Page 1
Procedure Manual
for the i-STAT
This Procedure Manual is intended to be a template for the Procedure Manual required by CLIA and laboratory accreditation
bodies. This Procedure Manual should be customized for site-specific policies and procedures. The Procedure Manual is
provided on disk for this purpose. This Procedure Manual is not intended to replace the System Manual.
®
System
ART: 714446-00C REV. DATE 07/12/04
Page 2

ART: 714446-00C REV. DATE 07/12/04
Page 3
PROCEDURE MANUAL FOR THE i-STAT SYSTEM
Contents
System Overview..............................................................................................................................................................1
Analyzers
Analysis Time
Cartridges
Glucose Test Strips
Central Data Station or Data Manager
Supplies and Storage Requirements............................................................................................................................1-2
Cartridges
Glucose Test Strips
Controls
Blood Specimens............................................................................................................................................................2-5
Blood Collection Equipment
Blood Volume
Suitable Specimens
Specimen Labeling
Specimen Collection and Handling
Criteria for Specimen Rejection
Precautions
Procedure for Analysis................................................................................................................................................6-10
Preparation for Use
Procedure for Cartridge Testing
Procedure for Glucose Test Strip Testing
Alternative Procedure
Results........................................................................................................................................................................11-18
Calculations
Displayed Results
Suppressed Results
Printing and Transmitting Results
Reference Ranges and Reportable Ranges
Critical Results
Interferences
Quality Control..........................................................................................................................................................19-23
Daily Procedures
Monthly Procedures
Periodic Procedures
Calibration......................................................................................................................................................................23
Clinical Significance .................................................................................................................................................24-26
Principles of Measurement.......................................................................................................................................27-28
ART: 714446-00C REV. DATE 07/12/04
Page 4

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
References.......................................................................................................................................................................28
Logs ................................................................................................................................................i-vii
ART: 714446-00C REV. DATE 07/12/04
Page 5

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
SYSTEM OVERVIEW
The i-STAT® System incorporates comprehensive components needed to perform blood analysis at the point of care. The
System consists of the following primary components:
Analyzers
Analyzers can be the i-STAT Portable Clinical Analyzer, the i-STAT1 Analyzer, or the Blood Analysis Module, which is
used in conjunction with the Philips Medical Systems (formerly Agilent Technologies) CMS and 24/26 Patient Monitor.
When a sample-filled i-STAT cartridge is inserted into an analyzer for analysis, the analyzer automatically controls all
functions of the testing cycle including fluid movement within the cartridge, calibration and continuous quality monitoring.
A MediSense
drop of whole blood is applied to the target area of the test strip.
Analysis Time
ACT cartridge: to detection of end point - up to 1000 seconds (16.7 min.)
PT/INR cartridge: to detection of end point – up to 300 seconds (5 min.)
cTnI cartridge: 600 seconds (10 min.)
Other cartridges: typically 130 to 200 seconds
®
Precision PCx™ or PCx™ Plus Glucose Test Strip is scanned and inserted into the i-STAT1 Analyzer and a
MediSense Precision PCx or PCx Plus Glucose Test Strip: 20 seconds
Cartridges
A single-use disposable cartridge contains microfabricated sensors, a calibrant solution, fluidics system, and a waste
chamber. Sensors for analysis of pH, PCO
, PO2, sodium, potassium, chloride, ionized calcium, glucose, lactate, creatinine,
2
urea nitrogen (BUN) and hematocrit are available in a variety of panel configurations. Cartridges are also available for
Celite-ACT, Kaolin-ACT, PT/INR, and Troponin I/cTnI (Table 1). A whole blood sample of approximately 1 to 3 drops is
dispensed into the cartridge sample well, and the sample well is sealed before inserting it into the analyzer.
Glucose Test Strips
The i-STAT1 Analyzer is capable of using the Abbott MediSense Precision PCx or PCx Plus Blood Glucose Test Strips.
Central Data Station or Data Manager
A dedicated desktop computer with the i-STAT Central Data Station program provides the primary information management
capabilities for the i-STAT System. IR Links for Portable Clinical Analyzers, Downloaders and Downloader/Rechargers for
the i-STAT1 Analyzers and a Philips installed server for Blood Analysis Modules allow for transmission of patient records
from a widely distributed network of analyzers to the Central Data Station program. Data can be stored, organized, edited,
and transferred to a laboratory information system or other computer system. Cartridge usage and efficiency reports can be
generated for management of the system.
SUPPLIES and STORAGE REQUIREMENTS
Cartridges
Cartridges are sealed in individual pouches or portion packs. Store the main supply of cartridges at a temperature between 2
to 8°C (35 to 46°F). Do not allow cartridges to freeze. (Freezing will cause higher than expected ionized calcium results).
Cartridges may be stored at room temperature (18 to 30°C or 64 to 86°F) for 14 days. Cartridges should not be returned to
the refrigerator once they have been at room temperature, and should not be exposed to temperatures above 30°C (86°F). If
the pouch has been punctured, the cartridge should not be used. Write the date on the cartridge box or individual cartridge
pouches to indicate the two-week room temperature expiration date. Cartridges should remain in pouches until time of use.
Do not use after the labeled expiration date.
1
ART: 714446-00C REV. DATE 07/12/04
Page 6

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
Glucose Test Strips
Test strips are sealed in individual foil packets. Store the strips at a temperature between 4 and 30°C (39 and 86°F). When
stored properly, the unopened test strips remain stable until the expiration date printed on the barcode label. Do not freeze
and keep out of direct sunlight.
Controls
i-STAT Controls for blood gases, electrolytes, and chemistries
Store at 2 to 8°C (35° to 46°F). Controls may be stored at room temperature (18 to 30°C or 64 to 86°F) for five days. Do not
use after expiration date on the box and ampules.
i-STAT Controls for ACT and PT/INR
Store at 2 to 8°C (35° to 46°F). Do not use after expiration date on the box and vials. Controls should be used immediately
after reconstitution.
i-STAT Controls for Cardiac Markers
Store at -18°C (-1°F) in a non-defrosting freezer. After thawing, the opened or unopened 1.0 mL vial is stable for 4 hours
when capped and stored at 2 to 8°C (35° to 46°F). Do not refreeze
™
Hematronix Meter Trax
Store upright at 2 to 8°C (35° to 46°F). Do not allow to freeze. Ensure control is completely mixed before using. Once
opened, bottles may be used for up to 31 days provided they have been resealed and refrigerated immediately after each use.
Write the date of opening on the bottle label. Do not use after expiration date on box and vials.
Whole Blood Reference Controls for hematocrit
Electronic Simulator
Store at room temperature and protect contact pads from contamination by replacing the plastic cap and placing the
Electronic Simulator in its protective case after use.
MediSense Precision Glucose Control Solutions for test strips
Store the controls at temperatures between 4 and 30°C (39 and 86°F). Do not freeze. Each bottle of control solution is stable
for 90 days after opening. Write the date of opening on the bottle label. Always make sure the cap is returned to the correct
bottle and tightly closed immediately after use.
BLOOD SPECIMENS
Blood Collection Equipment
Cartridges for Blood Gas/Electrolytes/Chemistries/Hematocrit
Skin puncture: lancet and capillary collection tube (plain, lithium heparin, or balanced heparin for electrolytes and
blood gases)
Venipuncture: lithium or sodium heparin collection tubes and disposable transfer device (e.g., 1cc syringe and a 16
to 20 gauge needle).
Arterial puncture: Plain syringe or blood gas syringe with heparin and labeled for the assays performed or with the
least amount of heparin to prevent clotting (10 U heparin/mL of blood)
Cartridges for ACT
Skin puncture: not recommended
Venipuncture and arterial puncture: plain plastic syringe without anticoagulant
Glucose Test Strips
Skin puncture: lancet and capillary collection tube with lithium heparin, sodium heparin, or EDTA or direct
application of sample to test strip
Venipuncture and arterial puncture: collection tube or syringe with lithium heparin, sodium heparin, or EDTA
2
ART: 714446-00C REV. DATE 07/12/04
Page 7
PROCEDURE MANUAL FOR THE i-STAT SYSTEM
Cartridges for PT/INR
Skin puncture: lancet only needed. Cartridge can be filled directly from the finger.
Venipuncture and arterial puncture: plain plastic syringe without anticoagulant.
Cartridges for Troponin I/.cTnI
Skin puncture: not recommended.
Venipuncture: lithium or sodium heparin collection tubes and disposable transfer device (e.g. 1 cc syringe and a 16
to 20 gauge needle). Alternately, a plain syringe or plain collection tube and disposable transfer device can be used
if the sample is tested within one minute of patient draw.
Blood Volume
See Table 1 below for cartridge volumes. For the glucose test strip, sufficient sample to cover target area - approximately
one drop, is required.
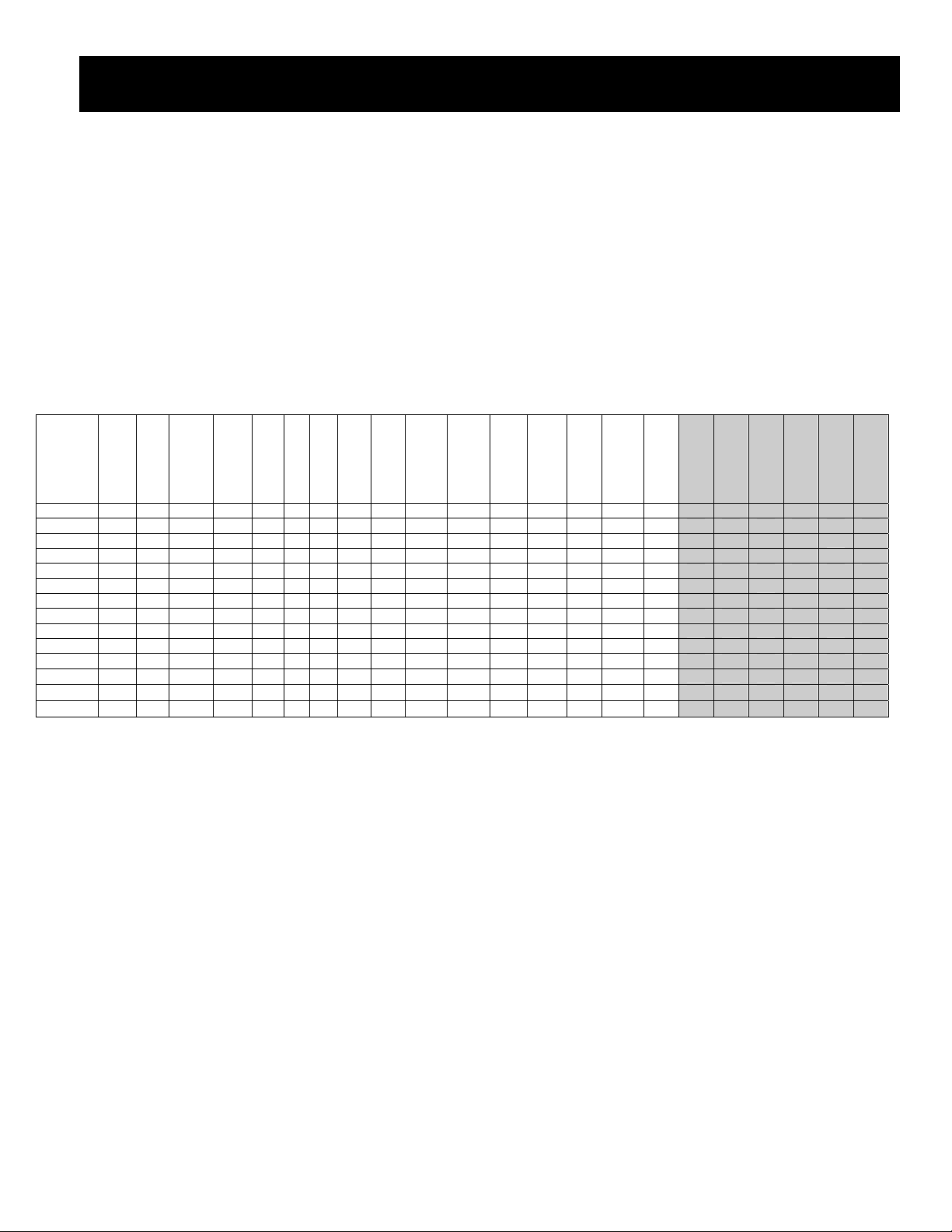
Table 1: Cartridge Panel Configurations and Blood Volume
2
µL
pH
Cartridge
CG8+ 95
EG7+ 95
EG6+ 95
CG4+ 95
G3+ 95
EC8+ 65
6+ 65
EC4+ 65
E3+ 65
G 65
Crea 65
ACT 40
PT/INR 20
cTnI 16
Vol.
• • • • •
• • • • •
• • • • •
• • •
• • •
• •
PO2
PCO
K
Na
• • •
• • •
• •
• •
Cl
iCa
Glu
BUN
• •
•
• •
• •
•
•
Lact
Creat
•
•
Hct
ACT
PT/INR
•
•
•
•
•
•
•
•
•
Suitable Specimens for Cartridges for Blood Gases, Electrolytes, Chemistries, and Hematocrit
Fresh whole blood collected in a plain capillary collection tube or capillary collection tube with balanced heparin.
Fresh whole blood collected in a collection tube with lithium or sodium heparin anticoagulant. Fill collection tubes
to capacity.
Fresh whole blood collected in a plain plastic syringe or in a blood gas syringe labeled for the assays to be
performed. Fill syringes for correct blood-to-heparin ratio.
Suitable Specimens for ACT
Fresh whole blood without anticoagulant collected in a plastic syringe. If from an indwelling line, flush the line
with 5mL saline and discard the first 5mL of blood or three to six dead space volumes of the catheter.
BE
cTnI
HCO3
• • • •
• • • •
• • • •
• • • •
• • • •
• •
•
SO2
TCO2
Anion Gap
• • •
Shading denotes calculated values
Hb
•
•
•
•
•
•
Fresh whole blood collected in a plastic tube without anticoagulant, clot activators, or serum separators. Device
used to transfer sample to cartridge must be plastic.
Suitable Specimens for PT/INR
Fresh whole blood without anticoagulant collected in a plastic syringe or plastic evacuated tube without clot
activators or serum separators. Device used to transfer sample to cartridge must be plastic.
Fresh capillary whole blood dispensed directly into the cartridge from the finger.
3
ART: 714446-00C REV. DATE 07/12/04
Page 8

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
Suitable Specimens for Glucose Test Strip
Fresh capillary whole blood collected in a capillary collection tube containing sodium heparin, lithium heparin, or
EDTA. Test immediately.
Fresh venous whole blood collected in a collection tube containing sodium heparin, lithium heparin, or EDTA.
Test within 30 minutes of collection.
Fresh arterial whole blood collected in a syringe containing sodium heparin, lithium heparin, or EDTA. Test
within 30 minutes of collection.
Suitable Specimens for Troponin I/cTnI
Fresh heparinized whole blood or plasma samples collected in syringes or evacuated tubes containing lithium or
sodium heparin. Collection tubes must be filled at least half full.
Non heparinized whole blood samples tested within one minute of patient draw collected into a plastic syringe or
plastic evacuated tube containing no additives.
Specimen Labeling
Unless the specimen is analyzed immediately after collection and then discarded, the specimen container must be labeled
with the following information:
Patient name, sex, age
Patient ID number
Time and date of collection
Phlebotomist ID
Doctor’s name
Specimen Collection and Handling
In-Dwelling Line
Back flush line with sufficient amount of blood to remove intravenous solution, heparin, or medications that may
contaminate the sample. Recommendation: three to six times the volume of the catheter, connectors, and needle. If
collecting sample for ACT, clear the line first with 5mL saline and discard the first 5mL of blood.
Arterial Specimens
For cartridge testing of blood gases, electrolytes, chemistries, and hematocrit, fill a plain syringe or fill a blood gas syringe,
labeled for the assays to be performed, to the recommended capacity, or use the least amount of liquid heparin anticoagulant
that will prevent clotting. Under-filling syringes containing liquid heparin will decrease results due to dilution and will
decrease ionized calcium results due to binding. For ionized calcium, balanced or low volume heparin blood gas syringes
should be used. Do not expose sample to air or PCO
above or increase if the value is below the PO
2
may decrease, pH may increase and PO2 may decrease if the value is
2
of room air (approximately 150 mmHg).
For cartridge testing of ACT, use only a plain, plastic syringe without anticoagulant.
For glucose test strips, fill to capacity a syringe or collection tube containing lithium heparin, sodium heparin, o r EDTA.
Mix blood and anticoagulant by rolling syringe between palms for at least 5 seconds each in two different directions, then
invert the syringe repeatedly for at least 5 seconds. Discard the first two drops of blood. For blood gas testing, avoid or
remove immediately any air drawn into syringe to maintain anaerobic conditions.
Test sample collected without anticoagulant immediately. Test samples for ACT and PT/INR immediately. Test samples for
lactate within 3 minutes of sample collection. For pH, blood gases and ionized calcium, test within 10 minutes of collection.
If not tested immediately, remix the sample and discard the first two drops of blood from a syringe before testing. For the
glucose test strip and other cartridge tests, test sample within 30 minutes of collection.
Venous Specimens
For cartridge testing of electrolytes, chemistries, and hematocrit, collect sample into an evacuated blood collection tube or a
syringe containing sodium, lithium, or balanced heparin anticoagulant. For ionized calcium measurements, balanced heparin
or 10 U of sodium or lithium heparin/mL of blood is recommended. Fill tubes to capacity; fill syringes for correct heparin-toblood ratio. Incomplete filling causes higher heparin-to-blood ratio, which will decrease ionized calcium results and may
4
ART: 714446-00C REV. DATE 07/12/04
Page 9

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
affect other results. The use of partial – draw tubes (evacuated tubes that are adjusted to draw less than the tube volume, e.g.
a 5 mL tube with enough vacuum to draw only 3 mL) is not recommended because of the potential for decreased measured
PCO2 results and calculated HCO
For cartridge testing of ACT or PT/INR, use only a plain, plastic syringe or collection tube containing no anticoagulant. Use
a plastic capillary tube, pipette, or syringe to transfer sample from a tube to a cartridge.
For glucose strip testing, EDTA is also an acceptable anticoagulant.
Mix blood and anticoagulant by inverting a tube gently at least ten times. Roll a syringe vigorously between the palms for at
least 5 seconds each in two different directions, then invert the syringe repeatedly for at least 5 seconds, then discard the first
two drops of blood. Note that it may be difficult to properly mix a sample in a 1 cc syringe.
Test Sample collected without anticoagulant immediately. Test samples for ACT and PT/INR immediately. Test samples for
lactate within 3 minutes of sample draw. Test samples for pH, PCO2, and ionized calcium within 10 minutes of samp le draw.
If not tested immediately, remix the sample before testing and discard the first two drops of blood from a syringe before
testing. For the glucose test strip and other cartridge tests, test sample within 30 minutes of collection.
Finger and Heelstick Specimens
For tests other than PT/INR, wipe away the first drop of blood, which contains excess tissue fluid which can increase the
potassium result and decrease other test results. Avoid drawing air into the capillary tube. Use balan ced heparin or plain
capillary tubes for ionized calcium. Test samples immediately to avoid clotting (especially in neonates). Capillary samples
are not recommended for ACT or Troponin I/cTnI.
and TCO2 values.
3
Criteria For Specimen Rejection
Evidence of clotting
Specimens collected in vacuum tubes with anticoagulant other than lithium or sodium heparin
Specimens for ACT or PT/INR collected in glass syringe or tube or with anticoagulant of any kind
Syringe for pH, PCO
Incompletely filled vacuum tube for the measurement of ionized calcium or PCO
Other sample types such as urine, CSF, and pleural fluid
, and PO2 with air bubbles in sample
2
2
Precautions: Avoid the Following Circumstances
Drawing a specimen from an arm with an I.V.
Stasis (tourniquet left on longer than one minute before venipuncture)
Extra muscle activity (fist pumping)
Hemolysis (alcohol left over puncture site, or a traumatic draw)
Icing before filling cartridge
Time delays before filling cartridge, especially lactate, ACT, and PT/INR
Exposing the sample to air when measuring pH, PCO
, and PO2
2
5
ART: 714446-00C REV. DATE 07/12/04
Page 10

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
PROCEDURE FOR ANALYSIS
Preparation for Use
An individual cartridge may be used after standing 5 minutes, in its pouch, at room temperature. An entire box should stand
at room temperature for one hour before cartridges are used.
Glucose test strips require no preparation for use.
Procedure for Cartridge Testing (other than PT/INR or Tropnin I/cTnI)
1. Remove the cartridge from its pouch. Avoid touching the contact pads or exerting pressure over the calibrant pack in
the center of the cartridge.
2. Following thorough mixing of the sample, direct the dispensing tip or capillary tube containing the blood into the
sample well.
3. Dispense the sample until it reaches the fill mark on the cartridge and the well is about half full.
4. Close the cover over the sample well until it snaps into place. (Do not press over the sample well.)
5. Insert the cartridge into the cartridge port on the analyzer until it clicks into place. When using an ACT cartridge, the
analyzer must remain horizontal during the testing cycle.
6. Never attempt to remove a cartridge while the LCK or “Cartridge Locked” message is displayed.
7. Enter an operator ID number. Repeat if required.
8. Enter the patient ID number. Repeat if required.
9. Select tests to be reported, if prompted.
10. Enter additional parameters on the Chart Page if required:
Patient temperature can be entered as degrees Centigrade or Fahrenheit. (Use the * key on the i-STAT Portable
Analyzer for a decimal point.)
FIO
Fields 1, 2, and 3 are user-defined fields, typically used for ventilator settings such as PIP or PEEP.
Choose the number corresponding to the type of sample used when prompted at the Sample Type field. Select
11. View results shown on the analyzer’s display screen.
can be entered as the number of liters or as a percentage of the oxygen a patient is receiving.
2
CPB for patient in cardiopulmonary bypass surgery.
Procedure for the i-STAT1 Analyzer with Information First
1. Turn the analyzer on and press 2 for i-STAT Cartridge.
2. Scan or enter the operator and patient IDs. Repeat if prompted.
3. Remove the cartridge from its pouch. Avoid touching the contact pads or exerting pressure over the calibrant pack in the
center of the cartridge.
4. Following thorough mixing of the sample, direct the dispensing tip or capillary tube containing the blood into the sample
well and dispense the sample until it reaches the fill mark on the cartridge and the well is about half full.
5. Close the cover over the sample well until it snaps into place. (Do not press over the sample well.)
6. Insert the cartridge into the cartridge port until it clicks into place. When using an ACT cartridge, the analyzer must
remain horizontal during the testing cycle.
7. Select tests to be reported, if prompted.
8. Enter additional parameters on the Chart page if required:
Choose the number corresponding to the type of sample used when prompted at the Sample Type field.
Fields 1, 2, and 3 are user-defined fields, typically used for ventilator settings such as PIP or PEEP.
Patient temperature can be entered as degrees Centigrade or Fahrenheit.
FIO
Choose 1-YES or 2-NO for CPB.
Press the → key to return to the results page.
can be entered as the number of liters or as a percentage of the oxygen a patient is receiving.
2
6
ART: 714446-00C REV. DATE 07/12/04
Page 11
PROCEDURE MANUAL FOR THE i-STAT SYSTEM
9. View results shown on the analyzer’s display screen.
10. Enter Comment Code if prompted.
Procedure for PT/INR Cartridge Testing
Skin Punctures
1. Remove cartridge from foil pouch and place the cartridge on a flat surface.
2. Prepare lancet device and set aside until needed.
3. Clean and prepare the finger to be sampled. Allow finger to dry thoroughly before sampling.
4. Prick the bottom side of the fingertip with the lancet dev ice.
5. Gently squeeze the finger, developing a hanging drop of blood and perform the test with the first sample of blood. Avoid
strong repetitive pressure, ("milking") as it may cause hemolysis or tissue fluid contamination of the specimen.
6. Touch the drop of blood against the bottom of the sample well. Once in contact with the sample well, the blood will be
drawn into the cartridge.
7. Apply sample until it reaches the fill mark indicated on the cartridge.
8. Fold the sample closure over the sample well.
9. Press the rounded end of the closure until it snaps into place.
10. Insert the cartridge into the cartridge port until it snaps into place.
11. Enter an operator ID number. Repeat if required.
12. Enter the patient ID number. Repeat if required.
13. Select tests to be reported, if prompted.
14. Enter additional parameters on the Chart Page, if required.
15. View result on the analyzer’s display screen.
Note: To further simplify the sample application into the test cartridge, it is possible to bring the cartridge to the finger
for easier application. Do ensure that the instrument remains on a flat vibration-free surface for testing.
Procedure for Troponin I/cTnI Testing
Note: The i-STAT cTnI cartridges can only be used with the i-STAT 1 Analyzer bearing the
symbol.
This symbol is located on the grey casing next to the lower right corner of the analyzer display screen. Before testing cTnI
cartridges on the i-STAT 1 Analyzer, the analyzer must be customized through the Central Data Station (CDS) or through
the analyzer’s Customization menu for the following options:
1. Cartridge Barcode Required, or
2. Cartridge Information First Required
AND Cartridge Lot Number Required.
7
ART: 714446-00C REV. DATE 07/12/04
Page 12
PROCEDURE MANUAL FOR THE i-STAT SYSTEM
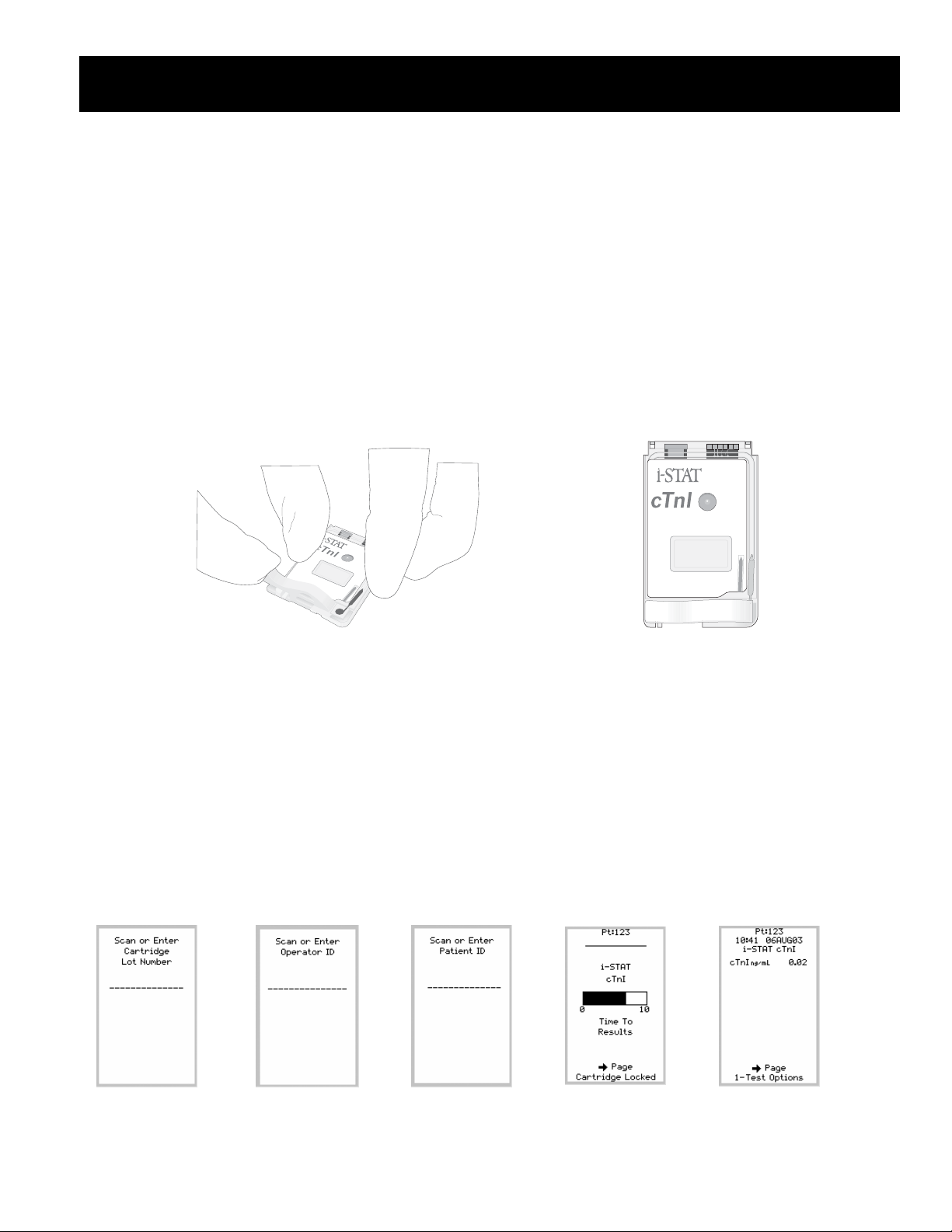
Cartridge Test Procedure (Non-Information First Customization)
1. Remove cartridge from portion pack. Do not immediately dispose of the portion pack, as the cartridge lot number listed
on it will be scanned into the analyzer during the testing procedure. Handle the cartridge from its edges. Avoid
touching the contact pads or exerting pressure over the center of the cartridge.
2. Following thorough mixing of the sample, direct the transfer device (either syringe tip or pipette tip) into the inlet port.
Apply a single drop of sample to the inlet port. If the cartridge fill is incomplete as seen via the fill indicator on the
cartridge label, apply a second small drop until the sample reaches the fill mark.
3. To close the cTnI cartridge:
a. first anchor the cartridge in place by using the thumb and index finger of one hand to grasp the cTnI cartridge
from its side edges away from the sample inlet.
b. use the thumb of the other hand to slide the plastic closure clip to the right until it locks into place over the
sample well. Note: When sliding the closure clip, the index finger of that same hand should not be placed
directly across from the thumb, as this could result in the sample being pushed onto the user’s glove. This
index finger should be placed just above the position of the sliding clip during closure or not used at all.
4. Insert the cartridge into the cartridge port. Do not attempt to remove the cartridge while th e Cartridge Locked message
is displayed.
5. Scan the Cartridge Lot number from the cartridge portion pack (Screen 1 below).
6. Scan or Enter Operator ID (Screen 2 below). Repeat if prompted.
7. Scan or Enter Patient ID (Screen 3 below). Repeat if prompted.
The analyzer must remain on a level surface with the display facing up during testing. Motion of the analyzer during
testing can increase the frequency of suppressed results or quality check codes.
8. Select tests to be reported, if prompted.
9. Enter sample type on chart page if applicable.
10. The Time to Results countdown bar will then be displayed (Screen 4 below). Once time has elapsed, view results on
analyzer’s display (Screen 5 below).
11. Remove cartridge after Cartridge Locked message disappears. The analyzer is ready for the next test immediately.
Screen 1 Screen 2 Screen 3 Screen 4 Screen 5
8
ART: 714446-00C REV. DATE 07/12/04
Page 13

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
Cartridge Test Procedure (Information First Customization)
1. Press the On/Off key to turn analyzer on.
2. Press 2 for i-STAT Cartridge from the Test Menu (Screen 1 below).
3. Scan or Enter Operator ID (Screen 2 below). Repeat if prompted.
4. Scan or Enter Patient ID (Screen 3 below). Repeat if prompted.
5. Scan Cartridge Lot number from the cartridge portion pack (Screen 4 below).
6. Remove cartridge from portion pack. Handle the cartridge by its edges. Avoid touching the contact pads or exerting
pressure over the center of the cartridge.
7. Following thorough mixing of the sample, direct the transfer device (either syringe tip or pipette tip) into the inlet port.
Apply a single drop of sample to the inlet port. If the cartridge fill is incomplete as seen via the fill indicator on the
cartridge label, apply a second small drop until the sample reaches the fill mark.
8. To close the cTnI cartridge:
a. First anchor the cartridge in place by using the thumb and index finger of one hand to grasp the cTnI cartridge
from its side edges away from the sample inlet.
b. Use the thumb of the other hand to slide the plastic closure clip to the right until it locks into place over the
sample well. Note: When sliding the closure clip, the index finger of that same hand should not be placed
directly across from the thumb, as this could result in the sample being pushed onto the user’s glove. This
index finger should be placed just above the position of the sliding clip during closure or not at all.
9. Insert cartridge into cartridge port (Screen 5 below). Do not attempt to remove the cartridge while the Cartridge Locked
message is displayed.
The analyzer must remain on a level surface with the display facing up during testing. Motion of the analyzer during
testing can increase the frequency of suppressed results or quality check codes.
10. Select tests to be reported, if prompted.
11. Enter sample type on chart page, if applicable.
12. The Time to Results countdown bar will then be displayed (Screen 6 below). Once time has elapsed, view results on
analyzer’s display (Screen 7 below).
13. Remove cartridge after Cartridge Locked message disappears. The analyzer is ready for the next test immediately.
Screen 1 Screen 2 Screen 3 Screen 4 Screen 5 Screen 6 Screen 7
9
ART: 714446-00C REV. DATE 07/12/04
Page 14

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
PCx Glucose Test Strip Procedure
1. Press the (On/Off) key to turn the analyzer on.
2. Press 3 for PCx Glucose Strip.
3. Press 1 for Patient.
4. Scan or enter operator ID. Repeat if prompted.
5. Scan or enter patient ID. Repeat if prompted.
6. Scan or enter test strip lot number.
7. Press 1 for Arterial/Capillary or 2 for venous sample if prompted.
8. Open foil packet, remove test strip and insert into analyzer test strip port with black contact
bars facing up and forward.
9. Apply drop of blood to target area of test strip. Cover the entire area. Do not touch the test
strip after sample is applied. (If test fails to start after second drop applied or if more than
30 seconds have passed, discard test strip and repeat the test.)
10. Enter chart page information if applicable.
11. View results on analyzer’s display.
12. Enter Comment Code if applicable.
13. Remove and discard test strip.
a. Do not handle test strip with wet or dirty hands.
b. Do not scan the barcode of another test strip.
c. Do not use test strips that are wet, scratched or damaged in any way.
d. Do not re-use test strips.
Alternative Procedure
Should the i-STAT System become inoperable for any reason, specimens should be collected and submitted to the laboratory
in accordance with the Laboratory Procedure Manual.
10
ART: 714446-00C REV. DATE 07/12/04
Page 15

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
RESULTS
Calculations
The i-STAT analyzer contains a microprocessor that performs all calculations required for reporting results.
Displayed Results
Results are displayed numerically with their units. Electrolyte, chemistry and hematocrit results are also depicted as bar
graphs with reference ranges marked under the graphs.
Suppressed Results
There are three conditions under which the i-STAT System will not display results:
1. Results outside the System’s reportable ranges are flagged with a < or > , indicating that the result is below the lower
limit or above the upper limit of the reportable range respectively. (See the table of Reportable Ranges.) The < > flag
indicates that the results for this test were dependant on the result of a test flagged as either > or <.
Action:
Send specimen(s) to the laboratory for analysis.
2. Cartridge results which are not reportable based on internal QC rejection criteria are flagged with ***.
Action:
Analyze the specimen again using a fresh sample and another cartridge. If the specimen integrity is not in question, the
results that are not suppressed should be reported in the usual manner. If the result is suppressed again, send
specimen(s) to the laboratory for analysis in accordance with the Laboratory Procedure Manual.
3. A Quality Check message will be reported instead of results if the analyzer detects a problem with the sample, calibrant
solution, sensors, or mechanical or electrical functions of the analyzer during the test cycle.
Action:
Take the action displayed with the message that identifies the problem. Refer to the i-STAT or i-STAT 1 System
Manual’s Troubleshooting section or the “Analyzer Coded Messages” Technical Bulletin if necessary.
Printing and Transmitting Results
Printing Results from the i-STAT Portable Clinical Analyzer to the HP Portable Printer (Note: The Martel Printer cannot
be used with the i-STAT Portable Clinical Analyzer.)
1. Place the analyzer in the cradle of an IR Link or align the IR windows of the analyzer and printer. Turn the printer on
(printer light red) or press the paper advance switch to reactivate.
2. To print the displayed test record, press the PRT key on the analyzer.
3. To print a stored test record(s), select “Print Results” from the Stored Results menu. Select records to be printed by
pressing the Key(s) corresponding to the numbers beside the record(s). Press the numbered key again to deselect a
record. Then press the PRT Key.
4. Do not move the analyzer while “Printing” is displayed.
Optional: Write the patient’s name on the “Pt Name” line and the physician’s name on the “Physician” line.
Note: Results printed on thermal paper will fade with time and are therefore not acceptable as a permanent chartable
record.
11
ART: 714446-00C REV. DATE 07/12/04
Page 16

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
Printing Results from the i-STAT1 Analyzer to the Martel Portable Printer (Note: The HP printer cannot be used with the
i-STAT 1 Analyzer.)
Without Downloader or Downloader/Recharger
1. Turn printer on if green power light is not on.
2. Align IR windows of analyzer and printer.
3. Display results.
4. Press the Print key.
5. Do not move analyzer or printer until printing is co mplete.
6. If printer is not powered from a wall outlet, turn printer off.
With Downloader or Downloader/Recharger
1. Place analyzer in Downloader or Downloader/Rechrager that is wired to the printer.
2. Display results.
3. Press the Print key.
4. Do not move analyzer or printer until printing is co mplete.
Printing more than one result
1. Turn the analyzer on.
2. Press the Menu key.
3. Press 2 for Data Review.
4. Press 7 for List.
5. Scroll through the test records using the
← and →keys.
6. Press the numbered key for the test record(s). (Press the numbered key again to deselect a record.)
7. Align analyzer and printer IR window or place in Downloader or Downloader/Recharger attached to printer. Press the
Print key.
Transmitting Results from the i-STAT Portable Clinical Analyzer to the Central Data Station
1. Place the analyzer in the cradle of an IR Link. The IR status light must be green.
2. With a test record on the display screen, press the * key.
3. Do not move the analyzer while “Transmitting” is displayed. During transmission the IR Link’s light will blink
alternately red and green. If transmission is successful, the IR Link will emit a single high-pitched beep and the light will
return to green. An unsuccessful transmission is indicated by three low tone beeps. In this case repeat the transmission
process. If unsuccessful the second time, notify the i-STAT System Coordinator.
Transmitting Results from the i-STAT1 Analyzer to the Data Manager
1. Place analyzer in a Downloader or Downloader/Recharger.
2. Do not move analyzer while the message “Communication in Progress” is displayed.
12
ART: 714446-00C REV. DATE 07/12/04
Page 17

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
Reference Ranges
1,2
, Reportable Ranges, and Test Unit Conversions
Reference range means the range of test values expected from 95% of fasting individuals presumed to be healthy. Reportable
range means the range of test values throughout which the measurement system’s results have been shown to be valid. The
following table contains the Reference Ranges (for adults) and Reportable Ranges applicable to the i-STAT System.
Cartridges
ANALYTE UNIT REFERENCE RANGE
(arterial) (venous)
Sodium
Potassium
Chloride
BUN
UREA
Glucose
mmol/L 138 – 146 138 - 146 100 – 180 mmol/L x 1 = mEq/L
mmol/L 3.5 – 4.9 3.5 - 4.9 2.0 – 9.0 mmol/L x 1 = mEq/L
mmol/L 98 – 109 98 – 109 65 – 140 mmol/L x 1 = mEq/L
mg/dL
mmol/L
mg/dL
g/L
mmol/L
8 – 26 8 – 26
2.9 – 9.4 2.9 – 9.4
70 – 105 70 – 105
0.70 – 1.05 0.70 – 1.05
3.9 – 5.8 3.9 – 5.8
REPORTABLE
RANGE
3 – 140
1 – 50
20 – 700
0.20 – 7.00
1.1 – 38.9
UNIT CONVERSION
Example:
140 mmol/L = 140 mEq/L
mg/dL BUN x 0.357 = mmol urea/L
Example:
20 mg/dL BUN = 7.1 mmol urea/L
mg/dL x 0.0556 = mmol/L
Example:
100 mg/dL = 5.55 mmol/L
g/L x 5.556 = mmol/L
Creatinine
Ionized Calcium
pH
PCO2
pO2
mg/dL
µmol/L
mmol/L
mg/dL
7.35 – 7.45 7.31 – 7.41 6.50 – 8.00 N/A
mm/Hg
kPa
mm/Hg
kPa
0.6 - 1.3 0.6 - 1.3
53 - 115 53 - 115
1.12 – 1.32 1.12 – 1.32
4.5 – 5.3 4.5 – 5.3
35 – 45 41 – 51
4.67 – 6.00 5.47 – 6.80
80 – 105
10.7 – 14.0
0.2 - 20.0
18 - 1768
0.25 – 2.50
1.0 – 10.0
5 – 130
0.67 – 17.33
5 – 800
0.7 – 106.6
mg/dL x 88.4 = mol/L
mmol/L x 4 = mg/dL
1.13 mmol/L x 4 = 4.52 mg/dL
mmHg x 0.133 = kPa
35 mmHg x 0.133 = 4.66 kPa
mmHg x 0.133 = kPa
83 mmHg x 0.133 = 11.04 kPa
Example:
Example:
Example:
13
ART: 714446-00C REV. DATE 07/12/04
Page 18

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
ANALYTE UNIT REFERENCE RANGE
(arterial) (venous)
REPORTABLE
UNIT CONVERSION
RANGE
Hematocrit
Lactate
HCO3*
TCO2*
BE
*
ecf
Anion Gap*
sO2*
Hb*
Celite ACT
%PCV
Fraction
38 – 51 38 – 51
0.38 – 0.51 0.38 – 0.51
10 – 75
0.10 – 0.75
% PCV x 0.01 =
Volume fraction
Example:
40% PCV = 0.40 PCV
mmol/L
mg/dL
0.36 –1.25 0.90-1.70
3.2 – 11.3 8.1–15.3
0.30 – 20.0
2.7 – 180.2
mmol/L x 9.01 = mg/dL
mmol/L 22 – 26 23 - 28 1.0 – 85.0 mmol/L x 1 = mEq/L
mmol/L 23 – 27 24 - 29 1 – 85
mmol/L (-2) – (+3) (-2) – (+3) (-30) – (+30)
mmol/L 10 – 20 10 – 20 (-10) – (+99)
% 95 – 98 0 - 100 % x 0.01 = fraction
saturated
g/dL
g/L
mmol/L
seconds 74 – 125 (PREWRM) 74 – 125 (PREWRM)
12 – 17 12 – 17
120 – 170 120 – 170
7 – 11 7 – 11
3.4 – 25.5
g/dL x 10 = g/L
34 – 255
2.1 – 15.8
50 - 1000
84 – 139 (NONWRM) 84 – 139 (NONWRM)
Kaolin ACT
seconds 74 – 137 (PREWRM) 74 – 137 (PREWRM)
50 - 1000
82 – 152 (NONWRM) 82 – 152 (NONWRM)
Troponin I/cTnI
Prothrombin
ng/mL (µg/L) 0.00 – 0.03** 0.00 –50.00
INR 0.9-8.0#
##
Time/PT
*Calculated values.
#Performance characteristics have not been established for INRs above 6.0.
**Represents the 0 – 97.5% range of results. Each facility should establish it’s own reference range using the i-STAT cTnI assay.
##
Performance characteristics have not been established for cTnI values above 35.00 ng/mL.
14
ART: 714446-00C REV. DATE 07/12/04
Page 19

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
Glucose Test Strip
UNIT REFERENCE RANGE REPORTABLE RANGE UNIT OF CONVERSION
mg/dL Fasting: 70 – 105
Two hours after meal: less
than 140
mmol/L Fasting: 3.9 – 5.8
Two hours after meal: less
than 7.8
20 – 600
1.1 – 33.3
mg/dL x 0.0556 = mmol/L
15
ART: 714446-00C REV. DATE 07/12/04
Page 20

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
Critical Results
3
Critical results are test results that fall outside high and low critical limits that define the boundaries of life-threatening values
for a test. Critical results represent an emergency condition and must be reported immediately to the patient’s attending
physician or nurse.
ANALYTE (units) ADULT CHILDREN NEONATES
Sodium (mmol/L)
low high
120 158
low high
121 156
low high
121 156
Potassium (mmol/L) 2.8 6.2 2.8 6.4 2.8 6.5
Chloride (mmol/L) 75 126 77 121 77 121
TCO2 (mmol/L)
11 40 11 39 – –
Ionized Calcium (mmol/L) 0.78 1.58 0.74 1.57 – –
pH 7.21 7.59 7.21 7.59 – –
PCO2 (mmHg)
PO2 (mmHg)
19 67 21 66 – –
43 – 45 124 37 92
BUN (mg/dL) – 104 – 55 – 55
Glucose (mg/dL) 46 484 46 445 32 328
Creatinine – 7.4 – 3.8 – –
Lactate
Hematocrit (%PCV) 18 61 20 62 33 71
Celite ACT
PT/INR
Kaolin ACT
Troponin I/cTnI
16
ART: 714446-00C REV. DATE 07/12/04
Page 21

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
Interferences
An interferent is a substance which, if present at significant levels in the blood specimen being analyzed, will produce an
error in the result of the analyte being measured. For example, in the table below, β-hydroxybutyrate at sample concentration
level of 16 mmol/L would decrease the measured sodium by 5 mmol/L.
ANALYTE INTERFERENT INTERFERENT CONCENTRATION EFFECT ON ANALYTE RESULT
Sodium β-hydroxybutyrate
Lactate
Bromide
Chloride β-hydroxybutyrate
Bromide
Lactate
Salicylate
Thiocyanate
Ionized Calcium Magnesium
β-hydroxybutyrate
Lactate
Salicylate
Glucose
(Cartridge)
Bromide
pH
16 mmol/L (166 mg/dL)
20 mmol/L
37.5 mmol/L
16 mmol/L (166 mg/dL)
12.5 mmol/L (100 mg/dL)
11 mmol/L (100 mg/dL)
4 mmol/L
24 mmol/L (140 mg/dL)
1.0 mmol/L above normal
20 mmol/L
20 mmol/L
4.34 mmol/L
37.5 mmol/L (300 mg/dL)
pH: per 0.1 pH units below 7.4 @ 37°C
pH: per 0.1 pH units above 7.4 @ 37°C
Decrease (↓) Na by 5 mmol/L
Decrease (↓) Na by 5 mmol/L
Increase (↑) Na by 5 mmol/L
Increase (↑) Cl by 3 mmol/L
Increase (↑) Cl by 30 mmol/L
Increase (↑) Cl by 3.5 mmol/L
Increase (↑) Cl by 5 mmol/L
May cause results to be suppressed (***)
Increase (↑) iCa by 0.04 mmol/L
Decrease (↓) iCa by 0.1 mmol/L
Decrease (↓) iCa by 0.05 mmol/L
Decrease (↓) iCa by 0.1 mmol/L
Decrease (↓) glucose by 30 mg/dL
Decrease (↓) glucose by 0.9 mg/dL (0.05
mmol/L)
Increase (↑) glucose by 0.8 mg/dL (0.04
mmol/L)
Oxygen
Hydroxyurea
Thiocyanate
Glucose
(Precision PCx
Test Strip)
Glucose
(Precision PCx
Plus Test Strip)
BUN/Urea Thiocyanate 24 mmol/L (140 mg/dL) Decrease (↓) urea by approx. 21%
Lactate
(continued on next
page)
Hematocrit
Acetominophen
See package insert
for full details.
Bromide
Cysteine
Hydroxyurea
less than 20 mmHg @ 37°C
PO
2
100 µmol/L
24 mmol/L (140 mg/dL)
<20%PCV
>70%
>100 µg/mL
25 mmol/L (200 mg/dL)
6.4 mmol/L (101 mg/dL)
100 µmol/L
May decrease (↓) glucose
Increase (↑) glucose 8 mg/dL (0.44
mmol/L)
Decrease (↓) glucose by approx. 23%
Increase (↑) glucose
Decrease (↓) glucose
Decrease (↓) glucose
Decrease (↓) lactate by 40%
Decrease (↓) lactate by 11%
Increase (↑) lactate 1.44 mg/dL (0.16
mmol/L)
17
ART: 714446-00C REV. DATE 07/12/04
Page 22

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
ANALYTE INTERFERENT INTERFERENT CONCENTRATION EFFECT ON ANALYTE RESULT
Glycolic Acid 10 mmol/L Increase (↑) lactate by approx. 1.96 mmol/L
from an initial Lactate concentration of 1.45
mmol/L
Creatinine
Acetaminophen
Ascorbate
Bromide
<2 mg/dL
PCO
2
>2 mg/dL
PCO
2
Hydroxyurea
Creatine
N-acetylcysteine
Hematocrit White Blood Count
(WBC)
Total Protein
Lipids
For every 1 mmol/L acetaminophen
0.227 mmol/L
12.5 mmol/L (100 mg/dL)
Above 40 mmHg
Below 40 mmHg
Above 40 mmHg
Below 40 mmHg
100 µmol/L
5 mg/dL creatine
16.6 mmol/L
Greater than 50,000 WBC/µL
For measured Hct<40%
For each g/dL below 6.5
For each g/dL above 8.0
For measured Hct≥40%
For each g/dL below 6.5
For each g/dL above 8.0
Abnormally high
Increase (↑) creatinine by 0.25 mg/dL
Increase (↑) creatinine by 0.7 mg/dL
Increase (↑) creatinine by 0.8 mg/dL
(71 µmol/L) from an initial Creatinine
concentration of 1.0 mg/dL (88 µmol/L)
Increase (↑) creatinine by 6.9% per 10
mmHg PCO
2
Decrease (↓) creatinine by 6.9% per 10
mmHg PCO
2
Decrease (↓) creatinine by 3.7% per 10
mmHg PCO
2
Increase (↑) creatinine by 3.7% per 10
mmHg PCO2
Increase (↑) 1.85 mg/dL (164 µmol/L)
Increase (↑) creatinine by 0.20 mg/dL
Increase (↑) creatinine by 0.4 mg/dL
May Increase (↑) hematocrit
Decrease (↓) Hct by 1% PCV
Increase (↑) Hct by 1% PCV
Decrease (↓) Hct by 0.75% PCV
Increase (↑) Hct by 0.75% PCV
Increase (↑) Hct
Celite ACT Aprotinin Falsely extends Celite ACT times
PCO
2
Propofol (Diprovan®)
Thiopental Sodium
For patients administered propofol or
thiopental sodium, i-STAT recommends the
use of G3+, CG4+, CG8+, EG6+, and
EG7+ cartridges, which are free from
clinically significant interference at all
relevant therapeutic doses. i-STAT does
not recommend the use of EC8+ cartridges
for patients receiving propofol or thiopental
sodium.
Diprivan is a registered trademark of the AstraZeneca group of companies.
18
ART: 714446-00C REV. DATE 07/12/04
Page 23

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
QUALITY CONTROL
Daily Procedures
Analyzer Verification
Verify the performance of each handheld analyzer or Blood Analysis Module in the i-STAT System using the internal or
external Electronic Simulator every 24 hours of use, or as needed for regulatory compliance. In the USA, verification is
required every 8 hours for blood gases, hematocrit, ACT, PT/INR, and cTnI.
Action:
If PASS is displayed on the analyzer screen (after using the external Electronic Simulator):
Remove the Electronic Simulator after the LCK or Simulator Locked message disappears from the display
screen.
Transmit the result to the Central Data Station.
Use the analyzer as required.
Note: If the internal Electronic Simulator is used, the “PASS” message will not be displayed on the analyzer
screen. The “PASS” record will appear in the analyzer’s stored results for transmission to the Central Data Station.
Remedial Action:
If FAIL is displayed on the analyzer screen:
Repeat the procedure with the same Electronic Simulator or rerun the cartridge if the internal Electronic
Simulator is being used. If PASS is displayed use the analyzer as required.
If FAIL is displayed repeat the procedure with a different external Electronic Simulator.
If PASS is displayed with the second Electronic Simulator:
Use the analyzer as required.
Deliver the questionable Electronic Simulator to the i-STAT System Coordinator.
If FAIL is displayed with the second Electronic Simulator:
DO NOT analyze patient samples with the analyzer.
Transmit the results to the Central Data Station.
Deliver the faulty analyzer to the i-STAT System Coordinator.
Record the failure in the i-STAT QC Log along with the action taken.
Verification of Cartridge Storage Conditions
Refrigerated Cartridges
Verify that the cartridges stored in the refrigerator are all within the expiration date printed on the boxes.
Deliver any expired cartridges to the i-STAT System Coordinator.
Verify that the refrigerator did not exceed the limits of 2 to 8°C (35 to 46°F).
Document in the i-STAT QC Log.
Action:
If the temperature of the cartridge storage refrigerator is within the range of 2 to 8°C (35 to 46°F) use
cartridges as required.
Remedial Action:
If the temperature is outside the range of 2 to 8°C (35 to 46°F), quarantine the cartridges in the storage
refrigerator. Notify the i-STAT System Coordinator immediately. DO NOT USE the cartridges from this
refrigerator. Record the QC failure in the i-STAT QC Log along with the action taken.
19
ART: 714446-00C REV. DATE 07/12/04
Page 24

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
Room Temperature Cartridges
Verify that all boxes of cartridges at room temperature have been out of the refrigerator less than two weeks.
Deliver any expired cartridges to the i-STAT System Coordinator.
Verify that room temperature has not exceeded 30 °C.
Document in the i-STAT QC log.
Action:
If the measured temperature of the room has been continuously below 30°C (86°F) use cartridges as required.
Remedial Action:
If the measured room temperature has exceeded 30°C (86°F) for any period of time:
Quarantine the cartridges.
Notify the i-STAT System Coordinator immediately.
DO NOT USE the cartridges.
Record the out-of-control event in the i-STAT QC Log and the action taken.
Verification of Glucose Test Strip
Two levels, usually the Low and High Controls, are tested daily.
1. Press the
(On/Off) key to turn the analyzer on.
2. Press 3 for PCx Glucose Strip.
3. Press 1 for Patient.
4. Scan or enter operator ID. Repeat if prompted.
5. Scan or enter patient ID. Repeat if prompted.
6. Scan or enter test strip lot number.
7. Press 1 for Arterial/Capillary or 2 for Venous sample if prompted.
8. Open foil packet, remove test strip and insert into analyzer test strip port with black contact bars facing up and forward.
9. Apply drop of blood to target area of test strip. Cover the entire area. Do not touch the test strip after sample is applied.
(If test fails to start after second drop applied or if more than 30 seconds have passed, discard test strip and repeat the
test.)
10. Enter chart page information if applicable.
11. View results on analyzer’s display.
12. Enter Comment Code if applicable.
13. Remove and discard test strip.
a. Do not handle test strip with wet or dirty hands.
b. Do not scan the barcode of another test strip.
c. Do not use test strips that are wet, scratched or damaged in any way.
d. Do not re-use test strips.
Action:
If the results are PASS, use the test strips as needed.
Remedial Action:
If the result is outside the acceptable range:
Check that the correct lot numbers for control and test strip were scanned.
Check storage conditions and that bottle has not been opened for more than 90 days.
Use a new test strip. If results are in range, continue to use the test strips. If not, do not use the strips from this lot and
notify the i-STAT System Coordinator.
20
ART: 714446-00C REV. DATE 07/12/04
Page 25

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
Monthly Procedures
Print Electronic Simulator Results
Print a copy of the Electronic Simulator results from the Central Data Station. Include the report in the i-STAT QC Log.
CDS version lower than 5: Click on System and Electronic Simulator.
CDS version 5 and above: Click on the Simulator Viewer.
Print Control Fluid Analysis Results
Print results for any control fluids analyzed from the Central Data Station. Include the report in the i-STAT QC Log.
CDS version lower than 5: Use the Trend function.
CDS version 5 and above: Click on the Control Results Viewer.
Periodic Procedures for Cartridges
For acceptance of newly received cartridge lots, check the Temperature Monitor and perform integrity testing.
Check Temperature Monitor
i-STAT cartridges are shipped refrigerated with a four-window indicator to monitor temperature during transit.
Action:
Fill out the record of receipt and forward materials to refrigerator.
If all windows are white or if only the A windows is blue or the 1 window is red, then transit temperatures were
satisfactory and the cartridges can be used.
Remedial Action:
If the B window is blue or the 2 window is red, contact the i-STAT System Coordinator before using cartridges.
If the C or D windows are blue, or the 3 or 4 windows are red:
Quarantine the suspect cartons.
Notify the i-STAT System Coordinator immediately.
DO NOT USE cartridges from the suspect cartons.
Record the out-of-control event in the i-STAT QC Log.
Integrity Testing
From each lot of blood gas/chemistry cartridges received, use a representational number of cartridges to analyze i-STAT
Level 1 and 3 Controls. If hematocrit is included, analyze Meter Trax Low and High Controls. For ACT cartridges,
analyze i-STAT Level 1 and Level 2 ACT Controls. For PT/INR cartridges, analyze i-STAT Level 1 and Level 2 PT
Controls. For cTnI cartridges, analyze i-STAT Level 1 and Level 3 Cardiac Marker Controls. Use any verified analyzer
for control testing. Transmit the results to the Central Data Station. Use the expected values p ublished in the pack age
inserts to verify the integrity of the cartridges.
Procedure for testing cartridges with i-STAT Level 1 and Level 3 Controls:
1. Prior to testing cartridges that measure PO2, ampules should stand at room temperature a minimum of 4 hours before
use. When testing other cartridges (G, Crea, E3+, EC4+, 6+ or EC8+), ampules may be used once the fluid has
reached room temperature, approximately 30 minutes for individual ampules. For best results, ampules, cartridges, and
analyzers should be at the same temperature. When using cartridges that contain sensors for measuring ionized
calcium, pH, PCO
, or PO2 (G3+, EG6+, EG7+, CG8+, or EC8+), a separate ampule must be used for each cartridge
2
being tested; if these sensors are not present (i.e., the 6+ cartridge), the conten ts of one ampule may be used to fill
more than one cartridge as long as the cartridges are filled and inserted into an analyzer within 10 minutes of opening
the ampule.
2. Immediately before use, shake the ampule vigorously for 5 to 10 seconds to equilibrate the liquid and gas phases. To
shake, hold the ampule at the tip and bottom with forefinger and thumb to minimize increasing the temperature of the
21
ART: 714446-00C REV. DATE 07/12/04
Page 26

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
solution. If necessary, tap the tip of the ampule to send solution back into the bottom section of the ampule. Protect
fingers with gauze, tissue, or glove, or use an ampule breaker to snap off the tip of the ampule at the neck.
3. Immediately transfer the solution from the ampule into a plain capillary tube or plain syringe, and then immediately
transfer the solution into a cartridge. Immediately seal the cartridge and insert it into an analyzer. It is important not to
expose the solution to room air since this will alter the results.
When using a capillary tube, fill from the bottom of the ampule. Avoid drawing solution from the surface by
covering the far end of the tube as it is inserted into the ampule. Once the open end of the tube rests at the bottom
of the ampule, uncover the other end to allow filling by capillary action.
When using a syringe (1cc or 3cc syringes with 16 to 20 gauge needles are recommended), slowly draw
approximately 1mL of solution from the bottom of the ampule. If air is trapped between the leading edge of the
solution and the plunger, do not invert the syringe to expel it; this will not affect solution near the tip of the
syringe. If air bubbles are continually drawn into the syringe, or if a bubble is trapped near the tip of the syringe,
discard the ampule and syringe and use a fresh ampule and syringe. Expel one or two drops from the syringe
before filling the cartridge.
Do not use solution left in the syringe, ampule, or capillary tube for additional testing of the cartridges that
contain sensors for ionized calcium, pH, PCO
, or PO2. However, cartridges without these sensors may be tested
2
with remaining fluids if within 10 minutes of opening the ampule.
4. Compare results to the package insert values. Check that the lot number on the control ampule matches the lot number
on the package insert and that the software version listed on the insert matches the software installed in the analyzer. If
all results are within expected ranges, use the cartridges as needed. Transmit the results to the Central Data Statio n.
Procedure for testing cartridges with Hematronix Meter Trax Controls for hematocrit
1. Warm Meter Trax to room temperature, 18 - 30°C (64 -86°F).
2. Roll the vials upright in the palms several times, then invert the vials and repeat rolling in the palms several times.
Continue inverting and mixing the vials for 2-3 minutes. Verify the uniform mixing of the vials by checking for
clumping on the sides and bottom of the vials. If clumping is present, continue to roll the vials until all clumps are
gone. If clumping remains after 5 minutes, discard the vial.
3. Fill and seal a cartridge and insert immediately into the analyzer. Note: The Control option from the Quality Tests
menu must be used on the i-STAT1 Analyzer for Meter Trax controls.
4. After completion of testing, wipe the rim of the cap of the vial with a lint-free wipe, recap and return to the refrigerator.
5. Compare results to the package insert values. If results are within the expected ranges, use the cartridges as needed.
Transmit results to the Central Data Station.
Remedial Action:
If any results are outside the published expected ranges:
DO NOT USE cartridges from the suspect lot.
Quarantine the suspect lot.
Notify the i-STAT System Coordinator immediately.
Record the QC failure in the i-STAT QC Action Log along with the action taken.
Procedure for testing cartridges with i-STAT Level 1 and Level 2 ACT or PT/INR Controls
1. Prior to use, allow one vial each of the lyophilized plasma and calcium chloride reconstituting fluid to stand at room
temperature for a minimum of 45 minutes.
2. Remove the cap and stopper from the vials and pour the entire contents of the calcium chloride vial into the
lyophilized plasma vial. Place the stopper back on the reconstituted vial.
3. Allow the vial to sit for 1 minute and then mix the contents by swirling gently for 1 minute, then inverting slowly for
30 seconds.
4. Use a plastic pipette, syringe, or capillary tube without anticoagulant to transfer the solution to an ACT cartridge.
22
ART: 714446-00C REV. DATE 07/12/04
Page 27

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
5. Immediately seal the cartridge and insert it into an analyzer. This process mu st be completed within 30 seconds of the
complete reconstitution of the control sample.
6. Compare results to the package insert values. If results are within the expected ranges, use the cartridges as needed.
Transmit results to the Central Data Station.
Remedial Action:
If any results are outside the published expected ranges:
DO NOT USE cartridges from the suspect lot.
Quarantine the suspect lot.
Notify the i-STAT System Coordinator immediately.
Record the QC failure in the i-STAT QC Action Log along with the action taken.
Procedure for testing
cTnI cartridges, analyze i-STAT Level 1, 2, or 3 Cardiac Marker Controls:
1. Remove vial from freezer and thaw at room temperature (18-30ºC) for 15 minutes.
2. Thoroughly mix by gently swirling the bottle. Avoid foaming of the sample.
3. Dispense a drop of sample directly from the vial into the i-STAT cTnI cartridge and seal the cartridge. If sh ort-term
storage (<4 hrs) is desired, tightly recap the bottle immediately, and store at 2-8ºC.
4. Insert cartridge into an i-STAT 1 Analyzer.
Target Values and Ranges: See value assignment sheet accompanying the control or calibration verification material.
The value assignment sheet displays target values and ranges expected when materials and equipment are performing
properly. Should results fall outside the range, refer to the System Manual.
Always ensure that the lot number and software revision on the value assignment sheet matches the lot number of the vial
in use and the software revision in the analyzer.
Target values are specific to the i-STAT System. Results may differ if used with other methods (i.e., other IVD
instrumentation).
Always remember to analyze the control material in the Control pathway and the calibration verification material in the
Cal Ver pathway under the Quality Tests option of the i-STAT 1 Analyzer Administration Menu.
Remedial Action:
If any results are outside the published expected ranges:
DO NOT USE cartridges from the suspect lot.
Quarantine the suspect lot.
Notify the i-STAT System Coordinator immediately.
Record the QC failure in the i-STAT QC Action Log along with the action taken.
Periodic Procedures for Glucose Test Strips
Two levels, usually the Low and High Controls, are tested:
When a new lot of test strips is opened.
When diabetes medication plan is adjusted.
When the strips have been exposed to temperatures outside the storage conditions (4-30°C, 39-86 °F).
CALIBRATION
For cartridges, calibration is automatically performed as part of the test cycle on each cartridge type, except coagulation and
immunoassay cartridges. Operator intervention is not necessary.
23
ART: 714446-00C REV. DATE 07/12/04
Page 28

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
For glucose test strips, lot-specific calibration information is encoded in the test strip barcode label.
CLINICAL SIGNIFICANCE
Analyte Some Causes of
Increased Values
Sodium
Potassium
Chloride
Dehydration
Diabetes insipidus
Salt poisoning
Skin losses
Hyperaldosteronism
CNS disorders
Renal glomerular disease
Adrenocortical insufficiency
Diabetic Ketoacidosis (DKA)
Sepsis
In vitro hemolysis
Prolonged diarrhea
Renal tubular disease
Hyperparathyroidism
Dehydration
Some Causes of
Decreased Values
Dilutional hyponatremia
(cirrhosis)
Depletional hyponatremia
Syndrome of inappropriate
ADH
Renal tubular disease
Hyperaldosteronism
Treatment of DKA
Hyperinsulinism
Metabolic alkalosis
Diuretic therapy
Prolonged vomiting
Burns
Salt-losing renal disease
Overhydration
Thiazide therapy
Ionized
Calcium
BUN
Glucose
Dehydration
Hyperparathyroidism
Malignancies
Immobilization
Thiazide diuretics
Vitamin D intoxication
Impaired renal function
Prerenal azotemia (e.g. shock)
Postrenal azotemia
GI bleeding
High protein diet
Diabetes mellitus
Pancreatitis
Endocrine disorders (e.g. Cushing’s syndrome)
Drugs (e.g. steroids, thyrotoxicosis)
Chronic renal failure
Stress
IV glucose infusion
Hypoparathyroidism
Early neonatal hypocalcemia
Chronic renal disease
Pancreatitis
Massive blood transfusions
Severe malnutrition
Pregnancy
Severe liver insufficiency
Overhydration
Malnutrition
Insulinoma
Adrenocortical insufficiency
Hypopituitarism/Massive liver
disease
Ethanol ingestion/Reactive
hypoglycemia
Glycogen storage disease
24
ART: 714446-00C REV. DATE 07/12/04
Page 29

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
Analyte Some Causes of
Increased Values
Creatinine
Lactate
pH
PCO
2
Impaired renal function
Hypoxia (shock, hypovolumia, left ventricular failure); diabetes mellitus,
neoplasia, liver disease; drug or toxins (ethanol, methanol, salicylates);
glycolic acid as a product of ethylene glycol metabolism
Respiratory alkalosis
Metabolic alkalosis
Acute Respiratory Acidosis:
• Depression of respiratory center
• Suppressed neuromuscular system
• Pulmonary disorders
• Inadequate mechanical ventilation
Chronic respiratory acidosis
• Decreased alveolar ventilation
• Hypoventilation
Compensation in metabolic alkalosis
Some Causes of
Decreased Values
Respiratory acidosis
Metabolic acidosis
Respiratory alkalosis:
• Increased stimulation of
respirator center
• Hypermetabolic states
• Mechanical
hyperventilation
Compensation in metabolic
acidosis
PO
2
HCO
3
Hematocrit
ACT Celite
Breathing oxygen-enriched air Carbon-monoxide exposure
Pulmonary disorders
Myocardial infarction
Congestive heart failure
Primary metabolic alkalosis
Primary respiratory acidosis
Dehydration
Burns
Impaired ventilation
Renal disorders
Administration of heparin for medical or surgical procedures.
Primary metabolic acidosis
Primary respiratory alkalosis
Hemolytic anemias
Iron deficiency
Marrow depression
Blood loss
Administration of aprotinin.
25
ART: 714446-00C REV. DATE 07/12/04
Page 30

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
Analyte Some Causes of
Increased Values
PT/INR
ACT Kaolin
cTnI
Administration of oral anticoagulant therapy.
Administration of heparin for medical or surgical procedures.
Trauma
Congestive heart failure.
Post-operative non cardiac surgery patients.
Drug toxicity, e.g. adriamycin.
Coronary Vasospasm
Inflammatory diseases e.g. myocarditis.
Post Percutaneous Coronary Intervention (PCI).
Pulmonary Embolism
Sepsis
Infiltrative diseases including amyloidosis, hemachromatosis,
sarcoidosis, and scleroderma.
Some Causes of
Decreased Values
26
ART: 714446-00C REV. DATE 07/12/04
Page 31

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
PRINCIPLES OF MEASUREMENT
Sodium, Potassium, Chloride, Ionized Calcium, pH, and PCO
are measured by ion-selective electrode potentiometry. Concentrations are calculated from the measured potential
through the Nernst equation.
Urea
is first hydrolyzed to ammonium ions in a reaction catalyzed by the enzyme urease. The ammonium ions are
measured by an ion-selective electrode and the concentration is calculated from the measured potential through the
Nernst equation.
Glucose
is measured amperometrically. Oxidation of glucose, catalyzed by the enzyme glucose oxidase, produces hydrogen
peroxide. The liberated hydrogen peroxide is oxidized at an electrode to produce an electric current which is
proportional to the glucose concentration
.
Creatinine
is hydrolyzed to creatine in a reaction catalyzed by the enzyme creatinine amidohydrolase. Creatine is then hydrolyzed
to sarcosine in a reaction catalyzed by the enzyme creatine amidinohydrolase. The oxidation of sarcosine, catalyzed by
the enzyme sarcosine oxidase, produces hydrogen peroxide. The liberated hydrogen peroxide is oxidized at the platinum
electrode to produce a current which is proportional to the creatinine concentration
2
.
Lactate
is measured amperometrically. The enzyme lactate oxidase, immobilized in the lactate biosensor, selectively converts
lactate to pyruvate and hydrogen peroxide. The liberated hydrogen peroxide is oxidized at the platinum electrode to
produce a current which is proportional to the sample concentration.
PO
2
is measured amperometrically. The oxygen sensor is similar to a conventional Clark electrode. Oxygen permeates
through a gas permeable membrane from the blood sample into an internal electrolyte solution where it is reduced at the
cathode. The oxygen reduction current is proportional to the dissolved oxygen concentration.
Hematocrit
is determined conductometrically. The measured conductivity, after correction for electrolyte concentration, is
inversely related to the hematocrit.
ACT
is determined amperometrically. The conversion of a thrombin substrate is initiated by mixing a whole blood sample
(without anticoagulant) with a particulate clotting activator – either Celite® brand diatomaceous earth or kaolin. The
substrate used in the electrogenic assay has an amide linkage that mimics the thrombin-cleaved amide linkage in
fibrinogen. The product of the thrombin-substrate reaction is the electroactive compound that is detected
amperometrically. The time of detection is measured in seconds and the result is reported as a whole blood time (WBT).
Glucose Test Strip
is determined amperometrically. Each strip includes an electrode containing the enzyme glucose oxidase (Precision
PCx) or glucose dehydrogenase (PCx Plus). When a drop of blood is applied to the target area of the test strip, the
glucose oxidase or dehydrogenase catalyzes the oxidation of glucose in the drop to produce gluconic acid. During the
reaction, electrons are transferred by an electrochemical mediator to the electrode surface. This generates a current that
is measured by the system. The size of the current generated is proportional to the amount of glucose present in the
blood drop.
27
ART: 714446-00C REV. DATE 07/12/04
Page 32

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
PT/INR
is determined amperometrically. The conversion of a thrombin substrate is initiated by mixing a whole blood sample
(without anticoagulant) with tissue thromboplastin. The substrate used in the electrogenic assay has as amide linkage
that mimics the thrombin–cleaved amide linkage in fibrinogen. The product of the thrombin–substrate reaction is the
electroactive compound that is detected amperometrically. The time of detection is measured in seconds and reported as
INR and/or seconds.
Tropononin I/cTnI
is determined amperometrically using a two-site ELISA method. Antibodies specific for human cardiac troponin I
(cTnI) are located on an electrochemical sensor fabricated on a silicon chip. Also deposited in another location on the
sensor silicon chip is an antibody/alkaline phosphatase enzyme conjugate specific to a separate portion of the cTnI
molecule. The whole blood or plasma sample is brought into contact with the sensors allowing the enzyme conjugate to
dissolve into the sample. The cTnI within the sample becomes labeled with alkaline phosphatase and is captured onto
the surface of the electrochemical sensor during an incubation period of approximately seven minutes. The sample, as
well as excess enzyme conjugate, is washed off the sensors. Within the wash fluid is a substrate for the alkaline
phosphatase enzyme. The enzyme bound to the antibody/antigen/antibody sandwich cleaves the substrate releasing an
electrochemically detectable product. The electrochemical (amperometric) sensor measures this enzyme product which
is proportional to the concentration of cTnI within the sample.
FOOTNOTES
1. Statland, B.E., Clinical Decision Levels for Lab Tests. Medical Economics Books, 1987.
2. Tietz, N.W., Tietz Textbook of Clinical Chemistry, third edition, Ed. C.A. Burtis, E.R. Ashwood, W.B. Saunders
Company, Philadelphia, 1999. Table 50 – 20, Appendix.
3. Kost, Gerald J., Using critical limits to improve patient outcome. Medical Laboratory Observer.
March 1993; 25(3): 22–27.
Prepared By:_________________________________________________________ Date: _______________________________________
Adopted: ___________________________________________________________ Date: _______________________________________
Reviewed:___________________________________________________________ Date: _______________________________________
Reviewed:___________________________________________________________ Date: _______________________________________
Reviewed:___________________________________________________________ Date: _______________________________________
Revised: ____________________________________________________________ Date: _______________________________________
28
ART: 714446-00C REV. DATE 07/12/04
Page 33

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
i-STAT QC Log: Incoming QC
Cartridge Type:__________________ Lot No.:__________________ Rec’d Date: ______________ Quant._____________ Temp.Strip_________
Control Name: ___________________ Lot No.: __________________ Level: _____________ Exp. Date: _______________ CLEW: _______________
Test
Range
Results
Results
Control Name: ___________________ Lot No.: __________________ Level: _____________ Exp. Date: _______________ CLEW: _______________
Test
Range
Results
Results
Control Name: ___________________ Lot No.: __________________ Level: _____________ Exp. Date: _______________ CLEW: _______________
Test
Range
Results
Results
Lot/Shipment accepted by: ____________________________________________ Date: ___________________________
i
ART: 714446-00C REV. DATE 07/12/04
Page 34

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
i-STAT QC Action Log
Date Cartridge
Type
Cartridge Lot
No.
Date Rec’d Quantity Test(s) Out of
Range
Corrective Action Inspector
ii
ART: 714446-00C REV. DATE 07/12/04
Page 35

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
i-STAT QC Log: Expiration Date and Storage Conditions: Refrigerated
Date Location Cartridge Type Lot # Exp. Date Quantity Temp. Action Inspector
iii
ART: 714446-00C REV. DATE 07/12/04
Page 36

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
i-STAT QC Log: Expiration Date and Storage Conditions: Room Temperature
Date Location Cartridge Type Lot # Exp. Date Quantity Temp. Action Inspector
iv
ART: 714446-00C REV. DATE 07/12/04
Page 37

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
i-STAT Electronic Simulator Log for Analyzer Serial Number:_______________________ Year:_________________________
Date Time Pass
Fail
Simulator
ID
Operator Time Pass
Fail
Simulator
ID
Operator Time Pass
Fail
Simulator
ID
Operator
v
ART: 714446-00C REV. DATE 07/12/04
Page 38

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
i-STAT Electronic Simulator Action Log
Date Time Analyzer Failure Code
or Letter
Simulator
ID
Action Pass
Fail
Operator
vi
ART: 714446-00C REV. DATE 07/12/04
Page 39

PROCEDURE MANUAL FOR THE i-STAT SYSTEM
i-STAT1 Analyzer PCx and PCx Plus Glucose Test Strip QC Log
Date Time
Control
Level
Control Lot Strip Lot
Pass
Fail
If Fail
Expected Range
Result Action Operator
vii
ART: 714446-00C REV. DATE 07/12/04
 Loading...
Loading...