories. . . . . . . . . . . . . . . . . . . . OP B-3
Technical Reference
Table 4-1. Comparison of pressure- and volume-based
mandatory breaths . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 4-2
Table 4-2. Compliance volume factors. . . . . . . . . . . . . . . . . . . . . . . TR 4-5
Table 5-1. Spontaneous breath delivery characteristics . . . . . . . . . . TR 5-1
Table 12-1. 840 ventilator modes and breath types. . . . . . . . . . . . . . TR 12-9
Table 13-1. Alarm urgency levels . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 13-2
Table 13-2. Alarm summary . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 13-5
Table 13-3. Applicability of high inspired tidal volume alarm symbols TR 13-26
Table 14-1. Inspiratory pause maneuver displays . . . . . . . . . . . . . . . . TR 14-9
Table 19-1. MISCA response . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . TR 19-3
840 Ventilator System Operator’s and Technical Reference Manual 4-070088-00 Rev F (10/06)
xx
Page 23
C
HAPTER
1
Introduction
The intended use of the Puritan Bennett
for acute and subacute care of infant, pediatric, and adult patients.
Software options, available from Puritan Bennett, provide
additional ventilation functions.
The
management, offers selectable modes of breath delivery, and
assists the practitioner in the selection of the most appropriate
ventilator control parameters for the patient. The user interface is
intuitive and easy to operate for those with prior knowledge of
ventilator operation.
The user interface includes
monitored patient data, for easy assessment of the patient’s
condition. The touch screens also display the current ventilator
control parameters.
The
preview the selected ventilator control parameters prior to active
ventilation of the patient.
The
specific information about the cause, and prompts the user with
actions to resolve the reported condition(s).
Ventilator System facilitates work of breathing
840
SandBox
SmartAlert
1
Ventilator System is
840
DualView
™ area on the touch screen allows the practitioner to
™ system intercepts alarms, or events, provides
™ touch screens that display
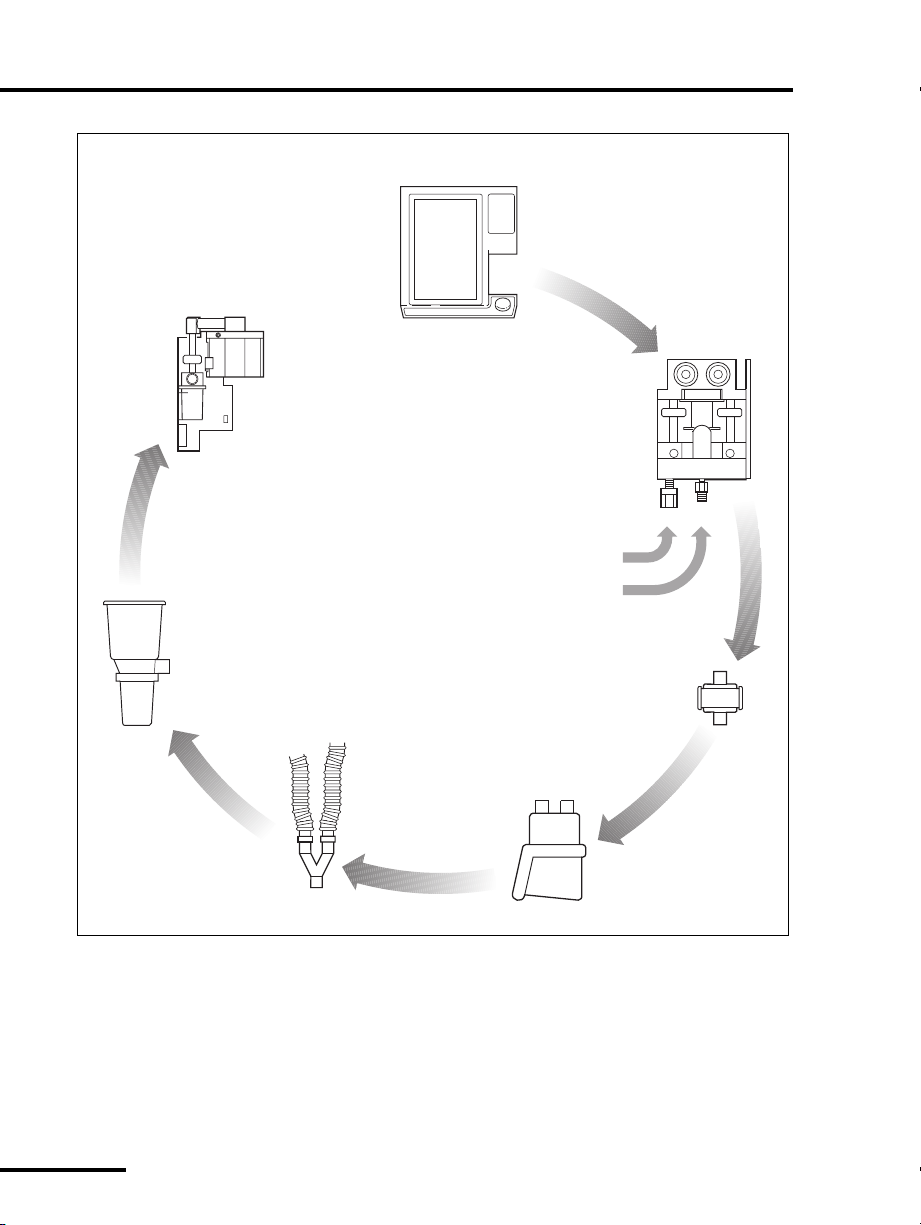
The breath delivery unit (BDU) comprises the pneumatics and the
patient circuit.
The ventilator uses two independent Central Processing Units
(CPUs):
• Breath delivery unit (BDU) CPU
• Graphic user interface (GUI) CPU
The BDU CPU uses the ventilator control parameters, selected by
the practitioner, to deliver breaths to the patient. The BDU CPU
also runs continuous and extensive operational background
checks to ensure proper operation of the ventilator.
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 1-1
Page 24

OP 1
Introduction
The GUI CPU monitors the ventilator and the ventilator/patient
interaction. The GUI CPU also monitors the operation of the BDU
CPU and prevents simultaneous failure of control and monitor
functions when a single fault is reported.
The
breaths with a preset level of positive end expiratory pressure
(PEEP), trigger sensitivity, and oxygen concentration. A
mandatory breath can either be pressure- or volume-controlled,
but it is always pressure-controlled in the optional
spontaneous breath allows patient inspiratory flows of up to
200 L/min, with or without pressure support.
The optional 806 Compressor unit provides compressed air to the
BDU, and can be used in place of wall or bottled air. The
compressor unit is powered through and communicates with the
BDU.
The 802 Backup Power Source (BPS) provides DC power to the
BDU and GUI in the event that AC power is lost. A new, fully
charged BPS runs the ventilator (without a compressor or a
humidifier) for at least 30 minutes, which allows transport of the
patient and the ventilator within the healthcare facility.
This manual tells you how to operate and perform simple
maintenance for the
this manual and accompanying labels before attempting to
operate or maintain the ventilator.
To ensure optimum performance of the
Puritan Bennett strongly recommends that certified biomedical
engineering technicians, or other personnel with equivalent
experience and training in the service of this type of equipment,
perform periodic maintenance on the ventilator. For more
information, contact your Puritan Bennett representative.
Ventilator System supplies mandatory or spontaneous
840
BiLevel
Ventilator System. Become familiar with
840
Ventilator System,
840
mode. A
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 1-2
Page 25

Introduction
1.1 Technical description
1.1.1 General background
The practitioner uses the GUI touch screens, the off-screen keys,
and GUI knob to select the ventilator control parameters and
input data (see Figure 1-1). The GUI CPU processes this
information and stores it in ventilator memory. The BDU CPU
uses this stored information to control and monitor the flow of
gas to and from the patient. The two CPUs communicate to
transfer and verify any new ventilator control parameters or alarm
limits. Each CPU then performs continuous background
verification of operational and data integrity.
OP 1
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 1-3
Page 26
OP 1
Exhalation
module:
Active exhalation valve
Pressure transducer
Flow sensor
Introduction
Graphic user
interface (GUI)
Inspiratory
module:
PSOLs
Safety valve
Oxygen sensor
Pressure transducers
Flow sensors
Collector
vial
supply
Oxygen
Expiratory
filter
(Expiratory
limb)
(Inspiratory
limb)
Patient
circuit
supply
Figure 1-1. 840 Ventilator System block diagram
Air
regulator
Air
Humidification
device
Oxygen
regulator
Inspiratory
filter
8-00001
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 1-4
Page 27
Introduction
OP 1
1.1.2 Pressure and flow triggering
The ventilator uses flow or pressure triggering to recognize patient
effort. When
pressure triggering
pressure in the patient circuit. As the patient draws gas from the
circuit and airway pressure drops by at least the value selected for
pressure sensitivity, the ventilator delivers a breath.
When
flow triggering (Flow-by
monitors the difference between the inspiratory and expiratory
flow sensor measurements. As the patient inhales, the ventilator
measures less exhaled flow while the delivered flow remains
constant. The result is an increase in the difference between the
inspiratory and expiratory flows. When the difference is at least
the operator-selected value for flow sensitivity, the ventilator
delivers a breath.
If the patient is not inhaling, any difference between the delivered
and exhaled flow is due to sensor inaccuracy or leaks in the
patient system. To compensate for leaks in the patient system
which can cause autotriggering, the operator can increase the flow
sensitivity setting.
As a backup method of triggering inspiration, a pressure
sensitivity of 2 cmH
O is also in effect. This setting is the most
2
sensitive setting that is still large enough to avoid autotriggering,
yet will trigger with acceptable patient effort.
is in effect, the ventilator monitors
) is in effect, the ventilator
1.1.3 Breathing gas mixture
Air and oxygen from cylinders, wall supplies, or compressor (air
only) enter the ventilator through hoses and fittings (the fittings
are available in several versions). Once inside the ventilator, air
and oxygen are regulated to pressures appropriate for the
ventilator, then mixed according to the selected O
The ventilator delivers the mixed air and oxygen through the
inspiratory module
and out to the patient. The oxygen
concentration of the delivered gas is monitored here, using a
galvanic oxygen sensor. The galvanic sensor generates a voltage
proportional to the oxygen concentration. The ventilator reports
an alarm if the O
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
sensor is enabled and monitored oxygen
2
%.
2
OP 1-5
Page 28

OP 1
Introduction
concentration is more than seven percent above or below the
O
% setting, or below 18% after the concentration stabilizes.
2
The inspiratory manifold also includes a safety valve to relieve
patient pressure if necessary (for example, if the patient circuit is
kinked or occluded). The inspiratory module also corrects for gas
temperature and humidity, based on the practitioner-set
humidification type.
1.1.4 Inspiratory pneumatics
Ventilator inspiratory pneumatics consist of two parallel circuits:
one for oxygen and one for air. The primary elements of the
inspiratory pneumatics are two proportional solenoid valves
(PSOLs), which control the flow of gas delivered to the patient. Air
and oxygen flow sensors, along with pressure signals from the
patient circuit, provide feedback that the BDU CPU uses to
control the PSOLs.
As a result, the ventilator supplies mixed breathing gas to the
patient, based on the practitioner-set ventilator control
parameters. The mixed air and oxygen passes through the patient
circuit external to the ventilator. The system delivers the
breathing gas mixture to the patient at the patient wye, located in
the external patient circuit.
1.1.5 Patient circuit
The
patient circuit
ventilator that route gas between the ventilator and the patient.
These components include:
•an
• a humidification device (optional) in line with the patient
• the inspiratory and expiratory limbs of the patient circuit that
•a
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 1-6
inspiratory filter
between the patient and ventilator
circuit
conduct the breathing gas to and from the patient
collector vial
bulk moisture in the exhaled gas
comprises the components external to the
that protects against contamination
that protects the expiratory pneumatics from
Page 29

Introduction
OP 1
•an
expiratory filter
particulates in the patient’s exhaled gas into the room air or
inside the ventilator exhalation pneumatics
The ventilator actively controls the exhalation valve that the
software accurately positions throughout the patient’s inspiration
and exhalation. The exhalation valve allows the ventilator to
deliver aggressive breaths while pressure overshoots are
minimized, PEEP is controlled, and excess patient pressures are
relieved. The exhalation system monitors the exhaled gas leaving
the patient circuit for spirometry.
Throughout the respiratory cycle, pressure transducers monitor
inspiratory, expiratory, and atmospheric pressures. The
temperature of the exhaled gas is heated to a temperature above
its dew point to prevent condensation in the exhalation
compartment. Refer to Appendix C for a detailed diagram of the
ventilator’s pneumatic system and patient circuit.
that limits the escape of microorganisms and
1.1.6 AC mains and backup power system
The ventilator derives its power to operate from the AC mains
(wall) power or the backup power system (BPS). The design of the
BDU integral power supply protects against excessive voltages,
temperatures, or current draws. A power cord retainer prevents
accidental disconnection of the BDU from the AC mains. A power
switch cover on the front face of the BDU protects against spills
and accidental AC power-off.
The ventilator connects to the 802 BPS, which supplies DC power
to the ventilator if AC power is lost. A fully charged BPS operating
under nominal ambient conditions, can power the ventilator for
at least 30 minutes (the BPS does not power the compressor unit
or the humidifier, if present). The GUI indicates when the
ventilator is operating on the BPS, rather than AC mains.
When AC power is connected, it recharges the BPS. The BPS
continues to recharge from the AC power during normal
ventilator operation.
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 1-7
Page 30

OP 1
Introduction
1.1.7 Ventilator emergency states
Emergency states include
. When a
(SVO)
includes the SVO state. A SVO state can also occur independent of
a
ventilator inoperative
The following describe the two ventilator emergency states:
•
Safety valve open (SVO)
enters a
oxygen supplies are lost, or an
occlusion is detected, or the ventilator
enters the
condition.
The safety valve open
the patient to breathe room air
unassisted by the ventilator. The
ventilator remains in the
caused the emergency state is corrected.
When the ventilator enters the
on the front face of the BDU illuminates, and a high-urgency
alarm sounds.
In case of a malfunction that prevents software from opening
the safety valve, there is also an analog circuit that opens the
safety valve if system pressure exceeds 100 to 120 cmH
•
Ventilator inoperative
declares a ventilator inoperative
condition if a hardware failure or
critical software error occurs that could
compromise safe ventilation of the
patient.
When a ventilator inoperative
condition occurs, the ventilator
inoperative indicator on the front face
of the BDU illuminates and the ventilator enters the
which in turns sounds a high-urgency alarm.
ventilator inoperative
state if both air and
SVO
Ventilator Inoperative
ventilator inoperative
condition occurs, it always
condition.
: The ventilator
state allows
(SVO)
state until the condition that
SVO
SVO
: The ventilator
and
state, the
safety valve open
indicator
SVO
O.
2
state,
SVO
If a ventilator inoperative condition occurs, immediately
remove the ventilator from use until qualified service
personnel evaluate and correct the
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 1-8
Vent Ino p
condition.
Page 31

Introduction
If the ventilator declares a ventilator inoperative state, the
power on self test (POST) must first verify that power levels to
the ventilator are acceptable and that the functions of the
major electronics systems are satisfactory before normal
ventilation can resume. Qualified service personnel must
repair the ventilator to correct the problem and execute EST
successfully before normal ventilation is allowed.
1.2 Graphic user interface
This section describes the graphic user interface (GUI), the GUI
keys, the GUI indicators, and the symbols you see on the GUI.
OP 1
The graphic user interface (GUI) of the
comprises the
below the touch screens, and a knob. Use the knob to set a given
ventilator control parameter to its desired value. Press the
key—the off-screen key above and right of the knob—to enter the
selected value or parameter into memory.
Figure 1-2 identifies the components of the GUI, and the location
of information on the
DualView
touch screens, the off-screen keys located
DualView
touch screens.
Ventilator System
840
ACCEPT
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 1-9
Page 32

OP 1
Introduction
Upper screen:
monitored
information
(alarms,
patient data)
Lower screen:
ventilator
control
parameters
Figure 1-2. 840 Ventilator System graphic user interface (GUI)
Vital patient data
Alarm and ventilator status
Assorted patient data,
including graphical displays
Active alarm log, if applicable
Primary patient parameters
Setup of ventilator control
parameters, alarm limits,
breath timing parameters,
and other parameters
Prompt
Symbol definitions
area
Status
indicators
Off-screen
keys
CLEAR
key
ACCEPT
key
Knob
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 1-10
Page 33

Introduction
1.3 User interface controls and indicators
Descriptions of the controls and indicators on the graphic user
interface are given in Table 1-1 below.
Table 1-1: 840 Ventilator System controls and indicators
Control or indicator Function
Screen lock key: When the yellow light on the screen lock key
is lit, the screen or off-screen controls (including the knob and
ACCEPT
screen lock key again. New alarms automatically unlock the
screen and controls.
The screen lock allows you to clean the touch screen and
prevents inadvertent changes to settings and displays.
Alarm volume key: Allows you to adjust the alarm volume
when you hold down this key while turning the knob. You
cannot turn off the alarm volume.
Alarm silence key: Turns off the audible alarm sound for two
minutes. The yellow light on the alarm silence key illuminates
during the silence period. An ALARM SILENCE IN PROGRESS
indicator displays on the lower touch screen, along with a
CANCEL button, if there is not a higher-priority alarm display
active. To exit out of the alarm silence, touch the CANCEL
button.
The system automatically exits the alarm silence when the
two-minute interval times out. High-urgency alarms such as
Device Alerts, Safety Valve Open, Occlusion, and loss of either
gas supply cancel the alarm silence.
Each time you press the alarm silence key, the silence period
resets to two minutes. Each time you press the alarm silence
key (whether or not there is an active alarm), the keypress is
recorded in the alarm log.
key) have no effect when touched until you press the
OP 1
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 1-11
Page 34

OP 1
Table 1-1: 840 Ventilator System controls and indicators (cont)
Control or indicator Function
Alarm reset key: Clears active alarms or resets high-urgency
alarms and cancels an active alarm silence., and is recorded in
the alarm log. Each time you press the reset key, it is recorded
in the alarm log, if there is an active alarm. You cannot reset a
DEVICE ALERT alarm.
Information key: Displays basic operating information about
the ventilator. Press the key to display a menu of information
topics, then touch the button corresponding to the desired
topic. Browse topical information using the , ,
, and buttons located in the information header.
GO BACK
Oxygen sensor calibration key: Delivers 100% oxygen (if
available) for two minutes and calibrates the oxygen sensor.
The green light on this key illuminates and a message (100%
Cal in Progress) on the lower touch screen indicates that
O
2
100% O
delivery is active. If you press the O2 key again, the
2
system restarts the two-minute delivery interval. Press
CANCEL to stop the calibration.
Use the procedure in Section D.2 to test the oxygen sensor
calibration.
DIAGRAM
Introduction
Manual inspiration key: In A/C, SIMV, and SPONT modes,
delivers one manual breath to the patient in accordance with
the current mandatory breath parameters. In BILEVEL mode,
transitions from Low PEEP (PEEP
) to High PEEP (PEEPH) (or
L
vice versa). To avoid breath stacking, a manual inspiration is
not delivered during inspiration or during the restricted phase
of exhalation.
You can use the
MANUAL INSP
key to supplement minute
volume or to assist measurement of a patient data parameter,
such as peak inspiratory pressure, or to run an
INSP PAUSE
maneuver in SPONT mode.
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 1-12
Page 35

Introduction
Table 1-1: 840 Ventilator System controls and indicators (cont)
Control or indicator Function
Expiratory pause key: Causes the ventilator to seal the
patient’s breathing circuit when the expiratory phase of a
designated breath, mandatory or spontaneous, is followed by
a time-cycled mandatory inspiration. An expiratory pause is
used to estimate PEEP
The ventilator performs two types of pause maneuver:
automatic, which you initiate by a momentary press of the
EXP PAUSE
key, and manual, which you control by a
continuous press of the
performs the maneuver until the pressure stabilizes, then
takes its measurements. The pause lasts at least 0.5 second
and does not exceed 3.0 seconds.
During a manual pause, the ventilator takes its measurements
as soon as the pressure stabilizes or the pause ends. The
ventilator continues the maneuver until you release the
PAU SE
key. The pause cannot exceed 20 seconds. Section 4.9
describes in detail how to use the
Inspiratory pause key: Causes the ventilator to seal the
patient’s breathing circuit at the conclusion of the gas delivery
phase of a designated, volume- or pressure-based mandatory
inspiration. The inspiratory pause maneuver provides a means
to measure the patient’s static lung-thoracic compliance
), static resistance (R
(C
STAT
The inspiratory pause maneuver maintains the inflated state
of the lungs.
The ventilator performs two types of pause maneuver: auto-
matic, which is initiated by the momentary press of the
PAU SE
key, and manual, which you control by a continuous
press on the key.
An automatic pause performs the maneuver until the pressure
stabilizes, then the system takes its measurements. The pause
event lasts at least 0.5 second but no longer than 2.0 seconds.
In a manual pause, the maneuver continues until you release
INSP PAUSE
the
key, but cannot exceed 7 seconds. The ventilator computes C
and displays the values at the end of the maneuver. P
computed and updated continuously during the plateau, and
its value is frozen at the end of the plateau. Section 4.10
describes in detail how to use the
and PEEPI (autoPEEP).
TOT
EXP PAUSE
), and plateau pressure (PPL).
STAT
and R
STAT
STAT
key. An automatic pause
EXP PAUSE
key.
at the end of the plateau
INSP PAUSE
key.
OP 1
EXP
INSP
is
PL
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 1-13
Page 36

OP 1
Table 1-1: 840 Ventilator System controls and indicators (cont)
Control or indicator Function
Knob: Adjusts the value of a setting. A highlighted button on
a touch screen means that the knob is linked to that setting.
Where applicable, a clockwise turn of the knob increases the
highlighted value, and a counterclockwise turn of the knob
decreases the highlighted value.
Clear: Cancels a proposed ventilator parameter value change.
Accept: Applies and saves new ventilator parameter value(s).
Introduction
Red high-urgency alarm indicator ( ! ! ! ): This alarm
indicator blinks rapidly if active; it is steadily lit if autoreset.
Yellow medium-urgency alarm indicator ( ! ! ): This alarm
indicator blinks slowly if active; it turns off if autoreset.
Yellow low-urgency alarm indicator ( ! ): This indicator is
steadily lit if active; it turns off if autoreset.
Green normal ventilator operation indicator: When
ventilation is active and no alarm states exist, this indicator is
steadily lit. This indicator is off if the ventilator is not in a
ventilation mode, for example, during service mode or short
self test (SST).
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 1-14
Page 37

Introduction
Table 1-1: 840 Ventilator System controls and indicators (cont)
Control or indicator Function
Gray normal ventilator operation indicator: No ventilator
inoperative condition exists when indicator is not illuminated.
Red ventilator inoperative indicator: The ventilator cannot
support ventilation and requires service. The ventilator enters
the safe state (safety ventilation) and discontinues detection
of new patient data or alarm conditions. Qualified service
personnel must repair the ventilator to correct the problem
and execute EST successfully before normal ventilation is
allowed. This indicator is accompanied by an audio signal and
cannot be reset.
OP 1
Gray normal GUI operation indicator: No loss of GUI
condition exists when indicator is not illuminated.
Red safety valve open (SVO) indicator: The ventilator has
entered its safe state and opened its safety valve to allow the
patient to breathe unassisted from room air.
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 1-15
Page 38

OP 1
Table 1-1: 840 Ventilator System controls and indicators (cont)
Control or indicator Function
Green BPS ready indicator: The ventilator senses that the
BPS is installed, operational, and has at least two (2) minutes
of estimated run time.
On battery power indicator: When the yellow bar to the
right of a lit BPS ready indicator (battery symbol) is lit, the
ventilator is operating on BPS, and AC power is insufficient to
support ventilator operation. During BPS operation, power to
the compressor unit and the humidifier outlet (if available) is
off.
Green compressor ready indicator: The compressor logic
cable and air supply hose are connected to the ventilator. The
compressor is up to operating pressure but not supplying gas
to the ventilator. The compressor motor turns on
intermittently to keep the compressor chamber pressurized.
Green compressor operating indicator: When symbol to
the right of a lit compressor unit ready indicator is lit,
compressor is supplying air to the ventilator. This indicator
does not light unless the compressor is actually supplying air
to the ventilator.
Introduction
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 1-16
Page 39

Introduction
OP 1
The indicators on the breath delivery unit are shown in Table 1-2.
Table 1-2: BDU indicators
Red ventilator inoperative indicator: The ventilator cannot
support ventilation and requires service. The ventilator enters
the safe state (safety ventilation) and discontinues detection
of new patient data or alarm conditions. Qualified service
personnel must repair the ventilator to correct the problem
and execute EST successfully before normal ventilation is
allowed. This indicator is accompanied by an audio signal and
cannot be reset.
Red safety valve open (SVO) indicator: The ventilator has
entered its safe state and opened its safety valve to allow the
patient to breathe unassisted from room air.
Red loss of GUI indicator: The ventilator has detected a
malfunction that prevents the GUI from reliably displaying or
receiving information.
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 1-17
Page 40

OP 1
1.3.1 Onscreen symbols and abbreviations
Touch an onscreen symbol to display its definition in the lower
left corner of the lower screen. Table 1-3 summarizes the symbols
and abbreviations the ventilator uses.
For example, if you touch:
V
MAX
21.8
The symbol definition area shows this message:
V
MAX
Table 1-3: 840 Ventilator System symbols and abbreviations
L
min
= Peak flow
Introduction
Symbol or
abbreviation
(blinking)
Definition
Additional active alarms that relate to the monitored
information are active. The symbol blinks when there is not
enough screen area to display all active alarms.
The upper alarm limit
The lower alarm limit
Press to access the alarm log
Alarm log contains events that you have not yet viewed
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 1-18
Page 41

Introduction
OP 1
Table 1-3: 840 Ventilator System symbols and abbreviations (cont)
Symbol or
abbreviation
P
%
RAMP SQUARE
Definition
Rise time percent
Flow pattern
The value you selected for a ventilator control parameter
exceeds its recommended limit (soft bound) and requires
acknowledgement to continue
or
The value selected exceeds its allowable minimum or
maximum limit (hard bound)
Press to view more patient data
Press to view patient data graphics
Press to view additional screens
X-axis (time or pressure) adjust of patient data graphics
Y-axis (pressure, volume, or flow) adjust of patient data
graphics
Baseline pressure (PEEP) adjust
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 1-19
Page 42

OP 1
Introduction
Table 1-3: 840 Ventilator System symbols and abbreviations (cont)
Symbol or
abbreviation
Definition
A/C Assist/control ventilation mode
AV Apnea ventilation
C
E
SENS
STAT
Static compliance
Spont expiratory sensitivity percentage
EST Extended self test
f Respiratory rate (ventilator control parameter)
f
TOT
↑
f
TOT
Total respiratory rate (monitored)
High respiratory rate alarm
GUI Graphic user interface
HME Heat-moisture exchanger
I:E Inspiratory to expiratory ratio
O
2
O
2
Monitored oxygen percentage (patient data)
Oxygen percentage (ventilator control parameter)
1
O2% High delivered O2% alarm
↓
%Low delivered O
O
2
% alarm
2
PC Pressure control (mandatory breath type)
P
MEAN
↑
P
PEAK
2 P
PEAK
3
P
PEAK
4
P
PEAK
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
Mean circuit pressure
High circuit pressure alarm
High circuit pressure alarm limit
Low circuit pressure alarm
Low circuit pressure alarm limit
OP 1-20
Page 43

Introduction
OP 1
Table 1-3: 840 Ventilator System symbols and abbreviations (cont)
Symbol or
abbreviation
P
PEAK
Peak circuit pressure (patient data)
Definition
PEEP Positive end expiratory pressure (ventilator control parameter)
PEEP
PEEP
PEEP
PEEP
PEEP
P
I END
P
P
H
I
L
TOT
I
PL
High PEEP (ventilator control parameter, BILEVEL mode only)
Intrinsic PEEP (patient data)
Low PEEP (ventilator control parameter, BILEVEL mode only)
Total PEEP (patient data)
End expiratory pressure (patient data)
Inspiratory pressure (ventilator control parameter)
End inspiratory pressure (patient data)
Plateau pressure (patient data)
POST Power on self test
PS Pressure support (spontaneous breath type)
P
SENS
Pressure sensitivity
P
P
↑P
SUPP
-TRIG
VENT
R
STAT
Pressure support (ventilator control parameter)
Pressure triggering
High internal ventilator pressure alarm
Static resistance
SIMV Synchronous intermittent mandatory ventilation mode
SPONT Spontaneous ventilation mode
SST Short self test
T
A
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
Apnea interval
OP 1-21
Page 44

OP 1
T
Introduction
Table 1-3: 840 Ventilator System symbols and abbreviations (cont)
Symbol or
abbreviation
T
E
T
H
T
I
1
T
I SPONT
2
T
I SPONT
T
L
T
PL
V
E SET
Expiratory time
High PEEP time (BILEVEL mode only)
Inspiratory time
High spontaneous inspiration time alarm
High spontaneous inspiration time alarm limit
Low PEEP time (BILEVEL mode only)
Plateau time
Set minute volume (calculated from ventilator control
Definition
parameters)
V
E SPONT
1
V
3V
E TOT
E TO
Exhaled spontaneous minute volume
High exhaled minute volume alarm
Low exhaled minute volume alarm
VC Volume control (mandatory breath type)
V
MAX
V
SENS
V
T
V
TE
1
V
TE
3
V
TE MAND
3
V
TE SPONT
V
TI
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
Peak flow (ventilator control parameter)
Flow sensitivity
Tidal volume
Exhaled tidal volume
High exhaled tidal volume alarm
Low exhaled mandatory tidal volume alarm
Low exhaled spontaneous tidal volume alarm
Inspired tidal volume
OP 1-22
Page 45

Introduction
OP 1
Table 1-3: 840 Ventilator System symbols and abbreviations (cont)
Symbol or
abbreviation
1
V
TI
V
TI MAND
1
V
TI MAND
V
TI SPONT
1
V
TI SPONT
V
-TRIG
*Refer to Section 13.10 for information regarding inspired tidal volume alarms.
High inspired (mandatory or spontaneous) tidal volume
alarm*
Inspired mandatory tidal volume
High inspired mandatory tidal volume alarm*
Inspired spontaneous tidal volume
High inspired spontaneous tidal volume alarm*
Flow triggering
Definition
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 1-23
Page 46

OP 1
1.4 Ventilator system labeling symbols
The following symbols appear on the various components of the
Ventilator System.
840
NOTE:
All labels shown are examples, and may not reflect the exact
configuration of your ventilator.
Power switch positions: I represents the power on position
.
and
located on the BDU front panel, turns ON/OFF the BDU and
the GUI. When the power switch is in the off position, the BPS
continues to charge if AC power is present.
Refer to manual: When this symbol appears on the product, it
means refer to documentation for information.
Type B equipment, per IEC 60601-1
represents power off position. The power switch,
Introduction
Potential equalization point (ground): Provides a means of
connection between the equipment and the potential
equalization busbar of the electrical connection. A common
grounding point for the entire ventilator.
Indicates the degree of protection provided by enclosure
(drip-proof)
Signifies compliance with the Medical Device Directive,
93/42/EEC
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 1-24
Page 47

Introduction
OP 1
CSA certification mark that signifies the product has been
evaluated to the applicable ANSI/Underwriters Laboratories
Inc. (UL) and CSA standards for use in the US and Canada.
Date of manufacture label
1996-05
SN
TEST
PTS 2000
Serial number
BPS charging indicator: When the ventilator is operating on
mains power, the top symbol (green indicator next to gray
battery icon) on the front of the BPS indicates that the BPS is
charged, and the bottom symbol (yellow indicator next to gray
battery icon) on the front of the BPS indicates that the BPS is
charging.
Data key connection
Caution
Do not remove the data key. The data key enables
software options and stores ventilator operational
hours, compressor unit operational hours, and the
serial numbers for the BDU and GUI. The ventilator
will not operate without its factory-installed data key.
TEST (service) button: After you touch the Short Self Test
(SST) onscreen key (available only during ventilator startup),
you must press the TEST button within 5 seconds in order to
access SST.
Puritan Bennett PTS 2000™ Performance Test System
connection, for use by qualified service personnel only.
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 1-25
Page 48

OP 1
Introduction
GUI connection
Circuit breaker for ventilator power supply, located in the BDU.
Ventilator circuit breaker for compressor and humidifier
NOTE:
A humidifier connection is only available on 100 - 120 V
ventilators.
Alternating current (at AC inlet and AC power indicator)
Maximum allowed output to auxiliary mains socket
(compressor electrical connection)
BPS electrical connection
Exhalation filter latch unlock/lock
Exhalation filter latch open indicator: This red indicator is
located on the surface behind the closed latch, and is easily
visible when the filter latch is open.
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 1-26
Page 49

Introduction
OP 1
GUI mounting latch unlock/lock
Remote alarm port
IOIOI
RS-232 port
Susceptible to electrostatic discharge
Electric shock hazard
Explosion hazard
Fire hazard
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 1-27
Page 50

OP 1
3
802 BPS product information label
Dc
Puritan-Bennett Corporation
Pleasanton, CA USA
Made in Ireland
GUI product information label
Made in Ireland
®
™
Puritan-Bennett Corporation
Pleasanton, CA USA
Introduction
4-072504-00 Rev C 0603
4-073044-00 Rev C 060
GUI ports label
Remote alarm and RS-232 port (9.4-inch GUI only). Refer to Appendix E for GUI remote
alarm and RS-232 port specifications.
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 1-28
Page 51

Introduction
Humidifier electrical label
(This label not visible unless cover plate over humidifier electrical connection is
removed. A humidifier connection is only available on 100 - 120 V ventilators.)
BDU gas inlet label
OP 1
BDU To patient label
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 1-29
Page 52

OP 1
Compressor gas connection label
Compressor information label
Introduction
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 1-30
Page 53

Introduction
BDU information label
OP 1
Puritan-Bennett Corporation
Pleasanton, CA USA
Authorized Representative
Tyco Healthcare UK LTD
Gosport PO13 0AS, U.K.
Made in Ireland
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
4-071587-00 Rev E 0603
OP 1-31
Page 54

OP 1
BDU cooling vent label
BDU I/O disconnect label
Introduction
BDU exhaust information label
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 1-32
Page 55

Introduction
BPS electrical connection label
Compressor lint filter label
Expiratory limb connector on exhalation filter
From patient
OP 1
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 1-33
Page 56

OP 1
Introduction
This page is intentionally blank.
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 1-34
Page 57

C
HAPTER
2
How to set up the 840 ventilator
Chapter 2 describes how to set up the ventilator:
• How to connect the electrical supply
• How to connect the air and oxygen supplies
• How to connect the patient circuit and accessories
A Puritan Bennett Customer Service Engineer (CSE) must first
install the ventilator and run an extended self test (EST), which
calibrates the exhalation valve, flow sensors, and atmospheric
pressure transducer, before you connect a patient to the ventilator
for the first time.
Warning
• When you lift the ventilator, use assistance and
appropriate safety precautions. Figure 2-1 shows the
proper technique to lift each ventilator component.
• To avoid interrupted ventilator operation or possible
damage to the ventilator, always use the ventilator on a
level surface in its proper orientation.
• To avoid the possibility of injury to the patient and
ensure proper ventilator operation, do not attach any
device to the port labeled EXHAUST unless the device is
specifically authorized by Puritan Bennett.
• To minimize the increased risk of fire due to an oxygenenriched environment, do not use the ventilator in a
hyperbaric chamber.
• To avoid raising the oxygen concentration of room air,
use the ventilator in an adequately ventilated room.
2
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 2-1
Page 58

OP 2
Lift the BDU
from horizontal
surfaces as shown.
Use two people to lift
the compressor from
the base and the handles.
How to set up the 840 ventilator
Lift GUI from
base and
handle
Lift the GUI from
the base and the handle.
8-00011
Figure 2-1. How to lift the ventilator components
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 2-2
Page 59

How to set up the 840 ventilator
Caution
• Do not connect or disconnect the ventilator’s graphic user
interface (GUI), backup power source (BPS), or compressor
while the power switch is on or the ventilator is connected to ac
power.
• All components must be securely mounted and connected by
qualified service personnel according to the appropriate
Puritan Bennett installation instructions.
• Do not obstruct the breath delivery unit (BDU), GUI, or
compressor cooling vents or fan vents.
• To avoid possible damage to ventilator components, do not use
the horizontal surfaces of the ventilator to place or stack
objects.
NOTE:
Before you use the ventilator for the first time, wipe the
ventilator exterior clean and sterilize its components
according to the instructions in Chapter 7 of this manual.
Follow your institution’s protocol for cleaning and sterilizing
the ventilator and its components.
OP 2
2.1 How to connect the electrical supply
Warning
• To minimize the risk of electrical shock, always connect
the ventilator power cord into a grounded AC power
outlet.
• The 802 BPS must always be installed. Without the BPS,
the ventilator is not protected against low or lost AC
power. Do not use the ventilator unless a BPS with at
least minimal charge is installed.
• When possible, connect the ventilator to an outlet
connected to the hospital emergency back-up power
system. Refer to Section A.4 for ventilator electrical
specifications.
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 2-3
Page 60

OP 2
How to set up the 840 ventilator
Normally the
BPS operates the ventilator when AC power is lost or drops below
a minimum level.
A new, fully charged BPS can operate the ventilator (without the
compressor or a humidifier) for at least 30 minutes; allowing the
ventilator to be used for transport purposes within the healthcare
facility.
Warning
The 802 BPS is intended for short-term use only, and is not
intended as a primary alternative power source. The BPS is
intended to power the BDU and GUI only. In case of AC
power loss, power is not available to run either the
compressor or the humidifier.
If you turn on the ventilator after it has been unplugged for an
extended period, the LOW BATTERY alarm may sound. If this
occurs, recharge the 802 BPS by leaving it connected to a
ventilator connected to AC power for up to 8 hours (ventilator
does not need to be turned on). If, after turning the ventilator
back on, the LOW BATTERY alarm is still active or if the
INOPERATIVE BATTERY alarm is active, qualified service
personnel must replace the BPS battery.
Ventilator System is mains-powered. The 802
840
Figure 2-2 shows how to connect the power cord to AC power.
Built-in power cord retainer tabs protect against accidental
disconnection. Ensure that the power cord is securely fastened
into the AC receptacle prior to operation. To remove the cord,
squeeze the tabs on the top and bottom of the plug and pull
outward.
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 2-4
Page 61

How to set up the 840 ventilator
Power
cord
To AC power
Figure 2-2. How to connect the ventilator power cord
OP 2
Power cord retainer tabs.
Squeeze tabs and pull outward to
disconnect power cord.
8-00002
Figure 2-3 shows the power switch and AC indicator. When
illuminated, the AC indicator indicates that the ventilator is
receiving AC power and that the 802 BPS will be recharged as
needed. The AC indicator is independent of the power switch, and
the power switch does not turn off AC power to the ventilator
power supply. When both the power switch and AC indicator are
on, power is available for the humidifier and compressor.
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 2-5
Page 62

OP 2
How to set up the 840 ventilator
AC indicator
Ventilator
power switch
AC panel
Humidifier
and compressor
circuit breaker
Ventilator
power supply
circuit breaker
Potential
equalization
(ground
point)
Compressor
connection
AC power
connection
8-00046
Figure 2-3. Ventilator power switch, AC indicator, and AC panel
If the ventilator power supply circuit breaker (located on the
ventilator's AC panel, Figure 2-3) opens but AC power is still
present and the ventilator is operating on BPS, power is still
available to the humidifier and compressor connectors (although
ventilator software disables compressor operation).
NOTE:
A humidifier connection is only available on 100 - 120 V
ventilators.
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 2-6
Page 63

How to set up the 840 ventilator
When the power cord is not in use, wrap the power cord around
the hook on the back of the cart for convenient storage
(Figure 2-4).
OP 2
8-00004
Figure 2-4. Power cord storage on the cart
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 2-7
Page 64

OP 2
How to set up the 840 ventilator
2.2 How to connect the air and oxygen supplies
The
or wall supplies. Follow these steps to connect the air and oxygen
supplies:
1. Ensure that the supply pressures are 35 to 100 psi
2. Connect the supply hoses to the inlet connectors at the rear of
Ventilator System can use air and oxygen from cylinder
840
(241 to 690 kPa).
Warning
Due to excessive restriction of certain hose assemblies
(listed in Table B-1), reduced ventilator performance may
result when oxygen or air supply pressures
(345 kPa) are employed.
the ventilator (see Figure 2-5).
Warning
• Connect only air to the air inlet, and only oxygen to the
oxygen inlet. Do not attempt to switch air and oxygen or
connect any other gas.
• Always connect at least two gas sources to the ventilator
to ensure that a constant gas supply is available to the
patient. There are three gas source connections: the
compressor, air inlet, and oxygen inlet.
• Do not use conductive, high-pressure supply hoses.
Doing so may negatively affect the ventilator’s ground
isolation characteristics.
• Use only high-pressure supply hoses recommended by
Puritan Bennett. Other hoses may be restrictive and may
cause improper ventilator operation.
< 50 psi
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 2-8
Page 65

How to set up the 840 ventilator
Caution
To prevent damage to the ventilator, ensure that the connections
to the air and oxygen supplies are clean and unlubricated, and
that there is no water in the air or oxygen supply gas.
If you suspect water in the air supply gas, use an external wall air
water trap to prevent water damage to the ventilator or its
components.
NOTE:
When you connect a pressurized air or oxygen source, the
ventilator air and oxygen regulators have a maximum bleed rate
of 3 L/min, even when the ventilator is not in use. Always take this
bleed rate into account when calculating air and oxygen usage.
When the air and oxygen hoses are not in use, you can wrap them
around the hook on the back of the cart for convenient storage
(Figure 2-5).
OP 2
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 2-9
Page 66

OP 2
Air inlet
connector
Oxygen
connector
How to set up the 840 ventilator
inlet
Oxygen hose
(from oxygen
supply)
Air hose
(from air
supply)
8-00005
Figure 2-5. How to connect the air and oxygen supplies
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 2-10
Page 67

How to set up the 840 ventilator
2.3 How to connect the patient circuit components
Warning
• To minimize the risk of bacterial contamination or
component damage, inspiratory and expiratory filters
must always be handled with care and connected to the
ventilator during use.
• To minimize the risk of patient injury, use only patient
circuits qualified for use in oxygen-enriched
environments with the 840 Ventilator System. Do not
use antistatic or electrically conductive tubing. To ensure
a leak-tight connection, only use connectors and tubes
with ISO-standard cone and socket fittings (or use
adapters to connect barbed cuff fittings to ISO-standard
fittings).
• If you use an external, pneumatically-powered nebulizer
with the 840 ventilator, it adds flow to the patient circuit
and can adversely affect spirometry, delivered O
delivered tidal volumes, and breath triggering.
Additionally, aerosolized particulates in the ventilator
circuit can lead to an increase in exhalation filter
resistance.
• Use one of the patient circuits listed in Appendix B to
ensure that the maximum pressure/flow values specified
by IEC 60601-2-12:2001 are not exceeded (see Table A-11
on page OP A-18 for patient circuit testing
specifications). Using a circuit with a higher resistance
does not prevent ventilation, but can cause a short self
test (SST) fault or compromise the patient’s ability to
breathe through the circuit.
2
%,
OP 2
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 2-11
Page 68

OP 2
How to set up the 840 ventilator
NOTE:
• Puritan Bennett recommends that you run SST every 15 days,
and between patients, and when you change the patient
circuit (particularly when you change circuit type, for example,
from adult to pediatric or neonatal).
• Puritan Bennett recognizes that the protocol for running
SST varies widely among health care institutions.
Puritan Bennett does not specify or require specific
practices that will meet the needs of all institutions, nor is
Puritan Bennett responsible for the effectiveness of
institutional practices.
2.3.1 How to select and connect a patient circuit
Use low-compliance patient circuits to ensure optimum
compliance compensation, and use pediatric patient circuits
when the patient ideal body weight (IBW) is greater than 7 kg
(15 lb) but less than or equal to 24 kg (53 lb). Use the
software option and neonatal patient circuits for patients whose
IBW is less than or equal to 7 kg.
NeoMode
For patients whose IBW is less than or equal to 24 kg, the
compliance compensation volume limit is four times the set tidal
volume, in addition to the set tidal volume. To avoid activating a
severe occlusion alarm, only use neonatal patient circuits with the
NeoMode
Table 2-1 shows IBW values and patient circuit types. The
“Allowed but not recommended” ranges require an override.
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 2-12
software option.
Warning
Recommended ranges exist to ensure patient safety. Only
those with the expertise to judge the appropriate
circumstances should override the recommended ranges.
Page 69

How to set up the 840 ventilator
Table 2-1: Patient circuit and IBW values
Recommendation Ideal body weight (IBW) in kg (lb)
Recommended Neonatal: 0.5-7.0 kg (1.1-15 lb)
OP 2
Pediatric: 7.0-24 kg (15-53 lb)
Adult: 25-150 kg (55-330 lb)
Allowed but not
recommended
Neonatal: Not applicable
Pediatric: 3.5-6.5 kg (7.7-14.3 lb), and
25-35 kg (55-77 lb)
Adult: 7-24 kg (15-53 lb)
Figure 2-6 shows how to connect the patient circuit, including the
inspiratory filter, humidifier (if used), inspiratory limb, patient
wye, expiratory limb, collector vial, and expiratory filter.
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 2-13
Page 70

OP 2
How to set up the 840 ventilator
(From patient)
Expiratory
filter
(To patient)
Patient wye
Inspiratory limb
of patient circuit
Figure 2-6. How to connect the patient circuit
Warning
To ensure that all patient circuit connections are leak-tight,
always perform a circuit leak test by running SST each time
you install the expiratory filter on the ventilator.
Expiratory limb
of patient circuit
Collector
vial
Inspiratory
filter
Tubing
Humidifier
8-00006
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 2-14
Page 71

How to set up the 840 ventilator
Warning
Adding accessories to the ventilator can increase system
resistance. Ensure that any changes to the recommended
ventilator circuit configurations do not exceed the specified
values for inspiratory and expiratory resistance
(Appendix A). If you add accessories to the patient circuit,
always run SST to measure circuit compliance before you
begin ventilation of the patient.
2.3.2 How to install the expiratory filter and collector vial
Install the expiratory filter and collector vial as follows:
1. Place the expiratory filter latch in the up position (see
Figure 2-7).
2. Slide the expiratory filter into the housing area with the
expiratory limb connection facing you.
3. Push the expiratory filter latch down; it will position the filter
properly.
OP 2
4. Attach the expiratory limb of the patient circuit to the filter’s
expiratory limb connection.
If you do not use a drain bag, be sure to cap the collector vial drain
port on the expiratory filter (Figure 2-8).
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 2-15
Page 72

OP 2
Pull latch up to
install filter, pull
down to hold filter
and collector vial
in place
Expiratory
filter
Expiratory limb
connection
(from patient)
Figure 2-7. How to install the expiratory filter and collector vial
How to set up the 840 ventilator
Slide filter rim
onto these tracks
Filter
housing
area
Collector vial
8-00018
If you use a drain bag:
Install the expiratory filter. (Refer to the instructions above.)
1
Install the clamp on the drain bag tubing, making sure that
2
the clamp is closed.
Uncap collector vial drain port at the base of the collector vial.
3
Connect the collector bag tubing to the vial drain port.
4
Connect the other end of tubing to drain bag.
5
If the ventilator is mounted on the cart, place the drain bag in
6
the cart drawer (Figure 2-8).
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 2-16
Page 73

How to set up the 840 ventilator
Tubing
Drain bag
OP 2
Place the drain bag
in the cart drawer
Clamp
The collector vial drain port
must be capped if you do not
use a drain bag
8-00007
Figure 2-8. How to use the collector vial with or without the drain bag
NOTE:
• The drain bag is designed to lie flat and should not be
suspended.
• Check the inspiratory and expiratory limbs of the patient
circuit, the collector vial, and the in-line water traps regularly
for water buildup. Under certain conditions, they can fill
quickly. Empty and clean the collector vial and in-line water
traps as necessary.
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 2-17
Page 74

OP 2
Flex arm
How to set up the 840 ventilator
2.3.3 How to install the flex arm
The flex arm supports the patient circuit between the ventilator
and the patient. Figure 2-9 shows how to install the flex arm onto
one of the two threaded sockets on the ventilator cart.
Threaded
socket
Threaded
socket in the cart
(one of two)
8-00008
Figure 2-9. How to install the flex arm
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 2-18
Page 75

How to set up the 840 ventilator
Caution
Use only the cart handles to move the ventilator. Do not pull or
push the ventilator with the flex arm.
OP 2
Flex arm replacement parts can be found in the
System Service Manual
.
840 Ventilator
2.3.4 How to install the humidifier
An electrical outlet for a humidifier is located on the front of the
BDU. Figure 2-10 shows how to install a Fisher & Paykel
humidifier onto the ventilator.
Warning
• When using a Fisher & Paykel humidifier with the
840 ventilator, use the appropriate Fisher & Paykel
humidifier chambers for adult, pediatric, and neonatal
patients.
• Take proper precautions to prevent water/condensate
from splashing into the patient circuit during circuit
disconnects and high peak flow rate conditions.
• To avoid possible patient injury or damage to the
ventilator system, follow your institution’s protocol for
proper patient circuit condensate management.
Caution
• Qualified service personnel must first install the humidifier
mounting hardware.
• To avoid equipment damage to the ventilator due to liquid
ingress:
- Install the plug cover when the humidifier is plugged into the
ventilator.
- Install the flat cover plate over the humidifier electrical outlet on
the front of the BDU when the humidifier is not plugged into the
ventilator.
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 2-19
Page 76

OP 2
How to set up the 840 ventilator
NOTE:
• To ensure uninterrupted ventilator operation, do not install a
humidifier whose maximum current capabilities exceed 2.3 A,
with a maximum power consumption of 270 VA.
• When you install a Fisher & Paykel humidifier, make sure the
humidifier has a right-angle electrical plug. A short power cord
is preferable.
• To ensure that ventilator occlusion detection operates
properly, do not use Puritan-Bennett Cascade humidifiers with
the 840 Ventilator System.
• If you have further questions about humidifiers qualified for
use with the 840 Ventilator System, contact your
Puritan Bennett representative.
• A humidifier connection is only available on 100 - 120 V
ventilators.
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 2-20
Page 77

How to set up the 840 ventilator
Plug cover
OP 2
BDU
Humidifier
Mounting
bracket on
front of
ventilator
Figure 2-10. How to install the humidifier
(Fisher & Paykel version shown)
8-00009
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 2-21
Page 78

OP 2
How to set up the 840 ventilator
2.3.5 How to use the ventilator cart
Figure 2-11 shows how to lock and unlock the cart’s front wheels.
Warning
To avoid interrupted ventilator operation or damage to
ventilator components, use the cart to move the ventilator.
Do not use the cables, the power cord, or patient circuit
components to push or pull the ventilator.
Press down
to lock
Unlocked position Locked position
Press down
to unlock
8-00010
Figure 2-11. How to lock and unlock the cart’s front wheels
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 2-22
Page 79

C
HAPTER
3
How to run Short Self Test (SST)
Chapter 3 tells you:
• When to run SST
• Required equipment for SST
• How to set up and run SST
• The SST tests and their functions
• How to understand the results of SST
3
3.1 Introduction to SST
SST uses an internal, programmed sequence of tests to:
• Verify proper function of the flow and pressure sensors
• Check the patient circuit for gas leaks
• Measure the expiratory filter resistance
• Measure patient circuit resistance
• Measure patient circuit compliance
SST requires approximately three minutes to complete.
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 3-1
Page 80

OP 3
Warning
• Always disconnect the ventilator from the patient before
you run SST. If you run SST while the ventilator is
connected to the patient, physical injury to the patient
may occur.
• An ALERT reported by SST indicates that the ventilator or a
related component has a defect. Repair the ventilator or
related component before you use the ventilator on a
patient, unless you can determine with certainty that the
defect cannot create a hazard for the patient, or add to the
risks that may occur from other hazards.
• When you run SST, configure the patient circuit exactly as
it will be used on the patient (for example, with same
accessories). If you add accessories to the patient circuit
after you run SST, you must rerun SST with the new
accessories installed before you begin to ventilate the
patient.
3.2 When to run SST
How to run Short Self Test (SST)
NOTE:
Puritan Bennett recognizes that health care institutions may
have their own ventilator protocols. However, Puritan
Bennett is not responsible for the effectiveness of any
institution’s protocols. Nor can Puritan Bennett specify, or
require, specific practices that will meet the internal needs of
every health care institution.
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 3-2
Page 81

How to run Short Self Test (SST)
Puritan Bennett recommends that you run SST when one or more
of the events below occurs:
• When you replace the patient circuit and the exhalation filter
after 15 days of use
• When you are ready to connect a new patient to the ventilator
• When you connect a different patient circuit to the ventilator
• When you install a new or sterilized expiratory filter
• When you change the patient circuit type
• When you change the humidification device type
• When you remove or add accessories to the patient circuit,
such as a humidifier, water trap, or drain bag
OP 3
Use SST at any time, provided that a patient is
ventilator, to:
• Check the patient circuit for gas leaks
• Calculate patient circuit compliance and resistance
• Calculate expiratory filter resistance
After SST begins, the system prompts you to prepare the ventilator
to conduct certain tests. The system waits indefinitely at a prompt
until you take action and respond appropriately.
3.3 SST components and requirements
When you conduct SST, you must have available the components
and equipment that you will use on the patient:
• Patient tubing
• Expiratory filter and collector vial
•Inspiratory filter
• Humidifier, as applicable
• Other accessories (e.g. water traps, drain bag), as applicable
Additional requirements include:
attached to the
not
• A No. 1 rubber stopper to block the airway at the patient wye
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 3-3
Page 82

OP 3
• Two gas sources (air and oxygen) connected to the ventilator
• Each gas source pressure must be between 35-100 psi
(241 to 690 kPa)
Caution
• To prevent SST failures due to leaks, ensure that any circuit
components such as collector vial drain port cap (if not using a
drain bag), the seal between the expiratory filter and collector
vial, and water trap (if used) seals are properly installed.
• If you are using a drain bag, ensure that the tubing is properly
installed on the collector vial drain port and that the tubing is
clamped. If the drain bag tubing is not clamped during SST,
large leaks and large compliance values are possible which may
cause SST to report ALERTs or FAILURES.
Wait at least 10 minutes after you turn on the ventilator before
you run SST. The warm up time of 10 minutes will stabilize the
ventilator and ensure the accuracy of the SST tests.
3.4 SST Procedure
How to run Short Self Test (SST)
Warning
Always disconnect the ventilator from the patient before
you run SST. If you run SST while the ventilator is
connected to the patient, physical injury to the patient may
occur.
1 Turn the power switch (located on the front of the BDU). The
system conducts the POST (power-on self test) and displays
the
Ventilator Startup
2 Allow the ventilator to stabilize for ten minutes with the
power on.
3 Install the patient circuit, the expiratory and inspiratory filters
that you will use to ventilate the patient.
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 3-4
screen.
Page 83

How to run Short Self Test (SST)
Caution
The patient circuit must be unobstructed and properly connected
to the ventilator to ensure accurate circuit resistance
measurement.
OP 3
4At the
Ventilator Startup
touch screen), then press the
screen, touch the SST button (lower
button (on the left side of
TEST
the BDU) within 5 seconds. (Refer to Figure 3-1 for location of
button.)
TEST
The system displays the
SST Setup
screen (lower touch screen).
NOTE:
You must press the TEST button within 5 seconds of touching
the SST button or SST will not start.
Test
button
Figure 3-1. Test button location
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 3-5
Page 84

OP 3
How to run Short Self Test (SST)
Caution
Do not press the test button when powering up the ventilator. This
may cause the ventilator to enter Service Mode. If you enter
Service Mode, do not attempt to run Extended Self Test (EST) with
a patient circuit. Doing so will cause EST to fail. If EST fails, the
ventilator will remain in a Ventilator Inoperative state until EST
successfully passes.
If you accidentally enter Service Mode, exit Service Mode by
touching the EXIT button on the lower GUI screen and then
pressing the ACCEPT key.
5Touch the
PATIENT CIRCUIT
key in the lower touch screen,
then use the knob to select either Adult, Pediatric, or Neonatal
(if
NeoMode
6Touch the
software option is installed) patient circuit.
HUMIDIFICATION TYPE
key in the lower touch
screen, then use the knob to select the humidification type
that you will use for patient ventilation.
If you will not use a humidifier, set the humidification type to
.
HME
7 Press
ACCEPT
to complete your selection of the patient circuit
and humidification types.
Warning
Incorrectly specifying the patient circuit type or changing
the patient circuit type after you have run SST can affect
the accuracy of the compliance calculation, the measured
exhaled tidal volume, and delivered/measured inspired
tidal volumes. You must rerun SST when you change the
circuit type.
Compliance calculation and tidal volume accuracy may also
be affected by incorrectly specifying or changing the
humidifier after running SST. If you change humidifiers,
ensure you change the humidification type as described in
Section 4.8. For optimum accuracy, rerun SST using the
new humidifier.
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 3-6
Page 85

How to run Short Self Test (SST)
8 The ventilator automatically starts the test sequence. Refer to
Table 3-1 for details regarding each SST test step.
The SST
Flow Sensor, Expiratory Filter, Circuit Resistance
Compliance Calibration
system will wait indefinitely for your response. Otherwise you
don’t need to do anything unless a test result is
FAILURE
, or SST is complete.
9 As each test is performed, the
results (see Table 3-2).
Warning
To ensure reliable SST results, do not repeat an individual
test with a different patient circuit if the test result is
FAILURE or ALERT. If you suspect a defective patient circuit,
replace the patient circuit and restart SST from the
beginning.
OP 3
, and
tests require your intervention. The
or
ALERT
SST Status
screen shows test
10 You can touch
touch
EXIT SST
EXIT SST
again to resume testing, or press
restart the ventilator (if SST has not detected an
FAILURE
).
during SST to halt testing. You can
ACCEPT
ALERT
to
or
Warning
To ensure correct compensation for circuit resistance and
compliance, do not exit SST until the entire SST is
successfully completed. Do not begin normal ventilation
until the entire SST is successfully completed with the
correct patient circuit installed.
11 When all of the tests in SST are complete, the
SST Status
screen
displays all individual test results and SST outcome. Table 3-3
summarizes overall SST outcomes and how to proceed in each
case.
12 To begin normal ventilation (if SST has not detected an
or
FAILURE
13 The ventilator reruns
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
), touch
EXIT SST
POST
, then press
.
ACCEPT
.
ALERT
OP 3-7
Page 86

OP 3
How to run Short Self Test (SST)
14 The ventilator displays the
with
Ventilator Startup
Ventilator Startup
to configure the system for the patient.
Table 3-1: SST test sequence
Test step Function Comments
SST Setup The system prompts you to
specify the patient circuit
type and humidification type
that you will use for the
patient ventilation.
1 Specify the patient circuit
type.
2 Specify the humidification
type.
You can select one of three
humidification types:
• Heated expiratory tube
• Non-heated expiratory
tube
• HME (heat-moisture
exchanger)
3 For non-HME humidifiers,
specify the dry humidifier
volume. Use the specified
volume, not the
compressible volume, of
the humidifier.
4 Press the
screen. Proceed
ACCEPT
key.
Warning
Select the correct
patient circuit type
and humidification
type. Otherwise,
faulty occlusion
detection and
erroneous expiratory
spirometry can result.
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 3-8
Page 87

How to run Short Self Test (SST)
Table 3-1: SST test sequence (cont)
Test step Function Comments
NOTE:
HUMIDIFIER VOLUME
The
HME.
button is not visible on the touch screen if you select
OP 3
SST Setup (cont) The system prompts you to
connect the patient circuit to
inspiratory filter.
Use Figure 2-6 on page OP
2-14 to connect the patient
circuit.
1 Connect the patient circuit
to the inspiratory filter—
but without the
humidifier.
2 Press
ACCEPT
the test.
NOTE:
Do not run the Flow Sensor Test with a humidifier
installed, even if you will use a humidifier when you
begin patient ventilation.
The system prompts you to
block the patient wye.
The system checks the
accuracy of the inspiratory
and expiratory flow sensors.
After the test completes, the
system prompts you to
connect the humidifier.
3 Block the wye with a
No. 1 stopper.
4 Press
If the status of the SST Flow
Sensor Test is
cannot use the
function.
ACCEPT
FAILURE
NOTE:
If you will use a humidifier during patient ventilation, connect the humidifier
to the patient circuit after the system passes the SST Flow Sensor Test. Refer to
Figure 2-6 on page OP 2-14 for connection information.
to begin
.
, you
OVERRIDE
Circuit Pressure Test The system verifies proper
function of the BDU pressure
sensors.
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
If the status of the Circuit
Pressure Test is FAILURE, you
cannot use the
function.
OVERRIDE
OP 3-9
Page 88

OP 3
How to run Short Self Test (SST)
Table 3-1: SST test sequence (cont)
Test step Function Comments
Circuit Leak Test The system determines the
ability of the circuit to hold
pressure.
The system displays the drop
in circuit pressure over a
10 second interval.
Expiratory Filter
Resistance Test
The system prompts you to
detach circuit tubing from
the expiratory filter.
At the conclusion of the
Expiratory Filter Resistance
Tes t, the system displays the
pressure drop across the
expiratory filter.
ALERT
If the system reports
and you choose to override
the alert status, the result can
be improper compliance
compensation, inaccurate
tidal volume delivery, or
autotriggering during patient
ventilation.
If the test detects excessive
leaks, the system reports a
FAILURE
1 Detach the patient circuit
2 Press
If the system reports an
for the Expiratory Filter
Resistance Test and you
override the
inaccurate patient pressure
estimation can result.
The system will report a
FAILURE
exhalation compartment
occlusion or an expiratory
filter occlusion.
If you do not correctly follow
the prompts to disconnect
and connect the patient
circuit, the system will report a
FAILURE
.
from the expiratory filter.
ACCEPT
the test.
if the test detects an
.
ALERT
to begin
, an
ALERT
The system prompts you to
reattach the patient circuit.
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 3-10
3 Reattach the patient
circuit to the expiratory
filter.
4 Press
ACCEPT
the next test.
to begin
Page 89

How to run Short Self Test (SST)
Table 3-1: SST test sequence (cont)
Test step Function Comments
OP 3
Circuit Resistance The system prompts you to
unblock the patient wye.
The system displays the
pressure drop across the
inspiratory and expiratory
limbs.
The reported pressure drop
includes the effect of all
devices installed on each
limb, such as filters, water
traps, or a humidifier.
Compliance
Calibration
The system prompts you to
block the patient wye.
If you selected a
humidification type of either
Heated exp tube or Nonheated exp tube, the
ventilator prompts you to
indicate if there is water in
the humidifier.
1 Remove the stopper from
the wye.
2 Press
If the system reports an
for the pressure drop across
the two limbs and you
override the
inaccurate patient pressure
estimation can result.
The system reports a
if the test detects excessive
high or low limb resistance, or
if you do not follow the
prompt to unblock the wye.
1 Block the wye with a
2 Press
3 Press ACCEPT to indicate
ACCEPT
the test.
No. 1 stopper.
ACCEPT
the patient circuit
compliance test.
YES
or CLEAR to indicate
NO
, as appropriate, to
indicate whether or not
there is water in the
humidifier.
ALERT
to begin
ALERT
, an
FAILURE
to begin
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 3-11
Page 90

OP 3
How to run Short Self Test (SST)
Table 3-1: SST test sequence (cont)
Test step Function Comments
Compliance
Calibration (cont)
3.5 SST Results
The
individual SST test results, and the overall SST outcome.
ALERT
You can override an
can determine with certainty that the defect in the ventilator or
related component cannot create a hazard for the patient, or add
to the risks that may arise from other hazards.
ventilator uses four status categories to characterize the
840
The system displays the
compliance of the patient
circuit.
The system prompts you to
unblock the patient wye.
reported for an individual test if you
ALERT
If the system reports an
for the patient circuit
compliance and you override
ALERT
the
compliance compensation or
inaccurate tidal volume
delivery can result.
The system reports a
if the test detects an out-ofrange compliance condition.
4 Remove the stopper from
5 Press
, improper
the patient wye.
ACCEPT
complete the SST test
sequence.
ALERT
FAILURE
to
NOTE:
If an ALERT is reported and you exit SST without overriding the
ALERT, the ventilator will enter the safety valve open (SVO)
state and cannot be used for normal ventilation until SST
passes or the ALERT is overridden.
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 3-12
Page 91

How to run Short Self Test (SST)
FAILURE
OP 3
When the system declares a
FAILURE
for an individual test in the
SST sequence, the ventilator enters the SVO state. When a
ventilator experiences a
FAILURE
, immediately remove the
equipment from clinical use until qualified service personnel have
completed and verified the necessary repairs.
OVERRIDDEN
OVERRIDDEN
is a final status of the overall SST outcome and
indicates that you used the override feature when the system
reported an
the test with an
PASS
is the final status of the overall SST outcome in which no
PASS
condition. (The ventilator must have ended
ALERT
condition.)
ALERT
alerts or failures were detected.
Refer to Table 3-2 and Table 3-3 to learn how to interpret and
respond to each of these SST status categories.
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 3-13
Page 92

OP 3
How to run Short Self Test (SST)
3.5.1 How to interpret individual SST test results
SST reports a test result status for each of the individual tests. Use
Table 3-2 to interpret SST test results and to determine how to
respond.
Table 3-2: Individual SST test results
If the test
status is:
PASSED
ALERT
FAILURE
It means: Do this:
The system did not
detect a fault for the
You do not need to do anything, unless you
are prompted by the ventilator.
individual test.
The test result is not
ideal, but is not
When the system prompts you, touch one of
these buttons, then press ACCEPT:
critical.
If SST is in progress, it
EXIT SST
halts further testing
and prompts you to
make a decision.
A critical problem has
been detected, and
RESTART SST
REPEAT
Touch one of these buttons, then press
ACCEPT:
SST cannot complete
until the ventilator
EXIT SST
passes the failed test.
RESTART SST
NEXT
Discontinue SST
Repeat SST from the
beginning
Proceed to the next test
Repeat the test
Discontinue SST
Repeat SST from the
beginning
REPEAT
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
Repeat the test
OP 3-14
Page 93

How to run Short Self Test (SST)
3.5.2 SST outcomes
When SST has completed all of the tests, use Table 3-3 to
determine how to proceed.
Table 3-3: Overall SST outcomes
OP 3
If the SST
outcome is:
PASSED
ALERT
It means: Do this:
All tests passed. Touch one of these buttons, then press
ACCEPT:
Exit SST and begin normal
ventilation
Repeat SST from the
beginning
Discontinue SST
One or more faults
were detected. If you
can determine with
certainty that this
EXIT SST
RESTART SST
Touch one of these buttons, then press
ACCEPT:
EXIT SST
cannot create a
hazard for the patient,
or add to the risks
which may arise from
other hazards, you
can choose to
override the ALERT
status and authorize
ventilation.
RESTART SST
OVERRIDE
Repeat SST from the
beginning
Press ACCEPT to override
the ALERT, as allowed by
your institution’s protocol.
Touch EXIT SST, then press
ACCEPT to begin normal
ventilation.
FAILURE
One or more critical
faults were detected.
The ventilator enters
the SVO state and
cannot be used for
Restart SST with a different patient circuit.
Touch one of these buttons, then press
ACCEPT:
EXIT SST
Discontinue SST
normal ventilation
until SST passes.
Service is required.
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
RESTART SST
Press ACCEPT to repeat
SST from the beginning. If
the failure persists, contact
qualified service personnel.
OP 3-15
Page 94

OP 3
How to run Short Self Test (SST)
This page is intentionally blank.
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 3-16
Page 95

C
HAPTER
4
How to use the 840 ventilator
Chapter 4 tells you:
• How the ventilator user interface is structured
• How to start up the ventilator for a new or previous patient
• How to change main settings
• How to change other settings
• How to set the humidification type, expiratory sensitivity, and
disconnect sensitivity
• How to enable or disable the oxygen sensor
• How to select and set the variable that remains constant when
the breath rate setting is changed
• How to set the alarm limits
• How to perform inspiratory and expiratory pause maneuvers
• How to interpret inspiratory pause maneuver displays
• How to use Non-invasive ventilation (NIV)
4
NOTE:
DualView
The
you touch the screen. To avoid a DEVICE ALERT alarm, do not
place any foreign substances or objects on the screen.
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
touch screens use light beams to detect where
OP 4-1
Page 96

OP 4
r
4.1 Structure of user interface
The following buttons are available on the upper and lower touch
screens. These buttons appear across the bottom portion of each
of the two touch screens.
Upper screen
How to use the 840 ventilator
Display More patient
graphics
vent setup (vent
type, mode,
breath types,
trigger type,
settings)
data (e.g. O2%,
P
I END
Diagnostic
code log
(system
diagnostic,
system
information,
EST/SST
diagnostic
logs)
VENT
SETUP
)
Current/proposed
apnea setup
Alarm log Active alarms
(time, event,
urgency, alarm,
analysis)
Operational
time log
(compressor,
ventilator
hours)
Lower screen
APNEA
SETUP
Communication
setup (printer/DCI,
baud rate, data bits,
parity mode)
SST result
log
ALARM
SETUP
Current/proposed
alarm settings
Ventilator
configuration
(revisions,
serial numbers,
part numbers,
installed
options)
Time/date
change
Other screens
Test
summary
(time, date,
outcome of
SST, EST)
Other screensCurrent/proposed
More settings
(humidification type,
sensor enable/
O
2
disable, disconnect
sensitivity, humidifie
volume)
Figure 4-1. Touch screen user interface
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 4-2
Page 97

How to use the 840 ventilator
4.2 Patient setup
Warning
Always complete the patient setup before you attach a
patient to the ventilator. If you attach a patient before the
setup procedure is complete, the ventilator issues a
procedure error and initiates the safety ventilation mode.
When you turn on the ventilator, the ventilator automatically
runs POST (Power On Self Test). After POST passes, the system
displays the
screen. The prompt area, located in the lower right corner of the
lower screen, contains setup instructions.
Ventilator Startup
OP 4
screen (see Figure 4-2) on the lower
Figure 4-2. Ventilator Startup screen
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
OP 4-3
Page 98

OP 4
How to use the 840 ventilator
4.2.1 How to ventilate with most recent control parameters
To continue ventilation with the most recent ventilator control
parameters, touch
Same Patient
and press
ACCEPT
. Ventilation
does not begin until a patient is connected. A flashing reminder
arrow prompts you to consider the previous Tube I.D. and Tube
Type if the prior Spontaneous Type used these parameters.
4.2.2 How to ventilate with new control parameters
Refer to Table A-12 in Appendix A for the descriptions, ranges,
resolutions, accuracies, and new patient values of the available
ventilator control parameters.
1Touch the
New Patient
parameters for patient ventilation.
2Touch the
(ideal body weight) button, then turn the knob
IBW
to adjust the IBW. The proposed value is highlighted.
Warning
Always enter the IBW that is appropriate for the patient.
The system uses the patient’s IBW to automatically set
certain values, alarm limits, and parameter boundary limits
for several initial parameters. (The IBW values that
correlate with patient height are listed in Table 4-1 and
Table 4-2.)
button to select new ventilator control
3 Touch
the
CONTINUE.
CONTINUE
If you want to return to the
RESTART
button.
4 The system displays the
(You must touch the
button will display.)
Ventilator Startup
New Patient Settings
button first before
IBW
screen, touch the
screen with the
following buttons, and uses the rotary knob or drop-down
menus to display the available selections.
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 4-4
Page 99

How to use the 840 ventilator
OP 4
Vent Type
•
INVASIVE
Determines the ventilation type
:
— conventional ventilation using either
endotracheal (ET) or tracheostomy (trach) tubes
•
non-invasive
NIV (
ventilation using full-face masks,
) —
nasal masks, infant nasal prongs, or uncuffed ET tubes
(see Section 4.12 for specific information on how to use
NIV)
Determines the type and sequence of breath delivery
Mode
:
•
(Assist/Control)
A/C
•
•
•
(Synchronous Intermittent Mandatory Ventilation)
SIMV
SPONT
BILEVEL
(Spontaneous)
(available only with
BiLevel
software option
when Vent Type is INVASIVE)
Mandatory Type:
Determines the type of mandatory breath
control
•
(Pressure Control)
PC
•
(Volume Control)
VC
• VC+ (Volume Control Plus available only with
Ventilation Plus (VV+
) software option when
Volume
Vent Type
INVASIVE)
is
(If the selected
Mode
is
SPONT
, the
Mandatory Type
applies to
manual inspirations only.)
Determines type of support for
Spontaneous Type
:
spontaneous breaths
•
(Pressure Support)
PS
•
(Tube Compensation available only with
TC
software
TC
option when Vent Type is INVASIVE)
•
(Volume Support available only with
VS
VV+
software
option when Vent Type is INVASIVE)
•
(Proportional Assist available only with
PA
PAV+
software option when Vent Type is INVASIVE)
•
4-070088-00 Rev. F (10/06) 840 Ventilator System Operator’s Manual
NONE
OP 4-5
Page 100

OP 4
How to use the 840 ventilator
(If the selected
Mode
is
A/C,
the
Spontaneous Type
button
does not appear.)
Determines the method used to detect patient
Trigger Type
:
inspiratory effort
•
•V-
(Pressure) (not available when Vent Type is NIV or
-
P
TRIG
when using the
(Flow)
TRIG
NeoMode
option)
Touch the button and turn the knob to adjust the desired
settings. When you complete your settings changes, touch
CONTINUE
5The final
.
New Patient Settings
screen appears. Touch the button
of each parameter you want to change, then turn the knob to
select its value. To cancel this change, press the
cancel all changes and start over, touch the
CLEAR
RESTART
NOTE:
The ventilator control parameter you are setting may be
dependent upon other ventilator settings that determine its
boundaries. Refer to the prompt area on the lower GUI screen
(Figure 1-2) for more information.
6 Press
ACCEPT
to put all of your ventilation control settings
into effect. Normal ventilation begins once a patient is
connected.
7The
Apnea Setup
screen appears. Apnea settings are
automatically determined based on IBW, circuit type, and
mandatory breath type, but you can change them. If you
change any apnea settings, press
ACCEPT
to apply.
Although you are not required to change or confirm apnea
settings, you should verify that they are appropriate for the
patient prior to ventilation.
8 Press the
ALARM SETUP
limit settings on the
button to review the current alarm
Alarm Settings
screen. Ensure that they
are appropriate for the patient. To change any limit, touch the
button and turn the knob. To cancel, touch
ALARM
. To apply the settings, press the
PROPOSED
ACCEPT
key.
key. To
button.
840 Ventilator System Operator’s Manual 4-070088-00 Rev. F (10/06)
OP 4-6
 Loading...
Loading...