Page 1

Valiant Navion™
Thoracic Stent Graft System—Instructions for Use
Instructions for Use
Caution: Federal law (USA) restricts this device to sale by or on the order of a physician.
Page 2

© 2018 Medtronic. All rights reserved. Medtronic and Medtronic logo are trademarks of Medtronic. ™* Third-party brands are trademarks of their respective
owners. All other brands are trademarks of a Medtronic company.
Page 3

Symbol glossary
Explanation of symbols that may appear on package labeling
Refer to the device labeling to see which symbols apply to this product.
Standard Title:
ISO 15223-1:2016 Cor 2017 : Medical Devices — Symbols to be used with medical device labels, labeling and information to
be supplied
ASTM F2503-13: Standard Practice for Marking Medical Devices and Other Items for Safety in the Magnetic Resonance
Environment.
Symbol Reference Symbol title Explanatory text
ISO 15223-1,
Clause 5.4.3
ISO 15223-1,
Clause 5.1.6
ISO 15223-1,
Clause 5.1.3
ISO 15223-1,
Clause 5.4.2
ISO 15223-1,
Clause 5.2.8
ISO 15223-1,
Clause 5.1.1
ISO 15223-1,
Clause 5.6.3
ISO 15223-1,
Clause 5.1.7
ISO 15223-1,
Clause 5.2.4
ISO 15223-1,
Clause 5.1.4
ASTM F2503 MR conditional An item that has been demonstrated to pose no
N/A Quantity Indicates the quantity of devices present in the
N/A Manufactured in Indicates the manufacturing site of the device. A
N/A CAUTION: Federal law (USA) restricts
Consult instructions for use at this
website
Catalog number Indicates the manufacturer's catalogue number so
Date of manufacture Indicates the date when the medical device was
Do not reuse Indicates a medical device that is intended for one
Do not use if package is damaged Indicates a medical device that should not be used
Manufacturer Indicates the medical device manufacturer.
Nonpyrogenic Indicates a medical device that is nonpyrogenic.
Serial number Indicates the manufacturer's serial number so that
Sterilized using irradiation Indicates a medical device that has been sterilized
Use by Indicates the date after which the medical device
this device to sale by or on the order
of a physician.
Indicates the need for the user to consult the
instructions for use.
that the medical device can be identified.
manufactured.
use, or for use on a single patient during a single
procedure.
if the package has been damaged or opened.
a specific medical device can be identified.
using irradiation.
is not to be used.
known hazards in a specified MR environment with
specified conditions of use.
package.
manufacturing site is the facility where the product
is produced, transformed, or assembled into a
medical device.
Indicates that the device is to be sold only by or on
order of a physician
1
Page 4

Valiant Navion™
Thoracic Stent Graft System—Instructions for Use
Table of contents
1. Device description ........................................................................................................................................................... 2
2. Indications for use ........................................................................................................................................................... 4
3. Contraindications ............................................................................................................................................................ 5
4. Warnings and precautions .............................................................................................................................................. 5
5. Adverse events ................................................................................................................................................................ 8
6. Patient selection, treatment, and device selection ...................................................................................................... 9
7. Patient counseling information .................................................................................................................................... 13
8. How supplied ................................................................................................................................................................. 13
9. Summary of Clinical Studies ........................................................................................................................................ 14
10. Directions for use .......................................................................................................................................................... 39
11. Troubleshooting techniques ......................................................................................................................................... 47
12. Follow-up imaging recommendations including MRI safety information ................................................................ 50
13. Additional surveillance and treatment ......................................................................................................................... 52
14. Device Registration ....................................................................................................................................................... 52
15. Disclaimer of warranty .................................................................................................................................................. 53
1. Device description
The Valiant Navion™ thoracic stent graft system is designed for the endovascular repair of lesions in the descending thoracic
aorta (DTA). When placed within the target lesion, the stent graft provides an alternative conduit for blood flow within the
patient’s vasculature by excluding the lesion from blood flow and pressure.
The stent graft system is composed of 2 main components: the implantable Valiant Navion thoracic stent graft and the
disposable delivery system. The stent graft is preloaded into the delivery system. The loaded delivery system is inserted
endoluminally via the femoral or iliac artery and tracked through the patient’s vasculature to deliver the stent graft to the target
site. Upon deployment, the stent graft self-expands to conform to the shape and size of the seal zones above and below the
lesion.
The Valiant Navion thoracic stent graft system does not contain natural rubber latex; however, during the manufacturing
process, it may have had incidental contact with latex-containing products.
1.1. Stent graft
A single, primary Valiant Navion thoracic stent graft may be used by itself if its length is sufficient to provide the desired
coverage. Alternatively, it may be used in combination with additional Valiant Navion thoracic stent graft configurations that
increase the graft length distally or proximally to the primary section.
All stent grafts are composed of a self-expanding stent scaffold made from nitinol wire sewn to a fabric graft with nonresorbable
sutures. The metal scaffolding is composed of a series of serpentine stents stacked in a tubular configuration. Radiopaque
(RO) markers are sewn onto each component of the stent graft to aid in visualization and to facilitate accurate placement. The
nitinol stents are also visible under fluoroscopy. Refer to Table 1 (Stent graft materials) for a summary of the stent graft
materials.
The appropriate device sizing is incorporated into the sizing guidelines. Refer to Section 6.3 (Recommended device sizing)
and Section 6.4 (Device sizing recommendations) for detailed sizing information for all stent graft components.
Table 1. Stent graft materials
Component Material
Stents Nitinol (nickel-titanium) alloy
RO markers Platinum-iridium alloy
Graft fabric Polyester (PET)
Suture Polyester (PET) and ultra-high-molecular-weight polyethylene (UHMWPE)
2 Instructions for Use English
Page 5

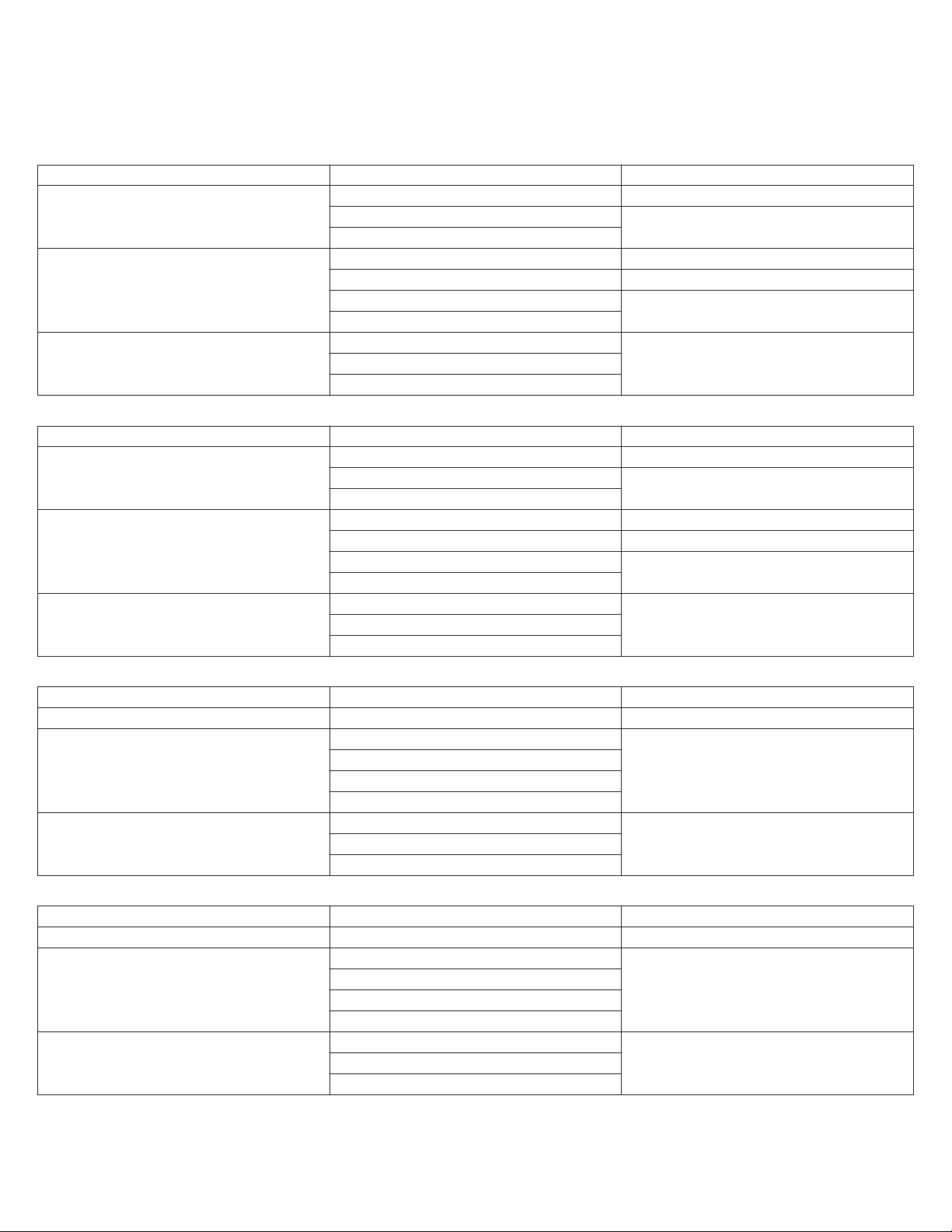
1.1.1. Stent graft configuration options
11
12
7
8
5
6
432
1
10
9
12
8
10
Figure 1. Stent graft configuration components
1. FreeFlo Straight
2. FreeFlo Tapered
3. CoveredSeal Straight
4. CoveredSeal Tapered
5. Proximal end
6. Distal end
7. FreeFlo stent
8. Internal stent
9. Support stent
10. RO marker
11. Covered length
12. Total length
Note: Figure 1 and all other product graphics appearing in this manual are not drawn to scale. They are for graphical
representation only, and the stent graft and delivery system components may appear differently under fluoroscopy.
Valiant Navion thoracic stent grafts are available in 4 configurations: FreeFlo Straight, FreeFlo Tapered, CoveredSeal Straight,
and CoveredSeal Tapered. Each stent graft configuration can be used either as a proximal or distal component; the proximal
end of a FreeFlo stent graft should never be placed inside the fabric-covered section of another graft. Stent grafts are available
in 18 Fr, 20 Fr, and 22 Fr delivery systems. Refer to Table 2 through Table 5 for stent grafts sizes in corresponding delivery
system sizes. Additional information on stent graft sizes is provided in Section 6.3 (Recommended device sizing)
and Section 6.4 (Device sizing recommendations).
FreeFlo Straight configuration
This configuration includes a FreeFlo proximal end and a CoveredSeal distal end. At the proximal end, a 6-peak (18 Fr or
20 Fr) or 7-peak (22 Fr) bare stent extends past the covered portion of the stent graft to provide additional fixation while
maintaining transvessel flow. The diameters of the proximal end and distal end of the FreeFlo Straight configuration are
constant throughout the covered length of the device.
The FreeFlo Straight configuration stent grafts are available in diameters ranging from 20 mm to 46 mm and covered lengths of
approximately 60 mm, 100 mm, 175 mm, and 225 mm.
Caution: The proximal end of a FreeFlo stent graft should never be placed inside the fabric-covered section of another graft as
doing so may result in abrasion of the fabric by the bare stent, resulting in graft material holes or broken sutures.
FreeFlo Tapered configuration
This configuration includes a FreeFlo proximal end and a CoveredSeal distal end. At the proximal end, a 6-peak (18 Fr or
20 Fr) or 7-peak (22 Fr) bare stent extends past the covered stent graft to provide additional fixation while maintaining
transvessel flow. The diameter of the proximal end of the FreeFlo Tapered configuration is larger than the diameter of the distal
end.
The FreeFlo Tapered configurations are available in proximal diameters ranging from 25 mm to 46 mm and distal diameters
ranging from 20 mm to 40 mm. The covered length is approximately 175 mm with a stent graft taper of 5 mm for the smallest
diameter configuration and 6 mm for the remaining sizes.
Caution: The proximal end of a FreeFlo stent graft should never be placed inside the fabric-covered section of another graft as
doing so may result in abrasion of the fabric by the bare stent, resulting in graft material holes or broken sutures.
Instructions for Use English 3
Page 6

CoveredSeal Straight configuration
1
1213
11
14
2
3
45
679
8
10
This configuration includes CoveredSeal proximal and distal ends. At the proximal end, a 6-peak (18 Fr or 20 Fr) or 7-peak
(22 Fr) internal stent with a 12-peak (18 Fr or 20 Fr) or 14-peak (22 Fr) W-stent are covered to provide additional fixation while
maintaining transvessel flow. The diameters of the proximal end and distal end of the CoveredSeal Straight configuration are
constant throughout the covered length of the device.
The CoveredSeal Straight configuration stent grafts are available in diameters ranging from 20 mm to 46 mm and covered
lengths of approximately 60 mm, 100 mm, 175 mm, and 225 mm.
CoveredSeal Tapered configuration
This configuration includes CoveredSeal proximal and distal ends. At the proximal end, a 6-peak (18 Fr or 20 Fr) or 7-peak
(22 Fr) internal stent with a 12-peak (18 Fr or 20 Fr) or 14-peak (22 Fr) W-stent are covered to provide additional fixation while
maintaining transvessel flow. The diameter of the proximal end of the CoveredSeal Tapered configuration is larger than the
diameter of the distal end.
The CoveredSeal Tapered configurations are available in proximal diameters ranging from 25 mm to 46 mm and distal
diameters ranging from 20 mm to 40 mm. The covered length is approximately 175 mm and 200 mm with a stent graft taper of
5 mm for the smallest diameter configuration and 6 mm for the remaining sizes.
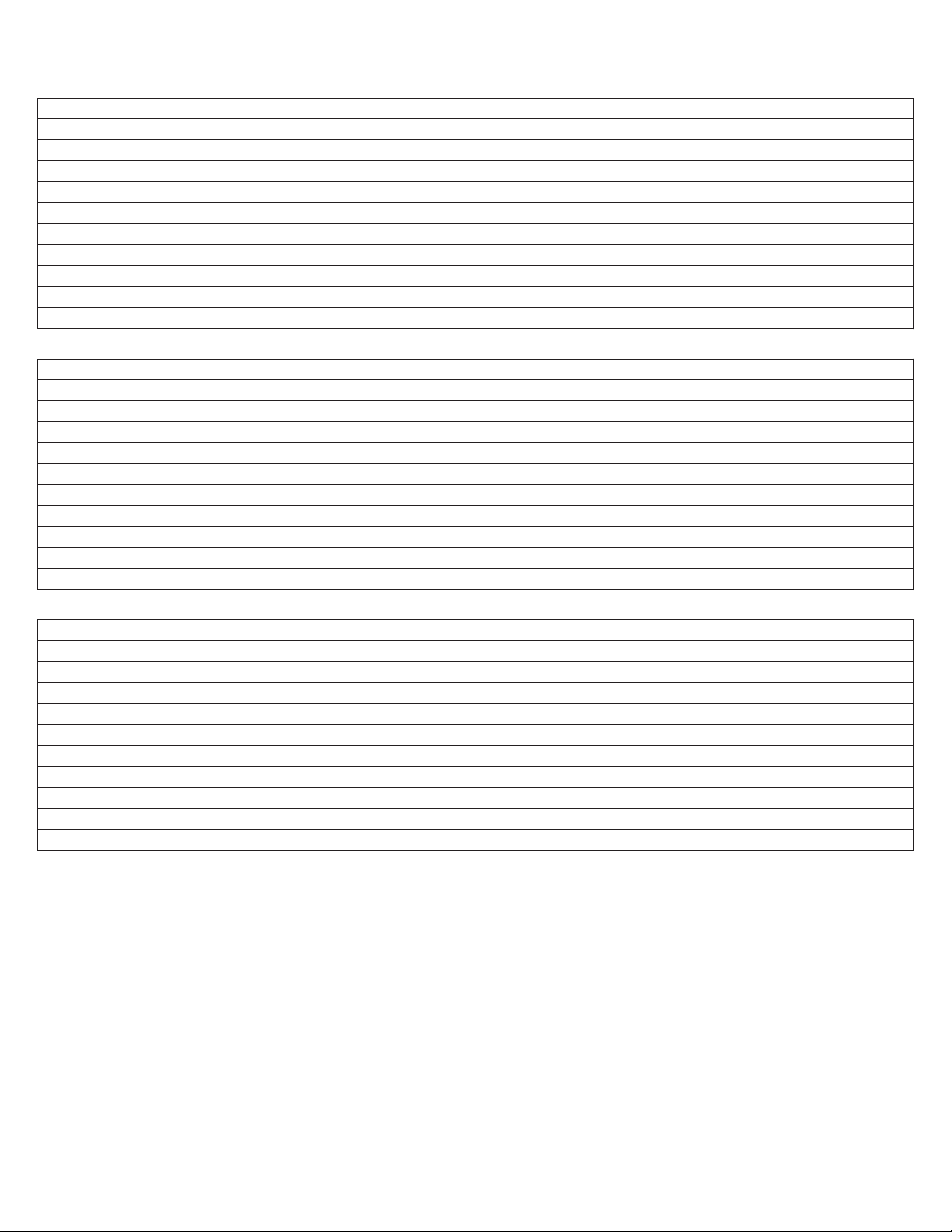
1.2. Delivery system
Figure 2. Delivery system
1. Luer connector
2. Screw gear
3. Slider handle
4. Trigger
5. Front grip
6. Graft cover
7. Stent stop
8. Tip capture mechanism
9. RO marker band
10. Tapered tip
11. Back-end lock
12. Tip capture release handle
13. Clamping ring
14. Flush port
The Valiant Navion delivery system consists of a single-use, disposable catheter with an integrated handle, intended to provide
controlled deployment. It is available in an outer diameter of 18, 20, and 22 Fr and a working length of 93 cm. The catheter
assembly is flexible and exclusively compatible with a 0.035 in (0.89 mm) guidewire.
A flexible tapered tip is attached to the end of the inner member and provides a smooth transition from the guidewire to the
outer graft cover. The external surfaces of the tapered tip and graft cover are coated with a lubricious hydrophilic coating. Once
activated with a sterile gauze saturated in saline, this coating facilitates vessel access and tracking through the anatomy. A
distal RO marker indicates the graft cover edge under fluoroscopy. The flush port includes a one-way valve that prevents
backflow of flush fluid and maintains hemostasis during the procedure, while allowing the delivery system to be flushed during
device preparation. The stent graft is deployed by rotating or retracting the integrated slider handle. The tip capture release
handle at the rear of the delivery system is unlocked and retracted to release the proximal end of the stent graft.
Note: The Reliant™ stent graft balloon catheter (packaged separately) can be used to remove wrinkles and folds from the graft
material and to assist in implanting the stent graft by modeling the covered stents.
2. Indications for use
The Valiant Navion thoracic stent graft system is indicated for the endovascular repair of all lesions of the descending thoracic
aorta (DTA) in patients having the appropriate anatomy including:
4 Instructions for Use English
Page 7

■
iliac or femoral artery access vessel morphology that is compatible with vascular access techniques, devices, or
accessories;
■
nonaneurysmal aortic diameter in the range of:
■
16 mm to 42 mm for fusiform and saccular aneurysms/penetrating ulcers
■
16 mm to 44 mm for blunt traumatic aortic injuries
■
19 mm to 45 mm for dissections;
■
proximal landing zone (nonaneurysmal aortic proximal neck length for fusiform and saccular aneurysms/penetrating ulcers
or nondissected length of aorta proximal to the primary entry tear for blunt traumatic aortic injuries and dissections) of:
■
≥ 20mm for FreeFlo configuration
■
≥ 25mm for CoveredSeal configuration; and
■
nonaneurysmal aortic distal neck length ≥ 20mm for FreeFlo and CoveredSeal configurations for fusiform and saccular
aneurysms/penetrating ulcers.
3. Contraindications
The Valiant Navion thoracic stent graft system is contraindicated in the following patient populations:
■
Patients who have a condition that threatens to infect the graft
■
Patients who are sensitive to or have allergies to the device materials (Table 1)
4. Warnings and precautions
4.1. Warnings and precautions - General Caution: Do not attempt to use the Valiant Navion thoracic stent graft system before completely reading and understanding the
information contained in the Instructions for Use. Failure to properly follow the instructions, warnings, and precautions may lead
to serious consequences or injury to the patient.
■
The Valiant Navion thoracic stent graft system should only be used by physicians and teams trained in vascular
interventional techniques, including training in the use of this device. Refer to Section 6.2.2 (Recommended skills and
training).
■
Always have a vascular surgery team available during implantation or re-intervention procedures in the event that
conversion to open surgical repair is necessary.
■
The long-term safety and effectiveness of the Valiant Navion thoracic stent graft system has not been established. All
patients should be advised that endovascular treatment requires lifelong, regular follow-up to assess the integrity and
performance of the implanted endovascular stent graft. Specific follow-up guidelines are described in Follow-up Imaging
Recommendations (Section 12). Of note, patients with specific clinical findings should receive enhanced follow-up.
Caution: Federal (USA) law restricts this device for sale by or on the order of a physician.
4.2. Warnings and precautions - patient selection, treatment, and follow-up
■
The Valiant Navion thoracic stent graft system is not recommended in patients who cannot undergo, or who will not be
compliant with, the necessary preoperative and postoperative imaging and implantation procedures described in Section 10
(Directions for use), Section 11 (Troubleshooting techniques), and Section 12 (Follow-up imaging recommendations).
■
The Valiant Navion thoracic stent graft system is not recommended in patients who cannot tolerate contrast agents
necessary for intra-operative and postoperative follow-up imaging. Refer to Section 12 (Follow-up imaging
recommendations).
■
The Valiant Navion thoracic stent graft system is not recommended in patients exceeding weight and/or size limits which
compromise or prevent the necessary imaging requirements.
■
Before the procedure, perform preoperative planning for access and placement. Refer to Section 6.3 (Recommended
device sizing). Key anatomic elements that may affect successful exclusion of the aneurysm include tortuosity, short landing
zones, and thrombus and/or calcium at the implantation sites. In the presence of anatomical limitations, a longer landing
zone may be required to obtain adequate sealing and fixation.
■
The use of this device requires administration of radiographic agents. Patients with preexisting renal insufficiency may have
an increased risk of renal failure postoperatively.
■
Inappropriate patient selection may contribute to poor device performance.
■
The Valiant thoracic stent graft systems have not been evaluated in the following patient situations and/or populations in
which:
■
The patient is pregnant.
■
The patient requires planned placement of the covered proximal end of the stent graft to occur in zones 0 or 1.
■
The patient has a thoracic aneurysm with a contained rupture or localized at the anastomosis of a previous graft
(pseudo-/false aneurysm).
■
The patient has a mycotic aneurysm.
Instructions for Use English 5
Page 8

■
The patient has a dissection (type A or B) or an intramural hematoma or an aortic rupture in addition to the thoracic
aneurysm.
■
The patient has received a previous stent or stent graft or previous surgical repair in the ascending and/or descending
thoracic aorta, and/or in the aortic arch.
■
The patient requires surgical or endovascular treatment of an infra-renal aneurysm at the time of implant.
■
The patient has had previous surgical or endovascular treatment of an infra-renal aortic aneurysm.
■
Treatment with the Valiant Navion thoracic stent graft would require intentional revascularization of the brachio-cephalic
artery, the left common carotid artery, or the celiac trunk.
■
The patient has had or plans to have a major surgical or interventional procedure within 30 days before or 30 days after
the planned implantation of the Valiant Navion thoracic stent graft. This does not include planned procedures that are
needed for the safe and effective placement of the stent graft (that is, carotid/subclavian transposition,
carotid/subclavian bypass procedure).
■
The patient has a significant and/or circumferential aortic mural thrombus at either the proximal or distal attachment
sites that could compromise fixation and seal of the implanted stent graft.
■
The patient has a connective tissue disease (for example, Marfan's syndrome, aortic medial degeneration).
■
The patient has a bleeding diathesis or coagulopathy, or refuses blood transfusion.
■
The patient has had an MI within 3 months of the procedure.
■
The patient has had a CVA within 3 months of the procedure.
■
The patient has a known allergy to anesthetic drugs.
■
The patient has a known hypersensitivity or contraindication to anticoagulants, or contrast media, which is not
amenable to pretreatment.
■
The patient has an active or systemic infection at the time of the index procedure.
■
The patient is less than 18 years old.
■
The patient has acute, uncomplicated Type B dissection.
■
The patient has chronic Type B dissection.
■
The patient has an aortic fistula.
■
The patient has aortitis or an inflammatory aneurysm.
■
All patients with endovascular repair must undergo periodic imaging to evaluate the stent graft and vessel. Significant
aneurysm enlargement (>5 mm), the appearance of a new endoleak, migration resulting in an inadequate seal zone, or
continued flow into the false lumen in the case of a dissection, should prompt further investigation and may indicate the
need for additional intervention or surgical conversion. An increase in aneurysm size and/or persistent endoleak may lead
to aneurysm rupture.
4.3. Warnings and precautions - implant procedure
■
Do not bend, kink, or otherwise alter the delivery system prior to implantation because it may cause deployment difficulties.
■
Do not advance the guidewire or delivery system if resistance is felt. The cause of resistance must be assessed in order to
avoid vessel or delivery catheter damage.
■
Stent graft wire fractures are more likely to occur in conditions with an excessively oversized endoprosthesis, flexion,
kinking, or bending during cardiac or respiratory cycles. Wire fractures may have clinical consequences, such as endoleak,
endoprosthesis migration, or adjacent tissue damage.
■
Oversize the aortic portion of the stent graft using the sizing guidelines in Section 6.3 (Recommended device sizing)
and Section 6.4 (Device sizing recommendations).
■
Strictly adhere to the Valiant Navion thoracic stent graft system sizing configurations and guidelines (Table 2
through Table 8) when selecting the device size. The appropriate device oversizing is incorporated into the sizing
guidelines. Sizing outside of this range can potentially result in endoleak, fracture, migration, infolding, or graft wear.
■
Oversizing of the stent graft to the vessel by more than 10% may be unsafe in the presence of dissecting tissue or
intramural hematoma.
■
An inadequate seal zone could increase the risk of endoleak or migration of the stent graft. Migration may also be caused
by deployment of the proximal stent into a thrombus filled or severely angled vessel. Refer to Section 6.1 (Patient
selection).
■
Manipulation of wires, balloons, catheters, and endografts in the thoracic aorta may lead to vascular trauma including aortic
dissection and embolization.
■
Wrinkling of graft material may promote thrombus formation. Inflate a conformable balloon within the deployed stent graft
lumen to reduce wrinkling of the graft material.
Note: Medtronic recommends the Reliant balloon for use with the Valiant Navion thoracic stent graft. Data is not available
for use of other balloons for remodeling the Valiant Navion thoracic stent graft.
6 Instructions for Use English
Page 9

■
Use the Reliant device according to the instructions for use supplied with the Reliant stent graft balloon catheter. Do not
attempt to use the Reliant device before completely reading and understanding the information supplied with the Reliant
stent graft balloon catheter.
■
Do not use the Reliant stent graft balloon catheter in patients with history of thoracic dissection disease. Do not overinflate the Reliant stent graft balloon within or outside of the graft material.
■
If the Reliant balloon's proximal and distal radiopaque markers are not completely within the covered portion of a stent
graft when expanding the prosthesis, there is an increased risk of vessel injury and/or rupture, and possible patient
death.
■
It is not recommended to position the Valiant Navion thoracic stent graft higher in the vessel in the presence of excessive
calcification or thrombus, due to the increased risk of dislodging material during distal repositioning of the Valiant Navion
thoracic stent graft. Refer to Section 10.5 (Positioning the delivery system).
■
Do not advance the Valiant Navion thoracic stent graft system when the stent graft is partially deployed and is apposed to
the vessel wall.
■
The proximal end of the covered Valiant Navion thoracic stent graft should not be placed beyond the origin of the left
common carotid artery (Zone 0 or Zone 1). See Figure 3.
Figure 3. Covered stent graft placement zones
■
Ensure that the Valiant Navion thoracic stent grafts are placed in an adequate landing zone comprised of suitable tissue.
Suitable tissue is defined as tissue without evidence of circumferential thrombus, intramural hematoma, ulceration, and/or
aneurysmal involvement. Failure to do so may result in inadequate exclusion or vessel damage, including perforation. Refer
to Section 6.1 (Patient selection).
■
Landing the proximal end of the device in dissected tissue could increase the risk of damage to the septum and could lead
to new septal tears, aortic rupture, retrograde dissection, or other complications.
■
When treating dissections, ensure the distal end of the device is in a straight portion of the aorta in order to reduce risk of
septum damage.
■
When treating acute dissections with multiple devices, it is recommended to deploy the proximal device first. Inadvertent
pressurization of the false lumen may result in retrograde dissection.
■
Consider adjunctive procedures to restore blood flow to malperfused branch vessels.
■
Any endoleak left untreated during the implantation procedure should be carefully followed after implantation.
■
Coverage of the left subclavian artery without revascularization may increase the risk of stroke.
■
Avoid occluding arterial branches that do not have collateral or protected perfusion to end organs or body structures. If the
LSA is to be covered, check the blood flow of the vertebral or cerebral arteries and the retrograde flow of the LSA. If
occlusion of the left subclavian artery ostium is required to obtain adequate neck length for fixation and sealing,
transposition or bypass of the LSA should be considered.
Caution: Patients with a patent LIMA-LAD (left internal mammary artery-left anterior descending artery) bypass should not
be considered for coverage of the LSA unless additional bypasses are performed prior to the stent graft procedure.
■
The proximal end of a FreeFlo stent graft should never be placed inside the fabric-covered section of another graft as doing
so may result in abrasion of the fabric by the bare stent, resulting in graft material holes or broken sutures.
Instructions for Use English 7
Page 10

4.4. Magnetic Resonance Imaging (MRI)
MRI may be used on the Valiant Navion thoracic stent graft only under specific conditions. Refer to Section 12.5 (MRI safety
information).
5. Adverse events
5.1. Potential adverse events
Adverse events or complications associated with the use of the Valiant Navion thoracic stent graft system that may occur or
require intervention include, but are not limited to:
■
Access failure
■
Access site complications (for example, spasm, trauma,
bleeding, rupture, dissection)
■
Adynamic Ileus
■
Allergic reaction (to contrast, antiplatelet therapy, stent
graft material)
■
Amputation
■
Anaphylaxis
■
Anesthetic complications
■
Aneurysm rupture
■
Angina
■
Aortic expansion (for example: aneurysm, false lumen)
■
Aortic valve damage
■
Aortic vessel rupture
■
Arrhythmia
■
Arterial stenosis
■
Atelectasis
■
Balloon rupture
■
Blindness
■
Bowel ischemia
■
Bowel necrosis
■
Bowel obstruction
■
Branch vessel occlusion
■
Breakage of the metal portion of the device
■
Buttock claudication
■
Cardiac tamponade
■
Catheter breakage
■
Cerebrovascular accident (CVA)/Stroke
■
Change in mental status
■
Coagulopathy
■
Congestive heart failure
■
Contrast toxicity
■
Conversion to surgical repair
■
Damage to the vessel
■
Death
■
Deployment difficulties/failures
■
Dissection, perforation, or rupture of the aortic vessel &
surrounding vasculature
■
Embolism
■
Endoleaks
■
Excessive or inappropriate radiation exposure
■
Extrusion/erosion
■
Failure to deliver the stent graft
■
Femoral neuropathy
■
Lymphocele
■
Myocardial infarction
■
Neck enlargement
■
Nerve injury
■
Neuropathy
■
Occlusion - Venous or Arterial
■
Pain/reaction at catheter insertion site
■
Paralysis
■
Paraparesis
■
Paraplegia
■
Paresthesia
■
Perfusion of the false lumen
■
Peripheral ischemia
■
Peripheral nerve injury
■
Pneumonia
■
Postimplant syndrome
■
Post-procedural bleeding
■
Procedural bleeding
■
Prosthesis dilatation
■
Prosthesis infection
■
Prosthesis rupture
■
Prosthesis thrombosis
■
Pseudoaneurysm
■
Pulmonary edema
■
Pulmonary embolism
■
Reaction to anesthesia
■
Renal failure
■
Renal insufficiency
■
Reoperation
■
Respiratory depression or failure
■
Retrograde type A dissection
■
Sepsis
■
Seroma
■
Sexual dysfunction
■
Shock
■
Spinal neurological deficit
■
Stenosis
■
Stent graft migration
■
Stent graft misplacement
■
Stent graft occlusion
■
Stent graft rupture (for example: holes, tears)
8 Instructions for Use English
Page 11

■
Fistula (including aortobronchia, aortoenteric, aortoeso-
■
Stent graft twisting or kinking
phogeal, arteriovenous, and lymph)
■
Gastrointestinal bleeding/complications
■
Genitourinary complications
■
Hematoma
■
Hemorrhage/bleeding
■
Hypotension/hypertension
■
Infection or fever
■
Insertion or removal difficulty
■
Intercostal pain
■
Intramural hematoma
■
Leg edema/foot edema
■
Loss of patency
■
Transient ischemic attack (TIA)
■
Thrombosis
■
Tissue necrosis
■
Vascular ischemia
■
Vascular trauma
■
Wound dehiscence
■
Wound healing complications
■
Wound infection
5.2. Adverse Event Reporting
Any adverse event or clinical incident involving the Valiant Navion thoracic stent graft system should be immediately reported to
Medtronic Vascular. To report an incident in the US, call (800) 465-5533.
6. Patient selection, treatment, and device selection
6.1. Patient selection
Patient selection factors should include, but are not limited to:
■
Patient age and life expectancy
■
Comorbidities (for example, cardiac pulmonary or renal insufficiency before surgery, morbid obesity, and so forth)
■
Patient’s suitability for open surgical repair
■
Patient’s anatomical suitability for endovascular repair
■
The risk of lesion rupture compared to the risks of endovascular repair
■
Ability to tolerate general, regional, or local anesthesia
■
Iliac or femoral access vessel morphology, such as thrombus, calcium formation, or tortuosity, that is compatible with
vascular access techniques, devices, or accessories
■
For treatment of aneurysms and penetrating atherosclerotic ulcer (PAU): non-aneurysmal aortic diameter in the range of
16 mm to 42 mm
■
For treatment of blunt traumatic aortic injuries (BTAI): non-aneurysmal aortic diameter in the range of 16 mm to 44 mm
■
For treatment of dissections: healthy, non-diseased aortic diameter in the range of 19 mm to 45 mm
■
Proximal landing zone (nonaneurysmal aortic proximal neck length for fusiform and saccular aneurysms/penetrating ulcers
or nondissected length of aorta proximal to the primary entry tear for blunt traumatic aortic injuries and dissections;) of:
■
≥ 20mm for FreeFlo configuration
■
≥ 25mm for CoveredSeal configuration; and
■
Nonaneurysmal aortic distal neck length ≥ 20mm for FreeFlo and CoveredSeal configurations for fusiform and saccular
aneurysms/penetrating ulcers.
6.2. Treatment
6.2.1. Individualization of Treatment
The warnings and precautions previously described in Section 4 should be carefully considered relative to each patient before
use of the Valiant Navion thoracic stent graft system. The risks and benefits should be carefully considered for each patient
before use of the Valiant Navion thoracic stent graft system.
Proper sizing of the device is the responsibility of the physician. Refer to Section 6.3 (Recommended device sizing).
Caution: Vessel damage such as dissection, perforation, or rupture may be caused by excessive oversizing of the stent graft in
relation to the diameter of the blood vessel. Oversizing of the stent graft to the vessel more than the recommended device
sizing as shown in Section 6.3 (Recommended Device Sizing), may be unsafe, especially in the presence of dissecting tissue
or intramural hematoma. Excessive or insufficient oversizing may also result in Type I endoleak. Consider vessel tortuosity
when selecting stent graft length. If preoperative case planning measurements are not certain, an inventory of system lengths
and diameters necessary to complete the procedure should be available to the physician. This approach allows for greater
intraoperative flexibility to achieve optimal procedural outcomes. Using the device outside the recommended anatomical sizing
may result in serious device-related adverse events. Physicians may consult with a Medtronic representative to determine
proper stent graft component dimensions based on the physician's assessment of the patient's anatomical measurements.
Instructions for Use English 9
Page 12

However, the final treatment decision is at the discretion of the physician and patient. The benefits and risks previously
described should be carefully considered for each patient before using the Valiant Navion thoracic stent graft system.
6.2.2. Recommended Skills and Training
The recommended skill/knowledge requirements for physicians using the Valiant Navion thoracic stent graft system are outlined
below:
Patient Selection
■
Knowledge of the natural history of thoracic aortic lesions, including but not limited to thoracic aortic aneurysms, thoracic
aortic dissections, and comorbidities associated with thoracic lesion repair
■
Knowledge of image interpretation, stent graft selection, and sizing
Physician Skills and Experience
All physicians must be trained in the use of the Valiant Navion thoracic stent graft system before using it.
Caution: The Valiant Navion thoracic stent graft system should only be used by physicians and teams trained in vascular
interventional techniques and in the use of this device.
The following list outlines the knowledge and skill requirements for physicians using the Valiant Navion thoracic stent graft
system:
■
Natural history and associated comorbidities of TAA, fusiform and saccular aneurysms or PAU, dissections, and BTAI
■
Radiographic, fluoroscopic, and angiographic image interpretation
■
Angioplasty
■
Appropriate use of anticoagulants (for example, heparin)
■
Appropriate use of radiographic contrast material
■
Embolization
■
Endovascular stent graft placement
■
Arterial cutdown, arteriotomy, and repair and percutaneous access and closure techniques
■
Nonselective and selective guidewire and catheter techniques
■
Snare techniques
■
Techniques to minimize radiation exposure
■
Device selection and sizing
Materials Recommended for Device Implantation
At the time of surgery, Medtronic recommends that the physicians have the following materials available:
■
All lengths and diameters of the devices necessary to complete the procedure, especially when preoperative case planning
measurements (treatment diameters/lengths) are not certain. This approach allows for greater intraoperative flexibility to
achieve optimal procedural outcomes.
■
Assorted angiographic catheters, angioplasty catheters, graduated pigtail catheters
■
Contrast media
■
Fluoroscope with digital angiography capabilities and the ability to record and recall imaging
■
Surgical suite in the event that emergency open conversion surgery is necessary
■
Heparin and heparinized saline solution
■
Transesophageal echocardiography (TEE)
■
Intravascular ultrasound catheter (IVUS)
■
Introducer sheaths for vascular access and to perform diagnostic imaging
■
Power injector
■
Radiopaque ruler
■
Reliant stent graft balloon catheter and other materials recommended by the Reliant Instructions for Use
■
Sterile lubricant
■
An assortment of stiff 0.035 in (0.89 mm) diameter guidewires, ≥ 260 cm in length
6.3. Recommended device sizing
Medtronic recommends that the Valiant Navion thoracic stent graft system be used according to the sizing configurations
provided in Table 2 through Table 5, and the sizing guidelines provided in Table 6 through Table 8. If preoperative case planning
measurements are not certain, an inventory of system lengths and diameters necessary to complete the procedure should be
available to the physician. This approach allows for greater intraoperative flexibility to achieve optimal procedural outcomes.
Using this device outside the recommended anatomical sizing may result in serious device-related adverse events or clinical
events.
10 Instructions for Use English
Page 13
The specific stent graft diameter used for treatment should be oversized relative to the nondiseased vessel, using the sizing
guidelines, to ensure appropriate radial fixation. Strict adherence to the sizing guidelines is expected when selecting the
appropriate device size. Table 6 through Table 8 describe the stent graft to vessel oversizing guidelines. Appropriate oversizing
has already been incorporated into the recommended sizes. Additional oversizing should not be incorporated. Sizing outside of
this range can result in endoleak, fracture, migration, infolding, or graft wear.
Table 2. FreeFlo Straight configurations
OD (Fr) Diameter (mm) Covered length (mm)
20 96
18
20
22
Table 3. CoveredSeal Straight configurations
OD (Fr) Diameter (mm) Covered length (mm)
18
20
22
Table 4. FreeFlo Tapered configurations
22
25
28 97, 174
31 97, 174, 229
34
37
40
46
20 94
22
25
28 90, 182
31 90, 182, 223
34
37
40
46
96, 185
59, 97, 174, 229
62, 103, 183, 22343
94, 180
52, 90, 182, 223
55, 95, 175, 21843
OD (Fr) Proximal × distal diameter (mm) Covered length (mm)
18 25×20 185
28×22
20
22
Table 5. CoveredSeal Tapered configurations
OD (Fr) Proximal × distal diameter (mm) Covered length (mm)
18 25×20 186
20
22
31×25
34×28
37×31
40×34
46×40
28×22
31×25
34×28
37×31
40×34
46×40
173
18543×37
207
20043×37
Instructions for Use English 11
Page 14
6.4. Device sizing recommendations
Table 6. Sizing guidelines for the treatment of aneurysms
Vessel diameter indication (mm) Graft diameter (mm)
16–17 20
18–19 22
20–22 25
23–25 28
26–28 31
28–31 34
30–33 37
33–36 40
36–39 43
39–42 46
Table 7. Sizing guidelines for treatment of dissections
Vessel diameter indication (mm) Graft diameter (mm)
19 20
20-22 22
23-25 25
26-28 28
29-30 31
31-33 34
34-36 37
37-39 40
39-42 43
42-45 46
Table 8. Sizing guidelines for treatment of BTAI
Vessel diameter indication (mm) Graft diameter (mm)
16-17 20
18-20 22
20-23 25
23-26 28
26-29 31
28-32 34
30-35 37
33-38 40
36-41 43
39-44 46
Caution: Proper sizing of the Valiant Navion thoracic stent graft is the responsibility of the physician. This stent graft sizing
incorporates the recommended device oversizing for anatomical dimension and was based on in vitro test data. Additional
oversizing should not be incorporated.
Caution: Oversizing of the stent graft to the vessel by more than 10% may be unsafe in the presence of dissecting tissue or
intramural hematoma.
When multiple stent grafts are needed to exclude the target lesion, and the component junction or overlapping connection is not
supported by the nondiseased vessel (that is, it is in the aneurysm sac), the diameter of the inside component should be
oversized by 6 mm relative to the outside component. In the case when a 20 mm stent graft is used as an outside component,
the diameter of the inside component should be oversized by 5 mm relative to the outside component. If it is supported by the
vessel, the stent graft should be oversized relative to the supporting native vessel, as described in Table 6. In order to provide
the appropriate oversizing at a component junction, tapered configurations may need to be used.
The order of deployment when using multiple stent graft configurations may vary, depending on the diameter of the aorta
proximal to and distal to the lesion. Table 9 should be followed to determine the order of deployment when using multiple stent
graft configurations to treat non-dissected lesions.
12 Instructions for Use English
Page 15

Caution: When treating acute dissections with multiple devices, deploy the proximal device first. Inadvertent pressurization of
the false lumen may result in retrograde dissection.
Note: If the vessel diameter and condition require variable proximal and distal diameter configurations, the smallest diameter
stent graft should be placed first, either at the proximal or distal end of the lesion.
Caution: The proximal end of a FreeFlo stent graft should never be placed inside the covered section of another stent graft.
Table 9. Order of deployment when using multiple stent graft component sections to treat non-dissected lesions
First section
implanted (primary section)
Second section
implanted
(additional section)
Proximal aortic diameter = distal
aortic diameter
Proximal main section implanted at
proximal end of lesion
Distal main section implanted with
correct junction oversizing. Due to
taper configuration of distal main
section, this fits a straight aorta cor-
Proximal aortic diameter > distal
aortic diameter
Distal main section (or other configuration if more appropriate) implanted at
distal end of lesion
Proximal main section implanted with
correct oversizing at junction with Distal
Main Section. Proximal telescoping of
devices fits this shape of aorta
Proximal aortic diameter <
distal aortic diameter
Proximal main section
implanted at proximal end of
lesion
Distal main section implanted with correct oversizing at
junction
rectly
Third section
implanted
(additional sec-
[Optional] additional sections implanted with correct oversizing at junction
[Optional] additional sections implanted
with correct oversizing at junction
[Optional] additional sections
implanted with correct oversizing at junction
tion)
7. Patient counseling information
The physician should review the following information when counseling the patient about this endovascular device and
procedure:
■
Details contained in the patient information booklet regarding possible complication after implantation of the device, such as
cardiac or neurological complications.
■
Differences between endovascular repair and open surgical repair
■
Risks related to open surgical repair
■
Risks related to endovascular repair
■
Pros and cons of open surgical repair and endovascular repair
■
Potential advantages of endovascular repair using a minimally invasive approach
■
Possibility that subsequent endovascular or open surgical repair may be required
■
Regular follow-up, including stent graft imaging, should be performed. For more information, refer to Section 12 (Follow-up
imaging recommendations).
■
Symptoms of aortic vessel rupture
■
Medtronic recommends that the physician disclose to the patient, in written form, all risks associated with treatment using
the Valiant Navion thoracic stent graft system. The list of potential risks occurring during and after implantation of the device
are provided in Adverse Events (Section 5). Medtronic also recommends that detailed patient specific risks also be
discussed. Additional counseling information can be found in the Patient Information Booklet.
8. How supplied
8.1. Sterility
Each Valiant Navion thoracic stent graft is individually contained within a delivery system. It is sterilized using electron beam
sterilization and is supplied sterile for single use only.
■
Do not reuse or attempt to resterilize.
■
Reuse of single-use devices may compromise the structural integrity of the device, essential material and design
characteristics, and/or lead to device failure.
■
If the device is damaged or the integrity of the sterilization barrier has been compromised, do not use the product. Contact
your Medtronic representative for return information.
8.2. Contents
■
One Valiant Navion thoracic stent graft system
■
One Instructions for Use or Web Leaflet
8.3. Storage
Store the system at room temperature in a dark, dry place.
Instructions for Use English 13
Page 16

9. Summary of Clinical Studies
The Valiant Navion thoracic stent graft system is Medtronic's next generation thoracic stent graft system, based on the
previously approved Valiant™ thoracic stent graft with the Captivia™ delivery system (also referred to as the Valiant Captivia
thoracic stent graft system). The changes were intended to increase the range of stent graft sizes offered (shorter and longer
lengths, smaller diameter, and increased stent graft taper offered), reduce the delivery system profile (18 Fr, 20 Fr, and 22 Fr
instead of 22 Fr, 24 Fr, and 25 Fr), allow for the use of the CoveredSeal configuration as either the proximal or the distal device
(previous Closed Web configuration was limited to use as the distal device), and allow for controlled delivery of all
configurations.
Because the Valiant Navion thoracic stent graft system is expected to perform similarly to Valiant Captivia thoracic stent graft
system, the clinical study (Valiant Evo IDE study) was designed to confirm that the device design modifications did not
negatively impact clinical performance. The study was limited to the use of the device for the treatment of descending thoracic
aortic aneurysms (DTAA) and penetrating aortic ulcers (PAU). The results from this study, with consideration of the clinical data
from the evaluation of the Valiant Captivia thoracic stent graft system, in combination with the nonclinical testing, supports the
broad indication of all lesions of the descending thoracic aorta (DTA). The aortic anatomy associated with descending thoracic
aortic aneurysms is technically most challenging, making them suitable patients to evaluate acute outcomes per the objectives
of the Valiant Evo IDE study. Patients with aneurysm have been shown to be a worst-case population for endovascular repair of
the thoracic aorta through prior clinical experience from the Valiant Captivia thoracic stent graft system. The aneurysm disease
state is worst case when compared to transection and dissection disease states because the aneurysm poses additional
challenge for the delivery system in traversing the aneurysm to reach the deployment target and deploying accurately within the
short landing zone proximal to the aneurysm.
Note: Information regarding the clinical evaluation of the Valiant Captivia thoracic stent graft system to treat traumatic
transections, acute complicated dissections and DTAA can be found in the IFU for this device; Medtronic's VALOR II study
(Section 6.3 of the Valiant Captivia thoracic stent graft system IFU), Medtronic Dissection Trial (Section 6.1 of the Valiant
Captivia thoracic stent graft system IFU) and RESCUE study (Section 6.2 of the Valiant Captivia thoracic stent graft system
IFU).
Note: The Valiant Navion thoracic stent graft system was called the "Valiant Evo thoracic stent graft system" during the clinical
study. Therefore, the device is referred to as the “Valiant Evo” in this clinical study summary.
A total of 100 subjects were enrolled as part of the Valiant Evo IDE study. Data on the first 87 of these subjects are presented in
this clinical study summary [52 US, 35 OUS (6 Canada, 1 Denmark, 11 Italy, 8 France, 4 Netherlands, 5 UK)]. These
87 subjects were recruited from 31 medical centers worldwide, with 18 of the clinical sites coming from the United States and
13 from Outside the United States (OUS) (2 Canada, 1 Denmark, 4 Italy, 3 France, 2 Netherlands, and 1 UK). This clinical
study is a prospective, multi-center, single arm study.
The primary objective of the Valiant Evo IDE study was to demonstrate the safety and effectiveness of the Valiant Evo thoracic
stent graft system in subjects with a descending thoracic aortic aneurysm who were candidates for endovascular repair. The
primary endpoint was defined as the proportion of subjects with access failures, deployment failures, and/or Major Device
Effects (MDE) within 30 days post index procedure. For this study, access failure is defined as the inability to insert the device
due to mechanical failure or anatomic exclusions of the femoral or iliac arteries. Deployment failure is defined as failure of
deployment due to subject anatomy or mechanical failure. MDEs are defined as the occurrence of any of the following: devicerelated secondary procedures, device-related mortality, conversion to open surgery, and thoracic aortic aneurysm rupture.
Notably, the definition of deployment failure used for this study does not include deployment accuracy, deployment without the
need for the use of bailout techniques, or the need for placing unintended additional devices.
This primary endpoint was selected based on Medtronic's review of the design characteristics/components that were leveraged
from the Valiant Captivia thoracic stent graft system to the Valiant Evo thoracic stent graft system. This review suggested that
the design changes should only potentially impact device delivery and acute clinical outcomes, not long-term device
performance. Access and deployment failures with the components of MDE comprise a clinically relevant measure of the
effects of the design modifications because this composite endpoint addresses the potential failures relevant to the
modifications. In addition, as MDEs are influenced little by aortic pathology, these measures are representative of device
performance and are relatively independent of lesion type. Finally, results of the VALOR II (IDE study for the Valiant Captivia
thoracic stent graft system in aneurysm conditions) clinical data showed that predominance of the MDEs occur within 30-days.
As a result, the Valiant Evo endpoint includes access and deployment failures and MDEs at 30 days that were defined to
include the potential clinical impacts that are related to the acute safety and effectiveness of stent graft placement.
Based on the Medtronic-sponsored VALOR II study results, the Valiant Evo IDE study was expected to meet the predetermined performance goal of 16% of MDE combined with access and/or deployment failures at 30 days. The sample size of
87 evaluable subjects provided 85% statistical power for the study hypothesis. The type I error was controlled with a one-sided
0.025. A total of 100 subjects, consecutively enrolled across 37 sites in all geographies, ensured that 87 evaluable subjects
(52 US, 35 OUS) were available at the 30-day primary endpoint for analysis.
14 Instructions for Use English
Page 17

Secondary objectives of the study included descriptive analyses of secondary endpoints, acute procedural observations and
clinical utility measures. Secondary endpoints included adverse events, MDEs, secondary procedures, all-cause mortality
(ACM), aneurysm-related mortality (ARM), loss of stent graft patency, endoleaks, stent graft migration and aneurysm
expansion.
Data were collected at baseline, during the implant procedure, and at discharge. Subjects were evaluated at 30 days and
12 months. For subjects enrolled in the US, an evaluation at 6 months was also required per the clinical investigation plan.
Safety and effectiveness data on the Valiant Evo thoracic stent graft system will be collected by following all enrolled subjects to
2 years and those who signed an updated Informed Consent Form for a total of 5 years.
A Clinical Events Committee (CEC) met to adjudicate MDEs, unanticipated adverse device effects (UADEs), unanticipated
serious adverse device effects (USADEs), deaths, and all aneurysm ruptures for the global cohort. A Data Monitoring
Committee (DMC) met to evaluate safety data during the course of the clinical study. A central imaging core lab was used to
provide independent evaluation of imaging findings.
9.1. Core Lab Imaging Accountability
A total of 100 subjects were enrolled in this study. The analysis for the study was based on the first 87 subjects evaluable for
the 30-day endpoint. The data cutoff for this analysis was 11/DEC/2017.
These 87 subjects were enrolled in this study between March 2016 and October 2017. All subjects underwent endovascular
repair with the Valiant Evo thoracic stent graft. Table 10 summarizes the subject accountability and compliance by study interval
in the global cohort for these 87 subjects.
Table 10. Subject and Core Lab Imaging Accountability – All Subjects
Follow-up
(Interval)
Subject Follow-up
Eligi-
ble
Clini-
low-
cal
Fol-
up
Imag-
ing
Fol-
low-
up
Subjects
with Imaging
(Core Lab)
CT
\MR
Other
Imag-
ing
Imag-
ing
Subjects with Adequate
Imaging to Assess the
Parameter (Core Lab)
Loss
of
PatencyEndo-
a
leak
Migra
tion
Aneur
ysm
Expa
nsion
Subject Events Occurring before Next
Visit
No
Impla
nt
Con-
ver-
sion
to
Surgery Death
With-
drawa
l/Earl
y Termina-
tion
Lost
to
Fol-
low-
up
Not
Due
for
Next
Visit
Enrollment 87 0
Events
after
Implant but
0 1 0 0 0
before 1Month Visit
1-Month
Visit
(Day 1-90)
86
85
(99%)84(98%)84(98%)0(0.0%)81(94%)81(94%)
Events
after 1Month but
0 4 2 0 29
before 6Month Visit
6-Month
Visit (Day
91-304)
b
51
36
(71%)36(71%)36(71%)0(0.0%)31(61%)31(61%)35(69%)36(71%)
Events
after 6Month but
0 1 0 0 26
before 12Month Visit
12-Month
Visit (Day
24
305-548)
a
Other imaging includes chest X-ray, angiogram, ultrasound, and other imaging of the stent graft region.
b
6-month data is not required per OUS protocol; therefore, the follow-up rate is lower when US and OUS results are combined at this timepoint.
22
(92%)21(88%)21(88%)0(0.0%)21(88%)21(88%)21(88%)21(88%)
Note: In Table 10, data analysis sample size varies for each of the timepoints above and in the following tables. This variability
is due to subject availability for follow-up, as well as, quantity and quality of images available from specific timepoints for
Instructions for Use English 15
Page 18

evaluation. For example, the number of quality images available for evaluation of endoleak at 1 months is different than the
number and quality of images available at 6 months due to variation in the number of images performed, the number of images
provided from the clinical site to the Core Lab, and/or the number of images with acceptable evaluation quality.
9.2. Subject Demographics
Table 11 displays the subject demographic data of the global cohort. The median age of the global cohort was 72.0 years
(ranging from 51 to 89 years) and was similar between the US and OUS cohorts and between genders. Of the 87 subjects
enrolled in the global cohort, a total of 37.9% (33/87) were female; the gender distribution in the US cohort was 50.0% female
(26/52), with the OUS cohort having a lower proportion of females (20.0%, 7/35 subjects). Racial data was only collected
among the US cohort, with 78.8% (41/52) of the US subjects reported as white.
Table 11. Subject Demographics
Subject Characteristics Statistics/Category Global Cohort
Gender
Female 37.9% (33/87)
Male 62.1% (54/87)
Age (years)
Total Population n 87
Mean ± SD 70.8 ± 8.7
Median 72.0
Min, max 51, 89
Female n 33
Mean ± SD 71.0 ± 8.7
Median 73.0
Min, max 51, 83
Male n 54
Mean ± SD 70.7 ± 8.7
Median 72.0
Min, max 54, 89
a
Race
White 78.8% (41/52)
Non-white 21.2% (11/52)
a
Race data were not collected in OUS per regulation.
9.3. Medical History
Baseline medical history characteristics from the global cohort are summarized in Table 12. The most prevalent medical history
diagnoses at baseline included:
■
Hypertension in 89.7% (78/87) of subjects
■
Hyperlipidemia in 73.3% (63/86) of subjects
■
Tobacco use in the last 10 years in 51.2% (44/86) of subjects
Overall, the US cohort presented with higher rates of comorbidities at baseline, compared to the OUS cohort, indicating the US
subjects were less healthy than OUS subjects. This trend is confirmed in Table 13, which discusses the classifications of the
majority of US subjects as Class III and Class IV based on the American Society of Anesthesiologists (ASA) Physical Status
Classification System, compared to OUS subjects as Class II or Class III.
Table 12. Medical History
Body System / Condition US (N=52) OUS (N=35) Global Cohort
Alcoholism 9.6% (5/52) 2.9% (1/35) 6.9% (6/87)
Cancer 32.7% (17/52) 11.4% (4/35) 24.1% (21/87)
Carotid Artery Disease 28.8% (15/52) 6.3% (2/32) 20.2% (17/84)
Diabetes 25.0% (13/52) 14.3% (5/35) 20.7% (18/87)
Hyperlipidemia 78.8% (41/52) 64.7% (22/34) 73.3% (63/86)
Hypertension 94.2% (49/52) 82.9% (29/35) 89.7% (78/87)
Tobacco Use in the Last 10 Years 54.9% (28/51) 45.7% (16/35) 51.2% (44/86)
Cardiac Disease
Angina 9.6% (5/52) 11.4% (4/35) 10.3% (9/87)
Arrhythmia 36.5% (19/52) 14.3% (5/35) 27.6% (24/87)
16 Instructions for Use English
Page 19

Body System / Condition US (N=52) OUS (N=35) Global Cohort
Congestive Heart Failure 19.2% (10/52) 2.9% (1/35) 12.6% (11/87)
Coronary Artery Disease 42.3% (22/52) 25.7% (9/35) 35.6% (31/87)
Coronary Artery Bypass
Graft (CABG)
Percutaneous Coronary
Intervention
Myocardial Infraction (MI) 13.5% (7/52) 20.0% (7/35) 16.1% (14/87)
Valvular Heart Disease (VHD) 11.5% (6/52) 8.6% (3/35) 10.3% (9/87)
Cardiac Valve Replacement
or Repair
Pulmonary
Chronic Obstructive Pulmonary
Disease (COPD)
Renal
Renal Insufficiency 26.9% (14/52) 14.3% (5/35) 21.8% (19/87)
Renal Failure 11.5% (6/52) 2.9% (1/35) 8.0% (7/87)
Cerebrovascular/Neurological
Stroke/Cerebral Vascular Accident (CVA)
Transient Ischemic Attack (TIA) 11.5% (6/52) 2.9% (1/35) 8.0% (7/87)
Paraparesis 0.0% (0/52) 0.0% (0/35) 0.0% (0/87)
Paraplegia 0.0% (0/52) 0.0% (0/35) 0.0% (0/87)
Vascular
Abdominal Aortic Aneurysm 21.2% (11/52) 31.4% (11/35) 25.3% (22/87)
Ascending Thoracic Aneurysm 17.3% (9/52) 2.9% (1/35) 11.5% (10/87)
Descending Thoracic Aneurysm 100.0% (52/52) 100.0% (35/35) 100.0% (87/87)
Family History of Aneurysm 12.5% (6/48) 12.5% (4/32) 12.5% (10/80)
Peripheral Vascular Disease 21.2% (11/52) 8.8% (3/34) 16.3% (14/86)
Connective Tissue Disease
Marfan Syndrome 0.0% (0/52) 0.0% (0/35) 0.0% (0/87)
Ehlers Danlos 0.0% (0/52) 0.0% (0/35) 0.0% (0/87)
Other Systemic Conditions
Bleeding Disorder 1.9% (1/52) 0.0% (0/35) 1.1% (1/87)
GI conditions 46.2% (24/52) 20.0% (7/35) 35.6% (31/87)
Liver Disease 7.7% (4/52) 0.0% (0/35) 4.6% (4/87)
Other Relevant Systemic Condi-
tion
Note: In Table 12, the subjects checked "unknown" or left blank for a certain question are not included in the denominator.
Other relevant systemic conditions in 55.2% (48/87) of subjects, which includes, but is not limited to: chronic kidney disease,
vocal cord paralysis, sleep apnea, gall stones, anxiety, cataracts, gout, and varicose veins.
31.8% (7/22) 22.2% (2/9) 29.0% (9/31)
54.5% (12/22) 77.8% (7/9) 61.3% (19/31)
16.7% (1/6) 33.3% (1/3) 22.2% (2/9)
40.4% (21/52) 20.6% (7/34) 32.6% (28/86)
9.6% (5/52) 8.6% (3/35) 9.2% (8/87)
65.4% (34/52) 40.0% (14/35) 55.2% (48/87)
9.4. ASA Classification
Based on their medical history and physical condition, all subjects were classified into five distinct categories according to the
ASA Physical Status Classification System. The purpose of this grading system was to assess the physical status of the subject
prior to the implant procedure.
The ASA Physical Status Classification on the 87 subjects enrolled in the global cohort is described in Table 13. The majority
(44.8%, 39/87) of all subjects were Class III; the majority (90.4%, 47/52) of US subjects were Class III or Class IV; the majority
(77.1%, 27/35) of OUS subjects were Class II or Class III.
Table 13. The American Society of Anesthesiologists (ASA) Physical Status Classification
ASA Physical Status Classification US OUS Global Cohort
I (Normal healthy subject) 0.0% (0/52) 17.1% (6/35) 6.9% (6/87)
II (Subject with mild systemic disease) 9.6% (5/52) 40.0% (14/35) 21.8% (19/87)
III (Subject with severe systemic disease) 50.0% (26/52) 37.1% (13/35) 44.8% (39/87)
Instructions for Use English 17
Page 20

ASA Physical Status Classification US OUS Global Cohort
IV (Subject with severe systemic disease that is a
40.4% (21/52) 5.7% (2/35) 26.4% (23/87)
constant threat to life)
V (Moribund subject who is not expected to sur-
0.0% (0/52) 0.0% (0/35) 0.0% (0/87)
vive without the operation)
Not Assessed 0.0% (0/52) 0.0% (0/35) 0.0% (0/87)
9.5. Baseline Aneurysm Characteristics
9.5.1. Baseline Vessel Measurements
Table 14, Table 15, and Table 16 display the baseline vessel diameter and length measurements obtained by the core lab.
The mean maximum aneurysm diameter of the global cohort reported by the core lab was 55.7 ± 13.1 mm, and the majority of
subjects (40.2%; 35/87) had a maximum aneurysm diameter between 50 to 60 mm. The US and OUS cohorts had similar
reported access vessel and aortic diameter measures.
Table 14. Pre-implant Vessel Diameters (mm) (Core Lab)
Vessel Diameters (mm) Statistics Global Cohort
D1: Aorta Diameter (2 cm proximal to aneurysm) n
a
87
Mean ± SD 29.3 ± 3.6
Median 29.2
Min, Max 20, 37
D2: Aorta Diameter (immediately proximal to the aneurysm)
a
n
87
Mean ± SD 31.6 ± 5.0
Median 31.5
Min, Max 20, 45
D3: Maximum Aneurysm Diameter
a
n
87
Mean ± SD 55.7 ± 13.1
Median 55.4
Min, Max 26, 98
<30 1.1% (1/87)
30 – <40 12.6% (11/87)
40 – <50 13.8% (12/87)
50 – <60 40.2% (35/87)
60 – <70 23.0% (20/87)
70 – <80 4.6% (4/87)
80 – <90 2.3% (2/87)
90 – <100 2.3% (2/87)
≥ 100 0.0% (0/87)
D4: Aorta Diameter (immediately distal to the aneurysm)
a
n
87
Mean ± SD 30.4 ± 5.4
Median 30.4
Min, Max 19, 42
D5: Aorta Diameter (2 cm distal to the aneurysm)
a
n
87
Mean ± SD 29.2 ± 4.7
Median 28.6
Min, Max 20, 40
D6: Minimum Left Common Iliac Diameter
a
n
86
Mean ± SD 9.7 ± 2.5
Median 9.7
Min, Max 5, 18
D7: Minimum Left External Iliac Diameter
a
n
85
Mean ± SD 7.7 ± 1.9
Median 7.4
Min, Max 4, 12
D8: Minimum Left Femoral Diameter
a
n
83
Mean ± SD 7.8 ± 1.7
18 Instructions for Use English
Page 21

Vessel Diameters (mm) Statistics Global Cohort
Median 7.7
Min, Max 5, 12
D9: Minimum Right Common Iliac Diameter
a
n
86
Mean ± SD 9.8 ± 2.5
Median 9.5
Min, Max 5, 18
D10: Minimum Right External Iliac Diameter
a
n
85
Mean ± SD 7.5 ± 1.8
Median 7.2
Min, Max 3, 12
D11: Minimum Right Femoral Diameter
a
n
83
Mean ± SD 7.7 ± 1.6
Median 7.5
Min, Max 5, 11
Aorta Diameter at Left Subclavian Artery
a
n
87
Mean ± SD 29.8 ± 4.2
Median 29.0
Min, Max 23, 43
Aorta Diameter 2 cm Distal to Left Common Carotid Artery
a
n
87
Mean ± SD 29.7 ± 4.1
Median 29.3
Min, Max 22, 42
Aorta Diameter 2.5 cm Distal to Left Common Carotid Artery
a
n
87
Mean ± SD 30.3 ± 4.8
Median 29.6
Min, Max 21, 42
Aorta Diameter 2.5 cm Proximal to Aneurysm
a
n
87
Mean ± SD 29.6 ± 3.5
Median 29.6
Min, Max 20, 38
Aorta Diameter 2 cm Proximal to Celiac Artery
a
n
87
Mean ± SD 28.9 ± 5.5
Median 27.9
Min, Max 19, 43
Maximum Infrarenal Aortic Diameter
a
n
87
Mean ± SD 26.4 ± 7.3
Median 25.8
Min, Max 15, 48
a
n =number of enrolled subjects with readable scans.
Table 15 summarizes the core lab reported pre-implant vessel lengths. Core lab reported aneurysm lengths were longer among
the US cohort (122.6 ± 70.3 mm) as compared to the OUS cohort (99.1 ± 72.1 mm). Distal neck lengths in OUS subjects
(121.5 ± 71.5 mm) were longer than those in US subjects (83.8 ± 63.4 mm). US subjects had slightly longer proximal neck
lengths (65.6 ± 51.2 mm) compared to OUS subjects (48.8 ± 28.4 mm).
Table 15. Pre-implant Vessel Length (Core Lab)
Vessel Lengths (mm) Statistics Global Cohort
Proximal Neck Length n
a
87
Mean ± SD 58.9 ± 44.1
Median 40.8
Min, Max 20, 210
L1: Length between Distal Edge of LCCA and Start of Aneur-
a
n
87
ysm (centerline)
Mean ± SD 75.1 ± 50.8
Median 54.7
Instructions for Use English 19
Page 22

Vessel Lengths (mm) Statistics Global Cohort
Min, Max 20, 216
L2: Length between Distal Edge of LSA and Start of Aneurysm
a
n
87
(centerline)
Mean ± SD 56.3 ± 50.2
Median 38.1
Min, Max -15, 197
L3: Aneurysm Length (centerline, D2 to D4)
a
n
87
Mean ± SD 113.1 ± 71.5
Median 109.0
Min, Max 15, 262
L4: Distal Neck Length (non-aneurysmal neck to celiac axis)
a
n
87
Mean ± SD 99.0 ± 68.9
Median 79.3
Min, Max 20, 296
a
n = number of included subjects with readable scans
Table 16 summarizes the core lab reported pre-implant vessel assessment for access and implant. Notably, similar rates of
severe, moderate, and mild access artery tortuosity were reported between the US and OUS cohorts.
The US and OUS cohorts had similar rates of proximal neck and thoracic aorta tortuosity. Globally, a total of 84.9% (73/86) of
subjects were reported as having mild abdominal aorta tortuosity, with similar rates of abdominal aorta tortuosity reported in
both the US and OUS cohorts.
Table 16. Pre-implant Vessel Assessment for Access and Implant (Core Lab)
Vessel Assessment (mm) Statistics Global Cohort
Access Artery Tortuosity None 0.0% (0/86)
Mild 10.5% (9/86)
Moderate 18.6% (16/86)
Severe 70.9% (61/86)
Access Artery Calcification None 8.1% (7/86)
Mild 54.7% (47/86)
Moderate 33.7% (29/86)
Severe 3.5% (3/86)
Proximal Neck Tortuosity None 0.0% (0/87)
Mild 74.7% (65/87)
Moderate 9.2% (8/87)
Severe 16.1% (14/87)
Abdominal Aorta Tortuosity None 0.0% (0/86)
Mild 84.9% (73/86)
Moderate 9.3% (8/86)
Severe 5.8% (5/86)
Thoracic Aorta Tortuosity Low 14.3% (11/77)
High 85.7% (66/77)
Thrombus Presented in the Intended Landing Zone No 83.7% (72/86)
Yes 16.3% (14/86)
Insignificant 15.1% (13/86)
Significant 1.2% (1/86)
Circumferential 0.0% (0/86)
Calcium Presented in the Intended Landing Zone No 37.9% (33/87)
Yes 62.1% (54/87)
Insignificant 60.9% (53/87)
Significant 1.1% (1/87)
Circumferential 0.0% (0/87)
20 Instructions for Use English
Page 23

9.5.2. Primary TEVAR Indication
The Valiant Evo stent graft was used to treat fusiform aneurysms, saccular aneurysms and penetrating atherosclerotic ulcers in
the Valiant Evo IDE study. The most common pathology treated by the Valiant Evo device in the global cohort was fusiform
aneurysm (42.5%; 37/87), followed by saccular aneurysm (36.8%; 32/87), as displayed in Table 17 below.
The US cohort was most commonly treated for fusiform aneurysms (46.2%; 24/52), and the OUS cohort was treated equally for
fusiform (37.1%; 13/35) and saccular aneurysms (37.1%; 13/35). Approximately one-fifth of the overall cohort was treated for a
penetrating atherosclerotic ulcer (PAU).
Table 17. Primary Indication for Thoracic Endovascular Aortic Repair (TEVAR)
Primary Indication for TEVAR US OUS Global Cohort
Fusiform Aneurysm 46.2% (24/52) 37.1% (13/35) 42.5% (37/87)
Saccular Aneurysm 36.5% (19/52) 37.1% (13/35) 36.8% (32/87)
Penetrating Atherosclerotic Ulcer 17.3% (9/52) 25.7% (9/35) 20.7% (18/87)
9.6. Device Use at Index Procedure
9.6.1. Number of Devices Implanted at Index Procedure
The total number of devices implanted at the index procedure are presented in Table 18. Since multiple stent graft
configurations may be used per subject, the number of devices implanted exceeds the number of subjects enrolled. The
majority of subjects (56.3%; 49/87) had 1 device implanted, and the mean number of devices used was 1.5 per subject. In the
US cohort, the majority of subjects (88.5%; 46/52) had 1 or 2 devices implanted. No subjects in the OUS cohort had more than
2 devices implanted.
Table 18. Total Number of Devices Implanted at Index Procedure
Devices Implanted per Subject Global Cohort
a
n
87
Mean ± SD 1.5 ± 0.7
Median 1.0
Min, Max 1, 4
1 56.3% (49/87)
2 36.8% (32/87)
3 4.6% (4/87)
4 2.3% (2/87)
≥ 5 0.0% (0/87)
a
n = number of enrolled subjects who received the test device.
A listing of the frequency of implantation of each device diameter used in the Valiant Evo IDE study, are presented in Table 19
(FreeFlo devices) and Table 20 (Closed Web devices).
Note: The CoveredSeal configuration was called the "Closed Web" configuration during the clinical study.
Table 19. Number of Devices Implanted by Diameter (FreeFlo)
FreeFlo devices
Proximal Diameter Number of implanted devices
28 2
31 7
34 12
37 24
40 14
43 9
46 7
*Devices ending in CU were devices implanted in US and devices ending in CE were implanted in OUS
Table 20. Number of Devices Implanted by Diameter (Closed Web)
Closed Web devices
Proximal Diameter Number of implanted devices
22 1
28 5
31 5
Instructions for Use English 21
Page 24

Closed Web devices
Proximal Diameter Number of implanted devices
34 7
37 14
40 15
43 7
46 4
9.6.2. Device Configurations at Index Procedure
The distribution of devices implanted as proximal pieces is presented in Table 21. The majority (74.7%; 65/87) of all subjects
received a FreeFlo configuration as the proximal device, with 56.3% (49/87) of subjects receiving the FreeFlo Straight
configuration. Proximal device configurations usage was similar in the US and OUS.
Table 21. Device Implanted as Proximal Configuration at Index Procedure
Device Configuration Global Cohort
FreeFlo 74.7% (65/87)
FreeFlo Straight 56.3% (49/87)
FreeFlo Tapered 18.4% (16/87)
Closed Web 25.3% (22/87)
Closed Web Straight 21.8% (19/87)
Closed Web Tapered 3.4% (3/87)
Note: In Table 21, denominator includes all enrolled subjects who received the test device. A subject may receive multiple
device types.
Distal configurations implanted at the index procedure are displayed in Table 22. There were more distal devices implanted in
US subjects (26) compared to OUS subjects (12).
Table 22. Device Implanted as Distal Configuration at Index Procedure
Device Configuration Global Cohort
FreeFlo 21.1% (8/38)
FreeFlo Straight 21.1% (8/38)
FreeFlo Tapered 0.0% (0/38)
Closed Web 78.9% (30/38)
Closed Web Straight 60.5% (23/38)
Closed Web Tapered 18.4% (7/38)
Note: In Table 22, the denominator includes subjects implanted with two or more devices. Subjects who had only one device
implanted were reported as proximal device in a separate table.
9.6.3. Implant Zone of Proximal Component
The landing zones of the proximal component implanted in all subjects are presented in Table 23. Stratified by geography,
proximal placement of the FreeFlo devices was most common in Zone 3 in the US (59.5%; 22/37), while Zone 4 was most
common in OUS (35.7%; 10/28). Closed Web devices were most commonly placed in Zone 4 in both the US (46.7%; 7/15) and
OUS (57.1%; 4/7).
Table 23. Implant Zone of Proximal Component
Implantation Zone of Proximal Component Global Cohort
FreeFlo
Zone 1 0.0% (0/65)
Zone 2 30.8% (20/65)
Zone 3 47.7% (31/65)
Zone 4 21.5% (14/65)
Closed Web
Zone 1 0.0% (0/22)
Zone 2 9.1% (2/22)
Zone 3 40.9% (9/22)
Zone 4 50.0% (11/22)
22 Instructions for Use English
Page 25

9.7. Procedural Data
Table 24 summarizes the acute procedural observations that were available at the time of implant for the 87 subjects analyzed.
In the US cohort, the mean duration of the procedure was 87.2 ± 44.2 minutes, which was comparable to the mean duration in
the OUS cohort, 91.0 ± 65.5 minutes. In the US, 98.1% (51/52) of subjects underwent general anesthesia, while 85.7% (30/35)
of OUS subjects underwent general anesthesia. The median hospital stay for the US cohort was similar to that of the OUS
cohort, with 5.0 days and 4.0 days, respectively. In both the US and OUS, one subject had a prolonged hospital stay of over
30 days.
A few notable data points differed between the two cohorts. Access type varied between cohorts, with percutaneous access
being the preferred method in the US (71.2%; 37/52), whereas surgical cut down was the preferred method OUS (80.0%;
28/35). Mean radiation exposure was twice as high in the US (1222.8 ± 1655.9 mGy) compared to OUS (521.3 ± 538.9 mGy).
Additionally, more US subjects were admitted to the ICU after the index procedure (47/52) compared to the OUS cohort
(16/35).
Table 24. Acute Procedure Observations and Clinical Utility Measures
Acute Procedural Data Statistics/Category Global Cohort
Duration of procedure (min) n 87
Mean ± SD 88.7 ± 53.4
Median 72.0
Min, Max 23, 281
Anesthesia Type % (m/n) General 93.1% (81/87)
Local 4.6% (4/87)
Epidural 0.0% (0/87)
Spinal 2.3% (2/87)
Access Type % (m/n) Surgical cut down 49.4% (43/87)
Percutaneous 50.6% (44/87)
Estimated Blood Loss (cc) n 85
Mean ± SD 94.0 ± 147.1
Median 50.0
Min, Max 0, 900
<750 cc 98.8% (84/85)
≥750 cc 1.2% (1/85)
Subjects Requiring Blood Transfusion % (m/n) 2.3% (2/87)
Volume of Blood Transfused (cc) n
a
2
Mean ± SD 600.0 ± 0.0
Median 600.0
Min, Max 600, 600
Volume of Contrast (mL) n 87
Mean ± SD 96.2 ± 52.8
Median 80.0
Min, Max 20, 300
Total Fluoroscopic Time (min) n 87
Mean ± SD 12.2 ± 8.8
Median 10.0
Min, Max 1, 53
Radiation Exposure (mGy) n 68
Mean ± SD 1016.5 ± 1452.5
Median 550.0
Min, Max 31, 8502
Time in ICU after Index Procedure (hours) n
b
63
Mean ± SD 67.4 ± 79.9
Median 46.0
Min, Max 14, 584
Days to Hospital Discharge n 86
Mean ± SD 7.1 ± 6.7
Instructions for Use English 23
Page 26

Acute Procedural Data Statistics/Category Global Cohort
Median 5.0
Min, Max 1, 35
a
Number of subjects who required blood transfusion.
b
Number of subjects who had an ICU stay after index procedure.
9.7.1. Adjunctive Procedures
Table 25 shows adjunctive procedures performed preoperatively and intraoperatively. The distribution of subjects with
complete, partial or no coverage of the left subclavian artery (LSA) is summarized in Table 26. A total of 3 subjects in the global
cohort had LSA coverage without a revascularization procedure, one with complete LSA coverage, and two with partial LSA
coverage.
In the US cohort, the most common intraoperative adjunctive procedure was CSF drainage (23.1%; 12/52). The most frequent
intraoperative adjunctive procedure in OUS subjects was usage of a balloon catheter (42.9%; 15/35).
Table 25. Adjunctive Procedures
Global Cohort
Preoperative Adjunctive Procedures
Left Subclavian Transposition 4.6% (4/87)
Left Carotid to Left Subclavian Bypass 12.6% (11/87)
Left Subclavian Embolization/Occlusion 4.6% (4/87)
Iliac Stenting 0.0% (0/87)
Other Adjunctive Procedures 6.9% (6/87)
Intraoperative Adjunctive Procedures
Left Subclavian Transposition 3.4% (3/87)
Left Carotid to Left Subclavian Bypass 6.9% (6/87)
Left Subclavian Embolization/Occlusion 11.5% (10/87)
Embolization of Aneurysm Sac 0.0% (0/87)
Uncovered Aortic Stent 0.0% (0/87)
Iliac Stenting 4.6% (4/87)
Rapid Cardiac Pacing during Deployment 9.2% (8/87)
Balloon Catheter 29.9% (26/87)
CSF Drainage 17.2% (15/87)
Other Adjunctive Procedures 4.6% (4/87)
Table 26 shows the percentage of subjects that had complete coverage, partial coverage, or no coverage of the left subclavian
artery (LSA).
When coverage of the LSA by the Valiant Evo device occurred, complete coverage of the LSA was the most common type of
coverage, reported in 21.8% (19/87) of the global cohort. Partial coverage of the LSA by the Valiant Evo device was reported in
3 subjects (3.4%; 3/87) in the global cohort. The US and OUS cohorts had similar rates of complete LSA coverage, while the
US cohort had the only cases of partial LSA coverage and revascularization.
Table 26. LSA Coverage
LSA Coverage Global Cohort
Complete 21.8% (19/87)
Subjects with revascularization procedure 20.7% (18/87)
Subjects without revascularization procedure 1.1% (1/87)
Partial 3.4% (3/87)
Subjects with revascularization procedure 1.1% (1/87)
Subjects without revascularization procedure 2.3% (2/87)
None 74.7% (65/87)
9.8. Global Study Endpoints
9.8.1. Primary Safety and Effectiveness Endpoint Evaluation
The primary endpoint for the global cohort is a composite endpoint of safety and effectiveness. It is defined as the proportion of
subjects with access failures, deployment failures, and/or Major Device Effects (MDEs) within 30 days post index procedure. As
shown in Table 27, the primary composite endpoint was met and was statistically significant, with a p-value of < 0.0001. A total
of 2.3% (2/87) subjects experienced the primary composite endpoint event within 30 days, with a 1-sided 97.5% upper
24 Instructions for Use English
Page 27

confidence limit of 8.06%, lower than the performance goal of 16% (p-value <.0001). It signifies that this study has met the prespecified performance goal.
Table 27. Primary Endpoint
1-sided 97.5%
Primary Endpoint Valiant Evo Upper Confidence
Performance Goal p-value
a
Limit
Access Failures;
2.3% (2/87) 8.06% 16% <.0001
Deployment Failures;
and/or MDEs within
30 Days Post Index
Procedure
a
p-value was based on a binomial distribution at the one-sided 0.025 statistical significance level.
Table 28 provides a breakdown of the primary composite endpoint analysis. MDEs consist of device-related secondary
procedure, device related mortality, conversion to open surgery, or thoracic aneurysm rupture. No subjects were reported as
having vessel access or deployment failures during the index procedure. A total of 2 (both OUS) subjects were reported having
a total of 4 MDEs (each subject had 2 MDEs) within 30 days of the index procedure. One subject had a device-related
secondary procedure and device-related mortality, both on day 1. A secondary procedure (open surgery) was performed in an
attempt to treat a retrograde type A dissection. The secondary procedure (adjudicated as device-related) was not successful,
and the subject died on day 1, with the mortality adjudicated as device-related. Another subject had a thoracic aortic aneurysm
rupture and device-related secondary procedure (additional stent graft endovascular procedure), both on day 28. The
secondary procedure (adjudicated as device-related) was performed to treat an aortic arch rupture caused by septicemia on
day 5 following infection in a peripheral venous catheter. This subject died on day 35; the death occurred outside of the 30-day
window, thus is not included in the primary endpoint. The poolability on the primary endpoint between US and OUS data were
assessed using Fisher's exact test. A p-value of 0.159 suggested no statistically significant heterogeneity between US and
OUS was observed in the primary endpoint.
Table 28. Primary Endpoint (Breakdown)
Breakdown of Primary Endpoint US OUS Global Cohort p-value
Overall Event Rates within 30 Days
b
0.0% (0/52) 5.7% (2/35) 2.3% (2/87) 0.159
a
Vessel Access Failure 0.0% (0/52) 0.0% (0/35) 0.0% (0/87)
Deployment Failure 0.0% (0/52) 0.0% (0/35) 0.0% (0/87)
Major Device Effects (MDE) 0.0% (0/52) 5.7% (2/35) 2.3% (2/87)
Device-related Secondary Proce-
c
dures
Device-related Mortality
c
0.0% (0/52) 5.7% (2/35) 2.3% (2/87)
0.0% (0/52) 2.9% (1/35) 1.1% (1/87)
Conversion to Open Surgery 0.0% (0/52) 0.0% (0/35) 0.0% (0/87)
Thoracic Aortic Aneurysm Rupture 0.0% (0/52) 2.9% (1/35) 1.1% (1/87)
a
Fisher's exact test for US and OUS data poolability.
b
Overall event rates are defined as the event rate of access and/or deployment failures; and/or MDEs within 30 days post index procedure. A subject may experience multiple events; hence, number of subjects
counted in the overall event rate or at upper level may not be the sum of those in each event at lower level.
c
Relationship to device was adjudicated by the Clinical Event Committee (CEC).
9.8.2. Secondary Endpoint Evaluation
Device Deficiencies
Site-Reported Device Deficiencies
A total of 9.2% (8/87) of subjects were reported having at least one device deficiency from 0-30 days, all occurring at the time
of implant, as shown in Table 29. The core lab does not review angiographic imaging from the procedure, and thus did not
report any imaging observations and/or related device deficiencies related to procedure. No device deficiencies were reported
in any subject beyond 30 days by the investigational sites. Refer to Section 10.8 and Section 10.9 for notes, cautions, and
instructions related to tip capture release and deploying the device.
Failure to Release Tip Capture
A total of 2 (2.3%) subjects had reported device deficiencies related to a failure of the tip capture release. Both failures of the tip
capture release were reported with the FreeFlo tapered configuration. In both cases, the physician employed the bailout
technique and disassembled the rear tip capture mechanism. The tip capture was released successfully, and the delivery
system was removed without any further complications. No adverse events were reported due to these device deficiencies. All
implanting investigators were required to complete updated device training in order to understand the correct troubleshooting
techniques needed to overcome tip capture release failure. Maneuvers include relieving the forward pressure in the delivery
system by gently moving the guidewire and delivery system off the aortic wall.
Instructions for Use English 25
Page 28

Deployment Difficulty - Distal Device Movement
A total of 4 (4.6%) subjects had deployment difficulty, distal device movement, reported. Of the 4 deployment difficulties,
1 subject experienced distal device movement with 2 devices (FreeFlo straight configuration). Of the remaining 3 subjects,
1 distal device movement was reported with a FreeFlo straight configuration while the other two were reported with a FreeFlo
tapered configuration. These subjects experienced distal device movement upon the deployment of the stent graft from the
delivery system. Additional proximal devices were added in 2 subjects to ensure adequate proximal seal. No adverse events
were reported related to these device deficiencies. All implanting investigators were required to complete updated device
training in order to minimize the occurrence of distal device movement during device implant. Maneuvers to reduce the
occurrence of distal device movement during deployment include rapid right ventricular pacing, controlled hypotension, and
maintaining apposition of the delivery system and guidewire to the greater curve of the aorta.
Difficulty to Remove Delivery System
A total of 2 (2.3%) subjects had difficulty to remove the delivery system reported. One subject reported the difficulty to remove
the delivery system with a FreeFlo straight configuration and the second subject with a FreeFlo tapered configuration. Both
subjects had the tip capture fitting caught in a bare stent after the stent graft deployment and tip release. After manipulation of
the delivery systems, the physicians were able to remove the device. One subject had no adverse events reported as
associated with this device deficiency. One subject, who was considered a failure of the primary endpoint, had an adverse
event (retrograde type A dissection) reported as related to this device deficiency, which resulted in the subject's death on day 1
(as reported in Table 37). A secondary procedure (open surgical repair) was performed to treat the retrograde type A
dissection. The secondary procedure (adjudicated as device-related) was not successful, and the subject died on day 1, with
the mortality adjudicated as device-related. All implanting investigators were required to complete updated device training in
order to understand the correct troubleshooting techniques needed to overcome difficulty removing the delivery system.
Maneuvers include relieving the forward pressure in the delivery system before attempting to actuate the tip capture (refer
to Section 10.8 for more information).
Other Type of Stent Graft Malfunction
There was 1 (1.1%) reported case of an “other type of malfunction of the stent graft” in a subject. This was reported in a
FreeFlo straight configuration. The physician reported that the Valiant Evo proximal device migrated 2 cm from the deployment
landing zone during deployment of the distal stent graft extension during the index procedure. The distal stent graft extension
was sized incorrectly for placement in an unsupported region of the aorta. The proximal seal zone was ballooned to prevent
further distal movement, and no additional proximal extension was needed. The final angiogram showed no endoleaks, and no
adverse events related to this event were reported.
Table 29. Device Deficiencies (Site-Reported)
Device Deficiencies 0-30 Days 31-183 Days 184-365 Days
Any Device Deficiencies
Any other failure/malfunction
a
9.2% (8/87) 0.0% (0/36) 0.0% (0/21)
1.1% (1/87) 0.0% (0/36) 0.0% (0/21)
of Stent Graft, specify
Failure to release tip capture 2.3% (2/87) 0.0% (0/36) 0.0% (0/21)
Deployment Difficulty 4.6% (4/87) 0.0% (0/36) 0.0% (0/21)
Difficulty to remove delivery
2.3% (2/87) 0.0% (0/36) 0.0% (0/21)
system
a
Number of subjects who had one or more device deficiencies reported. A subject may have device deficiencies in more than one category; hence, number of subjects with any device deficiencies may not be
the sum of those in each category. Each subject was only counted once in each category.
Note: In Table 29, denominator is number of subjects have reached the time period as indicated.
Sponsor-Assessed Device Deficiencies
There were 2 additional instances of distal device movement observed during the deployment process. The Sponsor assessed
these distal device movements as device deficiencies, neither of which were assessed to have serious adverse device effect
(SADE) potential. Neither subject was reported as having a clinical outcome related to these implant procedural observations.
Core Lab Reported Device Deficiencies
Table 30 shows the core lab reported device deficiencies. The core lab reported device deficiencies were observed in a Closed
Web straight configuration. Misalignment of the distal stent ring was observed in 1 subject, where the distal most stent ring was
not aligned perpendicular to the centerline of blood flow. Misalignment of distal stent ring was relative to the direction of the
blood flow. This caused a stent peak on the distal most stent ring to be angled into the lumen. The investigator did not
determine the imaging finding reported by the core lab to be a device deficiency. No adverse events were reported associated
with this device deficiency.
26 Instructions for Use English
Page 29

Table 30. Core Lab Reported Device Deficiency
Subject # Day of Fol- low-up
Image
10309-001 43 Any other failure/malfunction of Stent
Device Deficiencies observed on
the image
Graft specify:
Comments
Other Device Deficiency: Misalignment of distal stent ring relative to
direction of blood flow.
10309-001 225 Any other failure/malfunction of Stent
Graft, specify:
Other Device Deficiency: Misalignment of distal stent ring relative to
direction of blood flow.
FDA requested worst-case analysis (ad hoc analysis) for the primary endpoint including the 4 additional events that would
generally count against successful delivery and deployment, including inaccurate deployment, need for use of bailout
procedures and unplanned implantation of additional devices. The worst-case analysis met the performance goal of the Valiant
Evo IDE study and is provided in Table 31 below.
Table 31. Primary Endpoint Worst-Case Analysis per FDA’s Definition of Successful Deployment
Primary Endpoint with Worst Case Analysis per FDA Definition of Successful Deployment
Primary Endpoint Valiant Evo 1-sided 97.5% Upper
Performance Goal
Confidence Limit
Access Failures; Deployment Failures; and/or
6.9% (6/87) 14.41% 16%
MDEs within 30 Days Post Index Procedure
Table 32 and Table 30 outlines when the device deficiencies occurred during the study.
Table 32. Site Reported Device Deficiencies
Subject ID Device Deficiency Type Overall Subject Number
Overall Implant Order at Site
Enrolled in Study (out of 87)
00001-001 Any other failure/malfunction
3 1 of 2
of Stent Graft
00152-001 Deployment Difficulty 7 1 of 9
00020-004 Deployment Difficulty 18 3 of 10
00020-001 Failure to release tip capture 19 4 of 10
00003-001 Deployment Difficulty 27 1 of 2
00020-006 Deployment Difficulty + Failure
to release tip capture
a
10309-002 Difficulty to remove delivery
46 6 of 10
66 2 of 2
system
13046-004 Difficulty to remove delivery
74 3 of 3
system
a
This deployment difficulty was related to the severely tortuous anatomy.
Table 33. Core Lab Reported Device Deficiencies
Subject ID Device Deficiency Type Overall Subject Number
Overall Implant Order at Site
Enrolled in Study (out of 87)
10309-001 Any other failure/malfunction
39 1 of 2
of Stent Graft: Misalignment of
distal stent ring relative to the
blood flow
After completion of the refresher training to mitigate deployment difficulties and any other failure/malfunction of stent graft,
77 remaining subjects of the Valiant Evo IDE study were enrolled. One additional event (subject 00003-001) related to
deployment difficulty occurred after the refresher training. After the device deficiency occurred, the case was verbally
discussed, and the content of the refresher training was reiterated. No additional deployment difficulties were reported after this
event.
Post completion of the refresher training to mitigate failure to release tip capture and difficulty to remove delivery system, 30
and 15 subjects were enrolled, respectively.
Secondary Safety Endpoints
Table 34 summarizes the safety related secondary endpoints evaluated by the cohorts at each time point. In general, a
difference in AE rates between the US and OUS cohorts was notable. Between 0 and 30 days, 90.4% (47/52) of US subjects
Instructions for Use English 27
Page 30

experienced an adverse event. In the OUS cohort, 48.6% (17/35) subjects experienced an adverse event. Between 0 and
183 days, 95.9% (47/49) of US subjects experienced an adverse event. In the OUS cohort, 85.2% (23/27) subjects experienced
an adverse event.
Investigational study staff across both cohorts were trained thoroughly on event reporting requirements and all study sites used
the same AE reporting guidelines and definitions. Yet, a difference in occurrence rates was evident in this data set. There are 2
main reasons for the difference in AE reporting rates globally. The first reason is likely related to the different standard of care
practices for TEVAR between institutions in the US and OUS. For example, implant procedural standard of care in the US
involves usage of urinary catheters that could result in a higher rate of urinary tract infections post-procedure compared to OUS
where urinary catheters are less frequently used intraoperatively for TEVAR. Additionally, ICU stays are routinely longer in the
US, compared to OUS, which could lead to more reportable AEs. The second reason for AE reporting differences is that US
subjects had more comorbidities at baseline, which likely resulted in more reportable AEs after the implant procedure.
Table 34. Secondary Endpoints (Excluding Imaging Findings)
Time Period
US OUS Global Cohort
Secondary Endpoints
0 - 30 Days
Peri-operative Mortality 0.0% (0/52) 5.7% (2/35) 2.3% (2/87)
All Adverse Eventsa, b(AE) 90.4% (47/52) 48.6% (17/35) 73.6% (64/87)
Major Adverse Events (MAE) 38.5% (20/52) 14.3% (5/35) 28.7% (25/87)
Serious Adverse Events (SAE) 36.5% (19/52) 25.7% (9/35) 32.2% (28/87)
Secondary Procedures
b
0.0% (0/52) 5.7% (2/35) 2.3% (2/87)
Secondary Endovascular Procedures 0.0% (0/52) 2.9% (1/35) 1.1% (1/87)
Secondary Surgical Procedure 0.0% (0/52) 2.9% (1/35) 1.1% (1/87)
0 - 183 Days
All-cause Mortality 5.4% (2/37) 15.8% (3/19) 8.9% (5/56)
Aneurysm-related Mortality 0.0% (0/36) 15.8% (3/19) 5.5% (3/55)
Major Device Effectsb(MDE)
0.0% (0/36) 11.1% (2/18) 3.7% (2/54)
Device-related Secondary Procedures 0.0% (0/36) 11.1% (2/18) 3.7% (2/54)
Device-related Mortality 0.0% (0/36) 11.1% (2/18) 3.7% (2/54)
Conversion to Open Surgery 0.0% (0/36) 0.0% (0/16) 0.0% (0/52)
Thoracic Aortic Aneurysm Rupture 0.0% (0/36) 5.9% (1/17) 1.9% (1/53)
All Adverse Events
a, b
(AE)
95.9% (47/49) 85.2% (23/27) 92.1% (70/76)
Major Adverse Events (MAE) 51.0% (25/49) 22.2% (6/27) 40.8% (31/76)
Serious Adverse Events (SAE) 55.1% (27/49) 48.1% (13/27) 52.6% (40/76)
Secondary Procedures 2.8% (1/36) 11.1% (2/18) 5.6% (3/54)
Secondary Endovascular Procedures 2.8% (1/36) 5.9% (1/17) 3.8% (2/53)
Secondary Surgical Procedure 0.0% (0/36) 5.9% (1/17) 1.9% (1/53)
0 - 365 Days
All-cause Mortality 15.0% (3/20) 21.4% (3/14) 17.6% (6/34)
Aneurysm-related Mortality 0.0% (0/17) 21.4% (3/14) 9.7% (3/31)
Major Device Effectsb(MDE)
5.6% (1/18) 15.4% (2/13) 9.7% (3/31)
Device-related Secondary Procedures 0.0% (0/17) 15.4% (2/13) 6.7% (2/30)
Device-related Mortality 5.6% (1/18) 15.4% (2/13) 9.7% (3/31)
Conversion to Open Surgery 0.0% (0/17) 0.0% (0/11) 0.0% (0/28)
Thoracic Aortic Aneurysm Rupture 0.0% (0/17) 8.3% (1/12) 3.4% (1/29)
All Adverse Events
a, b
(AE)
95.9% (47/49) 88.5% (23/26) 93.3% (70/75)
Major Adverse Events (MAE) 55.1% (27/49) 26.9% (7/26) 45.3% (34/75)
Serious Adverse Events (SAE) 57.1% (28/49) 50.0% (13/26) 54.7% (41/75)
Secondary Procedures 5.6% (1/18) 15.4% (2/13) 9.7% (3/31)
Secondary Endovascular Procedures 5.6% (1/18) 8.3% (1/12) 6.7% (2/30)
Secondary Surgical Procedure 0.0% (0/17) 8.3% (1/12) 3.4% (1/29)
a
All Adverse Events including, but not limited to, MAEs and SAEs.
b
A subject may experience multiple events; hence, number of subjects counted in the overall event rate may not be the sum of those in each event.
Note: Denominators included all enrolled subjects who either had an event within the time period or were followed for at least
1, 91, or 305 days for the time periods of 30, 183, or 365 days, respectively.
28 Instructions for Use English
Page 31

All-Cause Mortality
0
0.0
0.2
0.4
0.6
0.8
1.0
30 90 180 270 365
2
1
3
Table 35 and Figure 4 display the Kaplan-Meier estimate of all-cause mortality (ACM) of the global cohort within 365 days of the
index procedure. Freedom from ACM was reported in 97.7% of subjects from treatment to 30 days.
Table 35. Kaplan-Meier Estimates of Freedom from All-cause Mortality through 365 Days
All-cause Mortality Treatment to 30 days 31 to 183 days 184 to 365 days
No. at Risk
a
87 78 44
No. of Events 2 3 1
No. Censored
Kaplan-Meier Estimate
b
c
7 31 24
0.977 0.928 0.898
Standard Error 0.016 0.032 0.043
a
Number of subjects at risk at the beginning of interval.
b
Subjects are censored because their last follow-up has not reached the end of the time interval or because they are lost to follow-up.
c
Estimate made at end of time interval.
Figure 4 shows the Kaplan-Meier estimate of freedom from ACM, which was 89.8% through 365 days in the global cohort.
Figure 4. Kaplan-Meier Estimates of Freedom from All-cause Mortality through 365 Days
1. Freedom from All-cause Mortality
2. Days from Initial Procedure
3. Number of subjects at risk
Aneurysm-Related Mortality
Aneurysm-related mortality (ARM), is defined as any death occurring within 30 days from either the initial procedure or any
secondary procedure intended to treat the aneurysm, unless there is evidence to the contrary. Additionally, deaths occurring as
a consequence of any procedure intended to treat the targeted aneurysm, aneurysm rupture, or a conversion to open repair are
also considered as ARM. Table 36 and Figure 5 display the Kaplan-Meier estimate of aneurysm-related mortality (ARM) of the
global cohort within 365 days of the index procedure. Freedom from ARM was reported in 97.7% of subjects from treatment to
30 days. The causes of ARM are presented in Table 37.
Table 36. Kaplan-Meier Estimates of Freedom from Aneurysm-related Mortality through 365 Days
Aneurysm-related Mortality Treatment to 30 days 31 to 183 days 184 to 365 days
No. at Risk
No. of Events 2 1 0
No. Censored
a
b
87 78 44
7 33 25
Instructions for Use English 29
Page 32

Aneurysm-related Mortality Treatment to 30 days 31 to 183 days 184 to 365 days
0
0.0
0.2
0.4
0.6
0.8
1.0
30 90 180 270 365
2
1
3
Kaplan-Meier Estimate
c
0.977 0.964 0.964
Standard Error 0.016 0.021 0.021
a
Number of subjects at risk at the beginning of interval.
b
Subjects are censored because their last follow-up has not reached the end of the time interval or because they are lost to follow-up.
c
Estimate made at end of time interval.
In Figure 5, a Kaplan-Meier analysis of freedom from ARM was performed and shows the freedom from ARM through 365 days
was 96.4% in the global cohort.
Figure 5. Kaplan-Meier Estimates of Freedom from Aneurysm-related Mortality through 365 Days
1. Freedom from Aneurysm-related Mortality
2. Days from Initial Procedure
3. Number of subjects at risk
Deaths
Table 37 below summarizes the 6 deaths that occurred in the global cohort in this analysis. A total of 2 mortalities occurred
within 30 days of the procedure, both aneurysm related. All deaths were adjudicated by the CEC, who provided an independent
evaluation based on their medical experience.
A total of 3 deaths were adjudicated as aneurysm related (10309-002, 11080-002, 11081-001). The CEC adjudicated the death
of subject 10309-002 as device and procedure related as it occurred within one day of the procedure. The CEC adjudicated the
death of subject 11080-002 as procedure related as it occurred within 30 days. There was no evidence in the source
documents provided to indicate device relatedness. The death of subject 11081-001 was due to an infection of the graft; if the
subject did not have the graft implanted, nor the procedure, the infection possibly would not have occurred, thus the death was
adjudicated as device and procedure related.
Please note that of the 6 deaths noted in Table 37, the retrograde Type A dissection in 10309-002 was caused by a device
deficiency associated with removing the delivery system. All implanting investigators were required to complete updated device
training in order to understand the correct troubleshooting techniques needed to overcome difficulty removing the delivery
system. Maneuvers include relieving the forward pressure in the delivery system before attempting to actuate the tip capture.
30 Instructions for Use English
Page 33

Table 37. Subject Deaths
0
0.0
0.2
0.4
0.6
0.8
1.0
30 90 180 270 365
2
1
3
CEC Adjudication
Subject # Adverse Events leading to Death Day from
Implant
10309-002 retrograde dissection type A
1 Yes Yes Yes
Device Related Procedure
Related
Aneurysm Related
AORTA
11080-002 Death
11081-001 aortic arch rupture due to septice-
a
24 No Yes Yes
35 Yes Yes Yes
mia
00223-001 Tracheal Hemorrhage 73 No No No
00020-006 Worsening COPD 147 No No No
00078-001 Bacterial sepsis 280 Yes Yes No
a
No death certificate was available; thus, the cause of death was unknown.
Major Device Effects
Major Device Effects (MDEs) are defined as the occurrence of any of the following: device-related secondary procedures,
device-related mortality, conversion to open surgery, and thoracic aortic aneurysm rupture.
Table 38 and Figure 6 shows the Kaplan-Meier Estimate of freedom from MDEs within the global cohort. From 0-30 days,
freedom from MDE was reported in 97.6% of subjects.
Table 38. Kaplan-Meier Estimates of Freedom from Major Device Effects through 365 Days
Major Device Effects (MDE) Treatment to 30 days 31 to 183 days 184 to 365 days
No. at Risk
a
87 77 44
No. of Events 2 0 1
No. Censored
Kaplan-Meier Estimate
b
c
8 33 24
0.976 0.976 0.946
Standard Error 0.017 0.017 0.034
a
Number of subjects at risk at the beginning of interval.
b
Subjects are censored because their last follow-up has not reached the end of the time interval or because they are lost to follow-up.
c
Estimate made at end of time interval.
Figure 6. Kaplan-Meier Estimates of Freedom from Major Device Effects through 365 Days
1. Freedom from Major Device Effects
2. Days from Initial Procedure
Instructions for Use English 31
Page 34

3. Number of subjects at risk
Details of the breakdown of MDEs are displayed in Table 39. Of the 6 MDEs reported within 365 days, 50% (3/6) were device
related mortalities, 33.3% (2/6) were device related secondary procedures, and 16.7% (1/6) was a TAA rupture. The events
associated with the two OUS subjects (10309-002 and 11081-001) are described in Section 9.8.1 above. The US subject
(00078-001) died of bacterial sepsis on Day 280 which was adjudicated as device related; the CEC acknowledged that the
event appeared not to be related to the specific Valiant Evo device, but rather is a known risk for any TEVAR procedure.
Table 39. CEC Adjudicated Major Device Effects (MDE) through 365 Days
Subject # Days from Implant CEC Term
10309-002 1 Device related mortality
10309-002 1 Device related secondary proce-
dure
11081-001 28 DTAA Rupture
11081-001 28 Device related secondary proce-
dure
11081-001 35 Device related mortality
00078-001 280 Device related mortality
Major Adverse Events (MAEs)
Table 40 shows the major adverse events (MAE) reported under the IDE. The percentage of subjects who experienced one or
more MAEs between 0-30 days was 28.7% (25/87) in the global cohort. The system organ class with the most MAEs was
Cardiac Disorders (17.2%;15/87). The most frequent MAEs reported were atrial fibrillation (4.6%; 4/87) and acute renal failure
(3.4%; 3/87). Of note, 2 subjects had aortic dissections reported between 0-30 days. One subject had a retrograde type A
dissection on day 1 post index procedure, which was attempted to be repaired via an open surgical repair, and led to death on
day 1 (details can be found in Table 37). Another subject had a segmental aortic dissection at the distal neck on day 1. The
subject experienced acute dorsal pain and a CT scan was performed which revealed a focal aortic dissection at the distal end
of the stent graft. Invasive pressure monitoring was initiated along with medications. At the time of the data snapshot, the
dissection was ongoing with the plan to continue monitoring and not to intervene.
The percentage of subjects who experienced one or more MAEs between 31-183 days was 10.3% (8/78) in the global cohort.
The system organ class with the most MAEs was Cardiac Disorders (5.1%; 4/78). The most frequently reported MAE was atrial
fibrillation (2.6%; 2/78). The percentage of subjects who experienced one or more MAEs between 184-365 days was 9.1%
(4/44) in the global cohort. Cardiac Disorders was the most commonly reported category of MAE with 4.5% (2/44) of subjects.
Table 40. Major Adverse Events (MAE) (All Subjects, Site-Reported)
System Organ Class 0-30 Days 31-183 Days 184-365 Days
Preferred Term ma = 87
Any Major Adverse Events (MAE b ) 28.7% (25/87) 10.3% (8/78) 9.1% (4/44)
Cardiac Disorders 17.2% (15/87) 5.1% (4/78) 4.5% (2/44)
Acute Myocardial Infarction 1.1% (1/87) 0.0% (0/78) 2.3% (1/44)
Angina Unstable 0.0% (0/87) 1.3% (1/78) 0.0% (0/44
Atrial Fibrillation 4.6% (4/87) 2.6% (2/78) 0.0% (0/44)
Atrial Tachycardia 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Atrioventricular Block 1.1% (1/87) 0.0% (0/78) 2.3% (1/44)
Atrioventricular Block First Degree 2.3% (2/87) 0.0% (0/78) 0.0% (0/44)
Bradycardia 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Cardiac Failure Acute 0.0% (0/87) 2.6% (2/78) 0.0% (0/44)
Cardiac Failure Congestive 2.3% (2/87) 1.3% (1/78) 2.3% (1/44)
Left Ventricular Failure 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Sinus Bradycardia 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Sinus Tachycardia 2.3% (2/87) 1.3% (1/78) 0.0% (0/44)
Supraventricular Tachycardia 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Tachycardia 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Torsade De Pointes 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Ventricular Extrasystoles 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Ventricular Tachycardia 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Infections and Infestations 0.0% (0/87) 1.3% (1/78) 2.3% (1/44)
ma = 78 ma = 44
32 Instructions for Use English
Page 35

System Organ Class 0-30 Days 31-183 Days 184-365 Days
Preferred Term ma = 87
ma = 78 ma = 44
Lung Infection 0.0% (0/87) 0.0% (0/78) 2.3% (1/44)
Pneumonia 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Injury, Poisoning and Procedural Complica-
2.3% (2/87) 1.3% (1/78) 0.0% (0/44)
tions
Fat Embolism 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Procedural Haemorrhage 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Vascular Pseudoaneurysm 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Investigations 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Blood Creatinine Increased 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Nervous System Disorders 5.7% (5/87) 0.0% (0/78) 2.3% (1/44)
Cerebrovascular Accident 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Embolic Stroke 2.3% (2/87) 0.0% (0/78) 0.0% (0/44)
Ischaemic Stroke 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Paraplegia 0.0% (0/87) 0.0% (0/78) 2.3% (1/44)
Spinal Cord Ischaemia 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Renal and Urinary Disorders 3.4% (3/87) 0.0% (0/78) 2.3% (1/44)
Renal Failure Acute 3.4% (3/87) 0.0% (0/78) 2.3% (1/44)
Respiratory, Thoracic and Mediastinal Disor-
4.6% (4/87) 1.3% (1/78) 0.0% (0/44)
ders
Acute Respiratory Failure 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Atelectasis 2.3% (2/87) 0.0% (0/78) 0.0% (0/44)
Pulmonary Congestion 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Pulmonary Embolism 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Respiratory Distress 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Vascular Disorders 5.7% (5/87) 1.3% (1/78) 0.0% (0/44)
Aortic Dissection 2.3% (2/87) 0.0% (0/78) 0.0% (0/44)
Aortic Rupture 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Femoral Artery Occlusion 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Peripheral Artery Thrombosis 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Peripheral Ischaemia 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
a
Number of subjects at risk at the beginning of the time interval and it is the denominator of event rate for the given time period.
b
Percent (number) of subjects who experienced one or more Major Adverse Events (MAEs) during the time period. A subject may report multiple adverse events and in different categories; hence, number of
subjects in each category may not be the sum of those in each subcategory. Each subject was only counted once in each category.
Serious Adverse Events (SAEs)
Table 41 shows the serious adverse events (SAE) reported under the IDE. The percentage of subjects who experienced one or
more SAEs between 0-30 days was 32.2% (28/87) in the global cohort. The system organ class with the most SAEs was
Cardiac Disorders (9.2%; 8/87), followed by Nervous System Disorders (8.0%; 7/87) and Vascular Disorders (8.0%; 7/87). The
percentage of subjects who experienced one or more SAEs between 31-183 days was 24.4% (19/78) in the global cohort. The
most frequently reported SAE were within the system organ classes of Respiratory, Thoracic and Mediastinal Disorders (6.4%;
5/78) and Vascular Disorders (6.4%; 5/78). The most commonly reported SAE was Chronic Obstructive Pulmonary Disease
(3.8%; 3/78).The percentage of subjects who experienced one or more SAEs between 184-365 days was 22.7% (10/44) in the
global cohort. Most SAEs reported were in the system organ classes of Infections and Infestations (6.8%; 3/44) and Vascular
Disorders (6.8%; 3/44).
Table 41. Serious Adverse Events (SAE) (All Subjects, Site-Reported)
System Organ Class 0-30 Days 31-183 Days 184-365 Days
Preferred Term ma = 87
Any serious AEs
b
32.2% (28/87) 24.4% (19/78) 22.7% (10/44)
ma = 78 ma = 44
Blood and Lymphatic System Disorders 2.3% (2/87) 1.3% (1/78) 0.0% (0/44)
Anaemia 1.1% (1/87) 1.3% (1/78) 0.0% (0/44)
Anaemia Of Chronic Disease 0.0% (0/87) 1.3% (1/78) 0.0% (0/44
Neutrophilia 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Cardiac Disorders 9.2% (8/87) 2.6% (2/78) 4.5% (2/44)
Instructions for Use English 33
Page 36

System Organ Class 0-30 Days 31-183 Days 184-365 Days
Preferred Term ma = 87
Acute Myocardial Infarction 1.1% (1/87) 0.0% (0/78) 2.3% (1/44)
Angina Unstable 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Atrial Fibrillation 3.4% (3/87) 1.3% (1/78) 0.0% (0/44)
Atrioventricular Block 1.1% (1/87) 0.0% (0/78) 2.3% (1/44)
Cardiac Failure Congestive 2.3% (2/87) 0.0% (0/78) 2.3% (1/44)
Left Ventricular Failure 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Tachycardia 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Ventricular Tachycardia 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Gastrointestinal Disorders 3.4% (3/87) 1.3% (1/78) 0.0% (0/44)
Colitis 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Faecal Incontinence 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Gastritis 0.0% (0/87) 0.0% (0/78) 0.0% (0/44)
Gastrointestinal Haemorrhage 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Ileus 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Pancreatitis Acute 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
General Disorders and Administration Site
Conditions
Death 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Pyrexia 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Stent-Graft Endoleak 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Hepatobiliary Disorders 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Cholecystitis Acute 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Immune System Disorders 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Anaphylactic Shock 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Infections and Infestations 4.6% (4/87) 3.8% (3/78) 6.8% (3/44)
Bacterial Sepsis 0.0% (0/87) 0.0% (0/78) 2.3% (1/44)
Device Related Infection 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Lung Infection 0.0% (0/87) 0.0% (0/78) 2.3% (1/44)
Pneumonia 0.0% (0/87) 1.3% (1/78) 2.3% (1/44)
Sepsis 2.3% (2/87) 1.3% (1/78) 0.0% (0/44)
Urinary Tract Infection Bacterial 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Urinary Tract Infection Staphylococcal 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Urosepsis 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Injury, Poisoning and Procedural Complications
Cervical Vertebral Fracture 0.0% (0/87) 0.0% (0/78) 2.3% (1/44)
Facial Bones Fracture 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Fat Embolism 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Hand Fracture 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Mental Status Changes Postoperative 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Overdose 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Post Lumbar Puncture Syndrome 2.3% (2/87) 0.0% (0/78) 0.0% (0/44)
Spinal Compression Fracture 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Tracheal Haemorrhage 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Vascular Pseudoaneurysm 1.1% (1/87) 1.3% (1/78) 0.0% (0/44)
Wound Dehiscence 0.0% (0/87) 0.0% (0/78) 2.3% (1/44)
Investigations 1.1% (1/87) 1.3% (1/78) 0.0% (0/44)
Blood Creatinine Increased 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Weight Decreased 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Metabolism and Nutrition Disorders 2.3% (2/87) 1.3% (1/78) 2.3% (1/44)
Fluid Overload 0.0% (0/87) 0.0% (0/78) 2.3% (1/44)
3.4% (3/87) 0.0% (0/78) 0.0% (0/44)
6.9% (6/87) 5.1% (4/78) 4.5% (2/44)
ma = 78 ma = 44
34 Instructions for Use English
Page 37

System Organ Class 0-30 Days 31-183 Days 184-365 Days
Preferred Term ma = 87
Hyponatraemia 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Malnutrition 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Vitamin D Deficiency 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Musculoskeletal and Connective Tissue Disorders
Arthritis 0.0% (0/87) 0.0% (0/78) 2.3% (1/44)
Muscular Weakness 1.1% (1/87) 1.3% (1/78) 0.0% (0/44)
Pain in Extremity 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Pseudarthrosis 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Neoplasms Benign, Malignant and Unspecified
(Incl Cysts and Polyps)
Bladder Cancer Recurrent 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Squamous Cell Carcinoma 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Nervous System Disorders 8.0% (7/87) 1.3% (1/78) 4.5% (2/44)
Cerebrovascular Accident 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Dementia with Lewy Bodies 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Embolic Stroke 2.3% (2/87) 0.0% (0/78) 0.0% (0/44)
Hypoaesthesia 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Ischaemic Stroke 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Metabolic Encephalopathy 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Paraplegia 0.0% (0/87) 0.0% (0/78) 2.3% (1/44)
Spinal Cord Ischaemia 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Transient Ischaemic Attack 0.0% (0/87) 0.0% (0/78) 2.3% (1/44)
Psychiatric Disorders 3.4% (3/87) 0.0% (0/78) 0.0% (0/44)
Delirium Tremens 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Mental Status Changes 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Suicidal Ideation 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Renal and Urinary Disorders 1.1% (1/87) 2.6% (2/78) 2.3% (1/44)
Renal Failure Acute 0.0% (0/87) 0.0% (0/78) 2.3% (1/44)
Ureteric Obstruction 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Urinary Bladder Polyp 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Urinary Incontinence 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Respiratory, Thoracic and Mediastinal Disorders
Acute Respiratory Failure 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Atelectasis 2.3% (2/87) 0.0% (0/78) 0.0% (0/44)
Chronic Obstructive Pulmonary Disease 1.1% (1/87) 3.8% (3/78) 0.0% (0/44)
Chylothorax 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Dyspnoea 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Hypoxia 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Pulmonary Congestion 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Pulmonary Embolism 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Respiratory Distress 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Vascular Disorders 8.0% (7/87) 6.4% (5/78) 6.8% (3/44)
Aortic Aneurysm 0.0% (0/87) 2.6% (2/78) 0.0% (0/44)
Aortic Dissection 2.3% (2/87) 0.0% (0/78) 0.0% (0/44)
Aortic Rupture 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Femoral Artery Occlusion 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Haemorrhage 0.0% (0/87) 0.0% (0/78) 2.3% (1/44)
Hypertension 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Hypertensive Crisis 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
1.1% (1/87) 2.6% (2/78) 2.3% (1/44)
0.0% (0/87) 2.6% (2/78) 0.0% (0/44)
5.7% (5/87) 6.4% (5/78) 0.0% (0/44)
ma = 78 ma = 44
Instructions for Use English 35
Page 38

System Organ Class 0-30 Days 31-183 Days 184-365 Days
Preferred Term ma = 87
ma = 78 ma = 44
Orthostatic Hypotension 0.0% (0/87) 1.3% (1/78) 2.3% (1/44)
Peripheral Artery Stenosis 0.0% (0/87) 0.0% (0/78) 2.3% (1/44)
Peripheral Artery Thrombosis 0.0% (0/87) 1.3% (1/78) 0.0% (0/44)
Peripheral Ischaemia 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
Thrombophlebitis 1.1% (1/87) 0.0% (0/78) 0.0% (0/44)
a
Number of subjects at risk at the beginning of the time interval and it is the denominator of event rate for the given time period.
b
Percent (number) of subjects who experienced one or more serious AEs during the time period. A subject may report multiple adverse events and in different categories; hence, number of subjects in each
category may not be the sum of those in each subcategory. Each subject was only counted once in each category.
Secondary Procedures
Table 42 displays the 3 secondary procedures that were performed through 365 days. All secondary procedures were
adjudicated by the CEC to determine if the intervention performed was an MDE (a Valiant Evo device related secondary
procedure). Two secondary procedures were adjudicated as device-related (10309-002 and 11081-001), and one secondary
procedure was not adjudicated as device-related (00341-001). Subject 10309-002 underwent an emergency pericardiocentesis
to treat a retrograde dissection type A. Subject 11081-001 had an implantation of another stent graft due to an aortic arch
rupture. Subject 00341-001 had a repair of a left subclavian pseudoaneurysm and coil embolization of a Type II endoleak.
Table 42. Secondary Procedures within 365 Days
Subject # Days from Implant Type of Secondary Procedure: Reason (AE Term)
10309-002 1 Secondary Surgical Procedure: retrograde dissection type A
AORTA
11081-001 28 Secondary Endovascular Procedure: aortic arch rupture due to
septicemia
00341-001 70 Secondary Endovascular Procedure: Type II Endoleak
Secondary Effectiveness Endpoints
Table 43, Table 44, and Table 45 show the secondary endpoints reported by core lab. At the time of the data snapshot, no loss
of stent graft patency or stent graft migration was reported by the core lab at any timepoint.
Table 43. Secondary Endpoints Based on Imaging Findings (Core Lab Reported)
Time Period Secondary Endpoints Global Cohort
1 Month
Loss of Stent Graft Patency at 1 Month 0.0% (0/81)
Endoleaks at 1 Month 2.5% (2/81)
6 Month
Loss of Stent Graft Patency within 6 Months 0.0% (0/32)
Endoleaks at 6 Months 6.3% (2/32)
Stent Graft Migration at 6 Months 0.0% (0/36)
Aneurysm Expansion >5 mm at 6 Months 2.7% (1/37)
12 Month
Loss of Stent Graft Patency within 12 Months 0.0% (0/21)
Endoleaks at 12 Months 9.5% (2/21)
Stent Graft Migration at 12 Months 0.0% (0/21)
Aneurysm Expansion >5 mm at 12 Months 9.5% (2/21)
Note: In Table 43, denominator is number of subjects evaluable for the endpoint; a subject either had an event during the time
period, or had an imaging assessment by the end of the time period. 6-month data is not required per OUS protocol, therefore,
the data reported at this timepoint may not add up to the total number of subjects evaluable at 1 month.
Endoleaks
A total of 2 endoleaks were reported globally at 1 month. A total of 2 endoleaks were reported globally at 6 months, one of
which (Type Ia) was continuing from 1 month, and one of which was a new Type Ib endoleak. A total of 2 endoleaks were
reported globally at 12 months, one of which (Type Ib) was continuing from 6 months, and one of which was a new Type Ib
endoleak. The core lab did not review imaging performed during the procedure. The breakdown of site-reported endoleaks by
type in the global cohort is displayed in Table 46 below.
Because the Valiant Evo trial is still ongoing, not all subjects have completed a 6- and 12-month follow-up visit. Thus, only 1month endoleak data is presented in the table below. At the 6-month time point, core lab analysis reported an endoleak in 2 out
36 Instructions for Use English
Page 39

of 32 subjects (6.3%). Please note that a 6-month follow-up visit is not required per protocol in OUS. At the 12-month follow-up,
core lab analysis identified 2 endoleaks in 21 subjects (9.5%).
Table 44. Endoleaks (All Subjects - Core Lab Reported)
Endoleaks 1 Month (1 – 90 Days)
Type I 1.2% (1/81)
Type Ia 1.2% (1/81)
Type Ib 0.0% (0/81)
Type Ic 0.0% (0/81)
Type II 1.2% (1/81)
Type III 0.0% (0/81)
Type IIIa 0.0% (0/81)
Type IIIb 0.0% (0/81)
Type IV 0.0% (0/81)
Type V 0.0% (0/81)
Type Undetermined 0.0% (0/81)
Subjects Had Endoleaks Of Any Type
a
A subject may have more than one type of endoleaks; hence, number of subjects with any type may not be the sum of those in each type.
a
2.5% (2/81)
Note: In Table 44, denominator is the number of subjects who had evaluable images in the time period.
Table 45. Endoleak Listing (Core Lab)
Subject # Follow-up Visit Day of Follow-up
Type of Endoleak
Image
13001-002 1-Month 33 Type IA
13044-002 1-Month 33 Type II
00152-001 6-Months 152 Type IB
13001-002 6-Months 159 Type IA
00152-001 12-Months 362 Type IB
13045-002 12-Months 379 Type IB
Upon completion of the index procedure at day 0, a total of 5 (5.7%) endoleaks were reported by the sites, 1 Type Ib, 2 Type II,
1 Type IV, and 1 undetermined Type. At the 1-month follow-up visit, a total of 2 (2.5%) endoleaks were reported by the sites,
both Type II endoleaks.At the 6-month follow-up visit, 2 (6.1%) Type II endoleaks were reported by the sites, 1 new and
1 continuing. At the 12-month follow-up visit, 1 (4.8%) new type Ib endoleak and 1 (4.8%) continuing Type II endoleak was
reported.
Because the Valiant Evo trial is still ongoing, not all subjects have completed a 6- and 12-month follow-up visit. Thus, only day
0 and 1-month endoleak data is presented in the table below.
Table 46. Endoleaks (All Subjects - Site Reported)
Endoleaks Day 0 1 Month
(1 – 90 Days)
Type I 1.1% (1/87) 0.0% (0/81)
Type Ia 0.0% (0/87) 0.0% (0/81)
Type Ib 1.1% (0/87) 0.0% (0/81)
Type Ic 0.0% (0/87) 0.0% (0/81)
Type II 2.3.% (2/87) 2.5% (2/81)
Type III 0.0% (0/87) 0.0% (0/81)
Type IIIa 0.0% (0/87) 0.0% (0/81)
Type IIIb 0.0% (0/87) 0.0% (0/81)
Type IV 1.1% (1/87) 0.0% (0/81)
Type V 0.0% (0/87) 0.0% (0/81)
Type Undetermined 1.1% (1/87) 0.0% (0/81)
Subjects Had Endoleaks Of Any Type
a
A subject may have more than one type of endoleaks; hence, number of subjects with any type may not be the sum of those in each type.
a
4.6% (4/87) 2.5% (2/81)
Note: Denominator is the number of subjects who had evaluable images in the time period.
Note: A type Ib endoleak was treated by secondary procedure on day 448 but was not reported in the site-reported images.
This event was included in endoleaks event rate calculations.
Instructions for Use English 37
Page 40

Change in Aneurysm Diameter
Table 47 and Table 48 display the change in aneurysm diameter and aneurysm expansion, respectively.
In the US cohort, all (100%; 30/30) subjects were reported by core lab to have aneurysm diameters that remained stable or had
aneurysm diameters that decreased more than 5 mm at 6 months, as compared to 1 month. At 12 months, the core lab
reported that 100% (12/12) of US subjects had maximum aneurysm diameters that remained stable or decreased more than
5 mm.
In the OUS cohort, (85.7%; 6/7) subjects were reported by core lab to have aneurysm diameters that remained stable at
6 months, as compared to 1 month. At 6 months, a total of 1 OUS subject (14.3%) was reported to have a maximum aneurysm
diameter than increased more than 5 mm as compared to 1 month. The core lab indicated that for this subject the PAU did not
increase in size, rather the increase in maximum aortic diameter is likely caused by expected dilatation of the aorta after a
TEVAR. No endoleaks were reported for this subject by the core lab nor the investigational site, and no interventions were
performed associated with this reported expansion. At 12 months, the core lab reported that 77.8% (7/9) of OUS subjects had
maximum aneurysm diameters that remained stable or decreased more than 5 mm. A total of 2 OUS subjects (22.2%) were
reported by core lab to have a maximum aneurysm diameter increase more than 5 mm between 1 month and 12 months; the
same subject that had the aneurysm expansion at 6 months was reported having this same observation at 12 months. The
second subject that had a maximum aneurysm diameter increase between 1 month and 12 months was reported having a
Type Ib endoleak due to distal aortic dilation resulting from aortic remodeling. A secondary procedure was performed on
day 448 to resolve the Type Ib endoleak and distal aortic dilation.
Table 47. Change in Aneurysm Diameter (Core Lab)
Change in Maximum Aneurysm Diameter US OUS Global Cohort
From 1 Month to 6 Months
a
Increase More Than 5 mm 0.0% (0/30) 14.3% (1/7) 2.7% (1/37)
Stable (within ± 5 mm) 83.3% (25/30) 85.7% (6/7) 83.8% (31/37)
Decrease More Than 5 mm 16.7% (5/30) 0.0% (0/7) 13.5% (5/37)
From 1 Month to 12 Months
a
Increase More Than 5 mm 0.0% (0/12) 22.2% (2/9) 9.5% (2/21)
Stable (within ± 5 mm) 66.7% (8/12) 66.7% (6/9) 66.7% (14/21)
Decrease More Than 5 mm 33.3% (4/12) 11.1% (1/9) 23.8% (5/21)
a
Change in aneurysm diameter was compared to the 1-month contrast enhanced imaging measurement. When 1-month imaging was not available, the pre-discharge imaging was used as the baseline.
Note: In Table 47, denominator is number of subjects evaluable for aneurysm diameter at both one month and the month as
indicated. 6-month imaging is not a standard of care visit for OUS subjects; fewer subjects were available for the 6-month
timepoint as a result.
Table 48. Aneurysm Expansion > 5 mm (Core Lab)
Subject # Follow-up Visit Day of Follow-up Image
11098-004 From 1 Month to 6 Months 232
11098-004 From 1 Month to 12 Months 351
13045-002 From 1 Month to 12 Months 379
Other Imaging Observations
Table 49 summarizes the other imaging findings reported by the core lab. A total of 2 other imaging observations were reported
by the core lab at the time of the database cutoff.
Table 49. Other Imaging Findings (Core Lab Reported)
Subject # Follow-up Visit Day of Follow-
Other imaging findings
up Image
00020-003 DISCHARGE 9 Stent not fully expanded
a
13045-002 12M FU 379 The anatomy of the thoracic aorta is changing due to the aneurysm
enlarging distally, which explains the change in distance values and tor-
tuosity
a
Note: The core lab reported that the stent was not fully expanded at discharge, on day 9. However, this observation was not reported by the site. No adverse events were reported as a result of this finding, and
the observation was not reported by the core lab at 1 month, 6 months or 12 months. Thus, this observation was not reported as a device deficiency by the core lab.
38 Instructions for Use English
Page 41

10. Directions for use
10.1. Vascular access
1. Establish vascular access for introducing the delivery system via a small oblique groin incision over the primary access
artery. Iliac conduits may be used to ensure the safe insertion of the delivery system. A secondary access site should be
used for diagnostic and imaging purposes. The secondary access site is determined at the discretion of the physician.
2. To reduce the risk of thromboembolism, it is recommended that patients be anticoagulated for the duration of the procedure
to achieve an Activated Clotting Time of 250 to 300 seconds, at the discretion of the physician. Antiplatelet therapy may
also be administered at the discretion of the physician.
Caution: Never advance or retract equipment from the vasculature without fluoroscopy.
10.2. Initial angiogram
1. Using continuous fluoroscopy, traverse a 0.035 in (0.89 mm) guidewire and graduated pigtail angiographic catheter (via the
secondary access site) to confirm the target landing zones.
2. Using angiographic imaging, confirm preoperative CT measurements. Refer to Table 2 through Table 8 to confirm device
diameter.
3. Leave the angiographic catheter in place during the procedure to aid in confirming the position of the graft.
Note: In order to enhance visualization of the thoracic aortic arch, an angulation of 45 to 60 degrees left anterior oblique
(LAO) may be chosen.
For dissections, it is also advisable to use transesophageal echocardiography (TEE) or intravascular ultrasound (IVUS).
10.3. Preparation of the Valiant Navion thoracic stent graft system
1. Carefully inspect all product packaging for damage or defects before use. Do not use if the Use-by date has elapsed, the
device is damaged, or the sterilization barrier has been compromised.
Note: The Valiant Navion thoracic stent graft system packaging consists of a single-pouch sterile barrier. Open the pouch
carefully, and transfer the delivery system into the sterile field.
2. While holding the tapered tip of the Valiant Navion thoracic stent graft system higher than the handle, flush the graft cover
using a syringe with heparinized saline solution via the flush port. Apply constant pressure to the syringe until fluid is
observed exiting from the junction of the graft cover and the tapered tip.
Caution: Do not use a power injector with the flush port.
Caution: If difficulties are encountered that prevent the complete flushing of the graft cover lumen, do not use the device.
3. Flush the guidewire lumen with heparinized saline solution via the luer connector until fluid is observed exiting from the
distal extent of the tapered tip.
Caution: Do not grip the tip capture release handle while flushing the delivery system.
4. Verify that the tip capture release handle is in its locked position. The handle should not be able to rotate clockwise while in
the locked position (Figure 7).
Figure 7. Tip capture release handle in locked position
1. Tip capture release handle (should not be able to rotate clockwise when in locked position)
2. Clamping ring
3. Screw gear
Caution: Initiating deployment of the stent graft with the tip capture release handle in its unlocked position (rotated
counterclockwise) may result in premature release of the proximal end.
10.4. Introducing the delivery system
1. If necessary, open narrow entry vessels with standard percutaneous transluminal angioplasty catheters or vessel dilators
before Valiant Navion thoracic stent graft implantation according to standard endovascular procedures. If necessary, dilate
the vessel with a tapered vessel dilator. A stepup approach is recommended for vessel dilation, at the discretion of the
physician.
Instructions for Use English 39
Page 42

2. Insert the delivery system over the guidewire. Before insertion into the vessel, activate the hydrophilic coating by wiping the
outer surface of the graft cover with a sterile gauze saturated in saline, until the graft cover is slippery to touch.
Note: The delivery system does not require a separate introducer sheath for the primary access site. If a separate
introducer sheath is used, refer to the Instructions for Use supplied with the introducer sheath for more information.
Figure 8. Introducing the delivery system
Caution: Manipulation of guidewires, balloons, catheters, and endografts in the thoracic aorta may lead to vascular trauma,
including aortic dissection and embolization.
Caution: Do not bend, kink, or otherwise alter the delivery system before implantation because it may cause deployment
difficulties.
Caution: If an obstruction in the vessel, such as a tortuous bend, stenosis, or calcification formation, prevents advancement of
the delivery system, do not use excessive force to advance the delivery system. The cause of the resistance must be assessed
in order to avoid vessel or delivery catheter damage.
Caution: Do not grip the tip capture release handle while introducing the delivery system.
Warning: Do not advance the delivery system without placing a guidewire, and do not remove the guidewire while the delivery
system is in the patient.
10.5. Positioning the delivery system
1. Slowly advance the delivery system to the targeted landing zone.
2. Position the delivery system by tracking to target location.
Caution: Avoid positioning the device higher in the presence of excessive calcification or thrombus, due to the increased risk of
dislodging material while distally repositioning of the stent graft.
Caution: Avoid or compensate for parallax or other sources of visualization error.
Caution: Do not advance the delivery system tip or guidewire across the aortic valve.
Caution: Do not grip the tip capture release handle while positioning the delivery system.
Note: Stent graft may also be tracked proximal to targeted landing zone.
10.6. Confirming stent graft position
1. Before deploying the Valiant Navion thoracic stent graft, confirm the proper position of the device using fluoroscopy.
2. When placing the stent graft, verify that the proximal RO markers are in the desired location (Figure 9). Placement of the
distal end is verified by ensuring that the distal markers are in the desired location. Additional stent grafts may be implanted
to extend the length of coverage and exclude the lesion. For additional information, refer to Section 10.11 (Implanting
additional configurations).
Note: The circumferential position of the RO markers will vary. The Valiant Navion thoracic stent graft is axisymmetric and does
not require rotational orientation to achieve the desired clinical results.
Note: To confirm stent graft position when implanting 2 or more Valiant Navion devices, the minimum overlap is achieved by
aligning the distal markers of the proximal graft with the mid-marker of the distal graft, except when using a distal stent graft
that is shorter than 90 mm. Refer to Section 10.11 (Implanting additional configurations).
Note: If using a stent graft that is shorter than 90 mm to extend proximal stent graft coverage, deploy the proximal graft
material edge of the stent graft no more than 10 mm proximal to the graft material edge of the adjacent stent graft. To extend
40 Instructions for Use English
Page 43

proximal landing zone coverage more than 10 mm, use a stent graft with a covered length of ≥90 mm. The most proximal stent
graft must meet the proximal landing zone requirements for either FreeFlo (≥20 mm) or CoveredSeal (≥25 mm).
Note: If using a stent graft that is shorter than 90 mm to extend distal stent graft coverage, deploy the distal graft material edge
of the stent graft no more than 10 mm distal to the graft material edge of the adjacent stent graft. To extend distal landing zone
coverage more than 10 mm, use a stent graft with a covered length of ≥90 mm. The most distal stent graft must meet the distal
landing zone requirement (≥20 mm for both FreeFlo and CoveredSeal). Refer to Section 6.1 (Patient selection).
Caution: In the presence of excessive calcification or thrombus formation, it is not recommended to position the device higher
and then reposition distally after partial stent graft deployment, due to increased risk of dislodging material.
Caution: Do not use stent grafts shorter than 90 mm at an unsupported joint or to connect 2 previously placed stent grafts.
Caution: Avoid or compensate for parallax or other sources of visualization error.
Caution: Do not grip the tip capture release handle while confirming the position of the delivery system.
Figure 9. Confirming stent graft position
10.7. Deploying the Valiant Navion thoracic stent graft
1. Ensure delivery system is along the greater curve in order to maintain stability during deployment.
2. Decreasing mean arterial blood pressure (MAP)—Upon confirming that the delivery system is positioned properly, it may be
appropriate to momentarily decrease the patient’s MAP (at the discretion of the physician) to avoid inadvertently displacing
the Valiant Navion thoracic stent graft upon withdrawal of the graft cover.
3. Deploying the proximal end—First, hold the delivery system stationary with one hand on the gray front grip. Then, slowly
withdraw the graft cover with the other hand by rotating the slider handle in the direction of the arrow (counterclockwise). It
may take multiple rotations before the graft cover separates from the tip, visualized by movement of the RO marker band.
The proximal end of the stent graft will be constrained by the tip capture mechanism. Withdraw the graft cover until at least
2 fabric-covered stents are exposed.
Caution: For stent grafts that are shorter than 90 mm, it is important not to deploy more than one covered stent before
repositioning the stent graft. Further deployment of the graft can impair the ability to move the graft to the desired landing
zone.
Caution: Do not place the proximal end of the covered stent graft beyond the distal edge of the left common carotid artery.
Caution: If the stent graft is deployed higher than the targeted landing zone, it is important to not deploy more than
2 covered stents before repositioning the stent graft.
Caution: Do not release the proximal end using the tip capture mechanism before the entire stent graft has been deployed,
as this may result in inaccurate deployment.
Caution: Ensure that the Valiant Navion devices are placed in a landing zone without evidence of circumferential thrombus,
intramural hematoma, ulceration, or aneurysmal involvement. Failure to do so may result in inadequate exclusion or vessel
damage, including perforation. Refer to Section 6.1 (Patient selection).
Note: A larger diameter stent graft may not fully appose to the vessel until 3 or more covered stents are exposed.
Note: If the system is tracked proximal to targeted landing zone and repositioned after 2 fabric covered stents are exposed,
it may be necessary to reestablish system position on the greater curve to avoid inadvertently displacing the stent graft
upon withdrawal of the graft cover.
Instructions for Use English 41
Page 44

Note: In the unlikely event of delivery system failure and concomitant partial stent graft deployment, refer to Section 11
2
1
2
1
(Troubleshooting techniques).
Note: The delivery system should be stabilized and remain stationary during stent graft deployment. Slight forward
pressure may be applied to maintain position.
Figure 10. Deploying the proximal end of the stent graft
1. FreeFlo configuration
2. CoveredSeal configuration
4. Verify position—Use angiography to verify the position of the stent graft in relation to the desired location. Use the proximal
RO markers to aid in visualizing the proximal end of the covered stent graft. If the stent graft was deployed higher than the
targeted landing zone, maintain the position of the slider handle and pull down on the entire delivery system until the
proximal RO markers indicating the top edge of the fabric are at the desired position. Restore system position on the
greater curve.
5. Deploy remainder of the stent graft—Continue withdrawing the graft cover. To rapidly deploy the stent graft, place one hand
firmly on the front grip and hold the system stationary. While maintaining support on the front grip, pull back the trigger to
engage the quick-release function of the slider handle. Pull the blue slider handle away from the front grip until the RO
marker band on the graft cover is beyond the distal stent. If excessive resistance is felt, release the trigger and rotate the
slider handle to complete deployment of the stent graft.
1. FreeFlo configuration
2. CoveredSeal configuration
42 Instructions for Use English
Figure 11. Deploying the remainder of the stent graft
Page 45

Caution: When using the trigger to rapidly deploy the stent graft, ensure that the gray front grip remains stationary. Failure
2
1
to do so will cause movement of the stent graft and will result in inaccurate deployment.
Caution: Do not rotate the delivery system during deployment, as this may torque the delivery system and cause the stent
graft to twist during deployment.
Caution: Do not advance the Valiant Navion thoracic stent graft system when it is partially deployed and apposed to the
vessel wall.
Caution: Once the entire covered portion of the stent graft has been deployed, do not attempt to adjust the position of the
stent graft.
Caution: If the graft cover is inadvertently withdrawn, the stent graft will prematurely deploy and will be placed incorrectly.
Note: If necessary, the stent graft can be repositioned distally to the desired location by retracting it, as long as no more
than 2 of the proximal stents have been deployed. For stent grafts shorter than 90 mm, the stent graft can be repositioned
distally as long as no more than one of the proximal stents has been deployed.
Note: Deployment of the stent graft in the aortic arch can increase the deployment force. Deployment forces can be further
increased by excessive tortuosity and a small radius aortic arch.
Note: In the unlikely event of delivery system failure and concomitant partial stent graft deployment due to graft cover
severance, a “handle disassembly” technique may permit the successful deployment of the stent graft. Refer
to Section 11.1 (Partial stent graft deployment).
10.8. Deploying tip capture mechanism
1. Hold the delivery system stationary with one hand on the front grip. Relieve forward pressure before attempting to actuate
the tip release handle.
Note: Using the guidewire as an indicator, relieve forward pressure by pulling back the delivery system until the guidewire
lumen moves off of the greater curve.
2. With the other hand, rotate the tip capture release handle in the direction of the arrow (counterclockwise) to unlock the tip
capture release handle.
Figure 12. Unlocking the tip capture release handle
1. FreeFlo configuration
2. CoveredSeal configuration
3. Pull the tip capture release handle back in a smooth motion until the tip capture mechanism is released and the proximal
end is completely open (Figure 13). Observe the proximal end opening under fluoroscopy and confirm that the stent graft
has been completely deployed.
Instructions for Use English 43
Page 46

2
1
Figure 13. Deploying the tip capture mechanism
1. FreeFlo configuration
2. CoveredSeal configuration
Note: In the unlikely event that the proximal end cannot be deployed, and resistance is felt in the tip release handle, it may
be necessary to pull back further on the delivery system to relieve forward pressure. If the tip release handle slides freely
and the proximal end cannot be deployed, refer to Section 11 (Troubleshooting techniques).
Caution: Keep the delivery system stationary while deploying the tip capture mechanism. Do not pull back or push forward
on the delivery system while deploying the tip capture mechanism, as it may cause the entire graft to move or cause the tip
capture mechanism to get caught on the proximal stent.
10.9. Removing the delivery system
Caution: Carefully monitor any delivery system movement and the retrieval of the delivery system tapered tip with fluoroscopy
to ensure that delivery system does not inadvertently cause movement of the Valiant Navion thoracic stent graft from its
deployed location.
Note: The guidewire may be repositioned (retracted slightly) to allow the delivery system to assume a more centralized position
in the aorta, which may aid in system closure and retraction.
Caution: It may be necessary to pull the entire delivery system back into a straight section of the aorta to aid in the closure of
the delivery system.
1. Continue to hold the delivery system with one hand on the front grip and the other hand on the slider.
2. Pull back the trigger and hold the slider handle stationary while bringing the front grip towards the slider handle (Figure 14).
Use continual fluoroscopy and watch the proximal end of the Valiant Navion thoracic stent graft while slowly pulling back
the tapered tip into the graft cover of the delivery system.
Caution: If the delivery system catches on the stent graft during removal, it may be necessary to carefully advance the
delivery system until the capture fitting starts to move. Then retract the guidewire to assume a more centralized position in
the aorta before repeating steps for removing the delivery system.
3. Push the tip capture release handle forward so that the capture fitting moves toward the tapered tip. Monitor the movement
of the capture fitting using fluoroscopy.
Caution: Do not complete step 3 before step 2. Doing so may cause the tip capture mechanism to get caught on the
proximal stents.
4. Gently remove the delivery system, using fluoroscopy to ensure that the stent graft does not move during the withdrawal.
44 Instructions for Use English
Page 47

2
1
Figure 14. Removing the delivery system
1. FreeFlo configuration
2. CoveredSeal configuration
10.10. Smoothing stent graft fabric and modeling the stent graft (optional)
The Reliant stent graft balloon catheter (available separately) can be used to remove wrinkles and folds from the graft material
and to assist in implanting the stent graft by modeling the covered stents. Refer to the Instructions for Use supplied with the
Reliant stent graft balloon catheter for more information. Use the balloon catheter to model the proximal and distal seal zones
and to improve suboptimal expansion of the self-expanding stent graft configurations.
Caution: Never use a balloon when treating a dissection.
Caution: Do not use the Reliant stent graft balloon catheter in patients with a history of aortic dissection disease. Do not
overinflate the balloon.
Caution: When expanding a vascular prosthesis using the Reliant stent graft balloon catheter, there is an increased risk of
vessel injury or rupture and patient death if the balloon’s proximal and distal RO markers are not completely within the covered
(graft fabric) portion of the prosthesis.
Note: Use caution when inflating the balloon, especially with calcified, tortuous, stenotic, or otherwise diseased vessels. Inflate
slowly. It is recommended that a backup balloon be available.
Note: The Reliant stent graft balloon catheter is recommended for use with the Valiant Navion thoracic stent graft system. No
data are available for the use of other balloon catheters in remodeling stent grafts.
10.11. Implanting additional configurations
If 2 or more Valiant Navion thoracic stent graft configurations are required to exclude the lesion, follow the steps below. Refer
to Table 9 for order of deployment.
Caution: The proximal end of a FreeFlo stent graft should never be placed inside the fabric-covered section of another graft as
doing so may result in abrasion of the fabric by the bare stent, resulting in graft material holes or broken sutures.
Caution: Failure to provide sufficient overlap may result in the separation of stent graft components.
Caution: Do not use stent grafts shorter than 90 mm at an unsupported joint or to connect 2 previously placed stent grafts.
Note: In vitro durability (fatigue) testing suggests that the long-term durability of the device may be compromised in conditions
with excessive device oversizing or deformation associated with cardiac and respiratory cycles. Wire fractures may have
unknown clinical consequences, which may include, but are not limited to, device migration, vessel perforation, loss of
aneurysm exclusion, false lumen enlargement, or death.
1. Refer to Section 10.3 (Preparation of the Valiant Navion thoracic stent graft system).
2. Refer to Section 10.4 (Introducing the delivery system). Advancement of the delivery system within the previously
implanted stent graft must be carefully monitored under fluoroscopy to ensure that the implanted stent graft does not move.
3. Refer to Section 10.5 (Positioning the delivery system).
4. Refer to Section 10.6 (Confirming stent graft position). Radiographically verify that the distal marker on the proximal graft
aligns with the mid-marker (between the third and fourth covered stents) on the distal graft to achieve the minimum overlap
distance, except when using a stent graft that is shorter than 90 mm. Refer to Figure 9, Figure 15, and Figure 16. Also,
verify that the markers on the additional stent graft indicate that the proximal and distal ends of the covered stent graft are
at the desired locations.
Instructions for Use English 45
Page 48

5. If using a stent graft that is shorter than 90 mm to extend proximal stent graft coverage, deploy the proximal graft material
1
2
4
3
1
3
4
2
1
1
4
3
4
3
2
2
edge of the stent graft no more than 10 mm proximal to the graft material edge of the adjacent stent graft. To extend
proximal landing zone coverage more than 10 mm, use a stent graft with a covered length of ≥90 mm. The most proximal
stent graft must meet the landing zone requirements for either FreeFlo (≥20 mm) or CoveredSeal (≥25 mm).
6. If using a stent graft that is shorter than 90 mm to extend distal stent graft coverage, deploy the distal graft material edge of
the stent graft no more than 10 mm distal to the graft material edge of the adjacent stent graft. To extend distal landing
zone coverage more than 10 mm, use a stent graft with a covered length of ≥90 mm. The most distal stent graft must meet
the distal landing zone requirement (≥20 mm). Refer to Section 6.1 (Patient selection).
7. Refer to Section 10.7 (Deploying the Valiant Navion thoracic stent graft).
8. Refer to Section 10.8 (Deploying tip capture mechanism).
9. Refer to Section 10.9 (Removing the delivery system).
10. Refer to Section 10.10 (Smoothing stent graft fabric and modeling the stent graft).
Figure 15. Alignment of additional sections (first graft placed proximally)
Figure 16. Alignment of additional sections (first graft placed distally)
1. Proximal RO marker
2. RO mid-marker
3. Minimum required overlap
4. Distal RO marker
10.12. Angiogram
Upon completing the implant procedure, perform angiography to verify stent graft apposition, seal, and any endoleaks at the
proximal and distal ends of the stent graft. Assess the stent graft for mid-graft and graft junction endoleaks.
46 Instructions for Use English
Page 49

Perform adjunctive maneuvers as needed, such as ballooning or insertion of additional devices. The most reliable course of
endoleak management (Type I or Type III) is remodeling the stent graft with a balloon and, if needed, placing an additional stent
graft (Section 10.10 and Section 10.11). A minor leak that does not seal after reballooning may seal spontaneously within
several days. If any adjunctive maneuvers are conducted, perform a final angiogram to confirm successful exclusion of the
lesion.
Caution: Do not use a balloon catheter to treat aortic dissection.
Caution: High pressure injections at the edges of the Valiant Navion thoracic stent graft immediately after implantation may
cause acute endoleaks.
Caution: Any endoleak left untreated during the implantation procedure must be carefully monitored after implantation.
10.13. Entry site closure
Remove all remaining accessories (for example, guidewire, introducer sheath, or angiogram catheter). Close the arteriotomy
site by standard surgical closure techniques.
11. Troubleshooting techniques
In the unlikely event of delivery system failure, the following bail-out techniques may be used.
11.1. Partial stent graft deployment
If partial stent graft deployment due to graft cover severance occurs, a screw gear handle disassembly technique may permit
successful deployment of the stent graft.
1. Use a scalpel or other sharp cutting tool to cut the front grip.
2. Slice the gray front grip along one of the grooves (Figure 17). Use caution to avoid cutting the strain relief and the graft
cover tubing underneath the front grip.
Figure 17. Slicing the front grip
1. Front grip
2. Screw gear
3. Remove the front grip from the screw gear and discard. Move the inner strain relief tube away from the screw gear to
improve access to the graft cover tube.
4. Activate the trigger and move the slider handle to the back of the screw gear. This will allow greater screw gear separation
and better access to the graft cover tube.
Note: Since the graft cover is severed, the slider can be retracted without further deploying the stent graft.
5. Separate the 2 screw gear halves in order to identify where the graft cover is severed.
Note: Stabilize the delivery system screw gear. Ensure that the screw gear is not inadvertently pushed or pulled during
manual deployment. Moving the screw gear could inadvertently cause the stent graft to move from its partially deployed
location.
6. Grip the graft cover manually or with hemostats and retract until the stent graft is fully deployed (Figure 18).
Instructions for Use English 47
Page 50

Figure 18. Gripping the graft cover
1. Inner strain relief
2. Screw gear
3. Graft cover
4. Slider handle
7. Continue to hold the screw gear stationary and deploy the tip capture release mechanism per Section 10.8 (Deploying the
tip capture mechanism).
Caution: Use fluoroscopy to carefully monitor any delivery system movement and the retrieval of the delivery system's
tapered tip. The use of fluoroscopy will ensure that the delivery system does not inadvertently cause the stent graft to move
from its deployed location.
8. Grip the screw gear and withdraw the system from the patient.
11.2. Nonrelease of tip capture mechanism
If nonrelease of the tip capture mechanism occurs, a rear grip handle disassembly technique may permit the successful
deployment of the proximal stent.
1. Ensure the delivery system remains stationary and continue to monitor stent graft position.
2. Slice the rear blue grip along one of the grooves and remove from the back end (Figure 19).
Figure 19. Slicing the rear grip
3. Use tweezers to release the tabs (Figure 20) and separate the 2 gray halves underneath the blue grip (Figure 21).
48 Instructions for Use English
Page 51

Figure 20. Releasing the handle halves
1. Tabs
Figure 21. Separate the handle halves
1. Clamping ring
2. Tab
4. Rotate the clamping ring clockwise until the slot aligns with the tab on the screw gear. Remove the back-end lock by sliding
it off the screw gear (Figure 22).
Figure 22. Removing the back-end lock
5. Spread the screw gear halves apart to gain access to the delivery system inner lumens (Figure 23).
Instructions for Use English 49
Page 52

Figure 23. Spreading the screw gear halves
6. Using a hemostat, grip the guidewire tube adjacent to the winged tip-release fitting. Using another hemostat, grip the
broken outer lumen adjacent to the end of the tube (Figure 24).
Figure 24. Gripping the guidewire tube (right) and tip capture tube (left)
1. Capture (outer) tube
2. Tip-release fitting
3. Guidewire tube
7. To release the proximal stent, hold the guidewire tube stationary and pull back the tip capture tube until the proximal stent
is fully released from the tip capture mechanism. Observe the proximal stent release under fluoroscopy and confirm that
the stent graft has been completely deployed.
8. Hold the delivery system with one hand on the front grip and the other hand on the slider. Pull back the trigger and hold the
slider stationary while bringing the front grip towards the slider as depicted in Removing the delivery system (Figure 14).
9. Gently remove the delivery system while maintaining backwards tension on the guidewire lumen to keep the tapered tip
seated within the graft cover. Use fluoroscopy to ensure that the stent graft does not move during the withdrawal.
12. Follow-up imaging recommendations including MRI safety information
12.1. General
All patients should be advised that endovascular treatment requires lifelong, regular follow-up to assess their health and the
performance of their endovascular graft. Patients with specific clinical findings (such as, endoleaks, enlarging aneurysms,
enlarging false lumens, or changes in the structure or position of the endovascular graft) should receive additional follow-up.
Patients should be counseled on the importance of adhering to the follow-up schedule, both during the first year and at yearly
intervals thereafter. Patients should be informed that regular and consistent follow-up is a critical part of ensuring the ongoing
safety and effectiveness of endovascular treatment of thoracic aortic lesions. This includes aneurysms, saccular aneurysms,
penetrating atherosclerotic ulcers, dissections, and BTAIs. Physicians should evaluate patients on an individual basis and
prescribe follow-up relative to the needs and circumstances of each individual patient.
Annual imaging follow-up may include chest X-ray and computed tomography angiogram (CTA), with and without contrast.
■
The combination of contrast and noncontrast CT imaging provides information on aneurysm diameter change, endoleak,
patency, tortuosity, progressive disease, fixation length, and other morphological changes.
■
The chest X-rays provide information on device integrity (separation between components and stent fracture).
50 Instructions for Use English
Page 53

Table 50 lists the recommended imaging follow-up for patients with the Valiant Navion thoracic stent graft. Ultimately, it is the
physician's responsibility, based on previous clinical results and the overall clinical picture, to determine the appropriate imaging
schedule for a particular patient.
Table 50. Imaging recommendations
Visit Imaging Modality
Pretreatment
1
X (optional)
Angiogram
CTA/MRA
1
X
2,3
Chest X-ray
2
Treatment X
1 Month
6 Month
12 Month (Annually thereafter)
1
Pre-treatment assessment should be done within 3 months before treatment.
2
A 6-month follow-up with CT Scan and Chest X-ray is recommended if an endoleak is reported at 1 month after the proce-
4
X
4
X
4
X
X
X
X
dure.
3
Magnetic resonance angiogram (MRA) may be used in patients with impaired renal function or intolerance to contrast media
4
If a Type I or III endoleak is present, prompt intervention and additional follow-up post-intervention is recommended.
12.2. Angiographic imaging
Angiographic images are recommended at pretreatment (within 3 months of implant) for centers without CTA 3D reconstruction
capabilities to assist in determining anatomic suitability. Angiographic images are also recommended during the treatment to
evaluate anatomy and device placement.
12.3. CTA images
CTA images are recommended pretreatment (within 3 months of implant) to determine anatomic suitability for the
Valiant Navion thoracic stent graft. CTA with 3D reconstruction is recommended in order to accurately assess the patient’s
anatomy. The physician determines the required preoperative care for patients with allergies to contrast or who have impaired
renal function.
CTA images are also recommended posttreatment for lesion and device assessment. The triphasic imaging protocol for followup CT should consist of an unenhanced, contrast-enhanced, and 5-minute delay scan. Refer to Table 51 (CTA imaging
guidelines) for optimal CTA results.
■
Film sets should include all sequential images at the lowest possible slice thickness (<3 mm). Do not perform large slice
thickness (>3 mm) or omit consecutive CT images or films sets, as this prevents precise anatomical and device
comparisons over time.
■
Both noncontrast and contrast runs are required, with matching or corresponding table positions.
■
Precontrast and contrast run slice thicknesses and intervals must match.
■
Do not change patient orientation or relandmark the patient between noncontrast and contrast runs.
Noncontrast and contrast-enhanced baseline and follow-up imaging are important for optimal patient surveillance. Table 51 lists
examples of accepted imaging protocols.
Table 51. CTA imaging guidelines
Injection volume (cc or mL) 100–150
Injection rate (cc/sec or mL/sec) 3–4 via 20G IV or larger (4–5 for obese pts >220 lbs (99.8 kg))
Bolus timing SmartPrep, carebolus, or equivalent
Scan range Thoracic inlet to aortic bifurcation
Scan diameter (FOV) Large
DFOV (cm) 24–30
Scan type Helical
Rotation speed (sec) 0.8
Slice thickness (mm) ≤2.5
Scan mode HS
Table speed (mm/rot) 15
Interval (mm) 1
kVp 120
mA 120 for Noncontrast/200 for contrast portion of study
Reconstruction (mm) 1 (Normal body habitus) to 2 (>220 lbs (99.8 kg))
Instructions for Use English 51
Page 54

12.4. X-ray
Chest X-rays may be used to assess device integrity such as stent graft fracture or separation between components.
Posterior/Anterior (PA) and lateral images are recommended for visualizing the stent graft. Ensure the entire device is captured
on images for device assessment.
12.5. MRI safety information
Patients with impaired renal function (that is, renal insufficiency) may also be considered for magnetic resonance imaging (MRI)
or angiography (MRA) at the discretion of the physician. Artifact may occur related to the stent, and care should be used to
ensure adequate imaging of the outer aortic wall to assess TAA or false lumen size. Volume measurement may be helpful if the
aneurysm or false lumen is not clearly shrinking. If there are concerns regarding imaging of calcified areas, fixation sites, or the
outer wall of the aneurysm sac or false lumen, adjunctive CT without contrast may be needed.
Nonclinical testing has demonstrated that the Valiant Navion thoracic stent graft is MR Conditional. A patient with this device
can be safely scanned in an MR system meeting the following conditions:
■
Static magnetic field of 1.5 and 3.0 tesla only
■
Maximum spatial field gradient of 2,000 gauss/cm (20 T/m)
■
Maximum MR System reported, whole-body-averaged specific absorption rate (SAR) of 4 W/kg (First Level Controlled
Mode)
Under the scan conditions defined above, the Valiant Navion thoracic stent graft is expected to produce a maximum
temperature rise of 2.8°C after 15 minutes of continuous scanning.
In nonclinical testing, the image artifact caused by the device extends approximately 6 mm from the Valiant Navion thoracic
stent graft when imaged with a gradient echo pulse sequence and a 3.0 Tesla MRI system. The artifact does not obscure the
device lumen.
12.6. Supplemental imaging
Note: Additional radiological imaging may be necessary to further evaluate the stent graft in situ based on findings revealed by
previous imaging assessments. The following recommendations may be considered.
■
If there is evidence of poor or irregular position of the stent graft, severe angulation, kinking, or migration of the stent graft
on chest X-rays, a spiral CT should be performed to assess lesion size and the presence or absence of an endoleak.
■
If a new endoleak or increase in lesion size is observed by spiral CT, adjunctive studies such as 3D reconstruction or
angiographic assessment of the stent graft and native vasculature may be helpful in further evaluating any changes of the
stent graft or lesion.
■
Spiral CT without contrast, MRI, or MRA may be considered in select patients who cannot tolerate contrast media or who
have renal function impairment. For centers with appropriate expertise, gadolinium or CO2 angiography may be considered
for patients with renal function impairment requiring angiographic assessment.
13. Additional surveillance and treatment
Additional endovascular repair or open surgical aneurysm repair should be considered for patients with evidence of enlarged
aneurysm (>5 mm), endoleak, migration, inadequate seal zone, false lumen enlargement, or fracture. Consideration for
reintervention or conversion to open repair should include the attending physician’s assessment of an individual patient’s
comorbidities, life expectancy, and the patient’s personal choices. Patients should be counseled that subsequent reintervention
may become necessary following an endograft procedure. This may include catheter-based or open surgical conversion.
14. Device Registration
The Valiant Navion thoracic stent graft system is packaged with additional specific information which includes the following:
■
Temporary Device Identification Card that includes both patient and stent graft information. Physicians should complete
this card and instruct the patient to keep it in their possession at all times. The patients should refer to this card anytime
they visit additional healthcare practitioners, particularly for an additional diagnostic procedure (for example, MRI). This
temporary identification card should only be discarded when the permanent identification card is received.
■
Device Tracking Form to be completed by the hospital staff and forwarded to Medtronic for the purposes of tracking all
patients who received a Valiant Navion thoracic stent graft (as required by Federal Regulation). The hospital's submission
of the device tracking form to Medtronic is also required for a patient to receive the permanent identification card.
Upon receipt of the completed Device Tracking Form, Medtronic will mail the patient a Permanent Device Identification Card.
This card includes important information regarding the implanted stent graft. Patients should refer to this card anytime they visit
healthcare practitioners, particularly for any diagnostic procedures (eg, MRI). Patients should carry this card with them at all
times. If a patient does not receive their permanent device identification card, or requires changes to the card, call
1-800-551-5544. In addition, a patient information booklet (PIB) will be provided to the physicians during training and additional
copies will be available upon request. The PIB will also be available online on the Medtronic website (www.medtronic.com).
This booklet provides patients with basic information on lesions of the descending aorta and endovascular repair therapy.
52 Instructions for Use English
Page 55

15. Disclaimer of warranty
ALTHOUGH THE MEDTRONIC VALIANT NAVION THORACIC STENT GRAFT SYSTEM HAS BEEN MANUFACTURED
UNDER CAREFULLY CONTROLLED CONDITIONS, MEDTRONIC, INC., MEDTRONIC VASCULAR, INC. AND THEIR
RESPECTIVE AFFILIATES (COLLECTIVELY “MEDTRONIC”) HAVE NO CONTROL OVER THE CONDITIONS UNDER
WHICH THIS PRODUCT IS USED. THE WARNINGS CONTAINED IN THE PRODUCT LABELING PROVIDE MORE
DETAILED INFORMATION AND ARE CONSIDERED AN INTEGRAL PART OF THIS DISCLAIMER OF WARRANTY.
MEDTRONIC, THEREFORE, DISCLAIMS ALL WARRANTIES, BOTH EXPRESSED AND IMPLIED, WITH RESPECT TO THE
PRODUCT, INCLUDING, BUT NOT LIMITED TO, ANY IMPLIED WARRANTY OF MERCHANTABILITY OR FITNESS FOR A
PARTICULAR PURPOSE. MEDTRONIC SHALL NOT BE LIABLE TO ANY PERSON OR ENTITY FOR ANY MEDICAL
EXPENSES OR ANY DIRECT, INCIDENTAL, OR CONSEQUENTIAL DAMAGES CAUSED BY ANY USE, DEFECT, FAILURE,
OR MALFUNCTION OF THE PRODUCT, WHETHER A CLAIM FOR SUCH DAMAGES IS BASED UPON WARRANTY,
CONTRACT, TORT, OR OTHERWISE. NO PERSON HAS ANY AUTHORITY TO BIND MEDTRONIC TO ANY
REPRESENTATION OR WARRANTY WITH RESPECT TO THE PRODUCT.
The exclusions and limitations set out above are not intended to, and should not be construed so as to, contravene mandatory
provisions of applicable law. If any part or term of this disclaimer of warranty is held to be illegal, unenforceable, or in conflict
with applicable law by a court of competent jurisdiction, the validity of the remaining portions of this disclaimer of warranty shall
not be affected, and all rights and obligations shall be construed and enforced as if this disclaimer of warranty did not contain
the particular part or term held to be invalid.
Instructions for Use English 53
Page 56

Medtronic, Inc.
*M982748A001*
710 Medtronic Parkway
Minneapolis, MN 55432
USA
+1 763 514 4000
www.medtronic.com
US CUSTOMER SERVICE / PRODUCT INQUIRIES:
Tel: (+1-800) 961-9055
© 2018 Medtronic
M982748A001 Rev. 1B
2018-10-19
 Loading...
Loading...