Page 1

Edwards SAPIEN 3 Transcatheter Heart Valve
with the Edwards Commander Delivery System
Instructions for Use
CAUTION: Federal (USA) law restricts these devices to sale by or on the order of a physician.
Implantation of the transcatheter heart valve should be performed only by physicians who have
received Edwards Lifesciences training. The implanting physician should be e xperienced in
balloon aortic valvuloplasty.
Please verify that you have the latest version of the instructions for use prior to u sing the device
by visiting http://THVIFU.edwards.com or by calling 1.800.822.9837. In order to access the
instructions for use, an IFU Code will be required.
STERILE: The valve is supplied sterilized with glutar aldehyde solution. The delivery system,
eSheath introducer set, and crimper are supplied sterilized with ethylene oxide gas.
Edwards, Edwards Lifesciences, the stylized E logo, Carpentier-Edwards, EDWARDS COMMANDER,
Edwards eSheath, Edwards SAPIEN, Edwards SAPIEN 3, eSheath, PARTNER, PART N ER I I, Qualcrimp,
SAPIEN, SAPIEN 3, TFX, and ThermaFix are trademarks of Edwards Lifesciences Corporation. All other
trademarks are the property of their respective owners.
1
Page 2

1.0 Device Description
• Edwards SAPIEN 3 Transcatheter Heart Valve- Model 9600TFX (Figure 1)
The Edwards SAPIEN 3 Transcatheter Heart Valve is comprised of a balloon-expandable, radiopaque,
cobalt-chromium frame, trileaflet bovine pericardial tissue valve, and polyethylene terephthalate (PET)
fabric skirt. The leaflets are treated according to the Carpentier-Edwards ThermaFix process.
Table 1
Valve Size Height
20 mm 15.5 mm
23 mm 18 mm
26 mm 20 mm
29 mm 22.5 mm
Table 2
Native Valve Annulus Size
Native Valve Annulus Size
(TEE)
16-19 mm 273 – 345 mm2 18.6-21 mm 20 mm
18-22 mm 338 – 430 mm
21-25 mm 430 – 546 mm
24-28 mm 540 – 683 mm
Valve size recommendations are based on native valve annulus size, as measured by transesophageal
echocardiography (TEE) or computed tomography (CT). Patient anatomical factors and multiple imaging
modalities should be considered during valve size selection. Note: Risks associated with undersizing and
oversizing should be considered.
Area
(CT)
Area Derived
Diameter
2
20.7-23.4 mm 23 mm
2
23.4-26.4 mm 26 mm
2
26.2-29.5 mm 29 mm
Valve Size
• Edwards Commander Delivery System (Figure 2)
The Edwards Commander delivery system is used for delivery of the Edwards SAPIEN 3 transcatheter
heart valve and consists of a Flex Catheter to aid in valve alignment to the balloon, tracking, and
positioning of the valve. The delivery system includes a tapered tip to facilitate crossing of the native
valve. The handle contains a Flex Wheel to control flexing of the Flex Catheter, and a Balloon Lock and
Fine Adjustment Wheel to facilitate valve alignment and positioning of the valve within the native annulus.
A stylet is included within the guidewire lumen of the delivery system. The Balloon Catheter has
radiopaque Valve Alignment Markers defining the working length of the balloon. A radiopaque Center
Marker in the balloon is provided to help with valve positioning. A radiopaque Triple Marker proximal to
the balloon indicates the Flex Catheter position during deployment. The inflation parameters for valve
deployment are:
Table 3
Model
9600LDS20 20 mm 11 mL 7 atm
9600LDS23 23 mm 17 mL 7 atm
9600LDS26 26 mm 23 mL 7 atm
9600LDS29 29 mm 33 mL 7 atm
Nominal
Balloon
Diameter
Nominal
Inflation
Volume
Rated Burst
Pressure
(RBP)
2
Page 3

Figure 2: Edwards Commander Delivery System
• Qualcrimp Crimping Accessory
The Qualcrimp crimping accessory (packaged with the Edwards Commander delivery system) is used
during crimping of the valve.
• Edwards eSheath Introducer Set
Refer to the Edwards eSheath Introducer Set instructions for use for device description.
• Edwards Crimper
Refer to the Edwards Crimper instructions for use for device description.
2.0 Indications
The Edwards SAPIEN 3 transcatheter heart valve, Model 9600TFX, and accessories are indicated for
relief of aortic stenosis in patients with symptomatic heart disease due to severe native calcific aortic
stenosis who are judged by a Heart Team, including a cardiac surgeon, to be at intermediate or greater
risk for open surgical therapy (i.e., predicted risk of surgical mortality ≥ 3% at 30 days, based on the
Society of Thoracic Surgeons (STS) risk score and other clinical co-morbidities unmeasured by the STS
risk calculator).
3.0 Contraindications
The valve and delivery systems are contraindicated in patients who cannot tolerate an
anticoagulation/anti pla tel et r egim en or who have active bacterial endocarditis or other active infections.
4.0 Warnings
• Observation of the pacing lead throughout the procedure is essential to avoid the potential risk of
pacing lead perforation.
• There ma y be an increased risk of stroke in transcatheter aortic valve replacement procedures, as
compared to balloon aortic valvuloplasty or other standard treatments in high or greater risk patients.
• The devices are designed, intended, and distributed for single use only. Do not resterilize or reuse
the devices. There are no data to support the sterility, nonpyrogenicity, and functionality of the
devices after reprocessing.
• Incorrect sizing of the valve may lead to paravalvular leak, migration, embolization and/or annul ar
rupture.
• Accelerated deterioration of the valve may occur in patients with an altered calcium metabolism.
• Prior to delivery, the valve must remain hydrated at all times and cannot be exposed to solutions
other than its shipping storage solution and sterile physiologic rinsing solution. Valve leaflets
3
Page 4

mishandled or damaged during any part of the procedure will require replacement of the valve.
• Caution should be exercised in implanting a valve in patients with clinically significant coronary artery
disease.
• Patients with pre-existing mitral valve devices should be carefully assessed prior to implantation of
the valve to ensure proper valve positioning and deployment.
• Do not use the valve if the tamper evident seal is broken, the storage solution does not completely
cover the valve, the temperature indicator has been activated, the valve is damaged, or the expiration
date has elapsed.
• Do not mishandle the delivery system or use it if the packaging or any components are not sterile,
have been opened or are damaged (e.g. kinked or stretched), or the expiration date has elapsed.
• Use of excessive contrast media may lead to renal failure. Measure the patient’s creatinine level prior
to the procedure. Contrast media usage should be monitored.
• Patient injury could occur if the delivery system is not un-flexed prior to removal.
• Care should be exercised in patients with hypersensitivities to cobalt, nickel, chromium, molybdenum,
titanium, manganese, silicon, and/or polymeric materials.
• The procedure should be conducted under fluoroscopic guidance. Some fluoroscopically guided
procedures are associated with a risk of radiation injury to the skin. These injuries may be painful,
disfiguring, and long-lasting.
• Valve recipients should be maintained on anticoagulant/antiplatelet therapy, except when
contraindicated, as determined by their physician. This device has not been tested for use without
anticoagulation.
• Do not add or apply antibiotics to the storage solution, rinse solutions, or to the valve.
5.0 Precautions
• Long-term durability has not been established for the valve. Regular medical follow-up is advised to
evaluate valve performance.
• Glutaraldehyde may cause irritation of the skin, eyes, nose and throat. Avoid prolonged or repeated
exposure to, or breathing of, the solution. Use only with adequate ventilation. If skin contact occurs,
immediately flush the affected area with water; in the event of contact with eyes, seek immediate
medical attention. For more information about glutaraldehyde exposure, refer to the Mater ia l Safet y
Data Sheet available from Edwards Lifesciences.
• To maintain proper valve leaflet coaptation, do not overinflate the deployment balloon.
• Appropriate antibiotic prophylaxis is recommended post-procedure in patients at risk for prosthetic
valve infection and endocar ditis .
• Safety, effectiveness, and durability have not been established for valve-in-valve procedures.
• Safety and effectiveness have not been established for patients with the following
characteristics/comorbidities:
o Non-calcified aortic annulus
o Severe ventricular dysfunction with ejection fraction < 20%
o Congenital unicuspid or congenital bicuspid aortic valve
o Mixed aortic valve disease (aortic stenosis and aortic regurgitation with predominant aortic
regurgitation > 3+)
o Pre-existing prosthetic heart valve or prosthetic ring in any position
o Severe mitral annular calcification (MAC), severe (> 3+) mitral insufficiency, or Gorlin
syndrome
4
Page 5

o Blood dyscrasias defined as: leukopenia (WBC < 3000 cells/mL), acute anemia
(Hb < 9 g/dL), thrombocytopenia (platelet count < 50,000 cells/mL), or history of
bleeding diathesis or coagulopathy
o Hypertrophic cardiomyopathy with or without obstruction (HOCM)
o Echocardiographic evidence of intracardiac mass, thrombus, or vegetation
o A known hypersensitivity or contraindication to aspirin, heparin, ticlopidine (Ticlid™), or
clopidogrel (Plavix™), or sensitivity to contrast media, which cannot be adequately premedicate d
o Significant aortic disease, including abdominal aortic or thoracic aneurysm defined as maximal
luminal diameter 5 cm or greater; marked tortuosity (hyperacute bend), aortic arch atheroma
(especially if thick [> 5 mm], protruding, or ulcerated) or narrowing (especially with calcification
and surface irregularities) of the abdominal or thoracic aorta, severe “unfolding” and tortuosity of
the thoracic aorta
o Access characteristics that would preclude safe placement of 14F or 16F Edwards eSheath
Introducer Set, such as severe obstructive calcification or severe tortuosity
o Bulky calcified aortic valve leaflets in close proximity to coronary ostia
6.0 Potential Adverse Events
Potential risks associated with the overall proc e dur e including potential access complications associated
with standard cardiac catheterization, balloon valvuloplasty, the potential risks of conscious sedation
and/or general anesthesia, and the use of angiography:
• Death
• Stroke/transient ischemic attack, clusters or neurological deficit
• Paralysis
• Permanent disability
• Respiratory insufficiency or respiratory failure
• Hemorrhage requiring transfusion or intervention
• Cardiovascular injury including perforation or dissection of vessels, ventricle, myocardium or valvular
structures that may require intervention
• Pericardial effusion or cardiac tamponade
• Embolization including air, calcific valve m ater ial or thr ombus
• Infection including septicemia and endocarditis
• Heart failure
• M yocar dial inf ar ction
• Renal insufficiency or renal failure
• Conduction system defect which may require a permanent pacemaker
• Arrhythmia
• Retroperitoneal bleed
• AV fistula or pseudoaneurysm
• Reoperation
• Ischemia or nerve injury
• Restenosis
• Pulm onary edema
• Pleural effusion
5
Page 6

• Bleeding
• Anemia
• Abnormal lab values (including electrolyte imbalance)
• Hypertension or hypotension
• Allergic reaction to anesthesia, contrast media, or device materials
• Hematoma
• Syncope
• Pain or changes at the access site
• Exercise intolerance or weakness
• Inflammation
• Angina
• Heart murmur
• Fever
Additional potential risks associated with the use of the valve, delivery system, and/or accessories
include:
• Cardiac arrest
• Cardiogenic shock
• Emergency cardiac surgery
• Cardiac failure or low cardiac output
• Coronary flow obstruction/transvalvular flow disturbance
• Device thrombosis requiring intervention
• Valve thrombosis
• Device embolization
• Device migration or malposition requiring intervention
• Valve deployment in unintended location
• Valve stenosis
• Structural valve deterioration (wear, fracture, calcification, leaflet tear/tearing from the stent posts,
leaflet retraction, suture line disruption of components of a prosthetic valve, thickening, stenosis)
• Device degeneration
• Paravalvular or transvalvular leak
• Valve regurgitation
• Hemolysis
• Device explants
• Nonstructural dysfunction
• Mechanical failure of delivery system, and/or accessories
• Non-emergent reoperation
6
Page 7

7.0 Directions for Use
Model
Edwards SAPIEN 3
Valve
Edwards Commander
Delivery System*
Edwards Balloon
Catheter
* Includes the Qualcrimp Crimping Accessory,2-piece Crimp Stopper and loader
** Or other compatible sheath provided by Edwards Lifesciences
7.1 Required Equipment
Product Name
20 mm System
(9600CM20A)
Table 4:
23 mm System
(9600CM23A)
26 mm System
(9600CM26A)
29 mm System
(9600CM29A)
Transcatheter Heart
Edwards eSheath
Introducer Set**
Edwards Crimper 9600CR
9600TFX (20 mm) 9600TFX (23 mm) 9600TFX (26 mm) 9600TFX (29 mm)
9600LDS20 9600LDS23 9600LDS26 9600LDS29
914ES 914ES 914ES 916ES
9350BC16 9350BC20 9350BC23 9350BC25
Inflation devices provided by Edwards Lifesciences
Additional Equipment:
• 20 cc syringe or larger (x2)
• 50 cc syringe or larger
• High-pressure 3-way stopcock (x2)
• Standard cardiac catheterization lab equipment
• Fluoroscopy (fixed, mobile or semi-mobile fluoroscopy systems appropriate for use in percutaneous
coronary interventions)
• Transesophageal or transthoracic echocardiography capabilities
• Exchange length 0.035 inch (0.89 mm) extra-stiff guidewire
• Temporary pacemaker (PM) and pacing lead
• Sterile rinsing basins, physiological saline, heparinized saline, 15% diluted radiopaque contrast
medium
• Sterile table for valve and device preparation
7.2 Valve Handling and Preparation
Follow sterile technique during device preparation and im plantat ion.
7.2.1 Valve Rinsing Procedure
Before opening the valve jar, carefully examine for evidence of damage (e.g. a cracked jar or lid, leakage,
or broken or missing seals).
CAUTION: Valves from containers f oun d t o be da ma ged, lea ki ng, with o ut adequate steril an t, or
missing intact se als m us t n ot be us ed for im pl antation.
7
Page 8

Step Procedure
1
2
Set up two (2) sterile bowls with at least 500 mL of sterile physiological saline to thoroughly rinse the
glutaraldehyde sterilant from the valve.
Carefully remove the valve/holder assembly from the jar without touching the tissue. Verify the valve
serial identification number with the number on the jar lid and record in the patient information
documents. Inspect the valve for any signs of damage to the frame or tissue.
Rinse the valve as follows: Place the valve in the first bowl of sterile, physiological saline. Be sure
the saline solution completely covers the valve and holder. With the valve and holder submerged,
slowly agitate (to gently swirl the valve and holder) back and forth for a minimum of 1 minute.
Transfer the valve and holder to the second rinsing bowl of sterile physiological sal ine and g ently
agitate for at least one more minute. Ensure the rinse solution in the first bowl is not used. The
3
valve should be left in the final rinse solution until needed to prevent the tissue from drying.
CAUTION: Do not allow the valve to come into contact with the bottom or sides of the rinse bowl
during agitation or swirling in the rinse solution. Direct contact between the identification tag and
valve is also to be avoided during the rinse procedure. No other objects should be placed in the
rinse bowls. The valve should be kept hydrated to prevent the tissue from drying.
7.2.2 Prepare the Com p o n ents
Refer to the Edwards eSheath Introducer Set, Edwards Crimper and Edwards Balloon Catheter
instructions for use for device preparation.
Step Procedure
Visually inspect all components for damage. Ensure the Edwards Commander delivery system is fully
unflexed and the balloon catheter is fully advanced in the flex catheter.
1
WARNING: To prevent possible damage to the balloon shaft, ensure that the proximal end of the
balloon shaft is not subjected to bending.
2 Flush the flex catheter.
3 Carefully remove the distal balloon cover from the delivery system.
Remove the stylet from the distal end of the guidewire lumen and set aside. Flush the guidewire
4
5
6
7
8
9
10
lumen with heparinized saline and insert the stylet back into the distal end of the guidewire lumen.
Note: Failure to insert the stylet back into the guidewire lumen may result in damage to the lumen
during crimping process.
Place the delivery system into the default position and make sure that the flex catheter tip is covered
by the proximal balloon cover. Unscrew the loader cap from the loader tube and flush the lo ader cap.
Place the loader cap over the proximal balloon cover and onto the flex catheter with the inside of the
cap oriented towards the distal tip.
Fully advance the balloon catheter in the flex catheter.
Peel off the proximal balloon cover over the blue section of the balloon shaft.
Attach a 3-way stopcock to the balloon inflation port. Partially fill a 50 cc or larger syringe with
15-20 mL diluted contrast medium and attach to the 3-way stopcock.
Fill the inflation device provided by Edwards Lifesciences with excess volume relative to the indicated
inflation volume. Lock the inflation device and attach to the 3-way stopcock.
Close the 3-way stopcock to the Inflation device provided by Edwards Lifesciences and de-air the
system using the 50 cc or larger syringe. Slowly release the plunger and leave zero-pressure in the
system.
Close the stopcock to the delivery system. By rotating the knob of the inflation device provided by
Edwards Lifesciences, transfer the contrast medium into the syringe to achieve the appropriate
volume required to deploy the valve.
8
Page 9

Step Procedure
Close the stopcock to the 50 cc or larger syringe. Remove the syringe. Verify that the inflation volu me
11
is correct and lock the Inflation device provided by Edwards Lifesciences.
CAUTION: Maintain the Inflation device provided by Edwards Lifesciences in the locked
position until valve deployment.
7.2.3 Mount and Crimp the Valve on the Delivery System
Step Procedure
1
2
3 Remove the valve from the holder and remove the ID tag.
4 Attach the 2-piece crimp stopper to the base of the crimper and click into place.
5
6
7
8 Crimp the valve until it reaches the Qualcrimp Stop located on the 2-piece Crimp Stopper.
9
10
Set up two (2) additional sterile bowls with at least 100 mL of sterile physiological saline to thoroughly
rinse the Qualcrimp crimping accessory.
Completely submerge the Qualcrimp crimping accessory in the first bowl and gently compress it to
ensure complete saline absorption. Slowly swirl the Qualcrimp crimping accessory for a minimum of
1 minute. Repeat this process in the second bowl.
With the crimper in the open position, gently place the valve into the crimper aperture. Gradually
crimp the valve until it fits into the Qualcrimp crimping accessory.
Place the Qualcrimp crimping accessory over the valve making sure the valve is parallel to the edge
of the Qualcrimp crimping accessory.
Place the valve and Qualcrimp crimping accessory in crimper aperture. Insert the delivery system
coaxially within the valve on the Valve Crimp Section (2-3 mm distal to the balloon shaft) with the
inflow (outer skirt) end of th e valve towards the distal end of the delivery system.
Gently remove the Qualcrimp crimping accessory from the valve. Remove the Qualcrimp Stop from
the Final Stop, leaving the Final Stop in place.
Fully crimp the valve until it reaches the Final Stop.
NOTE: Ensure that the Valve Crimp Section remains coaxial within the valve.
11 Repeat the full crimp of the valve two more times for a total of three full crimps.
12 Pull the balloon shaft and lock in the default position.
Flush the loader with heparinized saline. Immediately advance the valve into the loader until the
13
14
tapered tip of the delivery system is exposed.
CAUTION: To prevent possible leaflet damage, the valve should not remain fully crimped
and/or in the loader for over 15 minutes.
Attach the loader cap to the loader, re-flush the delivery system through the flush port and close the
stopcock to the delivery system.
Remove the stylet and flush the guidewire lumen of the delivery system.
CAUTION: Keep the valve hydrated until ready for implantation.
CAUTION: The physician must verify correct orientation of the valve prior to its implantation;
its inflow (outer skirt) end should be oriented distally towards the tapered tip.
7.3 Valvuloplasty and Valve Delivery
Valvuloplasty and valve delivery should be performed under conscious sedation and/or general
anesthesia with hemodynamic monitoring in a catheterization lab/hybrid operating room with fluoroscopic
and echocardiographic imaging capabilities.
Administer heparin to maintain the ACT at ≥ 250 sec during the procedure.
CAUTION: Use of excessive contrast media may lead to renal failure. Measure the patient’s
creatinine level prior to the procedure. Contrast media usage should be monitored.
CAUTION: Procedure may require an arterial cut-down with surgical closure of the puncture si te
due to the size of the arteriotomy.
9
Page 10

7.3.1 Baseline Parameters
Step Procedure
1 Per form a supra-aortic angiogram with fluorosc opic view perpendicular to the aortic valve.
2
3 Introduce a pacemaker (PM) lead until its distal end is positioned in the right ventricle.
4 Set the stimulation parameters to obtain 1:1 capture, and test pacing.
Evaluate the distance of the left and right coronary ostia from the aortic annulus in relation to the valve
frame height.
7.3.2 Valvuloplasty
Refer to Edwards Balloon Catheter Instructions for Use (IFU) for information on device
preparation and handling.
Note: Rapid ventricular pacing s h o u ld be performed when using the Edwards Balloon Catheter for
valvuloplasty prior to aortic transcatheter valve implantation.
After placement of the balloon at the intended site, begin rapid ventricular pacing. Once the systolic blood
pressure has decreased to 50 mmHg or below, balloon inflation can commence.
CAUTION: Valve implantation should no t b e carried out if the balloon canno t be ful ly inflated
during valvuloplasty.
7.3.3 Valve Delivery
Step Procedure
1
2 Insert the loader into the sheath until the loader stops.
3
Prepare and insert the Edwards eSheath Introducer Set. Refer to the Edwards eSheath Introducer
Set IFU for information on device preparation and handling.
Advance the Edwards Commander delivery system, with the Edwards logo facing up, through the
sheath until the valve exits the sheath. Retract the loader to the proximal end of the delivery system.
NOTE: Maintain the proper orientation of the flex catheter (with the Edwards logo facing up)
throughout the procedure.
CAUTION: If accessing femorally or via the iliac, the valve should not be advanced through
the sheath if the sheath tip is not past the aortic bifurcation.
CAUTION: To prevent possible leaflet damage, the valve should not remain in the sheath for
over 5 minutes.
In a straight section of the aorta, initiate valve alignment by disengaging the Balloon Lock and pulling
the balloon catheter straight back until part of the Warning Marker is visible. Do not pull past the
Warning Marker.
WARNING: To prevent possible damage to the balloon shaft, ensure that the proximal end of
the balloon shaft is not subjected to bending.
4
5
6
Engage the Balloon Lock.
Use the Fine Adjustment Wheel to position the valve between the valve alignment markers.
CAUTION: Do not turn the Fine Adjustment Wheel if the Balloon Lock is not engaged.
WARNING: Do not position the valve past the distal Valve Alignment Marker. This will prevent
proper valve deployment.
CAUTION: Maintain guidewire position in the left ventricle during valve alignment.
Advance the catheter and use the flex wheel, if needed, and cross the aortic valve.
NOTE: Verify the Edwards logo is facing up. The delivery system articula tes in a direction
opposite from the flush port.
If additional working length is needed, remove the loader by unscrewing the loader cap and peeling
the loader tubing from the delivery system.
10
Page 11

Step Procedure
Disengage the Balloon Lock and retract the tip of the Flex Catheter to the center of the Triple Marker.
blood pressure has decreased to 50 mmHg or below, balloon
7
8 Verify the correct position of the valve with respect to the aortic annulus.
9
10
11
Engage the Balloon Lock.
As necessary, utilize the Flex Wheel to adjust the co-axiality of the valve and the Fine Adjustment
Wheel to adjust the position of the valve.
Before deployment, ensure that the valve is correctly positioned between the Valve Alignment
Markers and the Flex Catheter tip is over the Triple Marker.
Begin valve deployment:
• Unlock the Inflation device provided by Edwards Lifesciences.
• Begin rapid pacing; once systolic
inflation can commence.
• Deploy the valve by inflating the balloon with the entire volume in the Inflation device provided by
Edwards Lifesciences, hold for 3 seconds and confirm that the barrel of the inflation device is
empty to ensure complete inflation of the balloon.
• Deflate the balloon. When the balloon catheter has been completely deflated, turn off the
pacemaker.
7.3.4 System Removal
Step Procedure
Unflex the delivery system while retracting the device, if needed. Verify that the Flex Catheter tip is
1
locked over the Triple Marker and remove the delivery system from the sheath.
CAUTION: Patient injury could occur if the delivery system is not unflexed prior to removal.
2
3
Remove all devices when the ACT level is appropriate. Refer to the Edwards eSheath Introducer Set
instructions for use for device removal.
Close the access site.
8.0 How Supplied
STERILE: The valve is supplied sterilized with glutaraldehyde solution. The delivery system is supplied
sterilized with ethylene oxide gas.
8.1 Storage
The valve must be stored at 10 °C to 25 °C (50 °F to 77 °F). Each jar is shipped in an enclosure
containing a temperature indicator to detect exposure of the valve to extreme temperature.
The delivery system should be stored in a cool, dry place.
9.0 MR Safety
MR Conditional
Non-clinical testing has demonstrated that the Edwards SAPIEN 3 transcatheter heart valve is MR
Conditional. A patient with this device can be scanned safely, immediately after placement of this device
under the following conditions:
• Static magnetic field of 1.5 tesla or 3 tesla
• Maximum spatial gradient field of 2500 gauss/cm (25 T/m) or less
• Maximum MR system reported, whole body averaged specific absorption rate (SAR) of 2 W/kg
(Normal Operating Mode)
Under the scan conditions defined above, the SAPIEN 3 transcatheter heart valve is expected to produce
a maximum temperature rise of 3.0 ºC after 15 minutes of continuous scanning.
11
Page 12

In non-clinical testing, the image artifact caused by the device extends as far as 14.5 mm from the implant
for spin echo images and 30 mm for gradient echo images when scanned in a 3.0T MRI system. The
artifact obscures the device lumen in gradient echo images.
The implant has not been evaluated in MR systems other than 1.5 or 3.0T.
10.0 Patient Information
Patient education brochures are provided to each site and should be given to the patient to inform them of
the risks and benefits of the procedure and alternatives in adequate time before the procedure to be read
and discussed with their physician. A copy of this brochure may also be obtained from Edwards
Lifesciences by calling 1.800.822.9837. A patient implant card request form is provided with each
transcatheter heart valve. After implantation, all requested information should be completed on this form.
The serial number may be found on the package and on the identification tag att ached to the t ranscathete r
heart valve. The original form should be returned to the Edwards Lifesciences address indicated on the form
and upon receipt, Edwards Lifesciences will provide an identification card to the patient.
11.0 Recovered Valve and Device Disposal
The explanted valve should be placed into a suitable histological fixative such as 10% formalin or 2%
glutaraldehyde and returned to the company. Refrigeration is not necessary under these circumstances.
Contact Edwards Lifesciences to request an Explant Kit.
Used delivery system may be disposed of in the same manner that hospital waste and biohazard ous
materials are handled. There are no special risks related to the disposal of these devices.
12.0 Clinical Studies
SUMMARY OF PRIMARY CLINICAL STUDY
The PARTNER II Trial Overview, SAPIEN 3 Valve
SAPIEN 3 High Risk and Inoperable Cohort: The SAPIEN 3 High Risk and Inoperable Cohort of the
PARTNER II trial (PIIS3HR) was a single arm, non-randomized, historical-controlled study to compare the
third generation Edwards SAPIEN 3 valve system with the first generation Edwards SAPIEN valve system
in patients who either have high risk for surgery or cannot undergo surgery (inoperable). The valve sizes
used in the PIIS3HR trial included only the 23, 26 and 29 mm sizes. The 20 mm valve size was
introduced into the trial after enrollment was completed with the three larger sizes, thus a separate nested
registry, NR7, with identical inclusion/exclusion criteria as the PIIS3HR Cohort except for the aortic
annulus diameter, was created to collect data for the 20 mm valve. Data from the PIIS3HR cohort and
NR7 are pooled for the statistical analyses. For convenience, this combined cohort is referred to as
“PIIS3HR” hereafter.
The database included 583 eligible patients enrolled at 29 investigational sites in the U.S.
The study used an independent Data Safety Monitoring Board (DSMB) that was instructed to notify
Edwards Lifesciences of any safety or compliance issues, a Clinical Events Committee (CEC) that was
responsible for adjudicating endpoint related events reported during the trial per a priori established
VARC 2 definitions
[1]
, an ECG core laboratory for independent analysis of rhythm, and an
echocardiographic core laboratory for independently analyzing all echocardiograms.
SAPIEN 3 Intermediate Risk Cohort: The PIIS3i Cohort of the PARTNER II trial was a single arm, non-
randomized, historical-controlled study to compare TAVR with the Edwards SAPIEN 3 valve system to the
surgical aortic valve replacement (SAVR) arm from the previous PARTNER II trial Cohort A (PIIA-SAVR)
in patients who were judged by a heart team to be at intermediate risk for open surgical therapy. The
valve sizes used in the PIIS3i study included the 20, 23, 26, and 29 mm sizes.
Patients in PIIS3i were treated between February 2014 and September 2014. Patients in PIIA-SAVR
were treated between January 2012 and November 2013. The database reflected data collected through
December 10, 2015 and included 1,078 patients in PIIS3i enrolled at 51 investigational sites in the U.S
and 1,021 patients in PIIA-SAVR enrolled at 57 investigational sites in the U.S.
12
Page 13

The PIIS3i study used an independent Data Safety Monitoring Board (DSMB) that was instructed to notify
SAP IEN 3
Access
Eligible Patient
Population (EPP)
Valve Implant
(VI) Population
Eligible Patient Population (EPP) consists of all enrolled patients who received
laboratory/hybrid suite.
Edwards Lifesciences of any safety or compliance issues and a Clinical Events Committee (CEC) that
was responsible for adjudicating endpoint related events reported during the trial in accordance with the
pre-specified, primarily Valve Academic Research Consortium-2 VARC-2 definitions
[1]
, with the following
exceptions:
• Prosthetic valve dysf uncti o n was adj udic at ed per VAR C -1
• Aortic valve reintervention was adjudicated per protocol definition
• Rehospitalization for symptoms of aortic stenosis and/or complications of the valve procedure
were adjudicated using the protocol and VARC-2 definitions as guidelines
The events in the PIIA-SAVR cohort were adjudicated by the CEC in accordance with the pre-specified,
primarily VARC-1 definitions, with the following exceptions:
• Acute Kidney Injury (AKI) was adjudicated with a modified VARC-1 definition in which the CEC
applied the 72-hour staging window to any AKI event that occurred within 30-days
• Aortic valve reintervention wer e adju dicat ed per the protocol definition
• Rehospitalization for symptoms of AS and/or complications of the valve procedure were
adjudicated using the protocol and VARC-1 as guidelines
• Bleeding events were adjudicated irrespective of whether there was an identifiable, overt source
of bleeding
An electrocardiogram (ECG) core laboratory was used for independent analysis of rhythm, an
echocardiographic core laboratory for echocardiograms, and a computerized tomography (CT) core
laboratory for baseline CTs for annulus dimensions.
PARTNER II SAPIEN 3 HIGH-RISK/INOPERABLE COHORT
Accountability
All 583 eligible patients were successfully implanted with a SAPIEN 3 valve, which constitutes the Valve
Implant (VI) population. Among the VI population, 491 patients were implanted via the transfemoral (TF)
access route, and 92 patients via the transapical (TA) or transaortic (TAo) access route.
Table 5:
Patient Accountability
SAP IEN 3
Valve
Overall
583 491 92
583 491 92
treatment assignment from the database and entered into the catheterization
laboratory/hybrid suite and who remained eligible to receive the implant.
Valve Implant (VI) Population consists of all enrolled patients who received a
SAPIEN 3 valve, and retained the valve upon leaving the catheterization
Study Populatio n Dem o gr a phic s a nd Bas el i ne Pa ra mete rs
The demographics of the study population are summarized in Table 6, which are typical of a TAVR study
performed in the U.S.
13
SAP IEN 3
Valve
Transfemoral
Access
Valve
Non-
Transfemoral
Page 14

Transfemoral
SAP IEN 3
Transfemoral
(N= 92)
Age, yr
82.6 ± 8.1
82.8 ± 8.2
81.7 ± 7.5
Male sex, no. (%)
338 (58.0%)
277 (56.4%)
61 (66.3%)
STS score
8.6 ± 3.7
8.4 ± 3.5
10.0 ± 4.3
New York Heart Association (NYHA) class, no. (%):
I/II
58 (9.9%)
51 (10.4%)
7 (7.6%)
III/IV
525 (90.1%)
440 (89.6%)
85 (92.4%)
Coronary artery disease, no. (%)
444 (76.2%)
360 (73.3%)
84 (91.3%)
Previous myocardial infarction, no. (%)
117 (20.1%)
87 (17.7%)
30 (32.6%)
Previous intervention, no. (%)
Coronary-artery bypass gr af ting (C ABG)
193 (33.1%)
145 (29.5%)
48 (52.2%)
Percutaneous coronary intervention (PCI)
199 (34.1%)
163 (33.2%)
36 (39.1%)
Prior aortic valvuloplasty
62 (10.6%)
49 (10.0%)
13 (14.1%)
Cerebral vascular accident ( CVA), no. (%)
64 (11.0%)
53 (10.8%)
11 (12.0%)
Peripheral vascular disease, no. (%)
205 (35.2%)
155 (31.6%)
50 (54.3%)
Chronic obstructive pulmonary disease (COPD),
no. (%):
Any
259 (44.6%)
216 (44.1%)
43 (47.3%)
Oxygen-dependent
68 (11.8%)
58 (11.9%)
10 (11.0%)
Atrial fibrillation, no. (%)
255 (43.7%)
212 (43.2%)
43 (46.7%)
Permanent pacemaker, no. (%)
95 (16.3%)
78 (15.9%)
17 (18.5%)
Severe pulmonary hypertension, no. (%)
30 (5.1%)
24 (4.9%)
6 (6.5%)
Frailty, no. (%)
180 (30.9%)
162 (33.0%)
18 (19.6%)
Chest deformities that preclude an open chest
procedure, no. (%)
4 (0.7%)
3 (0.6%)
1 (1.1%)
Cirrhosis, no. (%)
11 (1.9%)
9 (1.8%)
2 (2.2%)
Echocardiographic findings
Effective Orifice Area (EOA), cm2
0.7 ± 0.2
0.7 ± 0.2
0.7 ± 0.1
Mean aortic-valve gradient, mmHg
45.5 ± 14.3
45.7 ± 14.4
44.0 ± 13.2
Mean left ventricular ejection fraction (LVEF), %
56.4 ± 14.8
57.0 ± 14.5
53.2 ± 15.9
Moderate or severe mitral regurgitation, no./total
no. (%)
69/541
(12.8%)
63/461
(13.7%)
6/80
(7.5%)
Table 6:
Patient Demographics and Baseline Characteristics –
PIIS3HR VI Population
Characteristic
SAP IEN 3
Valve
Overall
(N= 583)
SAP IEN 3
Valve
Access
(N= 491)
Valve
Non-
Access
Safety and Effectiveness Results
Primary Endpoint
The composite rate of all-cause mortality, all stroke, and AI ≥ moderate at 30 days was 6.7% in the
SAPIEN 3 cohort and 15.6% in the SAPIEN cohort, as shown in Table 7. The resulting proportion
difference in the average treatment effect on the treated (ATT; [2]) was -6.9% (90% CI: [-13.3%, -0.5%]).
Since the upper limit of the CI was < 7.5%, the non–inferiority was met.
14
Page 15

Table 7:
Weighted Proportion
on the Treated (ATT)
Composite of Death, Stroke
and AI ≥ Moderate)
6.7%
[5.1%, 8.6%]1
15.6%
[12.6%, 19.5%]1
-6.9%
[-13.3%, -0.5%]2
1
For each individual study, the two-sided 90% stratified Wilson confidence interval was provided.
SAP IEN 3 Valve
(N = 583)
SAPIEN Valve
(N = 326)
No. Pts with
K-M Estimated
(95% CI)
No. Pts with
M Estimated Event
2.2%
([1.3%, 3.8%])
4.6%
([2.8%, 7.5%])
Cardiac
Death
1.4%
([0.7%, 2.7%])
3.1%
([1.7%, 5.7%])
1.6%
([0.8%, 3.0%])
4.3%
([2.6%, 7.2%])
1
Kaplan-Meier (K-M) estimates at 30 days used time to first event for each patient. Events occurring after 30 days
were not included in this analysis.
Primary Endpoint Analysis –
Non-Inferiority Test SAPIEN 3 Valve (PIIS3HR VI Population) vs. SAPIEN Valve
SAP IEN 3
Event at 30 days
Valve
(N = 583)
2
The Wald-type two-sided 90% confidence interval using weighted mean and SD is provided
SAPIEN
Valve
(N = 326)
Difference in Average
Treatment Effect
The Kaplan-Meier (K-M) estimates for all-cause mortality, cardiac mortality, and all stroke at 30 days for
the SAPIEN 3 cohort and the SAPIEN cohort are provided in Table 8.
Table 8:
Death and Stroke at 30 Days –
SAP IEN 3 Valve vs. SAPIEN Valve (VI Population)
Event at 30
Days
Death 13 13
All Stroke 9 9
No.
Events
8 8
Events
Event Rate1
No.
Events
15 15
10 10
14 14
Events
K-
Rate (95% CI)
Secondary Endpoints
Aortic insufficiency by visit is provided in Figure 3.
15
Page 16

Figure 3:
Aortic Insufficiency by V isit –
SAP IEN 3 Valve (PIIS3HR VI Population) vs. SAPIEN Valve
Weighted Proportion
Treated (ATT)
1
95% Clopper-Pearson Exact confidence interval.
The proportion of patients with AI ≥ moderate at 30 days was 3.0% in the SAPIEN 3 cohort and 14.3% in
the SAPIEN cohort, which were found to be statistically significantly different (p=0.0051; Table 9).
Table 9:
Aortic Insufficiency at 30 Days
(SAPIEN 3 Valve vs. SAPIEN Valve VI Population)
SAP IEN 3
Event at 30 Days
Valve
(N = 583)
AI ≥Moderate, n/Total
no. (%) [95% CI]
16/532
(3.0%)
[1.7%, 4.8%]
2
The Wald-type two-sided 90% confidence interval using weighted mean and SD is provided
SAPIEN Valve
(N = 326 )
1
40/280
(14.3%)
[10.4%,
18.9%]
1
Difference in Average
Treatment Effect on the
-13.1%
[-22.2%, -3.9%]
2
P-value
0.0051
The rate of major vascular complications at 30 days post implantation is shown in Figure 4. The rate was
5.0% for the SAPIEN 3 cohort and 10.1% for the SAPIEN cohort, which were foun d to be not statistically
significantly different (p=0.0578; Table 10).
16
Page 17

Figure 4:
Major Vascular Complications at 30 Days –
SAP IEN 3 Valve vs. SAPIEN Valve (VI Population)
Weighted
reatment
Treated (ATT)
Major Vascular
(%) [95% CI]
29/583
[3.4% , 7.1%]
33/326
[7.1% , 13.9%]1
1
95% Clopper-Pearson Exact confidence interval.
2
Table 10:
Major Vascular Complications at 30 Days –
SAP IEN 3 Valve vs. SAPIEN Valve (VI Population)
SAP IEN 3
Event at 30 Day
Valve
(N = 583)
Complications, n/Total no.
The Wald-type two-sided 90% confidence interval using weighted mean and SD is provided.
(5.0%)
SAPIEN
Valve
(N = 326)
(10.1%)
Proportion
Difference in
Average T
Effect on the
-8.0%
[-16.2%, 0.3%]2
P-value
0.0578
Table 11 lists the hypothesis testing of the two secondary endpoints conducted with p-values in
descending order for the Hochberg multiplicity adjustment steps. The largest p-value (p=0.0578 from
major vascular complications) was greater than 0.05. As such, the null hypothesis was not rejected for the
testing of major vascular complications at 30 days. The subsequent testing of AI ≥ moderate at 30 days
had a p-value of 0.0051, which was less than 0.025. As such, the null hypothesis was rejected for
AI ≥ moderate at 30 days, indicating that the SAPIEN 3 cohort was superior over the SAPIEN cohort in
regards to AI ≥ moderate at 30 days.
17
Page 18

Table 11:
Original
p-value
Major Vascular
Days
> 0.05; reject the alternative
testing
AI at 30 Days
0.0051
< 0.025; claim superiority
SAP IEN 3
Access
Composite Event Rate of Death, All Stroke and
AI ≥ Moderate, n/N (%)
Secondary Endpoints for Labeling –
SAP IEN 3 Valve vs. SAPIEN Valve (VI Population)
Endpoints
Complications at 30
0.0578
hypothesis. Proceed to the rest of
Inference
Adverse Events
The key CEC adjudicated adverse events at 30 days are presented in Table 12.
Table 12:
CEC Adjudicated Adverse Events at 30 Days
(PIIS3HR VI Population)
30 Day Adverse Events
SAPIEN 3 Valve
Overall
SAPIEN 3 Valve
Transfemoral
Access
TF
Valve
Non-
Transfemoral
37/545 (6.8 %) 27/463 (5.8 %) 10/82 (12.2 %)
Death
From Any cause, n/N (%) 13/583 (2.2%) 8/491 (1.6%) 5/92 (5.4%)
From cardiovascular cause, n/N (%) 8/583 (1.4%) 5/491 (1.0%) 3/92 (3.3%)
Stroke, n/N (%) 9/583 (1.5%) 8/491 (1.6%) 1/92 (1.1%)
AI ≥ moderate, n/N (%) 16/532 (3.0%) 12/455 (2.6%) 4 /77 (5.2%)
Myocardial Infarction, n/N (%) 3/583 (0.5%) 2/491 (0.4%) 1/92 (1.1%)
Major Vascular Complications, n/N (%) 29/583 (5.0%) 26/491 (5.3%) 3/92 (3.3%)
Acute Kidney Injury, Stage III, n/N (%) 6/583 (1.0%) 4/491 (0.8%) 2/92 (2.2%)
Disabling Bleeding Event, n/N (%) 37/583 (6.3%) 27/491 (5.5%) 10/92 (10.9%)
Aortic Valve Re-Intervention, n/N (%) 6/583 (1.0%) 4/491 (0.8%) 2/92 (2.2%)
Endocarditis, n/N (%) 1/583 (0.2%) 1/491 (0.2%) 0/92 (0.0%)
Conduction Disturbance Requiring Permanent
Pacemaker,
n/N (%)
Other Results
Procedural Information
Overall, the mean duration in the catheterization laboratory/hybrid suite was 192.8 ± 59.3 min, the mean
total procedure time was 86.3 ± 44.2 min, and the mean total anesthesia time was 193.7 ± 62.9 min.
These duration times were slightly shorter in the TF patients. General anesthesia was used in the vast
majority of cases; 15.9% of the TF patients had conscious sedation. Correct positioning of the valve was
achieved in 99.1% of the patients. Five patients (0.9%; including 3 TF patients) were implanted with a
second valve. One patient (0.2%) experienced valve embolization following rupture of the delivery balloon
on annular calcium. This patient was converted to surgical aortic valve replacement and later died from
aortic dissection.
76/583 (13.0%) 65/ 491 (13.2%) 11/ 92 (12.0%)
18
Page 19

Figure 5:
(PIIS3HR VI Population)
Figure 6:
(PIIS3HR VI Population)
Doppler Velocity Index
0.0
0.2
0.4
0.6
0.8
1.0
1.2
1.4
1.6
1.8
2.0
Baseline 30 Day
0.7
1.6
Mean Gradient (mmHg)
0
10
20
30
40
50
60
70
80
90
100
110
Baseline 30 Day
45.5
11.1
Valve Performance
The mean EOA increased from 0.7 ± 0.2 cm2 at baseline to 1.6 ± 0.4 cm2 at 30 days, as shown in
Figure 5.
Effective Orifice Area
The average mean gradient decreased from 45.5 ± 14.3 mmHg at baseline to 11.1 ± 4.5 mmHg at 30
days, as show n in Figure 6.
Mean Gradient
19
Page 20

Figure 7:
(PIIS3HR VI Population)
Figure 8:
(PIIS3HR VI Population)
Peak Gradient (mmHg)
0
10
20
30
40
50
60
70
80
90
100
110
Baseline 30 Day
75.8
21.2
None Trace Mild
Mild-Moderate Moderate Moderate-Severe
Severe
Percentage
0
20
40
60
80
100
Baseline 30 Day
16%
30%
32%
32%
34%
27%
10%
8%
6%
The mean peak gradient decreased from 75.8 ± 22.6 mmHg at baseline to 21.2 ± 8.5 mmHg at 30 days,
as shown in Figure 7.
Peak Gradient
The proportion of patients with AI ≥ moderate was 7.3% at baseline and 3.0% at 30 days, as shown in
Figure 8.
Aortic Insufficiency
20
Page 21

Figure 9:
(PIIS3HR VI Population)
Figure 10:
(PIIS3HR VI Population)
None
Trace Mild
Mild-Moderate Moderate Moderate-Severe
Severe
Percentage
0
20
40
60
80
100
30 Day
33%
29%
28%
8%
1 2
3 4
Percent
0
20
40
60
80
100
All Patients Transapical/Transaortic Transfemoral
Baseline 30 Day Baseline 30 Day
Baseline 30 Day
10%
60%
30%
45%
42%
11%
8%
64%
28%
36%
45%
14%
5%
10%
59%
31%
46%
42%
11%
The proportion of patients with aortic paravalvular leak (PVL) ≥ moderate was 2.9% at 30 days, as shown
in Figure 9.
Aortic Paravalvular Leak
NYHA
The NYHA class by visit is shown in Figure 10. For all patients, the mean NYHA class was 3.2 ± 0.6 at
baseline and 1.7 ± 0.7 at 30 days.
NYHA Class by Visit
21
Page 22

Six Minute Walk Test (6MWT)
The improvement in mean 6MWT distance was 38.5 ± 110.2 meters from baseline to 30 days for all
patients, 42.6 ± 107.8 meters for all TF patients, and 15.9 ± 121.2 meters for all TA/TAo patients.
Length of Stay (LoS)
The overall mean LoS was 6.8 ± 4.8 days, which included 3.0 ± 2.7 days in the ICU. The mean LoS was
6.1 ± 4.3 days (including 2.7 ± 2.3 days in the ICU) for the TF patients a nd 10.4 ± 5.4 days (including
4.8 ± 3.9 days in the ICU) for the TA/TAo patients.
Quality of Life (QoL)
QoL was measured using the visual analog scale (VAS) of the EuroQoL (EQ-5D) measure. The VAS is a
self-assessment in which patients rate their well-being on a scale from 0 to 100 where 0 is the worst state
they can imagine and 100 is the best state. During the trial, the mean improvement in VAS scale from
baseline to 30 days was 14.6 ± 22.2 for all patients, 15.1 ± 21.5 for the TF patients, and 11.5 ± 25.7 for
the TA/TAo patients.
Additional QoL instruments
The mean overall Kansas City Cardiomyopathy Questionnaire (KCCQ) summary score was 46.9 ± 22.6 at
baseline, and 67.5 ± 22.6 at 30 days for the entire VI population. Except for self-efficacy which showed a
small improvement, moderate to large improvements were observed in all other subscores at 30 days. In
general, improvements in the TF patients were slightly larger compared to those observed in the TA/TAo
patients.
Using the SF-36 norm based questionnaire, the physical component score for all patients improved from
32.0 ± 8.9 at baseline to 37.1 ± 9.7 at 30 days, and the mental component score improved from
46.9 ± 12.8 at baseline to 50.0 ± 12.5 at 30 days. In the TF patients, the physical component score
improved from 31.8 ± 8.7 at baseline to 37.3 ± 9.8 at 30 days, and the mental component score improved
from 46.8 ± 13.1 at baseline to 50.5 ± 12.2 at 30 days. In the TA/TAo patients, the physical component
score improved from 32.9 ± 10.0 at baseline to 35.9 ± 9.4 at 30 days, and the mental component scores
were 47.2 ± 11.1 at baseline and 47.2 ± 14.0 at 30 days.
SUMMARY OF SUPPLEMENTAL CLINICAL INFORMATION
Supplemental Clinical Study Design
Supplemental clinical data came from a study (referred to as “S3OUS” hereafter) conducted in Europe
and Canada.
The S3OUS study was a non-randomized, prospective, multi-center study in inoperable, high surgical
risk, and intermediate surgical risk patients who underwent implantation of the 23, 26, or 29 mm
SAPIEN 3 valve.
Except the intermediate surgical risk patients, the inclusion/exclusion criteria of the S3OUS trial were
largely similar to those of the PIIS3HR trial. The S3OUS study had a minimum age requirement
(≥ 75 years) and the upper limit for AVA was higher (< 1 cm
2
instead of ≤ 0.80 cm2). Additionally, the
S3OUS study included BAV within 30 days of the procedure (unless BAV was a bridge to procedure),
patients with planned concomitant surgical or transcatheter ablation for atrial fibrillation, hemodynamic or
respiratory instability requiring inotropic support, mechanical ventilation or mechanical heart assistance
within 30 days of screening; and the need for emergency surgery for any reason. Furthermore, the
exclusion criteria in the S3OUS study excluded senile dementia and any neurologic disease which
severely affected the ability to walk or perform everyday activities, and shortened the time interval
regarding confirmed stroke or TIA (within 3 months instead of 6 month of the procedure). The follow-up
periods were discharge or 7 days, whichever comes first, 30 days, 1 year, and annually thereafter to a
minimum of 5 years post procedure.
22
Page 23

SAPIEN 3 Valve
Overall
SAPIEN 3 Valve
Transfemoral Access
SAPIEN 3 Valve
Non-Transfemoral Access
All Treated
Population
Valve Implant
Population
All Treated
Population
All Treated
Population
102
101
57
56
45
45
All Treated (AT) Population consists of all patients who were enrolled in the trial and for whom the study
retained the valve upon leaving the catheterization laboratory/hybrid suite.
Table 14:
(S3OUS AT Population)
SAP IEN 3
(N = 102)
SAPIEN 3 Valve
(N = 57)
SAPIEN 3 Valve
(N = 45)
Age, yr
84.1 ± 5.0
85.1 ± 4.6
83.0 ± 5.3
Male sex, no.(%)
40 (39.2%)
23 (40.4%)
17 (37.8%)
STS score
8.0 ± 4.7
8.2 ± 4.2
7.9 ± 5.2
Logistic EuroSCORE
24.1 ± 13.0
22.3 ± 11.3
26.4 ± 14.7
New York Heart Association (NYHA)
class, no.(%):
I/II
11 (10.8%)
6 (10.5%)
5 (11.1%)
III/IV
91 (89.2%)
51 (89.5%)
40 (88.9%)
Coronary artery disease, no.(%)
68 (66.7%)
36 (63.2%)
32 (71.1%)
Previous myocardial infarction, no.(%)
20 (19.6%)
7 (12.3%)
13 (28.9%)
Previous intervention, no.(%)
Accountability of the S 3O US Coho rt
Patients were treated at 14 investigational sites. Note that the intermediate risk patients enrolled in the
S3OUS study were excluded from the analysis presented herein. The database included 102 “all treated”
(AT) inoperable and high surgical risk patients. “All treated” population is defined to include all patients
who were enrolled in the trial and for whom the study valve implantation procedures were started (i.e., the
anesthesia was started).
One patient was excluded from the VI population. This patient experienced an aortic root rupture caused
by displacement of a large lump of calcium with sharp edges through the native aortic annulus following
balloon expansion of the SAPIEN 3 valve. The patient was subsequently converted to SAVR. After the
patient was weaned off cardio-pulmonary bypass, bleeding in the region of the dorsal root occurred, and
the patient died on the operating table.
A total of 56 patients were successfully implanted with a SAPIEN 3 valve via the transf em or al acces s
route, and 45 via the transapical/transaortic access route, as shown in Table 13.
Table 13:
Patient Accountability (S3OUS)
(AT)
valve implantation procedures were started (i.e., anesthesia was started).
Valve Implant (VI) Population consists of all enrolled patients who received a SAPIEN 3 valve, and
(VI)
(AT)
Valve Implant
(VI) Population
(AT)
Study Populatio n Dem o gr a phic s a nd Bas el i ne Pa ra mete rs
The demographics of the S3OUS study population are shown in Table 14.
Patient Demographics and Baseline Characteristics
Demographics and Baseline
Characteristics
Valve
Overall
Transfemoral
Access
Valve Implant
(VI) Population
Non-Transfemoral
Access
23
Page 24

Table 14:
Patient Demographics and Baseline Characteristics
(S3OUS AT Population)
SAP IEN 3
(N = 102)
SAPIEN 3 Valve
(N = 57)
SAPIEN 3 Valve
(N = 45)
Coronary-artery bypass grafting
(CABG)
24 (23.5%)
10 (17.5%)
14 (31.1%)
Percutaneous coronary intervention
(PCI)
34 (33.3%)
16 (28.1%)
18 (40.0%)
Prior aortic valvuloplasty
10 (9.8%)
8 (14.0%)
2 (4.4%)
Stroke, no.(%)
7 (6.9%)
4 (7.0%)
3 (6.7%)
Peripheral vascular disease, no.(%)
27 (26.5%)
10 (17.5%)
17 (37.8%)
Chronic obstructive pulmonary disease
(COPD), no.(%):
Any
25 (24.5%)
13 (22.8%)
12 (26.7%)
Oxygen-dependent
1 (1.0%)
1 (1.8%)
0 (0%)
Atrial fibrillation, no.(%)
48 (47.1%)
22 (38.6%)
26 (57.8%)
Permanent pacemaker, no.(%)
15 (14.7%)
7 (12.3%)
8 (17.8%)
Severe pulmonary hypertension, no.(%)
10 (9.8%)
6 (10.5%)
4 (8.9%)
Severe liver disease / Cirrhosis, no.(%)
1 (1.0%)
1 (1.8%)
0 (0%)
Echocardiographic findings
Effective Orifice Area (EOA), cm2
0.6 ± 0.2
0.6 ± 0.2
0.6 ± 0.1
Mean aortic-valve gradie nt, mmHg
44.8 ± 15.3
45.2 ± 14.7
44.2 ± 16.1
Mean left ventricular ejection
fraction (LVEF), %
56.7 ± 9.1
57.7 ± 9.3
55.3 ± 8.7
Moderate or severe mitral
regurgitation, no./total no. (%)
23/85
(27.1%)
9/48
(18.8%)
14/37
(37.8%)
Plus–minus values are means ± SD.
Table 15:
(S3OUS AT Population)
SAPIEN 3
Access
SAPIEN 3
Transfemoral
Composite Event
n/N (%)
Death
Demographics and Baseline
Characteristics
Valve
Overall
Transfemoral
Access
Non-Transfemoral
Access
Safety and Effectiveness Results
Key Adverse Events
Key adverse events as adjudicated b y the CEC are presented in Table 15.
30 Day 1 Year
SAPIEN 3
Outcomes
Rate of Death, All
Stroke and AI ≥
Moderate,
Valve
Overall
13/88
(14.8%)
CEC Adjudicated Adverse Events at 1 Year
SAPIEN 3
Valve
Transfemoral
Access
3/50
(6.0%)
Valve
Non-
Transfemoral
10/38
(26.3%)
Valve
Overall
25/82
(30.5%)
24
SAPIEN 3
Valve
Access
9/47
(19.1%)
SAPIEN 3 Valve
Non-
Transfemoral
Access
16/35
(45.7%)
Page 25

Table 15:
CEC Adjudicated Adverse Events at 1 Year
(S3OUS AT Population)
30 Day
1 Year
SAPIEN 3
Access
SAPIEN 3
Transfemoral
From any
death, n/N (%)
8/102
(7.8%)
2/57
(3.5%)
6/45
(13.3%)
20/102
(19.6%)
7/57
(12.3%)
13/45
(28.9%)
From
cause, n/N (%)
3/102
(2.9%)
1/57
(1.8%)
2/45
(4.4%)
5/102
(4.9%)
2/57
(3.5%)
3/45
(6.7%)
Aortic
n/N (%)
Disabling Str oke,
n/N (%)
0/102
(0.0%)
0/57
(0.0%)
0/45
(0.0%)
1/102
(1.0%)
1/57
(1.8%)
0/45
(0.0%)
Myocardial
n/N (%)
Major Vascular
n/N (%)
Acute Kidney
n/N (%)
Disabling
n/N (%)
Valve Dysfunction
n/N (%)
Prosthetic Valve
n/N (%)
Conduction
n/N (%)
Outcomes
cardiovascular
Stroke, n/N (%)
Insufficiency (AI)
≥ Moderate,
Infarction,
Complications,
Injury - Stage III,
SAPIEN 3
Valve
Overall
7/102
(6.9%)
3/81
(3.7%)
2/102
(2.0%)
5/102
(4.9%)
0/102
(0.0%)
SAPIEN 3
Valve
Transfemoral
Access
2/57
(3.5%)
1/49
(2.0%)
2/57
(3.5%)
1/57
(1.8%)
0/57
(0.0%)
Valve
Non-
Transfemoral
5/45
(11.1%)
2/32
(6.3%)
0/45
(0.0%)
4/45
(8.9%)
0/45
(0.0%)
Valve
Overall
9/102
(8.8%)
1/62
(1.6%)
3/102
(2.9%)
SAPIEN 3
Valve
Access
2/57
(3.5%)
1/40
(2.5%)
2/57
(3.5%)
SAPIEN 3 Valve
Non-
Transfemoral
Access
7/45
(15.6%)
0/22
(0.0%)
1/45
(2.2%)
N/A N/A N/A
N/A N/A N/A
Bleeding Event,
Requiring
Intervention,
Endocarditis,
Abnormality
Requiring
Pacemaker,
6/102
(5.9%)
0/102
(0.0%)
0/102
(0.0%)
14/102
(13.7%)
3/57
(5.3%)
0/57
(0.0%)
0/57
(0.0%)
7/57
(12.3%)
3/45
(6.7%)
0/45
(0.0%)
0/45
(0.0%)
7/45
(15.6%)
N/A N/A N/A
N/A N/A N/A
1/102
(1.0%)
14/102
(13.7%)
0/57
(0.0%)
7/57
(12.3%)
(15.6%)
1/45
(2.2%)
7/45
The composite adverse event rate involving all-cause mortality, all stroke, and AI ≥ moderate at 30 days
for all patients is higher in the S3OUS cohort than PIIS3HR cohort (14.8% vs. 6.8%). This disparity is due
to the composition of the study populations, specifically the S3OUS cohort comprises 44.1% TA/TAo
patients vs. 15.8% TA/TAo patients in the PIIS3HR cohort. Note, the composite adverse event rate at 30
days for TF patients was similar, specifically, 6.0% in the S3OUS cohort and 5.8% in the PIIS3HR cohort.
The K-M estimates for all-cause mortality for all patients, the TF patients, and the TA/TAo patients are
shown in Figure 11.
25
Page 26

Figure 11:
All-Cause Mortality at 1 Year
(S3OUS AT Population)
Note: The confidence intervals are calculated without multiplicity adjustment. The
adjusted confidence intervals could be wider than presented here. As such, confidence
intervals are provided to illustrate the variability only and should not be used to draw
any statistical conclusion.
The K-M estimates for the stroke rate for all patients, the TF patients, and the TA/TAo patients are
shown in Figure 12.
26
Page 27

Figure 12:
(S3OUS AT Population)
any statistical conclusion.
Figure 13:
(S3OUS VI Population)
Effective Orifice Area (EOA)
0.0
0.2
0.4
0.6
0.8
1.0
1.2
1.4
1.6
1.8
2.0
Baseline 30 Day 1 Year
0.6 0.6 0.6
1.5 1.5 1.5
1.4
1.4 1.4
All Stroke at 1 Year
Note: The confidence intervals are calculated without multiplicity adjustment. The
adjusted confidence intervals could be wider than presented here. As such, confidence
intervals are provided to illustrate the variability only and should not be used to draw
Valve Performance
The mean EOA increased from 0.6 ± 0.2 cm
1 year, as shown in Figure 13.
Effective Orifice Area
2
at baseline to 1.5 ± 0.4 cm2 at 30 days and 1.4 ± 0.4 cm2 at
27
Page 28

The average mean gradient decreased from 44.8 ± 15.4 mmHg at baseline to 10.4 ± 4.1 mmHg at 30
Figure 14:
(S3OUS VI Population)
Figure 15:
(S3OUS VI Population)
Mean Gradient (mmHg)
0
10
20
30
40
50
60
70
80
90
100
110
Baseline 30 Day 1 Year
44.8 44.8 44.8
10.4 10.4 10.4
10.7 10.7 10.7
Peak Gradient (mmHg)
0
10
20
30
40
50
60
70
80
90
100
110
Baseline 30 Day 1 Year
77.5 77.5 77.5
21.0 21.0 21.0
21.5 21.5 21.5
days and maintained at 10.7 ± 4.1 mmHg at 1 year, as shown in Figure 14.
Mean Gradient
The mean peak gradient decreased from 77.5 ± 24.9 mmHg at baseline to 21.0 ± 7.7 mmHg at 30 days,
and maintained at 21.5 ± 8.2 mmHg at 1 year, as shown in Figure 15.
The proportion of patients with aortic insufficiency ≥ moderate was 9.8% at baseline, 3.7% at 30 days,
and 1.6% at 1 year, as shown in Figure 16.
Peak Gradient
28
Page 29

Figure 16:
Aortic Insufficiency
(S3OUS VI Population)
Figure 17:
(S3OUS VI Population)
None
Trace
Mild
Mild-Moderate
Moderate
Moderate-Severe
Severe
Percentage
0
20
40
60
80
100
Baseline
30 Day 1 Year
13%
37%
55%
37%
44%
32%
35%
12%
8%
5%
9%
None Trace Mild
Mild-Moderate Moderate Moderate-Severe
Severe
Percentage
0
20
40
60
80
100
30 Day 1 Year
40%
56%
42%
31%
12%
6%
5%
The proportion of patients with aortic PVL ≥ moderate was 3.7% at 30 days, and 1.6% at 1 year, as
shown in Figure 17.
Aortic Paravalvular Leak
NYHA
The NYHA class by visit is sho wn in Figure 18. For all patients, the mean NYHA class decreased from 3.0
± 0.5 at baseline to 1.6 ± 0.7 at 30 days and 1.8 ± 0.6 at 1 year.
29
Page 30

Figure 18:
NYHA Class by Visit
(S3OUS AT Population)
Patients
Population†
(VI)Population‡
†. Eligible Patient (EP) Population consists of all enrolled patients who were determined eligible after
the assigned valve, and retained the valve upon leaving the catheterization laboratory.
1 2 3
4
Percent
0
20
40
60
80
100
All Patients
Transapical/Transaortic Transfemoral
Baseline 30 Day 1 Year Baseline
30 Day 1 Year Baseline 30 Day 1 Year
11%
78%
11%
46%
47%
6%
33%
58%
8%
11%
73%
16%
34%
54%
9%
25%
64%
7%
11%
82%
7%
54%
43%
38%
54%
8%
PARTNER II SAPIEN 3 INTERMEDIATE RISK COHORT
Accountability
Table 16 presents patient accountability in the PIIS3i and PIIA-SAVR cohorts. Of the 1,074 eligible
patients (Eligible Pati ent or EP Population) in PIIS3i, 1,069 were successfully implanted with a SAPIEN 3
valve and constitute the PIIS3i Valve Implant (VI) population. Among the VI population, 943 patients were
implanted via the transfemoral (TF) access route, and 126 patients via a non-transfemoral (non-TF;
mainly transapical and trans aortic ) access route. Of the 938 eligible patients in the PIIA-SAVR cohort,
936 were successfully implanted with a surgical valve and constitute the PIIA-SAVR VI population.
Table 16: Patient Accountability
Eligible Patient (EP)
Valve Implant
SAPIEN 3 Cohort 1078 1074 1069
TF 952 948 943
Non-TF 126 126 126
All Enrolled
PIIA SAVR 1021 938 936
screening, entered into the catheterization laboratory and remained eligible to receive the assigned implant.
‡. Valve Implant (VI) Population is a subset of the EP Population who received
30
Page 31

Study Populatio n Dem o gr a phic s a nd Bas el i ne Pa ra mete rs
Table 17: Patient Demographics and Baseline Characteristics of the EP Population
514/938
225/937
712/937
623/938
166/938
45/938
96/938
301/938
279/932
326/938
113/938
15/938
The demographics of the PIIS3i and PIIA-SAVR EP populations are summarized in Table 17.
Demographics &
Characteristics
Overall
(N = 1074)
TF Only
(N = 948)
Non-TF Only
(N=126)
PIIA-SAVR
(N=938)
Age - years 81.9 ± 6.60 82.1 ± 6.57 80.7 ± 6.69 81.6±6.73
SAP IEN 3 Valve
Male sex 662/1074
(61.6%)
Society of Thoracic
5.3 ± 1.29 5.3 ± 1.29 5.6 ± 1.28 5.8±1.92
577/948
(60.9%)
85/126
(67.5%)
(54.8%)
Surgeons (STS) score
New York Heart Association (NYHA) class
I/II 294/1074
(27.4%)
III/IV 780/1074
(72.6%)
Coronary artery disease 748/1074
(69.6%)
Previous myocardial
infarction
172/1074
(16.0%)
262/948
(27.6%)
686/948
(72.4%)
652/948
(68.8%)
133/948
(14.0%)
32/126
(25.4%)
94/126
(74.6%)
96/126
(76.2%)
39/126
(31.0%)
(24.0%)
(76.0%)
(66.4%)
(17.7%)
Previous intervention
Coronary artery
bypass grafting
(CABG)
Percutaneous
coronary intervention
(PCI)
Prior aortic
valvuloplasty
Cerebral vascular accident
(CVA)
Peripheral vascular
disease
301/1074
(28.0%)
344/1074
(32.0%)
55/1074
(5.1%)
97/1074
(9.0%)
304/1074
(28.3%)
248/948
(26.2%)
299/948
(31.5%)
51/948
(5.4%)
81/948
(8.5%)
231/948
(24.4%)
53/126
(42.1%)
45/126
(35.7%)
4/126 (3.2%)
16/126
(12.7%)
73/126
(57.9%)
241/938
(25.7%)
254/938
(27.1%)
(4.8%)
(10.2%)
(32.1%)
Chronic obstructive pulmonary disease (COPD)
Any 321/1072
(29.9%)
Oxygen-dependent 53/1067
(5.0%)
Atrial fibrillation 385/1074
(35.8%)
Permanent pacemaker 142/1074
(13.2%)
Severe pulmonary
hypertension
25/1074
(2.3%)
Frailty 92/1074
(8.6%)
270/946
(28.5%)
46/942
(4.9%)
342/948
(36.1%)
121/948
(12.8%)
19/948
(2.0%)
86/948
(9.1%)
51/126
(40.5%)
7/125 (5.6%)
43/126
(34.1%)
21/126
(16.7%)
6/126 (4.8%)
6/126 (4.8%)
(29.9%)
26/925
(2.8%)
(34.8%)
(12.0%)
N/A
(1.6%)
31
Page 32
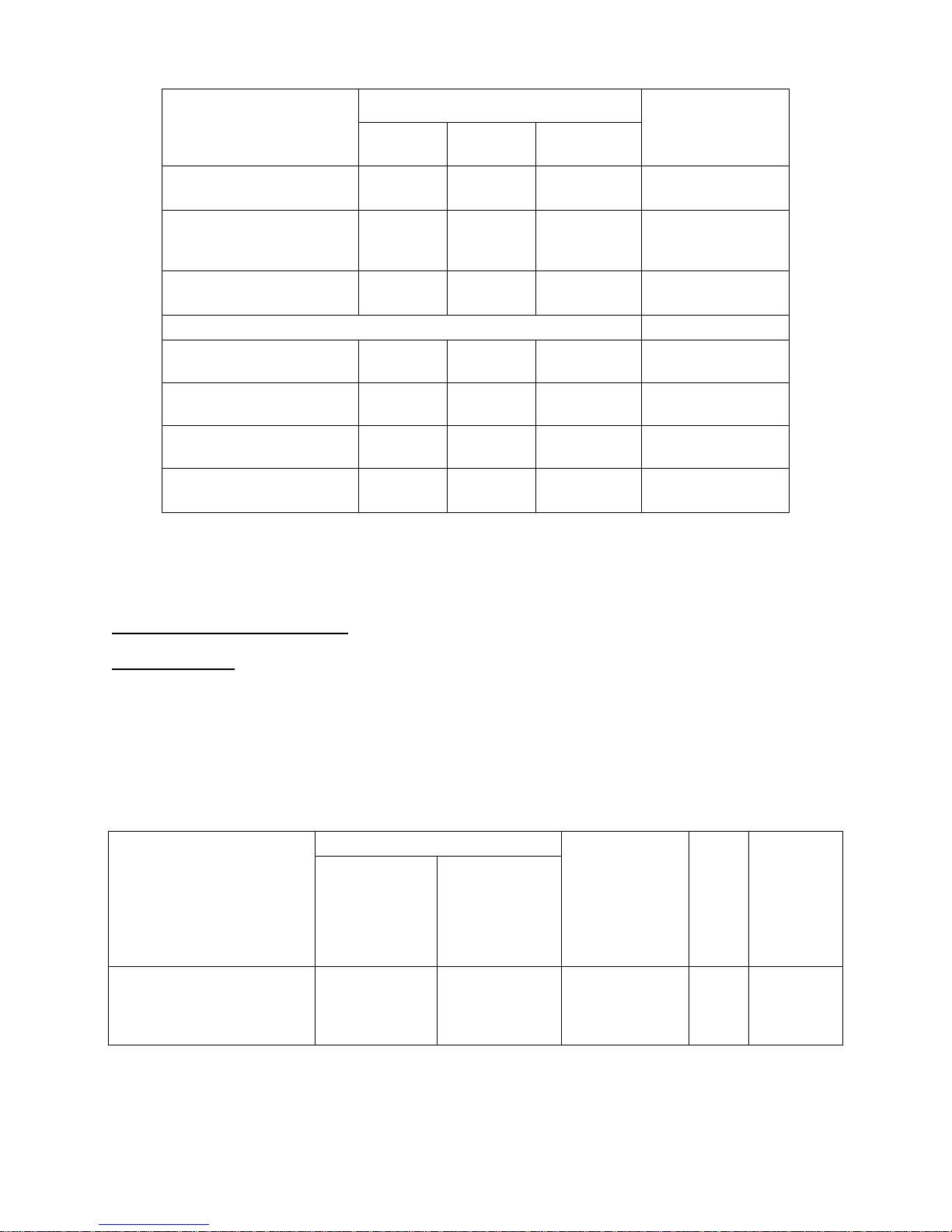
Table 17: Patient Demographics and Baseline Characteristics of the EP Population
Demographics &
0/938
(0.0%)
procedure
4/938
(EOA) - cm2
153/841
Continuous measures - Mean ± SD; Categorical measures – n/total no. (%)
Observed Event rate
[90% CI]†
Conclusion
Characteristics
Overall
(N = 1074)
Porcelain aorta 1/1074
(0.1%)
SAP IEN 3 Valve
TF Only
Non-TF Only
(N = 948)
1/948
0/126 (0.0%)
(0.1%)
PIIA-SAVR
(N=938)
(N=126)
Chest deformities that
preclude an open chest
Cirrhosis 4/1074
1/1074
(0.1%)
(0.4%)
1/948
(0.1%)
4/948
(0.4%)
0/126 (0.0%)
0/126 (0.0%)
0/938
(0.0%)
(0.4%)
Echocardiographic findings (Valve Implant Population)
Effective orifice area
Mean aortic-valve gradient
- mmHg
Mean left ventricular
ejection fraction (LVEF) %
Moderate or severe mitral
regurgitation
0.7 ± 0.17 0.7 ± 0.16 0.7 ± 0.18
46.1 ±
12.63
58.5 ±
13.36
91/1033
(8.8%)
46.1 ±
12.66
58.8 ±
13.24
87/909
(9.6%)
45.8 ± 12.47
56.0 ± 14.05
4/124 (3.2%)
0.7±0.20
44.7±12.55
55.4±11.75
(18.2%)
Safety and Effectiveness Results
Primary Endpoints
The primary endpoint was a composite of all-cause death, stroke, and AI ≥ moderate at 1 year. The
weighted proportion dif f erenc e of the prim ary endpoint was -9.2% (90% CI: [-12.4%, -6.0%]) using the
average treatment effect on the treated (ATT) method
[2]
, as shown in Table 18 and Figure 19. Since the
upper limit of the CI was < 7.5%, non–inferiority was met.
Table 18:
Primary Endpoint Non-Inferiority Test
(VI Population)
Propensity
Score Quintile
Pooled
SAP IEN 3
(N=1069)
PIIA-SAVR
(N=936)
Proportion
Difference(ATT
Margin
Method*)
for Non-
Inferiority
Test
Composite of all-cause
death, all stroke, and aortic
insufficiency (AI) ≥ moderate
13.0% 23.2%
[-12.4%, -6.0%]
at 1 year
* ATT: average treatment effect on the treated
†
Two-sided 90% Wald-type confidence interval
Figure 19: Forest Plot – Composite of All Death, All Stroke and AI ≥ Moderate (VI Population)
32
-9.2%
7.5% Pass
Page 33

(N= 1069)
(N = 936)
Estimate
Error
Estimate
Error
*
Events
†
The Kaplan-Meier (KM) estimates for all-cause death and all stroke at 1 year for the PIIS3i cohort and the
PIIA-SAVR cohort are provided in Table 19, as well as Figures 20 and 21, respectively.
Endpoints
All-cause death
at 1 year
Table 19:
All-Cause Death and All Stroke at 1 Year
(VI Population)
SAP IEN 3 Valve
Observed
Event Rate
Kaplan-Meier Event
Point
Rate
Standard
*
Observed
Event Rate
PIIA-SAVR
Kaplan-Meier Event Rate
Point
Standard
*
Proportion Difference
7.0% 7.1% 0.79% 12.4% 12.6% 1.09% -5.2%
Propensity Score
Quintile Pooled
(ATT Method†)
All stroke at 1
year
Kaplan-Meier estimates were calculated at 365 days and i ncluded only the first event for each patient.
occurring after 365 days were not included in this analysis.
ATT: average treatment effect on the treated
4.5% 4.6% 0.65% 7.9% 8.1% 0.91% -3.5%
33
Page 34

Figure 20: All-Cause Death through 1 Year (VI Population)
Figure 21: All Stroke through 1 Year
(VI Population)
Note: The confidence intervals were calculated without multiplicity adjustment. The adjusted
confidence intervals could be wider than presented here. As such, the confidence intervals are
provided to illustrate the variability only and should not be used to draw any statistical conclusion.
Note: The confidence intervals were calculated without multiplicity adjustment. The adjusted
confidence intervals could be wider than presented here. As such, the confidence intervals are
provided to illustrate the variability only and should not be used to draw any statistical conclusion.
The proportion of patients with AI ≥ moderate at 1 year was 1.6% for the PIIS3i cohort and 0.3%
for the PIIA-SAVR cohort, as shown in Table 20.
34
Page 35

Table 20: Aortic Insufficiency (AI) ≥ Moderate at 1 Year (VI Population)
Observed Event Rate
Propensity Score
(ATT Method*)
Conclusion
bleeding through
Quintile Pooled
SAP IEN 3 Valve
(N= 1069)
SAVR
(N= 936)
Proportion
Difference
Aortic insufficiency (AI) ≥ moderate 1.6% 0.3% 1.2%
* ATT: average treatment effect on the treated
Secondary Endpoints
The secondary endpoints were examined in a pre-specified order adjusted for the propensity quintiles
using the ATT method. Table 21 summarizes the statistical conclusions on the non-inferiority hypothesis
testing of the five secondary endpoints for labeling that were evaluated using a gatek eeping/ hi erar chic a l
multiplicity adjustment procedure to control the overall type I error to 0.05. For each second ary endpoint,
the upper limit of the confidence interval was less than the respective non-inferiority margin. Therefore,
for each of the secondary endpoints for labeling, the SAPIEN 3 valve was non-inferior to SAVR.
Table 21: Secondary Endpoints for Labeling – Gatekeeping/Hierarchical Method
(VI Population)
Weighted
Proportion
Difference in
Average
Treatment
Effect on the
Treated
[90% CI]
†
Margin
for Non-
Inferiority
Test
PreSpecified
Order for
Gatekeeping/
Hierarchical
Method
Endpoints
Observed Event Rate
SAPIEN 3 Valve
(N=1069)
PIIA-SAVR
(N=936)
Composite of all
death, all
strokes, life
threatening
No. 1
(disabling)/major
bleeding and
major vascular
complication at
30 days
Major vascular
No. 2
complication
through 30 days
Life threatening
No. 3
(disabling)/major
30 days
No. 4
No. 5
†
Two-sided 90% Wald-type confidence interval.
All-cause death
through 30 days
All stroke
through 30 days
18.3% 79.4%
5.8% 5.3%
14.6% 78.2%
0.9% 3.7%
2.6% 6.1%
-60.5%
[-63.5%, -57.4%]
0.3%
[-1.5%, 2.0%]
-63.2%
[-66.2%, -60.2%]
-2.7%
[-3.9%, -1.5%]
-3.2%
[-4.7%, -1.6%]
7.5% Pass
5.0% Pass
5.0% Pass
2.5% Pass
2.5% Pass
35
Page 36

The forest plots for all-cause death and all stroke at 30 days are provided in Figures 22 and 23,
Figure 22: Forest Plot – All-Cause Death at 30 Days (VI Population)
multiplicity per the gatekeeping approach.
Table 22: CEC-Adjudicated Adverse Events through 1 Year
(EP Population)
respectively.
Note: As part of a pre-specified hiearchy, the hypothesis for this endpoint was tested using a
hierarchical gatekeeping approach. The confidence interval shown here was not adjusted for
Figure 23: Forest Plot – All Stroke at 30 Days (VI Population)
Note: As part of a pre-specified hiearchy, the hypothesis for this endpoint was tested using a hierarchical
gatekeeping approach. The confidence interval shown here was not adjusted for multiplicity per the
gatekeeping approach.
Adverse Events
The key CEC-adjudicated adverse events through 1 year for the EP population are presented in Table 22.
Events
7 Days
Acute kidney injury: Stage III 5/1074 (0.5%) 3/948 (0.3%) 2/126 (1.6%) N/A
30 Days
Death 12/1074 (1.1%) 10/948(1.1%) 2/126 (1.6%) 35/938 (3.7%)
Cardiac death 10/1074 (0.9%) 9/948 (0.9%) 1/126 (0.8%) 26/938 (2.8%)
Non-cardiac death 2/1074 (0.2%) 1/948 (0.1%) 1/126 (0.8%) 9/938 (1.0%)
Stroke 29/1074 (2.7%) 24/948 (2.5%) 5/126 (4.0%) 57/938 (6.1%)
Major (disabling) stroke 11/1074 (1.0%) 7/948 (0.7%) 4/126 (3.2%) 41/938 (4.4%)
Overall TF Only Non-TF Only
SAP IEN 3 Valve
PIIA-SAVR
36
Page 37

Table 22: CEC-Adjudicated Adverse Events through 1 Year
(EP Population)
Events
Categorical measures - n. / total no. (%).
Site-reported Transfusion at Day 0 or Day 1; Categorical measures - n. / total no. (%)
SAP IEN 3 Valve
PIIA-SAVR
Overall TF Only Non-TF Only
Minor (non-disabling) stroke 18/1074 (1.7%) 17/948 (1.8%) 1/126 (0.8%) 16/938 (1.7%)
Myocardial infarction 3/1074 (0.3%) 3/948 (0.3%) 0/126 (0.0%) 17/938 (1.8%)
Major vascular complication 65/1074 (6.1%) 60/948 (6.3%) 5/126 (4.0%) 50/938 (5.3%)
Life threatening (disa bl ing) or
major bleeding
159/1074 (14.8%) 112/948 (11.8%) 47/126 (37.3%)
733/938 (78.1%)
Aortic valve re-intervention 1/1074 (0.1%) 1/948 (0.1%) 0/126 (0.0%) 0/938 (0.0%)
Any endocarditis 2/1074 (0.2%) 2/948 (0.2%) 0/126 (0.0%) 0/938 (0.0%)
Rhythm disturbance requiring
permanent pacemaker
108/1074 (10.1%) 99/948 (10.4%) 9/126 (7.1%)
68/938 (7.2%)
1 Year
Death 79/1074 (7.4%) 61/948 (6.4%) 18/126 (14.3%) 117/938 (12.5%)
Cardiac death 47/1074 (4.4%) 37/948 (3.9%) 10/126 (7.9%) 70/938 (7.5%)
Non-cardiac death 32/1074 (3.0%) 24/948 (2.5%) 8/126 (6.3%) 47/938 (5.0%)
Stroke 49/1074 (4.6%) 40/948 (4.2%) 9/126 (7.1%) 74/938 (7.9%)
Major (disabling) stroke 24/1074 (2.2%) 16/948 (1.7%) 8/126 (6.3%) 53/938 (5.7%)
Minor (non-disabling) stroke 25/1074 (2.3%) 24/948 (2.5%) 1/126 (0.8%) 22/938 (2.3%)
Aortic valve re-intervention 6/1074 (0.6%) 6/948 (0.6%) 0/126 (0.0%) 4/938 (0.4%)
Any endocarditis 8/1074 (0.7%) 7/948 (0.7%) 1/126 (0.8%) 6/938 (0.6%)
In addition, site-reported new-onset atrial fibrillation was 5.9% in the PIIS3i EP population and 29.2% in
the PIIA-SAVR EP population.
Bleeding Rate
The bleeding rates utilizing the number of units transfused are presented in Table 23.
Table 23:
Bleeding Rate Using Site-Reported Units Transfused (EP Population)
SAP IEN 3 Valve
(N = 1074)
PIIA-SAVR
(N = 938)
Transfusion units ≥ 2 and < 4 47/1074 (4.4%) 184/938 (19.6%)
Transfusion units ≥ 4 18/1074 (1.7%) 218/938 (23.2%)
Other Results
Procedural Information
In the PIIS3i EP population the mean duration in the catheterization laboratory was 187.3 ± 53.2 minutes,
the mean total procedure time was 84.2 ± 40.7 minutes, and the mean total anesthesia time was
186.9 ± 61.1 minutes, all of which were slightly shorter in the TF group. General anesthesia was used in
the vast majority of cases; 18.9% of the TF patients had conscious sedation. Correct positioning of the
valve was achieved in 99.3% of the patients. Four patients (0.4%, all TF patients) were implanted with a
second valve. One patient (0.1%) experienced valve embolization and 2 patients (0.2%) experienced
annular rupture.
37
Page 38

In the PIIA-SAVR EP population, the mean duration in the operating room was 333.2 ± 96.4 min, the
The measurements of EOA, mean gradient, peak gradient, total aortic regurgitation (AR), and aortic
paravalvular leak (PVL) are presented in Figures
gradient were sustained at 1 year.
6.2% at baseline, 3.9% at 30 days, and 1.6% at 1 year,
with tot
of patients with aortic PVL ≥ moderate was 3.8% at 30 days and 1.5% at 1 year
to
Figure 24: Effective Orifice Area (VI Population)
Figure 25: Mean Gradient (VI Population)
mean total procedure time was 237.5 ± 86.58 min, and the mean anesthesia time was
333.5 ± 108.42 min. General anesthesia was used in all patients.
Valve Performance
24-28. The increase in EOA and decrease in
In PIIS3i, the proportion of patients with total AR ≥ moderate was
while in PIIA-SAVR, the proportion of patients
al AR ≥ moderate was 12.0% at baseline, 0.7% at 30 days, and 0.3% at 1 year. The proportion
in PIIS3i, as compared
0.5% at 30 days and 0.3% at 1 year in PIIA-SAVR.
38
Page 39

Figure 26: Peak Gradient (VI Population)
Figure 27: Total Aortic Regurgitation (VI Population)
Figure 28: Aortic Paravalvular Leak (VI Population)
39
Page 40

NYHA
The NYHA classifications by vis it are presented in Figure 29. In PIIS3i, 72.6% of the patients
were in NYHA Class III or IV at baseline, which reduced to 6.3% at 30 days and 6.7% at 1 year,
while in PIIA-SAVR, the percentage of patients in NYHA Class III or IV was 76.0% at baseline,
13.6% at 30 days, and 6.7% at 1 year. A side-by-side comparison of the results by access
approach is presented in Figure 30.
40
Page 41

Figure 29: NYHA Class by Visit (EP Population)
Figure 30: NYHA Class by Visit – TF versus non-TF Access (EP Population)
Distance (m)
SAP IEN 3 Valve
All
TF
Non-TF
Six-Minute Walk Test (6MWT)
The improvements in mean 6MWT distance are presented in Table 24. As compared to the
SAPIEN 3 patients, the PIIA-SAVR patients had a decrease in mean 6MWT distance from
baseline to 30 days.
Table 24: 6MWT Distance (EP Population)
6MWT
41
PIIA-SAVR
Page 42

Baseline
193.9±118.1
194.1 ± 117.2
192.5 ± 125.5
179.3±
123.2
230.6±126.1
234.6 ± 123.6
199.0 ± 140.6
166.7 ±
126.4
133.8
SAP IEN 3 Valve
All
TF
Non-TF
Overall
5.5±5.7
5.0±5.2
9.3±7.7
11.9±7.6
ICU
2.7±3.0
2.5±2.6
4.2±4.9
5.6±6.1
Plus–minus values are means ± SD.
Figure 31: KCCQ Clinical Summary Score (EP Population)
30 days
1 year
Plus–minus values are means ± SD.
227.7 ± 134.7
230.6 ± 133.6 202.8 ± 142.1 219.2 ±
Length of Stay (LoS)
The results for LoS are presented in Table 25. Overall, the SAPIEN 3 patients had shorter LoS'
than the PIIA-SAVR patients.
Table 25: Length of Stay (EP Population)
Length of
Stay (days)
PIIA-SAVR
Quality of Life (QoL)
The QoL measurements using the Kansas City Cardiomyopathy Questionnaire (KCCQ) clinical
summary score are presented in Figure 31. Except for self-efficacy which showed a small
improvement, moderate to large improvements were observed in all other subscores at 30 days
and were sustained at 1 year in the PIIS3i EP population. A side-by-side comparison of the
results by access approach is presented in Figure 32. In general, improvements in the TF group
were slightly larger as compared to those o bs erve d in the Non-TF group.
42
Page 43

Figure 32: KCCQ Clinical Summary Score - TF versus non-TF Access
(EP Population)
43
Page 44

Additional QoL instruments
SAP IEN 3 Valve
All
TF
Non-TF
Baseline
60.3 ± 20.0
61.0 ± 19.8
55.1 ± 20.7
59.5 ± 20.5
30 days
74.0 ± 16.6
74.8 ± 16.6
68.5 ± 16.2
67.2 ± 19.5
1 year
74.4 ± 17.2
74.7 ± 17.1
71.8 ± 17.8
74.3 ± 16.7
SAP IEN 3 Valve
All
TF
Non-TF
Physical Component Score
Baseline
34.7±9.1
35.0±9.1
33.1±8.5
34.3±9.0
30 days
39.7±9.8
40.3±9.7
34.8±9.2
34.5±8.4
1 year
40.0±10.3
40.4±10.2
37.0±10.8
39.5±10.4
Mental Component Score
Baseline
48.0±11.8
48.1±11.8
47.0±12.3
48.0±12.3
30 days
51.8±10.6
52.3±10.4
47.8±11.3
45.5±13.3
1 year
52.5±10.7
52.7±10.8
50.7±10.1
52.0±11.3
Plus–minus values are means ± SD.
[1]
Kappetein AP, Head SJ, Généreux P, et al. Updated standardized endpoint definitions for
consensus document (VARC-2). Eur J Cardiothorac Surg 2012;42:S45-60.
[2]
Imbens G. W. (2004) Nonparametric Estimation of Average Treatment Effects under
86(1): 4–29.
QoL was also measured using the visual analog scale (VAS) of the EuroQoL (EQ-5D) measure
and the SF-36 Health Status Questionnaire. The VAS is a self-assessment in which patients rate
their well-being on a scale from 0 to 100 where 0 is the worst state they can imagine and 100 is
the best state. SF-36 uses 36 questions to measure functional health and well-being from the
patient’s point of view and is generally reported in two summary scores on a scale from 0 to 100
which evaluate physical (the Physical Summary Score) and mental (the Mental Summary Score)
health, with higher scores representing better functional health and well-being. The results of the
VAS and SF-36 measures are presented in Tables 26 and 27, respectively.
Table 26: EQ-5D Visual Analog Scale (EP Population)
EQ-5D Visual Analog Scale
Plus–minus values are means ± SD.
Table 27: SF-36 Health Status Questionnaire Score (EP Population)
SF-36 Health Status
Questionnaire Score
REFERENCES
PIIA-SAVR
PIIA-SAVR
transcatheter aortic valve implantation: the Valve Academic Research Consortium-2
Exogeneity: A Review. The Review of Economics and Statistics, February 2004,
These products are manufactured and sold under one or more of the following US patent(s): US Patent
No. 6,214,054; 6,547,827; 6,908,481; 7,214,344; 7,530,253; 7,585,321; 7,780,723; 7,846,203; 7,895,876;
7,993,394; 8,057,540; 8,382,826; 8,591,575; 8,690,936; 8,790,387; 9,301,840 and 9,301,841 and
corresponding foreign patents. Additional patents are pending.
44
Page 45

45
Page 46

Manufacturer
Edwards Lifesciences LLC
Telephone 949.250.2500
One Edwards Way
800.424.3278
Irvine, CA 92614 USA
FAX 949.250.2525
©Copyright 2016, Edwards Lifesciences LLC
All rights reserved.
Web IFU
08/2016
10001354002 A
46
 Loading...
Loading...