Page 1

Reference Manual
Model TAT-5000
Accuracy supported by more than 50 peer-reviewed
published studies for all ages from neonate to geriatric, and
in all clinical settings. Contact medical@exergen.com.
U.S.A. and Canada
EXERGEN
TemporalScanner™
A Kinder, gentler way to take temperature
Visit www.exergen.com/ww
Page 2

Page 3

Important Safety Instructions
READ ALL INSTRUCTIONS BEFORE USING
1
SAVE THESE INSTRUCTIONS.
When using the product, basic safety precautions should always be followed, including the following:
● Use this product only for its intended use as described in this manual.
● Do not take temperature over scar tissue, open sores or abrasions.
● The operating environmental temperature range for this product is 60° to 104°F (15.5° to 40° C).
● Always store and transport this thermometer in a clean, dry place where it will not become
excessively cold (-4°F/-20°C), or hot (122°F/50°C). Relative humidity 93% maximum,
non-condensing. Atmospheric pressure 50 kpa to 106 kpa.
● The thermometer is not shockproof. Do not drop it or expose it to electrical shocks.
● Do not autoclave. Please note cleaning and sterilizing procedures in this manual.
● Do not use this thermometer if it is not working properly, if it has been exposed to temperature
extremes, damaged, been subject to electrical shocks or immersed in water.
● There are no parts that you can service yourself except for the battery, which you should replace
when low by following the instructions in this manual. For service, repair, or adjustments, return
your thermometer to Exergen. WARNING: No modications of this equipment are allowed.
● Never drop or insert any object into any opening.
● If your thermometer is not used regularly, remove the battery to prevent possible damage due to
chemical leakage.
● Follow the battery manufacturer’s recommendations or your hospital policy for the disposal of
used batteries.
● Not suitable for use in the presence of ammable anaesthetic mixtures.
● If you have any additional questions regarding use or care of the thermometer, please see
www.exergen.com or call Customer Service at (617) 923-9900.
● Mode of Operation: Intermittent operation.
Page 4
2
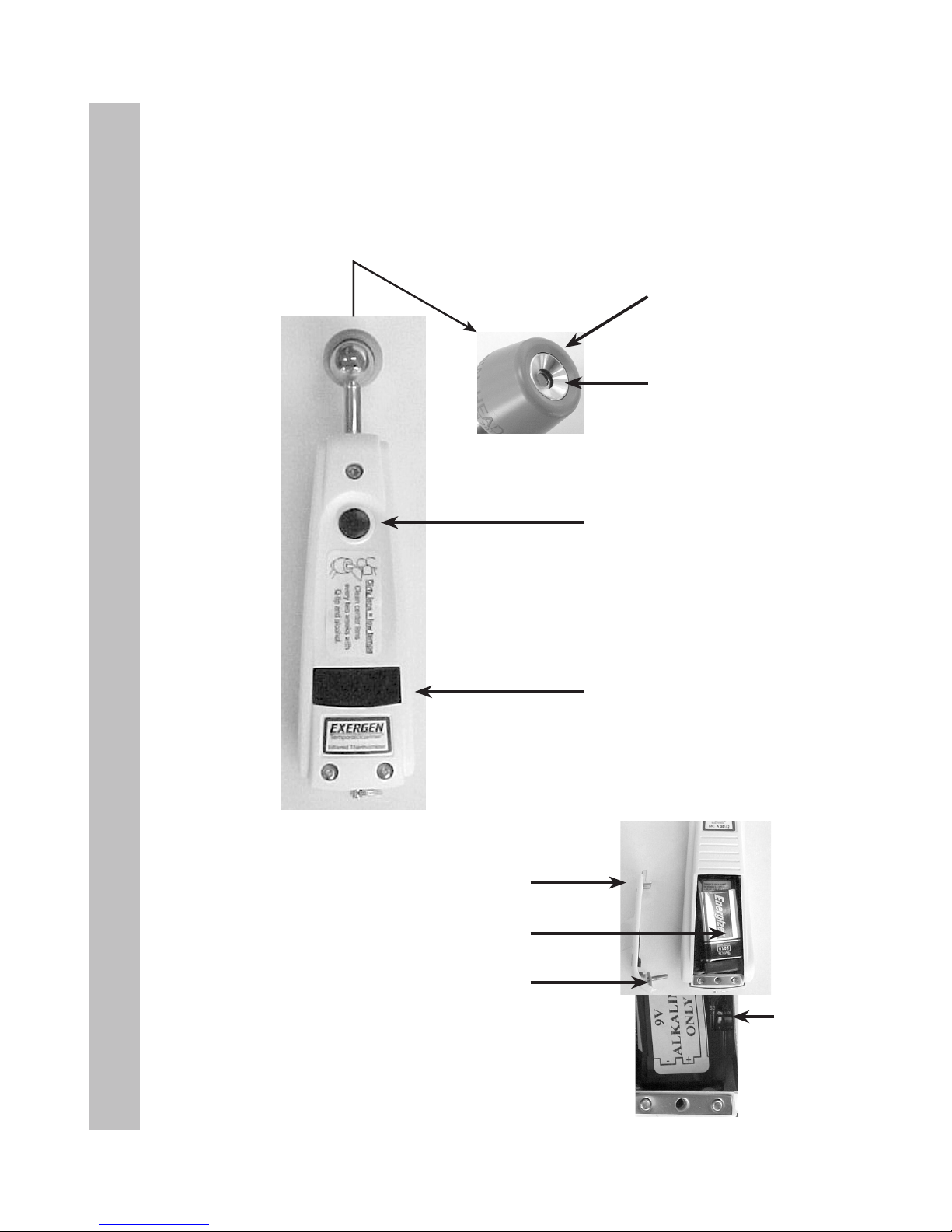
Product Map
Product Map
Probe Cone
Probe Lens
ON Button
Automatic turn-off in
30 seconds (when
measuring in body
temperature range,
otherwise 5 seconds).
LED Display Screen
Battery Compartment
9-Volt Battery
Battery Compartment Door
Compartment Door Screw
F/C Switch
Page 5
3
Introduction
Introduction to Temporal Artery Thermometry
The Method
Temporal artery thermometry (TAT) is a completely new method of temperature
assessment, using infrared technology to detect the heat naturally emitting from
the skin surface. In addition, and of key importance, the method incorporates a
patented arterial heat balance system to automatically account for the effects of
ambient temperature on the skin.
This method of temperature assessment has been shown to improve results and
reduce costs by non-invasively measuring body temperature with a degree of
clinical accuracy unachievable with any other thermometry method. The temporal
scanner is a type BF device.
Temperatures are more reliable than with other methods. Fevers are identied
sooner. Treatment can be initiated sooner. We trust you will nd temporal
artery thermometry is simply a better method.
Why the Temporal Artery
The TAT method was developed in response to the clinical requirements for a
truly non-invasive, accurate method of thermometry. Oral thermometry is
subject to many artifactual errors; rectal temperature meets with strong
resistance from patients, parents, and even many clinicians. Ear thermometers,
although convenient, are sensitive to technique. Some brands are known to miss
fevers, and it’s difcult to consider the use of an aural thermometer when 95% of
pediatric visits concern ear infections.
A site for detecting fevers with roots dating back to centuries before Christ, the
temporal artery demonstrated the necessary requirements to meet the stringent
demands of clinical medicine today: it is easily accessible, contains no mucous
membranes, and notably, maintains a relatively constant perfusion rate, ensuring
the stability of blood ow required for the measurement method.
As a site for temperature measurement, the temporal artery presents many
benets: it poses no risk of injury for patient or clinician, eliminates any need for
disrobing or unbundling, and is suitable for all ages.
Page 6

4
Table of Contents
Table of Contents
Page(s)
Important Safety Instructions 1
Product Map 2
Introduction to Temporal Artery Themometry 3
Familiarize Yourself with the TemporalScanner 5-6
Using the Instrument 7
Using the Instrument on a New Mother 8
Using the Instrument on an Infant 9
Frequently Asked Questions 10-13
Disposable Cover Options 13
Accessories 13
Guidelines for Patient Temperature Assessment 14-15
Comparing with other methods of thermometry
Determining a Fever Threshold 16
Body Sites for Temperature Assessment 17-18
An overview of temperature measuring sites
Reproducibility in Temperature Measurement 19
Forgotten Physiology 20-21
For Kids Only 22
Care and Maintenance of the Instrument 23-25
Page 7
5
Familiarize Yourself with the Instrument
Before Using, Familiarize Yourself with the Instrument
The Scan
One of the most important features of the thermometer is its ability to scan. It is a
patented feature of the instrument. Scanning is critical in obtaining the correct
temperature, since there are temperature gradients present not only inside the body,
but across the entire surface of the body.
The object of scanning is to capture the highest temperature, the peak, in the area
being scanned. As long as the button is depressed, the thermometer will be
continually sampling and recording the highest temperature it measures.
Test it rst on your hand to get comfortable with the concept.
Depress the red button, and keep it depressed. Scan the probe over the center area
of your palm, keeping the probe about a half an inch off the surface to avoid cooling
the skin. The display will ash SCAN, and there will be a soft but rapid clicking sound
each time the sensor detects a temperature higher than the one before. When the
ashing and clicking slow to a little less than 1 per second, the peak temperature
has been reached. Any of the above indications can be used to assure the peak
temperature has been reached.
Remove the instrument from your palm and release the button and note the reading
on the display.
The reading will be locked on the display for 30 seconds unless you press the button
before that time. Repeat the above steps and you should get the same, or very close
to the same number, since your hand will usually not appreciably change temperature
very quickly.
• To Scan: Depress the red button. The instrument will continually scan for the
highest temperature (peak) as long as the button is depressed.
• Clicking: Each fast click indicates a rise to a higher temperature, similar to a
radar detector. Slow clicking indicates that the instrument is still scanning, but not
nding any higher temperature.
• To Retain or Lock Reading: The reading will remain on the display for 30
seconds after the button is released. If measuring room temperature, the
temperature will remain on the display for only 5 seconds.
• To Restart: Depress the button to restart. It is not necessary to wait until the
display is clear, the thermometer will immediately begin a new scan each time the
button is depressed.
• Pulse Timer: The thermometer has a built-in pulse timer. To activate, you should
touch something >90°F (32°C) (skin), press the red button once and release. The
display will remain on for 30 seconds.
Page 8

6
Familiarize Yourself with the Instrument
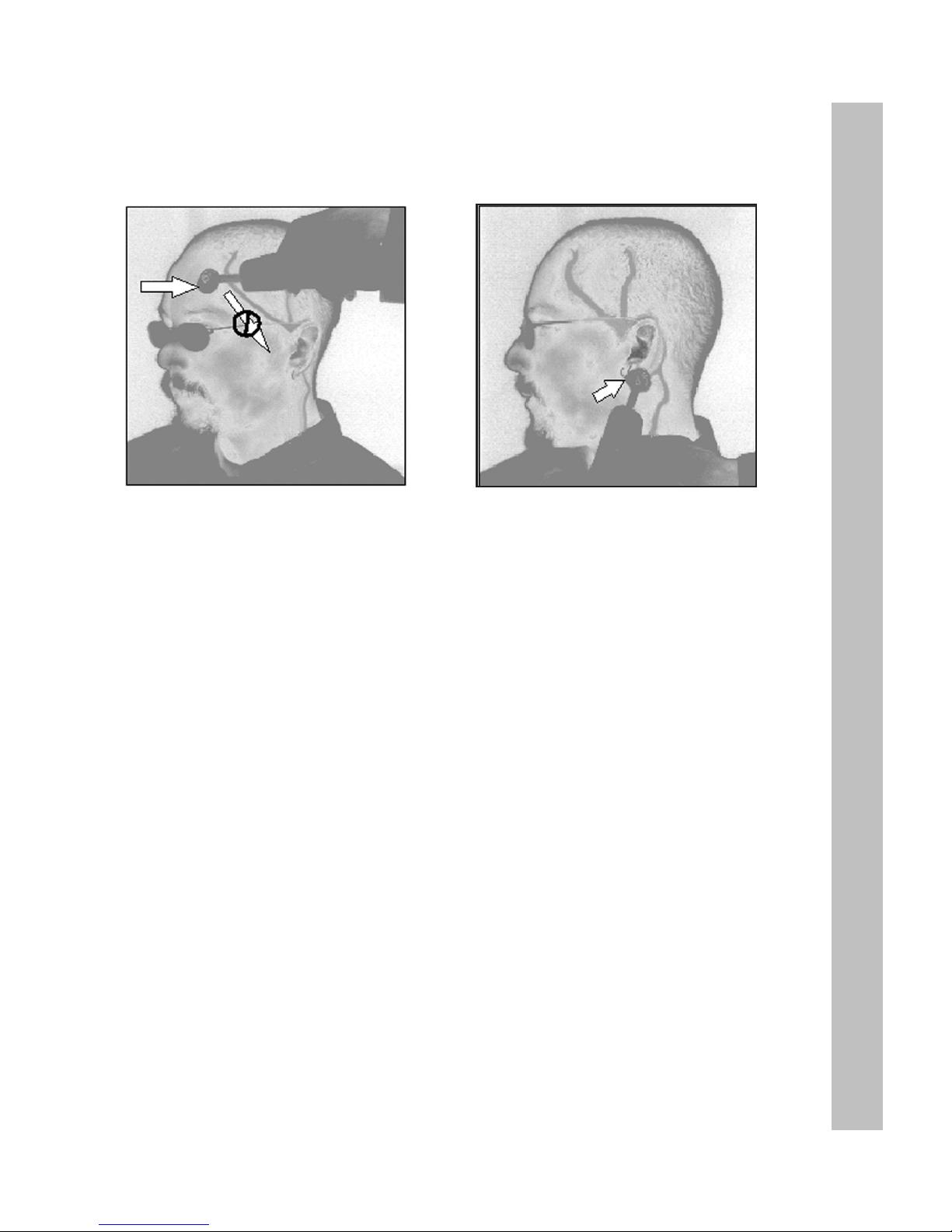
Practice Holding Your TemporalScanner
The TemporalScanner is ergonomically designed specically for
its application. It’s best to hold the instrument with your thumb
on the red button, much like you would hold a remote control.
Along with allowing you to easily read the temperature display,
you will automatically be using nger dexterity to gently position
the probe, providing comfort and safety for your patient, and
consistently accurate temperature readings.
Things to Know Before Taking Temperatures
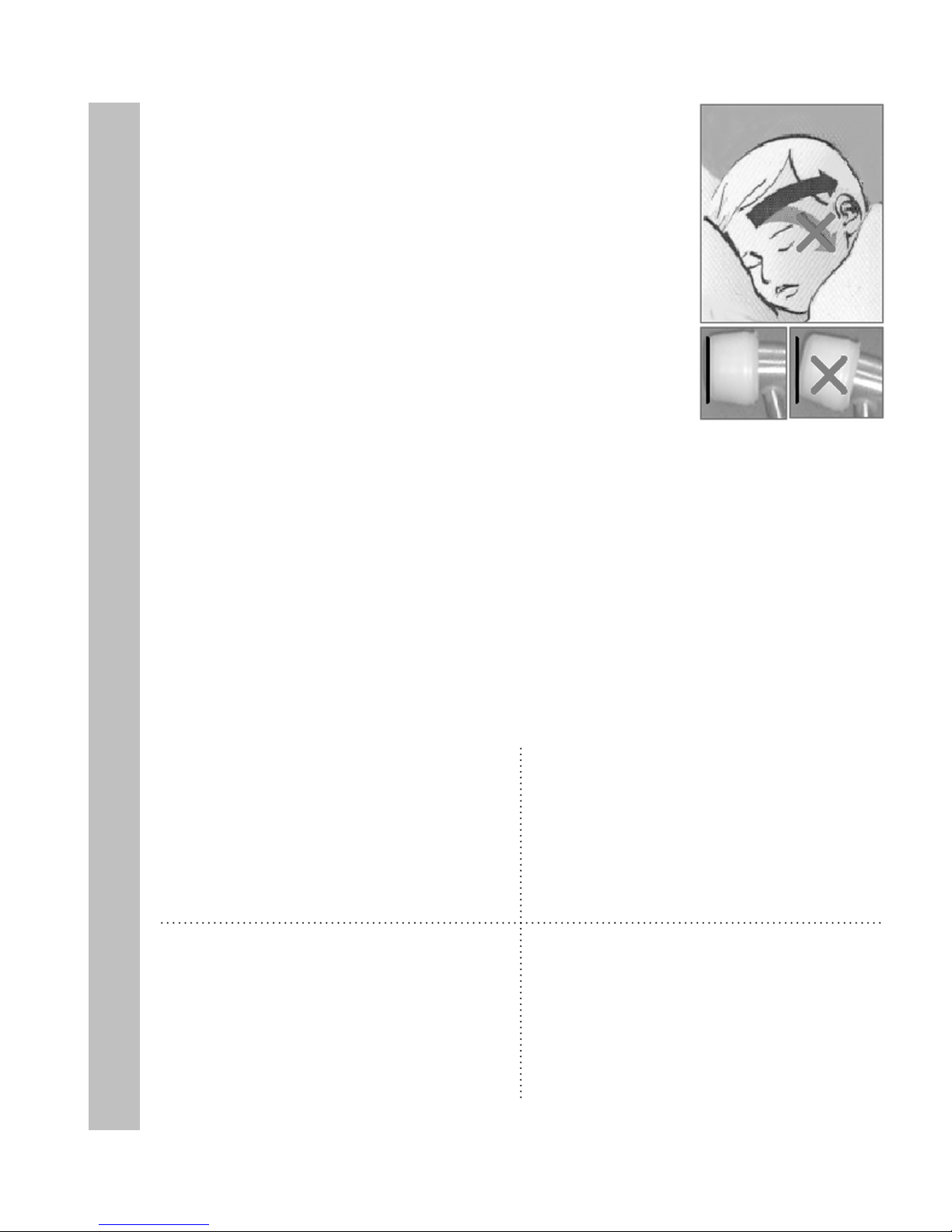
• Measure only the exposed side. Anything covering the area
to be measured would insulate it and prevent the heat from
dissipating, resulting in falsely high readings. Brush hair
aside if covering the TA, or the area behind the ear.
• Slide the thermometer straight across the forehead (midline),
and not down the side of the face. Midline over the TA area,
the TA is less than 2mm below skin surface, whereas as the
TA winds down the side of the face, it is further from the skin
surface. Although anatomically correct, sliding downwards
would result in falsely low readings.
• It is preferable to hold the instrument sideways, as illustrated
in Figure 2. Approaching your patient with the instrument
straight up and down could be somewhat intimidating.
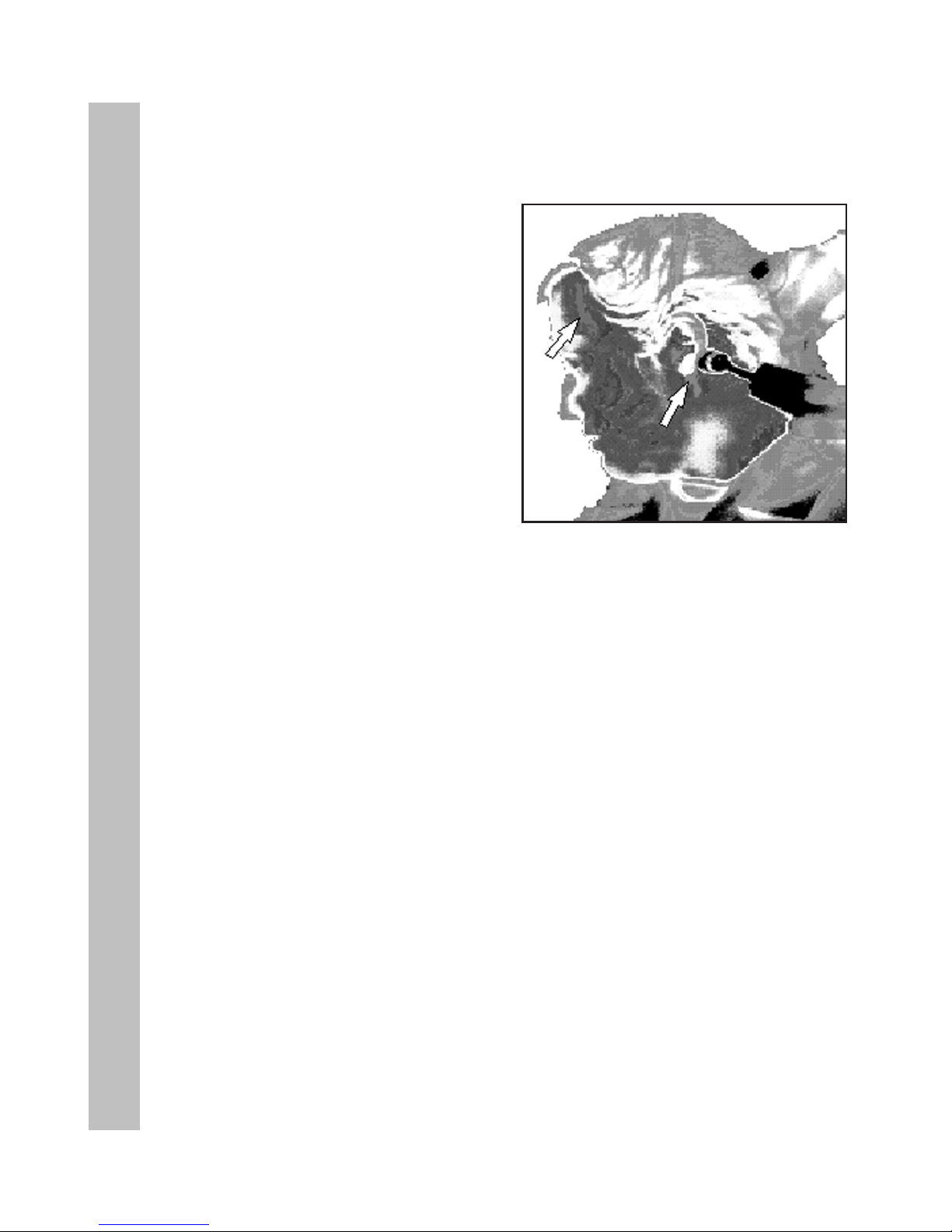
• When making the measurement behind the ear as in Figure 3,
tuck the thermometer under the ear lobe in the soft conical
depression on the neck just below the mastoid. This is the
place where a dab of perfume is typically applied.
Using on an Infant
An infant is apt to present bundled, with blankets and clothing
covering the neck area. Fortunately, the perfusion rate is
normally strong for infants, and unless visibly diaphoretic, one
measurement at the TA is typically all that is required.
Should you feel the temperature is low, then push aside any
clothing or blankets covering the neck area for ~30 seconds or
so, and repeat the measurement behind the ear.
1
2
3
4
Page 9
7
Using the TemporalScanner
Basics of Using the TemporalScanner
Measure only the exposed side.
Brush hair aside if covering the
TA area.
Brush hair away if covering ear.
1. With probe ush on the center of the forehead, depress red button,
keep depressed...
2. Slowly slide probe midline across forehead to the hair line, not down
side of face.
3. Lift probe from forehead and touch on the neck just behind the ear lobe.
4. Release the button, read, and record temperature.
Alternate sites when TA or BE are unavailable:
• Femoral artery: slowly slide the probe across groin.
• Lateral thoracic artery: slowly scan side-to-side in the area ~midway between
the axilla and the nipple.
• Axilla: insert probe in apex of axilla for 2-3 seconds.
Questions? Please call us at 800-422-3006
Page 10
8
Using the TemporalScanner on a New Mother
Using the TemporalScanner on a New Mother
• Measure exposed skin
• Keep the red button
depressed throughout
measurement
(Brush bangs aside if present)
1. With probe ush on the center of the forehead, depress red button.
2. Slowly slide probe across forehead to the hair line.
3. Lift probe from forehead.
Questions? Please call us at 800-422-3006
(Brush hair away if covering ear)
4. Touch probe to neck just behind the ear lobe.
5. Release button, read, and record temperature.
• Temperature will remain on display for 30 seconds after the
red button is released.
• Sequence can be restarted at any time without waiting for
display to clear.
Page 11

9
Using the TemporalScanner on an Infant
Temping Baby in Bassinette, Open Crib, or with Mom
Preferred site is the temporal
artery area. In this case, behind the
ear could be alternate site, as both
are exposed.
Questions? Please call us at 800-422-3006
• Instrument should be in same temperature environment as the baby for
approximately 20 minutes.
• Measurement site must be exposed.
• One measurement, preferably at the TA, is all that is required.
Temporal artery area is the only
option in this case, as the neck area
is not exposed.
Temperature at the Temporal Artery Area
1. Gently touch probe to center of forehead.
♥ Depress red button and keep depressed.
2. Slide probe over the TA area into hairline.
♥ If more convenient, slide from hairline towards center of forehead.
3. Release button, remove from head, and record.
Temperature Behind the Ear
1. Gently nestle probe on neck behind the ear.
♥ Depress red button and keep depressed.
2. Maintain skin contact until numbers stop.
3. Release button, remove from head, and record.
Preferred
Site
Preferred
Site
Page 12
10
Frequently Asked Questions
Frequently Asked Questions
What is the TemporalScanner?
The TemporalScanner is an infrared thermometer designed for accurate,
completely non-invasive temperature assessment by scanning the temporal artery
(TA). It is breakthrough technology.
How does it work?
Temperature is measured by gently stroking the TemporalScanner across the
forehead, and includes a momentary touch of the probe to the neck area behind
the ear lobe, to account for any cooling of the forehead as a result of diaphoresis.
The patented arterial heat balance technology (AHB™) automatically measures
the temperature of the skin surface over the artery and the ambient temperature.
It samples these readings some 1000 times a second, ultimately recording the
highest temperature measured (peak) during the course of the measurement.
The TemporalScanner emits nothing - it only senses the natural thermal radiation
emitted from the skin.
How accurate is it?
It has been clinically proven in premier university hospitals to be more accurate
than ear thermometry, and better tolerated than rectal thermometry. It is a superior
method for patient and clinician alike.
What if the TA area has been traumatized by burns or lacerations,
or is completely covered with dressings?
With head trauma, surgical or accidental, the temperature can be obtained from the
alternative site behind the ear lobe. As with diaphoresis, the perfusion will be high
in the presence of head trauma.
Why measure behind the ear lobe?
Sweat causes evaporative cooling of the skin on the forehead, and introduces the
possibility of a false low temperature. Fortunately for the method, during
diaphoresis the area on the head behind the ear lobe will always exhibit the high
blood ow necessary for the arterial measurement.
Page 13
11
Frequently Asked Questions
Why not use only the area behind the ear lobe?
Since the arterial branch is deeper behind the ear lobe than at the temple, under
normal conditions it is less accurate because of its variability. But under diaphoretic
conditions, the blood ow behind the ear lobe is as high as at the TA, making it
as accurate as the TA, but only during diaphoresis or with head trauma as
previously mentioned.
What are the benets of using temporal artery thermometry?
Besides the inherent accuracy of the method, TAT presents no risk of injury for
patient or clinician, eliminates the need for disrobing or unbundling, and is suitable
for all ages.
What is arterial temperature?
Arterial temperature is the same temperature as the blood owing from the heart via
the pulmonary artery. It is the best determinant of body temperature, and unaffected
by the artifactual errors and time delays present with oral and rectal methods.
How does the TemporalScanner compare to our old method?
Arterial temperature is close to rectal temperature, approximately 0.8ºF (0.4°C)
higher than oral temps. Expect larger differences at times, however, as the
dynamics of thermoregulation favor the temporal artery method.
High readings?
Temperatures measured with the TemporalScanner may be higher than your current
method, especially if you are used to oral or axillary temps. Oral and axillary
temperatures can be misleadingly lowered due to patient activity such as mouth
breathing, drinking, tachypnea, coughing, talking, etc, and periods of
vasoconstriction during the fever process. Any or all of these conditions may even
mask fevers that the TemporalScanner will detect.
Low readings?
A patient’s temperature measured with the TemporalScanner is normally never
appreciably lower than oral temperature. Lower temperatures are usually
from scanning too fast, not keeping the button depressed, a dirty lens, or a
sweaty forehead.
Page 14
12
Frequently Asked Questions
What else should I know?
False high readings:
• Measure only skin that is exposed to the environment.
Any covering, hair, hat, bandages, etc., would prevent
the heat from dissipating, causing the reading to be
falsely high.
False low readings:
• Multiple readings can cool the skin, so if you take
another measurement immediately, expect a slightly
lower reading.
• Slide the thermometer straight across the forehead,
not down the side of the face where the TA could be
embedded under cartilage or fat.
• Keep the probe ush on the skin, as in the picture on the right.
If angled, you will be measuring ambient air as well as the TA area.
Memorable solutions?
• Measure only the side exposed to the environment. The TemporalScanner assumes
the skin it measures has equilibrated to ambient, so a down or covered side could be
falsely high as heat is trapped and the skin is unable to equilibrate.
• If the up side is not the side closest to you, try scanning from the hairline towards the
center of the forehead.
• Scan slowly across the TA area; if you scan too quickly you can miss the peak.
• Bandages or pressure dressings covering
the forehead.
• Forehead abrasions, burns, sweat.
• Agitated or combative patient.
• Patient’s forehead in direct draft from vent
or fan.
• If accessible and dry, measure on the area
behind the ear lobe only.
• Consider using the alternate sites: femoral
artery, lateral thoracic, or axillary areas.
• Thermometer in different ambient
temperature than patient: i.e. window ledge
directly exposed to hot sun or cold weather,
or in direct line of air conditioning or fan.
• The TemporalScanner should be kept in the
same ambient temperature as your patient.
Each 10° difference in ambient can cause a
1° error in the reading.
Conditions that could affect a reading ...and their solutions
Page 15

13
Frequently Asked Questions
Disposable Cover Options
(Model Illustrated: TAT-5000)
• TAT-5000 can be used with either
disposable caps or full sheath. Can be used
without disposables if terminally cleaned
between patients.
• Can be cleaned with any hospital approved
disinfectant, alcohol, and even bleach
solutions. Use only alcohol solution for
sensor lens.
• ”bAtt” on the display indicates a low battery.
Replace with a 9-volt alkaline battery.
• Probe lens should be shiny clean. If not,
wipe an alcohol prep or Q-tip dipped
in alcohol. Occassionally follow with a damp
wipe of water to remove any alcohol
residue buildup.
• A LO or HI reading outside body
temperature range is indicative of the
instrument’s failsafe mode, signifying a
mechanical failure.
• Can be used in either ºC or ºF.
What should I know about the instrument?
No Cover
Terminal
Cleaning at
Patient.
No Cover
Disinfectant Wipe
Between Patients.
Probe Cap
Covers Entire
Probe.
Full Sheath
Covers Entire
Instrument.
Model TAT-5000 All Options
Accessories
1. Combination Unit
PN 134200
2. Instrument Holder (shown with security cable)
PN 134201
3. Cap Dispenser
PN 134202
4. Disposable Caps
PN 134203
5. Security Cables
8 ft. coiled cable - PN 124309
8 ft. coiled cable - Latex free - PN 124311
6 ft. vinyl-covered steel - PN 134302
8 ft. vinyl-covered steel - PN 134030
6. Keyless Self-Locking Wall Mount
PN 134305
7. Keyless Self-Locking Wall Mount
(shown with resposable cap dispenser)
PN 134306
Page 16

14
Guidelines for Patient Temperature Assessment
Guidelines for Patient Temperature Assessment
Comparing with Other Methods of Thermometry: Expect the Differences
Unless you are using PA catheters or Exergen aural thermometers with AHB for
temperature assessment, expect to see differences compared to your current
thermometers. Arterial temperature measurement leads all other methods
in identifying fever or defervescence, and is unaffected by patient activity.
Accordingly, it will sometimes be different – but correct.
The following chart presents the mean normal temperature at the common
temperature measurement sites under normal resting conditions.
Normal Body Temperature (BT)
Normal BT is not a single temperature, but a range of temperatures inuenced by age, time
of day, and the measurement site.
General Rule of Thumb
On a stable, resting patient, rectal temperature is ~2°F (1°C) higher than axillary and ~1°F
(0.5°C ) higher than oral temperature.1 On a stable, resting patient, arterial temperature
~rectal temperature.
Expect the Differences
Arterial temperature measurement (PA Catheter, TA Thermometry) leads all other methods
in identifying fever or defervescence, unaffected by activities of daily living. It will sometimes be different from your present methods — but accurate.
Arterial
97.4 - 100.1°F
(36.3 - 37.8°C)
Oronasal
96.6 - 99.0 °F
(35.9 - 37.2 °C)
Oral
96.6 - 99.5 °F
(35.9 - 37.5 °C)
Axillary
95.5 - 98.8 °F
(35.3 - 37.1 °C)
Esophageal
98.4 - 100.0 °F
(36.9 - 37.8°C)
Rectal
97.7 - 100.3°F
(36.5 - 37.9°C)
Page 17

15
Guidelines for Patient Temperature Assessment
Guidelines for Patient Temperature Assessment
1. Fever Denition: Clinically, fever is dened as a BT =1.8°F (1°C) above the
mean standard deviation at the site of recording.2 A single oral temperature of
101°F (38.3°C ) in the absence of obvious environmental causes is usually
considered fever. An oral temperature of 100.4°F (38.0°C) over at least 1 hour
indicates a fever state.
3
2. Oral Temperature Risks: Oral temperature can be clinically misleading, and
many febrile patients can have a “normal” temperature, even when tachypnea
was unobserved.
4
3. Rectal Temperature Risks: Rectal temperature should only be considered as a
good approximation of core temperature when the patient’s thermal balance is
stable. When monitored during or after surgery, rectal temperature measurement
is not suitable, and the possible delay in diagnosis of a thermal abnormality could
lead to an irreversible crisis.
5
4. Axillary Temperature Risks: Axillary temperature is contraindicated in critically ill
adults, and its use in the general patient population should be discouraged due to
its unreliable correlation with core temperature and its poor reproducibility.
6
5. Temporal Artery Temperature (TAT) Values: On a stable resting patient, TAT
is ~0.8°F (0.4°C) higher than an optimum oral temperature, and close to a rectal
temperature.7 However, during febrile episodes, the difference can be much
higher, mainly because of the artifacts of oral and rectal sites.
6. Comparison Between Sites: Review of published literature reveals mean
differences between non-TA sites of 0.4° to 3.1°F (0.2° to 1.7°C) with the actual
differences of up to 6.5°F (3.6°C) routinely reported, especially in febrile patients.
8
References:
1. Kuzucu EY. Measurement of temperature. Int Anesthesiol Clin, 3(3):435-49, May, 1965.
2. El-Radhi AS, Carroll JE. Fever in Paediatric Practice, Ch 2, pp 15-49, Oxford Blackwell Scientic
Publications, 1994.
3. Hughes WT et al. 1997 Guidelines for the use of antimicrobial agents in neutropenic patients with
unexplained fever. Infectious Diseases Society of America (IDSA).
4. Tandberg D et al. Effect of tachypnea on the estimation of body temperature by an oral thermometer.
NE J Med, 308, 945-46,1983.
5. O’Grady NP, Barie PS, Bartlett JG, et al. Practice guidelines for evaluating new fever in critically ill
adult patients. Task Force of the Society of Critical Care Medicine and the Infectious Diseases Society
of America. Clin Infect Dis 1998 May: 26(5):1042-59.
6. Houdas Y, et al. Human body temperature. Ch 5, p89 Plenum Press, 1982, USA, UK.
7. Exergen Corporation. Manufacturer’s data on le.
8. Review of subject material peer-reviewed journals.
Page 18

16
Determining a Fever Threshold
Determining a Fever Threshold for Temporal Artery Thermometry
Threshold Dening Fever
• A threshold for dening fever is the temperature level above which false positives
due to normal variations in temperature, including range of normal mean +
circadian effects + other effects (metabolic, ovulation, etc.) are unlikely.
Threshold for Fever Workup
• Not all fevers require a fever workup. A fever workup is an early management
tool in assessment of the likelihood of septicemia or bacteremia, and initiated
whenever an infectious source is suspected. The level of temperature triggering
such that investigatory workup is sufciently high to avoid false positives resulting
in unnecessary discomfort and expense for the patient, but low enough for early
identication and intervention.
Primary Points
• Temperatures measured with temporal artery thermometry may be higher than
normally seen with other clinical methods, and therefore require an adjustment in
both protocol and perception.
• No one value can apply to every temperature measurement site. Note old rule of
thumb: Rectal temperature is ~1°F higher than oral temperature and ~2°F higher
than axillary temperature.
• Recommended threshold for fever workup using arterial temperature assessment
is a single temperature >101.8°F, or a temperature >101.2°F sustained for more
than 1 hour.
• Adjustment of ~1°F is necessary to raise the temperature level normally mandated
for fever workups to prevent false positives, unnecessary cultures and blood
tests, etc.
Temperature Site
Core &
Temporal Artery
Oral & Temporal
Artery in Oral
Calibration
Axillary
Fever Workup
Recommendation
Single value
>101.8
Sustained values
(>1h) >101.2
Single value >101
Sustained values
(>1h) >100.4
Single value >99
1
Source on le at Exergen Corporation
Physician Recommended Guidelines for Fever Workup
1
Page 19

17
Body Sites for Temperature Assessment
Body Sites for Temperature Assessment
An Overview of Temperature Measuring Sites
Oral Temperature
Oral temperature measurement is by far the most common clinical method in use today, and is
responsible for masking the greatest number of fevers. Oral temperature can be
misleadingly lowered by patient activity such as tachypnea, coughing, moaning, drinking,
eating, mouthbreathing, snoring, talking, etc. Alarmingly, another cause of low oral
temperatures is the fever itself. For each 0.6°C (1°F) temperature elevation, the pulse rate
usually increases approximately 10 beats per minute, there is a 7% increase in oxygen
consumption, increasing the respiratory rate approximately 2 cycles per minute. The resulting
increase in respiration can further lower oral
temperature sufciently to mask a fever.
Figure 1 is of interest as it illustrates fever masking
even when clinicians had eliminated all obvious
mouth-breathers from the study. This emergency
room study presents the temperature difference
(rectal minus oral) in 310 patients with a wide
range of respiratory rates. The straight line of best
t is shown. The stippled area demonstrates the
traditional normal difference between rectal and
oral temperature (0.3°- 0.65°C). The investigators
concluded that many patients with tachypnea would
have oral temperatures in the normal range despite
the presence of clinical fever, seriously misleading
the clinician.
Rectal Temperature
Generally, rectal temperature is considered
an indicator of deep tissue and critical tissue
temperatures, but long standing data demonstrate that rectal temperature can be a lagging
and unsatisfactory index. Fifty years ago, Eichna et al reported differences between
intracardiac, intravascular and rectal temperatures on afebrile patients to be so insignicant
that for all practical purposes, the temperatures may be considered to be the same. Certainly
rectal temperature is far less invasive than a pulmonary artery catheter, however, in the same
study, data on febrile patients support sizeable differences.
Other comparisons between rectal, esophageal and aortic temperatures undertaken on
hypothermic patients by different researchers also conrm similar differences. Subsequent
but equally comprehensive comparisons on healthy volunteers further conrmed not only
temperature differences, but also quantied signicant lags in rectal temperature vs.
hypothalamic temperature by times of order one hour. This is of interest since the blood as it
enters and affects the critical tissue in the hypothalamus should have considerable
signicance in thermal homeostasis. However, this early data on hypothalamic temperature
was measured by a thermocouple inserted against (and often times perforating) the tympanic
membrane. With signicant improvements in the methodology, more recent clinical
observations show that the time constant of rectal temperature in critically ill patients may be
considerably longer, and in some cases, as much as a day.
Figure 1 Temperature Difference (Rectal minus Oral) in
310 Patients with a Wide Range of Respiratory Rates.
The straight line of best t is shown. The stippled area
demonstrates the traditional “normal” difference between
rectal and oral temperature (0.3 to 0.65°C).
Page 20

18
Body Sites for Temperature Assessment
Under certain conditions, rectal temperature is even contraindicated; for example, severe
arterial insufciency in one or both legs might be associated with falsely low readings, or in
conditions affecting peripheral blood ow such as cardiogenic shock. More common
contraindications include neutropenia, severe hemorrhoids, and recent anorectal surgery. A
less common but serious complication of rectal temperature measurement is perforation of the
rectum, which has even occurred in the absence of predisposing rectal pathology.
Rectal temperature measurement is not well tolerated, by either the patient or the caregivers,
and is uncomfortable and embarrassing. Rectal temperature is subject to inaccuracies of
placement, environment, and time of insertion. And although it is well established that a
rectal temperature requires two to ve minutes or more to reach optimum measurement with
a glass mercury thermometer, in practice many are withdrawn in just one minute, a technique
responsible for misleadingly low readings.
In fact, it is difcult to attribute any thermal signicance at all to the rectal area. It is not
known to contain any thermoreceptive elements and its geographical location distances it
from both the CNS and the crossroads of circulation at the heart, which are the vital
informational elements.
Tympanic Membrane and Ear Temperature
A temperature site of more recent onset is the ear. It is a compelling site, accessible, free from
bodily uids, and not easily inuenced by patient activity. This temperature is measured using
infrared technology, and there are three types of infrared thermometers: tympanic, ear, and
arterial heat balance. It has, however, become common practice to refer to any thermometer
making the measurement at the ear as a tympanic thermometer. Although the terms tympanic
and ear may be used interchangeably, they actually describe quite different measurements.
True Tympanic Membrane Temperature
The tympanic membrane is deep inside the skull, and is not subject to the artifactual errors
that can affect oral, rectal, axillary and ear temperatures. True tympanic thermometers
provide an uncorrected, direct reading of the temperature of the tympanic membrane, and
are preferred for continual measurement during certain surgical procedures, and for use in
extreme conditions such as military use, research, and sporting events.
There are two types of instruments used to make the measurement. One is a long thin
thermocouple probe, usually tted with cotton at the end, that must come in contact with the
tympanic membrane. There is much historical data on the efcacy of tympanic thermometry
using contact thermocouples, stemming originally from work done over thirty years ago.
However, this method never gained wide acceptance due to the risk of injury to the delicate
membrane. The second is an infrared device, the Exergen Ototemp 3000SD, which is inserted
deep into the ear canal and scanned to view the membrane, and is used in military and
sports medicine.
Ear Temperature
Ear thermometry is a method of measuring the temperature of the external portion of the ear
canal. For routine clinical use, ear thermometry has been preferred as a simpler, faster, and
more convenient alternative to true tympanic thermometry. The absolute temperature of the
outer ear, however, is lower, and more variable than tympanic membrane temperature. It is
subject to a cooling effect resulting from the body heat being radiated to the environment, and
a heat balance method is required in order to produce the requisite accuracy. When combined
with an arterial heat balance method, ear thermometry provides a highly accurate indication of
body temperature, but those ear thermometers without it have high rates of missed fevers.
Page 21

19
Reproducibility of Readings
Reproducibility in Temperature Measurement
Multiple temperature readings in the same area, mouth, rectum, axilla, ear or temporal artery, make
for variability with each separate measurement. This can be confusing for clinicians, since they
expect the same number with each measurement. The non-reproducibility of the readings, however,
is not a function of the devices, but simply a function of physiology. The human body is a myriad of
small gradients, and variability of readings will occur on every method of temperature measurement.
In addition, thermometers are at room temperature, nearly 30°F (17°C) cooler than the tissue being
measured. That said, it is then easily recognized how time of insertion, probe placement, and tissue
cool down all affect reproducibility of temperature readings, no matter what device is employed.
Oral Temperature
By far, the most common method of temperature measurement is
sublingual measurements. Placement of the probe under the
tongue, however, can result in substantial differences, and caused
by just a slight repositioning of the probe. The standard heat chart
commonly used by manufacturers of electronic thermometers on
the right illustrates a difference of nearly 2°F (1°C) depending on
exactly what area is being touched by the probe.
Differences from repeated oral temperatures can vary even
further, as they can superimpose artifactual errors over the thermal
gradients. Patient activities also affect the reading, these varying
by individual and activity. In fact, one large manufacturer cautions
waiting at least 15 minutes after ingesting hot or cold food or drink,
after exposure to extremely hot or cold weather, and after smoking.
Ear Temperature
The journals abound with citations addressing the lack of reproducibility of ear thermometers. In
fact, Thermoscan instructs the user to take three separate temperature measurements, and to
select the highest of the three. While much of this has to do with the device, physiology also plays a
large part. In such a small area, the difference of 30°F (17°C) between the room temperature probe
and the temperature of the ear being measured results in a noticeable tissue cool down. Geriatric
patients typically have a lower rate of perfusion than a younger individual, and it can take several
minutes for the ear to equilibrate following the use of an ear thermometer.
Rectal Temperature
Time and placement is critical for rectal temperature measurement. It has long been recommended
that the measurement be taken for at least ve minutes or more for accuracy. The measurement
is also dependent on the depth of insertion, and just a few centimeters can result in a noticeable
difference.
Temporal Artery Temperature
Because of the expanse of area being measured, and the normally strong perfusion of the artery
in particular, temporal artery temperatures should be as reproducible as any other method. There
may be slightly more variability observed in normothermic conditions compared to febrile conditions,
but it is minimal. Of interest, the temporal artery area will equilibrate in the shortest period of time
compared to any other site. For absolute accuracy, however, it is recommended to wait 30-60
seconds before repeating a temperature on the same side, although, depending on the individual,
the time involved can certainly be much shorter. The limitation in time is almost entirely the behindthe-ear measurement, as the perfusion rate per tissue mass is not quite as high as the temporal
artery. Since the method employs the area behind-the-ear with every measurement, this area is the
time limitation.
Page 22
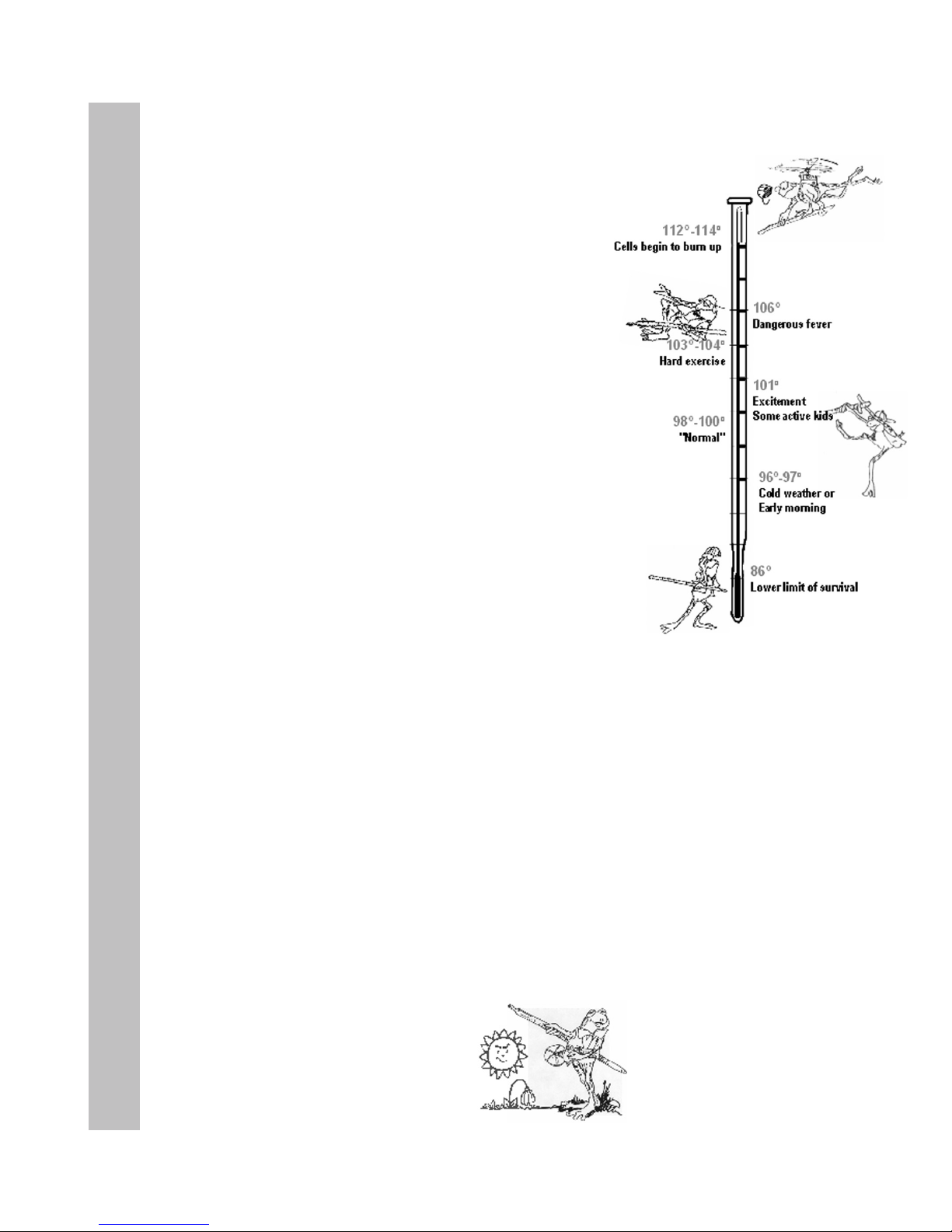
20
Forgotten Physiology
Normal Temperature
Normal human temperature is around 98.6 degrees. But
did you know that only 8% of the people in the world
have a normal temperature of exactly 98.6?
A temperature that is normal for you may even be
a whole degree or so above or below “normal.” It is
good to know what is normal for you. Try taking your
temperature at different times, like in the morning, after a
cold shower, or a ve-mile hike.
Fever
Fever is when your body’s temperature control is set
above normal. Fever is a sign that your body is ghting
off an infection. It is thought that fever does two things.
When the temperature rises, the body’s chemical actions
speed up so that damaged tissues can be repaired more
quickly. Also, virus or bacteria invaders don’t survive
well at high temperatures. Perhaps fever is the body’s
attempt to cook them into submission.
Chills
You have a high temperature and cold skin. You are hot
inside, but still you shiver. Chills are your body’s way
of creating a fever. The muscle action from shivering
produces heat, which raises your temperature in an
effort to ght off infection. When the crisis is over, your
temperature is set back to normal, the skin warms, and
you sweat.
Your Temperature
Hot Blood or Cold Blood?
A frog in a 70 degree pond is a 70 degree
frog. A frog in a 40 degree pond is a 40
degree frog, and is moving very slowly, if
at all.
A kid in a 70 degree pond is a 98 degree
kid. A kid in a 40 degree pond is still a
98 degree kid, although you can bet he’s
swimming as fast as he can to get out.
One difference between kids and frogs
is the difference between warm-blooded
and cold-blooded beings. People have
automatic climate control inside their
bodies. Their bodies keep themselves
at an even temperature by carefully
controlling the rate of burning in
their cells.
Cold blooded creatures have no internal
temperature control. Their rate of metabolism
is determined by their environment. When the
outside temperature drops way down, all their
body processes slow way down.
Humans, and all mammals, are souped-up hotblooded beings. Their metabolisms are speedy,
but are kept at an even keel. So no matter what
the temperature is outside, the climate on the
inside is ever warm and ready for action.
1
1
Excerpts from Blood and Guts: A Working Guide to Your Own Insides, Allison L. Katz., Little , Brown and Company, Boston, New York, Toronto, London
Frogs are cold blooded,
their temperature changes
depending on where they are.
Page 23
21
Forgotten Physiology
Perspiration
The TemporalScanner relies on the skin over the temporal artery to help provide an accurate
body temperature. In fact, it is measuring the inside by measuring the outside. Your skin is a
sensor, controlling body temperature in two ways: radiation and evaporation. Since most of us
don’t think about our skin as a sensor, this might be a good time to discuss a little physiology.
We live our entire lives with a body temperature that changes only a few degrees. This is
thanks to a very sophisticated climate control, of which the skin is a very important part.
Sweating, goose bumps, and heat loss from the skin all help maintain our normal
temperature, keeping us comfortable.
When your internal temperature rises, your brain signals your blood to increase circulation to
the skin. In this way, the body’s internal heat is carried to the surface by the blood, where it is
lost by radiation.
If this is not sufcient, your sweat glands sprint into action, and perspiration is released
through the pores. This liquid evaporates on your skin and you cool right down. When your
temperature drops, your brain signals that heat must now be saved. Less blood circulates to
the skin, and sweating stops.
Since there is a lot of cooling going on when you are sweating, both inside and out, it is a
good idea to wait till your forehead is dry before taking your temperature with the
TemporalScanner. If your forehead is sweaty, the reading would be low. Drying your forehead
could help shorten the wait, but there is another place to measure an accurate temperature
when perspiring. It is still on the head, but in the little soft depression just behind the ear lobe,
the place where young ladies are usually taught to apply perfume.
During perspiration, taking a temperature with the TemporalScanner in the area behind the ear
lobe has been proven to be as accurate as a temperature taken at the temporal artery area,
were it not wet. Since we sweat rst on the forehead, then on the hands and feet, the chances
of the area behind the ear lobe remaining dry for the measurement are excellent. And since
we already have increased circulation to the skin during perspiration, this area will have the
high blood ow necessary for the measurement.
Another instance when a high rate of blood ow on the neck can be assured is following head
trauma, either surgical and accidental. At such times the neck area behind the ear lobe can be
used as a primary site if the forehead is not available.
If perspiration or head trauma is not present, the area on the neck behind the ear lobe may
not have sufcient blood ow to be reliable, and should not be used as the primary
measurement site.
If there is heavy perspiration, including moisture behind the ears, wait until area is dry. For use
on exercising athletes or other non-clinical subjects, contact Exergen.
Page 24

Your ears. Now we’re down to ears. And please
pardon us, ears beat
rears. But, having your
ear pulled sure isn’t
fun, and when you have
an ear infection, it even
hurts.Temperature taken
in your ear should be
higher than in your mouth,
but not as high as in your rear.
Your heart. If we were to pick the
best place to measure temperature
it would be in the center of your
heart. But that’s pretty dangerous,
and surely not be something you
would think was fun. Arrrrghhh! In
case you’d like to know, though, temperature in your
heart is around 99.4°F.
Your temporal arteries.
There is a special place on
your head where we can
measure the same temperature
as the blood in the middle of
your heart. This is because
blood is pumped directly from
your heart to your head through
little tubes called arteries that
carry blood up the sides of your neck, up the side of
your face just under your skin, and stop at at a place
on your forehead called your temple. Guess what
they’re called?
Wow! Isn’t this the same place your mom
touches with her hand when you don’t feel
good?
Did you know that the forehead has been used
to detect fevers as far back in time that anyone
can remember, over 2000 years? There’s a new
technology that scans the same place your mom
touches, and it’s almost as gentle. It’s an infrared
thermometer called the TemporalScanner. It
measures your temperature with a quick and
gentle scan across your forehead. Most of the time,
temperature here is around 99.4°F, same as your
heart. Nothing goes in your mouth, your ear, or your
rear, and in just a second or two, done!
Did you know you always have a
temperature? Bet you thought you
only had a temperature when you
were sick. Absolutely everything
has a temperature, even icicles.
Brrrrrr!
When you don’t feel well, your
mom or a nurse might say “let’s see if you have a
temperature,” but what they really mean is “let’s
see if your temperature is different from normal.”
So, when you have your temperature taken, don’t
be fooled. Your mom and your doctor already
know you have a temperature, and are just
getting an idea of how things are going inside
your body.
Places to measure your temperature.
Your bum. Babies and little
kids get their temperature
taken in their bum. Poor little
kids, how embarrassing!
The temperature taken
in your bum is the hottest
of all the places to take
temperature. It’s around 99.6°F most of the time.
Your armpit. When kids get
a little bit older, they might
have their temp taken under
the arm instead of the bum.
This is better, but you have
to keep the thermometer in
your armpit with your arm
tight against your chest for a long time. It’s hard
to keep it from falling out and breaking, especially
if you y! I wonder if ying causes the armpit
temperature to be the lowest in your body. It’s
around 97.6°F most of the time.
Your mouth. Now, if you’re
reading this, you’re probably a
big kid and so you would most
likely have your temperature
taken in your mouth. Not too
bad, but everyone knows you
can trick your mom or your
doctor into thinking you’re sick by doing stuff with
that thermometer. Bet you already know of ways
to do that! Most of the time, a temperature in your
mouth is about 98.6°F. Well sort of...
22
For Kids Only
Now, where is the best place to take
your temperature?
Page 25

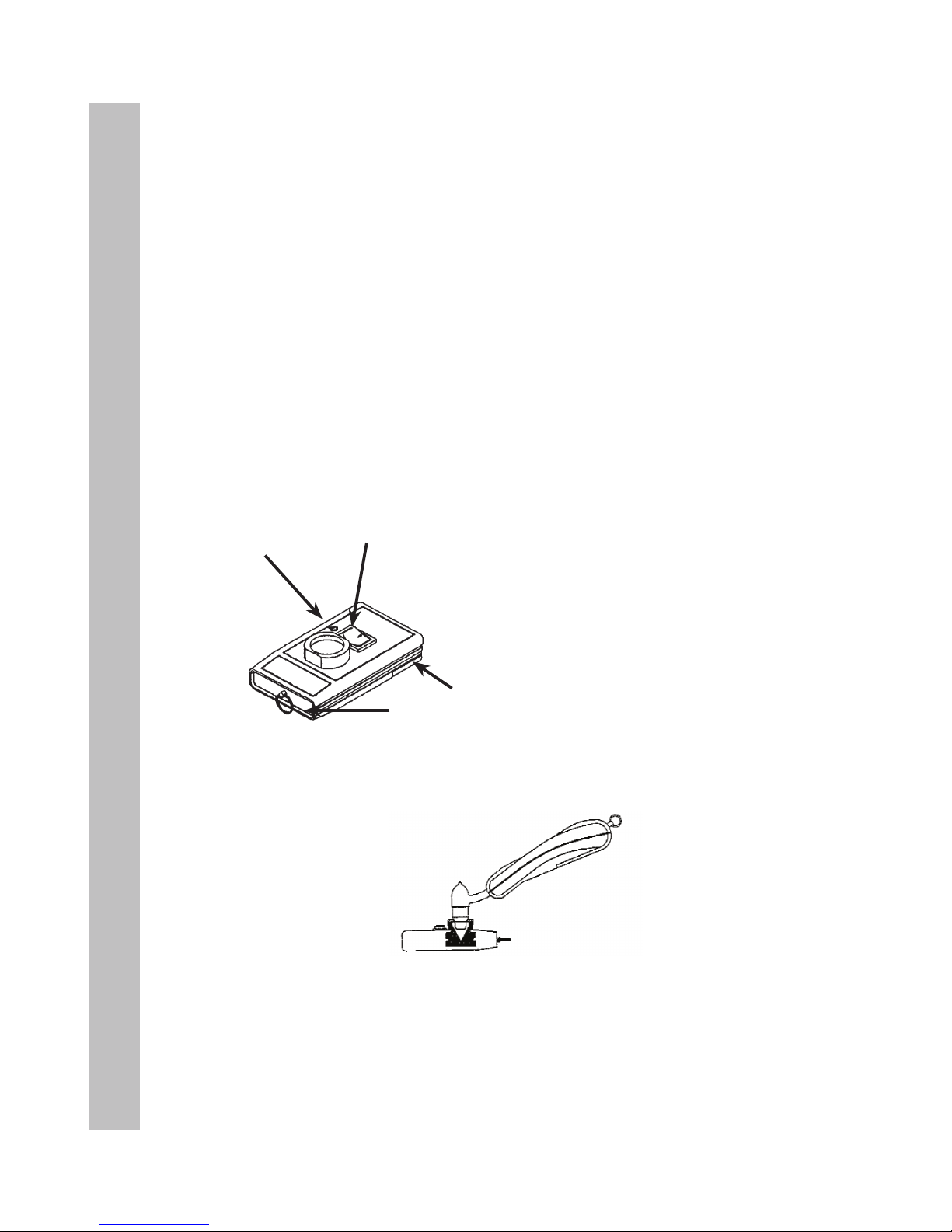
23
Care and Maintenance
Care and Maintenance
• Battery: A standard alkaline 9V battery provides
approximately 15,000 readings.**
To replace, loosen the single screw at the bottom of the
instrument and remove the battery cover. Disconnect the
old battery and replace with a new one in the same
location. Replace the cover, and tighten the screw. Use
only high quality alkaline batteries or equivalent.
• Handling: The TemporalScanner is designed and
built to industrial durability standards in order to provide
long and trouble-free service. However, it is also a high
precision optical instrument, and should be accorded the same degree of care in
handling as you would provide other precision optical instruments, such as
cameras or otoscopes.
• Cleaning the case: The TemoralScanner case can be wiped down with any
hospital approved disinfectant, including bleach.
• Cleaning the sensor lens: With normal use, the only maintenance required
is to keep the lens on the end of the probe clean. It is made of special mirror-like,
silicon infrared-transmitting material. However, dirt, greasy lms or moisture on
the lens will interfere with the passage of infrared heat and affect the accuracy of
the instrument. Regularly clean the lens with a cotton swab dipped in alcohol in
accordance with the instruction label on the instrument (see below). Use only light
force for cleaning, to avoid damaging the lens. Water can be used to remove any
residual lm left by the alcohol. Do not use bleach or other cleaning solutions on
the sensor lens.
• Sterilization: The industrial grade housing and design of the electronic
components allow for completely safe disinfecting with any accepted solution.
• Calibration: Factory calibration data is installed via a computer which
communicates with the TemporalScanner’s microprocessor. The instrument
automatically self-calibrates each time it is turned on using this data, and will
never require recalibration. If readings are not correct, the instrument should be
returned for repair.
CLEANING INSTRUCTIONS ON
THE TAT-5000
Page 26

24
Care and Maintenance
Instructions for Fahrenheit or Celsius Conversion
The TemporalScanner can be used in either °F or °C. To convert from one scale to
the other, the only tool necessary is a paper clip or the tip of a small screwdriver.
For °F/°C Conversion:
• Loosen single screw on bottom of case and remove
battery cover.
• Lift battery out of the way.
• Locate the little switch to the right of the battery as
indicated in the drawing, and with the tip of the paper
clip or screwdriver, slide up or down to the
opposite position.
• Remove the paper clip or screwdriver.
• Replace battery and cover.
°F
°C
Switch
DISPLAY DIAGNOSTICS CHART
The following chart summarizes the fault conditions, and the associated indications:
Condition Display Range
High Target HI >110 °F (43 °C)
Low Target LO <61 °F (16 °C)
High Ambient HI A >104 °F (40 °C)
Low Ambient LO A <60 °F (16 °C)
Low Battery bAtt
Dead Battery blank display
Processing Error Err
Restart. Return to
Exergen for repair if error
message persists.
Page 27

25
Care and Maintenance
Calibration Verication Procedure
All Exergen infrared thermometers are designed to permanently maintain their accuracy and normally
recalibration is not required unless the thermometer has been physically damaged or experiences
component failure. In the unlikely event recalibration might be required, the thermometer must be returned
to Exergen for the procedure.
However, calibration can be veried in the lab or clinical units quite easily using a device known as
a portable blackbody. A portable blackbody is a reference heat generator (Figure 1), which is a selfcontained device providing a stable reference target temperature in the clinical temperature range.
The device is then used to verify the calibration of any Exergen thermometer in question, or for quality
checks done on a routine basis. The verier operates with either a 9-volt power supply plugged directly
into any 120 vac wall receptacle, allowing extended use in the laboratory, or it can be completely powered
by a 9-volt battery for portable use on the nursing oors.
There are two ways to use the portable blackbody to verify the calibration accuracy of the thermometer
in question, either (1) with a certied master reference infrared thermometer, or (2) by using two identical
thermometers as a reference against the one in question.
Specications TAT-5000
Clinical Accuracy
± 0.2°F or 0.1°C
Per ASTM E1112
Temperature Range 61 to 110°F (16 to 43°C)
Arterial Heat Balance Range for
Body Temperature*
94 to 110°F (34.5 to 43°C)
Operating Environment 60 to 104° F (16 to 40°C)
Resolution 0.1°F or C
Response Time ~ 0.04 seconds
Battery Life 15,000 readings**
Time Displayed on Screen 30 seconds
Size
2.0” x 8.0” x 1.25”
(5 cm x 20 cm x 3 cm)
Weight 7.5 oz. (213 gm)
EMI and RFI Protection Complete copper coating on inside of casing.
Display Type and Size Large bright LED’s
Construction Method
• Industrial duty impact resistant casing
• Hermetically sealed sensing system
• Stainless steel probe
Warranty
Lifetime
*Automatically applied when temperature is within
normal body temperature range, otherwise reads
surface temperature.
** Approximate number of readings when scanning for 5
seconds and reading the temperature display for 3 seconds
before turning thermometer off.
Page 28
26
Care and Maintenance
Using the Portable Blackbody
1. Turn on the verier device, using either a 9-volt battery or the power supply. Make
sure the red LED is illuminated.
2. Allow device ~5 minutes for warm-up and stabilization time.
3. Allow certied master or the two reference thermometers and the instrument to be
tested to acclimate in the same ambient temperature for at least 10 minutes.
4. For all instruments, make sure the lens at the tip of the probe is clean. To clean,
use an alcohol prep or a swab dipped in alcohol, followed by a damp wipe with
water to remove any residue.
5. Alternately insert the reference instrument(s) and the instrument being veried
into the aperture opening, comparing the readings.
1
3
4
2
Portable Blackbody Calibration Verier
1. Power On LED
2. ON/OFF Switch
3. Battery Compartment
4. Power Supply Jack
Using a Certied Master Reference
Thermometer in a Portable
Blackbody to Verify Calibration
Figure 1
Page 29

27
Care and Maintenance
Power Source 9-volt battery, or 9-volt power supply.
Battery Life Approximately 1 hour continuous use.
Low Voltage Indicator Red LED shuts off when battery voltage drops below ~5 volts.
Temperature Range 97-104 ºF (36-40 ºC)
Cleaning
Wipe down with alcohol or any hospital approved disinfectant.
Do not immerse.
• Accuracy Limits: Comparison between the reference instrument(s) and the
instrument being veried should be within ±0.4 ºF (0.2 ºC) for acceptable limits.
If not, repeat the process. In the event they still differ by more than the
acceptable limits, call Exergen for repair or replacement of the failed instrument.
Verier Specications:
Repair
If repair is required:
• Contact Exergen at (617) 923-9900 for a Return Materials Authorization
(RMA) Number.
• Mark the RMA number on the outside of your package and packing slips.
• Include a description of the fault if possible.
• Send the instrument freight/postage prepaid to:
Exergen Corporation
400 Pleasant Street
Watertown, MA 02472
• The instrument will be returned freight/postage prepaid.
Page 30

Page 31

Page 32

EXERGEN CORPORATION • 400 PLEASANT STREET • WATERTOWN, MA 02472 • PH 617.923.9900
www.exergen.com
p/n 818528 r8
EXERGEN
Straight from the Heart
Symbol for Date of Manufacture
Symbol for Manufacturer
Type BF Applied Part
!
Consult Instructions for Use.
Caution, Consult Accompanying Documents
“On” (Only for part of Equipment)
Do not throw this device away in the trash, contact
Exergen Corp. for disposal and recycling instructions.
IPXO
Ordinary Equipment
Degree of
Protection
Against
Electric
Shock
Type BF, Battery Operated
 Loading...
Loading...