
Technique Manual
of
SIGN IM Nail & Interlocking Screw System
Insertion & Extraction Guide
www.sign-post.org
Revision # TM-2011.07.01

451 Hills Street, Suite B, Richland, WA 99354 USA
Phone: (509) 371-1107; Fax: (509) 371-1316
E-mail: signcom@sign-post.org
Web site: www.sign-post.org
Lewis G. Zirkle, M.D.
President & Founder
Dear SIGN Partner:
SIGN implants are made from stainless steel that satisfies ASTM implant-grade material
specifications acceptable to the U.S. FDA. Our orthopaedic hardware manufacturing operation is
being conducted in accordance with national good manufacturing practices and quality assurance
standards. The SIGN IM Nail is a legally distributed device in the United States.
Features of the SIGN nail
Interlocking can be accomplished without C-arm
Stainless steel-less adherence of biofilm than titanium alloy, easier to remove stainless steel
nail than titanium
Solid-stronger with less bending than hollow nails. Less infection as less area for biofilm to
adhere
Slots-allow for compression and distraction of fracture site to accelerate healing
9º bend in proximal nail
1-1/2º bend in distal end for easier insertion
The SIGN Surgical Database was implemented in August 2003 to record SIGN surgeries. We request
that each SIGN surgery be recorded in the database, photos of pre and post op x-rays are requested to
accompany each report. Follow-up x-rays are appreciated. We will answer your questions or
comments in the comment section.
We value your comments on any aspect of SIGN. It is a team effort. We can be reached by e-mail,
fax, or telephone.
The SIGN technique manual is updated frequently. For updates please visit our website at www.sign-
post.org and click on manual, username sign and password 03signtech. Please read this manual
several times before your first SIGN surgery. Refer to it for each step in the OR as you do your first
surgeries.
Sincerely,
Lewis G. Zirkle, M.D.
SIGN Founder & President
2

Index
Page Subject
6 Indication for SIGN Nails
7 Operating room equipment
8 SIGN instruments
10 SIGN Nails
11 Technique for all fractures in all locations
21 Extractor/Compressor
23 Tibia
26 Retrograde approach to femur
30 Antegrade approach to femur
34 Fin nail
36 Humerus
38 Distractor instructions
39 Removal of broken nail
39 Additional notes
41 Data collection sheets
3

FOR THE PERSONAL ATTENTION OF THE OPERATING SURGEON
SIGN STANDARD IM NAILS AND FIN NAILS
DESCRIPTION: SIGN intramedullary rods, fin nails and screws are designed to provide fixation of
tibial, femoral and humeral fractures while they heal.
INFORMATION FOR USE: The surgeon must select the type and size that best meets the patient’s
requirements for close adaptation and firm seating with adequate support.
INDICATIONS: The SIGN IM Nail is indicated for internal fixation of diaphyseal tibial fractures
and distal femur fractures including transverse fractures, oblique and spiral fractures, comminuted
fractures, fractures with bone loss, open fractures, corrective osteotomies, pathologic fractures,
pseudoarthrosis of the tibial shaft, nonunions, malunions and fractures of the proximal femur. The
SIGN Fin nail is indicated for internal fixation of stable fractures in the femur and humerus.
CONTRAINDICATIONS: Active or latent infection. Wounds should be closed and dry.
Osteoporosis, insufficient quantity or quality of bone/soft tissue. Material sensitivity. If suspected,
tests are to be performed prior to implantation. Patients who are unwilling or incapable of following
postoperative care instructions.
WARNINGS: For safe and effective use of this implant, the surgeon must be thoroughly familiar
with the implant, the method of application, instruments, and the recommended surgical technique for
this device. Device breakage or damage can occur when the implant is subjected to increased loading
associated with delayed union, nonunion, or incomplete healing. Improper insertion of the device
during implantation can increase the possibility of loosening and migration. The patient must be
cautioned, preferably in writing, about the use, limitations, and possible adverse effects of this
implant including the possibility of the device failing as a result of loose fixation and/or loosening,
stress, excessive activity, or weight bearing or load bearing, particularly if the implant experiences
increased loads due to delayed union, nonunion, or incomplete healing. The patient must be warned
that failure to follow postoperative care instructions can cause the implant and/or treatment to fail.
PRECAUTIONS: An implant shall never be reused. Previous stresses may have created
imperfections which can lead to device failure. Instruments shall be inspected for wear or damage
prior to usage. Protect implant appliances against scratching and nicking. Such stress concentrations
can lead to failure.
ADVERSE EFFECTS: Fracture of the implant due to excessive activity, prolonged loading upon
the device, incomplete healing, or excessive force exerted on the implant during insertion. Implant
migration and/or loosening. Metal sensitivity or histological or allergic reaction resulting from
implantation of a foreign material. Pain, discomfort, or abnormal sensations due to the presence of an
implant. Nerve damage resulting from surgical trauma. Necrosis of bone or bone resorption.
Necrosis of tissue or inadequate healing may occur with any fracture.
STERILITY: All Implants and Instruments are provided non-sterile. Sterilization must be
performed prior to surgery, using one of the following methods. For a gravity displacement autoclave,
set at 250ºF (121ºC) for 30 min., allow drying time of 45 min. For a prevacuum autoclave, set at
270ºF (132ºC) for 4 min., allow drying time of 30 min. or at 273ºF-279ºF (134ºC to 137ºC) for 3
4

min., allow drying time of 16 min. Please consider your equipment manufacturer’s written
instructions for the specific sterilizer and load configuration being used and current AORN standards
and recommended practices. NOTE: these parameters are for full loads using wrapped sets, rigid
containers and /or peel pouches.
STORAGE INSTRUCTIONS: Store in a cool dry place, and keep away from direct sunlight. Prior
to use, inspect product package for signs of tampering, damage, or water contamination. Use oldest
lots first.
SIGN INSTRUMENTS: SIGN instruments are reusable; however, they have a limited life span.
Prior to and after each use, the instruments must be inspected where applicable for sharpness, wear,
damage, proper cleaning, corrosion and integrity of the connecting mechanisms. Notify SIGN if they
should be replaced. Instrument breakage or damage can occur when an instrument is subjected to
excessive loads, speeds, or dense bone. Striking the cutting surfaces with other metal will cause these
surfaces to become dull.
CLEANING: SIGN instruments and accessories must be thoroughly cleaned before reuse.
Decontamination of reusable instruments should occur immediately after completion of the surgical
procedure. Excess blood or debris should be wiped off to prevent it from drying onto the surface.
Use an enzymatic-cleaning product such as Enzol.
NOTE: Even surgical instruments manufactured from high-grade stainless steel must be dried
thoroughly to prevent rust formation. All devices must be inspected for cleanliness of
surface and joints, proper function, and wear and tear prior to sterilization.
SHARPENING: The drill bits become dull if they are dinged by hitting the nail or other metal.
They should be protected during surgery, cleaning and sterilization. They are also dulled by pushing
drill bits into bone when they are not advancing. The drill bit heats up and becomes dull.
5

INDICATIONS FOR SIGN NAIL
FRACTURE TYPE
a. Closed at time of injury
Fractures that cannot be reduced or lose reduction.
b. Open-acute
Fractures that are Gustilo grade I, II, III a, debrided and closed within 24 hours of injury may
have immediate SIGN nail insertion. Sometimes this time limit is impossible, so we must
study the elapsed time between injury and surgery if antibiotics are given within 6 hours from
injury. If closure is delayed, the surgeon should determine when the SIGN nail is placed at
wound closure.
c. Open-delayed closure
Debrided and covered by skin, muscle or free flap, with no drainage, may have SIGN
nail insertion.
d. Fractures treated by external fixation
Risk of infection is increased if external fixation pins are present for over 10 days but we are
studying this as closure at 10 days may not be indicated.
e. Non-unions
PATIENT PREPARATION
Patient must have no infected areas or injuries that preclude surgery. Patient should be told about
risks, benefits of surgery and agree to insertion of SIGN nail. Please check the patient’s skin the night
before surgery. If possible, washing the patient’s leg should be done the night before. The cast may
be removed for washing.
Check list for the night before surgery
1. Any infections? Where? – Surgery should be postponed.
2. Skin of extremity washed well.
3. Range of motion of knee? – need 60° flexion to do retrograde femur approach.
4. Template X-rays to estimate size of nail, screws.
5. X-rays to be in OR.
6. Check appropriate lab work.
SURGEON PREPARATION
Read the technique manual and /or watch the technique CD. Be contemplative surgeons.
X-RAYS
X-rays should include knee and ankle on the same film to measure the nail. X-rays should be present
in OR during surgery. Look carefully for fracture comminution.
ANTIBIOTICS
Antibiotics are started 1 hour before surgery.
6

OPERATING ROOM EQUIPMENT
Be sure an assortment
of sizes are sterilized.
These materials, which are not part of the SIGN set, should be present in the operating room:
drill; chuck key; mallet; bone holding forceps; knife; forceps; clamps; cautery; suction; towel clips;
needle holders; sutures; retractors, bone reamer, curved awl and periosteal elevator.
All personnel must wear masks, hats, and cover as much skin as possible. Bacteria spread to the
wound on skin cells from people in the operating room. Traffic in the OR should be minimal.
(SIGN) EQUIPMENT NECESSARY FOR USE OF SIGN NAIL:
L-handle
Locking Bolt - (2) one is extra
Target Arm (Long Proximal Target Arm, Distal Target Arm)
Short Target Arm (for use with nails shorter than 280mm)
Distal Cap Screws - (4) two are extra
Shoulder Cap Screw - (2) one is extra
Combination Hex Wrench - (2) one end fits the Locking Bolt, Shoulder Cap Screw and Distal
Cap Screws. The other end fits the interlocking screws.
Cannula
Alignment Pin - (2)
Drill Guides - (2) (one large for large drill bits) (one small for small drill bits)
Drill Bits
o Large (2) (6.3mm) for near cortex
o Small (2) (3.5mm) for both near & far cortex
Screw Caddy and SIGN Interlocking screw assortment
SIGN IM nail assortment
Hex Driver (3.5mm)
Extractor/Compressor Set
o Extractor Rod Connector
o Extractor-Compressor Rod
o Slap Hammer Weight
Slot Finders: Cannulated, Solid and Curved (one of each)
11mm Wrench
Tissue Protector - (2) one is extra (these are reusable)
Depth Gauge
Step Drill
Screw Hole Broach
Care of SIGN Equipment:
It is essential that the equipment be well maintained as described on Page 4. Sometimes during the
surgery the cannula and drill bits become bloody. They should be washed off before the next
interlock, as they may stick due to the close fit. This also applies to the threads of caps screws.
NOTE: Please protect the drill bits, reamers and step drill from striking metal objects during
surgery and cleaning.
7

SIGN Instruments
8

9

SIGN NAILS
A solid nail decreases the risk of
infection. The 9º proximal bend can be
used in tibia, femur and humerus. The
1.5º bend makes canal penetration less
likely during insertion.
Standard Length – Tibia/Femur
Diameter = 8mm, 9mm, 10mm, 11mm and 12mm
Length = 280mm, 300mm, 320mm, 340mm, 360mm, 380mm, 400mm and 420mm
Standard Target Arm
Short Length to be used with the Short Target Arm
Diameter = 8mm, 9mm, 10mm
Length = 220mm, 240mm and 260mm
Short Target Arm for Fin, Hip and Pediatric Nails
10

Technique for fractures in all locations
Fig. 1
Fig. 2
Patient Preparation
Check for open wounds
Check the patient the night before the operation for open wound. Remove cast the night before to
check skin condition. Cancel surgery if open wound is present. Wash the extremity the night before to
decrease skin bacteria.
Antibiotic prophylaxis
Start IV antibiotics 1 hour before surgery. Patients with open fractures should be given antibiotics as
soon after surgery as possible. Antibiotic should be given to patients with closed fractures one hour
prior to incision.
Pre-op scrub for surgeon and patient, Hexachlorophene is best, Betadine is less effective.
Soft tissue evaluation
If the fracture is open, the wound should be debrided, irrigated and evaluated as to whether wound
closure can be done. Factors that must be considered are contamination by virulent bacteria, high
energy vs. low energy trauma, foreign bodies. Virulent bacteria occur from “barnyard injuries” or
areas where bacteria are prevalent. The degree of injury is also determined by the forces that cause the
injury. These forces may destroy large amounts of muscle which leaves a dead space after
debridement. This dead space must be closed before the nail can be inserted. Therefore, the wound
classification is divided into wounds that can be closed without risk of infection, and those that can’t.
Whenever a wound can be closed without risk of infection, a nail can be inserted.
Reduction of closed fracture
Closed reduction can often be accomplished if the fracture is less than
7-10 days old. If closed reduction is attempted, check stability in all
planes prior to the reduction so you can test and compare the stability
after the reamer or nail is inserted. The reamers are passed into both
fragments followed by the nail.
Open reduction is necessary if the fracture is beginning to heal.
Transverse fractures can be reduced after both ends have been freed
from soft tissue. Figure 1 demonstrates one method. Allow the tissues
to slowly elongate during reduction. Figure 2 demonstrates
reduction of oblique fractures. Before reduction is
accomplished, ream both sides of the fracture site. Stop
reaming at the metaphysis.
The reamer should be turned 360º in clockwise direction
both during insertion and removal of the reamer from the
canal. The cutting edges of the reamer are damaged by
reaming counterclockwise or to-fro reaming. Save the bone
in a bone cup. Do not place on a sponge or in saline. Use
gradual distraction and allow time for the tissues to stretch.
11

Technique for use of SIGN Distractor (for full illustrated version see page 38)
Fig. 3
Fig. 4
Free up both ends of the fracture fragments
completely. The fracture fragments should be parallel
when the clamps are applied, figure 3. Once they are
applied, place the clamps through the ends of the
distractor and use the pins to stabilize them.
There is one movable side of the distractor and one
that is immobile. The immobile side of course would
be placed on the fracture fragment that is immobile
such as the proximal fragment of a fractured femur.
Begin ratcheting to distract the fragment. Go slowly
as the quadriceps will be very tight. Stop periodically
to allow the tissues to stretch.
Once the distraction has reached 4 inches, remove the distractor and replace the clamps so that they
are close together. This will put less stress on the
ratchet arm.
Once the clamps have been placed close together,
flex the knee to further stretch the quadriceps
mechanism. Begin the distraction again. If there is
a very tight band in the quadriceps, release it. Be
sure your rotation is proper as you distract the
fragments and they will soon fit together
anatomically, figure 4.
It is important to go slowly so that the tissues can
stretch.
Please give us feedback about the distractor as the
design is an ongoing innovation.
12

Open fractures
Fig. 5
Adequate debridement is essential. The amount of tissue removed is dependent on vascular supply,
muscle damage, and bacterial contamination. Bone fragments that are completely devascularized
must be removed. Dead space must be closed. We must study proper timing of wound closure. If the
wound is cleaned and can be closed, the nail can be inserted. If not, external fixation is necessary. If
bone loss has occurred, consider methyl methacrylate insertion into the bone defect. At 6 weeks
remove the methyl methacrylate but do not disturb the membrane that formed. Place bone graft for
small defects. The membrane formed around the methyl methacrylate is bioactive and will accelerate
bone formation. Bone transport is used for large defects. If there is a large skin defect, consider
closing the wound with flaps. The nail should not be placed until the flaps are covered.
Reaming from bone entrance
Skin incision and location of bony entrance will be described in sections for specific fractures. Use
the reamers to extend the bone entrance hole into the diaphysis. Use the tissue protector to keep the
reamers from touching the skin. Ream until chatter and then select nail diameter 2mm smaller. Over
ream by 4mm for 4cm distal to the entrance hole. This will accommodate the bend in the nail. Apply
counter pressure as reaming becomes more forceful. Save the bone from the flutes of the reamer and
the fluid that comes out of the bone entrance when the reamer is withdrawn in a bone cup. It is best
not to place this bone on a sponge or mix with saline.
If you are unsure that the reamer or nail is in the
canal of the distal fragment, push the reamer or
nail until resistance is encountered. If there is
no resistance, the reamer or nail is not in the
canal. The length of the nail is determined by
placing a blunt reamer down to subchondral
bone and measuring this length in the tibia,
figure 5. The femur length of the nail is
measured by estimation using another reamer.
The reamers are marked at 320mm to help
determine the length of the nail.
Blocking screws can be used to aid in inserting
the nail in proximal and distal fractures of femur and tibia.
13

Nail Preparation
Fig. 8
Fig. 9
Fig. 6
Fig. 7
Assemble the Nail
Insert the locking bolt through the
hollow stem of the L-handle, figure 6.
Align the notches in the nail to the
corresponding protrusions on the stem
tube of the L-handle, figure 6. Be sure
the L-handle rests on the side for
proper interlock.
NOTE: Be sure the locking bolt rests as far down the stem tube as possible, figure 7.
Tighten the bolt into the nail, figure 7. If the locking is
not progressing easily through the L-handle and into
the nail, unscrew the locking bolt and reorient the
locking bolt so that it enters the canal of the nail easily.
Attach target arm
Attach the assembled L-handle and nail to the
proximal target arm using the shoulder cap screw,
figure 8. Place the screw on the preferred side of the
L-handle for interlocking. Push the shoulder cap screw
in and carefully tighten by hand. Use the hex wrench
to secure the target arm to the L-handle. If the
shoulder cap screw does not turn easily, adjust the
junction between the L-handle and the target arm.
Attach distal target arm to proximal target arm
Place the alignment pin through the end hole in the distal target arm and distal slot in the nail, figure 9.
The distal cap screws are now
placed to connect the proximal and
distal target arms. Leave 2 holes
between the two distal cap screws
for stability. Withdraw the
alignment pin so only the tip is in
the slot to check alignment of the
target arm as the distal cap screws
are hand tightened. Use progressive
alternative tightening; tighten one
screw a little and then the other a little at a time, final tightening by hex wrench. Recheck alignment of
alignment pin to the slot.
14

Fig. 10
Pearl: Insert caps screws downwards
The shoulder and distal cap screws are inserted easier if they are inserted in a downward direction so
the target arm is parallel to the floor and the cap screws are perpendicular to the floor. Removal is the
reverse. This avoids stripping the cap screw threads.
Remove the target arm
Remove the target arm from the L-handle,
leaving the L-handle attached to the nail,
figure 10.
15

Nail Insertion
Fig. 13
Fig. 11
Fig. 12
Use the tissue protector to prevent the
nail from touching the skin. Push the
nail into the canal as far as possible.
Many surgeons do not use a mallet to
insert the nail. If you decide to use a
mallet, use small taps and rotate the
nail 10º as it proceeds down the canal,
figure 11. Apply counter pressure to
allow advance. If the nail does not
advance with the small taps, consider
using a smaller diameter nail or
reaming more. Hitting the nail
forcibly will bend the nail and make
interlock more difficult.
Leave the proximal 3mm of the nail above the cortical bone to
provide additional stability. Remember the ring on the stem tube is
3mm above the nail, figure 12.
Distal Interlock
If you follow this technique, distal interlock without C-arm is
successful quickly in approximately 80% of your surgeries. Further
techniques to obtain distal interlock are listed after this technique.
Please send us your ideas.
The distal interlock is done before the proximal interlock so the nail
can be rotated to find the slot in the nail.
Reattach the target arm to the L-handle, figure 13.
Be sure the locking bolt is tight.
Decide whether you will use 1 or 2 interlocking
screws. If one interlocking screw is sufficient, place
the screw in the hole nearest the fracture. Use the
alignment pin to mark the location for the skin
incision. Be sure the skin incision is large enough
to place the cannula and your finger on the bone.
This finger is used to identify the location of the
cannula on the bone. If the cannula is directed by
the target arm so it does not hit the bone, loosen the
distal cap screws and adjust the target arm so the
cannula will direct the hole into the cortex. You
will find slot in nail for interlock by rotation of the
nail. Champher the hole with the screw hole broach
toward the bone.
16

Fig. 14
Fig. 15
Fig. 16
Incise the fascia but use the periosteal elevator
to spread the muscle down to the bone. Insert the
cannula on the bone, figure 14. Use a curved
clamp to remove soft tissue between the cannula
and the bone. Be sure no fascial bands are
pushing the cannula. Tap cannula lightly with a
mallet to secure to the bone.
Insert the small drill guide into the cannula and
use a small drill bit to drill a hole through the near
cortex. Avoid hitting the nail with the drill bit or it
will become dull.
Insert the large drill guide and use the step drill or
large drill bit to enlarge the pilot hole. Be sure the
step drill tip engages the pilot hole, figure 15.
Stop rotating the step drill or drill bit when it stops
suddenly after engaging in the slot of the nail.
Further twisting will break the step drill. If the step
drill does not progress, use the large drill bit.
Insert the solid slot finder through the hole
in the near cortex, figure 16. In hard bone
the screw hole broach inserted through the
cannula must be used to enlarge the hole
to allow the slot finders to enter the canal.
See figure 17 for comparison of screw
hole broach and step drill.
Push the solid slot finder with the flats in
the plane of the target arm. Rotation is not
used to place the slot finder. Push the slot
finder in. If the slot finder engages the slot
in the nail, 10-15º of rotation with a sharp
stop to the rotation will occur. This is the
“SIGN feel.” If the slot finder rotates 360º,
it is not in the slot or stuck in the hole in the cortex. Rotate the nail to orient the slot in the nail
parallel to the hole in the near cortex. If the solid slot finder enters the slot and the “SIGN feel” is felt,
place the cannulated slot finder. Test again for “SIGN feel.”
17

Screw Hole Broach
Step Drill
Fig. 17
Fig. 18
Fig. 19
Sometimes the cannulated slot finder will not proceed
through the hole in the near cortex because it is wider than
the solid slot finder. Use the screw hole broach to enlarge
the hole if this occurs.
If either slot finder does not enter the slot in the nail after
rotation of the nail, remove the target arm; use the
curved slot finder, figure 18, to locate the slot in the nail.
Find the slot in the nail by combination of rotation of the
nail by rotating the L-handle and slight pressure to push in
the curved slot finder. The surgeon should both rotate the
L-handle and manipulate the curved slot finder. Once the
slot in the nail has been discovered by “SIGN feel,” insert
the cannulated slot finder and drill the hole in the far
cortex.
If rotating the cannulated slot finder results in
the “SIGN feel,” place the small drill bit
through the cannulated slot finder to drill a
hole in the far cortex, figure 19.
18

Fig. 21
Fig. 20b
Fig. 20a
Measure the proper length of the screw by
placing the depth gauge through the cannulated
slot finder. Do not bend the depth gauge. The
depth gauge marks the hole. Remove the
cannulated slot finder and measure the depth of
the screw using the cannula and depth gauge,
figures 20a and 20b.
Add 5mm to the measurement so 2 threads can
be inserted through the far hole and the head of
the screw is 3mm prominent on the near cortex.
This will make screw removal much easier
should it be necessary.
Use your gentle tactile sense to determine when the tip is caught on edge of the hole.
Insert the screw through the holes in the cortex and
slot of the nail. Raise the cannula so the screw head
can be visualized in order not to insert the screw too
deeply, figure 21. Rotate the L-handle to be sure the
screw is in the slot after the screw has been inserted.
Compress the fracture as needed after the first
interlocking screw has been placed, see page 21.
19

Tips for interlocking
If either slot finder will not rotate after being placed into the hole in the near cortex, enlarge the hole
with the screw hole broach. Often bone will remain in the hole even though the step drill enters the
slot in the nail.
If the slot finder does not enter the slot in the nail, remove the target arm and use the curved slot
finder. This step is necessary approximately 20% of the time. Place the curved slot finder through the
hole in the near cortex and find the nail by tapping on it. Rotate the nail so the slot in the nail is
parallel with the hole in the cortex. If the curved slot finder partially enters the slot, rotate the nail to
allow it to fully enter the slot. Confirm location of the slot by using the solid slot finder and then the
cannulated slot finder. Once the cannulated slot finder has been placed and confirmed by the “SIGN
feel,” drill the hole in the far cortex. Measure and place the screw.
If the curved slot finder does not enter the slot, check the longitudinal orientation. Be sure the
reduction has not slipped. This will misalign the longitudinal orientation of the hole in the cortex and
slot of the nail. Correct this misalignment and place the slot finder. Check to be sure the nail has not
migrated proximally or distally which will also misalign the hole and slot in the longitudinal plane.
After placing the target arm on the L-handle, sometimes the cannula directs the small drill guide so it
is not in contact with the bone cortex. If this occurs, loosen the distal cap screws and adjust the target
arm so the pilot hole is directed through the cortex. In the femur this occurs in the anterior plane and
in the tibia the posterior plane. Proceed with enlarging the hole in the near cortex and use the curved
slot finder to find the slot in the nail. Sometimes it is necessary to champher the hole with the screw
hole broach to allow slot finder to enter slot in nail. Rotate the nail by rotating L-handle to position
slot in nail parallel with hole in near cortex.
20

EXTRACTION - EXTRACTOR/COMPRESSOR
Locking Bolt
Connector
Fig. 23
Fig. 22
Fig. 24
Fig. 25
If the fracture needs compression, place the extractor-compressor on the locking bolt and
attach the compressor rod with the slap hammer attached. Back slap the fracture.
1. First, make sure the locking bolt is connected tightly to the nail through the
L-handle, figure 22.
2. Place the connector on the locking bolt
by sliding the head of the bolt into the base
of the connector, figure 23.
3. Place the slap
hammer weight on the
connector rod,
figure 24.
4. Attach the connector rod to
the connector. The extractor-compressor
can now be used to extract the nail or
compress the fracture figure, 25.
21

Placement of the second distal interlocking screw
Fig. 26
Hole Slot
Fig. 27
The second distal interlocking screw is used for
additional stability.
Place the alignment pin in the hex of the head of the
screw which has been inserted, figure 26. An
assistant should be assigned to be sure this
alignment pin remains in the hex. Rotate the
L- handle and leave it in the center of the rotation.
The initial incision should be large enough to insert
the second interlocking screw. Use the same
procedure as the first distal interlocking screw.
Proximal interlocking screw fixation
Remove the alignment pin resting in the screw head of a distal interlocking screw. This is not
necessary for the proximal interlocking.
Finding the slot and hole in the proximal nail does not require slot finder. The cannula and small drill
guide are placed through the target arm and the hole is drilled through both near and far cortex. The
hole is enlarged in the near cortex. The depth gauge is used to measure the length of the screw using
the cannula and the proximal interlocking screws are placed. Remember the proximal apertures in the
nail are a slot and a hole, figure 27.
Proximal End of Nail
22

Using SIGN nail in the TIBIA
Fig. 28
Push
proximal
fragment
into flexion.
Fig. 30
Fig. 29
Position of patient for proximal
Proximal tibia fractures can be reduced in the figure 4 position.
Midshaft and distal tibia fractures can be treated
with the knee flexed to 110º using gravity and sterile
bump or triangle, figure 29.
Avoid pressure in the popliteal space, figure 30.
If open reduction is necessary, perform this prior
to the incision for the bone entrance of the nail.
23

Fig. 32
Fig. 31
Fig. 33
Tissue protector
keeps nail off
skin.
Fig. 34
Skin incision
Flex the knee to feel the patella tendon. Make the skin incision in the midportion of the tendon from
the patella to the tibial tubercle. Figures 31 and 32.
Bone entrance
Do not enter the fat pad. A curved awl is used to make the bone entrance. The more proximal the
fracture, the more proximal the entrance hole should be. Direct the awl anteriorly and shape the
entrance hole anteriorly especially in proximal fractures.
Reaming and placement of the nail
Proximal tibia fractures
Use figure 4 position for proximal fractures, figure 33. Push the proximal
fragment into flexion as the curved awl makes the bone entrance and during
reaming and insertion of the nail. Resistance to reaming and nail insertion is
provided by applying countertraction during reduction of the fracture. The
blocking screw may be used if this is unsuccessful. The blocking screw can
be any cortical or
cancellous screw or
even a K wire, figure
34. We use fewer
blocking screws
because flexion of the
proximal fragment
reduces the fracture.
As the fracture site is
approached, the distal
fragment should be
approximated to allow passage of the reamer
and nail. The proximal bend of the nail should
be placed apex posteriorly.
24

Mid and distal tibia fractures
Fig. 36
Fig. 37
Fig. 38
Fig. 35
Use gravity for other fractures. The awl is used to make the entrance
hole. Use the reamers to extend the hole into the diaphysis, figure 35.
Ream until chatter and then select diameter 2mm smaller. If you are
unsure that the nail is in the canal of the distal fragment, push the
reamer until resistance is encountered. If there is no resistance, the nail
is not in the canal. The length of the nail is determined by placing a
blunt reamer down to subchondral bone and measuring this length,
figure 36. The reamers are marked at 320mm to help determine the
length of the nail.
NOTE: See technique used in all approaches, page 11.
Proximal Interlock
Drilling
The target arm should now be firmly attached to the L-Handle. Insert the alignment pin tip to the skin
to mark the location of the skin incision. Make skin incision and clear soft tissue off the bone. Place
the cannula next to bone. Use the cannula, small drill guide and small drill bit to drill a hole through
the near cortex and far cortex, figure 37.
NOTE: The slot finder is not necessary to find
the nail slot for proximal interlock.
Screw insertion
Use the large drill guide and step drill to enlarge
the hole in the near cortex. Determine screw
length with help of the depth gauge. Insert the first
proximal interlocking screw. Retract the cannula
to view the head of the screw so it is not inserted
too deeply.
Remember someday the screw may need to be
removed. Insert the second proximal screw in the
same fashion. Remember the proximal aperture is
a hole and the distal is a slot.
25

Bone entrance
Fig. 1
Fig. 2
Retrograde Approach to FEMUR
SIGN technique that is used in all bones is recorded beginning on page 11.
Indications distal
Fractures in the distal femur should be treated with retrograde approach. This is surgeon preference. If
manipulation of the knee is done after the nail insertion and interlocking and range of motion
exercises follow postoperatively, full range of motion usually is achieved and maintained.
Position of the patient
Supine position with a sterile bump or triangle under the knee. 60º of knee flexion is desirable. Knee
extension and flexion allows better visualization of the femoral shaft.
Reduction of the closed fracture
Closed reduction can be done without C-arm in fresh fractures. Open reduction is accomplished by
the mini incision technique dissecting through the muscle fibers without cutting them.
Skin incision
Some surgeons make a medial parapatellar incision
for larger exposure. The median parapatellar
attachments can be released and the patella subluxed
slightly. This allows visualization of the femoral
notch. After more experience, the surgeon makes the
incision through the patellar tendon. This is done by
flexing the knee so the patellar tendon can be
palpated, incising the patellar tendon and removing a
window in the fat pad to see the medial aspect of the
femoral notch. See figure 32 in the tibia section on
page 24.
Bone entrance
Use curved awl to make entrance hole in the
medial aspect of the femoral notch above the
posterior cruciate ligament at junction of
articular surface, figure 1.
If the entrance is placed too far posteriorly, the
posterior cruciate blood supply will be
compromised. The patella does not articulate
with the articular surface in the area of the
entrance hole, figure 2. Stabilize the distal
femoral fragment as the bony entrance and
reaming take place. Look at the fracture site to
see the direction of the awl and subsequent
reamers.
26

Reaming
Fig. 3
High
stress
area
Fig. 4
Introduce the reamers after the bone entrance has been made using the awl. The reamers are rotated
360º in a clockwise manner. This is important to preserve the cutting edges which go only one way.
Look at the distal femur fragment if the fracture site is exposed to direct the reamer. Save the bone
from the flutes of the reamer in a bone cup for use as a bone graft. Do not place in sponge or saline.
Diameter of the nail is determined by noting the size of the reamer that creates chatter in the isthmus
of the femoral canal. Use a nail whose diameter is 2mm smaller than the reamer that created the
chatter.
Nail insertion
The bend of the nail is angled apex
anteriorly. The nail should not end at or
less than 6cm below the lesser trochanter,
figure 3. The nail may end short of this
high stress area or extend past it. We are
studying benefits of each length.
Stop advancing the nail when the ring
touches the articular cartilage on the medial
femoral condyle, figure 4. Check the
tightness of the locking bolt to the nail. The
nail should be inserted so the ring rests on
the articular surface of the medial femoral
condyle. The nail will then be just below the
articular surface, figure 4.
27

Distal interlock
Fig. 6
Fig. 5
Fig. 8
Fig. 7
The final location of the slots in the
distal nail depends on the curve of
the femur and the force necessary to
insert the nail. SIGN nail is a
straight nail. If it is inserted into the
canal without a great deal of force, it
will end up in the anterior portion of
the femur, figure 5. The longer the
nail, the more anterior the distal tip will be. Adjust the target arm (page 20) if the cannula rests too far
anterior.
If the nail is exerted with force it will
bend and be more centrally located in
the canal, figure 6. If the slots are in
a narrow part of the femur, they will
be more central in the canal, figure 6.
The target arm may have to be
adjusted to accommodate for bending of the nail. Loosen the distal cap screws and adjust the distal
target arm.
Figure 7 and figure 8 illustrate the
effect rotation has on the orientation of
the slots. Rotation of the nail will place
the slots in parallel with the hole in the
near cortex. This is especially
important with a curved slot finder.
Insert the solid slot finder. Keep the flat
of the handle in line with the nail. Push
it in the slot.
The second “SIGN feel” is rotating the
slot finder 10º when it is in the slot. If it
does not rotate, it may be stuck in the
bone hole or obliquely in the slot, figure
7. Sometimes the L-handle must be
rotated to orient the slot to the hole, figure 7 and figure 8, or the screw hole broach needed to enlarge
the hole.
NOTE: See technique used in all approaches on page 11.
If either slot finder cannot be placed, remove the target arm and use the curved slot finder. Be sure
the fracture has not shifted or the hole will not be in longitudinal orientation to the slot. Rotate the nail
to orient the slot to the hole. Practice this using the nail when not in the bone or use a sawbones.
After compression of fracture site
Some rotation is still possible if the proximal interlocking screw has been placed to impact the
fracture, page 29. Use the usual technique for finding the distal slot in the nail. If more rotation is
needed, the proximal screw closest to the knee may be removed to allow rotation. After the distal
interlock has been accomplished, place the proximal interlock. See figure 9 on page 29.
28

Fig. 10
Distal Interlock
Fig. 9
Proximal Interlock
NOTE: Distal and proximal refers to the nail rather than the bone, figure 9.
NOTE: If you wish to compress the fracture site, place one interlocking screw in the nail hole nearest
the knee. The locking bolt is struck to move the distal fracture fragment toward the proximal
fragment, figure 10. Different from the antegrade approach.
Proximal interlock
NOTE: See technique used in all approaches on page 11.
Manipulate the knee into flexion and extension after the nail insertion and interlock has been
accomplished. Continue range of motion and strengthening exercises after the surgery. If the fracture
is stable, we advise weight-bearing as tolerated.
29

Antegrade Approach to FEMUR
Fig. 1
Position of patient
Supine or lateral. Lateral is best for open reductions. Technique for lateral position will be described.
Patient must be stabilized in the lateral position to prevent shifting during surgery.
Reduction
If open reduction is indicated, perform this prior to skin incision for nail insertion. Incision should be
as short as possible. Identify the proximal fragment by abducting the leg. Incise the skin and fascia
over the end of this fragment. Dissect through muscle with your finger to identify the fracture site.
You can then extend the incision as needed. Free up each of the main fragments by removing soft
tissue attachments. Save the callus for bone graft. Ream each fragment from the fracture site. Do not
penetrate the metaphysis at either end of the bone. Save the bone from the flutes of the reamer for
bone graft. Secure the reduction with clamps and proceed to preparation for nail insertion.
Variations in reductions
If the fracture is comminuted over a long segment, free up only the 2 main fragments and do not
devascularize the fragments in the middle of the fracture. Pass the nail from the proximal fragment
into the distal fragment without disturbing the fragments within the fracture site.
If the fracture occurred within the past week, closed reduction may be attempted. If the reamers do
not pass immediately into the distal fragment, plan a mini open reduction and guide the reamers and
the nail into the distal fragment with a clamp or bone hook.
Skin incision
Extend from the superior greater trochanter posteriorly in the direction of the gluteus maximus fibers.
Dissect down to the greater trochanter in the region between the posterior and middle one third
junction. Dissect through muscle fibers with finger or periosteal elevator.
Bone entrance
Entrance should be placed in a junction between the
posterior and middle one third of the greater trochanter,
figure 1. We do not recommend placing the entrance
through the piriformis fossa. Hoop stresses are
generated when the bend passes through the piriformis
fossa. If you doubt this, place a nail into a sawbones
and note the hoop stresses. Use a curved awl to make
the entrance. If possible visualize the fracture site to
determine the direction of the awl. Sink the awl to the
hilt by rotation.
Reaming
Start with the smaller reamers and increase reamer sizes until chatter is heard. Be sure you can feel
the reamer rotating through a 360º arc to know the reamer is in the canal. Once chatter is felt for
4-6cm, over ream the proximal 6cm to allow room for the bend of the nail. Be aware of the reduction
during reaming. Nail diameter is 2mm smaller than the reamer which caused chatter.
30

Preparation of the nail
Fig. 2
Fig. 4
Fig. 3
NOTE: See technique used in all approaches on page 11.
Insertion of the nail
Use tissue protector to keep the nail off
the skin. Push the nail in as far as it will
go. If the nail stops, tap the locking bolt
with small taps. Rotate the nail 10º after
4 taps, figure 2. The 1-1/2º bend at the
end of the nail helps keep the nail from
being caught in the canal. If the nail does
not advance with light taps, it is not in
the canal or it is too large. Never hit the
nail with heavy blows. This will cause
the nail to bend and make interlocking
difficult. Never hit the L-handle or you
will ruin the L-handle for interlocking.
Check reduction as the nail advances.
Allow the nail to rotate as the bend in the nail slides into the canal, never force rotation. Leave nail
2mm prominent above bone cortex, figures 3 and 4.
Note the difference in orientation of slots, figures 3 and 4. Both directions allow stable interlock.
31

Fig. 5
Fig. 7
Fig. 6
Proximal interlock can be done through lateral to
medial or anterior to posterior direction, figure 5.
They are equally stable.
The proximal end of the nail should be 3mm higher
than the cortex of the greater trochanter, figure 5.
This adds to the stability of the nail as well as makes
removal easier.
Distal interlock
The final location of the
slots will vary depending
on their location in the
canal. If the end of the nail
is in the narrow part of the
canal, the slots will be
central, figure 6.
If nail ends in the wide part
of the canal, the slots will
be anterior, figure 7. The
SIGN nail does not have
an arc of radius and the
femur is curved.
Recognizing this
difference will determine
where the pilot hole is
made. The pilot hole
would be made in the center of the femur if the slots are in the narrow part of the canal and anteriorly
in the wide part of the canal. The incision for interlocking should be large enough so you can feel the
cannula on the bone to determine its location. Sometimes the target arm must be adjusted to account
for this. Loosen the distal cap screws to make this adjustment rather than bending the target arm.
NOTE: See page 20 for tips on interlocking.
32

Fig. 9
Fig. 8
Compression of fracture
After the first distal interlocking screw is placed, the fracture site may be
impacted, figure 8.
Proximal interlock
This may be directed from lateral to medial
or anterior to posterior, figure 9. We are
studying the stability of these interlocks.
Mechanism of interlock is the same as tibia.
in retrograde approach.
Manipulate the knee to full flexion.
33

240mm
Fin nail
240mm
Fig. 1
Cross section of fins
seated in bony canal
Fin nail
Fig. 2
Fin should be placed here.
The nail template will indicate
whether antegrade or retrograde
approach is optimal. Use
antegrade if you have a choice.
Use non-fractured side x-ray for
template.
Fig. 3
Description
The SIGN intramedullary fin nail is designed so the fin
takes the place of the distal interlocking screw, figure 1.
Proper technique including location of the fin will optimize
the fixation. The fin should end in the isthmus of the femur.
The fin comes in sizes 8mm, 9mm,
Please note the femoral canal is oblong so on one view of
the post-op x-ray the fin appears to be surrounded by bone
and the other x-ray reveals a gap between canal and fin on
one side.
SIGN is now manufacturing
8 – 10mm diameter, 240mm length and 9 - 10mm diameter, 280mm length fin nails for use in
femur and humeral fractures, figure 2.
NOTE: The nail length, such as 240mm, refers to the
distance between the nail notch (at the proximal end
of nail) and the end of the flutes as shown above,
figure 2.
SIGN reamers are designed with marks at 240mm, 280mm
and 320mm, figure 5. The marks show the reaming depth
of the LAST reamer used for the corresponding nail.
Indications
1. Location of the fracture. The fracture should be
located so that the fin of the nail rests in the isthmus of
the femur, figure 3. Fractures of the femur may be
treated in retrograde or antegrade and fractures of the
humerus may be treated antegrade. It is important to
use the template to estimate the length of the nail.
2. The fracture should be stable. We started using the fin
in stable fractures. This protocol has been expanded
so we must keep records. Follow up is essential so we
can modify the indications for the fin nail.
SIGN Technique for FIN NAIL
34

Instruments
240mm
Fig. 5
Fig. 4
The standard or short target arm is used for the proximal interlocking, figure 4.
Technique
Open or closed reduction can be used.
The technique used in standard SIGN nail is the same except for the reaming.
Triple Ream
First ream
Ream until chatter is felt for 4-6cm of the canal. The size of the fin is 1mm larger than this reamer.
Second ream
Ream with the next larger size reamer but stop at the mark pertaining to the length of the fin nail
selected, figure 5.
Third ream
Ream using the next 2 larger sizes to accommodate for the bend of the nail. This reamer only
penetrates 4cm.
Proximal interlocking
This procedure is similar to proximal interlocking of the standard SIGN nail. The proximal portion of
the standard target arm, short target arm, or hip and pediatric target arm may be used.
35

HUMERUS
Fig. 3
Fig. 1
Fig. 2
Bicipital
groove
Position
The patient is placed in beach chair position on the OR table, figure 1. All prominences must be
padded especially the radial nerve. The patient should be placed so the arm can hang off the table as
gravity may be used in the reduction.
Reduction
If open reduction is done first, avoid damage to the radial
nerve.
Skin incision
Palpate the bicipital groove and make the incision
posterior to the groove, figure 2. Use periosteal elevator to
dissect through the fibers of the deltoid muscle. Split the
rotator cuff so it can be repaired. This is very important.
Bony entrance
The hole should be placed in the greater tuberosity at the
junction of the articular surface. Use the curved awl,
figure 3.
36

Fig. 4
Apply counter pressure
to the olecranon during
insertion of nail into distal
fragment.
Reaming
Be sure the fracture site is not distracted during
reaming, figure 4.
Nail insertion
The diameter of the nail is 1mm less than the
largest reamer that achieved chatter. Be sure
the fracture site is not distracted during
placement of the nail. Rotate the nail so the
distal interlocking screws will not be in the
vicinity of the radial nerve. The nail should be
flush with the entrance hole. Place bone wax
over the end of the nail after the L-handle is removed.
Interlocking
Interlocking is done as described in the technique used in all approaches. The difference in the
proximal interlock is that the screw must not penetrate the joint space. Make the pilot hole and
enlarge using the step drill. Use the back end of the depth gauge and push this in until it reaches the
subchondral bone. Turn the depth gauge around for measurement of the length of the screw.
37

Distractor Instructions
Figure 1 Initial Clamp Placement Figure 2 Placing Distractor Over Clamps
NOTE: One fragment is mobile and one fragment is stationary. For example the proximal fragment
in a femur fracture is stationary. The ratchet should go on the moveable fragment.
Figure 3 Placing Retaining Pin Figure 4 Turn Handle to Distract the Bone
Fragments
NOTE: Must be done slowly. Sometimes it is necessary to incise tight bands in the quadriceps
mechanism. If the ratchet is distracted over 4 inches, reposition the clamps.
Figure 5 Once Distracted, Start Shaft Alignment Figure 6 Reduced Fragment
NOTE: Sometimes the distractor must be removed to do this.
38

Removal of Broken Nail
1. It is important to leave the proximal end of the nail and the screws prominent. Many times I
see that the nail has been placed inside the bone and I am concerned about removal later on. It
is much easier to find the interlocking screws if they are left prominent.
2. Try to use the same distal holes for interlocking in the replacement nail if the broken nail is
SIGN. Use the same length of nail, but a wider width. Four holes in the femur provide a stress
concentrator which may result in a fracture at the distal interlocking area. If the broken nail is
not SIGN try to line up at least one hole to SIGN slot.
3. Leave one screw present until the nail can be adequately secured and pulled out. Sometimes
after the distal interlocking screws have been removed a screw driver or other instrument can
be left in the slots of the nail so it does not slide down. We were also able to push the nail up
using this method.
4. The advantage of using stainless steel nails over titanium becomes manifest because the bone
does not grow into stainless steel as it does into titanium.
5. Reaming results in bone graft. Don't irrigate the hematoma because this contains a great deal
of BMP.
ADDITIONAL NOTES
Save bone from reaming or take bone from the entrance hole for bone grafting.
Sometimes casting or splinting after SIGN nail insertion is necessary for unstable fractures.
Weight bearing is encouraged in stable fractures. Crutches are used depending on patient’s
pain.
Fracture healing is a race between bone healing and implant failure. Therefore, if healing is
delayed past 3 months, consider bone grafting.
Implant removal should be delayed for 24 months. If the nail is removed, protect the bone by
crutch for 6 to 8 weeks after removal.
If you have a comment, problem or something to share with SIGN surgeons around the world,
please e-mail or place it in the comment section of the database.
Reaming the middle fragment of a segmental fracture. There is a great decrease in
vasculularity after power reaming. I don’t know if hand reaming also causes a decrease.
Inserting a smaller diameter nail without reaming is an option.
Keep your sharp instruments sharp
Our drill bits have been tested and will drill a hole 300 times without becoming dull. If the drill bit
hits another metal object and a nick is formed, the drill bit will become rapidly dull. No food or drink
should be allowed in the cleaning and sterilizing process area.
Step drills will become dull if they engage the slot in the nail.
Reamers will become dull if they are not rotated clockwise. The cutting edge only goes one way.
The threads on the locking bolts and cap screws will become dull if they’re forced into the hole.
Always thread using gravity.
39

Changes of SIGN interlocking procedure
Vietnam has soft bone. We used a hand drill and large drill bits to make the hole in the near cortex.
The bone was soft and the drill did not walk along the bone.
Bangladesh has hard bone. The large drill bit in the hand drill walked along the bone during the
attempt to drill a hole in the near cortex. We made a pilot hole and used a step drill to enlarge it. We
improved step drills in many ways. No matter how we improve them they become dull.
SIGN surgeons began to use a commercial drill which allowed them to drill faster and more
accurately. We were not satisfied with the sterility of the drill. A drill cover placed over the drill
with a chuck extension has allowed us to use commercial drills in a sterile manner.
We can use power so we are modifying our drill bits to enable the interlock holes to be drilled
quicker.
The slot finders have also changed. The curved slot finder has become very helpful. If the
longitudinal alignment has been maintained, the slot in the nail can always be found.
40

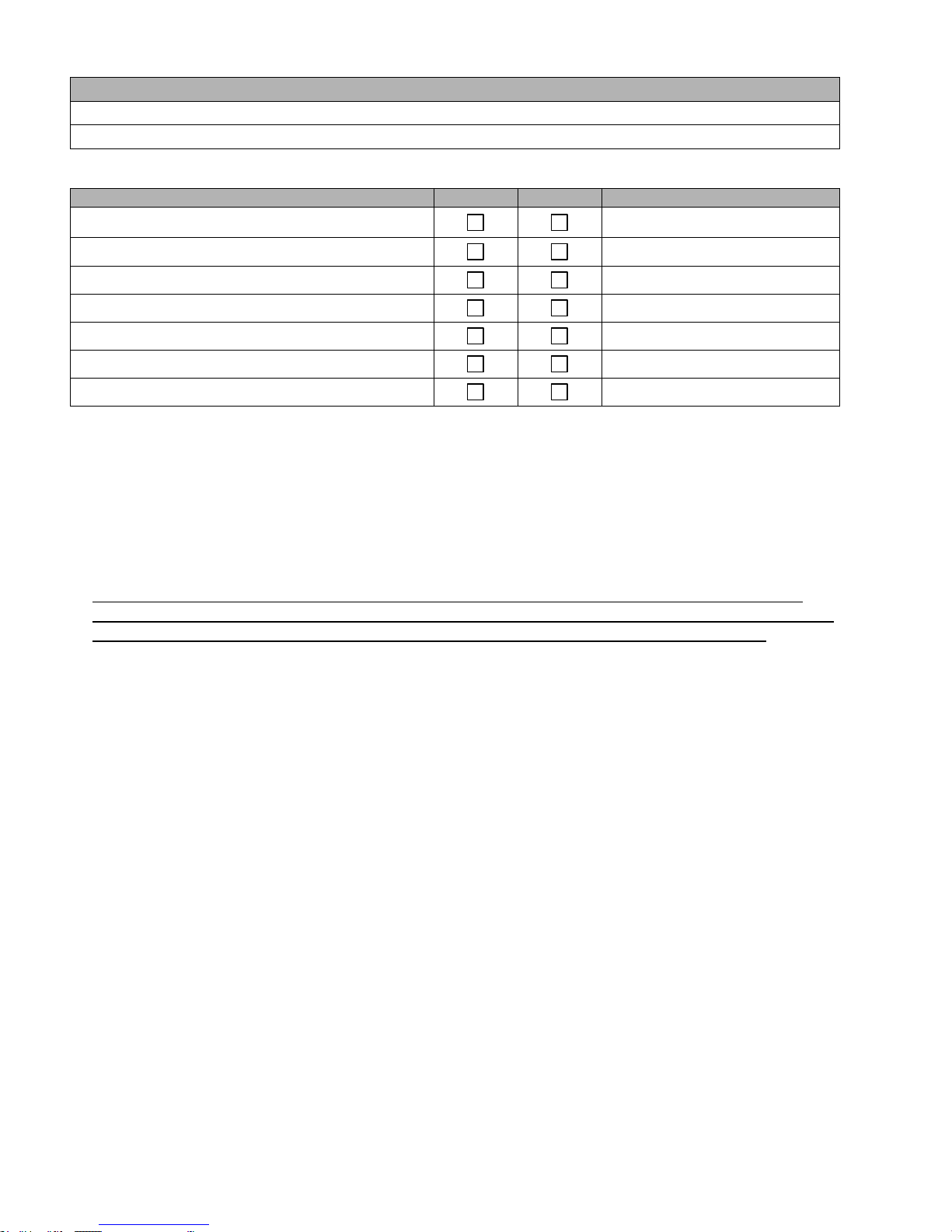
PATIENT CASE INFORMATION: (All fields are required unless otherwise noted.)
Hospital Name:
Case Number: (optional)
Patient Name:
Age:
Gender:
Weight:
Injury Date:
Optional Patient Contact Information: (This information will be available only to the applicable hospital).
Address:
Phone Number:
Email Address:
Data Collection Sheets
For Data Entry Into The SIGN Online Surgical Database
www.signsurgery.org
41

SURGERY INFORMATION: Copy this page for each additional surgery for this patient.
Surgery Date (month/day/year):
Surgeon Name(s):
1. Antibiotics Used? Yes No
If yes:
How long from time of injury? _____ hours _____ days
Name of Antibiotic: ________________________________
Duration of Antibiotic Coverage: _____ hours _____ days
2. Surgery Comments:
________________________________________________________________________________
________________________________________________________________________________
________________________________________________________________________________
________________________________________________________________________________
________________________________________________________________________________
________________________________________________________________________________
________________________________________________________________________________
________________________________________________________________________________
________________________________________________________________________________
________________________________________________________________________________
42

FRACTURE INFORMATION: (Copy pages 44, 45, and 46 for each additional fracture.)
Patient Name:
Case Number:
1. Fracture Side:
Left Right
2. Surgical Approach:
Antegrade Femur
Tibia
Antegrade Humerus
Hip Fracture
Retrograde Femur
3. Location of Fracture:
(check all that apply)
Proximal
Middle
Distal
Segmental
Femoral Neck
Intertrochanteric
Subtrochanteric
4. Type of Fracture:
Closed
Gustilo IIIa
Gustilo I
Gustilo IIIb
Gustilo II
Gustilo IIIc
5. Stability of Fracture: (Hip Fracture Only)
(check all that apply)
Stable
Unstable Lateral Femur Wall
Unstable Posterior Medial Fragment
6. Time from injury to Debridement: ____hours ____days
7. Time from injury to Skin Closure: ____days
8. Method of Wound Closure:
(check all that apply)
Primary
Skin Graft
Muscle Flap
Secondary
Other: __________________________
9. Nonunion:
Yes
No
10. Previous Implant Used:
Yes
No
If Yes, check all that apply:
External Fixation
Plate
IM Nail
Wire
If External Fixation:
1. How long was external fixation in place? ____days
2. Time between removal of ext. fixation and SIGN? ____days
11. Method of Reaming:
None
Hand
Power
12. Fracture Reduction:
Open
Closed
13. Comments:
_______________________________________________________________________________
_______________________________________________________________________________
_______________________________________________________________________________
_______________________________________________________________________________
_______________________________________________________________________________
_______________________________________________________________________________
_______________________________________________________________________________
_______________________________________________________________________________
43

FRACTURE INFORMATION (continued from previous page.)
Patient Name:
Case Number:
14. Nail Type Used: (Please mark the type of nail used to treat this fracture.)
200
220
240
260
280
300
320
340
360
380
400
420
Standard Nails
mm
mm
mm
mm
mm
mm
mm
mm
mm
mm
mm
mm
8 mm
9 mm
10 mm
11 mm
12 mm
Standard
160
190
240
280
Pediatric
Fin Nails
140
170
200
240
Fin Nails
mm
mm
mm
mm
mm
mm
mm
mm
7 mm
6 mm
8 mm
7 mm
9 mm
8 mm
10 mm
11 mm
12 mm
Standard Hip Nail
280
Fin Hip Nail
240
mm
mm
10 mm
10 mm
15. Screw Quantities Used: (Please enter the quantity of each type of screw used with this nail.)
Standard Interlocking Screws
Length in mm
25
30
35
40
45
50
55
60
65
70
75 #Proximal
#Distal
Compression Screws (maximum of 2 screws)
Length in mm
70
75
80
85
90
95
100
105
110
115
Qty
SHC Proximal Interlocking Screws (maximum of 1)
Length in mm
60
65
70
75
80
85
90
95
Qty
SHC Cortical Screws (maximum of 1)
Length in mm
30
35
40
45
Qty
16. SHC Components Used
Rod Plate
Yes
No
Rod Connector
Yes
No
Unicortical Screw
Yes
No
3 Hole Plate
Yes
No
44
FRACTURE INFORMATION (continued from previous page.)
Patient Name:
Case Number:
17. X-Rays Taken: (Please list the names of the digital image files for all x-rays of this fracture.)
Digital Image X-Ray File Name(s)
Pre-Op
Post-Op
Date Taken
Notes on uploading digital image x-ray files:
1. This table is provided for you to keep track of digital x-ray images so that the process of uploading
these images to the online database goes smoothly.
2. The time required to upload image files is determined by the size of your digital image files and
your internet connection speed.
3. VERY IMPORTANT: You can reduce the size of your digital image files by converting them to
grayscale (remove all color) and by reducing the dimensions of your pictures to approximately 640
x 480 pixels. Many digital cameras come with software programs capable of these tasks.
45

FOLLOW-UP INFORMATION: (Copy this sheet for each additional follow-up.)
Patient Name:
Case Number:
Date (month/day/year):
If multiple fractures, which fracture is this a follow-up for?
1. Infection:
Yes
No
If yes:
Incision of the wound:
Yes
No
Infection depth:
Superficial
Deep (patient returns to surgery)
Duration of infection:
_____ weeks
Osteomyelitis
Amputation
2. Partial weight bearing:
Yes
No
3. Painless full weight bearing:
Yes
No
4. Healing by x-ray:
Yes
No
5. Knee flexion greater than 90
degrees: (Not applicable for Hip Fracture)
Yes
No
6. Screw breakage:
Yes
No
7. Screw loosening:
Yes
No
8. Nail breakage:
Yes
No
9. Nail loosening:
Yes
No
10. Deformity:
Yes
No (under 10 degrees)
If yes:
Alignment:
Over 10 degrees varus
Over 10 degrees valgus
Over 20 degrees varus
Over 20 degrees valgus
Rotation:
Over 30 degrees
11. Repeat Surgery:
Yes
No
If Yes, check all that apply:
For Infection
For Deformity
For Non-union
If For Non-Union, check all that apply:
Dynamize
Exchange Nail
Iliac Crest Bone Graft
Other:____________________________________
13. X-Rays Taken: (Please list the names of the digital image files for all x-rays during this follow-up.)
Digital Image X-Ray File Name(s)
Date Taken
12. Comments:
________________________________________________________________________________
________________________________________________________________________________
________________________________________________________________________________
________________________________________________________________________________
46

Surgical Implant Generation Network
451 Hills Street, Suite B
Richland, WA 99354
USA
Phone: (509) 371-1107
Fax: (509) 371-1316
On the web: www.sign-post.org
© Copyright 2001 by Surgical Implant Generation Network. All Rights Reserved.
For more information on the Surgical Implant Generation Network (SIGN) or any of
the techniques described in this manual, please use the contact information listed above.
47
 Loading...
Loading...