Abbott 3660, 3661, 3662, 3663, 3665 User Manual
...
Proclaim™ Implantable Pulse Generator
Clinician's Manual
Models 3660, 3661, 3662, 3663, 3665, 3667
CAUTION: Federal (USA) law restricts this device to sale by or on the order of a physician.
State of California to cause cancer and birth defects or other reproductive harm. For more information, go to
www.P65Warnings.ca.gov.
™ Indicates a trademark of the Abbott group of companies.
‡ Indicates a third
Bluetooth and Bluetooth logo are registered trademarks of Bluetooth SIG, Inc.
Pat.
©
WARNING: This product can expose you to chemicals including ethylene oxide, which is known to the
http://www.abbott.com/patents
2020 Abbott. All Rights Reserved.
-party trademark, which is property of its respective owner.

i
Contents
Prescription and Safety Information ........................................................................... 1
Intended Use ....................................................................................................................... 1
Indications for Use ............................................................................................................... 1
Contraindications ................................................................................................................. 1
MRI Safety Information ......................................................................................................... 1
Warnings ............................................................................................................................. 1
Precautions .......................................................................................................................... 3
Adverse Effects .................................................................................................................... 6
Safety and Effectiveness Studies ........................................................................................... 6
System Overview ....................................................................................................... 6
Product Description ................................................................................................... 7
Package Contents ................................................................................................................ 8
Identifying the IPG ............................................................................................................... 8
Directions for Use ...................................................................................................... 8
Creating an IPG Pocket ........................................................................................................ 9
Connecting a Lead or Extension to the IPG ........................................................................... 9
Implanting the IPG ............................................................................................................. 11
Replacing the IPG .............................................................................................................. 12
Disposing of Explanted Components ................................................................................... 12
Checking the Status of the IPG Battery ..................................................................... 12
Technical Support ................................................................................................... 13
Appendix A: Product Specifications ......................................................................... 13
Storage Specifications ........................................................................................................ 13
Product Materials ............................................................................................................... 13
IPG Specifications .............................................................................................................. 14
Compatibility Guidelines for IPGs with Compatible Headers................................................. 15
Appendix B: System Components and Accessories .................................................. 16
IPGs .................................................................................................................................. 16
Programmers and Controllers ............................................................................................. 16
Leads and Extensions ......................................................................................................... 16
Adapters ............................................................................................................................ 17
Trial System ....................................................................................................................... 17
Appendix C: Battery Longevity Information ............................................................... 18
Energy Factors for Tonic Stimulation Parameters ................................................................ 19
Energy Factors for BurstDR™ Stimulation Parameters ........................................................ 23
Battery Longevity Graphs .................................................................................................... 25
Appendix D: Regulatory Statements ......................................................................... 26
Disposal Guidelines for Battery-Powered Devices ................................................................ 26
Statement of FCC Compliance ............................................................................................ 26
Statement of Compliance With License-Exempt RSS Standard (Canada) ............................. 26
Identification Information for Product Registration ............................................................... 27
Wireless Technology Information ........................................................................................ 27
Radio Transmitter, Cables, Transducers ............................................................................. 28
Quality of Service for Wireless Technology .......................................................................... 28
Appendix E: Symbols and Definitions ....................................................................... 30


1
Prescription and Safety Information
Read this section to gather important prescription and safety information.
Intended Use
This neurostimulation system is designed to deliver low-intensity electrical impulses to nerve
structures. The system is intended to be used with leads and associated extensions that are
compatible with the system.
Indications for Use
This neurostimulation system is indicated as an aid in the management of chronic, intractable
pain of the trunk and/or limbs, including unilateral or bilateral pain associated with the following:
failed back surgery syndrome and intractable low back and leg pain.
Contraindications
This system is contraindicated for patients who are unable to operate the system or who have
failed to receive effective pain relief during trial stimulation.
MRI Safety Information
Some models of this system are Magnetic Resonance (MR) Conditional, and patients with these
devices may be scanned safely with magnetic resonance imaging (MRI) when the conditions for
safe scanning are met. For more information about MR Conditional neurostimulation components
and systems, including equipment settings, scanning procedures, and a complete listing of
conditionally approved components, refer to the MRI procedures clinician's manual for
neurostimulation systems (available online at
about MR Conditional products, visit the Abbott Medical product information page at
neuromodulation.abbott/MRI-ready.
medical.abbott/manuals). For more information
Warnings
The following warnings apply to this neurostimulation system.
Poor surgical risks. Neurostimulation should not be used on patients who are poor surgical risks
or patients with multiple illnesses or active general infections.
Magnetic resonance imaging (MRI). Some patients may be implanted with the components that
make up a Magnetic Resonance (MR) Conditional system, which allows them to receive an MRI
scan if all the requirements for the implanted components and for scanning are met. A physician
can help determine if a patient is eligible to receive an MRI scan by following the requirements
provided by Abbott Medical. Physicians should also discuss any risks of MRI with patients.
Patients without an MR Conditional neurostimulation system should not be subjected to MRI
because the electromagnetic field generated by an MRI may damage the device electronics and
induce voltage through the lead that could jolt or shock the patient.
Diathermy therapy. Do not use short-wave diathermy, microwave diathermy, or therapeutic
ultrasound diathermy (all now referred to as diathermy) on patients implanted with a
neurostimulation system. Energy from diathermy can be transferred through the implanted system
and cause tissue damage at the location of the implanted electrodes, resulting in severe injury or
death.

2
Diathermy is further prohibited because it may also damage the neurostimulation system
components. This damage could result in loss of therapy, requiring additional surgery for system
implantation and replacement. Injury or damage can occur during diathermy treatment whether
the neurostimulation system is turned on or off.
Electrosurgery. To avoid harming the patient or damaging the neurostimulation system, do not
use monopolar electrosurgery devices on patients with implanted neurostimulation systems.
Before using an electrosurgery device, place the device in Surgery Mode using the patient
controller app or clinician programmer app. Confirm the neurostimulation system is functioning
correctly after the procedure.
During implant procedures, if electrosurgery devices must be used, take the following actions:
Use bipolar electrosurgery only.
Complete any electrosurgery procedures before connecting the leads or extensions to the
neurostimulator.
Keep the current paths from the electrosurgery device as far from the neurostimulation
system as possible.
Set the electrosurgery device to the lowest possible energy setting.
Confirm that the neurostimulation system is functioning correctly during the implant
procedure and before closing the neurostimulator pocket.
Implanted cardiac systems. Physicians need to be aware of the risk and possible interaction
between a neurostimulation system and an implanted cardiac system, such as a pacemaker or
defibrillator. Electrical pulses from a neurostimulation system may interact with the sensing
operation of an implanted cardiac system, causing the cardiac system to respond inappropriately.
To minimize or prevent the implanted cardiac system from sensing the output of the
neurostimulation system, (1) maximize the distance between the implanted systems; (2) verify
that the neurostimulation system is not interfering with the functions of the implanted cardiac
system; and (3) avoid programming either device in a unipolar mode (using the device’s can as
an anode) or using neurostimulation system settings that interfere with the function of the
implantable cardiac system.
Other active implanted devices. The neurostimulation system may interfere with the normal
operation of another active implanted device, such as a pacemaker, defibrillator, or another type
of neurostimulator. Conversely, the other active implanted device may interfere with the operation
of the neurostimulation system.
Interference with other devices. Some of this system’s electronic equipment, such as the
programmer and controller, can radiate radiofrequency (RF) energy that may interfere with other
electronic devices, including other active implanted devices. Avoid placing equipment
components directly over other electronic devices. To correct the effect of interference with other
devices, turn off the equipment or increase the distance between the equipment and the device
being affected.
Operation of machines, equipment, and vehicles. Patients using therapy that generates
paresthesia should turn off stimulation before operating motorized vehicles, such as automobiles,
or potentially dangerous machinery and equipment because sudden stimulation changes may
distract them from properly operating it. However, current data shows that most patients using
BurstDR™ stimulation therapy do not experience paresthesia. For patients who do not feel
paresthesia, sudden stimulation changes are less likely to occur and distract them while operating
motorized vehicles, machinery, or equipment.

3
Explosive and flammable gases. Do not use a clinician programmer or patient controller in an
environment where explosive or flammable gas fumes or vapors are present. The operation of
these devices could cause them to ignite, causing severe burns, injury, or death.
Keep the device dry. Programmer and controller devices are not waterproof. Keep them dry to
avoid damage. Advise patients to not use their device when engaging in activities that might cause
it to get wet, such as swimming or bathing.
Pediatric use. Safety and effectiveness of neurostimulation for pediatric use have not been
established.
Pregnancy and nursing. Safety and effectiveness of neurostimulation for use during pregnancy
and nursing have not been established.
Device components. The use of components not approved for use by Abbott Medical with this
system may result in damage to the system and increased risk to the patient.
Device modification. Equipment is not serviceable by the customer. To prevent injury or damage
to the system, do not modify the equipment. If needed, return the equipment to Abbott Medical
for service.
Application modification. To prevent unintended stimulation, do not modify the operating system
in any way. Do not use the application if the operating system is compromised (i.e., jailbroken).
Case damage. Do not handle the IPG if the case is pierced or ruptured because severe burns
could result from exposure to battery chemicals.
IPG disposal. Return all explanted IPGs to Abbott Medical for safe disposal. IPGs contain
batteries as well as other potentially hazardous materials. Do not crush, puncture, or burn the IPG
because explosion or fire may result.
Product materials. Neurostimulation systems have materials that come in contact or may come
in contact with tissue. A physician should determine whether or not a patient may have an allergic
reaction to these materials before the system is implanted.
Precautions
The following precautions apply to this neurostimulation system.
General Precautions
Clinician training. Implanting physicians should be experienced in the diagnosis and treatment of
chronic pain syndromes and have undergone surgical and device implantation training.
Patient selection. It is extremely important to select patients appropriately for neurostimulation.
Thorough psychiatric screening should be performed. Patients should not be dependent on drugs
and should be able to operate the neurostimulation system.
Infection. Follow proper infection control procedures. Infections related to system implantation
might require that the device be explanted.
Implantation of two systems. If two systems are implanted, ensure that at least 20 cm (8 in)
separates the implanted IPGs to minimize unintended interaction with other system components.
Implantation of multiple leads. If multiple leads are implanted, leads and extensions should be
routed in close proximity. Nonadjacent leads can possibly create a conduit for stray
electromagnetic energy that could cause the patient unwanted stimulation.
High stimulation outputs. Stimulation at high outputs may cause unpleasant sensations or motor
disturbances, or render the patient incapable of controlling the stimulator. If unpleasant
sensations occur, the device should be turned off immediately.

4
Electromagnetic interference (EMI). Some equipment in home, work, medical, and public
environments can generate EMI that is strong enough to interfere with the operation of a
neurostimulation system or damage system components. Patients should avoid getting too close
to these types of EMI sources, which include the following examples: commercial electrical
equipment (such as arc welders and induction furnaces), communication equipment (such as
microwave transmitters and high-power amateur transmitters), high-voltage power lines,
radiofrequency identification (RFID) devices, and some medical procedures (such as therapeutic
radiation and electromagnetic lithotripsy).
Lead movement. Patients should be instructed to avoid bending, twisting, stretching, and lifting
objects over 2 kg (5 lb) six to eight weeks after implantation of a neurostimulation system.
Extension of the upper torso or neck may cause lead movement and alter the stimulation field
(especially with leads in the cervical area), resulting in overstimulation or ineffective stimulation.
Patient training. Instruct patients to use their neurostimulation system only after an authorized
clinician has programmed the device and has trained the patient how to control stimulation and
safely use the system.
Programmer use. Allow only authorized use of the clinician programmer to avoid any
programming changes that may injure a patient.
Sterilization and Storage
Single-use, sterile device. The implanted components of this neurostimulation system are
intended for a single use only. Sterile components in this kit have been sterilized using ethylene
oxide (EtO) gas before shipment and are supplied in sterile packaging to permit direct introduction
into the sterile field. Do not resterilize or reimplant an explanted system for any reason.
Storage environment. Store components and their packaging where they will not come in contact
with liquids of any kind.
Handling and Implementation
Expiration date. An expiration date (or “use-before” date) is printed on the packaging. Do not use
the system if the use-before date has expired.
Handle the device with care. The clinician programmer and patient controller are sensitive
electronic devices that can be damaged by rough handling, such as dropping them on the
ground.
Care and handling of components. Use extreme care when handling system components prior
to implantation. Excessive heat, excessive traction, excessive bending, excessive twisting, or the
use of sharp instruments may damage and cause failure of the components.
Package or component damage. Do not implant a device if the sterile package or components
show signs of damage, if the sterile seal is ruptured, or if contamination is suspected for any
reason. Return any suspect components to Abbott Medical for evaluation.
Exposure to body fluids or saline. Prior to connection, exposure of the metal contacts, such as
those on the connection end of a lead or extension, to body fluids or saline can lead to corrosion.
If such exposure occurs, clean the affected parts with sterile, deionized water or sterile water for
irrigation, and dry them completely prior to lead connection and implantation.
System testing. To ensure correct operation, always test the system during the implant
procedure, before closing the neurostimulator pocket, and before the patient leaves the surgery
suite.
5
Hospital and Medical Environments
High-output ultrasonics and lithotripsy. The use of high-output devices, such as an
electrohydraulic lithotriptor, may cause damage to the electronic circuitry of an implanted IPG. If
lithotripsy must be used, do not focus the energy near the IPG.
Ultrasonic scanning equipment. The use of ultrasonic scanning equipment may cause
mechanical damage to an implanted neurostimulation system if used directly over the implanted
system.
External defibrillators. The safety of discharge of an external defibrillator on patients with
implanted neurostimulation systems has not been established.
Therapeutic radiation. Therapeutic radiation may damage the electronic circuitry of an implanted
neurostimulation system, although no testing has been done and no definite information on
radiation effects is available. Sources of therapeutic radiation include therapeutic X rays, cobalt
machines, and linear accelerators. If radiation therapy is required, the area over the implanted
IPG should be shielded with lead. Damage to the system may not be immediately detectable.
Home and Occupational Environments
Security, antitheft, and radiofrequency identification (RFID) devices. Some antitheft devices,
such as those used at entrances or exits of department stores, libraries, and other public places,
and airport security screening devices may affect stimulation. Additionally, RFID devices, which
are often used to read identification badges, as well as some tag deactivation devices, such as
those used at payment counters at stores and loan desks at libraries, may also affect stimulation.
Patients who are implanted with nonadjacent multiple leads and patients who are sensitive to low
stimulation thresholds may experience a momentary increase in their perceived stimulation, which
some patients have described as uncomfortable or jolting. Patients should cautiously approach
such devices and should request help to bypass them. If they must go through a gate or doorway
containing this type of device, patients should turn off their IPG and proceed with caution, being
sure to move through the device quickly.
Scuba diving or hyperbaric chambers. Patients should not dive below 30 m (100 ft) of water or
enter hyperbaric chambers above 4.0 atmospheres absolute (ATA). Pressures below 30 m
(100 ft) of water (or above 4.0 ATA) could damage the neurostimulation system. Before diving or
using a hyperbaric chamber, patients should discuss the effects of high pressure with their
physician.
Wireless use restrictions. In some environments, the use of wireless functions (e.g., Bluetooth®
wireless technology) may be restricted. Such restrictions may apply aboard airplanes, near
explosives, or in hazardous locations. If you are unsure of the policy that applies to the use of this
device, please ask for authorization to use it before turning it on.
Mobile phones. While interference with mobile phones is not anticipated, technology continues to
change and interaction between a neurostimulation system and a mobile phone is possible.
Advise patients to contact their physician if they are concerned about their mobile phone
interacting with their neurostimulation system.

6
Adverse Effects
In addition to those risks commonly associated with surgery, the following risks are associated
with using this neurostimulation system:
Unpleasant sensations or motor disturbances, including involuntary movement, caused by
stimulation at high outputs (If either occurs, turn off your IPG immediately.)
Undesirable changes in stimulation, which may be related to cellular changes in tissue
around the electrodes, changes in electrode position, loose electrical connections, or lead
failure
Stimulation in unwanted places (such as radicular stimulation of the chest wall)
Lead migration, causing changes in stimulation or reduced pain relief
Epidural hemorrhage, hematoma, infection, spinal cord compression, or paralysis from
placement of a lead in the epidural space
Cerebrospinal fluid (CSF) leakage
Paralysis, weakness, clumsiness, numbness, or pain below the level of the implant
Persistent pain at the electrode or IPG site
Seroma (mass or swelling) at the IPG site
Allergic or rejection response to implant materials
Implant migration or skin erosion around the implant
Battery failure
Safety and Effectiveness Studies
For information that supports the clinical use of this neurostimulation system, refer to the clinical
summaries manual for spinal cord stimulation (SCS) systems. This neurostimulation system is
similar in technology and intended use to the systems reported in the literature and clinical
studies. Therefore, the literature and clinical studies represent the safety and effectiveness of this
neurostimulation system.
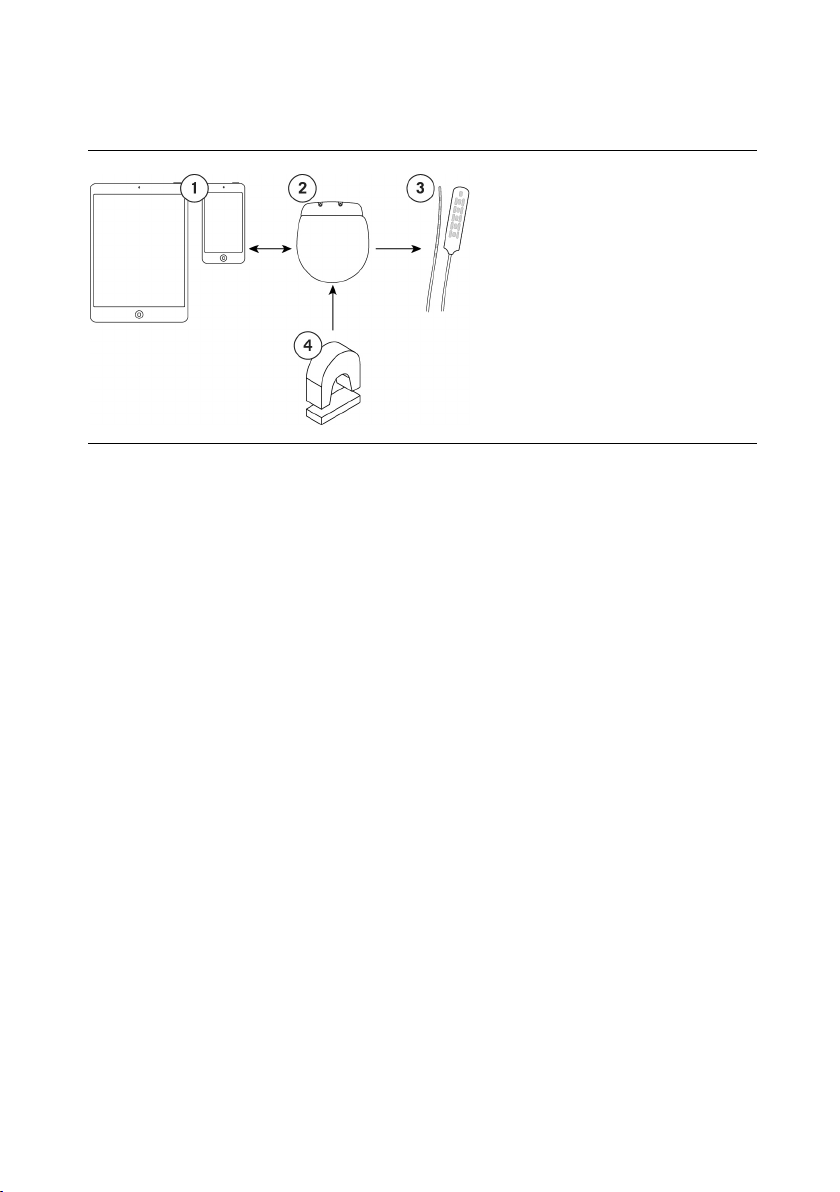
System Overview
This neurostimulation system is designed to deliver electrical stimulation to nerve structures. The
neurostimulation system includes the following main components:
Implantable pulse generator (IPG)
Leads
Clinician programmer
Patient controller
Patient magnet
The IPG delivers electrical pulses through the leads to electrodes near selected nerve fibers in
order to provide therapeutic stimulation. The patient magnet can turn the IPG on and off if the
physician enabled this functionality. Physicians use the clinician programmer to create and
modify programs for a patient. Patients use the patient controller to control their prescribed
programs.
7
The following image shows how the major system components are intended to interact.
Figure 1. Interaction among main system components
1. Clinician programmer or
patient controller
2. IPG
3. Leads
4. Patient magnet
NOTE: This manual provides instructions for implanting the IPG. For instructions for using
other components, see the applicable manuals for those components.
Product Description
This implantable pulse generator (IPG) is an electronic device designed to be connected to one or
more extensions or leads with up to 16 electrodes total. It is powered by a hermetically sealed
battery within a titanium case and uses microelectronic circuitry to generate constant-current
electrical stimulation. The IPG can deliver stimulation with a single program or with multiple
programs. Each program can provide stimulation to a single anatomical area or to multiple areas.
The IPG communicates wirelessly with system programmers and controllers, and IPGs are
available in small and large sizes to accommodate different power needs.
Some models support additional functions:
Upgradeability. Models can receive software upgrades after implantation to provide patients
with additional features as approved by the respective regulatory agencies. To upgrade
features on the IPG, a system programmer is needed.
Compatible header. Models with a compatible header are designed to allow the IPG to
connect to leads or extensions from another manufacturer that meet the compatibility
guidelines (referred to as "IPGs with compatible headers").
For more information about which models provide these additional functions, as well as other IPG
specifications, see the appropriate appendix in this manual.
NOTE: For more information about the neurostimulation system, see the clinician’s
programming manual for this system.
NOTE: In this document, the term "clinician programmer" refers to the St. Jude Medical™
Clinician Programmer device, "patient controller" refers to the St. Jude Medical™ Patient
Controller device, "clinician programmer app" refers to the St. Jude Medical™ Clinician
Programmer software application (app), and "patient controller app" refers to the St. Jude
Medical™ Patient Controller app.
 Loading...
Loading...