Page 1

Respironics V200/Esprit Ventilator
Service Manual
580-1000-02 H
Page 2
This work is protected under Title 17 of the United States copyright code and is the sole property of Respironics.
No part of this document may be copied or otherwise reproduced, or stored in any electronic information
retrieval system, except as specifically permitted under United States copyright law, without the prior written
consent of Respironics.
Copyright © 2004-2009. Respironics, Inc.
All rights reserved.
For Technical support, contact:
Respironics, Inc. Customer Service
Within the U.S.A. 1-800-345-6443
Outside the U.S.A. 724-387-4000
Facsimile 724-387-5012
service@respironics.com
United States of America
Respironics California, Inc.
2271 Cosmos Court
Carlsbad, CA 92011
USA
1-800-345-6443
or 724-387-4000
Authorized Representative
Respironics Deutschland, Inc.
Gewerbestrasse 17
D-82211 Herrsching Deutschland
+49-8-15-29-30-60
ii Respirionics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 3
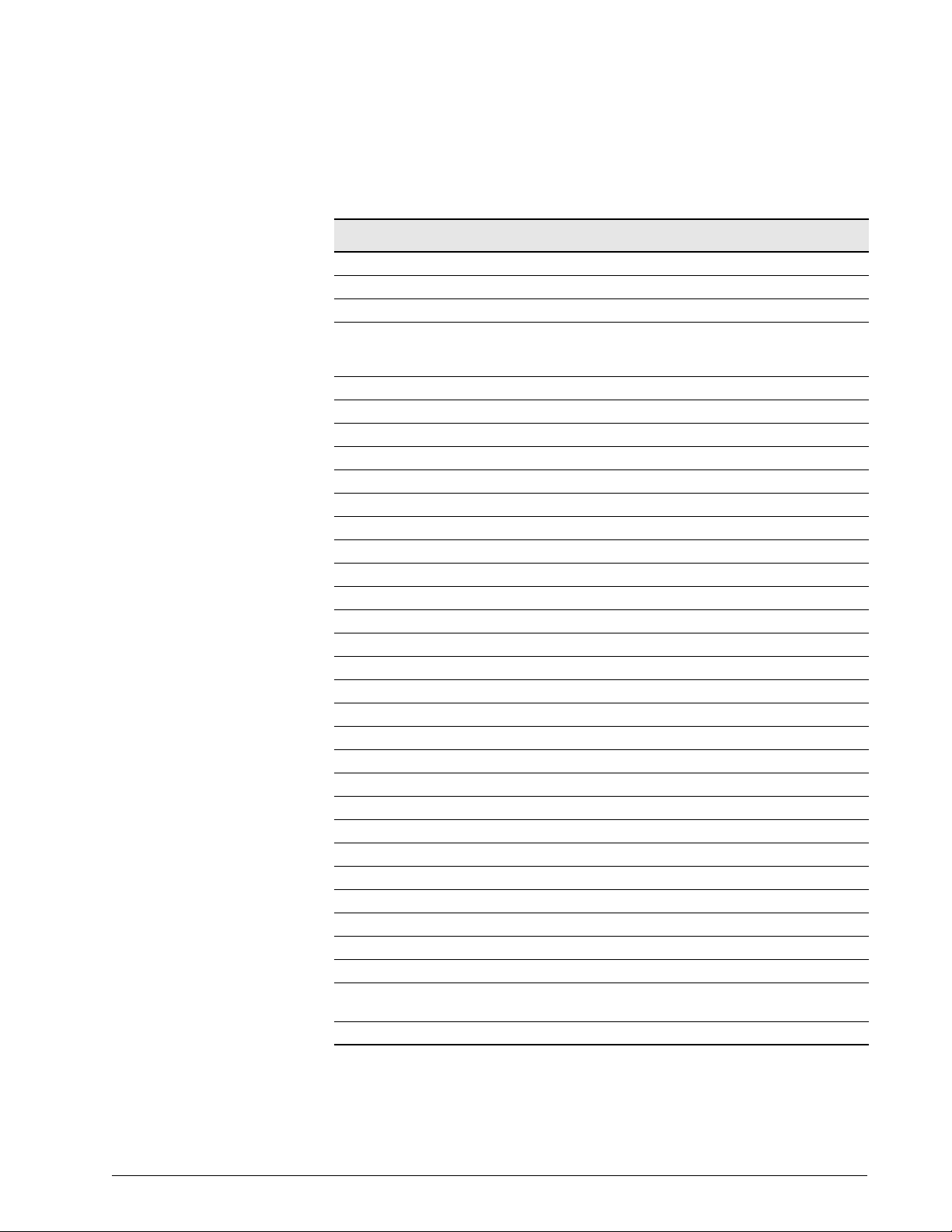
Table of Contents
1 Introduction and Intended Use . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1-1
1.1 Recommended Tools and Test Equipment . . . . . . . . . . . . . . . . . . . . . . . 1-2
2 Warnings, Cautions, and Notes. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2-1
2.1 General Warnings. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2-1
2.2 General Cautions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2-1
2.3 General Notes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2-2
3 Theory of Operation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-1
3.1 Pneumatic System . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-1
3.1.1 Blower Inlet Filter (F1) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-3
3.1.2 Muffler (Silencer). . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-3
3.1.3 Blower . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-3
3.1.4 Cooling Fan Filter. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-3
3.1.5 Cooling Coil. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-3
3.1.6 Cooling Coil Fan. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-3
3.1.7 Air Valve Assembly (AV) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-4
3.1.8 Air Flow Sensor (FS1). . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-4
3.1.9 Oxygen Water Trap/Inlet Filter Assembly (F2) . . . . . . . . . . . . . . . 3-4
3.1.10 Oxygen Inlet Connector (O
3.1.11 Oxygen Supply Pressure Switch (PS1) . . . . . . . . . . . . . . . . . . . . 3-4
3.1.12 Oxygen Regulator (REG 1) . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-4
3.1.13 Oxygen Valve (OV) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-5
3.1.14 Oxygen Flow Sensor (FS2) . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-5
3.1.15 Crossover Solenoid (SOL1) . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-5
3.1.16 Cross-Contamination Check Valve (CV5) . . . . . . . . . . . . . . . . . . . 3-5
3.1.17 Safety Valve Pilot Solenoid (SOL2) . . . . . . . . . . . . . . . . . . . . . . 3-5
3.1.18 Safety Valve (SV) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-6
3.1.19 Air System Check Valve (CV2) . . . . . . . . . . . . . . . . . . . . . . . . . . 3-6
3.1.20 Inspiratory Non-Rebreathing Check Valve (CV3) . . . . . . . . . . . . . 3-6
3.1.21 Pressure Relief Valve (PRV). . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-6
3.1.22 Oxygen Sensor (OS) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-6
3.1.23 Inspiratory Pressure Transducer (PT3) . . . . . . . . . . . . . . . . . . . . 3-6
3.1.24 Inspiratory Pressure Transducer Solenoid (SOL4) . . . . . . . . . . . . 3-7
3.1.25 Heated Exhalation Filter (F3) . . . . . . . . . . . . . . . . . . . . . . . . . . 3-7
3.1.26 Exhalation Pressure Transducer (PT2) . . . . . . . . . . . . . . . . . . . . 3-7
) . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-4
2
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. iii
Page 4

Table of Contents
3.1.27 Exhalation Pressure Transducer Solenoid (SOL3) . . . . . . . . . . . . 3-7
3.1.28 Exhalation Non-Rebreathing Check Valve (CV4) . . . . . . . . . . . . . 3-8
3.1.29 Exhalation Valve (EV) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-8
3.1.30 Exhalation Flow Sensor (FS3) . . . . . . . . . . . . . . . . . . . . . . . . . . 3-8
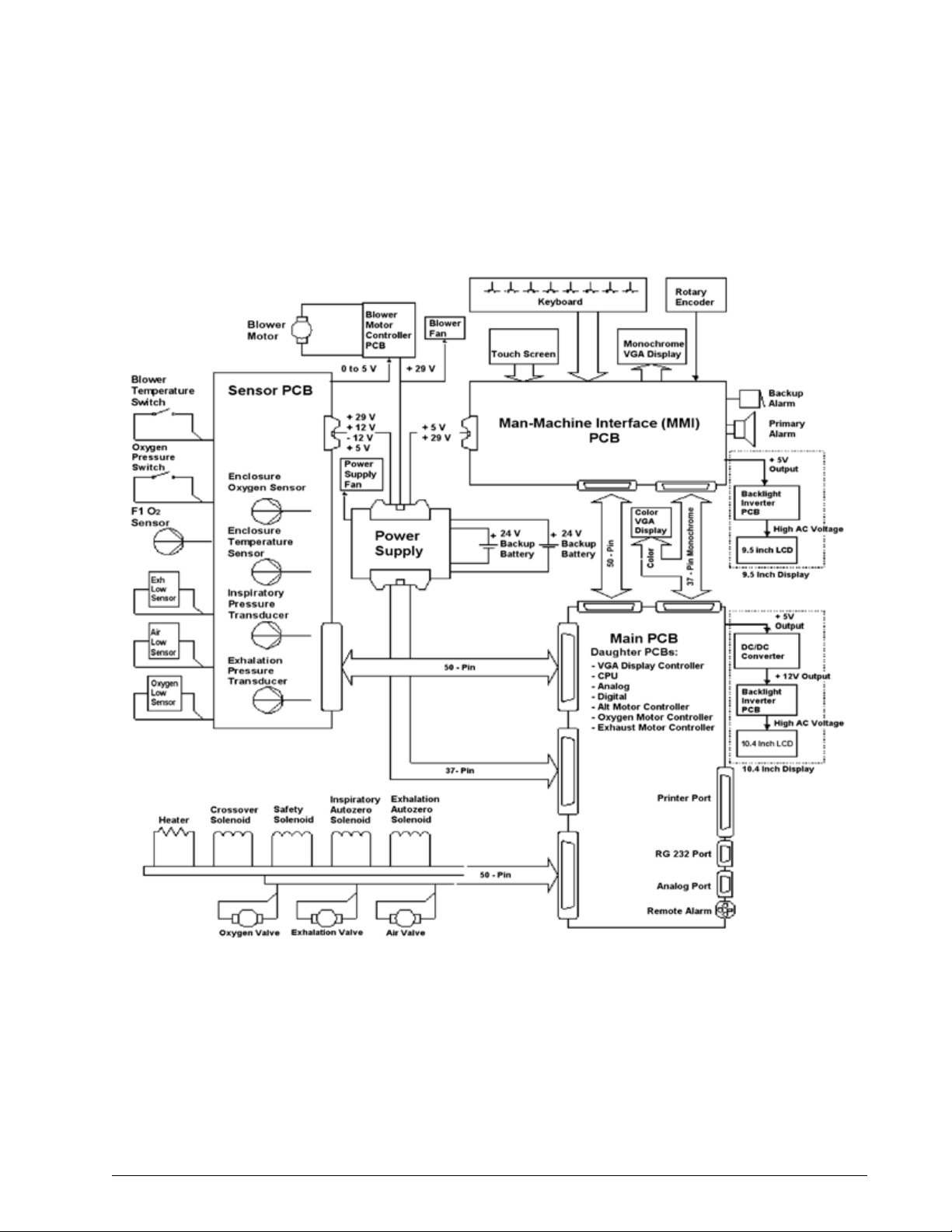
3.2 Ventilator System Electronics . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-9
3.2.1 Main PCB . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-12
3.2.2 CPU PCB . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-13
3.2.3 Analog PCB . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-13
3.2.4 Digital PCB . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-13
3.2.5 VGA Controller PCB . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-14
3.2.6 Blower Controller PCB . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-14
3.2.7 Motor Controller PCBs . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-14
3.2.8 Sensor PCB . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-14
3.2.9 Man-Machine Interface (MMI) PCB . . . . . . . . . . . . . . . . . . . . . 3-15
3.2.10 Power Supply . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-15
3.2.11 Backlight Inverter PCB . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-15
3.2.12 Real-Time Clock Battery . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-15
3.2.13 Backup Battery . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-16
3.2.14 External Battery. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-16
3.2.15 DC/DC Converter PCB. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-16
3.2.16 Optical Rotary Encoder. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-16
3.2.17 Graphic User Interface (GUI) . . . . . . . . . . . . . . . . . . . . . . . . . 3-16
3.2.18 Remote Alarm (Nurse Call) . . . . . . . . . . . . . . . . . . . . . . . . . . . 3-17
4 Periodic Maintenance . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4-1
4.1 Cleaning the Ventilator . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4-2
4.2 Annual PM . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4-3
4.3 12,500-Hour PM. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4-3
5 Diagnostic Mode and
Troubleshooting . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-1
5.1 Entering Diagnostic Mode. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-2
5.2 User Configuration . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-2
5.2.1 Setting the Date and Time . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-3
5.2.2 Setting Altitude . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-3
5.2.3 Enabling Circuit Compliance . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-4
5.2.4 Selecting 12 or 12 Hour Clock . . . . . . . . . . . . . . . . . . . . . . . . . 5-4
5.2.5 Confirm Backup Battery . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-4
5.3 Short Self Test (SST) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-5
5.4 Extended Self Test (EST) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-6
iv Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 5

Table of Contents
5.5 Software Screen . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-8
5.6 Diagnostic Codes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-9
5.7 Hardware Diagnostics. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-11
5.8 Pneumatic Component Troubleshooting . . . . . . . . . . . . . . . . . . . . . . . . 5-13
5.8.1 Oxygen Valve . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-14
5.8.2 Oxygen Flow Sensor . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-15
5.8.3 Oxygen Regulator . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-16
5.8.4 Air Valve . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-17
5.8.5 Air Flow Sensor . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-17
5.8.6 Inhalation and Exhalation Solenoids . . . . . . . . . . . . . . . . . . . . 5-18
5.8.7 Safety Valve and Safety Solenoid . . . . . . . . . . . . . . . . . . . . . . . 5-18
5.8.8 Pressure Relief Valve . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-19
5.8.9 Crossover Solenoid . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-20
5.8.10 Exhalation Flow Sensor. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-21
5.8.11 Check Valve 2 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-22
5.8.12 Check Valve 3 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-22
5.8.13 Check Valve 4 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-23
5.8.14 Filter Heater . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-23
5.8.15 Blower . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-24
5.8.16 Inhalation/ Exhalation Pressure Transducers and Exhalation
Valve . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-25
5.8.17 Oxygen Pressure Switch . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-26
5.8.18 External Oxygen Sensor . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-26
5.8.19 High Internal Oxygen Alarm Test . . . . . . . . . . . . . . . . . . . . . . . 5-26
5.8.20 Sensor PCB Voltage Indicators . . . . . . . . . . . . . . . . . . . . . . . . 5-27
5.9 Bacteria Filter Back Pressure Test . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5-28
6 Diagnostic Codes. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6-1
6.1 Diagnostic Code 1012 Troubleshooting . . . . . . . . . . . . . . . . . . . . . . . . 6-24
6.2 Diagnostic Code 5000 Troubleshooting . . . . . . . . . . . . . . . . . . . . . . . . 6-26
7 Ventilator Communications. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7-1
7.1 Downloading Software . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7-1
7.2 Programming the Ventilator Serial Number . . . . . . . . . . . . . . . . . . . . . . . 7-4
7.3 Enabling Options . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7-5
7.4 Setting Up the Serial Interface for DRPT . . . . . . . . . . . . . . . . . . . . . . . . 7-6
7.5 Generating a Diagnostic Report (DRPT) . . . . . . . . . . . . . . . . . . . . . . . . . 7-9
7.6 Analog Output Port (Chart Recorder) Pinout . . . . . . . . . . . . . . . . . . . . . 7-11
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. v
Page 6

Table of Contents
8 Performance Verification. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-1
8.1 Required Test Equipment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-4
8.2 Preliminary Cleaning, Inspection and Setup . . . . . . . . . . . . . . . . . . . . . . 8-5
8.3 Preliminary Pneumatic Calibration Analyzer Setup . . . . . . . . . . . . . . . . . 8-6
8.4 Certifier FA Plus Setup. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-7
8.4.1 Measurement Selection Screen . . . . . . . . . . . . . . . . . . . . . . . . . 8-7
8.4.2 Averaging Setup Menu . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-9
8.4.3 Trigger Options Menu . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-10
8.4.4 Configuration Menu . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-10
8.4.5 Saving Configurations. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-11
8.5 Performance Verification Procedures . . . . . . . . . . . . . . . . . . . . . . . . . . 8-13
8.5.1 Test 1: Electrical Safety . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-14
8.5.2 Test 2: Extended Self Test (EST). . . . . . . . . . . . . . . . . . . . . . . 8-15
8.5.3 Test 3: Air Flow Accuracy . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-16
8.5.4 Test 4: Oxygen Flow Accuracy . . . . . . . . . . . . . . . . . . . . . . . . . 8-19
8.5.5 Test 5: Pressure Accuracy. . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-21
8.5.6 Test 6: PEEP System . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-23
8.5.7 Test 7: Breath Rate . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-26
8.5.8 Test 8: Alarm/Analog Output Signals, Alarm Volume,
and Remote Alarm . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-27
8.5.9 Test 9: Gas Volume Accuracy . . . . . . . . . . . . . . . . . . . . . . . . . 8-30
8.5.10 Test 10: Oxygen Accuracy. . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-32
8.5.11 Test 11: Heated Exhalation Bacteria Filter, Power Fail Alarm,
and Display Intensity . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-34
8.5.12 Test 12: Neonatal Option Testing . . . . . . . . . . . . . . . . . . . . . . 8-36
8.5.13 Test 13: Backup Battery and External Battery (If Installed) . . . . 8-38
8.6 Returning Ventilator to Normal Operation . . . . . . . . . . . . . . . . . . . . . . . 8-40
8.7 Performance Verification Troubleshooting/Repair . . . . . . . . . . . . . . . . . 8-42
8.7.1 Test 1: Electrical Safety . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-42
8.7.2 Test 2: Extended Self Test . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-42
8.7.3 Test 3: Air Flow Accuracy . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-43
8.7.4 Test 4: Oxygen Flow Accuracy . . . . . . . . . . . . . . . . . . . . . . . . . 8-43
8.7.5 Test 5: Pressure Accuracy. . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-44
8.7.6 Test 6: PEEP System . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-44
8.7.7 Test 7: Breath Rate . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-44
8.7.8 Test 8: Alarm Output Signal, Volume, and Remote Alarm . . . . . 8-45
8.7.9 Test 9: Gas Volume Accuracy . . . . . . . . . . . . . . . . . . . . . . . . . 8-45
8.7.10 Test 10: Oxygen Accuracy. . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-45
8.7.11 Test 11: Heated Exhalation Bacteria Filter, Power Failure Alarm,
and Display Intensity . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-46
vi Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 7

Table of Contents
8.7.12 Test 12: Neonatal Option Test. . . . . . . . . . . . . . . . . . . . . . . . . 8-47
8.7.13 Test 13: Backup Battery and External Battery Test . . . . . . . . . . 8-48
8.8 Neonatal Option Data Form. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8-49
8.9 Electrical Safety/Extended Self Test (EST) Data Form . . . . . . . . . . . . . . 8-51
8.10 Performance Verification Data Form. . . . . . . . . . . . . . . . . . . . . . . . . . . 8-52
9 Esprit Ventilator Component
Removal/Installation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-1
9.1 Filter Replacement . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-3
9.2 Top Enclosure . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-5
9.3 Sensor PCB. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-6
9.4 Power Supply Fan/Shroud . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-8
9.5 Backlight Inverter PCB (9.5-in. GUI) . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-9
9.6 Backlight Inverter PCB (Original 10.4-in. GUI only) . . . . . . . . . . . . . . . 9-10
9.7 DC/DC Converter PCB (Original 10.4-in. GUI only) . . . . . . . . . . . . . . . . 9-11
9.8 Power Supply . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-12
9.9 Power Supply Fuses . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-15
9.10 MMI PCB (9.5-in. GUI) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-17
9.11 MMI PCB (10.4-in. GUI) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-20
9.12 GUI Assembly (9.5-in. GUI) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-22
9.13 GUI Assembly (Original 10.4-in. GUI) . . . . . . . . . . . . . . . . . . . . . . . . . 9-24
9.14 GUI Assembly (2nd Generation 10.4-in. GUI). . . . . . . . . . . . . . . . . . . . 9-25
9.15 Intensity and Volume Potentiometers (9.5-in. GUI) . . . . . . . . . . . . . . . . 9-28
9.16 Intensity and Volume Potentiometers (10.4-in. GUI’s). . . . . . . . . . . . . . 9-29
9.17 Rotary Encoder (9.5-in. GUI) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-30
9.18 Rotary Encoder (10.4-in. GUI’s) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-31
9.19 GUI Front Panel Overlay (10.4-in. GUI’s) . . . . . . . . . . . . . . . . . . . . . . . 9-32
9.20 VGA Display Assembly (9.5-in. GUI) . . . . . . . . . . . . . . . . . . . . . . . . . . 9-33
9.21 Touch Screen/LED Indicator Assembly and Front Panel Overlay
(9.5-in. GUI) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-34
9.22 Backlight Inverter PCB, VGA Display, and Touch Frame
(Original 10.4-in. GUI). . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-35
9.23 Transition PCB, LCD, IR Touch Frame, and Backlight Inverter PCB
(2nd Generation 10.4-in. GUI) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-36
9.24 GUI Cleaning and Dust Gasket Installation
(2nd Generation 10.4-in. GUI) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-38
9.25 Increased Minimum Alarm Volume Harness . . . . . . . . . . . . . . . . . . . . . 9-41
9.26 Backup Alarm . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-42
9.27 AC Distribution Panel. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-43
9.28 AC Cord Bracket . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-45
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. vii
Page 8

Table of Contents
9.29 Humidifier Receptacle Rotation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-46
9.30 Printed Circuit Boards (Daughter PCBs) (Except Main PCB) . . . . . . . . . . 9-48
9.31 CPU PCB with 4.10 or Greater . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-49
9.32 Main PCB . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-50
9.33 Remote Alarm Jack . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-53
9.34 Power Switch . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-54
9.35 FIO
9.36 Exhalation Flow Sensor . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-56
9.37 Exhalation Valve Assembly . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-58
9.38 Primary Alarm . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-61
9.39 Filter Heater Assembly . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-62
9.40 Oxygen Flow Sensor . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-63
9.41 Inspiratory Manifold Assembly . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-65
9.42 Installing the Cable Extension Kit . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-69
9.43 Three-Station Solenoid Assembly . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-71
9.44 Air Flow Sensor . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-72
9.45 Air Valve Assembly. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-73
9.46 Oxygen Valve Assembly . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-74
9.47 Oxygen Regulator Assembly (with Oxygen Pressure Switch) . . . . . . . . . . 9-76
9.48 Elapsed Time Meter . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-78
9.49 Oxygen Water Trap Assembly . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-79
9.50 Blower Motor Controller PCB (Original) . . . . . . . . . . . . . . . . . . . . . . . . 9-80
9.51 Blower Motor Controller PCB (Updated) . . . . . . . . . . . . . . . . . . . . . . . . 9-81
9.52 Blower Assembly . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-82
9.53 Blower Muffler Assembly . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-85
9.54 Cooling Fan/Cooling Coil Assembly . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-86
9.55 GUI Upgrades . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-88
9.56 Replacing the GUI (9.5-in. to original 10.4-in.) . . . . . . . . . . . . . . . . . . 9-90
9.57 Replacing the GUI (9.5-in. to 2nd Generation 10.4-in.) . . . . . . . . . . . . 9-95
Connector . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-55
2
9.56.1 Installing the CPU and DC/DC Converter PCBs . . . . . . . . . . . . . 9-93
9.56.2 Downloading Ventilator Software . . . . . . . . . . . . . . . . . . . . . . . 9-93
9.56.3 Calibrating the Screen . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-94
9.56.4 Enabling Options . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-94
9.56.5 Final Checkout . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-94
9.57.1 Installing the CPU PCB . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-96
9.57.2 Downloading Ventilator Software . . . . . . . . . . . . . . . . . . . . . . . 9-97
9.57.3 Calibrating the Screen . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-97
9.57.4 Enabling Options . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-97
9.57.5 Final Checkout . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-97
viii Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 9

Table of Contents
9.58 Replacing the GUI (Original 10.4-in. to 2nd Generation 10.4-in) . . . . . . 9-98
9.58.1 Installing the CPU PCB . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-102
9.58.2 Downloading Ventilator Software . . . . . . . . . . . . . . . . . . . . . . 9-102
9.58.3 Calibrating the Screen . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-103
9.58.4 Enabling Options . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-103
9.58.5 Final Checkout . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9-103
10 Respironics V200 Ventilator Component Removal/Installation . . . . . . . 10-1
10.1 Inlet Filters . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-3
10.1.1 Air Inlet Filter . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-3
10.1.2 Blower Inlet Filter . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-4
10.1.3 Oxygen Inlet Filter . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-5
10.2 GUI Assembly . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-6
10.2.1 GUI Assembly Removal/Installation . . . . . . . . . . . . . . . . . . . . . 10-6
10.2.2 Backlight Inverter PCB . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-8
10.2.3 Transition PCB . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-9
10.2.4 LCD Panel. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-9
10.2.5 Touch Frame and Alarm LED PCB . . . . . . . . . . . . . . . . . . . . . . 10-9
10.2.6 GUI Front Panel Overlays . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-10
10.2.7 GUI Cleaning and Dust Gasket Installation . . . . . . . . . . . . . . . 10-11
10.3 Separating the Top and Bottom Enclosures . . . . . . . . . . . . . . . . . . . . 10-14
10.4 Enclosure Brace . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-16
10.5 Sensor PCB. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-17
10.6 Intensity and Volume Potentiometers . . . . . . . . . . . . . . . . . . . . . . . . . 10-19
10.7 Rotary Encoder . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-20
10.8 Power Supply Shroud . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-21
10.9 Power Supply Fan . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-21
10.10 Power Supply . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-22
10.10.1Removal . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-22
10.10.2Installation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-24
10.11 Power Supply Fuses . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-25
10.12 MMI PCB . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-26
10.13 Backup Alarm . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-28
10.14 AC Distribution Panel. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-29
10.15 AC Power Cord Bracket and Power Cord . . . . . . . . . . . . . . . . . . . . . . . 10-31
10.16 Elapsed Time Meter . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-32
10.17 Printed Circuit Boards (Daughter PCBs) (Except Main PCB) . . . . . . . . . 10-33
10.18 Main PCB . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-34
10.19 Remote Alarm Jack . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-37
10.20 Power Switch . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-38
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. ix
Page 10

Table of Contents
10.21 FIO2 Connector . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-39
10.22 Exhalation Flow Sensor . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-40
10.22.1Removal . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-40
10.22.2Installation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-40
10.23 Exhalation Valve Assembly . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-42
10.23.1Removal . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-42
10.23.2Installation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-43
10.24 Primary Alarm . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-43
10.25 Filter Heater Assembly . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-44
10.26 Oxygen Flow Sensor . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-45
10.26.1Removal . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-45
10.26.2Installation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-46
10.27 Air Flow Sensor . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-47
10.28 Inspiratory Manifold Assembly . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-48
10.28.1Removal . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-48
10.28.2Installation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-50
10.29 Three-Station Solenoid Valve Assembly . . . . . . . . . . . . . . . . . . . . . . . 10-51
10.30 Air Valve Assembly. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-52
10.31 Oxygen Valve Assembly . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-53
10.32 Oxygen Water Trap/Inlet Filter Assembly . . . . . . . . . . . . . . . . . . . . . . 10-54
10.32.1Removal . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-54
10.32.2Installation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-55
10.33 Oxygen Regulator Assembly (with Oxygen Pressure Switch) . . . . . . . . . 10-56
10.33.1Removal . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-56
10.33.2Installation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-56
10.34 Blower Motor Controller PCB. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-58
10.35 Blower Assembly . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-59
10.35.1Removal . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-59
10.35.2Installation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-60
10.36 Blower Muffler Assembly . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-62
10.36.1Removal . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-62
10.36.2Installation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-62
10.37 Cooling Fan/Cooling Coil Assembly . . . . . . . . . . . . . . . . . . . . . . . . . . 10-63
10.37.1Removal . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-63
10.37.2Installation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-64
10.38 Installing the CPU PCB . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-66
10.38.1Downloading Ventilator Software . . . . . . . . . . . . . . . . . . . . . . 10-66
10.38.2Calibrating the Display Screen . . . . . . . . . . . . . . . . . . . . . . . 10-66
10.38.3Enabling Options . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-66
10.38.4Final Checkout . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10-66
x Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 11

Table of Contents
11 Where to Go for Help . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11-1
12 Respironics V200/Esprit Ventilator Replacement Parts List . . . . . . . . . 12-1
12.1 Major Components . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12-1
12.1.1 Electronics . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12-2
12.1.2 GUI Assembly . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12-3
12.1.3 Oxygen Pneumatics . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12-7
12.1.4 Air Pneumatics . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12-8
12.1.5 Exhalation Pneumatics . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12-10
12.1.6 Inspiration Pneumatics. . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12-11
12.1.7 Back Panel . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12-12
12.1.8 Cart . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12-13
12.2 Service Part Inventory List . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12-15
12.3 Complete Repair Parts List . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12-17
A Pneumatic Schematics for EST. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-1
A.1 Block Patient Wye (Test 1, Step 2) . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-1
A.2 Block Patient Wye (Test 1, Step 3) . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-2
A.3 Block Patient Wye (Test 1, Step 4) . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-3
A.4 Block Patient Wye (Test 1, Step 5) . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-4
A.5 Safety Valve (Test 2, Step 1) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-5
A.6 Safety Valve (Test 2, Step 2) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-6
A.7 Blower (Test 3, Step 1) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-7
A.8 Blower (Test 3, Step 2) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-8
A.9 Oxygen Supply (Test 4, Step 1) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-9
A.10 Oxygen Supply (Test 4, Step 2). . . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-10
A.11 Crossover Circuit (Test 5, Step 1) . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-11
A.12 Crossover Circuit (Test 5, Step 2) . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-12
A.13 Crossover Circuit (Test 5, Step 3) . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-13
A.14 Oxygen Delivery (Test 6, Step 1) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-14
A.15 Oxygen Sensor (Test 7, Step 1). . . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-15
A.16 Air Delivery (Test 8, Step 1) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-16
A.17 Pressure Relief Valve (Test 9, Step 1) . . . . . . . . . . . . . . . . . . . . . . . . . A-17
A.18 Exhalation Valve (Test 10, Step 1) . . . . . . . . . . . . . . . . . . . . . . . . . . . A-18
A.19 Exhalation Valve (Test 10, Step 2) . . . . . . . . . . . . . . . . . . . . . . . . . . . A-19
A.20 Patient Circuit (Test 11, Step 1) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-20
A.21 Patient Circuit (Test 11, Step 2) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-21
A.22 Heated Filter (Test 12, Step 1) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-22
A.23 Heated Filter (Test 12, Step 2) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . A-23
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. xi
Page 12

Table of Contents
B Field Communications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . B-1
C Respi-Link . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . C-1
Index . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Index-1
xii Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 13
Chapter 1. Introduction and Intended Use
The Esprit and Respironics V200 ventilators are microprocessor-controlled,
electrically powered mechanical ventilators. They are intended for use by
qualified medical personnel to provide continuous or intermittent ventilatory
support for adult, pediatric, and neonatal patients as prescribed by a
physician. They are intended for use in either invasive or non-invasive
applications in institutional environments.
The Esprit and Respironics V200 ventilators meet or exceed all applicable
safety requirements, consensus guidelines, U.S. regulatory statutes, and
international regulatory standards for life support/mechanical ventilation
devices.
Read this manual thoroughly prior to performing service or maintenance on the
ventilators. This manual contains advanced troubleshooting, calibration, and
maintenance instructions. All maintenance and repair work should be
performed by qualified biomedical technicians who have received appropriate
training and authorization to provide maintenance, repair, and service for the
Esprit and Respironics V200 ventilators.
Review the Esprit or Respironics V200 Operator’ s Manual and become familiar
with the operation before running tests, checking operational readiness, or
initiating patient use. The operator’s manual includes important information
about ventilator safety and operation.
Schematic diagrams of the Esprit and Respironics V200 ventilators are
available upon request.
For additional information about accessories or related equipment, such as
humidifiers and remote alarm systems, refer to the appropriate instruction
manual prior to operating the ventilator.
WARNING: Patients on life-support equipment should be visually monitored by competent
medical personnel, since life-threatening circumstances may arise that may
not activate alarms. Heed all appropriate alarms and follow the instructions
and warnings in this service manual and the operator’s manual. Always check
life-support equipment for proper operation before use.
NOTE: The Esprit or Respironics V200 Operator’s Manual lists all applicable
warnings and cautions. Review these notices thoroughly before operating
the ventilator.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 1-1
Page 14
Chapter 1
Introduction and Intended Use
1.1 Recommended
Tools and Test
Equipment
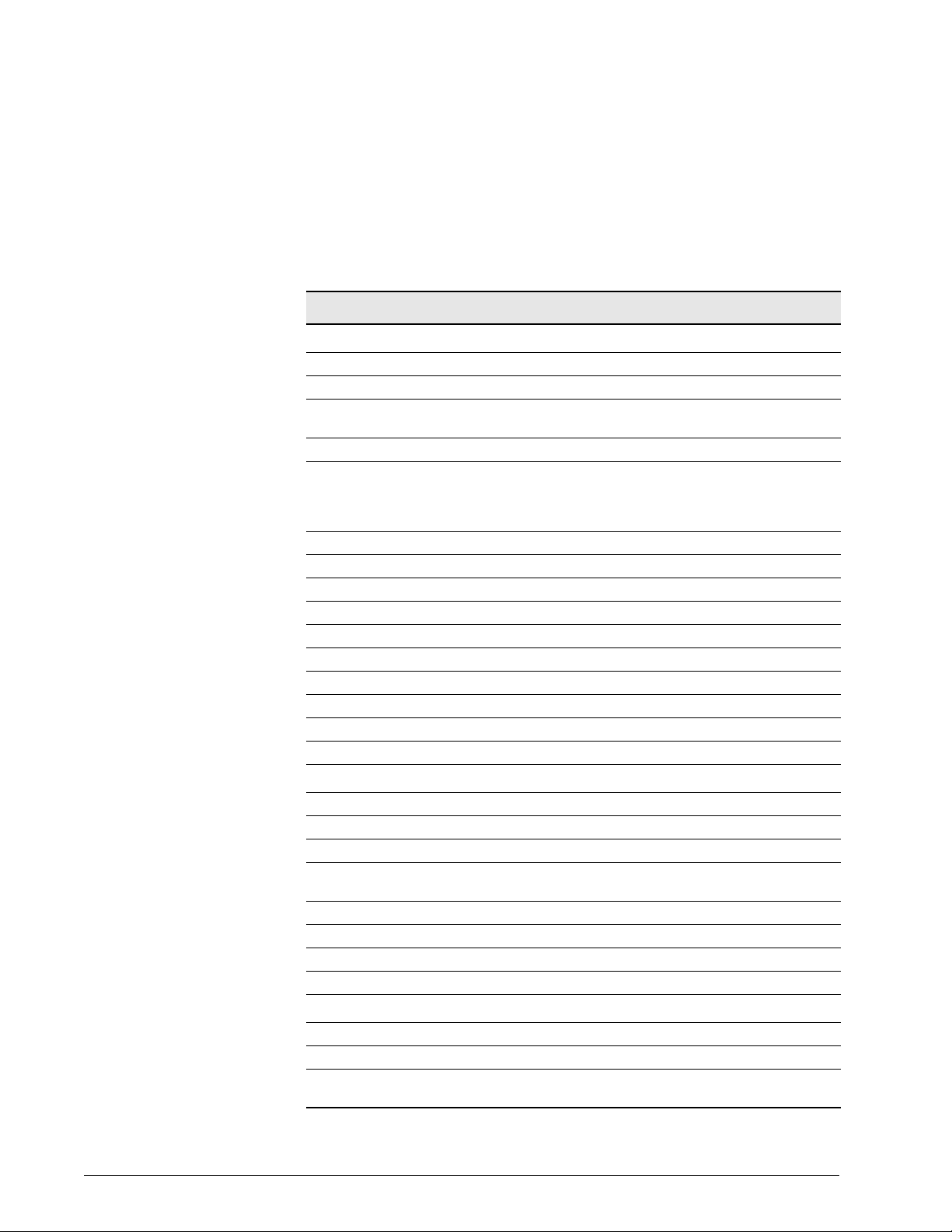
The following table lists the recommended tools, test equipment, and
materials required for ventilator service and maintenance (Table 1-1). Test
equipment must meet the requirements in Table 1-2.
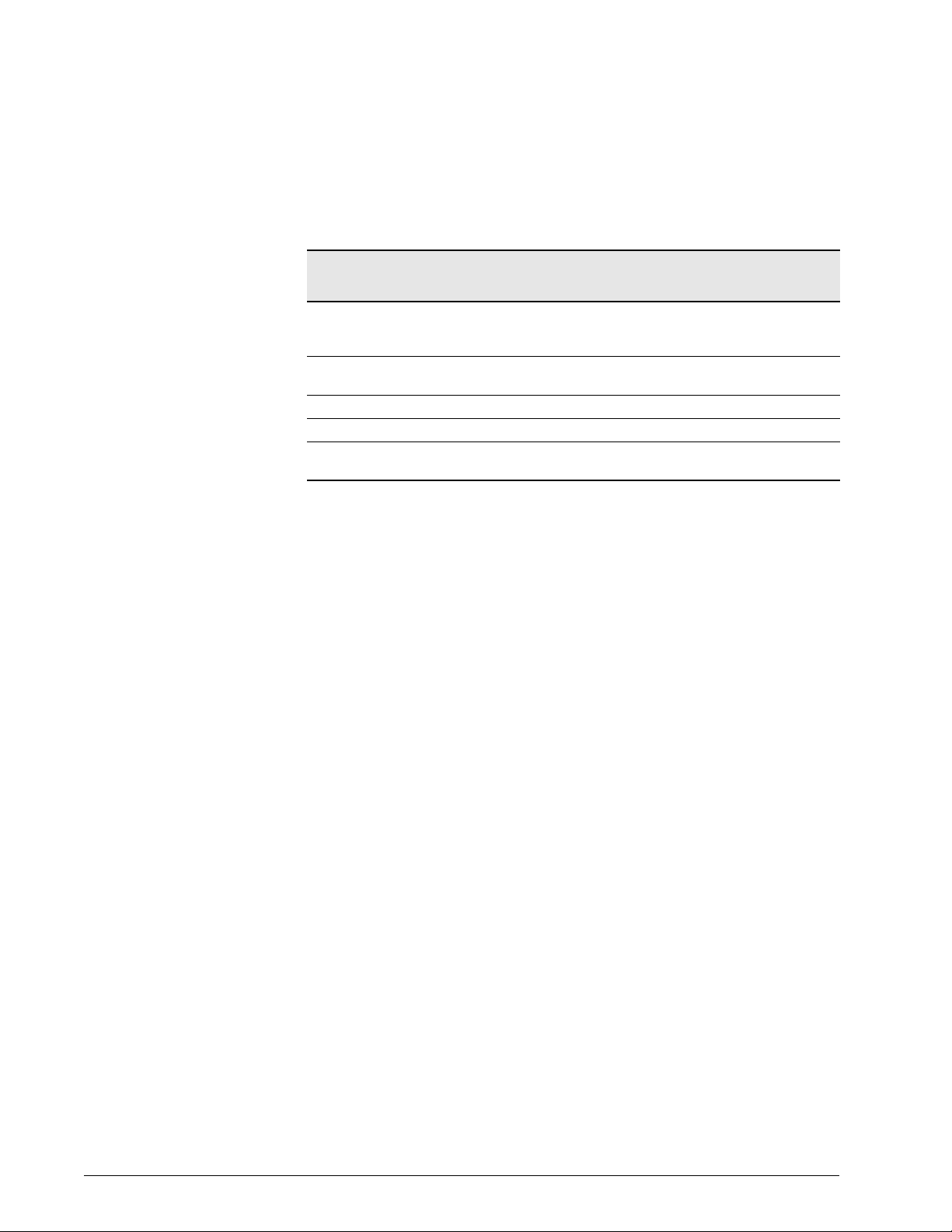
Table 1-1: Recommended Test Equipment, Tools, and Materials
Description Manufacturer and Model
Test Equipment
Adapter, USB to serial Respironics P/N 1022895
Analog output port signal selector Respironics P/N 1010891
Digital multimeter (DMM) and frequency counter
accurate to three decimal places
Electrical safety analyzer Dale LT 544D or equivalent
Pneumatic calibration analyzer capable of
measuring low pressure (cmH
(PSI), flow rate (LPM), volume (liters), and
oxygen concentration (accuracy ± 2%)
Syringe, 10-mL calibrated (neonatal testing) Hans Rudolph 5220 or equivalent
Service kit (*included in the kit) Respironics P/N 1021670
Adapter, oxygen regulator test * Respironics P/N 1001376
Adapter, parallel port * Respironics P/N 1004644
Cable, remote alarm test * Respironics P/N 1027818
Cable adapter, remote alarm test Respironics P/N 1027817
Cable assembly, null modem * Respironics P/N 1022815 or equivalent
Cork, silicone * Respironics P/N 1001735 or equivalent
Test lung, 1 L * Respironics P/N 1021671 or equivalent
O), high pressure
2
Local supplier
Certifier FA Plus Ventilator Gas Analyzer with
oxygen sensor kit (Respironics P/N 1040311
or 1040312) or equivalent
Ventilator Accessories
Adapter, oxygen sensor Respironics P/N 1001736 or equivalent
Connector, plastic, 22mm OD Respironics P/N C06335 or equivalent
Coupling, silicone rubber Respironics P/N C06348 or equivalent
Patient circuit tubes, adult, 42-in. smooth bore
(2 each)
Tee, plastic with silicone rubber coupling Respironics P/N C06260 or equivalent
Tubing, silicone, 3/16 in. ID x 6.5 ft., PAP Respironics P/N C06686 or equivalent
Wye, reusable, 22mm OD/15mm ID Respironics P/N 1003070 or equivalent
Respironics P/N 1003643 or equivalent
Hand Tools and Materials
ESD-safe field service vacuum cleaner 3M model 497-AJM or equivalent
Hex key set, metric (rounded ends), 1.5 to 4 mm Local supplier
Hex key set, standard (rounded ends), 0.050 to
5/32 in.
Local supplier
1-2 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 15
Introduction and Intended Use
Chapter 1
Table 1-1: Recommended Test Equipment, Tools, and Materials (Continued)
Description Manufacturer and Model
Loctite 222 Respironics P/N 200-1000-00
Lubricant, Dupont Krytox GPL226 Res pironics P/N 100-1012-00
Mild detergent or antiseptic wipes Local supplier
PC or laptop (for downloading software) with
Windows 95 or later, serial port and CD ROM
drive
Pliers Local supplier
Pliers, needle nose Local supplier
Ratchet, box, 8 mm Local supplier
Screwdriver, flat head, #2 Local supplier
Screwdriver, flat head, #3 Local supplier
Screwdriver, Phillips head, #2 Local supplier
Screwdriver, pen size flat head Local supplier
Screwdriver, pen size Phillips head Local supplier
Static dissipative field service kit Local supplier
Thread tape Local supplier
Tie wraps, 3 in. length Respironics P/N 500-1000-66 or equivalent
Tie wraps, 8 in. length Respironics P/N 500-1000-62 or equivalent
Tie wrap gun Local supplier
Torque driver capable of 5 to 25 in.-lbs. Local supplier
Tweezers, angled Local supplier
Wire cutters Local supplier
Wrench, open end, 7/32 in. Local supplier
Wrench, open end, 1/4 in. Local supplier
Wrench, open end, 5/16 in. Local supplier
Wrench, open end, 7/16 in. Local supplier
Wrench, open end, 1/2 in. Local supplier
Wrench, open end, 11/16 in. Local supplier
Wrench, open end, 5.5 mm Local supplier
Wrench, open end, 7 mm Local supplier
Wrench, open end or box, #10 Local supplier
Wrench, open end or socket, 3/16 in. Local supplier
Wrench, socket, 9/32 in. with removable 6-in.
extension bar
Wrench, socket, #10 Local supplier
Local supplier
Local supplier
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 1-3
Page 16
Chapter 1
Introduction and Intended Use
Table 1-2: Test Equipment Specifications
Unit of
Measurement
Pressure -25 to 150 cmH2O 0 to
Flow (standard) 0 to 300 SLPM ± 2% of reading ± 0.20 SLPM (whichever is
Torque 5 to 25 in-lb. ± 1 in-lb. of reading
Volume (STP) 0 to 10 L STP ± 2% of reading ± 0.20 L STP
Voltage DC: ± 5 to 50 V
Range Accuracy
100 psi
AC: 2 to 300 V
± 1% of reading or ± 0.20 cmH2O (whichever
is greater). ± 2% of reading @ -1 to 38ºC (30
to 100ºF)
greater)
± 2% of reading
1-4 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 17
Chapter 2. Warnings, Cautions, and Notes
Throughout this manual the following definitions apply:
WARNING: A condition that could cause injury to a patient or operator if the operating
instructions in this manual are not followed correctly.
CAUTION: A condition that could cause damage to, or shorten the service life of,
the Esprit/Respironics V200 Ventilator.
2.1 General Warnings WARNING: Do not obstruct the emergency air intake near the oxygen water trap/inlet
filter assembly.
WARNING: Never troubleshoot while a patient is connected to the ventilator, since normal
operation is suspended.
WARNING: If the ventilator has been operating, the exhalation filter heater conductor may
be hot. Use caution when removing the filter.
WARNING: To prevent disease transmission, use protective equipment when handling
contaminated bacterial filters or other patient accessories.
WARNING: To avoid personal injury, always disconnect external AC and DC power
sources and high-pressure oxygen sources from the ventilator before
servicing.
WARNING: Explosion hazard. Do no operate the ventilator in the presence of flammable
anesthetic agents.
2.2 General Cautions CAUTION: Troubleshooting and repair should be performed only by a qualified
service technician. Respironics Factory Service Training is highly
recommended prior to performing service procedures on the Respironics
Ventilator. Contact Customer Service at 1-800-345-6443 or 724-3874000 for more information.
CAUTION: Use only Respironics ventilator repair/service parts. Only Respironics
parts are designed for use in this ventilator. Use of non-Respironics repair
parts may alter ventilator reliability resulting in damage. Use of nonRespironics repair parts will affect your warranty. Contact Customer
Service at 1-800-345-6443 or 724-387-4000 for more information.
CAUTION: Do not modify oxygen diameter index safety systems (DISS) connector on
rear panel. Use only medical grade oxygen.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 2-1
Page 18

Chapter 2
Warnings, Cautions, and Notes
CAUTION: Always ensure that you are following proper electrostatic discharge (ESD)
grounding procedures before handling static-sensitive devices.
CAUTION: Be careful not to pull or crimp any cables, tubes, or wires.
2.3 General Notes NOTE: This manual covers multiple versions of the Esprit and Respironics V200
Ventilators. The information given may not exactly match your own
ventilator.
2-2 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 19
Chapter 3. Theory of Operation
The Esprit and Respironics V200 ventilators are microprocessor-controlled
devices that can deliver air, oxygen, or a mixture of air and oxygen to the
patient’s lungs in a predetermined manner to augment or replace the work
normally performed by the patient’s respiratory system. It uses
electromechanical control circuits, flow and pressure monitors, and software
programs to deliver breaths as a flow or pressure controller.
The ventilators include a graphic user interface (GUI), internal blower, and
inspiratory module that mixes air and oxygen. The ventilators can operate from
a 40 to 90 psig (276 to 620 kPa) medical grade oxygen source for enriched
oxygen operation. It also includes multiple communications interfaces and an
internal power supply that can run from a 100 to 240 V AC 50/60 Hz or 24 V
DC power sources.
Schematic diagrams of the Esprit and Respironics V200 ventilators are
available upon request.
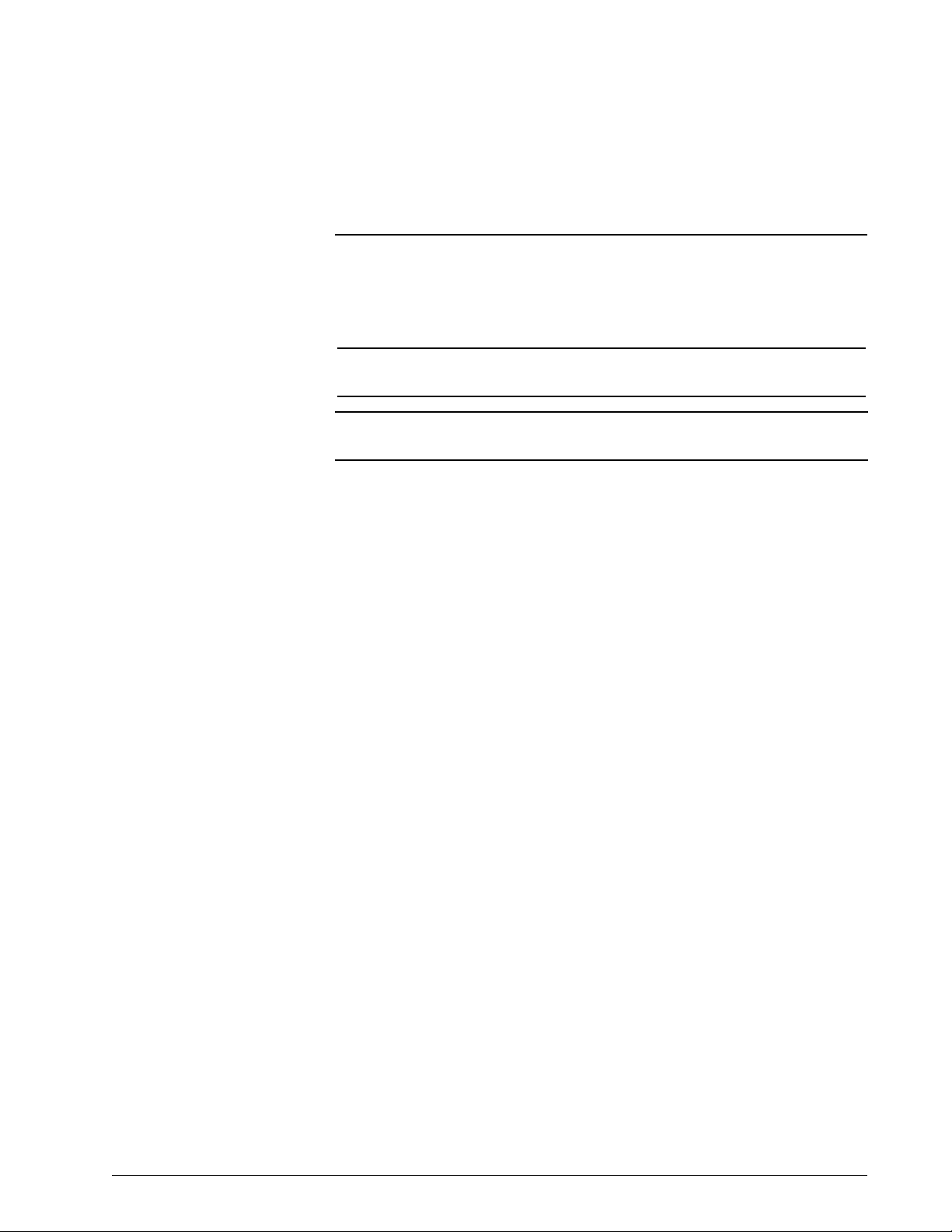
3.1 Pneumatic System
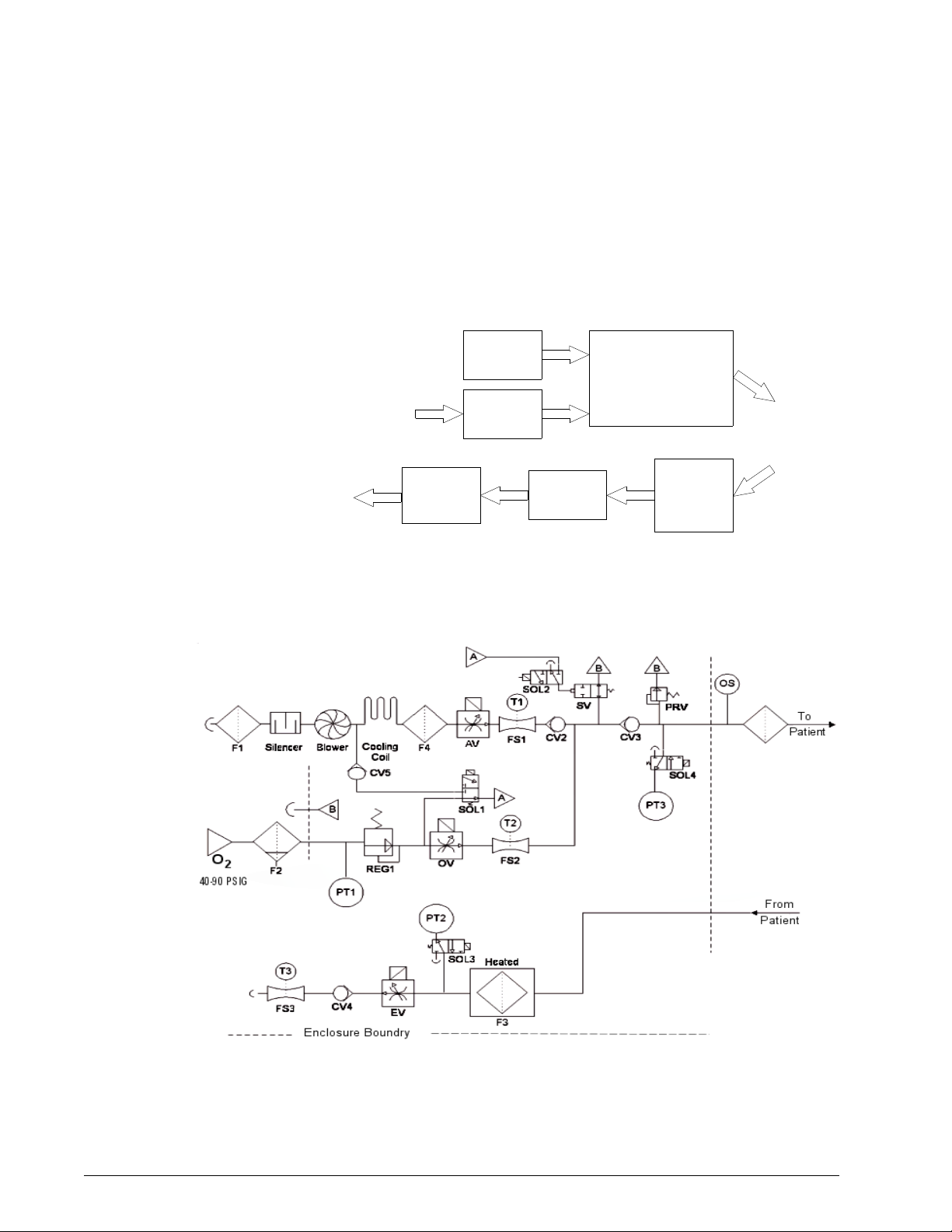
The pneumatic system consists of these subsystems (see Figure 3-1):
• Internal blower (air source)
• Oxygen regulator (oxygen source)
• Inspiratory module
• Heated exhalation filter assembly
• Exhalation valve assembly
• Expiratory flow sensor
The internal blower generates the air pressure necessary for breath delivery,
eliminating the need for an external source of medical-grade compressed air.
An internal oxygen regulator controls wall oxygen pressure. The ventilator
mixes air and oxygen in the inspiratory module before delivery to the patient.
Based on operator settings, the central processing unit (CPU) controls the air
valve, oxygen valve, and exhalation valve through stepper motor controller
printed circuit boards (PCBs). As flow is delivered to the patient, the air and
oxygen flow sensors and two pressure sensors provide feedback to the CPU.
The pressure relief and safety valves in the inspiratory module provide for
patient safety in the event of an over-pressure condition or any component or
system failure that could interfere with the patient’s ability to breathe when
connected to the ventilator.
REF 580-1000-02 H Esprit® / V200 Ventilator Service Manual © Respironics, Inc. 3-1
Page 20
Chapter 3
Blower
Oxygen
Regulator
Inspiratory Module
• Gas Mixing
• Pressure Relief Valve
• Safety Valve
To P at ien t
From Patient
Heated
Exhalation
Filter
Assembly
Exhalation
Valve
Expiratory
Flow
Sensor
Room
Air
Oxygen
Supply
Air
O
2
Theory of Operation
The exhalation filter reduces the risk of contamination or component damage
due to bacteria or moisture in expired gases. The exhalation filter is housed in
a heated sleeve, which reduces the relative moisture condensation in the
exhalation filter, exhalation valve, and expiratory flow sensor. Exhaled gas is
then vented to atmosphere.
Figure 3-1: Pneumatic System Block Diagram
Figure 3-2 shows the pneumatic system and its components.
3-2 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Figure 3-2: Pneumatic Schematic
Page 21

Chapter 3
Theory of Operation
3.1.1 Blower Inlet Filter (F1)
The blower draws room air through the blower inlet filter (F1) and the muffler
(silencer) and outputs flow to the air valve assembly (AV). The blower inlet
filter removes coarse particulate from ambient air as it is entrained into the
blower assembly. See Chapter 4 for periodic maintenance information.
3.1.2 Muffler (Silencer)
The muffler reduces the noise of air flow into the blower by channeling the air
through a baffled system lined with sound absorbing material.
3.1.3 Blower
The blower draws room air though the air inlet filter and outputs the air that is
delivered to the patient, and provides the pilot pressure that can actuate the
safety valve. The blower contains a DC motor and a series of stator and
impeller assemblies. It can provide at least 200 LPM of flow.
Blower speed is automatically adjusted to account for differences in gas
density due to altitude. The altitude can be adjusted from the hardware screen
in Diagnostics mode. The high pressure alarm limit setting also affects blower
speed.
3.1.4 Cooling Fan Filter
The cooling fan filter removes coarse particulate from ambient air entrained by
the cooling fan. See Chapter 4 for periodic maintenance information.
3.1.5 Cooling Coil
The cooling coil is a copper tube connected to the outlet of the blower
dissipate heat from gas leaving the blower before it reaches the air valve.
3.1.6 Cooling Coil Fan
The 24 V DC cooling coil fan removes the heat dissipated by the cooling coil
and blower.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 3-3
Page 22

Chapter 3
Oxygen
inlet
connector
Theory of Operation
3.1.7 Air Valve Assembly (AV)
The air valve assembly includes a stepper motor that meters air flow from the
blower to achieve the target flow under CPU control, based on operator
selected parameters. It can deliver up to 200 LPM of flow.
3.1.8 Air Flow Sensor (FS1)
The air flow sensor measures flow from the air valve. The ventilator uses this
measurement to provide closed loop control of the air valve and to compute the
flow and volume delivered to the patient. A thermistor in the flow sensor
measures the temperature of the air and provides the microprocessor with
information to compensate the delivered flow.
3.1.9 Oxygen Water Trap/Inlet Filter Assembly (F2)
The oxygen water trap/inlet filter assembly consists of a 5-micron (µ) filter to
remove particulate (both dry and liquid) from the oxygen gas supply, a bowl
with drain for accumulated water, and an oxygen inlet connector.
3.1.10 Oxygen Inlet Connector (O2)
The oxygen inlet connector provides a country-specific connection point for an
external oxygen gas supply of 40 to 90 psig (276 to 620 kPa).
3.1.11 Oxygen Supply Pressure Switch (PS1)
The oxygen supply pressure switch is part of the oxygen regulator. PS1 is a
normally open (NO) switch that monitors oxygen supply pressure by closing
when measured pressure is over 40 psig (276 kPa), and sends a signal to the
sensor PCB to indicate if supply pressure is adequate at the oxygen inlet.
PS1 opens if measured pressure is less than 35 psig (241.3 kPa). If the
oxygen supply pressure switch opens during normal ventilation (at O
> 21%),
2
a low oxygen supply alarm results.
3.1.12 Oxygen Regulator (REG 1)
The oxygen regulator reduces the oxygen supply pressure to the proper inlet
pressure for the oxygen valve (22-24 psig, or 152-165 kPa @ 180 LPM) and
supplies the regulated pressure to the crossover solenoid, which pilots the
safety valve.
3-4 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 23
Chapter 3
SOL2
Theory of Operation
3.1.13 Oxygen Valve (OV)
The oxygen valve assembly contains a stepper motor that meters flow from the
oxygen regulator to achieve the target flow under CPU control, based on
operator-selected parameters. It can deliver up to 200 LPM of flow.
3.1.14 Oxygen Flow Sensor (FS2)
The oxygen flow sensor measures the flow from the oxygen valve. The ventilator
uses this measurement to provide closed loop control of the oxygen valve and
to compute the flow and volume delivered to the patient. A thermistor
contained in the flow sensor measures the temperature of the oxygen and
provides temperature compensation information to the microprocessor for
delivered flow.
3.1.15 Crossover Solenoid (SOL1)
The crossover solenoid is a three-way valve that supplies either air or oxygen
pressure to pilot (hold) the safety valve closed during normal ventilation. In its
normal state, SOL1 is normally de-energized to pilot the safety valve with
oxygen. If oxygen pressure is lost, SOL1 is energized and air (rather than
oxygen) controls the safety valve.
3.1.16 Cross-Contamination Check Valve (CV5)
The cross-contamination check valve prevents the oxygen supply from entering
the air delivery system (blower) in the event of a crossover solenoid leak.
3.1.17 Safety Valve Pilot Solenoid (SOL2)
SOL2 directs the output of the crossover solenoid to the safety valve or vents
the pilot pressure line to atmosphere.
During normal operation, SOL2 is energized and directs pressure from the
crossover solenoid to close the safety valve. During a high priority alarm
condition such as an occlusion or ventilator failure (VENT INOP) mode, SOL2
is deenergized, the safety valve opens, and the patient can breathe room air.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 3-5
Page 24
Chapter 3
O ring
Diaphragm
Spring
CV2
CV3
PT3
Sensor PCB
Theory of Operation
3.1.18 Safety Valve (SV)
The safety valve contains a spring-loaded diaphragm that is controlled by
safety valve pilot solenoid (SOL2). Under normal conditions the safety valve is
closed, allowing delivered flow to reach the patient. In the event of a safety
valve open (SVO) condition, pilot pressure is vented to atmosphere, which
opens the safety valve and allows the patient to breathe room air through the
safety port at the back of the ventilator.
3.1.19 Air System Check Valve (CV2)
CV2 prevents oxygen from entering the air delivery system in the event of a
blower failure.
3.1.20 Inspiratory Non-Rebreathing Check Valve (CV3)
CV3 prevents the patient from exhaling through the inspiratory limb during a
safety valve open condition, which prevents the patient from rebreathing
exhaled gas.
3.1.21 Pressure Relief Valve (PRV)
The pressure relief valve provides a backup to the operator adjustable highpressure alarm and prevents excessive pressures in the patient circuit. The
pressure relief valve is spring-loaded to limit the maximum circuit pressure to
130 to 140 cmH
O.
2
3.1.22 Oxygen Sensor (OS)
The optional oxygen sensor is installed between the 22-mm inspiratory port
and the inspiratory bacteria filter. The galvanic oxygen sensor measures the
oxygen concentration of the blended gas as it leaves the inspiratory manifold.
The output signal from the sensor is used to determine whether measured
oxygen concentration is within 6% of the %O
setting. If not, a high or low
2
oxygen concentration alarm occurs.
3.1.23 Inspiratory Pressure Transducer (PT3)
PT3 on the sensor PCB monitors system pressure from the inspiratory side of
the patient circuit during exhalation pressure transducer autozeroing, ensuring
uninterrupted pressure monitoring. PT3 is also used with the exhalation
pressure transducer (PT2) to detect patient circuit occlusions.
3-6 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 25
Chapter 3
SOL4
PT2
Sensor PCB
SOL3
Theory of Operation
3.1.24 Inspiratory Pressure Transducer Solenoid (SOL4)
SOL4 periodically vents the inspiratory pressure transducer to atmosphere and
makes a measurement at zero (atmospheric) pressure. Periodically autozeroing
the transducer allows it to correct the slight zero voltage drift that can occur
over time, and improves the overall accuracy of the pressure measurement.
During normal operation, SOL4 is de-energized and applies patient circuit
pressure to the inspiratory pressure transducer. During an autozero, SOL4 is
energized, venting the transducer to atmosphere. This occurs during power on
self test (POST), at the beginning of a breath one minute after POST, six
minutes after POST, eleven minutes after POST, and hourly thereafter.
3.1.25 Heated Exhalation Filter (F3)
The heated exhalation filter includes a heated filter sleeve and a bacteria filter.
The heater protects the exhalation flow sensor and exhalation system
components from condensation by heating exhaled gas (which has cooled in
the exhalation limb) above its dew point.
The exhalation bacteria filter protects the exhalation flow sensor and
exhalation system component from contaminants and filters exhaled gas
before it is vented to atmosphere.
3.1.26 Exhalation Pressure Transducer (PT2)
The exhalation pressure transducer on the sensor PCB measures patient circuit
pressure from the exhalation side of the patient circuit. During normal
operation PT2 is the primary transducer for measuring patient pressures,
including peak inspiratory pressure (PIP), mean airway pressure (MAP), end
inspiratory pressure, and auto-PEEP. The exhalation pressure transducer
provides monitoring data for closed loop control.
3.1.27 Exhalation Pressure Transducer Solenoid (SOL3)
The exhalation pressure transducer solenoid periodically vents the exhalation
pressure transducer to atmosphere and measures zero (atmospheric) pressure.
Periodically autozeroing the transducer allows it to correct the slight zero
voltage drift that can occur over time, and improves overall pressure
measurement accuracy.
During normal operation, SOL3 is de-energized and applies patient circuit
pressure to the exhalation pressure transducer. During an autozero, SOL3 is
energized, venting the transducer to atmosphere. This occurs during POST, at
the beginning of a breath one minute after POST, six minutes after POST,
eleven minutes after POST, and hourly thereafter.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 3-7
Page 26
Chapter 3
CV4
Theory of Operation
3.1.28 Exhalation Non-Rebreathing Check Valve (CV4)
CV4 prevents the patient from inspiring room air through the exhalation limb of
the patient circuit. During normal operation, it blocks the exhalation system
from atmosphere, allowing the patient to trigger a breath.
3.1.29 Exhalation Valve (EV)
The exhalation valve is controlled by a stepper motor. At the beginning of an
inspiration, the exhalation valve shuts to create a closed circuit and allow the
patient system to pressurize. The exhalation valve opens at the beginning of
exhalation, allowing system pressure to vent to atmosphere.
The exhalation valve also regulates positive end expiratory pressure (PEEP) and
expiratory positive airway pressure (EPAP) levels during exhalation.
3.1.30 Exhalation Flow Sensor (FS3)
The exhalation flow sensor measures the flow leaving the ventilator, which
includes gas exhaled by the patient, tubing compliance volume, and bias flow
(if flow triggering or Auto-Trak triggering is selected). The ventilator uses the
exhaled flow measurement to compute flow and volume coming from the
patient and the circuit.
A thermistor in the flow sensor measures the temperature of the gas and
provides the microprocessor with information to compensate the measured
flow.
3-8 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 27
Chapter 3
Theory of Operation
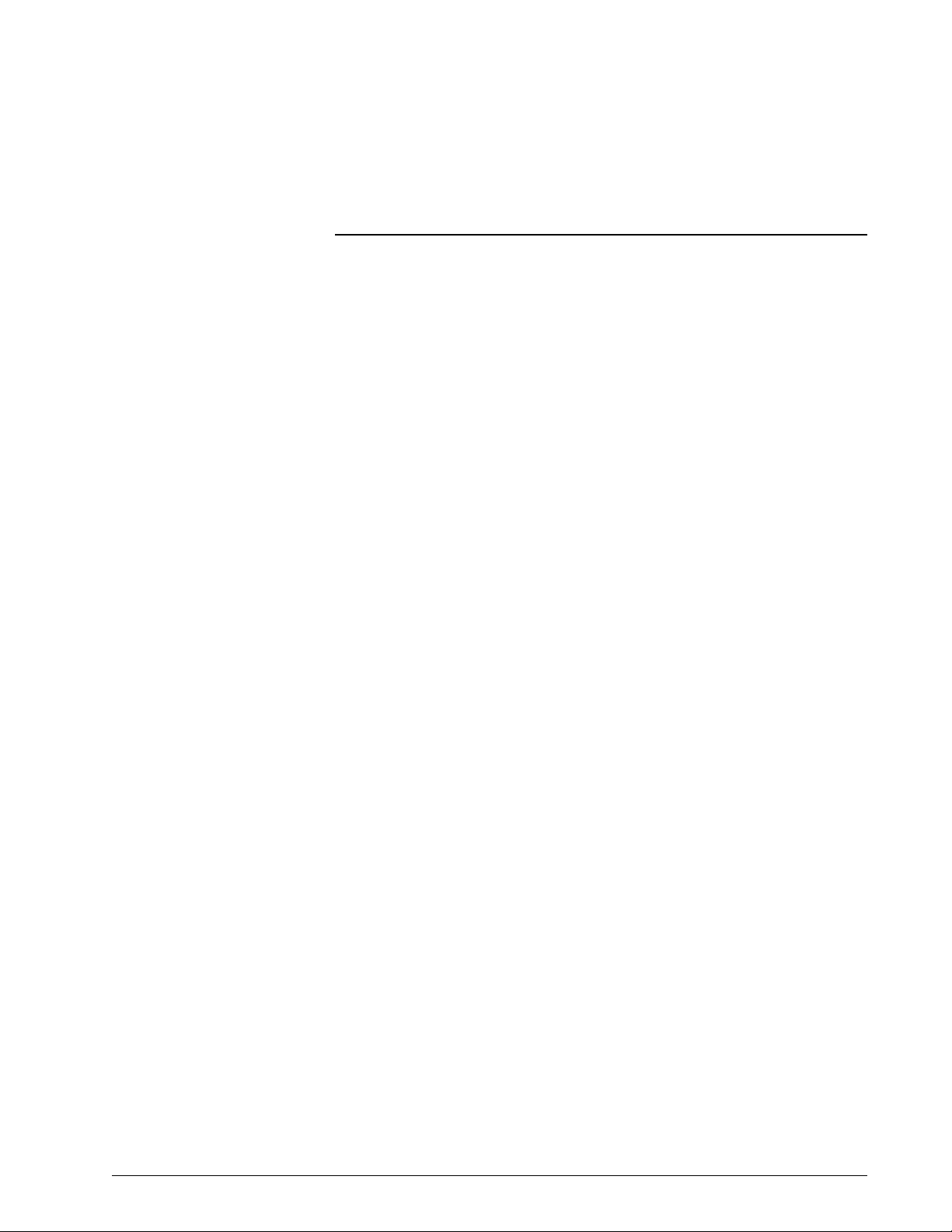
3.2 Ventilator System Electronics
Figure 3-3 shows the electronic system. Schematics are available upon
request.
Figure 3-3: Electronic System Diagram
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 3-9
Page 28
Chapter 3
Theory of Operation
The ventilator can be powered by a 100 to 240 VAC 50/60 Hz or external 24 V
DC power source (backup battery or external battery). The power supply
conditions the input voltage and distributes + 5 V, +12 V, -12 V, a n d + 2 9 V t o
the main PCB and blower motor controller to power digital electronics,
electropneumatic components, and displays. AC power to the humidifier port
can be used on 100-120 V units only.
The microprocessor on the CPU PCB and programs stored in memory control
the interaction of the pneumatic and electronic subsystems. Using inputs from
electropneumatic sensors and the operator, the CPU controls the flow,
pressure, and volume of air and oxygen to be delivered to the patient. The CPU
also monitors alarms and independently monitors software execution.
The the CPU PCB, digital PCB, analog PCB, VGA controller PCB, and three
stepper motor controller PCBs are vertically mounted on the main PCB.
Digital control signals from the CPU are sent to the analog PCB, where they are
converted into analog signals that control blower speed and chart recorder
outputs (pressure, flow, and volume). The sensor PCB conditions and converts
analog data from the flow, pressure, and oxygen sensors, then sends the data
to the analog PCB, where it is read by the CPU.
Ventilator data from the CPU is conditioned by the VGA and man-machine
interface (MMI) PCBs, then displayed on an LCD.
Table 3-1 summarizes the electronic signal path sequences for the ventilator
components.
Table 3-1: Signal Path Sequences
Component Signal Path Sequence
100% O
29 V enable Main PCB, CPU PCB, power supply
Air (AV), oxygen (OV), exhalation
(EV) valves
Air (FS1), oxygen (FS2), exhalation
(FS3) flow sensors
Alarm High indicator Front panel overlay, MMI PCB, main PCB, CPU PCB
Alarm Med/Low indicator Front panel overlay, MMI PCB, main PCB, CPU PCB
Alarm Silence indicator Front panel overlay, MMI PCB, main PCB, digital PCB, CPU
Backlight (9.5 in display, standard
on Esprit ventilator)
Backlight (10.4-in display,
optional on Esprit ventilator,
standard on Respironics V200
ventilator)
indicator Front panel overlay, MMI PCB, main PCB, digital PCB, CPU
2
PCB
Main PCB, motor controller PCB, CPU PCB
Sensor PCB, main PCB, analog PCB, CPU PCB
PCB
Backlight inverter PCB, DC/DC converter PCB, main PCB,
backlight control potentiometer
Backlight inverter PCB, DC/DC converter PCB, main PCB,
backlight control potentiometer
3-10 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 29
Chapter 3
Theory of Operation
Table 3-1: Signal Path Sequences (Continued)
Component Signal Path Sequence
Backup alarm MMI PCB, main PCB, digital PCB, CPU PCB
Battery/Charging indicator Front panel overlay, MMI PCB, power supply, main PCB,
CPU PCB
Battery/In Use indicator Front panel overlay, MMI PCB, main PCB, digital PCB, CPU
PCB
Battery/Low indicator Front panel overlay, MMI PCB, digital PCB, CPU PCB
Blower DAC Blower controller PCB, sensor PCB, main PCB, analog PCB,
Blower on/off Blower controller PCB, sensor PCB, main PCB, CPU PCB
Blower temperature switch Sensor PCB, main PCB, digital PCB, CPU PCB
Console: all keys Front panel overlay, MMI PCB, main PCB, CPU PCB
Crossover solenoid (SOL1) Main PCB, CPU PCB
Enclosure temperature sensor Sensor PCB, main PCB, analog PCB, CPU PCB
Exhalation pressure transducer
(PT2)
Exhalation pressure transducer
solenoid (SOL3)
External backup battery Power supply
External Battery indicator Front panel overlay, MMI PCB, power supply
Heater Main PCB, CPU PCB
Inspiratory pressure transducer
(PT3)
Inspiratory pressure transducer
solenoid (SOL4)
Mains indicator Front panel overlay, MMI PCB, power supply
Nonmaskable interrupt (NMI)
signal
Normal indicator Front panel overlay, MMI PCB, main PCB, CPU PCB
Oxygen Sensor (OS) Sensor PCB, main PCB, analog PCB, CPU PCB
Oxygen supply pressure switch
(PS1)
Primary alarm MMI PCB, main PCB, digital PCB, CPU PCB
Primary alarm potentiometer MMI PCB
Printer Main PCB, CPU PCB
Remote alarm (nurse call) Main PCB, CPU PCB
Rotary encoder MMI PCB, main PCB, digital PCB, CPU PCB
Safety Valve indicator Front panel overlay, MMI PCB, main PCB, CPU PCB
Safety valve pilot solenoid (SOL2) Main PCB, CPU PCB
Screen Lock indicator Front panel overlay, MMI PCB, main PCB, CPU PCB
Touch screen MMI PCB, main PCB, digital PCB, CPU PCB
Vent Inop indicator Front panel overlay, MMI PCB, main PCB, CPU PCB
CPU PCB
Sensor PCB, main PCB, analog PCB, CPU PCB
Main PCB, CPU PCB
Sensor PCB, main PCB, analog PCB, CPU PCB
Main PCB, CPU PCB
Sensor PCB, main PCB, CPU PCB
Sensor PCB, main PCB, digital PCB, CPU PCB
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 3-11
Page 30
Chapter 3
Theory of Operation
Table 3-1: Signal Path Sequences (Continued)
Component Signal Path Sequence
VGA backlight intensity
potentiometer (9.5 in display,
standard on Esprit ventilator)
VGA backlight intensity
potentiometer (10.4-in display,
optional on Esprit ventilator,
standard on Respironics V200
ventilator)
VGA display (9.5 in display,
standard on Esprit ventilator)
VGA display (10.4-in display,
optional on Esprit ventilator,
standard on Respironics V200
ventilator)
MMI PCB, backlight inverter PCB
Backlight inverter PCB
MMI PCB, main PCB, VGA controller PCB, CPU PCB
Main PCB, VGA controller PCB, CPU PCB
3.2.1 Main PCB
The CPU and other ventilator logic interact through the system data, address,
and control buses on the main PCB. The main PCB receives input signals from
various keys on the console or touch screen display and sends them to the
CPU. The main PCB also contains signal inputs for non-maskable interrupt,
running on AC, and running on external battery.
The main PCB receives control signals from the CPU and outputs them to
various pneumatic components and console indicators. The main PCB receives
signals from the digital PCB to turn on the indicators for alarm silence, 100%
oxygen, AC power, external battery power, and backup battery status. The main
PCB receives signal from the CPU PCB to turn on the backup alarm, enable
24V, and the Screen Lock, Battery/Chargi ng, and Vent Inop indicators. The
CPU PCB reads the Accept key from the main PCB.
The main PCB includes a normal open and normal closed relay that can trigger
the remote nurse call alarm. The main PCB also includes the RS-232, parallel
printer, analog output, and remote alarm connectors.
The main PCB also routes these signals: reset, MMI PCB reset, sensor PCB
reset, primary alarm, primary alarm failure detection logic, backup alarm,
remote alarm, printer, POST timer, clocked serial interface (CSI) signals, and
the battery backed +3.6 V.
3-12 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 31

Chapter 3
Theory of Operation
3.2.2 CPU PCB
The CPU PCB contains the microprocessor, memory, I/O ports, and associated
control circuitry that controls the ventilator:
• V851 microprocessor with a 25-MHz clock
• Static RAM that stores ventilator data
• EEPROM that stores patient settings
• Flash memory that contains ventilator operating software
• One time programmable (OTP) memory that stores the POST routine
• Internal RS-232 port that receives ventilator data from the touch
screen
• Nonmaskable interrupt that tells the CPU a power source has been
lost or interrupted
• 5-msec bus timer that monitors hardware operation
• 169-msec watchdog timer that monitors software operation
• Data address and control bus to the main PCB
• 2-MB memory capacity
3.2.3 Analog PCB
The analog PCB converts digital signals to analog signals to the blower
controller PCB and analog output port. The analog PCB connects directly to
the system bus on the main PCB, and includes these functional circuits:
• An eight-bit digital to analog converter (DAC) that converts digital
signals from the CPU to analog for the blower and external devices
such as chart recorders and bedside monitors
• Clocked serial interface (CSI), a high-speed communication link
between the air, oxygen, and exhalation motor controllers and flow
sensor lookup tables contained on the CPU and the voltage monitor
register
• A circuit that retrieves converted data from the sensor PCB
3.2.4 Digital PCB
The digital PCB conditions serial port signals coming from and going to the
CPU PCB. It also contains control circuitry for the power fail alarm, primary
alarm, backup alarm, RS-232 port, and rotary encoder.
Digital inputs include analog-to-digital converter (ADC) out of range,
compressor temperature switch, and oxygen present. Digital outputs include
the alarm silence indicator, 100% oxygen indicator, running on AC indicator,
running on external battery indicator, backup battery status indicators, printer
ready signal, and printer direction.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 3-13
Page 32

Chapter 3
Theory of Operation
3.2.5 VGA Controller PCB
The VGA controller PCB contains the date and real time clock and LCD VGA
display controller drivers.
3.2.6 Blower Controller PCB
The blower motor controller PCB controls the speed of the blower motor based
on analog input conditioned by the sensor PCB. It includes a lockup sensing
circuit, which monitors sensors in the blower motor to detect a locked rotor
condition. If the blower motor stops running, the lockup sensing circuit shuts
off power to the blower.
3.2.7 Motor Controller PCBs
There are three motor controller PCBs for the air valve, oxygen valve, and
exhalation valve. The three boards are physically the same and are
differentiated by the slot they occupy on the main PCB:
• Exhalation valve motor controller PCB: slot CN11
• Oxygen valve motor controller PCB: slot CN12
• Air valve motor controller PCB: slot CN13
Each motor controller PCB includes a microprocessor dedicated to controlling
the corresponding motor and driving the step positions of the motor based on
input from the CPU.
3.2.8 Sensor PCB
The sensor PCB contains an analog to digital converter (ADC) that converts
analog signals from various pneumatic components and the power supply into
digital signals for the CPU. Signals include: air flow and temperature, oxygen
flow and temperature, exhalation flow and temperature, inspiratory and
exhalation pressure, battery voltage, FIO
enclosure oxygen concentration.
The sensor PCB conditions blower speed analog input and the on/off control to
the blower controller PCB. It also routes signals for the oxygen pressure and
blower temperature switches.
, enclosure temperature, and
2
The sensor PCB also includes voltage LEDs that light to indicate under- and
over-voltage conditions.
3-14 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 33

Chapter 3
3.6-V lithium
battery (original
Esprit ventilator)
3.2-V button battery
(current Esprit/
Respironics V200
ventilator)
Theory of Operation
3.2.9 Man-Machine Interface (MMI) PCB
The MMI PCB interfaces the front panel overlay, VGA display, rotary encoder,
and touch screen to the CPU via the main PCB. The MMI PCB contains control
circuitry for the primary and back-up alarms, and includes the hard keys and
LEDs on the front panel membrane keypad.
3.2.10 Power Supply
The power supply converts AC voltage to DC voltage to be used by the system
electronics. The switching power supply can accept voltage from 100 to 240 V
AC (50/60 Hz), and converts it to +5 V, + 12 V, and +29 V DC voltages. In the
absence of AC voltage, the power supply converts the +24V DC input voltage
from an external DC power source (Backup Battery or External Battery). The
power supply also includes power fail logic and charging circuitry for the
backup battery.
The power supply is cooled by a 24 VDC fan housed in a shroud covering the
power supply PCB.
3.2.11 Backlight Inverter PCB
The backlight inverter PCB converts 12 V to approximately 500 V to drive the
backlight on the VGA display assembly.
WARNING: The backlight inverter PCB generates high voltage. To avoid personal injury,
verify that the AC and external DC power sources (backup battery or external
battery) are disconnected from the ventilator.
3.2.12 Real-Time Clock Battery
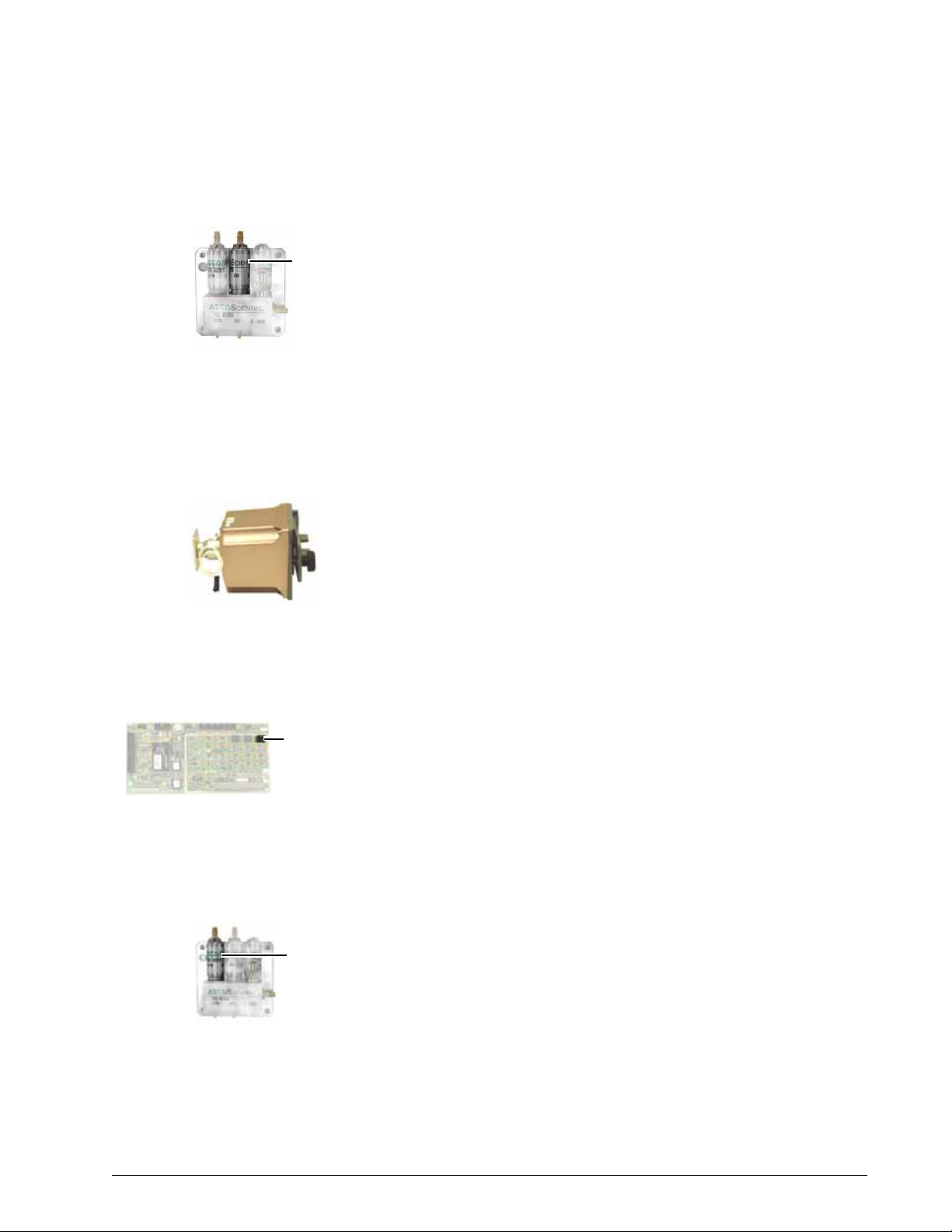
The Esprit ventilator originally included a 3.6-V lithium real-time clock/backup
alarm battery. The Esprit/Respironics V200 ventilators currently use a 3.2-V
button battery installed on the main PCB.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 3-15
Page 34

Chapter 3
Esprit
ventilator
backup
battery
Respironics
V200
ventilator
backup
battery
Respironics
V200
ventilator
GUI
Esprit
ventilator GUI
Theory of Operation
3.2.13 Backup Battery
The 24-V backup battery can power the ventilator for approximately 30
minutes at nominal settings in case of AC power loss.
3.2.14 External Battery
The optional external battery supplements the backup battery, and can provide
an additional two hours of ventilator operation (depending on ventilator
settings). The ventilator runs on AC power when available, then external
battery power if installed, and then backup battery power.
3.2.15 DC/DC Converter PCB
The DC/DC converter PCB converts a 5-V input to a 12-V output for the original
10.4-inch display backlight inverter PCB. This PCB is not used in current
displays.
3.2.16 Optical Rotary Encoder
The optical rotary encoder converts the mechanical position of the user
interface knob into a representative electrical signal using a patterned disk or
scale, a light source, and photosensitive elements.
3.2.17 Graphic User Interface (GUI)
The GUI includes an infrared (IR) touchframe that contains 24 vertical and 32
horizontal IR emitter detector pairs, each of which is sequenced at a high
frequency. When the screen is touched, breaking the IR beam, the x and y
coordinates that correspond to the position on the screen are communicated to
the microprocessor.
The GUI on Esprit ventilators is equipped with a 9.5-inch monochrome or a
10.4-in. color-capable liquid crystal display (LCD). The GUI on Respironics
V200 ventilators is equipped with a 10.4-inch color-capable LCD. The 10.4inch color-capable LCD is a 640 x 480 active matrix display.
3-16 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 35

Chapter 3
NO
NC
Common
Ring
Tip
Sleeve
Remote alarm
connector and cable
Theory of Operation
3.2.18 Remote Alarm (Nurse Call)
The remote alarm contacts provide remote alarm capability, allowing the
ventilator to annunciate an active medium or high priority alarm at a location
away from the ventilator. Pressing Alarm Silence mutes the remote alarm.
The ventilator signals an alarm condition using normally open (NO) or normally
closed (NC) relay contacts, where the deenergized state indicates an active
alarm. The remote alarm port is a standard ¼-in. phone jack (ring, tip, sleeve)
connector (Figure 3-4).
• When the ring and sleeve are used, the relay is open during normal
ventilator operation and closed when an alarm is active or the
ventilator is off.
• When the tip and sleeve are used, the relay is closed during normal
operation and open when an alarm is active or the ventilator is off.
CAUTION: The remote alarm port is intended to connect only to SELV (safety
extra low voltage and ungrounded system with basic insulation to
ground), in accordance with IEC 60601-1. To prevent damage to
the remote alarm, the signal input should not exceed the
maximum rating
1
mA.
of 24 VAC or 36 VDC at 500mA with a current of
Figure 3-4: Remote Alarm (Nurse Call) Connector
The 15-pin analog output (chart recorder) port of the ventilator can also be
used to connect to the Respironics Lifecare remote alarm system. The Lifecare
remote alarm sounds under these conditions:
• A high or medium priority alarm condition is active
• Ventilator power is turned off or disconnected.
• The Respironics Lifecare remote alarm system is disconnected from
the ventilator
• The ventilator runs POST
NOTE: To connect the Lifecare remote alarm system to the ventilator, a DB15 to
BNC cable adapter must be installed into the analog output port.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 3-17
Page 36

Chapter 3
Theory of Operation
(This page is intentionally blank.)
3-18 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 37

Chapter 4. Periodic Maintenance
Perform periodic maintenance (PM) procedures (Table 4-1) to ensure
consistent optimal ventilator operation. The annual and 12,500-hour PM kits
are intended to be installed only by a qualified service technician. The Esprit
or Respironics V200 Ventilator Operator’s Manual summarizes the PM
schedule.
Table 4-1: Periodic Maintenance Schedule
Frequency Component Maintenance
During ventilator
setup
At least daily, and as
recommended by
filter manufacturers
At least daily • Oxygen supply water trap and
• Inspiratory bacteria filter • Check filter for occlusions, cracks, and tears.
• Inspiratory and expiratory filters • Ensure that the ventilator functions normally with both filters in
• Ventilator and patient circuit
components
• Inspiratory and expiratory filters • Monitor filter performance and replace as needed. Changes in
filter
place.
• Perform Short Self-Test (SST) whenever circuit components are
changed (Chapter 5).
• Perform Extended Self-Test (EST) between patient uses (Chapter 5).
expiratory resistance that can indicate expiratory filter damage.
• Follow filter manufacturer recommendations regarding duration of
use, maintenance (for reusable filters), and disposal. Note that high
humidity and aerosol medications can reduce expiratory filter life,
increase expiratory resistance, or cause filter damage.
CAUTION: Do not operate the ventilator without a properly
functioning expiratory filter and heater. Doing so may
cause damage to delicate ventilator components, such
as the expiratory flow sensor, which may lead to
inaccurate spirometry or a Vent Inop condition.
WARNING: Vent Inop is a serious condition which is indicated by both
visual and audible alarms. If the ventilator is attached to a
patient when Vent Inop occurs, the patient must be
supported with another means of life support ventilation.
• Check and empty as required every shift.
At least every 250
hours
Annually • Annual PM kit (P/N 1034840). • Clean ventilator interior and exterior (section 4.1).
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 4-1
• Air inlet and fan filters • Inspect and clean. Lint and dust can accumulate more quickly in
some environments: inspect and clean more frequently if required.
• Install annual PM kit (section 4.2).
• Complete performance verification procedure (Chapter 8).
CAUTION: The annual preventive maintenance procedure is to be
performed only by a qualified service technician.
Page 38

Chapter 4
Periodic Maintenance
Table 4-1: Periodic Maintenance Schedule (Continued)
12,500 hours • 12,500-hour PM kit
As required • External oxygen sensor • Replace and run EST to recalibrate new sensor (Chapter 5).
4.1 Cleaning the Ventilator
(P/N 1001733).
• Backup battery • If the backup battery option is installed, charge and maintain
Clean the ventilator before installing a PM kit:
1. Generate a ventilator diagnostic report (DRPT) (Chapter 7).
• Clean ventilator interior and exterior (section 4.1).
• Install the12,500-hour PM kit (section 4.3).
• Complete performance verification procedure (Chapter 8).
CAUTION: The 12,500-hour preventive maintenance procedure is
to be performed only by a qualified service technician.
according to instructions in the Operator’s Manual.
2. Perform an extended self-test (EST) (Chapter 5.)
3. Turn the ventilator off, disconnect all power sources (AC and battery),
and disconnect oxygen.
4. If required, remove the ventilator from its cart.
5. Separate the top and bottom enclosures.
6. Remove the power supply shroud.
7. Use an ESD-safe vacuum to remove dust or debris from the top and
bottom enclosures, then inspect for any signs of corrosion or damage:
• Ensure that the exhalation flow sensor tube is clean, clear, and
moisture-free.
• Check for loose cables, screws, or pneumatic lines.
• Remove any dust from the power supply PCB, power supply fan
housing, and power supply fan.
8. Reinstall the power supply shroud, including electrical connections to
the GUI and fan.
9. Use a clean, lint-free cloth and vacuum to remove dust from the
interior of the power supply air inlet hose, then reinstall to the power
supply shroud.
10. Clean the GUI as described in the Operators Manual. If required, also
use an ESD-safe vacuum to clean the interior components.
11. Reassemble the top and bottom enclosures, then clean the ventilator
exterior as described in the Operator’s Manual.
NOTE: For component removal/installation instructions, see Chapter 9
(Esprit ventilator), or Chapter 10 (V200 ventilator).
4-2 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 39

4.2 Annual PM Follow these steps to install the annual PM kit:
• If harness has white terminal
block: do not replace.
• No white terminal on harness:
install replacement harness from
12,500-hour PM kit.
White terminal
block on harness
1. Clean the ventilator (section 4.1).
2. Replace these PM kit components:
• Air inlet filter.
• Blower inlet filter.
• Oxygen water trap filter.
3. Complete a performance verification (Chapter 8).
4. Apply these labels:
• PM label: complete and apply to upper right center of blower
shroud exterior
• Clear chemical-resistant label: apply to cover PM label
• Electrical safety label: apply to upper left center of blower shroud
exterior or as required.
Chapter 4
Periodic Maintenance
4.3 12,500-Hour PM Follow these steps to install the 12,500-hour PM kit:
1. Clean the ventilator (section 4.1).
2. With the top and bottom enclosures separated and the power supply
shroud removed, check the power supply to blower motor harness
(Figure 4-1):
• If the harness has a white terminal block, do not replace.
• If the harness does not have a white terminal block, replace the
harness.
Figure 4-1: Power Supply to Blower Motor Harness Versions
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 4-3
Page 40

Chapter 4
3.6-V lithium battery (original Esprit ventilator):
if present on power supply shroud, install
replacement battery from 12,500-hour PM kit.
3.2-V button battery (current Esprit/
Respironics V200 ventilator): if present on
main PCB, do not replace battery.
Periodic Maintenance
3. Determine whether the real-time clock battery must be replaced
(Figure 4-2):
• If the power supply shroud includes a 3.6-V lithium battery, install
the replacement battery from the 12,500-hour PM kit.
• If a main PCB with the 3.2-V button battery is installed, do not
replace the battery.
Figure 4-2: Real-Time Clock Battery Versions
4. Remove the power supply fan from the shroud and install the
replacement fan from the PM kit.
5. Reinstall the power supply fan shroud and its connections.
6. Remove the blower, cooling coil, cooling coil fan and mesh cup.
7. lnstall these replacement components from the PM kit:
• Cooling coil fan
• Blower assembly
• Mesh cup
8. Reassemble the ventilator and install these replacement components
from the PM kit:
• Air inlet filter.
• Blower inlet filter.
• Oxygen water trap filter.
9. Complete a performance verification (Chapter 8).
10. Apply these labels:
• PM label: complete and apply to upper right center of blower
shroud exterior
• Clear chemical-resistant label: apply to cover PM label
• Electrical safety label: apply to upper left center of blower shroud
exterior or as required.
4-4 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 41

Chapter 5. Diagnostic Mode and
Troubleshooting
Use diagnostic mode to:
• Set the date and time, set the correct altitude, enable or disable
automatic patient circuit compliance, select a 12 or 24 hour clock,
and enable or disable backup battery confirmation at startup (section
5.2).
• Run a short self test (SST) (section 5.3).
• Run an extended self test (EST) (section 5.4).
• View the software revision of the ventilator and installed options
(section 5.5).
• View diagnostic codes (section 5.6).
• Control and monitor pneumatic components and voltages for
troubleshooting in case the ventilator fails SST, EST, or performance
verification (section 5.7).
• Check bacteria filter resistance (section 5.9).
WARNING: Diagnostic mode suspends normal ventilation: disconnect the patient from the
ventilator before entering diagnostic mode.
CAUTION: Troubleshooting and repair should be performed only by a qualified
service technician. Respironics Factory Service Training is highly
recommended prior to performing service procedures on Esprit or
Respironics V200 Ventilator. Contact Customer Service at 1-800-3426443 or 724-387-4000 for more information.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 5-1
Page 42

Chapter 5
Diagnostic Mode and Troubleshooting
5.1 Entering
Diagnostic Mode
5.2 User
Configuration
To start ventilator diagnostics, simultaneously press the ALARM RESET and 100%
2 keys on the front panel for approximately five seconds while turning ventilator
O
power on. At the prompt, touch OK to enter diagnostic mode (Figure 5-1).
Figure 5-1: Entering Diagnostic Mode
Use the user configuration screen (Figure 5-2) to:
• Set the date and time (section 5.2.1)
• Set the correct altitude (section 5.2.2)
• Enable or disable automatic patient circuit compliance compensation
(section 5.2.3)
• Select a 12 or 24 hour clock (section 5.2.4)
• Enable or disable backup battery confirmation at ventilator startup
(section 5.2.5).
5-2 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 43

Chapter 5
Diagnostic Mode and Troubleshooting
To view the user configuration screen, touch User Config on the diagnostic
screen.
Figure 5-2: User Configuration Screen
5.2.1 Setting the Date and Time
1. Touch the button for the value you want to change.
2. Touch the Increase or Decrease bar or turn the knob to adjust the
value.
3. Press Accept (onscreen button or offscreen key) to confirm the
change.
4. Touch Apply Date or Apply Time to apply the change (changes do not
take effect until you touch the button).
5.2.2 Setting Altitude
Setting altitude to the correct value allows the ventilator to deliver tidal
volumes at optimal accuracy.
WARNING: Reenter the correct altitude setting whenever upgrading software. The altitud e
setting reverts to the default setting (9999 feet, displayed as ----) at every
software upgrade.
1. Verify the altitude using an altimeter if available, or estimate altitude
in feet or meters above sea level.
2. Touch Altitude.
3. Touch the Increase or Decrease bar or turn the knob to adjust the
value.
4. Press Accept.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 5-3
Page 44

Chapter 5
Diagnostic Mode and Troubleshooting
5.2.3 Enabling Circuit Compliance
The ventilator can use compliance correction to compensate for volume loss in
the patient breathing circuit due to the compressible volume of the tubing.
Touch Compliance to enable or disable compliance correction:
• Enabled: the ventilator adds the compliance volume measured during
• Disabled: the ventilator does not add compliance volume to delivered
• After downloading software, you must disable then re-enable
5.2.4 Selecting 12 or 12 Hour Clock
SST or EST to delivered volume, and improves the accuracy of volume
delivery during normal operation.
volume. Compliance correction is typically disabled during
performance testing.
compliance correction (even though compliance correction appears
enabled) to put compliance into effect.
Touch 24hr Clock to toggle between standard 12-hour and 24-hour time
format. The lower right corner of the diagnostic screen shows the selected
format.
5.2.5 Confirm Backup Battery
Touch Bkup Battery to enable or disable backup battery confirmation at
ventilator startup.
When enabled, ventilator startup is normal if the backup battery is connected.
If the backup battery is not connected, the ventilator displays a message at
startup (Figure 5-3) and logs a 5002 diagnostic code.
Figure 5-3: No Backup Battery Connected message
5-4 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 45

Chapter 5
Diagnostic Mode and Troubleshooting
5.3 Short Self Test (SST)
SST verifies the integrity of the patient circuit tubing by measuring its leak rate
and compliance. SST also tests some hardware, including the safety valve (SV),
flow sensor tables, autozero solenoids and the inspiratory non-rebreathing check
valve (CV3). Perform SST after every patient circuit change.
WARNING: Do not use a ventilator that has failed SST without verifying operational
readiness by other means. Doing so may place a patient at risk.
WARNING: Never initiate an SST while the patient is connected to the ventilator. The high
airway pressures generated during SST can injure a patient.
Required equipment: the intended patient circuit assembly and a rubber cork.
Follow these steps to run SST:
1. Connect the intended patient circuit to the ventilator.
2. Touch SST on the diagnostic screen (Figure 5-4).
3. Touch Start SST to begin the test.
4. When prompted, unblock the wye and touch OK.
5. When prompted, block the wye and touch OK.
6. When SST is completed successfully, touch OK. The SST screen
shows the results of each test. Diagnostic code 2000 indicates that
SST was successfully completed.
If any SST tests fail, the screen displays failure data, including diagnostic
code, measured value, and passing values.
• Touch RETEST to repeat the test.
• Touch CONTINUE to skip the failed test.
• Touch CANCEL to exit EST.
Figure 5-4: Starting SST
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 5-5
Page 46

Chapter 5
Diagnostic Mode and Troubleshooting
5.4 Extended Self Test (EST)
EST verifies the functional integrity of the ventilator by testing its hardware
subsystems and components. Perform EST between patients, during
preventive maintenance, performance verification, for oxygen sensor
calibration, or if ventilator operation is questionable.
WARNING: Do not use a ventilator that has failed EST without verifying operational
readiness by other means. Doing so may place a patient at risk.
WARNING: Never initiate an EST while the patient is connected to the ventilator . The high
airway pressures and gas flows generated during EST can injure a patient.
Required equipment:
• Reusable adult patient circuit assembly
• Rubber cork
• Regulated oxygen source
• Optional: an external oxygen sensor to perform the automatic oxygen
sensor test and calibration
• Optional: a remote alarm
Follow these steps to run EST:
1. Verify that the bacteria filters and oxygen sensor are connected to the
ventilator.
2. Connect the patient circuit to the ventilator.
3. Touch EST on the diagnostic screen (Figure 5-5).
4. Touch Start EST to begin the test. Follow the onscreen prompts and
touch OK to go to the next step.
Figure 5-5: Starting EST
5. Unblock wye and touch OK, then block the wye with the cork and
touch OK. Unblock wye at the prompt and touch OK.
5-6 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 47

Chapter 5
Diagnostic Mode and Troubleshooting
6. If prompted, connect oxygen to the ventilator and touch OK. (This
prompt does not appear if oxygen is already connected.) Disconnect
oxygen and touch OK, then reconnect oxygen when prompted and
touch OK.
7. Disconnect the patient circuit from the heated exhalation filter and
touch OK, then reconnect and touch OK.
NOTE: For neonatal circuits, touch OK to proceed through this step without
disconnecting the circuit.
8. At these messages, touch YES or NO to answer each question:
Is the primary audio alarm active?
Is the backup audio alarm active?
Is the remote alarm connected?
Is the remote alarm active?
9. At the prompts, touch YES or NO to indicate whether each front panel
LED lights.
10. Press the front panel keys as prompted.
11. When EST is completed successfully, touch OK. The EST screen
shows the results of each test. Diagnostic code 3000 appears in the
diagnostic log each time EST is successfully completed.
If any EST tests fail, the screen displays failure data, including diagnostic
code, measured value, and passing values.
• Touch RETEST to repeat the test.
• Touch CONTINUE to skip the failed test.
• Touch CANCEL to exit EST.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 5-7
Page 48

Chapter 5
Diagnostic Mode and Troubleshooting
5.5 Software Screen To view the software screen, touch Software on the diagnostic screen (Figure
5-6). The software screen displays:
• Ventilator serial number
• Part number and version of the flash and one time programmable
(OTP) software
• Version of the air stepper valve, oxygen stepper valve, exhalation
stepper valve, and display
• Air, oxygen, and exhalation flow sensor part numbers
• Options installed, if any.
Figure 5-6: Diagnostic Mode Software Screen
5-8 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 49

Diagnostic Mode and Troubleshooting
5.6 Diagnostic Codes The Esprit and V200 ventilators generate diagnostic codes when the
microprocessor detects a fault during normal operation, or if a failure occurs
during SST or EST. Chapter 6 lists diagnostic codes and recommended repair
procedures for each code.
To view the diagnostic code screen, touch Diag. Codes on the diagnostic screen
(Figure 5-7).
Chapter 5
Figure 5-7: Diagnostic Code Screen
The diagnostic code screen displays the following information:
1. Number: Diagnostic codes are numbered in reverse order of
occurrence, with the most recent code first.
2. Code: The number assigned to a specific failure, which can help
determine the cause of a failure. The first digit of the four-digit
diagnostic codes indicates the type of fault:
1xxx: Failure during power on self test (POST).
2xxx: Failure during short self test (SST).
3xxx: Failure during extended self test (EST).
4xxx: Continuous built-in test failure (during normal ventilation).
5xxx: Safety valve open/Backup battery not connected.
6xxx: Not used.
7xxx: Power supply failure.
8xxx: Software diagnostic information.
9xxx: Sensor/internal communication fault.
3. Repeat: If the same code occurs consecutively, the repeat column is
incremented (rather than displaying the code again). For example, if
code 1002 occurs three consecutive times, it is logged as code 1002
with 2 in the repeat column. The repeat column increments (up to a
maximum of 255) until a different code occurs.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 5-9
Page 50

Chapter 5
Diagnostic Mode and Troubleshooting
4. Time: Diagnostic codes are time-stamped in hour/minute/second
5. Date: Diagnostic codes are date-stamped in a month/day/year format
6. Corrupted: The microprocessor regularly cross checks the data in
7. Next Pg and Prev Pg buttons: The ventilator can log up to 20 error
8. Clear Codes button: Allows you to delete diagnostic codes.
format (for example, 09:15:23). The time is that of the most recent
occurrence of the code.
(for example, 09/12/01) to indicate the most recent occurrence of the
code.
memory. If it determines that the diagnostic code in memory has been
corrupted, a Yes entry indicates that its validity is suspect.
codes but can only display 10 on a screen. Touch the Next Pg button
to view the next group of codes, or Prev Pg to view the previous group.
NOTE: Diagnostic codes are the primary means of fault diagnosis and should
only be deleted by a qualified service technician.
To delete diagnostic codes, touch Clear Codes and at the following
prompt:
Are you sure you want to clear the codes?
Touch YES to clear the codes or NO to retain the codes.
5-10 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 51

Chapter 5
Diagnostic Mode and Troubleshooting
5.7 Hardware Diagnostics
The hardware screen (Figure 5-7) verifies components in case of a failure
during SST, EST, or performance verification. Use the hardware screen to:
• Set specific air and oxygen valve flow rates and step positions.
• Incrementally open and close the exhalation valve.
• Set various analog and digital voltages.
• Control power to the blower, filter heater, and 24-V components.
• Exercise the solenoids.
• View hardware status.
NOTE: On the hardware screen, a white background indicates that the button is
enabled or energized, and a gray background indicates that a button is
disabled or de-energized.
Figure 5-8: Diagnostic Mode Hardware Screen
Table 5-1 summarizes the hardware screen functions.
Table 5-1: Hardware Screen Functions
Button/Display Function
Air button Sets air flow from 0 to 200 LPM or step position from 0 to 2000 steps.
Oxygen button Sets oxygen flow from 0 to 200 LPM or step position from 0 to 2000 steps.
Exhalation button Opens or closes the exhalation valve from 0 (fully open) to 2000 (fully closed)
steps. (Although the exhalation stepper motor can be commanded to 2000 steps,
a maximum of 1800 steps is displayed.)
Monitors button Simulates voltages for pressure, volume, and flow analog output voltages. The
selected voltage (from 0 to 5 V) is sent to the analog output port (the DB15
connector on the ventilator back panel).
Voltage Wrap button Adjusts blower DAC voltage from 0 to 5 V, and compares it to the ADC output
voltage shown in the Voltage Wrap status display.
Blower button Adjusts blower voltage from 0 to 5 V.
Blower on/off button Turns the blower on and off.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 5-11
Page 52

Chapter 5
Diagnostic Mode and Troubleshooting
Table 5-1: Hardware Screen Functions (Continued)
Button/Display Function
Filter Heat on/off button Turns the filter heater on and off.
24V Power on/off button Turns all pneumatic components on and off simultaneously without disturbing
the display.
Inhalation button Toggles SOL4 between circuit pressure and atmospheric pressure.
Safety button Opens and closes SOL2, which controls the source pressure that opens or closes
the safety valve.
Exhalation button Toggles SOL3 between circuit pressure and atmospheric pressure.
Crossover button Toggles SOL1, which determines which gas provides source pressure to SOL2.
SOL1 uses air to provide source pressure to SOL2 when energized, and uses
oxygen when de-energized.
Air Flow status display Displays the measured flow passing through the air flow sensor.
Oxygen Flow status display Displays the measured flow passing through the oxygen flow sensor.
Exhalation Flow status display Displays the measured flow passing through the exhalation flow sensor.
Air Position status display Displays the step position of the air valve stepper motor for a specified flow rate
or air valve step position.
Oxygen Position status display Displays the step position of the oxygen valve stepper motor for a specified flow
rate or oxygen valve step position.
Exhalation Position status display Displays the step position of the exhalation valve.
Inhalation Pressure status display Displays the pressure measured by the inhalation pressure sensor.
Exhalation Pressure status display Displays the pressure measured by the exhalation pressure sensor.
Oxygen Supply status display Displays whether the oxygen inlet pressure switch detects an external oxygen
source is connected.
Oxygen Sensor status display Displays the oxygen concentration measured by the external oxygen sensor.
Bus Voltage status display Displays the measured voltage of the +29 V output (if AC is connected) or the
+24 V output from the backup or external battery.
Blower Fan status display Displays the status of the thermal switch attached to the blower housing, and is
ON during normal operation. A switch status of OFF indicates a switch is
malfunction or that the cooling fan is malfunctioning and temperature has risen
to 125 ºC.
PCMCIA Card status display Displays dashes when a PCMCIA card is not installed. If a PCMCIA card is
installed, displays SDP.
Enclosure Temp status display Displays the temperature inside the ventilator enclosure measured by the
temperature sensor on the sensor PCB. Typical temperature range is
approximately 35 to 50 ºC.
Internal Oxygen status display Displays the oxygen concentration within the enclosure in volts as measured by
the oxygen sensor located on the sensor PCB. Acceptable voltage is between
0.52 to 0.62 V.
Voltage Wrap status display Displays the ADC input voltage for comparison to the voltage wrap DAC output
voltage.
5-12 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 53

Chapter 5
Diagnostic Mode and Troubleshooting
5.8 Pneumatic
Component
Troubleshooting
This section tells you how to perform component troubleshooting in case of a
failure during SST, EST, or performance verification. Perform these tests as
needed, rather than in consecutive order.
WARNING: Troubleshooting suspends normal ventilation, and should never be performed
while a patient is connected to the ventilator.
NOTE: Always perform an EST and log diagnostic codes before troubleshooting.
NOTE: These troubleshooting procedures assume that all hardware begins in an
initialized state (all adjustable parameters set to zero), including Blower
voltage set to 4 V (blower voltage may vary depending on the altitude
setting), Blower on, Filter Heat off, 24V Power on, Crossover solenoid
energized (white background), and all other solenoids de-energized (gray
background).
NOTE: At the end of each test, return the hardware screen to its initialized state.
NOTE: The pneumatic calibration analyzer should always be in BTPS when
measuring volume, and in ATP when measuring flow.
NOTE: Use a known-good reusable patient tubing circuit and reliable exhalation
bacteria filter.
Perform all troubleshooting from the hardware screen in diagnostic mode.
Follow these steps to view the hardware screen:
1. Simultaneously press the Alarm Reset and 100% O
2 keys on the
ventilator front for five seconds while turning ventilator power on.
2. When prompted, touch OK to enter diagnostics mode.
3. Perform EST and log the diagnostic codes, or create a ventilator
diagnostic report (DRPT) (Chapter 7).
4. Touch the Hardware button to view the hardware screen.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 5-13
Page 54

Chapter 5
Diagnostic Mode and Troubleshooting
5.8.1 Oxygen Valve
1. Connect the oxygen source to the ventilator.
2. Disconnect the bacteria filter, patient circuit tube, and oxygen sensor
3. Touch User Config and note the altitude.
4. Touch Hardware.
5. Touch Safety to energize (white background) the safety solenoid.
6. Touch Oxygen and set the flow to 1 LPM.
7. Check that the Oxygen Position display is between 185 and 525
8. Touch Oxygen and set the flow to 180 LPM. Verify that the O2 Position
tee from the ventilator inspiratory outlet.
NOTE: The sensor readings on an actual Hardware screen vary from those
shown in Figure 5-9.
steps.
display corresponds to the set altitude:
Ventilator Altitude
Setting
0 - 2000 ft. 1175 - 1575 steps
2001 - 4000 ft. 1145 - 1540 steps
4001 - 6000 ft. 1120 - 1505 steps
6001 - 8000 ft. 1090 - 1470 steps
8001 - 10,000 ft. 1060 - 1435 steps
Oxygen Position
Display
Verify that the oxygen source is disconnected from the ventilator, and
verify that Oxygen Supply reads OFF.
9. Return the hardware screen to its initialized state.
Figure 5-9: Diagnostic Mode - Hardware Screen (Safety Solenoid Energized)
5-14 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 55

Diagnostic Mode and Troubleshooting
5.8.2 Oxygen Flow Sensor
1. Connect the oxygen source to the ventilator.
2. Connect a tube from the ventilator main outlet to the high flow port of
a calibrated analyzer (Figure 5-10).
Chapter 5
Figure 5-10: Flow Sensor Troubleshooting Setup
3. Set the analyzer to read LPM.
4. Set the analyzer’s gas flow to oxygen.
5. Touch Safety to energize (white background) the safety solenoid.
6. Check that set oxygen flow corresponds to measured flow:
Touch Oxygen and Set
the Flow to:
5 LPM 4.5 to 5.5 LPM
10 LPM 9 to 11 LPM
20 LPM 18 to 22 LPM
50 LPM 45 to 55 LPM
100 LPM 90 to 110 LPM
120 LPM 108 to 132 LPM
165 LPM 148.5 to 181.5 LPM
0 LPM 0 ± 0.1 LPM
Check that Analyzer and Oxygen
Flow Displays Read:
7. Disconnect the oxygen source from the ventilator.
8. Return the hardware screen to its initialized state.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 5-15
Page 56

Chapter 5
Oxygen valve
Connection to
oxygen valve
pressure port
Diagnostic Mode and Troubleshooting
5.8.3 Oxygen Regulator
1. Disconnect the bacteria filter, patient circuit tube, and oxygen sensor
2. Connect the oxygen source to the ventilator.
3. Use a pressure gauge capable of measuring 100 PSI, and set the
4. Connect the gauge to the oxygen valve pressure port (Figure 5-11).
tee from the ventilator inspiratory outlet.
pressure range to 100 PSI. Zero the gauge.
Figure 5-11: Oxygen High Pressure Connection
5. Touch Blower and Crossover to de-energize (gray backgrounds) the
blower and crossover solenoid.
6. Touch Oxygen and set the flow to 180 LPM.
7. Check that the gauge reads 23 ± 1 PSI. If not, adjust the oxygen
regulator pressure:
a. Loosen the locking nut.
b. Turn the adjusting shaft clockwise to increase or counterclockwise
to decrease so the gauge reads 23 ± 1 PSI, then tighten the
locking nut.
c. Touch Oxygen and set the flow to 0 LPM and then back to 180
LPM.
d. Check that the gauge still reads 23 ± 1 PSI. Repeat steps a to d if
necessary.
8. Disconnect the oxygen source from the ventilator.
9. Return the hardware screen to its initialized state.
10. Remove the gauge and reconnect tubing to the safety valve solenoid
tubing connection.
5-16 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 57

Diagnostic Mode and Troubleshooting
5.8.4 Air Valve
1. Disconnect the bacteria filter, patient circuit tube, and oxygen sensor
tee from the ventilator inspiratory outlet.
2. Touch User Config and note the altitude.
3. Touch Hardware.
4. Touch Safety to energize (white background) the safety solenoid.
5. Touch Air and set the flow to 1 LPM.
6. Check that the Air Position display is between 215 and 525 steps.
7. Touch Air and set the flow to 180 LPM.
8. Check that the Air Position display corresponds to the set altitude:
Chapter 5
Ventilator Altitude
Setting
0 - 2000 ft. 930 - 1215 steps
2001 - 4000 ft. 910 - 1190 steps
4001 - 6000 ft. 890 - 1165 steps
6001 - 8000 ft. 875 - 1145 steps
8001 - 10,000 ft. 855 - 1125 steps
Air Position
Display
9. Return the hardware screen to its initialized state.
5.8.5 Air Flow Sensor
1. Connect a tube from the ventilator main outlet to the high flow port of
a calibrated analyzer (Figure 5-14).
2. Set the analyzer to read LPM.
3. Set the analyzer’s gas flow to air.
4. Touch Safety to energize (white background) the safety solenoid.
5. Check that set air flow corresponds to measured flow:
Touch Air and Set the
Flow to:
5 LPM 4.5 to 5.5 LPM
10 LPM 9 to 11 LPM
20 LPM 18 to 22 LPM
50 LPM 45 to 55 LPM
100 LPM 90 to 110 LPM
120 LPM 108 to 132 LPM
165 LPM 148.5 to 181.5 LPM
0 LPM 0 ± 0.1 LPM
Check that Analyzer, Air Flow and
Exhalation Flow Displays Read:
6. Return the hardware screen to its initialized state.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 5-17
Page 58

Chapter 5
Diagnostic Mode and Troubleshooting
5.8.6 Inhalation and Exhalation Solenoids
NOTE: If pressure displays do not drop to 0 ± 0.1 cmH2O, cycle power to the
1. Connect the patient circuit to the ventilator and block the wye.
2. Touch Safety to energize (white background) the safety solenoid.
3. Touch Exhalation and set it to 2000 steps.
4. Touch Air and set the flow to 1 LPM.
5. Check that the Inhalation Pressure and Exhalation Pressure displays
6. Touch Inhalation to energize (white background) the inhalation
7. Check that the Inhalation Pressure display reads 0 ± 0.1 cmH
8. Touch Exhalation to energize (white background) the exhalation
9. Check that the Exhalation Pressure display reads 0 ± 0.1 cmH
10. Return the hardware screen to its initialized state.
ventilator to enter normal ventilation mode. After the ventilator completes
POST, cycle power to the ventilator to enter diagnostic mode and re-run
the test.
on the hardware screen are greater than 30 cmH
O.
2
solenoid.
solenoid.
O.
2
O.
2
5.8.7 Safety Valve and Safety Solenoid
NOTE: If pressure displays do not drop to 0 ± 0.1 cmH2O, cycle power to the
ventilator to enter normal ventilation mode. After the ventilator completes
POST, cycle power to the ventilator to enter diagnostic mode and re-run
the test.
1. Connect the patient circuit to the ventilator and block the wye.
2. Touch Exhalation and set it to 2000 steps.
3. Touch Air and set the flow to 1 LPM.
4. Check that the Inhalation Pressure display reads 0 ± 0.1 cmH
5. Touch Safety to energize (white background) the safety solenoid.
6. Check that the Inhalation Pressure display is greater than 30 cmH
7. Return the hardware screen to its initialized state.
O.
2
O.
2
5-18 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 59

Diagnostic Mode and Troubleshooting
5.8.8 Pressure Relief Valve
1. Set the analyzer to read cmH2O.
2. Connect the analyzer’s positive low pressure port to the patient circuit
(Figure 5-12).
Chapter 5
Figure 5-12: Pressure Relief Valve Troubleshooting Setup
3. Touch Safety to energize (white background) the safety solenoid.
4. Touch Exhalation and set it to 2000 steps.
5. Touch Air and set the flow to 1 LPM.
6. Check that the analyzer reads 130-140 cmH
O. If not, adjust the
2
relief pressure (Figure 5-13):
a. Turn the pressure relief valve hex cap clockwise to decrease or
counterclockwise to increase, so that analyzer reads 130-140
O.
cmH
2
b. Touch Safety to relieve system pressure, then Touch Safety to re-
pressurize.
c. Check that the analyzer reads 130-140 cmH
O. Repeat steps a to
2
c if necessary.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 5-19
Page 60

Chapter 5
Hex cap
Diagnostic Mode and Troubleshooting
7. Return the hardware screen to its initialized state.
Figure 5-13: Pressure Relief Valve Hex Cap
5.8.9 Crossover Solenoid
1. Disconnect the oxygen source from ventilator.
2. Touch Oxygen and set the flow to 100 LPM, then back to 0 LPM to
relieve any trapped oxygen pressure.
3. Connect patient circuit to ventilator and block wye with a cork.
4. Touch Safety to energize (white background) the safety solenoid.
5. Touch Exhalation and set it to 2000 steps.
6. Touch Air and set the flow to 1 LPM.
7. Check that the Inhalation Pressure display on the hardware screen
reads greater than 30 cmH
8. Remove cork from the wye.
9. Touch Crossover to de-energize (gray background) the crossover
solenoid, then block the wye.
10. Check that the Inhalation Pressure display reads 0 ± 0.1 cmH
11. Return the hardware screen to its initialized state.
O.
2
O.
2
5-20 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 61

Diagnostic Mode and Troubleshooting
5.8.10 Exhalation Flow Sensor
1. Connect the patient tubing from the ventilator to the high flow port of
a calibrated analyzer (Figure 5-14).
Chapter 5
Figure 5-14: Exhalation Flow Sensor Troubleshooting Setup
2. Set analyzer to read LPM.
3. Set analyzer’s gas flow to air.
4. Touch Safety to energize (white background) the safety solenoid.
5. Check that the set air flow corresponds to measured flow:
Touch Air and Set the
Flow to:
5 LPM 4.5 to 5.5 LPM
20 LPM 18 to 22 LPM
50 LPM 45 to 55 LPM
100 LPM 90 to 110 LPM
120 LPM 108 to 132 LPM
165 LPM 148.5 to 181.5 LPM
0 LPM 0 ± 0.1 LPM
Check that Analyzer, Air Flow and
Exhalation Flow Displays Read:
6. Return the hardware screen to its initial state.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 5-21
Page 62

Chapter 5
Diagnostic Mode and Troubleshooting
5.8.11 Check Valve 2
1. Connect the oxygen source to the ventilator.
2. Connect patient circuit to the ventilator, then block the wye.
3. Touch Safety to energize (white background) the safety solenoid.
4. Touch Crossover to de-energize (gray background) the crossover
5. Touch Blower to de-energize (gray background) the blower.
6. Touch Exhalation and set it to 2000 steps.
7. Touch Oxygen and set flow to 1 LPM.
8. Touch Air and set flow to 200 LPM.
9. Check that Inhalation Pressure display on the hardware screen reads
10. Check that the Air Flow display on the hardware screen reads 0 ± 0.1
11. Return the hardware screen to its initialized state.
solenoid.
greater than 30 cmH
LPM.
O.
2
5.8.12 Check Valve 3
1. Disconnect the oxygen source to the ventilator.
2. Connect the patient circuit to the ventilator, then block the wye.
3. Touch Safety to energize (white background) the safety solenoid.
4. Touch Exhalation and set it to 2000 steps.
5. Touch Air and set flow to 1 LPM.
6. Check that Inhalation Pressure display on the hardware screen reads
greater than 30 cmH
7. Touch Air and set flow to 0 LPM.
8. Touch Oxygen and set flow to 200 LPM.
9. Check that the Oxygen Flow display on the hardware screen reads 0 ±
0.1 LPM.
10. Return the hardware screen to its initialized state.
O.
2
5-22 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 63

Diagnostic Mode and Troubleshooting
5.8.13 Check Valve 4
WARNING: To prevent contamination, use two clean filters to perform this test.
WARNING: If the ventilator has been operating, the heater conductor may be hot.
1. Install a new, clean exhalation bacteria filter to the exhalation port of
the ventilator.
2. Connect an adult patient tube between the just-installed exhalation
filter end and a second bacteria filter.
NOTE: Install filters so that their flow arrows point away from the ventilator.
3. Gently inhale from the bacteria filter.
4. Check that the Exhalation Flow display on the hardware screen reads 0
± 0.1 LPM.
5. Return the hardware screen to its initialized state.
Chapter 5
5.8.14 Filter Heater
WARNING: If the ventilator has been operating, the filter heater sleeve may be hot.
1. Touch Filter Heat on the hardware screen to turn the filter heater on
(white background). Skip this step if the ventilator has been operating
in ventilation mode.
2. Wait 15 minutes. Skip this step if the ventilator has been operating in
ventilation mode.
3. Remove the exhalation filter and verify that it is very warm to the
touch.
4. Reinstall the filter and heater.
5. Return the hardware screen to its initialized state.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 5-23
Page 64

Chapter 5
Diagnostic Mode and Troubleshooting
5.8.15 Blower
1. Connect a tube from the ventilator main outlet to the high flow port of
2. Set the analyzer’s peak/continuous function to continuous.
3. Set analyzer’s gas flow to measure 180 LPM air. Zero the analyzer.
4. Touch Safety to energize (white background) the safety solenoid.
5. Touch Air and set the flow to 165 LPM.
6. Check that the analyzer reads 148.5 to 181.5 LPM.
7. Touch Blower to turn off the blower (gray background).
8. Check that the blower stops and the analyzer reads 0 ± 0.1 LPM.
9. Return the hardware screen to its initialized state.
pneumatic calibration analyzer (Figure 5-15).
Figure 5-15: Blower Troubleshooting Setup
5-24 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 65

Chapter 5
Diagnostic Mode and Troubleshooting
5.8.16 Inhalation/ Exhalation Pressure Transducers and Exhalation Valve
1. Connect patient circuit with tee to the ventilator.
2. Connect the analyzer’s positive low pressure port to the patient circuit
(Figure 5-16).
Figure 5-16: Inhalation and Exhalation Pressure Transducer Troubleshooting Setup
3. Set the analyzer to read cmH2O.
4. Touch Safety to energize (white background) the safety solenoid.
5. Touch Exhalation and set it to 1470 steps.
6. Touch Air and set the flow to 1 LPM.
7. Touch Exhalation and adjust the steps until the analyzer pressure
reads 100 ± 5 cmH
O.
2
8. Check that the Inhalation Pressure and Exhalation Pressure displays
on the hardware screen read within ± 10% of the analyzer display.
9. Unblock the tee and verify that the inhalation, exhalation, and
analyzer pressure displays read 0 ± 0.1 cmH
O.
2
10. Return the hardware screen to its initialized state.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 5-25
Page 66

Chapter 5
Diagnostic Mode and Troubleshooting
5.8.17 Oxygen Pressure Switch
1. Connect a wall or bottled oxygen source to the ventilator. The Oxygen
2. Disconnect the oxygen source from the ventilator.
3. Touch Oxygen and set the flow to 100 LPM, and then back to 0 LPM
4. The Oxygen Supply display should read OFF.
5. Return the hardware screen to its initialized state.
5.8.18 External Oxygen Sensor
Perform the performance verification oxygen accuracy test (Chapter 8).
5.8.19 High Internal Oxygen Alarm Test
Follow these steps if a High Internal O
1. Disconnect oxygen from the ventilator and wait 5 minutes to allow the
2. Power up the ventilator in diagnostic mode and touch the Hardware
3. Confirm that the Internal Oxygen display on the Hardware screen is
Supply display on the hardware screen should read ON.
to relieve any trapped oxygen pressure.
alarm occurs:
2
internal oxygen percentage to stabilize.
button to view the Hardware screen.
between 0.52 to 0.62 V. If the display is outside this range, replace
the sensor PCB.
5-26 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 67

Diagnostic Mode and Troubleshooting
D3D13
5.8.20 Sensor PCB Voltage Indicators
The sensor PCB includes LEDs (Figure 5-17) that indicate uner- and
overvoltage conditions, as summarized in Table 5-2.
Figure 5-17: Sensor PCB LEDs
Table 5-2: Sensor PCB Voltage LEDs
Sensor PCB LED Voltage Condition Recommended Repair
Chapter 5
D3 Power supply: -12 V under Replace power supply.
D4 Power supply: +12 V under Replace power supply.
D5 Power supply: +24 V under Replace power supply.
D6 Sensor PCB: +5 V under Replace sensor PCB.
D7 Sensor PCB: +5 V over Replace sensor PCB.
D8 MMI PCB: +5 V under Replace MMI PCB.
D9 MMI PCB: +5 V over Replace MMI PCB.
D10 Power supply: +10 V under Replace power supply.
D11 Power supply: +10 V over Replace power supply.
D12 Main PCB: +5 V over Replace main PCB.
D13 Main PCB: +5 V under Replace main PCB.
D49 Power Fail Replace power supply.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 5-27
Page 68

Chapter 5
Diagnostic Mode and Troubleshooting
5.9 Bacteria Filter
Back Pressure Test
Follow these steps to check the resistance of any bacteria filter:
1. Power up the ventilator in diagnostic mode and touch the Hardware
button to view the Hardware screen.
2. Use the default settings in the hardware screen EXCEPT:
• Set an air flow rate of 100 LPM
• Energize the safety solenoid
3. Connect a tube from the inspiratory gas outlet to the heated bacteria
filter’s inlet. Important: Do not connect anything to the filter outlet.
4. The displayed Inhalation Pressure is the measured back pressure of
the bacteria filter. The back pressure for a new filter is typically 2.5
cmH
O.
2
A back pressure over 4 cmH
fails the test if the back pressure is greater than 4 cmH
O indicates an occluded filter. The filter
2
O.
2
5-28 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 69

Chapter 6. Diagnostic Codes
The ventilator generates diagnostic codes when the microprocessor detects a
fault during normal operation, or if a failure occurs during SST or EST.
Table 6-1 lists diagnostic codes, and recommended repair procedures for each
code. Perform the repair procedures in the order listed until the problem is
resolved.
• See Chapter 5 describes how to use diagnostic mode for
troubleshooting.
• See Chapter 8 for performance verification procedures.
• See Chapter 9 for Esprit component replacement procedures.
• See Chapter 10 for Respironics V200 component replacement
procedures.
• See Appendix A for EST pneumatic schematics by test number.
NOTE: Because the troubleshooting procedures for two diagnostic codes (1012
and 5000) are more detailed, they are described in section 6.1 and
section 6.2.
The first digit of the four-digit diagnostic codes indicates the type of fault:
1xxx: Failure during power on self test (POST).
2xxx: Failure during short self test (SST).
3xxx: Failure during extended self test (EST).
4xxx: Continuous built-in test failure (failures during normal ventilation).
5xxx: Safety valve open/Backup battery not connected.
6xxx: Not used.
7xxx: Power supply failure.
8xxx: Software diagnostic information.
9xxx: Sensor/internal communication fault.
Diagnostic
Code
1 Ventilator normal mode startup. Air/
O
3 Diagnostic startup. Air/O
positions logged.
4 Unknown restart. Indicates
uncontrolled shutdown of the
system. Possible causes include
watchdog/bus activity timeout, main
PCB +5VDC failure, or loss of AC
power while in diagnostic mode.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 6-1
Code Description Recommended Repair
Occurs when ventilator is ON: no action
valve liftoff positions logged.
2
liftoff
2
required.
Occurs when diagnostics invoked: no
action required.
1. Verify AC connection at wall and
ventilator, check circuit breaker.
2. Replace CPU PCB.
3. Replace sensor PCB.
4. Replace main PCB.
5. Replace power supply.
Page 70

Chapter 6
Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
5 Depleted backup battery. Battery
depleted dialog displayed on the
screen.
1. Connect AC power cord and allow
battery to charge.
2. Replace backup battery.
3. Replace power supply.
1xxx: Failures During Power On Self Test (POST)
1001 Bus activity monitor test failure. 1. Replace CPU PCB.
2. Replace main PCB.
1002 Watchdog timer test failure. 1. Replace CPU PCB.
2. Replace main PCB.
1003 Processor test failure. Replace CPU PCB.
1004 OTP cyclic redundancy check (CRC)
failure.
1005 Flash CRC failure. 1. Repeat software download.
1006 Internal RAM test failure. Replace CPU PCB.
1007 External RAM test failure. Replace CPU PCB.
1008 Maximum system resets exceeded:
ventilator has reset 3 times within 2
hours.
1009 POST inhalation autozero test
failure. Possible causes include
crimped tube or transducer failure.
1010 POST exhalation autozero test
failure. Possible causes include
crimped tube or transducer failure.
1011 POST OTP flash compatibility test
failure.
1012 Air valve liftoff failure: measured
liftoff < 180 or > 500 steps
(default = 280 steps).
1013 Oxygen valve liftoff failure:
measured liftoff < 150 or > 500
steps (default = 280 steps).
Replace CPU PCB.
2. Replace CPU PCB.
Review the diagnostics log: the code in
memory prior to the 1008 occurrence
indicates the root cause.
1. Check for crimped tube between
three-station solenoid and the sensor
PCB.
2. Replace sensor PCB.
3. Replace analog PCB.
1. Check for crimped tube between the
three-station solenoid and the sensor
PCB.
2. Replace sensor PCB.
1. Repeat software download.
2. Replace CPU PCB.
See section 6.1.
1. Use RS-232 diagnostic report
(DRPT) command to obtain detailed
information.
2. If step position during liftoff is
outside range, replace oxygen valve.
3. Replace oxygen motor controller
PCB.
6-2 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 71

Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
1014 POST timer/24V failure: system has
reset 3 times within the first 30
seconds of operation. Once this code
occurs, it recurs at every power up or
reset until the ventilator enters
diagnostic mode.
2xxx: Failures During Short Self Test (SST)
2000 SST passed. No action required.
2100 Cancelled by user. No action required.
2106 Patient circuit leak.
Patient circuit test (test 11): this
code indicates that the ventilator
could not pressurize the tubing
O.
2
O.
2
O with a 5 LPM
2
O to <45
2
O. This
2
circuit to 50 cmH
air flow and the safety and
exhalation valves closed.
2107 Low inhalation pressure.
Patient circuit test (test 11): this
code indicates that circuit pressure
dropped from 50 cmH
cmH
O after exactly 100 ms.
2
2110 Check valve 3 (CV3) leak.
Patient circuit test (test 11): the
circuit is pressurized to 50 cmH
with the exhalation valve closed,
then the safety valve opens. After
two seconds, circuit pressure should
not drop below 35 cmH
code indicates that circuit pressure
was <35 cmH
2125 Inhalation and exhalation pressure
transducer disagreement.
Patient circuit test (test 11): the
difference between the inhalation
and exhalation pressure transducers
is >3 cmH
Review the diagnostic log: the code in
memory before or after the 1014
occurrence indicates the root cause.
If this code is not 4, 7xxx, or 8001:
1. Replace power supply.
2. Replace main PCB.
3. Replace CPU PCB.
4. Replace BMC PCB
1. Remove inspiratory bacteria filter and
external oxygen sensor and try
another patient circuit.
2. Block outlet of exhalation flow sensor
while running leak test. If leak stops,
replace exhalation valve.
3. Verify that connection between the
oxygen flow sensor and oxygen valve
is tight.
1. Check for patient circuit leaks.
2. Verify that O-ring is present in
external oxygen sensor or bypass
oxygen sensor.
3. Check inhalation pressure
transducer.
4. Check the connection between the
inspiratory manifold and inspiratory
autozero solenoid.
5. Check for kinks or cuts in the tube
between inhalation autozero solenoid
and inhalation pressure sensor.
6. Replace sensor PCB.
7. Replace three-station solenoid.
1. Check for patient circuit leaks.
2. Verify that O-ring is present in
2
oxygen sensor.
external oxygen sensor or bypass
O
3. Verify that CV3 is undamaged and in
12:00 position.
4. Check CV3. Replace as necessary.
5. Check tubing from inspiratory
solenoid to inspiratory manifold.
1. Check patient circuit for leaks.
2. Replace sensor PCB.
3. Replace analog PCB.
4. Replace main PCB.
Chapter 6
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 6-3
Page 72

Chapter 6
Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
2128 Circuit compliance out of range.
Patient circuit test (test 11): circuit
compliance is calculated by
measuring the time required to
achieve 50 cmH
code indicates that calculated
O at 5 LPM. This
2
compliance is < 0.50 ml/cmH
>9.0 ml/cmH
O.
2
2129 Pressure leak out of range.
Patient circuit test (test 11): the
patient circuit leak rate (based on
calculated compliance value) is
determined by measuring the
decrease in circuit pressure from 50
O after one second. This code
cmH
2
indicates that the pressure leak was
out of range, based on the
calculated compliance value.
2130 Safety valve cannot open.
Safety valve test (test 2): the
exhalation valve is opened then
closed to vent circuit pressure. The
safety valve solenoid (SOL2) is then
deenergized to open the safety valve,
and a 10 LPM air flow starts while
monitoring the inspiratory pressure
transducer (PT3). This code
indicates that PT3 is measuring >5
O.
cmH
2
2131 Patient wye not blocked.
Block patient wye (test 1): after the
prompt to block the wye, the safety
valve and exhalation valves close.
The ventilator starts a 5 LPM air
flow, and the inspiratory pressure
transducer (PT3) should measure
10 cmH2O. This code indicates
>
that PT3 is measuring <10 cmH
2134 Cannot read air flow sensor.
This code indicates that system
cannot read EEPROM from the air
flow sensor (FS1).
1. Remove inspiratory bacteria filter and
external oxygen sensor and try
another patient circuit.
2. Replace sensor PCB.
3. Replace analog PCB.
O or
2
1. Remove inspiratory bacteria filter and
external oxygen sensor and try
another patient circuit.
2. Rerun leak test while blocking
exhalation flow sensor outlet. If leak
stops, replace exhalation valve.
3. Replace sensor PCB.
4. Replace analog PCB.
1. Check safety valve and safety valve
solenoid.
2. Check for blocked vent tube between
the inspiratory manifold and the back
of the ventilator.
3. Replace three-station solenoid
assembly.
4. Install safety valve kit.
5. Replace inspiratory manifold
assembly.
6. Replace main PCB.
7. Replace CPU PCB.
1. Check that patient wye is blocked
and circuit is tightly connected.
2. Ensure that exhalation filter door is
securely closed.
3. Replace exhalation filter and rerun
test.
4. Replace 3-station solenoid assembly.
O.
2
1. Enter diagnostic mode, then turn
ventilator off and on.
2. Verify air flow sensor cable
connections.
3. Replace air flow sensor.
4. Replace CPU PCB.
5. Replace sensor PCB.
6. Replace analog PCB.
7. Replace main PCB.
6-4 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 73

Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
2135 Cannot read oxygen flow sensor.
This code indicates that system
cannot read EEPROM from the
oxygen flow sensor (FS2).
2136 Cannot read exhalation flow sensor:
This code indicates that system
cannot read EEPROM from the
exhalation flow sensor (FS3)
2137 Air flow sensor (FS1) failure.
This code indicates that information
stored on FS1 cannot be read.
2138 Oxygen flow sensor (FS2) failure.
This code indicates that information
stored on FS2 cannot be read.
2139 Exhalation flow sensor (FS3) failure.
This code indicates that information
stored on FS3 cannot be read.
2140 Flow sensors cannot erase table.
This code indicates that flow sensor
calibration tables stored on the CPU
PCB cannot be erased.
1. Enter diagnostic mode, then turn
ventilator off and on.
2. Verify oxygen flow sensor cable
connections.
3. Replace oxygen flow sensor.
4. Replace CPU PCB.
5. Replace sensor PCB.
6. Replace analog PCB.
7. Replace main PCB.
1. Enter diagnostic mode, then turn
ventilator off and on.
2. Verify exhalation flow sensor cable
connections.
3. Replace exhalation flow sensor.
4. Replace sensor PCB.
5. Replace CPU PCB.
6. Replace analog PCB.
7. Replace main PCB.
1. Enter diagnostic mode, then turn
ventilator off and on.
2. Replace CPU PCB.
3. Replace air flow sensor.
4. Replace sensor PCB.
5. Replace analog PCB.
6. Replace main PCB.
1. Enter diagnostic mode, then turn
ventilator off and on.
2. Replace CPU PCB.
3. Replace oxygen flow sensor.
4. Replace sensor PCB.
5. Replace analog PCB.
6. Replace main PCB.
1. Enter diagnostic mode, then turn
ventilator off and on.
2. Replace CPU PCB.
3. Replace exhalation flow sensor.
4. Replace sensor PCB.
5. Replace analog PCB.
6. Replace main PCB.
Replace CPU PCB.
Chapter 6
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 6-5
Page 74

Chapter 6
Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
2141 Inhalation autozero solenoid cannot
open.
Block patient wye (test 1): patient
circuit pressurized to 50 cmH
then inhalation autozero solenoid
commanded to energize (open), and
inspiration pressure transducer
(PT3) should measure 0 cmH
This code indicates that PT3
measured >3 cmH
O or <-3 cmH2O.
2
2
2142 Exhalation autozero solenoid cannot
open.
Block patient wye (test 1): patient
circuit pressurized to 50 cmH
then exhalation autozero solenoid
commanded to energize (open), and
exhalation pressure transducer (PT2)
should measure 0 cmH
indicates that PT2 measured >3
O or <-3 cmH2O.
cmH
2
O. This code
2
2152 Patient wye not unblocked.
Block patient wye (test 1): with the
wye unblocked and the safety and
exhalation valves closed, a 25-LPM
air flow should create a back
pressure <10 cmH
by inspiratory pressure transducer
O as measured
2
(PT3). This code indicates that PT3
measured a back pressure >
O.
cmH
2
10
2156 Inhalation transducer autozero
failure.
Block patient wye test (test 1): with
no pressure in the circuit, the
inspiratory pressure transducer
(PT3) and exhalation pressure
transducer (PT2) are cross-checked.
This code indicates that the PT3
measurement was out of range.
2157 Exhalation transducer autozero
failure.
Block patient wye test (test 1): with
no pressure in the circuit, the
inspiratory pressure transducer
(PT3) and exhalation pressure
transducer (PT2) are cross-checked.
This code indicates that the PT2
measurement was out of range.
1. Check inhalation autozero solenoid.
2. Replace three-station solenoid.
3. Replace sensor PCB.
4. Replace main PCB.
O,
2
O.
1. Check inhalation autozero solenoid.
2. Replace three-station solenoid.
3. Replace sensor PCB.
4. Replace main PCB.
O,
2
1. Verify that circuit is not a neonatal
circuit.
2. Check that patient wye is unblocked.
3. Try new inspiratory bacteria filter.
4. Check for occlusion in the inspiratory
limb of the patient circuit.
1. Check for crimped tube.
2. Check inhalation solenoid.
3. Replace sensor PCB.
4. Replace three-station solenoid.)
5. Replace main to sensor cable.
6. Replace analog PCB.
7. Replace main PCB.
1. Check for crimped tube.
2. Check exhalation solenoid.
3. Replace sensor PCB.
4. Replace three-station solenoid
assembly.
5. Replace main to sensor cable.
6. Replace analog PCB.
7. Replace main PCB.
6-6 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 75

Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
3xxx: Failures During Extended Self Test (EST)
NOTE: Test numbers refer to tests within EST and are illustrated in the
pneumatic schematics in Appendix A of this manual.
NOTE: Because EST requires a functioning blower, always verify that the
blower is operating before troubleshooting.
3000 EST passed. No action required.
3100 Cancelled by user. No action required
3103 Air flow out of range.
Air delivery test (test 8): flow rates
of 0 and 3 LPM (±1 LPM), 5, 10,
20, 23, 50, 100, 150 and 200 LPM
(±8 LPM) are set through the air
valve as measured at the air flow
sensor (FS1). This code indicates
that FS1 measured out of range
flows.
3104 Oxygen flow out of range.
Oxygen delivery test (test 6): flow
rates of 0 and 3 LPM (± LPM), 5,
10, 20, 23, 50, 100 and 150 LPM
(±8 LPM) are set through the oxygen
flow sensor (FS2). This code
indicates that FS2 measured out of
range flows.
3105 Exhalation flow outside range.
Heated filter back pressure test (test
12): a 100 LPM air flow rate is
established in the patient circuit
with the exhalation valve open. This
code indicates that the exhalation
flow sensor (FS3) measurement is
<90 LPM or >110 LPM, and the
FS3 measurement is displayed.
3106 Patient circuit leak.
Patient circuit test (test 11): this
code indicates that the ventilator
could not pressurize the tubing
circuit to 50 cmH
air flow and the safety and
exhalation valves closed.
O with a 5 LPM
2
1. Check air flow sensor accuracy.
Replace if necessary.
2. Check air valve.
3. Replace air valve assembly.
4. Replace air motor controller PCB.
1. Check oxygen valve.
2. Verify adequate source pressure and
flow rates.
3. Try another oxygen source:
flowmeters or other restrictions can
limit flow even with sufficient
pressure.
4. Check oxygen flow sensor.
5. Replace oxygen motor controller
PCB.
1. Check circuit integrity.
2. Replace exhalation filter.
3. Check exhalation flow sensor.
4. Check orientation of exhalation check
valve CV4.
1. Check for leaks at the connections
between the circuit, filters,
humidifier, and couplings.
2. Remove inspiratory bacteria filter and
external oxygen sensor and try
another patient circuit.
3. Verify that connection between
oxygen flow sensor and oxygen valve
is tight.
Chapter 6
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 6-7
Page 76

Chapter 6
Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
3107 Low inhalation pressure.
Patient circuit test (test 11): this
code indicates that circuit pressure
dropped from 50 cmH
O after exactly 100 ms.
cmH
2
O to <45
2
3108 Exhalation pressure outside range.
Exhalation valve test (test 10): the
exhalation valve is set to deliver
pressures of 0, 5, 10, and 20
O (tolerance ±2 cmH2O), 30
cmH
2
cmH
O (tolerance ± 3 cmH2O), and
2
35 cmH
O (tolerance ± 3.5 cmH2O)
2
as measured at the exhalation
pressure transducer (PT2). This code
indicates that PT2 measured out of
range pressures.
3109 Check valve 2 (CV2) leak.
Crossover circuit test (test 5): the air
valve is opened without the blower
running and an oxygen flow of 100
LPM is created. The air flow sensor
(FS1) should measure a flow of 0
LPM. This code indicates that FS1
measured >3 LPM.
3110 Check valve 3 (CV3) leak.
Patient circuit test (test 11): the
circuit is pressurized to 50 cmH
with the exhalation valve closed,
then the safety valve opens. After
two seconds, circuit pressure should
not drop below 35 cmH
or ped mode, or below 41 cmH
O in adult
2
Neo mode. This code indicates that
circuit pressure was <35 cmH
adult or ped mode, and <41 cmH
in Neo mode.
1. Check for patient circuit leaks.
2. Verify that O-ring is present in
external oxygen sensor of bypass
oxygen sensor.
3. Check inhalation pressure
transducer.
4. Check the connection between the
inspiratory manifold and inspiratory
autozero solenoid.
5. Check for kinks or cuts in the tube
between inhalation autozero solenoid
and inhalation pressure sensor.
6. Replace sensor PCB.
7. Replace three-station solenoid.
1. Replace exhalation bacteria filter.
2. Check exhalation solenoid for
operation and leaks.
3. Check exhalation pressure
transducer.
4. Check exhalation valve.
5. Check for kinks or cuts in the tube
between exhalation solenoid and
exhalation pressure sensor.
6. Replace sensor PCB.
7. Replace three-station solenoid.
Check CV2. Replace as necessary.
1. Check for patient circuit/filter leaks.
2. Verify that CV3 is in 12:00 position.
3. Verify that there is an O-ring in the
O
2
oxygen sensor or bypass.
4. Check CV3. Replace as necessary.
5. Check tubing from SOL4 to
inspiratory manifold.
O in
2
O in
2
O
2
6-8 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 77

Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
3111 Oxygen not connected.
Oxygen supply test (test 4): the
oxygen supply pressure switch (PS1)
is open when oxygen is not
connected. At the prompt to connect
oxygen, PS1 should close when 4090 PSI is connected. This code
indicates that PS1 remains open.
3112 Oxygen not disconnected.
Oxygen supply test (test 4): the
oxygen supply pressure switch (PS1)
is closed when oxygen is connected.
At the prompt to disconnect oxygen,
the oxygen valve opens and closes to
relieve pressure, and PS1 should be
open. This code indicates that PS1
remains closed.
3113 Oxygen sensor analog to digital
3115 Primary audio not sounding.
3116 Backup audio not sounding.
3117 Crossover circuit fault.
converter (ADC) sample out of range.
Oxygen sensor test (test 7): this
code indicates that the ADC
measurements are out of range and
assumes that the oxygen sensor is
not connected.
Audio test (test 13): ventilator
activates primary alarm and prompts
for a response that alarm is audible.
This code indicates that the primary
alarm is not working.
Audio test (test 13): ventilator
activates backup alarm and prompts
for a response that alarm is audible.
This code indicates that the backup
alarm is not working.
Crossover circuit test (test 5):
crossover solenoid (SO1) is
energized to supply air source gas to
close safety valve, and an air flow
rate of 5 LPM is established with the
exhalation valve closed. After three
seconds, the inspiratory pressure
transducer (PT3) should measure a
pressure of 50 cmH
This code indicates that PT3
measured <50 cmH
O or greater.
2
O.
2
1. Check that oxygen (minimum of
40PSI/276 kPa) is connected to the
ventilator.
2. Try another oxygen hose, outlet,
quick-connect, or external regulator.
3. Check oxygen pressure switch.
4. Check oxygen regulator assembly.
1. Check that oxygen is disconnected.
2. Check oxygen pressure switch.
3. Replace oxygen regulator assembly.
1. Replace external oxygen sensor.
2. Replace oxygen sensor cable.
3. Replace FIO
cable.
4. Replace sensor PCB.
5. Replace analog PCB.
1. Verify correct key press.
2. Replace primary alarm.
3. Replace digital PCB.
4. Replace the primary alarm to MMI
PCB cable.
5. Replace MMI PCB.
6. Replace main PCB.
1. Verify correct key press.
2. Replace the backup alarm.
3. Replace digital PCB.
4. Replace the primary alarm to MMI
PCB cable.
5. Replace MMI PCB.
6. Replace main PCB.
1. Check for patient circuit leaks,
bypass the oxygen sensor, and
replace exhalation bacteria filter.
2. Check crossover solenoid.
3. Replace crossover solenoid assembly.
4. Replace main PCB.
sensor to sensor PCB
2
Chapter 6
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 6-9
Page 78

Chapter 6
Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
3118 Blower not turned off.
Blower test (test 3): turns blower off
and opens air valve. Air flow sensor
(FS1) should measure flow less than
50 LPM within 20 seconds. This
code indicates that FS1 measured
50 LPM.
>
3119 Blower DAC failure.
Blower test (test 3): turns blower
controller switch on but sets analog
voltage that controls blower speed to
0 V. Blower should remain off, and
air flow sensor (FS1) should
measure flow less than 50 LPM
within two seconds. This code
indicates that FS1 measured >
LPM.
3120 Relief valve cracking pressure too
high (>170 cmH
O).
2
Pressure relief valve test (test 9): at
an oxygen flow of 1 LPM, the
exhalation pressure transducer (PT2)
should measure a stable pressure of
120-160 cmH2O within 60
seconds. This code indicates that
PT2 measured >170 cmH
O.
2
3121 Relief valve cracking flow not stable.
Pressure relief valve test (test 9): the
oxygen flow sensor (FS2) should
measure 1 LPM during this test.
This code indicates that FS2
measured <0.8 LPM or >1.2 LPM.
3122 Relief valve cracking pressure out of
range (<120 cmH
cmH
O).
2
O or >160
2
Pressure relief valve test (test 9): at
an oxygen flow of 1 LPM, the
exhalation pressure transducer (PT2)
should measure a pressure between
120-160 cmH
O. This code
2
indicates that PT2 measured <120
O or >160 cmH2O (but <170
cmH
2
O).
cmH
2
3123 Oxygen cracking flow out of range
(<0.7 LPM or >1.3 LPM).
Pressure relief valve test (test 9): the
oxygen flow sensor (FS2) should
measure a flow of 1 LPM. This code
indicates that FS2 measured <0.7
LPM or >1.3 LPM.
1. Check blower.
2. Replace blower controller PCB.
3. Replace sensor PCB.
4. Replace main PCB.
1. Check blower.
2. Replace blower controller PCB.
3. Replace sensor PCB.
4. Replace analog PCB.
50
1. Check pressure relief valve and
adjust if necessary.
2. Replace pressure relief valve.
3. Replace sensor PCB.
1. Check pressure relief valve and
adjust if necessary.
2. Replace pressure relief valve.
3. Replace sensor PCB.
1. Check pressure relief valve and
adjust if necessary.
2. Replace pressure relief valve.
3. Replace sensor PCB.
4. Replace analog PCB.
1. Replace oxygen valve assembly.
2. Replace oxygen flow sensor.
3. Replace sensor PCB.
6-10 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 79

Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
3125 Difference between air flow sensor
and exhalation flow sensor during air
delivery test 8.
Patient circuit test (test 11):
pressure measured by the inspiratory
pressure transducer (PT3) and the
exhalation transducer (PT2) are
sampled, averaged and compared.
This code indicates that
measurement difference was >3
O.
cmH
2
3126 Difference (>20 LPM) between
oxygen flow sensor and exhalation
flow sensor.
Oxygen delivery test (test 6): an
oxygen flow rate of 150 LPM is
established and compared to the
exhalation flow sensor (FS3)
reading. This code indicates that
FS3 measurement difference was
>20 LPM.
3127 Heated filter back pressure out of
range (<5 cmH
O or >15 cmH2O).
2
Heated filter test (test 12): at an air
flow reading of 100 LPM through
the patient circuit, the system
calculates the difference between
inspiratory pressure transducer
(PT3) measurements before and
after disconnecting the exhalation
limb from exhalation filter. This code
indicates that the difference is <5
O or >15 cmH2O.
cmH
2
3128 Circuit compliance out of range.
Patient circuit test (test 11): circuit
compliance is calculated by
measuring the time required to
achieve 50 cmH
O at 5 LPM. This
2
code indicates that calculated
compliance is <0.50 ml/cmH
>9.0 ml/cmH
O.
2
2
3129 Pressure leak out of range.
Patient circuit test (test 11): the
patient circuit leak rate (based on
calculated compliance value) is
determined by measuring the
decrease in circuit pressure from 50
O after one second. This code
cmH
2
indicates that the pressure leak was
out of range, based on the
calculated compliance value.
1. Check air and exhalation flows and
replace flow sensor(s) as necessary.
2. Replace sensor PCB.
3. Replace analog PCB.
4. Replace main PCB.
1. Check oxygen and exhalation flows
and replace flow sensor(s) as
necessary.
2. Replace sensor PCB.
3. Replace analog PCB.
4. Replace main PCB.
1. Replace the exhalation bacteria filter.
2. Check of occlusions in the patient
circuit.
3. Check CV4.
1. Remove inspiratory bacteria filter and
external oxygen sensor and try
another patient circuit.
2. Replace sensor PCB.
3. Replace analog PCB.
O or
1. Remove inspiratory bacteria filter and
external oxygen sensor and try
another patient circuit.
2. Rerun leak test while blocking
exhalation flow sensor outlet. If leak
stops, replace the exhalation valve.
3. Ensure that exhalation filter door is
securely closed.
4. Replace sensor PCB.
5. Replace analog PCB.
Chapter 6
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 6-11
Page 80

Chapter 6
Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
3130 Safety valve cannot open.
Safety valve test (test 2): the
exhalation valve is opened then
closed to vent circuit pressure. The
safety valve solenoid (SOL2) is then
deenergized to open the safety valve,
and a 10 LPM air flow starts while
monitoring the inspiratory pressure
transducer (PT3). This code
indicates that PT3 is measuring >
O.
cmH
2
3131 Patient wye not blocked.
Block patient wye (test 1): after the
prompt to block the wye, the safety
and exhalation valves close. The
ventilator starts a 5 LPM air flow and
the inspiratory pressure transducer
(PT3) should measure >
This code indicates that PT3 is
measuring <10 cmH
3132 Keyboard key not responding.
Keyboard test (test 15): the operator
is prompted to press each hard key
on the keyboard. This code indicates
an incorrect key response.
3133 Rotary encoder failure.
Keyboard test (test 15): the operator
is prompted to rotate the knob. This
code indicates no knob response.
3134 Cannot read air flow sensor.
This code indicates that system
cannot read EEPROM from the air
flow sensor (FS1).
3135 Cannot read oxygen flow sensor.
This code indicates that system
cannot read EEPROM from the
oxygen flow sensor (FS2).
10 cmH2O.
O.
2
1. Check safety valve and safety valve
solenoid.
2. Check for blocked vent tube between
the inspiratory manifold and the back
of the ventilator.
3. Replace three-station solenoid
assembly.
4. Install safety valve kit.
5. Replace inspiratory manifold
assembly.
5
1. Check that patient wye is blocked.
2. Check for patient disconnection in
patient circuit.
3. Ensure that exhalation filter door is
securely closed.
4. Replace exhalation filter and retest.
5. Replace 3-station solenoid assembly.
1. Check cable connections between
front panel overlay and MMI PCB.
2. Slave in replacement front panel
overlay and check for proper
operation.
3. Replace MMI PCB.
4. Replace CPU PCB.
1. Replace rotary encoder.
2. Replace MMI PCB.
3. Replace digital PCB.
4. Replace main PCB to MMI PCB
cable.
5. Replace CPU PCB.
6. Replace main PCB.
1. Enter diagnostic mode, then turn
ventilator off and on.
2. Verify air flow sensor cable
connections.
3. Replace air flow sensor.
4. Replace CPU PCB.
5. Replace sensor PCB.
6. Replace analog PCB.
1. Enter diagnostic mode, then turn
ventilator off and on.
2. Verify oxygen flow sensor cable
connections.
3. Replace oxygen flow sensor.
4. Replace CPU PCB.
5. Replace sensor PCB.
6. Replace analog PCB.
6-12 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 81

Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
3136 Cannot read exhalation flow sensor.
This code indicates that system
cannot read EEPROM from the
exhalation flow sensor (FS3).
3137 Air flow sensor (FS1) failure.
This code indicates that information
stored on FS1 cannot be read.
3138 Oxygen flow sensor (FS2) failure.
This code indicates that information
stored on FS2 cannot be read.
3139 Exhalation flow sensor (FS3) failure.
This code indicates that information
stored on FS3 cannot be read.
3140 Flow sensors cannot erase table.
This code indicates that flow sensor
calibration tables stored on the CPU
PCB cannot be erased.
3141 Inhalation autozero solenoid cannot
open.
Block patient wye (test 1): patient
circuit pressurized to 50 cmH
then inhalation autozero solenoid
commanded to energize (open), and
inspiration pressure transducer
(PT3) should measure 0 cmH
This code indicates that PT3
measured outside the range from -3
to 3 cmH
O.
2
2
2
1. Enter diagnostic mode, then turn
ventilator off and on.
2. Verify exhalation flow sensor cable
connections.
3. Replace exhalation flow sensor.
4. Replace sensor PCB.
5. Replace CPU PCB.
6. Replace analog PCB.
7. Replace main PCB.
1. Enter diagnostic mode, then turn
ventilator off and on.
2. Replace CPU PCB.
3. Replace air flow sensor.
4. Replace sensor PCB.
5. Replace analog PCB.
6. Replace main PCB.
1. Enter diagnostic mode, then turn
ventilator off and on.
2. Replace CPU PCB.
3. Replace oxygen flow sensor.
4. Replace sensor PCB.
5. Replace analog PCB.
6. Replace main PCB.
1. Enter diagnostic mode, then turn
ventilator off and on.
2. Replace CPU PCB.
3. Replace exhalation flow sensor.
4. Replace sensor PCB.
5. Replace analog PCB.
6. Replace main PCB.
Replace CPU PCB.
1. Check inhalation solenoid.
2. Replace three-station solenoid
assembly.
3. Replace sensor PCB.
O,
4. Replace analog PCB.
O.
Chapter 6
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 6-13
Page 82

Chapter 6
Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
3142 Exhalation autozero solenoid cannot
3143 Air stepper motor open position out
3144 Air stepper motor midpoint position
3145 Air stepper motor closed position out
3146 Oxygen stepper motor open position
open.
Block patient wye (test 1): patient
circuit pressurized to 50 cmH
then exhalation autozero solenoid
commanded to energize (open), and
exhalation pressure transducer (PT2)
should measure 0 cmH
indicates that PT2 measured outside
the range from -3 to 3 cmH
of range.
Air delivery test (test 8): air valve
stepper commanded to open
position (2000 ± 5 steps). This code
indicates that measured position
was outside the range of 1995 to
2005 steps.
out of range.
Air delivery test (test 8): air valve
stepper commanded to midpoint
position (1000 ± 5 steps). This code
indicates that measured position
was outside the range of 995 to
1005 steps.
of range.
Air delivery test (test 8): air valve
stepper commanded to closed
position (last measured liftoff
position ± 5 steps). This code
indicates that the measured position
was more than 5 steps above or
below the liftoff position.
out of range.
Oxygen delivery test (test 6): oxygen
valve stepper commanded to open
position (2000 ± 5 steps). This code
indicates that measured position
was outside the range of 1995 to
2005 steps.
O. This code
2
O.
2
1. Check inhalation solenoid.
2. Replace three-station solenoid
assembly.
3. Replace sensor PCB.
O,
2
4. Replace analog PCB.
1. Replace air motor controller PCB.
2. Replace air valve assembly.
3. Replace main to motors cable.
4. Replace CPU PCB.
5. Replace main PCB.
6. Replace analog PCB.
1. Replace air motor controller PCB.
2. Replace air valve assembly.
3. Replace main to motors cable.
4. Replace CPU PCB.
5. Replace analog PCB.
1. Replace air motor controller PCB.
2. Replace air valve assembly.
3. Replace main to motors cable.
4. Replace CPU PCB.
5. Replace analog PCB.
1. Replace oxygen motor controller
PCB.
2. Replace oxygen valve assembly.
3. Replace main to motors cable.
4. Replace CPU PCB.
5. Replace main PCB.
6-14 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 83

Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
3147 Oxygen stepper midpoint position
out of range.
Oxygen delivery test (test 6): oxygen
valve stepper commanded to
midpoint position (1000 ± 5 steps).
This code indicates that measured
position was outside the range of
995 to 1005 steps.
3148 Oxygen stepper motor closed
position out of range.
Oxygen delivery test (test 6): oxygen
valve stepper commanded to closed
position (last measured liftoff
position ± 5 steps). This code
indicates that the measured position
was more than 5 steps above or
below the liftoff position.
3149 Exhalation stepper motor open
position out of range.
Exhalation valve test (test 10):
exhalation valve stepper
commanded to open position (0 ± 5
steps). This code indicates that
measured position was outside the
range of 1795 to 1805 steps.
3150 Exhalation stepper motor midpoint
position out of range.
Exhalation valve test (test 10):
exhalation valve stepper
commanded to midpoint position
(1000 ± 5 steps). This code
indicates that measured position
was outside the range of 995 to
1005 steps.
3151 Exhalation stepper motor closed
position out of range.
Exhalation valve test (test 10):
exhalation valve stepper
commanded to closed position
(2,000 ± 5 steps). This code
indicates that the measured position
was more than 5 steps above or
below the closed position.
1. Replace oxygen motor controller
PCB.
2. Replace oxygen valve assembly.
3. Replace main to motors cable.
4. Replace CPU PCB.
5. Replace main PCB.
1. Replace oxygen motor controller
PCB.
2. Replace oxygen valve assembly.
3. Replace main to motors cable.
4. Replace CPU PCB.
5. Replace main PCB.
1. Replace exhalation motor controller
PCB.
2. Replace exhalation valve assembly.
3. Replace main to motors cable.
4. Replace CPU PCB.
5. Replace main PCB.
1. Replace exhalation motor controller
PCB.
2. Replace exhalation valve assembly.
3. Replace main to motors cable.
4. Replace CPU PCB.
5. Replace main PCB.
1. Replace exhalation motor controller
PCB.
2. Replace exhalation valve assembly.
3. Replace main to motors cable.
4. Replace CPU PCB.
5. Replace main PCB.
Chapter 6
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 6-15
Page 84

Chapter 6
Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
3152 Patient wye not unblocked.
Block patient wye (test 1): with the
wye unblocked and the safety and
exhalation valves closed, a 25-LPM
air flow should create a back
pressure <10 cmH
by inspiratory pressure transducer
(PT3). This code indicates that PT3
measured a back pressure >
O.
cmH
2
3153 Touch screen failure.
Keyboard test (test 15): checks
touch screen to verify that all
emitters, detectors, and the touch
screen controller on the MMI PCB
are working properly.
3154 LED indicator failure.
LED test (test 14): prompts the
operator to confirm that each LED
on the front panel lights as
described (constant or flashing).
This code indicates that correct LED
response was not received.
3155 Remote alarm not sounding.
Audio test (test 13): if operator
responds that a remote alarm is
connected to the ¼ inch phone jack
on ventilator back panel, this test
activates the nurse call relay.
Operator is prompted to confirm
remote. This code indicates that
confirmation of remote alarm
function was not received.
3156 Inhalation transducer autozero
failure.
Block patient wye test (test 1): with
no pressure in the circuit, the
inspiratory pressure transducer
(PT3) and exhalation pressure
transducer (PT2) are cross-checked.
This code indicates that the PT3
measurement was out of range.
O as measured
2
10
1. Verify that circuit is not a neonatal
circuit.
2. Check that patient wye is unblocked.
3. Try new inspiratory bacteria filter.
4. Check for occlusion in the inspiratory
limb of the patient circuit.
1. Clean screen and touch frame
assembly.
2. Verify cable connections.
3. Replace IR touch frame or GUI
assembly.
4. Replace MMI PCB.
5. Replace digital PCB.
6. Replace main PCB.
1. Verify correct key press.
2. Check ribbon cable connections.
3. Replace front panel overlay.
4. Replace digital PCB.
5. Replace MMI PCB.
6. Replace main PCB.
1. Verify correct key press.
2. Check nurse call.
3. Replace CPU PCB.
4. Replace main PCB.
1. Check for crimped tube.
2. Check inhalation solenoid.
3. Replace sensor PCB.
4. Replace three-station solenoid
assembly.
5. Replace main to sensor cable.
6. Replace analog PCB.
7. Replace main PCB.
6-16 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 85

Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
3157 Exhalation transducer autozero
failure.
Block patient wye test (test 1): with
no pressure in the circuit, the
inspiratory pressure transducer
(PT3) and exhalation pressure
transducer (PT2) are cross-checked.
This code indicates that the PT2
measurement was out of range.
3158 Exhalation Valve Test failure.
(Neonatal Option only)
This code indicates that the initial
pressure is outside of range during
exhalation valve test.
3159 Exhalation Valve Test failure.
(Neonatal Option only)
This code indicates that the final
pressure is outside of range during
exhalation valve test.
3160 Exhalation Valve Test failure.
(Neonatal Option only)
This code indicates that the
exhalation flow is outside of range
during exhalation valve test.
1. Check for crimped tube.
2. Check exhalation solenoid.
3. Replace sensor PCB.
4. Replace three-station solenoid
assembly.
5. Replace main to sensor cable.
6. Replace analog PCB.
7. Replace main PCB.
1. Check exhalation solenoid for
operation and leaks.
2. Check exhalation pressure
transducer.
3. Check exhalation valve.
4. Check for kinks in the tube between
exhalation solenoid and exhalation
pressure sensor.
5. Replace sensor PCB.
1. Check exhalation solenoid for
operation and leaks.
2. Check exhalation pressure
transducer.
3. Check exhalation valve.
4. Check for kinks in the tube between
exhalation solenoid and exhalation
pressure sensor.
5. Replace sensor PCB.
1. Check circuit integrity.
2. Check exhalation filter for occlusion
or leaks.
3. Check exhalation flow sensor.
4. Check orientation of exhalation check
valve CV4.
5. Replace exhalation flow sensor.
6. Replace sensor PCB.
Chapter 6
4xxx: Continuous Built-in Test Failures (*Vent Inop.)
4002* RAM test.
Memory test on CPU PCB.
4003* ADC/DAC test.
The 12-bit analog to digital
converter (ADC) and 8-bit digital to
analog converter (DAC) on the
analog PCB are tested.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 6-17
Replace CPU PCB.
1. Replace analog PCB.
2. Replace main to sensor cable.
3. Replace sensor PCB.
Page 86

Chapter 6
Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
4004* Inhalation autozero failure.
The inspiratory pressure transducer
solenoid (SOL4) is energized at
regular intervals. This code indicates
that the system failed to measure a
stable reading. Three consecutive
failures result in a Vent Inop
condition.
4005* Exhalation autozero failure.
The exhalation pressure transducer
solenoid (SOL3) is energized at
regular intervals. This code indicates
that the system failed to measure a
stable reading. Three consecutive
failures result in a Vent Inop
condition.
4006* High temperature (>65 ºC).
Fan(s) not running or blocked air
flow. The temperature sensor is on
the sensor PCB. A high-priority, nonresettable alarm.
4007 Exhalation valve stuck open.
When the exhalation valve is
commanded closed, the exhalation
flow sensor (FS3) still measures
flow.
4008 Air valve stuck open.
When the air valve is commanded
closed, the air flow sensor (FS1) still
measures flow.
1. Check for crimped tubes between
inhalation solenoid and transducers
on sensor PCBA.
2. Check inhalation solenoid.
3. Replace sensor PCB.
4. Replace three-station solenoid
assembly.
5. Replace main to sensor cable.
6. Replace analog PCB.
7. Replace main PCB.
1. Check for crimped tubes between
inhalation solenoid and transducers
on sensor PCBA.
2. Check inhalation solenoid.
3. Replace sensor PCB.
4. Replace three-station solenoid
assembly.
5. Replace main PCB to sensor PCB
cable.
6. Replace analog PCB.
7. Replace main PCB.
1. Check both cooling fans for proper
operation. If there is a fan failure,
measure voltage to the fan (it should
be 24 VDC). If voltage is correct,
replace fan. If voltage is incorrect,
replace power supply.
2. Check blower inlet filter and air
intake filter, and clean or replace as
necessary.
3. Replace sensor PCB.
1. Check exhalation flow sensor and
exhalation valve (test the exhalation
valve using the flow transducer test
described in Chapter 5).
2. Replace exhalation motor controller
PCB.
3. Replace exhalation valve assembly.
4. Replace exhalation flow sensor.
5. Replace exhalation flow sensor cable.
6. Replace main PCB.
1. Check air valve and air flow sensor.
2. Replace air motor controller PCB.
3. Replace air valve assembly.
4. Replace air flow sensor.
5. Replace air flow sensor cable.
6. Replace main PCB.
6-18 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 87

Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
4009* Oxygen valve stuck open.
When the oxygen valve is
commanded closed, the oxygen flow
sensor (FS2) still measures flow.
4010 Air valve stuck closed.
When air valve is commanded open,
no air flow is detectable.
4011 Oxygen valve stuck closed.
When oxygen valve is commanded
open, no oxygen flow is detected.
4013* CPU memory test.
Unable to read POST data on the
CPU.
4014* Flash CRC.
A memory test on the CPU PCB
failed.
4015 Primary alarm failure.
Electronic pulse detection circuitry
unable to confirm a functioning
main alarm.
4018* Flow table CRC.
Flow sensor data on the CPU does
not match flow sensor installed in
ventilator.
4019 Air motor error.
Unexpected air valve stepper motor
reading.
1. Check oxygen valve and oxygen flow
sensor.
2. Replace oxygen motor controller
PCB.
3. Replace oxygen valve assembly.
4. Replace oxygen flow sensor.
5. Replace oxygen flow sensor cable.
6. Replace main PCB.
1. Check air valve and air flow sensor.
2. Replace air flow sensor cable.
3. Replace air flow sensor.
4. Replace air motor controller PCB.
5. Replace air valve assembly.
6. Replace main PCB.
1. Check oxygen valve and oxygen flow
sensor.
2. Replace oxygen flow sensor cable.
3. Replace oxygen flow sensor.
4. Replace oxygen motor controller
PCB.
5. Replace oxygen valve assembly.
6. Replace main PCB.
Replace CPU PCB.
1. Repeat software download.
2. Replace CPU PCB.
1. Check MMI to primary alarm cable
and replace as necessary.
2. Replace primary alarm.
3. Replace digital PCB.
4. Replace MMI PCB.
5. Replace main PCB.
Replace CPU PCB.
1. Check air valve.
2. Replace air motor controller PCB.
3. Replace main to motors cable.
4. Replace air valve assembly.
5. Replace main PCB.
Chapter 6
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 6-19
Page 88

Chapter 6
Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
4020* Oxygen motor error.
Unexpected oxygen valve stepper
motor reading.
4021* Exhalation motor error.
Unexpected exhalation valve stepper
motor reading.
4022 Blower fan failure.
The thermal switch attached to the
blower housing measures 125 ºC or
there is an open circuit to the sensor
PCB.
1. Check oxygen valve.
2. Replace oxygen motor controller
PCB.
3. Replace oxygen valve assembly.
4. Replace main PCB.
1. Replace exhalation motor controller
PCB.
2. Replace exhalation valve assembly.
3. Replace main PCB.
1. Check that cooling coil fan is
working.
2. Check the J3/J4 connections on the
sensor PCB.
3. Check for open between thermal
switch contacts when temperature is
>125 ºF.
4. Replace sensor PCB.
5xxx: Status/Miscellaneous Codes
5000 Occlusion: safety valve open alarm.
A pressure difference between
inspiratory and expiratory limbs of
the circuit was detected.
5001 Gas supplies lost: safety valve open
alarm.
No air flow from the blower
detected, and the oxygen source is
either disconnected or not detected
by the oxygen pressure switch (PS1).
5002 Backup battery not connected.
Backup battery was not detected
during power up (POST).
5003 High internal O
alarm 1. Perform High Internal Oxygen Alarm
2
See section 6.2.
1. Check blower operation in normal
and diagnostic modes.
2. Check PS1.
3. Replace the sensor PCB.
4. Replace the CPU PCB.
1. If backup battery was not connected
during power up, disregard 5002.
2. Verify the backup battery is properly
connected to the ventilator.
3. Connect AC power and allow backup
battery to charge and perform backup
battery test.
4. Replace backup battery.
test.
2. With unit open, connect a high
pressure oxygen source to the unit
(power off). Listen for any pneumatic
leaks. Repair as required.
3. Power on unit and confirm both
cooling fans are operational.
4. With unit closed, operate in normal
mode (use default settings, except
set oxygen at 100%) for 20 minutes
on a test lung.
5. Replace sensor PCB.
6-20 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 89

Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
5004 Exhalation flow sensor thermistor
temperature outside range.
7xxx: Power Supply Failures (Vent Inop)
NOTE: A 7xxx code that precedes a 1008 or 1014 in the diagnostic log
indicates that the power supply output voltage has dropped below
tolerance three times. Always confirm fuse integrity before replacing
power supply.
7000 Power failure, power fail. Replace power supply.
7002 Power failure, power fail. 1. If code 7002 occurs in conjunction
7004-7014 Various combinations of +12V, -12V,
and power fail failures.
7016-7030 Various combinations of 24V, +12V,
-12V, and power fail failures.
7032-7062 Sensor PCB +5V failure and/or
various combinations of +12V, -12V,
24V, and power fail failures.
7064-7094 MMI PCB +5V failure and/or various
combinations of +12V, -12V, 24V,
and power failures.
7096-7126 MMI PCB +5V failure and/or various
combinations of sensor PCB +5V,
+12V, -12V, 24V, and power fail
failures.
7128-7158 Various combinations of +10V,
+12V, -12V, 24V, and power fail
failures.
7160-7190 +10V failure and various
combinations of sensor PCB +5V,
+12V, -12V, 24V, and power fail
failures.
7192-7222 +10V failure and various
combinations of MMI PCB +5V,
+12V, -12V, 24V, and power fail
failures.
7224-7254 +10V failure and various
combinations of MMI PCB +5V,
sensor PCB +5V, +12V, -12V, 24V,
and power fail failures.
1. Perform the air flow accuracy test.
2. Verify cooling fans are functioning
and are both installed in the proper
orientation.
3. Replace exhalation flow sensor.
with code 1008 or 1014, slave in
replacement power switch and
replace if the problem is resolved.
2. Replace power supply.
Replace power supply.
1. Confirm power cord is fully
connected.
2. Replace power supply.
1. Replace sensor PCB.
2. Replace power supply.
1. Replace MMI PCB.
2. Replace power supply.
1. Replace MMI PCB.
2. Replace sensor PCB.
3. Replace power supply.
Replace power supply.
1. Verify power supply harness
connections.
2. Replace sensor PCB.
3. Replace power supply.
1. Verify power supply harness
connections.
2. Replace MMI PCB.
3. Replace power supply.
1. Verify power supply harness
connections.
2. Replace sensor PCB.
3. Replace MMI PCB.
4. Replace power supply.
Chapter 6
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 6-21
Page 90

Chapter 6
Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
8xxx: Software Faults
8001 Recoverable condition.
Software has detected an
unexpected condition.
8002 Alarm corrupt status. 1. Replace CPU PCB.
8003 Software option button failure or
attempt to reuse button.
8004 Insufficient blower current.
Blower startup is confirmed by
comparing current draw before and
after blower startup.
Use RS-232 diagnostic report (DRPT)
command to obtain detailed information
and contact technical support.
Use RS-232 diagnostic report (DPRT)
command to obtain detailed information
and contact technical support.
1. If this code is accompanied by a
1012 code in the diagnostic log, see
section 6.1.
2. If this code is not accompanied by a
1012 code, disregard.
9xxx: Flow Sensor Faults (Vent Inop)
9001 Flash programming error.
An error occurred while writing flow
sensor calibration data to memory.
9002 Flow sensor mismatch.
The calibration (lookup) tables
stored on the flow sensor and CPU
do not match.
9003 Flow sensor failure.
Flow sensor data is not being
communicated to the CPU.
9004 Pressure sensor failure.
A/D converter out of range.
1. Replace the CPU PCB.
2. Replace the sensor PCB.
1. Reprogram the CPU flow sensor
tables by powering up in diagnostic
mode.
2. Slave in a known-good flow sensor
and cable to each connector (J10,
J11, J12) on the sensor PCB, then
power up until diagnostic mode is
accessible.
3. Replace the sensor PCB.
4. Replace the CPU PCB.
5. Replace the main PCB.
1. Attempt to access diagnostic mode/
EST.
2. Slave in a known-good flow sensor
and cable to each connector (J10,
J11, J12) on the sensor PCB, then
power up until diagnostic mode is
accessible.
3. Replace the sensor PCB.
4. Replace the CPU PCB.
5. Replace the analog PCB.
6. Replace the main PCB.
1. Replace sensor PCB.
2. Replace analog PCB.
6-22 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 91

Diagnostic Codes
Diagnostic
Code Code Description Recommended Repair
9005 Sensor failure.
Generic sensor failure due to flow
sensor, pressure transducer, or
communication problem.
9007 Air flow sensor cable misconnected
to the oxygen connector (J10) on
sensor PCB.
9008 Oxygen flow sensor cable
misconnected to the air (J12) or
exhalation (J11) connector on
sensor PCB.
9009 Flow sensor calibration data out of
range or lookup table cannot be
read.
1. Slave in a known-good flow sensor
and cable to each connector (J10,
J11, J12) on the sensor PCB, then
power up until diagnostic mode is
accessible.
2. Replace the sensor PCB.
3. Replace the CPU PCB.
4. Replace the analog PCB.
5. Replace the main PCB.
Connect air flow sensor cable to J12 on
sensor PCB.
1. Connect oxygen flow sensor cable to
J10 on sensor PCB.
2. Replace sensor PCB.
1. Check cable connections.
2. Reprogram the CPU flow sensor
tables by powering up in diagnostic
mode.
3. Slave in a known-good flow sensor
and cable to each connector (J10,
J11, J12) on the sensor PCB, then
power up until diagnostic mode is
accessible.
4. Replace the sensor PCB.
5. Replace the CPU PCB.
6. Replace the main PCB.
Chapter 6
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 6-23
Page 92

Chapter 6
Diagnostic Codes
6.1 Diagnostic Code
1012
Troubleshooting
A 1012 (air liftoff failure) code indicates an out of range air liftoff value. As
part of power-on self-test (POST), the microprocessor starts the blower and
opens the air valve until the air flow sensor reads a flow rate of 1 LPM. The
step position of the air stepper motor is recorded at this point, and is called
the liftoff value.
The liftoff value is recorded during normal (diagnostic code 1) and diagnostic
mode (diagnostic code 3) startup sequences. The liftoff value (and other
diagnostic information) is also recorded when a 1012 code occurs. If the
blower fails to start spinning, the difference in current draw is zero, and an
8004 diagnostic code is logged. To view the information recorded during 1012
or 8004 events, generate a ventilator diagnostic report (DRPT) (Chapter 7).
NOTE: Disregard an 8004 code without an accompanying 1012 code in the
diagnostic log.
Possible causes for a 1012 diagnostic code include:
• The air valve opening position is too low or too high.
• The blower motor has seized or is drawing too much current.
• The blower controller PCB is not operating properly.
• The air flow sensor is not reading accurately.
• The power supply is not providing the 29 VDC (24 VDC if running on
battery) output to the blower controller PCB.
• The sensor PCB is not operating properly.
• Faulty harness connections between the blower controller PCB and
power supply or sensor PCB.
Follow these steps to determine the cause and repair for a 1012 diagnostic
code:
1. Determine if the blower is working: listen for the blower to start
spinning at startup, or use the Hardware screen (Chapter 5) to set an
air flow: if there is flow, the blower is working.
2. If the blower is not working, determine if the cooling coil fan on the
bottom of the unit is operating by looking, feeling for air flow, or
carefully probing with a slender flexible object such as a wire or tie
wrap. (The blower and this cooling fan share the same output from the
power supply.)
3. If both the blower and the fan are not working, check for 29 VDC (24
VDC if running on battery) at the blower controller PCB:
a. Enter diagnostic mode.
b. Place DMM leads on the red and black wires on the green terminal
block on the blower controller PCB mounted next to the blower.
c. Make sure the wires to the terminal block are securely connected.
Check the other end of this harness and verify it is securely
connected to power supply connector J1.
6-24 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 93

Chapter 6
Diagnostic Codes
d. If F1 and/or F2 are open, replace fuses.
e. If 24/29 VDC is not present, replace the power supply.
4. If the blower is not working but the fan is, check the LED (which
indicates an overcurrent condition) on the blower controller PCB
during a normal startup attempt. If the LED lights, either the blower
motor or the blower controller PCB is not functioning correctly.
a. If you can hear the blower attempt to start running, and then the
LED lights, replace the blower.
b. If the blower still does not work and the LED still lights, reinstall
the original blower and replace the blower controller PCB. You can
slave in and connect the replacement blower controller PCB to see
if it corrects the problem before replacing the original PCB.
5. If the blower doesn’t start, 24/29 VDC is present at the terminal block,
and the LED on the blower controller PCB does not light:
a. Check the continuity and connections of the harness between J9
on the sensor PCB and J3 on the blower controller PCB. If there is
a continuity problem, replace the cable.
b. If the blower still doesn’t work, replace the sensor PCB.
6. If the blower is working, check the DRPT liftoff value (Chapter 7).
7. If the liftoff value is below 180 steps, there may be foreign material in
the valve that prevents it from closing all the way.
a. Cycle the air flow rate from closed to fully open several times to
expel any foreign material. Use the hardware screen to open the
air valve to its maximum position (2,000 steps), then toggle
between the hardware screen and any other screen in the
diagnostic mode to cycle the valve.
b. Reattempt normal startup.
c. If the value is still below 180 steps, replace the air valve.
8. If the value is over 525 steps, either the air valve or the airflow sensor
is not functioning correctly, perform the air flow accuracy test of the
performance verification (Chapter 8):
• If the air flow accuracy test passes, replace the air valve.
• If the test fails, replace the air flow sensor.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 6-25
Page 94

Chapter 6
Diagnostic Codes
6.2 Diagnostic Code
5000
Troubleshooting
A diagnostic code 5000 occurs when a significant pressure differential is
detected between the Inspiratory and exhalation sides of the tubing circuit.
This pressure differential can be caused by blocked tubing (due to liquid
accumulation or a pinched circuit), increased exhalation filter resistance, or
increased resistance caused by additional bacteria filters in line for nebulizer
treatments.
When the ventilator enters an occlusion state, it opens the exhalation valve and
safety valve, then closes them and attempts to deliver a patient breath. If the
pressure differential still exists, the ventilator repeats the process (up to 40
times per minute). During an occlusion state, the ventilator enters the safety
valve open (SVO) state (not VENT INOP).
NOTE: If pressure displays do not drop to 0 ± 0.1 cmH2O, cycle power to the
ventilator to enter normal ventilation mode. After the ventilator completes
POST, cycle power to the ventilator to enter diagnostic mode and re-run
the test.
Follow these steps to determine the cause and repair for a 5000 diagnostic
code:
1. Connect a patient circuit, including test lung, to the ventilator and
turn the ventilator ON in diagnostic mode.
2. Touch Hardware to view the Hardware screen, then select these
settings:
• Touch Air and set to 1 LPM.
• Touch Exhalation and set to 2000 Steps.
• Touch Safety to energize (white background indicates energized).
3. Block the patient wye, then watch the Inhalation Pressure and
Exhalation Pressure displays on the Hardware screen as they rise from
0 cmH
the difference between the pressure displays is greater than 2 cmH
O to the highest stable point (the PRV cracking pressure). If
2
O
2
at any time, note which is higher.
4. Unblock the patient wye to allow pressures to return to 0 ± 0.1
cmH
O, then repeat for Air settings of 2, 3, 4, and 5 LPM.
2
5. With circuit pressure at the PRV cracking pressure, touch Inhalation
and verify that the pressure displays drop to 0 ± 0.1 cmH
O
2
immediately when energized (white background) and returns to circuit
pressure when deenergized, without displaying any pressures between
0 cmH
O and PRV cracking pressure.
2
6. With circuit pressure at the PRV cracking pressure, touch Exhalation
and verify that the pressure displays drop to 0 ± 0.1 cmH
O
2
immediately when energized (white background) and returns to circuit
pressure when deenergized, without displaying any pressures between
0 cmH
O and PRV cracking pressure.
2
6-26 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 95

Chapter 6
Diagnostic Codes
7. If the difference between the Inhalation Pressure and Exhalation
Pressure displays on the Hardware screen is greater than 2 cmH
any time, note which is higher, then swap the INSP and EXH tubes on
the sensor PCB and retest.
• If the pressures are now higher on the opposite pressure display,
replace the 3-station solenoid assembly.
• If pressures remain higher on the same pressure display, replace
the sensor PCB.
8. Return the INSP and EXH tubes to their correct positions on the
sensor PCB.
O at
2
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 6-27
Page 96

Chapter 6
Diagnostic Codes
(This page is intentionally blank.)
6-28 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 97

Chapter 7. Ventilator Communications
This section describes ventilator communications functions, including:
• Downloading software
• Programming the serial number
• Enabling options
• Setting up the serial interface to generate a diagnostic report (DRPT)
• Generating a DRPT
7.1 Downloading Software
The CPU PCB in the ventilator contains nonvolatile memory that allows the
software to be upgraded electronically using a personal computer (PC) or
laptop computer. If the CPU PCB is replaced, the serial number and any
installed options (such as color or graphics) must be reprogrammed.
Writing the ventilator’s serial number to the CPU disables any installed
options. Downloading a new software revision by itself does not disable
options. If you are downloading software after replacing the CPU PCB, you can
reprogram the ventilator serial number as part of the software download as
described in section 7.2.
Follow these steps to download software to the ventilator:
1. Turn PC on and ventilator off.
2. Double-click on SETUP.EXE from the software CD to start the program.
NOTE: The software CD is configured to autorun if the PC has autorun enabled.
To manually start the software, insert the CD into the tray and click Start
> Run, then enter the CD drive location (e.g.: D:\Setup.exe where D is the
CD drive letter.)
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 7-1
Page 98

Chapter 7
Ventilator Communications
3. The Setup screen appears (Figure 7-1). Click Next to continue or
Cancel to exit.
Figure 7-1: Setup Screen
4. The Select Language screen (Figure 7-2) appears. Select a language,
then click Next to continue or Cancel to exit.
Figure 7-2: Select Language Screen
5. The Prepare Hardware screen appears (Figure 7-3). Connect a
standard 9-pin male-female RS-232 null modem cable between the
PC serial port and the ventilator serial port and select the COM port in
use.
6. While turning the ventilator on, simultaneously press the two Options
keys (the two keys to the left of the Accept key) on the ventilator front
panel for five seconds. The message Looking for a download server
appears on the ventilator display, and the backup alarm sounds.
7-2 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
Page 99

Chapter 7
Ventilator Communications
Figure 7-3: Prepare Hardware Screen
7. Click Finish on the Prepare Hardware screen. The download sequence
begins, and after approximately five minutes, the PC displays a
message indicating that software has been successfully downloaded.
If there is a communication problem between the PC and the
ventilator, an error message appears (Figure 7-4). Check the cable
connection and verify that the correct serial port is selected, then try
the download sequence again.
Figure 7-4: Software Download Communication Error
8. If the download is successful, the ventilator displays these messages:
Initializing memory, please wait
Initialization Complete
Programming flow sensor tables, please wait
Programming Complete
9. When the download is complete, click OK on the PC screen. The
ventilator automatically reboots in diagnostics mode.
10. Touch the Software key on the ventilator screen.
11. Verify that the Flash Version is the same as the version on the
Respironics software CD-ROM.
REF 580-1000-02 H Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. 7-3
Page 100

Chapter 7
Ventilator Communications
IMPORTANT: Reset the altitude and turn compliance off then back on
to reactivate compliance compensation (use the User Configuration
screen in diagnostic mode as described in Chapter 5).
12. Disconnect the null-modem cable from the ventilator.
13. Perform EST (Chapter 5).
7.2 Programming the
Ventilator Serial
Number
The serial number of each Respironics V200 or Esprit ventilator is stored in
nonvolatile memory on its CPU PCB, and must be reprogrammed if you replace
the CPU PCB. There are two ways to program the serial number:
• You can program the serial number during a software download
(replacement CPU PCBs are shipped without the Respironics V200
Ventilator software installed).
• You can program the serial number without downloading software (use
this method to save time if you’ve already downloaded software but
have not yet reprogrammed the serial number).
CAUTION: Programming the ventilator serial number disables any installed options,
such as color or graphics. Be sure to program the serial number before
enabling an option.
To program the serial number during a software download:
1. While turning the ventilator on, simultaneously press the two Options
keys on the ventilator front panel for five seconds. The message
Looking for a download server appears on the ventilator display, and
the backup alarm sounds.
2. With the Esprit/V200 software installation CD in the CD drive, click on
Start > Run, then enter D:\setup.exe -vs to begin a software
download, where D is the CD drive letter.
Enter the command exactly as shown, in lowercase letters with a space
between exe and -vs. (This is the same procedure as described in
section 7.1, except that you enter the above command rather than
double-clicking on SETUP.EXE.)
3. At the end of the download, a dialog box prompts you to enter the
ventilator serial number. Enter the serial number (VSxxxxxxx) after the
ventilator has restarted in diagnostic mode, where xxxxxxx is the
seven-digit ventilator serial number. Enter VS in uppercase letters.
7-4 Respironics V200/Esprit Ventilator Service Manual © Respironics, Inc. REF 580-1000-02 H
 Loading...
Loading...