Page 1

Medtronic Integrity Coronary Stent System
INSTRUCTIONS FOR USE
CAUTION: Federal (USA) law restricts this product for sale by or on the order of a physician.
Page 2

Page 3

Integrity Coronary Stent System
Instructions for Use
Table of Contents
1.0 DEVICE DESCRIPTION...................................................................................................................... 2
2.0 INDICATIONS FOR USE..................................................................................................................... 3
3.0 CONTRAINDICATIONS...................................................................................................................... 3
4.0 WARNINGS AND PRECAUTIONS....................................................................................................3
5.0 POTENTIAL ADVERSE EVENTS ..................................................................................................... 5
6.0 INDIVIDUALIZATION OF TREATMENT....................................................................................... 5
7.0 PATIENT COUNSELING .................................................................................................................... 6
8.0 HOW SUPPLIED ................................................................................................................................... 6
9.0 DIRECTIONS FOR USE ...................................................................................................................... 7
10.0 IMAGING GUIDELINES ................................................................................................................. 14
12.0 SUMMARY OF CLINICAL STUDY............................................................................................... 15
DISCLAIMER OF WARRANTY ............................................................................................................ 25
1
Page 4

1.0 DEVICE DESCRIPTION
The Medtronic Integrity Coronary Stent System (Integrity Stent) consists of a
balloon-expandable intracoronary stent pre-mounted on either the MicroTrac Rapid
Exchange (RX) or MicroTrac Over-the-Wire (OTW) stent delivery system. The
balloon delivery system has two radiopaque markers to aid in the placement of the
stent during fluoroscopy. The Integrity Stent is manufactured from a cobalt alloy and
is formed from a single wire bent into a continuous sinusoid pattern and then laser
fused back onto itself (Figure 1). The stents are provided in multiple lengths and
diameters. Both delivery systems are compatible with 0.014 inch (0.36mm)
guidewires. The MicroTrac RX (Figure 2) and the MicroTrac OTW (Figure 3)
delivery systems have an effective length of 140cm.
Figure 1. Medtronic Integrity Stent
Figure 2: MicroTrac RX Delivery System (with Stent)
Figure 3: MicroTrac OTW Delivery System (with Stent)
2
Page 5

2.0 INDICATIONS FOR USE
The Integrity Coronary Stent is indicated for improving coronary luminal diameter in
patients with symptomatic ischemic heart disease due to discrete de novo or restenotic
lesions, with reference vessel diameters of 2.25–4.0 mm and ≤30 mm in length, using
direct stenting or predilatation.
3.0 CONTRAINDICATIONS
• Patients in whom antiplatelet and/or anticoagulation therapy is contraindicated.
• Patients who are judged to have a lesion that prevents complete inflation of an
angioplasty balloon or proper placement of a stent or stent delivery system.
4.0 WARNINGS AND PRECAUTIONS
The long-term effects of stents and the risks associated with lifelong carrying of these
implants are unknown. This lack of knowledge should be considered in making a
risk/benefit assessment for the patient prior to implantation.
• The Integrity Coronary Stent System is provided sterile, for one procedure only.
Do not resterilize. Use by the “Use By” date noted on the package.
• Only physicians who have received appropriate training should perform
implantation of the stent. Use of the Integrity Coronary Stent System requires
advanced coronary angioplasty technical skills. The instructions will give
technical guidance, but do not obviate the need for formal training in the use of
the device.
• Patients allergic to cobalt alloy may suffer an allergic reaction to this implant.
• Do not remove the stent from the stent delivery system; the stent can not be
removed and placed on another balloon catheter for deployment.
• Do not try to straighten a kinked shaft or hypotube. Straightening a kinked metal
shaft may result in breakage of the shaft. If the device is kinked, it should not be
used.
3
Page 6

• Significant amounts of air in the balloon may cause uneven expansion of the stent
and difficulty in deployment of the stent. Do not pre-inflate balloon prior to stent
deployment. Use balloon preparation technique described within this instructional
material.
• The Integrity Coronary Stent System does not provide for distal dye injections or
pressure measurements through the guidewire lumen.
• Expansion of the stent should not be undertaken if the stent is not appropriately
positioned in the vessel. If the position of the stent is not optimal, it should not be
expanded. (Refer to section 9.6 “Removal of an Unexpanded Stent”.)
• Incomplete deployment of the stent (i.e., stent not fully expanded) may cause
procedural complications resulting in patient injury.
• Advancement of an Integrity Coronary Stent System through a previously stented
segment may cause procedural complications resulting in patient injury.
• Placement of the stent has the potential to compromise side branch patency.
• Administer appropriate anticoagulant/antiplatelet and coronary artery vasodilator
therapy according to current medical guidelines and manufacturer’s instructions.
• Caution must be taken when using ancillary equipment, such as intravascular
ultrasound catheters, to avoid dislodgement or deformation of the stent.
• When multiple stents are required, stent materials should be of similar
composition. Placing multiple stents of different materials in contact with each
other may increase the potential for corrosion. Data obtained from in vitro
corrosion tests using a Cobalt alloy stent (Medtronic Integrity BMS Coronary
Stent) in combination with a stainless steel alloy stent (Boston Scientific
Liberte™ Coronary Stent) do not suggest an increased risk of in vivo corrosion.
• When using two wires, care should be taken when introducing, torquing and
removing one or both guidewires to avoid entanglement. It is recommended that
one guidewire be completely withdrawn from the patient before removing any
additional equipment.
• Stent placement should only be performed at hospitals where emergency coronary
artery bypass graft surgery can be readily performed.
• Judicious selection of patients is necessary since the use of this device carries the
associated risk of subacute thrombosis, vascular complications and/or bleeding
events. Administration of appropriate anticoagulant, antiplatelet and coronary
vasodilator therapy is critical to successful stent implantation and follow-up.
• Subsequent restenosis may require repeat dilatation of the arterial segment
containing the stent. The long-term outcome following repeat dilatation of
endothelialized coronary stents is unknown at present.
4
Page 7

5.0 POTENTIAL ADVERSE EVENTS
The following complications may be associated with the use of coronary stenting
devices or PTCA:
• Acute myocardial infarction
• Allergic reaction to contrast medium/stent material/medications
• Arrhythmias (including ventricular fibrillation & ventricular tachycardia)
• Arteriovenous fistula
• Bleeding complications
• Cardiac tamponade
• Cerebrovascular accident/stroke
• Death
• Dissection of coronary artery
• Drug reactions
• Embolization (air, stent, tissue or thrombotic)
• Emergency coronary artery bypass graft surgery (CABG)
• Endocarditis
• Failure to deliver the stent
• Stent deformation, collapse or fracture
• Hematoma
• Hemorrhage requiring transfusion
• Injury of the coronary artery
• Myocardial ischemia/infarction
• Pain and tenderness at the insertion site
• Perforation
• Peripheral Ischemia
• Peripheral nerve injury
• Pseudoaneurysm (coronary/femoral/radial)
• Pyrogenic reaction
• Restenosis of the dilated artery or stented segment
• Sepsis/infection
• Short-term hemodynamic deterioration (hypotension/hypertension)
• Stent thrombosis or occlusion
• Total occlusion of coronary artery
• Unstable angina
• Vascular thrombosis
• Vessel dissection/perforation/spasm
6.0 INDIVIDUALIZATION OF TREATMENT
The risks and benefits described above should be carefully considered for each
patient before use of the Medtronic Coronary Integrity Stent System. Patient
selection factors to be assessed should include a judgement regarding risk of
prolonged anticoagulation. Stenting should be generally avoided in those patients at
heightened risk of bleeding (e.g., those patients with recently active gastritis or peptic
ulcer disease, See Contraindications). Each Integrity Stent must be sized appropriate
to fit the patient’s particular coronary anatomy. Proper sizing of the device (diameter
and length) is the responsibility of the physician and it is recommended that the
Integrity Stent cover the stenotic lesion. The risks and benefits previously described
5
Page 8

should be carefully considered for each patient before use of the Integrity Coronary
Stent System (Refer to section 5).
Co-morbidities that increase the risk of poor initial results or the risks of emergency
referral for bypass surgery (diabetes mellitus, renal failure, and severe obesity) should
be reviewed.
Thrombosis following stent implantation is affected by several baseline angiographic
and procedural factors. These include vessel diameter less than 3.0mm, interprocedural thrombosis, poor distal flow, and/or dissection following stent
implantation. In patients that have undergone coronary stenting, the persistence of a
thrombus or dissection is considered a marker for subsequent thrombotic occlusion.
These patients should be monitored very carefully during the first month after stent
implantation.
7.0 PATIENT COUNSELING
The physician should review the risks, benefits and potential adverse events when
counseling the patient about this device and procedure. Medtronic can provide
physicians with a Patient Guide which includes information on Medtronic, Inc., the
implant procedure and Medtronic coronary stents.
The Medtronic Integrity Coronary Stent System is packaged with additional specific
information:
• A Coronary Stent Implant Card that includes patient information, stent
implant information and MRI guidelines. All patients will be instructed to
keep this card in their possession at all times for procedure/stent
identification.
8.0 HOW SUPPLIED
• Package contains one coronary stent pre-mounted on a custom stent delivery
system with its accessories (a compliance chart, and a 29 gauge cannula and
looper). Sterilized by EtO gas diffusion. Sterile, non-pyrogenic in unopened,
undamaged packages. Store at room temperature. Use by the “Use By” date noted
on the package. It is intended for single use only. Do not resterilize.
WARNING: This device is single use. This device is intended to contact body
tissues. Do not reuse, reprocess or resterilize. Reprocessing may compromise the
structural integrity of this device. Reuse of this device creates a potential risk of
patient infections due to contamination. This contamination of the device may lead
to injury, illness or death of the patient.
CAUTION: Should there be damage to the package, do not use.
• The Medtronic Integrity Coronary Stent System is intended to perform as a
system. The Medtronic Integrity Stent is not designed to be crimped onto another
delivery device.
6
Page 9

r
(
k
9.0 DIRECTIONS FOR USE
Carefully inspect the sterile package before opening. It is not recommended that the
product be used after the “Use By” date. If the integrity of the sterile package has
been compromised prior to the product “Use By” date (e.g., damage of the package)
contact your local Medtronic Representative for return information. If the sterile
package appears intact, carefully remove the system from the package and inspect for
bends, kinks and other damage. Verify that the stent is located between the
radiopaque markers. Verify that there is no visible damage to the stent or to the
balloon. Do not use if any defects are noted.
9.1 Selection of Stent Size
Careful stent sizing is important to successful stenting. In general, the stent size
should be chosen to match the diameter of the reference vessel and to correspond
with the length of the lesion. Slight stent oversizing is preferable to undersizing.
CAUTION: The inflated balloon diameter measures slightly larger than the labelled
stent diameter to allow for stent recoil upon expansion.
9.2 Preparation of the Delivery System
Materials Required:
Quantity Material
Appropriate guiding cathete
1 20 cc syringe
Heparinized normal saline
1 0.36mm
0.014 inch) x 180 cm guidewire
1 Rotating hemostatic valve
Contrast medium diluted 1:1 with heparinized normal saline
1 Inflation device
1 Torque device
Optional Three-way stopcoc
• Remove the stent delivery system from the package. Special care must be taken
not to handle the stent or in any way disrupt its placement on the balloon. This is
most important during catheter removal from packaging, placement over
guidewire, and advancement through the rotating hemostatic valve and guiding
catheter hub. Excessive manipulation, e.g., rolling the mounted stent, may cause
dislodgement of the stent from the delivery balloon.
WARNING:
• Should there be movement of or damage to the stent, or to the balloon, do not
use.
• Do not attempt pre-inflation technique to purge balloon lumen.
7
Page 10
• Use only the appropriate balloon inflation media. Do not use air or any
gaseous medium to inflate the balloon as it may cause uneven expansion and
difficulty in deployment of the stent.
• Do not pull negative pressure on inflation device before beginning the
preparation step.
CAUTION:
• Do not put bending force on the stent delivery system when applying
negative pressure with the syringe.
• Do not wipe with gauze sponges as fibers may disrupt the stent.
• Make sure the rotating hemostatic valve has a large bore and is fully open
while passing the stent through it. If resistance is encountered, do not force
passage. Resistance may indicate damage to the stent or the stent delivery
system.
Preparation of Delivery System:
Step Action
1 Prepare the guiding catheter and guidewire according to the manufacturer’s instructions.
Both Medtronic Integrity Stent Delivery Systems (RX and OTW) are compatible with
0.014 inch (0.36mm) guidewire. Refer to product labelling for specific compatibility.
2 Remove the stent delivery system from the package.
3 Remove protective sheath covering from the stent/balloon. Removing the protective
sheath will also remove the stylette. Inspect the stent to assure it has not been damaged
or displaced from its original position on the balloon.
4 Inspect the stent to assure it has not been damaged or displaced from its original position
on the balloon. Verify that the stent is positioned between the proximal and distal balloon
markers. Verify that there is no visible damage to the stent or the balloon.
Note: Should there be movement of or damage to the stent, do not use.
5 Flush Stent Delivery System guidewire lumen with heparinized normal saline in routine
manner.
6 Fill a 20cc syringe with 5cc of contrast/heparinized normal saline mixture (1:1).
7 Attach to delivery system and apply negative pressure for 20-30 seconds.
8 Slowly release pressure to allow negative pressure to draw mixture into the balloon
lumen
9 Detach syringe and leave a meniscus of mixture on the hub of the balloon lumen.
10 Prepare inflation device in standard manner and purge to remove all air from syringe and
tubing.
11 Attach inflation device to catheter directly ensuring no bubbles remain upon connection.
12 Leave on ambient pressure (neutral position). Note: Do not pull negative pressure on
inflation device after balloon preparation and prior to delivering the stent.
13 Moisten the stent with heparinized normal saline by submerging the stent in a sterile
bowl containing the solution.
Note: Do not use gauze sponges to wipe down the stent as fibers may disrupt the stent.
14 Advance the stent delivery system along the guidewire through a large bore rotating
hemostatic valve using conventional angioplasty techniques.
15 Carefully advance the stent delivery system into the hub of the guiding catheter. Do not
deliver the stent system while under negative pressure.
8
Page 11
CAUTION: If resistance is encountered, do not force passage. Resistance may
indicate damage to the stent or stent delivery system.
9.3 Stent Delivery
Delivery Procedure
Step Action
1 Prepare vascular access site according to standard PTCA practice.
2 Pre-dilate the lesion/vessel with appropriate diameter balloon having a ratio of 1:1 with
the diameter of the vessel. This step may be eliminated if direct stenting is performed.
3 Maintain neutral pressure on inflation device. Open rotating hemostatic valve to allow for
easy passage of the stent.
Note: If resistance is encountered, do not force. Resistance may indicate a problem and
may result in damage to the stent if it is forced. Remove and examine the system.
4 Carefully advance the Stent Delivery System into the hub of the guiding catheter. Ensure
guiding catheter stability before advancing the Stent System into the coronary artery.
5 Note: If the physician encounters resistance to the Stent Delivery System prior to exiting
the guiding catheter, do not force passage. Resistance may indicate a problem and may
result in damage to the stent if it is forced. Maintain guidewire placement across the
lesion and remove the Stent Delivery System as a single unit (see Section 9.6 “Removal
of an Unexpanded Stent”
6 Advance delivery system through the guiding catheter to the target lesion under direct
fluoroscopic visualization. Utilize the proximal and distal radiopaque markers on the
balloon as a reference point. Expansion of the stent should not be undertaken if the stent
is not properly positioned in the target lesion. If the position of the stent is not optimal, it
should be carefully removed. (see Section 9.6 “Removal of an Unexpanded Stent”)
7 Optimal stent placement requires the distal end of the stent to be placed approximately
1mm beyond the distal end of the lesion
8 Sufficiently tighten the rotating hemostatic valve. The Stent is now ready to be deployed.
9
Page 12

9.4 Deployment Procedure
Stent Deployment Procedure
Step Action
1 Position the stent across the lesion using the proximal and distal radiopaque markers on the
balloon as a reference point. Optimal placement requires the proximal end of the stent to be
deployed approximately 1mm proximal to the beginning of the target lesion.
2 Prior to stent expansion, utilize high resolution fluoroscopy to verify the stent positioning.
3 Inflate the balloon to the nominal pressure to expand the stent. Refer to the compliance
chart for the proper inflation pressure. The Integrity Stent System may be reinflated without
repositioning, up to rated burst, to assure complete apposition of the stent to the artery wall.
Note: Do not exceed Rated Burst Pressure
4 Maintain inflation pressure for 15-30 seconds for full expansion of the stent.
Note: Under-expansion of the stent may result in stent movement. Care must be taken to
properly size the stent to ensure the stent is in full contact with the arterial wall upon
deflation of the of the balloon
Placement Precautions:
• If the initial guiding catheter position is lost, avoid pulling or pushing the
guiding catheter over the stent. If this is done, the distal end of the guiding
catheter may damage the stent.
• If the stent delivery system does not readily advance, do not force. If the stent
will not advance in spite of good guiding catheter support, consider dilating
proximal obstructing plaque.
• Expansion of the stent should not be undertaken if the stent is not properly
positioned in the stenotic segment of the vessel. If the position of the stent is
not optimal, it should be repositioned or removed. (Refer to Section 9.6
“Removal of an Unexpanded Stent”.)
• Inadequate expansion of the stent may result in stent migration.
• Do not exceed rated burst pressure as indicated on the label and compliance
chart. Use of a higher pressure range than specified on the compliance chart
may result in a ruptured balloon or oversizing of the stent with possible
intimal damage.
• Oversizing of the stent and use of higher than recommended inflation
pressures may cause vessel dissection. It is recommended that the stent size
chosen closely approximate the diameter of the vessel and that recommended
stent inflation pressures be used for stent deployment. If the target lesion is
incompletely stented, use additional stents as necessary to adequately treat
the lesion.
10
Page 13

• Do not prepare or pre-inflate the Stent Delivery System prior to stent
deployment, other than as directed. Use balloon purging technique described
in section 9.2 Preparation of Delivery System.
• Implanting a stent may lead to dissection of the vessel distal and/or proximal
to the stented portion, and may cause acute closure of the vessel requiring
additional intervention (e.g., CABG, further dilatation, placement of
additional stents).
• When treating multiple lesions, the distal lesion should be initially stented,
followed by stenting of the proximal lesion. Stenting in this order obviates
the need to cross the proximal stent with a stent delivery system and reduces
the chances of dislodging the proximal stent.
• Do not expand the stent if it is not properly positioned in the vessel
• Placement of the stent has the potential to compromise side branch patency.
• Stent retrieval methods (use of additional wires, snares and/or forceps) may
result in additional trauma to the coronary vasculature and/or the vascular
access site. Complications can include bleeding, dissection, perforation,
hematoma, pericardial effusion, cardiac tamponade or pseudoaneurysm
Post-Implant– Precautions:
• Care must be exercised when crossing a newly deployed stent with an
intravascular ultrasound (IVUS) catheter, a coronary guidewire, or a balloon
catheter to avoid disrupting the stent geometry.
9.5 Removal Procedure
Step Action
1 Deflate the balloon by pulling negative pressure on the inflation device. Allow adequate
time for full balloon deflation (at least 15 seconds). Longer stents may require more time
for deflation.
2 Open the hemostatic valve to allow removal of the delivery system.
3 Maintain position of the guiding catheter and guidewire to prevent it from being drawn
into the vessel. Withdraw the balloon from the stent maintaining negative suction,
allowing the movement of the myocardium to gently dislodge the balloon from the stent.
4 After removal of the delivery system, tighten the hemostatic valve.
5 Repeat angiography and visually assess the vessel and the stent for proper expansion.
6 A second balloon inflation may be required to ensure optimal stent expansion of the stent.
In such instances, the Integrity Stent System may be reinflated up to rated burst pressure
or a non-compliant, higher-pressure balloon of adequate size (the same size at the Stent
Delivery System balloon or larger) and length may be used to accomplish this.
Note: In smaller or diffusely diseased vessels, the use of high balloon inflation pressure
may expand the vessel distal to the stent and could result in vessel dissection.
Do not exceed Rated Burst Pressure.
7 The final internal stent diameter should be equal to or slightly larger than the proximal and
distal reference vessel diameters.
8 Repeat angiography to evaluate and determine procedure status or termination.
11
Page 14

NOTE: Observation of the patient and angiographic evaluation of the stent site should be
performed periodically within the first 30 minutes after stent placement. If stent
placement is associated with the onset of thrombus or suspected thrombus in the region
of the stented segment, intracoronary infusions of a thrombolytic agent is recommended.
Stent / Delivery System Removal Precautions:
Failure to follow these steps and/or applying excessive force to the Stent Delivery
System can potentially result in loss or damage to the stent and/or Stent Delivery
System components such as the balloon.
• If removal of a stent system is required prior to deployment, ensure that
the guide catheter is coaxially positioned relative to the stent system
and cautiously withdraw the stent system into the guide catheter.
• Should unusual resistance be felt at any time when withdrawing the
stent towards the guide catheter, the Stent Delivery System and the
guiding catheter should be removed as a single unit. This must be
done under direct visualization with fluoroscopy.
• The guiding catheter and the Stent Delivery System should be carefully
removed from the coronary artery as a single unit. When removing the
Stent Delivery System and Guiding Catheter as a single unit:
o Do not retract the Stent Delivery System into the guiding catheter.
o Maintain guidewire placement across the lesion and carefully pull
back the Stent Delivery System until the proximal balloon marker
of the Stent Delivery System is aligned with the distal tip of the
guiding catheter.
o The system should be pulled back into the descending aorta
toward the arterial sheath. As the distal end of the guiding catheter
enters into the arterial sheath, the catheter will straighten,
allowing safe withdrawal of the Stent Delivery System into the
guiding catheter and the subsequent removal of the Stent Delivery
System and the guiding catheter from the arterial sheath.
• Inspect the Stent Delivery System post removal to ensure that the stent is present
on the stent delivery system.
9.6 Removal of an Unexpanded Stent
If removal of a stent system is required prior to deployment, ensure that the guide
catheter is coaxially positioned relative to the stent system and cautiously
withdraw the stent system into the guide catheter. Should unusual resistance be
encountered when withdrawing the stent towards the guide catheter, the stent
system and the guide catheter should be removed as a single unit. This must be
done under direct visualization with fluoroscopy.
12
Page 15

9.7 Further Dilation of Stented Segments
If the deployed stent size is still inadequate with respect to the vessel diameter, a
larger balloon may be used to further expand the stent to its optimal size. If the
initial angiographic results are suboptimal, the stent may be further deployed
using a low profile, high pressure, non-compliant balloon catheter. If required, the
stented segment should be recrossed carefully with a prolapsed guidewire to
avoid dislodging the stent. All efforts should be taken to assure that the stent is
not under dilated.
CAUTION: Do not deploy the Integrity Coronary Stent System beyond the
Rated Burst Pressure shown on the compliance chart provided with the
package. Do not dilate the 3.0 - 4.0mm stents to greater than 5.0mm. Do not
dilate the 2.25 - 2.75mm stents to greater than 3.50mm.
9.8 Instructions for Simultaneous Use of Two Devices in Guide Catheter
(Kissing Balloon Technique/Kissing Stent Technique)
Note: The safety and effectiveness of the simultaneous use of two devices (PTCA
catheter and/or coronary stent) in a guide catheter to treat bifurcation lesions has
not been evaluated.
• 6F (2mm) Compatibility - Any combination of one Integrity RX Coronary Stent
(models 2.25mm – 3.50mm) and one Sprinter Legend RX Balloon (models
1.25mm – 3.50mm) can be used simultaneously within a 6F (2mm)/GC/MID
1.8mm (0.070”) guide catheter.
• 7F (2.33mm) Compatibility - Any combination of two Integrity RX Coronary
Stents (models 2.25mm – 3.50mm) and/or Sprinter Legend RX Balloons (models
1.25 mm – 3.50mm) can be used simultaneously within a 7F (2.33mm)/GC/MID
2.0mm (0.080”) guide catheter.
• Delivery of the Integrity Stent:
■ Insert the stent using the instructions provided (refer to Section 9.3 “Stent
Delivery”). Position one guidewire and its associated balloon catheter at the
first target site prior to inserting a second guidewire and its associated balloon
catheter.
• Deployment of the Integrity Stent:
■ Deploy the stent using the instructions provided (refer to Section 9.4
“Deployment Procedure”).
• Removing the Catheters:
■ Remove one catheter and its associated guidewire completely prior to
removing the second catheter and its associated guidewire.
13
Page 16

10.0 MRI GUIDELINES
Non-clinical testing has demonstrated the Integrity Stent up to a total length of
120 mm is MR Conditional. It can be scanned safely under the following
conditions:
• Static magnetic field of 1.5 and 3 Tesla.
• Spatial gradient field of 1000 Gauss/cm or less
• Maximum whole body averaged specific absorption rate (SAR) of 2.0 W/kg or
less under normal operating mode only, for 15 minutes of scanning.
1.5T:
Based on non-clinical testing and modelling, a 38 mm Integrity stent was calculated
to produce an in-vivo temperature rise of less than 2.4°C, and overlapped stents with
a maximum length of 120 mm was calculated to produce an in-vivo temperature rise
of less than 3.9°C at a maximum whole body averaged specific absorption rate (SAR)
of 2.0 W/kg for 15 minutes of MR scanning per sequence in a 64 MHz whole body
transmit coil, which corresponds to a static field of 1.5 Tesla. These calculations do
not take into consideration of the cooling effects of perfusion and blood flow. The
maximum whole body averaged specific absorption rate (SAR) was derived by
calculation.
3T:
Based on non-clinical testing and modelling, a 38 mm Integrity stent was calculated
to produce an in-vivo temperature rise of less than 3.3°C, and overlapped stents with
a maximum length of 120 mm was calculated to produce an in-vivo temperature rise
of less than 4.0°C at a maximum whole body averaged specific absorption rate (SAR)
of 2.0 W/kg for 15 minutes of MR scanning per sequence in a 3 Tesla GE SIGNA
HDx with software version 14\LX\MR release 14.0.M5A.0828.b. These calculations
do not take into consideration of the cooling effects of perfusion and blood flow. The
maximum whole body averaged specific absorption rate (SAR) was derived by
calculation.
1.5 T and 3 T:
The Integrity stent should not move or migrate when exposed to MR scanning
immediately post-implantation. MRI at 1.5 and 3 Tesla may be performed immediately
following the implantation of the stent. Non-clinical testing at field strength greater than
3 Tesla has not been performed to evaluate stent migration and heating.
MR image quality may be compromised if the area of interest is in the same area or
relatively close to the position of the device. Therefore, it may be necessary to optimize
MR imaging parameters for the presence of this implant. The image artifact extends
approximately 1 cm from the device, both inside and outside the device lumen when
scanned in non-clinical testing using the spin echo and gradient echo sequences specified
in ASTM F2119-07; the device lumen was always obscured during scanning. This
14
Page 17

testing was completed using a 3 Tesla GE SIGNA HDx with software version 14\LX\MR
release 14.0.M5A.0828.b.
11.0 SUMMARY OF CLINICAL STUDIES
The Integrity Stent was designed through process improvements made to the
Driver/MicroDriver stent, leveraging its consistent clinical safety and efficacy
profile. The conclusions presented in the clinical investigations are applicable to
both Driver/Micro-Driver RX and Integrity RX.
The clinical investigations that support the use of the Integrity Coronary Stent
System are compiled mainly from three multi-center clinical investigations of the
Driver/Micro-Driver stent: the Class Study (with a subset of patients from the
Lancelot trial), the Driver Registry, the Micro-Driver Registry and the Endeavor II
Study. Between these trials, a total of 1,138 patients were enrolled.
11.1 The CLASS study:
The Class study was a pre-approval study conducted in multiple European
centers. The primary objective of this prospective, non-randomized, multi-center
study was to evaluate the safety and efficacy of the Driver Coronary Stent System
for the treatment of single de novo lesions in native coronary arteries.
In this study, 202 patients with unstable angina pectoris or a positive functional
study and a planned procedure of a single de novo lesion in a native coronary
artery were enrolled in 13 clinical sites across Europe.
The primary safety endpoint was the percentage MACE free patients at 6 months.
MACE was defined as death, Q wave MI, non-Q wave Mi, emergent bypass
surgery and target lesion revascularization (TLR) (CABG or PTCA). The primary
efficacy endpoint was the angiographic success rate. This endpoint was defined as
post procedural stenosis of <50% diameter measured by core laboratory analysis.
Clinical follow-up was performed at 30 days and a clinical angiographic followup at 6 months.
15
Page 18

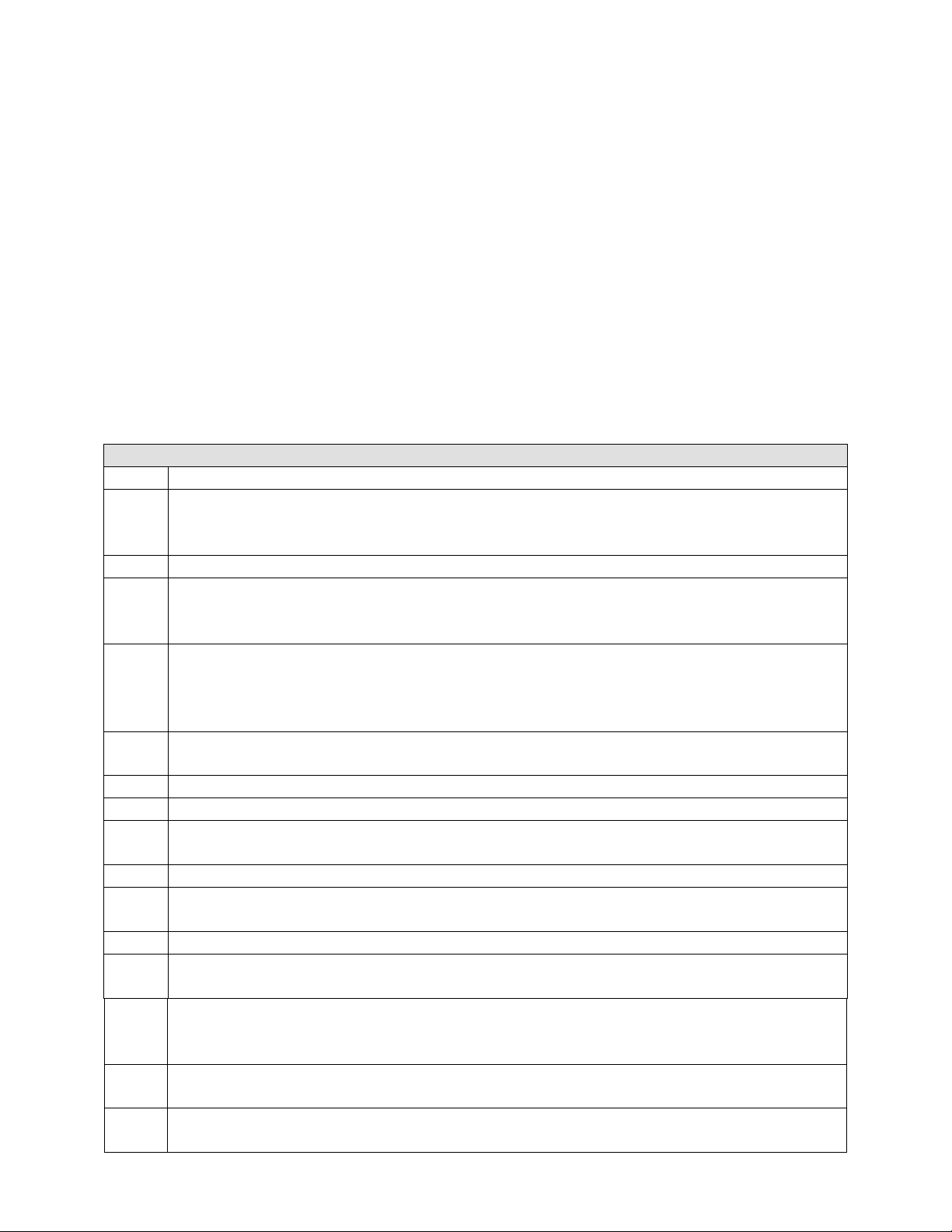
Table 2: Summary of the CLASS study
CLASS STUDY
• Multi-center in Europe (n=13)
Study Type
• Prospective
• Non-Randomized
Number of patients
• Total: 202
• Single de novo lesion in native
Lesion criteria
coronary artery ≤ 13mm in length and
with a diameter of ≥ 3.0 to ≤ 4.0 mm
• Medtronic Driver Coronary Stent
Device used
• Diameters: 3.0, 3.5 and 4.0 mm
• Lengths: 9,12 and 15 mm
• Aspirin indefinitely, and Ticlopidine or
Antiplatelet therapy
Clopidogrel discontinued after 14-28
Days
• Clinical follow up at 30±5 days
• Clinical and angiographic (
Follow up
stent) follow-up at 6 months
• Quantitative Coronary Angiography (QCA)
at baseline and 6 months follow-up
Status
• Final report completed (29th April
2004).
*CLASS Study: Clinical and angiographic analysis with a cobalt alloy coronary stent (Driver) in stable and
unstable angina pectoris. Legrand V, Kelbaek H, Hauptmann KE, Glogar D, Rutsch W, Grollier G,
Vermeersch P, Elias J, De Cock CC. American Journal of Cardiology 2006 Feb 1; 97(3):349-52.
16
Page 19

CLASS study - Results:
A total of 25 patients experienced one or more MACE and 4 patients experienced
stent thrombosis. Stent thrombosis was defined as “angiographic thrombus or subacute closure within the stented vessel at the time of the clinically driven
angiographic restudy for documented ischemia (chest pain and electrocardiogram
(ECG) changes)”. Any death not attributed to a non-cardiac cause within the first
30 days was considered a surrogate for stent thrombosis in the absence of
documented angiographic stent patency.
Table 3 shows the MACE and stent thrombosis rate which occurred during the
study. During the hospital stay, 5 patients had suffered from MACE (2.5%) and 3
patients from stent thrombosis (1.5%). At 30 day follow-up, three additional
patients suffered from MACE (total 4.0%) and one additional patient suffered
from stent thrombosis (total 2.0%). At 6 months follow-up, a total of 25 patients
had suffered from MACE (12.4%) and 4 from stent thrombosis (2.0%). Therefore,
the total percentage MACE free patients at 30 days was 96.0% and at 6 months
87.6%.
Table 3: The Class Study -Major Adverse Events
Major Adverse
Events
Death
Q-Wave MI
Non Q-Wave MI
CABG
TLR
Total % MACE
Patients
MACE Free Survival
Stent Thrombosis
In-Hospital 30 Days 6 Months
% n % n % n
0 0/202
0 0/202
2.5 5/202
0 0/202
1.0 2/202
2.5 5/202
97.2 197/202
1.5 3/202
1.5 3/202
0 0/202
2.5 5/202
0 0/202
1.0 2/202
4.0 8/202
96.0 194/202
2.0 4/202
1.5 3/202
0 0/202
3.0 6/202
0.5 1/202
9.4 19/202
12.4 25/202
87.6 177/202
2.0 4/202
Five (5) patients suffered a MI all non Q-wave, before hospital discharge. Two
were TLRs involving dissections. One patient, with a lesion treated at a
bifurcation of the distal right coronary artery (RCA) showed signs of an acute MI
one hour after the procedure. Percutaneous reintervention was performed when
repeat angiography showed a thrombotic stent reocclusion at the distal part of the
stent (stent thrombosis), likely due to a dissection. A second patient, with the
target lesion located in the circumflex artery, covering a small side branch,
developed chest pain with minimal inferior ST and CK elevation indicative of an
MI. Repeat angiography revealed stent thrombosis caused by a distal dissection
likely due to overstretching with a large stent with the side branch still open. With
reintervention of the target lesion a second stent was placed distal to the first
stent. A third patient suffered from stent thrombosis. The patient experienced
acute chest pain with ECG and Creatine Kinase/Creatine Kinase myocardial-band
isoenzyme (CK/CKMB) values indicative of an MI in hospital after the
procedure.
17
Page 20

30 day follow up:
At 30 day follow-up, in addition to the 5 patients with in-hospital MACE, 3
patients had died: one noncardiac related suicide in a patient with a history of
depression; one event of sudden dyspnea (assessed as cardiac related with stent
thrombosis per protocol because no autopsy was performed); and a MI without
stent thrombosis. At 30 day follow-up, a total of 4.0% of the patients (8/202) had
suffered from MACE. Therefore, the percentage of MACE free patients was
96.0%.
6 months follow up:
At 6 months follow-up, an additional 17 patients had experienced MACE. One
patient had a non Q-wave MI 3.5 month’s post-procedure. A repeat
revascularization of the target lesion was performed when repeat angiography
revealed restenosis. Another patient suffered from stable angina pectoris class III,
3.5 months post-procedure. A coronary artery bypass graft (CABG), involving the
target lesion, was performed when a repeat angiography showed a restenosis
(obtuse marginal) as well as a stenosis of the left main stem. According to one of
the adverse event committee members, a significant main stem stenosis was
already present at study start.
CLASS study - Conclusion:
4.0% of the patients had experienced a MACE at 30 day follow-up and 12.4% of
the patients had experienced a MACE at 6 months follow-up. Therefore the
percentage of MACE free patients at 30 days was 96.0% and at 6 months the
percentage of MACE free patients was 87.6%. The angiographic success rate was
100% and the procedural success rate was 98.0%. The delivery success rate of the
Driver Coronary Stent was 99.5%. The 6 months in-stent binary restenosis rate
was 12.6%. The average of 6 months in-stent late loss was 0.8mm.
These results show that the Driver Coronary Stent is both effective and safe, with
high angiographic, delivery and procedural success and an acceptable MACE
rate.
11.2 The DRIVER Registry
This study was a pre-market prospective, multi-center, non-randomized study
designed to evaluate to demonstrate the safety and efficacy of the Driver
Coronary Stent System for the treatment of single de novo and restenotic (non instent) lesions in native coronary arteries.
A total of 298 patients were enrolled in over 23 centers across the US. Based on
the performance of the Driver stent in this registry and the demonstrated safety
profile, this information supported the PMA approval of the devices in October
2003.
The primary end point was the incidence of MACE events defined as death, MI,
emergency bypass surgery, or TLR 180 days after enrollment. Quantitative
coronary angiography was performed before and after the index stent deployment
and repeated at 6 months in 83 patients.
18
Page 21

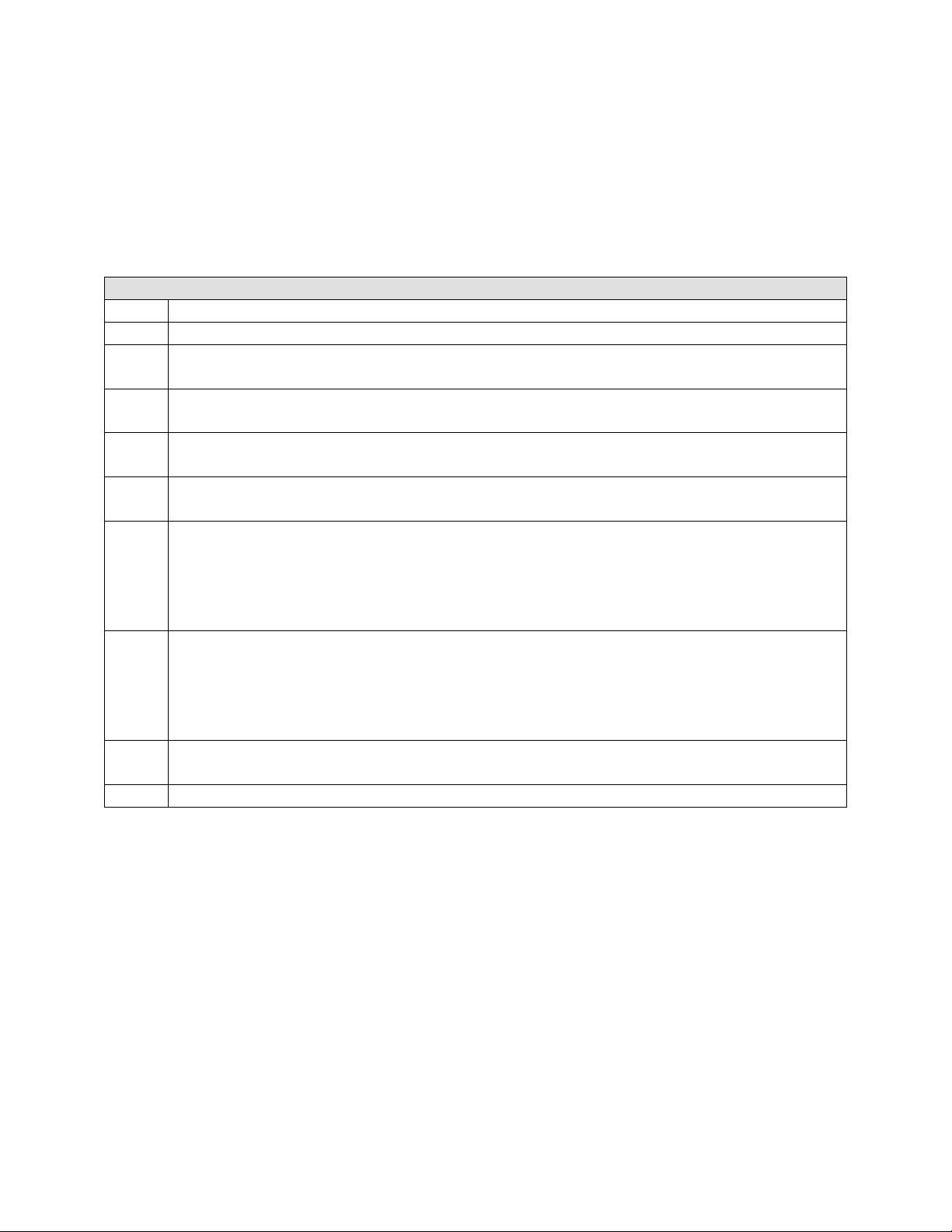
Table 4: Summary of the Driver Registry
The Driver Registry
• Multi-center US Study(n=23)
Study Type
Number of patients
Lesion criteria
Device used
Anti-platelet therapy
Follow up
Status
*DRIVER Registry: Evaluation of the Medtronic (Driver) cobalt-chromium alloy coronary stent system.
Sketch MH Jr, Ball M, Rutherford B, Popma JJ, Russell C, Kereiakes DJ; Driver investigators. American
Journal of Cardiology 2005 Jan 1; 95(1):8-12.
• Prospective
• Non-Randomized
• Total: 298
• Single de novo lesion in native
coronary artery ≤ 30mm in length and
with a diameter of ≥ 3.0 to ≤ 4.0 mm
• Medtronic Driver Coronary Stent
• Diameters: 3.0, 3.5 and 4.0 mm
• Lengths: 9, 12 and 15 mm
• Aspirin indefinitely, and Ticlopidine or
Clopidogrel discontinued after 14-28
Days
• Primary End-Point: MACE at 180 days
follow-up
• Angiographic follow-up at baseline and
at 6 months in 83 patients (off-line
QCA of coronary angiograms)
• Secondary End-Point: Clinical follow up out to 270 days
• Data published Jan 1, 2005
Driver Registry - Results:
The device and lesion success rates were 100%. The procedural success rate was
98.3%. 5 procedures were considered unsuccessful because of the occurrence of a
non–Q-wave MI on the day of the procedure. These 5 cases accounted for the
1.7% in-hospital incidence of MACE. In 284 patients, for whom data were
available, the post-procedure in-lesion Minimum Luminal/Lumen Diameter
(MLD) was 2.55 ± 0.50 mm, with a post-procedure in-lesion percent diameter
stenosis of 15.0%. The post-procedure in-stent MLD was 2.90 ± 0.41 mm, with a
post-procedure in-stent percent diameter stenosis of 3.0%.
19
Page 22

Table 5: Driver Registry- Acute and Long-term Clinical and Angiographic Outcome
Acute and Long-term Clinical and Angiographic Outcomes
(n=298) Outcome Efficacy Measure Outcome
Acute Success:
Device:
Lesion:
Procedural:
Reference Vessel
Diameter (mm):
Out of Hospital:
MACEs
TLR
TVR
TVF
100%
100%
98.3%
3.01±0.48
At 180 d
4.0% 8.4%
3.4% 7.0%
4.4% 8.1%
5.0% 8.1%
At 270 d
In-Hospital
MACE:
MLD (mm)
In Stent:
In Lesion:
Angiographic
Binary Restenosis
In-Stent:
In-Lesion:
In-Stent Late Loss:
In-Lesion Late Loss:
1.7%
2.90±0.41
2.55±0.50
15.7% (13/83)
15.7% (13/83)
0.94±0.54
0.62±0.56
Long-term (180-and 270-day) clinical outcomes:
The primary end-point showed an incidence of MACE at 180 days to be 5.7%. By
180 days, 10 of the 298 patients (3.4%) required TLR; 8 (2.7%) underwent
percutaneous transluminal coronary angioplasty, and 2 (0.7%) underwent
coronary artery bypass graft surgery. By 270 days, an additional 11 patients
(3.7%) had undergone percutaneous transluminal coronary angioplasty, for an
overall TLR rate of 7.0%.
Although the primary end-point was to 180 days, secondary end-points were
evaluated out to 270-days. The 270-day Kaplan-Meier estimate of freedom from
TLR was 91.2% (95% confidence interval 86.5% to 95.8%), from target vessel
revascularization 90.0% (95% confidence interval 85.1% to 95.0%), from target
vessel failure 88.3% (95% confidence interval 83.1% to 93.6%), and from MACE
87.7% (95% confidence interval 82.4% to 93.1%).
Clinical events reported between hospital discharge and the 270-day follow-up
included 4 non-cardiac deaths (1.3%), 1 cerebrovascular accident (0.3%), and 1
bleeding complication (0.3%). Through follow-up, 2 patients (0.7%) experienced
vascular complications. Overall, including the in-hospital and out-of-hospital
events, 10 of 298 patients (3.4%) experienced a total of 12 vascular
complications: 5 pseudoaneurysms, 1 arteriovenous fistula, 5 hematomas >5 cm
in diameter, and 1 incident of peripheral ischemia that was repaired surgically.
Two of these patients had multiple vascular complications; 1 patient had a non–
Q-wave MI and a bleeding complication, and 1 had a non–Q-wave MI and a
vascular complication. No incidents of stent thrombosis, subacute closure, or
abrupt closure were reported during the 270-day follow-up period.
20
Page 23

Driver Registry - Conclusion
The results of this registry further displayed the Driver’s safety and performance
profile in clinical practice and supported the PMA approval of these devices in
the US in 2003.
11.3 The Micro-Driver Registry
The Micro-Driver Registry was a pre-market, prospective, multi-center, nonrandomized registry, which evaluated the Micro-Driver Coronary Stent System in
patients with symptomatic ischemic heart disease due to single de novo lesions
and eligible for percutaneous transluminal coronary angioplasty (PTCA) in native
coronary arteries with a reference vessel diameter of 2.25 – 2.75 mm and 21 mm
in length or less.
Micro-Driver was evaluated at 17 investigational sites throughout the United
States. Based on the performance of the Micro-Driver stent in this registry and the
demonstrated safety profile, this information supported the PMA approval of the
devices in April 2006.
The primary objective of this study was to demonstrate the safety and efficacy of
the Micro-Driver Coronary Stent for the treatment of single de novo lesions in
small diameter native coronary arteries. The primary endpoint was MACE which
included: death, Q wave or Non-Q wave MI, emergent bypass surgery, or TLR
within 30 days of the index procedure.
Table 6: Summary of Data from the Micro-Driver Registry
The Micro-Driver Registry
• Multi-center US Study(n=17)
Study Type
Number of patients
Lesion criteria
Device used
Anti-platelet therapy
Follow up
Status
• Prospective
• Non-Randomized
• Total: 135
• Single de novo lesion in native coronary
artery ≤ 21mm in length and
with a diameter of ≥ 2.25 to ≤ 2.75 mm
• Medtronic Driver Coronary Stent
• Diameters: 2.25, 2.5 and 2.75 mm
• Lengths: 8, 12, 18 and 24 mm
• Per hospital policy or physician discretion
• Primary End-Point: MACE at 30 days
follow-up
• 180 Days= clinical and angiographic
• 270 Days= Telephone Assessment
• Final report completed May 18,2005
21
Page 24

Micro-Driver Registry – Results
The primary endpoint of this investigation, the 30 day MACE rate, was 0.7%
(1/135) in the Intent-to-Treat (ITT) group and 0.0% (0/133) in the Per-Protocol
group. Diabetic patients accounted for 31.9% (43/135) of the patient population.
The one MACE event reported through 30 days occurred in a diabetic patient.
For the ITT population, procedure success and device success were 99.3% and
lesion success was 100%;
The Micro-Driver MACE rate at 30 days for both the ITT and the Per-Protocol
population showed to be statistically non-inferior to the Objective Performance
Criterion of 4%, thus meeting the primary endpoint of the study. Device delivery
success and procedure success were high. Six month TLR was low and compares
favorably with other small vessel stent trials despite the inclusion of smaller
vessels and higher proportion of diabetic patients. Nine month TLR increased
slightly from 6 months proportionate to what would be expected based on
experience with larger vessels.
The 6 months angiographic and 9 months clinical data further demonstrate the
safety and effectiveness of the Micro-Driver Coronary stent. Several pre-specified
secondary endpoints, including acute procedure/device success rates, various
complication rates, and TVF rates, are also relevant measures of the Micro-Driver
performance and safety.
Micro-Driver Registry – Conclusion
Cumulatively, these endpoints strongly support the Micro-Driver stent as a safe
and effective treatment of ischemic heart disease due to discrete de novo lesions
with reference vessel diameter of 2.25 – 2.75 mm and ≤ 24 mm in length. In
showing very high acute procedural success, low 30 day MACE and excellent
clinical outcomes to 9 months, the data supports the safety and efficacy of the
Micro-Driver Coronary Stent System for non-emergent treatment of de novo
native coronary lesions.
Based on the performance of the Micro-Driver stent in this registry and the
demonstrated safety profile, this information supported the PMA approval of the
devices in April 2006.
11.4 The ENDEAVOR II Study:
The Endeavor II Study was designed as a prospective, multi-center, double-blind,
two-arm randomized controlled study. Endeavor II enrolled 1,200 patients and
was conducted at 72 centers across Asia, Australia, Europe, Israel, and New
Zealand.
This trial was performed to evaluate the safety and efficacy of the Medtronic
Endeavor Zotarolimus-eluting Coronary Stent Systems (drug coated
Driver/Micro-Driver stents) in comparison to the Medtronic Driver/Micro-Driver
Bare Metal Stent in the treatment of single lesions in de novo native coronary
arteries 2.25-3.5 mm in diameter.
22
Page 25

Table 7: Summary of the Endeavor II study
ENDEAVOR II STUDY
• Multi-center study in Europe, Asia
Pacific, Israel, New Zealand, and
Study Type
Number of patients
Lesion criteria
Devices available
Antiplatelet therapy
Follow up
Status
Australia (n=72)
• Prospective
• Double-Blind, Randomized
• Total: 1,200 patients
600= Driver Stent, 114/600 were Micro-Driver.
600= Endeavor Stent
• Single de novo lesion in native
coronary artery 14-27 mm in length and
with a diameter of ≥ 2.25 to ≤ 3.5 mm
• Medtronic Driver/Micro-Driver Coronary Stent:
• Micro-Driver : 2.25, 2.5 diameters with lengths
8, 18, 24, and 30mm
• Driver: 3.0 and 3.5 diameters in lengths, 9, 18,
24 and 30mm
• Medtronic Endeavor Coronary Stent
• Aspirin indefinitely and Ticlopidine or
Clopidogrel ≥3 Months
• IVUS first 300 patients at 8 months
• Angiography first 600 patients at 8
months
• Primary Endpoint= TVF at 9 Months
• Secondary Endpoint= MACE at 30
Days and 9 Months, BR at 8 months
• F/U through 5 years
• Data from presentation at PCR 2009 prior to 5years
Final Report.
The primary endpoint for this trial was the target vessel failure (TVF) rate,
defined as a composite of target vessel revascularization (TVR), Q wave or non-Q
wave MI or cardiac death that could not be clearly attributed to a vessel other than
the target vessel at 270 days post index procedure.
MACE was one of the secondary endpoints and was defined as death, MI (Q
wave and non-Q wave), emergent cardiac bypass surgery or TLR reported at 30
days and 6, 9, 12, 24, 36 and 48 months and reported in the 5 year follow-up.
23
Page 26

Endeavor II Study - Results:
The cumulative data shows that the incidence of TVF in the Driver/Micro-Driver
arm of the study is 22.4 % at 5 years. At the 5 year close out, the overall MACE
in the Driver/Micro-Driver arm was shown to be 24.6%.
The patients treated with Driver//Micro-Driver had a low rate of TVR at five
years (20.1%). With regards to Death, the rate was low at 7.6% at 5 years.
Similarly, the rate of MI was low at 4.8% (see Table 10).
Table 8: Summary of clinical events at 5 years
Endeavor II
Driver n= 599 patients
Events at 5 years % (n)
Death (all)
Cardiac
MI (all)
Non-Q Wave
Death (cardiac) + MI(all)
TLR
TVR (non-TL)
TVR
MACE
TVF
16.3% (n=95)
20.1% (n=117)
24.6% (n=143)
7.6% (n=44)
3.6% (n=21)
4.8% (n=28)
3.6% (n=21)
8.4% (n=49)
6.2% (n=36)
24.4% (142)
The Driver group showed a very low degree of early stent thrombosis (1.2%), late
(0.2%), very late (0.3%), and overall stent thrombosis (1.7) after 5 years (see
Table 9).
24
Page 27

Table 9: Endeavor II study: Summary of ARC Stent Thrombosis to 5 years
Endeavor II
Driver n=599 patients
ARC Def/Prob % (n)
Stent Thrombosis
Early: 0-30 days
Late: 31-360 days
Very late: 361-1800 days
Endeavor II Study - Conclusion:
1.7 (n=10)
1.2 (n=7)
0.2 (n=1)
0.3% (n=2)
From the Driver/Micro-Driver control arm of the Endeavor II study, the rates of
MACE and TVF (primary end-points) support the consistent safety and efficacy
profile of the Driver/Micro-Driver coronary stent. The secondary end-points of
TVR, death, MI, and thrombosis out to 5 years demonstrate further evidence of
the Driver and Micro-Driver stents consistent safety and performance profile out
to 5 years. The Endeavor II study shows that the Driver and Micro-Driver stent
remains an effective and safe treatment option for patients undergoing coronary
artery stenting.
DISCLAIMER OF WARRANTY
ALTHOUGH THE CORONARY STENT SYSTEM, HEREAFTER REFERRED TO AS
“PRODUCT,” HAS BEEN MANUFACTURED UNDER CAREFULLY CONTROLLED
CONDITIONS, MEDTRONIC INC. AND THEIR RESPECTIVE AFFILIATES
(COLLECTIVELY, “MEDTRONIC”) HAVE NO CONTROL OVER CONDITIONS UNDER
WHICH THIS PRODUCT IS USED. MEDTRONIC, THEREFORE, DISCLAIMS ALL
WARRANTIES, BOTH EXPRESSED AND IMPLIED, WITH RESPECT TO THE PRODUCT,
INCLUDING, BUT NOT LIMITED TO, ANY IMPLIED WARRANTY OF MERCHANTABILITY
OR FITNESS FOR A PARTICULAR PURPOSE. MEDTRONIC SHALL NOT BE LIABLE TO
ANY PERSON OR ENTITY FOR ANY MEDICAL EXPENSES OR ANY DIRECT,
INCIDENTAL OR CONSEQUENTIAL DAMAGES CAUSED BY ANY USE, DEFECT,
FAILURE OR MALFUNCTION OF THE PRODUCT, WHETHER A CLAIM FOR SUCH
DAMAGES IS BASED UPON WARRANTY, CONTRACT, TORT OR OTHERWISE. NO
PERSON HAS ANY AUTHORITY TO BIND MEDTRONIC TO ANY REPRESENTATION OR
WARRANTY WITH RESPECT TO THE PRODUCT.
The exclusions and limitations set out above are not intended to and should not be
construed so as to contravene mandatory provisions of applicable law. If any part or term
of this Disclaimer of Warranty is held to be illegal, unenforceable or in conflict with
applicable law by a court of competent jurisdiction, the validity of the remaining portions
of this Disclaimer of Warranty shall not be affected.
25
Page 28

MANUFACTURER:
MEDTRONIC, INC.
710 Medtronic Parkway NE
Minneapolis, MN 55432
U.S.A.
Tel: (+1-763) 514-4000
Fax: (+1-763) 514-4879
www.medtronic.com
US CUSTOMER SERVICE / PRODUCT INQUIRIES:
Tel: (+1-888) 283-7868
Fax: (+1-800) 838-3103
*M728550B001* Rev 1A
© 2011 Medtronic, Inc.
All Rights Reserved
 Loading...
Loading...