Page 1

Understanding
R2 ImageChecker
MAN-00934 Rev 002
®
9.1
Page 2

Page 3
Mammography
Understanding
R2 ImageChecker
PN MAN-00934 Rev 001
®
9.1
Page 4

Technical Support
For support in North America contact:
Toll Free: +1.866.243.2533 (+1.866.CHECKED)
Email: r2support@hologic.com
Hours: Monday – Friday, 6:00 AM – 5:00 PM, PT (GMT –8:00)
Website: www.hologic.com
For support in Europe, South America, or Asia, contact your local dealer or distributor.
© 2008, Hologic, Inc. All rights reserved. Duplication or distribution without written permission
is prohibited. Hologic reserves the right to revise this manual. Issued June 2008.
Protected by one or more of the following U.S. Patents: 5133020, 5452367, 5491627, 5537485,
5622171, 5657362, 5673332, 5729620, 5732697, 5740268, 5815591, 5828774, 5832103,
5917929, 6014452, 6035056, 6075879, 6078680, 6185320, 6198838, 6263092, 6266435,
6301378, 6404908, 6434262, 6477262, 6574357, 6580818, 6640001, 6628815, 6909795,
7054473, 7072498, 7146031, 7174515
Hologic, the Hologic logo, Cenova, Citra, DigitalNow, EmphaSize, ImageChecker, LesionMetrics,
Malc, PeerView, Quantra, RightOn, R2, R2 Technology, SecurView
trademarks or registered trademarks of Hologic in the USA. MAMMOMAT is a registered
trademark of Siemens Medical Solutions in the USA.
, and Selenia are
DX
Hologic Inc.
35 Crosby Drive
Bedford, MA 01730-1401 USA
Tel: +1.781.999.7300
Sales: +1.781.999.7453
Fax: +1.781.280.0668
Asia Pacific
Room 302, Hung Kei Building
5-8 Queen Victoria Street
Central, Hong Kong
Tel: +852.3102.9200
Hologic N.V.
Authorized Representative
Leuvensesteenweg 250A
1800 Vilvoorde, Belgium
Tel: +32.2.711.4680
Fax: +32.2.725.2087
ii Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002
Page 5

Contents
Part 1: Introduction....................................................... 1
1.1. Intended Use......................................................... 1
1.2. Resources Available ................................................... 2
1.3. Warnings and Precautions .............................................. 3
1.4. Overview of ImageChecker CAD.......................................... 5
1.5. Benefits of ImageChecker CAD........................................... 6
1.6. Devices Used with ImageChecker CAD .................................... 7
Image Acquisition Systems .............................................. 7
R2 Cenova Server ..................................................... 8
Diagnostic Review Workstations and PACS Devices ........................... 8
1.7. ImageChecker Features ................................................ 9
Input Ports .......................................................... 9
Citra Core ........................................................... 9
RightOn CAD Marks.................................................. 10
EmphaSize.......................................................... 10
PeerView Digital ..................................................... 10
LesionMetrics ....................................................... 10
Operating Points ..................................................... 11
Part 2: Data Inputs and Outputs
2.1. System Data Flows................................................... 13
......................................... 13
Digital CAD Systems .................................................. 13
Digital CAD with DICOM 6000 Overlay ................................... 15
Digital and Film-Based CAD with DigitalNow .............................. 16
2.2. CAD Inputs and Supported Views ....................................... 18
Images with Breast Implants ............................................ 18
2.3. Image and Case Processing ............................................ 19
Selecting Images for Case Processing ...................................... 19
2.4. CAD Outputs........................................................ 21
DICOM 6000 Overlays ................................................ 21
Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 iii
Page 6
Contents
Part 3: Algorithm Description ............................................ 23
3.1. ImageChecker CAD Algorithm .......................................... 23
3.2. RightOn CAD Marks .................................................. 24
Limiting the Number of Marks .......................................... 24
3.3. EmphaSize Marks .................................................... 25
3.4. PeerView Digital ..................................................... 26
3.5. LesionMetrics ....................................................... 27
3.6. What the Algorithm Detects............................................ 28
Calcifications........................................................ 28
Masses/Architectural Distortions......................................... 29
3.7. Detecting Calcifications ............................................... 31
Image Processing for Calcifications ....................................... 31
Case Processing for Calcifications ........................................ 32
3.8. Detecting Masses .................................................... 33
Image Processing for Masses ............................................ 33
Case Processing for Masses ............................................. 34
3.9. CAD Operating Points................................................. 35
Index .................................................................. 39
iv Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002
Page 7

Part 1: Introduction
f 1.1. Intended Use
f
1.2. Resources Available
f
1.3. Warnings and Precautions
f
1.4. Overview of ImageChecker CAD
f
1.5. Benefits of ImageChecker CAD
f
1.6. Devices Used with ImageChecker CAD
f
1.7. ImageChecker Features
R2 ImageChecker® is a software algorithm used for analyzing mammography images.
The software was originally developed by R2 Technology, and is now available as a
licensed option with Hologic’s R2 Cenova™ digital mammography server.
The R2 Cenova server provides a second application, R2 Quantra™, which is used for
volumetric assessments of breast tissue. For more information, refer to the manual
Understanding Quantra 1.1. (Quantra is not available in the United States.)
The information in this manual is intended to serve as a reference for radiologists and
clinic personnel who need to understand how computer-aided detection (CAD) can
be integrated into their practices.
1.1. Intended Use
ImageChecker is a software application intended to identify and mark regions of
interest on routine screening and diagnostic mammograms to bring them to the
attention of the radiologist after the initial reading has been completed.
ImageChecker assists the radiologist in minimizing observational oversights by
identifying areas on the original mammogram that may warrant a second review.
Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 1
Page 8

Part 1: Introduction
1.2. Resources Available
In addition to this manual, the following resources are available to assist you when
working with ImageChecker and the R2 Cenova server.
•
R2 Member Center: This website provides quick access to electronic (pdf) versions
of Hologic | R2 manuals and training materials. You can find the R2 Member
Center by visiting the Hologic website (
accompanies this product for instructions on accessing the R2 Member Center.
•
Manuals: The manuals for the R2 Cenova server and its applications are listed
below:
– Understanding R2 ImageChecker
– Understanding R2 Quantra
– R2 Cenova User Manual
– R2 Cenova Service Manual
– R2 Cenova Release Notes
– R2 Cenova DICOM Conformance Statement
www.hologic.com). See the R2U flyer that
– R2 Cenova Cybersecurity Best Practices
– R2 Cenova IHE Integration Statement
You can obtain additional copies of printed manuals through your Hologic
Account Manager. The DICOM Conformance Statement and Cybersecurity Best
Practices documents are available at
•
Training: The Hologic Applications team is available to train your staff, should you
www.hologic.com.
feel they need additional training. To purchase additional personalized instruction,
contact your Hologic Account Manager.
•
Technical Support and Service: For support in North America contact:
Toll Free:
Email:
+1.866.243.2533 (+1.866.CHECKED)
r2support@hologic.com
Hours: Monday – Friday, 6:00 AM – 5:00 PM, PT (GMT –8:00)
Website:
www.hologic.com
For support in Europe, South America, or Asia, contact your local dealer or
distributor.
2 Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002
Page 9

1.3. Warnings and Precautions
Note: For Warnings and Cautions related to the installation, operation, and
maintenance of the R2 Cenova server, refer to the R2 Cenova User Manual.
• The radiologist should base interpretation only on diagnostic-quality images and
not depend on ImageChecker CAD marks for interpretation.
• The device is a detection aid, not an interpretative aid. ImageChecker CAD marks
should be activated only after the first reading.
• The device does not enhance what the user sees; rather it helps to identify regions
on mammograms that should be re-examined.
• The ImageChecker software marks calcification features with triangles (Calc
marks) and mass features with asterisks (Mass marks). The software marks mass
and calcification features that occur at the same location on the image with
pointed crosses (Malc marks). These features may not represent cancer, and the
skill of the user is still required for proper interpretation of the marked areas.
• EmphaSize (variable-size) marks – Sites may choose to display prominence detail,
in which case the size of a Calc, Mass, or Malc mark is proportional to the ranking
of the feature by the algorithm. The marked features may not represent cancer,
and the skill of the user is still required for proper interpretation of areas marked
by the device.
1.3. Warnings and Precautions
• During routine interpretation of mammograms and results produced by
ImageChecker CAD, Hologic recommends use of a mammography workstation
that has been FDA-approved, recently calibrated, and employs a CAD marking
schema authorized by Hologic.
• ImageChecker software does not identify all areas that are suspicious for cancer.
– The software does not mark all lesions and a user should not be dissuaded from
working up a finding if the software fails to mark that site.
– The software is not designed to detect changes from prior mammograms.
– The software is not designed to detect skin thickening or nipple retractions.
– Conditions of the breast that diminish mammographic sensitivity, such as
density of normal tissue, also diminish the sensitivity of the software.
– The software is more sensitive for detection of calcifications than masses, and the
sensitivity depends on the site-specific operating points chosen. For sensitivity
values, see ‘
algorithm has a lower sensitivity for masses greater than 2.5 cm in diameter.
– Individual practice patterns may influence results obtained when using
ImageChecker CAD. Therefore, each facility and radiologist should carefully
monitor the results that the software has on their practice of mammography in
order to optimize its effectiveness.
3.9. CAD Operating Points’. In addition to not marking all masses, the
• For images with breast implants, send only Implant Displaced views to the system.
Images with more than 2.5 cm (1 in) of the breast implant appearing on the image
may not be processed correctly.
Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 3
Page 10
Part 1: Introduction
• The performance of the software has not been characterized for special diagnostic
views (e.g., magnified views or spot-compressed views).
• Images of partial views of the breast that are not correctly identified as such, may
be processed by the software, although the software has not been designed for that
purpose.
• On rare occasions for a lesion on or near the pectoral muscle, the system may
report a negative value for the chest wall distance.
4 Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002
Page 11
1.4. Overview of ImageChecker CAD
The R2 Cenova server configured with ImageChecker software analyzes digital
mammography images produced by full-field digital mammography (FFDM)
systems. The proprietary ImageChecker algorithm identifies regions of interest, which
can include clusters of bright spots (suggestive of calcification clusters), and dense
regions with or without radiating lines (suggestive of masses or architectural
distortions). The server generates results in the form of Mammography CAD SR
(Structured Report) objects that include CAD marks and other data identifying and
characterizing the regions of interest. At the review workstation, the results are
matched with the digital mammography images produced by the FFDM system.
After making an initial interpretation from the original diagnostic-quality images, the
radiologist displays the ImageChecker results and chooses whether or not to reinspect
the marked regions on the original images. The ImageChecker algorithm marks
visually perceptible structures that have some of the generally accepted geometric
characteristics of calcifications or masses. The marked areas may be something other
than an actual abnormality, which is generally recognized by the radiologist upon a
second review of the original images.
1.4. Overview of ImageChecker CAD
Examination is
Performed
Note: The appearance of the images on the workstation is dependent upon the
acquisition modality and the workstation’s display capabilities, and is not affected by the
ImageChecker software.
The R2 Cenova server and the ImageChecker algorithm are designed for sites that
process only digital mammography images; the server does not scan films or support
CAD with analog (film) mammograms. For information on systems that perform
film-screen CAD, contact your Hologic Account Manager.
For Presentation Images
For Processing Images
ImageChecker CAD
Analyzes the Images
Workflow with ImageChecker CAD
Mammography
CAD SR
Radiologist
Reviews Images
Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 5
Page 12

Part 1: Introduction
1.5. Benefits of ImageChecker CAD
The interpretation of mammograms is challenging. Normal breast tissue varies widely
among women, even for the same woman over time or at different times of the
month. The radiologist also has to balance the need for accurate detection with the
need to limit the number of unnecessary procedures. The combination of viewing a
large number of cases, radiologist fatigue, the complex image of the breast structure,
and the subtle nature of certain observable characteristics of the disease can result in
false-negative readings. In fact, studies show that half of undetected cancers are
missed due to observational oversights. The prevalence of observational oversights is
not strongly related to experience and may be inevitable with human observers.
ImageChecker CAD functions like a spellchecker for medical images. It is designed to
help radiologists in reducing the number of false-negative readings due to
observational oversight by drawing their attention to areas that may warrant a second
review. Retrospective clinical studies using the film-based ImageChecker algorithm
have shown that use of ImageChecker CAD can result in earlier detection of up to
23.4% of the cancers currently detected with screening mammography in those
women who had a prior screening mammogram 9–24 months earlier. Early detection
is the key to higher survival rates, better prognosis, and lower treatment costs.
6 Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002
Page 13

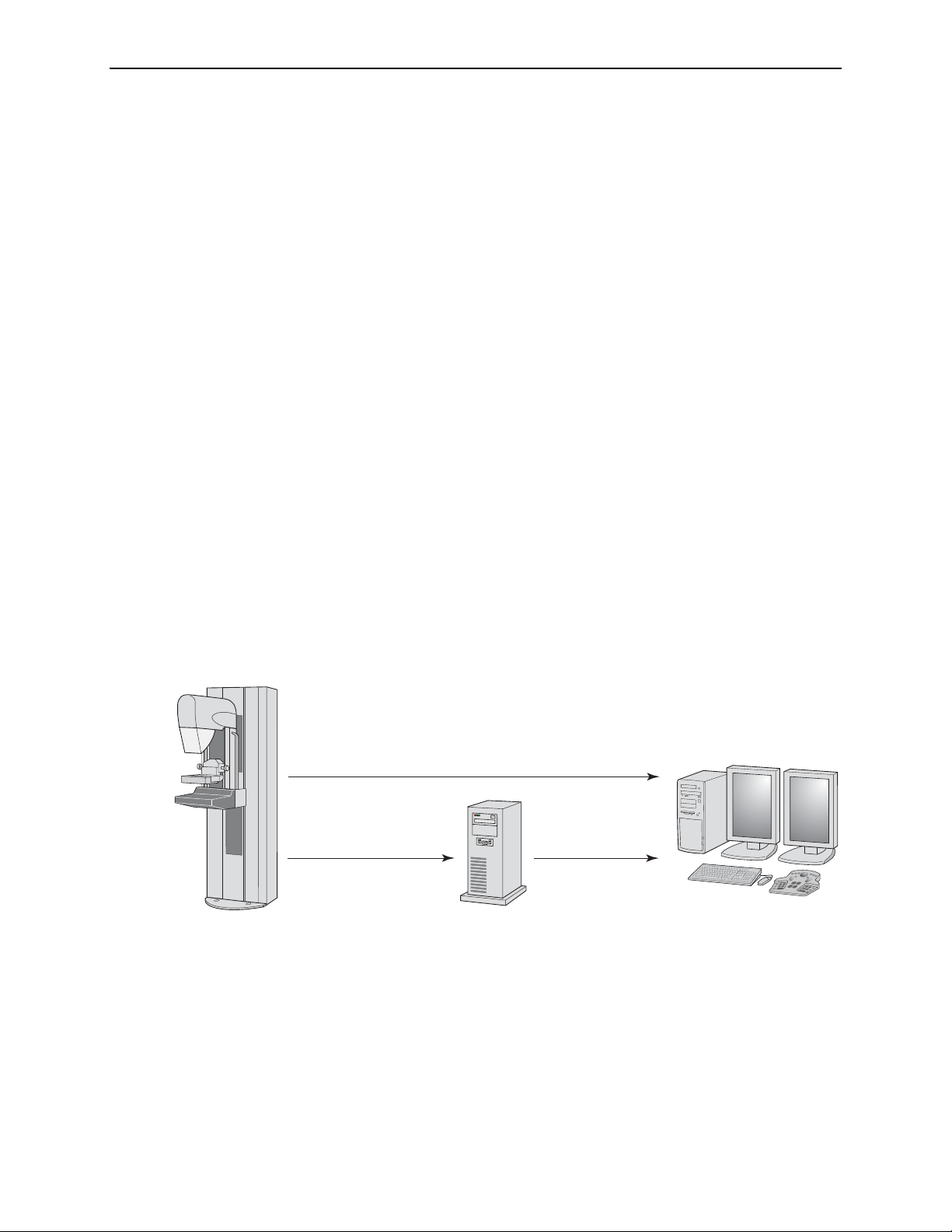
1.6. Devices Used with ImageChecker CAD
All systems with ImageChecker include the following devices:
• Digital mammography image acquisition system(s)
• R2 Cenova server configured with the ImageChecker option
• Diagnostic review workstation or PACS
The ImageChecker software can accept digital mammography images from a
supported Full-Field Digital Mammography (FFDM) system or a PACS (picture
archiving and communication system). Once received, the server performs the CAD
algorithm processing and sends the study results (CAD marks and related data) to
one or more devices such as Hologic’s SecurViewdx diagnostic workstation or a
PACS for storage.
The system devices are connected by a computer network and can be in the same
room, different rooms, the same building, different buildings, or even different cities.
The server can send results to several different output devices.
Image Acquisition Systems
1.6. Devices Used with ImageChecker CAD
ImageChecker processes mammography images originating from the following image
acquisition systems:
• Hologic Selenia
• GE Senographe 2000D, GE Senographe DS, and GE Senographe Essential
• Siemens Mammomat Novation
dr
In addition, ImageChecker processes mammography images originating from the
following image acquisition systems:
• Selenia Dimensions (2D Only)
• Fuji CRm
Important! The FDA has not approved the use of ImageChecker 9.1 with images
originating from the Selenia Dimensions and Fuji CRm systems in the United States.
R2 Cenova does not process mammography images originating from the Fischer
SenoScan system.
R2 Cenova can process images originating from up to four image acquisition devices.
The DICOM header for each image includes an identifier (e.g., a serial number) that
indicates the device from which the image originated. Each image-acquisition device
is mapped to an input port on the server. For each R2 Cenova server, you can
purchase licenses for up to four ImageChecker input ports.
Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 7
Page 14

Part 1: Introduction
R2 Cenova Server
The ImageChecker software is supplied on the R2 Cenova server, a high-performance
computer that can be located in any non-patient environment, provided it is
connected to the mammography network. The server receives and processes digital
mammography images and supports up to four ImageChecker ports (each port
licensed to a specific detector).
R2 Cenova integrates easily into the clinical workflow. Following a mammography
examination, the FFDM system sends digital mammography images to the clinic’s
review workstation, PACS, and the R2 Cenova server. The server accepts and
processes each For Processing image and sends the results to the review workstation
and PACS.
For more information on the server, refer to the R2 Cenova Server User Manual.
Diagnostic Review Workstations and PACS Devices
Mammography CAD SR results produced by R2 Cenova can be sent to a variety of
PACS devices and diagnostic review workstations (including SecurViewdx available
from Hologic, Inc.).
For diagnostic review workstations and PACS devices that do not support
Mammography CAD SR, but do support DICOM 6000 overlays, Hologic’s DICOM
6000 Interface server can be used to convert Mammography CAD SR objects. For
more information, contact your Hologic Account Representative.
8 Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002
Page 15

1.7. ImageChecker Features
Each R2 Cenova server with ImageChecker software is delivered with a number of
licensed features in place. Upon installation, the Hologic | R2 field service engineer
will tailor the software to enable or disable selected features based on the preferences
of site personnel. Thereafter, your Hologic | R2 representative can help you add new
licenses and enable or disable features as needed.
Input Ports
The R2 Cenova server can process images originating from up to four FFDM systems.
The DICOM header for each image includes an identifier (e.g., a serial number) that
indicates the device from which the image originated. Each image-acquisition device
is mapped to an input port on the server.
For each R2 Cenova server, you can purchase licenses for up to four ImageChecker
input ports. Similarly, you can obtain licenses for up to four Quantra input ports.
The server can also process images sent from any number of PACS devices, as long as
the images originated from one of the licensed FFDM systems.
Citra Core
1.7. ImageChecker Features
The standard set of ImageChecker features is included in the Citra™ Core license
group, which includes the following features:
• RightOn™ CAD Marks
• EmphaSize™
• PeerView Digital™
• LesionMetrics™
EmphaSize, PeerView Digital, and LesionMetrics are exclusive Hologic | R2 features
supported by some diagnostic review workstations. When these features are licensed,
the ImageChecker software includes extra CAD information in the Mammography
CAD SR output. When viewed at the workstation, the results help radiologists
understand better why a region of interest received a CAD mark.
The Citra Core features are discussed in the following pages. For additional
information, see ‘
Part 3: Algorithm Description’.
Important! Display of results from each ImageChecker feature depends upon several
factors, in particular:
• The feature must be licensed and enabled on the R2 Cenova server.
• The workstation must be equipped with software that can interpret the output
produced by the server.
Individual Citra Core features can be disabled either at the R2 Cenova server or, in most
cases, at the diagnostic workstation. Some workstations can interpret only a subset of
Citra Core features. Consult with your workstation vendor concerning availability and
integration of ImageChecker features with your workstation.
Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 9
Page 16

Part 1: Introduction
RightOn CAD Marks
The ImageChecker software provides three types of RightOn CAD marks (Mass, Calc,
and Malc) that can appear in the results shown on the review workstation. You can
choose to display any or all of the three types of marks. Each mark identifies a region
of interest for the radiologist to review.
EmphaSize
The server is configured by default to convert the CAD marks to EmphaSize marks.
The feature allows the review workstation to display marks of variable size that
correlate to feature significance. When the algorithm determines that a region is more
significant, the CAD mark appears larger, indicating that the region should receive
more emphasis from the radiologist. EmphaSize marks can be disabled if clinic staff
choose not to use them. For more information see ‘
Calc – Marks regions suggestive of calcifications.
Mass – Marks regions suggestive of masses or architectural distortions.
Malc – Marks regions where Calc and Mass marks are coincident.
3.3. EmphaSize Marks’.
PeerView Digital
PeerView Digital enables the radiologist to understand better why a region of interest
was marked. On advanced review workstations such as Hologic’s SecurViewdx,
PeerView Digital highlights physical features found by the algorithm. For more
information see ‘
LesionMetrics
LesionMetrics provides data computed by ImageChecker CAD for each region of
interest marked by the algorithm. Depending upon the type of lesion, the software
can compute metrics such as lesion size, distance to nipple, distance to chest wall,
degree of spiculation, calcification contrast, number of calcifications, and mass
density. For more information see ‘
3.4. PeerView Digital’.
3.5. LesionMetrics’.
10 Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002
Page 17

Operating Points
1.7. ImageChecker Features
The ImageChecker algorithm offers three operating points (i.e., CAD algorithm
thresholds) to accommodate differing radiologist preferences: operating point 0,
which emphasizes specificity (a low false-mark rate), operating point 1, which is a
balanced intermediate point, and operating point 2, which emphasizes sensitivity.
The algorithm performance for each of the operating points is summarized below:
Operating Point 0 1 2
Calcification Sensitivity 95% 96% 97%
Mass Sensitivity 83% 88% 90%
False Marks per Case 1.0 1.5 2.0
When your system is installed, the server is configured to use operating point 1 for
masses and operating point 2 for calcifications. You can choose other settings, or your
service representative can change the operating points at a later time. For new
customers, Hologic | R2 recommends using the default settings for the first four to six
weeks to allow you to become familiar with the R2 marks and algorithm behavior.
Hologic ’s ImageChecker algorithm provides the medical-imaging industry’s highest
sensitivity at any given false-mark rate. ImageChecker CAD was the first computeraided detection software approved by the FDA for full-view diagnostic and screening
mammograms. Since that first approval, the ImageChecker software has been refined
many times, resulting in an algorithm that is highly sensitive with few false marks. For
more information, see ‘
3.9. CAD Operating Points’.
Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 11
Page 18

Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 12
Page 19

Part 2: Data Inputs and Outputs
f 2.1. System Data Flows
f
2.2. CAD Inputs and Supported Views
f
2.3. Image and Case Processing
f
2.4. CAD Outputs
Part 2 explains how information flows through systems with ImageChecker CAD, the
supported mammography views, and the result formats.
2.1. System Data Flows
This section describes the flow of data among the various Hologic | R2 devices.
Mammography systems may have different configurations, depending upon the
devices installed at your site:
f Digital CAD Systems
f
Digital CAD with DICOM 6000 Overlay
f
Digital and Film-Based CAD with DigitalNow
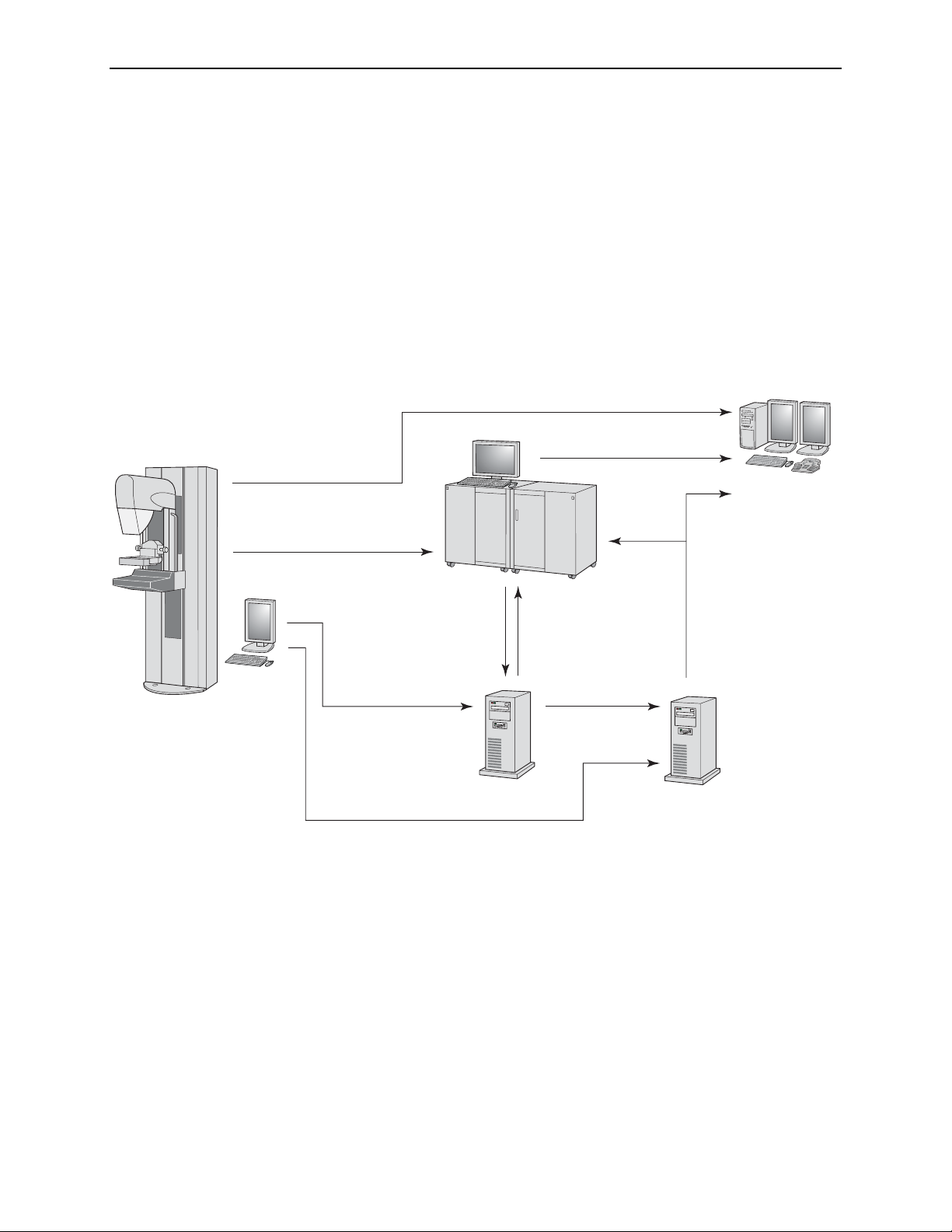
Digital CAD Systems
To follow the data flows, refer to the diagram on the following page.
Image Acquisition Device(s)
1, 2, 3: FFDM systems can be configured to send Digital Mammography X-Ray
images to any device that conforms to the Digital Imaging and Communications in
Medicine (DICOM) standard. The FFDM device sends two types of images, For
Processing images to the R2 Cenova server, and For Presentation images to the
diagnostic review workstation(s) and PACS.
Note: The DICOM standard specifies two classes of archivable digital mammography
images with the following designations:
• Digital Mammography X-Ray Image Storage – For Processing images
• Digital Mammography X-Ray Image Storage – For Presentation images
R2 Cenova Server
4, 5: R2 Cenova servers send results (Mammography CAD SR objects) to one or more
diagnostic review workstation(s) and/or PACS devices simultaneously.
Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 13
Page 20

Part 2: Data Inputs and Outputs
Diagnostic Review Workstation(s) and PACS
4, 7: The review workstation(s) are configured to receive the For Presentation images
and CAD results, which are then reviewed by the radiologist.
6, 7: The PACS can be configured to send:
• For Processing Digital Mammography X-Ray images to R2 Cenova (6), which
processes the images and distributes the CAD results according to its
configuration, and/or
• CAD results and/or For Presentation Digital Mammography X-Ray images to the
review workstations (7).
3
For Presentation Images
For Presentation Images
2
For Processing Images
(if archived)
For Presentation Images
7
Mammography
CAD SR Objects
PACS
SecurView
(or other diagnostic
workstations)
DX
Image Acquisition
System(s)
Note: Elements shown in
italic type are optional.
For Processing Images
6
1 For Processing Images
(if archived)
Digital CAD System
R2 Cenova
Mammography
5
CAD SR Objects
4
Mammography
CAD SR Objects
14 Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002
Page 21
Digital CAD with DICOM 6000 Overlay
Typically, diagnostic review workstations and PACS devices support the Mammography CAD SR results format. If the review workstation or PACS does not support
Mammography CAD SR, but does support DICOM 6000 overlays, a supplementary
interface computer can be installed.
The DICOM 6000 Interface server creates a copy of the For Presentation image with
an overlay containing the CAD results that can be viewed on the diagnostic
workstation. (Refer to paths 4, 8, and 9 in the diagram below. The earlier diagram
provides information on data flows 1–7.)
For more information about the Hologic DICOM 6000 interface option, contact your
Hologic Account Representative.
3
For Presentation Images
2
For Presentation Images
For Processing Images
(if archived)
For Presentation Images
7
PACS
2.1. System Data Flows
Diagnostic
Workstation(s)
Image Acquisition
System(s)
Note: Elements shown in
italic type are optional.
6
For Processing Images
For Processing Images
1
8
For Presentation Images
(if archived)
R2 Cenova
Mammography
5
CAD SR Objects
4
Mammography
CAD SR Objects
Digital CAD System with DICOM 6000 Interface
For Presentation Images
9
with DICOM 6000 Overlays
DICOM 6000
Interface
Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 15
Page 22

Part 2: Data Inputs and Outputs
Digital and Film-Based CAD with DigitalNow
Some facilities with analog (film-based) mammography systems, or those with large
film libraries may wish to acquire one of Hologic | R2’s film-scan systems (R2 DMax
or R2 LS). With these systems, the scanned films can be analyzed using ImageChecker
CAD, or they can be converted to archivable digital images using Hologic | R2’s
DigitalNow feature.
To follow the data flows, refer to the diagram on the next page. The earlier diagrams
provide information on data flows 1–7.
Films
8: Film priors are fed into the processing unit with film scanner, which scans
(digitizes) the films and processes the resulting images.
Processing Unit with Film Scanner
9: The R2 processing unit with film scanner can be configured to send ImageChecker
results (processed from digitized film images) and/or the For Presentation Digital
Mammography X-Ray images themselves to a PACS or review workstation.
When scanning films for digital review, sites need the ability to retrieve patient
information in order to add the required identification information to the resulting
Digital Mammography X-Ray images. Sites can use the R2 Patient ID feature to either
enter patient data manually or retrieve the data from a PACS or RIS (Radiology
Information System).
16 Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002
Page 23

Image Acquisition
System(s)
3 For Presentation Images
2
For Presentation Images
For Processing Images
(if archived)
6
For Processing Images
(if archived)
For Presentation Images
7
Mammography
CAD SR Objects
PACS
5
Mammography
CAD SR Objects
2.1. System Data Flows
SecurView
(or other diagnostic
workstations)
DX
1 For Processing Images
R2 Cenova
9 For Presentation Images
8
Films
R2 Processing Unit
with Film Scanner
from Digitized Films
4 Mammography
CAD SR Objects
Note: Elements shown in
italic type are optional.
Digital CAD with DigitalNow
Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 17
Page 24

Part 2: Data Inputs and Outputs
2.2. CAD Inputs and Supported Views
The ImageChecker software analyzes digital mammography images that conform to
the Digital Imaging and Communications in Medicine (DICOM) standard.
If your system has the ImageChecker license, all images are CAD-processed if the
views are supported by the software. The following table lists the views and view
modifiers supported by the ImageChecker software:
Supported DICOM Views
and View Modifiers
Screening Views Cranio-Caudal CC
Medio-Lateral Oblique MLO
Equivalent Views Medio-Lateral ML
Cranio-Caudal Exaggerated XCC
Cranio-Caudal Exaggerated Laterally XCCL
Cranio-Caudal Exaggerated Medially XCCM
Reversed Equivalent
Views
Cranial-Caudal From Below FB
Superolateral to Inferomedial Oblique SIO
View Modifiers Axillary Tail (modifies MLO views only) AT
Rolled Inferior …RI
Rolled Lateral …RL
Rolled Medial …RM
Rolled Superior …RS
Implant Displaced …ID
Tangential TAN
The ImageChecker software does not support the following view modifiers:
Unsupported
View Modifiers
Cleavage (modifies CC views only) CV
Magnification M…
Spot Compression S…
*American College of Radiology Mammography Quality Control Manual 1999
Images with Breast Implants
Latero-Medial LM
Latero-Medial Oblique LMO
ACR MQCM 1999*
View Label
ACR MQCM 1999*
View Label
The ImageChecker software does attempt to process images with breast implants. For
images with breast implants, send only Implant Displaced views to the system. Images
with more than 2.5 cm (1 in) of the breast implant appearing on the image may not
be processed correctly.
18 Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002
Page 25

2.3. Image and Case Processing
During processing, the ImageChecker software analyzes each received image, as long
as the view is supported by the software. The algorithm searches for patterns
suggestive of calcification clusters and masses or architectural distortions,
characterizes each suspected lesion, and finally determines the location and numbers
of CAD marks for the image. This initial analysis is known as image processing.
The R2 Cenova server reads the DICOM header of each received image and groups
successive images from a single patient into a study. There is no specified limit to the
number of images that can be included in a study. However, for many patients, a
study consists of the four screening views:
2.3. Image and Case Processing
• LCC – Left Cranio-Caudal
• LMLO – Left Medio-Lateral Oblique
As an additional step when a study includes two or more views, the ImageChecker
algorithm selects up to four views and compares the images to each other in a process
known as case processing. By checking for similarities and differences between the
images, the algorithm can further refine its findings for the four selected views. When
case processing is complete, the ImageChecker algorithm compiles the results into a
single Mammography CAD SR object that includes results for the images selected for
case processing and the remaining images.
As a result of the case processing analyses, ImageChecker may produce a different set
of CAD marks for an individual image than when the image is part of a case. When
ImageChecker applies the more sophisticated case processing rules it may add or
discard marks. For example:
• Some large masses are marked only when the image is part of the bilateral
asymmetry analysis used for case processing.
• Some marks may be discarded when the image is subjected to the mark capping
limitations used for case processing). For more information, see ‘
Number of Marks
For more information about image and case processing, see ‘
Calcifications
’ and ‘3.8. Detecting Masses’.
’ in ‘3.2. RightOn CAD Marks’.
• RCC – Right Cranio-Caudal
• RMLO – Right Medio-Lateral Oblique
Limiting the
3.7. Detecting
Selecting Images for Case Processing
The ImageChecker algorithm uses the following criteria to determine which images
will be case-processed:
• If a study includes one image for each of the four screening views or their
equivalents, then all images are case-processed.
• When a study includes multiple images of the same view and laterality (e.g., two
RCC views), case processing is performed on the last image produced by the
FFDM device for each of the four screening views or their equivalents. The imageacquisition time is included in the DICOM header for each image. (Refer to the
diagram on the following page.)
• If a study does not include one or more of the four screening views, then the
equivalent views (or the reversed equivalent views) are case-processed, if they are
Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 19
Page 26

Part 2: Data Inputs and Outputs
present. Screening views are given preference over equivalent views, which in turn
are given preference over reversed equivalent views.
• The view modifiers, if present, do not affect which images are selected for case
processing.
• When a study includes multiple equivalent (or reversed equivalent) views, the
views selected for case processing are based on the following preference order:
For example, if a study includes the four screening views plus two additional RMLO
images (as is shown in the figure below), all the images are image-processed
separately. However, when selecting images for case processing, the ImageChecker
algorithm includes only the last RMLO image acquired by the FFDM device (along
with the other three screening views). As is shown below, the algorithm would select
the RMLO 3 image for case processing.
Preference
Order
1 CC MLO
2 FB ML
3 XCC LM
4 XCCL LMO
5 XCCM SIO
CC Equivalent MLO Equivalent
Acquisition Time
LMLORMLO 1 RMLO 2 RMLO 3 LCCRCC
Image
Processing
Image and Case Processing
Image plus Case
Processing
Mammography
CAD SR
As a further example, for a study with segmented breast views including multiple CC
images, you may choose to image the anterior (ductal) region of the breast last in the
sequence to ensure that that image is case-processed.
20 Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002
Page 27

2.4. CAD Outputs
The server can be configured to send results in one or more of the following formats:
•
•
•
In most facilities, results produced by the R2 Cenova server are compiled into
DICOM-conformant Mammography CAD SR objects. The Mammography CAD SR
format is the DICOM standard format for CAD results. For more information, refer
to the R2 Cenova DICOM Conformance Statement.
2.4. CAD Outputs
Mammography CAD SR 9.1 results are derived from the latest version of the
ImageChecker algorithm. The 9.1 format can provide the complete range of
Hologic | R2 features, depending upon the license options purchased by the site,
the features that are enabled, and the capabilities of the review workstation.
Mammography CAD SR 5.x provides backward compatibility with previous
releases of ImageChecker 5.x products. The 5.x format provides only RightOn Calc
and Mass Marks and PeerView Digital.
CAD Radiotherapy Structured Set (RTSS). This CAD results format was
developed specifically for GE review workstations. In earlier ImageChecker
software versions (5.x and 8.1) it was labeled ‘CAD DICOM Int’. This object
should not be stored to PACS.
Mammography CAD SR objects are most useful when viewed with the images on an
advanced workstation such as Hologic’s SecurViewdx diagnostic workstation. Most
dedicated mammography workstations display the Mammography CAD SR format as
overlays on the underlying images. With certain advanced mammography
workstations, radiologists can work with CAD results interactively.
Although some PACS do not support Mammography CAD SR, there is increasing
support for storing Mammography CAD SR objects on PACS devices. In recent years,
an increasing number of PACS workstation models have been developed that can
display Mammography CAD SR content, partly in response to the Mammography
Image Profile released by IHE (Integrating the Healthcare Enterprise).
If the results are not archived, they can be recreated at a later time if the For
Processing images have been archived. In most cases, the same results (ImageChecker
CAD marks, PeerView Digital data, etc.) should be generated each time the images
are reprocessed.
DICOM 6000 Overlays
For diagnostic review workstations and PACS devices that do not support
Mammography CAD SR or RTSS, but do support DICOM 6000 overlays, Hologic’s
DICOM 6000 Interface server can be used to convert Mammography CAD SR objects
(see ‘
Digital CAD with DICOM 6000 Overlay’ on page 15). For more information, see
the DICOM 6000 Interface User Manual, or contact your Hologic Account
Representative.
Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 21
Page 28

Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 22
Page 29

Part 3: Algorithm Description
f 3.1. ImageChecker CAD Algorithm
f
3.2. RightOn CAD Marks
f
3.3. EmphaSize Marks
f
3.4. PeerView Digital
f
3.5. LesionMetrics
f
3.6. What the Algorithm Detects
f
3.7. Detecting Calcifications
f
3.8. Detecting Masses
f
3.9. CAD Operating Points
Part 3 describes the algorithm used by the ImageChecker software when analyzing
mammography images.
3.1. ImageChecker CAD Algorithm
The ImageChecker algorithm looks for characteristics commonly associated with
cancer – specifically, calcifications and masses (including architectural distortions).
The algorithm ranks its findings by likelihood, places marks on those regions above a
fixed threshold of likelihood (operating point), and then sends the results to the
review workstation. The algorithm offers three operating points to accommodate
differing radiologist preferences. For more information, see ‘
Points
’.
3.9. CAD Operating
Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 23
Page 30

Part 3: Algorithm Description
3.2. RightOn CAD Marks
ImageChecker provides three types of CAD marks. Each mark indicates a region of
interest for the radiologist to review. There are two basic types of marks plus one
composite mark, as summarized below.
Calc – Marks regions suggestive of calcifications
Mass – Marks regions suggestive of densities/masses/architectural distortions
Malc – Composite mark indicates Calc and Mass marks occurring in the same
location on the image
Note: Not all mammography workstations can display Malc marks. Consult with your
workstation vendor concerning availability and integration of ImageChecker features with
your workstation.
Limiting the Number of Marks
The software limits or ‘caps’ the number of CAD marks for each image and case. The
actual number of CAD marks produced depends upon the individual case and the
operating point selected for the CAD algorithm.
Views Per Image Limit Per Case Limit
Screening views
(RCC, LCC, RMLO, LMLO)
Extra views
*For cases with more than four views, the maximum number of marks per case
depends upon the number of images in the case.
When ImageChecker processes an individual image, it may show a set of CAD marks
different from the marks reported when the image is part of a case. The differences
are due to the fact that ImageChecker first processes the images individually before
analyzing the case. When ImageChecker applies the more sophisticated case
processing rules (such as bilateral asymmetry analysis), it may discard marks for
regions that are less suspicious. For more information, see ‘
Processing
’.
ImageChecker CAD Marks
3 Calc marks
2 Mass marks
2 Malc marks
3 Calc marks
2 Mass marks
2 Malc marks
8 Calc marks
4 Mass marks
4 Malc marks
Dependent upon the
number of images*
2.3. and Case
Image
24 Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002
Page 31

3.3. EmphaSize Marks
EmphaSize is an optional feature that provides variable-size CAD marks that scale
according to feature significance. When the ImageChecker algorithm considers a
region to be more significant, it increases the size of the EmphaSize CAD mark. The
size of the mark does not correlate to the size of the lesion.
As the algorithm evaluates regions of interest, each region is given a ranking. This
ranking along with the selected algorithm operating point determines whether or not
the region of interest is marked with a CAD mark.
The system normally displays all CAD marks at the same size regardless of ranking. If
your site has enabled the EmphaSize feature and configured the review workstation to
use it, the ImageChecker algorithm adjusts the size of each mark according to its
ranking. The EmphaSize feature can be disabled if you do not want to use it.
3.3. EmphaSize Marks
CAD without EmphaSize CAD with EmphaSize
• Calcifications: The size of a suspected lesion is of variable significance, since small
lesions may be highly significant and large lesions may be nonactionable.
However, there are other key characteristics. For calcifications, the algorithm looks
at characteristics such as signal intensity, number of calcifications in a cluster,
shape of the calcifications (i.e., pleomorphism), and other important features to
determine lesion significance.
•
Masses: For masses, the algorithm looks at characteristics such as degree of
spiculation, lesion shape, contrast to surrounding tissue, and other important
features which help determine lesion significance.
•
Masses with Calcifications (Malc Marks): Regions containing both a mass and
calcifications are suspicious and should be carefully evaluated.
Note: Not all mammography workstations can display EmphaSize marks. Consult
with your workstation vendor concerning availability and integration of ImageChecker
features with your workstation.
Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 25
Page 32
Part 3: Algorithm Description
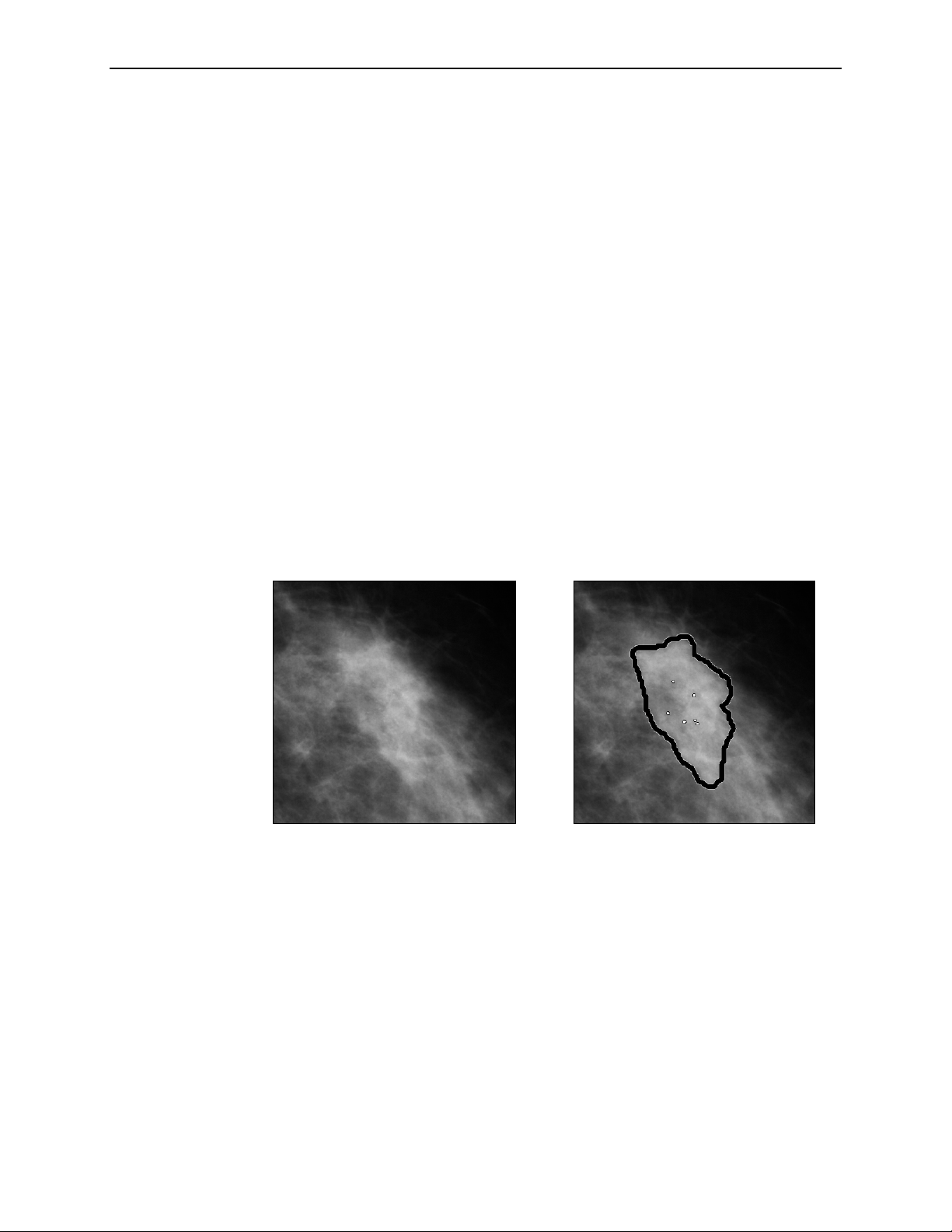
3.4. PeerView Digital
PeerView Digital is an optional, licensed feature designed to help radiologists better
understand why a region of interest was marked. When licensed, PeerView Digital
adds graphical information to the Mammography CAD SR output. At the review
workstation, the radiologist can use PeerView Digital to highlight regions of interest
detected by the ImageChecker algorithm.
•
Calcifications: PeerView Digital highlights individual calcifications in the cluster
marked by the algorithm. PeerView Digital may not highlight all calcifications in a
cluster, and it may show features suggestive of calcifications that are not
calcifications.
•
Masses: PeerView Digital defines and outlines the central density of the mass so
the radiologist can evaluate the margin, shape, and interior characteristics of the
CAD-detected mass or distortion. The outline does not generally include
spiculations associated with the mass, although the shape of the central density
may lead the eye to larger spicules.
•
Masses with Calcifications: For composite Malc marks, which indicate that one or
more Mass and Calc marks occur at the same location on the image, PeerView
Digital highlights the calcifications and outlines the central density of the mass
and/or distortion found in the CAD analysis. The same region is shown with and
without a PeerView Digital Malc mark (mass with calcifications).
Note: Not all mammography workstations can display PeerView Digital highlights.
Consult with your workstation vendor concerning availability and integration of
ImageChecker features with your workstation.
26 Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002
Page 33

3.5. LesionMetrics
3.5. LesionMetrics
LesionMetrics is an optional, licensed feature that provides data computed by the
ImageChecker algorithm for each marked region of interest marked. When licensed,
LesionMetrics are included as part of the Mammography CAD SR object for each
image processed by the algorithm. The LesionMetrics are summarized in the
following table.
LesionMetric Description Calc Mass Malc
R2 CAD Score
Number of
Calcifications
Size (long axis) Long axis in cm for the calcification cluster or mass.
Distance to Nipple*
Distance to
Chest Wall*
Calcification
Contrast (%)
Mass Density (%)
Degree of
Spiculation (%)
Operating Point
A number from 0 to 100 that reflects the prominence of the
features detected by the algorithm for the region of interest. The
higher the number the more prominent the features. The R2 CAD
Score is not linearly related to probability of malignancy.
Number of individual calcifications detected by the algorithm at
the current operating point.
The radial distance in cm from the center of the lesion to the
estimated nipple location.
The estimated perpendicular distance in cm from the center of
the lesion to the chest wall. For lesions in an upper quadrant, this
metric may resolve to the perpendicular distance to the pectoral
muscle, which can be reported as a negative value.
The average difference in brightness between the individual
calcifications and their immediate background normalized on a
scale of 0 to 100.
The average brightness of a lesion relative to its immediate
background normalized on a scale of 0 to 100.
A measurement proportional to the number of pixels that lie on
lines pointing to a common origin inside the potential lesion,
reported on a normalized scale of 0–100 containing the entire
spectrum of biopsy-proven malignant masses.
The selected operating points (algorithm thresholds) for
calcifications and masses.
*Note: The accuracy of the measurement is subject to the positioning of the patient and
other factors such as confluence of tissue and radiographic exposure. In any given image the
distance can be determined manually using the workstation measurement tool.
The LesionMetrics feature is implemented on a limited number of review
workstations. On SecurViewdx (version 6-0 or later) you can enable or disable any or
all of the LesionMetrics. Refer to your workstation’s documentation to determine
whether these features are implemented and, if they are, how to use them.
Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 27
Page 34

Part 3: Algorithm Description
3.6. What the Algorithm Detects
The ImageChecker algorithm searches an image for clusters of bright spots that are
suggestive of calcification clusters, for patterns of dense regions, and for dense regions
with radiating lines suggestive of masses or architectural distortions.
Calcifications
The algorithm marks:
• Clusters with three or more elements
• Elements that are at or within 3 mm of each other
• Where each element is at least 150 microns in size
The algorithm does not mark:
• Clusters with fewer than three elements*
• Clusters where each element is separated by more than 3 mm
• Elements it considers to be of benign morphology
• Low-contrast elements
• Lead skin markers or clips
*Note: The algorithm marks two elements if the elements have significant contrast or
shape, as defined by the cluster filter. See ‘
The algorithm occasionally marks:
• Calcified arteries
• Cluster or rim benign calcifications
• Crossing linear tissues
Calcified Artery
Benign Calcifications
To be considered a cluster, elements need only be at or within 3 mm of another
element within the cluster, as shown next:
3.7. Detecting Calcifications’.
Cluster or Rim
Crossing Linear
Tissues
≤ 3 mm square Each element is
at or within 3 mm
28 Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002
Page 35

When features in the mammogram meet the ImageChecker criteria, the algorithm
places a triangular CAD mark over the center of that region (not over a particular
element), as is shown next:
Masses/Architectural Distortions
To detect masses, the ImageChecker algorithm searches the image in a progressive
manner looking for circular, dense regions and lines radiating from a common
center. The algorithm marks:
• Regions suggestive of masses/architectural distortions
• Dense regions
• Regions with radiating lines
3.6. What the Algorithm Detects
Less pronounced radiating lines but
with a central mass
No central mass but pronounced
radiating lines
The algorithm occasionally marks:
• Ducts and tissue radiating from the nipple
• Inadvertent crossing of parenchymal tissue
• Well circumscribed masses
• Lymph nodes
• Vague opacities, skin thickening, or nipple retraction
Ducts and tissue
radiating from nipple
Inadvertent crossing of
parenchymal tissue
Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 29
Page 36

Part 3: Algorithm Description
The likelihood of a mass/architectural distortion being marked is affected by:
• Margin of the mass (the greater the spiculation, the more likely)
• Degree of density (the higher the density, the more likely)
• Presence of left/right breast asymmetry
Lobulated Ill-Defined Slightly
Spiculated
Increasing Likelihood
Low Density Medium Density High Density
Mostly
Spiculated
Spiculated
When the algorithm finds patterns associated with masses, it places an asterisk at the
point of maximum convergence on the image.
30 Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002
Page 37

3.7. Detecting Calcifications
To detect calcifications, the ImageChecker algorithm performs a series of analyses.
3.7. Detecting Calcifications
DICOM For Processing
Mammography Image
Information From Other Images
(Similarity/Asymmetry)*
*For case processing the four
screening views or their equivalents
Breast Area
Segmentation
Calcification Detection
(SIANN)
Calcification Cluster
Detection
Statistical Pattern Recognition
(Combining/Ranking)
Case Processing
Results
Mark Number
Limit Applied
Image Processing
Results
Image Processing for Calcifications
For each image, the algorithm uses two filters (artificial neural networks) to identify
calcifications and their features:
• First, it runs each image through a Shift-Invariant Neural Network (SIANN), a
calcification detection filter that has been optimized using R2 Technology’s large
training database. SIANN is a patented technology developed through more than
10 years of research at the University of Chicago.
• Then, it analyzes the resulting calcifications using a cluster filter that weights over
a dozen different features, including contrast, shape, and size.
In addition, the algorithm segments the breast and identifies the location of the
cluster within the breast.
Mammography
CAD SR
Operating Point Applied
Results Display
on Workstation
Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 31
Page 38

Part 3: Algorithm Description
Case Processing for Calcifications
In addition to processing images individually, the ImageChecker algorithm selects up
to four images that represent the screening views – RCC, LCC, RMLO, and LMLO (or
their equivalents). The algorithm reviews the findings from each image and looks for
similarities in the findings by comparing complementary orthogonal views (for
example, LMLO and LCC):
Similarity
It also looks for asymmetries between views from each side, for example, LMLO and
RMLO:
Asymmetry
The algorithm combines the results of these various analyses, analyzes the resulting
cluster and context data, and employs statistical pattern recognition against the
training database to determine the ranking for each of the possible clusters. It then
selects the Calc marks that best meet the algorithm criteria (mark capping), and
applies the selected operating point, thereby limiting the number of marked features.
Finally, if the algorithm determines that a selected Calc mark is coincident with a
Mass mark, then the marks are converted into a Malc mark.
For more information see ‘
2.3. and Case ProcessingImage ’.
32 Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002
Page 39

3.8. Detecting Masses
To detect masses, the ImageChecker algorithm performs a series of analyses.
3.8. Detecting Masses
DICOM For Processing
Mammography Image
Information From Other Images
(Similarity/Asymmetry)*
*For case processing the four
screening views or their equivalents
Breast Area
Segmentation
Mass Detection
Statistical Pattern Recognition
(Combining/Ranking)
Case Processing
Mark Number
Limit Applied
Results
Radiating Line
Detection
Image Processing
Results
Image Processing for Masses
For each image, the algorithm uses patented technology to segment the breast. It then
identifies masses by evaluating structures based on their density, shape, and margin
characteristics. It also searches for structures appearing as radiating lines, and, if they
are present, the degree of spiculation.
Mammography
CAD SR
Operating Point Applied
Results Display
on Workstation
Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 33
Page 40

Part 3: Algorithm Description
Case Processing for Masses
In addition to processing images individually, the ImageChecker algorithm selects up
to four images that represent the screening views – RCC, LCC, RMLO, and LMLO (or
their equivalents). The algorithm reviews the findings from each image and looks for
similarities in the findings by comparing complementary orthogonal views (for
example, LMLO and LCC):
Similarity
It also looks for asymmetries between views from each side, for example, LMLO and
RMLO:
Asymmetry
The algorithm then runs the resulting data against the training database to determine
the ranking for each of the possible masses. Finally, the algorithm either marks or
does not mark the masses, based on the ranking and operating point.
The algorithm combines the results of these various analyses, analyzes the resulting
cluster and context data, and employs statistical pattern recognition against the
training database to determine the ranking for each of the possible clusters. It then
selects the Calc marks that best meet the algorithm criteria (mark capping), and
applies the selected operating point, thereby limiting the number of marked features.
Finally, if the algorithm determines that a selected Mass mark is coincident with a
Calc mark, then the marks are converted into a Malc mark.
For more information see ‘
34 Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002
2.3. and Case ProcessingImage ’.
Page 41

3.9. CAD Operating Points
ImageChecker allows each site to choose between three different operating points
(i.e., CAD algorithm thresholds). You can choose a different operating point for
calcifications than for masses, which provides a total of nine options for operating
point combinations. The operating points are summarized below:
Operating point 0 trades off a lower false-mark rate for a lower overall sensitivity.
•
This operating point is suited for sites that prefer the system to display the fewest
false marks.
•
Operating point 1 represents a balanced intermediate point. Improvements in the
algorithm have allowed points 0 and 2 to be set quite far apart, and some sites may
want balanced behavior from the CAD algorithm.
•
Operating point 2 focuses on sensitivity. It gives the best performance for marking
regions of interest (i.e., CAD sensitivity), with a higher false-mark rate. It is suited
for sites that want the system to be as sensitive as possible, regardless of the higher
false-positive mark rate.
For example, if you want high sensitivity for calcifications but a moderate balance
between sensitivity and false positives for masses, choose operating point 2 for
calcifications and operating point 1 for masses.
3.9. CAD Operating Points
Each system is shipped with a default set of operating points for both masses and
calcifications. You can discuss the choices that are right for your site with your
Applications Specialist or, if you would like to change configurations, contact your
Hologic | R2 Technical Service Representative.
Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 35
Page 42

Part 3: Algorithm Description
The table below gives the sensitivity and false-mark rate values for the three operating
points for ImageChecker software version 9.1, as measured on Hologic | R2’s large
film test database of biopsy-proven malignancies and confirmed normal cases for the
four screening views (RCC, LCC, RMLO, and LMLO).
Operating Point: 0 1 2
Calcification Cases (n = 588)
Mean Sensitivity1
95% Confidence Interval
95%
93.1–96.7%
96%
94.0–97.2%
97%
95.5–98.3%
Mass Cases (n = 767)
Mean Sensitivity
95% Confidence Interval
Overall (n = 1355)
Mean Sensitivity
95% Confidence Interval
False-Positive Marks2
Calcification FP/Image
Mass FP/Image
Total False-Positive Marks/Case
Specificity2
95% Confidence Interval
1
1
83%
79.8–85.2%
88%
86.2–90.0%
0.09
0.17
1.0
48.3%
43.7–53.0%
88%
85.6–90.2%
91%
89.7–92.7%
0.12
0.25
1.5
35.1%
30.6–39.5%
90%
87.7–92.0%
93%
91.5–94.3%
0.16
0.35
2.0
24.5%
20.5–28.5%
1. ‘Sensitivity’ refers only to the sensitivity of the CAD algorithm, not to the sensitivity of the
radiologist using the device.
2. ‘False-Positive’ and ‘Specificity’ data were developed from a review of 445 confirmed
normal cases (defined as those with a subsequent normal screening study). ‘FP/Image’
refers to the average number of false-positive marks per image measured on normal cases.
‘Specificity’ refers to the percentage of normal cases that, when processed, show no CAD
marks.
Note: Earlier versions of the ImageChecker algorithm (before version 8.0) produce
slightly different performance results. For further information, see the manuals provided
with those systems.
To determine false-mark rates, Hologic | R2 processes normal screening cases (defined
as those with a subsequent normal screening study) through the ImageChecker
software and measures the number of false marks per image. More extraordinary
screening cases, such as those with additional views, and or those from diagnostic
studies, may have a very different make-up of images and, as such, may produce
results that fall outside the measured normal case mark rate. Since the mark rate is
measured per image, a larger number of images in a case should correspond on
average with a higher total mark count for that case. While clinical experience
demonstrates some variation in mark rates, Hologic | R2 has not found the false-mark
rate to vary dramatically when averaged over a large number of cases.
36 Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002
Page 43

3.9. CAD Operating Points
The following graphs shows plots of algorithm sensitivity vs. false-mark rate based on
cases with the four screening views, with data points for each of the three operating
points.
98
96
2
1
94
92
90
Algorithm Sensitivity (%)
88
86
0.0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1.0
0
False Mark Rate
(False Positives/Case)
Calcification Performance
91
90
89
88
87
1
2
86
85
84
Algorithm Sensitivity (%)
83
82
81
0.0 0.5 1.0 1.5 2.0
0
False Mark Rate
(False Positives/Case)
Mass Performance
Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 37
Page 44

Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 38
Page 45

Index
A
algorithm, ImageChecker, 11, 23–37
operating points, 35–37
what is detected by, 28
architectural distortions
what the algorithm detects, 29
with PeerView Digital, 26
C
CAD marks, 5, 10, See also
ImageChecker
archiving, 21
EmphaSize (variable-size), 3, 10
maximum number of, 24
overlapping, 26
types, 24
variable-size, 25
Calc marks, 24
maximum number of, 24
variable-size, 25
with EmphaSize, 25
with LesionMetrics, 27
with PeerView Digital, 26
calcifications, 24
analysis by algorithm, 31
case processing for, 32
image processing for, 31
what the algorithm detects, 28
case processing, 19–20
for calcifications, 32
for masses, 34
Citra Core, 9
clinical workflow, 7
customer support resources, 2
D
data flows, 13–17
DICOM, 18, 21
conformance statement, 21
image classes, 13
DICOM 6000 interface, 8, 21
in system data flow, 15
digital ports. See ports, input
DigitalNow, 16
E
EmphaSize, 25
overview, 10
precautions, 3
F
false-mark rate, 11, 35–37
FFDM systems, 7
in clinical workflow, 7
in system data flow, 13–17
models supported, 7
films, processing, 16
Fuji CRm System, 7
G
GE Medical Systems, 7, 21
H
Hologic Selenia systems, 7
I
image processing, 19–20
for calcifications, 31
for masses, 33
image specifications, 18
ImageChecker
algorithm, 23–37
benefits of, 6
case and image processing, 19–20
image specifications, 18
intended use, 1
overview, 5
overview of features, 9–11
performance specifications, 35–37
result formats, 21
supported views, 18
warnings and precautions, 3–4
implants, 18
Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002 39
Page 46

Index
precautions, 3
R
R2 CAD score, 27
L
LesionMetrics
described, 27
overview, 10
R2 Cenova server, 5
clinical workflow with, 7
in system data flow, 13–17
R2 Patient ID, 16
results
M
Malc marks, 24
identification of, 32, 34
maximum number of, 24
variable-size, 25
with EmphaSize, 25
with LesionMetrics, 27
with PeerView Digital, 26
Mammography CAD SR, 5, 8, 9, 13,
15, 19, 21, 26, 27
formats, 21
images selected for case processing,
19–20
review workstations, 5, 7
features supported by, 9
in clinical workflow, 7
in system data flow, 13–17
models supported, 8
RightOn CAD marks. See CAD marks
RTSS format, 21
mammography reporting system, 16
Mass marks, 24
maximum number of, 24
variable-size, 25
with EmphaSize, 25
with LesionMetrics, 27
with PeerView Digital, 26
masses, 24
analysis by algorithm, 33
S
screening views, 19, 36
SecurViewdx diagnostic review
workstation, 7, 14, 17, 21, 27
sensitivity, 11, 35–37
Siemens Mammomat Novation
System, 7
specificity, 11, 36
case processing for, 34
image processing for, 33
what the algorithm detects, 29
T
thresholds, algorithm. See operating
points
O
training, 2
operating points, 11, 35–37
V
P
PACS, 7, 21
in system data flow, 13–17
partial view images, 4
variable-size marks. See EmphaSize
views
CAD-supported, 18
screening, 19, 36
PeerView Digital
described, 26
overview, 10
ports, input, 7, 9
precautions, 3–4
W
warnings, 3–4
workflow, clinical, 5, 7
workstations. See FFDM systems;
review workstations
40 Understanding R2 ImageChecker 9.1 – PN MAN-00934 Rev 002
Page 47

Page 48

 Loading...
Loading...