GC EUROPE Fuji VIII GP User Manual

Which
Restorative?
A guide to the selection and use of glass
ionomer restoratives from GC.
Guide to the selection
and use of glass
ionomer technology from GC.
Restorative materials on today’s market have evolved over time offering differences in
performance, cost, ease of use, aesthetic appeal, long-term effectiveness and safety.
This means that different clinical situations call for different materials.
Which restorative
you select is important
In today’s Minimum Intervention Treatment Plan concept,
created by GC, managing patient’s mouth’s and oral cavities
over time is key. Dentistry has evolved from a purely mechanical discipline to one that takes a more medical approach.
With this in mind, the type of restorative you choose for a
particular indication is paramount as it can influence both
the long-term outcome of the clinical procedure and how
satisfied your patient is. Your choice can also impact your
practice profitability, particularly if you routinely use one
material. This is where differences in restoratives – ease
of and time to use or accessories such as bonding agents
– really come to the fore. And in some cases, you might
need to combine materials to obtain the best result.
Staying practical is key: first decide which restorative or
combination is best for the indication.
In general, it’s a good idea to fully grasp each material’s
characteristics before you choose your restorative. Next,
match these to how the material will have to perform in
specific clinical situations.
Things to carefully consider: where will the restoration
be – posterior or anterior? Where is the cavity and how
big is it? What is the patient’s risk of caries? How does it
integrate into the Minimum Intervention Treatment Plan?
Minimum
Intervention
However, suitability for the indication isn’t your only concern – you need to take the material’s other characteristics
into account. Take the ‘safe to use’ aspect. If you know your
patient is extremely sensitive to certain monomers, consider
non-resinous materials.
Choosing a material which nicely balances performance
and the cost and ease of use, may also prove critical,
particularly if you frequently perform restorations and
you need to keep an eye on patient turnover per hour. In
these situations, choosing an easy-to-use restorative that
works in a moist environment might be your best option.
GC GLASS IONOMER RESTORATIVES:
essential in every dental practice.
2
The most successful adherent system –
clinically proven!
A recent systematic review of adhesive clinical trials ranked
glass ionomer cement Number 1 in superior retention and
clinical performance over resin adhesive systems (in other
words, superior to etch and self etch, 3-step, 2-step and
1-step adhesives)*.
* Peumans M, Kanumilli P, De Munck J, Van Landuyt K, Lambrechts P, Van
Meerbeck B. Clinical effectiveness of contemporary adhesives: A systemic
review of current clinical trials. Dent Mater 2005;21:864-881.
Which Restorative
Glass ionomers are so effective as an
adhesive interface because they:
• arewater-basedcementswithauniquematrix
structure – perfect for the oral environment
• toleratemoistureduringplacement*
• chemicallybondtodentine,enamelandcementum
to create a strong, stable and chemically-fused seal
• withstandpulpaluidow(unlikeresinadhesive
systems)
• protectthesurroundingtoothstructurebyreleasing
fluoride and strontium ions
• helpstimulateinternalremineralisationwhich
releases strontium and fluoride ions, ultimately
boosting the hardening process**
• eliminatebacteriainearlystages
• achieveapositivepulpalresponsethankstogood
biocompatibility
• haveacoefcientofthermalexpansionsimilarto
dentine
* they require protection from moisture contamination
straight after placement until the initial set has been
reached.
** Remineralisation of carious dentine exposed to a
glass ionomer, an in-vivo study. Ngo H, Mount GJ, Mor-
ris M McIntyre, Tuisuva J, Von Doussa R. J Dent Res 80
(IADR Abstract no 919) 2001.”
3
The fundamentals of glass ionomer
technology
To achieve optimum clinical results, a clean, caries-free
periphery around the dentin-enamel junction will allow the
glass ionomer to help remineralise the underlying dentine.
For teeth with deep lesions and a symptomless pulp, leave
softened dentine on the cavity floor rather than risk pulpal
exposure. GC glass ionomers use strontium containing glass,
which are reported to be more effective at remineralising soft
dentine.
Condition the cavity to remove any surface debris left
after you’ve prepared the cavity. This also improves surface energy, so the glass ionomer will flow more smoothly
and adapt to the cavity floor and walls for optimum chemical adhesion. What’s more, conditioning minimises the
risk of air entrapment and voids. The polyacrylic acid in
Cavity Conditioner also prepares dentine and enamel for
chemical adhesion without opening the dentine tubules,
which rules out post-operative sensitivity. After washing
off the conditioner, gently dry to remove excess moisture
without desiccating the tooth.
The formation of a strong, chemically-fused seal: the
most significant benefit you’ll reap in using glass ionomer
as the adhesive interface with the tooth.
Reminerialisation
Hyperminerialisation
Reminerialisation
Dentine surface with smear layer intact
Dentine surface after treatment with polyacrylic
acid conditioner
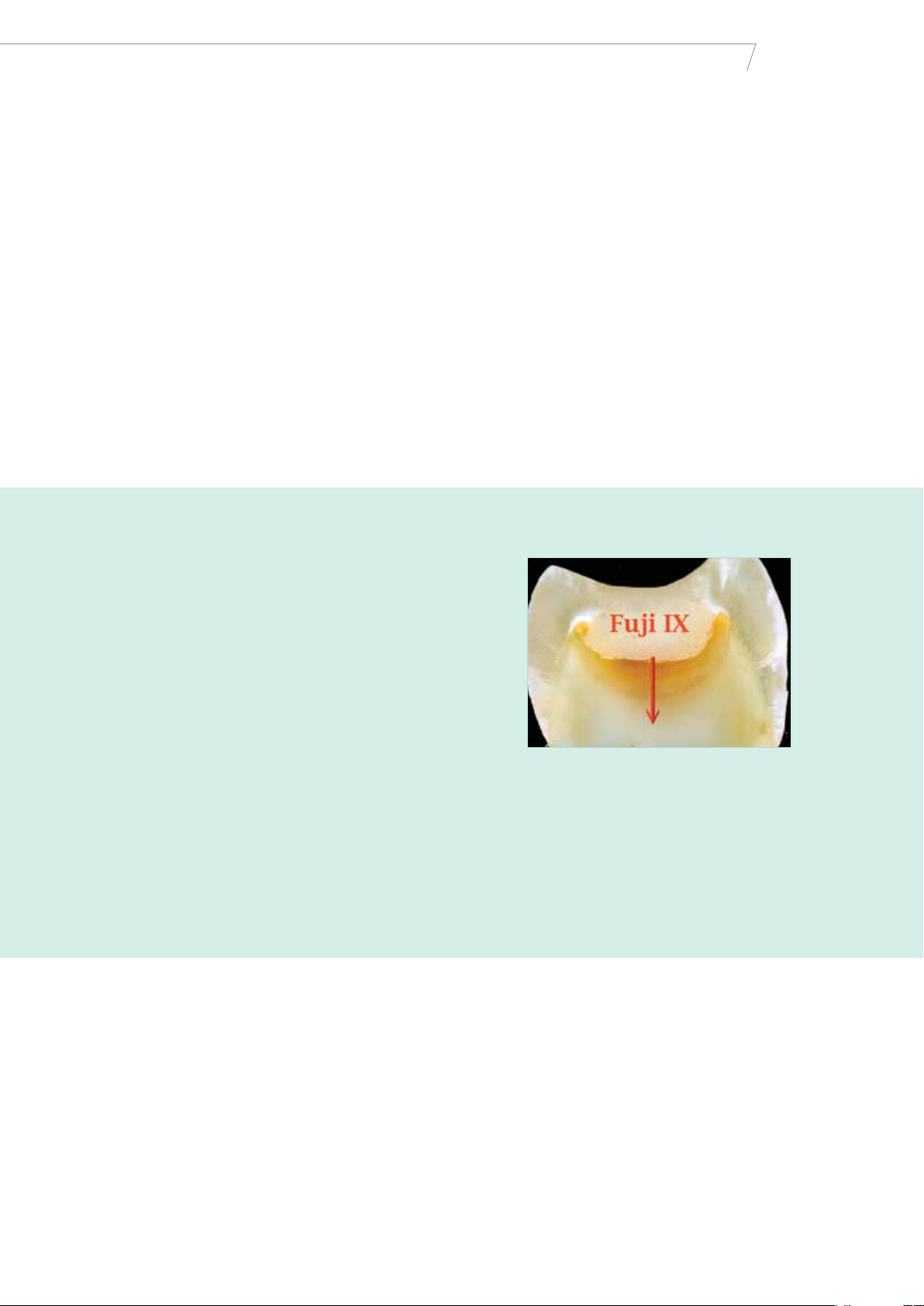
In this SEM image, the acid-resistant chemically-fused
seal appears as a raised ridge between Fuji IX GP and
dentine. The specimen was taken from a tooth which had
been restored with Fuji IX GP and subsequently extracted
for unrelated reasons nine months later. The specimen
was polished and etched for ten seconds to remove the
smear layer. Then a resin impression was taken for SEM
Dr. H. Ngo
evaluation.
4
Proof that glass ionomer restorations
greatly exceed expectations
Which Restorative
In 1995, this patient required replacement of a Class II
composite restoration. After checking the occlusion and
load-bearing factors, the operator decided to apply the
terior use: Fuji IX. Why? This new glass ionomer provided a
long-lasting seal, enduring protection and sufficient aesthetic appeal – all in one. The results speak for themselves …
world’s first high-strength glass ionomer material for pos-
1995
Prepared cavity after
conditioning
1995
Final result after fi-
nishing and polishing
1998
The same restoration
three years later
2001
The same restoration
six years later
2007
The same restoration
twelve years later
GC Fuji IX: used in more than 250 million restorations worldwide
GC’S ONGOING COMMITMENT to glass ionomer research and innovation has
driven recent developments: based on its proven glass ionomer technology.
Dr. J. Neo
Lamination strengthening
- achieving optimum maturation.
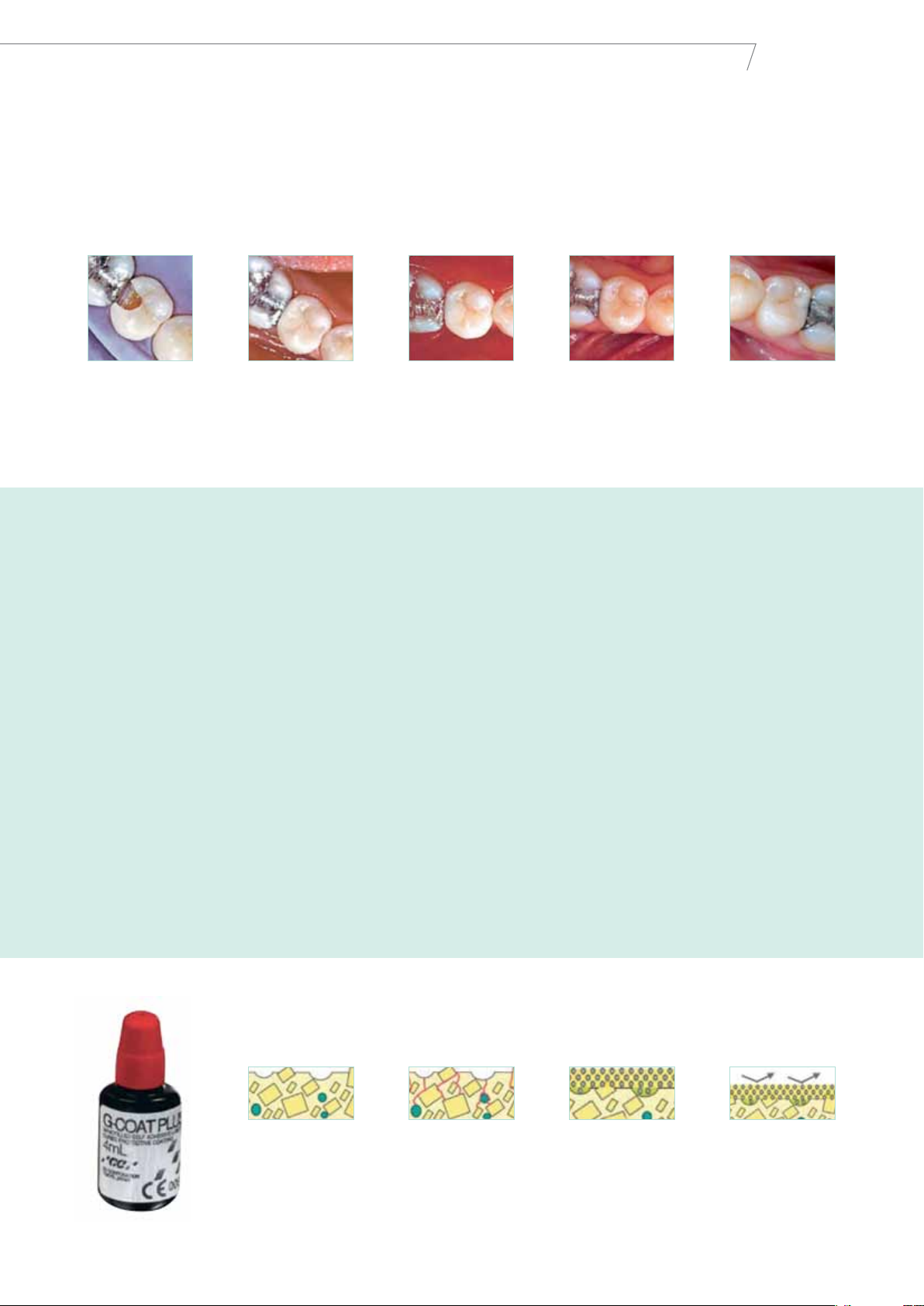
G-Coat PLUS is a tough, nanofilled, self-adhesive coating
that chemically bonds to Fuji IX GP and surrounding tooth
surfaces. When applied to glass ionomer cements, this
means that G-Coat PLUS hardens the lamination, markedly
increasing the fracture restoration toughness as well as resistance to early wear and acid.
Glass ionomer restoration gather strength in two ways:
internally and externally. Internally, the chemical reactions
mature and strengthen the cement, and externally, the
uptake of calcium and phosphate from saliva strengthens
the cement’s surface. Based on our R&D findings, you’ll
achieve the greatest improvement by coating glass ionomer restoration with a protective layer. This allows the
core of the restoration to mature and then over time allow
delayed exposure to saliva to start the surface hardening
process through uptake of calcium and phosphate. If this
is what you need to do, you’ll find no better coating material than G-Coat PLUS.
Glass ionomer
surface
Mechanical stress
concentrates on sur-
face voids leading to
crack propagation
G-Coat PLUS bonds
to the surface and fills
voids
Mechanical stress
is dispersed by the
toughened laminate
layer
5
 Loading...
Loading...