
Micra™ AV
Transcatheter Pacemaker
Patient Manual
Caution: Federal law (USA) restricts this device to sale by or on
the order of a physician.

We are there when you need us.
The following list includes trademarks or registered trademarks of Medtronic in
the United States and possibly in other countries. All other trademarks are the
property of their respective owners.
CareLink, Medtronic, Medtronic CareLink, SureScan

Information about you and your pacemaker
Your personal information
Your name
Your doctor’s name
Specialty Phone
Your doctor’s name
Specialty Phone
Your medications
Emergency contact information
Name/address/phone
Name/address/phone
3

Your pacemaker information
Type or model of pacemaker
Serial #
Date of implant
Hospital where implanted
4

How to contact Medtronic
Contact us by phone
Our Patient Services group can answer any questions or concerns
about your pacemaker. To speak with a Patient Services Specialist,
call 1-800-551-5544. Our sta is available Monday through Friday from
7:00 AM to 6:00 PM (Central Time).
Contact us online
For up-to-date information about your pacemaker, visit:
• Medtronic website: www.medtronic.com
• Patient Services website: www.medtronic.com/rhythms
To submit questions, suggestions, or requests, use the online form at
www.medtronic.com/us-en/about/contact-us.html.
5

Contact us by mail or fax
Medtronic Inc.
Patient Services Department
Mail Stop MVS 14
8200 Coral Sea Street NE
Mounds View, MN 55112
Fax: (763) 367-5809
Contacting Medtronic about your ID Card
To update information on your ID card or if you have questions about your
ID card, see “Your pacemaker ID card” on page 80.
6

Contents
Chapter 1
Introduction 13
Chapter 2
Frequently asked questions 15
Chapter 3
Your heart has a natural rhythm 23
The anatomy of the heart 24
Electrical conduction in the heart 27
The heart is very sensitive to the body’s needs 29
How abnormal heart rhythms aect the heart 29
Bradycardia 30
7

Chapter 4
About your pacemaker 35
What is a pacemaker? 36
What is a transcatheter pacemaker, and how is it dierent from other
pacemakers? 36
What are the components of my pacemaker? 39
How does a pacemaker work? 40
What is pacing, and what does it feel like? 41
What types of pacing can my pacemaker provide? 41
AV synchronous pacing 42
Fixed rate pacing 42
Rate-responsive pacing 42
Chapter 5
Your implant procedure and recovery 45
The implant procedure 46
How the procedure is done 46
Potential risks after the implant procedure 46
Recovering after your implant procedure 47
8

When to call your doctor or nurse 48
Follow-up appointments 49
Chapter 6
Living life with your pacemaker 51
Food and medications 51
Your physical activity 52
Recreation and activities 52
Driving a car 53
What you need to know about electromagnetic compatibility (EMC) 53
Proper grounding of electrical items 55
Avoiding interference from electrical or magnetic items 56
Household and recreational items 56
Communications and electronics 61
Tools and industrial equipment 68
Industrial equipment that may require special precautions 69
Vehicles and related items 70
Security systems 72
Mechanical interference 73
9

Precautions about medical procedures 74
Medical procedures that are not recommended 74
Medical procedures that require some precautions 75
Acceptable medical procedures 78
Chapter 7
Registering your pacemaker 79
Pacemaker registration 79
Your pacemaker ID card 80
Keep your pacemaker ID card with you all the time 80
Requesting a new ID card or updating personal information 81
If you change your doctor 81
Medtronic pacemaker travel card 82
Chapter 8
Follow-up care 83
Follow-up appointments 83
Reviewing information saved by your pacemaker 84
Remote monitoring 84
10

Medtronic programmer 85
Pacemaker replacement 86
Chapter 9
Caring for yourself 87
Dealing with anxiety and getting support 88
Shaping a positive attitude about life with your heart device 89
Medical care 90
Planning for an emergency 90
What your family and friends should know 91
Glossary 93
Medtronic Warranty 103
Index 105
11

12
Introduction
1
This manual is for people who are about to receive or already have a
Medtronic Micra AV transcatheter pacemaker. This manual describes
your pacemaker and its therapies. It also explains the implant procedure
and what you can expect afterward. Encourage your family and
caregivers to review this manual.
If you have questions about your pacemaker that are not covered in this
manual or you want more information about your pacemaker, contact
Medtronic Patient Services (see page 5).
Your doctor or doctors should be your rst source of information about
your heart condition and your general health.
Words in bold are dened in the glossary starting on page 93.
13
Why read this manual?14

Frequently asked questions
2
New patients often have the same concerns about their pacemakers.
Here are some of the questions new patients often ask.
Why do I need this pacemaker?
A pacemaker is designed to relieve symptoms of a slow heart rate. This
condition is called bradycardia. The heart beats at 60 beats per minute
or less during normal activities. A pacemaker improves the heart’s ability
to pump blood and oxygen to the body.
This pacemaker does not prevent or cure your heart condition. However,
it should improve your quality of life. Based on your health condition,
your doctor has determined that a pacemaker may help to improve your
symptoms.
Although your pacemaker is not a cure, it does help to protect you from
heart rhythms that can weaken or even endanger your health. Many
patients say that this pacemaker gives them and their families a sense of
security.
15

Who should not receive this pacemaker?
Patients who already have an implanted medical device or certain health
conditions may not be eligible. Ask your doctor if this pacemaker is right for
you.
Is it safe for me to have an MRI scan?
A magnetic resonance imaging (MRI) scan is a type of diagnostic that
creates an internal view of the body.
The energy elds present during an MRI scan may harm a traditional
pacemaker, which could endanger a patient’s health. However, your
SureScan pacemaker was designed to reduce these risks to a very low
level.
You can safely have an MRI scan if you meet the eligibility requirements
that Medtronic provides to your heart doctor.
Before you receive an MRI scan, tell the doctor that you have a pacemaker.
Show them your ID card. Your doctor will verify that you are eligible and that
your pacemaker is functioning properly. Your doctor will then turn on the
SureScan feature.
During the MRI scan, you are monitored to ensure your safety.
After the MRI scan, your doctor will turn o the SureScan feature.
Why read this manual?16

If you wonder if you can have an MRI scan, contact your doctor or nurse.
If any of your doctors have questions, they should contact a Medtronic
representative or Medtronic Technical Services. See page 5.
Will I be able to drive?
Whether you will be able to drive depends on your individual heart condition.
Many people with pacemakers can resume driving if their doctors approve
and if allowed by the laws and insurance regulations in their states. For
more information, see ”Driving a car” on page 53. If you have concerns,
talk with your doctor.
Will I be able to travel?
You should be able to travel if you follow your doctor’s instructions.
Wherever you travel, your pacemaker monitors your heart. It provides
pacing when you need it.
If your pacemaker triggers the security gates at airports or other secure
buildings, present your pacemaker ID card. If a security operator is
using a handheld screening wand, ask the operator not to hold it over
your pacemaker or wave the wand back and forth over your pacemaker.
Directions on how to safely scan your pacemaker are available in several
languages on a pacemaker travel card. This card is especially useful for
international travel. See page 82 for information on how to request one.
Chapter 2 17

Can I walk through antitheft systems found in public places?
Yes, simply walk through the antitheft system at a normal pace. If you
stop near them, the systems in stores, libraries, and other places may
temporarily interfere with your pacemaker. The interference stops when you
move away from the equipment.
Can I use a mobile phone?
Yes. However, mobile phones, including cellular phones and other wireless
phones, may cause electrical interference with your pacemaker when the
phone is turned on and held too close to your pacemaker.
Some accessories, such as earbuds or cases with magnets, may also
interfere with your pacemaker. Any eect is temporary. If you move the
phone or the accessory away, the pacemaker will return to its previous
state of operation. To avoid interference with your pacemaker, keep mobile
phones and their accessories at least 6 inches (15 centimeters) away from
your pacemaker. Do not carry your mobile phone close to your pacemaker,
such as in a shirt pocket.
For more information about using mobile phones and other wireless
communication devices, see ”Avoiding interference from electrical or
magnetic items” on page 56.
Why read this manual?18

Can I use a microwave oven and other electrical items?
Yes, you can use a microwave oven as well as major appliances, electric
blankets, and heating pads. See “Living life with your pacemaker” on
page 51 for information about electrical items and any restrictions or
cautions you should know about.
Will my pacemaker need to be replaced?
Yes. Your pacemaker uses a battery sealed inside the pacemaker. When
the battery power falls to a low level, you will need a new pacemaker. The
pacemaker battery typically lasts 7 to 12 years.
How long your battery lasts depends on several factors, including the nature
of your heart condition and how often your pacemaker provides therapy to
your heart.
The battery power is checked at each follow-up appointment. Your doctor or
nurse will let you know when you need a new pacemaker.
How often will my doctor need to check my pacemaker?
Your rst appointment is usually scheduled about 1 month after your
implant. Additional appointments are scheduled every 3 to 6 months. How
often they are scheduled depends on your doctor’s practice and your
medical condition.
Chapter 2 19

For more information, see ”Follow-up appointments” on page 83.
How do I know if my pacemaker battery is still working?
Your battery is checked during your follow-up appointments. The battery is
sealed inside your pacemaker and cannot be recharged. You will need a
new pacemaker when the battery power is low. For more information, see
“Pacemaker replacement” on page 86.
Can I have sexual relations?
Most people resume sexual activity, based on their doctor’s instructions.
How are my pacemaker and data secured?
Your pacemaker has built-in safeguards that protect your pacemaker and
your device data from cyber attacks. Specialists in patient safety work with
the Micra team to design and deliver pacemakers that are secure. Also, the
therapies provided by your pacemaker can only be programmed by your
doctor or nurse during an oce visit.
Why read this manual?20

Chapter 2 21

Why read this manual?22

Your heart has a natural rhythm
3
This chapter describes the anatomy of the heart and one common
abnormal heart rhythm condition. To understand how your pacemaker
works, you need to know how the heart functions and how abnormal heart
rhythms can aect the heart.
This chapter includes these topics:
• The anatomy of the heart (see page 24)
• Electrical conduction in the heart (see page 27)
• How abnormal heart rhythms aect the heart (see page 29)
23

The anatomy of the heart
The heart is a st-sized pump that circulates blood throughout the body.
Arteries carry blood with oxygen and nutrients to all parts of the body.
Veins carry blood depleted of oxygen and nutrients back to the heart.
The heart is a large, hollow muscle divided into four chambers. The two
upper chambers are the right atrium and the left atrium. Atria, the plural
of atrium, refers to both the right atrium and the left atrium.
The lower chambers of the heart are the right ventricle and the left
ventricle. The septum is the muscled wall dividing the right and left sides
of the heart.
The right atrium draws blood in from the body and pumps it into the right
ventricle. The right ventricle then pumps the blood into the lungs to be
reoxygenated. The left atrium draws oxygen-rich blood in from the lungs
and pumps it into the left ventricle. The left ventricle then pumps the blood
out to the rest of the body.
Each chamber contracts by squeezing its muscles together. Each
contraction pushes blood from one chamber to the next chamber or
out into the body. Heart valves regulate the ow of blood between each
Your heart has a natural rhythm24

chamber and keep the blood owing in one direction. What we hear as a
heartbeat is actually the opening and closing of the valves.
After each chamber contracts completely, pushing out most of the
blood, it relaxes and lls with more blood again. In a healthy heart, each
chamber contracts in a coordinated eort with the other chambers of the
heart. See Figure 1.
Chapter 3 25

Right atrium
Left atrium
Left ventricle
Right ventricle
Septum
Figure 1 . Four chambers of the heart contract in a controlled sequence
to circulate blood throughout the body.
Your heart has a natural rhythm26

Electrical conduction in the heart
Electrical impulses cause the cells of the heart to contract and relax. The
sinoatrial node (or SA node) generates these impulses. The SA node is
found on the upper inside wall of the right atrium.
When the SA node releases an electrical impulse, the impulse travels
across the top of the atria and down through the atria. The atria
contract from the top down, pushing blood into the ventricles. When the
electrical impulse reaches the lower wall of the atria, it stimulates the
atrioventricular node (or AV node). The AV node delays the impulses
just long enough for the atria to nish pushing blood into the ventricles.
Then it passes the impulse along organized thread-like paths into the
ventricles. See Figure 2.
Chapter 3 27
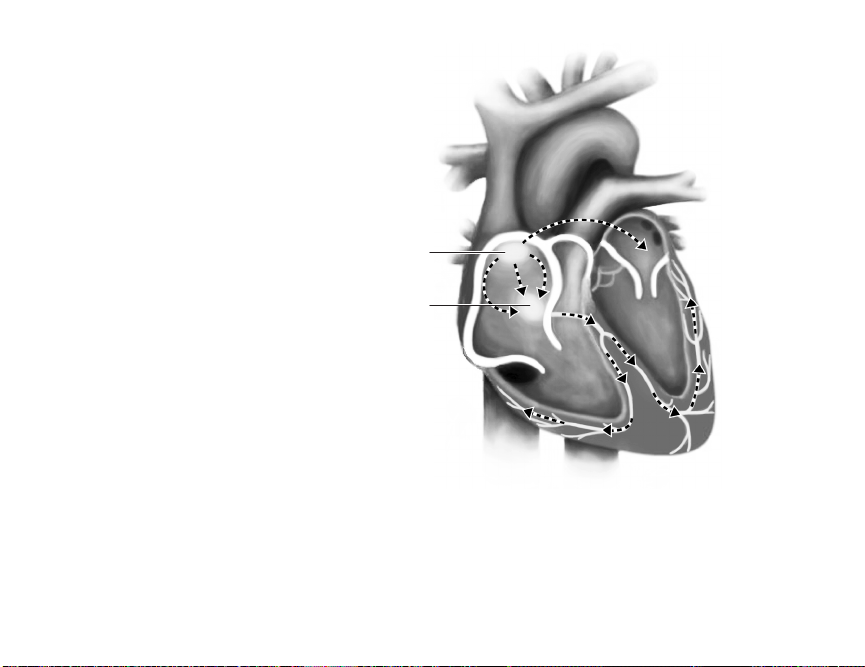
Sinoatrial (SA) node
Atrioventricular (AV) node
Figure 2. The electrical impulses that cause the heart to contract start
at the SA node and move through the atria to the AV node. The AV node
controls when the impulse is released to travel through the ventricles.
Your heart has a natural rhythm28

The AV node controls how quickly the impulse travels through the rest of
the heart. The proper coordination between the contracting chambers of
the heart maintains adequate blood ow between the heart and the rest of
the body.
The electrical impulse then travels to the bottom of the ventricles. The
impulse sweeps across the surface of the ventricles from the bottom up,
causing the ventricles to contract from the bottom up. This action pushes
the blood out of the valves into the lungs (from the right ventricle) and to
the rest of the body (from the left ventricle).
The heart is very sensitive to the body’s needs
The brain and the autonomic nervous system control how fast the
chambers of the heart contract.
For example, if you start to jog instead of walk, your body’s demand for
blood increases. Your heart automatically contracts faster when you are
active to supply more blood to your body.
How abnormal heart rhythms aect the heart
Disease, defect, or injury can cause the heart’s conduction system to
become unreliable. The areas that control heart rhythm can malfunction,
Chapter 3 29

causing slow, fast, erratic, or uncoordinated heart rhythms. These
abnormal heart rhythms aect the amount of blood supplied to the body.
The eects of abnormal heart rhythms can range from severe fatigue to
sudden cardiac arrest (SCA).
When the heart is not beating normally because of a problem with
its conduction system, the problem may be bradycardia, a common
abnormal heart rhythm condition.
This condition can be treated with medications or by implanting a
pacemaker. Sometimes it is treated with both methods. Your pacemaker
can treat bradycardia.
Bradycardia
Bradycardia is a slower than normal heart rate, usually less than 60 beats
per minute. The heart cannot pump enough blood to the body to support
daily activities or mild exercise. See Figure 3.
Your heart has a natural rhythm30
 Loading...
Loading...