CRU RAX215DC Installation Manual
Curr Pediatr Res 2017; 21 (1): 148-157
ISSN 0971-9032
www.currentpediatrics.com
Curr Pediatr Res 2017 Volume 21 Issue 1
148
Introduction
According to the International Association for the Study of
Pain (IASP) Pain is “an un-pleasant sensory and emotional
experience associated with actual and potential tissue
damage”. Pain has also been dened as “existing whenever
they say it does rather than whatever the experiencing
person says” [1-4]. It is one of the most dreading and
devastating symptom commonly propagated in peoples
with advanced chronic conditions including cancer patents.
Pediatric patients are the most under treated and present to
hospital for pain compared to adults; because of the wrong
belief that they neither suffer pain nor they remember
painful experiences [5]. The quality of life experienced
by the patient can greatly reduce, regardless of their basic
diagnosis. Thus, if pain will be poorly managed, it can
reect the inuence on family and careers causing different
which may leads to increased rates of hospital admission
[5,6]. Uncontrolled pain has also direct impact on health
outcomes and more than a few effects on all areas of life.
The emotional, cognitive, and behavioral components of
pediatric patient are also important to assess pain and to
simplify the management practices [7,8].
A long-term negative effect of untreated pain on pain
sensitivity, immune functioning, neurophysiology,
attitudes, and health care behavior are supported with
numerous evidences. Health care professionals’ who care
for children are mainly responsible for abolishing or
assuaging pain and suffering when possible [5,7,9]. The
practice of pediatric pain treatment protocol has made
great progress in the last decade with the development
and validation of pain valuation tools specic to pediatric
patients. Almost all the major children hospitals now
have dedicated pain services to provide evaluation and
immediate treatment of pain in any child [10,11].
In pediatric age, it is more difcult to assess and treat pain
effectively relatively to adults. The lack of ability to notice
pain, immaturity of remembering painful experiences
and other reasons are the reection of persistence of
myths related to the infant’s ability to perceive pain [12].
However, the treatment of pain in childhood is like the adult
management practice which includes pharmacological and
non-pharmacological interventions. On the other hand,
it critically depends on an in-depth understand of the
developmental and environmental factors that inuence
nociceptive processing, pain perception and the response
to treatment during maturation from infancy to adolescence
[13,14].
The practice of assessing pain and its management in
pediatric patients can show a discrepancy based on the
different countries and their respective health institutions.
So, this review focused on the contemporary practice
and new advances in pediatric pain assessment and its
management.
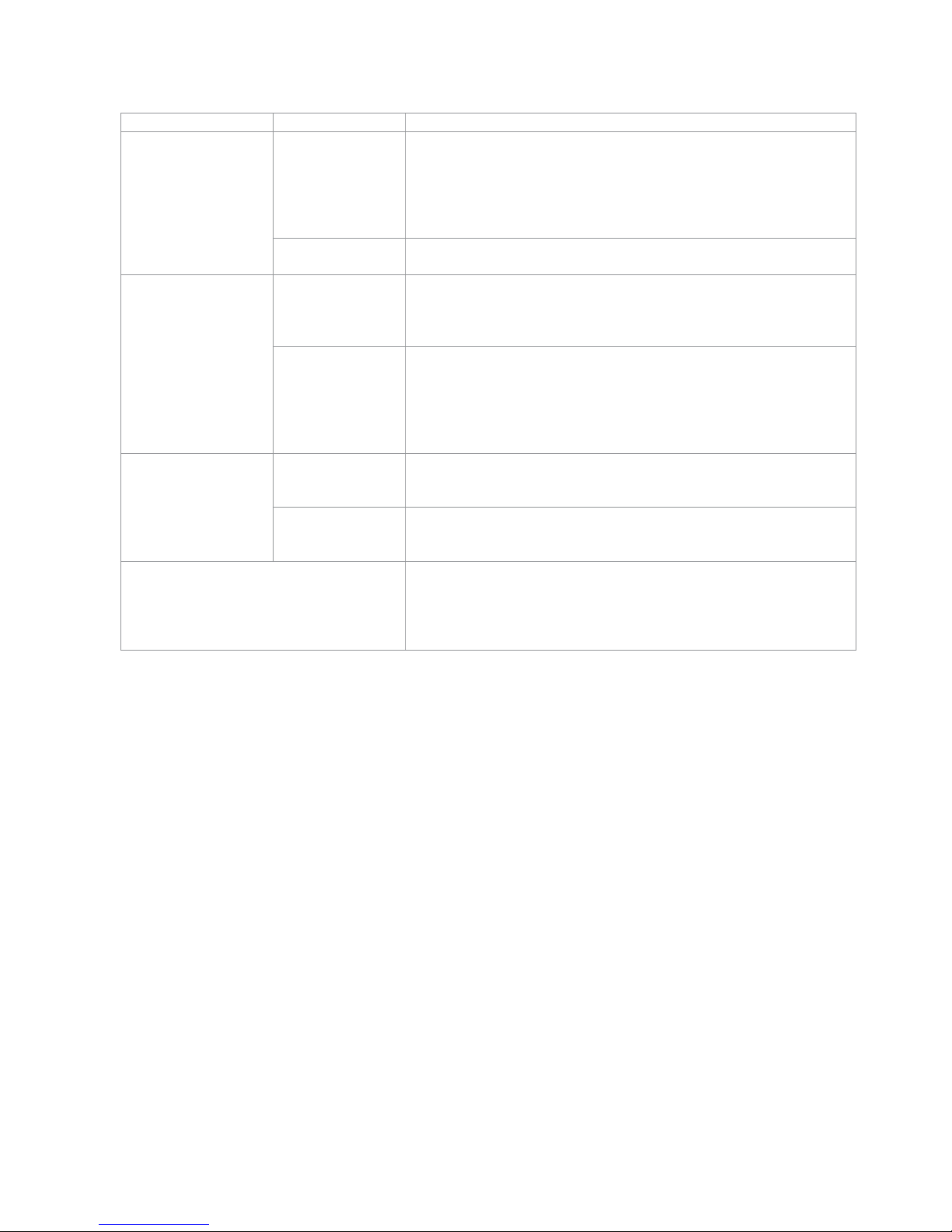
Classication of Pain
Many classication systems are used to describe the
different types of pain. The most common classication
schemes refer to pain as acute or chronic; malignant or
nonmalignant; and nociceptive or neuropathic [15]. Most
studies are agreed with the following classication of pain
(Table 1).
Assessment and treatment of pain in pediatric patients.
Halefom Kahsay
Department of Pharmacy, Collage of Health Science, Adigrat University, Adigrat, Ethiopia.
Pediatric patients experience pain which is more difcult to assess and treat relatively to
adults. Evidence demonstrates that controlling pain in the pediatrics age period is benecial,
improving physiologic, behavioral, and hormonal outcomes. Multiple validated scoring
systems exist to assess pain in pediatrics; however, there is no standardized or universal
approach for pain management. Healthcare facilities should establish pediatrics pain control
program. This review summaries a collection of pain assessment tools and management
practices in different facilities. This systematic approach should decrease pediatric pain and
poor outcomes as well as improve provider and parent satisfaction.
Abstract
Keywords: Pain, Pain assessment, Pain management, Pediatric patients.
Accepted January 30, 2017
Assessment and treatment of pain in pediatric patients.
Curr Pediatr Res 2017 Volume 21 Issue 1
149
Assessment of Pain in Pediatrics
Pain is often referred to as the “fth vital sign” and it should
be assessed and recorded as often as other vital signs.
The appropriate intervention of pain is planned based
on the accurate valuation of pain. Organized and routine
pain assessment by using the standardized and validated
measures is accepted as a corner stone for effective pain
management in patients, unrelatedly to the age or other
conditions [21]. A study in Brazil suggests that consistent
accomplishment of assessments of pain using ordinary
scales, such as Face, Legs, Activity, Cry and Consolability
score and other bodily parameters are mandatory to
optimize pain management in pediatric intensive care
units [22]. As pain is a subjective experience, individual
self-reporting is the favorite method for assessing
pain. However, when valid self-report is not available
as in children who cannot communicate due to age or
developmental status, the observational and behavioral
assessment tools are acceptable substitutions [5,7,22].
The use of the pain management algorism on Stollery
children’s hospital shows signicant improvement for
assessment of pain in pediatrics. The pre and post analysis
indicated in a staff (n=17) given that a feedback of 41.2%
felt that the algorism improved their ability to assess and
manage pain in children equally, 35% felt that it increased
their capacity to communicate a child’s pain with other
health care team members, 52.9% felt that the algorism
should be further applied on other units across the hospital
[23]. Even though, the assessment of pain symptoms is
easy in adults, selection of appropriate pain assessment
tools should consider age, cognitive level and the presence
of eventual disability, type of pain and the situation in
which pain is occurring in children. Therefore, healthcare
professionals need to be aware of their limitations in
addition to trained in the use of pain assessment tools
[7,24,25].
The assessment in Canadian pediatric teaching hospitals
indicated out of 265 children, majority (63%) of them
found with a minimum of one documented pain assessment
tool, 30% of children had at least two assessment tools,
17% had 3-5 measurement tools and 16% had at least
six assessments in 24 h of admission. Most (63%) of
the children were nd a different document of 666 pain
assessment tools, with a median of three assessments per
one child [14]. Parent, patient, as well as staff satisfaction
is positively associated with accurate assessment of pain in
addition to well improvement of pain management. Brief
and well validated tools are available for the assessment
of pain in non-specialist settings. Nevertheless, each tool
cannot be broadly suggested for assessment of pain in all
Category Sub-classication Description
Pathophysiological
Nociceptive pain
This type of pain arises as the tissue injury activates specic pain receptors
named nociceptors, which are sensitive to noxious stimuli. These
receptors’ can respond to different stimulus and chemical substances
released from tissues in response to oxygen deprivation, tissue disruption
or inammation. It can be somatic or visceral pain based on the site of
the activated receptors.
Neuropathic pain
This type of pain arises when the abnormal processing of sensory input
recognized by the peripheral or central nervous system.
Etiologically
Non-malignant
It includes the pain due to chronic musculoskeletal pains, neuropathic
pains, visceral pain (like distension of hollow viscera and colic pain) and
chronic pain in some specic anemia. Rehabilitation care is there main
treatment protocol.
Malignant
This is the pain in potentially life-limiting diseases such as multiple
sclerosis cancer, HIV/AIDS, end stage organ failure, amyotrophic lateral
sclerosis, advanced chronic obstructive pulmonary disease, Parkinsonism
and advanced congestive heart failure. These illnesses are indicating for
similar pain treatment that emphases more on symptom control than
function.
Based on duration
Acute
This is pain of recent onset and probable limited duration. It usually has
an identiable temporal and causal relationship to injury or disease. Most
acute pain resolves as the body heals after injury.
Chronic
It is the pain which lasts a long time mostly 6 months, which commonly
persisting beyond the time of curing of an injury and may be without any
clearly identiable cause.
Based on location
When Pain is often classied by body site (e.g. on head, on the back
or neck) or it can be the anatomic function of the affected tissue (e.g.
vascular, rheumatic, myofascial, skeletal, and neurological). It does not
provide a background to resolve pain, but it can be useful for differential
diagnoses.
Table 1. The general classication of pain in pediatrics [3,4,8,15-20]

Kahsay
Curr Pediatr Res 2017 Volume 21 Issue 1
150
after observing the infant for 1 min. Among two observers
a reliability of FLACC was established in a total of 30
children in the post anesthetics care unit (PACU) (r=0.94).
After analgesic administration, validity was established
by demonstrating a proper decrease in FLACC scores.
Correspondingly, a high degree of association was found
between PACU nurse’s global pain rating scale, FLACC
scores, and with the objective scores of pains scale. This
tool has been established in various settings and in diverse
patient populations and nds that as reliable and valuable.
It provides a simple background for computing pain
behaviors in children who may not be able to put into words
the incidence or severity of pain. Lastly, the constructed
validity is supported by analgesic administration as the
scores decreases signicantly. Another recent studies
have demonstrated that FLACC was the most chosen in
terms of sensible qualities by clinicians at their respective
institutions [27,29,32-35]. Although the tool can be
used by clinicians, it is more effective with parent input
to provide a description of ‘baseline’ behavior. This is
supported by the ndings of the Malvinas study, which
suggested that the addition of unique descriptors allowed
parents to augment the tool with individual behaviors
unique to their children. In addition, for infants who show
good comprehension and motor skills, this pain assessment
tool can be used as an alternative [36]. The FLACC scale
has 98% sensitivity and 88% specicity in assessing pain
levels [34]. Therefore, those different studies concluded
that FLACC scale is the most appropriate measurement
tool for pain assessment in infants (Table 3).
Cries Pain Rating Scale
0 1 2
Crying No high pitched inconsolable
Requires O
2
for sat >95% No <30% >30%
Increased vital signs HR and BP <or=pre-op
HR and BP;
Increased <20% of
pre-op
HR and BP; Increased >20% of
pre-op
Expression None Grimace Grimace/grunt
Sleepless No
Wakes at frequent
intervals
Constantly awake
Table 2. Neonatal pain rating scale [27-29]
children and across all settings. Individual needs of the
children lead to assess and re-evaluate of pain consistently
as a mandatory in every situation. On top of that,
ethnicity, language, and cultural factors should be under
consideration as they may inuence pain assessments and
its expression [5,12,26].
Most formal and commonly used means of pediatric
assessment tools for pain are available and categorized
depending the pediatrics age.
Pain Assessment in Neonates
Neonates pain rating scale (NPR-S): Major guidelines
indicate that the assessment of pain in neonates (term
babies up to 4 weeks of age) had better be use the Crying,
Requires oxygen for saturation above 95%, Increasing
vital signs, Expression and Sleepless (CRIES) scale
(Table 2) [2,24,27-30].
Several other pain scales have been designed for the
objective assessment of neonatal pain, including the
COMFORT (“behavior”) score, pain assessment tool, scale
for use in newborns, distress scale for ventilated newborns
and infants. Although these assessments are validated as
research tools, the mainstay of appropriate management
includes the caregiver’s awareness, knowledge of clinical
situations where in pain occurs, and sensitivity to the
necessity of preventing and controlling pain [31].
Assessment of pain in infants: On a study in Australia
hospitals, Infants (1 month to approximately 4 years) were
scored using the face, leg, activity, cancelability and cry
(FLACC) measuring tool. Scoring should be done by staff
FLACC Behavioral Pain Assessment Tool
0 1 2
Face
No particular expression
or smile
Occasional grimace/frown withdrawn or
disinterested
Frequent/constant quivering
chin, clenched jaw
Legs
Normal position or
relaxed
Uneasy, restless or tense Kicking or legs drawn up
Activity
Lying quietly, normal
position, moves easily
squirming, shifting back and forth, tense Arched, rigid or jerking
Cry
No cry Moans or Whimpers, occasional complaint
Crying steadily, screams or
sobs, frequent complaints
Cancelability
Content or relaxed
Reassured by occasional touching,
hugging or being talked to, distractible
Difcult to console or comfort
Table 3. FLACC assessment tool [27,29,32-35]
 Loading...
Loading...