Page 1
PD-L1 IHC 22C3 pharmDx
Interpretation Manual – Urothelial Carcinoma
FDA-approved for in vitro diagnostic use
Page 2

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
For countries outside of the United States, see the local KE YTRUDA product label for approved
indications and expression cutoff values to guide therapy.
2
Page 3
Table of Contents
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Intended Use 04
Introduction 06
PD-L1 Overview 08
PD-L1 IHC 22C3 pharmDx Overview 10
Kit Configuration (SK006) 11
Technical Considerations 12
Specimen Preparation 12
In-house Control Tissue 12
Optional Additional In-house Control: Tonsil Tissue 13
Tissue Processing 13
PD-L1 IHC 22C3 pharmDx Staining Procedure 14
Technical Checklist 17
Slide Evaluation 18
General Considerations 18
Specimen Adequacy 18
Evaluating Controls 19
Slide Evaluation Flowchart 23
Combined Positive Score 24
Definition of Combined Positive Score (CPS) 24
CPS Numerator Inclusion and Exclusion Criteria 24
Determining Combined Positive Score 25
Suggested Methods 27
Interpretation of CPS 30
Identifying Patients With Urothelial Carcinoma for Treatment 31
PD-L1 IHC 22C3 pharmDx Testing Scheme 32
Reporting Results 33
Combined Positive Score Summary and Examples 34
Key Considerations in Scoring PD-L1 IHC 22C3 pharmDx 34
Stained Specimens
Image Guide for Interpretation of PD-L1 IHC 22C3 pharmDx 35
Staining in Urothelial Carcinoma
CPS < 10 Case Examples 49
CPS≥10CaseExamples 53
Near Cut-off Case Examples 59
(CPS Range of Greater Than 1 but Less Than 10)
Near Cut-off Case Examples 63
(CPS Range of Greater Than or Equal to 10 but Less Than or Equal to 20)
Artifacts 66
Troubleshooting Guide 71
Clinical Performance Evaluation 72
References 74
3
Page 4
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Intended Use
For in vitro diagnostic use.
PD-L1 IHC 22C3 pharmDx is a qualitative immunohistochemical assay using
Monoclonal Mouse Anti-PD-L1, Clone 22C3 intended for use in the detection of
PD-L1 protein in formalin-fixed, paraffin-embedded (FFPE) non-small cell lung
cancer (NSCLC), gastric or gastroesophageal junction (GEJ) adenocarcinoma,
cervical cancer and urothelial carcinoma tissues using EnVision FLEX
visualization system on Autostainer Link 48.
Non-Small Cell Lung Cancer (NSCLC)
PD-L1 protein expression in NSCLC is determined by using Tumor Proportion
Score (TPS), which is the percentage of viable tumor cells showing partial or
complete membrane staining at any intensity. The specimen should be considered
tohavePD-L1expressionifTPS≥1%andhighPD-L1expressionifTPS≥50%.
PD-L1 IHC 22C3 pharmDx is indicated as an aid in identifying NSCLC patients for
treatment with KEYTRUDA
for expression cutoff values guiding therapy in specific clinical circumstances.
®
(pembrolizumab). See the KEYTRUDA® product label
Gastric or Gastroesophageal Junction (GEJ) Adenocarcinoma
PD-L1 protein expression in gastric or GEJ adenocarcinoma is determined by
using Combined Positive Score (CPS), which is the number of PD-L1 staining
cells (tumor cells, lymphocytes, macrophages) divided by the total number of
viable tumor cells, multiplied by 100. The specimen should be considered to
havePD-L1expressionifCPS≥1.
PD-L1 IHC 22C3 pharmDx is indicated as an aid in identifying gastric or GEJ
®
adenocarcinoma patients for treatment with KEYTRUDA
(pembrolizumab).
Cervical Cancer
PD-L1 protein expression in cervical cancer is determined by using Combined
Positive Score (CPS), which is the number of PD-L1 staining cells (tumor cells,
lymphocytes, macrophages) divided by the total number of viable tumor cells,
multiplied by 100. The specimen should be considered to have PD-L1 expression
ifCPS≥1.
PD-L1 IHC 22C3 pharmDx is indicated as an aid in identifying cervical cancer
®
patients for treatment with KEYTRUDA
(pembrolizumab).
Urothelial Carcinoma
PD-L1 protein expression in urothelial carcinoma is determined by using
Combined Positive Score (CPS), which is the number of PD-L1 staining cells
(tumor cells, lymphocytes, macrophages) divided by the total number of viable
tumor cells, multiplied by 100. The specimen should be considered to have PD-L1
expressionifCPS≥10.
KEYTRUDA is a registered trademark of
Merck Sharp & Dohme Corp., a subsidiary of
Merck & Co., Inc.
4
PD-L1 IHC 22C3 pharmDx is indicated as an aid in identifying urothelial carcinoma
®
patients for treatment with KEYTRUDA
(pembrolizumab). See the KEYTRUDA®
product label for specific clinical circumstances guiding PD-L1 testing.
Page 5
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
5
Page 6

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Introduction
PD-L1 IHC 22C3 pharmDx is the only companion diagnostic approved by the
FDA as an aid in identifying patients with urothelial carcinoma for treatment with
KEYTRUDA
This Interpretation Manual is provided as a tool to help guide pathologists and
laboratory personnel in achieving correct and reproducible results in assessing
PD-L1 expression in formalin-fixed, paraffin-embedded urothelial carcinoma
specimens. PD-L1 expression evaluation may be used to identify patients for
anti-PD-1 immunotherapy.
The manual provides detailed scoring guidelines and technical information
from the PD-L1 IHC 22C3 pharmDx Instructions for Use (IFU) to ensure
high-quality staining and diagnostic assessment. To help familiarize you with
the requirements for scoring urothelial carcinoma stains with PD-L1 IHC 22C3
pharmDx, example cases of various PD-L1 expression levels are provided
as references. These example cases and in-depth recommendations for
interpretation of urothelial carcinoma specimens stained with PD-L1 IHC 22C3
pharmDx can help individual labs achieve reproducible and reliable results.
®
(pembrolizumab).
PD-L1 IHC 22C3 pharmDx is considered a qualitative immunohistochemical
assay. PD-L1 expression in urothelial carcinoma is determined by using
Combined Positive Score (CPS), which is the number of PD-L1 staining cells
(tumor cells, lymphocytes, macrophages) divided by the total number of viable
tumor cells, multiplied by 100.
Urothelial carcinoma tissue specimens that are tested for PD-L1 expression are
scored and divided into two groups based on their Combined Positive Score (CPS):
– CPS < 10
– CPS≥10
For more details on staining and interpretation, please refer to the current version
of the IFU provided with PD-L1 IHC 22C3 pharmDx, Code SK006 or visit
www.agilent.com.
6
Page 7

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Assay Interpretation
The clinical interpretation of any staining, or the absence of staining, must be
complemented by the evaluation of proper controls. Evaluation must be made by
a qualified pathologist within the context of the patient’s clinical history and other
diagnostic tests. This product is intended for in vitro diagnostic (IVD) use.
Reporting Results
To help understand what information should be reported to the treating physician,
please refer to the Reporting Results section of this manual on page 33.
Photomicrographs
The included photomicrographs are of urothelial carcinoma unless otherwise noted.
Note: Photomicrograph magnification levels may appear different than indicated
in respective annotations due to adjustment of image size.
Tissue samples supplied by Asterand Bioscience.
Tissue samples were provided by the Cooperative Human Tissue Network which is funded by the National Cancer Institute.
Other investigators may have received specimens from the same subjects.
Data and tissue used in this project were provided by Tumorgenetics Ltd., Budapest, Hungary with appropriate ethics approval
and through Trans-Hit Biomarkers Inc.
7
Page 8
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
PD-L1 Overview
The PD-1/PD-L1 Pathway
Controls the Immune
Response in Normal Tissue
The Tumor Escapes
Detection by Utilizing the
PD-1/PD-L1 Pathway
Anti-PD-1 Therapy Enables
the Immune Response
Against Tumors
Programmed death-ligand 1 (PD-L1) is a transmembrane protein that binds to
the programmed death-1 receptor (PD-1) during immune system modulation.
The PD-1 receptor is typically expressed on cytotoxic T-cells and other immune
cells, while the PD-L1 ligand is typically expressed on normal cells. Normal cells
use the PD-1/PD-L1 interaction as a mechanism of protection against immune
recognition by inhibiting the action of T-cells (Figure 1). Inactivation of cytotoxic
T-cells downregulates the immune response such that the inactive T-cell is
exhausted, ceases to divide, and might eventually die by programmed cell
death, or apoptosis.
Many tumor cells are able to upregulate the expression of PD-L1 as a mechanism
to evade the body’s natural immune response. Activated T-cells recognize the
PD-L1 marker on the tumor cell, similar to that of a normal cell, and PD-L1
signaling renders the T-cell inactive (Figure 2). The tumor cell escapes the
immune cycle, continues to avoid detection for elimination, and is able
to proliferate.
PD-1/PD-L1 interaction between tumor cells and activated T-cells (Figure 3) is a
mechanistic pathway used by immunotherapeutic agents. When the tumor cell
is unable to interact with the activated T-cell, the immune system remains active,
helping to prevent immunosuppression.
PD-L1 IHC 22C3 pharmDx
Detects PD-L1 in Urothelial
Carcinoma Specimens
8
Detection of PD-L1 upregulation in urothelial carcinoma is a biomarker for
response to anti-PD-1 therapy. PD-L1 IHC 22C3 pharmDx is the only companion
®
diagnostic used in the KEYTRUDA
to evaluate the relationship between PD-L1 expression and clinical efficacy.
KEYTRUDA is a humanized monoclonal PD-1-blocking antibody.
(pembrolizumab) clinical trial (KEYNOTE-052)
Page 9

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
PD-L1 expressing cell
Inactive cytotoxic T-cell
PD-L1
PD-1
Figure 1: Inactivation of T-cells limits damage to normal tissue.
Tumor cell
Inactive cytotoxic T-cell
PD-L1
PD-1
Figure 2: Inactivation of T-cells reduces tumor cell death and elimination.
Tumor cell
Active cytotoxic T-cell
Anti-PD-1
therapy
Figure 3: Blocking the PD -1/PD- L1 interaction helps to enable active T-cells and tumor cell death
and elimination.
9
Page 10
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
PD-L1 IHC 22C3 pharmDx Overview
What is PD-L1 IHC 22C3 pharmDx?
PD-L1 IHC 22C3 pharmDx is the only companion diagnostic indicated as an aid
in identifying patients with urothelial carcinoma for treatment with
®
KEYTRUDA
PD-L1 IHC 22C3 pharmDx is a qualitative immunohistochemical (IHC) assay intended
for use in the detection of PD-L1 protein in formalin-fixed, paraffin-embedded
(FFPE) urothelial carcinoma tissue samples using Autostainer Link 48.
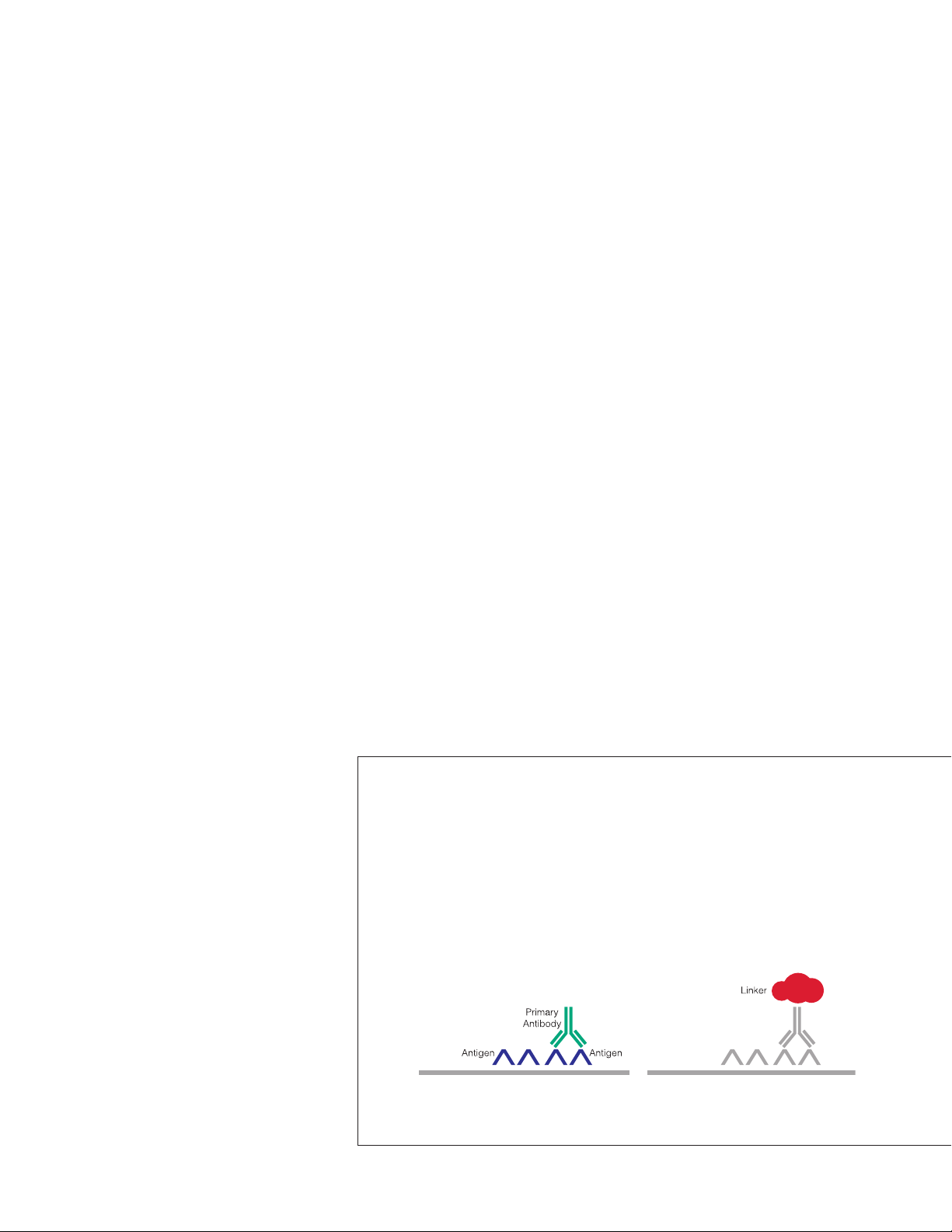
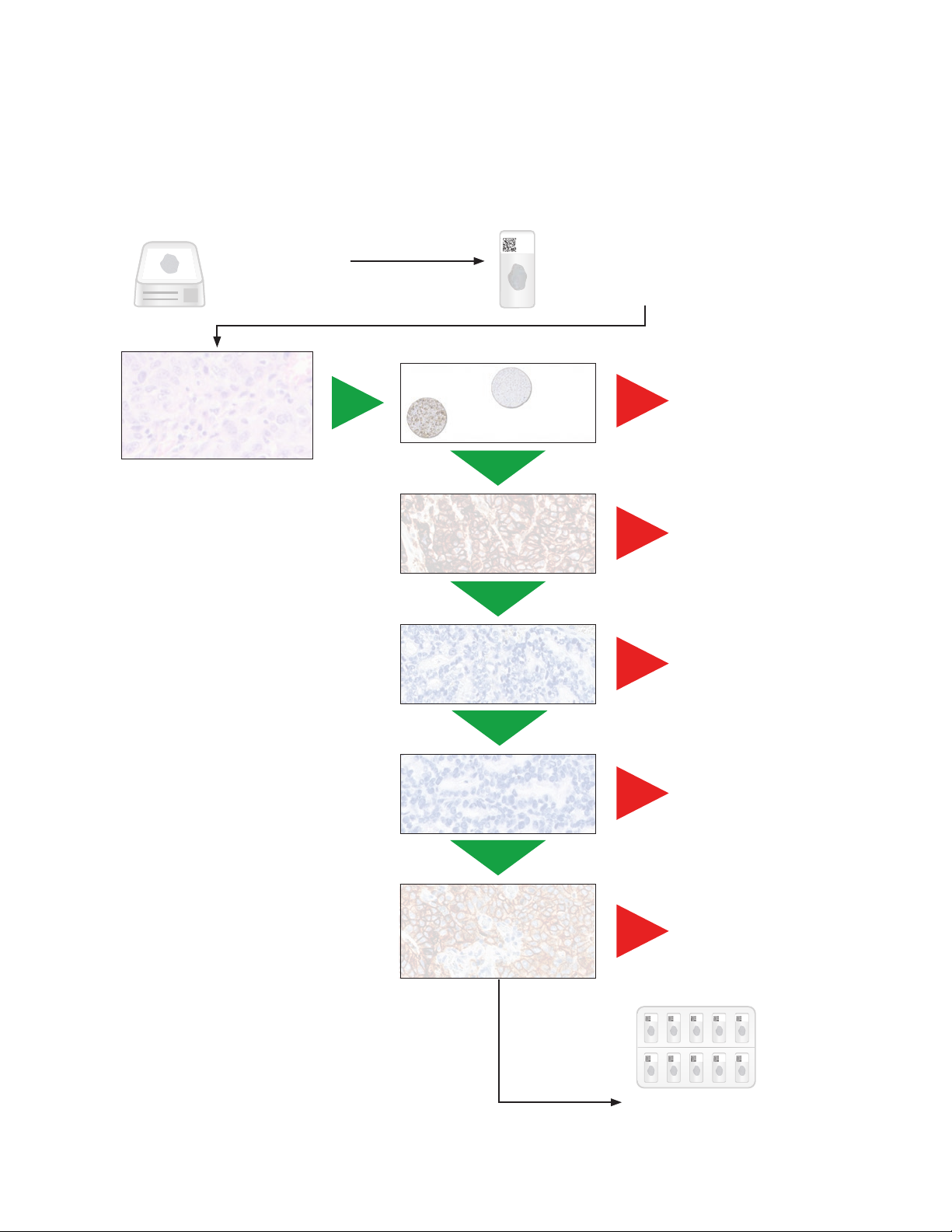
Components of PD-L1 IHC 22C3 pharmDx
PD-L1 IHC 22C3 pharmDx contains optimized reagents to perform an IHC
staining procedure using a linker and a chromogen enhancement reagent
(Figure 4). Deparaffinization, rehydration, and target retrieval is performed
using a 3-in-1 procedure on PT Link. Following peroxidase block, specimens are
incubated with the monoclonal mouse primary antibody to PD-L1 or the Negative
Control Reagent. Specimens are then incubated with a Mouse LINKER, followed
by incubation with a ready-to-use Visualization Reagent consisting of secondary
antibody molecules and horseradish peroxidase molecules coupled to a dextran
polymer backbone.
(pembrolizumab).
The enzymatic conversion of the subsequently added chromogen results in
precipitation of a visible reaction product at the site of the antigen. The color of
the chromogenic reaction is modified by a chromogen enhancement reagent.
The specimen may then be counterstained and coverslipped. Results are
interpreted using a light microscope of diagnostic quality.
Application of primary antibody. Application of Linker.
10
Figure 4: PD-L1 IHC 22C3 pharmDx staining procedure.
Page 11
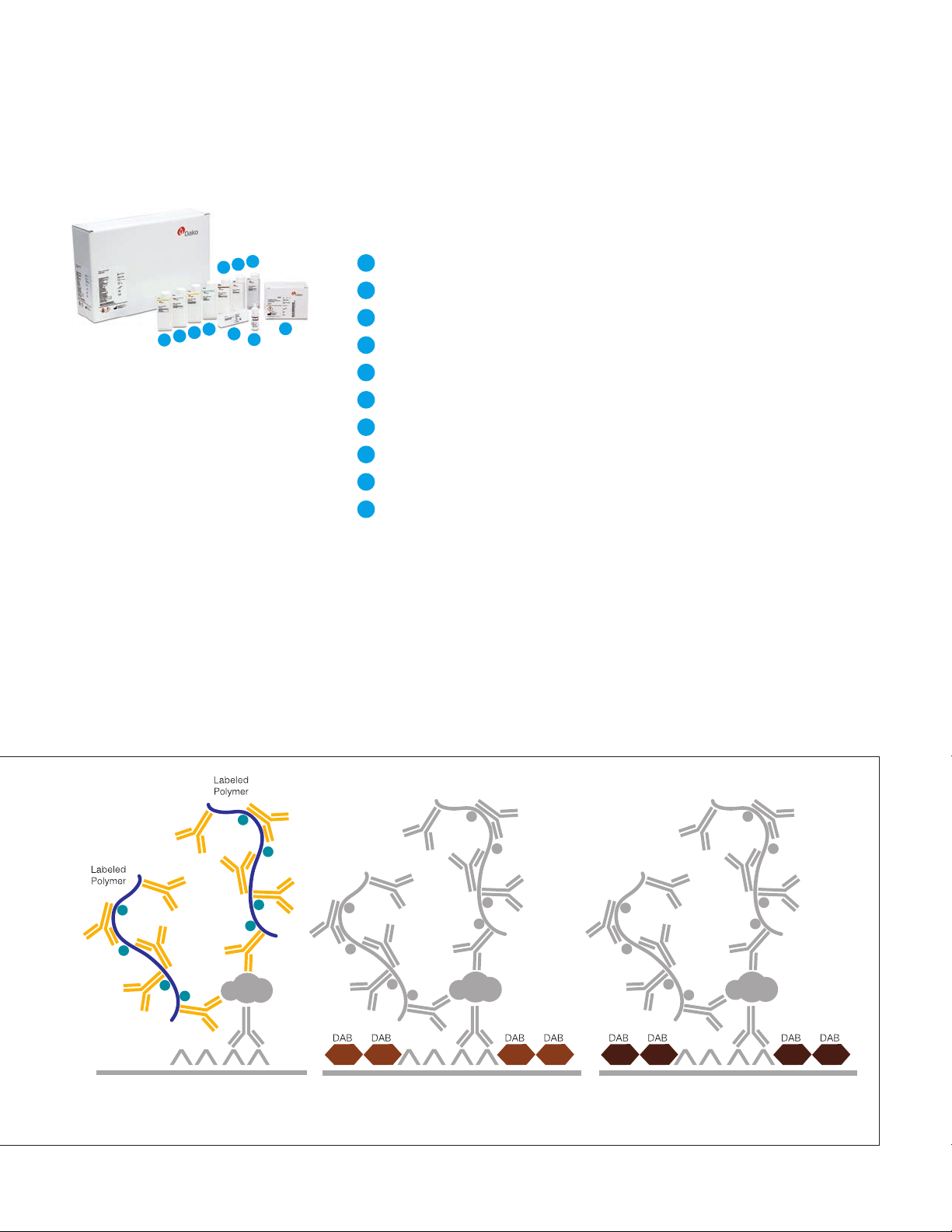
Kit Configuration
4
9
7
5
6
2
3
Figure 5: PD-L1 IHC 22C3
pharmDx components.
* Dr. AF Gazdar and Dr. JD Minna at NIH are acknowledged
for their contribution in developing NCI-H226
(ATCC Number: CRL-5826™)
10
1
8
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
PD-L1 IHC 22C3 pharmDx (Code SK006) contains reagents to perform 50 tests
in up to 15 individual runs (Figure 5):
1
EnVision FLEX Target Retrieval Solution, Low pH (50×)
2
Peroxidase-Blocking
3
Primary antibody: Monoclonal Mouse Anti-PD-L1, Clone 22C3
4
Negative Control Reagent
5
Mouse LINKER
6
Visualization Reagent-HRP
7
DAB+ Substrate Buffer
8
DAB+ Chromogen
9
DAB Enhancer
10
PD-L1 IHC 22C3 pharmDx Control Cell Line Slides*
Reagent
EnVision FLEX Wash Buffer, (20×) (Code K8007) and EnVision FLEX Hematoxylin
(Code K8008) are required but not included in the kit.
Application of Visualization Reagent. Application of DAB+ Substrate
Chromogen Solution.
Application of DAB Enhancer.
11
Page 12

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Technical Considerations
Technical problems related to PD-L1 IHC 22C3 pharmDx may arise and can be attributed to
two factors: specimen collection and preparation prior to performing the test, and the actual
performance of the test itself. Technical problems are generally related to procedural deviations
and can be controlled and minimized through training and, where necessary, clarification of the
product instructions.
Specimen Preparation
In-house Control Tissue
Specimens must be handled to preserve the tissue for immunohistochemical
staining. Determine intact tumor morphology and the presence of sufficient tumor
cells for evaluation. Use standard methods of tissue processing for all specimens.
Differences in processing and embedding in the user’s laboratory may produce
significant variability in results. Include positive and negative in-house control
tissue in each staining run, in addition to the PD-L1 IHC 22C3 pharmDx Control
Cell Line Slide.
Select positive and negative control tissue from fresh specimens of the same
tumor indication as the patient specimen. Fix, process, and embed the control
tissue in the same manner. Control tissues processed differently from the patient
specimen validate reagent performance only and do not verify tissue preparation.
The ideal positive control tissue provides a complete dynamic representation of
weak-to-moderate staining of tumor cells and tumor-associated mononuclear
inflammatory cells (MICs: lymphocytes and macrophages). The negative control
tissue should demonstrate no staining in tumor cells and only a few staining
immune cells.
12
Page 13

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Optional Additional In-house
Control: Tonsil Tissue
Tissue Processing
Tonsil stained with PD-L1 should be pre-screened to exhibit strong staining in
portions of the crypt epithelium and weak-to-moderate staining of the follicular
macrophages in the germinal centers. PD-L1 expression of the endothelium,
fibroblasts, as well as the surface epithelium should be negative.
Formalin-fixed, paraffin-embedded tissues have been validated for use. Block
specimens into a thickness of 3 mm or 4 mm, fix in formalin and dehydrate
and clear in a series of alcohols and xylene, followed by infiltration with melted
paraffin. The paraffin temperature should not exceed 60 °C. Feasibility studies
onNSCLCtissuesampleswereperformedwithfixationin10%neutralbuffered
formalin for 12–72 hours. Fixation times of 3 hours or less should not be used
for PD-L1 assessment. The use of PD-L1 IHC 22C3 pharmDx on decalcified
tissues or tissues processed with other fixatives has not been validated and is
not recommended.
Cut tissue specimens into sections of 4–5 µm. After sectioning, tissues should
be mounted on Dako FLEX IHC microscope slides (Code K8020) or Fisherbrand
Superfrost Plus slides, and then placed in a 58 ± 2 °C oven for 1 hour. Store tissue
sections in the dark at 2–8 °C (preferred) or at room temperature in the dark up
to 25 °C to preserve antigenicity, and stain within the time period given in the IFU
for each temperature condition.
13
Page 14

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
PD-L1 IHC 22C3 pharmDx Staining Procedure
The PD-L1 IHC 22C3 pharmDx reagents and instructions have been designed for optimal
performance. Further dilution of the reagents, alteration of incubation times, temperatures, or
materials may give erroneous results. All of the required steps and incubation times for staining
are pre-programmed in the DakoLink software.
Reagent Storage
Store all components of PD-L1 IHC 22C3 pharmDx, including Control Cell Line
Slides, in the dark at 2–8 °C when not in use.
Reagent Preparation
Equilibrate all components to room temperature (20–25 °C) prior to
immunostaining. Do not use after the expiration date printed on the outside
of the package.
EnVision FLEX Target Retrieval Solution, Low pH
Dilute EnVision FLEX Target Retrieval Solution, Low pH, (50×) 1:50 using
distilled or deionized water (reagent-quality water). One 30 mL bottle of
concentrate provides 1.5 L of working solution, which is sufficient to fill one
PT Link tank. Discard 1× EnVision FLEX Target Retrieval Solution, Low pH after
3 uses or 5 days after dilution.
EnVision FLEX Wash Buffer
Dilute EnVision FLEX Wash Buffer, (20×) 1:20 using distilled or deionized water
(reagent-quality water). Store unused 1× buffer at 2–8 °C for no more than
one month. Discard if cloudy in appearance.
14
Page 15

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
DAB+ Substrate-Chromogen Solution
Add 1 drop of DAB+ Chromogen per mL of DAB+ Substrate Buffer and mix.
Prepared DAB+ Substrate-Chromogen is stable for 5 days if stored in the dark
at 2–8 °C. Mix the DAB+ Substrate-Chromogen Solution thoroughly prior to use.
Any precipitate developing in the solution will not affect staining quality.
– If using an entire bottle of DAB+ Substrate Buffer, add 9 drops of DAB+
Chromogen. Although the DAB+ Substrate Buffer label states 7.2 mL, this is the
usable volume and does not account for the “dead volume” of DAB+ Substrate
Buffer in the bottle
– The color of the DAB+ Chromogen may vary from clear to lavender brown.
This will not affect the performance of the product. Dilute per the guidelines
above. Adding excess DAB+ Chromogen to the DAB+ Substrate Buffer results
in deterioration of the positive signal
Controls to Assess Staining Quality
The following quality controls should be included in each staining run:
– One PD-L1 IHC 22C3 pharmDx Control Cell Line Slide stained with
the primary antibody
– Positive and negative in-house control tissues stained with the
primary antibody
– Subsequent sections of each patient specimen stained with the
Negative Control Reagent
15
Page 16

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Deparaffinization, Rehydration, and Target Retrieval
Use PT Link to perform a Deparaffinization, Rehydration, and Target Retrieval
3-in-1 procedure.
– Set Preheat and Cool to 65 °C, and set Heat to 97 °C for 20 minutes
– Fill PT Link tanks with 1.5 L per tank of 1× EnVision FLEX Target Retrieval
Solution, Low pH working solution to cover the tissue sections
– Preheat the Target Retrieval Solution, Low pH to 65 °C
– Immerse Autostainer racks containing mounted, FFPE tissue sections into
the preheated Target Retrieval Solution, Low pH in PT Link tank. Incubate
for 20 minutes at 97 °C
– When incubation has been completed and the temperature has cooled to
65 °C, remove each Autostainer slide rack with slides from the PT Link tank
and immediately place the slides into a tank (e.g., PT Link Rinse Station,
Code PT109) containing room temperature 1× EnVision FLEX Wash Buffer
working solution
– Leave Autostainer rack with slides in room temperature 1× EnVision FLEX
WashBufferfor5minutes
Staining and Counterstaining
– Place the Autostainer rack with slides on the Autostainer Link 48
– Ensure slides remain wet with buffer while loading and prior to initiating the
run. Dried tissue sections may display increased non-specific staining
– Select the PD-L1 IHC 22C3 pharmDx protocol. The instrument performs the
staining and counterstaining procedures by applying the appropriate reagent,
monitoring the incubation time, and rinsing slides between reagents
– Counterstain slides using EnVision FLEX Hematoxylin, Code K8008
Mounting
Use non-aqueous permanent mounting media. To minimize fading, store slides
in the dark at room temperature (20–25 °C).
16
Page 17
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
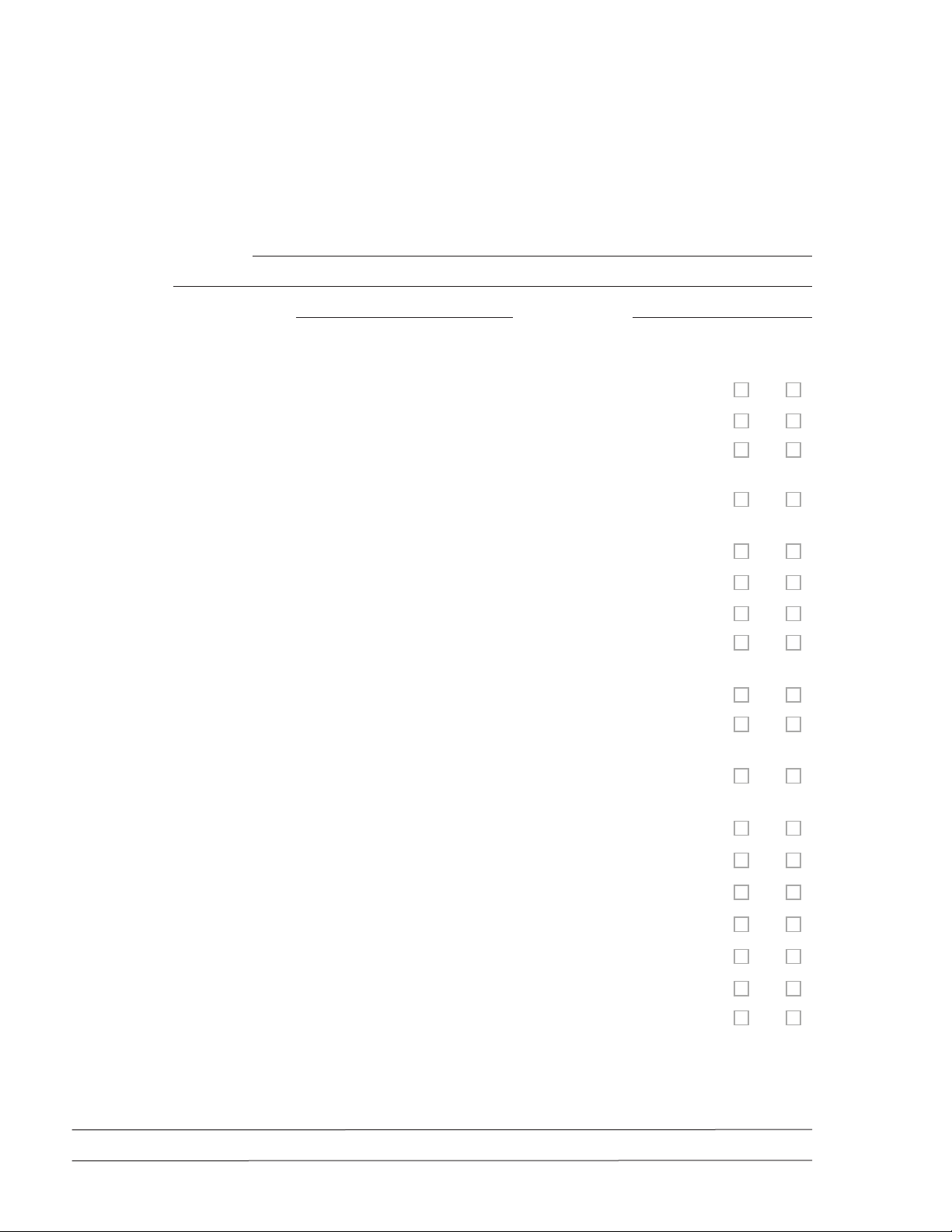
Technical Checklist
Use the checklist below to ensure correct usage of PD-L1 IHC 22C3 pharmDx:
Customer Name/Institution
Name and Title
Autostainer Link 48 Serial Number Software Version
Regular preventive maintenance is performed on the Autostainer Link 48 and PT Link?
PD-L1 IHC 22C3 pharmDx is used before the expiration date printed on the outside of the box?
All PD-L1 IHC 22C3 pharmDx components, including Control Cell Line Slides, are stored in the dark
at 2–8 °C?
All PD-L1 IHC 22C3 pharmDx components, including Control Cell Line Slides, are equilibrated to
room temperature (20–25 °C) prior to immunostaining?
Yes No
Appropriate positive and negative control tissue from urothelial carcinoma are identified?
Tissues are fixed in neutral buffered formalin?
Tissues are infiltrated with melted paraffin, at or below 60 °C?
Tissue sections of 4–5 µm are mounted on Dako FLEX IHC Microscope Slides or Fisherbrand
Superfrost Plus charged slides?
Specimens are oven-dried at 58 ± 2 °C for 1 hour?
Specimens are stained within the time period(s) given in the IFU when stored in the dark at 2–8 °C
(preferred) or at room temperature in the dark up to 25 °C?
EnVision FLEX Target Retrieval Solution, Low pH is prepared properly? pH of 1× Target Retrieval
Solution must be 6.1 ± 0.2.
EnVision FLEX Wash Buffer is prepared properly?
DAB+ Substrate-Chromogen Solution is prepared properly?
Slides are counterstained with EnVision FLEX Hematoxylin?
The Deparaffinization, Rehydration, and Target Retrieval 3-in-1 procedure is followed using PT Link?
Slides remain wet with buffer while loading and prior to initiating run on Autostainer Link 48?
The PD-L1 IHC 22C3 pharmDx protocol is selected on Autostainer Link 48?
Do you have all the necessary equipment to perform the PD-L1 IHC 22C3 pharmDx according
to protocol? If not, specify what is missing in comments below.
Additional observations or comments:
17
Page 18
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Slide Evaluation
General Considerations
Specimen Adequacy
PD-L1 IHC 22C3 pharmDx evaluation should be performed by a qualified
pathologist using a light microscope of diagnostic quality. Details of the PD-L1
IHC 22C3 pharmDx interpretation guidelines are reviewed on page 30. Before
examining the patient specimen for PD-L1 staining, it is important to examine the
controls to assess staining quality.
PD-L1 interpretation is best assessed by requesting 3 serial tissue sections (H&E,
PD-L1 stain, and NCR stain) so that if the H&E is first assessed and is acceptable,
IHC staining of the remaining 2 serial sections is likely to be acceptable.
Each PD-L1 IHC 22C3 pharmDx is configured with Control Cell Line Slides that
should be included in each IHC run. Guidelines on interpreting the Control Cell
Line Slide are reviewed to the right. In-house control tissue slides should also be
assessed with every IHC run.
Confirm the Presence of at Least 100 Viable Tumor Cells
A hematoxylin and eosin (H&E) stained section is recommended for the
evaluation of specimen adequacy. PD-L1 IHC 22C3 pharmDx and the H&E
staining should be performed on serial sections from the same paraffin block
of the specimen.
A minimum of 100 viable tumor cells must be present in the PD-L1
stained slide for the specimen to be considered adequate for
PD-L1 evaluation.
Instructions for Patient Specimens With Less Than 100 Viable
Tumor Cells
Tissue from a deeper level of the block, or potentially another block, could have
a sufficient number of viable tumor cells for PD-L1 IHC 22C3 pharmDx testing.
18
Page 19

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Evaluating Controls
Figure 6: Each Control Cell Line Slide
contains sections of cell pellets with
positive and negative PD-L1 expression.
PD-L1 IHC 22C3 pharmDx Control Cell Line Slide
Examine the PD-L1 IHC 22C3 pharmDx Control Cell Line Slide to determine that
reagents are functioning properly. Each slide contains sections of cell pellets
with positive and negative PD-L1 expression (Figure 6). Assess the percentage
of positive cells and the staining intensity. If any staining of the Control Cell
Line Slide is not satisfactory, all results with the patient specimens should be
considered invalid.
Evaluate the overall staining intensity using the following guide:
0 Negative
1+ Weak intensity
2+ Moderate intensity
3+ Strong intensity
Positive Control Cell Pellet
The following staining is acceptable for the PD-L1 positive cell pellet (Figure 7):
– Cellmembranestainingof≥70%ofcells
– ≥2+averagestainingintensity
– Non-specific staining < 1+ intensity
Figure 7: Positive cell pellet with acceptable staining of PD- L1 IHC 22C3 pharmDx Control Cell
Line Slide (20× magnification).
19
Page 20
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
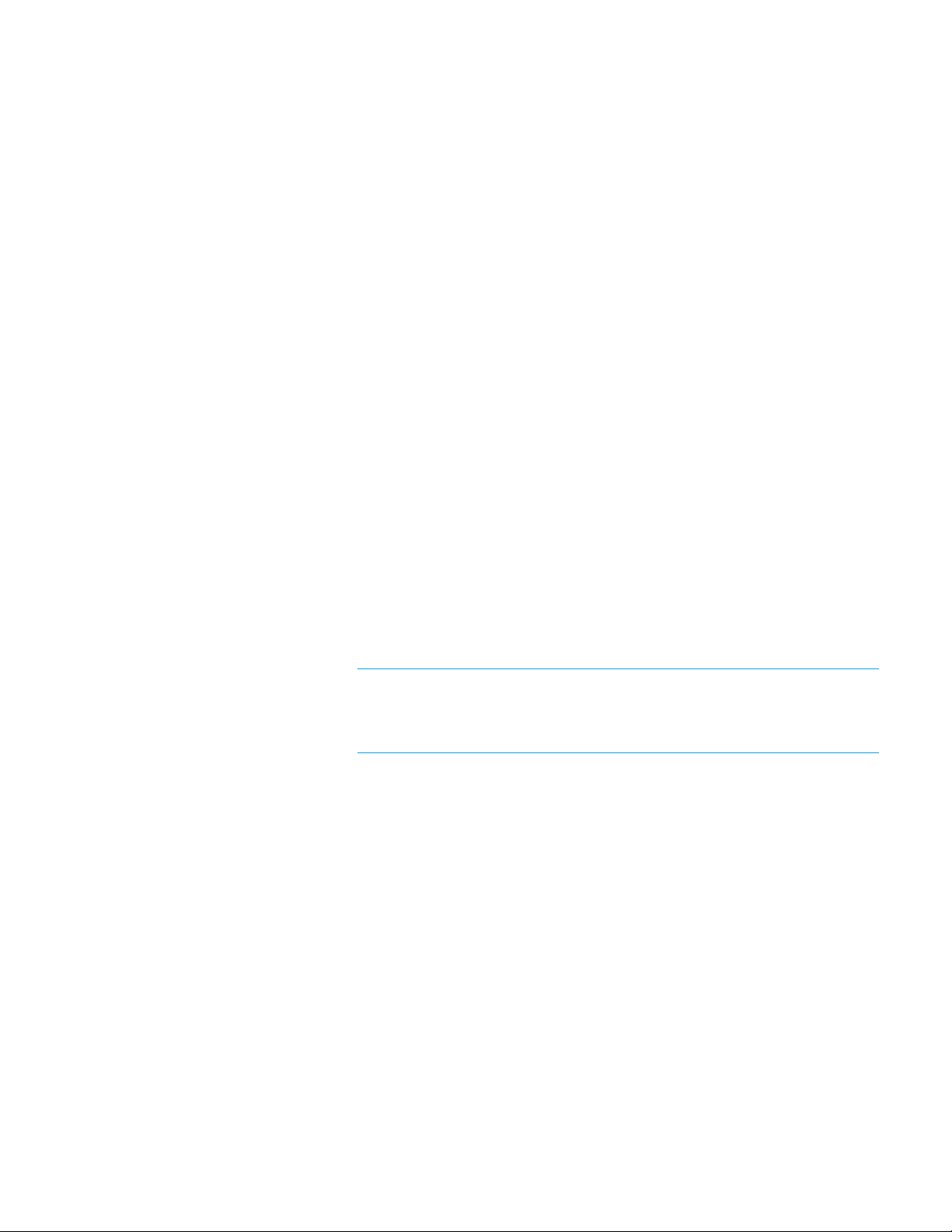
Negative Control Cell Pellet
For the PD-L1 negative cell pellet, the following staining is acceptable (Figure 8):
– The majority of cells should demonstrate no staining. Note: The presence of
10 or fewer cells with distinct cell membrane staining is acceptable
– Any background staining is less than 1+ staining intensity
Figure 8: Negative cell pellet with no staining of PD -L1 IHC 22C3 pharmDx Control Cell Line Slide
(20× magnification).
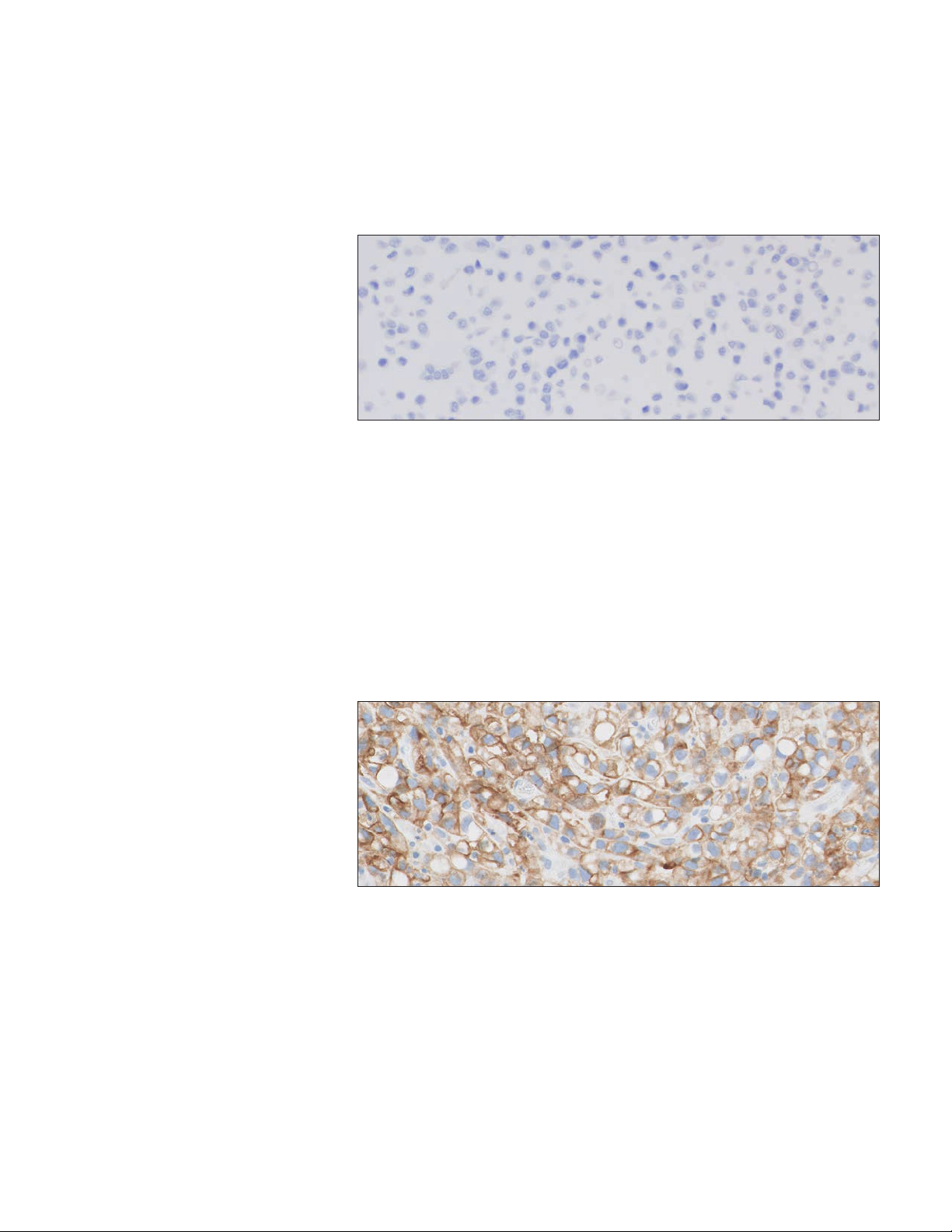
Positive and Negative In-house Control Tissue (Urothelial Carcinoma)
Examine the positive in-house urothelial carcinoma control tissue to determine
that the tissues are correctly prepared and reagents are functioning properly.
The ideal positive control tissue provides a complete dynamic representation of
weak-to-moderate staining of tumor cells and tumor-associated mononuclear
inflammatory cells (MICs) (Figure 9). If staining of positive in-house control
tissue is not satisfactory, all results with the patient specimen should be
considered invalid.
Figure 9: Ideal positive in-house control tissue (20× magnification).
The ideal negative control tissue should demonstrate no staining on tumor cells
and immune cells (Figure 10). However, because prevalence of PD-L1 expression
on immune cells is high, staining immune cells are acceptable. Examine the
negative in-house control tissue to determine the expected staining. The variety
of different cell types present in most tissue sections offers internal negative
control sites; this should be verified by the user.
If unwanted staining occurs in the in-house control tissues, results with the
patient specimen should be considered invalid.
20
Page 21
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Figure 10: Ideal negative in -house control tissue demonstrating PD -L1 positive expression of
CPS < 1 (20× magnification).
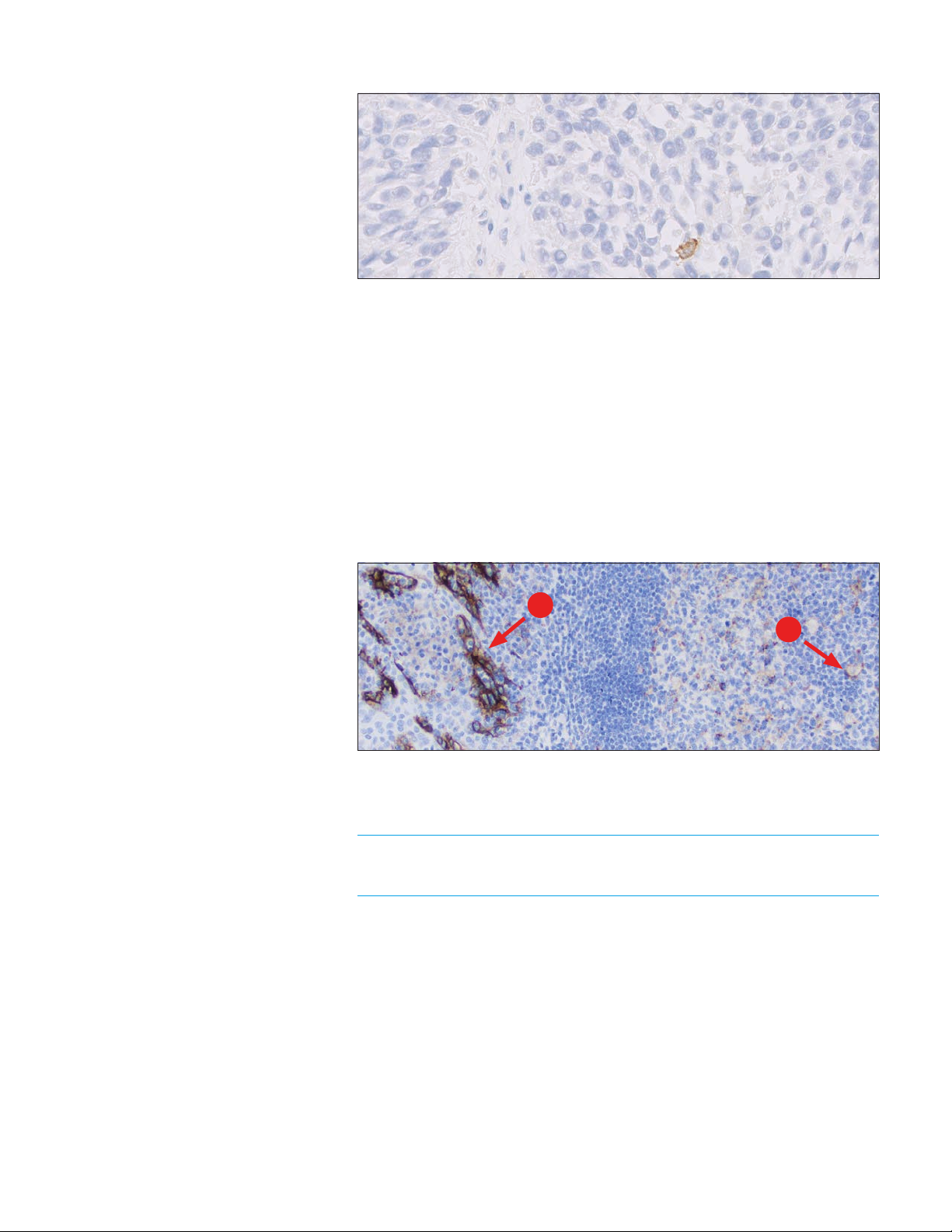
Optional Control Tissue
In addition to the Control Cell Line Slide and in-house control tissues, FFPE tonsil
may also be used as an optional control specimen. Tonsil stained with PD-L1
should exhibit strong membrane staining in portions of the crypt epithelium
and weak-to-moderate membrane staining of the follicular macrophages in the
germinal centers (Figure 11).
PD-L1 expression of the endothelium, fibroblasts, and the surface epithelium
should be absent.
A
B
Figure 11: Tonsil stained with PD -L1 primary antibody exhibiting strong membrane staining
in portions of the crypt epithelium (A) and weak-to-moderate membrane staining of follicular
macrophages in the germinal centers (B) (10× magnification).
Do not use in-house control tissue as an aid in interpretation of
patient results.
21
Page 22
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
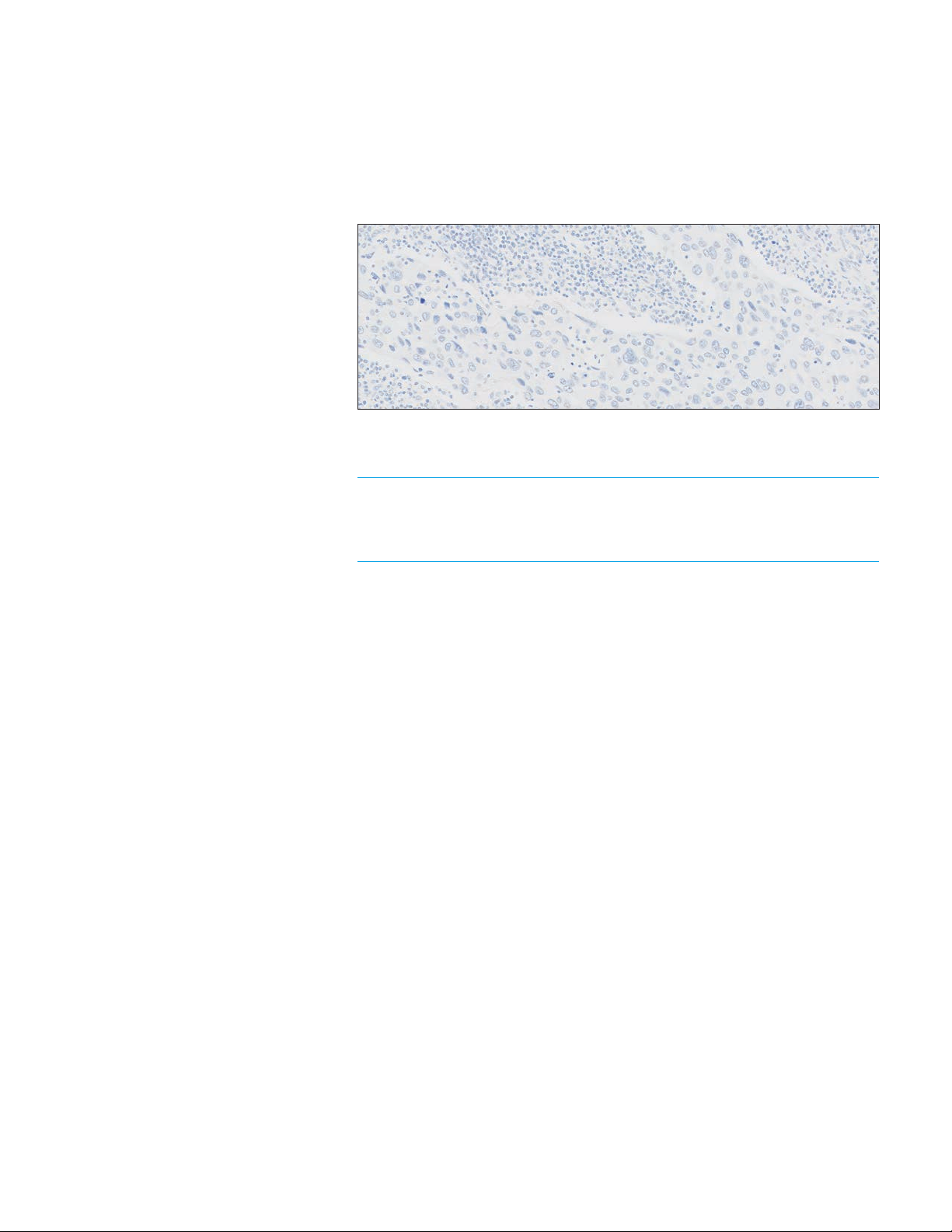
Negative Control Reagent (NCR)
Examine the slides stained with the NCR to identify non-specific background
staining that may interfere with PD-L1 staining interpretation, making the
specimen non-evaluable. Satisfactory performance is indicated by the absence
of staining (Figure 12).
Figure 12: Ideal negative in-house control tissue stained with Negative Control Reagent showing
no specific staining (20× magnification).
Negative Control Reagent stained slides indicate non-specific
background staining and allow for better interpretation of patient
specimens stained with the primary antibody.
22
Page 23
Slide Evaluation Flowchart
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Tissue Block
3 serial sections are
cut/prepared
One section is stained with
H&E (H&E Patient Specimen)
Is H&E slide adequate?
(intact, well-preserved,
urothelial carcinoma)
Yes
Control Cell Line
Slide adequate?
Yes
Positive control
tissue adequate?
Yes
Negative control
tissue adequate?
Sections of 4–5 µm thickness
are mounted on glass
microscope slides
No
No
No
Repeat
staining run
Repeat
staining run
Repeat
staining run
Figure 13: Recommended order of slide evaluation.
Yes
Patient specimen stained with
Negative Control Reagent
adequate?
Yes
Patient specimen stained with
primary antibody exhibiting
≥ 100 viable tumor cells?
Scored by
Pathologist
No
Repeat staining run
No
with a deeper cut in
the block or a new
patient specimen
Provide case report
Repeat
staining run
23
Page 24

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Combined Positive Score
Definition of Combined
Positive Score (CPS)
* Macrophages and histiocytes are
considered the same cells
CPS Numerator Inclusion
and Exclusion Criteria
PD-L1 expression in urothelial carcinoma is determined by using Combined
Positive Score (CPS), which is the number of PD-L1 staining cells (tumor cells,
lymphocytes, macrophages*) divided by the total number of viable tumor cells,
multiplied by 100. Although the result of the calculation can exceed 100, the
maximum score is defined as CPS 100.
CPS is defined accordingly:
# PD-L1 staining cells (tumor cells,
CPS =
Any convincing partial or complete linear membrane staining (≥ 1+) of
viable tumor cells that is perceived as distinct from cytoplasmic staining
is considered PD-L1 staining and should be included in scoring.
Any convincing membrane and/or cytoplasmic staining (≥ 1+) of
lymphocytes and macrophages (mononuclear inflammatory cells, MICs)
within tumor nests and/or immediately adjacent supporting stroma
is considered PD-L1 staining and should be included in scoring. Only
mononuclear inflammatory cells (MICs) directly associated with the
response against the tumor are scored.
lymphocytes, macrophages)
× 100
Total # viable tumor cells
See Table 1 on page 26 for additional CPS numerator inclusion/
exclusion criteria.
24
Page 25

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Determining Combined
Positive Score
– At lower magnifications (4×, 10×), examine all well-preserved tumor areas.
Evaluate overall areas of PD-L1 staining and non-staining tumor cells, keeping
in mind that partial membrane staining or 1+ membrane staining may be
difficult to see at low magnifications. Ensure there are at least 100 viable
tumor cells in the sample
A minimum of 100 viable tumor cells must be present in the PD-L1 stained
°
slide (biopsy and resection) for the specimen to be considered adequate
for evaluation
– For specimens with less than 100 viable tumor cells, tissue from a deeper
level of the block or potentially another block could have a sufficient number
of tumor cells for evaluation of PD-L1 expression
– At higher magnification (20×), evaluate PD-L1 expression and calculate CPS:
Determine the total number of viable tumor cells, both PD-L1 staining and
°
non-staining (CPS denominator)
Determine the number of PD-L1 staining cells (tumor cells, lymphocytes,
°
macrophages) (CPS numerator; see Table 1 on page 26 for additional CPS
numerator inclusion/exclusion criteria)
Calculate CPS
°
– Evaluation of membrane staining should be performed at no higher than
20× magnification. Slide reviewer should not perform the CPS calculation
at 40× magnification
25
Page 26
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Table 1: CPS numerator inclusion/exclusion criteria
Tissue Elements
Tumor Cells Convincing partial or complete linear
Included in the Numerator Excluded from the Numerator
– Non-staining tumor cells
membrane staining (at any intensity)
of viable urothelial carcinoma tumor
cells including:
– High grade papillary carcinoma
– Tumor cells with only
cytoplasmic staining
– Low grade papillary carcinoma
§
– Carcinoma in situ (CIS)
– Any lamina propria, muscularis, or
serosal invasion
– Metastatic carcinoma
Immune Cells Membrane and/or cytoplasmic*
staining (at any intensity) of
mononuclear inflammatory cells (MICs)
within tumor nests and adjacent
supporting stroma
†
:
– Lymphocytes (including
lymphocyte aggregates)
– Macrophages
‡
Only MICs directly associated with the
response to the tumor are scored
– Non-staining MICs
– MICs (including lymphoid
aggregates) associated with
ulcers, chronic cystitis, and other
processes not associated with
the tumor
– MICs associated with
normal structures
– Neutrophils, eosinophils,
and plasma cells
– BCG**-induced granulomas
Other Cells Not included
– Normal cells
– Stromal cells
(including fibroblasts)
– Necrotic cells and/or
cellular debris
* In MICs, membrane and cytoplasmic staining are often indistinguishable due to high nuclear to cytoplasmic ratio. Therefore,
membrane and/or cytoplasmic staining of MICs are included in the score
†
Adjacent MICs are defined as being within the same 20× field as the tumor. However, MICs that are NOT directly associated
with the response to the tumor should be excluded
‡
Macrophages and histiocytes are considered the same cells
§
If the tumor consists entirely of low grade papillary carcinoma, the result should be flagged as such
** bacillus Calmette-Guérin
Table 2: CPS denominator inclusion/exclusion criteria
Tissue Elements Included in the Denominator Excluded from the Denominator
Tumor Cells All viable tumor cells including:
– High grade papillary carcinoma
– Any necrotic or non-viable tumor cells
– Low grade papillary carcinoma
– Carcinoma in situ (CIS)
– Any lamina propria, muscularis, or
serosal invasion
– Metastatic carcinoma
Immune Cells Not included All immune cells of any type
Other Cells Not included
– Normal cells
– Stromal cells (including fibroblasts)
– Necrotic cells and/or cellular debris
††
If the tumor consists entirely of low grade papillary carcinoma, the result should be flagged as such
††
26
Page 27
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Suggested Methods
Agilent recommends that scoring be performed within the context of the
pathologist’s past experience and best judgment in interpreting IHC stains. We
offer three different examples of techniques that may be used when determining
the respective Combined Positive Scores (CPS) of various staining patterns.
The entire IHC slide should be reviewed to determine which of the following
example techniques may be used.
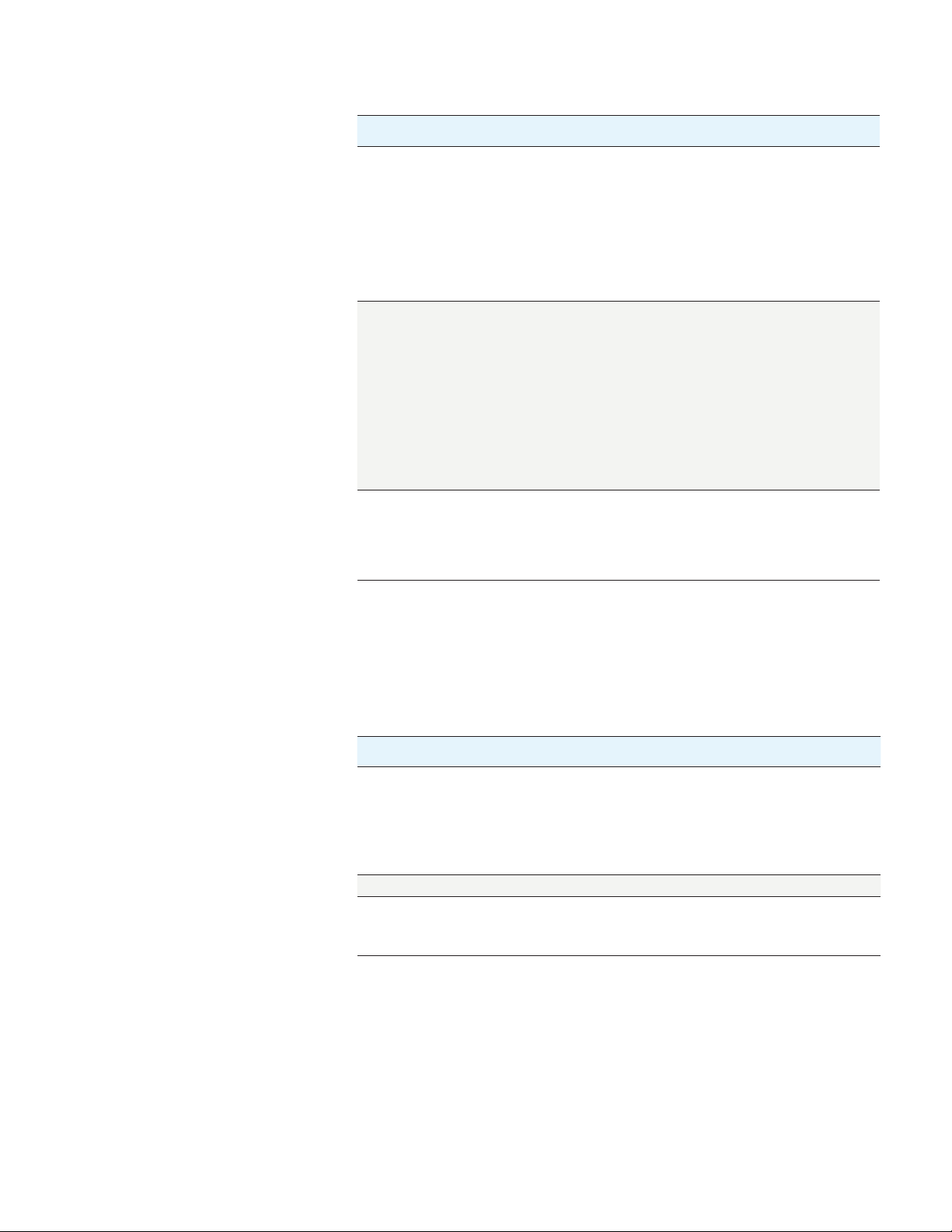
Example 1: Calculation of Combined Positive Score in a Small Tumor Area With Staining
At lower magnifications (4×, 10×): Evaluate the tumor
area for convincing staining as described in “Determining
Combined Positive Score” on page 25.
Assessment: 10% of area with staining, 90% of area
without staining
All tumor
At higher magnification (20×): Confirm there is no
staining in areas that appeared void of staining at
lower magnifications. Evaluate the area of staining to
estimate the number of PD-L1 staining cells (tumor cells,
lymphocytes, macrophages). Also estimate the total
number of viable tumor cells (PD-L1 staining and
non-staining tumor cells).
Assessment: There are approximately 100 viable tumor
cells and about 80 PD-L1 staining cells (per the
CPS numerator)
90%unstained
10%stained
Calculate the Combined Positive Score of the entire tumor area:
Assessment:
CPS of area with staining:
CPS
= × 100 =
Total # viable tumor cells
# PD-L1 staining cells*
CPS of entire tumor area:
10%×80=~CPS8
~80 PD-L1 staining cells
100 tumor cells
× 100 = 80
PD-L1 staining tumor cell
PD-L1 non-staining tumor cell
PD-L1 staining mononuclear
inflammatory cell (MIC)
PD-L1 non-staining
mononuclear inflammatory
cell (MIC)
Clinical Interpretation: CPS < 10
* Including tumor cells, lymphocytes, macrophages
Figure 14: Example of tumor with small staining area.
27
Page 28

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
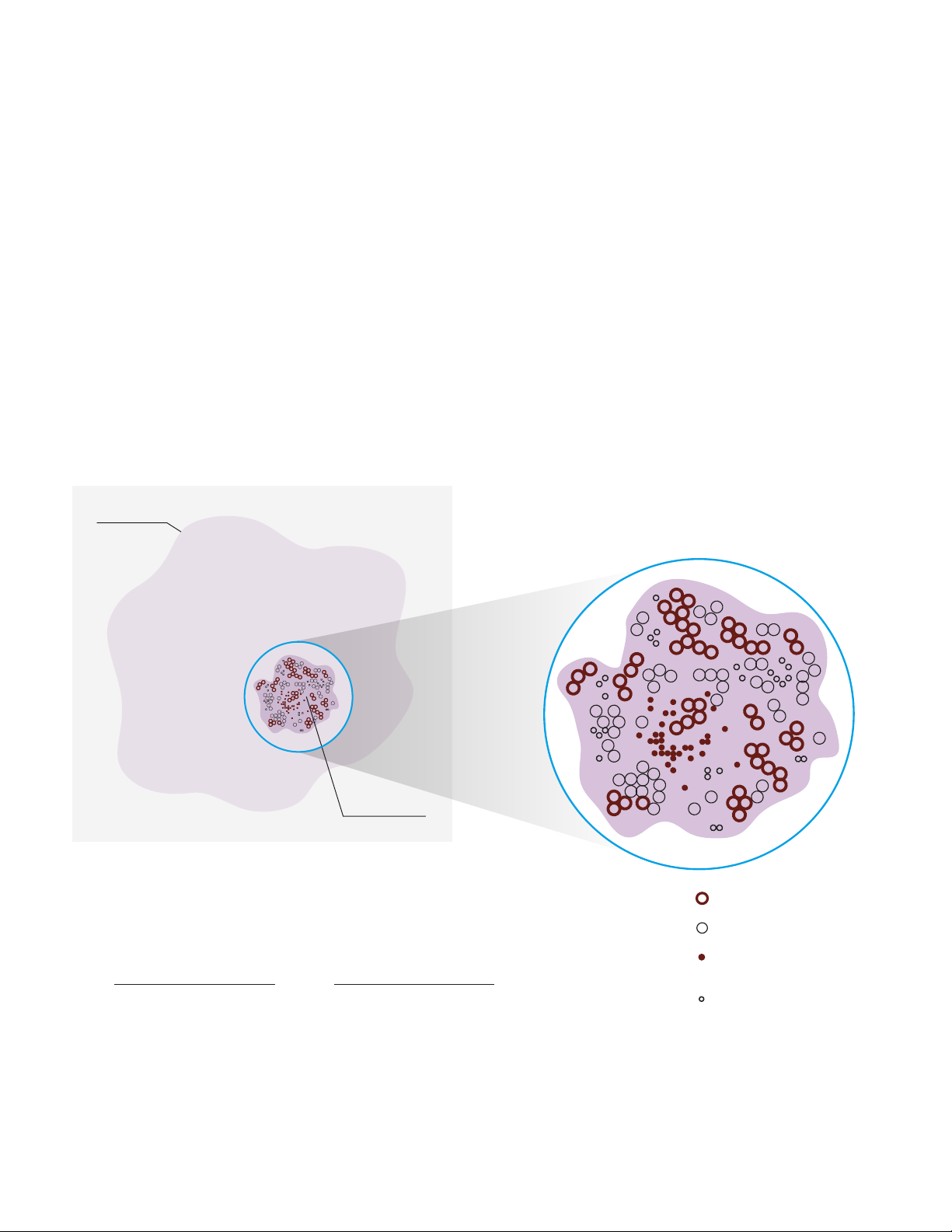
Example 2: Calculation of Combined Positive Score in a Heterogeneous Tumor Area
At lower magnifications (4×, 10×): Visually divide the tumor
area into regions with equal numbers of tumor cells.
At higher magnification (20×): Observe each region and
estimate the total number of viable tumor cells and PD-L1
staining cells (tumor cells, lymphocytes, macrophages).
Calculate the Combined Positive Score for each region.
Assessment: The four sections have ~80, ~30, ~50,
and ~100 PD-L1 staining cells (tumor cells, lymphocytes,
macrophages). Each section has a total of 100 tumor cells
(including PD-L1 staining cells). The CPS for each section:
~CPS 80, ~CPS 30, ~CPS 50, and ~CPS 100
~CPS 80 ~CPS 30
~CPS 50
PD-L1 staining tumor cell
PD-L1 non-staining tumor cell
PD-L1 staining mononuclear
inflammatory cell (MIC)
Calculate the Combined Positive Score of the entire tumor area:
Assessment:
Combined Positive Score:
(80 + 30 + 50 + 100) / 4 = ~CPS 65
# PD-L1 staining cells (tumor cells,
lymphocytes, macrophages)
CPS =
Total # viable tumor cells
ClinicalInterpretation:CPS≥10
~CPS 100
× 100
Figure 15: Example with heterogeneous tumor area.
28
Page 29
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
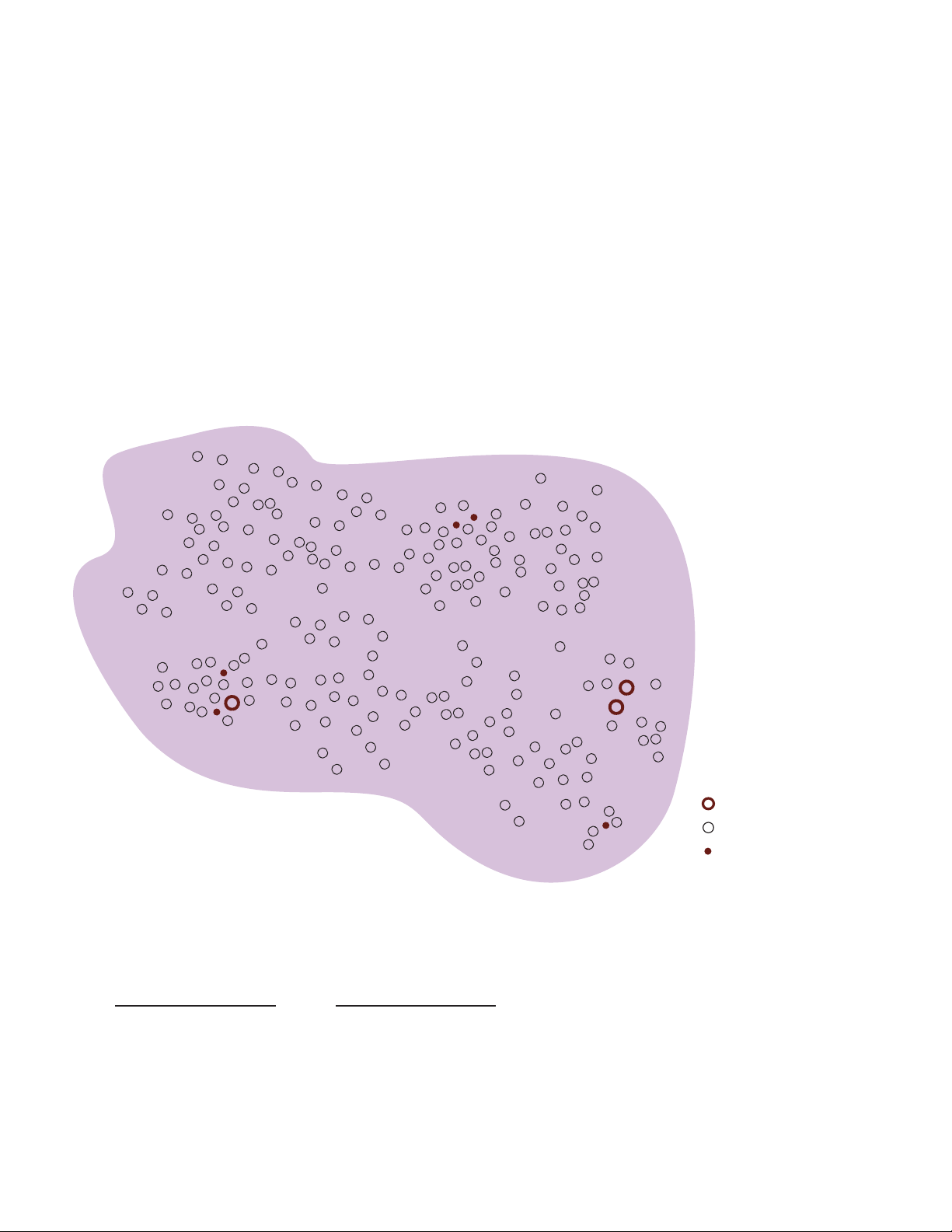
Example 3: Calculation of Combined Positive Score for a Near Cut-off Specimen (CPS 1–20)
At lower magnifications (4×, 10×): Evaluate the specimen
for convincing staining as described in “Determining
Combined Positive Score” on page 25.
At higher magnification (20×): Confirm that there is no
staining in areas that appeared void of staining at lower
magnifications. Evaluate all staining areas and estimate
the total number of PD-L1 staining cells (tumor cells,
lymphocytes, macrophages). Then re-evaluate the entire
specimen (staining and non-staining areas) and estimate
the total number of viable tumor cells (PD-L1 staining and
non-staining tumor cells). Calculate the Combined
Positive Score.
Assessment: Four areas of the tumor specimen have
convincing staining. There are 8 PD-L1 staining cells (tumor
cells, lymphocytes, macrophages) in the four staining areas.
There are approximately 200 viable tumor cells present in the
entire specimen
Calculate the Combined Positive Score of the entire tumor area:
Assessment:
Combined Positive Score:
# PD-L1 staining cells*
= × 100 =
CPS
Total # viable tumor cells
8 PD-L1 staining cells
200 tumor cells
Clinical Interpretation: CPS < 10
* Including tumor cells, lymphocytes, macrophages
Figure 16: Example of near cut-off specimen (CPS 1–20).
PD-L1 staining tumor cell
PD-L1 non-staining tumor cell
PD-L1 staining mononuclear
inflammatory cell (MIC)
× 100 = CPS 4
29
Page 30
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Interpretation of CPS
The Combined Positive Score describes the PD-L1 expression of the specimen.
See the table below for scoring guideline examples.
Table 3: CPS and PD-L1 expression
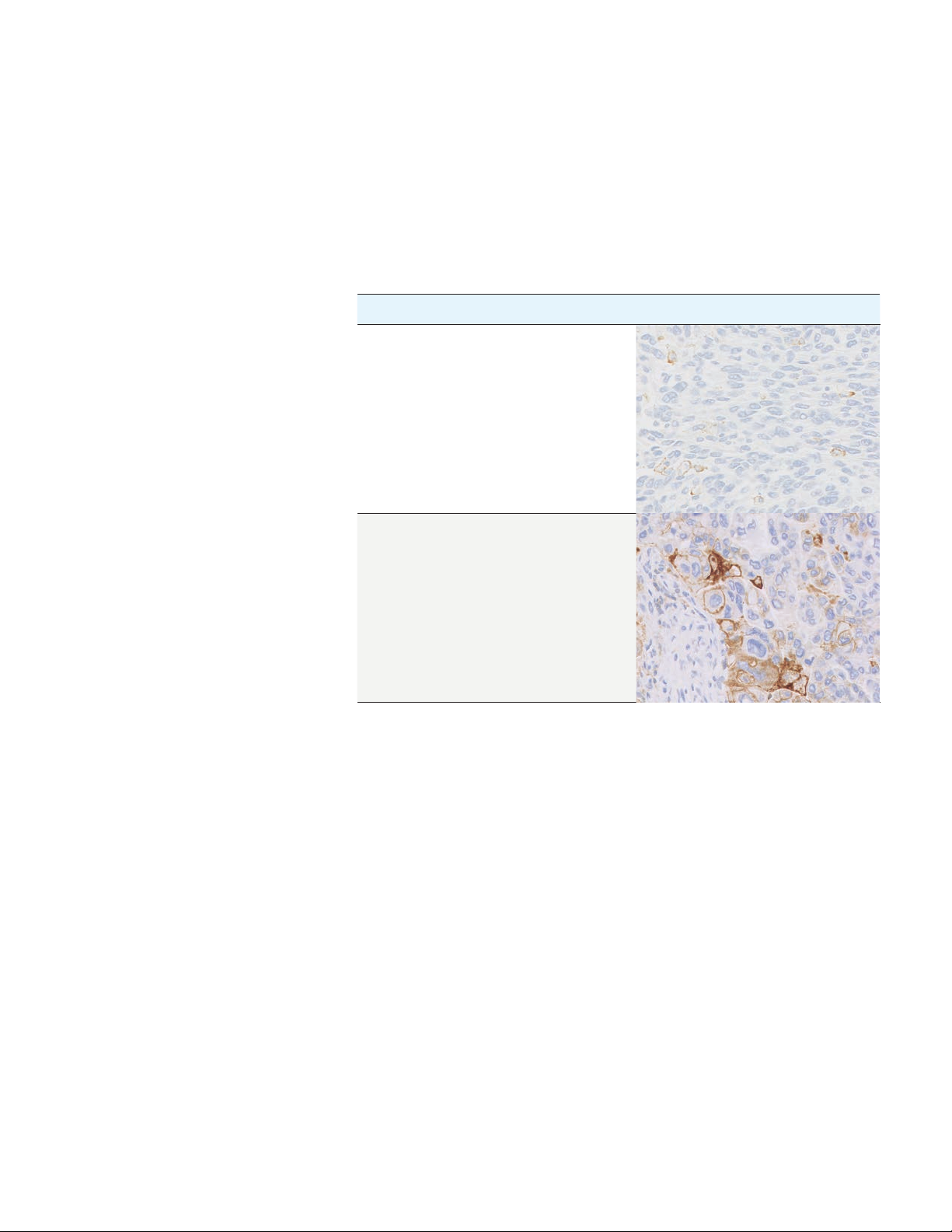
CPS PD-L1 Expression Image (20×)
< 10 CPS is less than 10
≥ 10 CPS is greater than or equal to 10
30
Page 31
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Identifying Patients With
Urothelial Carcinoma
for Treatment
* Based on all enrolled subjects into KEYNOTE-052 (n=370)
†
9 patients had unknown PD-L1 status
PD-L1 IHC 22C3 pharmDx is the only companion diagnostic indicated
as an aid in identifying patients with urothelial carcinoma for treatment with
®
KEYTRUDA
(pembrolizumab).
Clinical Validation of PD-L1 IHC 22C3 pharmDx in Locally Advanced
or Metastatic Urothelial Carcinoma Patients Not Eligible for
Cisplatin-containing Chemotherapy
The clinical validity of PD-L1 IHC 22C3 pharmDx in evaluating PD-L1 expression
in patients not eligible for cisplatin-containing chemotherapy with locally
advanced or metastatic urothelial carcinoma is based on the KEYTRUDA
KEYNOTE-052 study sponsored by Merck Sharp & Dohme Corp. Specimens from
patients were tested for PD-L1 expression using PD-L1 IHC 22C3 pharmDx. Thirty
percent of enrolled patients had tumors that expressed PD-L1 with a Combined
PositiveScore(CPS)ofgreaterthanorequalto10(CPS≥10).
Clinical efficacy of KEYTRUDA treatment is presented in the Clinical Performance
Evaluation section on pages 72–73.
Table 4: PD-L1 prevalence in patients with urothelial carcinoma enrolled in KEYNOTE-052*
PD-L1 Expression CPS < 10 CPS ≥ 10
Prevalence (n)
†
69.5% (251) 30.5% (110)
31
Page 32

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
PD-L1 IHC 22C3 pharmDx
Testing Scheme
Use the following flowchart to help you understand which patients are indicated
®
for treatment with KEYTRUDA
(pembrolizumab) based on their CPS and
treatment history.
Locally advanced or metastatic urothelial carcinoma patient
specimen ineligible for cisplatin-containing chemotherapy
Use PD-L1 IHC 22C3 pharmDx to determine PD-L1 expression
Pathologist reports numerical CPS and CPS category
CPS < 10
Oncologist determines treatment
Locally advanced or metastatic urothelial carcinoma patients ineligible
for cisplatin-containing chemotherapy are indicated for treatment with
KEYTRUDAifCPS≥10
CPS ≥ 10
Figure 17: Testing algorithm for PD-L1 IHC 22C3 pharmDx.
32
Page 33
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Reporting Results
Suggested information to include when reporting results for urothelial carcinoma with PD-L1 IHC 22C3 pharmDx.
PD-L1 IHC 22C3 pharmDx Summary of Sample Tested
Date of Run: __________________________________________________________________________________________________________________
PD-L1 IHC 22C3 pharmDx Lot: ________________________________________________________________________________________________
Staining Run Log ID: __________________________________________________________________________________________________________
Specimen ID: _________________________________________________________________________________________________________________
Patient Identifiers: ____________________________________________________________________________________________________________
Type of Service: IHC Stain with Manual Interpretation
Other: ________________________________________________________________________________________________________________________
PD-L1 Included in Urothelial Carcinoma Comprehensive Panel: Yes:
No:
PD-L1 Testing Results
Control Cell Line Slide Results: Pass: Fail:
AdequateTumorCellsPresent(≥100cells): Yes: No:
PD-L1 IHC 22C3 pharmDx Result to Treating Physician
Combined Positive Score: ____________________________________________________________________________________________________
CPS≥10: CPS < 10:
Other Comments to Treating Physician:
_______________________________________________________________________________________________________________________________
_______________________________________________________________________________________________________________________________
_______________________________________________________________________________________________________________________________
33
Page 34
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Combined Positive Score Summary and Examples
Key Considerations in Scoring
PD-L1 IHC 22C3 pharmDx
Stained Specimens
By definition, PD-L1 staining cells in urothelial carcinoma are:
– Tumor cells with convincing partial or complete linear membrane staining
(at any intensity) that is perceived distinct from cytoplasmic staining
– Lymphocytes and macrophages (mononuclear inflammatory cells, MICs)
within the tumor nests and/or immediately adjacent supporting stroma
with convincing membrane and/or cytoplasmic staining (at any intensity).
Mononuclear inflammatory cells (MICs) must be directly associated with the
response against the tumor
PD-L1 expression status in urothelial carcinoma is determined by Combined
Positive Score (CPS), which is the number of PD-L1 staining cells (tumor cells,
lymphocytes, macrophages) divided by the total number of viable tumor cells,
multiplied by 100.
# PD-L1 staining cells (tumor cells,
CPS =
This section will define and illustrate all scoring inclusions and exclusions for
accurate determination of Combined Positive Score. All images are urothelial
carcinoma unless otherwise noted in the figure caption.
lymphocytes, macrophages)
× 100
Total # viable tumor cells
34
Page 35
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Image Guide for Interpretation
of PD-L1 IHC 22C3
pharmDx Staining in
Urothelial Carcinoma
PD-L1 Staining Cells Included in the CPS Numerator
Tumor cells, lymphocytes, and macrophages exhibiting appropriate PD-L1
expression are defined as PD-L1 staining cells. All PD-L1 staining cells are
included in the CPS numerator for determination of the Combined Positive
Score (see Table 1 on page 26 for additional CPS numerator inclusion/exclusion
criteria). Below are common staining characteristics of PD-L1 staining cells that
must be included in the CPS numerator. All images are urothelial carcinoma
unless otherwise noted in the figure caption.
Linear Membrane Staining: Tumor Cells
Tumor cells exhibiting convincing partial and/or complete linear membrane staining
are considered PD-L1 staining cells. Linear membrane staining can be present at
any intensity and must be convincing at no higher than 20× magnification.
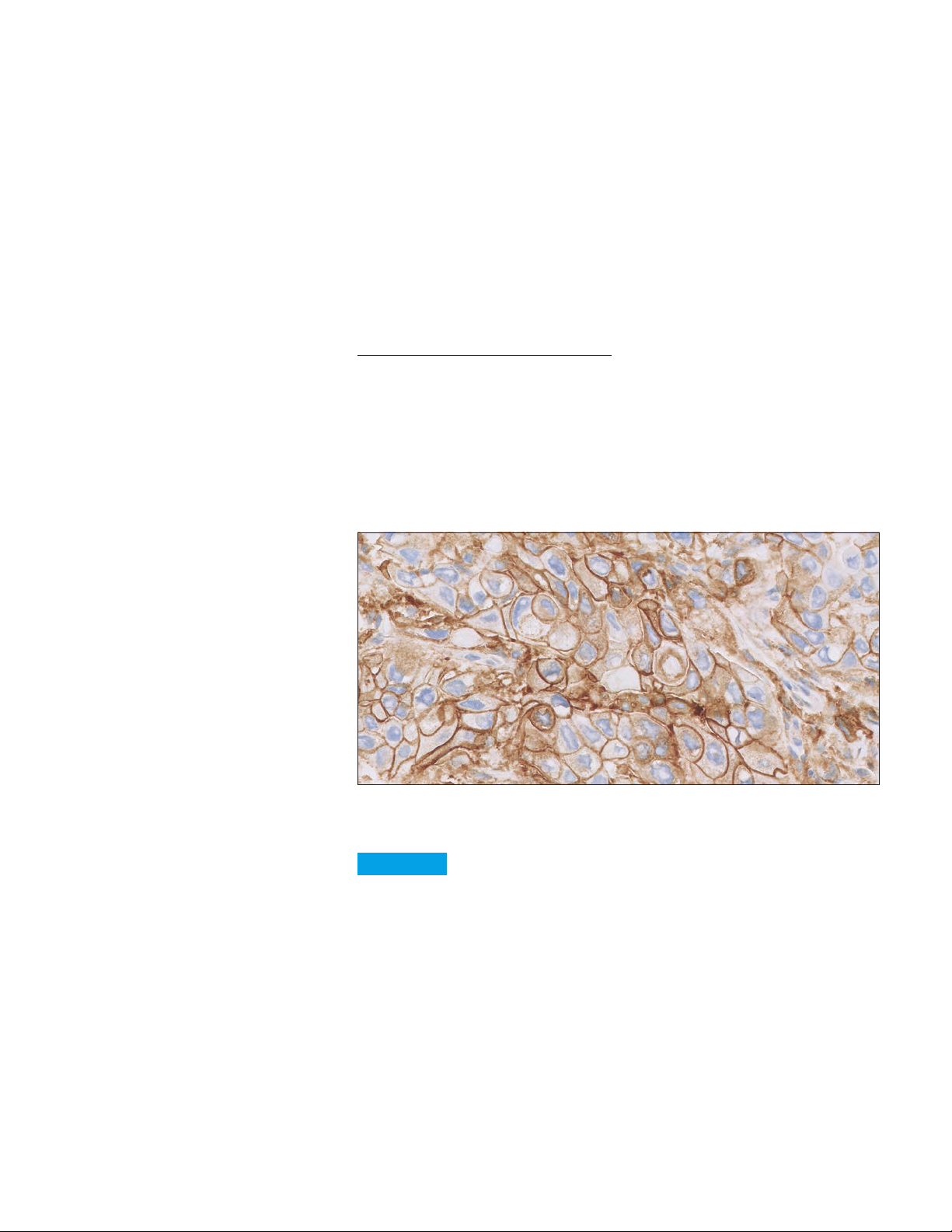
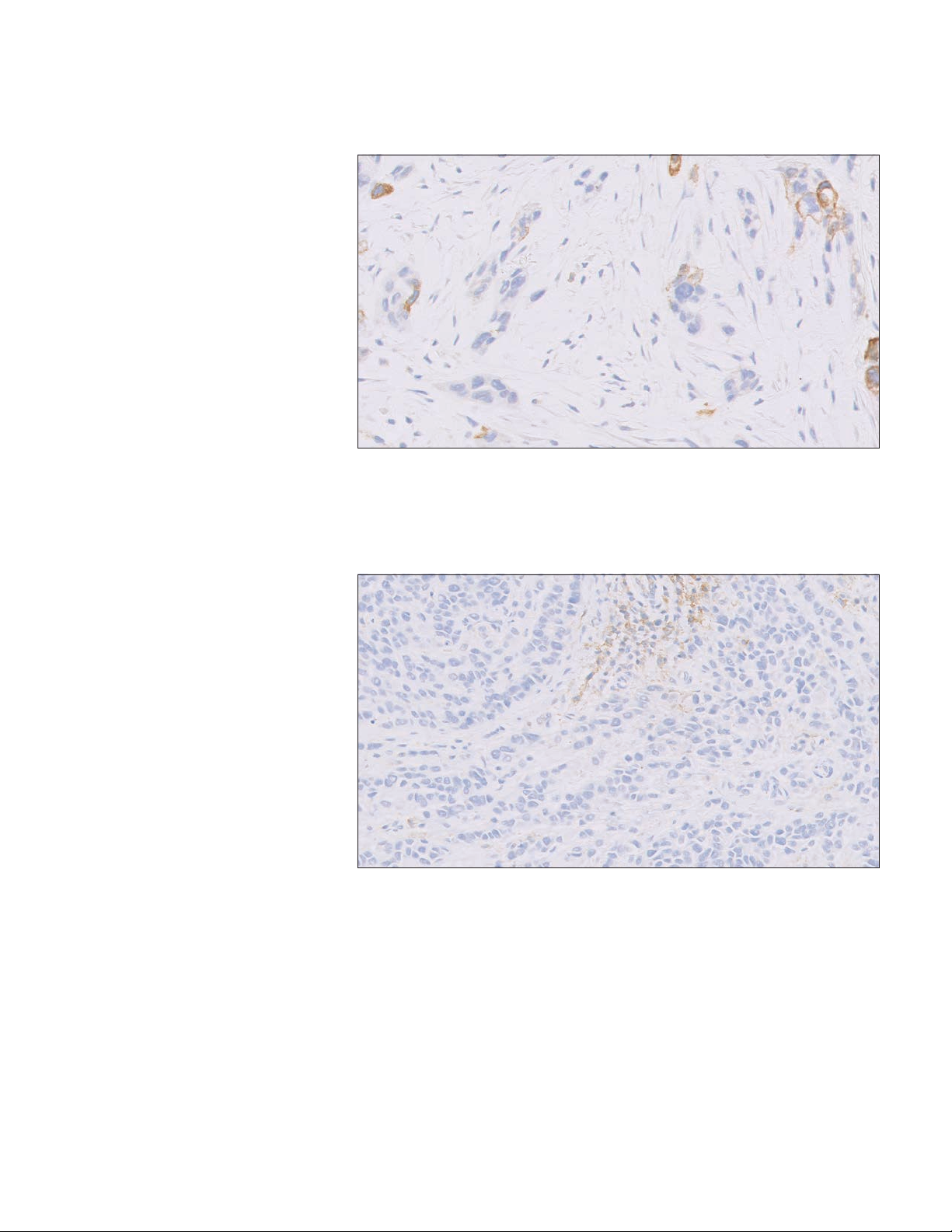
Figure 18: PD-L1 primary antibody exhibiting linear membrane staining of tumor cells
(20× magnification).
Key point
Convincing linear membrane staining of tumor cells should be
included in the CPS numerator
35
Page 36

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Partial and Complete Linear Membrane Staining: Tumor Cells
Tumor cells commonly exhibit partial and/or complete linear membrane staining.
Any partial or complete linear membrane staining observed at any intensity and
convincing at no higher than 20× magnification must be included in the
CPS numerator.
Figure 19: PD-L1 primary antibody exhibiting par tial (A) and complete (B) linear membrane
staining of tumor cells (20× magnification).
A
B
Key point
Convincing partial and/or complete membrane staining of tumor
cells should be included in the CPS numerator
Weak Linear Membrane Staining: Tumor Cells
Tumor cells must exhibit convincing membrane staining at any intensity,
including weak 1+ intensity, at no higher than 20× magnification.
Figure 20: PD-L1 primar y antibody exhibiting weak but perceptible and convincing membrane
staining of tumor cells (arrows) (20× magnification).
Key point
Weak 1+ convincing membrane staining of tumor cells should be
included in the CPS numerator
36
Page 37

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Linear Membrane and Cytoplasmic Staining: Tumor Cells
Tumorcellswithbothconvincinglinearmembranestaining(≥1+intensity)and
cytoplasmic staining at no higher than 20× magnification should be included in
the CPS numerator.
A
B
Figure 21: PD-L1 primary antibody exhibiting linear membrane (A) staining distinct from
cytoplasmic (B) staining (20× magnification).
Key point
Tumor cells exhibiting convincing linear membrane staining that is
distinct from cytoplasmic staining is included in the CPS numerator
37
Page 38

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Membrane and Cytoplasmic Staining:
Tumor-associated Lymphocytes and Macrophages
Tumor-associated lymphocytes and macrophages (mononuclear inflammatory
cells, MICs) exhibiting convincing membrane and/or cytoplasmic staining at no
higherthan20×magnification(≥1+intensity)areconsideredPD-L1stainingcells
and should be included in the CPS numerator. Tumor-associated mononuclear
inflammatory cells (MICs) are present within the tumor nests and/or immediately
adjacent supporting stroma, and are directly associated with the response
against the tumor.
Note: PD-L1 staining lymphocytes often have indistinguishable membrane and
cytoplasmic staining due to a high nuclear to cytoplasmic ratio; PD-L1 staining
macrophages often have distinct membrane staining and low cytoplasmic staining.
All PD-L1 staining tumor-associated mononuclear inflammatory cells (MICs)
should be included in the CPS numerator.
B
A
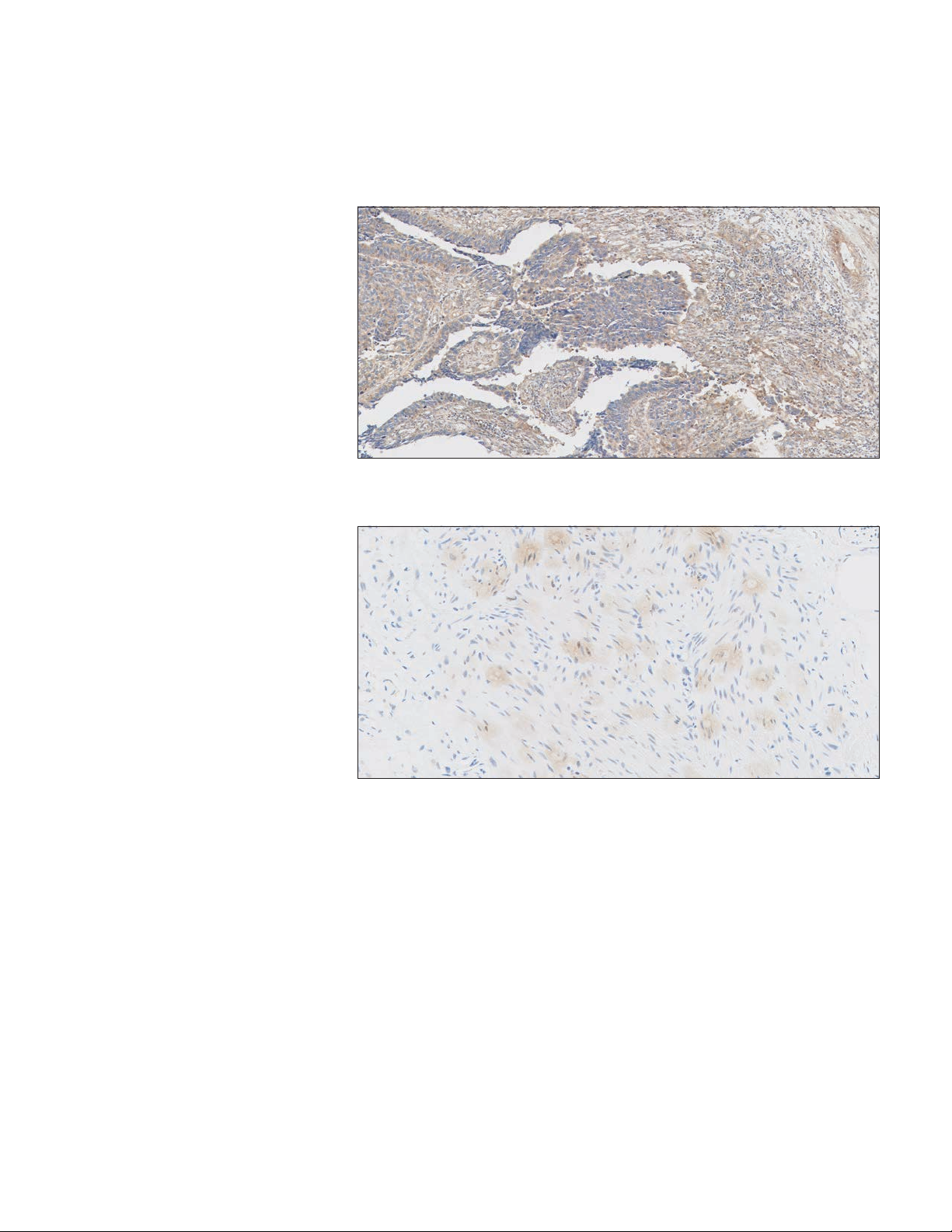
Figure 22a: PD-L1 primary antibody exhibiting staining of tumor (A) and tumor-associated
mononuclear inflammatory cells (MICs) (B) (20× magnification).
38
Page 39
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
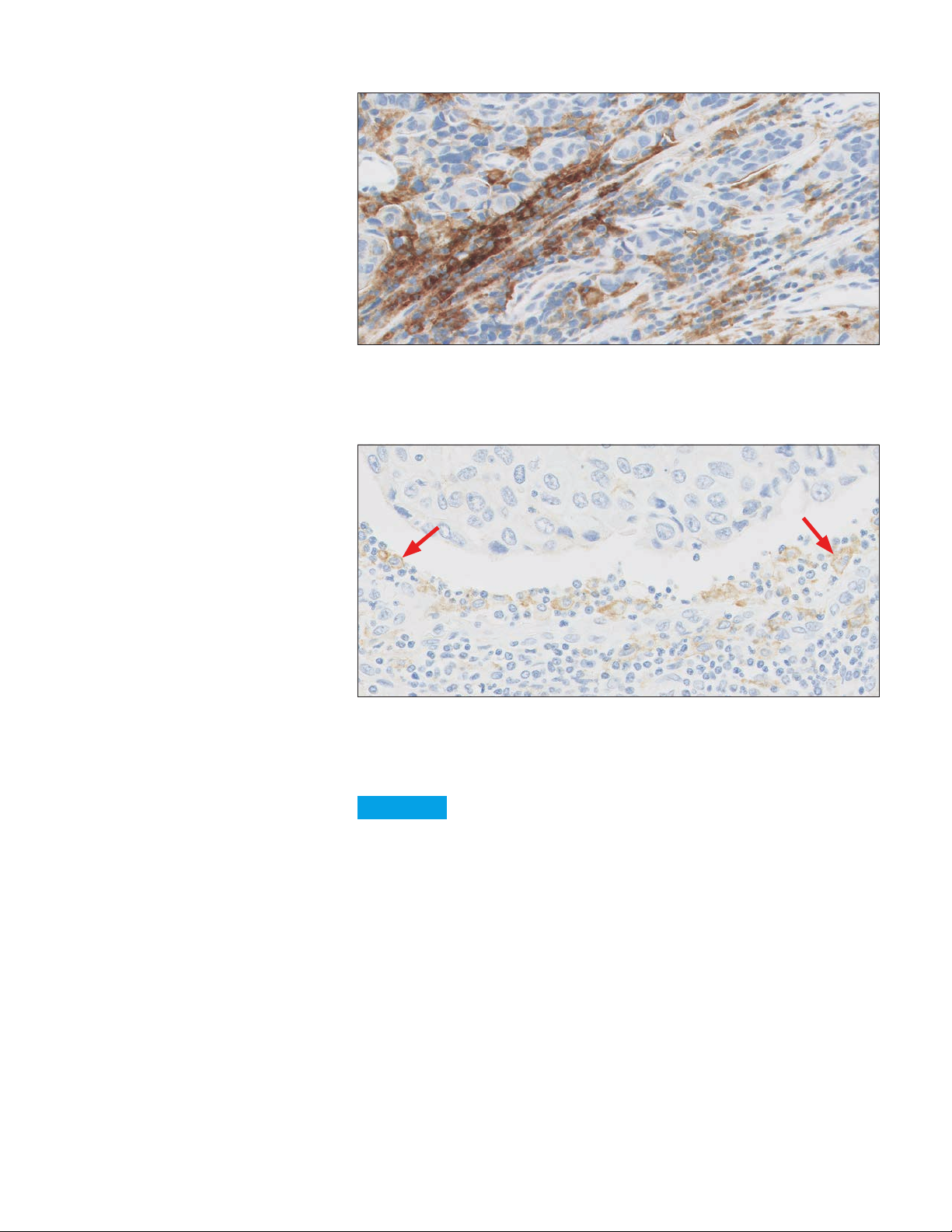
Figure 22b: PD-L1 primary antibody exhibiting staining of tumor-associated lymphocytes
(20× magnification). Note: Tumor-associated lymphocytes are present within the tumor
nests and/or immediately adjacent supporting stroma, and are directly associated with
the response against the tumor.
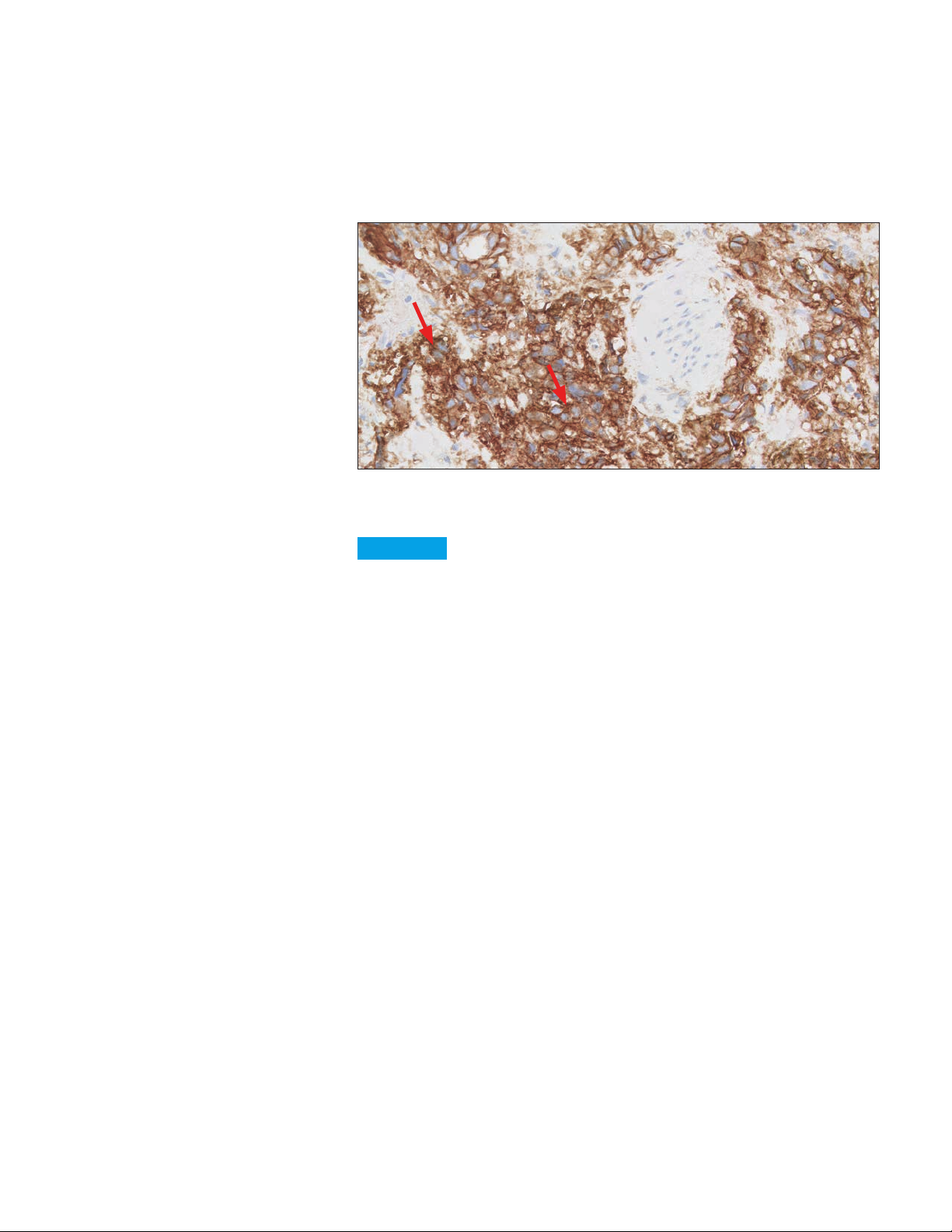
Figure 22c: PD-L1 primary antibody exhibiting moderate staining of tumor-associated
macrophages (arrows) (20× magnification). Note: Tumor-associated macrophages are
present within the tumor nests and/or immediately adjacent supporting stroma, and are
directly associated with the response against the tumor.
Key point
Tumor-associated lymphocytes and macrophages with convincing
membrane and/or cytoplasmic staining should be included in the
CPS numerator
39
Page 40
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Weak Staining: Tumor-associated Mononuclear Inflammatory Cells (MICs)
Tumor-associated lymphocytes and macrophages (mononuclear inflammatory
cells, MICs) exhibiting weak membrane and/or cytoplasmic staining at no higher
than20×magnification(≥1+intensity)areconsideredPD-L1stainingcellsand
should be included in the CPS numerator.
Note: Tumor-associated mononuclear inflammatory cells (MICs) are present within
the tumor nests and/or immediately adjacent supporting stroma, and are directly
associated with the response against the tumor.
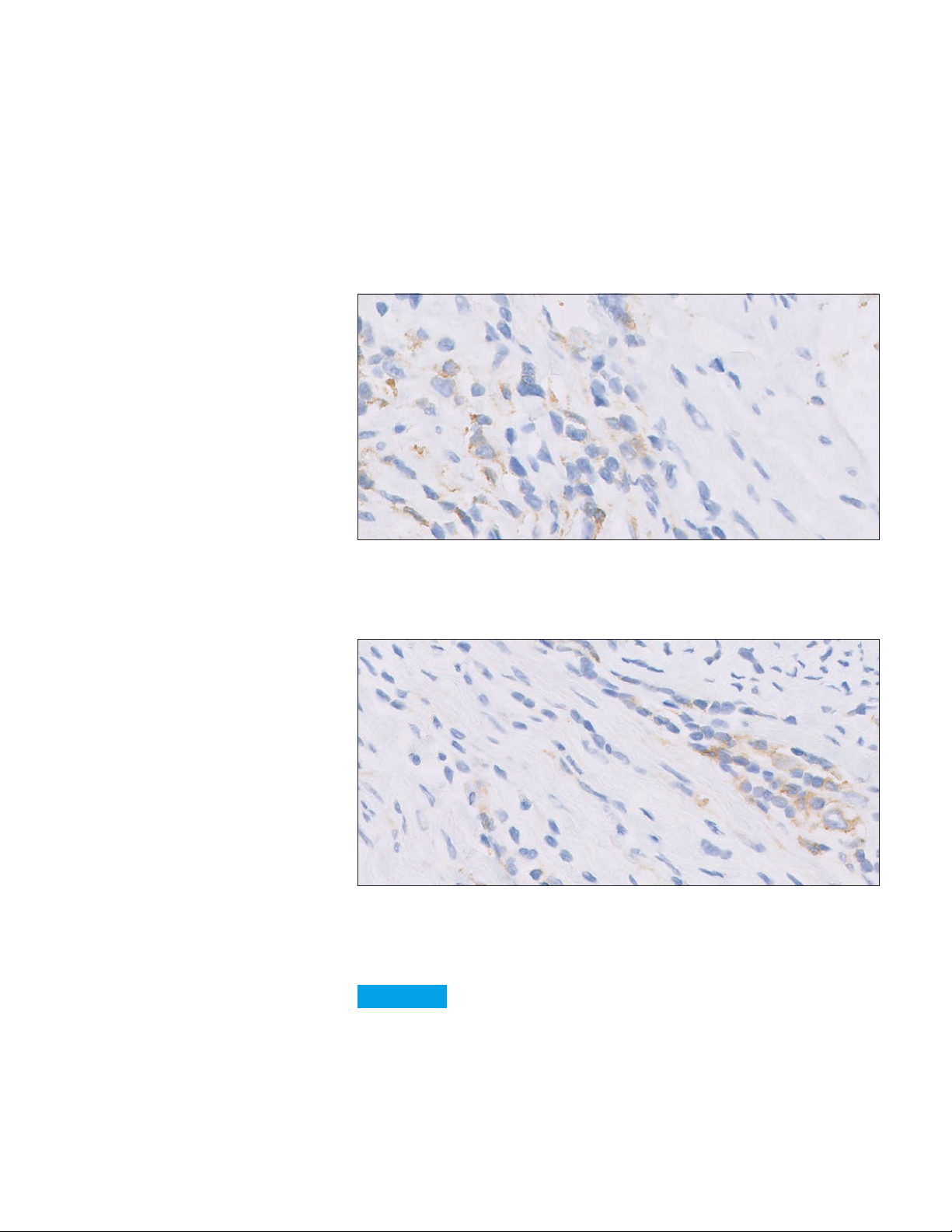
Figure 23a: PD-L1 primary antibody exhibiting weak staining of tumor-associated
mononuclear inflammatory cells (MICs) (20× magnification). Note: Tumor-associated
mononuclear inflammatory cells (MICs) are present within the tumor nests and/or immediately
adjacent supporting stroma, and are directly associated with the response against the tumor.
Figure 23b: PD-L1 primary antibody exhibiting weak staining of tumor-associated
mononuclear inflammatory cells (MICs) (20× magnification). Note: Tumor-associated
mononuclear inflammatory cells (MICs) are present within the tumor nests and/or immediately
adjacent supporting stroma, and are directly associated with the response against the tumor.
Key point
Tumor-associated lymphocytes and macrophages with weak
membrane and/or cytoplasmic staining should be included in the
CPS numerator
40
Page 41
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
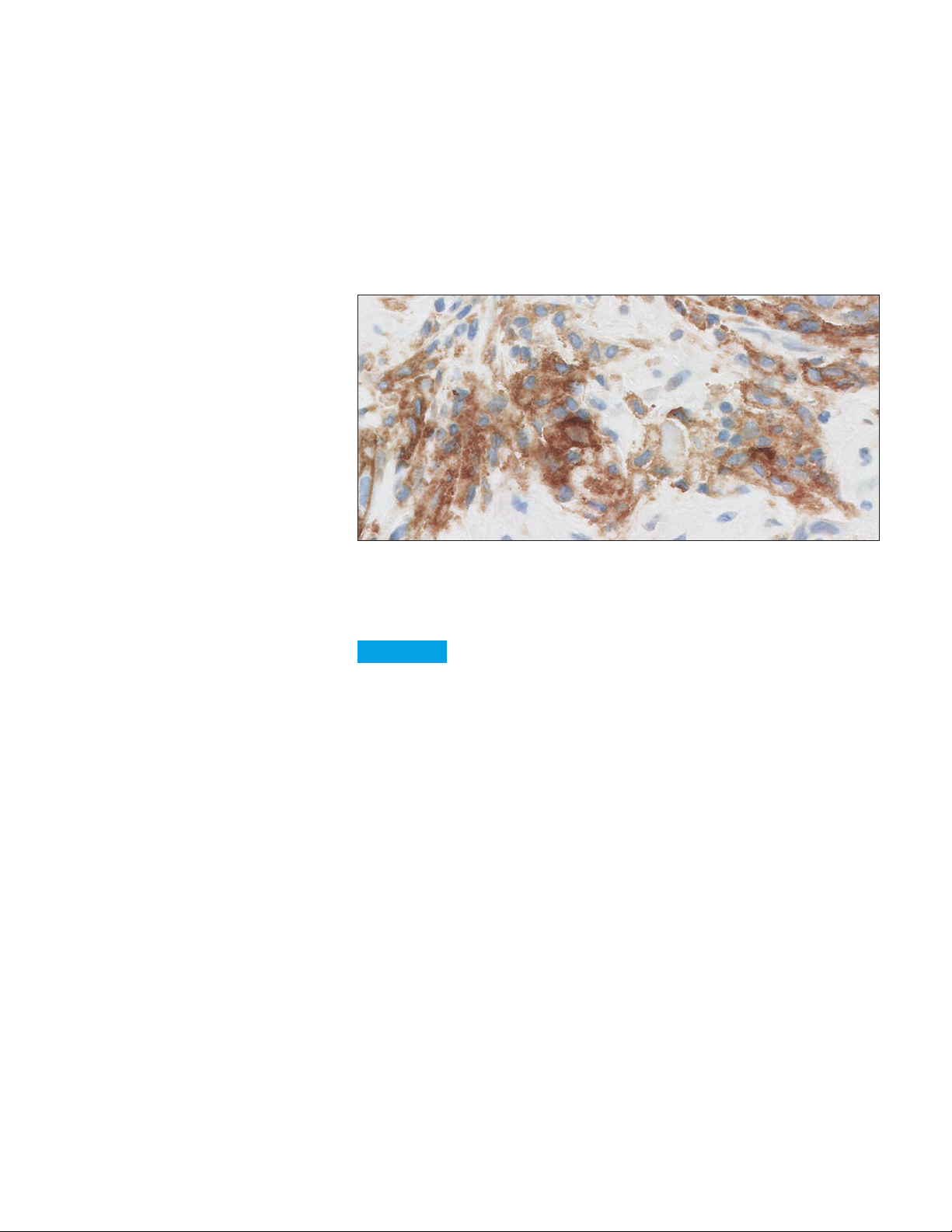
Strong Staining: Tumor-associated Lymphocytes and Macrophages
Tumor-associated lymphocytes and macrophages (mononuclear inflammatory
cells, MICs) exhibiting strong membrane and/or cytoplasmic staining at no
higherthan20×magnification(≥1+intensity)areconsideredPD-L1stainingcells
and should be included in the CPS numerator.
Note: Tumor-associated mononuclear inflammatory cells (MICs) are present
within the tumor cells and/or immediately adjacent supporting stroma, and are
directly associated with the response against the tumor.
Figure 24: PD-L1 primary antibody exhibiting strong staining of tumor-associated
mononuclear inflammatory cells (MICs) (20× magnification). Note: Tumor-associated
mononuclear inflammatory cells (MICs) are present within the tumor nests and/or immediately
adjacent supporting stroma, and are directly associated with the response against the tumor.
Key point
Tumor-associated lymphocytes and macrophages with strong
membrane and/or cytoplasmic staining should be included in the
CPS numerator
41
Page 42

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Heterogeneous Staining Intensities
Convincing staining of tumor cells (linear membrane) and tumor-associated
lymphocytes and macrophages (membrane and/or cytoplasmic) is often
heterogeneous, with various staining intensities present. At no higher than
20× magnification, any convincing staining of tumor cells and tumor-associated
lymphocytes and macrophages at any intensity should be included in the
CPS numerator.
B
A
C
Figure 25a: PD-L1 primary antibody exhibiting heterogeneous staining intensities of mononuclear
inflammatory cells (MICs) (A: 1+ intensity, B: 2+ intensity, C: 3+ intensity) (20× magnification).
Note: Tumor-associated mononuclear inflammatory cells (MICs) are present within the tumor
nests and/or immediately adjacent supporting stroma, and are directly associated with the
response against the tumor.
A
B
C
Figure 25b: PD- L1 primary antibody exhibiting heterogeneous staining intensities of tumor cells
(A: 1+ intensity, B: 2+ intensity, C: 3+ intensity) (20× magnification).
Key point
Convincing staining of tumor cells and tumor-associated
lymphocytes and macrophages at all intensities should be
included in the CPS numerator
42
Page 43
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Granular Staining
Tumor cells can exhibit a granular membrane staining pattern where membrane
and cytoplasmic staining are indistinguishable. Only convincing membrane staining
oftumorcells(≥1+intensity)observedatnohigherthan20×magnificationshould
be included in the CPS numerator.
Figure 26: PD- L1 primary antibody exhibiting granular membrane staining pattern (arrows)
(20× magnification).
Key point
Granular staining of tumor cells must exhibit a convincing linear
membrane pattern to be included in the CPS numerator
43
Page 44

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Indistinguishable Tumor and Immune Cells
Tumor cells and tumor-associated lymphocytes and macrophages may
be indistinguishable from each other when examining the slide with PD-L1
antibody staining due to small tumor cell size and staining characteristics. It is
recommended to use the corresponding H&E slide to distinguish cell morphology.
This is especially important when determining the denominator.
Figure 27a: Tumor and tumor-associated mononuclear inflammatory cells (MICs) are
indistinguishable from each other and exhibit PD-L1 primary antibody staining (20× magnification).
Figure 27b: Corresponding H&E to reference when tumor and tumor-associated mononuclear
inflammatory cells (MICs) are indistinguishable from each other (20× magnification).
Key point
Use the H&E slide to determine cell morphology when tumor
cells and tumor-associated lymphocytes and macrophages
are indistinguishable from each other in the PD-L1 slide
44
Page 45

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Morphological Patterns Included in CPS
Lamina Propria Invasion
In addition to muscle invasion, lamina propria invasion is also commonly
demonstrated in urothelial carcinoma. Any tumor cells and/or PD-L1 staining
tumor-associated mononuclear inflammatory cells (MICs) in the lamina propria
should be included in the CPS calculation.
Figure 28: PD-L1 primary antibody exhibiting staining of tumor-associated mononuclear
inflammatory cells (MICs) in lamina propria invasion (10× magnification).
Key point
All invasive tumor cells and staining tumor-associated mononuclear
inflammatory cells (MICs) in the lamina propria should be included in
the CPS calculation
45
Page 46

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
What to Exclude from CPS
Only tumor cells exhibiting PD-L1 membrane staining and mononuclear
inflammatory cells (MICs) exhibiting PD-L1 membrane and/or cytoplasmic
staining should be included in the CPS numerator. Below are other cells that can
exhibit PD-L1 expression but should be excluded from the CPS calculation (CPS
numerator or denominator).
Tumor Cells With Only Cytoplasmic Staining
Tumor cells exhibiting only cytoplasmic staining and/or membrane staining
that is only convincing at 40× magnification should not be included in the CPS
numerator, as this is considered non-specific staining. They should, however, still
be included in the CPS denominator.
Figure 29: PD-L1 primary antibody exhibiting staining of tumor cytoplasm only (arrows)
(20× magnification).
Key point
Tumor cells exhibiting only cytoplasmic staining should not be
included in the CPS numerator
46
Page 47

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Non-tumor-associated Mononuclear Inflammatory Cells (MICs)
Mononuclear inflammatory cells (MICs, lymphocytes and macrophages)
commonly exhibit PD-L1 staining in urothelial carcinoma specimens. Only
PD-L1 staining mononuclear inflammatory cells (MICs) that are tumor-associated
(present within tumor nests and/or immediately adjacent supportive stroma;
directly associated with the response against the tumor) should be included in
the CPS calculation.
PD-L1 staining mononuclear inflammatory cells (MICs) that are not
tumor-associated must be excluded from the CPS calculation. Examples of
non-tumor-associated mononuclear inflammatory cells (MICs) include those
associated with papilloma, ulceration, normal cells, and other processes not
associated with the tumor.
Figure 30a: PD-L1 primar y antibody exhibiting staining of non-tumor associated mononuclear
inflammatory cells (MICs) (20× magnification). This cluster of partially staining lymphocytes
does not appear to be associated with any tumor and therefore should be excluded from the
CPS calculation.
Figure 30b: PD-L1 primar y antibody exhibiting staining of cells associated with BCG-induced
granulomas (20× magnification).
Key point
Non-tumor-associated mononuclear inflammatory cells (MICs)
should be excluded from the CPS calculation
47
Page 48

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Stromal Cells
Various tissue elements can exhibit PD-L1 staining, but only PD-L1 staining
tumor cells and tumor-associated lymphocytes and macrophages should be
included in the CPS numerator. Normal cells, stromal cells (including fibroblasts),
eosinophils, and plasma cells should be excluded from the CPS calculation.
Figure 31a: PD-L1 primary antibody exhibiting staining of stromal cells (arrows) (20× magnification).
Figure 31b: PD-L1 primary antibody exhibiting staining of a fibroblast (arrow) (20× magnification).
Key point
PD-L1 staining normal cells, stromal cells, eosinophils, and plasma
cells should be excluded from the CPS calculation
48
Page 49

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
CPS < 10 Case Examples
Case 1: CPS < 10
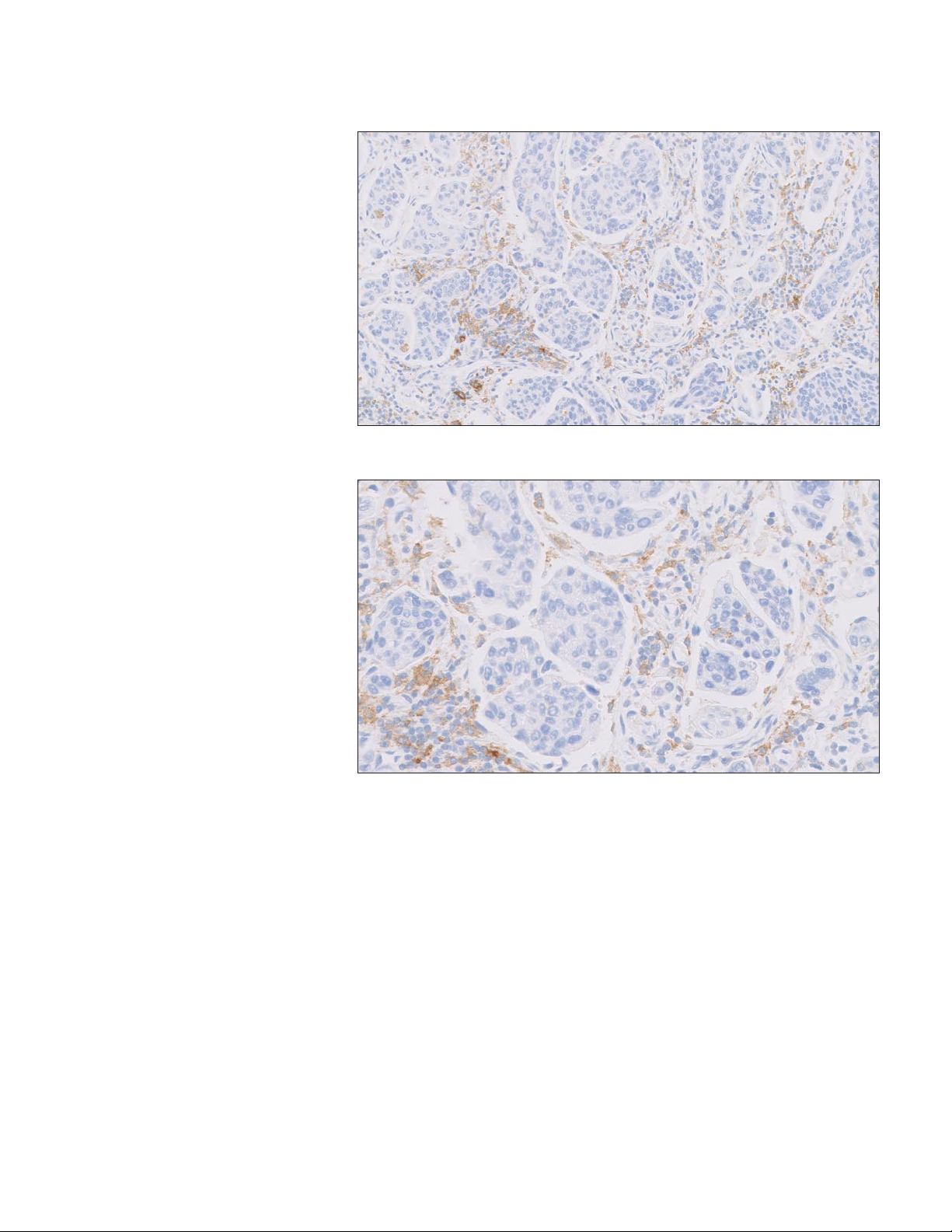
Figure 32a: 10× magnification.
Figure 32b: 20× magnification.
Figure 32a–32b: PD-L1 antibody exhibiting CPS < 10 at 20× magnification.
Note: Photomicrograph magnification levels may appear different than indicated
in respective annotations due to adjustment of image size.
49
Page 50
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
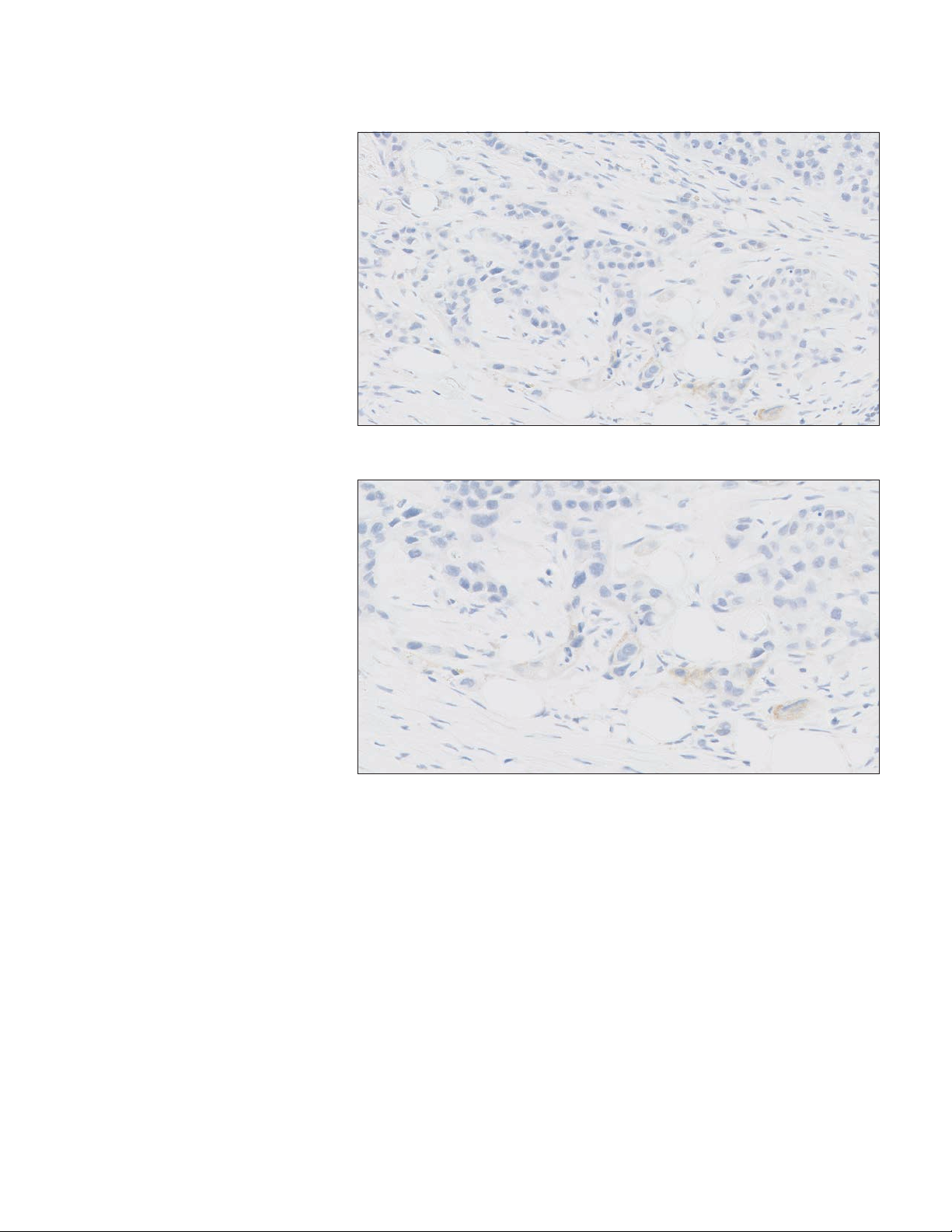
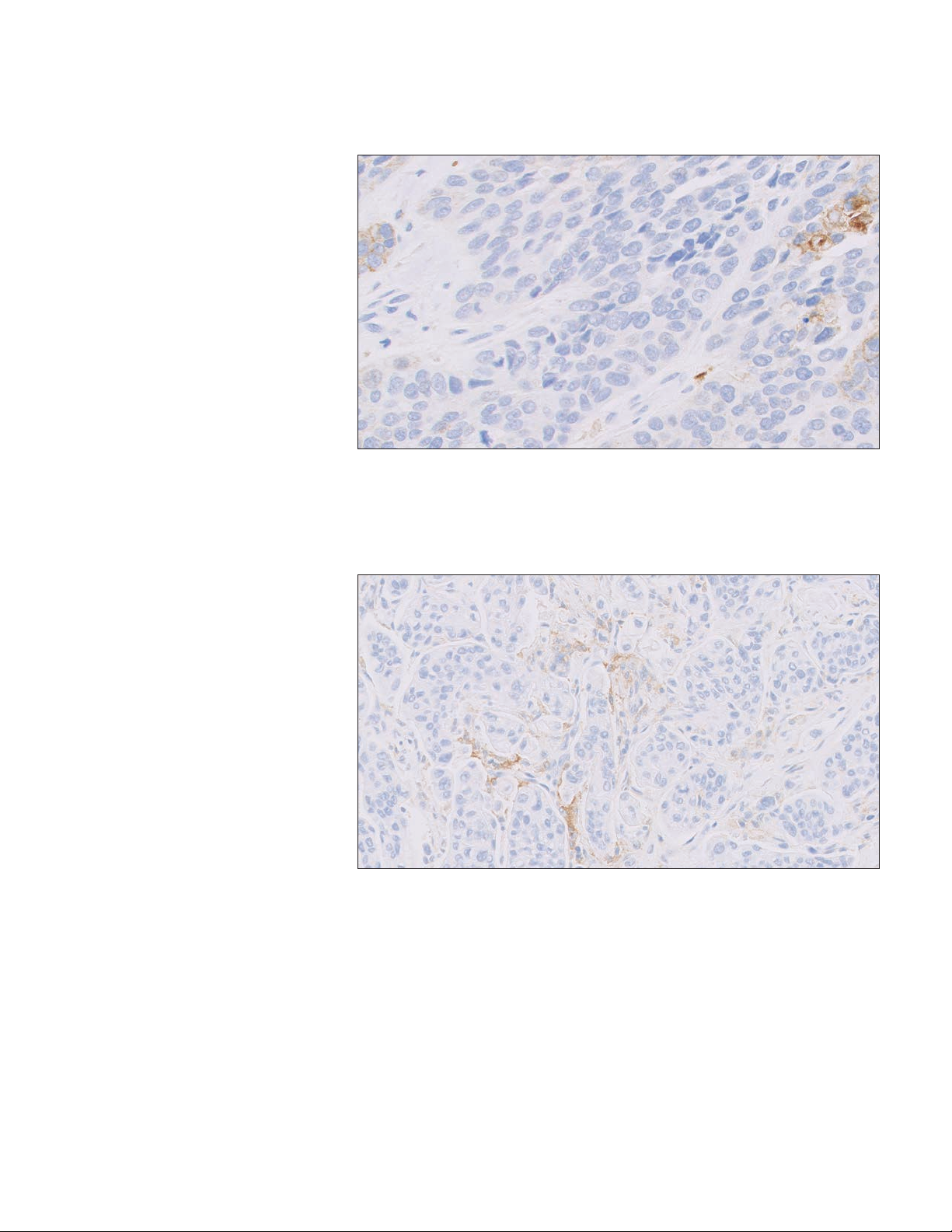
Case 2: CPS < 10
Figure 33a: 10× magnification.
Figure 33b: 20× magnification.
Figure 33a–33b: PD-L1 antibody exhibiting CPS < 10 at 20× magnification.
50
Page 51

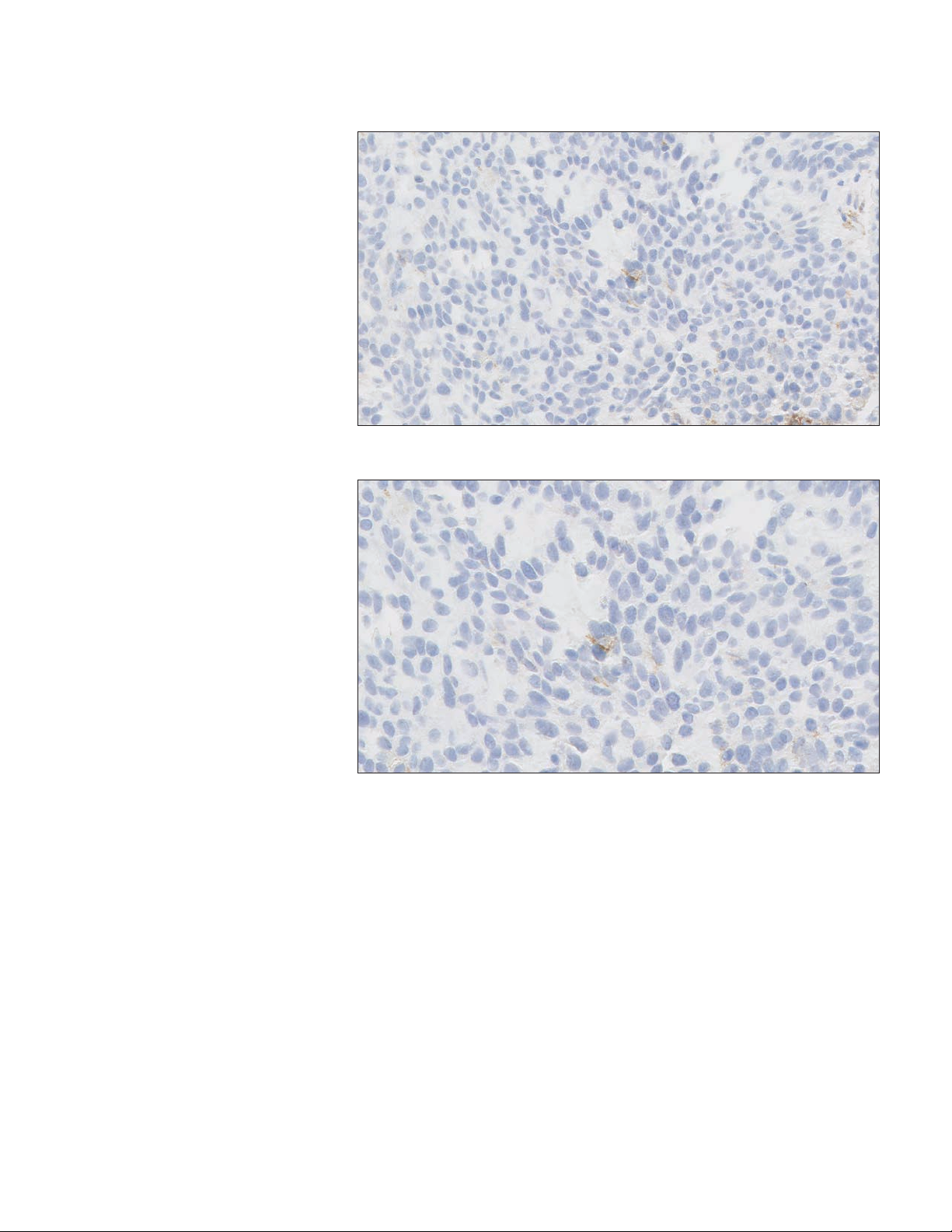
Case 3: CPS < 10
Figure 34a: 10× magnification.
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Figure 34b: 20× magnification.
Figure 34a–34b: PD-L1 antibody exhibiting CPS < 10 at 20× magnification.
51
Page 52
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Case 4: CPS < 10
Figure 35a: 10× magnification.
Figure 35b: 20× magnification.
Figure 35a–35b: PD-L1 antibody exhibiting CPS < 10 at 20× magnification.
52
Page 53

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
CPS ≥ 10 Case Examples
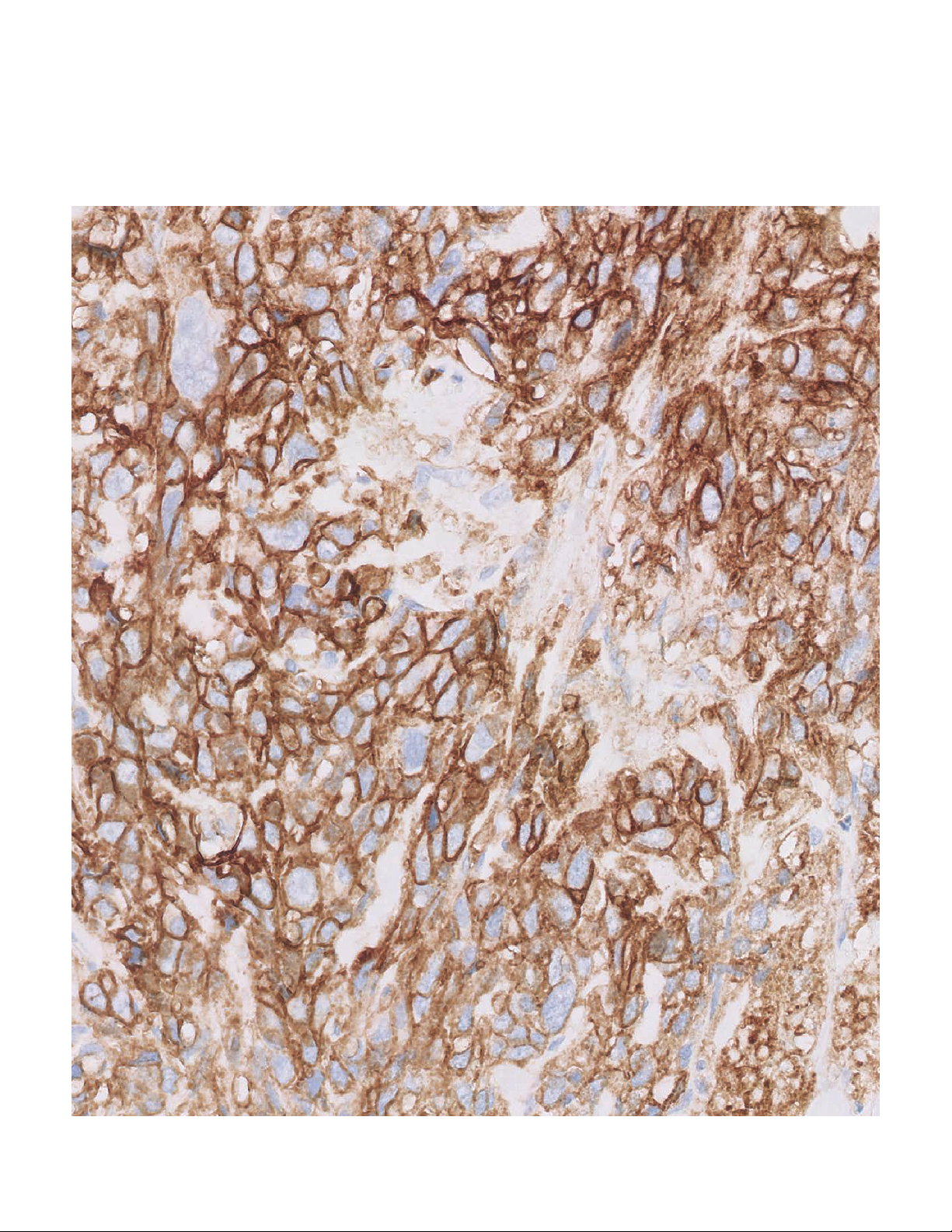
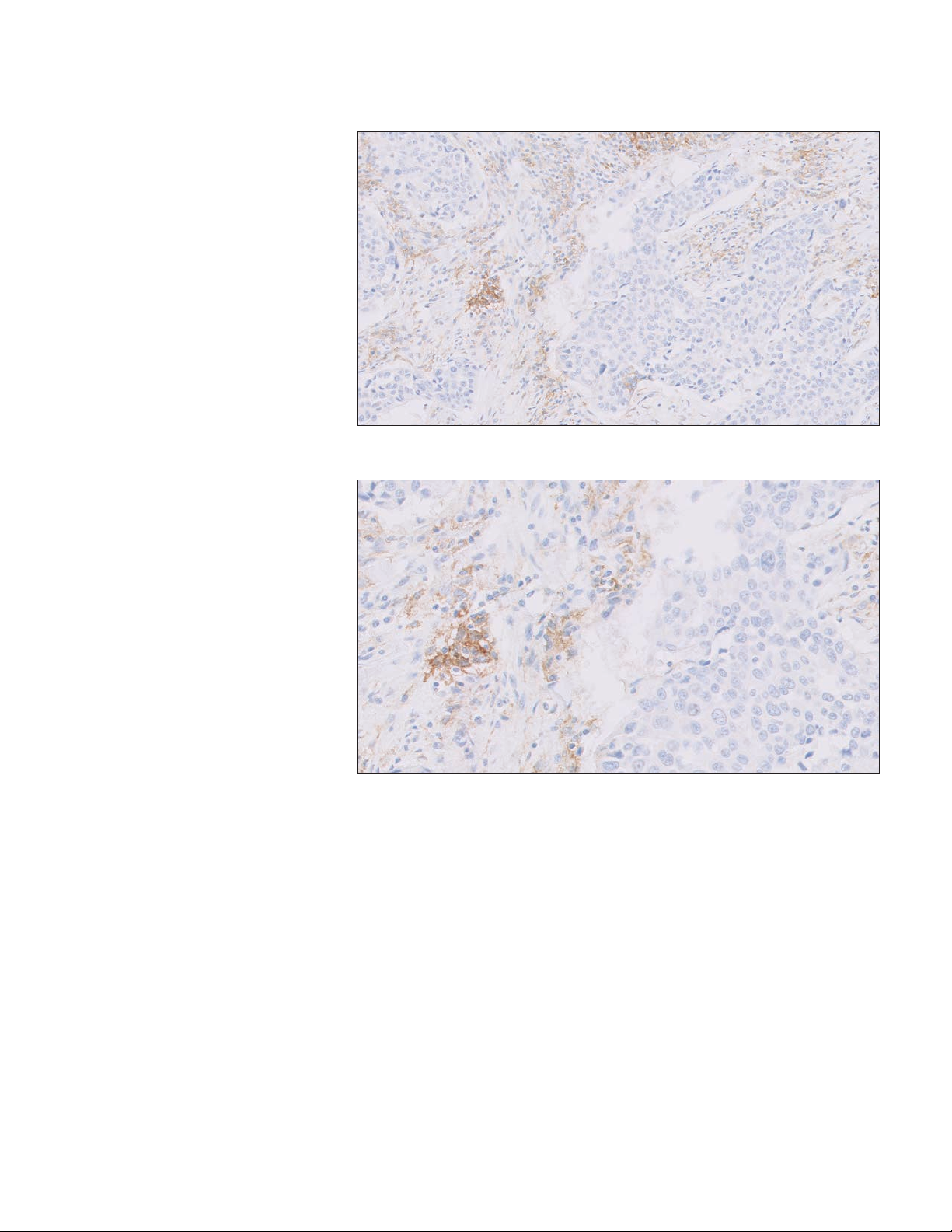
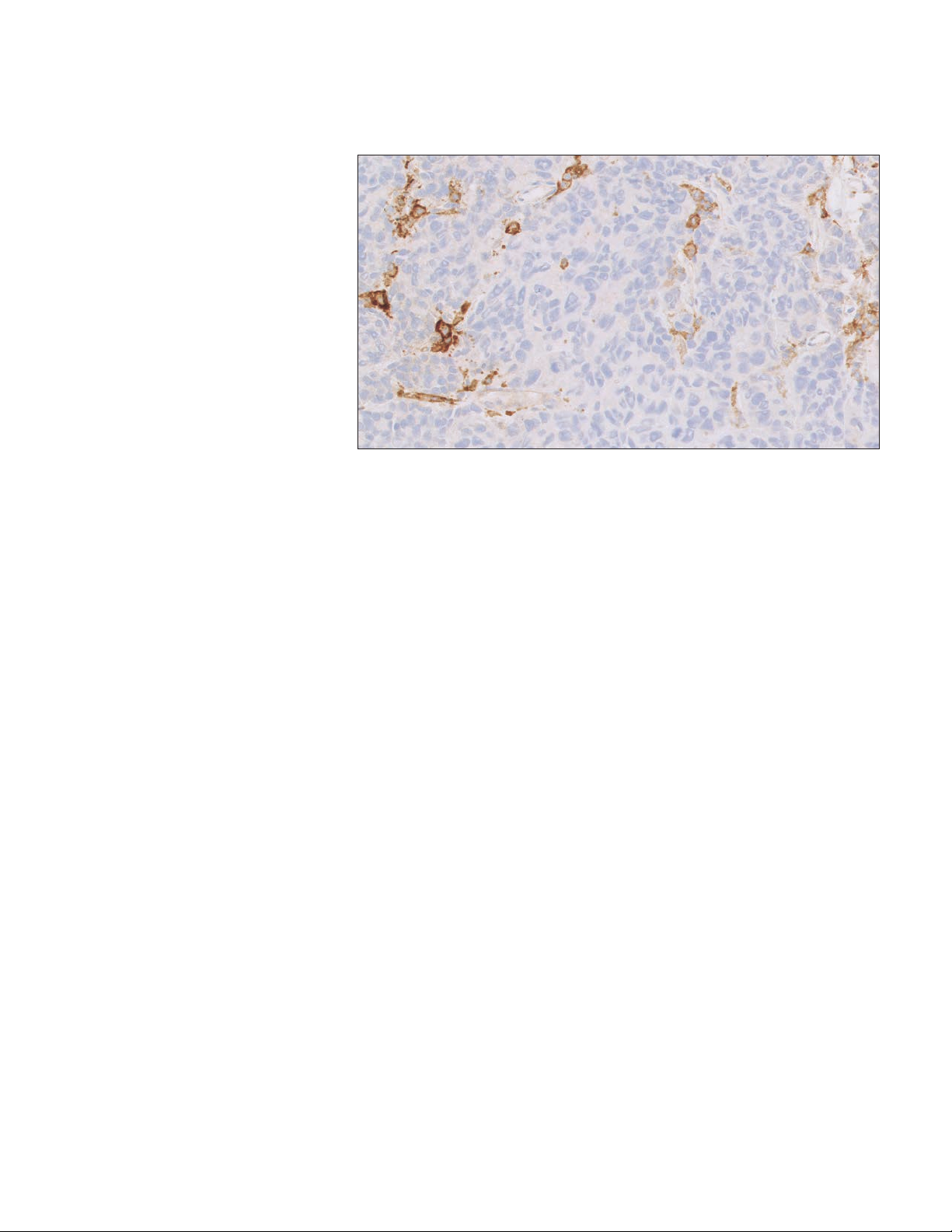
Case 5: CPS ≥ 10
Figure 36a: 10× magnification.
Figure 36b: 20× magnification.
Figure 36a–36b: PD-L1antibodyexhibitingCPS≥10at20×magnification.
53
Page 54

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
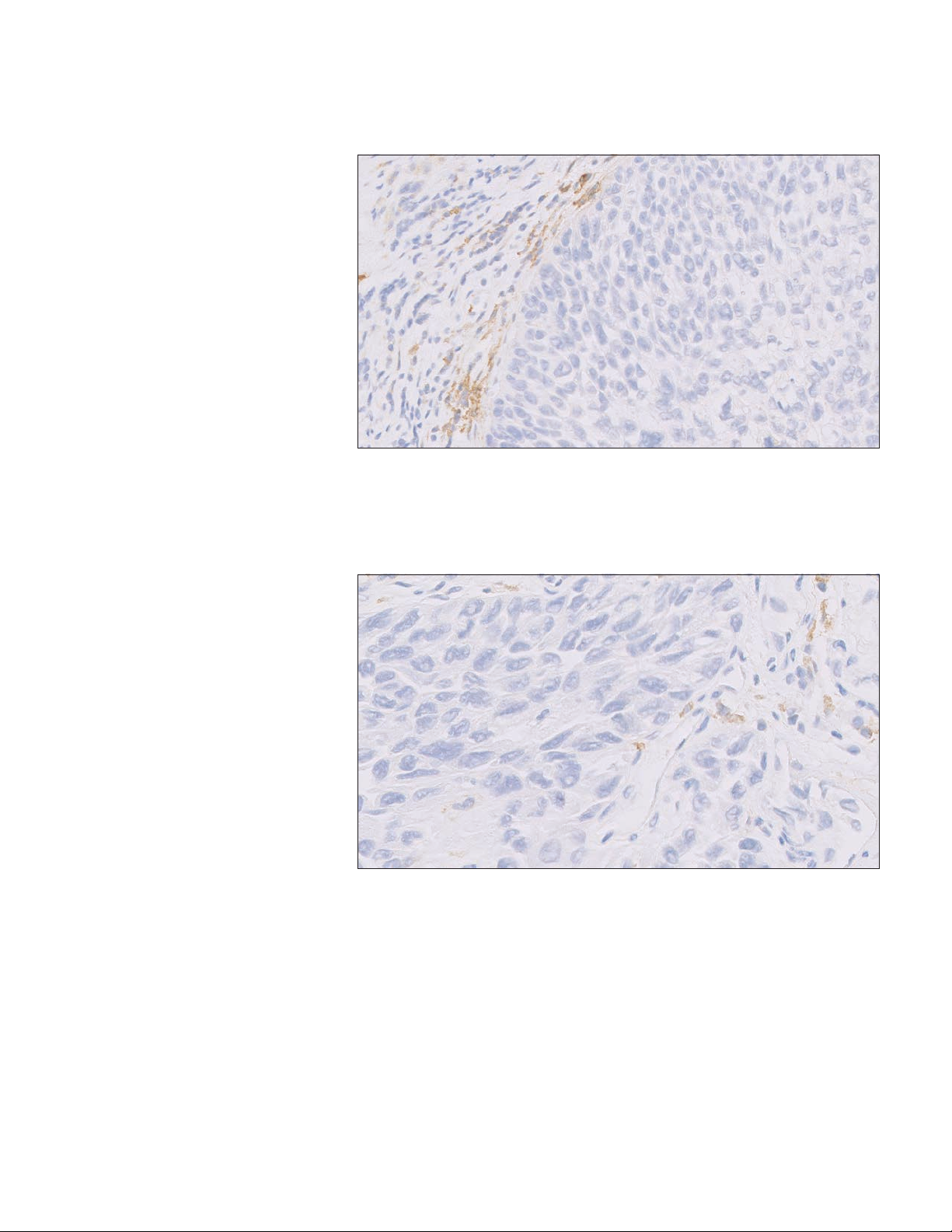
Case 6: CPS ≥ 10
Figure 37a: 10× magnification.
Figure 37b: 20× magnification.
Figure 37a–37b: PD-L1antibodyexhibitingCPS≥10at20×magnification.
54
Page 55
Case 7: CPS ≥ 10
Figure 38a: 10× magnification.
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Figure 38b: 20× magnification.
Figure 38a–38b: PD-L1antibodyexhibitingCPS≥10at20×magnification.
55
Page 56

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Case 8: CPS ≥ 10
Figure 39a: 10× magnification.
Figure 39b: 20× magnification.
Figure 39a–39b:PD-L1antibodyexhibitingCPS≥10at20×magnification.
56
Page 57

Case 9: CPS ≥ 10
Figure 40a: 10× magnification.
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Figure 40b: 20× magnification.
Figure 40a–40b:PD-L1antibodyexhibitingCPS≥10at20×magnification.
57
Page 58
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Case 10: CPS ≥ 10
Figure 41a: 10× magnification.
Figure 41b: 20× magnification.
Figure 41a–41b:PD-L1antibodyexhibitingCPS≥10at20×magnification.
58
Page 59
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Near Cut-off Case Examples
(CPS Range of Greater Than
1 but Less Than 10)
Challenging Case 1: Near Cut-off
(CPS Range of Greater Than 1 but Less Than 10)
Figure 42: PD-L1 antibody exhibiting CPS 8 at 20× magnification.
Challenging Case 2: Near Cut-off
(CPS Range of Greater Than 1 but Less Than 10)
Figure 43: PD-L1 antibody exhibiting CPS 8 at 20× magnification.
59
Page 60

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Challenging Case 3: Near Cut-off
(CPS Range of Greater Than 1 but Less Than 10)
Figure 44: PD-L1 antibody exhibiting CPS 5 at 20× magnification.
Challenging Case 4: Near Cut-off
(CPS Range of Greater Than 1 but Less Than 10)
Figure 45: PD-L1 antibody exhibiting CPS 7 at 20× magnification.
60
Page 61

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Challenging Case 5: Near Cut-off
(CPS Range of Greater Than 1 but Less Than 10)
Figure 46: PD-L1 antibody exhibiting CPS 7 at 20× magnification.
Challenging Case 6: Near Cut-off
(CPS Range of Greater Than 1 but Less Than 10)
Figure 47: PD-L1 antibody exhibiting CPS 7 at 20× magnification.
61
Page 62
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Challenging Case 7: Near Cut-off
(CPS Range of Greater Than 1 but Less Than 10)
Figure 48: PD-L1 antibody exhibiting CPS 6 at 20× magnification.
62
Page 63
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Near Cut-off Case Examples
(CPS Range of Greater Than
or Equal to 10 but Less Than
or Equal to 20)
Challenging Case 8: Near Cut-off (CPS Range of Greater Than or
Equal to 10 but Less Than or Equal to 20)
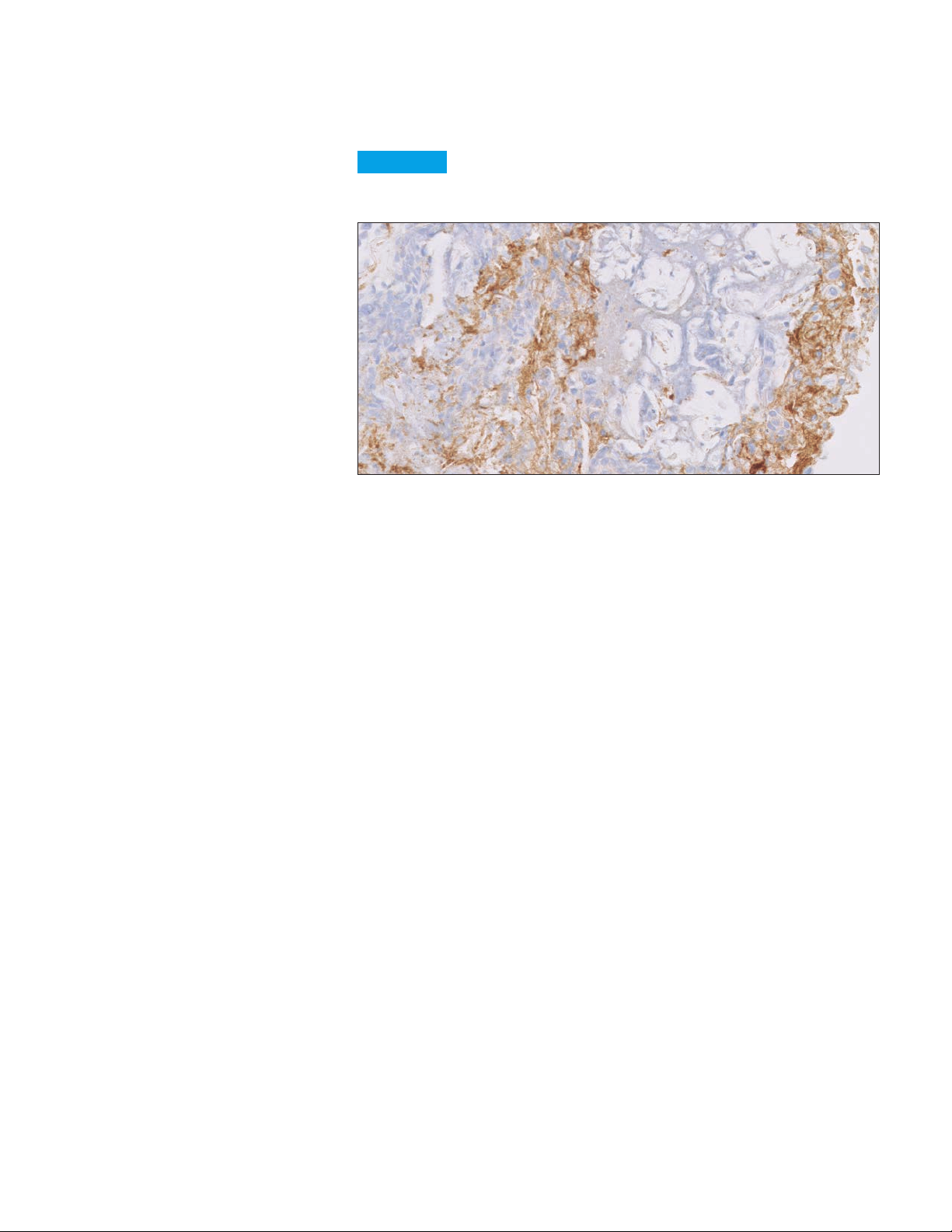
Figure 49: PD- L1 antibody exhibiting CPS 10 at 20× magnification.
Challenging Case 9: Near Cut-off (CPS Range of Greater Than or
Equal to 10 but Less Than or Equal to 20)
Figure 50: PD-L1 antibody exhibiting CPS 10 at 20× magnification.
63
Page 64
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Challenging Case 10: Near Cut-off (CPS Range of Greater Than or
Equal to 10 but Less Than or Equal to 20)
Figure 51: PD-L1 antibody exhibiting CPS 13 at 20× magnification.
Challenging Case 11: Near Cut-off (CPS Range of Greater Than or
Equal to 10 but Less Than or Equal to 20)
Figure 52: PD-L1 antibody exhibiting CPS 10 at 20× magnification.
64
Page 65

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Challenging Case 12: Near Cut-off (CPS Range of Greater Than or
Equal to 10 but Less Than or Equal to 20)
Figure 53: PD-L1 antibody exhibiting CPS 15 at 20× magnification.
Challenging Case 13: Near Cut-off (CPS Range of Greater Than or
Equal to 10 but Less Than or Equal to 20)
Figure 54: PD-L1 antibody exhibiting CPS 20 at 20× magnification.
65
Page 66

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Artifacts
The following pages provide examples of artifacts you may see when staining with
PD-L1 IHC 22C3 pharmDx.
Non-specific
Background Staining
Background staining is defined as diffuse, non-specific staining of a specimen.
It is caused by several factors. These factors include, but are not limited to,
pre-analytic fixation and processing of the specimen, incomplete removal of
paraffin from sections, and incomplete rinsing of slides during staining.
The use of fixatives other than neutral buffered formalin may be a source of
background staining. Background staining with PD-L1 IHC 22C3 pharmDx is rare.
Possible Causes of Background
– Improper drying of slides; ensure slides remain wet with buffer while loading
onto Autostainer Link 48 and prior to initiating run
– Improper deparaffinization procedure
– Incomplete rinsing of reagents from slides
The non-specific background staining of the NCR-stained test specimen is useful
in determining the level of background staining in the positive test specimen. All
specimensmusthave≤1+non-specificbackgroundstaining.
Key point
All specimens must have ≤ 1+ non-specific background staining
Figure 55a: Negative Control Reagent (NCR) exhibiting unacceptable non-specific background
staining (5× magnification).
66
Page 67
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Figure 55b: PD-L1 primary antibody exhibiting blush staining; blush should be excluded from
scoring (10× magnification).
Figure 55c: Staining caused by DAB droplets should be excluded from scoring (20× magnification).
67
Page 68
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Edge Artifact
Commonly, edge artifacts are linked to the pre-analytic handling of the tissue.
– Inadequate processing of thick tissue samples may mimic edge artifact by
rendering the central portion of the tissue suboptimally fixed relative to the
peripheral areas. In these circumstances, the immunoreactivity based on the
suboptimal central portion may be mistakenly interpreted as non-staining as
optimal fixation is only present at the periphery
– Increased staining is observed around the periphery of the tissue specimen,
known as the “edge artifact”
– Edge artifacts can be due to drying of the tissue specimen prior to fixation or
during the staining procedure
– If the positive reaction is only at the edge of the tissue section (i.e., a few
cell layers of staining at the periphery and ending abruptly with penetration
into the centrally located tumor), scoring at the edge of the tissue specimen
should be avoided
Key point
Scoring of the edge of a specimen should be avoided if staining is
inconsistent with the rest of the specimen
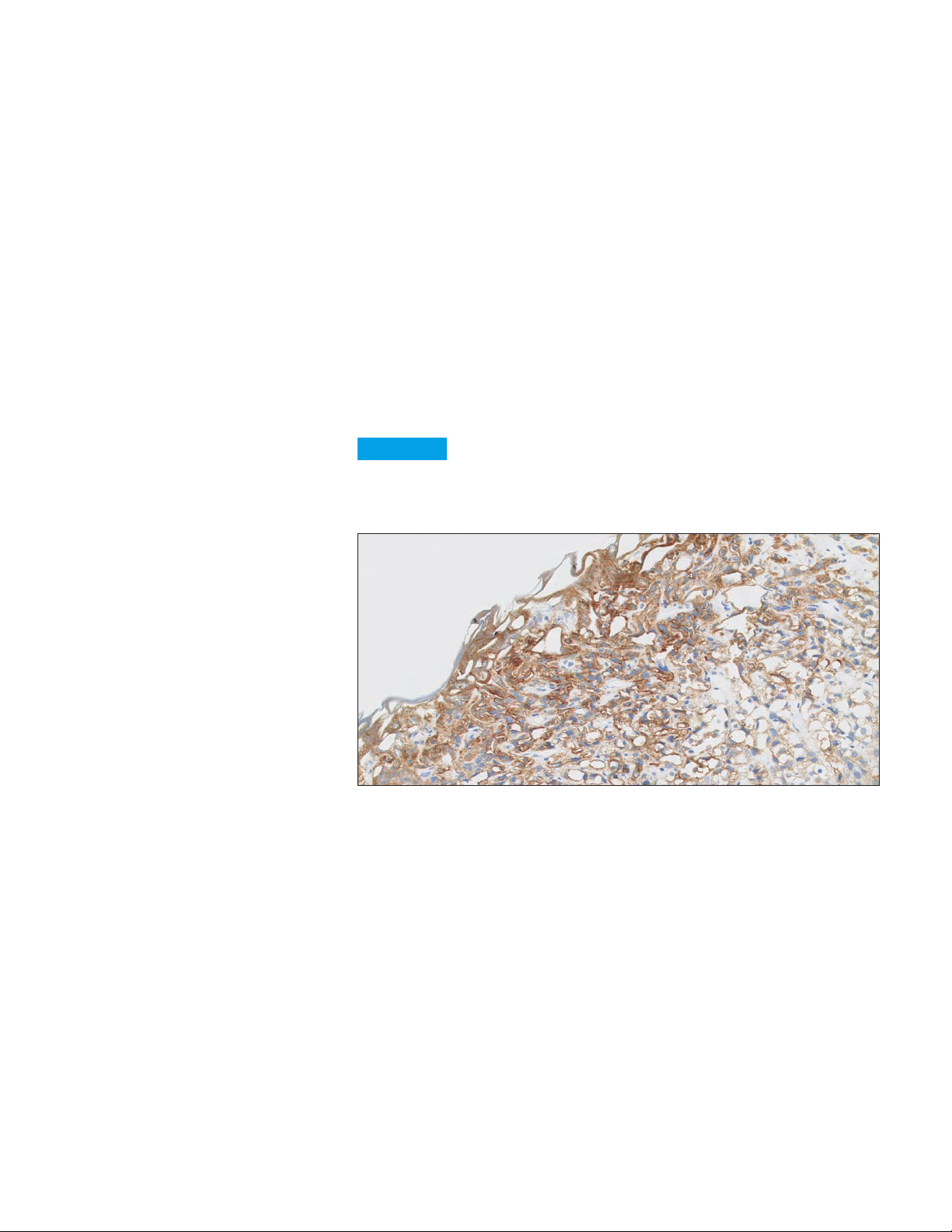
Figure 56: PD-L1 primary antibody exhibiting edge artifact staining; edge staining should be
excluded from scoring (10× magnification).
68
Page 69
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Poor Fixation
Standardization of fixation is very important when using PD-L1 IHC 22C3
pharmDx. Suboptimal fixation of tissues may give erroneous results.
Key point
Proper fixation is important for accurate diagnosis
Figure 57: PD-L1 primary antibody exhibiting poor tissue fixation (20× magnification).
69
Page 70

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Necrosis
Necrosis can be described as morphological changes indicative of cell death
with undefined cellular detail. Necrosis is often present in urothelial carcinoma
specimens and should be excluded from scoring.
Key point
Scoring of necrotic areas should be excluded from the
CPS calculation
Figure 58: PD-L1 primary antibody exhibiting staining of necrosis; necrosis should not be scored
(20× magnification).
70
Page 71

Troubleshooting Guide
PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Troubleshooting Guidelines
for PD-L1 IHC 22C3 pharmDx
For further troubleshooting help, contact your local Agilent representative.
Problem Probable Cause Suggested Action
Verify that the PD-L1 IHC 22C3 pharmDx
No staining of slides
Weak staining of
specimen slides
Weak staining of
specimen slides or of
the positive cell line
on the Control Slide
provided with the kit
Excessive background
staining of slides
Tissue detached
from slides
Excessively strong
specific staining
Target Retrieval Solution
is cloudy in appearance
when heated
Programming error
Lack of reaction with DAB+
Substrate-Chromogen
Solution (DAB)
Sodium azide in wash buffer Use only Dako Wash Buffer (Code K8007)
Degradation of Control Slide
Inappropriate fixation
method used
Insufficient reagent
volume applied
Inappropriate wash buffer used Use only Dako Wash Buffer, Code K8007
Inadequate target retrieval
Inappropriate wash buffer used Use only Dako Wash Buffer, Code K8007
Paraffin incompletely removed
Slides dried while loading onto
Autostainer Link 48
Non-specific binding of
reagents to tissue section
Inappropriate fixation
method used
Use of incorrect
microscope slides
Inadequate preparation
of specimens
Inappropriate fixation
method used
Inappropriate wash buffer used Use only Dako Wash Buffer, Code K8007
When heated, the Target
Retrieval Solution turns cloudy
in appearance
program was selected for programming
of slides
Verify that DAB+ Substrate-Chromogen
Solution was prepared properly
Check kit expiration date and kit storage
conditions on outside of package
Ensure that only neutral buffered formalin
fixative and approved fixation methods
are used
Check size of tissue section and reagent
volume applied
Verify that the 3-in-1 pre-treatment
procedure was correctly performed
Verify that the 3-in-1 pre-treatment
procedure was correctly performed
Ensure slides remain wet with buffer
while loading and prior to initiating run
Check for proper fixation of the specimen
and/or the presence of necrosis
Ensure that only neutral buffered formalin
fixative and recommended fixation
methods are used
Use Dako FLEX IHC Microscope Slides,
(Code K8020), or Fisherbrand Superfrost
Plus slide
Cut sections should be placed in a
58 ± 2 °C oven for 1 hour prior to staining
Ensure that only approved fixatives
and fixation methods are used
This is normal and does not
influence staining
Note: If the problem cannot be attributed to any of the above causes, or if the
suggested corrective action fails to resolve the problem, please call Agilent
Technical Support for further assistance. Additional information on staining
techniques and specimen preparation can be found in Dako Education Guide:
Immunohistochemical Staining Methods (5) (available from Agilent).
71
Page 72

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Clinical Performance Evaluation
The efficacy of KEYTRUDA was investigated in Study KEYNOTE 052 (NCT02335424),
a multicenter, open-label, single-arm trial in 370 patients with locally advanced
or metastatic urothelial carcinoma who were not eligible for cisplatin-containing
chemotherapy. The trial excluded patients with autoimmune disease or a medical
condition that required immunosuppression.
Patients received KEYTRUDA 200 mg every 3 weeks until unacceptable toxicity or
disease progression. Patients with initial radiographic disease progression could
receive additional doses of treatment during confirmation of progression unless
disease progression was symptomatic, was rapidly progressive, required urgent
intervention, or occurred with a decline in performance status. Patients without
disease progression could be treated for up to 24 months. Tumor response
assessments were performed at 9 weeks after the first dose, then every 6 weeks
for the first year, and then every 12 weeks thereafter. The major efficacy outcome
measures were ORR according to RECIST 1.1 as assessed by independent
radiology review and duration of response.
PD-L1 status was determined using PD-L1 IHC 22C3 pharmDx. Data
from the first 100 patients enrolled, the training set, were used to determine the
CPS≥10cutoff.Datafromtheremaining270patients,thevalidationset,were
usedtoclinicallyvalidatetheCPS≥10cutoff.
Amongthe370patients,30%(n=110)hadtumorsthatexpressedPD-L1with
CPS≥10andPD-L1statuswasunknownfor9patients.Baselinecharacteristics
ofthesepatientswere:medianage73years,68%male,and88%White.EightytwopercenthadM1disease,and18%hadM0disease.Eighty-onepercenthada
primarytumorinthelowertract,and18%ofpatientshadaprimarytumorinthe
uppertract.Seventy-sixpercentofpatientshadvisceralmetastases,including11%
withlivermetastases.Reasonsforcisplatinineligibilityincluded:45%withbaseline
creatinineclearanceof<60mL/min,37%withECOGperformancestatusof2,10%
withECOG2andbaselinecreatinineclearanceof<60mL/min,and8%withother
reasons (Class III heart failure, Grade 2 or greater peripheral neuropathy, and Grade
2 or greater hearing loss). Ninety percent of patients were treatment naïve, and
10%receivedprioradjuvantorneoadjuvantplatinumbasedchemotherapy.
Amongthe270patientsinthevalidationset,30%(n=80)hadtumorsthat
expressedPD-L1withCPS≥10.Baselinecharacteristicsofthesepatientswere:
medianage72years,68%male,and86%White.Seventy-onepercenthadM1
disease,and26%hadM0disease.Seventy-ninepercenthadaprimarytumor
inthelowertract,and20%ofpatientshadaprimarytumorintheuppertract.
Seventy-eightpercentofpatientshadvisceralmetastases,including8%with
livermetastases.Reasonsforcisplatinineligibilityincluded:41%withbaseline
creatinineclearanceof<60mL/min,43%withECOGperformancestatusof2,11%
withECOG2andbaselinecreatinineclearanceof<60mL/min,and5%withother
reasons (Class III heart failure, Grade 2 or greater peripheral neuropathy, and
Grade 2 or greater hearing loss). Ninety percent of patients were treatment naïve,
and10%receivedprioradjuvantorneoadjuvantplatinum-basedchemotherapy.
72
Page 73

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
Efficacy results are summarized in Table 5.
Table 5: Efficacy Results in KN052
Endpoint
Objective Response Rate*
ORR (95% CI) 22% (16, 28) 51% (40, 63)
Complete response rate 2% 16%
Partial response rate 20% 35%
Duration of Response
Median in months (range) 9.7 (1.4+ - 11.0+) NR (1.4+ - 11.1+)
+ Denotes ongoing
NR = not reached; * excludes patients with unknown PD-L1 status
CPS < 10 in
Validation Set (N=185)
CPS ≥ 10 in
Validation Set (N=80)
KEYNOTE-361 (NCT02853305) is an ongoing, multicenter, randomized study
in previously untreated patients with metastatic urothelial carcinoma who are
eligible for platinum-containing chemotherapy. The study compares KEYTRUDA
with or without platinum-based chemotherapy (i.e., cisplatin or carboplatin with
gemcitabine) to platinum-based chemotherapy alone. The trial also enrolled a
third arm of monotherapy with KEYTRUDA to compare to platinum-based
chemotherapy alone. The independent Data Monitoring Committee (iDMC) for the
study conducted a review of early data and found that in patients classified as
having PD-L1 expression of CPS < 10, those treated with KEYTRUDA monotherapy
had decreased survival compared to those who received platinum-based
chemotherapy. The iDMC recommended to stop further accrual of patients
with PD-L1 expression of CPS < 10 in the monotherapy arm, however, no other
changes were recommended, including any change of therapy for patients
who had already been randomized to and were receiving treatment in the
monotherapy arm.
73
Page 74

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
References
– Keytruda [prescribing information]. Kenilworth, NJ: Merck & Co.; 2018.
– PD-L1 IHC 22C3 pharmDx [package insert]. Carpinteria, CA: Dako, Agilent
Pathology Solutions; 2018.
– Herbst RS, Soria JC, Kowanetz M, et al. Predictive correlates of response
to the anti-PD-L1 antibody MPDL3280A in cancer patients. Nature.
2014;515(7528):563-567.
– Tumeh PC, Harview CL, Yearley JH, et al. PD-1 blockade induces responses
by inhibiting adaptive immune resistance. Nature. 2014;515(7528):568-571.
– Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell.
2011;144(5):646-674.
– Sharpe AH, Freeman GJ. The B7-CD28 superfamily. Nat Rev Immunol.
2002;2(2):116-126.
– Keir ME, Butte MJ, Freeman GJ, Sharpe AH. PD-1 and its ligands in tolerance
and immunity. Annu Rev Immunol. 2008;26:677-704.
– Freeman GJ, Long AJ, Iwai Y, et al. Engagement of the PD-1 immunoinhibitory
receptor by a novel B7 family member leads to negative regulation of
lymphocyte activation. J Exp Med. 2000;192(7):1027-1034.
– Dong H, Strome SE, Salomao DR, et al. Tumor-associated B7-H1 promotes
T-cell apoptosis: a potential mechanism of immune evasion. Nat Med.
2002;8(8):793-800.
– Brahmer JR, Tykodi SS, Chow LQ, et al. Safety and activity of anti-PD-L1
antibody in patients with advanced cancer. N Engl J Med.
2012;366(26):2455-2465.
– Topalian SL, Hodi FS, Brahmer JR, et al. Safety, activity, and immune
correlates of anti-PD-1 antibody in cancer. N Engl J Med.
2012;366(26):2443-2454.
74
Page 75

PD-L1 IHC 22C3 pharmDx Interpretation Manual – Urothelial Carcinoma
75
Page 76

For PD-L1 testing,
Choose PD-L1 IHC 22C3 pharmDx–
the ONE assay clinical trial-proven
with KEYTRUDA® (pembrolizumab)
KEYNOTE
FDA
ONE
The ONE assay used to assess PD-L1
across KEYTRUDA clinical trials
The ONE assay established with
KEYTRUDA in the pivotal NSCLC studies
The ONE assay FDA-approved as an
aid in identifying patients for treatment
with KEYTRUDA
In ONE all-inclusive kit that delivers
reproducible, repeatable, and clinically
validated results for diagnostic confidence
Learn more:
https://www.agilent.com/chem/PDL122C3
For countries outside of the United States, see the local KEYTRUDA product
label for approved indications and expression cutoff values to guide therapy.
This information is subject to change without notice.
© Agilent Technologies, Inc. 2018
Published in the USA, 2021JAN14
29276 2021JAN06
U.S. and Canada
1-800-227-9770
agilent_inquiries@agilent.com
 Loading...
Loading...