Page 1
Curves and Loops
in Mechanical Ventilation
Frank Rittner
Martin Döring
Page 2

Curves and Loops
in Mechanical Ventilation
Frank Rittner
Martin Döring
Page 3

5
Contents
Ventilation curve pattern
■ Pressure-time diagram 6
■ Flow-time diagram 10
■ Volume-time diagram 12
■ Interpretation of curve patterns 14
Loops – a good thing all round
■ PV loops 21
■ The static PV loop 21
■ The dynamic PV loop in ventilation 23
■ Interpretation of PV loops in ventilation 26
■ PV loops before and after the tube 34
■ Loops – other possibilities 38
■ Flow-volume loop 38
Trends reviewed
■ Documentation of a weaning process 41
■ Lung parameters based on peak and
plateau pressure
43
Capnography – locating problem areas
■ The physiological capnogram 46
■ Interpretations of capnograms 47
Page 4
6
Ventilation curve pattern
All the ventilators of the Evita family offer graphic
representation of the gradual changes in ventilation
pressure and breathing gas flow. Evita 4, EvitaScreen
and the PC software EvitaView additionally show the
gradual changes in the breathing volume. Two or in
some monitors three curves can be shown on the
screen at the same time, and particularly the fact
that pressure, flow and volume can be displayed
simultaneously makes it easier to detect changes
caused by the system or the lungs. The gradual
change in pressure, flow and volume depend to an
equal extent on the properties and settings of the
ventilator, as well as on the respiratory properties of
the lung.
One respiratory cycle comprises an inspiratory and
an expiratory phase. Under normal conditions these
two periods contain a flow phase and a no flow pause
phase. No volume passes into the lung during the no
flow phase during inspiration.
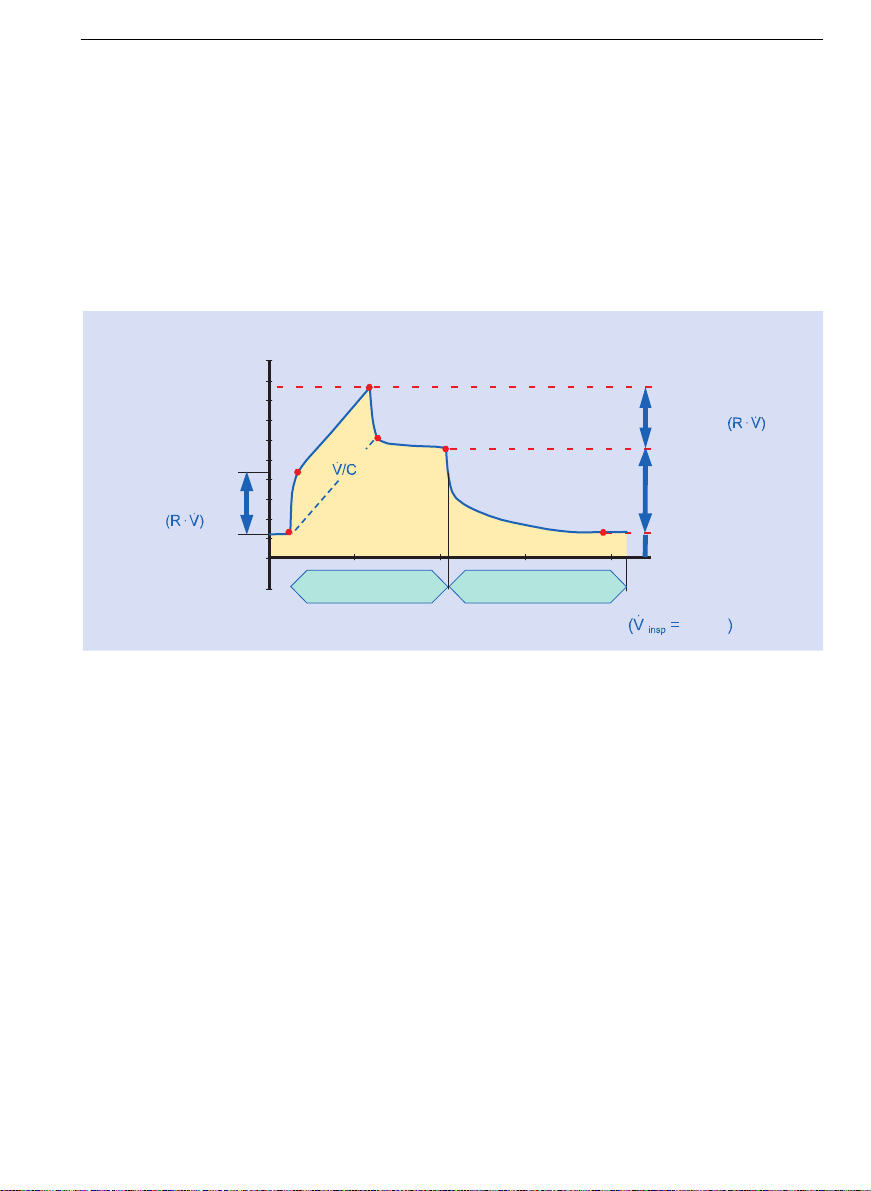
Pressure-time diagram
Volume-controlled, constant flow
The pressure-time diagram shows the gradual
changes in the airway pressure. Pressure is given in
mbar (or in cmH
2
O,) and time in seconds.
At a preset volume (volume-controlled ventilation)
and constant flow the airway pressure depends on the
alveolar pressure and the total of all airway
resistances, and can be affected by resistance and
compliance values specific to the ventilator and the
lung. As the ventilator values are constant, the
pressure-time diagram allows conclusions to be drawn
about the status of the lung and changes to it.
The gradual changes in
pressure, flow and volume
depend to an equal extent
on the properties and
settings of the ventilator, as
well as on the respiratory
properties of the lung.
Page 5
Ventilation curve pattern 7
Resistance = airway resistance
Compliance = compliance of the entire system
(lungs, hoses etc.)
At the beginning of inspiration the pressure between
points A and B increases dramatically on account of
the resistances in the system. The level of the pressure
at break point B is equivalent to the product of
resistance R and flow (
*).
∆p = R ∗*
This relationship, as well as the following examples, is
only valid if there is no intrinsic PEEP. The higher the
selected Flow * or overall resistance R, the greater
the pressure rise up to point B. Reduced inspiratory
flow and low resistance values lead to a low pressure
at point B.
Pressure
(mbar)
Time (s)
Resistance
Pressure
Plateau pressure
Pausephase
Gradient
Peak pressure
"Resistance
pressure"
"Compliance
pressure"
(V
T
/C)
Inspiration time
"PEEP"
A
Flowphase
B
C
D
E
F
Expiration time
const.
Pressure-time diagram for
volume controlled constant
flow ventilation.
Page 6
Ventilation curve pattern8
After point B the pressure increases in a straight line,
until the peak pressure at point C is reached. The
gradient of the pressure curve is dependent on the
inspiratory flow * and the overall compliance C.
∆p/∆t = * / C
At point C the ventilator applies the set tidal volume
and no further flow is delivered (* = 0).
As a result, pressure p quickly falls to plateau
pressure. This drop in pressure is equivalent to the
rise in pressure caused by the resistance at the
beginning of inspiration. The base line between points
A and D runs parallel to the line B - C.
Further on there may be a slight decrease in
pressure (points D to E). Lung recruitment and leaks
in the system are possible reasons for this. The level of
the plateau pressure is determined by the compliance
and the tidal volume. The difference between plateau
pressure (E) and end-expiratory pressure F (PEEP) is
obtained by dividing the delivered volume V
T
(tidal
volume) by compliance C.
∆P = P
plat
- PEEP
By reversing this equation the effective compliance
can easily be calculated.
C = V
T
/∆p
The level of the plateau
pressure is determined by
the compliance and the tidal
volume.
Page 7
Ventilation curve patterns 9
During the plateau time no volume is supplied to the
lung, and inspiratory flow is zero. As already
mentioned, there is a displacement of volume on
account of different time constants, and this results in
pressure compensation between different
compartments of the lung.
Expiration begins at point E. Expiration is a passive
process, whereby the elastic recoil forces of the thorax
force the air against atmospheric pressure out of the
lung. The change in pressure is obtained by
multiplying exhalation resistance R of the ventilator by
expiratory flow *
exp
.
∆p = R ∗*
exp.
Once expiration is completely finished, pressure once
again reaches the end-expiratory level F (PEEP).
Pressure-oriented
In pressure-oriented ventilation (e.g. PCV/BIPAP) the
pressure curve is quite different.
PCV
T
insp
T
exp.
P
insp.
PEEP
BIPAP
Pressure-time diagramm
for pressure controlled
ventilation.
Page 8

Ventilation curve pattern10
Pressure increases rapidly from the lower pressure
level (ambient pressure or PEEP) until it reaches the
upper pressure value P
Insp.
and then remains constant
for the inspiration time T
insp.
set on the ventilator.
The drop in pressure during the expiratory phase
follows the same curve as in volume-oriented
ventilation, as expiration is under normal conditions a
passive process, as mentioned above. Until the next
breath pressure remains at the lower pressure level
PEEP.
As pressure is preset and regulated in the case of
pressure-oriented ventilation modes such as BIPAP,
pressure-time diagrams show either no changes, or
changes which are hard to detect, as a consequence of
changes in resistance and compliance of the entire
system.
As a general rule it can be said that the pressure
curves displayed reflect the development of pressure
measured in the ventilator. Real pressures in the lung
can only be calculated and assessed if all influential
factors are taken into account.
Flow-time diagram
The flow-time diagram shows the gradual changes in
the inspiratory and expiratory flows *
insp
and *
exsp
respectively. Flow is given in L/min and time in
seconds. The transferred volume is calculated as the
integration of the flow * over time, and is thus
equivalent to the area underneath the flow curve.
During inspiration the course of the flow curve is
dependent on or at least strongly influenced by the
ventilation mode set on the ventilator. Only the
course of the flow in the expiratory phase permits
conclusions to be drawn as to overall resistance and
compliance of the lung and the system.
The course of the flow in the
expiratory phase permits
conclusions to be drawn as
to overall resistance and
compliance of the lung and
the system.
Page 9
Ventilation curve pattern 11
In normal clinical practice constant flow and
decelerating flow have become established as the
standard forms for ventilator control.
As yet there has been no evidence to suggest that
particular therapeutic success could be achieved
using other flow forms.
In the case of constant flow the volume flow rate
during inspiration remains constant throughout the
entire flow phase. When inspiration starts the flow
value very quickly rises to the value set on the
ventilator and then remains constant until the tidal
volume V
T
, likewise set on the ventilator, has been
delivered (this is the square area under the curve.) At
the beginning of the pause time (plateau time) the
flow rapidly returns to zero. At the end of the pause
time expiratory flow begins, the course of which
depends only on resistances in the ventilation system
and on parameters of the lung and airways. Constant
flow is a typical feature of a classic volume-oriented
mode of ventilation.
Flow
Time
T
plat
T
insp
Flow
Time
decelerating Flowconstant Flow
Flow-time diagram
Page 10

Ventilation curve pattern12
In decelerating flow the flow falls constantly after
having reached an initially high value. Under normal
conditions the flow returns to zero during the course
of inspiration. Decelerating flow is a typical feature of
a pressure-oriented ventilation mode.
The difference in pressure between the pressure in
the lung (alveoli) and the pressure in the breathing
system, maintained by the ventilator at a constant
level, provides the driving force for the flow.
As the filling volume in the lung increases the
pressure in the lung also rises. In other words,
the pressure difference and thus the flow drop
continuously during inspiration. At the end of
inspiration the pressure in the lung is equal to the
pressure in the breathing system, so there is no
further flow.
If at the end of inspiration and at the end of
expiration flow =0, compliance can also be calculated
in a pressure-oriented ventilation mode using the V
T
measured by the ventilator.
C = V
T
/ ∆P
where ∆P = P
insp.
- PEEP
Volume-time diagram
The volume-time diagram shows the gradual changes
in the volume transferred during inspiration and
expiration. Volume is usually given in ml and time in
seconds.
During the inspiratory flow phase the volume
increases continuously. During the flow pause
(plateau time) it remains constant as there is no
further volume entering the lung. This maximum
volume value is an index of the transferred tidal
At the end of inspiration the
pressure in the lung is equal
to the pressure in the
breathing system, so there is
no further flow.
Page 11
Ventilation curve patterns 13
volume and does not represent the entire volume in
the lung. The functional residual capacity (FRC) is
not taken into account. During expiration the
transferred volume decreases as a result of passive
exhalation.
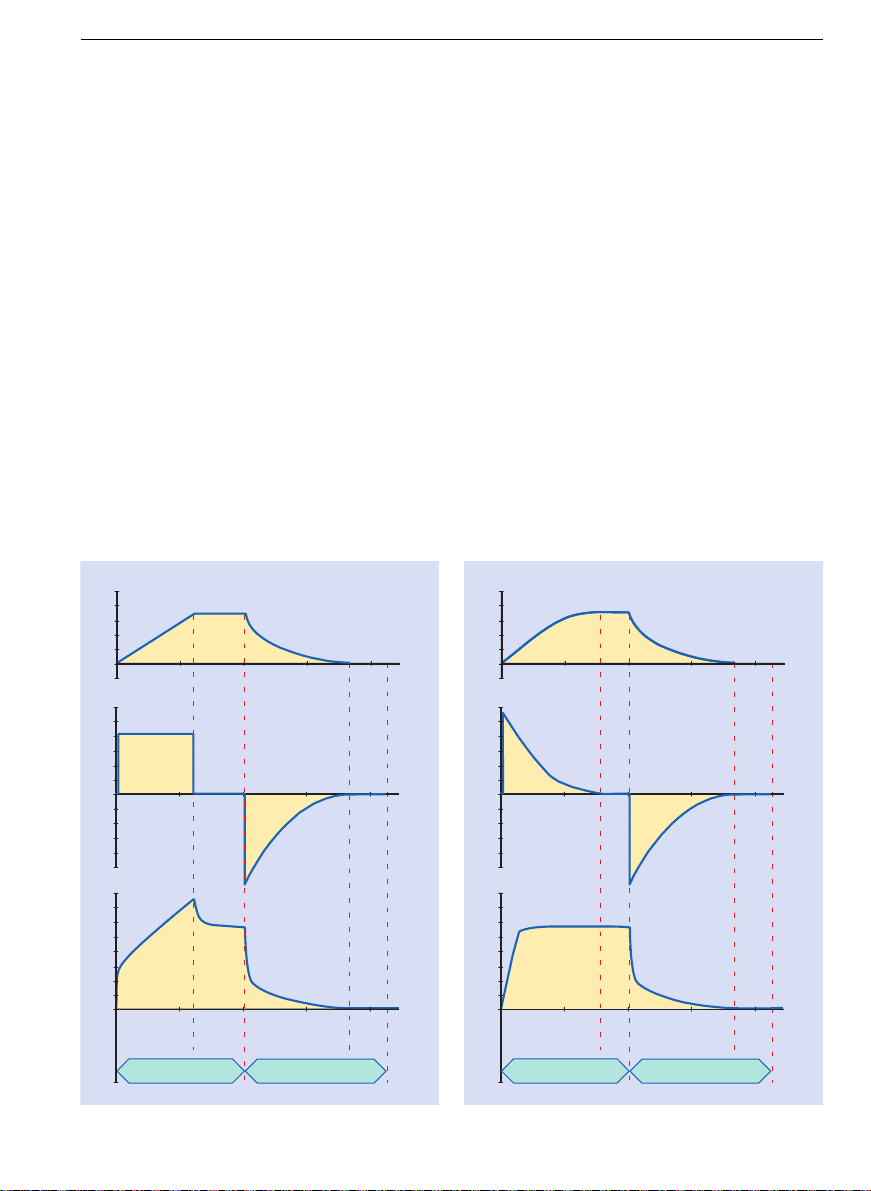
The relationships between pressure, flow and
volume are particularly obvious when these
parameters are all displayed at the same time.
Pressure, flow and volume
diagram of volume-oriented
and pressure-oriented
ventilation
Pressure
Flow
Volume Pressure oriented
Flow-phase
Pausephase
Inspiration Expiration
Flow-phase
phase
Time
Time
Time
Pause-
Pressure
Time
Flow
Time
Volume Volume oriented
Time
Inspiration Expiration
Flow-phase
Pausephase
Pausephase
Flow-phase
Page 12
Ventilation curve pattern14
Changes in compliance
When compliance changes the plateau and peak
pressures change by the same amount of the pressure
difference ∆p.
increasing compliance → plateau and peak pressures
fall
decreasing compliance → plateau and peak pressures
rise
Paw
Pressure
Time
Interpretation of curve
patterns
Page 13
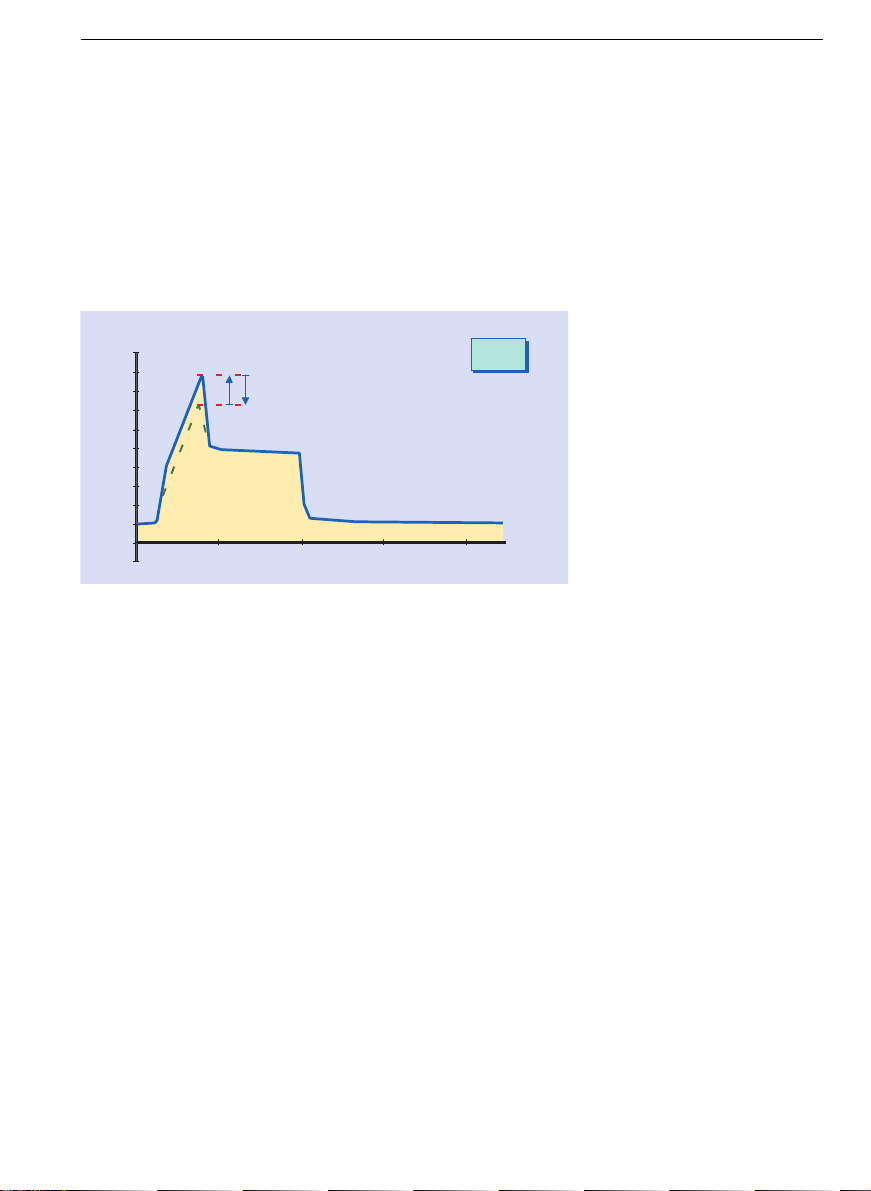
Ventilation curve pattern 15
Changes in inspiratory airway resistance
When the inspiratory airway resistance changes the
peak pressure changes and the plateau pressure
remains the same.
increasing resistance → peak pressure rises
decreasing resistance → peak pressure falls
The expiratory lung resistance cannot be seen on
the pressure curve as the alveolar pressure would
need to be known. Conclusions can be drawn however
from the expiratory f low curve (see «Flow curve at
increased expiratory resistances»).
p
peak
Paw
Time
Pressure
The expiratory lung
resistance cannot be seen
on the pressure curve as
the alveolar pressure would
need to be known.
Page 14
Ventilation curve pattern16
Spontaneous breathing
During a ventilator breath the patient will try to
breathe spontaneously, and will «fight» against the
machine. Reducing the amount of time for inspiration
or, even better, changing to a mode of ventilation
where the patient is allowed to breathe spontaneously
even during a mandatory breath, is an option worth
thinking about. BIPAP or AutoFlow
®
are examples of
suitable modes.
Paw
Pressure
Time
Inspiration Expiration
Page 15
Ventilation curve pattern 17
Adaptation of the flow curve
In volume-controlled modes of ventilation, AutoFlow
®
results in automatic flow adaptation with the aim of
applying the set tidal volume at the lowest possible
airway pressure. The constant flow typical of volumeoriented ventilation modes (square) becomes at the
same time a decelerating flow form, while tidal
volume remains constant even if the compliance in
the patient’s lung changes.
Pressure limitation at a constant tidal volume can
also be achieved in Dräger ventilators by using the
P
max
setting. If the compliance of the patient changes
this set value may need to be checked and reset.
automatic flow adaption in
pressure-oriented ventilation mode
PCV, BIPAP and in volume-oriented
mode with Autoflow
®
Flow
Time
Flow
Page 16
Ventilation curve pattern18
The flow curve in the case of insufficient inspiration time
If the flow does not return to zero during inspiration
this means that the inspiration time is insufficient to
apply the volume which could be achieved for the set
pressure.
T
I
Flow does not return
to zero during inspiration
Time
Flow
Flow
Page 17
Ventilation curve pattern 19
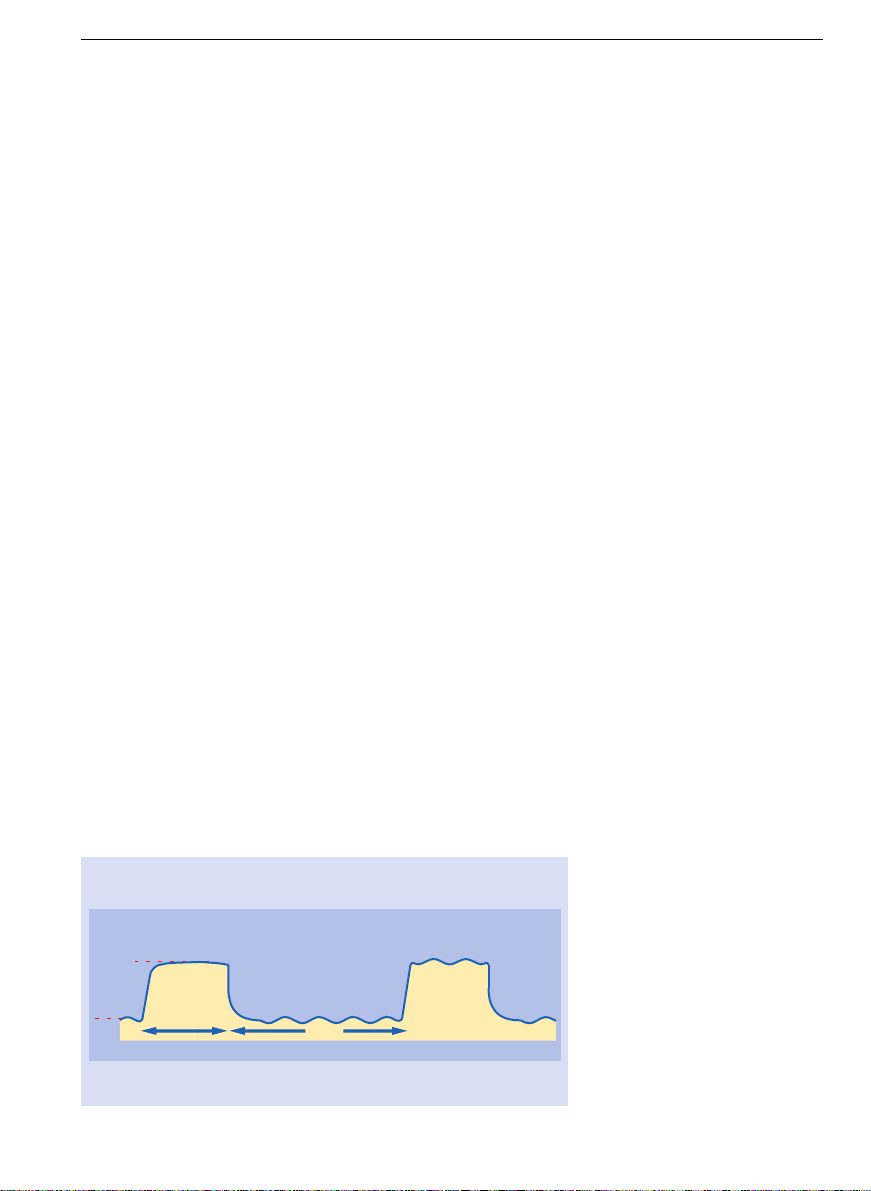
The flow curve in the case of insufficient expiration time
If the flow does not return to zero during expiration,
the expiration time is not sufficient for full expiration.
This indicates the presence of an intrinsic PEEP.
This results in an increase in lung pressure in the
case of volume-controlled ventilation.
In Evita ventilators it is possible to measure
intrinsic PEEP and trapped volume directly. An
intrinsic PEEP can have considerable effects on the
exchange of gases and pulmonary blood circulation.
In some applications, however, there may be
attempts to establish an intrinsic PEEP on purpose
(Inverse Ratio Ventilation IRV), due to the fact that
this will probably then only occur in certain desired
sections of the lung, while a PEEP set on the ventilator
will affect the entire lung.
T
E
Expiration flow does
not return to zero
Flow
Time
Flow
In Evita ventilators it is
possible to measure intrinsic
PEEP and trapped volume
directly.
Page 18
Ventilation curve pattern20
Flow curve in the case of increased expiratory resistances
A more gentle expiratory flow curve indicates
increased expiratory resistances which may be caused
by expiratory filters which have become damp or
blocked as a result of nebulization. This may lead to a
considerable increase in expiration time and a
deviation from the set PEEP value.
Flow
Time
Flow
Page 19

21
Loops – a good thing all round
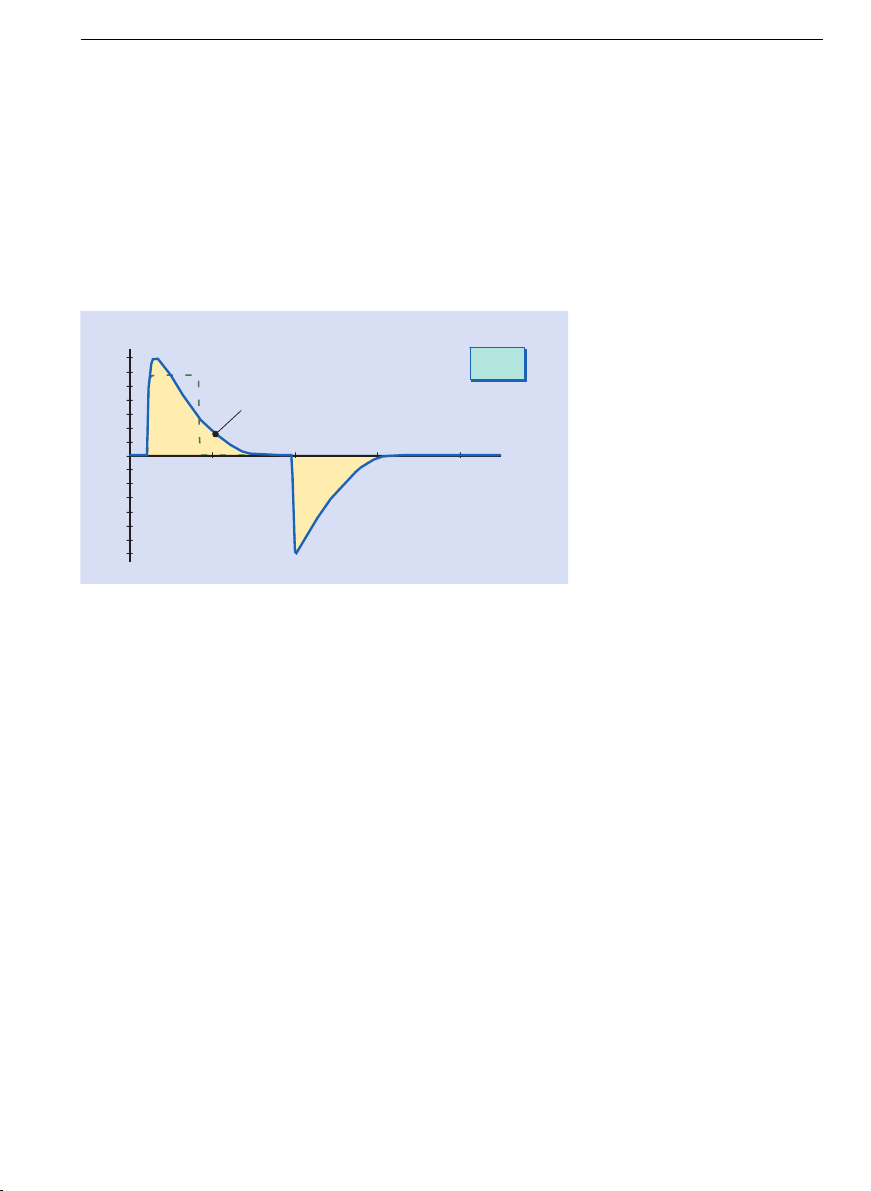
The static PV loop (classic)
The static PV loop (pressure-volume curve) is obtained
as a result of the «super-syringe» method, and is used
predominantly in scientific papers [1]. Most of what is
known about the PV loop is thus based on this method.
The most important feature of this PV loop is that the
individual points of measurement (pressure and
volume) are recorded when breathing gas flow = 0.
Using a super-syringe, the volume in the lung is
increased step by step. A few seconds after each
increase in volume the resulting pressure is measured
[2]. By connecting the individual points the PV loop is
created.
PV Loops
Pressure
[mbar]
V
Points of measurement
classic PV-Loop
continuous pressure
measurement
PV-Loop measured by
«super-syringe» method.
Page 20

Loops – a good thing all round22
The static PV loop (classic)
V
Pressure
[mbar]
IPPV
Ppeak
PEEP
t
P
A B C
BIPAP
Pinsp.
PEEP
t
P
upper "Inflection Point"
lower "Inflection Point"
Page 21

Loops – a good thing all round 23
The relationship of volume to pressure reflects
compliance (C = ∆V / ∆P). Thus the PV loop shows how
compliance develops as volume increases. The lower
and upper inflection points can be taken from the PV
loop. When the super-syringe method is used the
volume measured value does not return to zero during
expiration, but the reasons for this are as yet not
entirely clear. However, errors in measurement and
oxygen consumption during measurement play a
significant role [2].
In the lower section (A) the pressure per volume
increase rises particularly rapidly and only continues
in a straight line (B) once a lung-opening pressure
(lower inflection point) has been exceeded. If the lung
reaches the limits of its compliance, the rise in
pressure per volume increase becomes bigger again
(upper inflection point) (C).
It is generally accepted that ventilation should take
place as far as possible within the linear compliance
area (B), as dangerous shear forces occur as a result
of the collaborating and reopening of individual areas
of the lung. The lower inflection point can be
overcome by setting a PEEP. The ventilation volume
(in IPPV/CMV, SIMV) or inspiratory pressures (in
BIPAP, PCV) must then be selected such that the upper
inflection point will not be exceeded.
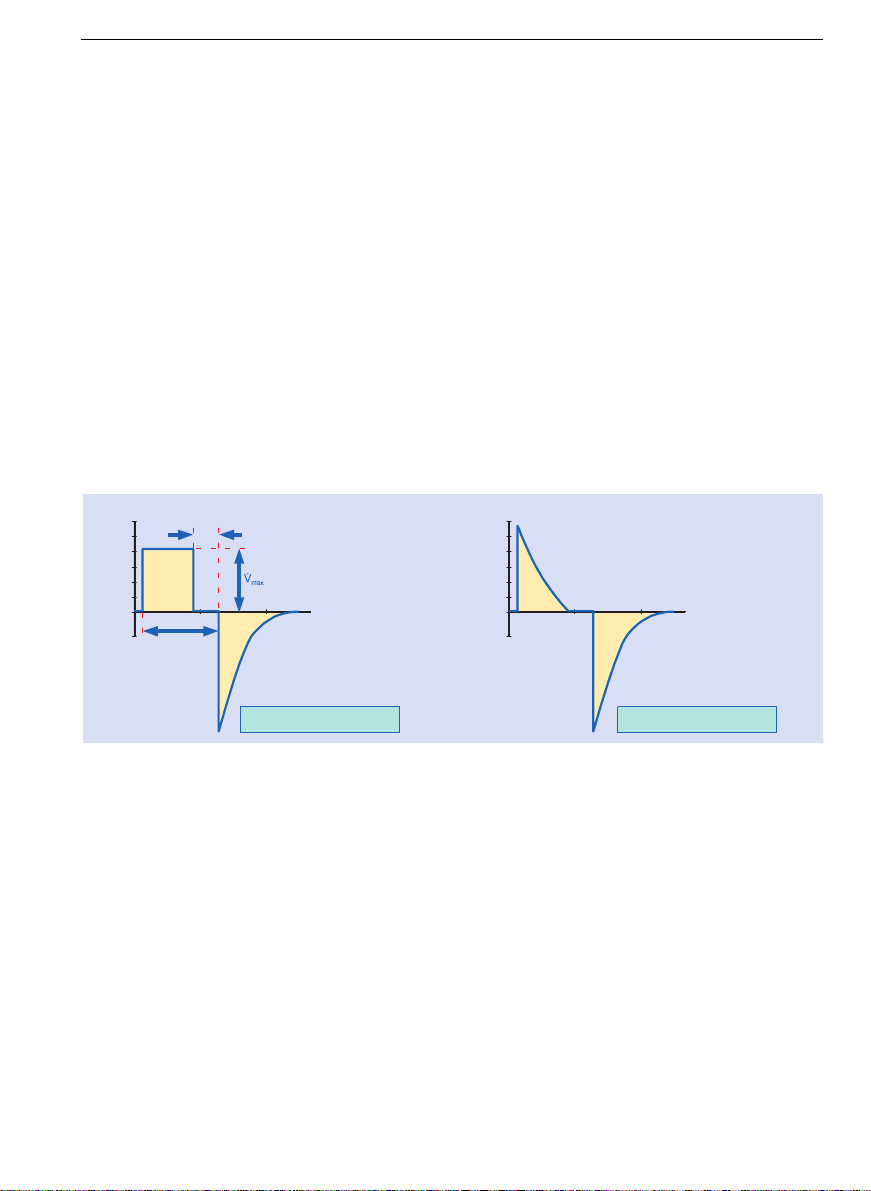
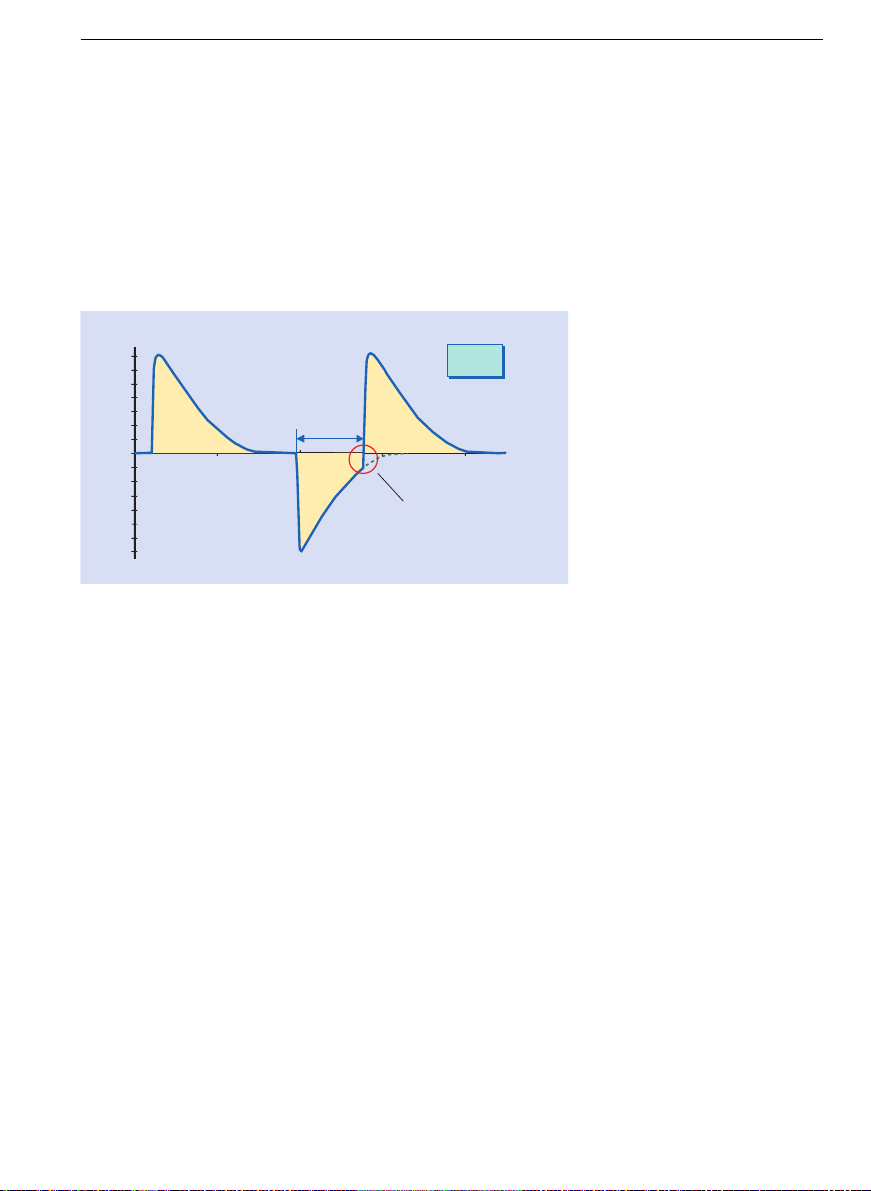
Dynamic PV loops in ventilation
PV loops which are generated during ventilation
do not fulfil the condition that at the time when
the individual measured values are recorded the
breathing gas flow should equal zero. The breathing
gas flow generates an additional pressure gradient
due to the inherent resistances like tube, airways etc.
(see also page 7).
PV-Loop with upper and
lower inflection point.
Page 22

Loops – a good thing all round24
For this reason the PV loop does not give an accurate
picture of the course of compliance. The greater the
inspiratory breathing gas f low the greater the
additional pressure gradient and thus the degree of
inaccuracy.
Pressure
[mbar]
V
Ventilator
static
PV-loop
Ventilator
pressure
pressure
behind tube
drop in pressure
due to tube
drop in pressure
due to airways
resistance
Pressure
[mbar]
V
static
PV-loop
PV-loop recorded
by the ventilator
(Flow 30 L/min)
PV-loop recorded
by the ventilator
(Flow 80 L/min)
Page 23

Loops – a good thing all round 25
Since ventilators open the exhalation valve either to
ambient pressure or set PEEP at the beginning of
expiration, the pressure displayed by the PV loop also
falls almost immediately to this value.
In the static PV loop, on the other hand, the
reduction is again a gradual process.
As regards the PV loop obtained for controlled
ventilation it can generally be said that the slower the
lung is filled the better the rising branch reflects the
course of compliance.
A number of studies and publications have shown that
PV loops recorded during the course of ventilation
correlate well with loops from standard procedures, so
long as the inspiratory flow is constant [3]. The
studies are based on the assumption that the drop in
pressure resulting from inspiratory resistances will
also remain constant at constant flow, and that the
steepness of the inspiratory loop will thus reflect only
the elastance of thorax and lung. Although as a result
the PV loop recorded by the ventilator is offset (the
rising branch shifts position), it otherwise retains its
original shape, on the basis of which conclusions can
be drawn about compliance.
This also shows that in ventilation modes with
decelerating flow (BIPAP, PCV etc.) it is not possible to
draw conclusions from the PV loop concerning the
development of compliance of the lung.
In ventilation modes with
decelerating flow (BIPAP,
PCV etc.) it is not possible to
draw conclusions from the
PV loop concerning the
development of compliance
of the lung.
Page 24

Loops – a good thing all round26
Volume-controlled ventilation with constant flow
During inspiration the lung is filled with a preselected
constant flow of gas, during which process the
pressure in the breathing system gradually increases.
The pressure in the lung increases to the same extent
and, at the end of inspiration, reaches the same value
as the pressure in the breathing system (plateau
pressure).
During expiration the ventilator opens the
exhalation valve wide enough to maintain the level of
PEEP set. Due to the pressure difference, which is
now inverted (pressure in the lung greater than PEEP
pressure), the breathing gas now flows out of the lung
and the lung volume slowly falls. This is why PV loops
during controlled ventilation run anti-clockwise.
Interpretation of PV loops in
ventilation.
Inspiration
Expiration
Pressure
PV-Loop
Volume
Page 25

Loops – a good thing all round 27
Pressure-controlled ventilation (decelerating flow)
Even during pressure-controlled ventilation the
PV loops run anti-clockwise. However, in this case the
lung is not filled with an even gas flow. At the
beginning of inspiration the ventilator generates a
greater pressure in the ventilation system than in the
lung, which is then kept constant by the ventilator
throughout the entire inspiration. As a result of this
difference in pressure air flows into the lung and the
volume of the lung slowly increases. As the volume
increases the pressure in the lung also rises and the
difference between the lung pressure and the pressure
in the breathing system becomes smaller.
Pressure
Time
Flow
Time
Pressure difference in
ventilation system and lung
Pressure in the
ventilation system
Pressure in
the lung
Page 26

Loops – a good thing all round28
Since due to the laws of physics the difference in
pressure determines the resulting breathing flow,
the breathing flow becomes ever smaller during
inspiration, thus creating a decelerating flow.
The pressure in the breathing system is kept at a
constant level by the ventilator throughout inspiration,
giving the PV loop during pressure-controlled
ventilation a more or less box-like shape.
Assumptions cannot be made on the basis of this loop
about the course of lung compliance. When the
breathing gas flow is equal to zero at the end of
inspiration, however, the steepness of a line drawn
between the start of inspiration (A) and the point at
the end of inspiration (B) does represent a measure of
dynamic compliance. This presupposes, however, that
flow equals zero both at the end of inspiration and at
the end of expiration.
Inspiration
Expiration
Pressure
PV-Loop
Volume
A
B
Page 27

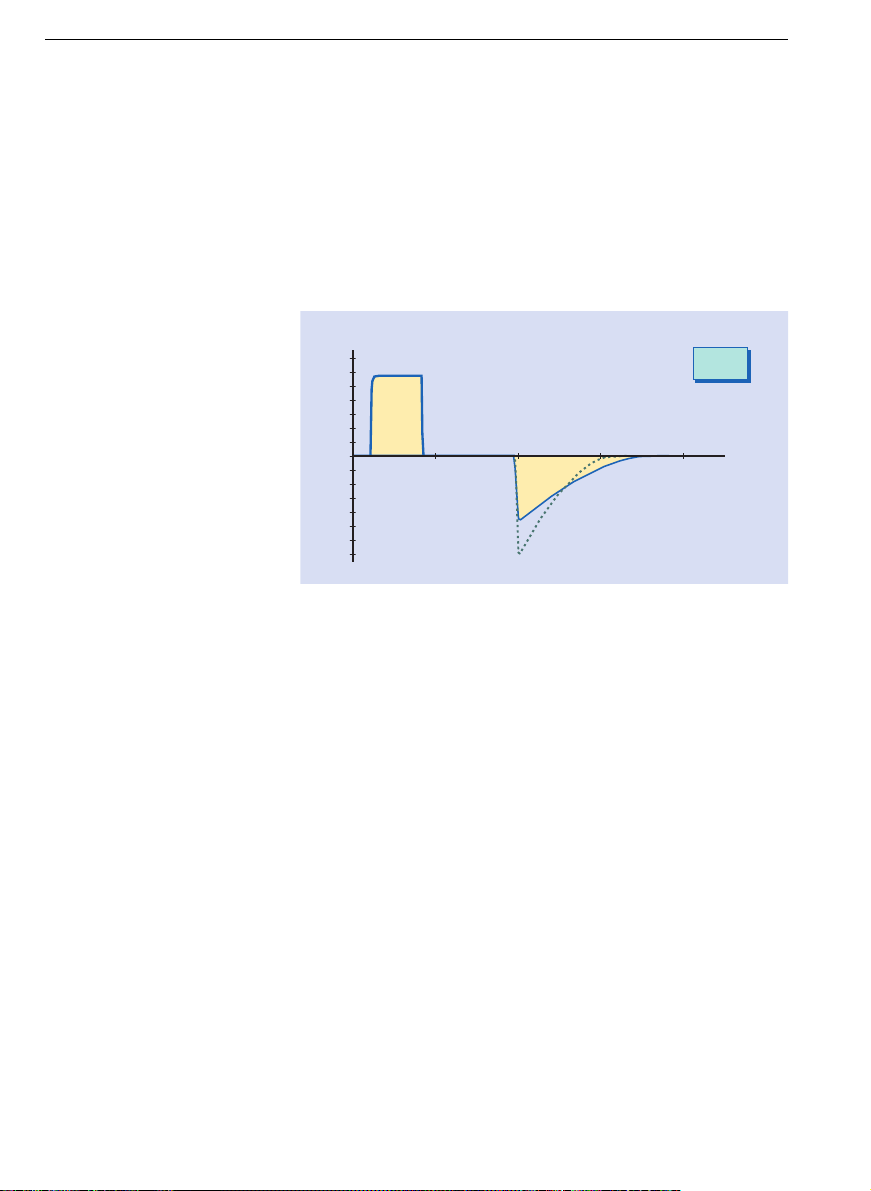
Loops – a good thing all round 29
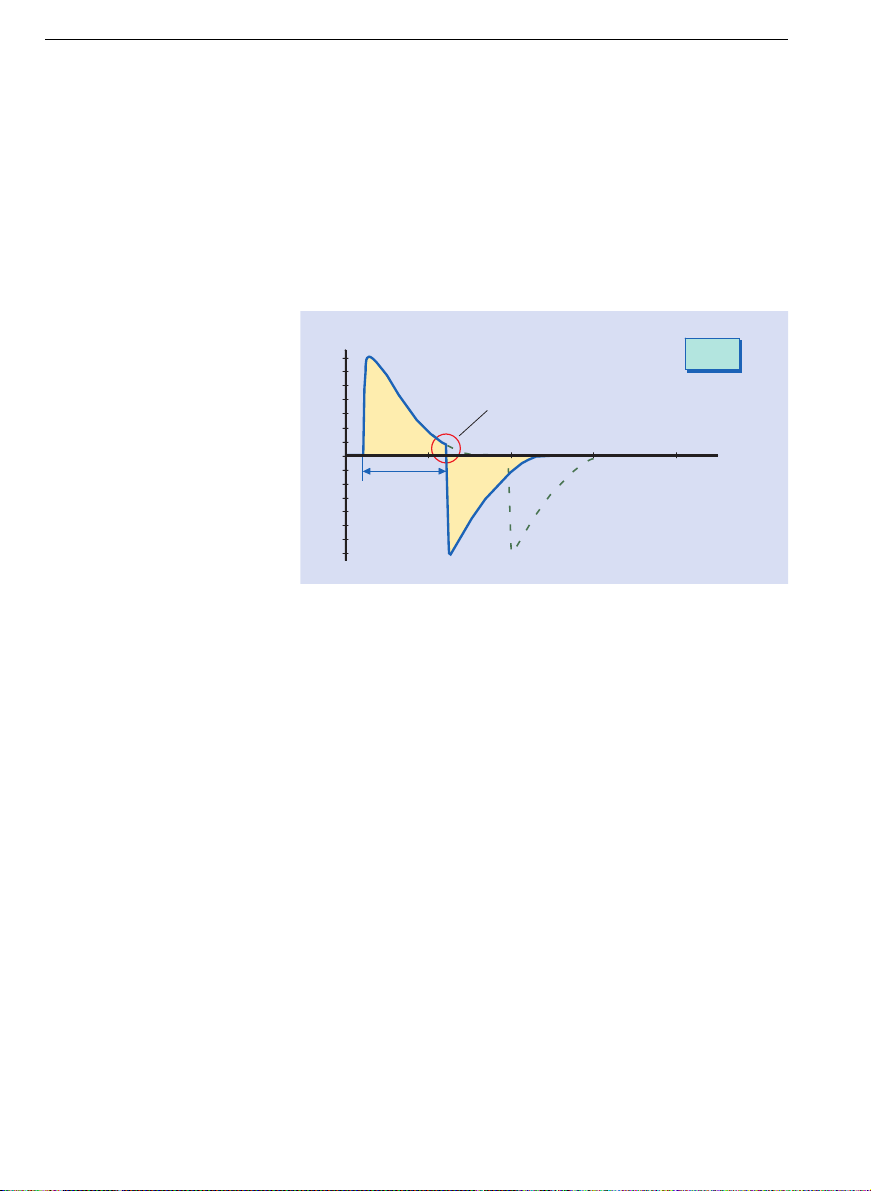
CPAP spontaneous breathing
In spontaneous breathing the PV loops run clockwise.
The patient’s inspiratory effort creates a negative
pressure in the lung, which then has an effect in the
breathing system where the pressure is measured by
the ventilator.
The ventilator always tries to supply the patient with
enough breathing gas to ensure that the set CPAP
pressure is maintained at a constant level, although a
slight negative deviation is inevitable. The area to the
left of an imaginary vertical axis (A) at the set CPAP
pressure is thus a measure of the patient’s efforts to
combat the inspiratory resistances of the ventilator.
Inspiration
Expiration
Pressure
PV-Loop
Volume
CPAP Pressure
(A)
Page 28

Loops – a good thing all round30
PV loop in CPAP with ASB/P.supp.
A characteristic feature of respiratory support
synchronized with the inspiratory effort of the patient
(ASB/P.supp., SIMV etc.) is a small twist just above the
zero point. The patient first generates a negative
pressure in the lung. Once the trigger threshold has
been passed, however, the ventilator generates a
positive pressure in the breathing system. The area to
the left of the vertical axis which is enclosed by the
small twist (A) is a measure of how much work the
patient needs to do to trigger the ventilator. The area
to the right of the axis (B) represents the work done by
the ventilator to support the patient, in so far as the
patient only triggers and does not actually breathe as
well.
Inspiration
Expiration
A
B
Pressure
PV-Loop
Volume
Page 29

Loops – a good thing all round 31
PV loops in the case of compliance changes
As compliance decreases, in other words as the lung
becomes less elastic, and the ventilator settings
remain the same, the PV loop in volume-controlled
ventilation takes an increasingly flat course.
The change in steepness of the inspiratory branch
of the PV loop is proportional to the change in lung
compliance.
Pressure
PV-Loop
Volume
The change in steepness
of the inspiratory branch of
the PV loop is proportional
to the change in lung
compliance.
Page 30

Loops – a good thing all round32
PV loops in the case of resistance changes
If resistance changes during constant flow ventilation
the steepness of the right branch of the loop remains
unchanged, but changes position.
PV loop section reflecting lung over-extension
If during constant flow ventilation the loop starts
to become flatter in the upper part of the inspiratory
branch, then this could be an indication of overextension of certain areas of the lung. See also
«The static PV loop».
PV-Loop
Volume
Pressure
PV-Loop
Volume
Pressure
change in
lung compliance
Page 31

Loops – a good thing all round 33
PV loop in ASB/P.supp.
If during ASB/P.supp. the patient is only able to
manage the trigger impulse and then does not
continue to breathe, then only a volume equal to the
support pressure in accordance to current lung
compliance will be reached. However, if the patient
continues an inspiratory effort throughout the entire
support phase then he or she will be able to inhale
greater volumes, whilst the support pressure
remaining unchanged.
A change in the height of the PV loop is thus a
measure of the strength of the patient’s inspiratory
effort.
A patient is only prompted to make an inspiratory
effort if the tidal volume which can be achieved by the
set pressure support (without the patient’s own
breathing) is smaller than the patient’s individual
needs. On the other hand, the support pressure should
at least compensate for the artificial airway
resistances (tube) (see also «PV loops before and after
the tube»).
PV-Loop
with patient's
own breathing
without patient's
own breathing
Pressure
Volume
Page 32

Loops – a good thing all round34
PV loops before and after the tube
The PV loop measured by the ventilator gives only half
the picture. As described in the section «dynamic PV
loop», further pressure drops occur after the point
where the ventilator takes the pressure measurement
(Y-piece) e.g. across the tube length and the physiological airways.
PV loop in CPAP before and after the tube
The PV loop displayed by the ventilator shows a narrow
loop for purely spontaneous patient breathing at an
increased pressure level (CPAP). The narrower the
area to the left of the vertical axis, the less additional
work of breathing needs to be done to combat the
ventilator’s inspiratory resistances. The area to the
right of the axis, on the other hand, is only determined by the expiratory resistances of the ventilator.
The entire area which the loop encompasses is thus
at the same time a measure of the quality of the
ventilator, although it should be remembered that for
the purposes of a direct comparison of ventilators the
same system of measurement needs to be used for all
ventilators, since the specifications of the various
systems may differ considerably from one another. A
further consideration is the fact that some ventilators
apply a small additional support pressure (some
3 mbar) even when no support pressure has been set,
thus making a direct comparison no longer possible.
The narrower the area to the
left of the vertical axis, the
less additional work of
breathing needs to be done
to combat the ventilator’s
inspiratory resistances.
Page 33

Loops – a good thing all round 35
The belief that a narrow PV loop is synonymous with
less work of breathing for the patient is not correct in
every case.
A comparison with a loop recorded directly after
the tube shows that this loop covers a considerably
greater area. Due to the comparatively small diameter
of the tube the patient must do considerably more
work of breathing.
PV-Loop
Area determined
by the expiratory
resistances of
the ventilator
work of
breathing due
to the ventilator
Pressure
Volume
CPAPlevel
Page 34

Loops – a good thing all round36
The smaller the tube diameter the more the patient
has to work to combat the tube’s resistance [4], a fact
which is shown by the different area covered by the
loops recorded after the tube.
A PV loop taken downstream from pathologically
increased airway resistances would cover an even
greater area.
Volume
Pressure
[mbar]
Ventilator
Pressure measurement
ventilator
Pressure after
the tube
Pressure after
pathologically
increased airway
resistances
Volume
Pressure
[mbar]
ETT8
ETT6,5
PV-loop ventilator
ETT8 = ETT6,5
CPAPlevel
PV-loop recorded after
the tube by use of
different tube diameters
Page 35

Loops – a good thing all round 37
Assistance from pressure support (ASB)
Increased airway resistances, whether caused by
disease or intubation, thus result in increased work of
breathing for the patient.
The reason for setting assisted spontaneous breathing (ASB/P.supp.) is generally to try to compensate for
these airway resistances. A comparison with loops
recorded during CPAP shows that the area of the loop
taken after the tube can also be reduced with
ASB/P.supp.
If the inspiratory branch of the loop lies exactly on the
vertical line of the CPAP set value, the tube resistance
will only just be compensated for. If the inspiratory
branch lies to the right of the CPAP line then support
is provided above and beyond merely compensating for
the tube resistance, thus compensating for possible
pathological resistances in the lower airways. If the
Volume
Pressure
[mbar]
CPAPlevel
ASBlevel
Ventilator
Page 36

Loops – a good thing all round38
support pressure is inadequate and the patient is
being forced to inhale, however, negative pressure
may still occur at the distal end of the tube.
Unfortunately, the PV loop at the distal end of the
tube is not usually available. Taking a pressure
measurement at the tip of the tube is also extremely
prone to errors due to the collection of secretion and
mucous etc. An incorrect measurement could then
easily result in misinterpretations.
However, research is underway to find ways to
improve this situation.
For the time being we have to estimate the
optimal pressure support to compensate for airway
resistances.
Loops – other possibilities
In addition to pressure-volume (PV) loops, other
combinations of parameters are also possible. Some of
these are already used in pulmonology but are not
particularly widespread in intensive care medicine.
Some diagnostic procedures require the patient’s
cooperation.
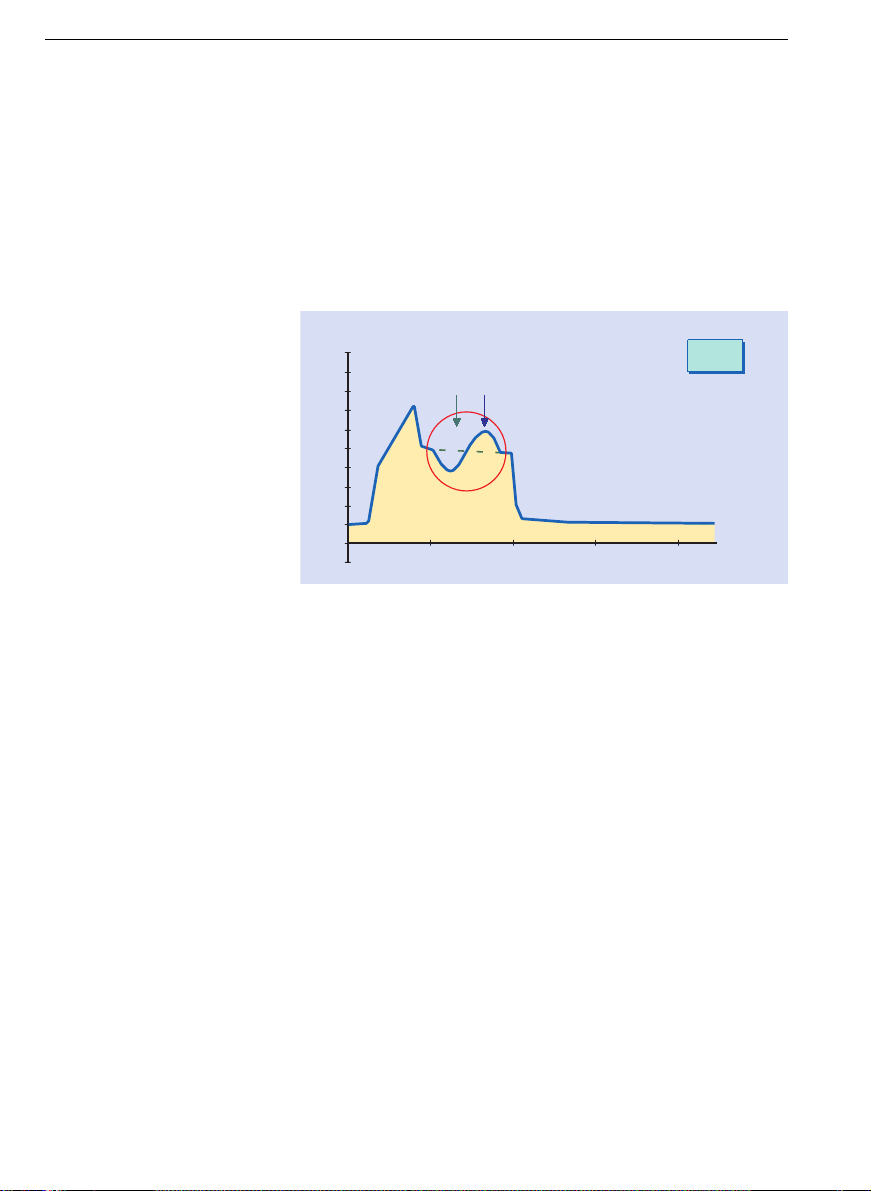
Flow-volume loop
The flow-volume loop is occasionally used to obtain
information about airway resistance, when aspiration
should be carried out and about the patient’s reaction
to bronchial therapy.
Increased airway resistances as a result of sputum
etc. can in many patients be recognized by a sawtoothed-shape loop. A smoother loop then verifies that
measures such as suctioning which have been taken
to improve airway resistance have been successful. [5]
In patients with obstructive diseases the expiratory
branch of the loop only changes shape when the set
Page 37

Loops – a good thing all round 39
PEEP is greater than intrinsic PEEP. The fact that the
shape of the loop does not change, however, does not
necessarily have anything to do with flow limitation.
[1]
Flow-Volume-Loop
Volume
Volume
Flow
Page 38

40
Trends reviewed
Graphic trend displays enable ventilation processes to
be assessed at a later stage, with the development of
continuously measured values displayed in graphic
form. Trend displays may be of interest in a variety of
different applications, and each application will
require a different period of observation. For instance,
for assessing a process of weaning, several days or
even weeks will need to be displayed in one diagram,
while an event which occurs suddenly calls for as
much detail as possible to be shown in the diagram.
The areas of application for trend displays in ventilation
are extremely varied due to the wide range of possible
combinations of the individual parameters. The
following are just a few examples, designed to make
the reader think of further possible applications.
Page 39

Trends reviewed 41
Documentation of a weaning process
In the above trend it can be seen how the SIMV frequency was gradually reduced. Each time the frequency
was reduced there was a drop in minute volume (MV),
although this drop was compensated for after a short
time by the MV (MVspont.) spontaneously breathed by
the patient.
[1/min]
20
0
14.06. 1996 06:40 (8 h) 14.06. 1996 10:40 14.06. 1996 14:40
f
[L/min]
15
0
14.06. 1996 06:40 (8 h) 14.06. 1996 10:40 14.06. 1996 14:40
MV
MV
[L/min]
15
0
14.06. 1996 06:40 (8 h) 14.06. 1996 10:40 14.06. 1996 14:40
MVsp
Page 40

Trends reviewed42
The second trend display shows the further course of
the weaning process and its effects. Above a particular
IMV frequency this was kept constant and only the
pressure support was reduced. Initially this reduction
was also compensated for by the patient, though later
on a lasting reduction in MV can be seen, after which
the ventilator support was once again increased.
[mbar]
25
0
14.06. 1996 14:40 (8 h) 14.06. 1996 18:40 14.06. 1996 22:40
ASB
[L/min]
15
0
14.06. 1996 14:40 (8 h) 14.06. 1996 18:40 14.06. 1996 22:40
MV
MV
[L/min]
15
0
14.06. 1996 14:40 (8 h) 14.06. 1996 18:40 14.06. 1996 22:40
MVsp
Page 41

Trends reviewed 43
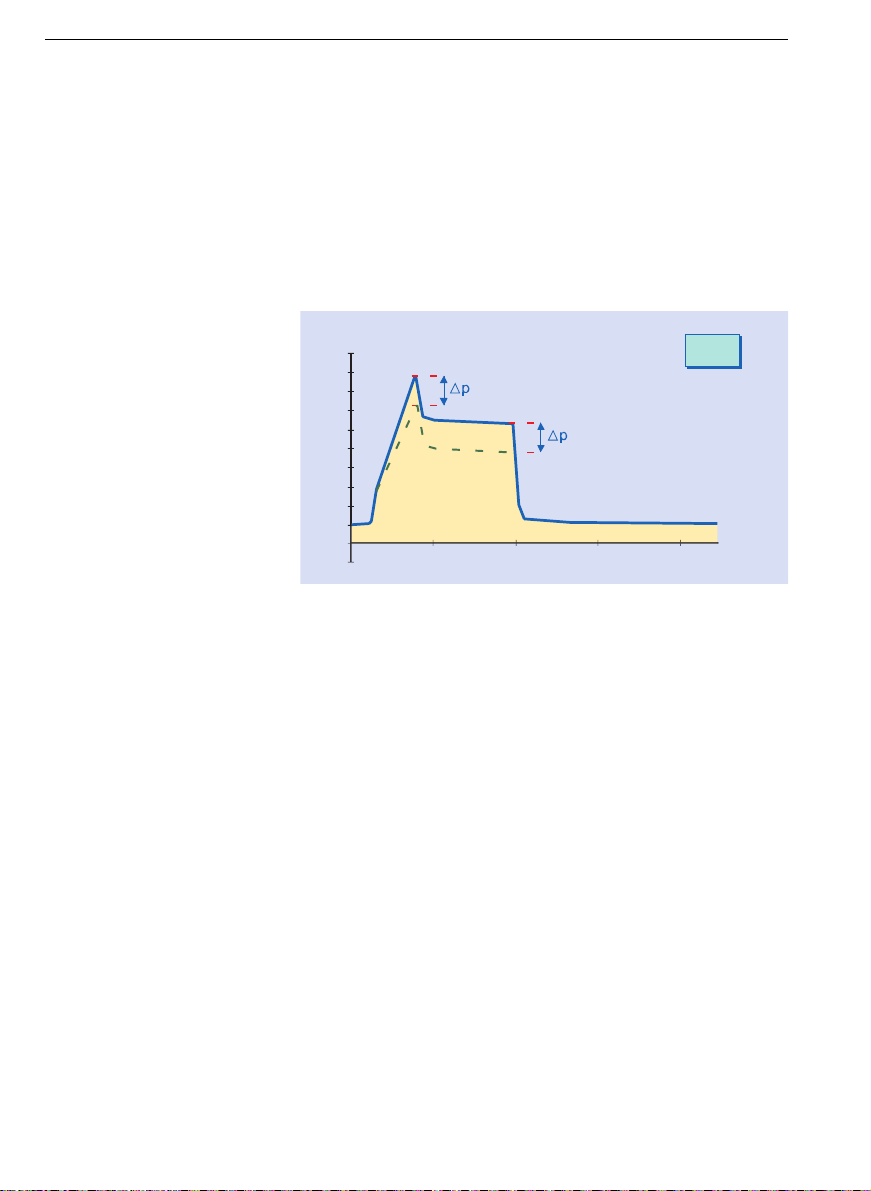
Lung parameters based on peak and plateau pressure
As already described in the chapter on curves, the
changes in peak pressure and plateau pressure allow
statements to be made about airway resistance and
lung compliance. Thus the trend display of both these
parameters is at the same time a trend of R and C.
If during volume-controlled ventilation without
pressure-limiting peak pressure (Ppeak) increases
while plateau pressure (Pplat) remains constant, then
this indicates an increase in airway resistance. This
may be caused among other things by constriction of
the airways by secretion on account of insufficient
aspiration.
If both peak pressure (Ppeak) and plateau pressure
(Pplat) increase, then this indicates falling compliance.
[mbar]
50
0
14.06. 1996 05:20 (2 days) 15.06. 1996 05:20 16.06. 1996 05:20
[mbar]
50
0
14.06. 1996 05:20 (2 days) 15.06. 1996 05:20 16.06. 1996 05:20
Pplat
[mbar]
50
0
14.06. 1996 05:20 (2 days) 15.06. 1996 05:20 16.06. 1996 05:20
PEEP
Ppeak
Resistance-increase Start of compliance-changes
Page 42

44
Capnography –
locating problem areas
Modern patient monitoring permits all kinds of
different data to be recorded, displayed and processed.
Depending on the parameters selected and the experience of the observer, a wide variety of ventilation
variables and the display of these variables in realtime curves allow conclusions to be drawn about the
patient’s status and the success of treatment.
Capnograms, as graphic representation of CO
2
partial pressure during a particular respiratory cycle
or as trend display of end-tidal CO
2
partial pressure
over a longer period of time, are often able to locate
problem areas. The cause of an unphysiological
capnogram might be anywhere along the route taken
by CO
2
through the human body, and in the case of
ventilation there are a number of other influential
factors as a result of medical intervention. The complex dependence of CO
2
concentration on metabolism,
circulatory parameters, gas exchange and ventilation
of the lung as well as on ventilator settings makes it
possible to monitor these functions simultaneously
and detect problems at an early stage. Considerable
imrovements as regards the patient’s safety can be
achieved using CO
2
measurement. On the other hand,
the causes of an unphysiological capnogram are often
so complex that interpretation is difficult.
CO
2
measurement often allows problems to be
detected at an early stage, but these problems then
have to be examined further using other means.
The ventilators of the Evita family use a main-
stream sensor close to the patient to measure CO
2
partial pressure during the inspiratory and expiratory
phases, then display the values in real-time curves
which allows the anatomic dead space and CO
2
production to be determined.
Page 43

Capnography – locating problem areas 45
The endtidal CO2partial pressure measured by the
ventilator is displayed and its development can then
be followed back over a long period of time in the
trend display.
The following pages include a physiological
capnogram and a selection of deviating CO
2
curve
shapes and trend displays with a short interpretation
and examples of possible causes.
Evita 2
CO
2
curve
CO2
etCO2 = 38 mmHg
VCO2 = 285 mL/min
Vds = 152 mL = 22 %
Ti : 1,2
adult
SIMV
20
40
60
80
t(s)
1 2 3
Page 44

Capnography – locating problem areas46
The physiological capnogram
A - B: Emptying of the upper dead space of the airways
The CO
2
concentration in this section of the curve
equals zero, as this is the first phase of expiration
during which air from the upper airways, which has
not been involved in the process of gas exchange, is
analysed.
B - C: Gas from the lower dead space and alveoli
The CO
2
concentration increases continuously, as the
air being analysed comes partly from the upper
airways and partly from the alveoli which are rich in
CO
2
.
C - D: Alveolar gas
This phase is described as the «alveolar plateau». The
curve rises very slowly. The air being analysed comes
mainly from the alveolar area.
D: Endtidal CO
2
partial pressure
Represents the highest possible concentration of
exhaled CO
2
and is reached at the end of expiration.
This point is described as endtidal CO
2
(etCO2) and
represents the final portion of air which was involved
in the exchange of gases in the alveolar area. It thus
represents under certain conditions a reliable index of
CO
2
partial pressure in the arterial blood.
Normal values for endtidal CO
2
concentration
approx. 5.0-5.3 %, 5.1-5.3kPa or 38-40 mmHg
D - E: Inspiration
The CO
2
concentration falls rapidly, as fresh gas not
containing CO
2
forces its way into the airways at the
beginning of inspiration.
Page 45

Capnography – locating problem areas 47
Paw
t
t
Flow
t
paCO
2
C
D
B
A
E
Page 46

Capnography – locating problem areas48
Exponential fall in pCO
2
Possible causes:
Cardiopulmonary bypass
Cardiac arrest
Pulmonary embolism
Large loss of blood
Sudden drop in blood pressure
20
6,0
8,0
10,0
40
60
80
4 8 12 s
(mmHg) (kPa)
etCO
2
CO2-curve shapes
0
4,0
2,0
20
2,0
4,0
6,0
8,0
10,0
40
60
80
10 20 30 min
(mmHg) (kPa)
etCO
2
CO2-trend display
0
Interpretations of
capnogram
Page 47

Capnography – locating problem areas 49
A persistently low pCO
2
Possible causes:
Hyperventilation as a result of high minute volume
Low body temperature
Following shock
20
2,0
4,0
6,0
8,0
10,0
40
60
80
4 8 12 s
(mmHg) (kPa)
etCO
2
CO2-curve shapes
0
20
2,0
4,0
6,0
8,0
10,0
40
60
80
10 20 30 min
(mmHg) (kPa)
etCO
2
CO2-trend display
0
Page 48

Capnography – locating problem areas50
A persistently low pCO
2
without plateau
Possible causes:
Insufficient alveolar ventilation
COPD
Obstruction of upper airways
Tube partly closed
20
2,0
4,0
6,0
8,0
10,0
40
60
80
4 8 12 s
(mmHg) (kPa)
etCO
2
CO2-curve shapes
0
20
2,0
4,0
6,0
8,0
10,0
40
60
80
10 20 30 min
(mmHg) (kPa)
etCO
2
CO2-trend display
0
Page 49

Capnography – locating problem areas 51
Sudden drop in pCO
2
to around zero
Possible causes:
Accidental extubation
Complete airway stenosis
Disconnection
Oesophageal intubation (drop after 1-2 tidal volumes)
20
2,0
4,0
6,0
8,0
10,0
40
60
80
4 8 12 s
(mmHg) (kPa)
etCO
2
CO2-curve shapes
0
20
2,0
4,0
6,0
8,0
10,0
40
60
80
10 20 30 min
(mmHg) (kPa)
etCO
2
CO2-trend display
0
Page 50

Capnography – locating problem areas52
Gradual increase in pCO
2
Possible causes:
Increase in metabolism and body temperature
(with MV=const.)
Beginning of hypoventilation
Reduction in effective alveolar ventilation
20
4,0
6,0
8,0
10,0
40
60
80
4 8 12 s
(mmHg) (kPa)
etCO
2
CO2-curve shapes
0
2,0
20
2,0
4,0
6,0
8,0
10,0
40
60
80
10 20 30 min
(mmHg) (kPa)
etCO
2
CO2-trend display
0
Page 51

Capnography – locating problem areas 53
Sudden drop in pCO
2
, but still above zero
Possible causes:
Leaks in hose system (tube)
Partial airway stenosis
Tube in laryngopharynx
20
2,0
4,0
6,0
8,0
10,0
40
60
80
4 8 12 s
(mmHg) (kPa)
etCO
2
CO2-curve shapes
0
20
2,0
4,0
6,0
8,0
10,0
40
60
80
10 20 30 min
(mmHg) (kPa)
etCO
2
CO2-trend display
0
Page 52

Capnography – locating problem areas54
pCO
2
plateau not horizontal
Possible causes:
Asthma
Ventilatory distribution problems
(asynchronous emptying)
20
4,0
6,0
8,0
10,0
40
60
80
4 8 12 s
(mmHg) (kPa)
etCO
2
CO2-curve shapes
0
2,0
Page 53

Capnography – locating problem areas 55
A constantly high pCO
2
Possible causes:
Respiratory depression due to drugs
Metabolic alkalosis (respiratory compensation)
Insufficient minute ventilation
20
2,0
4,0
6,0
8,0
10,0
40
60
80
4 8 12 s
(mmHg) (kPa)
etCO
2
CO2-curve shapes
0
20
2,0
4,0
6,0
8,0
10,0
40
60
80
10 20 30 min
(mmHg) (kPa)
etCO
2
CO2-trend display
0
Page 54

56
Literature
[1] A. Nahum, Use of Pressure and Flow Waveforms to
Monitor Mechanically Ventilated Patients,
Yearbook of Intensive Care and Emergency
Medicine 1995, 89-114
[2] Sydow M.,Burchardi H.,Zinserling J., Ische H.,
Crozier Th.A., Weyland W. Improved determination
of static compliance …; Intensive Care Med (1991)
17:108-114
[3] Marco Ranieri, Rocco Giuliani, Tommaso Fiore,
Michele Dambrosio, Joseph Milic-Emili. VolumePressure Curve of the Respiratory System Predicts
Effects of PEEP in ARDS: «Occlusion» versus
«Constant Flow» Technique. Am J Respir Crit Care
Med.; Vol 149. pp 19-27, 1994
[4] Michael Shapiro, MD; R. Keith Wilson, MD;
Gregorio Casar, MD; Kim Bloom, MD; Robert B.
Teague, MD. Work of breathing through different
sized endotracheal tubes. Critical Care Medicine,
Vol. 14, No. 12
[5] Jurban A, Tobin MJ (1994) Use of Flow-Volume
curves in detecting secretions in ventilator
dependent patients. Am J Respir Crit Care Med
150:766-769
Page 55

57
Page 56

58
Page 57

90 97 421 / SD 5664.510 e / 127D / Subject to modifications · Printed in Germany / chlorinefree - ecological
Dräger Medizintechnik GmbH
Germany
Moislinger Allee 53 – 55
D-23542 Lübeck
Telephone (4 51) 8 82 - 23 05
Telefax (4 51) 8 82 - 40 89
Telex 2 6 807 - 0
http://www.draeger.com
 Loading...
Loading...