Nobel Biocare GS 1000 User Manual
Clinical images: courtesy of Dr L. de Stavola.
GalvoSurge Dental Implant Cleaning System GS 1000
Clinical Considerations
This document summarizes the clinical considerations identified by Drs C. Hämmerle, M. Danesh-Meyer, I. Urban, L.
de Stavola, O. Gonzalez, F. Lambert, N. Nänni, I. Rocchietta, and G. Tabanella based on their first-user experience
with the product and does not constitute a quick guide nor replace the Instructions for Use (IFU).
Please review the Instructions for Use at www.galvosurge.com/ifu before using the product.
Workflow and clinical considerations
1. Diagnosis with
peri-implantitis
- Assess the severity and defect morphology, and evaluate patient
expectations to help determine the best treatment plan
- Depending on defect morphology, guided bone regeneration (GBR) may be
required to regain function and esthetics
- Smaller lesions may be more predictably managed with resective surgery
providing they are not in a high esthetic area
2. Suitability
assessment for
treatment with
GalvoSurge
- Carefully evaluate oral parameters (presence of plaque, bleeding on
probing, present or prior periodontitis), etiology of peri-implantitis
(inappropriate implant diameter or position, occlusal overload, poor
prosthetic design), morphology of the bone defect (maximum vertical defect
size 8 mm from implant shoulder), and soft tissue characteristics for
optimized treatment plan (see classification of bone defects on reverse for
more details)
- General contraindications include inability to undergo oral surgery, allergy to
any materials used during GalvoSurge cleaning, etc.; consult IFU for the full
list of contraindications
3. Optional:
Presurgical
periodontal and
anti-infective
therapy
- Reduce inflammation to limit risk of complications, particularly if complex
regenerative procedures are planned
- Recommended therapy includes scaling, air powder cleaning, local and/or
systemic antibiotics (in case of recurrent episodes or aggressive infection),
or local disinfectants
4. Local anesthesia
- Ensure a large enough area around the site to be treated is anesthetized
- Apply block anesthesia in the proximity of major vascular-nerve trunks (e.g.,
Inferior Dental Nerve Block in mandible, incisive canal in maxilla)
- If block anesthesia is contraindicated, apply palatal and labial infiltration
anesthesia and extend it to neighboring teeth
5. Flap elevation
- Full thickness muco-periosteal flap at infra-bony defects with bone
dehiscence; flap design should follow the GBR needs
- Resective therapy when GBR is not indicated
- Soft tissue grafting may be performed independent of flap design
- Limited full thickness flap can be performed in case of infra-bony defects
without bone dehiscence
6. Manual removal of
granulation tissue
and hard deposits
- Remove hard deposits with hard instruments (e.g. curettes) and/or other
suitable devices (e.g. Ti brushes)
- When GBR is contemplated, take care not to unnecessarily damage the
implant surface
7. Implant cleaning
with GalvoSurge
- Prior to GalvoSurge treatment, inform patients about a strong salty taste
of the solution during treatment and that there is reasonable volume of
liquid that will flow into the mouth (which will be suctioned out)
- Warning: use nonmetallic suction only. Do not place suction tips too close to
the treated area to ensure that the implant is being continuously covered by
the cleaning solution
- Appearance of bubbles within the solution indicates the correct use of
GalvoSurge system
- On completing the GalvoSurge, it is recommended to thoroughly flush the
area around the implant and under the flap with sterile saline to clear away
any residual coagulum or solution
8. Optional:
GBR, connective
tissue graft
- Evaluate suitability for a successful GBR procedure and possible risks as for
regular GBR treatment
- Wound dehiscence and graft exposure may result in re-infection of the site
- As with any complex surgical procedure apply state-of-the-art tissue
management to support quick and successful wound healing
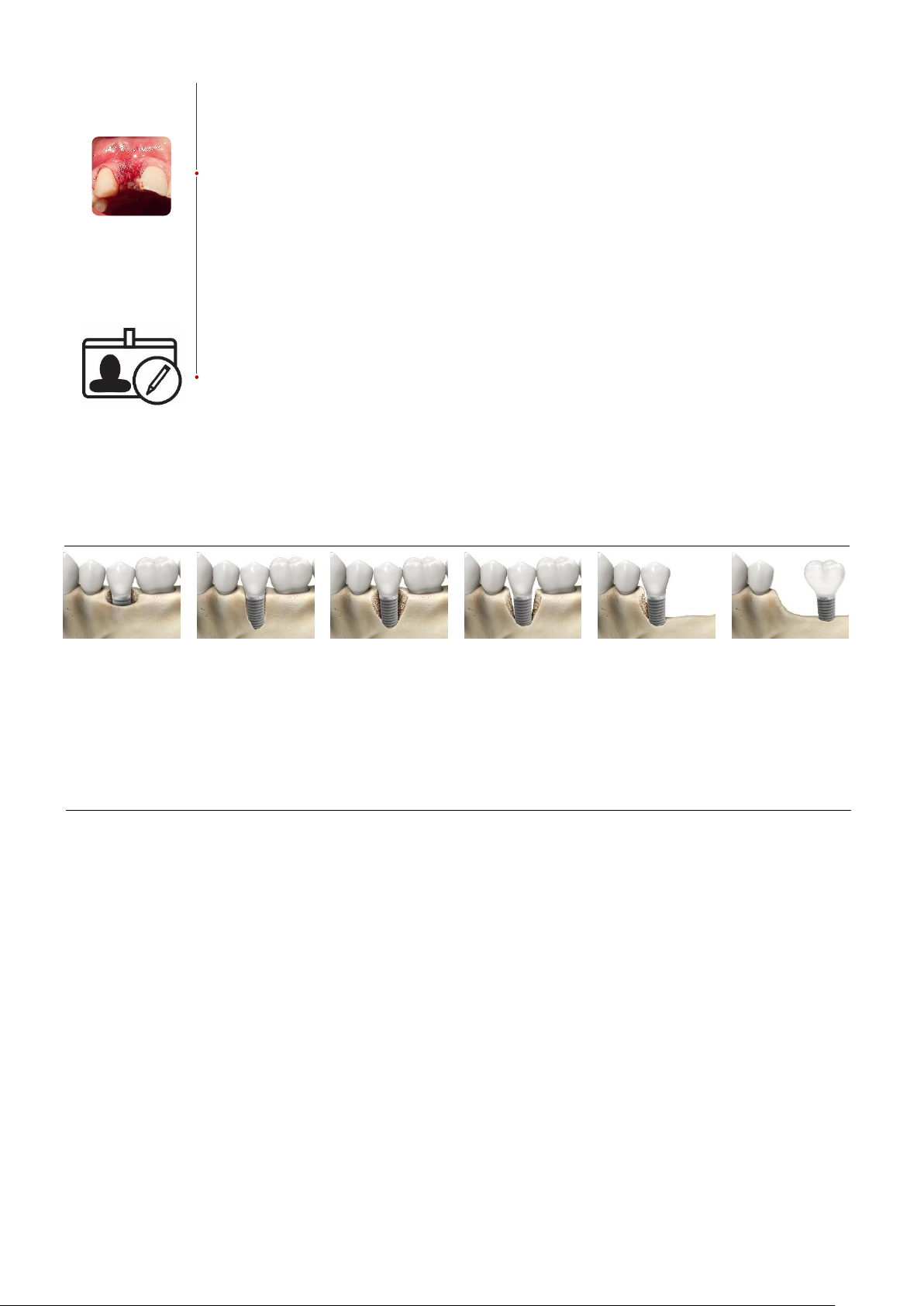
Classification of bone defect types
Modification of the defect types originally described by Renvert and Giovannoli in Chapter 6: Treatments. In: Renvert S, Giovannoli
JL, editors. Peri-Implantitis. France: Quintessence International; 2012.
Class I
Infra-bony defect
with all 4 walls
present
Class IIa
Narrow infra-bony
defect with 3 walls
and a dehiscence,
most frequently on
the buccal side
Class IIb
Infra-bony defect
with 3 walls
present
Class III
Infra-bony defect
with 2 intact walls
and large
dehiscence, usually
on the buccal side
and extended to
the proximal area
Class IV
Infra-bony defect
with 1 intact wall
Class V
Supra-bony defect,
with supra-crestal
threads exposed
and no wall support
Frequently asked questions
FAQ: How do I position the sponge in narrow spaces, for example in the pre-molar area?
A: The sponge becomes very elastic once it is wet and it is then easy to adapt to narrow spaces to enable good connection with the
implant.
FAQ: How do I know if the treatment was successful?
A: Close monitoring showing limited or no plaque accumulation and limited or no bleeding on probing, stable bone levels based on
radiographs, and no suppuration indicate a successful decontamination of the implant surface and absence of reinfection.
FAQ: What complications could occur after the surgical intervention?
A: Particular attention should be given to those cases where GBR procedures were performed since there is a risk of wound
dehiscence and graft exposure, thus creating a possibility of re-infection and failure of the bone graft.
FAQ: When should I perform a bone augmentation procedure?
A: Certain clinical situations favor GBR, while others suggest implant removal should be considered. Follow the summary shown
below for key clinical considerations to facilitate your decision making.
9. Flap closure
- Closed healing environment with the placement of a sterile cover screw or a
short healing abutment strongly advised in case complete regeneration is
planned
- Consider adjusting treatment to bone defect type (see below for
classification)
- Class I-II defects: resorbable membrane, 4-6 months healing time
- Class III-V defects: non-resorbable membrane, 6-9 months healing time
- Transmucosal healing is applied only when closed healing is not possible or
when complete regeneration is not planned
- Use tension-free flap closure (e.g., periosteal releasing incision and
horizontal mattress sutures)
10. Patient follow-up
- Treatment success defined in part by patient expectations (functional vs.
functional and esthetic)
- Successful decontamination if peri-implant soft tissue parameters (bleeding
on probing (BoP), pocket depth (PD), no pus) indicate absence of
inflammation/infection and radiographic bone levels remain stable (at 6-8
months post-surgery)
- Successful functional and esthetic treatment outcome is assessed based on
regular X-ray examinations (stable bone levels over time, bone gain after
GBR), and clinical examinations (absence of BoP, no increase in PD,
improved/stable clinical attachment levels)
- Regular local professional cleaning, regular assessment of plaque removal
and regular hygiene instructions as needed
- Be aware that GalvoSurge ensures an effective cleaning of the implant
surface but will not eliminate the possible cause/contributing factors
Favorable for GBR
Unfavorable for GBR
- Viable soft tissue (thick soft tissue with good vascularization,
sufficient width of keratinized mucosa, good suture properties
to allows tension-free flap closure)
- Appropriate implant position – correct axis, offers anchorage
to the prosthesis, implant diameter consistent with ridge
dimensions
- No or minimal interproximal bone resorption
- Bone defects class I-II
- Consider implant removal
- Poor soft tissue properties (thin soft tissue with poor
vascularization, insufficient width of keratinized mucosa,
spongy morphology that cannot sustain a firm suture, loss of
vestibular fixed mucosa)
- Inappropriate implant position – implant placed too far
buccally or its axis does not offer sufficient prosthetic support
- Advanced interproximal bone resorption
- Bone defects class III - V
 Loading...
Loading...