Page 1
M8000-9001F
1Table Of Contents
1 Basic Operation 1
Introducing the IntelliVue Family 1
IntelliVue MP20/MP20Junior/MP30 2
MP20/MP30 Major Parts and Keys 2
IntelliVue MP40/MP50 3
MP40/MP50 Major Parts and Keys 4
IntelliVue MP60/MP70 5
MP60/MP70 Major Parts and Keys 5
MP80/MP90 Major Parts and Keys 6
Remote Alarm Device 6
Docking Station 7
Related Products 7
Flexible Module Server (M8048A) 7
Measurement Modules 8
Multi-Measurement Server (M3001A) 9
Measurement Server Extensions 10
M3014A, M3015A and M3016A Capnography Extensions 10
M3012A Hemodynamic Measurement Server Extension 11
Operating and Navigating 12
Selecting Screen Elements 13
Using the Setup Menu 13
Using the Touchscreen 13
Disabling Touchscreen Operation 13
Using the SpeedPoint 14
Using the Navigation Point 15
Using a Mouse or Trackball 15
Using Keys 15
Permanent Keys 15
SmartKeys 16
Hardkeys 17
Pop-Up Keys 17
Using the On-Screen Keyboard 17
Using the On-Screen Calculator 18
Operating Modes 19
Standby Mode 19
Understanding Screens 20
Switching to a Different Screen 20
Changing a Screen’s Content 20
Using a Second Display 21
Using the Visitor Screen 21
Understanding Profiles 22
Swapping a Complete Profile 23
i
Page 2
Swapping a Settings Block 23
Default Profile 23
Locked Profiles 23
Understanding Settings 24
Changing Measurement Settings 24
Switching a Measurement On and Off 24
Switching Numerics On and Off 25
Adjusting a Measurement Wave 25
Changing Wave Speeds 25
Changing the Wave Group Speed 25
Changing Wave Speed for a Channel 25
Freezing Waves 26
Freezing An Individual Wave 26
Freezing All Waves 26
Measuring Frozen Waves 26
Changing The Wave Speed 26
Updating The Frozen Wave 26
Releasing Frozen Waves 27
Using Labels 27
About Label Sets 27
Changing Measurement Labels (e.g. Pressure) 27
Resolving Label Conflicts 28
Changing Monitor Settings 29
Adjusting the Screen Brightness 29
Adjusting Touch Tone Volume 29
Setting the Date and Time 29
Checking Your Monitor Revision 29
Getting Started 30
Inspecting the Monitor 30
Switching On 30
Setting up the Measurement Servers and Modules 30
Starting Monitoring 30
Disconnecting from Power 31
Monitoring After a Power Failure 31
Networked Monitoring 31
Using Remote Applications 31
Remote Application Popup Keys 32
2 What’s New? 33
What’s New in Release C.0? 33
What’s New in Release B.1? 34
What’s New in Release B.0? 35
What’s New in Release A.2? 37
3 Alarms 39
Visual Alarm Indicators 40
ii
Page 3
Audible Alarm Indicators 40
Alarm Tone Configuration 40
Traditional Audible Alarms (HP/Agilent/Philips/Carenet) 41
ISO/IEC Standard 9703-2 Audible Alarms 41
Changing the Alarm Tone Volume 41
Minimum Volume for No Central Monitoring INOP 41
Acknowledging Alarms 42
Acknowledging Disconnect INOPs 42
Alarm Reminder (ReAlarm) 42
Pausing or Switching Off Alarms 42
To Pause All Alarms 43
To Switch All Alarms Off 43
To Switch Individual Measurement Alarms On or Off 43
While Alarms are Paused or Off 43
Restarting Paused Alarms 44
Resetting Arrhythmia Alarm Timeouts 44
Extending the Alarm Pause Time 44
Alarm Limits 44
Viewing Individual Alarm Limits 44
Viewing All Alarm Limits 45
Changing Alarm Limits 46
About Automatic Alarm Limits (AutoLimits) 47
Documenting Alarm Limits 47
Reviewing Alarms 48
Alarm Messages Window 48
Review Alarms Window 48
Understanding Alarm Messages 49
Latching Alarms 49
Viewing the Alarm Latching Settings 49
Alarm Latching Behavior 50
Silencing Latched Alarms from an Information Center 50
Testing Alarms 50
Alarm Behavior at On/Off 50
4 Patient Alarms and INOPs 51
Patient Alarm Messages 51
Technical Alarm Messages (INOPs) 57
5 Managing Patients 75
Admitting a Patient 75
Patient Category and Paced Status 76
Admitting a Centrally-Monitored Patient 76
Quick Admitting a Patient 76
Editing Patient Information 77
Discharging a Patient 77
Transferring Patients 78
iii
Page 4
Transferring a Centrally-Monitored Patient 78
Transferring a Patient with an MMS (no Central Station) 79
Data Upload from an MMS 79
Data Exchange Between Information Centers 80
Resolving Patient Information Mismatch 80
Manually Resolving Patient Mismatch 80
Patient Mismatch - If One Set of Patient Data is Correct 81
Patient Mismatch - If Neither Patient Data Set is Correct 81
Patient Mismatch - If Both Patient Data Sets Are Correct 82
Automatically Resolving Patient Mismatch 82
Care Groups 82
Understanding the Care Group Overview Bar 83
Viewing the My Care Group Window 84
Viewing the Other Bed Window 85
Other Bed Pop-Up Keys 86
Visual Alarm Status Information in the Other Bed Window 86
Care Group Alarms 86
Telemetry Data Overview 87
Unpairing a Telemetry Device 87
Telemetry Data Overview Screen Element 87
Silencing Telemetry Alarms from the Bedside 88
Suspending Telemetry Alarms 88
Using Standby 88
6 ECG, Arrhythmia, and ST Monitoring 89
Skin Preparation for Electrode Placement 89
Connecting ECG Cables 89
Selecting the Primary and Secondary ECG Leads 90
Checking Paced Status 90
Understanding the ECG Display 91
Monitoring Paced Patients 91
Setting the Paced Status (Pace Pulse Rejection) 92
Avoiding Pace Pulse Repolarization Tails 92
Changing the Size of the ECG Wave 92
To Change the Size of an Individual ECG Wave 92
To Change the Size of all the ECG Waves 93
Changing the Volume of the QRS Tone 93
Changing the ECG Filter Settings 93
Choosing EASI or Standard Lead Placement 94
About ECG Leads 94
ECG Leads Monitored 94
Changing Lead Sets 94
ECG Lead Fallback 95
ECG Lead Placements 95
Standard 3-Lead Placement 96
Standard 5-Lead Placement 96
iv
Page 5

Chest Electrode Placement 97
10-Lead Placement 98
Conventional 12-Lead ECG 98
Modified 12-Lead ECG 99
Choosing Standard or Modified Electrode Placement 99
Labelling 12-Lead ECG Reports 99
Capture 12-Lead 100
EASI ECG Lead Placement 100
ECG, Arrhythmia, and ST Alarm Overview 102
Using ECG Alarms 103
Extreme Alarm Limits 103
ECG Alarms Off Disabled 103
HR Alarms When Arrhythmia Analysis is Switched Off 103
HR Alarms When Arrhythmia Analysis is Switched On 103
ECG Safety Information 103
About Arrhythmia Monitoring 105
Arrhythmia Options 105
Where Can I Find More Information? 105
Switching Arrhythmia Analysis On and Off 106
Choosing an ECG Lead for Arrhythmia Monitoring 106
Aberrantly-Conducted Beats 106
Atrial Fibrillation and Flutter 106
Intermittent Bundle Branch Block 107
Understanding the Arrhythmia Display 107
Viewing Arrhythmia Waves 107
Arrhythmia Beat Labels 107
Arrhythmia Status Messages 108
Rhythm Status Messages 108
Ectopic Status Messages 109
Arrhythmia Relearning 109
Initiating Arrhythmia Relearning Manually 109
Automatic Arrhythmia Relearn 110
Arrhythmia Relearn and Lead Fallback 110
Arrhythmia Alarms 110
Yellow Arrhythmia Alarms 111
Arrhythmia Alarms and Latching 111
Switching Individual Arrhythmia Alarms On and Off 111
Switching All Yellow Arrhythmia Alarms On or Off 111
Adjusting the Arrhythmia Alarm Limits 111
Arrhythmia Alarm Timeout Periods 111
What is a Timeout Period? 112
Resetting the Timeout Period 112
How are Yellow Arrhythmia Alarms Indicated? 112
Behavior of Unsilenced Arrhythmia Alarms 112
Behavior of Silenced Arrhythmia Alarms 112
Arrhythmia Alarm Chaining 113
v
Page 6
Understanding PVC-Related Alarms 114
About ST Monitoring 115
Switching ST On and Off 115
Selecting ST Leads for Analysis 115
Understanding the ST Display 116
Updating ST Baseline Snippets 117
Recording ST Segments 117
About the ST Measurement Points 118
Adjusting ST Measurement Points 118
ST Alarms 120
Single- or Multi-lead ST Alarming 120
Changing ST Alarm Limits 120
Viewing ST Maps 120
Current View 120
Tre n d V i ew 121
Viewing an ST Map 122
Working in the ST Map Task Window 122
Switching Between ST Map Views 122
Displaying an ST Reference Baseline 123
Updating an ST Map Reference Baseline 123
Changing the Scale of the ST Map 123
Changing the Trending Interval 123
Printing an ST Map Report 123
7 Monitoring Pulse Rate 125
Entering the Setup Pulse Menu 125
System Pulse Source 125
Switching Pulse On and Off 126
Using Pulse Alarms 126
Selecting the Active Alarm Source: HR or Pulse? 126
Alarm Source Selection Disabled 127
Changing HR/Pulse Alarm Limits 127
Extreme Alarm Limits 127
QRS Tone 127
8 Monitoring Respiration Rate (Resp) 129
Lead Placement for Monitoring Resp 129
Optimizing Lead Placement for Resp 129
Cardiac Overlay 129
Lateral Chest Expansion 130
Abdominal Breathing 130
Understanding the Resp Display 130
Changing Resp Detection Modes 130
Auto Detection Mode 130
Manual Detection Mode 131
Resp Detection Modes and Cardiac Overlay 131
vi
Page 7
Changing the Size of the Respiration Wave 131
Changing the Speed of the Respiration Wave 131
Using Resp Alarms 132
Changing the Apnea Alarm Delay 132
Resp Safety Information 132
9 Monitoring SpO
2
SpO2 Sensors 133
Applying the Sensor 133
Connecting SpO2 Cables 134
Measuring SpO
2
134
Assessing a Suspicious SpO2 Reading 135
Understanding SpO2 Alarms 136
Adjusting the Alarm Limits 136
Adjusting the Desat Limit Alarm 136
Pleth Wave 136
Perfusion (Pleth) Indicator 137
Setting SpO2/Pleth as Pulse Source 137
Setting Up Tone Modulation 137
Setting the QRS Volume 137
Calculating SpO2 Difference 137
10 Monitoring NBP 139
Introducing the Oscillometric NBP Measurement 139
Measurement Limitations 140
Measurement Methods 140
Reference Method 140
Preparing to Measure NBP 140
Correcting the Measurement if Limb is not at Heart Level 141
Understanding the NBP Numerics 141
Starting and Stopping Measurements 142
Enabling Automatic Mode and Setting Repetition Time 142
Choosing the NBP Alarm Source 143
Assisting Venous Puncture 143
Calibrating NBP 143
133
11 Monitoring Temperature 145
Making a Temp Measurement 145
Selecting a Temperature for Monitoring 145
Extended Temperature Label Set 146
Calculating Temp Difference 146
12 Monitoring Invasive Pressure 147
Setting up the Pressure Measurement 147
Selecting a Pressure for Monitoring 148
Extended Pressure Label Set 148
vii
Page 8
Zeroing the Pressure Transducer 148
Zeroing ICP (or IC1/IC2) 149
Determining a Pressure’s Most Recent Zero 149
Zeroing a Pressure Measurement 149
Using the Zero Hardkey 149
Zeroing All Pressures Simultaneously 150
Troubleshooting the Zero 150
Adjusting the Calibration Factor 150
Displaying a Mean Pressure Value Only 150
Changing the Pressure Wave Scale 151
Optimizing the Waveform 151
Non-Physiological Artifact Suppression 151
Choosing the Pressure Alarm Source 151
Calibrating Reusable Transducer CPJ840J6 152
Making the Pressure Calibration 152
Troubleshooting the Pressure Calibration 153
Calculating Cerebral Perfusion 153
Calculating Pulse Pressure Variation 153
Measuring Pulmonary Artery Wedge Pressure 154
Editing the Wedge 155
Identifying the Pressure Analog Output Connector 155
13 Monitoring Cardiac Output 157
Hemodynamic Parameters 158
Using the C.O. Procedure Window 159
Accessing the Setup C.O. and Setup CCO Menus 160
Entering the HemoCalc Window 160
Measuring C. O. Using the PiCCO Method 160
Measuring Continuous Cardiac Output 160
Measuring Systemic Vascular Resistance 160
Setting Up the PiCCO C.O. Measurement 161
Performing PiCCO C.O. Measurements 162
Editing PiCCO C.O. Measurements 162
Saving and Calibrating PiCCO C.O. Measurements 163
CCO Calibration Status Indicators 163
Measuring C.O. Using the Right Heart Thermodilution Method 164
Setting up RH C.O. Measurements 164
Ice-Bath Setup for RH Thermodilution C.O. Measurements 164
Setting the Computation Constant 165
Performing RH C.O. Measurements 165
Editing and Saving RH C.O. Measurements 165
Documenting C.O. Measurements 165
C.O. Injectate Guidelines 166
Guidelines for Right Heart Thermodilution C.O. Injectate 166
Guidelines for PiCCO C.O. Injectate 166
Injectate Volume, Patient Weight and ETVI Values (PiCCO Only) 166
viii
Page 9
C.O./CCO Curve Alert Messages 167
C.O./CCO Prompt Messages 168
C.O./CCO Warning Messages 169
C.O./CCO Safety Information 169
14 Monitoring Carbon Dioxide 171
Using the Capnography Extension (M3014A) 172
Preparing to Measure Mainstream CO
Attaching and Removing the CO2 Sensor 172
Zeroing the CO2 Sensor 173
2
Using the Mainstream CO2 Extension (M3016A) 174
Preparing to Measure Mainstream CO
Checking Transducer Accuracy 174
Calibrating the Transducer 175
Attaching and Removing the CO2 Tra n s d u c e r 175
2
Using the Microstream CO2 Extension (M3015A) 176
Preparing to Measure Microstream CO2 176
Setting up Microstream CO2 Measurements 176
Using Microstream Accessories 176
Using the FilterLine and Airway Adapter 177
Removing Exhaust Gases from the System 177
Suppressing Zero Calibration 177
Suppressing Sampling 178
Setting up Mainstream and Microstream 178
Adjusting the CO2 Wave S c ale 178
Setting up CO2 Corrections 178
Changing CO2 Alarms 179
Changing the Apnea Alarm Delay 179
Deriving Alarms From awRR 180
Changing awRR Alarm Limits 180
172
174
15 Monitoring tcGas 181
Identifying tcGas Module Components 181
Setting the tcGas Sensor Temperature 182
Using the tcGas Site Timer 182
Setting the tcGas Site Timer 182
Restarting the tcGas SiteTimer 183
Disabling the tcGas Site Timer 183
Setting the tcGas Barometric Pressure 183
Remembraning the tcGas Transducer 183
New/Dried Out Transducers 184
Storing tcGas Transducers 184
Calibrating the tcGas Transducer 185
Calibration Failure 186
Troubleshooting tcGas Calibration 186
Applying the tcGas Transducer 187
ix
Page 10
Selecting the tcGas HeatPowerDisplay Mode 188
Zeroing the tcGas Relative Heat Power 188
Finishing tcGas Monitoring 188
TcGas Corrections 188
Temperature Correction for tcpCO
Metabolism Correction for tcpCO
2
2
188
188
16 Monitoring SvO
Preparing to Monitor SvO
2
2
190
Carrying out a Pre-insertion Calibration 190
Inserting the Catheter 191
Performing a Light Intensity Calibration 191
Performing In-Vivo Calibration 192
Setting Up the In-Vivo Calibration 192
Making the In-Vivo Calibration 192
Calculating Oxygen Extraction 192
17 Monitoring EEG 193
EEG Monitoring Setup 194
Using the EEG Impedance/Montage Window 194
Choosing an EEG Electrode Montage 195
Changing the Impedance Limit 195
About Electrode-to-Skin Impedance 196
Impedance Indicators 196
About Compressed Spectral Arrays (CSA) 197
Displaying CSAs 198
Changing EEG Settings 198
Switching EEG Numerics On and Off 198
Changing the Scale of the EEG Waves for Display 198
Changing Filter Frequencies 199
Changing the Speed of the EEG Wave 199
EEG Reports 199
EEG Safety Information 200
EEG and Electrical Interference 200
189
18 Monitoring BIS 201
BIS Monitoring Setup 202
Monitoring BIS Using the DSC and BIS Engine 202
Monitoring BIS using the BISx 203
Manufacturer’s Information 204
BIS Continuous Impedance Check 204
BIS Cyclic Impedance Check 204
Starting a Cyclic Impedance Check 204
Stopping a Cyclic Impedance Check 204
BIS Window 205
BIS Impedance Indicators 205
x
Page 11
Changing the BIS Smoothing Rate 206
Switching BIS and Individual Numerics On and Off 206
Changing the Scale of the EEG Wave 206
Switching BIS Filters On or Off 206
BIS Safety Information 207
19 Trends 209
Viewing Trends 209
Viewing Graphic Trends 210
Viewing Vital Signs Trends 210
Tre n ds Po p - U p K e y s 211
Setting Up Trends 211
Making Segment Settings 212
Expanded View 212
Trend Scales for Segment Measurements 212
Optimum Scale 212
Tr e n d Gr o u p 2 1 2
No. of Segments 212
Tre n d Gr o u p s 213
Tre n d I n te r v a l 213
Tre n d Pr i o r i t y 213
Trend Parameter Scales 213
Graphical Trend Presentation 214
Documenting Trends 214
Trends Databases 215
Aperiodic Trends Database 215
Trending Multiple-Value Measurements 215
Screen Trends 215
Setting the Screen Trend Time 216
Changing the Selection of Screen Trends Displayed 217
Activating the Cursor for Screen Trends 217
Changing the Screen Trend View 217
Tabular View 217
Horizon View 218
Setting the Horizon 218
Setting the Horizon Trend Scale 218
20 Calculations 219
Viewing Calculations 219
Calculations Windows 220
Calculations Pop-Up Keys 220
Reviewing Calculations 221
Performing Calculations 221
Entering Values for Calculations 222
Automatic Value Substitution 222
Automatic Unit Conversion 222
xi
Page 12
Manual Unit Conversion 222
BSA Formula 222
Documenting Calculations 223
21 High Resolution Trend Waves 225
Changing the Hi-Res Trend Waves Displayed 225
Hi-Res Trend Wave Scales 225
Hi-Res Trend Waves and OxyCRG 225
Printing Hi-Res Trend Wave Reports 226
Hi-Res Trend Wave Recordings 226
22 Event Surveillance 227
Levels of Event Surveillance 227
Event Groups 228
Event Episodes 228
Events Pop-Up Keys 229
Event Triggers 230
Event Retriggering 231
Event Notification 231
Setting Triggers for NER and Basic Event Surveillance 231
Setting Triggers and Notification for Advanced Event Surveillance 232
Triggering Events Manually 233
The Events Database 233
Viewing Events 233
Event Counter 233
Counting Combi-Events 234
Counting Neonatal Event Review (NER) Events 234
Event Summary Window 235
Event Review Window 235
Event Episode Window 236
Annotating Events 237
Documenting Events 237
Documenting Event Review 237
Documenting an Event Episode 238
Event Recordings 238
Event Review Recordings 238
Event Episode Recordings 239
Event Reports 239
Event Review Reports 240
Event Episode Reports 241
Event Summary Reports 241
23 Using Timers 243
Viewing Timers 243
Notification 243
Timer Types 244
xii
Page 13
Timer Setup Pop-up Keys 244
Setting Up Timers 244
Timer Label 244
Run Time 245
Timer Counting Direction 245
Displaying Timers On The Main Screen 245
Main Screen Timer Pop-up Keys 246
Displaying A Clock On The Main Screen 246
24 Recording 247
Starting and Stopping Recordings 248
Quickstarting Recordings 248
Extending Recordings 249
Stopping Recordings 249
Recording Without a Template 249
Overview of Recording Types 249
All ECG Waves Recordings 250
Creating and Changing Recordings Templates 250
Changing ECG Wave Gain 251
Recording Priorities 252
Sample Recording Strip 252
Recording Strip Code 252
Recorded Waveforms 253
Maintaining Recording Strips 253
Reloading Paper 254
Recorder Status Messages 255
25 Printing Patient Reports 257
Starting Reports Printouts 257
Stopping Reports Printouts 258
Setting Up Reports 258
Setting Up ECG Reports 258
Setting Up Vital Signs and Graphic Trend Reports 259
Setting Up Auto Reports 259
Setting Up Individual Print Jobs 260
Checking Printer Settings 260
Switching Printers On Or Off for Reports 261
Dashed Lines on Reports 261
Unavailable Printer: Re-routing Reports 261
Printer Status Messages 262
Sample Report Printouts 262
Alarm Limits Report 263
Realtime Report 264
Cardiac Output Report 265
ECG Reports 266
Other Reports 266
xiii
Page 14
26 Using the Drug Calculator 267
Accessing the Drug Calculator 267
Performing Drug Calculations 268
About the Rule of Six 268
Performing Calculations for a Non-Specific Drug 268
Performing Calculations for a Specific Drug 269
Charting Infusion Progress 270
Using the Titration Table 270
Documenting Drug Calculations 270
27 VueLink Modules 271
Connecting an External Device 272
Changing VueLink Waves and Numerics Displayed 272
Viewing the VueLink Device Data Window 272
Using VueLink Screens 273
Switching VueLink On and Off 273
Alarms/INOPs From External Devices 273
Language Conflict with External Device Drivers 274
28 Respiratory Loops 275
Viewing Loops 275
Capturing and Deleting Loops 276
Showing/Hiding Loops 276
Changing Loops Display Size 277
Using the Loops Cursor 277
Changing Loops Type 277
Source Device 277
Documenting Loops 278
29 Care and Cleaning 279
General Points 279
Cleaning 280
Disinfecting 280
Cleaning Monitoring Accessories 280
Sterilizing 281
Cleaning the Recorder Printhead (M1116B only) 281
Cleaning the Batteries and Battery Compartment 281
30 Using the Batteries 283
Battery Power Indicators 284
Battery LED 284
Battery Status on the Main Screen 284
Battery Status Window 286
Viewing Individual Battery Status 286
Recording Battery Status 286
xiv
Page 15
Printing Battery Reports 286
Checking Battery Charge 286
Replacing Batteries 287
Optimizing Battery Performance 287
Display Brightness Setting 288
Charging Batteries 288
Conditioning Batteries 288
Unequally-Charged Batteries 288
Battery Safety Information 289
31 Maintenance and Troubleshooting 291
Inspecting the Equipment and Accessories 291
Inspecting the Cables and Cords 291
Maintenance Task and Test Schedule 292
Troubleshooting 293
Disposing of the Monitor 293
Disposing of Empty Calibration Gas Cylinders 293
32 Accessories 295
ECG/Resp Accessories 295
Tr u nk C a b l e s 295
3-Electrode Cable Sets 295
5-Electrode Cable Sets 296
10-Electrode Cable Sets 296
3-Electrode One Piece Cables 296
5-Electrode One Piece Cables 296
Set Combiners and Organizers 297
NBP Accessories 297
Adult/Pediatric Multi-Patient Comfort Cuffs and Disposable Cuffs 297
Reusable Cuff Kits 297
Adult/Pediatric Antimicrobial Coated Reusable cuffs 298
Adult/Pediatric Soft Single Patient Single-Hose Disposable Cuffs 298
Neonatal/Infant Cuffs (Disposable, non-sterile) 298
Invasive Pressure Accessories 299
SpO2 Accessories 299
Temperature Accessories 303
Cardiac Output (C.O.) Accessories 304
Mainstream CO2 Accessories (for M3014A) 304
Mainstream CO2 Accessories (for M3016A) 305
Microstream CO2 Accessories 306
tcGas Accessories 306
EEG Accessories 307
BIS Accessories 307
BIS Sensors 307
Other BIS Accessories 308
SvO2 Accessories 308
xv
Page 16

Recorder Accessories 309
33 Installation and Specifications 311
Intended Use 311
Indication for Use 311
Manufacturer’s Information 312
BIS Manufacturer’s Information 312
Responsibility of the Manufacturer 312
Trademark Acknowledgement 313
Symbols 314
Installation Safety Information 315
Connectors 315
MP20/MP30 316
MP40/MP50 317
MP60/MP70 318
MP80/MP90 320
Altitude Setting 321
Monitor Safety Specifications 321
Physical Specifications 322
Environmental Specifications 323
M4605A Battery Specifications 326
Monitor Performance Specifications 326
Measurement Specifications 332
ECG/Arrhythmia/ST 332
Respiration 334
SpO
2
NBP 336
Invasive Pressure and Pulse 337
Te m p 339
CO
2
Cardiac Output / Continuous Cardiac Output 341
tcGas 342
SvO
2
EEG 343
BIS 344
Safety and Performance Tests 345
Electromagnetic Compatibility (EMC) Specifications 345
Accessories Compliant with EMC Standards 345
Electromagnetic Emissions 345
Avoiding Electromagnetic Interference (Resp and BIS) 345
Electromagnetic Immunity 346
Recommended Separation Distance 346
Recommended separation distances from portable and mobile RF communication equipment347
Electrosurgery Interference/Defibrillation/Electrostatic Discharge 348
Fast Transients/Bursts 348
Restart time 348
334
339
343
xvi
Page 17
34 Default Settings Appendix 349
Alarm Default Settings 350
ECG, Arrhythmia, and ST Default Settings 350
Pulse Default Settings 353
Respiration Default Settings 354
SpO2 Default Settings 354
NBP Default Settings 355
Temperature Default Settings 355
Invasive Pressure Default Settings 356
Cardiac Output Default Settings 357
CO2 Default Settings 358
tcGas Default Settings 358
SvO2 Default Settings 359
EEG Default Settings 359
BIS Default Settings 359
VueLink Default Settings 360
xvii
Page 18

xviii
Page 19

1
1Basic Operation
These Instructions for Use are for clinical professionals using the IntelliVue MP20/MP30 (M8001A/
M8002A), MP40/50 (M8003A/M8004A) and MP60/70/80/90 (M8005A/M8007A/M8008A/
M8010A) patient monitors.Unless otherwise specified, the information here is valid for all the above
IntelliVue patient monitors.
The basic operation section gives you an overview of the monitor and its functions. It tells you how to
perform tasks that are common to all measurements (such as entering data, switching a measurement
on and off, setting up and adjusting wave speeds, working with profiles). The alarms section gives an
overview of alarms. The remaining sections tell you how to perform individual measurements, and how
to care for and maintain the equipment.
Familiarize yourself with all instructions including warnings and cautions before starting to monitor
patients. Read and keep the Instructions for Use that come with any accessories, as these contain
important information about care and cleaning that is not repeated in this book.
This guide describes all features and options. Your monitor may not have all of them; they are not all
available in all geographies. Your monitor is highly configurable. What you see on the screen, how the
menus appear and so forth, depends on the way it has been tailored for your hospital and may not be
exactly as shown here.
In this guide:
•A warning alerts you to a potential serious outcome, adverse event or safety hazard. Failure to
observe a warning may result in death or serious injury to the user or patient.
•A caution alerts you to where special care is necessary for the safe and effective use of the product.
Failure to observe a caution may result in minor or moderate personal injury or damage to the
product or other property, and possibly in a remote risk of more serious injury.
• Monitor refers to the entire patient monitor. Display refers to the physical display unit. Display
Screen and Screen refer to everything you see on monitor’s display, such as measurements, alarms,
patient data and so forth.
Introducing the IntelliVue Family
The Philips IntelliVue family of patient monitors offers a monitoring solution optimized for the
surgical, cardiac, medical and neonatal care environments. Combining patient surveillance and data
management, it allows multi-measurement monitoring by linking separate modules with “plug-andplay” convenience.
1
Page 20
1 Basic Operation Introducing the IntelliVue Family
1
4
5
6
7
3
Your monitor stores data in trend, event, and calculation databases. You can see tabular trends (vital
signs) and document them on a local or remote printer. You can view measurement trend graphs, with
up to three measurements combined in each graph, to help you identify changes in the patient’s
physiological condition. You can view fast-changing measurement trends with beat to beat resolution
and see up to four high resolution trend segments. Event surveillance enhances documentation and
review of physiologically significant events by automatically detecting and storing up to 50 userdefined clinical events over a 24 hour period.
There is a choice of monitor configurations, as explained below. All models can also use computer
devices such as a mouse, a trackball and a keyboard.
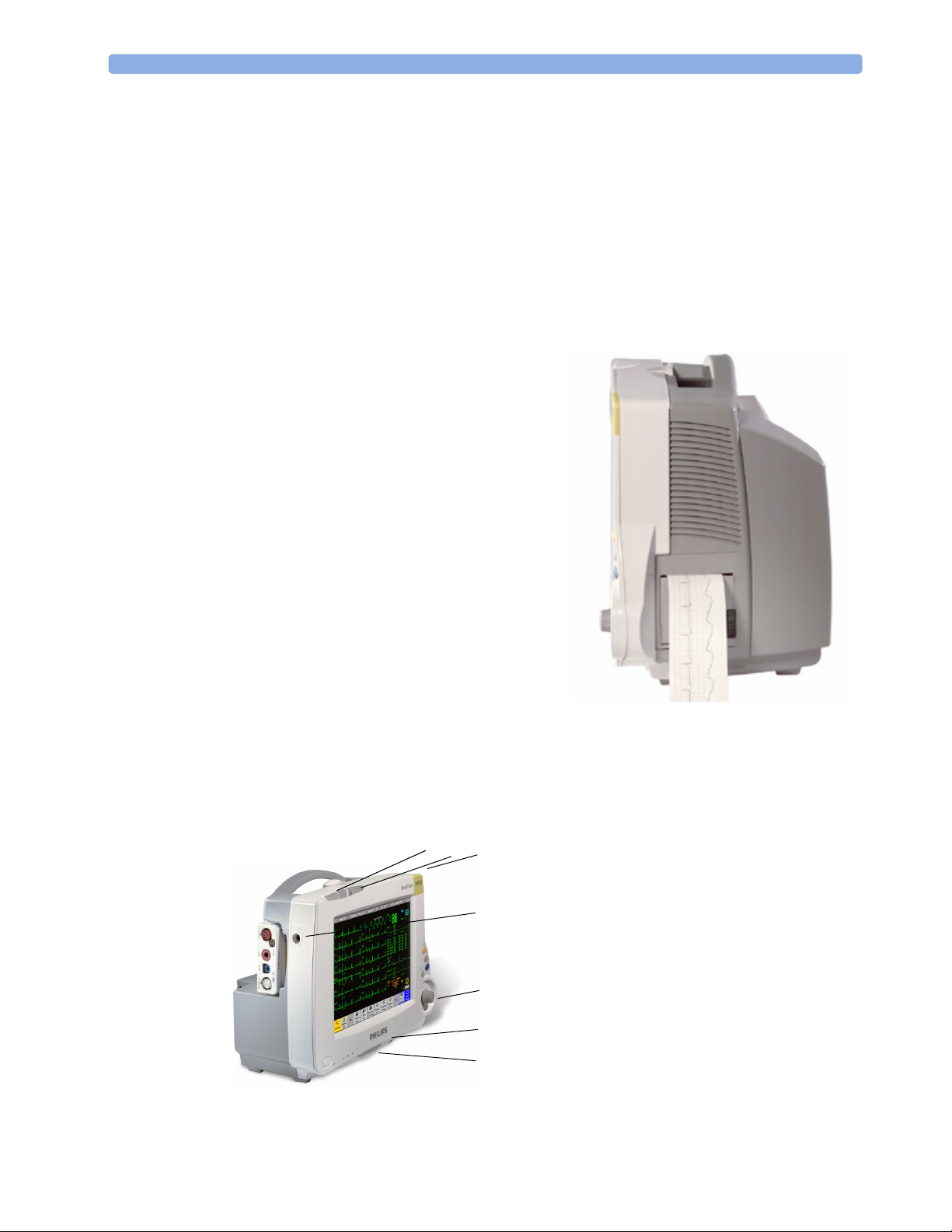
IntelliVue MP20/MP20
The IntelliVue MP20/MP20Junior/MP30 (M8001A/
M8002A) patient monitor has a 10-inch TFT LCD
flat panel SVGA display. The standard input devices
for the MP30 are the Touchscreen and integrated
navigation point; the MP20 is supplied with an
integrated navigation point only. Up to six waves can
be shown on MP20/MP30 Screens (USA - up to four
waves, MP20Junior - up to 3 waves). 12 ECG traces
can be shown on the 12-Lead ECG Screen.
The MP20/MP30 can be connected to one MultiMeasurement Server (MMS) and any one of the
measurement server extensions. There is an optional
built-in recorder. The Flexible Module Server
(M8048A) and all plug-in modules cannot be used
with the MP20/MP30. With an optional Interface
board Bispectral Index (BIS) monitoring is possible.
MP20Junior is an option of MP20 (M8001A) and is
not referred to separately in these Instructions for Use.
Junior
/MP30
MP20/MP30 Major Parts and Keys
MP20/MP30 left side
12
2
3
4
5
6
7
1 Color-coded alarm lamps
2 Alarms off lamp
3 Model indicator
4 ECG out
5 Navigation Point
6 Part number and serial number
7 Mounting quick-release lever
2
Page 21
Introducing the IntelliVue Family 1 Basic Operation
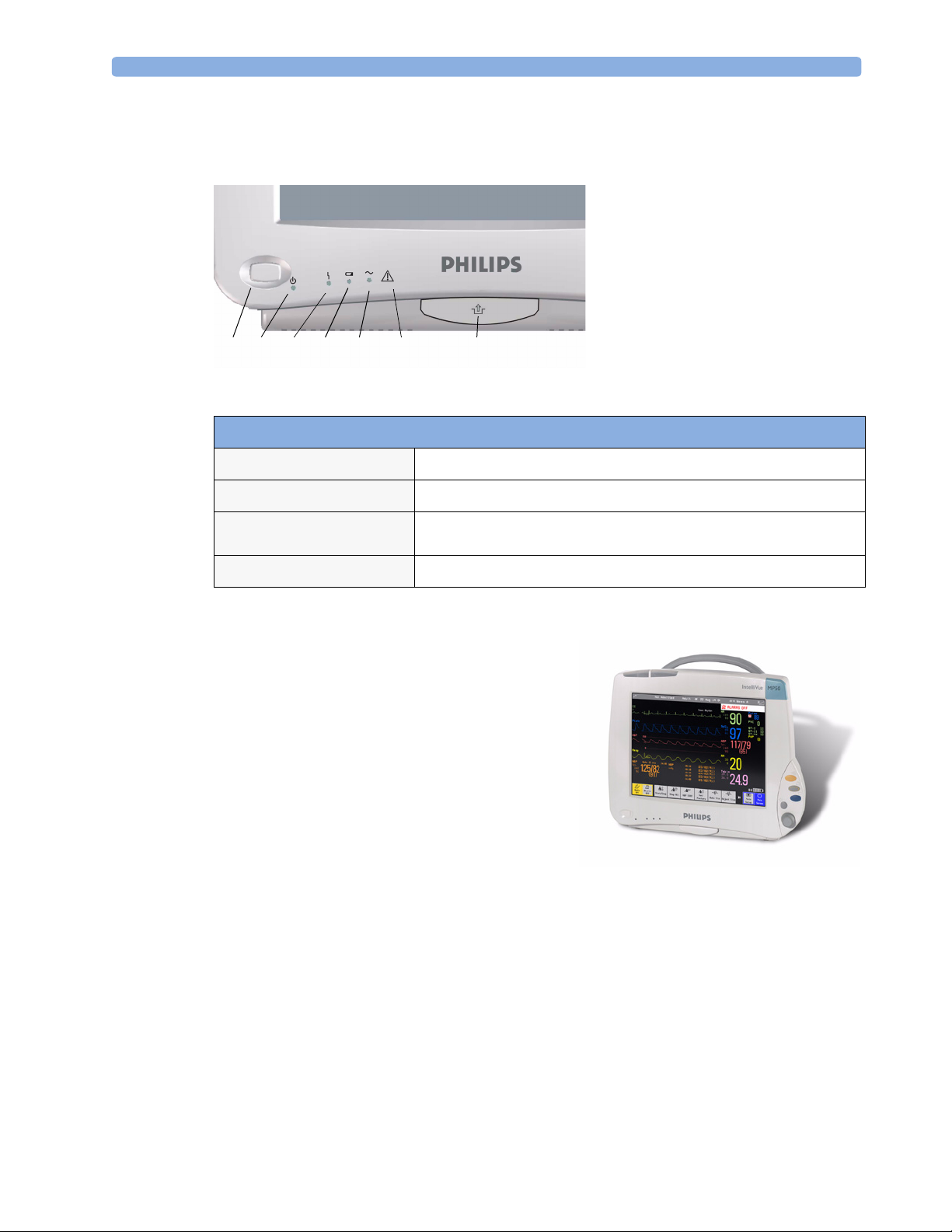
MP20/MP30 front panel
1
On/Standby switch
2
On/Standby LED
3
Error LED
4
Battery status LED
5
AC power operation LED
6 “read the documentation”
symbol
7
Mounting quick-release lever
123 4 5 67
MP20/MP30 LED Colors and their Meanings
On/Standby LED
Error LED
Battery LED
AC Power LED
IntelliVue MP40/MP50
The IntelliVue MP40/MP50 (M8003A/M8004A)
patient monitor has a 12-inch TFT LCD flat panel
SVGA display. The standard input devices for the MP50
are the Touchscreen and integrated navigation point; the
MP40 is supplied with an integrated navigation point
only. Up to six waves can be shown on MP40/MP50
Screens, 12 ECG traces can be shown on the 12-Lead
ECG Screen.
The MP40/MP50 can be connected to one MultiMeasurement Server (MMS) and any one of the
measurement server extensions. The IntelliVue family
plug-in measurement modules can be connected to its
four integrated plug-in module slots with plug-and-play convenience (the only exception is the SvO
module, M1021A, which cannot be used with the MP40/MP50). The Flexible Module Server
(M8048A) cannot be used with the MP40/MP50.
Green when monitor is switched on
Red if there is a problem with the monitor
Green, yellow, and red.
See the section on Using the Batteries for details
Green while the monitor is connected to AC power (mains)
2
3
Page 22
1 Basic Operation Introducing the IntelliVue Family
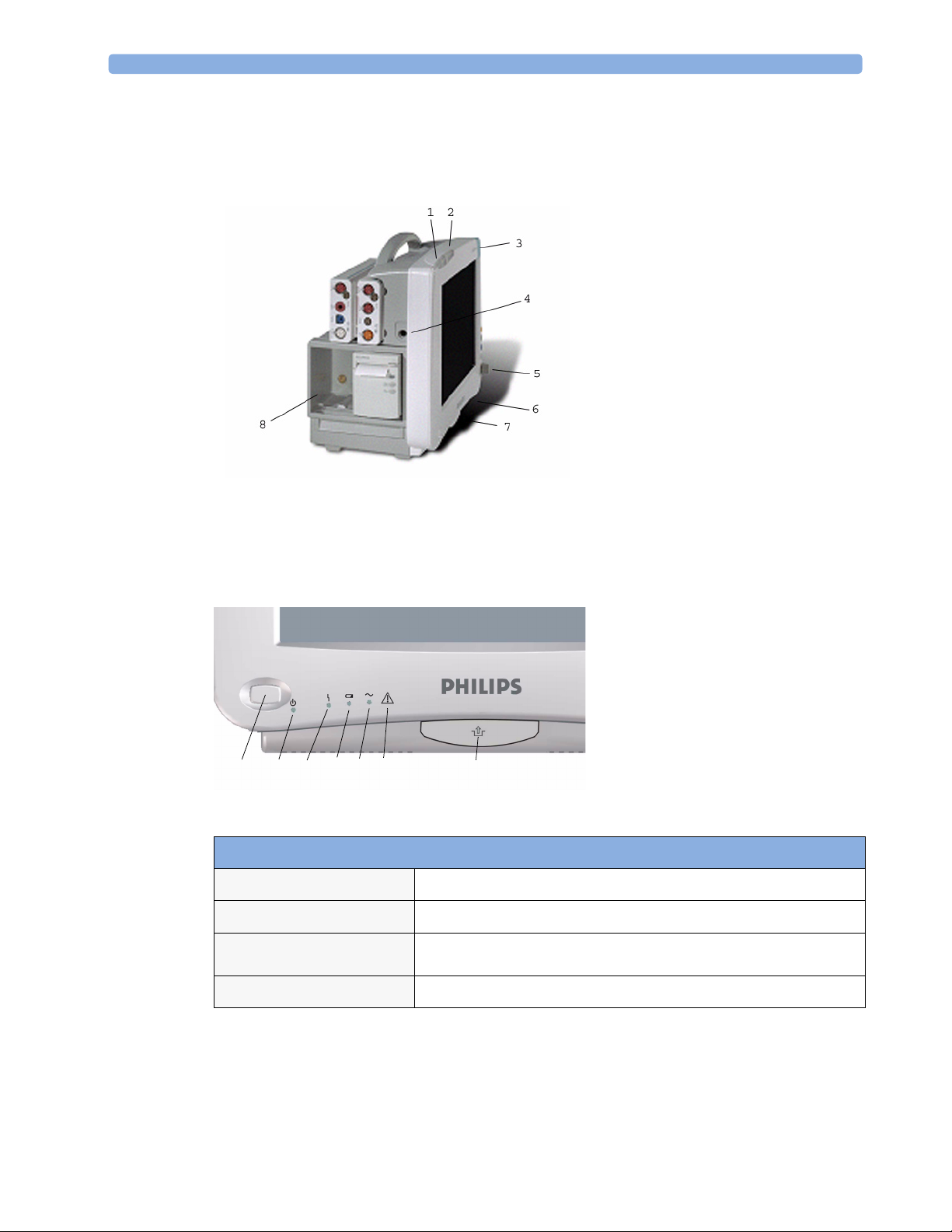
MP40/MP50 Major Parts and Keys
MP40/MP50 left side
1 Color-coded alarm lamps
2 Alarms off lamp
3 Model indicator
4 ECG out
5 Navigation Point
6 Part number and serial number
7 Mounting quick-release lever
8 Plug-in module slots
MP40/MP50 front panel
1
456 7
32
MP40/MP50 LED Colors and their Meanings
On/Standby LED
Error LED
Battery LED
AC Power LED
Green when monitor is switched on
Red if there is a problem with the monitor
Green, yellow, and red.
See the section on Using the Batteries for details
Green while the monitor is connected to AC power (mains)
1
On/Standby switch
2
On/Standby LED
3
Error LED
4
Battery status LED
5
AC power operation LED
6 “read the documentation”
symbol
7
Mounting quick-release lever
4
Page 23

Introducing the IntelliVue Family 1 Basic Operation
IntelliVue MP60/MP70
The IntelliVue MP60/MP70 (M8005A/M8007A) patient monitors integrate the display unit, with a
15” color LCD display, and the data processing unit into one. Up to eight waves can be shown on the
screens, as well as the 12-Lead ECG Screen. The MP60 uses the SpeedPoint as its primary input device
while the MP70 uses touch screen operation but may have an optional SpeedPoint.
The monitors can be connected to the Multi-Measurement Server (MMS) and any one of the
measurement server extensions, and to the Flexible Module Server (M8048A). The IntelliVue family
plug-in measurement modules can be connected to its FMS module slots with plug-and-play
convenience.
The MP60/MP70 has two integrated slots for plug-in modules. You can combine one each of the
following modules in these slots: Pressure, Temperature, C.O., SpO
the two-slot recorder module in the integrated slots.
and VueLink. You can also use
2
MP60/MP70 Major Parts and Keys
1 Color coded alarm lamps
1
2
891011 7
3
6
4
5
2 Alarms Off lamp
3Display
4Model indicator
5 SpeedPoint (optional for MP70)
6 Part number and serial number
7 Mounting quick-release lever
8AC power LED
9Error LED
10 Power on/standby switch
11 Power on LED
5
Page 24

1 Basic Operation Introducing the IntelliVue Family
MP80/MP90 Major Parts and Keys
In the MP80 and MP90, the display and the processing unit are separate components. They offer both
touchscreen and the Remote SpeedPoint as standard input devices.
AC Power LED
Power on LED
Display Unit
Remote Alarm Device
The Remote Alarm Device provides audio and visual indicators of alarms, in addition to those shown
on the display.
1
5
Error LED
Processing Unit
2
1 Two color coded alarm lamps (right-hand lamp flashes
red or yellow for patient alarms, left-hand lamp flashes
light blue for INOPs)
2 Alarms off lamp - when illuminated it indicates that all
alarms are deactivated.
3
4
3 Speaker - for alarm prompts, QRS tones and so forth
4 Monitor power on /standby switch. Press to switch
monitor on remotely. Press and hold for one second to
turn monitor off.
5 Power on LED - green when monitor is on
Power on Switch
6
Page 25

Related Products 1 Basic Operation
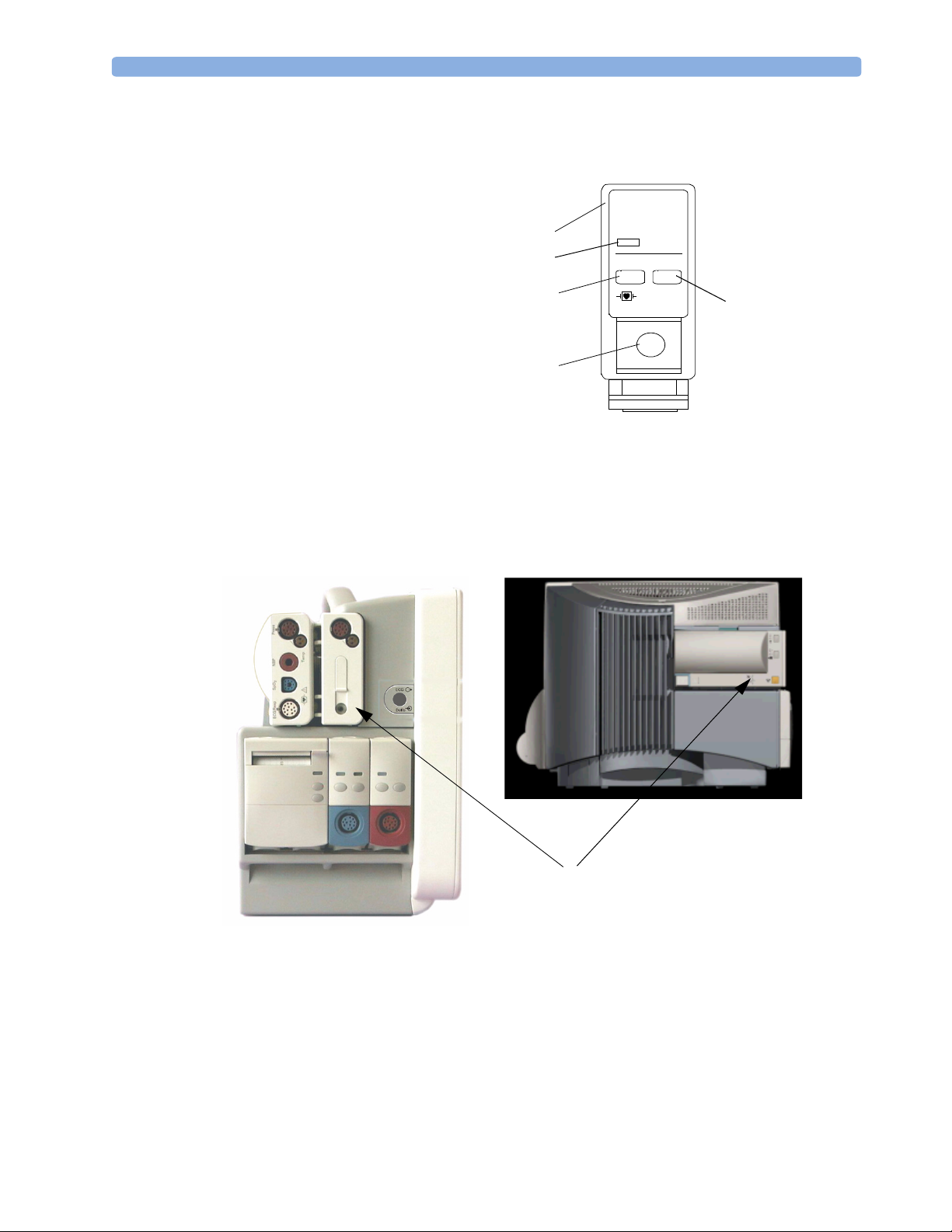
Docking Station
MP20/30/
40/50 only
The docking station provides quick mounting and connections in a one-step operation. By placing the
monitor on the docking station and closing the lever you can make the connection to power and to a
wired network, if present.
Data Connector
Open Position
Power On LED
Related Products
Power Connector
Locked Position
Related products extend the measurement capabilities of your monitor. None of the related devices
have their own power on/standby switches. They take their power from the monitor, and switch on
automatically when you turn on the monitor. A green power-on LED indicates when they are drawing
power from the monitor. A permanently illuminated, or flashing, red LED indicates a problem with
the unit that requires the attention of qualified service personnel.
Flexible Module Server (M8048A)
MP60/70/80
/90 only
The flexible module server (FMS) lets you use up to eight plug-in physiological measurement modules.
With the MP60/70/80 you can connect only one FMS. With the MP90 (M8010A) you can connect
two FMSs to use up to 10 measurement modules. For individual modules, the maximum that can be
used simultaneously in an FMS is: five pressure modules, four temperature modules, four VueLink
modules.
Connect the FMS to the monitor via the measurement server link cable (MSL). Use the MSL
connector on the left-hand side to connect additional measurement servers. Use the connector on the
right to connect to the monitor.
7
Page 26

1 Basic Operation Related Products
1
1
2
3
Multi-Measurement
Server
2
Measurement server
mount
3
Flexible Module Server
4 Power on LED
5
Interruption indicator
5
4
Measurement Modules
You can use up to eight measurement modules with the Flexible Module Server (M8048A), two
additional modules in the integrated module slots in the MP60/MP70, and up to four in the integrated
slots in the MP40/MP50. Available modules are:
• Invasive blood pressure (M1006B)
• Temperature (M1029A)
• Oxygen saturation of arterial blood (SpO
) (M1020B)
2
• Cardiac output (M1012A), and Continuous cardiac output with M1012A Option #C10
• Transcutaneous gas (M1018A)
• Mixed venous oxygen saturation - SvO
(M1021A) MP60/70/80/90 monitor only
2
• Recorder (M1116B)
• VueLink device interface (M1032A)
• EEG (M1027A)
• Bispectral Index - BIS (M1034A)
You can plug and unplug modules during monitoring. Insert the module until the lever on the module
clicks into place. Remove a module by pressing the lever upwards and pulling the module out.
Reconnecting a module to the same monitor restores its label and measurement settings, such as alarms
limits. If you connect it to a different monitor, the module remembers only its label.
The connector socket on the front of each module is the same color as the corresponding connector
plug on the transducer or patient cable.
Press the Setup key on the module’s front to display the measurement’s setup menu on the monitor
screen. When the setup menu is open, a light appears above the key. Some modules have a second key.
On the pressure module, for example, it initiates a zeroing procedure.
8
Page 27
Related Products 1 Basic Operation
Example Module (Pressure)
1Module name
2Setup key LED
3 Setup key to enter setup menu of
measurement modules or VueLink
device data window
4 Connector socket for patient cable/
transducer
5 Second module-specific key, for
example Zero
Multi-Measurement Server (M3001A)
The Multi-Measurement Server (MMS) can simultaneously monitor 3-, 5- or 10-lead ECG (including
arrhythmia and ST monitoring), respiration, SpO
Depending on the monitor model, you can connect it to the monitor via a cable or mount it either on
the left side of the FMS or on the back of the monitor, as shown here.
PRESS
1
2
3
80x80
Press
5
4
, NBP and either invasive pressure or temperature.
2
MMS mounted on rear of MP40/MP50
(left) and MP60/MP70
9
Page 28

1 Basic Operation Related Products
M3001A Connectors and Symbols
1 White ECG/Resp connector
2 Blue SpO
5
3 Red NBP connector
4 & 5Combined pressure (red) and temperature
(brown) connector - connect either invasive
4
3
pressure transducer or temperature probe.
You might have a version of the MMS that
does not have this connector.
connector
2
2
1
6
NBP Start/Stop key -
6
7
starts or stops NBP
measurements
7
NBP STAT key - starts NBP
STAT series of
measurements
9
8
8
9
Measurement Server Extensions
The measurement server extensions connect to the MMS and use the MMS settings and power. Trend
data and measurement settings from the measurements in the extensions are stored in the measurement
server.
The measurement server extensions are not intended to be disconnected from the MMS. To exchange
an extension, you should exchange the measurement server and extension together.
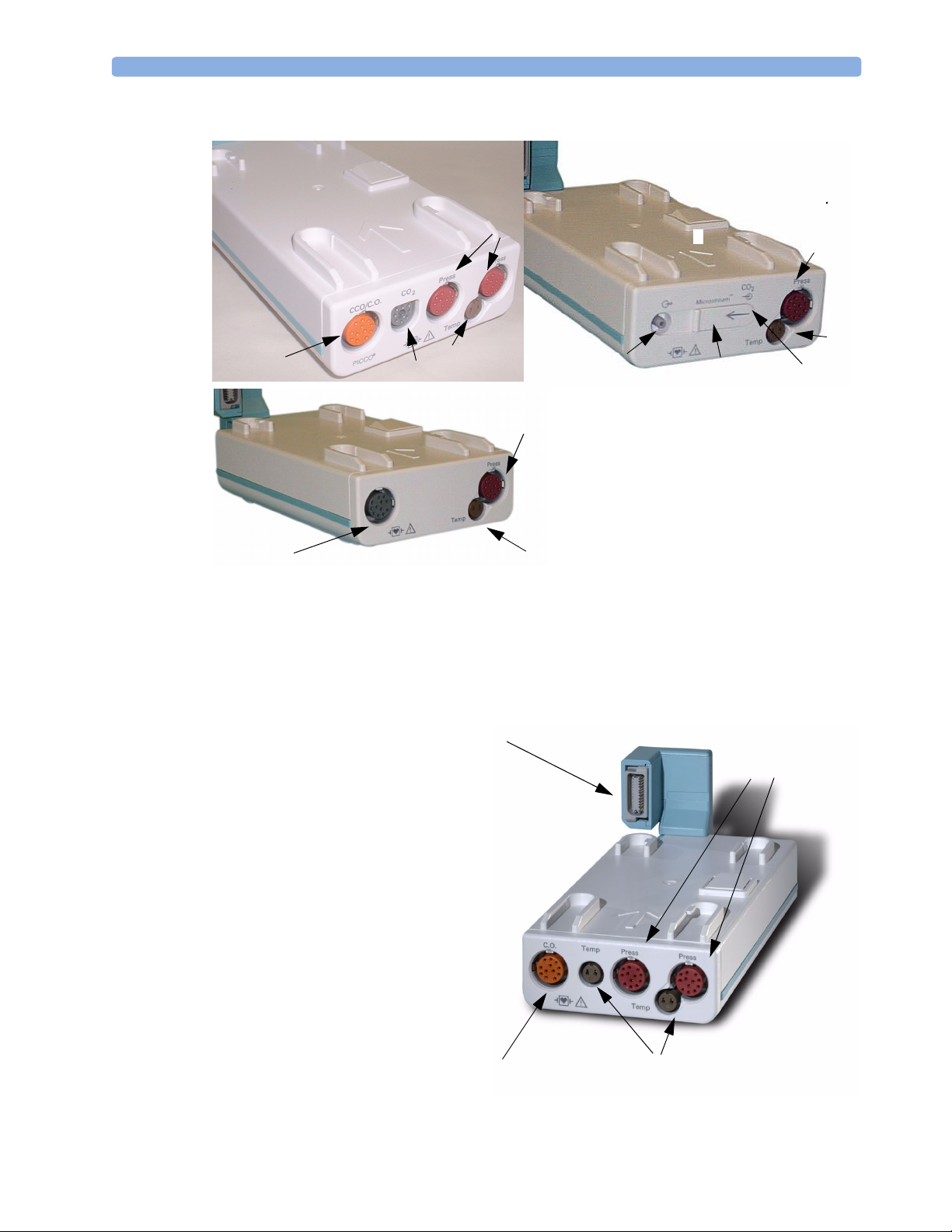
M3014A, M3015A and M3016A Capnography Extensions
The M3014A Capnography Extension adds mainstream capnography, and optionally one pressure
plus either a pressure or a temperature, Cardiac Output and Continuous Cardiac Output to the MMS.
The optional M3015A Microstream CO
either pressure or temperature to the MMS. The optional M3016A Mainstream CO
mainstream capnography and optionally either pressure or temperature to the MMS.
Extension adds microstream capnography and optionally
2
OR
Zero key - initiates a zero procedure for the
connected pressure transducer when
pressed and held for a second
Silence: acknowledges all active
alarms by switching off audible
alarm indicators and lamps
MSL cable connector to the monitor
Extension adds
2
10
Page 29
Related Products 1 Basic Operation
M3014A Capnography
4
M3016A Mainstream
3
Pressure connectors (red)
1
Temperature connector (brown)
2
Mainstream connector CO2 (optional)
3
Cardiac Output connector
4
M3015A Microstream
1
1
2
2
3
7
6
5
1
2
Inlet
5
Microstream
6
Gas sample outlet
7
connector CO
2
M3012A Hemodynamic Measurement Server Extension
Connection to MMS
The M3012A Hemodynamic
Measurement Server Extension
(HMSE) can be connected to the
M3001A Multi-Measurement Server to
provide the following additional
measurements: Temperature, Pressure,
an additional Pressure or Temperature,
and C.O. and CCO measurements.
Cardiac Output (orange;
optional)
Pressure connectors
(red)
Temperature connectors (brown)
11
Page 30
1 Basic Operation Operating and Navigating
Operating and Navigating
Everything you need to operate the monitor is contained on its screen. Almost every element on the
screen is interactive. Screen elements include measurement numerics, waveforms, screen keys,
information fields, alarms fields and menus.
The configurability of the monitor means that often you can access the same element in different ways.
For example, you might be able to access an item through its on-screen setup menu, via a hard key, or
via a SmartKey. These Instructions for Use always describe how to access items via an on-screen menu.
You may use whichever way you find most convenient.
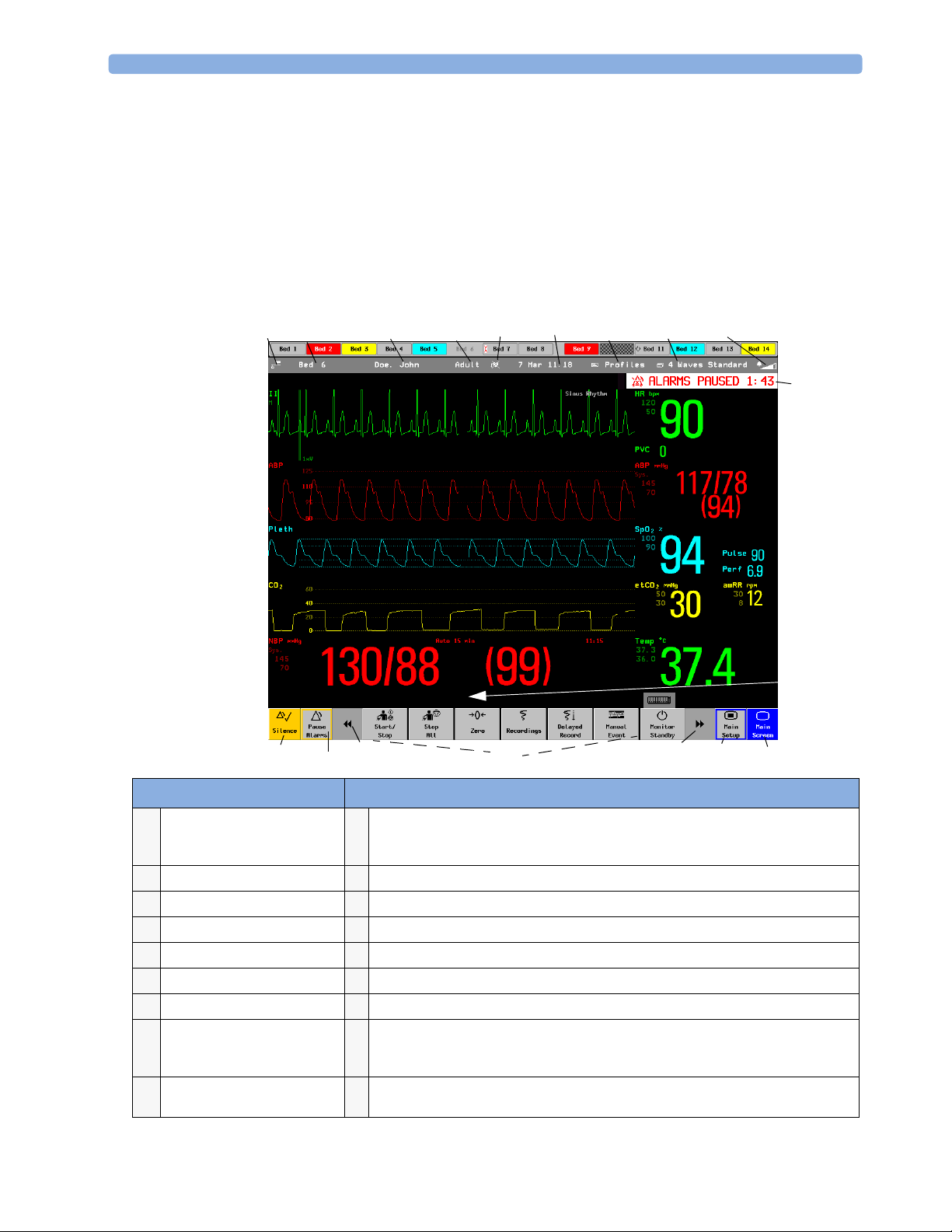
2
1
ABP Zero done at 11 Nov 02 7:31 am
18 16
17
3
5
4
67 8
9
10
11
15
14
13
12
Monitor information line Other screen elements
12
network connection indicator
1
(documented in Information
Center Instructions for Use)
bed label
2
patient identification
3
patient category
4
paced status
5
date and time
6
access the profiles menu
7
current screen name/enter
8
change screen menu
adjust alarm volume/level
9
indicator
alarm status area - shows active alarm messages
10
status line - shows information messages and prompting you for action
11
close all open menus and windows and return to main screen
12
enter Main Setup menu
13
scroll right to display more SmartKeys
14
SmartKeys - these change according to your monitor’s configuration
15
scroll left to display more SmartKeys
16
Pause Alarms - pauses alarm indicators. Pause duration depends on monitor
17
configuration. If pause duration is infinite, this key is labeled Alarms Off. Select again to
immediately re-enable alarm indicators.
Silence - acknowledges all active alarms by switching off audible alarm indicators and
18
lamps permanently or temporarily, if alarm reminder (ReAlarm) is configured on.
Page 31

Operating and Navigating 1 Basic Operation
Selecting Screen Elements
Select a screen element to tell the monitor to carry out the actions linked to the element. For example,
select the Patient Identification element to call up the Patient Demographics window, or
select the HR numeric to call up the Setup ECG menu. Select the ECG wave segment to call up the
ECG lead menu.
Note that the space between each line of a menu may be configured to wide or narrow to facilitate your
most common method of operation, either touch, Speedpoint or navigation point, or mouse.
Using the Setup Menu
MP20/MP30/
MP40/MP50
Only
Setup
Alarm Messages
Alarm Limits
Alarm Volume
My Care Group
Change Screens
Profiles
Admit/Dischrg
Paced No
Network
Bed Information
Date, Time
For the MP20/MP30 and MP40/MP50 monitors, the
elements at the top of the Screen are grouped together for
ease of navigation. Select any item at the top of the Screen
to open the Setup menu; scroll down the menu to
highlight the element you want then press the navigation
point to select the element.
Using the Touchscreen
Select screen elements by pressing them directly on the monitor’s screen.
Disabling Touchscreen Operation
♦ To temporarily disable touchscreen operation of the monitor, press and hold the Main
Screen permanent key. A padlock will appear on the Main Screen permanent key.
♦ Press and hold the Main Screen permanent key again to re-enable the touchscreen operation.
13
Page 32

1 Basic Operation Operating and Navigating
Using the SpeedPoint
1
2
3
4
5
integrated SpeedPoint
(MP60/MP70 only)
1 Silence - acknowledges all active alarms by switching off audible alarm indicators and lamps. Behavior
follows the Silence permanent key configuration.
2 Alarms Off/Pause Alarms- pauses alarm indicators. Behavior follows the Pause Alarms permanent key
configuration.
3 Main Screen - close all open menus and windows and return to the main screen.
4 Back - go back one step to the previous menu.
5 SpeedPoint knob - rotate and tilt to highlight elements. Press to select.
6 Function keys on remote SpeedPoint - function identical to the first five SmartKeys configured for a
screen.
7 On/standby key
6
7
Remote SpeedPoint
(all monitors)
Rotate the SpeedPoint knob left or right. With each click, the highlight jumps to the neighboring
screen element. Alternatively, tilt the knob to move it in the direction of a screen element. A cursor
moves across the screen, following the direction of the knob. Any screen element under the cursor is
highlighted. When you reach the screen element you want, press the knob to select the element.
Using the remote SpeedPoint, you can operate the monitor from a distant location such as at the foot
of the bed. The remote SpeedPoint can be used with all monitors.
14
Page 33

Operating and Navigating 1 Basic Operation
Using the Navigation Point
MP20/MP30/
MP40/MP50
Only
1Silence - acknowledges all active alarms by
switching off audible alarm indicators and
lamps. Exact behavior depends on permanent
key configuration
2Alarms Off/Pause Alarms - pauses alarm
indicators. Exact behavior depends on Pause
Alarms permanent key configuration
3 Main Screen -
windows and return to the main screen.
4Back - takes you back one step to the previous
menu.
5 Navigation Point knob
closes all open menus and
To use the navigation point, rotate it left or right. With each click, the highlight jumps to the
neighboring screen element. The element under the cursor is highlighted. When you reach the screen
element you want, press the knob to select the element.
Using a Mouse or Trackball
If you are using a mouse or trackball, select screen elements by clicking on them (press and release the
left mouse button). While you are moving the mouse, a cursor appears and a highlight shows your
current position.
Using Keys
The monitor has four different types of keys.
Permanent Keys
A permanent key is a graphical key that remains on the screen all the time to give you fast access to
functions.
Pause Alarms - pauses alarm indicators. Pause duration depends on monitor
configuration. If pause duration is infinite, this key is labeled
Select again to immediately re-enable alarm indicators.
Silence - acknowledges all active alarms by switching off audible alarm indicators and
lamps.
Alarms Off.
Main Screen - close all open menus and windows and return to the main screen.
Main Setup - enter main setup menu.
15
Page 34

1 Basic Operation Operating and Navigating
SmartKeys
A SmartKey is a configurable graphical key, located at the bottom of the main screen. It gives you fast
access to functions. The selection of SmartKeys available on your monitor depends on your monitor
configuration and on the options purchased.
enter profile menu change Screen
show BIS Sensor
freeze waves quick admit a patient
set alarm limits
change alarm volume end case to discharge a patient
change QRS volume
enter standby mode - suspends patient
monitoring. All waves and numerics
disappear from the display. All settings
and patient data information are
retained.
review beat labels (annotate
arrhythmia wave)
previous Screen
enter patient identification menu to
admit/discharge/transfer
view information for patients in other
beds
change screen brightness (not for
independent displays)
re-learn arrhythmia
16
change amplitude (size) of ECG wave enter cardiac output procedure
- start/stop manual NBP measurement
- start auto series
- stop current automatic measurement
within series
start veni puncture (inflate cuff to
subdiastolic pressure)
access patient reports zero invasive pressure transducer
start NBP STAT measurement
stop automatic or STAT NBP
measurement and measurement series
set the NBP repeat time
Page 35

Operating and Navigating 1 Basic Operation
start a delayed recording
set wide automatic alarm limits set narrow automatic alarm limits
access wedge procedure window access the Loops window
review vital signs trend review graph trend
access event surveillance access calculations
access the calculator access the Drug Calculator
gas monitor - exit standby mode suppress <gas measurement> zero
unpair equipment access ST Map application
Realtime Record SmartKey to access popup recording keys
start 12-Lead Capture (only available
if Information Center is connected)
access EEG CSA access the EEG montage
display VueLink information access timers
Hardkeys
A hardkey is a physical key on a monitoring device, such as the zero pressure key on the MMS or a
setup key on a module.
Pop-Up Keys
Pop-up keys are task-related graphical keys that appear automatically on the monitor screen when
required. For example, the confirm pop-up key appears only when you need to confirm a change.
Using the On-Screen Keyboard
Use this as you would a conventional keyboard. Enter the information by selecting one character after
another. Use the
single characters, or use the Clr key to delete entire entries. Select Enter to confirm what you have
entered and close the on-screen keyboard.
Shift and capital Lock keys to access uppercase letters. Use the Back key to delete
access remote applications (if Application
Server is connected)
17
Page 36

1 Basic Operation Operating and Navigating
If a conventional keyboard is connected to the monitor, you can use this instead of or in combination
with the on-screen keyboard.
Using the On-Screen Calculator
You can use the on-screen calculator to perform any of
the standard operations for which you would normally
use a handheld calculator.
♦ To access the on-screen calculator, select the
Calculator SmartKey, or select Main Setup
-> Calculations -> Calculator.
Calculator
MR
MC
M+
√
Back
C/CE
18
Page 37

Operating Modes 1 Basic Operation
Operating Modes
When you switch the monitor on, it starts up in monitoring mode. To change to a different mode:
1 Select the Main Setup menu.
2 Select Operating Modes and choose the mode you require.
Your monitor has four operating modes. Some are passcode protected.
• Monitoring Mode: This is the normal, every day working mode that you use for monitoring
patients. You can change elements such as alarm limits, patient category and so forth. When you
discharge the patient, these elements return to their default values. Changes can be stored
permanently only in Configuration Mode. You may see items, such as some menu options or the
altitude setting, that are visible but ‘grayed out’ so that you can neither select nor change them.
These are for your information and can be changed only in Configuration Mode.
• Demonstration Mode: Passcode protected, this is for demonstration purposes only. You must not
change into Demonstration Mode during monitoring. In Demonstration Mode, all stored trend
information is deleted from the monitor’s memory.
• Configuration Mode: Passcode protected, this mode is for personnel trained in configuration tasks.
These tasks are described in the Configuration Guide. During installation the monitor is configured
for use in your environment. This configuration defines the default settings you work with when
you switch on, the number of waves you see and so forth.
• Service Mode: Passcode protected, this is for trained service personnel.
When the monitor is in Demonstration Mode, Configuration Mode, or
Service Mode, this is indicated by a box with the mode name in the center
of the Screen and in the bottom right-hand corner. Select this field to
change to a different mode.
Standby Mode
Standby mode can be used when you want to temporarily interrupt monitoring.
To e n t e r Stan d y m o de ,
♦
♦ select Main Setup, followed by Monitor Standby.
The monitor enters Standby mode automatically after the End Case function is used to discharge a
patient.
Standby suspends patient monitoring. All waves and numerics disappear from the display but all
settings and patient data information are retained. A special Standby screen is displayed. If a patient
location is entered at the Information Center, this will also be displayed on the Standby screen
(availability depends on Information Center revision).
To resume monitoring,
♦ Select anything on the screen or press any key.
Config
select the Monitor Standby SmartKey or
19
Page 38

1 Basic Operation Understanding Screens
Understanding Screens
Your monitor comes with a set of preconfigured Screens, optimized for common monitoring scenarios
such as OR adult, or ICU neonatal. A Screen defines the overall selection, size and position of waves,
numerics and SmartKeys on the monitor screen when you switch on. You can easily switch between
different Screens during monitoring. Screens do NOT affect alarm settings, patient category and so
forth.
When you switch from a complex to a less complex Screen layout, some measurements may not be
visible but are still monitored in the background. If you switch to a more complex Screen with, for
example, four invasive pressure waves but you have only two pressures connected to the monitor, the
“missing” two pressures are either left blank or the available space is filled by another measurement.
Switching to a Different Screen
1 To switch to a different Screen, select the current Screen name in the monitor info line,
or select the Change Screen SmartKey.
2 Choose the new Screen from the pop-up list.
Changing a Screen’s Content
If you do not want to change the entire Screen content, but only some parts of it, you can substitute
individual waves, numerics, high-res waves, or trends. Be aware that these changes cannot be stored
permanently in Monitoring Mode.
To change the selection of elements on a Screen,
1 Select the element you want to change.
2 From the menu that appears, select Change Wave, Change Numeric, or
Change HiResTrend, and then select the wave or numeric you want, or select the highresolution trend wave you want from the list of available waves.
If you do not see Change Numeric in the menu, this Screen may be configured to always
display the numeric beside its wave. Changing the wave will automatically change the numeric.
The changed Screen is shown with an asterisk in the monitor info line.
20
Page 39

Using a Second Display 1 Basic Operation
In the Change Screen menu, the changed Screen is
shown linked to the original Screen and marked with an
asterisk.
Up to three modified Screens can be accessed via the
Change Screen menu.
To recall Screens, either
♦ select the name of the Screen in the
Change Screen menu
or
♦ use the previous/next arrows at the top of the
Change Screen menu to move back and forth in the
Screen history. The ten most recently-used Screens
including up to three modified Screens can be
accessed.
After a patient discharge, the monitor’s default Screen is
shown. Modified Screens are still available in the
Change Screen menu.
If the monitor is switched off and then on again, modified Screens are erased from the monitor’s
memory and cannot be recalled. If a modified Screen was the last active Screen when the monitor was
switched off, it is retained (unless Automat. Default is configured to Yes).
Change Screen
6 Waves A
Split Screen A
Loops
Cardiac Output
Vital Signs A
Vital Signs A*
Using a Second Display
A second display, showing the same Screen as the main display, can be connected to any of the
monitors, for viewing only.
A second display showing a different Screen can be connected to the MP90. The second display can
also be operated using standard input devices. There are two separate modes of operation depending on
whether one person is operating both displays or each display has its own operator. This is set in the
monitor’s Service Mode. In Service Mode you can also define which display you want windows to
appear on, when the setup keys on the modules are pressed or when a window is automatically opened.
The content of each Screen can be changed individually as described in the previous section. If you are
operating two displays, you can choose Screens for both displays from one location:
1 Select Profiles in the monitor info line of the first display,
2 Select Display 1, then select the Screen you want to display on the first display from the list of
available Screens.
3 Select Display 2, then select the Screen you want to display on the second display from the list
of available Screens.
The second display Screen may take a few seconds to load.
Using the Visitor Screen
If a visitor Screen is configured for your monitor, you can use it to clear the screen of all waves and
numerics but continue to monitor the patient with active alarms and trend storage at the bedside and
Information Center. You can change the name of the visitor Screen in Configuration Mode.
21
Page 40

1 Basic Operation Understanding Profiles
To activate this Screen, select the Screen name in the monitor info line to open the Screen
♦
menu, then select the name of the visitor Screen configured for your monitor from the list of
available Screens.
♦ Select any element on the Screen to open the Screen menu and select a different Screen to show
waves and numerics again.
Understanding Profiles
Profiles are predefined monitor configurations. They let you change the configuration of the whole
monitor so you can adapt it to different monitoring situations. The changes that occur when you
change a complete profile are more far reaching than those made when you change a Screen. Screens
affect only what is shown on the display. Profiles affect all monitor and measurement settings.
The settings that are defined by Profiles are grouped into three categories. Each category offers a choice
of ‘settings blocks’ customized for specific monitoring situations. These categories are:
• Display (screens)
– Each profile can have a choice of many different predefined screens. If you are using a second
display, each display can have its own individual screen selection. When you change the profile,
the screen selection configured for the new profile becomes active.
• Monitor Settings
– Each profile can have a choice of different predefined monitor settings. These relate to the
monitor as a whole; for example, display brightness, alarms off/paused, alarm volume, QRS tone
volume, tone modulation, prompt tone volume, wave speed, resp wave speed, pulse source.
• Measurement Settings
– Each profile can have a choice of different predefined measurement settings. These relate directly
to individual measurements, for example, measurement on/off, measurement color, alarms limits,
NBP alarm source, NBP repeat time, temperature unit (
Profiles
Profile : Profile A
Patient Category: Adult
Paced : No
Display : S-014
Meas Settings: Measurement A
Monitor Settings: Monitor A
o
F or oC) pressure unit (mmHg or kPa).
Measurement A
Measurement B
Measurement C
Measurement D
22
Profiles Menu, showing current settings Available choices in measurement
menu
Page 41

Understanding Profiles 1 Basic Operation
You can change from one complete profile to another or swap individual settings blocks (display
screen/monitor settings/measurement settings) to change a subset of a profile. Changes you make to
any element within the settings blocks are not saved when you discharge the patient, unless you save
them in Configuration Mode.
You might find it helpful to think of the three categories in terms of a restaurant menu. The Screens
are like the first course, offering you a choice of “starters” (many different screen configurations from
which you can choose the one that best suits your requirements). The Monitor Settings category is like
the main course, offering a choice of different “main dishes” from which you can pick one. The
Measurement Settings are like the dessert course. From these you build your meal. You can choose one
from the “starters”, one from the main course, then one from the dessert or simply pick one or two
courses without having a full meal.
Depending on your monitor configuration, when you switch on or discharge a patient the monitor
either continues with the previous profile, or resets to the default profile configured for that monitor.
WARNING If you switch to a different profile, the patient category and paced status normally change to the setting
specified in the new profile. However some profiles may be setup to leave the patient category and
paced status unchanged. Always check the patient category, paced status, and all alarms and settings,
when you change profiles.
When you leave Demonstration Mode, the monitor uses the default profile.
Swapping a Complete Profile
1 Select Profiles in the monitor info line, or select the Profiles Smartkey.
2 In the Profiles menu, select Profile.
3 Chose a profile from the pop-up list.
4 Confirm your selection.
Swapping a Settings Block
1 Select Profiles in the monitor info line, or select the Profiles Smartkey.
2 In the Profiles menu, select Display or Measmnt. Settings or
Monitor Settings
3 Choose a settings block from the pop-up list.
4 Confirm your selection.
to call up a list of the settings blocks in each category.
Default Profile
Your monitor has a default profile that it uses when you leave Demonstration, or Service modes, or
when you discharge a patient. This profile is indicated by a diamond .
Locked Profiles
Some profiles are locked, so that you cannot change them, even in Configuration Mode. These are
indicated by this lock symbol.
23
Page 42

1 Basic Operation Understanding Settings
Understanding Settings
Each aspect of how the monitor works and looks is defined by a setting. There are a number of
different categories of settings, including,
Screen Settings, to define the selection and appearance of elements on each individual Screen
Measurement settings, to define settings unique to each measurement, for example, high and low
alarm limits
Monitor settings, including settings that affect more than one measurement or Screen and define
general aspects of how the monitor works, for example, alarm volume, reports and recordings, and
display brightness.
You must be aware that, although many settings can be changed in Monitoring Mode, permanent
changes to settings can only be done in the monitor’s Configuration Mode. All settings are reset to the
stored defaults:
• when you discharge a patient
•when you load a Profile
• when the monitor is switched off for more than one minute (if Automat. Default is set to
Yes).
Changing Measurement Settings
Each measurement has a setup menu in which you can adjust all of its settings. You can enter a setup
menu:
• via the measurement numeric - select the measurement numeric to enter its setup menu. For
example, to enter the
• via the Setup hardkey (on plug-in modules) - press the Setup hardkey on the module front.
•via the Main Setup SmartKey - if you want to setup a measurement when the measurement is
switched off, use the Main Setup SmartKey and select Measurements. Then select the
measurement name from the popup list. With this SmartKey you can access any setup menu in the
monitor.
• via the Measurement Selection key.
This guide always describes the entry method using the setup menu. But you can use any method you
prefer.
Setup ECG menu, select the HR (heart rate) numeric.
Switching a Measurement On and Off
When a measurement is off, its waves and numerics are removed from the monitor’s screen. The
monitor stops data acquisition and alarming for this measurement. A measurement automatically
switches off if you disconnect its module or measurement server. If you disconnect a transducer, the
monitor replaces the measurement numeric with question marks.
1 Enter the measurement’s setup menu and select the measurement.
24
2 Select the measurement name to toggle between on and off. The screen display indicates the active
setting.
Page 43

Changing Wave Speeds 1 Basic Operation
Switching Numerics On and Off
For some measurements, such as EEG, you can choose which numerics to view on the screen.
♦ In the measurement’s setup menu, select the numeric name to toggle between on and off.
For example in the Setup EEG menu, select the EEG numeric name to toggle between on and
off.
Adjusting a Measurement Wave
♦ To quickly adjust wave-related measurement settings (such as speed or size), select the
measurement wave itself. This displays the measurement
related measurement settings.
Wave menu, which has only wave-
Changing Wave Speeds
Lowering the wave speed compresses the wave and lets you view a longer time period. Increasing the
speed expands the waveform, giving you a more detailed view.
The monitor distinguishes three groups of wave speed settings,
• RespiratorySpeed, for all respiratory waves: CO
• EEG Speed, for all EEG and BIS waves
• Global Speed, for all waves not included in the other two groups.
Changing the Wave Group Speed
The wave speed group setting defines the speed of all the waves in the group.
To change the wave speed of a wave speed group,
1 Select Main Setup -> User Interface
2 Select Global Speed, RespiratorySpeed, or EEG Speed as required
3 Select a value from the list of available speeds.
Changing Wave Speed for a Channel
To change the wave speed of an individual wave channel,
1 Enter the Wave menu for a measurement by selecting its wave.
2 Select Change Speed.
3 To set the speed to the wave group speed, select RespiratorySpeed, EEG Speed, or
Global Speed.
To set an individual channel speed, select a numeric value from the list of available speeds. This
overrides the wave group speed setting and set the speed for the individual wave channel on the
monitor Screen. The wave channel speed is independent of the wave (label) depicted in the
channel, if you change the wave, the new wave will retain the set channel speed.
, Resp. anesthetic agents and O
2
2
25
Page 44

1 Basic Operation Freezing Waves
Freezing Waves
You can freeze waves on the screen and measure parts of the wave using cursors. The waves are frozen
with a history of 20 seconds so that you can go back and measure what you have seen.
Freezing An Individual Wave
To freeze a wave,
1 Enter the Wave menu for the measurement by selecting the wave on the screen.
2 Select Freeze Waves.
The realtime wave is replaced with the frozen wave.
Freezing All Waves
To freeze all waves on the screen,
1 Select the Freeze Waves SmartKey.
All realtime waves are replaced with frozen waves.
Measuring Frozen Waves
To measure a frozen wave,
1 Select the frozen wave.
If you are using touch, this automatically positions the vertical cursor. The cursor can be
repositioned by touching the required point on the wave, or
2 Using the Speedpoint or another pointing device or touch: use the right/left arrow keys to move
the vertical cursor.
The vertical cursor moves through the time axis and the current value is displayed next to the
cursor.
3 Use the up/down arrow keys to activate and move the horizontal cursor.
The horizontal cursor measures the wave value, which is displayed above the cursor line.
Changing The Wave Speed
Lowering the wave speed compresses the wave and lets you view a longer time period. Increasing the
speed expands the waveform, giving you a more detailed view.
To change the wave speed:
1 Select the frozen wave.
2 Select Change Speed.
3 Select a speed from the list.
Updating The Frozen Wave
To update the wave, that is freeze the current wave:
1 Select the frozen wave.
2 Select Freeze Again.
26
Page 45

Using Labels 1 Basic Operation
Releasing Frozen Waves
To release frozen waves,
1 Select a frozen wave.
2 Select Unfreeze Waves.
All frozen waves are released.
Using Labels
You can measure multiple invasive pressures, temperatures, and SpO2 simultaneously. The monitor
uses labels to distinguish between them. The default settings defined in the profile (such as
measurement color, wave scale, and alarm settings) are stored within each label. When you assign a
label to a measurement, the monitor automatically applies these default settings to the measurement.
The labels assigned are used throughout the monitor, in reports, recordings, and in trends.
About Label Sets
Your monitor may be configured to use a Restricted or Full label set. The Full label set
provides extra labels for Pressure and Temp. See the sections in this Instructions for Use on Pressure
and Temp for more information.
If you connect a measurement server from a monitor using a Full label set to an IntelliVue monitor
using a Restricted label set or an M3/M4 monitor, any additional labels switch to labels available
in the target monitor. This may cause a label conflict with other monitored measurements.
Be aware that connecting a monitor using the Full label set to an Information Center with certain
software revisions may affect the availability of measurement information from the additional labels on
the Information Center. See the Information Center documentation and your monitor’s
Configuration Guide for information on label set compatibility.
Changing Measurement Labels (e.g. Pressure)
To change a measurement label of a measurement with multiple labels (invasive pressure, temperature,
or SpO
1 Enter the Wave menu of the measurement.
2 Select Label.
3 Choose a label from the list.
The monitor automatically applies the scale, color, etc. settings stored in the Profile for the label you
select. You can change scale settings in Monitoring Mode, but color can only be changed in the
monitor’s Configuration Mode.
Any labels already being used in the monitor are shown “grayed-out” in the list and cannot be selected.
Give me an example Let’s imagine you used a Press module to monitor your previous patient’s CVP.
Now you want to use the same module to measure ABP with a new patient. You’ve set up your arterial
line. When you connect the pressure transducer to the module, the pressure shown on the screen still
uses the CVP color and wave scale and is labeled CVP. To rectify this, just change the pressure label to
ABP. Now the pressure has the correct color, the wave is shown in the correct scale, and the
appropriate alarm limits for ABP are active.
),
2
27
Page 46

1 Basic Operation Using Labels
Resolving Label Conflicts
Each label must be unique, that is, it can only be assigned once. You cannot monitor two pressures
labelled “ICP” at the same time. If you need to use two identical pressures, you must assign different
labels to them, for example, P and ICP.
Measurement labels are stored in the measurement device (module or measurement server). If you try
to use two measurement devices that have identical labels, this causes a label conflict in the monitor.
Depending on your configuration, the monitor will either
• resolve the conflict automatically, by assigning a new, generic label
to the most recently connected conflicting label (e.g. a second FAP
label could be changed to ABP)
•display the Measurement Selection window automatically
for you to resolve the conflict
• take no action, you must enter the Measurement
Selection window and resolve the conflict
All the currently available measurement devices are depicted in the Measurement Selection
window. Any measurement labels causing a label conflict are shown in red. If a measurement device is
connected but currently unavailable, for example, because it was deactivated due to a label conflict, the
device is shown “grayed-out”.
measurement selection key
with question marks
indicating a label conflict
Conflicting measurement
Measurement Selection
labels are shown in red
SpO2
SpO2 BIS
Tskin C.O.
EcgRsp NBP ABP
De-activated labels are
grayed-out
CO2
Temp
To resolve a label conflict,
1 Select the measurement selection key or select Main Setup -> Measurement Selection
to display the Measurement Selection window.
2 Select the device whose label you want to correct.
3 Use the measurement selection pop-up keys to resolve the conflict. Select either:
– Change Label to assign a different label to the conflicting label
– De-activate: to disable the conflicting device. It retains its label for future use but becomes
invisible to the monitor, as though it had been unplugged. When the device has been deactivated
the question marks under the measurement selection key will be replaced by XXX.
– Setup <Measurement label>: to enter the Setup menu for the measurement and change
the conflicting device’s label to a different label.
– Modify Driver (VueLink only) - change the VueLink device driver.
28
Page 47

Changing Monitor Settings 1 Basic Operation
Changing Monitor Settings
♦ To change monitor settings such as date and time, brightness, or QRS tone volume, select the
Main Setup SmartKey and then select the setting you want to change, or select User
Interface to enter a submenu where you can change user interface settings.
Adjusting the Screen Brightness
1 Select the Brightness SmartKey.
2 Select the appropriate setting for the screen brightness. 10 is the brightest, 1 is the least
bright.
Your monitor may be configured with a lower brightness for Standby mode and also (for battery
powered monitors) for transport to conserve battery power.These settings can only be changed in the
monitor’s Configuration Mode.
If you are using an MP80 or MP90 with an external display, the Brightness SmartKey does not
adjust the brightness of this display. See the instructions supplied with the external display for
instructions.
Adjusting Touch Tone Volume
The touch tone volume is the tone you hear when you select any field on the monitor screen. To adjust
the touch tone volume,
1 In the Main Setup menu, select User Interface
2 Select TouchToneVolume, then select the appropriate setting for the touch tone volume: 10 is
the loudest and 1 is the quietest. Selecting zero switches the touch tone volume off.
Setting the Date and Time
If your monitor is connected to an Information Center, the date and time are automatically taken from
this. Once it is set, the internal clock retains the setting even when you switch off the monitor.
WARNING Changing the date or time will affect the storage of trends and events.
1 Select the Date, Time screen element from the monitor’s info line to enter the Date, Time
menu.
2 Select, in turn, the Year, Month, Day, Hour (in 24 hour format, only) and Minute as
necessary. Select the correct values from the pop-up list.
3 Select Store Date, Time to change the date and time.
Checking Your Monitor Revision
1 Select Main Setup -> Revision to open the Monitor Revision menu.
2 Select the correct device from the device pop-up keys.
3 From the Monitor Revision menu, select the monitor component for which you need
revision information.
29
Page 48

1 Basic Operation Getting Started
Getting Started
Once you understand the basic operation principles, you can get ready for monitoring.
Inspecting the Monitor
WARNING If the monitor is mechanically damaged, or if it is not working properly, do not use it for any
monitoring procedure on a patient. Contact your service personnel.
1 Before you start to make measurements, carry out the following checks on the monitor including
all connected Measurement Servers, modules, or measurement server extensions.
– Check for any mechanical damage.
– Check all the external cables, plug-ins and accessories.
2 Plug the power cord into the AC power source. If you are using battery power, ensure that the
battery has sufficient power for monitoring. When you use a battery for the first time, you must
charge it, following the instructions given in the section on Charging Batteries.
3 Check all the functions of the instrument that you need to monitor the patient, and ensure that the
instrument is in good working order.
Switching On
♦ Press the on/off switch on the monitor for one second. The monitor performs a self test and is then
ready to use. If you see a message such as
starting monitoring that measurement. Connected devices usually take their power from the
monitor. External devices such as gas monitors and those connected via VueLink have their own
power switches.
CO2 Sensor Warmup wait until it disappears before
Setting up the Measurement Servers and Modules
1 Decide which measurements you want to make.
2 Connect the required modules, Measurement Servers, or measurement server extensions.
3 Check that you have the correct patient cables and transducers plugged in. The connectors are
color-coded to the patient cables and transducers for easy identification.
Starting Monitoring
After you switch on the monitor,
1 Admit your patient to the monitor.
2 Check that the profile, alarm limits, alarm and QRS volumes, patient category and paced status
and so forth are appropriate for your patient. Change them if necessary.
3 Refer to the appropriate measurement section for details of how to perform the measurements you
require.
30
Page 49

Disconnecting from Power 1 Basic Operation
Disconnecting from Power
The On/Standby switch does not disconnect the monitor from the ac power source. To disconnect,
unplug the power cable.
Monitoring After a Power Failure
If the monitor is without power for less than one minute, monitoring will resume with all active
settings unchanged. If the monitor is without power for more than one minute, the behaviour depends
on your configuration. If Automat. Default is set to Yes, the default profile will be loaded
when power is restored. If Automat. Default is set to No, all active settings are retained, if power
is restored within 48 hours. The Automat. Default setting is made in Configuration Mode.
Networked Monitoring
If your monitor is connected to a network, a network symbol is displayed in the upper left corner next
to the bed label. To see details about the Care Group, the monitoring equipment, and technical
information about the network,
♦ MP20/MP30/MP40/MP50 - select the monitor info line to enter the Setup menu, then select
Bed Information.
♦ MP60/MP70/MP80/MP90 - in the monitor info line, select the bed label.
Be aware that some network-based functions may be limited for monitors on wireless networks in
comparison to those on wired networks.
Using Remote Applications
If your monitor is connected to a Philips Application Server, you can access applications hosted
remotely on the Application Server and display and operate them on the bedside monitor screen. The
Application Server provides portal technology to allow information access through a web browser,
terminal emulation, or served applications. The applications available depend on the Application
Server configuration: see the device documentation for details. A Remote Application window can also
be embedded in a monitoring Screen.
To display remote applications on the monitor,
1 In the Main Setup menu, select Remote Applics, or select the
Remote Applications SmartKey.
2 Select the required application from the pop-up list of available applications.
3 Operate the application with your preferred monitor input device: touchscreen, SpeedPoint,
navigation point, keyboard or mouse.
31
Page 50

1 Basic Operation Using Remote Applications
Remote Application Popup Keys
Pop-Up Keys Selecting this pop-up key lets you....
Minimize
minimize the Remote Application window; the session continues running in the
background. Select the Remote Application symbol to show the window at full size
again.
Keyboard
Refresh
Close
start a keyboard application to show a keyboard on the display. This key is not
available if the keyboard application is not installed or not supported on the Philips
Application Server.
update the content of the Remote Application window.
close the Remote Application session.
The Remote Application window occupies a pre-defined area on the monitor Screen. The maximum
size of the area depends on the resolution of your display. If the pre-defined area for the Remote
Application covers the full monitor Screen (on independent second displays only), the pop-up keys are
not displayed. In this case a small window appears with two keys: one (with the Remote Application
symbol) to display the pop-up keys and another to move the small window if it is obstructing viewing.
If you change the monitor Screen while a Remote Application is running, and the pre-defined area on
the second Screen is smaller, the Remote Application cannot be shown at full size. You must select a
suitable monitor Screen to display the Remote Application again.
32
Page 51

This section lists the most important new features and improvements to the monitor and its user
interface introduced with each release. Further information is provided in other sections of this book.
You may not have all of these features, depending on the monitor configuration purchased by your
hospital.
What’s New in Release C.0?
IntelliVue MP80
The MP80 patient monitor is a new addition to the IntelliVue patient monitor family. The
functionality is similar to that of the MP70 but with the flexibilty of component modularity as in the
MP90.
M3014A Capnography Extension
2
2What’s New?
The M3014A Capnography Extension offers a new measurement combination - mainstream CO
cardiac output, invasive pressure and invasive pressure/temperature.
M8045A Docking Station
The docking station provides quick mounting and connections for the MP20/MP30/MP40/MP50 in
a one-step operation. By placing the monitor on the docking station and closing the lever you can
make the connection to AC power and to a network, if present.
BIS Interface Board
This interface board allows use of Bispectral Index monitoring with the MP20 and MP30.
Timers Application
The new Timers application allows you to set timers to notify you when a specific time period has
expired. The timers can have varying characteristics and can be located on the Main screen for easy
viewing.
IntelliVue Instrument Telemetry (USA only)
Wireless network capabilities via the IntelliVue Instrument Telemetry network using a built-in
interface (MP20/MP30) or an external adapter (MP40/MP50).
Remote Applications
Remote applications can now be embedded in a monitoring Screen. The display colors for remote
applications have been enhanced.
Basic Operation
,
2
• Selection and order of SmartKeys can now be configured in the monitor’s Configuration mode.
33
Page 52

2What’s New? What’s New in Release B.1?
• A new SmartKey exits Standby mode at the gas monitor.
• Direct operation of a second independent display with the MP90, using standard input devices.
• Networked monitors can now show Telemetry information for the “Own Bed” in an overview
window or embedded in a Screen.
• Overview bed information can be configured to display in the colors used at the Information Center
(with Information Center System G or higher).
• Support for Unit-based Care Group model for up to 64 beds (with Information Center System G or
higher).
• Battery status information on the main screen now includes estimated monitoring time available
during battery charging.
• Barcode reader support during patient admission.
• Direct entry to graphical trends when a limit alarm is selected in alarm review and to the event
episode window when an event alarm is selected.
• MP90: screen trends can now also be viewed on the second display.
Trends
• In graphical trends, a segment menu allows direct adjustment of trend scales, automatic scale
optimization, expanded view for an individual segment.
• In graphical and horizon Screen Trends a cursor is available.
• In the Vital Signs window, the values can be shown with the parameter color.
Events
• Events can be configured to be signaled as alarms (advanced event surveillance only).
• Deviation triggers can be set which trigger an event when measured values change by a defined
amount over a set time (advanced event surveillance only).
• Up to six event groups can be active simultaneously (advanced event surveillance only).
Measurements
• Pulse Pressure Variation is a new derived measurement calculated from beat-to-beat arterial pressure
values.
• MAC value calculations
Applications
• Improved Drug Calculator meeting JCAHO requirements.
• The ST Map application shows ST changes over time in two multi-axis spider diagrams.
• Freeze and measure waves on the Main Screen.
What’s New in Release B.1?
34
IntelliVue MP20/MP30
The MP20/MP30 patient monitor is a new addition to the IntelliVue patient monitor family. It is
smaller and lighter than the MP40/MP50 monitors and can be powered by battery. It can be used with
the measurement server and server extensions and has a built-in recorder.
Page 53

What’s New in Release B.0? 2What’s New?
Basic Operation
• New Measurement Selection window makes it easier to resolve measurement label conflicts
• New Previous/Next Screen function provides access to the ten most recently modified Screens
• Wave speeds can now be set for individual wave channels
Trends
• Cursor in graphical trend window improves navigation in the trends database
• Vital Signs and Graphical Trend screen elements can be embedded on a Screen
• New band style format for displaying trends of measurements with multiple numerics
• Horizon trend is a new format for screen trends, showing the deviation from a stored baseline
• Aperiodic measurements now stored with a timestamp in Vital Signs
• New symbol representing NBP measurements in Graphical Trends
Measurements
• ST numerics in the Alarm Limits window can be shown and hidden
• ST Point can be set directly by selecting a numeric value
• New NBP countdown timer shows the time remaining until the next NBP measurement in a series
• Networked monitors can now show Other Bed information embedded on Screen
• Additional labels available for Pressure and Temp
• Additional options for SpO
• Suppress Zero function for Microstream CO
Applications
• Drug Calculator can now be configured to include a list of commonly-used drugs
• Cursor in the Loops window improves navigation through the stored loops
• Volume-flow loops added to the list of respiratory loops types
• Loops Report for documentation of stored loops
• EEG CSA can now be called up and viewed in a window over the currently displayed Screen
, support for an extended list of accessories
2
What’s New in Release B.0?
IntelliVue MP40/MP50 The MP40/MP50 patient monitor is a new addition to the IntelliVue
patient monitor family. It uses the same measurement devices as the MP60/MP70/MP90 monitors
and shares the same technological platform and user interface, but is more compact in size and can be
operated by battery.
2
M3012A Measurement Server Extension The new Hemodynamic Measurement Server Extension
extends measurement capability by adding two additional pressures and Cardiac Output.
M1020B SpO
measurement without the need to use the VueLink module. Two options are available:
– Option A01 for use with Philips reusable and disposable sensors and Nellcor “R-Cal” disposable
sensors.
Module New SpO2 measurement module, M1020B, enables dual SpO2
2
35
Page 54

2What’s New? What’s New in Release B.0?
– Option A02 for use with Nellcor OxiMax sensors, including the MAX-FAST forehead sensor.
M1020B Option A02 for use with Nellcor OxiMax sensors may not be available in all countries.
PV Loops: compares graphic representations of airway waves to help detect changes in the patient
airway condition.
High-resolution waves per Screen: the number of high-resolution waves that can be shown on a
Screen is increased, limited only by the Axx Option purchased.
Alarms symbols: New alarm symbols are introduced, and “short” yellow alarms were renamed “onestar” yellow alarms (yellow arrhythmia alarms).
Aperiodic measurements available as Screen Trends: patient trend information for NBP, C.O., C.I.,
and Wedge can now be permanently displayed on the Screen in tabular and graphical form.
36
Page 55

What’s New in Release A.2? 2What’s New?
What’s New in Release A.2?
12-Lead ECG recordings: 12-Lead ECG waves and numerics can be sent to a connected recorder
High-Resolution Trend Report: high-resolution trend report can be sent to a connected printer
ST Snippets ST snippets, showing a one second wave segment for each measured ST lead, can be
permanently displayed on the Screen or called up as required.
EEG Wave Speed: new EEG-specific wave speeds have been added to the list of wave speeds available
Drug Calculator: this new feature helps you to calculate drug dosages for your patients
On-Screen Calculator: a mathematics calculator can be used on the Screen
Visitor Screen: this new Screen is designed to hide sensitive patient information from the Screen.
Monitoring and alarm generation function as usual.
Touch selection volume control: The volume of the audio prompt given when a screen element is
selected is now adjustable
VueLin k i nterface : the VueLink on-screen appearance and controls are improved
M3001A: Trend upload from the Multi-Measurement Server (M3001A) improved
Screen Trends: lets you display patient trend information in graphic form permanently on the Screen
Alarm Limits Page: lets you view and control alarm settings for all measurements in one window
New Option for Event Surveillance: a new neonatal event review option #C04 is introduced
Second display To simultaneously show two different Screens, a second display can be connected to
the MP90. The second display is for viewing only.
37
Page 56

2What’s New? What’s New in Release A.2?
38
Page 57

3
3Alarms
The alarm information here applies to all measurements. Measurement-specific alarm information is
discussed in the sections on individual measurements.
The monitor has three alarm levels: red, yellow, and INOP.
Red and yellow alarms are patient alarms. A red alarm indicates a high priority patient alarm such as a
potentially life threatening situation (for example, asystole). A yellow alarm indicates a lower priority
patient alarm (for example, a respiration alarm limit violation). Yellow arrhythmia alarms are specific to
arrhythmia-related patient conditions (for example, ventricular bigeminy).
INOPs are technical alarms, they indicate that the monitor cannot measure or detect alarm conditions
reliably. If an INOP interrupts monitoring and alarm detection (for example, LEADS OFF), the
monitor places a question mark in place of the measurement numeric and an audible indicator tone
will be sounded. INOPs without this audible indicator indicate that there may a problem with the
reliability of the data, but that monitoring is not interrupted.
Alarms are indicated after the alarm delay time. This is made up of the system delay time plus the
trigger delay time for the individual measurement. See the specifications section for details.
If more than one alarm is active, the alarm messages are shown in the
alarm status area in succession. An arrow symbol next to the alarm
message informs you that more than one message is active.
The monitor sounds an audible indicator for the highest priority alarm. If more than one alarm
condition is active in the same measurement, the monitor announces the most severe. Your monitor
may be configured to increase alarm indicator volume automatically during the time when the alarm is
not acknowledged.
↑ ** HR HIGH
39
Page 58

3Alarms Visual Alarm Indicators
Visual Alarm Indicators
Alarm message: An alarm message text appears in the alarm status area at the top of the screen
indicating the source of the alarm. If more than one measurement is in an alarm condition, the message
changes every two seconds, and has an arrow ( ) at the side. The background color of the alarm
message matches the alarm priority: red for red alarms, yellow for yellow alarms, and light blue for
INOPs. The asterisk symbols (*) beside the alarm message match the alarm priority: *** for red alarms,
** for yellow alarms, * for yellow arrhythmia alarms. INOPs are displayed without asterisks.
Depending on how your monitor is configured, it may display alarm limit violation messages
• in text form, for example “**SpO2 LOW” or
• in numeric form, for example “**SpO2 94<96”, where the first number shows the maximum
deviation from the alarm limit, and the second number shows the currently set limit.
Flashing numeric: The numeric of the measurement in alarm flashes.
Bright alarm limits: If the alarm was triggered by an alarm limit violation, the corresponding alarm
limit on the monitor screen is shown more brightly.
Alarm lamp: A lamp on the monitor’s front panel flashes. This has the same color as the alarm
priority.
Nurse call systems: Alarm conditions are indicated on any device connected to the nurse call relay, if
configured to do so.
Audible Alarm Indicators
The audible alarm indicators configured for your monitor depend on which alarm standard applies in
your hospital. Audible alarm indicator patterns are repeated until you acknowledge the alarm by
switching it off or pausing it. or until the alarm condition ceases (if audible alarm indication is set to
non-latching).
WARNING Do not rely exclusively on the audible alarm system for patient monitoring. Adjustment of alarm
volume to a low level or off during patient monitoring may result in patient danger. Remember that
the most reliable method of patient monitoring combines close personal surveillance with correct
operation of monitoring equipment.
Alarm Tone Configuration
The audible alarm indicators of your monitor are configurable. In the monitor’s Configuration Mode,
you can:
• increase the alarm volume of unacknowledged alarms at regular intervals
• change the interval between alarm sounds (ISO/IEC Standard 9703-2 alarms only)
40
• change the base volume of the red and yellow alarm tones and the INOP tones
• change the alarm sound to suit the different alarm standards valid in different countries.
Page 59

Audible Alarm Indicators 3Alarms
Traditional Audible Alarms (HP/Agilent/Philips/Carenet)
• Red alarms: A high pitched sound is repeated once a second.
• Two-star yellow alarms: A lower pitched sound is repeated every two seconds.
• One-star yellow alarms (arrhythmia alarms): The audible indicator is the same as for yellow alarms,
but of shorter duration.
• INOPs: an INOP tone is repeated every two seconds.
ISO/IEC Standard 9703-2 Audible Alarms
• Red alarms: A high pitched tone is repeated five times, followed by a pause.
• Two-star yellow alarms: A lower pitched tone is repeated three times, followed by a pause.
• One-star yellow alarms (arrhythmia alarms): The audible indicator is the same as for yellow alarms,
but of shorter duration.
• INOPs: a lower pitched tone is repeated twice, followed by a pause.
Changing the Alarm Tone Volume
♦ The alarm volume symbol at the top right of the monitor screen gives you an
indication of the current volume. To change the volume, select the volume symbol
and then select the required volume from the pop-up selection.
♦ If you want to see a numerical indication of the current alarm volume on a scale
from zero to 10, select the Alarm Volume SmartKey. The volume scale pops up.
The current setting is indented. To change the setting, select the required number
on the scale. Any settings that are inactive (“grayed out”) have been disabled in the
monitor’s Configuration Mode.
When the alarm volume is set to zero (off), the alarm volume symbol reflects this. If you
switch the alarm volume off, you will not get any audible indication of alarm conditions.
Minimum Volume for No Central Monitoring INOP
If your monitor is connected to an Information Center, and the connection is interrupted, the INOP
message No Central Monit. will appear within 30 seconds, accompanied by an INOP tone. To
help ensure that this INOP, and any other active alarm, is not overlooked, the INOP and alarm tones
may be configured to have a minimum volume. In this case, INOP and alarm tones will sound even if
the monitor alarm volume is set to zero.
Alarm
41
Page 60

3Alarms Acknowledging Alarms
Acknowledging Alarms
To acknowledge all active alarms and INOPs, select the Silence permanent
key. This switches off the audible alarm indicators and alarm lamps. Alternatively,
you can acknowledge alarms by pressing the Silence hardkey on the MMS or
on the SpeedPoint. The hardkeys follow the behavior configured for the
permanent key.
A check mark beside the alarm message indicates that the alarm has been
acknowledged. If the monitor is configured to re-alarm, a dashed check mark will
be shown.
Silence
If the condition that triggered the alarm is still present
after the alarm has been acknowledged, the alarm message
stays on the screen with a check mark symbol beside it.
If the alarm condition is no longer present, all alarm indicators stop and the alarm is reset.
Switching off the alarms for the measurement in alarm, or switching off the measurement itself, also
stops alarm indication.
Acknowledging Disconnect INOPs
Acknowledging an INOP that results from a disconnected transducer switches off the associated
measurement. The only exception is ECG/Resp: acknowledging a disconnect INOP for ECG leads
does not switch off the ECG and Resp measurements. Acknowledging a disconnect INOP at the
Information Center switches off the audible INOP indicator but does not switch off the measurement.
Unplugging an MMS or a plug-in module automatically switches off its measurements.
Alarm Reminder (ReAlarm)
If Alarm Reminder is configured on for your monitor, you will get an audible reminder of alarm
conditions that remain active after you have acknowledged the alarm. This reminder may take the form
of a repetition of the alarm tone for a limited time, or an unlimited repetition of the alarm tone (this is
the same as a new alarm). There is no alarm reminder for INOPs.
In Configuration Mode, you can set the interval between silencing the alarm and sounding the
reminder tone to one, two, or three minutes.
APNEA
Pausing or Switching Off Alarms
If you want to temporarily prevent alarms from sounding, for example while you are moving a patient,
you can pause alarms. Depending on your monitor configuration, alarms are paused for one, two, or
three minutes, or infinitely.
To view the alarm pause setting chosen for your unit,
1 Select Main Setup -> Alarm Settings
2 Check the Alarms Off setting.
This setting can only be changed in Configuration Mode.
42
Page 61

Pausing or Switching Off Alarms 3Alarms
To Pause All Alarms
♦ Select the Pause Alarms permanent key. If your monitor is configured to
infinite pause time, the permanent key is labelled Alarms Off, and selecting it
switches alarms off.
♦ Or press the Alarms hardkey on the SpeedPoint or Navigation Point. The hardkey
follows the behavior configured for the permanent key.
Pause
Alarms
To Switch All Alarms Off
You can only switch alarms off permanently if your monitor is configured to allow infinite alarms
pause and the permanent key is labelled Alarms Off.
♦ Select the Alarms Off permanent key.
♦ Or press the Alarms hardkey on the SpeedPoint or Navigation Point. The
hardkey follows the behavior configured for the permanent key.
Pausing alarms infinitely is the same as switching them off.
Alarms
Off
To Switch Individual Measurement Alarms On or Off
1 Select the measurement numeric to enter its setup menu.
2 Select Alarms to toggle between On and Off.
The alarms off symbol is shown beside the measurement numeric.
While Alarms are Paused or Off
• The red Alarms Paused lamp on the monitor front panel is lit.
•
In the alarm field, the monitor displays the message
Alarms Paused or Alarms Off, together with
the alarms paused symbol and the remaining pause
time in minutes and seconds, or alarms off symbol.
• No alarms are sounded and no alarm messages are
shown.
• INOP messages are shown but no INOP tones are
sounded.
The only exceptions are the INOPs Battery/Batteries Empty, Battery/
Batteries Malfunction, Batt 1/2 Missing, and NBP Cuff Overpressure.
These INOPs are sounded even if alarms are paused or off.
ALARMS PAUSED 1:28
ALARMS OFF
• The nurse call relay is not active.
If a disconnect INOP is present and alarms are paused or switched off, the measurement in question is
switched off.
43
Page 62

3Alarms Alarm Limits
Restarting Paused Alarms
♦ To manually switch on alarm indication again after a pause, select the permanent key
Pause Alarms (or Alarms Off ) again.
Alarm indication starts again automatically after the pause period expires. If the monitor is configured
to stay paused infinitely, you must select Alarms Off again to restart alarm indication.
Resetting Arrhythmia Alarm Timeouts
♦ To reset the arrhythmia alarm timeout period, select the Alarms Off or Pause Alarms
permanent key and then reselect it.
Extending the Alarm Pause Time
If your monitor has extended alarm pause enabled, you can extend the alarm pause time. Use this to
prevent alarms being indicated, for example, while you are washing a patient or carrying out a
procedure. Only extend the alarm pause time when you are sure that clinical personnel are available to
monitor the patient’s condition closely.
To extend the alarm pause time to five or 10 minutes,
1 Select one of the alarm fields. This calls up the Alarm Messages window.
2 Select either the pop-up key Pause Al. 5 min or the pop-up key Pause Al. 10 min.
Each time you select one of these pop-up keys, the Alarm Pause Time is reset to five (or 10)
minutes.
Alarm Limits
The alarm limits you set determine the conditions that trigger yellow and red limit alarms. For some
measurements (for example, BIS and SpO
alarm limit to 100 switches the high alarm off, and setting the low alarm limit to 0 switches it off. In
these cases, the alarms off symbol is not displayed.
WARNING Be aware that the monitors in your care area may each have different alarm settings, to suit different
patients. Always check that the alarm settings are appropriate for your patient before you start
monitoring.
Viewing Individual Alarm Limits
HR
120
85
50
Alarm limits
You can usually see the alarm limits set for each measurement next to the
measurement numeric on the main screen.
If your monitor is not configured to show the alarm limits next to the numeric,
you can see them in the appropriate measurement setup menu. Select the
measurement numeric to enter the menu and check the limits.
), where the value ranges from 100 to 0, setting the high
2
44
Page 63

Alarm Limits 3Alarms
Viewing All Alarm Limits
The Alarm Limits overview window lists the currently set alarm limits for all measurements. If an
Apnea alarm delay time is set, this is also shown. The Alarms Off symbol is shown beside the
measurement label of any measurement whose alarm switched off.
To open the Alarm Limits window, either select any alarm field to open the Alarm
Messages window, then select the Alarm Limits pop-up key, or select the Alarm
Limits SmartKey, if configured.
Alarm Limits
ST-V4
ST-V5
ST-V6
SpO2
Pulse (SpO2)
NBPs
Graphic view of current
yellow and red alarm
limits and currently
monitored measurement
value
Off indicates the
measurement is switched
off
ABPs
PAPd
awRR
Apnea Time
Measurement labels, with alarms
off symbol where appropriate
♦ Select Show ST Limits to expand the list of ST leads and view the currently set alarm limits.
Off
sec
Current alarm limits
Selecting Hide ST Limits hides the list again.
You can use the pop-up keys that open with the Alarm Limits window to perform common tasks:
– All Al. On/All Al. Off,
– All Lim. Narrow/All Lim. Wide to set narrow or wide alarm AutoLimits for all
measurements.
– Print Limits/Record Limits to print a list of all current alarm limit settings on a
connected printer or recorder.
45
Page 64

3Alarms Alarm Limits
These pop-up keys are not available in the window for changing individual alarm limits which you
access by selecting the measurement label in the Alarm Limits window.
Changing Alarm Limits
To change individual measurement alarm limits using the measurement’s Setup Menu,
1 in the measurement’s setup menu, select the alarm limit you want to change. This calls up a list of
available values for the alarm limit.
2 Select a value from the list to adjust the alarm limit.
Alternatively, you can use the keys in the measurement Change Limits window, which you access by
selecting the measurement label in the Alarm Limits window.
High red alarm (view only)
HR
Alarms
On/Off
High yellow alarm field
Up/down arrow keys for
changing high yellow alarm
limits
Alarms On/Off key - select to
toggle between alarms on or off
Preview Alarm AutoLimits for a
measurement before applying
Select to apply wide AutoLimits
Select to apply narrow
AutoLimits
Up/down arrow keys for
changing low yellow alarm limits
46
15-min trend, showing alarm
limits and monitored
measurement values
(MP40/50/60/70/90 only)
Graphic view of alarm limits
with currently measured value
Low red alarm (view only)
Low yellow alarm field
To change alarm limits,
1 In the Change Limits window,
– if you are using touch, select the up or down arrow buttons to adjust the high and low alarm
limits as required.
– if you are using a SpeedPoint or Navigation Point, position the cursor in the high yellow alarm
field, then press the knob inwards. Rotate the knob to the left or right to adjust the limit. Press
the knob again to set the displayed limit.
2 Repeat to set the low yellow alarm limit.
Page 65

Alarm Limits 3Alarms
If you set the yellow alarm limit outside the red alarm limit, the monitor will automatically set the red
alarm to the yellow alarm limit.
When an ST measurement is in the Change Limits window there are also two pop-up keys
available labeled All ST Narrow/All ST Wide. With these keys you can set Auto Limits for all
ST Leads.
About Automatic Alarm Limits (AutoLimits)
The monitor can automatically set alarm limits suited to your individual patient, using the Automatic
Alarm Limits function. This tells the monitor to adapt the alarm limits of selected measurements to the
measured vital signs within a defined safe limit. The monitor calculates safe AutoLimits for each
patient based on the measured values from the last 12 seconds.
The defined safe limits never exceed the non-pathological range.
Limits Narrow sets limits close to the currently measured values for situations where it is critical
for you to be informed about small changes in your patient’s vital signs.
Limits Wide sets limits further away from the currently measured values for situations where small
changes are not so critical.
♦ Use the keys in the Change Limits window to apply AutoLimits for individual measurements.
These keys are not available if AutoLimits have been disabled for the measurement in the monitor’s
Configuration Mode.
Alarm
limits
AutoLimits are not available for all measurements. The list of measurements for which AutoLimits can
be used is defined in the monitor’s Configuration mode.
Use the Change Limits window to check AutoLimits before you apply them to ensure that they are
appropriate for your individual patient and their clinical condition. Once applied, AutoLimits are
shown on the monitor screen just like manually-set alarm limits. If the AutoLimits are not appropriate
for your patient, you must set alarm limits manually. The limits remain unchanged until you set them
again or change them manually.
Documenting Alarm Limits
The alarm limits pop-up keys appear with the Alarm Limits and Change Limits windows.
Lower limit
clamps
Upper limit
clamps
High alarm limit, wide
High alarm limit, narrow
Low alarm limit, narrow
Low alarm limit, wide
Measurement value
♦ Select the Print Limits pop-up key to print an overview of all alarm limits on a connected
printer.
♦ Select the Record Limits pop-up key to send a recording of the alarm limits to a recorder.
47
Page 66

3Alarms Reviewing Alarms
Reviewing Alarms
To review the currently active alarms and INOPs, select any of the alarm status areas on the monitor
screen. The Alarm Messages window pops up. All alarms and INOPs are erased from the
monitor’s alarm history when you discharge a patient, or if you change to Demonstration Mode.
Alarm Messages Window
The Alarm Messages window shows all the currently active alarms and INOPs in chronological
order, beginning at the top with the most recent. INOPs are shown on the left hand side and patient
alarms are shown on the right hand side. Any active red alarms are shown first, followed by yellow
alarms. Acknowledged alarms or INOPs are shown with the check mark symbol.
The Alarm Messages window pop-up keys appear when the window is opened. If alarm pause
extension is disabled, the pause pop-up keys are inactive (“grayed-out”). Selecting the Review
Alarms pop-up key opens the Review Alarms window.
Alarm
Limits
Review Alarms Window
The Review Alarms window
contains a list of up to 100 of the most
recent alarms and INOPs with date and
time information. If configured to do so ,
each alarm is shown with the alarm limit
active when the alarm was triggered and
the maximum value measured beyond
this limit. The Review Alarms
window also shows any changes made to
the Alarms On/Off or Silence status.
If you select a high or low limit alarm in
the list, the Graphical Trends
window will open to provide further
data. If you select an alarm resulting
from an event alarm notification, the Event Episode window for that event will open. When you
close these windows you will return to the Review Alarms window.
The information in the Review Alarms window is deleted when a patient is discharged, when the
monitor is switched off for longer than one minute, and when you leave Demonstration Mode.
Review
Alarms
Pause Al.
5 Min.
Review Alarms
5 Apr 16:55:18 *** Apnea
5 Apr 16:55:18 ** ABPs HIGH (120 >95)
5 Apr 16:55:18 Alarms On
5 Apr 16:45:15 ** SpO2 NON-PULSAT.
5 Apr 16:44:57 Alarms Off
5 Apr 16:44:46 ** awRR LOW (14<15)
5 Apr 16:44:39 ** SpO2 LOW (95<99)
5 Apr 16:44:28 ** ABPs HIGH
Pause Al.
10 Min.
48
The Review Alarms window pop-up keys appear when the window is opened. If alarm pause
extension is disabled, the pause pop-up keys are inactive. Selecting the Active Alarms pop-up key
opens the Alarm Messages window.
Alarm
Limits
Active
Alarms
Pause Al.
5 Min.
Pause Al.
10 Min.
Page 67

Understanding Alarm Messages 3Alarms
Understanding Alarm Messages
If you do not immediately understand an INOP or alarm message, refer to its help text.
♦ In the Alarm Messages window, select the INOP message. This calls up a help window with
an explanation of the INOP message and, where appropriate, a suggested solution for the problem.
Alarm Messages
Resp LEADS OFF
LL LEAD OFF
** awRR LOW
The lead LL has become detached from the
patient or the lead set has been changed.
Attach the missing electrode or select <New
Lead Setup> to confirm the new lead set
Latching Alarms
The alarm latching setting for your monitor defines how the alarm indicators behave when you do not
acknowledge them. When alarms are set to non-latching, their indicators end when the alarm
condition ends. Switching alarm latching on means that visual and/or audible alarm indications are still
displayed or announced by the monitor after the alarm condition ends. The indication lasts until you
acknowledge the alarm.
Viewing the Alarm Latching Settings
To see the alarm latching setting for your monitor
1 In the monitor’s Main Setup menu, select Alarms.
2 Select Alarm Settings, and see the Visual Latching and Audible Latching
settings.
This setting can only be changed in Configuration Mode. You should be aware of the settings chosen
for your unit. There are three possible choices each for visual and audible latching, Red, Red and
Yellow, and Off. These choices can be combined to give the following settings:
Visual Latching
Audible latching
R = red alarms, Y = yellow alarms
R&Y R&Y R&Y RROff
R&Y ROffROffOff
49
Page 68

3Alarms Testing Alarms
Alarm Latching Behavior
Red and Yellow Measurement
Alarms
Alarm has not been
acknowledged.
Alarm has been
acknowledged.
Alarm condition
still present.
Alarm condition
no longer present.
Alarm condition
still present.
Alarm condition
no longer present.
Non-latching
alarms
Alarm tone on. Alarm lamp on. Alarm message. Flashing numerics.
All audible and visual
alarm indicators
automatically stop.
Audible alarm acknowledged. Alarm lamp off. Alarm message. Flashing
numerics. Audible alarm reminder (if configured).
Audible and visual alarm indicators automatically stop.
Visual and audible
latching
Alarm tone on.
Alarm lamp on.
Alarm message.
Flashing numerics.
All INOPs except DISCONNECT and UNPLUGGED INOPs from measurement servers and modules
are non-latching. See “Yellow Arrhythmia Alarms” on page 111 for information on short yellow
arrhythmia alarms latching behavior.
Silencing Latched Alarms from an Information Center
Alarms set to visual latching only cannot be silenced at an Information Center. If you need to be able
to silence bedside monitor alarms at an Information Center, you must make sure that the configured
latching settings include an audible element.
Visual latching,
audible non-latching
Alarm message. Flashing
numerics.
Audible alarm indicators
automatically stop.
Testing Alarms
When you switch the monitor on, a selftest is started. You must check that the alarms lamps light, one
after the other, and that you hear a single tone. This indicates that the visible and audible alarm
indicators are functioning correctly.
Alarm Behavior at On/Off
When you switch alarms on, the settings defined in the currently active Profile are used.
If the monitor is switched off for longer than one minute and then switched on again, or after a loss of
power lasting longer than one minute, or when a patient is discharged, the monitor can be configured
to restore either the alarm settings from the monitor's configured default Profile, or the most recently
used alarm settings. After any of these situations, you should check that the alarm settings are
appropriate for your patient, and if necessary, select the correct Profile and patient category.
If power is lost for less than one minute, the alarm settings prior to the power loss are restored.
50
Page 69

4Patient Alarms and INOPs
This chapter lists patient alarms and technical alarms (INOPs) alphabetically, irrespective of their
priority. INOPs start on page 57.
For information on alarms and INOPs from the gas modules see the Essential Gas Module and
Anesthetic Gas Module Instructions for Use.
Patient Alarm Messages
The measurement labels and abbreviations for pressure, temperature, SpO2, and anesthetic agent
alarms are explained in the individual chapters.
Some alarms may be shown at the Information Center in shortened form, when transferred through
IntelliVue Instrument Telemetry (USA only). These shortened alarm texts are included in the list and
identified with the note “at Information Center”.
4
Note that yellow arrhythmia alarms (“short yellow alarms”) may be shown with one or with two stars,
depending on your monitor configuration and the Information Center revision you are using.
See the Essential Gas Module and Anesthetic Gas Module Instructions for Use for patient alarms and
INOPs from the gas modules.
Alarm Message From Condition Indication
***APNEA or
***APNEA xxx sec
***ASYSTOLE ECG No QRS detected for a period greater
**awRR HIGH CO2, Resp,
**awRR LOW CO2, Resp,
**BIS HIGH BIS The Bispectral Index value has exceeded
**BIS LOW BIS The Bispectral Index value has dropped
CO2, Resp,
AGM
AGM
AGM
Respiration has stopped for longer than
the preset apnea time. “xxx” denotes the
Apnea duration.
than the asystole threshold (in the
absence of Vfib or chaotic ECG).
The airway respiration rate has exceeded
the high alarm limit.
The airway respiration rate has dropped
below the low alarm limit.
the high alarm limit.
below the low alarm limit.
numeric flashes, red alarm
lamp, alarm tone.
numeric flashes, red alarm
lamp, alarm tone.
numeric flashes and high limit
is highlighted, yellow alarm
lamp, alarm tone.
numeric flashes and low limit
is highlighted, yellow alarm
lamp, alarm tone.
numeric flashes and high limit
is highlighted, yellow alarm
lamp, alarm tone.
numeric flashes and low limit
is highlighted, yellow alarm
lamp, alarm tone.
51
Page 70

4 Patient Alarms and INOPs Patient Alarm Messages
Alarm Message From Condition Indication
***BRADY (Pulse)
or
***BRADY xxx<yyy
**CCO/CCI HIGH CCO Continuous Cardiac Output or CC
**CCO/CCI LOW CCO Continuous Cardiac Output or CC
**CPP HIGH CPP The CPP value has exceeded the high
**CPP LOW CPP The CPP value has fallen below the low
***DESAT or
***DESAT xxx<yyy
**et <Agent label>
HIGH
**et <Agent label>
LOW
**etCO2 HIGH CO2, Resp,
**etCO2 LOW CO2, Resp,
**etO2 HIGH O2, AGM The end tidal O2 high alarm limit has
**etO2 LOW O2, AGM The end tidal O2 value has fallen below
*/**/***
EVENT:<GRP>
*/**/*** EVENT
at Information center
***EXTREME BRADY ECG The bradycardia limit has been
***EXTREME TACHY ECG The tachycardia limit has been
Press, SpO2The heart rate from the Pulse signal has
fallen below the bradycardia limit. xxx
denotes the lowest measured value; yyy
is the bradycardia limit.
Index is above the high alarm limit.
Index is below the low alarm limit.
alarm limit.
alarm limit.
SpO
2
AGM The end tidal agent high alarm limit has
AGM The end tidal agent value has fallen
AGM
AGM
Event
surveillance
Event
surveillance
The SpO2 value has fallen below the
desaturation alarm limit. xxx denotes
the lowest measured value, and yyy is
the desaturation limit.
been exceeded.
below the low alarm limit.
The end tidal CO2 high alarm limit has
been exceeded.
The end tidal CO2 value has fallen
below the low alarm limit.
been exceeded.
the low alarm limit.
An event has occurred and the event
notification is configured to alarm.
<GRP> is the event group
An event has occurred and the event
notification is configured to alarm.
Check on the monitor for more details
on event group.
exceeded.
exceeded.
numeric flashes and alarm
limit is highlighted, red alarm
lamp, alarm tone.
numeric flashes and high alarm
limit is highlighted, yellow
alarm lamp, alarm tone.
numeric flashes and low alarm
limit is highlighted, yellow
alarm lamp, alarm tone.
numeric flashes and high limit
is highlighted, yellow alarm
lamp, alarm tone
numeric flashes and low limit
is highlighted, yellow alarm
lamp, alarm tone.
numeric flashes, red alarm
lamp, alarm tone.
numeric flashes and high limit
is highlighted, yellow alarm
lamp, alarm tone.
numeric flashes and low alarm
limit is highlighted, yellow
alarm lamp, alarm tone.
numeric flashes and high limit
is highlighted, yellow alarm
lamp, alarm tone.
numeric flashes and low limit
is highlighted, yellow alarm
lamp, alarm tone.
numeric flashes and high limit
is highlighted, yellow alarm
lamp, alarm tone.
numeric flashes, and low limit
is highlighted, yellow alarm
lamp, alarm tone.
event group name flashes,
yellow or red alarm lamp and
alarm tone
(on monitor) event group
name flashes, yellow or red
alarm lamp and alarm tone
numeric flashes and alarm
limit is highlighted, red alarm
lamp, alarm tone.
numeric flashes and alarm
limit is highlighted, red alarm
lamp, alarm tone.
52
Page 71

Patient Alarm Messages 4 Patient Alarms and INOPs
Alarm Message From Condition Indication
**HR HIGH ECG The heart rate high alarm limit has been
exceeded.
**HR LOW ECG The heart rate has fallen below the low
alarm limit.
**imCO2 HIGH CO2, Resp,
AGM
**in <Agent label>
HIGH
**in <Agent label>
LOW
**inN2O HIGH N2O, AGM The inspired N2O high alarm limit has
**inO2 HIGH O2, AGM The inspired O2 high alarm limit has
**inO2 LOW O2, AGM The inspired O2 value has fallen below
***inO2 LOW OXYGEN O2, AGM The inspired O2 value has fallen below
*/**IRREGULAR HR ECG/
*/**MISSED BEAT ECG/
*/**MULTIFORM PVCs ECG/
**NBP HIGH NBP The measured NBP value is above the
**NBP LOW NBP The measured NBP value is below the
AGM The inspired agent high alarm limit has
AGM The inspired agent value has fallen
Arrhythmia
Arrhythmia
Arrhythmia
The inspired minimum CO2 high alarm
limit has been exceeded.
been exceeded.
below the AGT low alarm limit.
been exceeded.
been exceeded.
the low alarm limit.
18 vol.%.
Consistently irregular heart rhythm. numeric flashes, yellow alarm
No beat detected for 1.75*R-R interval,
or if HR>120bpm no beat detected for
one second (non-paced patients only).
Two differently shaped Vs detected,
each occurring at least twice within the
last 300 beats and at least once within
the last 60 beats.
high alarm limit.
s, d, or m after the label indicates
whether the systolic, diastolic or mean
pressure has crossed the limit.
low alarm limit.
s, d, or m after the label indicates
whether the systolic, diastolic or mean
pressure has crossed the limit.
numeric flashes and high limit
is highlighted, yellow alarm
lamp, alarm tone. The sound
switches off after 5 seconds if
Arrhythmia is On.
numeric flashes and low limit
is highlighted, yellow alarm
lamp, alarm tone. The sound
switches off after 5 seconds if
Arrhythmia is On.
numeric flashes and high limit
is highlighted, yellow alarm
lamp, alarm tone.
numeric flashes, high limit is
highlighted, yellow alarm
lamp, alarm tone.
numeric flashes, low limit is
highlighted, yellow alarm
lamp, alarm tone.
numeric flashes, high limit is
highlighted, yellow alarm
lamp, alarm tone.
numeric flashes, high limit is
highlighted, yellow alarm
lamp, alarm tone.
numeric flashes, low limit is
highlighted, yellow alarm
lamp, alarm tone.
numeric flashes, low limit is
highlighted, red alarm lamp,
alarm tone.
lamp, short yellow audible
alarm.
numeric flashes, yellow alarm
lamp, short yellow audible
alarm.
numeric flashes, yellow alarm
lamp, short yellow audible
alarm.
numeric flashes and high limit
is highlighted, yellow alarm
lamp, alarm tone.
numeric flashes and low limit
is highlighted, yellow alarm
lamp, alarm tone.
53
Page 72

4 Patient Alarms and INOPs Patient Alarm Messages
Alarm Message From Condition Indication
*/**NON-SUSTAIN VT ECG/
Arrhythmia
A run of Vs having a ventricular HR>VTach HR limit, but lasting for less than
the V-Tach Run limit has been
detected.
*/**PACER NOT CAPT ECG/
Arrhythmia
A missed beat with a pace pulse was
detected.
(paced
patients only)
*/**PACER NT
PACING
ECG/
Arrhythmia
A missed beat without a pace pulse was
detected.
(paced
patients only)
*/**PAIR PVCs ECG/
Arrhythmia
A non-ventricular contraction, followed
by two ventricular contractions,
followed by a non-ventricular
contraction has been detected.
*/**PAUSE ECG/
Arrhythmia
***<Pressure>
PRESS The pressure is non-pulsatile and the
DISCONNECT
No beat detected for a period greater
than the pause threshold.
mean pressure is continuously less than
10mmHg (1.3kPa). This alarm occurs
only with arterial pressures (P, ABP,
ART, Ao, BAP, FAP, PAP, UAP).
**<Pressure> HIGH PRESS The measured pressure value is above
the high alarm limit. s, d, or m after the
label indicates whether the systolic,
diastolic or mean pressure has crossed
the limit.
**<Pressure> LOW PRESS The measured pressure value is below
the low alarm limit. s, d, or m after the
label indicates whether the systolic,
diastolic or mean pressure has crossed
the limit.
**PULSE HIGH PRESS
SpO
2
**PULSE LOW PRESS
SpO
2
*/**PVCs/min HIGH ECG/
Arrhythmia
The pulse rate has exceeded the high
alarm limit.
The pulse rate has dropped below the
low alarm limit.
More premature ventricular
contractions have been detected in a
minute than the limit.
*/**R-ON-T PVCs ECG/
Arrhythmia
For HR <100, a PVC with R-R interval
< 1/3 the average interval followed by a
compensatory pause of 1.25 x average
R-R interval or two such Vs without
compensatory pause occurring within 5
minutes of each other. (When HR
>100, 1/3 R-R interval is too short for
detection.).
numeric flashes, yellow alarm
lamp, short yellow audible
alarm.
numeric flashes, yellow alarm
lamp, short yellow audible
alarm.
numeric flashes, yellow alarm
lamp, short yellow audible
alarm.
numeric flashes, yellow alarm
lamp, short yellow audible
alarm.
numeric flashes, yellow alarm
lamp, short yellow audible
alarm.
numeric flashes, red alarm
lamp, alarm tone.
numeric flashes, high limit is
highlighted, yellow alarm
lamp, alarm tone.
numeric flashes and low limit
is highlighted, yellow alarm
lamp, alarm tone.
numeric flashes and high limit
is highlighted, yellow alarm
lamp, alarm tone.
numeric flashes and low limit
is highlighted, yellow alarm
lamp, alarm tone.
numeric flashes, yellow alarm
lamp, short yellow audible
alarm.
numeric flashes, yellow alarm
lamp, short yellow audible
alarm.
54
Page 73

Patient Alarm Messages 4 Patient Alarms and INOPs
Alarm Message From Condition Indication
**RR HIGH RESP The respiration rate has exceeded the
high alarm limit.
**RR LOW RESP The respiration rate has dropped below
the low alarm limit.
*/**RUN PVCs HIGH ECG/
Arrhythmia
**<SpO2 label>
SpO
HIGH
**<SpO2 label> LOW SpO
2
2
A run of PVCs greater than 2 was
detected.
The arterial oxygen saturation has
exceeded the high alarm limit.
The arterial oxygen saturation has fallen
below the low alarm limit.
**ST<n> HIGH ECG/
Arrhythmia
**ST<n> LOW ECG/
Arrhythmia
**ST MULTI <n>,<n> ECG/
Arrhythmia
The ST elevation in lead <n> is higher
than the limit.
The ST depression in lead <n> is lower
than the limit.
The ST depression or elevation is
outside of the limit in two or more leads
<n> and <n>
**ST MULTI
at Information Center
ECG/
Arrhythmia
The ST depression or elevation is
outside of the limit in two or more
leads. Check on the monitor for more
details about which leads are affected.
**SvO2 HIGH SvO
2
The SvO2 value has exceeded the high
limit.
**SvO2 LOW SvO
2
The SvO2 value has fallen below the low
limit.
*/**SVT ECG/
Arrhythmia
A run of supraventricular beats greater
than the SVT run limit has been
detected and the HR has exceeded the
SVT HR limit.
***TACHY (Pulse)
or
***TACHY xxx>yyy
Press, SpO2The heart rate from the Pulse signal has
exceeded the tachycardia limit. xxx
denotes the highest measured value; yyy
is the tachycardia limit.
**Tblood HIGH C.O. The blood temperature value has
exceeded the high alarm limit.
**Tblood LOW C.O. The blood temperature value has fallen
below the low alarm limit.
**tcpO2 HIGH/
**tcpCO2 HIGH
tcGas The tcpO2 or tcpCO2 value has
exceeded the high alarm limit.
numeric flashes and high limit
is highlighted, yellow alarm
lamp, alarm tone.
numeric flashes and low limit
is highlighted, yellow alarm
lamp, alarm tone.
numeric flashes, yellow alarm
lamp, short yellow audible
alarm.
numeric flashes and high limit
is highlighted, yellow alarm
lamp, alarm tone.
numeric flashes and low limit
is highlighted, yellow alarm
lamp, alarm tone.
numeric flashes and high alarm
limit is highlighted, yellow
alarm lamp, alarm tone.
numeric flashes and low alarm
limit is highlighted, yellow
alarm lamp, alarm tone.
numeric flashes, yellow alarm
lamp, alarm tone
(on monitor) numeric flashes,
yellow alarm lamp, alarm tone
numeric flashes and high alarm
limit is highlighted, yellow
alarm lamp, alarm tone.
numeric flashes and low alarm
limit is highlighted, yellow
alarm lamp, alarm tone.
numeric flashes, yellow alarm
lamp, alarm tone.
numeric flashes, alarm limit is
highlighted, red alarm lamp,
alarm tone.
numeric flashes, high alarm
limit is highlighted, yellow
alarm lamp, alarm tone.
numeric flashes, low alarm
limit is highlighted, yellow
alarm lamp, alarm tone.
numeric flashes, high alarm
limit is highlighted, yellow
alarm lamp, alarm tone.
55
Page 74

4 Patient Alarms and INOPs Patient Alarm Messages
Alarm Message From Condition Indication
**tcpO2 LOW/
**tcpCO2 LOW
**<Temperature
label> HIGH
**<Temperature
label> LOW
*/**VENT BIGEMINY ECG/
***VENT FIB/TACH ECG A fibrillatory waveform for 4
*/**VENT RHYTHM ECG/
*/**VENT TRIGEMINY ECG/
***VTACH ECG,
**/***VueLink
ALARM
at Information Center
tcGas The tcpO2 or tcpCO2 value has fallen
below the low alarm limit.
TEMP The temperature has exceeded the high
alarm limit.
TEMP The temperature has fallen below the
low alarm limit.
A dominant rhythm of N, V, N, V (N =
Arrhythmia
Arrhythmia
Arrhythmia
Arrhythmia
VueLink A yellow (**) or red (***) patient alarm
supraventricular beat, V = ventricular
beat) was detected.
consecutive seconds was detected.
A dominant rhythm of adjacent Vs >
vent rhythm limit and ventricular HR <
VTach HR limit was detected.
A dominant rhythm of N, N, V, N, N,
V (N = supraventricular beat, V =
ventricular beat) was detected.
Ventricular tachycardia has been
detected (Consecutive PVCs exceed V-
Tach Run limit and HR exceeds V-
Tach HR limit).
is present on the VueLink module.
Check the monitor display for more
detailed alarm information.
numeric flashes, low alarm
limit is highlighted, yellow
alarm lamp, alarm tone.
numeric flashes and high limit
is highlighted, yellow alarm
lamp, alarm tone.
numeric flashes and low limit
is highlighted, yellow alarm
lamp, alarm tone.
numeric flashes, yellow alarm
lamp, short yellow audible
alarm.
numeric flashes, red alarm
lamp, alarm tone.
numeric flashes, yellow alarm
lamp, short yellow audible
alarm.
numeric flashes, yellow alarm
lamp, short yellow audible
alarm.
numeric flashes, yellow alarm
lamp, short yellow audible
alarm.
(on monitor) yellow or red
alarm lamp, alarm tone
56
Page 75

Technical Alarm Messages (INOPs) 4 Patient Alarms and INOPs
Technical Alarm Messages (INOPs)
The measurement labels and abbreviations for pressure, temperature, SpO2, anesthetic agent, and
VueLink INOP messages are explained in the individual chapters.
INOP Message, Indication Source What to do
ABP INOPS PRESS See <Pressure label> INOPS (under Pressure).
ALL ECG ALARMS OFF ECG/
Arrhythmia
Ao INOPS PRESS See <Pressure label> INOPS (under Pressure).
ART INOPS PRESS See <Pressure label> INOPS (under Pressure).
Bad Serverlink
INOP tone
BAP INOPS PRESS See <Pressure label> INOPS (under Pressure).
BATTERIES EMPTY or BATT 1/
BATT 2 EMPTY
INOP tone, battery LED flashes
During this INOP, alarms cannot be
paused or switched off.
BATTERIES INCOMPAT or BATT
1/BATT 2 INCOMPAT
INOP tone
BATTERIES LOW or BATT 1/
BATT 2 LOW
INOP tone
BATTERIES MALF or BATT 1/
BATT 2 MALFUNCTION
INOP tone, battery LED flashes
During this INOP, alarms cannot be
paused or switched off unless the
monitor is connected to mains power.
BATT 1/BATT 2 MISSING
INOP tone.
During this INOP, alarms cannot be
paused or switched off.
BIS CABLE INCOMPAT
INOP tone.
BIS CABLE USAGE
INOP tone.
Monitor 1) An MMS with an incompatible software revision is
Batteries The estimated remaining battery-powered operating time of
Batteries The indicated battery or batteries cannot be used with this
Batteries The estimated battery-powered operating time remaining is less
Batteries The monitor cannot determine the battery status. If this INOP
Batteries The monitor requires two batteries but can detect only one
BIS The semi-reusable sensor cable connected is unknown or not
BIS The semi-reusable sensor cable has exceeded the maximum
All ECG alarms have been switched off, or the HR alarm
source is not ECG. To resume ECG alarm generation, switch
ECG alarms on or select ECG as the alarms source.
connected to the monitor. This combination does not allow
monitoring, OR
2) You cannot use this combination of monitor, MMS and
cable. Switch off the monitor and contact your service
personnel.
the indicated battery or batteries is less than 10 minutes.
Replace the batteries immediately.
If the condition persists and the monitor is not connected to
mains power, this INOP is re-issued two minutes after you
acknowledge it.
monitor. Replace with the correct batteries
than 20 minutes.
persists, replace the faulty battery or batteries. If the condition
persists and the monitor is not connected to mains power, this
INOP is re-issued two minutes after you acknowledge it.
Place the batteries in a different monitor or in a battery charger.
If the same INOP is shown, contact your service personnel.
battery. Insert the missing battery immediately.
supported by your software revision. Replace it with a Philipssupported sensor cable.
number of uses. Replace the cable.
(M4605A).
57
Page 76

4 Patient Alarms and INOPs Technical Alarm Messages (INOPs)
INOP Message, Indication Source What to do
BIS DSC DISCONN
INOP tone
BIS DSC INCOMPT
INOP tone
BIS DSC MALFUNC BIS Electrocautery used during self-test OR malfunction in the
BIS DSC UPDATE
INOP tone
BIS ELECTR. DISC
INOP tone.
BIS ENGINE DISC.
INOP tone
BIS ENGINE INCOMPT
INOP tone
BIS ENGINE MALFUNC
INOP tone
BIS EQUIP MALF
INOP tone
BIS HIGH IMPEDANCE
INOP tone may sound
BIS IMPEDANCE CHCK
INOP tone may sound
BIS DSC is not properly connected OR either DSC or BIS engine
may be faulty.
Make sure that the DSC is properly connected to the BIS
Engine. If INOP persists, replace DSC with a known good one
of the same type.
If INOP persists replace BIS engine.
Silencing this INOP switches the measurement off.
BIS DSC is not supported by the BIS engine or new DSC
connected to an old BIS engine. A software upgrade may be
required. Contact your service personnel.
DSC hardware.
Make sure not to use electrocautery during the self-test
procedure. Disconnect and reconnect the DSC to the BIS
engine. If the INOP persists, replace the DSC or contact your
service personnel.
BIS DSC update currently being carried out. This INOP will
disappear when the DSC update is finished. Do not disconnect
the DSC during the update. No action is needed.
BIS One or more electrodes are not connected to the semi-reusable
sensor cable. Check all electrode connections.
BIS BIS engine not connected OR Module Cable defective.
Make sure that the Module Cable is properly connected. If
INOP persists, replace the Module Cable.
Silencing this INOP switches the measurement off.
BIS BIS engine software is not supported. A software upgrade may
be required. Contact your service personnel.
MP20/30 - BIS engine not supported.
BIS Malfunction in the BIS engine hardware. Disconnect and
reconnect the BIS engine. If the INOP persists, replace BIS
engine.
BIS There is a malfunction in the BIS hardware. Unplug and replug
the BIS module. If the INOP persists, contact your service
personnel.
BIS Impedance of one or more electrode(s) is above the valid range,
most often caused by bad skin preparation. Check the sensor
montage and press the electrode pads firmly. If this INOP
persists, replace the sensor(s) in question using correct skin
preparation.
If INOP persists, contact your service personnel.
BIS The Cyclic Impedance check is running. It will stop
automatically if all impedances are within the valid range. If
any electrodes do not pass the impedance test, check the sensor
montage and press the electrode pads firmly.
To manually stop the Cyclic Impedance Check, select
Cyclic Check Off in the Setup BIS menu.
BIS ISOELECTRC EEG BIS No discernible EEG activity is detected for longer than one
minute.
Check the patient. Check that the electrodes are properly
connected.
58
Page 77

Technical Alarm Messages (INOPs) 4 Patient Alarms and INOPs
INOP Message, Indication Source What to do
BIS LEAD OFF
INOP tone may sound
BIS OVERCURRENT
INOP tone
BIS SENSOR DISCONN
INOP tone
BIS SENSOR INCOMPAT
INOP tone
BIS SENSOR MALFUNC
INOP tone
BIS SENSOR USAGE
INOP tone
BIS SQI < 15% (INOP tone)
OR
BIS SQI < 50% (no INOP tone)
BIS UNPLUGGED
INOP tone
BISx DISCONNECTED
INOP tone
BISx INCOMPATIBLE
INOP tone
BIS One or more electrodes have no skin contact and therefore
impedances cannot be measured. Check the sensor montage
and press the electrode pads firmly.
If this INOP persists, replace the sensor(s) in question, using
correct skin preparation.
BIS Unplug and replug the BIS module or, f or the MP20/MP30,
disconnect and reconnect the BISx from the Interface board. If
the INOP persists, contact your service personnel.
BIS The sensor is not properly connected to the patient interface
cable (PIC) and/or the PIC is not properly connected to the
DSC or BISx, or the sensor or PIC or DSC or BISx may be
faulty.
Check all the connections.
Disconnect and reconnect the sensor, PIC, DSC, BISx.
If the INOP persists, replace the sensor.
If the INOP persists, replace PIC. If INOP persists, contact
your service personnel.
Silencing this INOP switches the measurement off.
BIS Unsupported sensor connected or sensor type unknown or not
supported by your software revision. Replace the sensor, using
only Philips supported sensors.
BIS Malfunction in the sensor hardware, most often caused by
liquids permeating into the connectors OR patient interface
cable (PIC) or DSC or BISx may be faulty.
Replace the sensor. Manually initiate a Cyclic Impedance
Check. Make sure all electrodes pass the test. Make sure that
the both sides of the PIC connector (between PIC and sensor)
are dry. If you are not sure that the connector is dry, replace the
PIC until it has dried. If this INOP persists, contact your
service personnel.
BIS Excessive sensor usage. Replace sensor.
A Cyclic Impedance Check will start automatically.
BIS If the signal quality is below 50%, BIS numerics cannot be
reliably derived.
If the signal quality is below 15%, no BIS numerics can be
derived.
This may occur as a result of artifacts such as those generated
from motion or the presence of electrocautery devices. Make
sure the sensor is properly attached to the patient. Manually
initiate a Cyclic Impedance Check. Make sure all electrodes
pass the test. Make sure the patient is completely relaxed (even
small motions of the facial muscles affect the signal quality).
BIS Plug in the BIS module. Silencing this INOP switches off the
measurement.
BIS The BISx is not connected to the BIS module or the BIS
interface board. Silencing this INOP switches the measurement
off.
BIS The BISx software is not compatible with the BIS module or
with the MP20/MP30 monitor software. A software upgrade
may be required. Contact your service personnel.
59
Page 78

4 Patient Alarms and INOPs Technical Alarm Messages (INOPs)
INOP Message, Indication Source What to do
BISx MALFUNCTION
INOP tone
CANNOT ANALYZE ECG ECG/
CANNOT ANALYZE ST ST The ST algorithm cannot generate a valid ST value. Possible
CCI NO BSA
CCI numeric unavailable
INOP tone
CCO BAD PRESS SIGN
numeric displays -?INOP tone
CCO NO <Pressure label>
numeric displays -?INOP tone may sound
CCO NO CALIBRATION
numeric displays -?-
CCO NO PRESS
at Information Center
CCO NOT SUPPORTED
numeric displays -?INOP tone
CCO/CCI OVERRANGE
numeric displays -?INOP tone
CCO <Pressure label>
INVALID
numeric displays -?INOP tone may sound
BIS The BISx is faulty. Disconnect and reconnect it to the module
or BIS interface board. If the INOP persists, replace the BISx.
MP20/MP30 - Malfunction on interface board. If the INOP
persists, contact your service personnel.
The arrhythmia algorithm cannot reliably analyze the ECG
Arrhythmia
C.O. CCI cannot be calculated because the patient's body surface
C.O. The arterial pressure wave can currently not be used for pulse
C.O. CCO/CCI cannot be calculated. Make sure that the pressure
C.O. The CCO measurement is currently not calibrated.
C.O. CCO/CCI cannot be calculated. Make sure that the pressure
C.O. A catheter for transpulmonary C.O. measurements has been
C.O. The measured CCO or CCI value is not within the specified
C.O. The arterial pressure selected for pulse contour calculation for
data. Check the ECG signal quality of the selected primary and
secondary leads. If necessary, improve lead position or reduce
patient motion.
If you have arrhythmia analysis on, and you are not getting a
reliable HR because the signal is below a minimum amplitude,
unstable, or contains artifact, and you have tried to improve the
system performance by choosing another lead and changing
electrodes, you should consider turning arrhythmia analysis off.
causes are large variations in the measured ST values for
consecutive beats, or ventricular paced beats. Review the ECG
signal quality and the ST measurement points.
If the patient has a ventricular pacemaker, ST analysis is not
possible.
area is unknown. Enter the patient weight and height to
provide the BSA for CCI calculation.
contour calculation for CCO or CCI measurement. Possible
causes are air bubbles in the tubing or a physiological
condition, for example severe arrhythmia.
chosen in the
matches the pressure measured with the arterial catheter for
CCO measurement. A VueLink pressure cannot be used. Select
another pressure label, either ABP, Ao, ART, BAP, FAP, or
UAP.
chosen in the
matches the pressure measured with the arterial catheter for
CCO measurement. A VueLink pressure cannot be used. Select
another pressure label, either ABP, Ao, ART, BAP, FAP, or
UAP.
unplugged and replaced with a Right Heart C.O. catheter, or
the measurement mode has been changed manually. Silencing
this INOP switches the measurement off.
range for CCO/CCI measurement.
CCO is available but currently invalid. Make sure the pressure
transducer is connected and the zero calibration is valid.
Setup CCO menu under CCO From
Setup CCO menu under CCO From
60
Page 79

Technical Alarm Messages (INOPs) 4 Patient Alarms and INOPs
INOP Message, Indication Source What to do
CCO PRESS INVALID
at Information Center
CCO PRESS OVERRANG
numeric displays -?INOP tone
CCO PULSE OVERRANG
numeric displays -?INOP tone
CCO/Tbl NO TRANSD
Numeric displays -?INOP tone
CCO RECALIBRATE
numeric displays -?-
Charge BATT1/BATT2 now
INOP tone
CHARGER MALFUNCT
INOP tone, battery LED may flash
Check Alarm Lamps
INOP tone.
CHECK BATT TEMP
INOP tone
Check Flex Texts
INOP tone
CheckInternVoltage
INOP tone.
Check Keyboard
INOP tone
Check Main Board 2
INOP tone.
Check Monitor Temp
INOP tone
Check Mouse Device
INOP tone.
Check MSL Voltage
INOP tone
Check Network Conf
INOP tone
C.O. The arterial pressure selected for pulse contour calculation for
CCO is available but currently invalid. Make sure the pressure
transducer is connected and the zero calibration is valid.
C.O. The mean value of the arterial pressure values used for pulse
contour calculation for CCO is below 0 mmHg or above 300
mmHg.
C.O. The pulse rate of the pressure used for pulse contour
calculation for CCO is below 30 bpm or above 240 bpm.
C.O. No transducer attached to the module or catheter
disconnected.
C.O. The most recent CCO or CCI calibration was made over 8
hours ago. You should recalibrate CCO or CCI with
transpulmonary C.O. measurements at least every 8 hours or
when the hemodynamic condition of the patient has changed.
Batteries Battery must be charged. Connect the monitor to mains power
or exchange the battery.
Batteries There is a problem with the battery charger in the monitor.
Connect the monitor to mains power and contact your service
personnel.
Monitor Perform a visual check of the alarm lamp to establish whether
there is a problem. Contact your service personnel to check the
internal connections to the alarm lamps.
Battery The temperature of one or both batteries is too high. Check
that ventilation openings are not blocked and monitor is not
exposed to heat.
Monitor Check the names of the monitor menus, for example the labels
for screens, profiles, event or trend group names, before you
resume monitoring. If they are unexpected, there may be a
problem with the monitor software. Contact your service
personnel.
Monitor There is a problem with the voltages (5V,12V) in the monitor.
Contact your service personnel.
Monitor Perform a visual and functional check of the keyboard. Contact
your service personnel.
Monitor There is a problem with the second main board in the monitor.
Contact your service personnel.
Monitor The temperature inside the monitor is too high. Check that the
monitor ventilation is not obstructed. If the situation
continues, contact your service personnel.
Monitor Perform a visual and functional check of the mouse input
device. Contact your service personnel.
Monitor/
Measuremt
Server
Monitor The monitor is receiving network topology information from
There is a problem with the voltage of the Measurement Server
Link (MSL). Contact your service personnel.
more than one source, e.g.the Database Server and an
Application Server. Contact your service personnel.
61
Page 80

4 Patient Alarms and INOPs Technical Alarm Messages (INOPs)
INOP Message, Indication Source What to do
Check Nurse Relay
INOP tone
Check Screen Res
INOP tone
Monitor There is a problem with the connection to the nurse relay.
Contact your service personnel.
Monitor The Screen you have selected uses a resolution which is not
supported by the display. The monitor will show a generic
Screen instead until you select a different Screen.
Contact your service personnel if you want the Screen deleted
from the Profile(s) to avoid this in future.
Check Settings
INOP tone
Monitor If this INOP appears, check the monitor and patient settings
before you resume monitoring. If the settings are unexpected,
there may be a problem with the monitor software. Contact
your service personnel.
Check Speedpoint
INOP tone.
Monitor Perform a visual and functional check of the SpeedPoint input
device. Contact your service personnel.
Check Touch Input Monitor Perform a visual and functional check of the touch input
device. Contact your service personnel.
Check Waves
INOP tone
Monitor The options purchased with this monitor may not support the
number of waves required to show the selected Screen, so some
waves or high resolution trends are missing from the Screen.
Select a different Screen with fewer waves.
Contact your service personnel if you want the Screen deleted
from the Profile(s) to avoid this in future.
C LEAD OFF
HR numeric is displayed with a -?- for
10 seconds. INOP tone.
ECG The C electrode (AAMI: V electrode) has become detached
from the patient or the lead set has been changed. Reattach the
electrode or select
New Lead Setup in the Setup ECG
menu to confirm the new lead set.
CO2 AUTO ZERO
Numeric is replaced by a - ? if the Autozero lasts >15 sec, INOP
tone sounds.
CO2 CAL MODE
numeric displays current CO2
CO
2
value for accuracy check
CO2 CAL RUNNING
CO
CO
CO
2
The automatic zero calibration is in progress. This typically
takes 10 seconds. During this time the CO
values may not be
2
updated, or they may be replaced by -?-. Wait until the zero
calibration is complete to resume monitoring.
2
Currently no calibration is running. Accuracy can be checked
by placing the transducer on the two cells of the calstick and
starting calibration. To start monitoring, leave Cal. Mode.
2
Wait until calibration is finished.
Numeric is replaced by a - ? -
CO2 CHANGE SCALE CO
2
The CO2 wave is clipped. Select a more appropriate wave scale
to display the whole wave.
CO2 CHECK ADAPTER
Numeric is replaced by a - ? INOP tone.
CO2 CHECK CAL
Numeric is replaced by a - ? INOP tone.
C.O. EQUIP MALF
Numeric is replaced by a - ? -
CO
2
Check that the sensor is connected to the airway adapter, clean
the airway adapter, if necessary. Perform a zero calibration. If
the INOP persists, contact your service personnel.
CO
2
The CO2 value is outside the measurement range. Perform an
accuracy check for both calstick cells and, if necessary,
recalibrate the transducer.
C.O. There is a problem with the C.O. hardware. Contact your
service personnel.
INOP tone.
CO2 EQUIP MALF
Numeric is replaced by - ? INOP tone.
CO
2
The Measurement Server Extension is faulty. Unplug and
replug the Measurement Server with Extension. If you are
using the mainstream method, unplug and replug the
transducer or try another transducer. If the INOP persists,
contact your service personnel.
62
Page 81

Technical Alarm Messages (INOPs) 4 Patient Alarms and INOPs
INOP Message, Indication Source What to do
CO2 FAILED CAL
CO
Numeric is replaced by -?INOP tone.
CO2 NO SENSOR
CO
Numeric is replaced by - ? INOP tone.
CO2 NO TRANSDUC
CO
Numeric is replaced by - ? INOP tone.
CO2 NO TUBING
CO
Numeric is replaced by - ? INOP tone.
CO2 OCCLUSION
CO
Numeric is replaced by a - ? INOP tone.
CO2 OVERRANGE
CO
Numeric is replaced by - ? INOP tone.
CO2 PUMP OFF
CO
Numeric is replaced by a - ? -.
CO2 PURGING
CO
Numeric is replaced by a - ? INOP tone.
CO2 SENSOR WARMUP
CO
Numeric is displayed with a - ? Microstream CO2: INOP tone.
Mainstream CO
C.O. UNPLUGGED
: no INOP tone
2
C.O. Plug in the C.O. module. Silencing this INOP switches off the
numeric displays -?INOP tone.
CO2 UPDATE FW
CO
Numeric is replaced by a - ? INOP tone.
CO2 WAIT CAL2
CO
Numeric is replaced by a - ? -
CO2 ZERO FAILED
CO
Numeric is replaced by a - ? INOP tone.
CO2 ZERO REQUIRED
CO
Numeric is replaced by a - ? INOP tione
CO2 ZERO RUNNING CO
CPP CHK SOURCES
CPP Not all measurements or values required to perform the
Numeric is replaced by a - ? -
2
Make sure that the Cal cell was changed between CAL1 and
CAL2. Repeat the calibration. If the INOP reappears, try
another transducer. If the INOP persists, contact your service
personnel.
2
2
There is no CO2 sensor connected. If you silence this INOP
the CO
measurement will be switched off.
2
There is no CO2 transducer connected. If you replace the
transducer, the new transducer must be calibrated. If you
silence this INOP the CO
2
Either the FilterLine is disconnected, or an incorrect line is
measurement will be switched off.
2
attached. Check the connection. If necessary, connect another
Microstream
Filterline (only Microstream accessories can be
used).
If you silence this INOP, the measurement will be switched off.
2
The FilterLine or exhaust tube is blocked. Check the FilterLine
and exhaust tube, then disconnect and reconnect the
FilterLine. If the INOP persists, connect a new FilterLine.
2
The CO2 value is higher than the measurement range. If you
suspect a false high value, contact your service personnel.
2
2
The pump has been switched off for fifteen minutes. To switch
it on again, select Pump On in the Setup CO
menu.
2
The Filterline is being purged to remove an occlusion in the
line or airway adapter. If the occlusion is removed, the INOP
will disappear. If not, the INOP CO2 OCCLUSION is
displayed.
2
Wait until the sensor reaches operating temperature and the
INOP disappears.
measurement.
2
The software in the Measurement Server Extension does not
match the software in the MMS. Contact your service
personnel.
2
Calibration on the first calstick cell is complete. Place the
transducer on the other calstick cell and start the CAL2
calibration cycle.
2
An error occurred during the last zero calibration. Check the
airway adapter and clean, if necessary. Perform another zero
calibration. If the INOP persists, contact your service
personnel.
2
Perform zero calibration for the CO2 sensor. If the INOP
persists, contact your service personnel.
2
Wait until zero calibration is finished.
calculation are available. Check the measurement sources.
63
Page 82

4 Patient Alarms and INOPs Technical Alarm Messages (INOPs)
INOP Message, Indication Source What to do
CPP CHK UNITS
Numeric is replaced by a - ? -
CUFF NOT DEFLATED
Numeric is displayed with a - ? INOP tone.
During this INOP, alarms cannot be
paused or switched off.
CVP INOPS PRESS See <Pressure label> INOPS (under Pressure).
ECG EQUIP MALF
Numeric is displayed with a - ? INOP tone.
<ECG LEAD> LEAD OFF
Numeric is displayed with a - ? INOP tone.
ECG EL. NOISY <ECG LEAD> ECG The ECG signal from the named ECG electrodes [RA, LA, LL,
ECG NOISY SIGN.
INOP tone.
EcgOut EQUIP MALF
INOP tone
EEG EQUIP MALFUNC
INOP tone
EEG IMPEDANCE HIGH or
EEG1 and/or EEG2 IMPED.
HIGH
EEG<X> LEAD OFF <n>
[X = channel, n = electrode]
EEG<X> LEAD OFF
[X = channel]
at Information Center
EEG<X> LEADS OFF
[X = channel]
EEG LINE NOISE
EEG 1 or 2 LINE NOISE
CPP The monitor has detected a conflict in the units used for this
calculation. Check the unit settings.
NBP Remove the cuff from the patient. Make sure that the tubing is
not kinked or twisted and that the correct patient category is
selected. Try repeating the measurement.
You can silence the INOP, but the INOP message remains
visible until the next NBP measurement is started or the Stop
All SmartKey is selected.
[Adult or pediatric patients: The NBP cuff pressure has exceeded
15mmHg (2kPa) for more than 3 minutes.
Neonatal patients: The NBP cuff pressure has exceeded
5mmHg (0.7kPa) for more than 90 seconds.]
ECG Contact your service personnel.
The ECG hardware is faulty.
ECG Not all the required leads for ECG monitoring are connected.
Check the ECG connections and make sure that the electrode
indicated by <ECG lead> [RA, LA, LL, RL, V or C] electrodes
is attached. In EASI mode, all 5 electrodes must be connected.
RL, V (or C)] is noisy. Check the ECG connections and make
sure that the electrode indicated is attached.
ECG The ECG signal is too noisy. Check that the electrodes are
properly placed and have not dried out. Remove any possible
sources of signal noise (such as power cords) from the area
around the cable and the patient.
The ECG signal may be saturated or overloaded.
ECG Check that the ECG out cable is securely connected. Contact
your service personnel.
EEG The EEG hardware is faulty. Contact your service personnel.
EEG The signal electrode in one or both channels exceeds the user-
selected impedance limit, or the impedance of a single electrode
exceeds the limit. Check the impedance. If the impedance is
too high, reconnect the electrodes according to the EEG
monitoring setup guidelines.If the INOP persists, contact your
service personnel.
EEG Reconnect specified electrode.
EEG One or more electrodes are not connected. Check in the EEG
Impedance/Montage window on the monitor which
electrode(s) are affected and reconnect the electrodes.
EEG Two or more electrodes are not connected. Check in the EEG
Impedance/Montage window which electrodes are
affected and reconnect the electrodes.
EEG Excessive line noise has been detected in either channel EEG1
or EEG2, or in both EEG channels.
Keep all cables together and away from metallic bodies, other
cables & radiated fields.
64
Page 83

Technical Alarm Messages (INOPs) 4 Patient Alarms and INOPs
INOP Message, Indication Source What to do
EEG MUSCLE NOISE
EEG 1 or 2 MUSCLE NOISE
EEG NO TRANSDUCER
INOP tone
EEG UNPLUGGED
INOP tone
EEG OVERRANGE, or
EEG<X> OVERRANGE
FAP INOPS PRESS See <Pressure label> INOPS (under Pressure).
FMS UNPLUGGED
INOP tone.
FMS UNSUPPORTED
INOP tone.
IC1/IC2INOPS PRESS See <Pressure label> INOPS (under Pressure).
ICP INOPs PRESS See <Pressure label> INOPS (under Pressure).
Indep.Dsp Malfunc.
INOP tone
Internal.Comm.Malf
INOP tone
LA LEAD OFF
Numeric is displayed with a -?- for 10
seconds; INOP tone.
LAP INOPs PRESS See <Pressure label> INOPS (under Pressure).
LEADS OFF
Numeric is displayed with a -?- for 10
seconds; INOP tone.
LL LEAD OFF
Numeric is displayed with a -?- for 10
seconds; INOP tone.
Measserv Unsupportd Monitor The measurement server is not supported by the monitor.
MMS UNPLUGGED
INOP tone.
MMS UNSUPPORTED
INOP tone.
MSL Power High Monitor The power consumption of the devices connected to the
EEG Too much power above 30 Hz has been detected in channel
EEG1 or EEG2, or both.
Check the Electrode-to-Skin Impedance and reposition the
electrode away from possible muscle activity, if necessary.
EEG The trunk cable is disconnected from the EEG plug-in module.
Reconnect the trunk cable.Silencing this INOP switches the
measurement off.
EEG Plug in module. Silencing this INOP switches off the
measurement.
EEG Input signal is too high in one or both channels. This is usually
caused by interfering signals such as line noise or
electrosurgery. X denotes the EEG channel.
FMS Make sure that the Flexible Module Server is connected to the
monitor. All FMS measurements are off while the FMS is
unplugged.
FMS The Flexible Module Server is not supported by your monitor.
Contact your service personnel.
Display There is a problem with the independent display. Contact your
service personnel.
Monitor There is a problem with I2C Bus communication in the
monitor. Contact your service personnel.
ECG The LA electrode has become detached from the patient or the
lead set has been changed. Reattach the electrode or select
Lead Setup
new lead set.
ECG Check that all of the required ECG leads are attached, and that
none of the electrodes have been displaced.
ECG The LL electrode has become detached from the patient or the
lead set has been changed. Reattach the electrode or select
Lead Setup
new lead set.
Contact your service personnel.
MMS Make sure that the Multi-Measurement Server is connected to
the monitor. All MMS measurements are off while the MMS is
unplugged.
MMS The Multi-measurement Server is not supported by your
monitor. Contact your service personnel.
Measurement Server Link (MSL) cable is too high. If this
situation continues, the MSL will be switched off. Contact
your service personnel.
in the Setup ECG menu to confirm the
in the Setup ECG menu to confirm the
New
New
65
Page 84

4 Patient Alarms and INOPs Technical Alarm Messages (INOPs)
INOP Message, Indication Source What to do
MSL Power Off
INOP tone.
MSL Power Overload
INOP tone.
NBP CUFF OVERPRESS
Numeric displayed with -?- ; INOP
tone.
During this INOP, alarms cannot be
paused or switched off.
NBP EQUIP MALF
Numeric is displayed with a -?INOP tone.
NBP INTERRUPTED
Numeric is displayed with a -?INOP tone.
NBP MEASURE FAILED
Numeric may be displayed with a -?INOP tone.
No Central Monit.
INOP tone
NO PPV FROM MeasSrv
at Information Center
NO PPV FROM <Server> MMS or
P/P1/P2/P3/P4 INOPS PRESS See <Pressure label> INOPS (under Pressure).
PAP INOPS PRESS See <Pressure label> INOPS (under Pressure).
PPV BAD <Pressure Label>
SIGNAL
Monitor The power consumption of the devices connected to the
Measurement Server Link (MSL) cable was too high for too
long and the MSL has been switched off. Contact your service
personnel.
Monitor The power consumption of the devices connected to the
Measurement Server Link (MSL) cable is much too high or
there has been a short circuit. The MSL has been switched off.
Contact your service personnel.
NBP The NBP cuff pressure exceeds the overpressure safety limits.
Remove the cuff from the patient. Make sure that the tubing is
not kinked or twisted and that the correct patient category is
selected. Try restarting the measurement.
You can silence this INOP, but the INOP message remains
visible until the next measurement is started or the Stop All
SmartKey is selected.
NBP Remove the cuff from the patient. The NBP hardware is faulty.
Contact your service personnel.
You can silence this INOP, but the INOP message remains
visible until the next measurement is started or the Stop All
SmartKey is selected.
NBP Check the tubing and cuff for leakages or kinks. Check that
you are using the correct cuff size and placement, and that the
correct patient category is selected. Try restarting the
measurement.
If the INOP occurs repeatedly, contact your service personnel.
You can silence this INOP, but the INOP message remains
visible until the next measurement is started or the Stop All
SmartKey is selected.
This INOP arises when the measurement needed longer than
the maximum time for inflation, deflation or the total
measurement.
NBP Check that you are using the correct cuff size and placement,
and that the correct patient category is selected. Try restarting
the measurement.
If numerics are displayed, the monitor is able to measure mean
only and the alarm source is set to S, D or S&D.
You can silence this INOP, but the INOP message remains
visible until the next measurement is started or the Stop All
SmartKey is selected.
Check the condition and suitability of the patient for NBP
monitoring. Use another cuff to continue measuring.
Monitor There is a problem with the communication to the network.
Central monitoring is currently not possible (no patient alarms
or information). Check the connection. Contact your service
personnel.
MMS or
FMS
FMS
PRESS The arterial pressure source selected for PPV is not providing a
The measurement server does not supply a beat-to-beat arterial
pressure value. Contact your service personnel.
The measurement server does not supply a beat-to-beat arterial
pressure value. Contact your service personnel.
pulsatile signal.
66
Page 85

Technical Alarm Messages (INOPs) 4 Patient Alarms and INOPs
INOP Message, Indication Source What to do
PPV BAD SIGNAL
at Information Center
PPV CHK SOURCES PRESS The arterial pressure source selected for PPV is unplugged or
<Pressure label> ARTIFACT
Numeric displayed with -?-
<Pressure label>
DEACTIVATED
INOP tone
<Pressure label> EQUIP
MALF
Numeric displayed with -?INOP tone.
<Pressure label> NO
TRANSDUCER
Numeric is displayed with a -?INOP tone.
<Pressure label> NOISY
SIGNAL
Pulse numeric is displayed with a -?INOP tone.
<Pressure label> NONPULSATILE
Pulse numeric is displayed with a -?INOP tone.
<Pressure label>
OVERRANGE
Numeric is displayed with a -?INOP tone.
<Pressure label> REDUCE
SIZE
<Pressure label> TRANSDUC
MALF
Numeric is displayed with a -?INOP tone.
<Pressure label>
UNPLUGGED
PRESS The arterial pressure source selected for PPV is not providing a
pulsatile signal.
switched off. When this INOP has displayed for 1 minute PPV
will be switched off.
PRESS A non-physiological event is detected (for example, a flush or
blood sample). A resulting high limit alarm will be suppressed.
PRESS A Pressure measurement label in the measurement server or
extension has been deactivated, either by connecting a Temp
transducer in the shared Press/Temp socket, or by deactivating
the label in the Measurement Selection window.
The measurement automatically disappears from the display.
To switch the measurement on again, either reconnect a
Pressure transducer or reactivate the measurement label in the
Measurement Selection window.
PRESS Contact your service personnel.
The pressure hardware is faulty.
PRESS Make sure that the pressure transducer is connected to the
measurement server or module server.
If you silence this INOP, the measurement will be switched off.
PRESS This INOP can only arise when a pressure is selected as the
pulse source. It occurs when the pulse detector finds a pulse
rate above 350bpm. This is usually caused by movement
artifact or electrical interference.
PRESS This INOP can only arise when a pressure is selected as the
pulse source. It occurs when the pulse rate being measured is
less than 25 beats per minute or the amplitude is less than three
mmHg.
Check the catheter and connections to the patient.
PRESS Make sure that the measurement has been properly prepared
and zeroed, and that the transducer is level with the heart. If
this INOP persists, try another transducer.
Possible causes are a measured pressure outside the allowed
pressure range, or a broken wire to the transducer.
PRESS Increase the scale for the pressure wave.
PRESS Contact your service personnel.
The transducer is faulty.
PRESS A Pressure measurement label has been deactivated, either by
unplugging a module, or by deactivating the label in the
Measurement Selection window.
The measurement automatically disappears from the display.
To switch the measurement on again, either replug the module
or reactivate the measurement label in the Measurement
Selection window.
67
Page 86

4 Patient Alarms and INOPs Technical Alarm Messages (INOPs)
INOP Message, Indication Source What to do
<Pressure label>
PRESS Perform a zero and check the calibration of the transducer.
ZERO+CHECK CAL
Numeric is displayed with a -?-
RA LEAD OFF
Numeric is displayed with a -?INOP tone.
ECG The RA electrode has become detached from the patient or the
lead set has been changed. Reattach the electrode or select
Lead Setup
in the Setup ECG menu to confirm the
New
new lead set.
RAP INOPS PRESS See <Pressure label> INOPS (under Pressure).
Rem.Alarmdev.Malf
INOP tone
RESP EQUIP MALF
Monitor There is a problem with the connection to the remote alert
device. Contact your service personnel to check the remote
alert device and its connections.
RESP Contact your service personnel. The RESP hardware is faulty.
Numeric is displayed with a -?INOP tone.
RESP ERRATIC
Numeric is displayed with a -?-
RESP The monitor has detected too many artifacts in the measured
Resp signal. Check that the RA and LL electrodes are correctly
attached and have not dried out.
RESP LEADS OFF
Numeric is displayed with a -?-
RESP Not all the required leads for Resp monitoring are attached.
Make sure that the RA and LL leads are attached.
INOP tone.
RL LEAD OFF
Numeric is displayed with a -?- for 10
seconds; INOP tone.
ECG The RL electrode has become detached from the patient or the
lead set has been changed. Reattach the electrode or select
Lead Setup
in the Setup ECG menu to confirm the
New
new lead set.
Settings Malfunc.
INOP tone.
Monitor The monitor cannot use the predefined settings for
monitoring. Contact your service personnel.
SOME ECG ALARMS OFF Arrhythmia This message appears (if configured to do so) when the on/off
settings of the yellow arrhythmia alarms differ from the current
Profile.
Speaker Malfunct.
INOP tone
∆SpO
CHK SOURCES
2
Numeric is displayed with a -?-
∆SpO
CHK UNITS
2
Numeric is displayed with a -?-
<SpO2 label> DEACTIVATED
INOP tone
Monitor Contact your service personnel to check the speaker and the
connection to the speaker.
SpO
2
Difference
SpO
2
Difference
SpO
2
Not all measurements or values required to perform the
calculation are available. Check measurement sources.
The monitor has detected a conflict in the units used for this
calculation. Check the unit settings.
You have connected a measurement server that uses a label the
monitor has already assigned to a different source. To activate
the new source, choose a new label in the Measurement
Selection window.
<SpO2 label> EQUIP MALF
Numeric is replaced by a -?-
SpO
2
The MMS is faulty. Unplug and replug the MMS. If the INOP
persists, contact your service personnel.
INOP tone.
<SpO2 label> ERRATIC
Numeric is replaced by a -?-
SpO
2
Check the sensor placement. Try another adapter cable and
sensor. If the INOP persists, contact your service personnel.
INOP tone.
<SpO2 label> EXTD. UPDATE
Label is displayed with a -?(questionable numeric)
SpO
2
The update period of displayed values is extended due to an
NBP measurement on the same limb or an excessively noisy
signal.
68
Page 87

Technical Alarm Messages (INOPs) 4 Patient Alarms and INOPs
INOP Message, Indication Source What to do
<SpO2 label> INTERFERNCE
Numeric is replaced by a -?INOP tone.
<SpO2 label> LOW PERF
Label is displayed with a -?(questionable numeric)
<SpO2 label> NOISY SIGN.
Numeric is replaced by a -?INOP tone.
<SpO2 label> NON-PULSAT.
Numeric is replaced by a -?INOP tone.
<SpO2 label> NO SENSOR
Numeric is replaced by a -?INOP tone.
<SpO2 LABEL> POOR SIGNAL
Label is displayed with a - ? (questionable numeric)
<SpO2 LABEL> PULSE?
Numeric is replaced by -?INOP tone
<SpO2 LABEL> SEARCHING
Numeric unavailable
<SpO2 label> SENSOR MALF
Numeric is replaced by a -?INOP tone.
<SpO2 LABEL> SENSOR OFF
Numeric is replaced by -?INOP tone
<SpO2 LABEL> UNKN.SENSOR
Numeric is replaced by a - ? -
<SpO2 LABEL> UPGRADE
Label is displayed with a -?-, numeric is
unavailable
Sp - vO2 CHK SOURCES
Numeric is displayed with a -?-
Sp - vO2 CHK UNITS
Numeric is displayed with a -?-
SvO2 CAL FAILED
Sv
O2 numeric is displayed with ?
SvO2 CAL MODE
Sv
O2 numeric displays -?-
SpO
2
There is too much interference, caused by a high level of
ambient light and/or electrical interference. Cover the sensor to
minimize ambient light. If the INOP persists, make sure that
the sensor cable is not damaged or positioned too close to
power cables.
SpO
2
Accuracy may be compromised due to very low perfusion.
Stimulate circulation at sensor site. If INOP persists, change
the measurement site.
SpO
2
Excessive patient movement or electrical interference is causing
irregular pulse patterns. Try to reduce patient movement or to
relieve the cable strain on the sensor.
SpO
2
Check the perfusion at measurement site. If necessary,
stimulate circulation or change measurement site. If the INOP
is due to NBP measurement on the same limb, wait until the
NBP measurement is finished.
SpO
2
Make sure the SpO2 sensor is connected. If the INOP persists,
try another adapter cable and sensor. If you silence this INOP,
the measurement will be switched off.
SpO
2
The signal condition of the SpO2 measurement is poor and
measurement accuracy may be compromised.
SpO
2
The detectable pulsations of the SpO2 signal are outside the
specified pulse rate range.
SpO
2
SpO2 is analyzing the patient signal to derive Pulse, SpO2 and
Perf values. Please wait until the search analysis is complete.
SpO
2
The SpO2 sensor or adapter cable is faulty. Try another adapter
cable and sensor. If the INOP persists, contact your service
personnel.
SpO
2
The SpO2 sensor is not properly applied to the patient. Apply
the sensor following the instructions supplied by the
manufacturer.
SpO
SpO
2
2
The connected sensor or adapter cable is not supported by the
SpO
measurement. Use only specified sensors and cables.
2
The SpO2 measurement is currently in UPGRADE mode.
Monitoring is not possible in this mode.
Sp - vO2Not all measurements or values required to perform the
calculation are available. Check measurement sources.
Sp - vO2The monitor has detected a conflict in the units used for this
calculation. Check the unit settings.
O
Sv
2
The calibration failed. Check the catheter-to-Optical-Module
connection. Manually restart the calibration. Try another
catheter and Optical Module. If the catheter is already inserted,
perform an in-vivo calibration.
O
Sv
2
Pre-insertion calibration is complete, but the catheter tip is still
inside the optical reference. The catheter is now ready for
insertion.
69
Page 88

4 Patient Alarms and INOPs Technical Alarm Messages (INOPs)
INOP Message, Indication Source What to do
SvO2 CAL REQUIRED
Sv
O2 numeric displays -?-.
Sv
INOP tone may sound
SvO2 CONFIGURATION
O2 numeric displays -?-.
Sv
Sv
INOP tone
SvO2 CONNCT OPTMOD
O2 numeric displays -?-.
Sv
Sv
INOP tone
SvO2 EQUIP MALF
Sv
O2 numeric displays -?-.
Sv
INOP tone
SvO2 IN-VIVO CALIB
O2 numeric displays -?-.
Sv
SvO2 LIGHT INTENS
O2 numeric displays -?- or numeric
Sv
Sv
Sv
is displayed with ?
INOP tone with -?- display
SvO2 LOW LIGHT
Sv
O2 numeric displays -?- or numeric
Sv
is displayed with ?
INOP tone may sound
SvO2 NO OPTMOD
Sv
O2 numeric displays -?-.
Sv
INOP tone
SvO2 OPTMOD DEFECT SvO
SvO2 OPTMOD WARMUP
O2 numeric is displayed with ?
Sv
SvO2 PRE-INS CALIB
O2 numeric displays -?-
Sv
Sv
Sv
INOP tone
SvO2 UNABL TO MEAS
O2 numeric displays -?-.
Sv
Sv
INOP tone
SvO2 UNPLUGGED
Sv
O2 numeric displays -?-.
Sv
INOP tone
SVR/SVRI CHK SOURCES
SVR/SVRI Not all measurements or values required to perform the
Numeric is displayed with a -?-
SVR/SVRI CHK UNITS
SVR/SVRI The monitor has detected a conflict in the units used for this
Numeric is displayed with a -?-
SVR/SVRI SET CVP USED
SVR/SVRI A CVP value is required for this calculation, but is not
numeric displays - ? -
O
2
There is no valid calibration data in the Optical Module.
Perform either a pre-insertion or an in-vivo calibration.
O
2
The Optical Module has been configured to SaO2 Mode. Use
Change to SvO2 in the Setup SvO2 menu to
reconfigure to SvO
O
2
The Optical Module was disconnected during data storage.
Mode.
2
Reconnect the Optical Module for at least 20 seconds.
O
2
The SvO2 Module or Optical Module is faulty. Unplug and
replug the Optical Module and SvO
module. Exchange the
2
modules. If the INOP persists, contact your service personnel.
O
2
The in-vivo calibration is not yet complete. Lab values must be
stored to the Optical Module to complete the calibration.
Either continue with the next steps of the current calibration or
recall the previous calibration.
O
2
The intensity changed considerably since the last light intensity
calibration. This may indicate that the catheter tip is positioned
against a blood vessel wall or that there is low blood flow.
Reposition the catheter and perform a light intensity
calibration.
O
2
The optical signal levels are too low. Check that the catheter is
either in the optical reference or inserted into the patient.
Check the catheter-to-Optical Module connection. If INOP
persists, try another catheter and Optical Module.
O
2
Connect the Optical Module. If the INOP persists, try another
Optical Module. Silencing this INOP switches the
measurement off.
2
The Optical Module memory is faulty, and calibration data
cannot be stored for transport or during power failure. If this
feature is needed, use another Optical Module.
O
2
The Optical Module has not yet reached the operating
temperature. Wait a few minutes until warm-up is finished.
O
2
The pre-insertion calibration is running. This typically takes
one minute. During this time Sv
O2 alarms are switched off.
Wait until the calibration is complete.
O
2
The signal is out of the normal range, and no SvO2 value can
be derived. Perform an in-vivo calibration. If the INOP
persists, try another Optical Module and catheter.
O
2
Measurement switched on and SvO2 module unplugged from
the rack.
The measurement automatically disappears from the display.
Silencing this INOP switches off the measurement.
calculation are available. Check measurement sources.
calculation. Check the unit settings.
currently being measured. The monitor is using the CVP value
preset in the
Setup SVR menu.
70
Page 89

Technical Alarm Messages (INOPs) 4 Patient Alarms and INOPs
INOP Message, Indication Source What to do
T/T1/T2/T3/T4 INOPs TEMP See <Temp label> INOPs (under Temp)
Tamb INOPs TEMP See <Temp label> INOPs (under Temp)
Tart INOPs TEMP See <Temp label> INOPs (under Temp)
Tblood NO TRANSDUC
Numeric displays -?INOP tone
Tblood OVERRANGE
Numeric displays -?-
Tcereb INOPS TEMP See <Temp label> INOPs (under Temp)
Tcore INOPs TEMP See <Temp label> INOPs (under Temp).
tcpO2 (or tcpCO2 or tcGas)
CAL FAILED
Numeric displays -?INOP tone.
tcpO2 (or tcpCO2 or tcGas)
CAL REQUIRD
Numeric displays -?INOP tone.
tcpO2 (or tcpCO2 or tcGas)
CAL RUNNING
Numeric displays first -?- , then
numeric is displayed with a ?
tcpO2 (or tcpCO2 or tcGas)
CHECK TIME
tcpO2 (or tcpCO2 or tcGas)
CHANGE SITE
If Heat Switch Off is configured to
Yes, numeric displays -?INOP tone.
tcpO2 (or tcpCO2 or tcGas)
EQUIP MALF
Numeric displays -?INOP tone.
tcpO2 (or tcpCO2 or tcGas)
NO TRANSDUC
Numeric displays -?INOP tone.
tcpO2 (or tcpCO2 or tcGas)
STABILIZING
Numeric is displayed with a ?
tcpO2 (or tcpCO2 or tcGas)
UNPLUGGED
Numeric displays -?INOP tone.
<∆Temp> CHK SOURCES
Numeric is displayed with a -?-
C.O. No transducer attached to the module or catheter
disconnected.
C.O. Tblood out of range 17°C - 43°C.
tcGas A calibration failed. Check the cal. unit, gas pressure, and
tubing connections, then restart the cal. If the cal. has failed
more than once, remembrane the transducer and restart the
calibration. If this INOP persists, contact your service
personnel.
tcGas Calibration is required before applying the transducer to the
patient.
Insert a membraned transducer into the cal. chamber on the
module, connect the cal. unit to the cal. chamber, open the gas
valve and start the calibration. If this INOP occurs during a
calibration, there may be a module or transducer malfunction:
contact your service personnel.
tcGas Wait until the tcpO2/tcpCO2 calibration is finished.
tcGas Site Timer due to time out in 15 minutes or less.
tcGas Site Timer has timed out. Change the application site to avoid
skin burns. To reset the Site Timer, either calibrate and change
the measurement site, or change the measurement site and reset
the Site Timer manually by selecting the appropriate site time
from the
tcGas There is a malfunction in the transducer or module. Connect
another transducer. If this INOP persists, contact your service
personnel.
tcGas No transducer is connected to the tcpO2/tcpCO2 module.
Silencing the alarm switches off the measurement.
tcGas The transducer has not yet reached the selected temperature
and/or skin hyperemization is not yet finished. This INOP will
disappear within three minutes.
tcGas The measurement is switched on but the module is unplugged.
The measurement automatically disappears from the display.
Silencing this INOP switches off the measurement.
TEMP
Difference
Not all measurements or values required to perform the
calculation are available. Check measurement sources.
Setup TCGas menu.
71
Page 90

4 Patient Alarms and INOPs Technical Alarm Messages (INOPs)
INOP Message, Indication Source What to do
<∆Temp> CHK UNITS
Numeric is displayed with a -?-
<Temp label> DEACTIVATED
INOP tone
<Temp label> EQUIP MALF
Numeric is displayed with a -?INOP tone.
<Temp label> NO
TRANSDUCER
Numeric is displayed with a -?INOP tone.
<Temp label> UNPLUGGED
INOP tone
<Temp label> OVERRANGE
Numeric is displayed with a -?INOP tone.
Tesoph INOPS TEMP See <Temp label> INOPs (under Temp).
TimeExpired:<timer label>
INOP tone
Tnaso INOPS TEMP See <Temp label> INOPs (under Temp).
Trect INOPS TEMP See <Temp label> INOPs (under Temp).
Tskin INOPS TEMP See <Temp label> INOPs (under Temp).
Ttymp INOPS TEMP See <Temp label> INOPs (under Temp)
Tven INOPS TEMP See <Temp label> INOPs (under Temp).
Tvesic INOPS TEMP See <Temp label> INOPs (under Temp)
UAP INOPS PRESS See <Pressure label> INOPS (under Pressure).
Unsupported LAN
INOP tone
User I/F Malfunct.
INOP tone.
UVP INOPS PRESS See <Pressure label> INOPS (under Pressure).
V LEAD OFF
Numeric is displayed with a -?- for 10
seconds; INOP tone.
TEMP
Difference
TEMP A Temp measurement label in the measurement server or
TEMP Contact your service personnel.
TEMP Make sure the TEMP probe is connected to the MMS or
TEMP A Temp measurement label has been deactivated, either by
TEMP Try changing the application site of the transducer.
Monitor The time has expired for the timer indicated in the INOP text.
Monitor There is a problem with the communication to the network
Monitor Perform a visual and functional check of all the monitor input
ECG The V electrode (IEC: C electrode) has become detached from
The monitor has detected a conflict in the units used for this
calculation. Check the unit settings.
extension has been deactivated, either by connecting a Pressure
transducer in the shared Press/Temp socket, or by deactivating
the label in the Measurement Selection window.
The measurement automatically disappears from the display.
To switch the measurement on again, either reconnect a Temp
transducer or reactivate the measurement label in the
Measurement Selection window.
The temperature hardware is faulty.
module.
If you silence this INOP, the measurement will be switched off.
unplugging a module, or by deactivating the label in the
Measurement Selection window.
The measurement automatically disappears from the display.
To switch the measurement on again, either replug the module
or reactivate the measurement label in the Measurement
Selection window.
[The temperature is less than -1
Clearing the timer clears the INOP.
and central monitoring is currently not possible. Check the
connection.If the INOP persists, switch off the monitor and
contact your service personnel.
devices. Contact your service personnel.
the patient or the lead set has been changed. Reattach the
electrode or select
menu to confirm the new lead set.
New Lead Setup in the Setup ECG
°C, or greater than 45°C.]
72
Page 91

Technical Alarm Messages (INOPs) 4 Patient Alarms and INOPs
INOP Message, Indication Source What to do
<VueLink option> CHK
CABLE
INOP tone.
<VueLink option> CHK
CONF.
INOP tone.
<VueLink option> CHECK
SETUP
INOP tone.
VueLnk EQUIP MALF
INOP tone.
VueLnk NO CONFIG
INOP tone.
VueLnk UNPLUGGED
INOP tone.
VueLink No cable or the wrong cable connected to the VueLink
module, or incorrect device selected. Silencing this INOP
switches the measurement off.
VueLink INOP abbreviations may differ slightly depending on
the device category.
VueLink The wrong external device has been selected on the VueLink
module, or the external device has not been correctly setup, or
the wrong cable has been used to connect the device to the
VueL i nk m odul e .
VueLink INOP abbreviations may differ slightly depending on
the device category.
VueLink No information was received from the external device. The
device may be switched off or disconnected.
VueLink INOP abbreviations may differ slightly depending on
the device category.
VueLink Malfunction in the VueLink module. If this message appears
repeatedly, the module must be replaced. Contact your service
personnel.
VueLink INOP abbreviations may differ slightly depending on
the device category.
VueLink The VueLink module has not been configured during
installation. The installation process should be completed by
either your biomedical engineering department or the Philips
service engineer.
VueLink INOP abbreviations may differ slightly depending on
the device category.
VueLink The VueLink module has been unplugged from the rack, or the
whole rack has been disconnected. The measurement
automatically disappears from the display. Silencing this INOP
switches off the measurement.
VueLink INOP abbreviations may differ slightly depending on
the device category.
73
Page 92

4 Patient Alarms and INOPs Technical Alarm Messages (INOPs)
74
Page 93

Use the Patient Demographics window and its associated pop-up keys to admit, discharge, and transfer
(ADT) patients.
All patient demographic and ADT information is shared between the patient monitor and the
Information Center, for example, patients admitted to the monitor are automatically admitted to a
connected Information Center.
Admitting a Patient
The monitor displays physiological data and stores it in the trends as soon as a patient is connected.
This lets you monitor a patient who is not yet admitted. It is however important to admit patients
properly so that you can identify your patient on recordings, reports, and networked devices.
During admission you enter data that the monitor needs for safe and accurate operation. For example,
the patient category setting determines the algorithm the monitor uses to process and calculate some
measurements, the safety limits that apply for some measurements, and the alarm limit ranges.
5
5Managing Patients
To admit a patient,
1 Select the patient name field or select the
Admit/Dischrge SmartKey to open the
Patient Demographics window.
2 Clear any previous patient data by selecting
Dischrge Patient or End Case
the
pop-up key and then Confirm.
If you do not discharge the previous patient,
you will not be able to distinguish data from
the previous and current patients, for
example, in the trend database.
3 Select Admit Patient.
4 Enter the patient information: select each
field and use the on-screen keyboard or
choose from the pop-up list of alternatives to
input information. If a conventional
keyboard or a barcode scanner is connected to the monitor you can use this to enter patient
information.
Last name: Enter the patient’s last name (family name), for example Smith.
–
Patient Demographics
Last Name
First Name
MRN
Patient Cat.
Paced
Height
Weight
BSA (D)
Date of Birth
Age
Gender
Notes (1):
Notes (2):
Adult
No
75
Page 94

5 Managing Patients Quick Admitting a Patient
– First name: Enter the patient’s first name, for example Joseph.
– MRN: Enter the patient’s medical record number (MRN), for example 12345678.
– Patient Cat: Choose the patient category, either Adult, Pediatric, or Neonatal.
Paced: Choose Yes or No (You must use “Yes” if your patient has a pacemaker).
–
Height: Enter the patient’s height.
–
Weight: Enter the patient’s weight.
–
BSA: The monitor calculates the body surface area automatically.
–
Date Of Birth: Enter the patient’s date of birth. Enter this in the form dd/mm/yyyy.
–
Age: The monitor calculates the patient age automatically.
–
Gender: Choose Male or Female.
–
Notes: Enter any extra information about the patient or treatment.
–
5 Select Confirm. The patient status changes to admitted.
Patient Category and Paced Status
The patient category setting determines the algorithm the monitor uses to process and calculate some
measurements, the safety limits that apply for some measurements, and the alarm limit ranges.
The paced setting determines whether the monitor shows pacemaker pulses or not. When Paced is
set to No, pace pulses are filtered and therefore do not show in the ECG wave.
WARNING Patient Category and Paced status will always contain a value, regardless of whether the
patient is fully admitted or not. If you do not specify settings for these fields, the monitor uses the
default settings from the current profile, which might not be correct for your patient.
Patient category Changing the patient category may change the arrhythmia and NBP alarm limits.
Always check alarm limits to make sure that they are appropriate for your patient.
Paced status For paced patients, you must set
could mistake a pace pulse for a QRS and fail to alarm during asystole.
Paced to Yes. If it is incorrectly set to No, the monitor
Admitting a Centrally-Monitored Patient
You can admit a patient at either the bedside or the Information Center. When you admit a patient,
the patient’s name appears on the bedside monitor and the Information Center.
If you do not fill in all patient information required by the Information Center, the Information
Center may reject the admission. Complete all the required fields and try again to admit the patient.
Quick Admitting a Patient
Use Quick Admit only if you do not have the time or information to fully admit a patient. Complete
the rest of the patient demographic details later. If you do not, the patient name will not be written on
reports and on information stored in the database or sent to an Information Center.
76
1 Select the Quick Admit SmartKey.
2 Enter the required data (MRN or Last Name depending on configuration) with the keyboard or a
barcode scanner.
Page 95

Editing Patient Information 5 Managing Patients
Select Enter.
3
4 In the confirmation window, select Confirm to discharge the previous patient (if confirmation is
configured).
5 Check that patient category and paced status are correct for the new patient.
If the monitor is connected to an Information Center and only the MRN is entered, the patient name
is set to - - - . The patient name field on the monitor shows
space on printed reports is blank. To fully admit this patient, select Admit
complete all required fields.
Not Admitted and the patient name
Patient again and
Editing Patient Information
To edit the patient information after a patient has been admitted, select the patient name field on the
Main Screen to open the
Patient Demographics window, and make the required changes.
Discharging a Patient
You should always perform a discharge even if your previous patient was not admitted. A discharge:
– clears the information in the Patient Demographics window
– erases all patient data (such as trend, event, and calculation data) from the monitor, measurement
servers and Information Center
– resets patient category and paced settings to the settings defined in the default Profile
– resets all monitor and measurement settings as well as the active Screen to the settings defined in
the default Profile
– discharges the patient from the Information Center.
When a patient is discharged from the monitor or from an Information Center, all patient data is
deleted. Make sure that you have printed out any required reports before discharging. Check that a
functioning local or central printer is available before you use End Case.
To discharge a patient,
1 Select the patient name field to display the Patient Demographics window and associated
pop-up keys.
2 Select the pop-up key for either:
– End Case - to print any configured end case reports or vital signs recording, discharge the
patient and clear the patient database, then enter standby mode. If an End Case SmartKey is
configured for your monitor, you can also select this instead and then confirm.
To see which end case reports are set up for your monitor, select Main Setup -> Reports ->
Auto Reports. For each auto report, if End Case Report is set to On, this report will
be printed when you select End Case. See the section on AutoReports for information on
setting up end case reports.
– Dischrge Patient - to discharge the patient without printing any reports.
77
Page 96

5 Managing Patients Transferring Patients
Transferring Patients
To save you from having to enter the same patient data multiple times and enable patient transfer
without loss of data, information can be shared between measurement servers, patient monitors, and
Information Centers.
– patient demographic information is shared between connected measurement servers, patient
monitors, and Information Centers
– measurement settings and calibration data can be uploaded from an MMS to a patient monitor, if
configured
– trend information can be uploaded from an MMS to a patient monitor, if configured.
Different sets of patient- and measurement-related data are stored in the monitor and the MultiMeasurement Server. Understanding this will help you to understand what happens to patient data
when you transfer patients.
Patient Information Stored in Monitor Stored in MMS and extensions
Patient demographics (name,
DOB, MRN)
Monitor settings (alarm pause
time, alarm volume)
Measurement settings for all
measurements (alarm limits,
measurement on/off, etc.)
Trend data
Calculation data (HemoCalc
data)
Events data
WARNING If the monitor is not battery-powered, you cannot monitor during transport.
yes yes
yes no
yes yes, for all MMS and extensions
measurements
yes, for all MMS and extensions
measurements (up to a maximum
of 16 or 32, depending on your
database configuration)
yes no
yes no
most recent 8 hours of
information, for all MMS and
extensions measurements
Transferring a Centrally-Monitored Patient
78
Scenario: A centrally-monitored patient is moved to another monitoring location on the same
Information Center database server without interrupting the collection of patient trend information.
1 Before you disconnect the MMS from the monitor, select the patient name in the monitor info line
to enter the Patient Demographics window, then select the Transfer pop-up key. If
the patient is not admitted or not monitored by an Information Center, the Transfer key is
inactive (“grayed-out”).
This step preserves the patient’s demographic data during the transfer.
Page 97

Data Upload from an MMS 5 Managing Patients
Remove the MMS and any connected extensions from the monitor. Do not separate any connected
2
extensions from the MMS, as this will erase all settings and trend data stored in the MMS for the
extension measurements.
3 Connect the MMS to the transfer monitor and monitor your patient during the move.
4 At the new location, connect the MMS to the monitor. If the monitor detects a patient conflict,
the patient selection window will be displayed.
5 Select Continue MMS and Confirm your selection. This re-admits the patient from the
transfer list to the new monitor, completing the transfer. This will upload the patient
demographics, and, if configured, the measurement settings and trend data stored in the MMS to
the receiving monitor.
6 Verify that the settings for patient category and paced mode are correct.
If you accidentally transfer a patient, use
Center. If you are not connected to the network, select
patient data remains in the monitor.
Re-admit to restore this patient’s data to the Information
Clear Transfer to leave transfer mode.The
Transferring a Patient with an MMS (no Central Station)
Scenario: A patient is moved to another monitoring location using a transport monitor and readmitted at the new monitor.
1 Disconnect the MMS from the original monitor and silence the resulting MMS UNPLUGGED
INOP.
If you are sure that the patient will not be returning to this monitor, you should perform a
discharge or end-case. This prevents data from the next patient accidentally being mixed up with
your current patient’s data.
2 Connect the MMS to the transport monitor and move the patient.
3 At the new monitoring location, remove the MMS from the transport monitor and connect it to
the new monitor.
4 If prompted, re-admit the patient to the new monitor: in the Patient Selection window,
select Continue MMS to retain the data in the MMS. This will upload the patient
demographics, and, if configured, the measurement settings and trend data stored in the MMS to
the monitor. Verify that the settings for patient category and paced mode are correct.
Data Upload from an MMS
The Multi-Measurement Server stores eight hours of patient trend data at one-minute resolution. It
also stores patient demographic information and the measurement settings and calibration data for the
measurements carried out by the MMS and any connected extensions. This data can be uploaded to an
IntelliVue patient monitor, if your monitor is configured to do so and if at least five minutes of trend
information is stored in the MMS.
Your monitor’s data upload settings are defined in Configuration Mode to suit your patient transfer
use model.
How data is uploaded to the host monitor depends on the configuration mode settings
MMS Trend Upload and MMS Settings Upload.
If there is a patient conflict and you select Continue Monitor, no data will be uploaded from the
MMS.
79
Page 98

5 Managing Patients Data Exchange Between Information Centers
Data Exchange Between Information Centers
You can transfer demographic data and trend data from one IIC to another by selecting Transfer
on the patient monitor. Trend data is not shared between Information Centers and monitors.
Resolving Patient Information Mismatch
When you connect an MMS to a monitor, or a monitor to the network, the monitor compares patient
category, paced status, and a unique patient identification number that is internally stored in both the
MMS and the monitor. The monitor indicates a mismatch if the information is not identical.
Depending on your monitor’s configuration, this mismatch may be automatically resolved or you may
have to resolve it manually. If your monitor is configured to resolve mismatches automatically,
depending on the configuration, either the monitor or the Multi-Measurement Server data is
automatically retained.
WARNING USA only When a monitor is connected to an Information Center by the wireless IntelliVue
Instrument Telemetry interface, the patient data will automatically be merged in the case of a transfer.
This means there is no patient discharge at the monitor and settings and trend data will be retained.
You will see a message on the monitor and the Patient Demographics window will automatically
appear so that you can check the data and change it if necessary.
Manually Resolving Patient Mismatch
The patient mismatch is indicated by question marks (???) beside the questionable fields in the Monitor
Info Line and in the Patient Demographics window. The monitor displays a message such as
Different patients in Central and Monitor. The Patient Selection window
automatically opens so you can decide which patient data to use. You do not have to resolve the
mismatch immediately, however, the indicators remain until you do. There can be up to three columns
of data in the Patient Selection window if the patient is different in the Information Center,
monitor, and MMS.
After you resolve the mismatch, the monitor displays a confirmation window that explains the
consequences of your choice, telling you where the patient will be continued/discontinued. Confirm
your choice. The monitor automatically displays the Patient Demographics window after
confirmation. Verify that the settings shown are correct for the patient.
Gender, date of birth, height, weight, and nursing notes do not generate a mismatch. If these fields are
different on different devices, the monitor resolves them itself. For example, it may take date of birth
from the Information Center, whilst taking gender from the MMS. Always check the Patient
Demographics after combining patients, to ensure that you are satisfied with the results. Change them
if necessary.
WARNING After resolving a patient mismatch, check that the monitor settings (especially patient category, paced
status and alarm limits) are correct for the patient.
80
Page 99

Resolving Patient Information Mismatch 5 Managing Patients
Patient Mismatch - If One Set of Patient Data is Correct
♦ If there is a mismatch between an
Information Center and a monitor,
choose the data set you want to
continue using for this patient,
either:
Continue Central: to continue with
the patient demographics from the
Information Center, discharge the
patient in the monitor, and use the
default monitor profile.
Continue Monitor: to continue with
the patient in the monitor and
discharge the patient in the
Information Center, permanently
deleting all data in the Information
Center.
♦ If there is a mismatch between a
monitor and a measurement server,
choose the data set you want to
continue using for this patient,
either:
Continue Monitor: to continue with
the patient demographics, trend
data, and settings in the monitor.
This discharges the patient in the
measurement server, and resets all
MMS settings to the defaults
currently active for the monitor.
Continue MMS: to upload the data
- patient demographics, trend data
(if configured), and measurement
settings (if configured) - stored in the MMS to the monitor. This clears all data in the monitor,
resets the monitor to the default Profile, and discharges the patient in the monitor.
Patient Selection
Central Monitor
Last name DOE MILLER
First name JOHN
MRN 1234HG9556
Patient Cat Adult Neo
Paced No Yes
Continue
Central
Patient Selection
Last name MILLER ADAMS
First name PETER
MRN
Patient Cat Neo Neo
Paced Yes No
Continue
Monitor
Continue
Monitor
Monitor MeasServ
Continue
MMS
New
Patient
New
Patient
Same
Patient
Same
Patient
Patient Mismatch - If Neither Patient Data Set is Correct
A patient mismatch where neither set of patient data is correct might occur if you connect a new MMS
to a monitor in order to prepare for a new patient, before you actually start measuring.
♦ Select New Patient if you are sure that none of the information is correct. This discharges all
patients, erases all data in both the monitor and MMS, resets all settings to the default Profile, and
lets you admit a new patient.
81
Page 100

5 Managing Patients Care Groups
Patient Mismatch - If Both Patient Data Sets Are Correct
A patient mismatch where both sets of patient data are correct might occur if you admit a new patient
at the monitor (or Information Center) before the patient arrives at your unit and then connect the
MMS that was used during the patient transport to the monitor.
♦ Select Same Patient if the patient information is different, but you are sure it is the same
patient. This merges the demographics and updates them in the Information Center, monitor, and
MMS, according to this table. Be aware that your monitor may be configured to merge trend data
from the MMS and the monitor, and to upload measurement settings from the MMS to the
monitor.
Patient Information This information is taken from...
Patient name the monitor, if the patient was admitted there. For centrally-admitted
MRN
Screen Notes
Patient Category the Multi-Measurement Server. if connected, otherwise the data is
Date of Birth
Height
Weight
Gender
Paced Status Paced status is always set to Yes where there is a conflict in patient
Trend data if there is newer trend data stored in the MMS, it is uploaded to the
patients, this information is taken from the Information Center.
taken from the monitor.
information.
monitor.
Automatically Resolving Patient Mismatch
Your monitor can be configured to automatically resolve mismatches in one of two ways.
• continue using the patient in the MMS, and delete the old data in the monitor. This is suitable for
transport monitors.
• continue with the patient in the monitor, and delete the data in the MMS.
Care Groups
If your monitor is connected to an Information Center, you can group bedside monitors into Care
Groups. This lets you:
• view information on the monitor screen from another bed in the same or in a different Care Group.
• be notified of yellow or red alarm conditions at the other beds in the Care Group.
• see the alarm status of all the beds in the Care Group on each monitor screen.
There are two main types of Care Groups:
• standard care group (Bed-based Care Group) - up to 12 patients monitored by up to 4
Information Centers
•unit group (Unit-based Care Group) - for a complete unit with up to 64 patients
monitored by up to 4 Information Centers
82
 Loading...
Loading...