Page 1
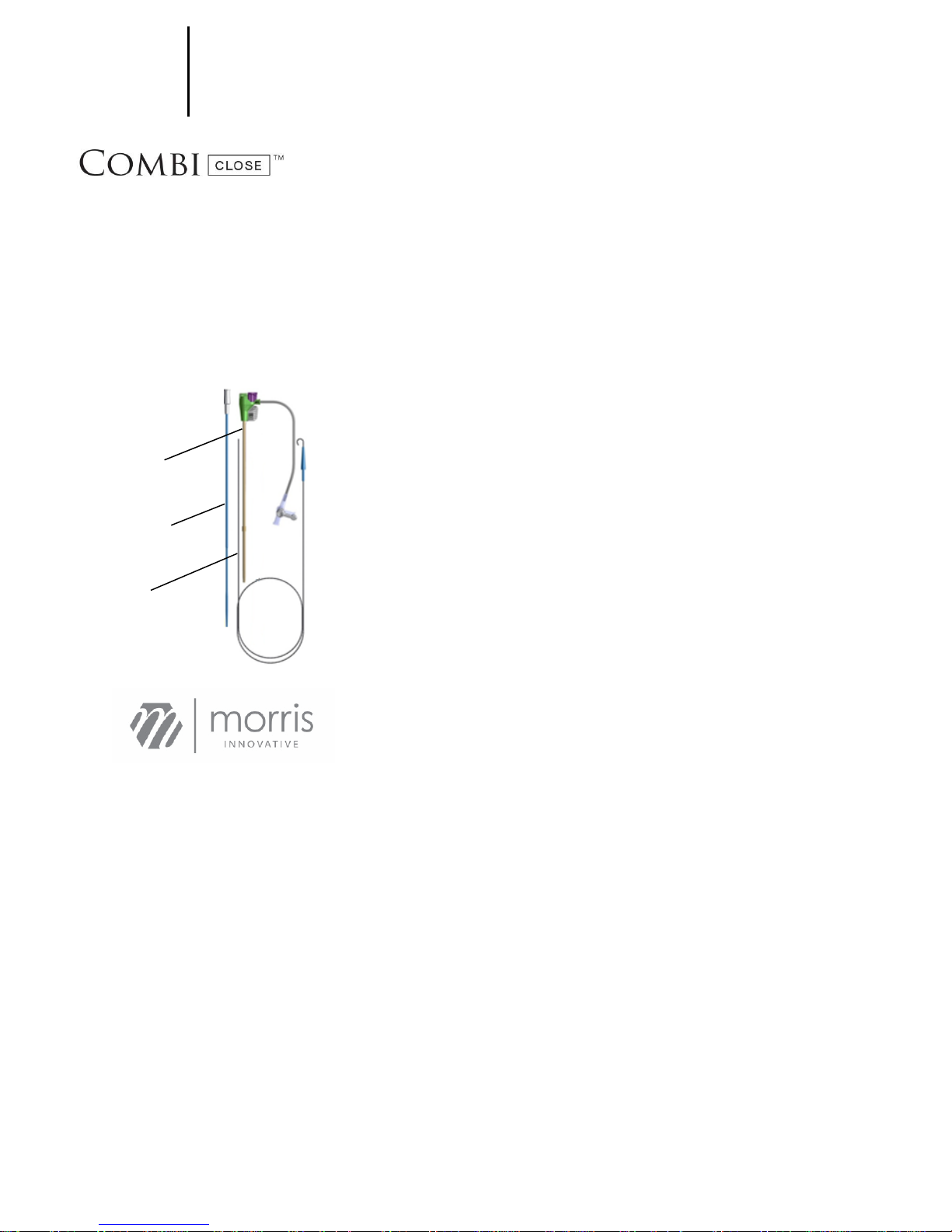
F I S H ™ S
Introducer
Closure Patch
Vessel Dilator
Guide wire
DEVICE P
FEMORAL INTRODUCER S HEATH & HEMOSTASIS
DEVICE
INSTRUCTIONS FOR USE
Read instructions before use.
Caution:
‘Federal law restricts this device for use by or on the order of a physician (or allied healthcare
professionals authorized by or under the direction of such physicians) who have been trained by an
authorized representative of MI, Inc. in the use of the FISH™ Device.”
CONTENTS:
Sheath with
907 W. Second Street, Bloomington, IN 47403 | 1-888-647-4465
SYSTEM COMPONENTS / DESCRIPTION
A. Introducer Sheath with Closure Patch
The Femoral Introducer Sheath and Hemostasis Device (FISH™ Device) facilitates percutaneous entry of an
intravascular device and aids in reducing time to hemostasis and ambulation for femoral arterial access. French
sizes of the FISH™ Device indicated by color coding. Listed below are the two available French sizes and their
corresponding color.
FRENCH COLOR
6 (2.0 mm) Green
8 (2.7mm) Orange
B. Vessel Dilator
The vessel dilator atraumatically transitions the guide wire to the introducer sheath through a tapered tip, which
opens the tissue from the skin to the vessel below.
C. Guide Wire
The guide wire is provided to maintain access to the vessel upon removal of an 18 or 21 gauge introducer needle
during the insertion of the FISH™ Device.
NOTE: The introducer needle is not included in the kit, so a sterile 18 or 21 gauge needs to be provided by the user
according to preference.
INDICATIONS
The Femoral Introducer Sheath and Hemostasis device (FISH™ Device) is intended for hemostatic closure of the
femoral artery access sites. The system is indicated for use in reducing time to hemostasis and time to
ambulation in patients who have undergone diagnos tic procedures using 5, 6, 7, or 8 French procedural sheaths.
CONTRAINDICATIONS
This product should not be used in patients who have a known sensitivity or allergy to porcine derived material of
resorbable sutures.
WARNINGS
Do not use with Lipiodol contrast media, Ethiodal*, or contras t media that includes components of these agents.
Do not leave the FISH™ Device in the artery for prolonged per iods of time (> 24 hrs.) without an obturator or
catheter assisting and supporting the cannula wall.
The FISH™ Device is for one use only. The function and/ or performance of the device may be destroyed by
reusing, resterilizing, or cleaning the device. Additionally, adverse patient reactions may result. Morris
Innovative, Inc. will not be responsible for any damages or expenses that may result for reusing the
FISH™ device.
If the package of the FISH™ Device is damaged, stained, or appears tampered with/opened prior to use do not
use.
Do not autoclave. The introducer s heath and its components may be damaged by ex posure to temperatures
above 54° C (130° F).
Do not expose device to organic solvents.
*Thiokol is a trademark of Guerbet S.A.
PRECAUTIONS
Prior to use, make sure the French size is correct for the catheter to be used.
When the FISH™ Device is used, the entire procedure should occur aseptically.
A power injector should not be used through the 3-way stopcock to the side tube.
Note expiration date on the device, and do not use the device if it is labeled as being expired.
Store FISH™ devices in a dark, cool, dry place. A void humidity and direct sunlight.
Use of the FISH™ System in diagnostic patients has not been evaluated in patients receiving glycoprotein
IIb/IIIa inhibitors.
Do not use the FISH™ Device if the puncture is made through the posterior wall of the femoral artery or if there
are multiple punctures as such punctures may result in a retroperitoneal hematoma.
Special Patient Populations
The safety and effectiveness of the FISH™ Device has not been established in the following patient populations:
Patients who are pregnant or lactating
Patients who are < 18 or > 80 years of age
Patients with bleeding diathesis or known hypercoagu lable disorders
Patients with bleeding or platelet disorders
Patients having uncontrolled hyper tension (systolic BP > 180mmHg)
Patients having auto-immune disorders
Patients having vascular grafts at the puncture site
Patients receiving glycoprotein IIb/IIIa inhibitors
Patients with: Pseudoaneurysm, AV fistula, intraluminal thrombus, or arterial dissection present in the
ipsilateral femoral artery prior to arterial closure
Patients having intra-procedural bleeding around access site
Patients having a palpable ipsilateral hematoma of any size obs erved during the catheterization procedure
Patients developing absent pedal pulses in the ips ilateral lower extremity during the catheterization procedure
Patients needing a procedure requiring an introducer s heath size of > 8F or < 4F
Patients having arterial closure site depth > 7.5cm
Patients having ACT > 400 seconds at the time of introducer sheath removal
Adverse Effects of the Device on Health
The FISH™ System was evaluated in a randomized controlled clinical investigation involving 206 diagnostic
patients enrolled at 8 United States clinical sites; 139 subjects (67%) received the FISH™ Device and 67 subjects
received (33%) the control, Manual Compression (MC). Prior to enrollment of r andomized patients, each site
enrolled non-randomized roll-in patients for training purposes. There were a total of 19 roll-in patients in the
diagnostic study.
There was one (1) death reported during the randomized investigation, which w as not device-related. This patient
was randomized to the FISH™ device.
Closure method related adverse events seen in the clinical study were:
Hematoma
Bleeding Requiring Transfusion
Pseudoaneurysm Requiring Thrombin Injection
Potential complications of allergic reaction, adhesion formation, infection or abscess, foreign body reaction,
wound dehiscence, or vessel occlusion were not seen. The following table (Table 1) shows the adverse events
from the diagnostic clinical study.
Page 2
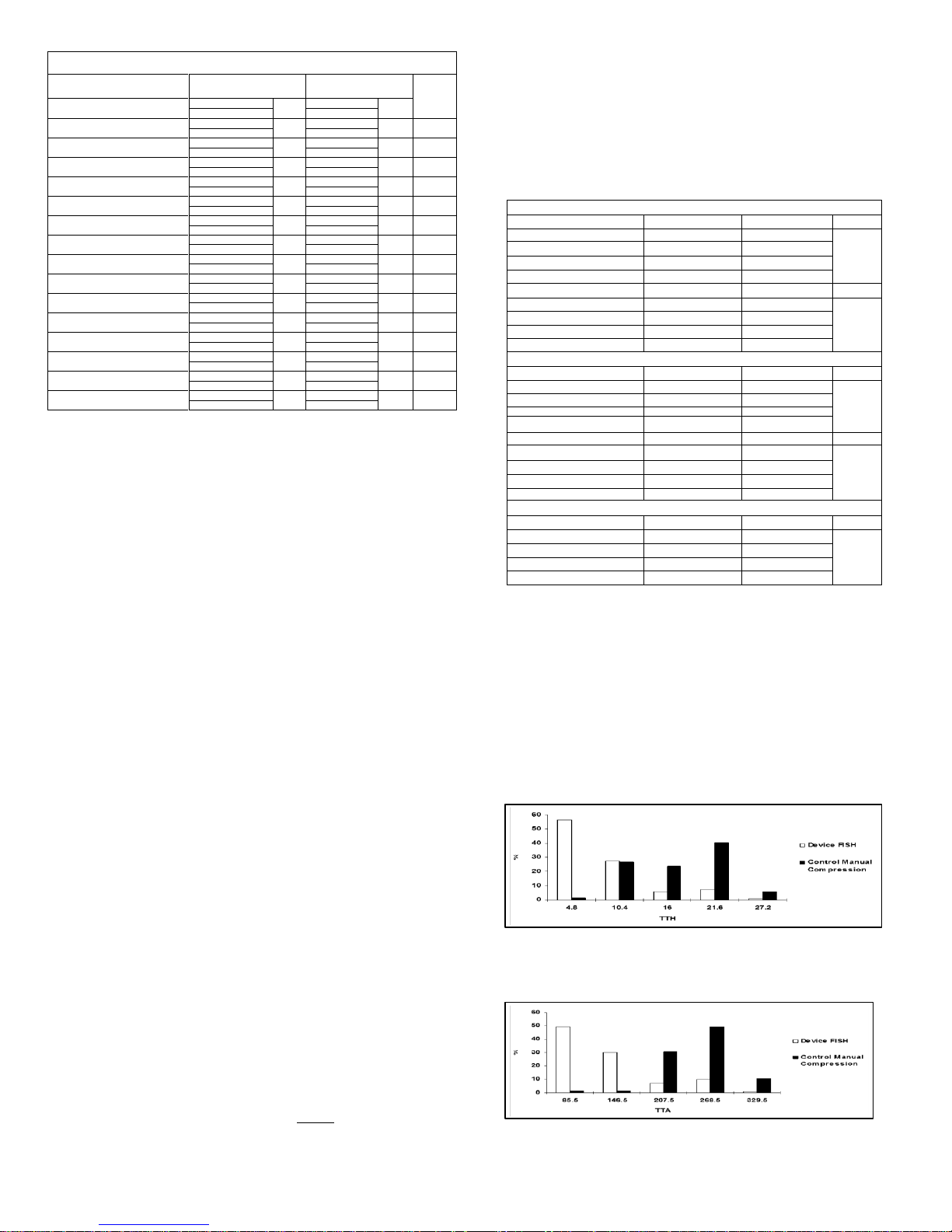
Cumulative Major and Minor Complications – Blackwater Test for Equivalence
Randomized Subjects N = 206
FISH Device (n=139)
Manual Comp. (n=67)
p-value
**
% of patients
No. of
Events
% of patients
No. of
Events
95% CI*
95% CI*
Combined Major Complications
0.72% 1 0%
0
<0.0001
(0.02%, 3.94%)
(0.0%, 5.36%)
Access-site related bleeding requiring transfusion
0.72% 1 0
0
<0.0001
(0.01%, 2.88%)
(0.0%, 3.42%)
New ischemia in ipsilateral leg
0 0 0
0
-(0.0%, --)
(0.0%, --)
Vascular surgical repair, US-guided compression,
Transcatheter embolization, or stent graft
0 0 0
0
-(0.0%, --)
(0.0%, --)
Surgery for access-site related nerve injury
0 0 0
0
-(0.0%, --)
(0.0%, --)
Permanent access-site related nerve injury
0 0 0
0
-(0.0%, --)
(0.0%, --)
Access-site related infection requiring IV
antibiotics and/or extended hospitalization
0 0 0
0
-(0.0%, --)
(0.0%, --)
Combined Minor Complications
2.88% 4 1.49%
1
0.039
(0.79%, 7.20%)
(0.04%, 8.04%)
Access-site related hematoma > 6cm
2,16% 3 1.49%
1
0.012
(0.45%, 6.18%)
(0.04%, 8.04%)
Pseudoaneurysm treated with ultrasound-guided
thrombin injection
0.72% 1 0
0
<0.0001
(0.13%, 3.73%)
(0.02%, 5.14%)
Pseudoaneurysm treated with ultrasound-guided
fibrin adhesive injection
0 0 0
0
--
(0.0%, --)
(0.0%, --)
Non-treated pseudoaneurysm (documented by
ultrasound)
0 0 0
0
--
(0.0%, --)
(0.0%, --)
Non-treated AV fistula (documented by
ultrasound)
0 0 0
0
--
(0.0%, --)
(0.0%, --)
Device Success***
99%
--
--
--
--
137/139
--
Procedure Success****
100%
--
100%
--
--
139/139
67/67
Primary Effectiveness
Time to Hemostasis (Minutes)
FISH™
Manual Compression
p-value
N
138
67
< 0.0001
Mean (SD)
8.9 (6.65)
17.2 (6.7)
Median
6
17
Min – Max
2 - 40
7 – 55
Time to Ambulation (Hours)
FISH™
Manual Compression
p-value
N
130
65
<0.0001
Mean (SD)
2.4 (2.1)
4.3 (1.0)
Median
2.0
4.2
Min – Max
0.9 – 19.6
1.3 – 7.3
Secondary Effectiveness
Time to Eligible Discharge (Hours)
FISH™
Manual Compression
p-value
N
129
65
<0.0001
Mean (SD)
3.0 (3.1)
5.5 (4.0)
Median
2.3
4.5
Min – Max
1 – 22.4
1.5 - 24.2
Time to Discharge (Hours)
FISH™
Manual Compression
p-value
N
126
65
<0.0001
Mean (SD)
16.2 (43.1)
24.9 (53.1)
Median
3.0
4.9
Min – Max
1.5 - 263
3.4 – 217.9
Equivalence Study At 30 Days
Discomfort (Subjective Scale 0-10)
FISH™
Manual Compression
p-value
N
138
67
0.147
Mean (SD)
0.51 (1.5)
0.21 (1.0)
Median
0
0
Min – Max
0 - 8
0 – 6
Table 1 – Major and Minor Complications through 30 Days – Diagnostic ITT Patients
* Exact 95% confidence interval based on Clopper-Pearson method
** Blackwater’s test with an equivalent limit of 0.05. The significance level of 0.041 was used for the interim
*** Device Success – the ability to achieve hemostasis without major adverse events of the use of mechanical compression and
within the allotted time (60 minutes).
**** Procedure Success – the ability to establish hemostasis in a given subject within any time period using any method.
Table 1 shows that the overall MACE rates were 0.72% and 0.0% for FISH™ device and control group, respectively.
The overall Minor Adverse Event rates were 2.88% and 1.5% for the FISH device and control group respectively.
Clinical Studies
The FISH closure device was studied in an open-label, randomized, multi- center clinical trial which enrolled 297
diagnostic and interventional patients. This United States based trial evaluated the FISH device to manual
compression. The study included both diagnostic ( N=206) and interventional (N=91) patients requiring a
procedure with and 8Fr or smaller sheath size. The study of interventional patients with the FISH™ device is
currently ongoing. Data from the interventional study is not discussed here. Each investigator had the
opportunity to enroll up to 2 roll-in patients which were non r andomized patients. There were a total of 28 roll -in
patients combined in the diagnostic and interventional study. The patients were randomized on a 2 to 1
randomization scheme (FISH™ device vs. manual compression). Of the 206 diagnostic patients enrolled in the
study, 139 received the FISH™ device and 67 received manual compression.
This study included 8 U.S. sites and enrolled patients between January 2004 and June of 2006. There were a
total of 40 investigators which enrolled patients for the study.
All patients enrolled in the study provided a signed written informed consent and agreed to return for a follow-up
evaluation at 30 ± 5days. The study included patients who were undergoing diagnostic or therapeutic coronary or
peripheral procedure performed percutaneously via the common femoral artery. The candidates were required
to meet general inclusion and exclusion criteria. The patients did not require a femoral artery angiogram prior to
placement of the FISH Device.
The null hypothesis for safety was that the experimental device had a major adverse event rate that exceeded
that of the control by a delta of 5%. The alternate hypothesis was that the exper imental device has a pr imary
safety endpoint rate less than that of the control or exceeding that of the contr ol by no more than the delta 5%.
Null Hypothesis
MII FISH (%MACE) > Manual Compression (%MACE) + 5% delta
Alternative Hypothesis
MII FISH (%MACE) < Manual Compression (%MACE) + 5% delta
For the diagnostic patients, the FISH device demonstrated safety with a total adverse event rate of 0.7% (1/139)
versus the control 0.0% (0/67). The one event for the FISH device was a site related bleeding requiring
transfusion. These rates for MACE in the diagnostic patients were found to be equivalent (p < 0.0001) under the
experimental conditions outlined prospectively in the investigational plan.
The minor adverse event rate was low for both the FISH device (2 .9%) and the control (1.5%), the tests for
equivalence showed these to be equal (p=0.039). The events for the device include 3 hematomas > 6cm and 1
Pseudoaneurysm. For the control there was one hematoma > 6cm. During the course of this clinical trial ther e
was one patient death (1 FISH, 0 Manual Compression). The death was not related to the use of the device.
There were no Unanticipated Access Site Related Adverse Events.
Effectiveness Results
In all effectiveness endpoints the FISH device proved s uperior in diagnostic patients compared to the control
manual compression. The median time for hemostasis in the FISH patients was 6 minutes versus 17 minutes for
the control group manual compression. The median time for ambulation for the FISH device was 2 .0 hours for the
FISH group versus 4.2 hours for the control. The median time to eligible discharge for the FISH device was 2.3
hours versus 4.5 hours for the control. The median time to eligible discharge for the FISH device was 2.3 hours
versus 4.5 hours for the control manual compression. The median time to discharge was 3.0 hours for the FISH
patients versus 4.9 hours for the control group manual compression. The following table (Table 2) shows the
effectiveness results.
Table 2 – Diagnostic Procedures: Primary Effectiveness Results ITT
The effectiveness calculations were based on the Wilcoxon Two-Sample Test using a normal approximation and two-sided criteria
(Pr > Z < .0001).
The results of the statistical analyses demonstrate that the FISH™ device is superior to Manual Compression in
terms of effectiveness measures for vascular hemostasis, ambulation, eligible discharge, discharge and
equivalent relative to discomfort subjectively measured at 30 days post pr ocedure. The FISH device has
demonstrated safety through its low incidence of complications in diagnos tic patients when compared to manual
compression.
Effectiveness Endpoints
Time to Hemostasis (TTH) was measured from the time of introducer sheath pull to the time the patient
achieved hemostasis. For this study, the time of hemostasis was defined as “Absence of oozing blood that is
readily treated by light compression methods (e.g. sandbags, pressure dressing, light manual pressure)”. The
study was designed to demonstrate TTH superiority as compared to the control therapy.
Figure 1 Histogram of Percentage of Patients vs. Time to Hemostasis (in minutes)
Time to Ambulation (TTA) – this was measured from the time of introducer sheath removal to the time when
the patient stood at the bedside and walked at least 20 feet without evidence of re-bleeding. The study w as
designed to demonstrate TTA superiority as compared to the control therapy.
Figure 2 Histogram of Percentage of Patients vs. Time to Ambulation (in minutes)
Time to Eligible Discharge (TTED) – this was measured from the time of introducer sheath pull to the time when
the patient was deemed eligible for discharge from the hospital based onl y on the condition of the access site.
The study was designed to demonstrate TTED superiority as compared to the control therapy.
Page 3

-1.5
-1
-0.5
0
0.5
1
1.5
2
2.5
Device FISH
Control Manual
Compression
Cohort
Discomfort
Figure 2
Figure 3
Figure 4
Figure 5
Figure 1
Figure 3 Histogram of Percentage of Patients vs. Time to Eligible Discharge (in minutes)
Time to Discharge (TTD) – this was measured from time of introducer sheath removal to the time the patient
was discharged. The study was designed to demonstrate TTD superiority as compared to the control therapy.
Figure 4 Histogram of Percentage of Patients vs. Time to Discharge (in minutes)
Patient Discomfort – All patients were subjectively asked at the 30 day follow up to rate their site related
discomfort from 0 to 10, with 0 being no pain and 10 being the worst pain imaginable. The results from this
subjective study showed the device to be equal to the control.
Figure 5 Average and Standard Deviation of Patients Discomfort (Subjective Scale 0-10)
PROCEDURE SUCCESS RATE
Procedure Success Rate (defined as the number of patients in which hemostasis was achieved with freedom from
major complications vs. the number attempted). This includes hemostasis w hich was achieved using adjunctive
compression (such adjunctive compression is typically for ≤ 5mintues).
Device failure was defined as an instance in which hemostasis could not be achieved using the FISH™ Device
within an allotted time (60 minutes) or with Manual Compression (Contr ol) – that is when additional means s uch
as a fem-stop or a mechanical compression de vice were required to achieve hemostasis. Four cases of device
failure were reported – all but one were interventional subjects.
CONCLUSIONS DRAWN FROM STUDIES
Based on the results from the clinical, in vivo and in vitro studies there is valid scie ntific evidence and reasonable
assurance that the FISH™ device is safe and effective when used in accordance with the instructions for use.
The FISH™ device has demonstrated safety through its low incidence of complications in diagnostic patients when
compared to manual compression. The FISH™ Device has demonstrated effectiveness by achieving hemostasis
and ambulation earlier than the control group manual compression.
RECOMMENDED PROCEDURE
The procedures and their techniques presented in these instructions are not representative of all acceptable
protocols. Additionally, they are not meant to replace or override the physician’s judgment in treating a patient.
The procedure listed below involves four processes: 1) ins erting the needle, 2) placing the patch, 3) advancing the
introducer sheath, and 4) removing the introducer sheath.
NOTE: The introducer needle is not included in the kit, so a sterile 18 or 21 gauge needs to be provided by the user
according to preference.
Needle Insertion
1. Using controlled sterile technique, remove the FISH™ Device and its contents fr om the package.
2. Remove air from the FISH™ Device by flushing it with a suitable isotonic solution, leave flush port OPEN to
facilitate bleedback.
3. Insert the vessel dilator through the introducer sheath hemostas is valve. At the hub, snap it into place. Flush
the dilator with a suitable isotonic solution.
4. CAUTION: After the dilator is in the introducer sheath, do not attempt to remove the dilator or it may displace
the release wire allowing the patch to be independent prematurely.
5. Using aseptic technique, introduce the cannula of the needle into the vessel (Figure 1).
6. Securing the needle by holding it in place, insert the flexible end of the guide wire through the needle and into
the vessel. In the case that a J tip is used, slide the guide wire introducer over the J in order to straighten it
before insertion. Advance the guide wire to the proper depth (Figure 2).
7. Withdraw the needle while holding the guide wire in place. Apply pressure to the puncture site until the
introducer sheath is inserted.
Patch Placement
1. Place the FISH™ Device over the guide wire. (Figure 3). A release wire that travels from within the proximal
hub to the tip of the patch will hold the patch until it is placed in the vessel wall.
2. Keeping the seam portion of the cuff facing down toward the skin and the “numbers” on the introducer sheath
hub (B, Figure 4) facing up, VERY SLOWLY advance the assembly through the tissue and into the vessel.
There are two methods for confirming proper patch placement:
A. The user may feel the positive stop or resistance of the cuff ( A Figure 4) as it approached the artery wall.
B. Leave the side port of the introduc er sheath open to visualize bleed back.
3. Once proper patch placement is achieved, stop advancing the introducer sheath.
CAUTION: At this point if the device needs to be retrie ved, grasp all of the sutures along with introducer
sheath and remove over guide wire.
4. Pull the release wire completely out of the introducer sheath and discard (Purple cap marked #2) (Figure 5).
5. Detach the suture compression tab (#3) and place it anterior to the access site. The suture should be kept
straight and in view of the operator (Figure 6).
Advancement
1. With the release wire removed, the introducer sheath must be advanced into working position (with hub
touching the skin), which releases the patch inside the artery. Observing no movement of the compression tab
and suture during introducer sheath advancement is an indic ation of proper patch placement (Figure 6).
Page 4

ONLY
CAUTION: Federal (USA) law
Batch Code
Use by
Sterilized using Ethylene Oxide
CAUTION: Refer to
Do not reuse
2
Latex Free
Latex
Figure 6
Figure 7
Figure 9
Figure 8
Compression
1. While applying pr essure to keep introducer sheath in place, pull the compression tab about 5 inches on a line
parallel to the introducer sheath and guide wire ( Figure 7). The knots on the compression suture serve as a
visual reference and will slide toward each other as the intravascular portion of the patch is cinched agains t
the artery wall. The suture knots should be approximately 1.5 to 2.5 inches apart.
2. Cut sutures at a point below the skin level to avoid potential infection. If knots are c loser than 1 inch, the cuff
may have been placed inside of the artery and proper closure will not be possible. If this is the case, proceed
with “Removal of both FISH and Patch” instructions below.
Removal of Both FISH™ and Patch Instructions
If the operator believes the FISH™ Device is misplaced or out of position or needs to be exchanged for a larger
French size, the following steps should be taken:
A. Insert guide wire into intr oducer sheath
B. Pull the r elease wire on the introducer sheath to free the patch from introducer sheath
C. With the guide wire in place, remove the introducer sheath. The patch may now be removed over the guide
wire by pulling both the compression and tabbed sutures s imultaneously.
Repuncture
If an additional procedure is required within 30 days, please access the opposite femoral ar tery (preferred) or
access 1 cm above the current FISH™ device access site. The device has an intra-arterial sleeve and an extravascular positioning cuff.
Suggested Aftercare
The following are the recommended times for aftercare and discharge for both non-heparinized and heparinize d
patients:
Procedural (If using FISH only for closing, proceed to Introducer Sheath Removal below)
1. With the introducer sheath and patch in working position, detach the dilator from the hub and withdraw both the
guide wire and dilator.
CAUTION: The introducer sheath tip can become damaged if the dilator is removed prior to the introducer s heath
being fully advanced to the working position.
2. Before placement of wires or catheters through the introducer sheath, aspirate and flush from the side port to
remove any potential air. To aid in the prevention of thrombus, a heparinized saline d rop via the side port should
be considered.
3. To introduce a selected catheter into the hemostatic hub use one of the following methods:
A. Straighten the catheter by hand and insert by holding as close to the tip as possible OR
B. Insert a guide wire into the introducer sheath hub, then load the catheter onto the wire.
NOTE: If measuring right atrial pressure and/or determining cardiac output by thermodilution methods,
discontinue infusion through the side port to prevent errors in measurement. Reconnect after measurements are
taken. If exchanging a catheter, slowly remove the catheter from the introducer sheath hub and repeat insertio n
process.
NOTE: Once the introducer sheath is in working position, if the patch needs to be retrieved, first insert guide wire,
remove the introducer sheath, and remove the patch by pulling sutures over the guide wire.
Introducer Sheath Removal
1. With the intr oducer sheath and patch in working position, detach the dilator from the hub and withdraw both
the guide wire and dilator.
2. If the introducer sheath was not used as a procedural sheath, leave the introducer sheath in the patient for
approximately 3-5 minutes to allow the SIS material to fully hydrate.
3. To remove the introducer sheath, place firm downward pressure a t the site and slowly remove the intr oducer
sheath (Figure 8).
4. Maintain firm pressure at the site as needed to allow the SIS plug to naturally fill the puncture site and attain
hemostasis (Figure 9).
5. Ensure sutures are not visible: treat puncture site appropriately to minimize the risk of infection.
Patients receiving the FISH™ device should avoid bathing in a tub, swimming or sitting in a hot tub for 3 days post
procedure, however patients may shower, pat site dry and apply clean dressing.
Sterility
The FISH™ Device and its components are provided sterile and non- pyrogenic in its unopened packaging. The
contents are sterilized with ethylene oxide and are intended for single use only. Do not resterilize. The device and
components are latex free. Store in a cool dry place.
How supplied
Femoral Introducer Sheath and Hemostasis Device
6 French Device List Number/ REF 16-06-05 -S
Contains: Guide wire
6 French Introducer Sheath with Closure Patch
6 French Dilator
8 French Device List Number/ REF 16-08- 05-S
Contains: Guide wire
8 French Introducer Sheath with Closure Patch
8 French Dilator
Graphic Symbols for Medical device Labeling
restricts this device for use
by or on the order of a
physician
Distributed in the U.S. by Morris Innovative, Inc.
907 W. Second Street
Bloomington, IN 47403
Toll free Customer Service: 888.647.4465
Manufactured by MI, Inc. under the following U.S. Patent: 6,790,220
accompanying Documents
16-040, Rev. AI
 Loading...
Loading...