Page 1

REF 1054728
1072919
JH 6/7/10
CLINICAL MANUAL
CLINICAL MANUAL
Page 2

FOR CLINICIAN’S USE ONLY
Accessing Prescription Setting Screens
WARNING
The information on this page is ONLY for health care professionals. Remove this page from the manual
before giving the manual to the patient!
Full Menu Access Mode
The ventilator has two levels of menu access, Full and Limited. Full
Menu Access allows you to alter all available settings. Limited Menu
access permits the user to alter only those prescription parameters
that aect patient comfort, such as Rise Time, Flex, and Ramp Start
Pressure, if those parameters are available as part of the prescription.
The ventilator defaults to Full Menu Access mode.
After accessing the Main Menu, if the device is in Limited Menu
Access mode, you can use the following Setup key sequence to enter
Full Menu Access mode and be able to change prescription settings:
• Press the Down button and the Alarm Indicator/Audio
Pause button simultaneously for several seconds. This will
temporarily place the device in Full Menu Access mode.
When you perform this key sequence from the Monitor screen,
the Main Menu screen appears and an audible indicator sounds
indicating you are now in Full Menu Access mode.
When you perform this key sequence when the airow is o, the
Setup screen appears and an audible indicator sounds.
You can go into the Options menu and permanently change the
Menu Access setting to Full Menu Access. Otherwise, the device
will return to the Menu Access mode stored in the setting once you
exit the menu screens or if one minute passes without pressing any
device buttons. If you are in the Setup mode, and an SD card is in the
device, “Write Event Log to SD Card” will appear in the menu.
Note: The Full Menu Access key
sequence can be performed
either from the Power O screen
or from the Monitor screen.
Note: When the airow is o
and AC power is removed from
the device for more than 5
minutes, the device will enter
a low power mode to save
battery life. When the device is
in low power mode, the Setup
key sequence will be ignored.
Press the Start/Stop button, or
connect AC power, or insert an
SD card to exit the low power
mode.
Note: Philips Respironics
recommends that after you are
nished changing prescription
settings, and you give the
device to the patient, you set
the device back to Limited
Menu Access mode so
patients cannot change their
prescription settings.
Page 3
REF 1054728
1072919
JH 6/7/10
Page 4

© 2010 Koninklijke Philips Electronics N.V. All rights reserved.
Page 5

Page 6

Trilogy200
clinical manual
Table of Contents
FOR CLINICIAN’S USE ONLY Accessing Prescription Setting Screens ................................................... i
Chapter 1. Introduction....................................................................................................................................... 1
Package Contents ................................................................................................................. 1
Intended Use .......................................................................................................................... 2
Warnings and Cautions ......................................................................................................3
Warnings ......................................................................................................................... 3
Cautions ..........................................................................................................................8
Notes ..............................................................................................................................10
i
Contraindications ...............................................................................................................11
System Overview ................................................................................................................11
Symbols ..................................................................................................................................12
Front Panel ...................................................................................................................12
Rear and Side Panels .................................................................................................12
How to Contact Philips Respironics .............................................................................13
Chapter 2. System Description ........................................................................................................................15
Front Panel Features ..........................................................................................................15
Buttons ..........................................................................................................................15
Visual Indicators .........................................................................................................16
Display Screen .............................................................................................................16
Side and Rear Panel Features .........................................................................................17
Table of Contents
Page 7

ii
Chapter 3. Modes, Features, and Alarms......................................................................................................19
Therapy Modes ....................................................................................................................19
Breath Types.................................................................................................................20
Therapy Mode Table .................................................................................................21
Pressure Control Ventilation Therapy Modes ...................................................22
Volume Control Ventilation Therapy Modes ....................................................27
Therapy Mode Features ...................................................................................................30
Flex Comfort Feature ................................................................................................30
Ramp ..............................................................................................................................31
Rise Time .......................................................................................................................32
AVAPS Feature .............................................................................................................32
Flow Pattern Types ....................................................................................................33
Sigh Feature .................................................................................................................35
Dual Prescription Feature .......................................................................................35
Triggering ....................................................................................................................36
BTPS Compensation..................................................................................................41
Ventilator Alarms ................................................................................................................41
Loss of Power Alarm ..................................................................................................41
Ventilator Inoperative Alarm .................................................................................41
Ventilator Service Required Alarm .......................................................................41
Check Circuit Alarm ..................................................................................................42
Low Circuit Leak Alarm ...........................................................................................42
High Expiratory Pressure Alarm ...........................................................................42
Low Expiratory Pressure Alarm ............................................................................42
High Internal Oxygen Alarm .................................................................................42
Circuit Disconnect Alarm ........................................................................................43
Apnea Alarm ...............................................................................................................43
High Vte Alarm ............................................................................................................43
Low Vte Alarm ............................................................................................................43
Trilogy200 clinical manual
Page 8

High Vti Alarm .............................................................................................................44
Low Vti Alarm .............................................................................................................44
High Respiratory Rate Alarm .................................................................................44
Low Respiratory Rate Alarm ..................................................................................44
High Inspiratory Pressure Alarm ..........................................................................44
Low Inspiratory Pressure Alarm ...........................................................................45
High Minute Ventilation Alarm ............................................................................45
Low Minute Ventilation Alarm ..............................................................................45
Low Battery Alarm .....................................................................................................46
High Temperature Alarm .......................................................................................46
Replace Detachable Battery Alarm ......................................................................46
Ventilator Service Recommended Alarm ..........................................................46
AC Power Disconnected Alarm .............................................................................47
Keypad Stuck Alarm .................................................................................................47
Battery Discharging Stopped due to Temperature Info Message ............ 47
iii
Battery Not Charging due to Temperature Info Message ..........................47
Battery Not Charging Info Message ....................................................................47
Check External Battery Info Message .................................................................48
Battery Depleted Info Message ...........................................................................48
External Battery Disconnected Info Message ..................................................48
Detachable Battery Disconnected Info Message ...........................................48
Start On Battery Info Message ..............................................................................48
Card Error Info Message .........................................................................................48
Chapter 4. Ventilator Setup ...............................................................................................................................49
Position the Device ............................................................................................................50
Install the Air Filter .............................................................................................................50
Supply Power to the Device............................................................................................50
Using AC Power ..........................................................................................................51
Using DC Power ..........................................................................................................52
Device Power Source Indicators ...........................................................................54
Table of Contents
Page 9

iv
Battery Disposal..........................................................................................................56
First Time Use ..............................................................................................................56
Connect the Breathing Circuit to the Ventilator ......................................................57
Connect a Water Trap .......................................................................................................60
Connect Supplemental Oxygen (Optional) ..............................................................61
Connect the Remote Alarm (Optional) .......................................................................62
Chapter 5. Viewing and Changing Settings ................................................................................................63
Keypad Lock Feature .........................................................................................................63
Accessing the Startup and Monitor Screens ............................................................64
Monitor Screen Indicators ......................................................................................66
On-Screen Button Panel ..........................................................................................71
Navigating the Menu Screens ........................................................................................71
Changing and Viewing Settings in Full Menu Access Mode ...............................72
Changing the Device Settings and Alarms .......................................................73
Device Settings Common to All Therapy Modes ...................................73
Additional Settings Specic to Therapy Modes .....................................78
Viewing and Changing Options Menu Items ..................................................86
Viewing the Alarm Log ............................................................................................89
Trilogy200 clinical manual
Continuous Positive Airway Pressure (CPAP) Mode ..............................78
Spontaneous (S) Mode ....................................................................................80
Spontaneous/Timed (S/T) Mode .................................................................82
Timed (T) Mode .................................................................................................82
Pressure Control (PC) Mode...........................................................................83
Pressure Control Synchronized Intermittent Mandatory
Ventilation (PC-SIMV) Mode ..........................................................................83
Control Ventilation (CV) Mode .....................................................................84
Assist Control (AC) Mode ................................................................................85
Synchronized Intermittent Mandatory Ventilation
(SIMV) Mode........................................................................................................85
Page 10

Viewing the Event Log .............................................................................................90
Viewing Device Information ..................................................................................90
Updating Prescriptions Using the SD Card ...............................................................91
Changing and Viewing Settings in Limited Menu Access Mode .......................94
Activating Your Primary or Secondary Prescription ......................................95
Viewing and Changing My Settings Menu Items ...........................................96
Connecting the Ventilator to the Patient ...................................................................98
Chapter 6. Ventilator Alarms ............................................................................................................................99
Audible and Visual Alarm Indicators .........................................................................100
Audio Pause and Alarm Reset Features ................................................................... 105
What to Do When An Alarm Occurs ..........................................................................106
Alarm Summary Table .................................................................................................... 107
Chapter 7. Cleaning and Maintenance .......................................................................................................121
Cleaning the Ventilator .................................................................................................. 121
Cleaning and Replacing the Air Inlet Filter .............................................................122
Replacing the Air Inlet Path Foam .............................................................................123
v
Cleaning the Patient Circuit .........................................................................................124
Cleaning Instructions (Reusable Circuits) ...................................................... 124
Preventive Maintenance ...............................................................................................126
Chapter 8. Troubleshooting ............................................................................................................................129
Chapter 9. Accessories ......................................................................................................................................133
Adding a Humidier ....................................................................................................... 133
Adding Supplemental Oxygen to the Device ....................................................... 133
Using a Remote Alarm Unit..........................................................................................134
Using a Nurse Call System ............................................................................................ 135
Using a Secure Digital (SD) Card ................................................................................135
Using the Philips Respironics DirectView Software ............................................136
Using the Optional In-Use Bag ...................................................................................136
Traveling with the System ............................................................................................ 137
Airline Travel ...................................................................................................................... 137
Table of Contents
Page 11

vi
Chapter 10. System Checkout Procedures ................................................................................................139
Tools Required .................................................................................................................. 139
Visual Inspection ..............................................................................................................139
Initial Setup ........................................................................................................................140
Settings and Alarms Tests ............................................................................................. 140
Battery Function Verication ....................................................................................... 148
Alarm and Event Log Clean-Up ..................................................................................150
Results .................................................................................................................................150
Chapter 11. Technical Specications ...........................................................................................................151
Chapter 12. Glossary .........................................................................................................................................155
Chapter 13. EMC Information ........................................................................................................................161
Index ........................................................................................................................................................................165
Limited Warranty .................................................................................................................................................169
Trilogy200 clinical manual
Page 12
ap
Trilogy200
clinical manual
1. Introduction
This chapter provides an overview of the Trilogy200 device.
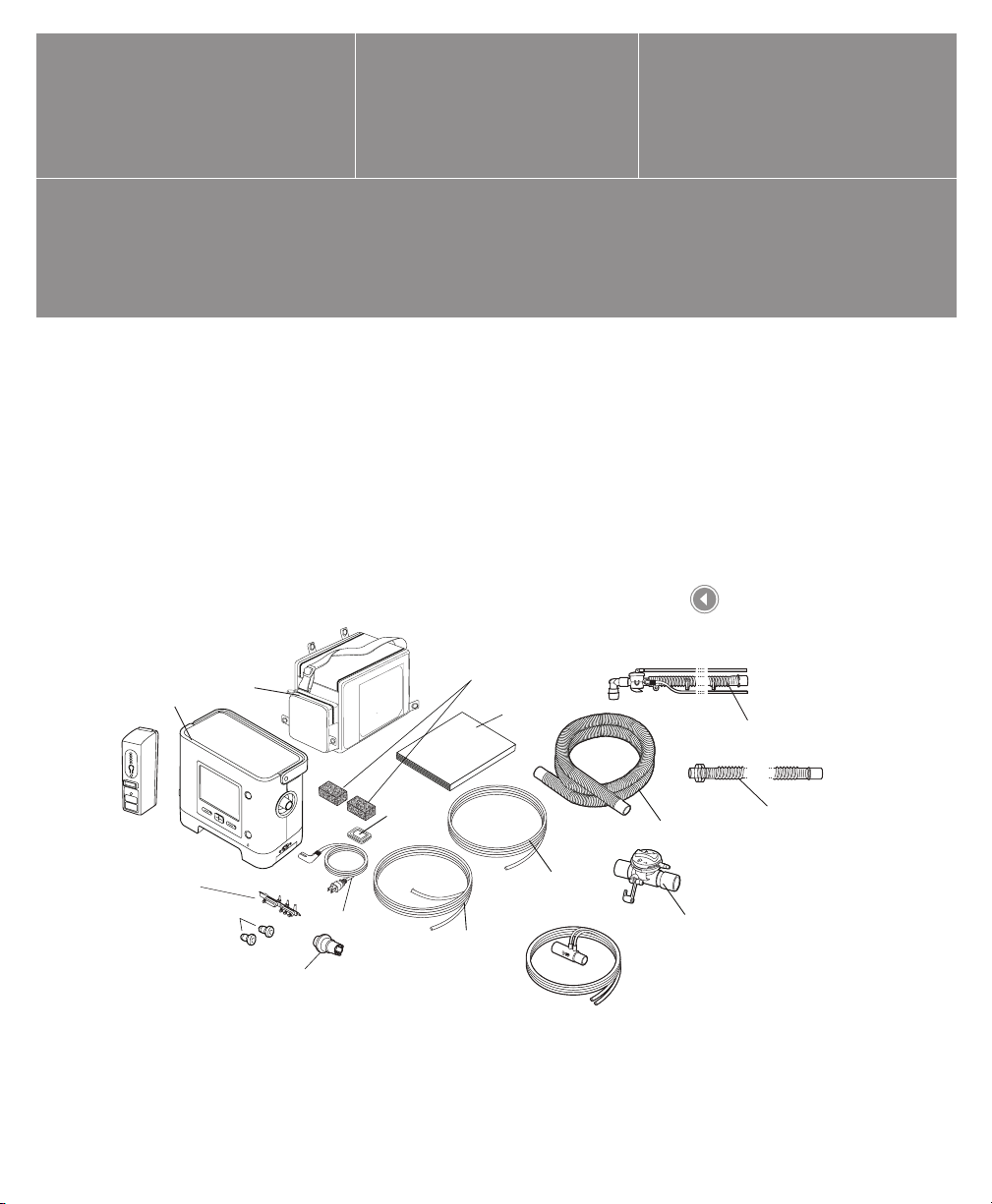
Package Contents
The Trilogy200 system may include the following components.
Some components are optional accessories that may not be
packaged with the device.
1
In-Use Bag
Trilogy200
Detachable
Battery
Universal Porting Block
(pre-installed)
O2 Inlet
Quick Connects
AC Power Cord
Whisper Swivel II
Secure Digital
(SD) Card
(pre-installed)
Reusable Gray Foam Filters
Clinical Manual
Exhalation Valve
Line (pre-assembled
to AED)
Proximal
Pressure Line
(pre-assembled
to AED)
Flow Sensor
Package Contents
Disposable Active Circuit, No Water Trap
Flexible Tubing
Active Exhalation
Device (AED)
Disposable Passive Circuit, No Water Tr
Flexible Trach Adapter
(Not Shown)
Chapter 1 Introduction
Page 13

2
Intended Use
The Philips Respironics Trilogy200 system provides continuous
or intermittent ventilatory support for the care of individuals who
require mechanical ventilation. Trilogy200 is intended for pediatric
through adult patients weighing at least 5 kg (11 lbs.).
The device is intended to be used in home, institution/hospital, and
portable applications such as wheelchairs and gurneys, and may be
used for both invasive and non-invasive ventilation. It is not intended
to be used as a transport ventilator.
The system is recommended to be used only with various
combinations of Philips Respironics-approved patient circuit
accessories, such as patient interface devices, humidiers, water
traps, and circuit tubing.
Trilogy200 clinical manual
Page 14

Warnings and Cautions
Caution: U.S. federal law restricts this device to sale by or on the order of a physician.
Warnings
A warning indicates the possibility of injury to the user or operator.
Patient Monitoring Prior to placing a patient on the ventilator, a clinical assessment should
be performed to determine:
• The device alarm settings
• Needed alternative ventilation equipment
• If an alternative monitor (i.e., an alarming Pulse Oximeter or
Respiratory Monitor) should be used
Alternative
Ventilation
Patient Disconnect
Protection
For ventilator dependent patients, always have alternate ventilation
equipment, such as a back-up ventilator, manual resuscitator, or similar
device, available.
Ventilator dependent patients should be continuously monitored by
qualied personnel. These personnel should be prepared to provide
alternate therapy in the event of ventilator failure or inoperative
equipment.
For ventilator dependent patients, do not rely on any single alarm
to detect a circuit disconnect condition. The Low Tidal Volume, Low
Minute Ventilation, Low Respiratory Rate, and Apnea alarms should
be used in conjunction with the Circuit Disconnect and Low Peak
Inspiratory Pressure alarms.
Test the operation of the circuit disconnect function daily and
whenever a change is made to the patient circuit. An increase in circuit
resistance can prevent proper operation of some alarms.
Speaking valves, Heat Moisture Exchangers (HMEs), and lters create
additional circuit resistance and may aect the performance of alarms
chosen for circuit disconnect protection.
Do not set the Low Peak Inspiratory Pressure alarm too low, or the
system may not detect large circuit leaks or a patient disconnect.
3
Chapter 1 Introduction
Page 15
4
Personnel
Qualications
Modes of
Ventilation
SD Card
Prescription
Changes
Electrical
Interference
Battery Back-up
Power
Trilogy200 is a restricted medical device designed for use by
Respiratory Therapists or other trained and qualied caregivers under
the supervision of a physician.
The prescription and other device settings should only be changed on
the order of the supervising physician.
The operator of the ventilator is responsible to read and understand
this manual before use.
The device can provide therapies typically associated with both
ventilator dependent and non-dependent patients. The mode of
ventilation, circuit type, and alarm strategies should be chosen after a
clinical evaluation of each patient’s needs.
C-Flex, Bi-Flex, and AVAPS are intended for use by adult patients.
When you change the device prescription, alarms, and other settings
using the SD card, Trilogy200 requires that the caregiver review and
verify the changes prior to the changes being used by the device. The
caregiver or health care professional is responsible to ensure that the
prescription settings are correct and compatible with the patient after
using this feature. Installing the wrong prescription for a particular
patient may result in improper therapy, lack of appropriate safety
monitoring, and risk of death or injury to the patient.
This device is intended for use in the electromagnetic environment
specied in Chapter 13 of this manual. The user of this device should
make sure it is used in a compatible environment.
Portable and mobile RF communications equipment should be
used no closer to any part of the device, including cables, than the
recommended separation distance calculated using the information
provided in Chapter 13 of this manual.
The internal battery is NOT intended to serve as a primary power
source. It should only be used when other sources are not available or
briey when necessary; for example, when changing power sources.
The ventilator has a two-stage low battery alarm. The medium priority
alarm indicates that approximately 20 minutes of operation remain,
and the high priority alarm indicates that less than 10 minutes of
operation remain. Actual run time may be more or less than this and
varies with battery age, environmental conditions, and therapy.
Immediately seek an alternate power source when the “Low Battery”
alarm appears. Complete power failure and loss of therapy is imminent.
Trilogy200 clinical manual
Page 16
5
Operating
and Storage
Temperatures
Do not use this device if the ambient temperature is warmer than
40˚ C (104˚ F). If the device is used at room temperatures warmer than
40˚ C, the temperature of the airow may exceed 43˚ C. This could
cause system alarms, thermal irritation, or injury to the patient’s airway.
Bacteria Filter Philips Respironics recommends that a main line outlet bacteria lter
(Part Number 342077) be used whenever the device is used for invasive
therapy or if the ventilator may be used on multiple patients.
Patient Circuits
(General)
The ventilator should only be used with patient interfaces (e.g., masks,
circuits and exhalation ports) recommended by Philips Respironics.
Proper operation of the device, including alarms, with other circuits has
not been veried by Philips Respironics and is the responsibility of the
health care professional or respiratory therapist.
When adding any components to the breathing system, the ow
resistance and dead space of the added components such as
humidiers, speaking valves, Heat Moisture Exchangers (HMEs) and
lters should be carefully considered in relation to the potential for
adverse eects on the patient’s ventilatory management and device
alarms.
Passive Circuits An exhalation port is required when using a passive circuit.
For the passive circuit, at low expiratory pressures, the ow through
the exhalation port may be inadequate to clear all exhaled gas from
the tubing – some rebreathing may occur. Rebreathing of exhaled air
for longer than several minutes can in some circumstances lead to
suocation.
Active Circuits Only use the active exhalation devices designed for Trilogy200. Philips
Respironics has not veried proper operation of other active exhalation
devices, and their use may result in improper or unsafe device
operation.
With active exhalation circuits, the exhalation device must be operating
properly for the ventilator to deliver therapy. The exhalation device
should be inspected on a daily basis and replaced whenever necessary.
System Checkout Do not use the ventilator on a patient until a system checkout has been
performed. See Chapter 10 of this manual.
To make sure the device is operating properly at start-up, always verify
that the audible tone sounds and the alarm LEDs light red and then
yellow momentarily. Contact Philips Respironics or an authorized
service center for service if these indications do not occur at start-up.
Chapter 1 Introduction
Page 17

6
Remote Alarms When using a remote alarm, make sure you fully test the remote alarm
connector and cable by verifying that:
– Annunciated alarms on the ventilator are also
annunciated on the remote alarm.
– Disconnecting the remote alarm cable from the
ventilator or from the remote alarm results in an alarm
notication at the remote alarm.
The remote alarm should be tested daily.
Oxygen When administering xed-ow supplemental oxygen, the oxygen
concentration may not be constant. The inspired oxygen concentration
will vary, depending on the pressures, patient ows and circuit leak.
Substantial leaks may reduce the inspired oxygen concentration to less
than the expected value. Appropriate patient monitoring should be
used, as medically indicated, such as an alarming pulse oximeter.
This device DOES NOT alarm for loss of the low ow oxygen supply.
This device is intended to be connected to a low ow (0-15 l/min)
oxygen source such as an oxygen concentrator or other oxygen source
equipped with a pressure regulator (set to 50 PSI or less) and a ow
regulator/meter.
Do not connect the device to an unregulated or high pressure oxygen
source.
The device may result in incorrect ow and tidal volume measurements
and improper operation of related alarms if you add low ow oxygen
directly into the patient circuit or mask instead of using the oxygen
inlet on the back of the ventilator.
Oxygen supports combustion. Oxygen should not be used while
smoking or in the presence of an open ame.
If oxygen is used with the device, the oxygen ow must be turned
o when the device is not in use. Explanation of the Warning:
When the device is not in operation and the oxygen ow is left on,
oxygen delivered into the tubing may accumulate within the device’s
enclosure.
Fire or Explosion The ventilator should not be operated in the presence of ammable
gasses. This could cause a re or explosion.
Trilogy200 clinical manual
Page 18

Alarms Respond immediately to any alarm. It may indicate a potentially
life-threatening condition. Refer to the Alarms and Troubleshooting
chapters for more information.
Visually monitor the patient and ventilator at all times during an Alarm
Silence period. Allowing alarms to continue without intervention may
result in harm to the patient.
If the high priority “Low Internal Battery” message appears,
immediately connect the ventilator to an alternate power source. If no
alternate power source is available, immediately place the patient on
an alternate source of ventilation.
If the “Ventilator Inoperable” alarm occurs, immediately place the
patient on an alternate source of ventilation.
You should not rely on any single alarm to detect a circuit disconnect
condition. The Low Tidal Volume, Low Minute Ventilation, Low
Respiratory Rate, and Apnea alarms should be used in conjunction with
the Circuit Disconnect alarm.
Make sure the alarm volume is set loud enough to be heard by the
caregiver. Consider the use of a remote alarm.
Trilogy200 oers the following circuit type selections:
• Passive
• Active Flow
• Active PAP (Proximal Airway Pressure )
7
Improperly
Functioning
Ventilator
The Passive circuit type provides an ESTIMATE of Vte.
Only the Active Flow circuit type directly measures exhaled tidal
volume (Vte).
The Active PAP circuit type DOES NOT measure Vte and only provides
for an indication of the delivered tidal volume (Vti).
If you notice any unexplained changes in the performance of the
device, if it is making unusual sounds, if the device or detachable
battery are dropped, if water is spilled into the enclosure, or if the
enclosure is cracked or broken, discontinue use and contact Philips
Respironics or an authorized service center for service.
Chapter 1 Introduction
Page 19
8
Maintenance Follow the service recommendations provided in Chapter 7 of this
manual.
Periodically inspect electrical cords, cables, and the detachable battery
pack for damage or signs of wear. Discontinue use and replace if
damaged.
Repairs and adjustments must be performed by Philips Respironicsauthorized service personnel only. Unauthorized service could cause
death or injury, invalidate the warranty, or result in costly device
damage.
Cleaning
(Refer to Chapter 7
for detailed cleaning
instructions.)
To avoid electrical shock, always unplug the power cord from the wall
outlet before cleaning the ventilator.
Do not immerse the device in any uids or spray the device with water
or cleaners. Clean the device with a cloth dampened with an approved
cleaner.
If the device has been exposed to rain or dampness, dry the device
including the area around the power cord connection with the power
cord disconnected from the device before applying AC power.
Cautions
A caution indicates the possibility of damage to the device.
Storage The internal and detachable batteries will self-discharge in storage. If it
is desired to keep the batteries fully charged (for example, as a backup ventilator), plug the device into AC power for about eight hours
every 16 days. Alternatively, the ventilator may be left continuously
connected to AC power without battery degradation.
Allowing the batteries to fully discharge will not harm the batteries or
lose device settings, but may require a longer battery charge time prior
to use.
Trilogy200 clinical manual
Page 20
9
Operating
and Storage
Temperatures
The device may only be operated at temperatures between 5˚ C and
40˚ C (41˚ F and 104˚ F).
Do not operate the device in direct sunlight or near a heating
appliance because these conditions can increase the temperature of
the airow delivered to the patient.
Prolonged operation or storage at elevated temperatures may reduce
the service life of the battery and other internal components of the
ventilator.
The ventilator has an internal and detachable Lithium-Ion Battery. Do
not expose the device or detachable battery to temperatures above
40˚ C (104˚ F) during use, or above 60˚ C (140˚ F) during storage. This
will reduce battery life and may increase the risk of re or damage the
battery.
Condensation Condensation may aect operation or accuracy of the device. If the
device has been exposed to either very hot or very cold temperatures
during storage, allow it to adjust to ambient temperature before
starting therapy.
Air Filter The reusable foam inlet lter is required to protect the ventilator from
dirt and dust. Wash periodically and replace when damaged for proper
operation.
Cooling Air Vents Do not block the cooling air vents located on the base and the rear
of the device. This may cause the device to overheat in high ambient
temperatures or at high therapy settings.
Battery Life The internal and detachable batteries wear out based on the amount
of use (hours or full charge-discharge cycles). The battery capacity and
life are also reduced by operation at higher temperatures.
Detachable Battery Only use the Philips Respironics Trilogy Detachable Battery with the
ventilator.
Cleaning Do not steam autoclave the ventilator. Doing so will destroy the
ventilator.
Do not immerse the device in liquid or allow any liquid to enter the
enclosure or inlet lter.
Do not spray water or any other solutions directly onto the ventilator.
Do not use harsh detergents, abrasive cleaners, or brushes to clean the
ventilator system. Use only cleaning agents and methods listed in this
manual.
Chapter 1 Introduction
Page 21
10
Patient Circuit Exhalation valves, patient circuits, and water traps are shipped clean,
not sterile. Cleaning and disinfection of these parts should follow
individual institution processes and conform to guidelines provided by
Philips Respironics with each accessory.
External DC Power Do not use the same external battery to operate both the ventilator
and any other equipment such as power chairs.
An external battery should only be connected to the ventilator using
the Philips Respironics Trilogy External Battery Cable. This cable is
fused, pre-wired, and properly terminated to ensure safe connection
to a standard deep-cycle, lead acid battery. Use of any other adapter or
cable may cause improper operation of the ventilator.
The ventilator should only be connected to an automotive electrical
system using the Philips Respironics Trilogy Automotive Adapter
(when available). This adapter is fused, ltered, and designed for safe
connection to a standard automotive electrical system. Use of any
other adapter or cable may cause improper operation of the ventilator.
Do not operate the ventilator from a car electrical system when
starting the vehicle or jump-starting the vehicle. Electrical transients
during starting may cause improper operation of the ventilator.
Electrostatic
Discharge (ESD)
Do not use antistatic or conductive hoses or conductive patient tubing
with the device.
Notes
• This product does not contain natural latex rubber or dry
natural rubber in patient or operator accessible areas or
in the air path or breathing circuit.
Trilogy200 clinical manual
Page 22

Contraindications
If the patient has any of the following conditions, consult their health
care professional before using the device in a non-invasive mode:
• Inability to maintain a patent airway or adequately clear
secretions
• At risk for aspiration of gastric contents
• Diagnosed with acute sinusitis or otitis media
• Epistaxis, causing pulmonary aspiration of blood
• Hypotension
System Overview
This ventilator provides both pressure control and volume modes of
therapy. The device can provide non-invasive or invasive ventilation.
It can be used to provide total therapy to patients as they progress
from non-invasive to invasive ventilation.
11
When prescribed, the device provides numerous special features to
help make patient therapy more comfortable. For example, the ramp
function allows you to lower the pressure when trying to fall asleep.
The air pressure will gradually increase until the prescription pressure
is reached. Additionally, the Flex comfort feature provides increased
pressure relief during the expiratory phase of breathing.
The ventilator can be operated using several dierent power
sources, including an internal Lithium-Ion battery. This battery is
automatically used when the detachable Lithium-Ion battery pack,
external Lead Acid battery, or AC power are not available.
Chapter 1 Introduction
Page 23
12
O
2
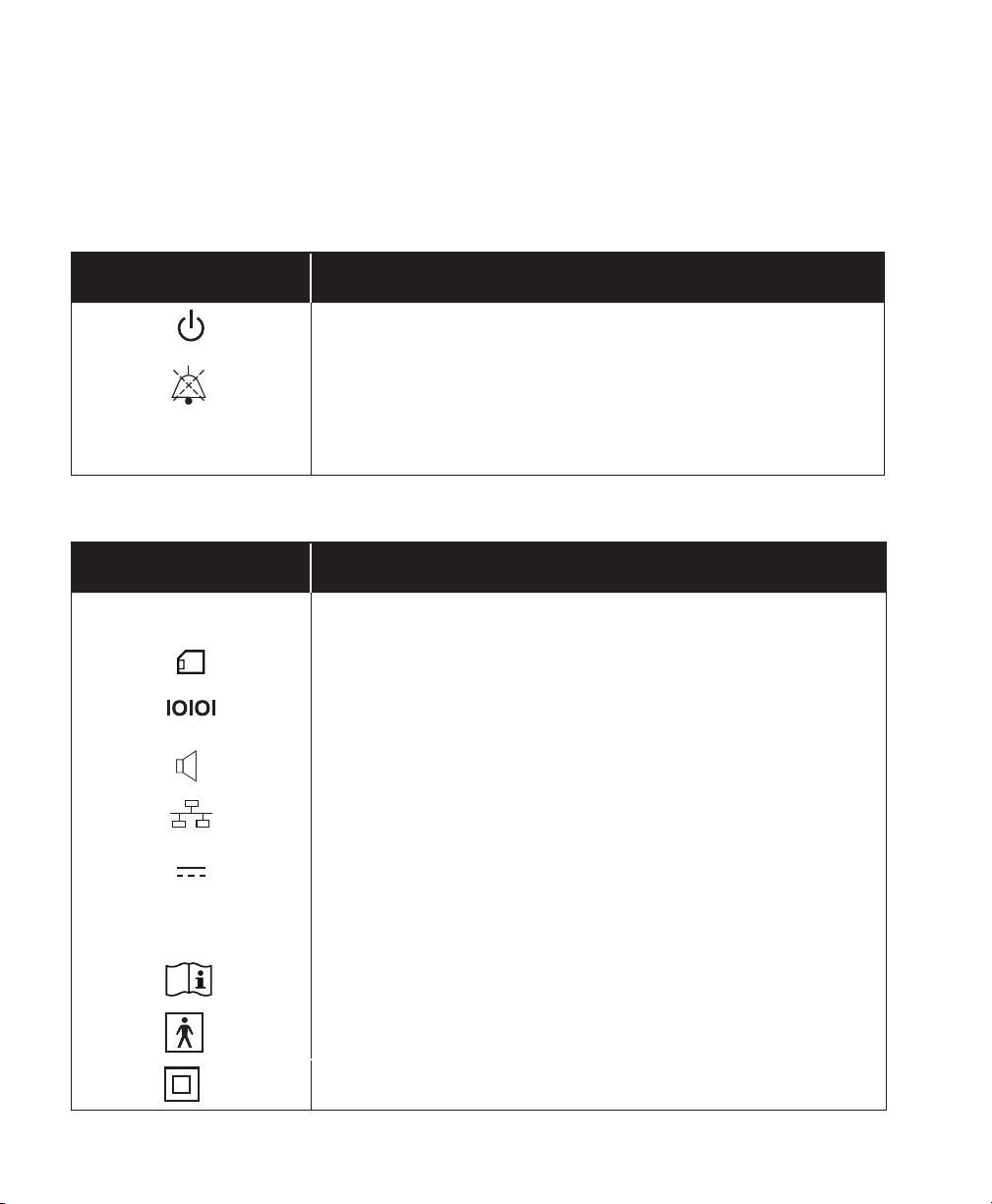
Symbols
The following symbols appear on the device.
Front Panel
Symbol Description
Therapy Start/Stop
Alarm Indicator/Audio Pause
~
AC Power Indicator
Rear and Side Panels
Symbol Description
~
AC Power Connector
Secure Digital (SD) Card Slot
Serial Port Connector
Remote Alarm Connector
Ethernet Connector
DC Power Connector
Oxygen Inlet
Consult accompanying instructions for use.
Type BF Applied Part
Class II (Double Insulated)
Trilogy200 clinical manual
Page 24
Drip Proof Equipment
For Airline Use. Complies with RTCA-D0160F section 21, category M.
How to Contact Philips Respironics
To have your device serviced, contact Philips Respironics Customer
Service department at 1-724-387-4000 or 1-800-345-6443.
13
Chapter 1 Introduction
Page 25

14
Trilogy200 clinical manual
Page 26
Trilogy200
clinical manual
2. System Description
This chapter describes the front and rear panel device controls and
features.
15
2
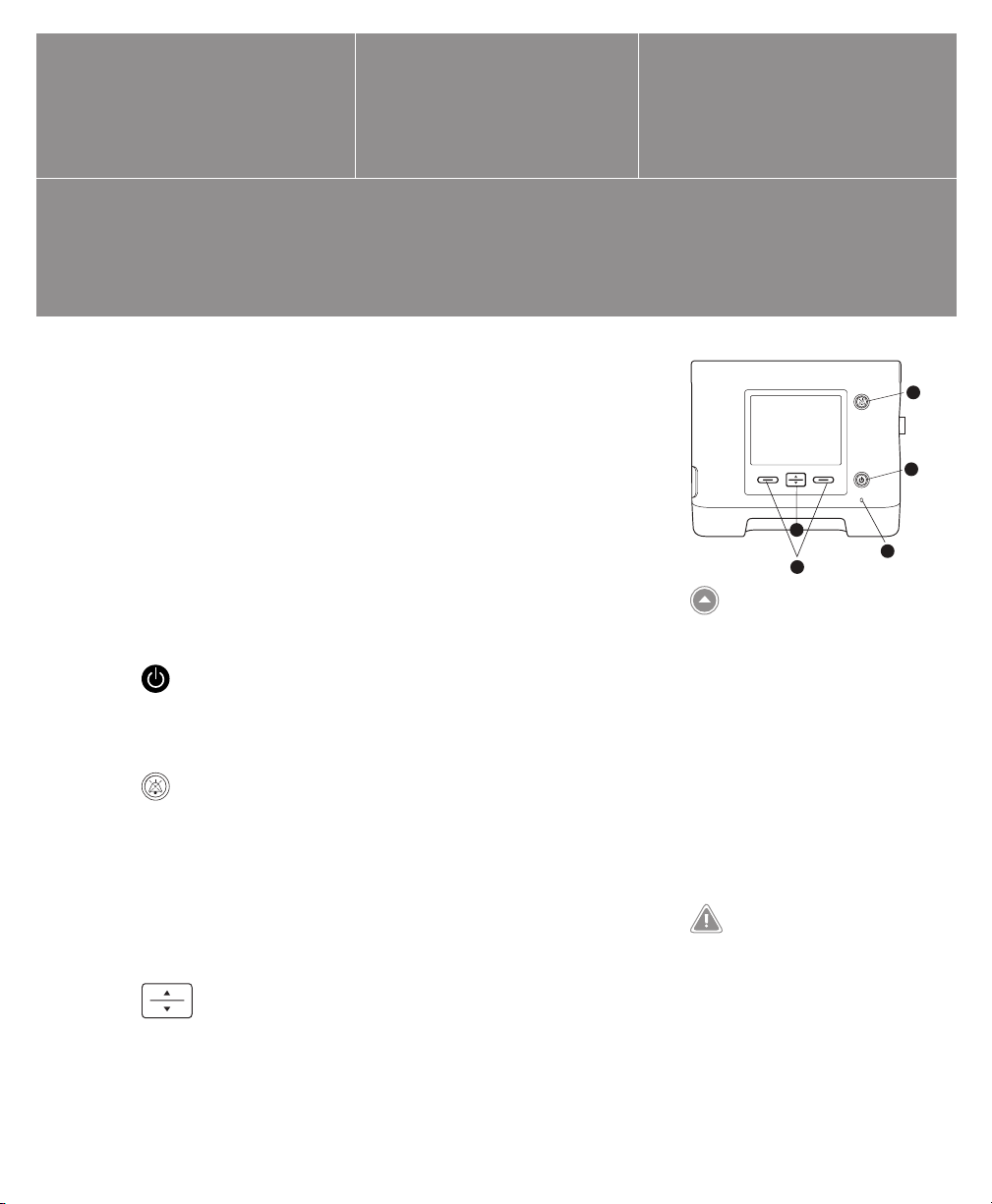
Front Panel Features
The front panel contains the control buttons, visual indicators, and
display screen.
Buttons
The following buttons are included on the front panel of the device.
1. Start/Stop Button
This button turns the airow on or o, starting or stopping
therapy.
2. Alarm Indicator and Audio Pause Button
This button serves two purposes: it temporarily silences
the audible portion of an alarm, and it also acts as an alarm
indicator. When silencing an alarm, if the cause of the alarm is
not corrected, the alarm sounds again after one minute. Each
time the button is pressed, the alarm silence period resets to one
minute. See Chapter 6 for more information.
3. Up/Down Button
This button allows you to navigate the display menu and edit
device settings.
1
3
4
Front Panel Controls and
Display Screen
Note: When you start therapy,
the display backlight and the
backlights on the buttons turn
on, the red and yellow alarm
LEDs turn on momentarily, and
an audible indicator sounds
to indicate that therapy has
started. The Startup screen
appears on the display.
WARNING
To make sure the device is operating
properly at start-up, always verify
that the audible tone sounds and
the alarm LEDs light red and then
yellow momentarily. Contact Philips
Respironics or an authorized service
center for service if these indications
do not occur at start-up.
Chapter 2 System Description
5
Page 27

16
4. Left and Right Buttons
These buttons allow you to select display options or perform
certain actions specied on-screen.
Visual Indicators
Several power and alarm indicators appear on the front panel.
5. AC Power LED
In the lower right corner of the front panel, a green LED (~)
indicates that AC power is applied to the device. This light
remains on as long as adequate AC power is available.
6. Keypad Backlight LEDs
The Start/Stop, Up/Down, and Left/Right buttons all have a white
LED that lights up if the keypad backlight is turned on in the
device Options menu. See Chapter 5 for more information.
7. Red Alarm LED
On the Alarm Indicator/Audio Pause button, a red light ashes to
indicate a high priority alarm.
8. Yellow Alarm LED
On the Alarm Indicator/Audio Pause button, a yellow light
ashes to indicate a medium priority alarm. A solid yellow light
indicates a low priority alarm.
Display Screen
The display screen allows you to view settings, system status
information, real-time patient data, alarms, and logs. You can also
modify certain settings on the display screen.
See Chapter 5 for more information on viewing and modifying
device settings.
Trilogy200 clinical manual
Note: See Chapter 6 for more
information about high,
medium, and low priority
alarms.
Page 28
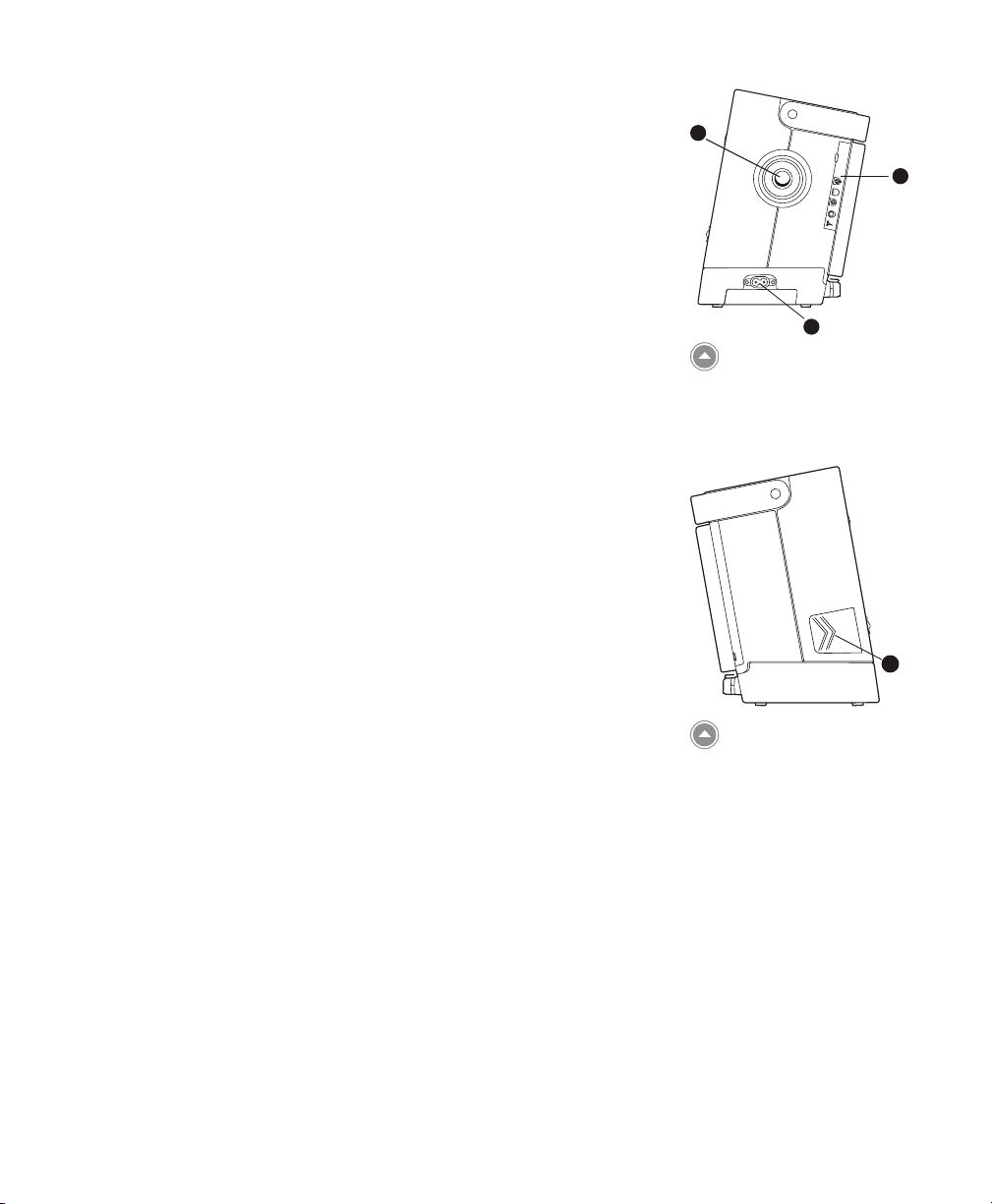
Side and Rear Panel Features
The ventilator’s side and rear panels contain the following connectors
and features, shown at right.
1. AC Power Inlet
You can plug the AC power cord into this connector, located on
the right side of the ventilator.
17
2
3
2. Breathing Circuit Connection
The breathing circuit connector is located on the right side of
the device. You can connect your circuit tubing system here. See
Chapter 4 for details.
3. Exhalation Porting Block
The porting block used here depends on the type of exhalation
device you are using. The Universal Exhalation Porting Block is
shown here. See Chapter 4 for more information.
4. Secure Digital (SD) Card Slot
On the left side of the device is a slot for the optional SD Card.
You can have the patient record usage and therapy information
from the device on the SD card.
1
Right Side Panel
4
Left Side Panel
Chapter 2 System Description
Page 29
18
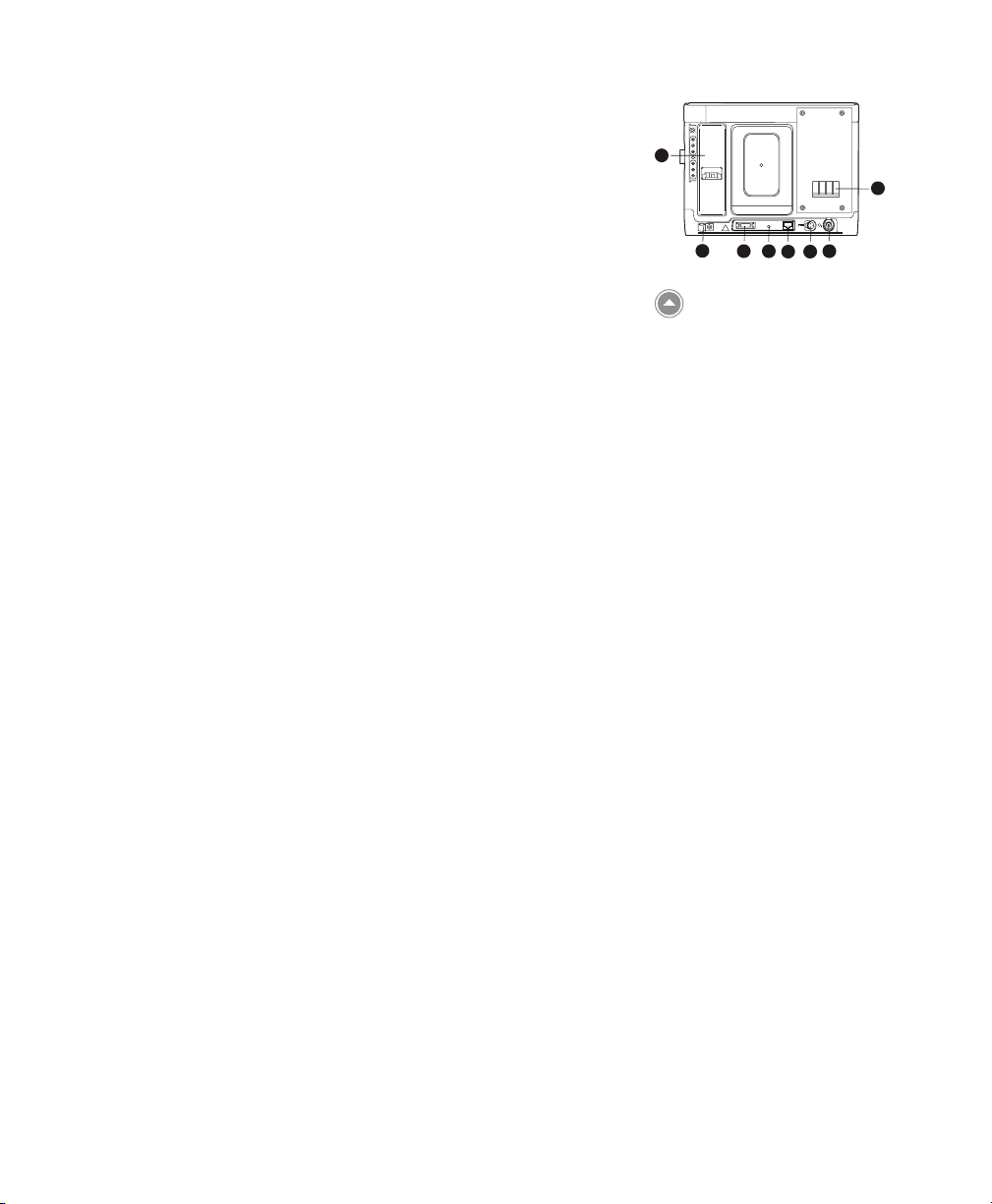
5. Serial Connector
You can use this connector to connect the device to a computer
running PC Direct or Sleepware software or to other Philips
Respironics devices such as Alice 5 and AOM. Use the Trilogy
RS232 Serial Cable to connect the ventilator to the external
device or computer.
6. Remote Alarm/Nurse Call Connector
If you are using an optional remote alarm or nurse call system
with the ventilator, you can connect the Philips Respironics
remote alarm adapter cable or nurse call adapter cable to this
connector.
7. Ethernet Connector (when available)
You can connect a PC or router to this connector to upload
therapy information to a secure web site so you can review
therapy information remotely or remotely troubleshoot and
service the device.
8. External Battery Connector (DC Power Inlet)
You can connect an external, stand-alone lead acid battery here,
using the Trilogy External Battery cable.
9. Oxygen (O2) Inlet Connector
11
12
Rear Panel
10
8
5
6
9
7
If using low ow supplemental oxygen, connect the oxygen
source to this connector using one of the O2 Inlet Quick Connects
provided with the device.
10. Air Inlet and Filter
Insert the lter supplied with the device into the air inlet.
11. Detachable Battery Pack Slot
If you are using the Philips Respironics Lithium-Ion detachable
battery pack to power the device, attach it here.
12. Cord Retainer
Secure the power cord using the cord retainer to prevent
someone from accidentally disconnecting the power cord. See
Chapter 4 for more information.
Trilogy200 clinical manual
Page 30
Trilogy200
clinical manual
3. Modes, Features, and Alarms
Therapy Modes
The device provides Pressure Control Ventilation (PCV) and Volume
Control Ventilation (VCV) for non-invasive and invasive patients.
Pressure Control ventilation delivers a prescribed pressure to
the patient according to set breath rate and set inspiration time
parameters. This means that each breath is controlled so that a
prescribed amount of pressure is delivered to the patient. The device
oers six dierent Pressure Control modes of operation:
19
• CPAP – Continuous Positive Airway Pressure
• S – Spontaneous Ventilation
• S/T – Spontaneous/Timed Ventilation
• T – Timed Ventilation
• PC – Pressure Control Ventilation
• PC-SIMV – Pressure Controlled Synchronized Intermittent
Mandatory Ventilation
Volume Control ventilation delivers a prescribed inspired tidal
volume to the patient according to set breath rate and set inspiratory
time parameters. This means that each breath is controlled so that a
prescribed tidal volume is delivered to the patient. The device oers
three dierent Volume Control modes of operation:
• AC – Assist Control Ventilation
• CV – Control Ventilation
• SIMV – Synchronized Intermittent Mandatory Ventilation
Chapter 3 Modes, Features, and Alarms
Page 31

20
Breath Types
There are four breath types that apply to the Volume Control and
Pressure Control ventilation therapy modes:
• Spontaneous
• Mandatory
• Assisted
• Sigh
Spontaneous Breath
A Spontaneous breath is triggered by the patient. Breaths are
initiated by the patient’s inhalation eort, and air delivery is
controlled based on the current pressure or volume setting. Breaths
are terminated by either the ventilator settings or by the patient’s
exhalation eort, depending on the mode selected.
Mandatory Breath
A Mandatory breath (or machine breath) is completely controlled by
the ventilator. The ventilator controls both the beginning (triggering)
and end (cycling) of the inspiratory phase.
Assisted Breath
An Assisted breath is controlled by both the patient and the ventilator.
Breaths are initiated by the patient’s eort and air delivery is controlled
by the current pressure or volume settings. Volume Assisted breaths
will deliver the prescribed Tidal Volume within the prescribed
Inspiratory Time. Pressure Assisted breaths will deliver the prescribed
Inspiratory Pressure for the prescribed Inspiratory Time. Breaths are
terminated when the Inspiratory Time setting has been reached.
Sigh
A Sigh breath is a breath where 150% of the prescribed volume
is delivered. The device will deliver this breath once every 100
Mandatory or Assist breaths when the Sigh setting is enabled. Sigh
breaths are only available in volume modes of ventilation.
Trilogy200 clinical manual
Page 32

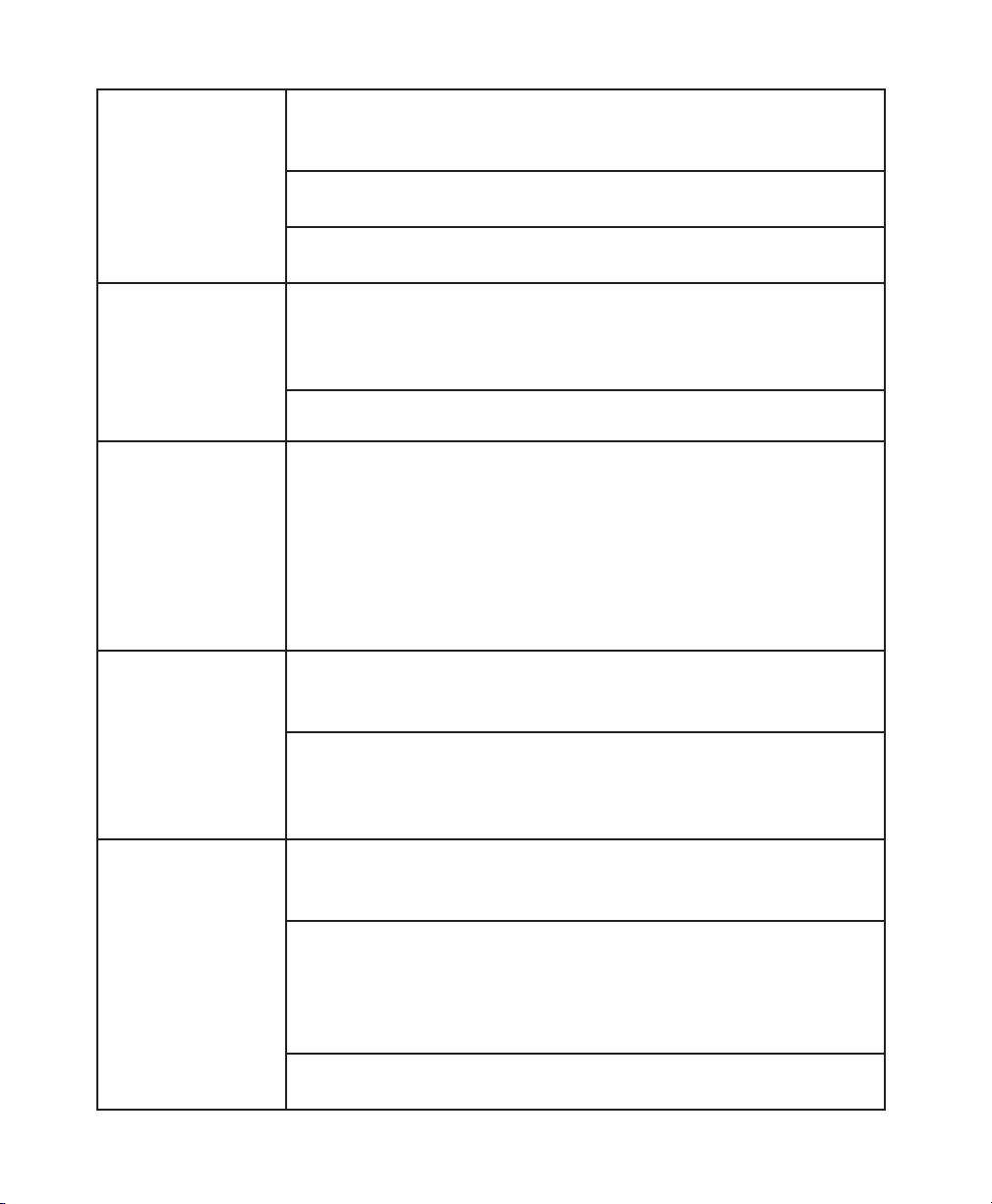
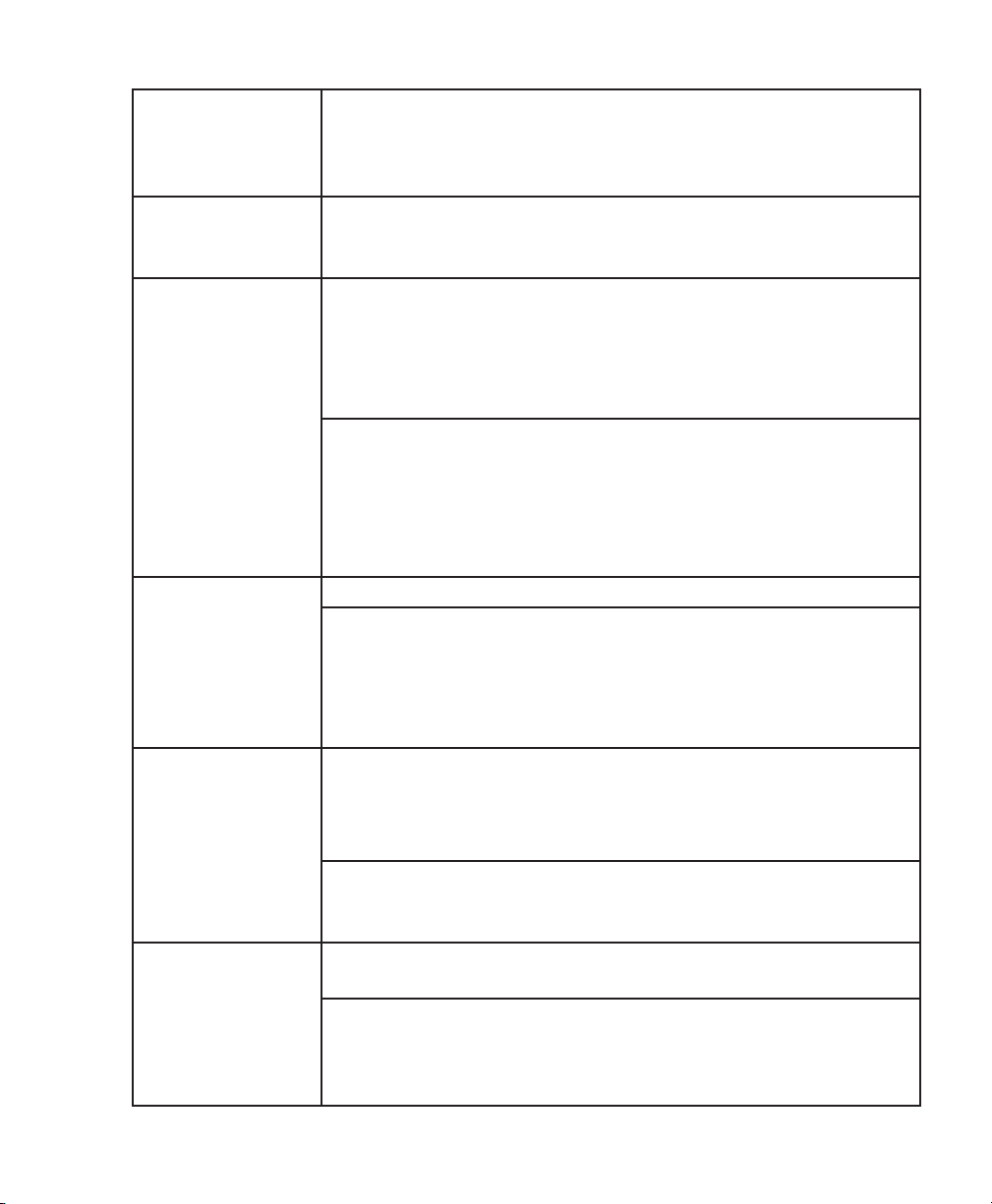
Therapy Mode Table
The following table summarizes all of the therapy modes and the settings available in each mode. Some settings in the table
are dependent upon other settings. For instance, if the circuit type is set to Active with Flow, then the Flow Trigger Sensitivity,
Leak Compensation, and Flow Cycle settings will display.
Note: Pressure Support, referred to in the table below and later in this manual, is dened as IPAP - EPAP or Pressure PEEP (PC-SIMV).
Therapy Modes
CPAP S S/T T PC PC-SIMV CV AC SIMV
Dual Prescription √ √ √ √ √ √ √ √ √
Circuit Type √ √ √ √ √ √ √ √ √
CPAP √
IPAP √ √ √ √
AVAPS (On, O)* √ √ √ √
IPAP Max Pressure √ √ √ √
IPAP Min Pressure √ √ √ √
EPAP √ √ √ √
Pressure √
Pressure Support (PS) √ √
PEEP √ √ √ √
Tidal Volume √ √ √ √ √ √ √
Breath Rate √ √ √ √ √ √ √
Inspiratory Time √ √ √ √ √ √ √
Trigger Type* √ √ √ √ √ √ √
Flow Trigger Sensitivity √ √ √ √ √ √ √
Leak Compensation √ √ √ √ √ √ √
Flow Cycle Sensitivity √ √ √ √ √
Ramp Length √ √ √ √ √
Ramp Start Pressure √ √ √ √ √
Flex * √ √
Rise Time √ √ √ √ √ √
Flow Pattern √ √ √
Therapy Parameters
Sigh √ √ √
Circuit Disconnect √ √ √ √ √ √ √ √ √
Apnea √ √ √ √ √ √ √ √ √
Apnea Rate √ √ √ √ √ √ √ √
High Vte* √ √ √ √ √ √ √ √ √
Low Vte* √ √ √ √ √ √ √ √ √
High Vti* √ √ √ √ √ √ √ √ √
Low Vti* √ √ √ √ √ √ √ √ √
High Minute Ventilation √ √ √ √ √ √ √ √ √
Low Minute Ventilation √ √ √ √ √ √ √ √ √
High Respiratory Rate √ √ √ √ √ √ √ √ √
Low Respiratory Rate √ √ √ √ √ √ √ √ √
High Inspiratory Pressure √ √ √
Low Inspiratory Pressure √ √ √
* Trigger Type, AVAPS, and Flex settings are only available with the Passive circuit type. High Vte and Low Vte settings are only
available for Passive and Active Flow circuit types. High Vti and Low Vti settings are only available with the Active PAP circuit
type. Leak compensation is only available with the Active Flow circuit type.
21
Chapter 3 Modes, Features, and Alarms
Page 33

22
Pressure Control Ventilation Therapy Modes
Pressure Control ventilation modes deliver a prescribed pressure to
the patient.
Continuous Positive Airway Pressure (CPAP) Mode
In the Continuous Positive Airway Pressure (CPAP) mode, the device
delivers a continuous pressure to the patient at all times. All breaths
in this mode are Spontaneous breaths.
Spontaneous (S) Mode
In Spontaneous (S) mode, the device delivers bi-level pressure
support. This mode provides only spontaneous breaths. In this
mode, an Inspiratory Positive Airway Pressure (IPAP) is delivered
during inhalation and a lower Expiratory Positive Airway Pressure
(EPAP) is delivered during exhalation. The following illustration
describes these concepts.
PRESSURE
26
20
10
6
Enter S mode
5 10 15 20
Trilogy200 clinical manual
IPAP = 26 cm H2O
EPAP = 6 cm H
PS = IPAP-EPAP = 20 cm H
5 seconds 4 seconds 8 seconds
1 1 1
O
2
O
2
= Pressure Supported
1
Spontaneous Breath
1
S Mode
TIME
Page 34

Spontaneous/Timed (S/T) Mode
In Spontaneous/Timed (S/T) mode, the device delivers bi-level
pressure support. This mode provides Spontaneous and Mandatory
breaths. A Mandatory breath is delivered if the patient does not
spontaneously breathe within the prescribed Breath Rate (BPM)
setting. This ensures that the patient receives a minimum number
of breaths per minute. In this mode, an IPAP is delivered during
inhalation and a lower EPAP is delivered during exhalation. The
duration of a Spontaneous breath is determined by the patient eort.
The duration of a Mandatory breath is determined by the inspiratory
time setting. The following illustration describes these concepts.
23
PRESSURE
26
20
10
6
Enter S/T mode
IPAP = 26 cm H
EPAP = 6 cm H
Rate = 10 BPM
PS = IPAP-EPAP = 20 cm H
O
2
O
2
6 seconds
1 1
O
2
6 seconds 6 seconds
= Pressure Supported
1
Spontaneous Breath
= Mandatory Breath
2
(note longer inspiratory
time)
2
5 10 15 20
S/T Mode
1
TIME
Chapter 3 Modes, Features, and Alarms
Page 35

24
Timed (T) Mode
In Timed (T) mode, the device delivers bi-level pressure support.
This mode delivers Mandatory breaths only. A Mandatory breath
is delivered according to the prescribed BPM and inspiratory time
settings. This also means that the ventilator will not respond to
patient eort. In this mode, an IPAP is delivered during inhalation and
a lower EPAP is delivered during exhalation. The following illustration
describes these concepts.
PRESSURE
26
20
10
6
IPAP = 26 cm H2O
EPAP = 6 cm H
Rate = 10 BPM
PS = IPAP-EPAP = 20 cm H
O
2
O
2
6 seconds 6 seconds 6 seconds 6 seconds
2 2 22
Enter T mode
5 10 15 20 25
= Mandatory Breath
2
TIME
T Mode
Trilogy200 clinical manual
Page 36

Pressure Control (PC) Mode
In Pressure Control (PC) mode, the device delivers bi-level pressure
support. This mode delivers Assist and Mandatory breaths. This
mode is identical to S/T mode, except that all breaths have a xed
inspiratory time.
25
PRESSURE
26
20
10
6
IPAP = 26 cm H
EPAP = 6 cm H
Rate = 10 BPM
PS = IPAP-EPAP = 20 cm H
6 seconds
3 3
Enter PC mode
5 10 15 20
O
2
O
2
O
2
6 seconds 6 seconds
3
2
= Mandatory Breath
2
= Assist Breath
3
TIME
Pressure Control - Synchronized Intermittent Mandatory
Ventilation (PC-SIMV) Mode
The Pressure Control – Synchronized Intermittent Mandatory
Ventilation (PC-SIMV) mode provides Spontaneous, Assist, and
Mandatory breaths. This mode uses a time window to decide
what type of breaths should be delivered. This time window is the
maximum time between breaths according to the set Breath Rate.
When you enter PC-SIMV mode, the time window is started. If
the patient does not trigger a breath, the ventilator will provide
a Mandatory breath when the time expires and then begin the
process again. Mandatory breaths deliver the Pressure setting during
inhalation and a lower Peak End Expiratory Pressure (PEEP)
during exhalation.
PC Mode
Chapter 3 Modes, Features, and Alarms
Page 37

26
During the time window, if patient eort is detected, either a
Spontaneous or an Assist breath is delivered for the rst eort. If the
last breath delivered was Mandatory, then a Spontaneous breath is
delivered for the rst patient eort of the window. If the last breath
delivered was an Assist or Spontaneous breath, then an Assist breath
is delivered for the rst patient eort of the window. Assist breaths
deliver the Pressure setting during inhalation and the PEEP setting
during exhalation.
During the time window, if patient eort continues to be detected
(after the rst patient triggered breath), Spontaneous breaths are
delivered for the remainder of the window. The gure below provides
example breath patterns in PC-SIMV mode.
PRESSURE
26
20
10
6
Pressure = 26 cm H2O
Pressure Support = 10 cm H
PEEP = 6 cm H
Rate = 5 BPM
12 seconds
S S
2
Enter PC-SIMV mode
O
2
12 seconds 12 seconds 12 seconds
3
O
2
111
= Spontaneous
1
Breath
= Mandatory Breath
2
= Assist Breath
3
M MM M
= Mandatory Window
M
= Spontaneous Window
S
5 10 15 20 25 30 35 40 45
Sample Breath Patterns in
2
TIME
PC-SIMV Mode
Trilogy200 clinical manual
Page 38

Volume Control Ventilation Therapy Modes
Volume Control ventilation modes deliver a prescribed inspired tidal
volume according to a set Breath Rate and a set Inspiratory Time.
Control Ventilation (CV) Mode
In Control Ventilation (CV) mode, the device delivers volume control
therapy. This mode provides only Mandatory breaths. A Mandatory
breath is delivered according to the prescribed BPM setting for the
prescribed Inspiratory Time. This also means that the ventilator
will not respond to patient eort. In this mode, the Tidal Volume is
delivered during inhalation and PEEP is delivered during exhalation.
The following illustration describes these concepts.
27
50
-50
FLOW
0
Enter CV mode
Tidal Volume = 500 mL
Rate = 10 BPM
Inspiratory Time = 1.5 seconds
Flow Pattern = Square
2 2 2
5
= Mandatory Breath
2
6 seconds 6 seconds6 seconds 6 seconds
15 10
20
Control Mode
TIME
Chapter 3 Modes, Features, and Alarms
Page 39

28
Assist Control (AC) Mode
In Assist Control (AC) mode, the device delivers volume control
therapy. This mode provides Assist and Mandatory breaths. An Assist
breath is started when there is patient eort, but it is ended when
the Inspiratory Time setting has been met. A Mandatory breath
is delivered if the patient does not spontaneously breathe within
the prescribed BPM setting. This ensures that the patient receives
a minimum number of breaths per minute. In this mode, the Tidal
Volume is delivered during inhalation and PEEP is delivered during
exhalation. The following illustration describes these concepts.
= Mandatory Breath
6 seconds6 seconds 5 seconds
15 10
2
= Assist Breath
3
20
TIME
50
-50
FLOW
0
Tidal Volume = 500 mL
Rate = 10 BPM
Inspiratory Time = 2.0 seconds
Flow Pattern = Square
Enter A/C mode
2 3 2
5
Assist Control Mode
Synchronized Intermittent Mandatory Ventilation (SIMV) Mode
In Synchronized Intermittent Mandatory Ventilation (SIMV) mode, the
device delivers both volume control and pressure control therapy.
This mode provides Spontaneous, Assist, and Mandatory breaths.
This mode uses a time window to decide what type of breaths should
be delivered. This time window is the maximum time between
breaths according to the set Breath Rate.
When you enter SIMV mode, the time window is started. If the
patient does not provide any eort, the ventilator will provide a
Mandatory Volume breath when the time expires and then begin the
process again. Mandatory breaths deliver the Tidal Volume setting
during inhalation and provide a lower Peak End Expiratory Pressure
(PEEP) during exhalation.
Trilogy200 clinical manual
Page 40

During the time window, if patient eort is detected, either a
Spontaneous or an Assist breath is delivered for the rst eort. If the
last breath delivered was Mandatory, then a Spontaneous breath is
delivered for the rst patient eort of the window. If the last breath
delivered was an Assist or Spontaneous breath, then an Assist breath
is delivered for the rst patient eort of the window. Assist breaths
deliver the prescribed Tidal Volume during inhalation and the PEEP
setting during exhalation.
During the time window, if patient eort continues to be detected
(after the rst patient triggered breath), Spontaneous breaths are
delivered for the remainder of the window. Spontaneous breaths
deliver the prescribed Pressure Support setting above PEEP during
inhalation and PEEP during exhalation. The gure below provides
example breath patterns in SIMV mode.
29
Tidal Volume = 500 mL
Breath Rate = 5 BPM
Inspiratory Time = 3.0 seconds
Pressure Support = 10 cm H
PEEP= 6 cm H
PRESSURE
26
20
10
2
6
Enter SIMV mode
5 10 15 20 25 30 35 40 45
O
O
2
2
S S
3
= Pressure Supported
1
Breath
= Mandatory Breath
2
= Assist Breath
3
111
= Mandatory Window
M
= Spontaneous Window
S
M MM M
12 seconds12 seconds12 seconds12 seconds
2
SIMV Mode
TIME
Chapter 3 Modes, Features, and Alarms
Page 41

30
Therapy Mode Features
The device has several additional features that enhance patient
comfort.
Flex Comfort Feature
The device consists of a special comfort feature called Flex. The
device provides the Flex feature in CPAP mode and S mode. This
feature is only available when Auto-Trak is enabled.
C-Flex
When in CPAP mode, if C-Flex is enabled, it enhances patient comfort
by providing pressure relief during the expiratory phase of breathing.
In the following diagram, the dashed lines represent normal CPAP
therapy in comparison to the bold line representing C-Flex. C-Flex
levels of 1, 2, or 3 progressively reect increased pressure relief.
PRESSURE
CPAP
Inhalation Exhalation
1
2
3
TIME
Note: Flex is not available if
AVAPS is enabled or if an active
circuit is used.
Note: The patient has access to
this setting, if Flex is enabled.
Note: C-Flex is not available if
CPAP is set to 4 cm H2O.
Note: C-Flex, Bi-Flex and AVAPS
are intended for use by adult
patients.
C-Flex in Comparison to
Traditional CPAP Therapy
C-Flex pressure relief is determined by the C-Flex setting and the
amount of patient ow. C-Flex returns to the set pressure by the end
of exhalation, when the airway is most vulnerable to closure.
Trilogy200 clinical manual
Page 42

Bi-Flex
PRESSURE
In S mode, the Bi-Flex attribute adjusts therapy by inserting a small
amount of pressure relief during the latter stages of inspiration and
during the beginning part of exhalation. In the following diagram,
the bold lines represent Bi-Flex in comparison to the dashed line
representing normal BiPAP therapy. Bi-Flex levels of 1, 2, or 3
progressively reect increased pressure relief that will take place at
the end of inspiration and at the beginning of expiration.
31
Note: Bi-Flex is only available
up to 25 cm H2O in S mode.
IPAP
EPAP
Bi-Flex
BiPAP
1
2
3
TIME
Ramp
The device is equipped with a linear ramp function. In CPAP, S, S/T, T,
and PC modes, the Ramp feature will reduce the pressure and then
gradually increase (ramp) the pressure to the prescription pressure
setting so patients can fall asleep more comfortably. The gure below
illustrates how the ramp function works.
Bi-Flex in Comparison to
Traditional Bi-Level Therapy
Note: IPAP will not ramp below
4 cm H2O.
The Ramp Function
TIME
Chapter 3 Modes, Features, and Alarms
Page 43

32
Rise Time
Rise Time
In S, S/T, PC, T, PC-SIMV, and SIMV modes, rise time is the amount
of time it takes the device to change from the expiratory pressure
setting to the inspiratory pressure setting. Rise time levels of 1, 2,
3, 4, 5, or 6 progressively reect slowed response of the pressure
increase that will take place at the beginning of inspiration. Adjust
the rise time to nd the most comfortable setting for the patient.
PRESSURE
IPAP
EPAP
TIME
AVAPS Feature
Average Volume Assured Pressure Support (AVAPS) is a feature
available in the S, S/T, PC, and T modes. It helps patients maintain
a tidal volume (VT) equal to or greater than the target tidal volume
(Volume setting in the ventilator) by automatically controlling the
pressure support (PS) provided to the patient. The AVAPS feature
adjusts PS by varying the IPAP level between the minimum (IPAP Min)
and maximum (IPAP Max) settings. AVAPS averages VT and changes
the PS value gradually. This occurs over several minutes. The rate of
change is slow, so that the patient is not aware of breath-to-breath
pressure changes.
As patient eort decreases, AVAPS automatically increases PS to
maintain the target tidal volume. The IPAP level will not rise above
IPAP Max, even if the target tidal volume is not reached. Conversely,
as patient eort increases, AVAPS will reduce PS. IPAP will not fall
below IPAP Min, even if the target tidal volume is exceeded.
Rise Time
Note: AVAPS is only available if
you are using a passive circuit.
Note: C-Flex, Bi-Flex and AVAPS
are intended for use by adult
patients.
If the Ramp function has been activated, it will take precedence over
the AVAPS feature. Once ramp is complete, AVAPS will resume.
Trilogy200 clinical manual
Page 44

IPAP Max
PRESSURE
IPAP Min
EPAP
VOLUME
Target
Volume
15 30 45 60
33
TIME
AVAPS Feature
15 30 45 60
TIME
Flow Pattern Types
Two ow patterns are available in Volume Control ventilation therapy
modes:
• Square
• Ramp
Square
With a square wave pattern, airow is generally constant throughout
inspiration of the breath.
FLOW
TIME
Square Flow Pattern
Chapter 3 Modes, Features, and Alarms
Page 45

34
Ramp
With a ramp ow pattern, the airow starts high and decreases
throughout inspiration of the breath.
FLOW
50% of
Peak Flow
TIME
For the active circuit in volume modes, peak ow is required to be
a minimum of 20 l/min. The wave form may be attened when the
combination of Inspiratory Time and Tidal Volume set points would
result in a ow of less than 20 l/min. Therefore, for some settings,
a Ramp ow pattern may provide a pattern that more closely
resembles a Square ow pattern.
Ramp Waveform Pattern
Trilogy200 clinical manual
Page 46

Sigh Feature
FLOW
The sigh feature is available for Volume ventilation modes only.
When the sigh feature is enabled, the ventilator delivers a sigh breath
in place of every 100th mandatory or assisted breath delivered
regardless of the mode of operation (i.e., AC, CV, and SIMV). The Sigh
breath is delivered using a volume equal to 150% of the set volume
that was in eect when the breath was initiated.
Dual Prescription Feature
35
Example of Sigh Feature
The device provides a dual prescription feature that allows you
to enter a primary prescription and a secondary prescription for
the patient if needed. For example, you can set a primary daytime
prescription and secondary nighttime prescription. See Chapter 5 for
more information on the dual prescription feature.
Chapter 3 Modes, Features, and Alarms
Note: Both prescriptions must
use the same circuit type.
Page 47

36
Triggering
The device can be set to trigger breaths using the Auto-Trak or Flow
Trigger sensitivity features.
Digital Auto-Trak Sensitivity
An important characteristic of the device is its ability to recognize
and compensate for unintentional leaks in the system and to
automatically adjust its trigger and cycle algorithms to maintain
optimum performance in the presence of leaks. This feature is known
as Digital Auto-Trak Sensitivity. The following sections examine this
function in detail by describing the leak tolerance function and
sensitivity.
Leak Tolerance
A microprocessor monitors the total ow of the patient circuit and
calculates patient ow values.
A. Leak Estimation: Average and Parabolic
The device uses two leak estimation algorithms. A conservation
of mass algorithm is used to compute the average leak for a given
pressure support relationship. This average leak is used when large
leak variations are present in the system. Average leak is a high
estimate during EPAP pressure and a low estimate during IPAP
pressure. A better leak estimate, enabled by the digital system, is the
parabolic leak algorithm. Parabolic leak is proportional to the square
of the patient pressure; therefore, the leak estimate is correlated to
the changing patient pressure. Both algorithms include unintentional
circuit leak and are averaged over several breaths.
B. Patient Flow
The total circuit ow is comprised of the circuit leak and the patient
ow. The calculated patient ow is the total ow minus the circuit
leak. Patient ow is a primary input into the triggering and cycling
mechanisms.
Trilogy200 clinical manual
Page 48

Auto-Trak Sensitivity
An essential feature of the device while operating in all modes is
its ability to eectively sense spontaneous breathing eorts, which
causes the ventilator to trigger to inspiration and cycle to expiration.
Because no preset sensitivity threshold can assure patient and
machine synchrony with changing breathing eorts and circuit
leaks, the device continuously tracks patient breathing patterns
and automatically adjusts sensitivity thresholds to ensure optimum
sensitivity as breathing patterns change or as circuit leaks change.
The algorithms used to ensure optimum sensitivity are the Volume
Trigger, Shape Signal, Spontaneous Expiratory Threshold (SET), Flow
Reversal, Maximum IPAP Time, and Volume Control Cycle.
Volume Trigger (Expiration to Inspiration):
The volume trigger is one method used to trigger inspiration during
spontaneous breathing in all modes except T and CV. The volume
trigger threshold is 6 ml of accumulated patient inspiratory volume.
When patient eort generates inspiratory flow causing 6 ml of
volume, inspiration is triggered.
37
Note: Auto-Trak is only
available if you are using a
passive circuit.
Shape Trigger/Shape Cycle (Expiration to Inspiration) (Inspiration to
Expiration):
The shape trigger/cycle is another method used to trigger inspiration
and/or cycle from inspiration to expiration during spontaneous
breathing in all modes except T and CV. This method continuously
tracks patient inspiratory and expiratory flow and adjusts the
spontaneous trigger and cycle thresholds for optimum sensitivity.
The Shape Signal appears as a shadow image of the patient’s actual
flow. The shape signal functions as a sensitivity threshold at either
inspiration or expiration. When the patient’s flow rate crosses the
shape signal the unit changes pressure levels. The following gure
illustrates how the shape signal is super-imposed onto the actual
waveform to trigger and cycle o IPAP. The shape signal is created
by osetting the signal from the actual patient flow by 15 l/min and
delaying it for a 300 msec period. This intentional delay causes the
shape signal to be slightly behind the patient’s flow rate.
Chapter 3 Modes, Features, and Alarms
Page 49

38
IPAP
A sudden change in patient flow will cross the shape signal, causing
the pressure level to change.
Pressure
EPAP
Cycle to
Shape
Signal
EPAP
Crossover
Point
Flow
Estimated
Patient
Flow
Trigger to
IPAP
Crossover
Point
Tracking the patient’s flow pattern with the Shape Signal provides a
sensitive mechanism to trigger to inspiration or cycle to expiration in
response to changing breathing patterns and circuit leaks.
Shape Signal
Trilogy200 clinical manual
Page 50

Spontaneous Expiratory Threshold (Inspiration to Expiration):
IPAP
A second method used to cycle to expiration during spontaneous
breathing in all modes except T, CV, AC, and SIMV, is called
Spontaneous Expiratory Threshold (SET). The SET rises in proportion
to the inspiratory flow rate on each breath. When the SET and actual
patient flow value are equal, the unit cycles to expiration.
Pressure
EPAP
Spontaneous
Expiratory
Threshold
Flow
39
Spontaneous Expiratory
Threshold
Flow Reversal (Inspiration to Expiration):
As ow begins to decrease during inspiration, a ow reversal can
occur due to a large leak around the mask or because the patient’s
mouth is open. When the device senses this ow reversal, it
automatically cycles to expiration.
Maximum IPAP Time (Inspiration to Expiration):
The maximum inspiratory time is determined by the adjustment of
the Inspiratory time setting. A maximum IPAP time of 3.0 seconds
acts as a safety mechanism to limit the time spent in inspiration
during spontaneous breathing. For mandatory or assisted breaths,
the maximum inspiratory time will equal the Inspiratory time setting
up to 5.0 seconds.
Chapter 3 Modes, Features, and Alarms
Page 51

40
Volume Control Cycle (Inspiration to Expiration) (Only available
during Volume Control Therapy)
An Inspiratory Time setpoint limits the time spent in inspiration
during breathing in all modes. Once the time limit is reached, the unit
automatically cycles to expiration.
Flow Trigger
Flow trigger provides a manual setting that allows for breath
initiation and termination based on a set ow trigger sensitivity and
ow cycle sensitivity.
Flow Trigger Sensitivity (Expiration to Inspiration):
The ow trigger initiates when the patient’s inspiratory eort creates a ow
equal to or greater than the ow trigger sensitivity setting. The method of
the ow trigger is dependent upon the circuit type that is chosen.
Leak Compensation:
When using the Passive Circuit conguration, compensation for both the
intentional and unintentional leak is included in the triggering method.
When using the Active PAP Circuit conguration, leak compensation
is not available.
When using the Active Flow Circuit conguration, ow trigger with
leak compensation may be enabled. The default setting when using
the Active Flow Circuit is Leak Compensation On. The clinician has
the option to turn o leak compensation; however, unintentional
leak will not be compensated. Both options measure the ow at the
proximal ow sensor.
Flow Cycle Sensitivity (Inspiration to Expiration):
This cycling method is only active if the Flow Trigger has been
selected for the Trigger Type. As ow begins to decrease during
inspiration, if the patient ow is less than the ow cycle sensitivity
setting, the device will cycle to expiration.
For example: if the ow cycle sensitivity setting is set to 75%, when
the ow has decreased by 25% of the peak ow, the device will cycle
to the EPAP/PEEP level.
Trilogy200 clinical manual
Note: Enabling Leak
Compensation when using the
Active Flow Circuit conguration
only aects triggering and does
not aect tidal volume delivery
or Vte measurement.
Page 52

BTPS Compensation
All ows and volumes used in Trilogy are expressed in BTPS - Body
Temperature atmospheric Pressure Saturated with H2O.
All pressures are expressed relative to atmospheric pressure.
Ventilator Alarms
This section describes all of the ventilator alarms and informational
messages in order of priority, from high priority alarms to low priority
alarms and nally informational messages. Refer to Chapter 6 for
more information on alarms.
Loss of Power Alarm
This is a high priority alarm. It may occur when a complete power
failure has occurred and power was lost while the device was
providing therapy. This may happen if the internal battery was the
only power source in use and was completely depleted.
41
Ventilator Inoperative Alarm
This is a high priority alarm. It occurs when the ventilator detects an
internal error or a condition that may aect therapy. The device will
shut down if the cause of the failure indicates that the device cannot
deliver therapy safely. If the device can deliver therapy at a limited
level, the device will continue to deliver limited therapy.
Ventilator Service Required Alarm
This is a high priority alarm. It occurs when the device cannot
perform to specication, a backup safety feature is compromised,
or the delivery of therapy is compromised. The device continues to
operate (possibly in a reduced capacity mode). If the problem is not
corrected, the device will generate a reminder message once per
hour until the issue is corrected. Additionally, if therapy is stopped, a
reminder message will immediately appear when therapy is turned
on again.
Chapter 3 Modes, Features, and Alarms
Page 53

42
Check Circuit Alarm
This is a high priority alarm. It occurs when the device detects a
problem with the patient circuit, such as pinched or detached tubing,
water condensation in the proximal pressure lines, or problems with
the active exhalation device.
Low Circuit Leak Alarm
This is a high priority alarm that only occurs with the passive circuit.
It occurs when the system detects a problem with the leak device in
the passive circuit.
High Expiratory Pressure Alarm
This is a high priority alarm. It occurs when the delivered pressure
exceeds the target patient pressure during the expiratory phase by
5 cmH2O. This may be due to pinched tubing or the patient having
a fast breath rate. The device continues to operate. The alarm will
automatically terminate when the delivered pressure comes within
5 cmH2O of the target patient pressure during the expiratory phase.
Low Expiratory Pressure Alarm
This is a high priority alarm. It occurs when the delivered pressure
is 5 cmH2O or more below the target patient pressure during the
expiratory phase. The device continues to operate. The alarm will
automatically terminate when the delivered pressure comes within
5 cmH2O of the target patient pressure during the expiratory phase.
High Internal Oxygen Alarm
This is a high priority alarm. It occurs when there is a leak in the
internal air delivery system that allows oxygen to build up inside
the device. The alarm is generated when the internal oxygen
concentration reaches 5% above ambient levels.
Trilogy200 clinical manual
Page 54

Circuit Disconnect Alarm
This is a high priority alarm. It occurs when the breathing circuit
is disconnected or has a large leak. The device continues to
operate. The alarm will automatically terminate when the circuit is
reconnected or the leak is xed.
Apnea Alarm
This is a high priority alarm. It occurs when the patient has not
triggered a breath within the time specied in the apnea alarm
setting. The device continues to operate. The alarm will automatically
terminate when two consecutive patient breaths are detected that
meet the apnea alarm time setting.
High Vte Alarm
This is a high priority alarm. It occurs when the estimated exhaled
tidal volume is greater than the High Vte alarm setting for three
consecutive breaths. The device continues to operate. The alarm will
automatically terminate when a breath occurs in which the exhaled
tidal volume does not reach the High Vte alarm setting.
43
WARNING
You should not rely on any
single alarm to detect a circuit
disconnect condition. The Low
Tidal Volume, Low Minute
Ventilation, Low Respiratory
Rate, and Apnea alarms should
be used in conjunction with
the Circuit Disconnect alarm.
The Apnea alarm is only
intended for spontaneously
breathing patients.
Low Vte Alarm
This is a high priority alarm. It occurs when the estimated exhaled
tidal volume is lower than the Low Vte alarm setting for three
consecutive breaths. The device continues to operate. The alarm will
automatically terminate when a breath occurs in which the exhaled
tidal volume exceeds the Low Vte alarm setting.
When AVAPS is on, this alarm will occur when the calculated tidal
volume is less than 90% of the target tidal volume setting. The alarm
will automatically terminate when a breath occurs in which the
exhaled tidal volume is equal or greater to 90% of the target tidal
volume setting.
Chapter 3 Modes, Features, and Alarms
Page 55

44
High Vti Alarm
This is a high priority alarm. It occurs when the delivered tidal
volume is greater than the High Vti alarm setting for three
consecutive breaths. The device continues to operate. The alarm will
automatically terminate when a breath occurs in which the delivered
tidal volume does not reach the High Vti alarm setting.
Low Vti Alarm
This is a high priority alarm. It occurs when the delivered tidal volume
is less than the Low Vti alarm setting for three consecutive breaths.
The device continues to operate. The alarm will automatically
terminate when a breath occurs in which the delivered tidal volume
exceeds the Low Vti alarm setting.
High Respiratory Rate Alarm
This is a high priority alarm. It occurs when the respiratory rate is greater
than the High Respiratory Rate alarm setting. The device continues to
operate. The alarm will automatically terminate when the measured
respiratory rate is less than the High Respiratory Rate alarm setting.
Low Respiratory Rate Alarm
This is a high priority alarm. It occurs when the respiratory rate is less
than the Low Respiratory Rate alarm setting. The device continues to
operate. The alarm will automatically terminate when the measured
respiratory rate is greater than the Low Respiratory Rate alarm setting.
High Inspiratory Pressure Alarm
This alarm occurs in several stages and escalates from an audible beep for
the rst two occurrences to a high priority alarm if the problem continues.
It is detected dierently for volume and pressure therapy modes.
For volume modes, the alarm will sound if the measured patient
pressure exceeds the High Inspiratory Pressure setting specied by
the clinician. The alarm will automatically terminate when the peak
inspiratory pressure is less than or equal to the High Inspiratory
Pressure alarm setting.
Trilogy200 clinical manual
Page 56

For pressure modes, the alarm occurs when the delivered pressure
exceeds the target patient pressure by 5 cmH2O or more during
the inspiratory phase. The device will automatically cycle to
the expiratory phase and continue to operate. The alarm will
automatically terminate when the delivered pressure falls within 5
cmH2O of the target patient pressure during the inspiratory phase.
Low Inspiratory Pressure Alarm
This is a high priority alarm. It is detected dierently for volume and
pressure therapy modes.
For volume modes, the alarm will sound if the measured patient
pressure is less than the Low Inspiratory Pressure setting specied by
the clinician. The alarm will automatically terminate when the peak
pressure at the end of the breath is greater than or equal to the Low
Inspiratory Pressure alarm setting.
For pressure modes, the alarm occurs when the delivered pressure
is 5 cmH2O or more below the target patient pressure during the
inspiratory phase. The alarm will automatically terminate when
the delivered pressure comes within 5 cmH2O of the target patient
pressure during the expiratory phase.
45
High Minute Ventilation Alarm
This alarm is a high priority alarm. It occurs when the patient’s
minute ventilation is greater than the High Minute Ventilation alarm
setting. The device continues to operate. The alarm will automatically
terminate when the calculated minute ventilation is less than the
High Minute Ventilation alarm setting.
Low Minute Ventilation Alarm
This alarm is a high priority alarm. It when the patient’s minute
ventilation is less than the Low Minute Ventilation alarm setting. The
device continues to operate. The alarm will automatically terminate
when the calculated minute ventilation is greater than the Low
Minute Ventilation alarm setting.
Chapter 3 Modes, Features, and Alarms
Page 57

46
Low Battery Alarm
The Low Battery alarm occurs when the last battery available is
low or nearly depleted. This alarm occurs in two stages. When
approximately 20 minutes of battery run time remains, a medium
priority alarm is generated, and the device continues to operate. If
no action is taken and the battery continues to deplete, the alarm
escalates to a high priority alarm when approximately 10 minutes of
battery run time remains.
High Temperature Alarm
This alarm occurs when the estimated patient airstream temperature
or the ventilator internal temperature is too high. The alarm occurs in
several stages. The ventilator continues to operate. Internal fans are
started when the medium priority alarm is generated. If the condition
causing the high temperature is not corrected and the temperature
continues to rise, the alarm will escalate to the high priority alarm.
Replace Detachable Battery Alarm
The Replace Detachable Battery alarm occurs when the detachable
battery is nearing the end of its useful life or a failure in the
detachable battery that prevents it from charging or discharging has
been detected.
WARNING
Immediately seek an alternate
power source when the “Low
Battery” message appears.
Complete power failure and loss
of therapy is imminent.
WARNING
The ventilator has a two-stage
low battery alarm. The medium
priority alarm indicates that
approximately 20 minutes of
operation remain, and the high
priority alarm indicates that less
than 10 minutes of operation
remain. Actual run time may be
more or less than this and varies
with battery age, environmental
conditions, and therapy.
The alarm occurs in several stages, from low to high priority. The
device continues to operate when the alarm is the low priority
alarm. If the alarm is reset without removing the battery, the alarm
will be regenerated once every hour until the detachable battery is
removed. The device continues to operate, the detachable battery
is not used, and the power source is switched to the next available
power source if the alarm is the high priority alarm.
Ventilator Service Recommended Alarm
This is a medium priority alarm. It occurs when the device has
detected an error, but the error will not aect device performance
or safety. The device continues to operate. Therapy and safety are not
compromised.
Trilogy200 clinical manual
Page 58

If the problem is not corrected, the device will generate a reminder
message once per day, or whenever power is cycled, until the issue
is corrected. Additionally, if the device is powered o, a reminder
message will immediately appear when the device is turned on again.
AC Power Disconnected Alarm
This is a medium priority alarm. It occurs when the AC power source
was lost, and the device has switched to an alternate power source
(either a detachable or external battery, if connected, or the internal
battery if no other source is available). The device continues to
operate. If AC power returns, the ventilator will beep, but no message
will appear on the display.
Keypad Stuck Alarm
This is a low priority alarm. It occurs when a key becomes lodged
inside the case of the device.
Battery Discharging Stopped due to Temperature
47
Info Message
This info message occurs when the detachable or internal battery
becomes overheated while providing power for the device. The
device continues to operate. The battery is not used and the power
source is switched to the next available power source.
Battery Not Charging due to Temperature Info Message
This info message occurs when the detachable or internal battery
becomes too hot while charging or the device was in too cold an
environment before charging started. The device continues to
operate. Battery charging stops until the battery cools or warms
suciently.
Battery Not Charging Info Message
This info message occurs when the device has detected an error
condition with the battery that prevents it from accepting a charge.
The device continues to operate. Battery charging stops.
Chapter 3 Modes, Features, and Alarms
Page 59

48
Check External Battery Info Message
This info message occurs when a bad connection exists to the
external battery or the external battery failed. The device continues
to operate using power from the detachable battery, if available, or
the internal battery.
Battery Depleted Info Message
This info message occurs when the aected battery is fully depleted.
The device continues to operate using the next available power source.
External Battery Disconnected Info Message
This info message occurs when the external battery power source is
lost and the device has switched to an alternate power source (either
a detachable battery, if connected, or the internal battery if no other
source is available). If external battery power returns, the ventilator
will beep, but no message will appear on the display.
Detachable Battery Disconnected Info Message
This info message occurs when the detachable battery power source
is lost and the device has switched to an alternate power source (the
internal battery if no other source is available). If detachable battery
power returns, the ventilator will beep, but no message will appear
on the display.
Start On Battery Info Message
This info message indicates that the ventilator has started on battery
power and no AC power is available. The device operator should
verify that this is what is wanted.
Card Error Info Message
This info message occurs when an unusable SD card is inserted into
the ventilator. The device continues to operate but data cannot be
logged onto the SD card.
Trilogy200 clinical manual
Page 60

Trilogy200
clinical manual
4. Ventilator Setup
49
This chapter provides instructions on how to assemble the ventilator.
It includes the following setup information:
• Properly positioning the device
• Installing the air lter
• Supplying power to the device
• Connecting the breathing circuit
• Connecting a water trap (optional)
• Connecting a remote alarm (optional)
WARNING
Ventilator dependent patients
should be continuously
monitored by qualied
personnel. These personnel
should be prepared to provide
alternate therapy in the event of
ventilator failure or inoperative
equipment.
WARNING
Do not use the ventilator on a
patient until a system checkout
has been performed. See
Chapter 10 of this manual.
WARNING
For ventilator dependent
patients, always have alternate
ventilation equipment, such as
a back-up ventilator, manual
resuscitator, or similar device,
available.
CAUTION
Do not operate the ventilator at
temperatures below 5° C (41° F)
or above 40° C (104° F).
Chapter 4 Ventilator Setup
Page 61

50
Position the Device
Place the ventilator on a at, level surface. Or, as an alternative, you
can place the device in the optional in-use bag. The in-use bag is
required for portable use in order to properly secure the ventilator.
Do not operate the ventilator while on its side, upside-down, or in
any other orientation. Make sure that the air inlet on the back of the
device is not blocked. If you block the air ow around the device, the
ventilator may not work properly.
Install the Air Filter
The device uses a gray foam filter that is washable and reusable. The
reusable filter screens out normal household dust and pollens. The
filter must be in place at all times when the device is operating. Two
reusable gray foam filters are supplied with the device. If the filter is
not already installed when you receive the device, you must install
the filter before using the ventilator.
CAUTION
The reusable foam inlet lter is
required to protect the ventilator
from dirt and dust. Wash
periodically and replace when
damaged for proper operation.
To install the filter, insert the gray foam filter into the filter area as
shown.
Supply Power to the Device
The device can operate on AC or DC power. The ventilator accesses
power from potential sources in the following order:
• AC Power
• External Battery
• Detachable Battery Pack
• Internal Battery
Trilogy200 clinical manual
Installing the Filter
Note: See Chapter 7 for
information on how to clean
and replace the air lter.
Page 62

51
Using AC Power
An AC power cord is provided with the device.
1. Plug the socket end of the AC power cord into the AC power inlet
on the side of the device. To prevent accidental removal of the
AC power cord from the device, you may secure the AC power
cord to the device using the AC power cord retainer located on
the back of the device.
2. Plug the pronged end of the cord into a wall outlet not
connected to a wall switch.
3. Ensure that all connections are secure. If AC power is connected
correctly and the device is operating properly, the green AC
Power LED should be on.
Note: This device is activated
(i.e., ‘powered on’) when the AC
power cord is connected or any
of the three battery sources is
available. Pressing the Start/Stop
button turns the airflow on or o.
CAUTION
The device may only be operated
at temperatures between 5˚ C
and 40˚ C (41˚ F and 104˚ F).
WARNING
Periodically inspect the power
cord for damage or signs of
wear. Discontinue use and
replace if damaged.
Note: To remove AC power,
disconnect the power supply
cord from the electrical outlet.
Connecting the AC Power
Cord
Chapter 4 Ventilator Setup
Page 63

52
4. If desired, secure the power cord using the cord retainer on the
back of the device, as shown below. To secure the power cord,
use a screwdriver to remove the screw on the cord retainer.
Insert the cord as shown into the cord retainer, and then reattach the cord retainer to the device by re-attaching the screw.
Using DC Power
You can operate the ventilator using an external battery, detachable
battery, or the internal battery.
Securing the Power Cord
Using the Cord Retainer
External Battery
The ventilator can operate from a 12 VDC deep cycle marine-type
(lead acid) battery using the Philips Respironics Trilogy External
Battery Cable. This cable is pre-wired and properly terminated to
ensure safe connection of an external battery to the ventilator.
Battery operating time depends on the characteristics of the battery
and usage of the device.
Due to a variety of factors, including battery chemistry, battery age,
and use prole, the capacity of the external battery as shown on the
device display is only an estimate of the actual remaining capacity.
Refer to the instructions supplied with the Philips Respironics Trilogy
External Battery Cable for detailed information on how to operate
the device using an external battery.
Trilogy200 clinical manual
CAUTION
Do not use the same external
battery to operate both the
ventilator and any other equipment
such as power chairs.
CAUTION
An external battery should only
be connected to the ventilator
using the Philips Respironics
Trilogy External Battery Cable.
This cable is fused, pre-wired and
properly terminated to ensure
safe connection to a standard
deep cycle lead acid battery. Use
of any other adapter or cable
may cause improper operation
of the ventilator.
Page 64

Detachable Battery Pack
Philips Respironics oers a detachable Lithium-Ion battery pack. To
use the detachable battery pack, snap the battery into place on the
back of the ventilator, as shown in the following illustration. When
the device is not connected to an AC power source or an external
battery, the detachable battery will power the device, if attached.
The length of time the ventilator will operate on battery power
depends on many factors such as device settings, battery charge
level, and condition or age of the battery. When fully charged, a new
battery can power the ventilator for approximately three hours under
typical patient conditions.
Whenever the ventilator is connected to AC power, it will
automatically recharge the detachable battery pack. A completely
discharged detachable battery will reach 80% charge status within 8
hours, when charging at approximately 23˚ C ambient temperature.
Insert and securely latch the detachable battery into the device as
shown below.
CAUTION
The detachable and internal
batteries wear out based on
the amount of use (hours or full
charge-discharge cycles). The
battery capacity and life are also
reduced by operation at higher
temperatures.
CAUTION
Only use the Philips Respironics
Trilogy Detachable Battery with
the device.
53
Insert
Detachable
Battery
Properly Installed
Detachable
Battery
Attaching the Detachable
Battery
CAUTION
Prolonged operation or storage
at elevated temperatures may
reduce the service life of the
detachable or internal battery
and other internal components
of the ventilator.
Chapter 4 Ventilator Setup
Page 65

54
One side of the detachable battery has a set of LEDs that indicate the
amount of charge left on the battery. You can press the button below
the LEDs to view how much charge remains:
LED Battery Capacity
All 5 LEDs are lit 80-100% capacity
4 LEDs are lit 60-79% capacity
3 LEDs are lit 40-59% capacity
2 LEDs are lit 20-39% capacity
1 LED is lit 10-19% capacity
1 LED ashes 1 to 9% capacity
0 LEDs are lit 0% capacity
Internal Battery
The device contains an internal battery that can be used as a backup power source. It is intended for use during short periods while
switching between external power sources, emergency situations, or
short durations when the user needs to be mobile. The length of time
the ventilator will operate on internal power depends on many factors
such as device settings, battery charge level, and condition or age of the
battery. When fully charged, a new battery can power the ventilator for
approximately three hours under typical patient conditions.
Whenever the ventilator is connected to AC power, it will
automatically recharge the internal battery. A completely discharged
internal battery will reach 80% charge status within 8 hours when
charging at approximately 23˚ C ambient temperature.
Device Power Source Indicators
There are many power source indicators on the device and the
display screen. These indicators are described in detail below.
AC Power Indicator
Detachable Battery LEDs
WARNING
The internal battery is NOT
intended to serve as a primary
power source. It should only be
used when other sources are
not available, or briey when
necessary; for example when
changing power sources.
When AC power is applied to the device, the green AC LED indicator
(~) on the front of the device lights.
Trilogy200 clinical manual
Page 66

55
DC Power Indicators
The internal, detachable, and external battery symbols that will
display on the Monitoring screen are shown below. The detachable
and external battery symbols will only appear on-screen if a
detachable or external battery is attached to the device.
Battery Symbol
Internal Battery
Note: Under normal operating
conditions, the internal battery
symbol will always display on
the Monitoring screen. If the
symbol appears as an empty
red battery on your screen,
contact Philips Respironics
or an authorized service
representative to have your
device serviced.
Detachable Battery
External Battery
There are several DC power indicators that will display on the
Monitoring screen to indicate which battery is in use (if applicable), if
the batteries are low, charging, or discharged, etc. The following table
explains all of the DC power indicators.
DC Power Indicator Description
Battery In Use Indicator A black box will appear around the battery that is in use. For instance, if
the external battery is currently in use, the symbol appears on the
Monitoring screen.
Green Fully Charged
Battery Indicator
Partially Charged
Battery Indicator
When a battery is charged to greater than 90% of its capacity, all of the
bars in the battery symbol will appear in green.
When a battery is partially charged, some of the bars in the battery
symbol will appear in green, while others will be clear. For instance, if
the external battery is 50% charged, the following symbol displays onscreen:
Yellow Low Battery
Indicator (Medium
Priority)
When the device detects that an in-use battery’s charge is low (has
approximately 20 minutes of charge left), the inside of the box
surrounding the battery symbol turns yellow. (In addition to the
battery indicator on the Monitoring screen, a medium priority alarm
message will display indicating “Low Battery.” See Chapter 6 for more
information. The yellow indicator is for the last available battery source.
Chapter 4 Ventilator Setup
Page 67

56
DC Power Indicator Description
Red Low Battery
Indicator
Yellow Battery
Recharging Symbol ( )
When the device detects that an in-use battery’s charge is nearly
depleted (has approximately 10 minutes of charge left), the inside
of the box surrounding the battery symbol turns red. In addition to
the battery indicator on the Monitoring screen, a high priority alarm
message will display indicating “Low Battery.” See Chapter 6 for more
information. The red indicator is for the last available battery source.
Whenever AC power is applied to the device, the internal and
detachable batteries will recharge as needed. If the internal battery is
being recharged, the symbol displays. If the detachable battery is
being recharged, the symbol displays.
Battery Disposal
Dispose of the batteries in accordance with local regulations.
First Time Use
When setting up the device for the rst time or after annual service,
apply AC power to the ventilator before turning on the blower.
Attempting to use the ventilator without rst applying AC power,
such as installing a detachable battery pack and starting the blower,
will cause the internal battery to be displayed in red as an empty
battery. When in this state, the internal battery will not be usable
until AC power is applied.
Trilogy200 clinical manual
Page 68

57
Connect the Breathing Circuit to the Ventilator
Complete the following steps to set up your patient circuit.
1. If you are using a bacteria lter, connect one end of the exible
tubing to the outlet of the bacteria lter, and connect the
bacteria lter inlet to the breathing circuit connection located on
the side of the ventilator.
If you are not using a bacteria lter, connect the tubing directly
to the device’s breathing circuit connection.
Trilogy Breathing Circuit
Connection
Flexible Tubing
Bacteria Filter
2. Connect the other end of the exible tubing to a separate
exhalation device.
a. If your circuit type is Passive and you are using a Philips
Respironics Passive Exhalation Device:
1. Connect the exible tubing to the rotating end of the
Passive Exhalation Device.
WARNING
Philips Respironics recommends
that a main line outlet bacteria
lter (Part Number 342077) be
used whenever the device is
used for invasive therapy or if
the ventilator may be used on
multiple patients.
Connecting the Breathing
Circuit to the Device
Note: The device can be used
with reusable or disposable
circuits. For detailed instructions
on how to set up your device
using a disposable circuit, refer
to the instructions included with
the disposable circuit.
2. Connect the other end of the Passive Exhalation Device to
the patient interface (e.g., the mask).
Flexible
Tubing
Whisper
Swivel II
Bacteria Filter
Passive
Exhalation
Device
Flexible
Tubing
Bacteria Filter
Refer to the instructions included with the Passive
Exhalation Device for more detailed setup information.
Connecting the Passive
Exhalation Device
Note: The device does not
provide circuit compliance
compensation in volume modes.
Chapter 4 Ventilator Setup
Page 69

58
b. If your circuit type is Active PAP:
Active Exhalation Device
with Proximal Pressure
1. Connect the exible tubing to an active exhalation device
with proximal pressure.
A. Connect the active exhalation device with proximal
pressure to the exible tubing that attaches to the
ventilator and to the patient interface (e.g., the
tracheostomy tube).
2. Connect the proximal pressure line and the exhalation
valve line to the active exhalation device with proximal
pressure and the Universal Porting Block on the device as
described below.
A. Attach the proximal pressure line (.476 cm or 3/16”
line) to the proximal pressure port as shown in the
next illustration.
B. If not attached, connect the other end of the proximal
pressure line to the Trilogy Universal Active PAP Tube
Adapter as shown in the next illustration.
C. Connect the Trilogy Universal Active PAP Tube Adapter
to the top, striped port on the Universal Porting Block
on the ventilator.
D. Connect the exhalation valve line (.317 cm or 1/8” line)
to the exhalation valve port on the top of the active
exhalation device with proximal pressure.
E. Connect the other end of the exhalation valve line
to the exhalation valve port on the Universal Porting
Block.
Note: Passive circuit ventilation
provides leak compensation
in both volume and pressure
modes. Active PAP circuit
ventilation does not provide
leak compensation. Particular
care should be used at low tidal
volumes to ensure adequate
monitoring of exhaled tidal
volume.
WARNING
For ventilator dependent
patients, always have alternate
ventilation equipment, such as
a back-up ventilator, manual
resuscitator, or similar device,
available.
Note: Make sure that
components marked with an
arrow are oriented properly.
When attaching an active
exhalation device with proximal
pressure to the patient, make
sure the proximal pressure port
faces away from the patient.
Note: The symbol
appears next to the Exhalation
Valve port on the Universal
Porting Block to indicate where
the active exhalation valve line
connects.
Trilogy200 clinical manual
Page 70

59
Universal Porting Block
Exhalation Valve Port
Proximal
Pressure
Port
Exhalation Valve Line
Proximal
Pressure
Line
Trilogy Universal Active
PAP Tube Adapter
Exhalation Valve Port
on Universal Porting
Block
Refer to the instructions included with the Active Exhalation
Device for more information.
c. If your circuit type is Active Flow:
1. Connect the Flow Sensor to an active exhalation device as
shown below.
Flow Sensor
2. Connect the other end of the exible tubing to the active
exhalation device.
A. Connect the active exhalation device to the exible
tubing that attaches to the ventilator.
B. Connect the ow sensor to the patient interface (e.g.,
the tracheostomy tube).
Connecting an Active Device
with Proximal Pressure
Connecting the Flow Sensor
Note: If the active exhalation
device has the proximal pressure
line connected when you are
setting up an active ow circuit
type, remove the proximal
pressure line and cap the
proximal pressure port before
attaching to the exible tubing.
Note: Make sure that
components marked with an
arrow are oriented properly.
Chapter 4 Ventilator Setup
Page 71

60
C. Connect the ow lines and the exhalation valve line to
the Universal Porting Block on the ventilator as shown
below.
• Connect the White Striped Flow Line to
the top, striped port on the Universal
Porting Block on the device.
• Connect the other Flow Line to the
middle port on the Universal porting
Block.
• Connect the Exhalation Valve Line to the
Exhalation Valve port on the top of the
active exhalation device, and connect the
other end of the line to the Exhalation
Valve port on the Universal Porting Block.
White Striped
Flow Line
Exhalation Valve Port
Universal Porting Block
on Trilogy Device
Note: When using an active
exhalation device with proximal
ow, ensure that any additional
proximal ports are capped.
Note: The symbol
appears next to the Exhalation
Valve port on the Universal
Porting Block to indicate where
the active exhalation valve line
connects.
Flow Line
Exhalation Valve Line
Exhalation Valve Port
on Porting Block
Refer to the instructions included with the active exhalation
device for more information.
Connect a Water Trap
If you are using an optional water trap, connect it to the patient
circuit according to the manufacturer’s instructions.
Trilogy200 clinical manual
Connecting the Active
Exhalation Device with
Proximal Flow Sensor
Page 72

Connect Supplemental Oxygen (Optional)
t
To attach supplemental oxygen to the device:
1. Connect the oxygen tubing to the Oxygen Inlet Quick Connect.
Then, connect the Quick Connect to the Oxygen Inlet on the
back of the ventilator.
Oxygen Inlet
Oxygen Inlet
Quick Connec
61
Oxygen Source
Tubing
2. Make sure you press the Oxygen Inlet Quick Connect rmly into
the inlet. You should hear a click, and the latch at the top of the
inlet will pop up.
This device is only compatible with a low ow oxygen source
providing up to 15 l/min.
Attaching the O2 Tubing
Press Tubing in and Latch
Pops Up
CAUTION
Do not connect an unregulated
or high pressure oxygen source
to this connector on the device.
Chapter 4 Ventilator Setup
Page 73

62
Connect the Remote Alarm (Optional)
You can use a remote alarm as a nurse call system or in-house remote
alarm system. It can generate an alarm at a distance of up to
91 meters (300 feet) from the ventilator. An audible tone sounds
and a red light blinks to indicate that an alarm condition exists. The
remote alarm will sound when any of the following conditions exist:
• The ventilator is o.
• Any alarm occurs and is not silenced or reset.
Refer to the Accessories chapter of this manual for information on
which remote alarm systems are compatible with the device. Refer to
the instructions included with the Remote Alarm Adapter Cable for
information on how to connect a remote alarm to the ventilator.
WARNING
When using a remote alarm,
make sure you fully test the
remote alarm connector and
cable by verifying that:
- Annunciated alarms on
the ventilator are also
annunciated on the remote
alarm.
- Disconnecting the remote
alarm cable from the
ventilator or from the remote
alarm results in an alarm
notication at the remote
alarm.
WARNING
The remote alarm should be
tested daily.
Trilogy200 clinical manual
Page 74

Trilogy200
clinical manual
5. Viewing and Changing Settings
63
This chapter explains how to scroll through the ventilation screens
and change ventilation settings. It also describes how to connect the
ventilator to the patient once the settings are complete.
Keypad Lock Feature
There is a Keypad Lock feature that users can enable from the
Options menu. It is intended to prevent accidental changes to device
settings. This feature will lock the navigation keys (Up, Down, Stop,
Left, and Right keys). If the Keypad Lock is enabled, a Keypad Unlock
message will display on the bottom of the screen any time you press
one of the navigation keys.
If the keypad is locked, you must unlock it before you can enter the
Menu. To unlock the keypad and enter the menu, you must rst hold
the Right button for 5 seconds to unlock the keypad. An audible
indicator sounds when the keypad is successfully unlocked. Once the
display is unlocked, you can enter the Menu as you normally would
by pressing the Up button.
Note: There is a keypad lock
inactivity time-out period. After
you have unlocked the keypad
as indicated, the keypad will
re-lock after ve minutes of
inactivity to prevent someone
from accidentally pressing a
button and changing any of the
settings.
Note: When Keypad Lock is
enabled, the Left, Right, and Up/
Down buttons are locked while
the ventilator is turned on. The
Alarm Indicator/Audio Pause
continues to function normally.
The Start/Stop button is locked
only when this button is used to
stop therapy.
Note: The keypad will
automatically unlock if an
alarm or informational message
occurs and will remain unlocked
the entire time alarms are active.
Note: Pressing the Left (Cancel)
button will cancel the Keypad
Unlock action.
Chapter 5 Viewing and Changing Settings
Page 75

64
Accessing the Startup and Monitor Screens
1. After you press the button to begin therapy, the Startup
screen appears momentarily, indicating the device name and the
software version.
2. The next screen that appears is the Monitor screen.
The appearance of this screen will vary, depending on how you
set up the device. If Detailed View is turned o in the Options
menu, your screen will look like the screen shown below.
Monitor Panel
Date and Time
Panel
Status Panel
– The top section of the screen, called the Monitor panel,
shows the therapy mode and, if you set up a dual
prescription for the patient, the Prescription indicator
appears, indicating Primary or Secondary prescription. The
patient breath symbol also displays during a patient-triggered
breath, and a bar graph displays the current pressure level.
Note: The symbols that appear
on the Monitor screen are
described in detail later in this
chapter.
Monitor Screen – Detailed
View O
Note: No Soft Buttons display
on the Monitor screen if Keypad
Lock is enabled.
– The center section of the screen displays the current date
and time.
– The bottom section, called the Status panel, displays certain
symbols that indicate features being used, such as Ramp, as
well as battery status.
Trilogy200 clinical manual
Page 76

If Detailed View is turned on in the Options menu, the Monitor
Measured Settings
screen will look like the screen shown below.
Monitor Panel
65
Panel
Status Panel
This screen contains more detailed information about the
therapy.
– The top Monitor panel contains the Prescription indicator
if a dual prescription exists, the therapy mode, a graph
displaying the current pressure, and the current date and
time. Additionally, this panel also displays patient pressure,
respiratory rate (RR), exhaled tidal volume (Vte), and leak.
– The second panel in Detailed view is the Measured
Settings panel. It provides patient-related data including
Peak Inspiratory Pressure (PIP), Minute Ventilation, Peak
Inspiratory Flow, Mean Airway Pressure (MAP), and I:E Ratio.
– The third panel is the Status panel and shows the same
information displayed in the Detailed View O screen,
including features in use such as Ramp and battery status.
Monitor Screen – Detailed
View On
Chapter 5 Viewing and Changing Settings
Page 77

66
Monitor Screen Indicators
This section describes the following indicators:
• Monitor Panel Indicators
• Measured Settings Panel Indicators
• Status Panel Indicators
Monitor Panel Indicators
Note: Dashes on the display
screen indicate that the device
was unable to compute the
parameters. For example, when
the device is rst connected to a
patient, the tidal volume, minute
ventilation, and leak may be
dashed until the device is able
to accurately calculate these
patient parameters.
All of the indicators that may appear on the Monitor Panel are
described in detail in the following table.
Indicator Description
Prescription If you set up a dual prescription for the patient, the words
“Primary” or “Secondary” appear in the top left corner of the panel
to indicate which prescription is active.
Therapy Mode The current therapy mode displays at the top of the panel (for
example, CPAP, S, S/T, etc.). If a special feature such as Flex, AVAPS,
or Sigh is active, this feature will appear next to the therapy
mode.
Date and Time If you are in Detailed view, the current date and time appear
in the top right corner of the panel. (In Detailed View O, they
appear in the center panel.)
Patient Breath This symbol displays during a patient-triggered breath.
Airway Pressure
Manometer and
Peak Pressure
Symbol
The manometer (bar graph) displays the airway pressure in the
patient circuit at all times. The manometer bar moves to the
right as pressure increases during inhalation, and moves to the
left as pressure decreases during exhalation. The peak pressure
is also indicated on this bar. It is positioned according to the
maximum patient pressure reached during each breath. The Peak
Pressure symbol appears as a blue bar on the manometer. If a
High Inspiratory Pressure alarm occurs, the Peak Pressure symbol
changes from blue to red.
Trilogy200 clinical manual
Page 78

Indicator Description
67
Low Pressure
Indicator
L
If you enable a volume therapy mode, this indicator appears
below the manometer bar, indicating the low pressure alarm
setting.
High Pressure
Indicator
H
If you enable a volume therapy mode, this indicator appears
below the manometer bar, indicating the high pressure alarm
setting.
Pressure This indicator displays the current patient pressure. This only
appears in detailed view.
Respiratory Rate (RR) This indicator displays the measured respiratory rate in Breaths
Per Minute (BPM). This only appears in detailed view.
Exhaled Tidal
Volume (Vte)
This indicator displays the estimated exhaled tidal volume in
milliliters and reects compensation for BTPS. This only appears in
detailed view when Passive Circuit is selected.
Inhaled Tidal
Volume (Vti)
This indicator displays delivered tidal volume in milliliters and
reects compensation for BTPS. This only appears in detailed view
when the Active with PAP Circuit is selected.
Leak This indicator displays the total leak (non-returned ow), between
the unit outlet and the patient, averaged over the previous
breath. This only appears in detailed view when the Passive
Circuit is selected.
Chapter 5 Viewing and Changing Settings
Page 79

68
Measured Settings Panel
All of the indicators that may appear on the Measured Settings panel
(available only in Detailed view), are described in the following table.
Indicator Description
PIP Peak Inspiratory Pressure displays the maximum pressure
delivered to the patient during the previous breath.
I:E Ratio Displays a comparison of the time spent in inspiration to the time
spent in expiration during the previous breath.
Peak Flow Displays the maximum inspiratory ow delivered to the patient
during the previous breath in l/min BTPS.
MAP Displays the Mean Airway Pressure, which is the weighted
average of pressure in the patient’s airway over 6 breaths.
MinVent Minute ventilation displays the amount of air delivered to the
patient over the last minute in l/min BTPS.
Trilogy200 clinical manual
Page 80

Status Panel Indicators
All of the indicators that may appear on the Status Panel are
described in the following table.
Indicator Description
Indicates that the device is in Full Menu Access mode, which
means you can adjust all prescription settings. Philips Respironics
recommends that you change the device to Limited Menu Access
mode before giving the device to the patient, so patients cannot
adjust their prescription settings. Only trained health care
professionals and clinicians should adjust prescription settings.
Displays when a Secure Digital (SD) memory card is inserted in
the ventilator.
Displays when the ventilator detects an error with the SD card.
Displays at all times when an external battery is attached to
the ventilator. The level of green shading shown in the symbol
indicates the battery capacity and will go down as the battery
charge level decreases. When the entire symbol is green, the
battery is fully charged.
69
Displays at all times when a detachable battery is attached to
the ventilator. The level of green shading shown in the symbol
indicates the battery capacity and will go down as the battery
charge level decreases. When the entire symbol is green, the
battery is fully charged.
Displays at all times, indicating the status of the internal battery. The
level of green shading shown in the symbol indicates the battery
capacity and will go down as the battery charge level decreases.
When the entire symbol is green, the battery is fully charged.
Chapter 5 Viewing and Changing Settings
Page 81

70
Indicator Description
A black box displays around the battery that is currently
supplying power to the ventilator when AC power is not available.
(In the status panel shown above, the external battery is in use, so
the symbol displays.)
A yellow lightning bolt symbol displays with the Detachable or
Internal battery symbol to indicate when the battery is charging.
(In the status panel shown on the previous page, the detachable
battery is being charged, so the symbol displays.)
Displays when the Alarm Indicator/Audio Pause button has been
pressed and Audio Pause is active. The alarm is silenced for one
minute when the Alarm Indicator/Audio Pause button is pressed.
Displays when the Ramp feature is active.
Note: If a battery in use is very low (less than 20 minutes remaining), the inside of the box surrounding the
battery symbol will change to yellow and all of the bar indicators in the battery will be empty. If a battery in use
is near depletion (less than 10 minutes remaining), the inside of the box surrounding the battery symbol will
change to red, and all of the bar indicators in the battery will be empty. These color changes only occur for the
last available battery source.
Trilogy200 clinical manual
Page 82

On-Screen Button Panel
The illustration below shows the on-screen button panel on the Main
Menu screen, in relation to the buttons on the front of the device.
On-Screen
Button
Panel
At the very bottom of the display screen is the on-screen button
panel. This panel corresponds with the control buttons on the
ventilator:
• The left on-screen button species the action for the Left
button on the device.
• The center on-screen button species the action for the
Up/Down buttons on the device.
• The right on-screen button species the action for the
right button on the device.
71
Example On-Screen Button
Panel
Note: The on-screen buttons
will vary depending on which
screen is displayed and what
settings are enabled on your
device.
Navigating the Menu Screens
To navigate through all of the menu screens and settings:
• Use the Up/Down button to scroll through the menu
options and settings.
• Use the Left and Right buttons to perform the actions
specied on the screens’ left and right on-screen buttons.
Chapter 5 Viewing and Changing Settings
Page 83

72
Changing and Viewing Settings in Full Menu
Access Mode
Clinicians can view and change settings using the Menu screens
when the device is in Full Menu Access mode. To enter the Menu
screens from the Monitor screen, press the Up button on the
ventilator. The Main Menu screen shown below appears.
Choose from the following selections on the Main Menu screen:
• Safely Remove SD Card - This option will appear if an SD
card is inserted in the ventilator. Select this option when
you want to remove the SD card. When the “Remove SD
Card” conrmation message appears, remove the card.
If you press the left (cancel) button or don’t remove the
card within 30 seconds, the conrmation message will
close and the ventilator will continue writing to the card.
• Settings and Alarms: View and change prescription
settings and alarms.
• Options: View and change device settings, such as Full or
Limited Access mode, Detailed View, Language, etc.
• Alarm Log: View a list of the 20 most recent alarms that
have occurred.
• Event Log: View a list of all events that have occurred,
such as ventilator setting changes, ventilator inoperative
conditions, alarms, etc.
• Information: View detailed information about the device,
such as the device’s software version and serial number.
Note: For some therapy
settings, once you reach the
highest or lowest setting
available, pressing the Up/
Down button again will cycle
back through the settings.
For the parameters that do
not wrap, when you reach
the highest or lowest setting
possible, a “Limit Reached”
message appears in the Menu
Banner on-screen.
Main Menu Screen Example
Note: In the example Main
Menu screen shown, the 2/6
that appears in the Menu
banner indicates that item 2 is
highlighted from a total of 6
items in the menu.
Note: If you change a setting
but decide you do not want to
save it, you can press the Left
button to cancel the change.
Trilogy200 clinical manual
Page 84

73
Changing the Device Settings and Alarms
From the Main Menu screen, use the Up/Down button to highlight
the Settings and Alarms menu, and press the Right button to select
the menu.
Device Settings Common to All Therapy Modes
Some of the settings on this menu will vary depending on the
therapy mode you select. The section below describes all of the
settings that are common to all therapy modes.
Dual Prescription Setting
You can turn the dual prescription setting on or o. Enable the
setting if you want to create two separate prescriptions for the
patient. For instance, you may want to set up a daytime prescription
and then a separate nighttime prescription. If you enable this setting,
then the menu options on the Main Menu will change to include
three new options:
• Switch to Primary/Secondary Settings
• Primary Settings and Alarms
• Secondary Settings and Alarms
Note: In the Options menu
described later in this chapter,
you can specify the Pressure
Units displayed by the device,
choosing either cm H2O, hPa, or
mBar. The default setting is
cm H2O, so this manual uses cm
H2O throughout.
The Main Menu screen will look like the screen below.
Main Menu Screen with Dual
Prescription Enabled
Chapter 5 Viewing and Changing Settings
Page 85

74
Mode Setting
You can change the Mode setting on the Settings and Alarms screen
to one of the following therapy modes:
• CPAP
• S
• S/T
• T
• PC
• PC-SIMV
• CV
• AC
• SIMV
Circuit Type
There are three circuit types you can select:
• Passive
• Active PAP
• Active Flow
The Passive circuit type uses the Whisper Swivel II passive exhalation
device. The Active PAP circuit type uses an active exhalation device
with a proximal air pressure sensing connection. The Active Flow circuit
type uses an active exhalation device with a proximal ow sensor.
When using the Passive circuit, the ventilator displays estimated
patient pressures based on the resistance of the standard patient
circuit (Whisper Swivel II with 1.8 meter tubing). Adding accessories
to the patient circuit (humidier, water trap, etc.) may cause an
increase in circuit resistance and cause the device to display slightly
higher pressures than what is actually delivered to the patient.
Note: See Chapter 3 for detailed
information about each therapy
mode.
Note: Refer to the chart in
Chapter 3 to easily review all of
the settings available in each
therapy mode.
Note: This chapter describes
how to enable all of the device
settings, including device
alarms. For detailed information
about each alarm, please refer
to Chapter 6.
Note: To change the circuit
type, you must be in the
Setup screen with the airow
turned o. See the Full Menu
Access Mode section for more
information.
Note: When the Circuit Type
setting is set to Passive Circuit,
all Ramp Start Pressure settings
in all modes will maintain the
minimum range.
Note: When the Circuit Type
setting is set to Active PAP or
Active Flow, the Flex and AVAPS
features are unavailable.
With the Active PAP or Active Flow circuit type selected, patient
pressure is measured directly and is not aected by any change in
circuit resistance.
Trilogy200 clinical manual
Page 86

The Passive circuit provides leak compensation. When using the Passive
circuit in Volume Ventilation, the set Vti is delivered to the patient
above the calculated circuit and cu (or mask) leak. This is dierent
from traditional active circuit ventilation where the cu (or mask) leak
reduces the tidal volume delivered to the patient. Volume ventilation
with the Passive circuit delivers an inspiratory tidal volume close to
the device setting regardless of leak; this should be considered when
transitioning a patient from an active to a passive circuit. With a Passive
circuit, Vte is estimated based on the calculated sum of circuit and cu
(or mask) leak.
The Active Flow circuit monitors proximal ow and proximal
pressure. When using the Active Flow circuit conguration, ow
trigger with leak compensation may be enabled. The default setting
when using the Active Flow Circuit is Leak Compensation On. The
clinician has the option to turn o leak compensation; however,
unintentional leak will not be compensated. Both options measure
the ow at the proximal ow sensor. Leak compensation is not
available in the Active with PAP circuit conguration.
Circuit Disconnect
This setting enables or disables the circuit disconnect alarm. If
enabled, an audible alarm will sound when a large, continuous air
leak (such as mask removal) has been detected in the circuit.
You can choose O to disable the alarm. Or, you can increase or
decrease the setting from 5 to 60 seconds in 5 second increments.
For example, a setting of 10 means that the alarm will sound after the
circuit has been disconnected for 10 seconds.
75
WARNING
You should not rely on any
single alarm to detect a circuit
disconnect condition. The Low
Tidal Volume, Low Minute
Ventilation, Low Respiratory
Rate, and Apnea alarms should
be used in conjunction with the
Circuit Disconnect alarm.
Apnea
This setting enables or disables the apnea alarm. If enabled, an
audible alarm will sound when an apnea is detected.
You can choose O to disable the alarm. Or, you can increase or
decrease the setting from 10 to 60 seconds in 5 second increments.
For example, a setting of 10 means that the alarm will sound if the
time between spontaneous breaths exceeds 10 seconds.
Chapter 5 Viewing and Changing Settings
Page 87

76
Low Vte
This setting enables or disables the Low Vte alarm. The alarm
activates when the estimated exhaled tidal volume is less than or
equal to this setting. You can choose O to disable this alarm, or you
can increase or decrease the setting from 40 ml to 2000 ml in 5 ml
increments. It cannot be set higher than the High Vte setting.
When AVAPS is On, the alarm activates when the calculated tidal
volume is less than 90% of the target tidal volume setting. This alarm
can be set to on or o.
High Vte
This setting enables or disables the High Vte alarm. The alarm
activates when the estimated exhaled tidal volume is greater than or
equal to this setting. You can choose O to disable this alarm, or you
can increase or decrease the setting from 50 ml to 2000 ml in 5 ml
increments. It cannot be set lower than the Low Tidal Volume setting,
except to be turned o.
Low Vti
This setting enables or disables the Low Vti alarm. The alarm activates
when the measured inhaled tidal volume is less than or equal to this
setting. You can choose O to disable this alarm, or you can increase
or decrease the setting from 40 ml to 2000 ml in 5 ml increments. It
cannot be set higher than the High Vti setting.
Note: The High and Low Vte
alarms are available when the
Passive or Active Flow Circuit is
selected.
Note: The High and Low Vti
alarms are only available when
the Active PAP Circuit is selected.
High Vti
This setting enables or disables the High Vti alarm. The alarm
activates when the measured inhaled tidal volume is greater than or
equal to this setting. You can choose O to disable this alarm, or you
can increase or decrease the setting from 40 ml to 2000 ml in 5 ml
increments. It cannot be set lower than the Low Vti setting, except to
be turned o.
Trilogy200 clinical manual
Page 88

Low Minute Ventilation
This setting enables or disables the Low Minute Ventilation alarm. The
alarm activates when the calculated minute ventilation is less than or
equal to this setting. You can choose O to disable this alarm, or you
can increase or decrease the setting from 0.1 l/min to 99 l/min.
High Minute Ventilation
This setting enables or disables the High Minute Ventilation alarm.
The alarm activates when the calculated minute ventilation reaches
or exceeds this setting. You can choose O to disable this alarm, or
you can increase or decrease the setting from 1 l/min to 99 l/min
in 1 l/min increments. It cannot be set lower than the Low Minute
Ventilation setting except to be turned o.
Low Respiratory Rate
This setting enables or disables the Low Respiratory Rate alarm. The
alarm activates when the measured respiratory rate is less than or
equal to this setting. You can choose O to disable this alarm, or you
can increase or decrease the setting from 4 BPM to 80 BPM in 1 BPM
increments. It cannot be set higher than the High Respiratory Rate.
77
Note: You can increase or
decrease the Low Minute
Ventilation setting in
0.1 l/min increments from
0.1 to 0.99 l/min and 1 l/min
increments from 1 to 99 l/min.
High Respiratory Rate
This setting enables or disables the High Respiratory Rate alarm.
The alarm activates when the measured respiratory rate reaches or
exceeds this setting. You can choose O to disable this alarm, or you
can increase or decrease the setting from 4 BPM to 80 BPM in 1 BPM
increments. It cannot be set lower than the Low Respiratory Rate
except to be turned o.
Chapter 5 Viewing and Changing Settings
Page 89

78
Low Inspiratory Pressure
This setting congures the Low Inspiratory Pressure alarm. It is only
user-settable in CV, AC, and SIMV modes. It cannot be set lower than
PEEP + 2 cm H2O or higher than the High Inspiratory Pressure. For
passive circuits, you can increase or decrease the Low Inspiratory
Pressure from 6 to 40 cm H2O in increments of 1 cm H2O. For active
circuits, you can increase or decrease the setting from 2 to 40 cm H2O
in increments of 1 cm H2O. For pressure modes, this alarm is not usersettable.
High Inspiratory Pressure
This setting enables or disables the High Inspiratory Pressure alarm. It
is only user-settable in CV, AC, and SIMV modes. The High Inspiratory
Pressure cannot be set lower than the Low Inspiratory Pressure. You
can increase or decrease the High Inspiratory Pressure from 10 to 80
cm H2O in increments of 1 cm H2O. For pressure modes, this alarm is
not user-settable.
Additional Settings Specic to Therapy Modes
The Settings and Alarms menu also contains many additional
settings specic to the various therapy modes. The specic settings
for each therapy mode are described below.
Continuous Positive Airway Pressure (CPAP) Mode
In addition to the general settings described in the previous section
of this manual, you can also set the following settings in CPAP mode.
1. CPAP
You can increase or decrease the CPAP pressure setting from 4 to
20 cm H2O in increments of 1.
2. Trigger Type
The device can be set to trigger breaths based on automatic ow
thresholds or specic ow settings. You can select Auto-Trak or
Flow Trigger as the Trigger Type. When Auto-Trak is selected, the
Auto-Trak trigger initiates based on automatic ow thresholds.
Trilogy200 clinical manual
Note: If the CPAP pressure is
set to 4 (the minimum setting),
the Ramp Length setting will be
unavailable.
Note: Trigger Type is not
available when an Active PAP
or Active Flow circuit is selected.
Flow trigger is the triggering
method used for Active PAP and
Active Flow circuits.
Page 90

79
When Trigger Type is set to Flow Trigger, Flow Trigger Sensitivity
Leak Compensation, and Flow Cycle Sensitivity become active,
and the trigger initiates based on the Flow Trigger Sensitivity
setting.
3. Flow Trigger Sensitivity
If you set the Trigger Type to Flow Trigger, the Flow Trigger
Sensitivity setting displays. You can increase or decrease the
setting from 1 to 9 l/min in 1 l/min increments.
The ow trigger initiates when the patient’s inspiratory eort
creates a ow equal to or greater than the ow sensitivity
setting.
4. Leak Compensation
If you are using an Active Flow circuit, you can turn Leak
Compensation On or O.
5. Flow Cycle Sensitivity
If you set the Trigger Type to Flow Trigger, the Flow Cycle
Sensitivity setting displays. You can increase or decrease the
setting from 10 to 90 percent (%) in 1% increments.
Note: Auto-Trak is only
available if the Passive Circuit is
selected.
Note: Flow Trigger with leak
compensation is only available if
the Active Flow circuit is selected.
Note: Enabling Leak
Compensation when using the
Active Flow Circuit conguration
only aects triggering and does
not aect tidal volume delivery
or Vte measurement.
Note: A ow cycle sensitivity
set at 90% will result in the
most sensitivity. If the ow cycle
sensitivity is set at 10%, this will
result in the least sensitivity.
As ow begins to decrease during inspiration,
if the patient ow is less than the ow cycle set
point, the device will cycle to expiration. For
example: if the ow cycle is set to 75%, when the
ow has decreased by 25% of the peak ow, the
device will cycle to the EPAP/PEEP level.
6. Ramp Length
The Ramp Length allows you to set the ramp time.
You can disable Ramp by selecting O, or you
can increase or decrease the Ramp Length setting from 5 to 45
minutes in 5-minute increments.
Flow Cycle Sensitivity
Chapter 5 Viewing and Changing Settings
Page 91

80
7. Ramp Start Pressure
You can increase or decrease the ramp start pressure in
increments of 1 from 4 cm H2O to the CPAP pressure setting. The
patient also has access to this setting, unless the ramp length is
set to O.
8. Flex
You can enable or disable the Flex setting. O disables the
setting and prevents the patient from using Flex. To enable the
setting, set Flex to 1, 2, or 3. The patient also has access to this
setting, if Flex is enabled. The Flex feature is not available when
using an active circuit type.
Spontaneous (S) Mode
The following settings, described in the CPAP mode section of this
chapter, also are available in S mode:
• Flex
• Trigger Type
• Flow Trigger Sensitivity
• Flow Cycle Sensitivity
• Ramp Length
• Ramp Start Pressure
In addition to those settings, the settings below are also available in
S mode.
1. AVAPS
AVAPS is only available if Flex is not enabled.
You can disable AVAPS by selecting O, or you can enable AVAPS
by selecting On. If you select O, the IPAP setting displays. If you
select On, the IPAP Max Pressure and IPAP Min Pressure display.
Note: The Ramp Start Pressure
setting will not display if the
Ramp Length is set to O or if
the CPAP pressure is set to
4 cm H2O.
Note: Ramp Start Pressure is
less than or equal to CPAP - 1 cm
H2O in CPAP mode.
Note: In CPAP mode, Flex is only
available when CPAP is greater
than 4 cm H2O.
Note: In S mode, Flex is only
available when EPAP is greater
than or equal to 4 cm H2O and
IPAP is less than or equal to
25 cm H2O.
Note: Flex is only available
when Auto-Trak is enabled.
Note: Ramp is not available in
the Passive Circuit when IPAP =
EPAP = 4 cm H2O or when IPAP
Min = EPAP = 4 cm H2O.
Note: Ramp Start Pressure is
less than or equal to EPAP - 1 cm
H2O in S, S/T, T, and PC modes.
Note: Ramp Start Pressure is
greater than or equal to 0 cm
H2O when the circuit type is
Active PAP or Active Flow in S,
S/T, T, and PC modes.
Note: Ramp Start Pressure
is greater than or equal to 4
cm H2O when the circuit type
is Passive in S, S/T, T, and PC
modes.
Note: AVAPS is only available if
the Passive Circuit is selected.
Trilogy200 clinical manual
Page 92

2. IPAP
The IPAP setting displays if AVAPS is O. You can increase or
decrease the Inspiratory Positive Airway Pressure (IPAP) from 4
to 50 cm H2O in increments of 1. IPAP is limited to a maximum of
25 cm H2O when Flex is enabled. You cannot set the IPAP setting
lower than the EPAP setting.
3. IPAP Max Pressure
The IPAP Max Pressure setting displays if AVAPS is enabled.
You can increase or decrease the setting from 4 to 50 cm H2O
in increments of 1. The IPAP Max Pressure must be equal to or
greater than the IPAP Min value.
4. IPAP Min Pressure
The IPAP Min Pressure setting displays if AVAPS is enabled.
You can increase or decrease the setting from 4 to 50 cm H2O
in increments of 1. The IPAP Min Pressure must be equal to or
greater than the EPAP value, and it must be less than or equal to
the IPAP Max Pressure.
5. EPAP
You can increase or decrease the Expiratory Positive Airway
Pressure (EPAP) from 4 to 25 cm H2O in increments of 1. For
active circuits, EPAP can be set to zero.
81
Note: IPAP, IPAP Max, or IPAP
Min cannot be set to more than
30 cm H2O above EPAP.
Note: EPAP cannot be set to
more than 30 cm H2O below
IPAP, IPAP Max, or IPAP Min.
When AVAPS is disabled, the EPAP setting must be less than
or equal to the IPAP setting. When AVAPS is enabled, the EPAP
pressure must be less than or equal to the IPAP Min Pressure.
6. Tidal Volume
The Tidal Volume setting displays if AVAPS is enabled. You can
increase or decrease the setting from 50 to 2000 ml in 5 ml
increments. Use this setting to establish the target volume of
gas which the ventilator will produce and deliver during each
Spontaneous breath.
Chapter 5 Viewing and Changing Settings
Note: In CV, AC, and SIMV
modes, the tidal volume setting
is limited by the Inspiratory
Time, to maintain the system’s
minimum and maximum peak
ows.
Page 93

82
7. Rise Time
You can adjust the rise time to nd the most comfortable setting
for the patient. Increase or decrease the setting from 1 to 6
until you nd the right setting. The rise time levels from 1 to 6
progressively reect slowed response of the pressure increase
that will take place at the beginning of inspiration.
8. Apnea Rate
If the Apnea alarm is enabled, you can set the Apnea Rate from
4 to 60 BPM in 1 BPM increments. In S mode, the Apnea Rate is
greater than or equal to 1:2 I:E ratio.
Spontaneous/Timed (S/T) Mode
All of the settings described in the S Mode section are also available
in S/T mode, except for the Flex setting. In addition to those settings,
the settings below are also available in S/T mode.
1. Breath Rate
In AC mode, you can increase or decrease the Breath Rate setting
from 0 to 60 BPM, while in all other modes, you can increase
or decrease the setting from 1 to 60 BPM in 1 BPM increments.
Use the Breath Rate setting to establish the minimum rate of
mandatory breaths that the ventilator will deliver per minute.
2. Inspiratory Time
You can adjust the Inspiratory Time setting from 0.3 to 5.0
seconds in 0.1 second increments. Inspiratory Time is the
duration for the inspiratory phase of a mandatory breath.
Timed (T) Mode
All of the settings available in S/T mode are available in T mode,
except for the Trigger Type setting. Please refer to the descriptions in
the S and S/T Mode sections of this chapter for detailed information
on the T mode settings.
Note: The Rise Time setting only
displays if Flex is disabled. If Flex
is enabled, the device will use a
rise time of 3.
Note: In S/T, T, PC, PC-SIMV,
SIMV, CV, and AC modes, the
Apnea Rate is greater than or
equal to the Breath Rate and is
limited by the current Inspiratory
Time setting to maintain a
minimum 1:1 I:E ratio.
Note: In volume modes, the
Breath Rate range is limited by
the current Inspiratory Time
setting to maintain a minimum
1:1 I:E ratio.
Note: In pressure modes, the
inspiratory time range is limited
by the current Breath Rate
setting to maintain a minimum
1:1 I:E ratio.
Note: In volume modes, the
inspiratory time range is limited
by the current Tidal Volume and
Breath Rate settings to maintain
a minimum 1:1 I:E ratio and
the system’s minimum and
maximum peak ow.
Trilogy200 clinical manual
Page 94

Pressure Control (PC) Mode
All of the settings available in S/T mode are available in PC mode,
except for the Flow Cycle Sensitivity setting (when Flow Trigger is
enabled). Please refer to the descriptions in the S and S/T Mode
sections of this chapter for detailed information on the PC mode
settings.
Pressure Control Synchronized Intermittent Mandatory Ventilation
(PC-SIMV) Mode
The following settings, described in the S and S/T mode sections of
this chapter, also are available in PC-SIMV mode:
• Breath Rate
• Inspiratory Time
• Trigger Type
• Flow Trigger Sensitivity (if Trigger Type is set to Flow
Trigger)
• Flow Cycle Sensitivity (if Trigger Type is set to Flow
Trigger)
• Rise Time
83
In addition to these, the following settings are also available in PCSIMV mode.
1. Pressure
You can increase or decrease the Pressure setting from 4 to 50
cm H2O in increments of 1. This is the pressure the ventilator will
deliver during the inspiratory phase of a mandatory or assist
breath.
2. Pressure Support
You can increase or decrease the Pressure Support setting from
0 to 30 cm H2O in increments of 1. This is the pressure support
the ventilator will deliver during the inspiratory phase of a
Spontaneous breath.
Chapter 5 Viewing and Changing Settings
Note: In PC-SIMV mode, you
cannot set up Pressure Support
for Mandatory and Assist
breaths (Pressure - PEEP) greater
than 30 cm H2O.
Note: The Pressure Support and
PEEP settings together cannot
exceed 50 cm H2O.
Page 95

84
3. PEEP
The Positive End Expiratory Pressure (PEEP) setting can be
increased from 0 to 25 cm H2O in active circuits and 4 to 25 cm
H2O in passive circuits, in increments of 1. PEEP is the positive
pressure maintained in the patient circuit during exhalation. The
PEEP must be less than or equal to the pressure setting.
Control Ventilation (CV) Mode
The following settings, described in the previous sections of this
chapter, are also available in CV mode:
• Tidal Volume
• Breath Rate
• Inspiratory Time
• PEEP
• High Inspiratory Pressure
• Low Inspiratory Pressure
In addition to these, the following settings are also available in CV
mode.
1. Flow Pattern
You can choose either Ramp or Square for the Flow Pattern setting.
2. Sigh
You can enable or disable the Sigh setting by selecting On or O.
A Sigh is a breath that is delivered every 100 breaths at 150% of
the normal volume.
Trilogy200 clinical manual
Note: The Flow Pattern setting
might be limited to only Ramp
or Square based on the Tidal
Volume, Inspiratory Time, and
Breath Rate settings to maintain
the minimum and maximum
peak ows.
Page 96

Assist Control (AC) Mode
The AC mode contains the following settings described in the S, S/T,
PC-SIMV, and CV mode sections in this chapter. Please refer to the
descriptions in those sections for detailed information.
• Tidal Volume
• Breath Rate
• Inspiratory Time
• Flow Pattern
• PEEP
• Trigger Type
• Flow Trigger Sensitivity
• Sigh
• High Inspiratory Pressure
• Low Inspiratory Pressure
Synchronized Intermittent Mandatory Ventilation (SIMV) Mode
The SIMV mode contains the following settings described in the S,
S/T, PC-SIMV, and CV mode sections in this chapter. Please refer to the
descriptions in those sections for detailed information.
85
Note: The Low Inspiratory
Pressure is limited to PEEP +2 in
CV, AC, and SIMV modes.
Note: Flow Cycle Sensitivity is
not available in AC mode.
• Tidal Volume
• Breath Rate
• Inspiratory Time
• Pressure Support
• Flow Pattern
• PEEP
• Trigger Type
• Sigh
• Rise Time
• High Inspiratory Pressure
• Low Inspiratory Pressure
Chapter 5 Viewing and Changing Settings
Page 97

86
Viewing and Changing Options Menu Items
From the Main Menu screen, select the Options item.
The Options menu appears, shown in the screen below.
The following settings are available on the Options menu.
• Menu Access – You can select Full or Limited menu
access. Full menu access allows operators to access all
ventilator and prescription settings. Limited menu access
allows operators to access only certain settings and
does not allow them to change prescription settings. To
prevent patients from changing prescription settings, do
not give them Full menu access.
• Detailed View – You can turn Detailed View on or o
using this setting. Detailed view displays additional
settings and therapy information on the Monitor screen.
Options Menu
• Language – The next item on the Options menu allows
you to select the Language that the software will appear
in (English, French, German, etc.). The information on the
screens will display in the language selected here.
• Pressure Units – The next item allows you to select the
pressure units that will display on the screens. You can
choose either:
- cm H2O
- hPa
- mBar
Trilogy200 clinical manual
Page 98

All pressure units on the screens will display in the unit of
measure selected here.
87
• Alarm Volume – You can adjust the volume of the device
alarms using this setting. Select either Loud or Soft as the
alarm volume options.
• Keypad Lock – You can enable or disable the Keypad
Lock feature, which is described in detail earlier in this
chapter. Enabling the Keypad Lock feature can prevent
someone from accidentally pressing a button and
changing any of the settings. Select On to enable the
feature or O to disable it.
• Keypad Backlight – The next item you can set is the
Keypad Backlight. You can turn the backlight On or O
using this setting. Whenever you press the button to
begin therapy, the keypad backlight temporarily lights
up. Once therapy is being provided, the keypad will be lit
according to this Keypad Backlight setting. If the setting
is On, the backlight remains on while therapy is provided.
If the setting is O, the backlight remains o while
therapy is provided.
• LCD Brightness – The LCD display is lit by a backlight.
The backlight turns on when the initial Startup screen
displays. You can adjust the brightness of the LCD
backlight from 1 – 10, with 1 being the dimmest setting
and 10 being the brightest.
• Screen Saver – You can change the screen saver to
reduce power consumption or dim the screen in a dark
room. You can choose the following settings:
- O: No screen saver displays and the LCD backlight remains
lit at your brightness setting.
WARNING
Make sure the alarm volume is
set loud enough to be heard by
the caregiver. Consider the use of
a remote alarm.
Note: Setting the screen saver
to Black allows the device to run
for a longer period of time on
battery power.
- Breath: The display appears as a black screen, with only the
patient breath indicator and manometer visible.
- Black: The display’s backlight is turned o and the display is
black with no information visible.
Chapter 5 Viewing and Changing Settings
Page 99

88
- Dim: The display’s backlight is decreased, so that the display
is still visible but not as bright.
If enabled, the screen saver will display after 5 minutes of no
keypad activity. Pressing any button on the device will exit the
screen saver. And, any alarm or informational message will also
exit the screen saver.
• Date Format – You can choose either mm/dd/yyyy or
dd/mm/yyyy as the date format that will display on the
device screens.
• Time Format – You can choose to display either an AM/
PM time format or 24 Hour time format (for example,
2:49 PM or 14:49).
• Month – The month defaults to the current month. The
adjustable range is from 1 (January) – 12 (December).
• Day – The day defaults to the current day. The adjustable
range is from 1 – 31. The maximum value is based on the
selected month.
• Year – The year defaults to the current year. The
adjustable range is from 2000 – 2099.
• Hour – The hour defaults to the current hour. The
adjustable range is from 12 AM – 12 PM or 0-23,
depending on the selected Time Format.
• Minute – The minute defaults to the current minute. The
adjustable range is from 0 – 59.
• IP Address Mode – You can change the IP address
mode to either DHCP or Static, depending on the type of
network you are using (if applicable).
Trilogy200 clinical manual
Page 100

• Operational Hours – The operational hours displays
the total number of hours that the device blower has
been on since the last time this value was reset. You can
reset this value to zero (0) if desired (e.g., each time you
give the device to a new patient). This value helps you
determine how often the patient is using the device. The
Operational Hours shown here diers from the Blower
Hours shown on the Information screens. The Blower
Hours displayed in the Information screen is the total
number of hours that the blower has been working over
the life of the device. You cannot reset this value.
Viewing the Alarm Log
From the Main Menu screen, you can select Alarm Log to access the
Alarm Log screen. An example is shown below.
89
Note: In the Alarm Log screen,
the 1/2 shown in the Menu
banner indicates that page 1
of 2 alarm log pages is being
viewed at this time.
The alarm log displays the alarms in chronological order with the
most recent events displayed rst. It lists the 20 most recent alarms
or messages that appeared on the device display. When the device is
in Limited Menu access mode, the alarm log cannot be cleared. It can
be cleared when in Full Menu access mode. Depending on how many
alarms have occurred, the alarm log may be several pages long. The
entries in the alarm log use the same names that displayed when the
alarm initially occurred and was displayed in the Alarm View.
Chapter 5 Viewing and Changing Settings
Alarm Log Screen
Note: In Full Menu access mode,
you can press the Right (Clear)
button to clear the alarm log if
desired.
 Loading...
Loading...