Page 1
Victoreen® 6000-529
Mammographic Ion Chamber
March 2005
Manual No. 6000-529-1 Rev. 2
©2004, 2005 Fluke Corporation, All rights reserved. Printed in U.S.A.
All product names are trademarks of their respective companies
Users Manual
Page 2

Fluke Biomedical
Radiation Management Services
6045 Cochran Road
Cleveland, Ohio 44139
440.498.2564
120 Andrews Road
Hicksville, New York 11801
516.870.0100
www.flukebiomedical.com/rms
Page 3

Table of Contents
Section 1: General Information................................................................................... 1-1
1.1 Introduction .................................................................................................. 1-1
1.2 Application ................................................................................................... 1-1
1.3 Specifications............................................................................................... 1-1
1.4 Receiving Inspection.................................................................................... 1-3
1.5 Storage ........................................................................................................ 1-3
1.6 Procedures, Warnings and Cautions ........................................................... 1-3
1.7 Installation.................................................................................................... 1-4
1.8 Electrical Interface ....................................................................................... 1-4
1.9 Setup ........................................................................................................... 1-4
Section 2: Theory of Operation................................................................................... 2-1
2.1 Theory of Operation..................................................................................... 2-1
2.2 Sample Applications .................................................................................... 2-1
Section 3: Maintenance, Calibration and Troubleshooting...................................... 3-1
3.1 Maintenance ................................................................................................ 3-1
3.2 Calibration.................................................................................................... 3-1
3.3 Troubleshooting ........................................................................................... 3-1
i
Page 4

(Blank Page)
Page 5

General Information
Introduction
1
Section 1
General Information
1.1 Introduction
The Model 6000-529 Mammographic Ion Chamber is an ion chamber especially designed to measure low
energy x
1.2 Application
The Model 6000-529 Mammographic Ion Chamber is specifically designed for measurement of exposure
rate from the output of mammographic x-ray tubes.
-ray exposure as encountered in mammography.
1.3 Specifications
Volume 3.3 cm3
Size 41 mm x 14 mm high
Window Material Polycarbonate
2
Window Thickness 9.5 mg/cm
Sensitivity 1 nC/R, nominal (0.087 nC/Gy)
Energy Dependence Within ± 5% from 0.2 mm AI HVL to 5.0 mm AI
Angular Response ± 2% for radiation incidence of up to 30° from normal
Max. Exposure Rate 13 R/min at 300 V bias for 99% collection efficiency
Accessories Custom carrying case and detachable acrylic stem
Cable Length 10 meters
Cable Termination BNC signal and banana HV or BNC Triax
Weight 128 g
1-1
Page 6

Victoreen 6000-529
V
Operators Manual
Figure 1-1. Model 6000-529 Ion Chamber (shown with handle attached)
Model 6000-529 Energy Response
(normalized to 0.3 mm AI HVL)
Response
alue Layer (mm AI)
Half-
Figure 1-2. Model 6000-529 Energy Response
1-2
Page 7

General Information
Receiving Inspection
1.4 Receiving Inspection
Upon receipt of the package:
1. Inspect the cartons (s) and contents for damage. If damage is evident, file a claim with the carrier
and notify Fluke Biomedical, Radiation Management Services at 440.248.9300.
2. Remove the contents from the packing material.
3. Verify that all items listed on the packing list have been received and are in good order.
1.5 Storage
The storage requirements for this instrument are listed below.
1. The instrument shall be stored in a cool, dry location.
2. If the instrument is taken from its current location and is to be placed in a new location with a
different ambient temperature, allow the instrument to reach the new location’s ambient
temperature before applying power.
1.6 Procedures, Warnings and Cautions
1
The equipment described in this manual is intended to be used for the detection and measurement of
ionizing radiation. It should be used only by persons who have been trained in the proper interpretation of
its readings and the appropriate safety procedures to be followed in the presence of ionizing radiation.
Although the equipment described in this manual is designed and manufactured in compliance with all
applicable safety standards, certain hazards are inherent in the use of electronic and radiometric
equipment.
Warnings and Cautions are presented throughout this document to alert the user to potentially
hazardous situations. A Warning is a precautionary message preceding an operation that has the
potential to cause personal injury or death. A Caution is a precautionary message preceding an operation
that has the potential to cause permanent damage to the equipment and/or loss of data. Failure to comply
with Warnings and Cautions is at the user's own risk and is sufficient cause to terminate the warranty
agreement between Fluke Biomedical, Radiation Management Services and the customer.
Adequate warnings are included in this manual and on the product itself to cover hazards that may be
encountered in normal use and servicing of this equipment. No other procedures are warranted by Fluke
Biomedical. It shall be the owner's or user's responsibility to see to it that the procedures described here
are meticulously followed, and especially that Warnings and cautions are heeded. Failure on the part of
the owner or user in any way to follow the prescribed procedures shall absolve Fluke Biomedical and its
agents from any resulting liability.
Indicated battery and other operational tests must be performed prior to each use to assure that the
instrument is functioning properly. If applicable, failure to conduct periodic performance tests in
accordance with ANSI N323-1978 (R1983) Radiation Protection Instrumentation Test and Calibration,
paragraphs 4.6 and 5.4, and to keep records thereof in accordance with paragraph 4.5 of the same
standard, could result in erroneous readings or potential danger. ANSI N323-1978 becomes, by this
reference, a part of this operating procedure.
1-3
Page 8

Victoreen 6000-529
Operators Manual
1.7 Installation
CAUTION
Ensure all power is removed prior to installing the
Model 6000-529 Ion Chamber.
Installation of the Model 6000-529 consists of connecting the ion chamber to a Model 4000M+, 4000+,
6000B, 6000M, RAD-CHECK® Plus, or any medical grade electrometer.
The Model 6000-529 may also be used with the Model 6000-531 preamplifier for interfacing with the 4000
or 6000 series of instruments. Refer to the 6000-531 manual for interface details.
A handle is also included with the ion chamber for supporting the ion chamber for in-air measurements.
1.8 Electrical Interface
Final electrical interface connections between the preamplifier, the Ion Chamber, and the host instrument
are listed in Table 2-1.
Table 2-1. Electrical Interface Connections
Connector Description
BNC Ion Chamber Output
HV (BIAS) Ion Chamber High Voltage
1.9 Setup
Because the Model 6000-529 Ion Chamber may be used with many commercially available electrometers
and dosimeters, please refer to the applicable instrument manual for set up and calibration.
1-4
Page 9

Theory of Operation
Theory of Operation
2
Section 2
Theory of Operation
2.1 Theory of Operation
An ionization chamber consists of a defined volume of air in which ions produced by radiation passing
through the chamber can be collected and measured. The Model 6000-529 is a parallel plate ion
chamber, consisting of a guarded center electrode placed near a conductive plate that serves as a
window as well as an electrode. A potential difference in the range of approximately 200 - 300 volts is
placed across the plates of the ion chamber (the high voltage applied to the ion chamber will depend on
the host instrument used). When ionizing radiation passes through the chamber, ion pairs are produced,
each pair consisting of one positive and one negative ion. Under the influence of the electric field
produced by the potential between the plates, the ions move toward their oppositely charged plate. Upon
arrival, they are neutralized by the free charges on the plates, taking an electron from the negative plate
and adding an electron to the positive plate. This causes a current to flow through the external electronics
connected to the plates, the magnitude of which is proportional to the rate of exposure to radiation.
The sensitivity of an ion chamber depends on the number of air molecules in the chamber, in fact these
quantities are directly proportional. The number of molecules is a function of volume, temperature, and
pressure. The volume of air in the chamber is fixed, but since it communicates with the atmosphere,
temperature and pressure will vary. The chambers are calibrated at Fluke Biomedical at a temperature of
22°C and a pressure of 760 mmHg. A correction factor should be applied to the reading given by the ion
chamber, based on the ambient temperature and barometric pressure at the time the measurement is
made. For diagnostic x-ray use, this is usually unnecessary since the errors are on the order of 0.3% per
degree Celsius and 0.1% per mmHg. However, if you are using the 6000-529 at an elevation greatly
different than sea level, the error could be significant. The correction factor is calculated by the following
expression:
760 T +
cf =
P
Where T is the temperature in degrees Celsius and P is the pressure in mmHg.
x
273.16
295.16
2.2 Sample Applications
Beam Quality Measurements
Beam quality is an indication of the penetrating ability of diagnostic x-rays. The quantity being measured
is the half-value layer (HVL) and is reported is units of millimeters of aluminum. The HVL is defined as the
thickness of an absorbing material (aluminum in this case) required to reduce the intensity of the x-ray
beam to one half its unattenuated intensity. Also, by definition of the HVL, radiation scatted by the
absorber must not be included in the measurement, thereby necessitating care to be taken in setting up
the measurement geometry.
To perform a beam quality measurement, one makes several exposure (or air kerma) measurements with
the Model 6000-529 ionization chamber, while increasing the thickness of an absorbing material from
zero to a sufficient quantity to reduce the reading to less than one half the reading measured with no
absorber. A logarithmic interpolation formula is then used to interpolate between the measurement made
2-1
Page 10

Victoreen 6000-529
Operators Manual
with enough aluminum to give a reading just below one-half the unattenuated reading and that made with
aluminum to give a reading just greater than one-half the unattenuated reading.
When making beam quality measurements at mammographic energies, it is recommended that you use
99% pure aluminum. Alloy 1100 aluminum has been used, however studies show that an error as great
as 7.5% may result.
To perform a beam quality test, follow these steps:
1. Raise the compression paddle to its highest position. Mount the 6000-529 ionization chamber on a
ring stand so there is approximately 5 cm of space between the bottom of the chamber and table.
The chamber should be centered in the beam laterally, and approximately 4 cm from the chest wall.
2. Collimate the beam, using the light field, so that the entire chamber is included in the beam. The
field should be approximately 6 cm x 6 cm. If necessary, relocate the chamber such that it is
centered in the field.
3. Set the kVp selector at a kVp setting that is frequently used for making mammograms. Set manual
timing, and set the mAs to provide an exposure reading of at least 500 mR. Refer to the instruction
manual for the electrometer or other instrument used to measure charge generated in the 6000-529
chamber.
4. Make an exposure. Note the reading and label it X
. If you are using an electrometer that reads in
0
nC or some other instrument that would normally require the application of a correction factor, you
may note the raw reading without corrections. This is so because all subsequent readings are
normalized to X
.
0
5. Place a sheet of aluminum 0.2 mm thick on the compression paddle. Using the collimator light, be
sure the entire ionization chamber is in the shadow of the aluminum sheet. Make an exposure.
Record the reading and label it X
exposure. Label it t
.
1
; also record the thickness of aluminum used to make the
1
6. Place an additional 0.01 mm of aluminum on top of the aluminum absorber(s) already in place.
Make an exposure. Record the reading, labeling it with sequential indices. Also, record the total
thickness of aluminum used in making the measurement, labeling it as t
number of filtered exposures taken so far. If X
is less than one half of X0 proceed to step 7,
N
where N is the total
N
otherwise, repeat step 6.
7. It is now assumed that you have compiled a list of data pairs, labeled "t
" and "Xi"- If N is the total
i
number of filtered exposures, then the half-value layer may then be calculated using the following
formula:
It is recommended that the HVL be in the following range:
If your calculated HVL is lower than this range, you may be in violation of Federal or State regulation. For
more information, see American College of Radiology Medical Physicist's Manual.
2-2
Page 11

Theory of Operation
Sample Applications
2
Measuring Breast Entrance Exposure and Mean Glandular Dose
Breast entrance exposure is the radiation exposure that would be measured at the point of radiation entry
to the breast, free-in-air with the breast removed from the beam. Mean glandular dose is the dose to
glandular tissue in a typical 50-50 adipose-glandular composition breast, compressed to a thickness of
4.5 cm, and averaged over the extent of the glandular tissue.
To measure entrance exposure, follow these recommended steps:
1. Set up the x-ray machine for a typical mammographic technique. Place a loaded cassette in the
cassette holder, of the size and type consistent with the examination being simulated. Set the
machine in the AEC mode and set the density control to the position most commonly used for the
examination.
2. Place a mammographic phantom on the cassette holder assembly at the position normally
occupied by the breast. Be sure the phantom completely covers the AEC sensor. Now, place the
Model 6000-529 ionization chamber just to the side of the phantom. The entrance window of the ion
chamber should be flush with the top of the phantom, and the chamber should be placed as close
as possible to the chest wall edge of the x-ray field being sure that the entire chamber is in the field
and that it does not shadow the AEC sensor. Now, lower the compression paddle until it contacts
the phantom and chamber. Take care not to put any mechanical stress on the chamber.
3. Connect the chamber cable to an electrometer, NERO, 4000M+ or other charge-measuring
instrument. Follow the instructions accompanying the instrument for details of instrument operation.
4. Make an exposure. Record the reading from the electrometer or other instrument. Apply whatever
corrections are necessary to yield an accurate exposure reading. If you are using the Model 6000531 preamplifier, and have set it up according to the instructions, the only correction that may be
necessary would be air density correction (see section page 2-1). If you are using a charge-reading
electrometer, you should multiply the electrometer reading (in nanocoulombs) by the calibration
factor (in Roentgens per nanocoulombs) listed on the calibration report that accompanied the
chamber. Record the result.
5. Repeat step 4 three more times. Average all four results. The final result is the breast entrance
exposure. You should now repeat the procedure for all other clinically used techniques.
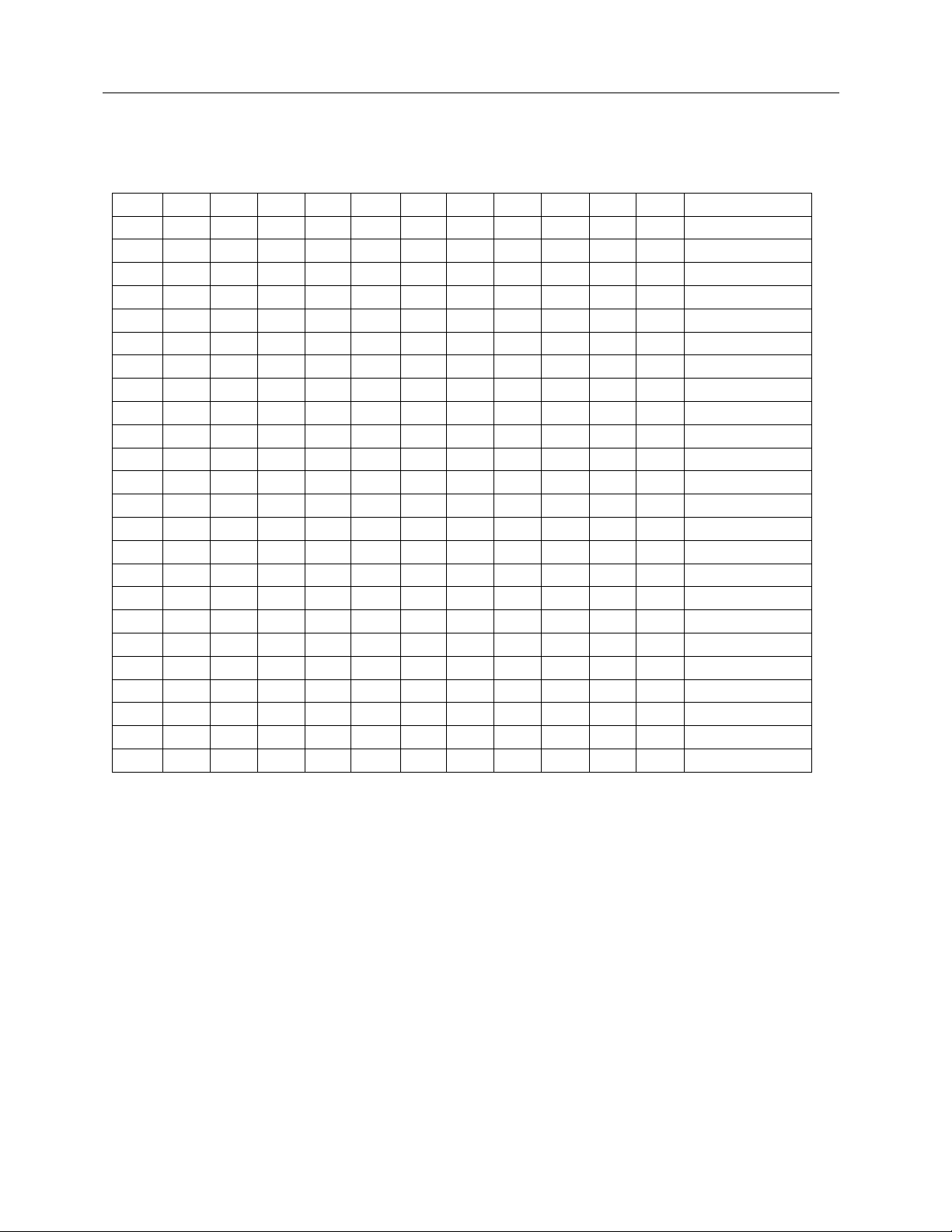
6. To compute mean glandular dose, refer to Table 2-1. In the column labeled "HVL", locate the value
closest to the half-value-layer you measured in step 4 for the kVp setting used in making the
entrance exposure measurement. Now, for Mo/Mo tubes, find the column labeled by the same kVp.
Alternatively for W/AI tubes, locate the column labeled “W/AI." The number located at the
intersection of the column thus located and the row designated by the proper HVL should be noted.
This number, when multiplied by the entrance exposure in Roentgens will give mean glandular
dose in millirads.
2-3
Page 12
Victoreen 6000-529
Operators Manual
Table 4-1. Glandular Dose for 4.5 cm Breast Thickness - 50% Adipose/50% Glandular
Breast Tissue (in mrad/R)
Mo/Mo Target-Filter X-Ray Tube Voltage (kVp)
HVL 23 24 25 26 27 28 29 30 31 32 33 W/AI Target-Filter
Combination
0.23 109
0.24 113 116
0.25 117 120 122
0.26 121 124 126 128
0.27 126 128 130 132 134
0.28 130 132 134 136 138 139
0.29 135 137 139 141 142 143 144
0.30 139 141 143 145 146 147 148 149 170
0.31 144 146 147 149 150 151 152 153 154 175
0.32 148 150 151 153 154 155 156 158 159 160 160 180
0.33 153 154 155 157 158 159 160 162 163 164 164 185
0.34 157 159 160 161 162 163 164 166 167 168 168 190
0.35 163 164 166 167 168 169 170 171 172 172 194
0.36 168 170 171 172 173 174 175 176 176 199
0.37 174 175 176 177 178 178 179 180 204
0.38 179 180 181 182 182 183 184 208
0.39 184 185 186 186 187 188 213
0.40 189 190 191 192 192 217
0.41 194 195 196 196 221
0.42 200 200 225
0.43 204 230
0.44 234
0.45 238
2-4
Page 13
Maintenance, Calibration and Troubleshooting
Maintenance
Section 3
Maintenance, Calibration and Troubleshooting
3.1 Maintenance
The Model 6000-529 Ion Chamber requires no routine maintenance, other than routine inspection of the
chamber for damage.
3.2 Calibration
The Model 6000-529 Ion Chamber is accompanied by the chamber's sensitivity on the calibration report.
If this report is not available, the ion chamber may be returned to Fluke Biomedical so that a new
sensitivity factor may be obtained, or by the customer by intercomparison with a know ion chamber.
3
Obtain the value of chamber sensitivity in
dimensions of exposure per unit charge or air
Kerma per unit charge (see the calibration report
which accompanied the chamber), and the charge
calibration factor for the host instrument in
dimensions of charge per displayed exposure unit,
prior to referring to the applicable preamplifier
manual.
NOTE
3.3 Troubleshooting
Extreme care must be used when troubleshooting a
system that has power applied. All standard
troubleshooting precautions apply.
Once a problem has been located, remove all
power before continuing with the repair.
Personnel performing the troubleshooting must be
familiar with the operation of the system and the
location of each piece of equipment used.
Troubleshooting consists of checking the wiring and verifying inputs/outputs are present on all
connectors. If a problem develops with the Ion Chamber, return the chamber to Fluke Biomedical.
WARNING
WARNING
CAUTION
3-1
Page 14

Victoreen 6000-529
Operators Manual
NOTE
If a problem cannot be resolved by applying the
troubleshooting procedures described above,
contact Fluke Biomedical at 440.248.9300 for
assistance.
3-2
Page 15

(Blank Page)
Page 16

Fluke Biomedical
Radiation Management Services
6045 Cochran Road
Cleveland, Ohio 44139
440.498.2564
120 Andrews Road
Hicksville, New York 11801
516.870.0100
www.flukebiomedical.com/rms
 Loading...
Loading...