Two Steps forward in Ventilation
Ernst Bahns
Bahns · BIPAP Ventilation

Important Note:
Medical knowledge changes constantly as
a result of new research and clinical
experience. The author of this introductory
guide has made every effort to ensure that
the information given is completely up to
date, particularly as regards applications
and mode of operation. However,
responsibility for all clinical measures must
remain with the reader.
Author’s address:
Dr. Ernst Bahns,
Drägerwerk Aktiengesellschaft,
Moislinger Allee 53/55,
23542 Lübeck.
All rights, in particular those of duplication
and distribution, are reserved by
Drägerwerk AG. No part of this work may
be reproduced or stored in any form using
mechanical, electronic or photographic
means, without the written permission of
Drägerwerk AG.

3
BIPAP –
Two Steps Forward in Intensive-Care Ventilation
An introductory guide to Evita ventilation

4
Introduction
Modern ventilators enable therapy to be specifically directed at a
wide range of respiratory disorders and can do far more than just
maintain vital functions. The continued development of pneumatics
and electronics and, above all, of computer technology means that
today selective measures can be taken to manage problems with
the control and mechanics of ventilation and with gas exchange.
Because there has been so much technical development, it is
extremely difficult to keep track of all the therapeutic measures
available. For instance, there are now more than a dozen different
ventilation modes. The accompanying expansion in the number of
terms used has tended to create confusion rather than clarity. It is,
therefore, essential to ask the question:
Do we really need yet another new ventilation mode?
The answer can only be »yes«, provided that an attempt is also
made to tackle some of the confusion. Complexity could be reduced, if it is possible to use the same mode from the beginning of
ventilation through to weaning.

5
Introduction
The success of ventilation therapy depends on several factors. It is
an important factor that ventilation is provided with minimum intervention at the right time and with the right intensity. Ventilation
therapy should adapt to the changing needs of the patient. Ideally,
such a »universal ventilation mode« would accompany the patient
throughout ventilation therapy.
This introductory guide covers two basic aspects of modern intensive-care ventilation. It describes new approaches for hospital staff
and presents new information on the effect on patients. Wherever
possible the guide avoids the use of abbreviations and technical
terms.
One of the main principles in the design of Evita was to simplify
ventilation. Following the same principle, this introductory guide
aims to make ventilation easier to understand and easier to use.

6
Introduction
Outline
The BIPAP1)(Biphasic Positive Airway Pressure) ventilation mode
is a modern ventilation method which has been an important feature of the Evita ventilator since it was first introduced. This guide
is designed to make the subject easy to understand.
Research which has been published in medical literature on the
theory and clinical applications of BIPAP ventilation is summarized
in simplified form in this introductory guide to assist busy clinical
staff.
Since both the theory and the practice have developed from wellknown principles, BIPAP does not demand that users think along
entirely new lines. All that is required is an interest in new ideas.
The introductory guide is divided into four sections, as follows:
1. Description of BIPAP:
This section gives a brief outline of how BIPAP was developed
and how it is classified according to performance.
2. BIPAP and conventional ventilation:
This section compares BIPAP with standard mandatory ventilation
and spontaneous breathing.
3. Setting BIPAP:
This section describes how BIPAP operates in the Evita 1 ventilator and how this has been simplified for the Evita 2 ventilator.
4. Using BIPAP:
This section deals with intensive-care ventilation using BIPAP,
gives instructions for weaning and discusses special applications.
A bibliography is provided at the end of the guide.
1) Trademark under license
7
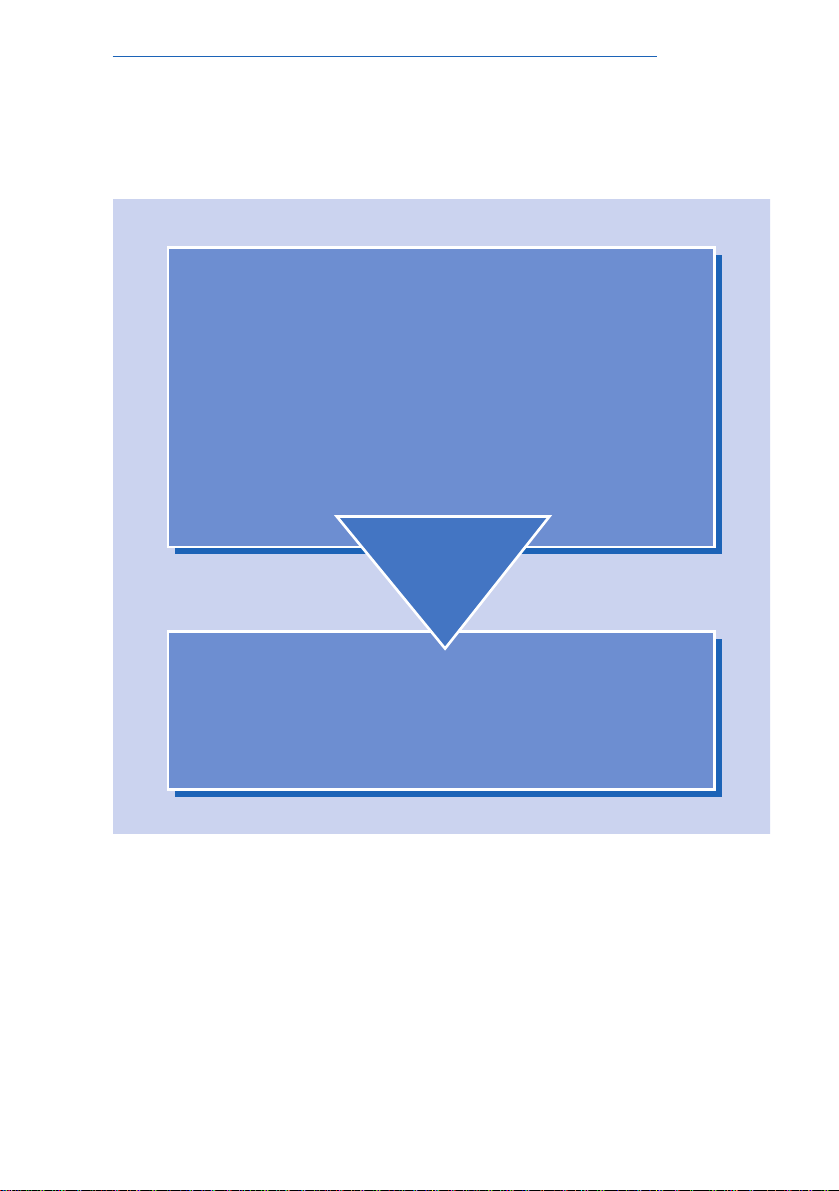
Fig.1: Aims and structure of the BIPAP booklet.
Four sections are divided into sub-sections. Each sub-section
deals with a separate topic on two pages with text and figures.
Introduction
Introduction to BIPAP
BIPAP and conventional ventilation
BIPAP operation
Ventilating and weaning with BIPAP
To the patient with regard to therapy
To the staff with regard to handling
?
Benefits

8
BIPAP definition
BIPAP in brief
BIPAP ventilation ranges across the whole spectrum from purely
mechanical ventilation to purely spontaneous breathing. This range
can cover the entire course of therapy from intubation to the completion of weaning. For this reason BIPAP has come to be known
as a »universal ventilation mode«.
In contrast to conventional ventilation, BIPAP does not feature
separate modes for controlled ventilation and spontaneous breathing, but merely variations of the same ventilation mode. The
boundaries between the variations are completely flexible as
they are defined primarily by the patient's ability to breathe
spontaneously.
The diagram in Figure 2 shows that the lung being ventilated with
BIPAP can be thought of as a balloon with two forces acting on it.
The positive pressure generated by the ventilator, combined with
the negative pressure produced by the inspiratory muscles, produce a flow. In BIPAP ventilation these two forces never oppose
one another.
BIPAP's broad spectrum gives staff more freedom and flexibility
for ventilation therapy.
9
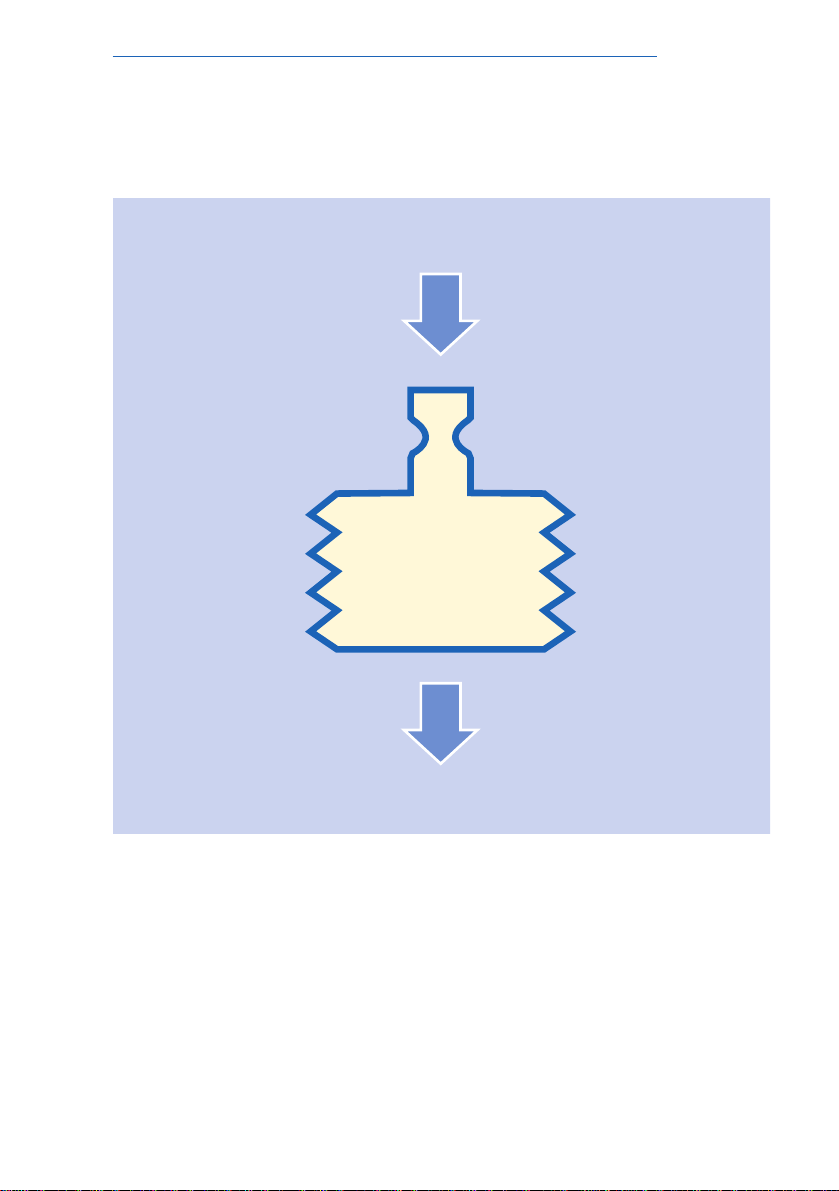
Fig.2: Mechanical model of the lungs illustrating BIPAP ventila-
tion.
Ventilation of the lungs involves two forces. The ventilator generates a positive pressure whilst the inspiratory muscles produce a
negative pressure. The two forces combine to produce a change
of volume in the lungs.
BIPAP definition
Respiratory muscles (breath)
Lung
volume
Ventilator (pressure)

10
BIPAP definition
A story in brief:
The origins of BIPAP
BIPAP was first described in a study published in 1985 by a group
led by M. Baum and H. Benzer and it was incorporated in the Evita
ventilator in the same year. Earlier studies conducted by Downs et
al. used the term APRV (Airway Pressure Release Ventilation) [7] to
describe a method of ventilation which used the same mechanical
principle as BIPAP, but started from a different premise.
The authors describe BIPAP as pressure-controlled ventilation
with freedom of respiration and spontaneous breathing on two
CPAP levels. Figure 3 is from the study published by Baum
et al. [1].
The workgroup of Baum represented a new approach to ventilation techniques. Before 1989, though ventilation modes
employed a mixture of mechanical ventilation and spontaneous
breathing (augmented ventilation), they were all based on the
same principle for maintaining minimum ventilation, namely mechanical breaths alternating with spontaneous breaths.
The clinical problems which arose from alternating between
mechanical ventilation and spontaneous breathing were the starting point for the development of BIPAP: patients often failed to
accept the enforced respiratory rate or the interruption of their
spontaneous breathing by the mandatory breaths.
Baum and Benzer realized that BIPAP was particularly important
from the clinical point of view because ventilation was accurately
matched to the patient's spontaneous breathing and because it
was straightforward to use. These advantages were thought to be
particularly significant for weaning, because there was no alternation between pure mechanical ventilation and augmented ventilation. Decisions about when to start the weaning process
become totally unnecessary – with the new BIPAP mode weaning
is possible right from the start.
11
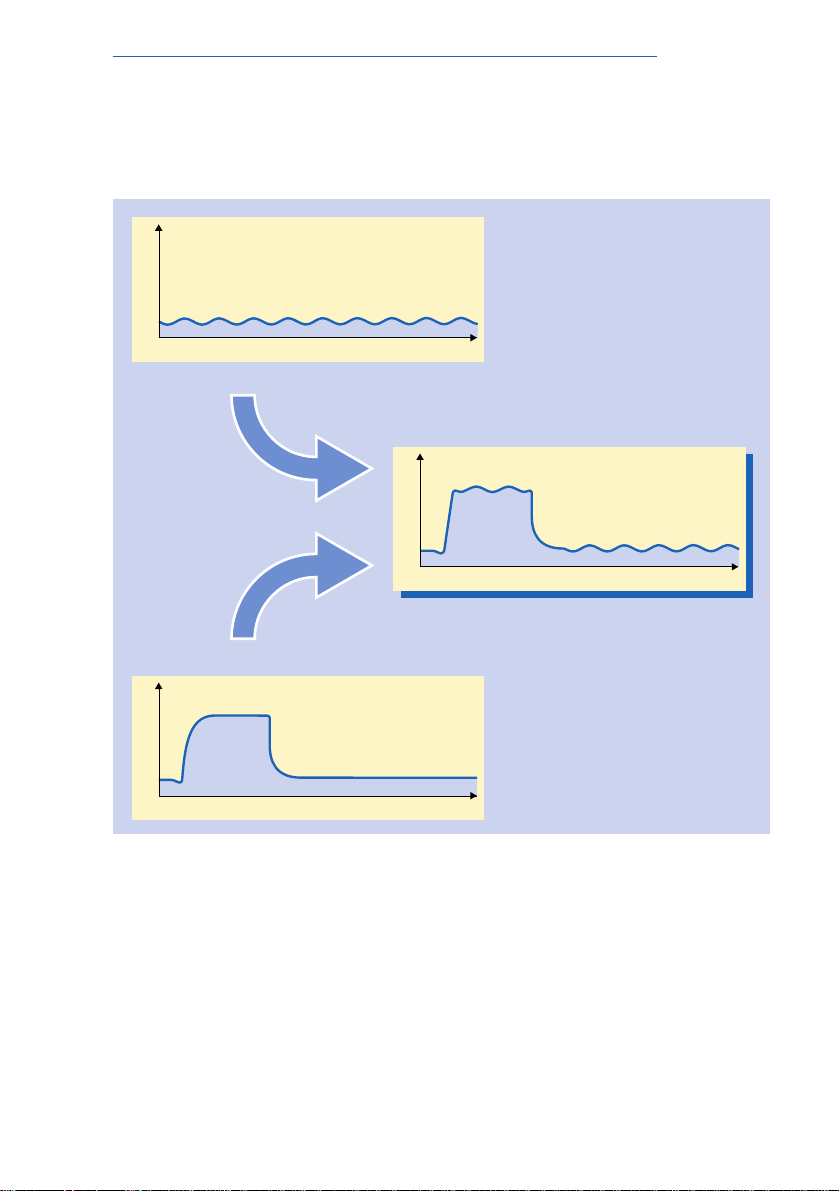
Fig.3: Schematic view of BIPAP principles.
The figure shows the principle of mixed mechanical ventilation and
spontaneous breathing. In contrast to conventional ventilation,
mechanical and spontaneous breathing occur at the same time in
BIPAP.
BIPAP definition
P
BIPAP
t
P
t
Spontaneous breathing
t
P
Pressure-controlled
ventilation

12
BIPAP definition
Simply a matter of form:
A versatile ventilation mode
BIPAP can take many forms depending on how it is being used.
On the one hand, it can provide pressure-controlled ventilation in a
system which always permits unrestricted spontaneous breathing
but it can also be viewed as a CPAP system with time-cycled
changes between different CPAP levels.
Basically there are two processes involved when ventilating the
lungs with BIPAP as shown in Figure 2. The flow is generated in
two ways – firstly, mechanically by alternating between two pressure levels and, secondly, by the action of the inspiratory muscles.
The relative contribution made by these two processes governs
the form of BIPAP. The graph in Figure 4 is taken from a paper by
Hörmann et al. [5]. It describes the BIPAP spectrum in conventional ventilation terminology and classifies the various forms
according to the proportion of mechanical ventilation involved.
1. IPPV-BIPAP with no spontaneous activity on the part of the
patient. Ventilation is pressure-controlled and time-cycled. All
ventilation activity is carried out by the ventilator.
2. SIMV-BIPAP with spontaneous breathing on the lower
pressure level only. Increased pressure at the upper level
delivers a machine-generated flow.
3. »Genuine« BIPAP: Here, the patient breathes spontaneously at
both the upper and the lower pressure levels. Mechanical
ventilation is superimposed on the spontaneous breathing as a
result of step changes in pressure, but spontaneous breathing
is not impeded.
4. BIPAP after the two pressure levels become the same (CPAP).
Spontaneous breathing is continuous. The patient takes over
the total ventilation.
The next section describes BIPAP ventilation in two ways: firstly
compared to conventional controlled ventilation and then in conjunction with supported spontaneous breathing.
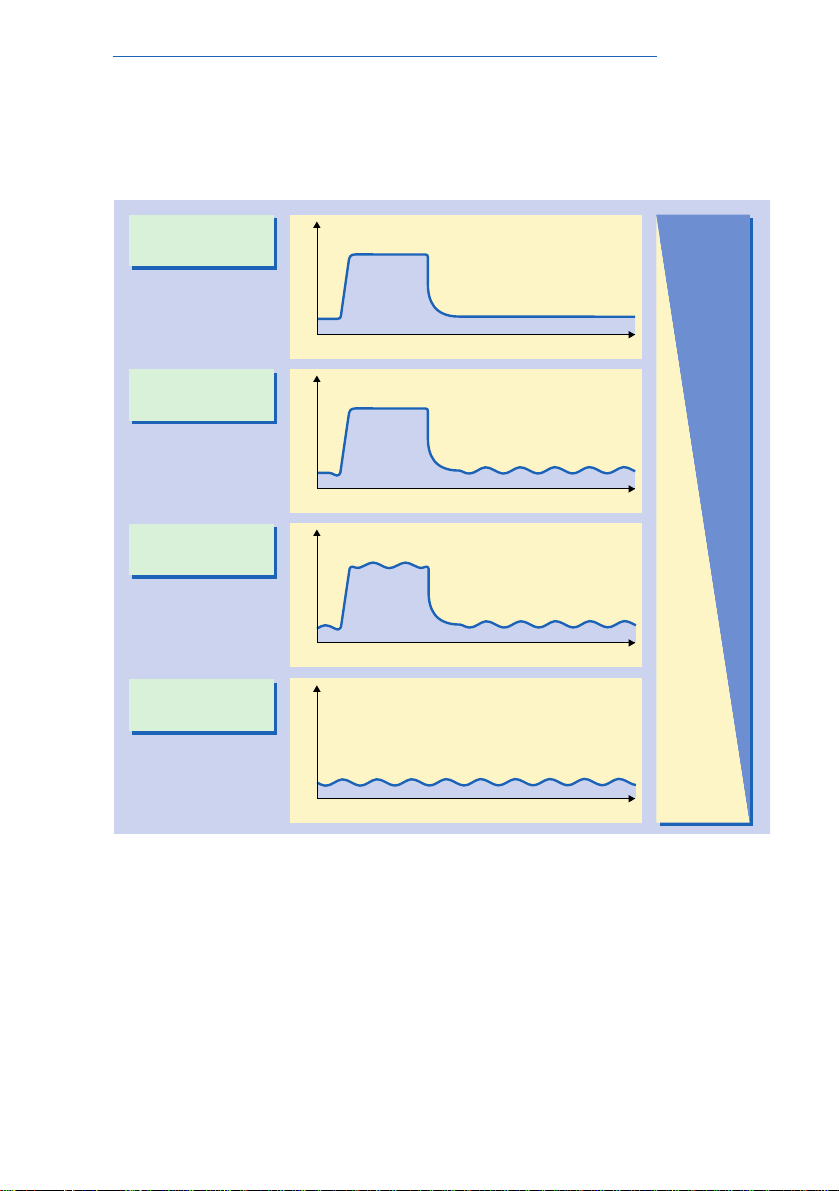
13
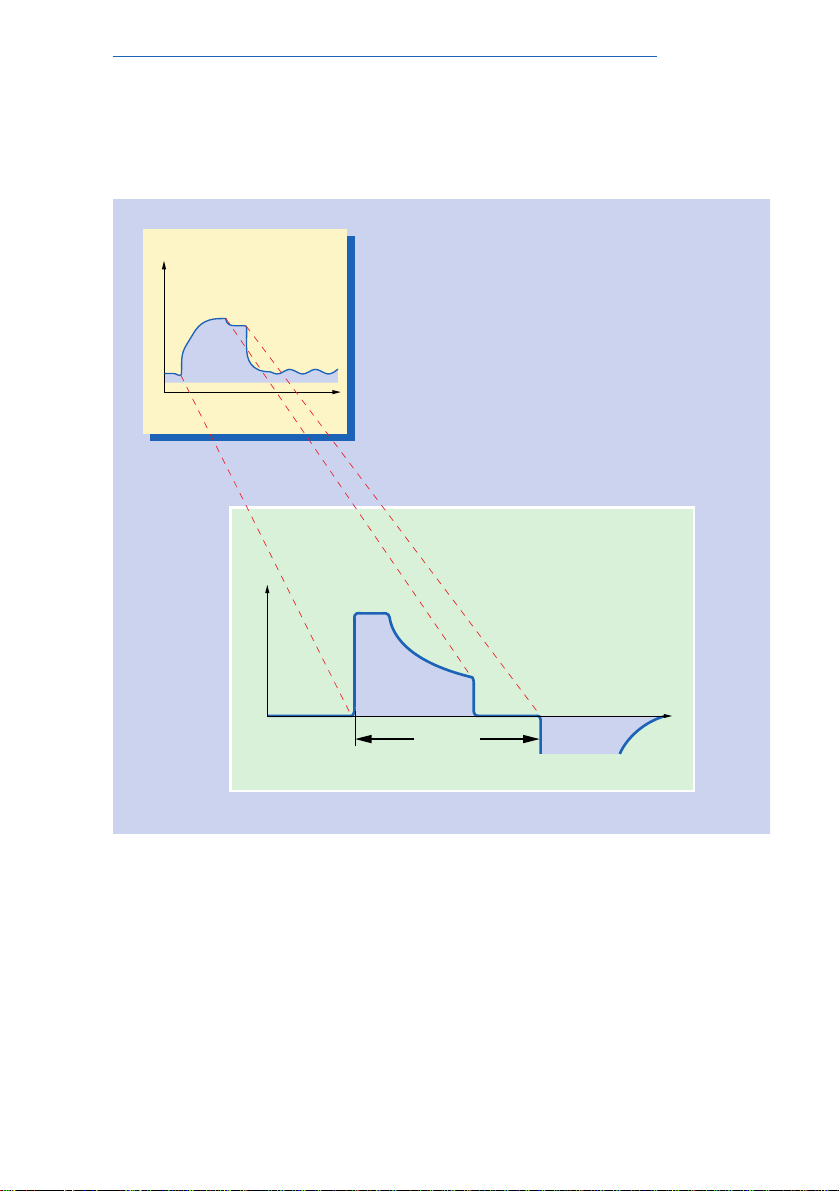
Fig.4: BIPAP forms described in conventional ventilation
terms.
The various forms of BIPAP are classified according to the
respective proportions of mechanical ventilation and spontaneous
breathing. IPPV-BIPAP: no spontaneous breathing; SIMV-BIPAP:
spontaneous breathing only at lower pressure level; »genuine«
BIPAP: continuous spontaneous breathing at two pressure levels;
CPAP: continuous spontaneous breathing, both pressure levels
are equal.
BIPAP definition
IPPV - BIPAP
SIMV - BIPAP
»genuine« BIPAP
CPAP
Mechanical
ventilation
Spontaneous
breathing
t
P
t
P
P
t
P
t

14
BIPAP and conventional ventilation
A need for order:
Conventional variety of definitions
BIPAP is a single ventilation mode which covers the entire spectrum from mechanical ventilation to spontaneous breathing. Conventional ventilation has a variety of ventilation modes, each of
which covers a specific range of applications.
Conventional ventilation is divided into three categories with different modes depending on the relative proportion of mechanical
ventilation. Figure 5 shows these categories.
In controlled ventilation all the work is performed by the ventilator.
With pure controlled ventilation, the interval between mandatory
breaths is completely independent of the patient.
Augmented ventilation involves contributions by both the machine
and the patient and thus represents a mixed mode of mechanical
ventilation and spontaneous breathing. Conventional augmented
ventilation has two varieties: intermittent and pressure-supported
ventilation.
In intermittent ventilation, mechanical breaths alternate with spontaneous breaths and the frequency and duration of these breaths
can be selected by clinical staff. In pressure-supported ventilation,
on the other hand, the frequency and duration of mechanical support depends on the patient and only the intensity of the machine
support is set.
It is clear, therefore, that conventional ventilation has two important
characteristics which distinguish it from BIPAP. Firstly, it usually
involves alternating between various modes during therapy and,
secondly, there are two different modes of augmented ventilation,
not just one.
15
Fig.5: The spectrum of conventional ventilation.
The ventilation modes are classified according to the relative proportions of mechanical ventilation and spontaneous breathing.
Controlled: pure mechanical ventilation without spontaneous
breathing; intermittent augmented: alternate spontaneous breathing and mechanical ventilation; augmented pressure-supported:
machine support of spontaneous breathing.
BIPAP and conventional ventilation
Controlled
Augmented
intermittent
Augmented
pressure-supported
Spontaneous
P
CPAP
t
ASB
P
t
t
P
IPPV
t
P
SIMV
Mechanical
ventilation
Spontaneous
breathing

16
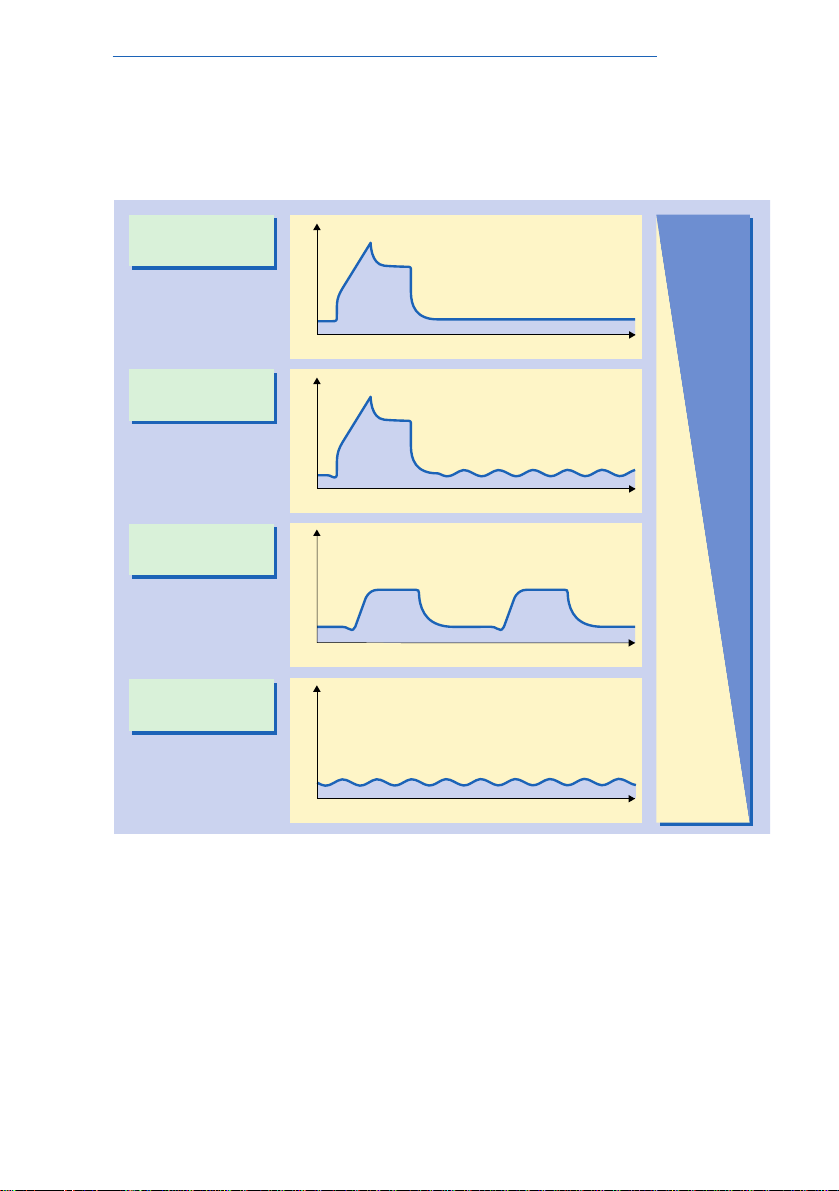
BIPAP and conventional ventilation
Ventilation strategies:
Volume or pressure control
The classification of ventilation modes according to their contribution to breathing activity, given in Figure 6, is particularly relevant in the weaning process. Ventilation modes can also be classified according to primary objectives and strategies of the therapy.
Volume-constant and pressure-controlled ventilation differ in the
way they react to changes in lung mechanics. Both forms of ventilation have specific advantages and disadvantages for particular
areas of application.
The figure shows the spectrum from volume-constant ventilation to
pressure-controlled ventilation as it is offered by Evita 2.
Volume-constant ventilation is the term used when the set tidal
volume is administered while pressure is maintained below a preset maximum. Pressure-controlled ventilation is the term used to
describe a situation where the preset maximum airway pressure is
set at plateau values and the flow is administered for the duration
of the inspiratory time. An intermediate mode, which is possible
with the Evita ventilator, is pressure-limited ventilation where the
maximum airway pressure chosen is such that the set tidal volume
can still just be administered. The first three waveforms in the
graph illustrate volume-constant, pressure-limited and pressurecontrolled ventilation.
BIPAP is a variation of pressure-controlled ventilation. It differs
from conventional pressure-controlled ventilation as far as the
mechanical breaths are concerned in that spontaneous breathing
is always possible. BIPAP permits spontaneous breathing not only
during expiration, but also during mandatory breaths. This is
shown in the fourth waveform in the graph.
17
Fig.6: The spectrum of volume-constant and pressure-control-
led ventilation.
The different modes of ventilation are classified in terms of volume
and pressure control. Volume-constant: administration of a constant tidal volume with constant flow; volume-controlled/pressurelimited: constant tidal volume administered with decelerating flow;
pressure-controlled (conventional): volume-inconstant; pressurecontrolled BIPAP: pressure-controlled, but with freedom to
breathe spontaneously.
BIPAP and conventional ventilation
Constant-volume
Constant-volume/
pressure-limited
Pressure-controlled
Pressure-controlled
(open system)
t
P
PLV
t
P
PCV
P
BIPAP
t
t
P
SIMV
Volumeorientated
Pressureorientated

18
BIPAP and conventional ventilation
Volume-constant ventilation:
Stress due to uneven gas distribution
Volume-constant ventilation provides constant ventilation even if
lung mechanics change. The Evita ventilator ensures the delivery
of a constant flow, and a time profile and tidal volume which are
fixed.
Volume-constant ventilation is seen as particularly useful when
ventilating an intact lung primarily to reduce the CO
2
concentra-
tion.
Ventilation involving a constant tidal volume and constant flow may,
however, lead to local mechanical stress if the inspired gas is not
distributed in the lung at a uniform rate, and problems of this kind
have been reported in diseased lungs.
The two-compartment model in Figure 7 shows that gas distribution problems can be caused, for example, by localized increases
in resistance. If a tidal volume with a constant high flow rate is
administered in these circumstances, the compartment with the
lower resistance will be inflated first.
Differences in ventilation may cause a variety of mechanical stresses in the pulmonary tissue. Apart from temporary over-inflation of
the compartment with low resistance and a difference in pressure
between the two compartments, local shear forces may occur
between the compartments.
This mechanical stress can produce local tissue damage, which if
allowed to continue, can lead to acute pulmonary failure.
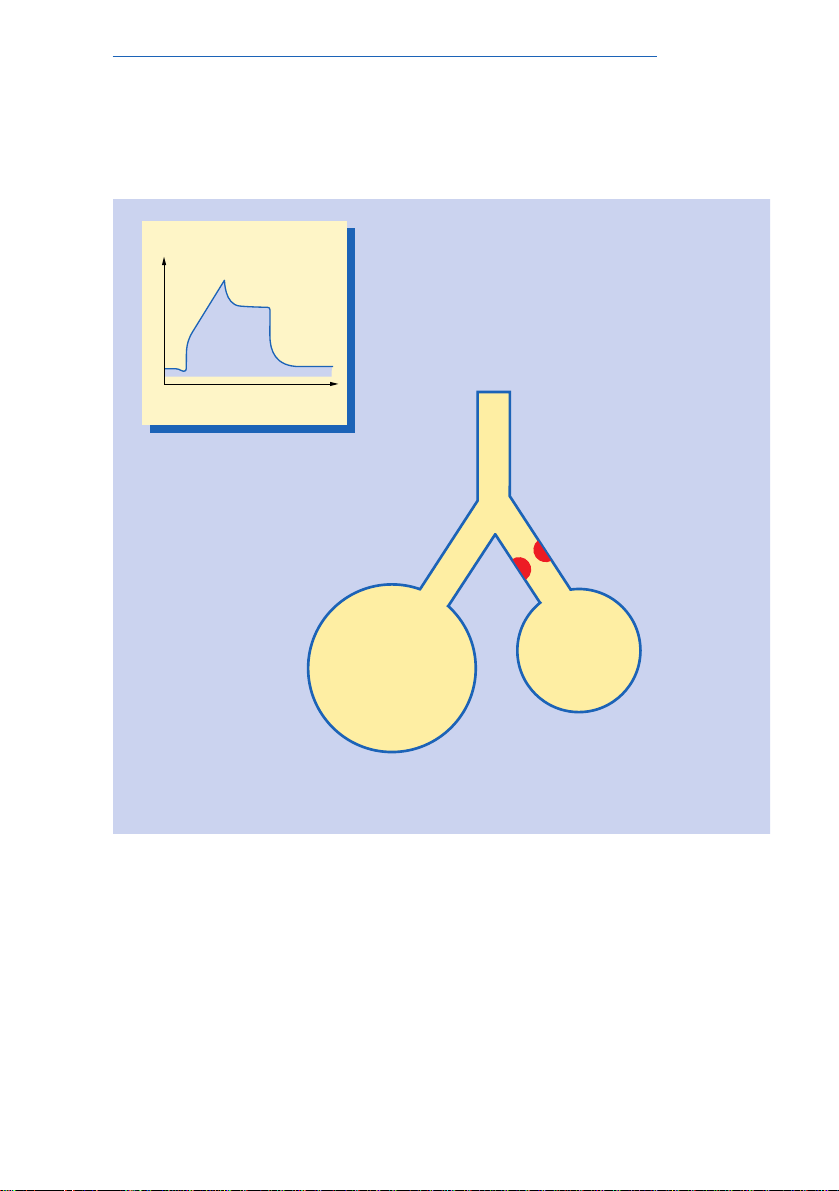
19
Fig.7: Two-compartment model illustrating effects of volume-
controlled ventilation.
The increased airway resistance (R) in the right compartment
results in faster inflation and over-distention of the left compartment. Pressure (P) differences and different inflation volumes
between the compartments produce severe mechanical stress.
BIPAP and conventional ventilation
P!
R
P
t
P
IPPV

20
BIPAP and conventional ventilation
Pressure-limited ventilation:
An »intelligent« decelerating flow
Even when a patient’s lungs are healthy, ventilation therapy produces changes in lung mechanics. Resistance may increase and
compliance decrease during lengthy treatment. Unfortunately,
these mechanical changes may not be distributed uniformly over
the lung.
With a two compartment model it can be illustrated how negative
effects of volume-constant long-term ventilation can be minimized
by using pressure-limited ventilation where the airway pressure is
limited by the maximum pressure (P
max
) set.
With pressure-limited ventilation the tidal volume is always applied
but the flow only reaches the value set by the operator at the start
of the mechanical breath. As soon as the airway pressure reaches
the P
max
value, the Evita ventilator automatically reduces the flow
(decelerating flow). Figure 8 shows the change of airway pressure
with time.
A major advantage of pressure-limited ventilation with the Evita
ventilator is that the flow adapts continuously to changes in lung
mechanics. The Evita ventilator does not produce a fixed decelerating flow but determines the optimum flow profile for every
single breath when administering the tidal volume required. The
set pressure limit is not exceeded and tidal volume is applied as
quickly as possible.
The extent to which the flow profile is being affected by lung
mechanics is easily seen on the Evita ventilator’s screen. If, for
example, resistance is reduced following bronchial suction, a
distinct change in the flow waveform is apparent.
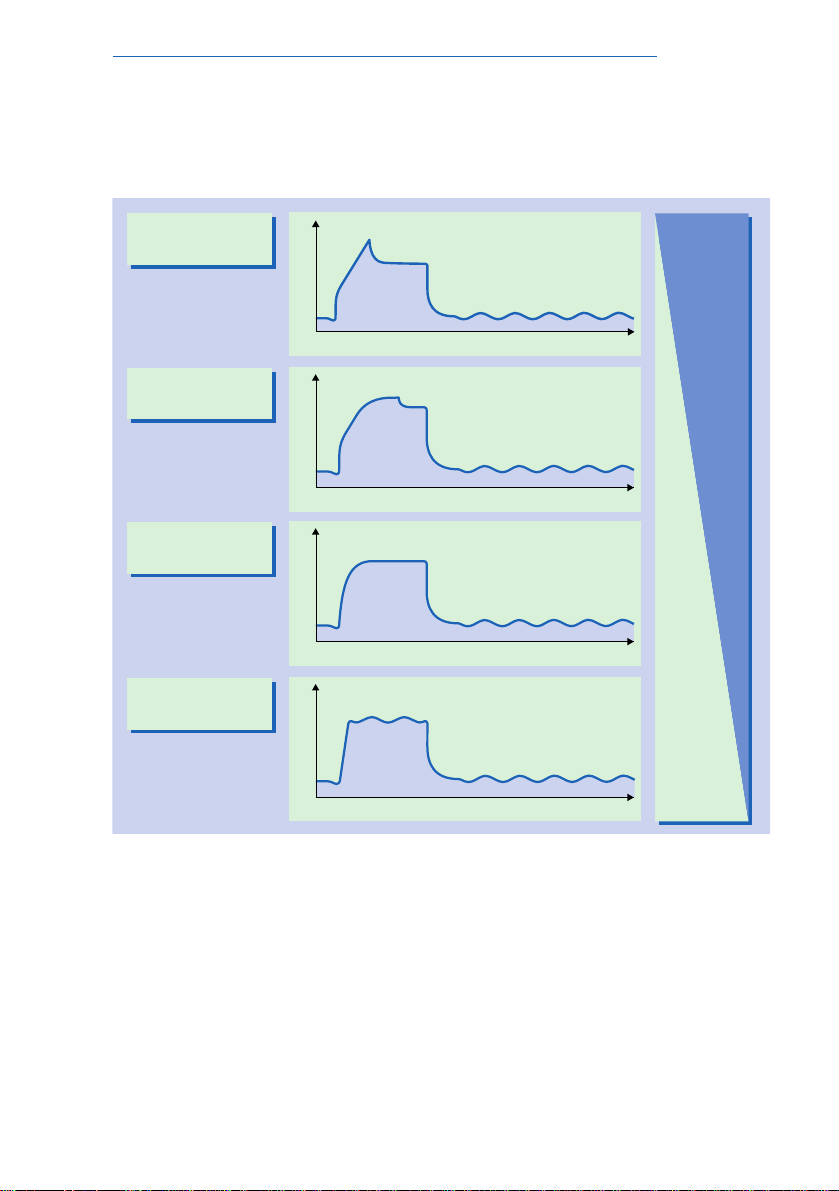
21
Fig.8: Variation in pressure and flow with time during pres-
sure-limited ventilation.
A set constant flow is generated in the first phase. As soon as the
set maximum airway pressure is reached, the Evita ventilator
reduces the flow progressively (decelerating flow). The ventilator
terminates the flow once the set tidal volume has been completely
administered.
BIPAP and conventional ventilation
T
insp
t
P
PLV
Patient-dependent
decelerating flow
t
V
.
