Page 1
Medical Procedure and EMI Warnings, Precautions, and
Guidance
for implanted pacemakers and defibrillators
Manual for Health Care Professionals
Page 2

Medtronic, Medtronic with rising man logo, and Medtronic logo are trademarks of Medtronic. Third-party trademarks (“TM*”) belong to
their respective owners. The following list includes trademarks or registered trademarks of a Medtronic entity in the United States and/or
in other countries.
Adapta™, EnPulse™, Kappa™, MVP™, Relia™, Sensia™, SureScan™, Versa™
Page 3

Contents
1 Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3
2 Overview of electromagnetic interference (EMI) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
2.1 Types of EMI . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
2.2 Applicable standards for safety and electromagnetic compatibility . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
3 Device responses to EMI . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
3.1 Oversensing . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
3.2 Device reset . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
3.3 Reversion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
4 General guidelines for patients in the presence of EMI . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
5 Perioperative management of patients with implanted pacemakers or ICDs . . . . . . . . . . . . . . . . . . . 7
6 Warnings and precautions for medical procedures and equipment . . . . . . . . . . . . . . . . . . . . . . . . . . 7
6.1 Medical procedures and equipment that require warnings, precautions, and guidance for health care
professionals . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
6.2 Medical procedures and devices that are acceptable for patients with implanted pacemakers and
ICDs . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 19
6.3 How to initiate asynchronous pacing in a Medtronic pacemaker with a Medtronic Model 9466 patient
magnet . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 19
6.4 How to suspend tachyarrhythmia detection and therapies in a Medtronic ICD with a Medtronic Model 9466
patient magnet . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 20
6.5 Medtronic Model 9466 patient magnet . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21
7 Warnings, precautions, and guidance for EMI for patients with an implanted pacemaker or
ICD . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 22
7.1 Items with no distance restriction from an implanted pacemaker or ICD . . . . . . . . . . . . . . . . . . . . . . . . . . 22
7.2 Items with a 15 cm (6 in) distance restriction from an implanted pacemaker or ICD . . . . . . . . . . . . . . . . . 23
7.3 Items with a 30 cm (12 in) distance restriction from an implanted pacemaker or ICD . . . . . . . . . . . . . . . . 25
7.4 Items with a 60 cm (24 in) distance restriction from an implanted pacemaker or ICD . . . . . . . . . . . . . . . . 26
7.5 Items with low potential for EMI at extended distances from an implanted pacemaker or ICD . . . . . . . . . 27
7.6 Items and environments with special considerations for EMI for patients with implanted pacemakers and
ICDs . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 27
7.7 Non-EMI environments with special consideration for patients with implanted pacemakers and
ICDs . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 28
1 Introduction
This manual is for physicians and other health care professionals who treat patients who have the following
Medtronic implanted cardiac devices:
• Pacemakers, including cardiac resynchronization therapy pacemakers (CRT-P)
• Cardioverter defibrillators (ICD), including cardiac resynchronization therapy defibrillators (CRT-D)
Note: The warnings, precautions, and guidance in this manual do not apply to patients who have leadless
transcatheter cardiac devices or implantable cardiac monitors.
To view or download this manual online, see the Medtronic eManuals website at www.medtronic.com/manuals.
Chapter 2 provides a short overview of electromagnetic interference (EMI).
3
Page 4

Chapter 3 describes the most common device responses to electromagnetic interference (EMI).
Chapter 4 provides EMI guidelines for clinicians to discuss with their patients.
Chapter 5 provides guidance for the perioperative care of patients with implanted devices for medical procedures.
Chapter 6 provides information related to EMI for health care professionals who perform medical procedures on
patients with Medtronic implanted cardiac device systems, in consultation with patient cardiologists. This section
provides warnings, precautions, and guidance for medical therapies and diagnostic procedures that present
potential risk to the patient or to the operation or physical integrity of the Medtronic system. Some common medical
procedures that pose no risk for EMI are also listed. This chapter also includes technical and procedural
information for the application of a Medtronic Model 9466 patient magnet. The patient magnet can mitigate the
effects of EMI on an implanted device. Use of the patient magnet is suggested for a number of the medical
therapies and diagnostic procedures described in this chapter.
Chapter 7 provides precautions and other information related to EMI that is helpful to patients in their daily living.
Health care professionals can review the information with their patients and use it as a reference for post-implant
consultations.
For guidance on medical procedures or potential EMI scenarios that are not documented in this manual,
customers can contact the following Medtronic resources:
• Customers in the USA can contact Medtronic Technical Services at +1 800 505 4636 for pacemakers and
CRT-Ps or +1 800 723 6243 for ICDs and CRT-Ds. You can also submit questions to tshelp@medtronic.com
or to your Medtronic representative.
• Customers outside of the USA can contact a Medtronic representative.
2 Overview of electromagnetic interference (EMI)
This chapter details the types of EMI and lists the electromagnetic field intensity limits for Medtronic implanted
pacemakers and ICDs.
2.1 Types of EMI
Medtronic pacemakers and ICDs comply with standards for testing of implanted cardiac devices in the presence
of EMI. These devices operate properly when a patient is exposed to the electromagnetic fields commonly
encountered at work, at home, or in other environments. Medtronic advises patients, their clinicians, and their
employers to consult with each other to consider EMI safety before the patient returns to work after receiving a
pacemaker or an ICD.
Note: See Section 2.2, Applicable standards for safety and electromagnetic compatibility, page 5 for more
information.
There are 3 principal types of EMI:
• Conducted interference occurs when the patient is in direct contact with the electrical source. The greatest
risk occurs from poorly maintained or ungrounded electrical equipment or items. Patients with an implanted
pacemaker or ICD must avoid conducted current.
• Radiated fields are signals propagated through the air. They can induce current that is detectable by an
implanted pacemaker or ICD. Common sources of these fields include high-voltage power lines, radio
transmission towers, or two-way wireless communication equipment.
• Static magnetic fields are produced by permanent magnets or direct current (DC) electro-magnets.
Permanent magnets are the most common type of magnet in consumer products.
See Chapter 3, Device responses to EMI, page 5 for details on how EMI affects implanted pacemakers and
ICDs.
4
Page 5
2.2 Applicable standards for safety and electromagnetic compatibility
Medtronic pacemakers and ICDs conform to the following industry standards for active implantable medical
devices for safety and electromagnetic compatibility:
• ANSI/AAMI/ISO 14117
• EN 45502-1
• EN 45502-2-1
• EN 45502-2-2
• ISO 14708-1
• ISO 14708-2
• ISO 14708-6
3 Device responses to EMI
This chapter describes the most common device responses to electromagnetic interference (EMI).
Potential EMI impact on implanted pacemakers and ICDs – Table 1 describes the potential impact of EMI on
implanted pacemakers and ICDs.
Note: If you remove the source of EMI or if the patient moves away from or turns off the source of EMI, the implanted
cardiac device resumes normal operation.
Table 1. Potential EMI impact on implanted pacemakers and ICDs
EMI source Potential impact on a pacemaker Potential impact on an ICD
Conducted interference; radiated electric / magnetic fields
Static magnetic fields (direct
current)
a
EMI oversensing can cause both pacemakers and ICDs to provide insufficient pacing support. If pacing therapy
is inhibited, pacemaker-dependent patients can be deprived of adequate cardiac output.
b
See Section 3.3, Reversion, page 6 for more information.
c
Application of pacing therapy at an excessive rate such that it causes symptoms or compromised cardiac
hemodynamics.
d
Inadequate tachyarrhythmia therapy (failure to provide anti-tachyarrhythmia pacing, cardioversion, or
defibrillation therapy).
e
Pacemakers will switch their operating mode and rate in the presence of a strong magnet. For pacemakers that
have not reached recommended replacement time (RRT) or elective replacement indication (ERI), the device
will operate in an asynchronous mode at 85 min–1. For pacemakers that have reached RRT or ERI, the
pacemaker will operate in an asynchronous mode at 65 min–1. Asynchronous pacing can induce an arrhythmia.
f
Tachyarrhythmia detection and anti-tachyarrhythmia pacing therapy are available in some models of
pacemakers. Exposure to static magnetic fields can result in inadequate tachyarrhythmia therapy.
g
Static magnetic fields do not affect pacing in ICDs.
Inhibition of pacing therapya; noise
reversionb; high-rate pacing
c
Asynchronous pacinge; suspension of
tachyarrhythmia detection, and suspension of anti-tachyarrhythmia pacing
therapy
f
Inhibition of pacing therapya; suspension of tachyarrhythmia detection, and
suspension of therapyd; high-rate pacingc; delivery of inappropriate highvoltage therapy
Suspension of tachyarrhythmia detection which will prevent tachyarrhythmia
therapy delivery
d,g
5
Page 6

3.1 Oversensing
Oversensing is the most common consequence of device overexposure to EMI. Oversensing occurs when a
device detects EMI in addition to intrinsic cardiac signals. Several factors can trigger oversensing, such as the
duration of EMI exposure or the path of the electrical or magnetic current.
Inappropriate sensing of tachyarrhythmias – Some medical procedures use equipment that can create EMI
that an implanted pacemaker or ICD does not filter out but interprets as a rapid heart rate. If this interference
persists, it can meet the criteria for tachyarrhythmia detection for which the device can deliver inappropriate
tachyarrhythmia therapy.
Inhibition of pacing and cardiac resynchronization therapy – Oversensing can inhibit pacing or cardiac
resynchronization therapy in pacemakers and ICDs. If a patient is pacemaker-dependent, prolonged pacing
inhibition can cause hemodynamic instability.
3.2 Device reset
Device reset, also known as a power on reset (POR) or an electrical reset, is a recovery response to an unexpected
device event. Device reset is a rare response to EMI or to ambient radiation. A device reset can also occur in
response to the direct exposure to some types of therapeutic ionizing radiation.
Device reset settings are safe for most patients, but they can be therapeutically suboptimal. Perform the following
steps if an implanted device reports a device reset:
1. Schedule an immediate clinic appointment with your patient.
2. Restore the patient’s parameter values for pacing, arrhythmia detection, and arrhythmia therapy with a
Medtronic programmer or a Medtronic device manager.
3. Download the saved device data file according to the procedure provided in the instructions for use for your
Medtronic programmer or Medtronic device manager. This file includes the device memory image that
Medtronic uses to analyze the device.
4. Contact Medtronic Technical Services for further guidance.
3.3 Reversion
Reversion, also known as noise reversion, initiates asynchronous pacing in the presence of strong EMI. It
minimizes the effect of EMI that can inhibit pacing. During reversion, a pacemaker responds as follows:
• Pacing occurs at the sensor-indicated rate for all rate responsive modes (excludes VVIR and VDIR).
• Pacing occurs at the programmed lower rate for all non-rate responsive modes (includes VVIR and VDIR).
The device resumes normal operation when the EMI source is removed.
4 General guidelines for patients in the presence of EMI
Advise patients to observe the following general guidelines in the presence of EMI:
• Area restrictions – consult with your clinician before entering an area where signs are posted that warn persons
with an implanted pacemaker or ICD.
• Symptoms of EMI – if you become dizzy or feel rapid or irregular heartbeats while using an electrical item,
release whatever you are touching or move away from the item. The implanted cardiac device should
immediately return to normal operation. If symptoms do not improve when you move away from the item, notify
your clinician. If you have an ICD and you receive a therapy shock while using an electrical item, release the
item or move away from it, then notify your clinician.
• Proper grounding of electrical items – To avoid interference from electrical current that can leak from
improperly grounded electrical items and pass through the body, observe the following precautions:
– Confirm that all electrical items are properly wired and grounded.
6
Page 7
– Confirm that electrical supply lines for swimming pools and hot tubs are properly installed and grounded
according to local and national electrical code requirements.
5 Perioperative management of patients with implanted pacemakers or ICDs
Perioperative care of a patient with an implanted pacemaker or an implanted ICD requires thorough
communication between the procedure team and the device team. The procedure team includes the clinicians
who perform the medical procedure. The device team includes the clinicians who monitor the device function. The
device team leader is an electrophysiologist, a cardiologist, an anesthesiologist, or a surgeon with expertise in
device management. If the patient’s device team is not available, a resident device team can evaluate the patient
and provide recommendations to the procedure team.
Observe these general precautions:
• The perioperative management of devices must consider the health of the patient, the type of device, and the
procedure.
• The procedure team informs the device team of the type of procedure and any sources for EMI.
• The device team gives the procedure team a prescription for the perioperative management of the patient in
consideration of the potential to the device for EMI. For most patients, the prescription can be made from a
review of records maintained by the device clinic. Consult with device specialists if clinic records are not
available.
6 Warnings and precautions for medical procedures and equipment
This chapter describes the potential for EMI from medical procedures and equipment to patients with a Medtronic
implanted pacemaker or a Medtronic implanted ICD.
Table 2. Acceptability of medical equipment and procedures for patients with an implanted pacemaker or an implanted ICD
Acceptability Acceptability criteria
Acceptable The equipment and procedure have a low potential for EMI with an
implanted device, and they are safe if the equipment is in proper working
condition and used as intended.
Acceptable with precautions The equipment and procedure have some potential for EMI with an
implanted device. You can mitigate the effects of the EMI if the equipment
is in proper working condition and used as intended, and if you follow the
precautions in this document.
Not recommended The equipment and procedure have a high potential for EMI with an
implanted device, and they are not safe. You cannot mitigate the effects of
the EMI.
Note: The off-label use of any medical equipment or procedure described in this document voids these
acceptability criteria.
6.1 Medical procedures and equipment that require warnings, precautions, and guidance for health care professionals
This section describes medical procedures and equipment that require precautions for patients with a Medtronic
implanted pacemaker or ICD:
• A pacemaker can be a single-chamber pacemaker, a dual-chamber pacemaker, or a CRT-P.
• An ICD can be a single-chamber ICD, a dual-chamber ICD, or a CRT-D.
7
Page 8
For a list of commonly performed medical procedures that are acceptable without precautions for patients with
implanted cardiac devices, see Section 6.2, Medical procedures and devices that are acceptable for patients with
implanted pacemakers and ICDs, page 19.
Ablation
Cryogenic ablation – Acceptable. Cryogenic ablation is indicated for the treatment of atrial fibrillation. This
procedure creates lesions in the cardiac tissue near the pulmonary veins with cryothermal energy (pressurized
liquid nitrous oxide).
Radiofrequency (RF) or microwave ablation – Acceptable with precautions. RF or microwave ablation is
a surgical technique in which energy creates heat to destroy cells. Common types of ablation include, but are not
limited to, intracardiac ablation and endometrial ablation.
RF or microwave ablation used for cardiac device patients can result in, but is not limited to, ventricular tachyarrhythmias, oversensing, unintended tissue damage, or unintended device function.
Observe the following precautions when you administer RF or microwave ablation to a patient with an implanted
pacemaker or ICD:
• Make sure that temporary pacing and defibrillation equipment is available.
• Avoid direct contact between the ablation catheter and the implanted system.
• Consider using at least 2 methods to monitor the patient during ablation. These methods can include arterial
pressure display, ECG, manual monitoring of patient rhythm (taking pulse), ear or finger pulse oximetry, or
Doppler pulse detection.
To mitigate the effects of oversensing EMI during therapy, consider the following procedures if patient condition
allows:
Pacemakers See Section 6.3, How to initiate asynchronous pacing in a Medtronic pacemaker with a
Medtronic Model 9466 patient magnet, page 19.
ICDs See Section 6.4, How to suspend tachyarrhythmia detection and therapies in a Medtronic
ICD with a Medtronic Model 9466 patient magnet, page 20.
Acupuncture, alternating current (AC)
Acceptable with precautions. AC acupuncture, also known as electroacupuncture, passes a small electrical
current between pairs of acupuncture needles.
AC acupuncture introduces electrical current into the body that can cause oversensing in a pacemaker or an ICD.
Patients should consult with their clinicians to determine if their cardiac condition allows them to undergo exposure to AC acupuncture.
To mitigate the effects of oversensing EMI during therapy, consider the following procedures if patient condition
allows:
Pacemakers See Section 6.3, How to initiate asynchronous pacing in a Medtronic pacemaker with a
Medtronic Model 9466 patient magnet, page 19.
ICDs See Section 6.4, How to suspend tachyarrhythmia detection and therapies in a Medtronic
ICD with a Medtronic Model 9466 patient magnet, page 20.
Bone growth stimulators
A bone growth stimulator provides supplemental therapy to promote bone healing. There are 3 types of bone
growth stimulators:
Stimulator that introduces direct current (DC) into the body – Acceptable. A DC bone growth stimulator
generates insufficient EMI to affect an implanted pacemaker or an ICD.
Stimulator that introduces alternating current (AC) into the body – Acceptable with precautions. An AC
bone growth stimulator uses electrodes to introduce electrical current into the body. There is a potential for EMI
with an implanted pacemaker or ICD with the electrodes attached to the torso. When the electrodes are attached
to an extremity, the stimulator generates insufficient EMI to affect an implanted pacemaker or ICD.
8
Page 9
Bone growth stimulators
To mitigate the effects of oversensing EMI during therapy, consider the following procedures if patient condition
allows:
Pacemakers See Section 6.3, How to initiate asynchronous pacing in a Medtronic pacemaker with a
Medtronic Model 9466 patient magnet, page 19.
ICDs See Section 6.4, How to suspend tachyarrhythmia detection and therapies in a Medtronic
ICD with a Medtronic Model 9466 patient magnet, page 20.
Stimulator that produces an alternating magnetic field – Acceptable with precautions. This bone growth
stimulator delivers a short, high-intensity pulse to a coil in an insulated cuff to produce a therapeutic magnetic
field. This therapy does not introduce conducted current into the body. When the insulated cuff is on a patient’s
leg, the stimulator generates insufficient EMI to affect an implanted pacemaker or ICD. However, when the
insulated cuff is on a patient’s wrist or arm, maintain a 30 cm (12 in) distance between the cuff and the implanted
pacemaker or ICD.
Bone scan
Bone scans are used to diagnose and evaluate bone diseases and conditions. There are 3 types of bone scans.
X-ray bone scan (skeletal scintigraphy) – Acceptable. An x-ray bone scan uses small amounts of a radio-
pharmaceutical to show contrast between abnormal and healthy bone tissue. An x-ray bone scan generates
insufficient EMI to affect an implanted pacemaker or ICD.
Ultrasound bone scan (sonography or musculoskeletal ultrasound) – Acceptable. An ultrasound bone
scan uses a transducer to transmit high-frequency sound waves to create an image of bone tissue. An ultrasound
bone scan generates insufficient EMI to affect an implanted pacemaker or ICD.
Bone densitometry (dual-energy x-ray absorptiometry – DEXA) – Acceptable with precautions. Bone
densitometry is an enhanced form of x-ray technology used to measure bone density. It uses a small dose of
ionizing radiation to produce images used to diagnose osteoporosis and to assess patient risk for developing
fractures. These images are usually of the lower spine and the pelvis.
The accumulated dose of radiation from DEXA is insufficient to damage or interfere with the operation of an
implanted pacemaker or ICD. However, do not allow an implanted pacemaker or ICD to undergo direct exposure
to the radiation beam.
Capsule endoscopy
Contact Medtronic Technical Services. Capsule endoscopy, also known as video capsule endoscopy, uses
an ingestible digital camera that captures a video record of the patient’s digestive tract. The camera is in a
capsule with light-emitting diodes, a battery, and a transmitter. Transmission of the video data occurs in short
bursts of radiofrequency energy, approximately 2 per s, for an 8-hour diagnostic period.
Note: Contact Medtronic Technical Services to confirm that your capsule endoscopy system is safe for your
patient.
Central venous access catheter
Acceptable with precautions. Also known as a central line or a central venous line, a central venous access
catheter is placed into a large vein or into the heart. It administers medication or fluids that cannot be taken orally
or that can harm a smaller peripheral vein.
If transvenous leads are acute (within 30 days of implant), verify that they are actively fixed in the endocardium.
Confirm lead fixation with an x-ray or through a review of the stored device lead impedance and short interval
count data (if available). If a lead has dislodged, do not insert a central venous access catheter into the patient’s
heart.
Observe these precautions when you insert the guide wire of a central venous access catheter into the heart of
a patient who has an implanted pacemaker or ICD:
9
Page 10
Central venous access catheter
• The presence of a guide wire can trigger an arrhythmia in the patient, independent of the implanted cardiac
device.
• Contact between a guide wire and sensing electrodes can cause inappropriate pacing or oversensing in an
implanted cardiac device.
• Contact between a guide wire and a coil can cause inappropriate shock or an electrical short in an implanted
ICD.
To mitigate the potential effects of a central venous access catheter, consider the following procedures if patient
condition allows:
Pacemakers See Section 6.3, How to initiate asynchronous pacing in a Medtronic pacemaker with a
Medtronic Model 9466 patient magnet, page 19.
ICDs See Section 6.4, How to suspend tachyarrhythmia detection and therapies in a Medtronic
ICD with a Medtronic Model 9466 patient magnet, page 20.
Dental equipment
Acceptable with precautions. Dental procedures that use equipment such as apex locators, ultrasonic scal-
ers, drills, and pulp testers, pose no potential for EMI with an implanted pacemaker or ICD.
Accessories, such as office pillows or headrests, can contain magnets that can affect sensing or initiate asyn-
chronous pacing in an implanted pacemaker or ICD. Keep an implanted pacemaker or ICD at least 15 cm (6 in)
from these magnets.
Note: See “Electrosurgery” for guidance with electrosurgery used in periodontal surgery.
Diagnostic radiology (CT scans, fluoroscopy, mammograms, x-rays)
Diagnostic radiology includes the following procedures: computerized axial tomography (CT or CAT scan),
fluoroscopy, mammograms, and x-rays.
Normally, the accumulated dose of radiation from diagnostic radiology is insufficient to damage an implanted
pacemaker or ICD. If the implanted pacemaker or ICD is not directly in the radiation beam, there is no potential
for EMI, except where noted here.
CT scan – Acceptable with precautions. Oversensing can occur only when the implanted pacemaker or ICD
is directly in the CT scan beam.
Pacemakers If the device is in the CT scan beam for more than 4 s, see Section 6.3, How to initiate
asynchronous pacing in a Medtronic pacemaker with a Medtronic Model 9466 patient
magnet, page 19.
ICDs If the device is in the CT scan beam for more than 4 s, see Section 6.4, How to suspend
tachyarrhythmia detection and therapies in a Medtronic ICD with a Medtronic Model 9466
patient magnet, page 20.
Fluoroscopy at < 1 cGy/min – Acceptable. Fluoroscopy at < 1 cGy/min generates insufficient EMI to affect an
implanted pacemaker or ICD.
Fluoroscopy at ≥ 1 cGy/min – Not recommended. EMI from fluoroscopy at ≥ 1 cGy/min can cause oversensing in an implanted pacemaker or ICD.
Mammography – Acceptable. Mammography generates insufficient EMI to affect an implanted pacemaker or
ICD.
X-ray – Acceptable. X-rays generate insufficient EMI to affect an implanted pacemaker or ICD.
Diagnostic ultrasound
Acceptable. Diagnostic ultrasound is an imaging technique that visualizes muscles and internal organs, their
size, structures, and motion, as well as any pathological lesions. It can also monitor a fetus, and it can detect and
measure blood flow. Diagnostic ultrasound generates insufficient EMI to affect an implanted pacemaker or ICD.
For precautions about therapeutic ultrasound, see “Diathermy (3 types)”.
10
Page 11

Diathermy (3 types)
Diathermy involves the therapeutic heating of body tissues. There are 3 types of diathermy: shortwave diathermy,
microwave diathermy, and ultrasonic diathermy, also known as therapeutic ultrasound. Shortwave diathermy or
microwave diathermy can cause serious injury, or they can damage an implanted pacemaker or ICD. Do not use
shortwave diathermy or microwave diathermy. Ultrasonic diathermy is acceptable, with precautions.
Shortwave diathermy – Not recommended. Shortwave diathermy can cause serious patient injury. It can
damage an implanted pacemaker or ICD. Do not perform shortwave diathermy on patients who have an implanted pacemaker or ICD.
Microwave diathermy – Not recommended. Microwave diathermy can cause serious patient injury. It can
damage an implanted pacemaker or ICD. Do not perform microwave diathermy on patients who have an implanted pacemaker or ICD.
Therapeutic ultrasound – Acceptable with precautions. Therapeutic ultrasound (including physiotherapy,
high intensity therapeutic ultrasound, and high intensity focused ultrasound) uses ultrasound at higher energies
than diagnostic ultrasound to bring heat or agitation into the body. Therapeutic ultrasound does not produce EMI
fields capable of inducing significant energy levels in pacing leads; however, the mechanical energy can physically damage internal device components.
Therapeutic ultrasound is acceptable with a minimum separation distance of 15 cm (6 in) between the applicator
and the implanted device and lead system. Also, point the ultrasonic beam away from the device and lead
system.
EECP (enhanced external counterpulsation therapy)
Acceptable with precautions. EECP is a noninvasive outpatient therapy for treatment of angina. It uses inflat-
able cuffs to compress the blood vessels in the lower limbs to increase blood flow to the heart. If the rate response
feature of an implanted pacemaker or an implanted ICD is programmed to On, the pacing rate can increase if the
implanted device detects EECP-induced vibration.
Consider programming an implanted pacemaker or an implanted ICD to a non-rate-responsive pacing mode
before you administer EECP.
Enteral magnetic navigation
Acceptable with precautions. Enteral magnetic navigation allows a clinician to steer catheter-based diag-
nostic and therapeutic devices throughout the digestive system.
An enteral magnetic navigation procedure can initiate asynchronous pacing in a pacemaker or suspend tachyar-
rhythmia detection in an ICD.
To mitigate the effects of oversensing EMI during an enteral magnetic navigation procedure, consider the fol-
lowing procedures if patient condition allows:
Pacemakers See Section 6.3, How to initiate asynchronous pacing in a Medtronic pacemaker with a
Medtronic Model 9466 patient magnet, page 19.
ICDs See Section 6.4, How to suspend tachyarrhythmia detection and therapies in a Medtronic
ICD with a Medtronic Model 9466 patient magnet, page 20.
ECT (electroconvulsive therapy)
Acceptable with precautions. ECT, also known as electroshock therapy, provides relief from psychiatric ill-
nesses. ECT delivers a measured electrical pulse to induce a seizure that can last for several minutes. The
electrical current that this procedure introduces into the body can affect an implanted pacemaker or an implanted
ICD. Clinicians who administer ECT to patients with an implanted pacemaker or an implanted ICD should consult
with their cardiologists to evaluate the potential for EMI.
A pacemaker or an ICD will respond in the following ways during a typical 1 to 2 s ECT electrical pulse:
11
Page 12

ECT (electroconvulsive therapy)
Pacemakers The electrical pulse can inhibit pacing for 1 to 2 s. If the rate response feature is programmed
to On, the pacing rate can increase during the seizure period. If an ECT electrical pulse is
longer than 8 s, reversion can occur.
ICDs An ICD will inhibit pacing for the duration of the electrical pulse. If the rate response feature
is programmed to On, the pacing rate can increase during the seizure period. The potential
is low that an ICD will deliver a shock during a 1 to 2 s electrical pulse. If an ECT electrical
pulse is longer than 8 s, an ICD can deliver a shock.
EMG (electromyography)
Acceptable. EMG records muscle response to electrical stimuli during muscle rest and during muscle con-
traction. It helps to diagnose a number of muscular or neuromuscular conditions.
EMG is typically administered with an NCS (nerve conduction study), where an NCS measures nerve response
to electrical stimuli. See “NCS (nerve conduction study)” for more information and precautions.
There are 2 types of EMG:
• sEMG: surface electromyography. sEMG delivers electrical stimuli to a single patch electrode or to an array
of patch electrodes attached via a skin adhesive over the tested muscle.
• NEMG: needle electromyography. NEMG delivers electrical stimuli to a single needle electrode or to an array
of needle electrodes inserted into the tested muscle.
EMG is acceptable for patients with an implanted pacemaker or ICD.
Electrolysis
Acceptable with precautions. Electrolysis permanently removes hair by inserting an electrified needle (AC or
DC) into the hair follicle. Electrolysis introduces electrical current into the body, which can cause oversensing.
Patients should consult with their clinicians to determine if their cardiac condition allows them to undergo electrolysis.
To mitigate the effects of EMI during electrolysis, consider the following procedures if patient condition allows:
Pacemakers See Section 6.3, How to initiate asynchronous pacing in a Medtronic pacemaker with a
Medtronic Model 9466 patient magnet, page 19.
ICDs See Section 6.4, How to suspend tachyarrhythmia detection and therapies in a Medtronic
ICD with a Medtronic Model 9466 patient magnet, page 20.
Electrosurgery
Acceptable with precautions. Electrosurgery (including electrocautery, argon plasma coagulation, electro-
surgical cautery, advanced energy surgical technology, and hyfrecator) uses an electric probe to control bleeding, cut tissue, or remove unwanted tissue. Electrosurgery performed on patients with an implanted pacemaker
or ICD can result in, but is not limited to, the following complications:
• Potential pacing interruption during and up to 5 s immediately after exposure to electrosurgery.
• Oversensing.
• Unintended tissue damage.
• Tachyarrhythmias.
• Lead or device damage.
• Device malfunction.
If electrosurgery is required, consider the following precautions:
• Ensure that temporary pacing and defibrillation equipment is immediately available.
• If possible, use a bipolar electrosurgery system or advanced energy surgical technology. If a unipolar electrosurgery system is used, position the return electrode patch so that the electrical current pathway passes
12
Page 13

Electrosurgery
no closer than 15 cm (6 in) from the device and leads. Contact Medtronic Technical Services for further
guidance with unipolar electrosurgery.
• Use short, intermittent, and irregular bursts at the lowest clinically appropriate energy levels.
• Always monitor the patient during electrosurgery. If the ECG tracing is not clear due to interference, manually
monitor the patient’s rhythm (take pulse); alternatively, monitor by some other means such as ear or finger
pulse oximetry, Doppler pulse detection, or arterial pressure display.
To mitigate the effects of oversensing during electrosurgery, consider the following procedures if patient condition allows:
Pacemakers See Section 6.3, How to initiate asynchronous pacing in a Medtronic pacemaker with a
Medtronic Model 9466 patient magnet, page 19.
ICDs See Section 6.4, How to suspend tachyarrhythmia detection and therapies in a Medtronic
ICD with a Medtronic Model 9466 patient magnet, page 20.
External defibrillation and cardioversion
Acceptable with precautions. External defibrillation and cardioversion are therapies that deliver an electrical
shock to the heart to convert an abnormal heart rhythm to a normal rhythm.
Medtronic pacemakers and ICDs are designed to withstand exposure to external defibrillation and cardioversion.
While damage to an implanted pacemaker or ICD from an external shock is rare, the probability increases with
increased energy levels. These procedures can also temporarily or permanently elevate pacing thresholds or
temporarily or permanently damage the myocardium.
Follow these precautions when you deliver external defibrillation or cardioversion:
• Use the lowest clinically appropriate energy.
• Position the patches or paddles at least 15 cm (6 in) from the implanted pacemaker or ICD.
• Use a Medtronic programmer or a Medtronic device manager to evaluate the implanted pacemaker or ICD
if you deliver external defibrillation or cardioversion.
Hearing aids and cochlear implants, in ear or hardwired
Acceptable. Hearing aids or cochlear implants worn in the ear or hardwired to an acoustical detector have no
potential for EMI with an implanted pacemaker or ICD.
Hearing aids with transmitting loop antenna
Acceptable with precautions. A hearing aid with a transmitting loop antenna, worn around the neck, radiates
a magnetic field that is coupled with the T-coil in the earpiece. Advise patients to keep the loop antenna at least
15 cm (6 in) from an implanted pacemaker or ICD.
If the loop antenna is closer than 15 cm (6 in) to a pacemaker or ICD, there is a potential for pacemaker reversion,
pacing inhibition, or ICD shock.
Advise patients to reposition the loop antenna to the shoulder opposite the implant site. If that is not possible,
advise patients to use an alternative transmitting antenna that can be worn at least 15 cm (6 in) from the implant
site.
Note: This precaution also applies to transmitting loop antennae attached to audio equipment.
Note: Bluetooth hearing aids without a transmitting loop antenna are acceptable.
Hyperbaric therapy (including hyperbaric oxygen therapy, or HBOT)
Acceptable with precautions. Hyperbaric therapy is the medical use of air or 100% oxygen at a higher pressure
than atmospheric pressure. Hyperbaric therapy treats several conditions, including decompression sickness,
carbon monoxide poisoning, serious infections, and persistent wounds. Hyperbaric therapies with pressures
exceeding 4.0 ATA, approximately 30 m (100 ft) of seawater, can affect the function of or damage an implanted
13
Page 14

Hyperbaric therapy (including hyperbaric oxygen therapy, or HBOT)
pacemaker or ICD. To avoid or mitigate risks to an implanted pacemaker or ICD, do not expose patients to
pressures exceeding 4.0 ATA.
Interferential current therapy
Acceptable with precautions. Physical therapists use interferential current therapy to relieve pain and to pro-
mote soft-tissue healing. If interferential current therapy is administered on the torso, it introduces an electrical
current that can affect an implanted pacemaker or ICD. Patients should consult with their clinicians to determine
if their cardiac condition allows them to undergo interferential current therapy.
Note: The potential is low for a pacemaker or an ICD to detect interferential current therapy when it is administered to the extremities.
To mitigate the effects of oversensing EMI during therapy, consider the following procedures if patient condition
allows:
Pacemakers See Section 6.3, How to initiate asynchronous pacing in a Medtronic pacemaker with a
Medtronic Model 9466 patient magnet, page 19.
ICDs See Section 6.4, How to suspend tachyarrhythmia detection and therapies in a Medtronic
ICD with a Medtronic Model 9466 patient magnet, page 20.
Lithotripsy
Acceptable with precautions. Lithotripsy uses mechanical shock waves to break up kidney stones or gall-
bladder stones. Lithotripsy can damage an implanted pacemaker or ICD if it is at the focal point of the lithotripter
beam. Keep the focal point of the lithotripter beam at least 2.5 cm (1 in) away from the implanted pacemaker or
ICD.
To mitigate the effects of oversensing EMI during therapy, consider the following procedures if patient condition
allows:
Pacemakers See Section 6.3, How to initiate asynchronous pacing in a Medtronic pacemaker with a
Medtronic Model 9466 patient magnet, page 19.
ICDs See Section 6.4, How to suspend tachyarrhythmia detection and therapies in a Medtronic
ICD with a Medtronic Model 9466 patient magnet, page 20.
Magnetic resonance imaging (MRI)
A Medtronic implanted pacemaker, ICD, or lead is either MR Conditional or MR Unsafe.
Use any of the following resources to confirm if a pacemaker, an ICD, or a lead is MR Conditional or MR Unsafe:
• See the Medtronic MR Conditional Product Search for Cardiac Devices at www.medtronic.com/mrc.
• See the Medtronic MRI Resource Library at http://manuals.medtronic.com/manuals/mri/region.
• If you are in the USA, you can call +1 877 674 7677 for MRI technical consultation.
• If you are outside of the USA, you can contact a Medtronic representative for MRI technical consultation.
Patients with an implanted pacemaker system or an implanted ICD system (implanted
device, implanted leads, and any abandoned leads) that is MR Conditional can undergo
an MRI scan under specified conditions. For details, refer to the MRI technical manual for
the pacemaker or ICD, or contact the listed Medtronic resources.
An implanted pacemaker system or ICD system (implanted device, implanted leads, and
any abandoned leads) is MR Unsafe if any system component or item poses unacceptable
risks to the patient, medical staff or other persons within the MR environment. Patients with
an implanted pacemaker system or ICD system that is MR Unsafe cannot undergo an MRI
scan. An MRI scan on a patient with an MR Unsafe system can result in serious patient
injury or induction of tachyarrhythmias. An MRI scan on an MR Unsafe system can damage
or impact the function of the implanted pacemaker system or the implanted ICD system.
14
Page 15

MET (microcurrent electrical therapy)
Not recommended. MET is an in-home treatment for acute, chronic, and postoperative or post-traumatic pain.
MET delivers an electrical current that can affect an implanted pacemaker or ICD, depending on where MET is
applied to the body.
The potential is low that an implanted pacemaker or ICD will detect an MET pulse if the pulse is applied to the
cranium or extremities. However, if MET is applied to the torso, it can inhibit pacing in a pacemaker or an ICD, or
it can cause pacemaker reversion or ICD shock. Because MET is marketed for use in the home, its misapplication
cannot be anticipated. MET, therefore, has a high potential to affect an implanted pacemaker or ICD.
NCS (nerve conduction study)
Acceptable with precautions. An NCS, also known as a nerve conduction velocity (NCV) test, records the
speed that an electrical pulse is conducted through a nerve. This study can determine nerve damage or nerve
destruction that causes abnormal muscle response. An NCS delivers mild electrical pulses between 2 patch
electrodes. These electrodes are attached over the tested nerve with a conductive skin adhesive. One electrode
delivers the pulse, and the other electrode records the pulse and calculates its speed along the tested nerve.
An NCS is typically administered with EMG (electromyography), where EMG measures muscle response to
electrical stimuli. See “EMG (electromyography)” for more information.
Type 1: manual test – During a manual NCS, the clinician applies discretionary electrical pulses. If an implanted
pacemaker or ICD detects a pulse, it can inhibit pacing for 1 to 2 s. If the clinician separates pulses by > 10 s, the
inhibited pacing does not cause symptoms in most patients. If it is necessary to apply pulses more frequently
than once every 10 s, the implanted pacemaker or ICD can mistake the therapy for oversensing. However, if both
NCS electrodes are on the same extremity and not on the torso, the pulses are unlikely to affect an implanted
pacemaker or ICD.
To mitigate the effects of oversensing EMI during a manual NCS, consider the following procedures if patient
condition allows:
Pacemakers See Section 6.3, How to initiate asynchronous pacing in a Medtronic pacemaker with a
Medtronic Model 9466 patient magnet, page 19.
ICDs See Section 6.4, How to suspend tachyarrhythmia detection and therapies in a Medtronic
ICD with a Medtronic Model 9466 patient magnet, page 20.
Type 2: automated test – An automated NCS applies a programmed sequence of pulses to a nerve that can
affect an implanted pacemaker or ICD.
In an automated NCS, the pulse sequence is sent from the sending patch electrode to the receiving patch
electrode at a rate of 2 to 5 pulses/s for 250 pulses. If an implanted pacemaker or ICD detects the pulse sequence,
there is the potential for pacemaker reversion or pacing inhibition, or for an inappropriate ICD shock. However,
if both NCS electrodes are on the same extremity and not on the torso, the pulses are unlikely to affect an
implanted pacemaker or ICD.
To mitigate the effects of oversensing EMI during an automated NCS, consider the following procedures if patient
condition allows:
Pacemakers See Section 6.3, How to initiate asynchronous pacing in a Medtronic pacemaker with a
Medtronic Model 9466 patient magnet, page 19.
ICDs See Section 6.4, How to suspend tachyarrhythmia detection and therapies in a Medtronic
ICD with a Medtronic Model 9466 patient magnet, page 20.
Ocular procedures
A patient must remain motionless during critical junctures of an ocular procedure. A cardiac event or implanted
cardiac device therapy that is delivered during an ocular procedure can cause a patient to move and sustain
injury to the eye.
Pacemakers – Acceptable. Ocular procedures are acceptable for patients with pacemakers.
ICDs (monitored patients) – Acceptable with precautions. Suspend tachyarrhythmia detection with a
Medtronic patient magnet (see Section 6.4, How to suspend tachyarrhythmia detection and therapies in a
15
Page 16

Ocular procedures
Medtronic ICD with a Medtronic Model 9466 patient magnet, page 20), a Medtronic programmer, or a
Medtronic device manager. If appropriate for the patient, program the ICD to an asynchronous pacing mode.
Remove the magnet or restore ICD parameters with the programmer or the device manager after completing the
ocular procedure.
ICDs (unmonitored patients) – Not recommended. A cardiac event or a device therapy delivered during an
ocular procedure can cause a patient to move and sustain trauma to the eye. It is more important that the patient
receive the appropriate arrhythmia therapy if needed. Therefore, the occurrence of VT or VF in an unmonitored
ICD patient with tachyarrhythmia detection suspended would result in unexpected patient motion and, potentially, sudden cardiac death.
PEMF (pulsed electromagnetic field therapy)
Not recommended. PEMF generates a pulsed magnetic field that can cause serious injury, induction of
tachyarrhythmias, or implanted system malfunction or damage. Patients with an implanted pacemaker or ICD
should not use PEMF devices or therapies.
PET (positron emission tomography) / SPECT (single photon emission computed tomography)
Acceptable. PET and SPECT are noninvasive nuclear imaging technologies. They scan radioactive tracers
injected into the bloodstream to produce three-dimensional images.
PET and SPECT generate insufficient EMI to affect an implanted pacemaker or an implanted ICD.
RFID (radiofrequency identification devices)
Acceptable with precautions. RFID is an autoidentification technology used to decrease cost and improve
patient safety, particularly in an operating room. Wireless technology used in this setting has the potential to
interfere with implanted pacemakers and ICDs. EMI from RFID technology depends on distance and frequency
of the RF source. It is stronger at lower frequencies and at closer distances, and it peaks with direct contact
between an RFID reader and an RFID tag. Do not place an RFID tag within 30 cm (12 in) of an implanted
pacemaker or ICD.
If an RFID tag is placed more than 30 cm (12 in) from an implanted pacemaker or ICD, the generated EMI is
insufficient to interfere with the device.
Standard autoidentification systems, like systems used in consumer merchandising, present a low potential for
EMI with an implanted pacemaker or ICD.
Stereotaxis
Acceptable with precautions. Stereotaxis allows clinicians to steer catheter-based diagnostic and therapeutic
devices throughout the body by using magnetic navigation. During a stereotaxis procedure, the magnetic field
can initiate magnet mode (asynchronous pacing) in a pacemaker or suspend tachyarrhythmia detection in an
ICD. The implanted pacemaker or ICD resumes normal programmed operation after the stereotaxis procedure.
Clinicians should consult with cardiologists to determine if a stereotaxis procedure is safe for their patients with
an implanted pacemaker or ICD.
To mitigate the effects of oversensing EMI during therapy, consider the following procedures if patient condition
allows:
Pacemakers See Section 6.3, How to initiate asynchronous pacing in a Medtronic pacemaker with a
Medtronic Model 9466 patient magnet, page 19.
ICDs See Section 6.4, How to suspend tachyarrhythmia detection and therapies in a Medtronic
ICD with a Medtronic Model 9466 patient magnet, page 20.
Therapeutic radiation (radiosurgery and radiotherapy)
Radiosurgery – Acceptable with precautions. Also known as stereotactic radiosurgery, radiosurgery delivers
intense doses of radiation from a linear accelerator to destroy tumors with submillimeter precision.
16
Page 17

Therapeutic radiation (radiosurgery and radiotherapy)
Do not subject an implanted pacemaker or ICD to direct radiosurgery exposure. Accumulated radiation dosage
must not exceed 500 cGy.
Radiotherapy – Acceptable with precautions. Radiotherapy is a cancer treatment that uses radiation to
control cell growth and destroy tumors. Types of radiotherapy include high-energy photon radiation and proton
beam therapy (PBT).
Do not subject an implanted pacemaker or ICD to direct radiotherapy exposure. Accumulated radiation dosage
must not exceed 500 cGy.
Note: Contact your Medtronic representative for additional guidance to monitor the implanted pacemaker or ICD
during radiosurgery or radiotherapy.
Pacemaker and ICD shielding and radiation modeling – Discuss a shielding plan with the radiation oncologist and physicist responsible for treating the patient. The plan includes modeling of the radiation to be absorbed by the implanted pacemaker or ICD — the accumulated radiation dosage must not exceed 500 cGy.
Pacemaker and ICD repositioning – If the modeling of the radiation indicates that the accumulated radiation
dosage will be > 500 cGy, consider repositioning the implanted pacemaker or ICD. If you must reposition the
implanted pacemaker or ICD, use lead extenders to implant the device in an alternate location. If possible,
implant the pacemaker or ICD in its original location after you deliver the therapy.
Pacemaker and ICD interference from radiosurgery or radiotherapy – If a patient undergoes radiosurgery
or radiotherapy, an implanted pacemaker or ICD can sense direct or scattered radiation as cardiac activity for the
duration of the procedure. Average dose rates at the pacemaker or ICD of less than 1 cGy/min are unlikely to
produce pacemaker or ICD interference. Decreasing the dose rate (for example, by increasing the distance
between the beam and the implanted pacemaker or ICD) decreases the potential for interference.
The programmer or device manager can detect pacemaker or ICD interference during the initial therapy, shown
as unexpected activity in the programmer marker channel or the device manager event markers. If interference
does not occur, it is unlikely to occur during future treatments with the same therapy.
Note: Interrogate the implanted pacemaker or ICD to evaluate it following radiosurgery or radiotherapy.
To mitigate the effects of oversensing EMI during therapy, consider the following procedures if patient condition
allows:
Pacemakers See Section 6.3, How to initiate asynchronous pacing in a Medtronic pacemaker with a
Medtronic Model 9466 patient magnet, page 19.
ICDs See Section 6.4, How to suspend tachyarrhythmia detection and therapies in a Medtronic
ICD with a Medtronic Model 9466 patient magnet, page 20.
Device reset following radiation – A device reset (also called an electrical reset) does not indicate damage to
the implanted pacemaker or ICD; however, a reset requires device interrogation. In rare cases, a device reset can
occur several days following exposure to radiation.
Report a device reset to Medtronic Technical Services. Download the device data file with your programmer’s
save-to-media function and include it with your report. This file contains the device memory image.
How to evaluate a pacemaker or ICD for a device reset – If an implanted pacemaker or ICD has had a device
reset, a device reset warning message displays immediately upon interrogation. Reprogram the device to restore
normal operation.
Inform your Medtronic representative if your patient’s device has reset.
Pacemaker or ICD damage from radiosurgery or radiotherapy – Radiation can affect electronic circuitry, so
an accumulated radiation dosage of > 500 cGy can damage an implanted pacemaker or ICD. However, radiation
damage is sometimes not immediately apparent. If a patient requires radiosurgery or radiotherapy from any
source, do not expose an implanted pacemaker or ICD to an accumulated radiation dosage that exceeds the
recommended limit. Record and monitor the accumulated radiation dosage to implanted devices for patients
who undergo multiple radiosurgeries or courses of radiation treatment.
Tests have shown damage to implanted Medtronic pacemakers and ICDs with accumulated radiation dosage >
500 cGy. Medtronic therefore cannot predict the operation of implanted pacemakers and ICDs that have with-
17
Page 18

Therapeutic radiation (radiosurgery and radiotherapy)
stood radiation overdose. Monitor devices exposed to radiation overdose after each radiosurgery or radiotherapy treatment and consider them for replacement. Consider an augmented follow-up schedule following the
completion of all procedures.
TENS (transcutaneous electrical nerve stimulation)
Not recommended. TENS (including NMES – neuromuscular electrical stimulation) is a pain control technique
that uses electrical impulses passed through the skin to stimulate nerves. A TENS device is not recommended
for in-home use by cardiac device patients due to a potential for oversensing, inappropriate therapy, inhibition of
pacing, or asynchronous pacing. If a TENS device is determined to be medically necessary, contact a Medtronic
representative for more information.
Tissue expanders with magnetic aiming guides
Not recommended. Tissue expanders are used by plastic surgeons to prepare for reconstructive breast sur-
gery. Some tissue expanders incorporate magnets to direct a needle that is used to fill the expander with fluid.
These magnets are often close enough to initiate magnet mode in a pacemaker or suspend tachyarrhythmia
detection in an ICD.
Do not use tissue expanders with magnetic aiming guides on patients with pacemakers or ICDs. Instead, use
tissue expanders that do not have magnetic aiming guides.
TMS (transcranial magnetic stimulation)
Acceptable with precautions. TMS is a treatment that provides relief from major depressive disorder. TMS
therapy delivers rapid magnetic pulses over an extended period to stimulate nerve cells in areas of the brain
thought to control mood. TMS produces an effect similar to electroconvulsive therapy but with minimal side
effects. The magnetic current that TMS introduces into the body can affect an implanted pacemaker or ICD.
To mitigate the effects of oversensing EMI during therapy, consider the following procedures if patient condition
allows:
Pacemakers See Section 6.3, How to initiate asynchronous pacing in a Medtronic pacemaker
with a Medtronic Model 9466 patient magnet, page 19.
ICDs See Section 6.4, How to suspend tachyarrhythmia detection and therapies in a
Medtronic ICD with a Medtronic Model 9466 patient magnet, page 20.
TUNA (transurethral needle ablation), TUMT (transurethral microwave therapy), and TURP (transurethral resection of the prostate)
Acceptable with precautions. TUNA, TUMT, and TURP are surgical procedures that treat urinary symptoms
caused by benign prostatic hyperplasia (BPH). These procedures use precisely focused energy to ablate prostate tissue. Patients with implanted cardiac devices can conditionally undergo procedures that use a TUNA,
TUMT, or TURP system. To avoid affecting an implanted pacemaker or ICD when performing a TUNA, TUMT, or
TURP procedure, position the return electrode on the lower back or lower extremity at least 15 cm (6 in) away from
the implanted pacemaker or ICD.
Virtual colonoscopy (CT scan)
Acceptable with precautions. This procedure diagnoses colon and bowel disease, including polyps, diver-
ticulosis, and cancer. The procedure is performed with a CAT scan. See “Diagnostic radiology” for more information on this procedure.
Virtual colonoscopy (MRI)
Acceptable with precautions. This procedure diagnoses colon and bowel disease, including polyps, diver-
ticulosis, and cancer. As this procedure is performed with an MRI, it can only be performed on patients with
implanted cardiac devices and leads that are MR Conditional. See magnetic resonance imaging (MRI) for more
information.
18
Page 19

6.2 Medical procedures and devices that are acceptable for patients with implanted pacemakers and ICDs
The following medical procedures and devices, when in proper working condition and used as intended, generate
insufficient EMI to affect an implanted pacemaker or an ICD.
Acceptable procedures and devices for patients with implanted pacemakers and ICDs
Acupuncture, direct current (DC) DC acupuncture is safe for patients with an implanted pacemaker or
ICD.
Colonoscopy Diagnostic colonoscopy is safe for patients with an implanted pace-
maker or ICD.
Digital infrared thermal imaging
(DITI)
Dysphagia treatment devices Dysphagia treatment devices apply neuromuscular electrical stimu-
Echocardiography Echocardiography uses diagnostic ultrasound to examine the heart.
Electrocardiography (ECG) Electrocardiography senses the electrical activity of the heart.
Electroencephalography (EEG) Electroencephalography detects electrical activity in the brain.
Electronystagmography (ENG) Electronystagmography is a diagnostic test that uses passive elec-
Esophageal pH test An esophageal pH test measures and records esophageal pH to
Iontophoresis Transdermal drug delivery via iontophoresis (also known as electro-
Laser surgery Laser (light energy only) is safe for patients with an implanted pace-
Motion sickness relief band A motion sickness relief band prevents motion sickness. This device
Photodynamic therapy (PDT) Photodynamic therapy is a cancer treatment that uses a drug, called a
Sleep apnea therapy — CPAP
machine
Digital infrared thermal imaging is an imaging technique. It monitors
the infrared radiation that the skin surface emits. It uses a passive
device that does not introduce electrical current into the body.
lation to the throat to treat swallowing disorders.
trodes on the head to record involuntary movements of the eye caused
by nystagmus. This test helps to diagnose the causes of vertigo, dizziness, or balance disorders.
assess for gastroesophageal reflux disease. The test works by temporarily attaching a small capsule to the wall of the esophagus to
measure pH levels. The capsule transmits data to a receiver that the
patient wears on a belt.
motive drug administration – EMDA) relies on delivering a small level
of localized DC current.
maker or ICD. See the precautions for performing electrocautery if you
plan to combine laser surgery with electrocautery.
delivers a small electrical pulse at the wrist area.
photosensitizer or photosensitizing agent. The photosensitizing agent
interacts with a specific wavelength of light to produce a form of oxygen that kills nearby cells.
CPAP (continuous positive airway pressure) keeps airways open in
patients with moderate to severe obstructive sleep apnea. If the CPAP
mask uses magnetic clips, keep the magnets at least 15 cm (6 in) from
the implanted pacemaker or ICD.
6.3 How to initiate asynchronous pacing in a Medtronic pacemaker with a Medtronic Model 9466 patient magnet
All Medtronic pacemakers, including all MR Conditional and MR Unsafe models, enter “magnet operation” with the
application of a magnet. During magnet operation, a pacemaker paces in an asynchronous mode at either
19
Page 20

85 min–1 or 65 min–1, depending upon whether the pacemaker battery voltage is above or below its elective
replacement threshold. Sensing is suspended during asynchronous pacing to prevent pacing inhibition by EMI.
Note: As an alternative, you can program asynchronous pacing during a telemetry session with a Medtronic
programmer or with a Medtronic device manager. If telemetry is established with an implanted pacemaker, a
Medtronic Model 9466 patient magnet will not initiate magnet operation.
Note: Tap the [End Now] button to end a programmer session with a Kappa, EnPulse, Adapta, Versa, Sensia, or
Relia pacemaker. If you do not tap the [End Now] button, a 1-hour period must elapse before you can initiate
asynchronous pacing with a Medtronic Model 9466 patient magnet.
Review pacemaker labeling, available at www.medtronic.com/manuals, for information on specific pacemaker
response to a Medtronic magnet.
6.3.1 Magnet application procedure
If appropriate for the patient, perform the following steps to initiate asynchronous pacing in an implanted
pacemaker with a Medtronic Model 9466 patient magnet:
1. Locate the implanted pacemaker by gently feeling for the device under the skin. The typical location is in the
left or right pectoral area.
2. Place the patient magnet directly over the pacemaker. This action initiates asynchronous pacing in the
device.
3. To return the pacemaker to its programmed operation, remove the patient magnet.
6.3.2 Magnet operation in a pacemaker
When you position a Medtronic Model 9466 patient magnet over a pacemaker, magnet operation implements the
following changes:
• Single-chamber atrial pacing modes switch to AOO asynchronous pacing.
• Single-chamber ventricular pacing modes switch to VOO asynchronous pacing.
• Dual-chamber pacing modes, including MVP modes, switch to DOO asynchronous pacing.
• The pacing rate switches to 85 min–1 (700 ms) if the pacemaker has not reached Recommended Replacement
Time (RRT).
• The pacing rate switches to 65 min–1 (920 ms) if an RRT indicator or a device reset has occurred.
• Tachyarrhythmia detection, available in some models, is suspended.
When you remove the patient magnet, the pacemaker resumes operation as programmed.
Note: Some pacemakers deliver the first 3 paces in magnet operation at 100 min–1, followed by 85 min–1.
Note: Magnet operation does not occur if telemetry is established between the pacemaker and a Medtronic
programmer or a Medtronic device manager, or if the MRI SureScan feature is programmed to On.
6.4 How to suspend tachyarrhythmia detection and therapies in a Medtronic ICD with a Medtronic Model 9466 patient magnet
All Medtronic ICDs, including all MR Conditional and MR Unsafe models, enter “magnet operation” with the
application of a magnet. In magnet operation, an ICD sounds a steady magnet alert tone, suspends
tachyarrhythmia detection, and suspends therapy delivery. With magnet application, suspension of
tachyarrhythmia detection and suspension of therapy delivery prevent inappropriate shock therapy.
Review ICD labeling, available at www.medtronic.com/manuals, for information on specific ICD model response
to a Medtronic Model 9466 patient magnet.
Warning: An ICD suspends tachyarrhythmia detection and therapy delivery while the patient magnet is in place.
A patient magnet does not affect bradycardia pacing in an ICD. Remove the magnet to restore the ICD to its
programmed operation.
20
Page 21

See Section 6.4.3, How to program asynchronous pacing in an ICD, page 21 for additional information.
Warning: To ensure the availability of needed tachyarrhythmia therapy, the patient should not carry, store, or leave
the patient magnet positioned over the ICD. The patient should be careful to avoid sources of electromagnetic
interference (EMI) while applying the patient magnet.
6.4.1 Magnet application procedure
1. To suspend tachyarrhythmia detection and therapies, place the patient magnet over the ICD.
2. To resume tachyarrhythmia detection and therapies, remove the patient magnet from the ICD.
Note: You can also suspend and resume tachyarrhythmia detection and therapies with a Medtronic programmer
or a Medtronic device manager.
6.4.2 ICD device tones
There are 2 types of ICD or CRT-D tones, the magnet tone, and the patient alert tone.
Magnet tone – The magnet tone is a steady tone. It sounds when an ICD or CRT-D senses a magnetic field. If a
patient hears a magnet tone, instruct them to look for a magnetic object on them or near them. If a patient is
ambulatory when they hear the tone, instruct them to move away from the magnetic source, or to move to a different
location if they cannot identify the magnetic source.
Patient alert tone – The patient alert tone is either a beeping tone or an alternating high/low tone. If a patient alert
tone is programmed to On, the tone sounds when its related alert is triggered. The patient alert tone continues to
sound as scheduled, either once every 4 hours or once every 24 hours, until you interrogate the device. A patient
alert tone will also sound if an alert is in effect and the ICD or CRT-D senses a magnetic field. Tell your patient to
contact you if they hear a patient alert tone.
If you hear an alert tone when you apply a Medtronic Model 9466 patient magnet, interrogate the ICD or CRT-D for
alert conditions, for device errors, or for a device reset.
Note: ICD or CRT-D tones sound in the presence of EMI that includes a magnetic field.
Note: Magnets are designed into many consumer products, including clothing and clothing accessories. Patients
may not be aware of these magnets because they can be difficult to locate. If a patient is unsure if a product has
a magnet, the patient can contact the product manufacturer for further information. Patients can also search
consumer products with a ferrous metal object, such as a paper clip, to see if any magnets attract it.
6.4.3 How to program asynchronous pacing in an ICD
Some medical procedures and therapies generate enough EMI to inhibit pacing in an ICD. If your ICD patient is
pacemaker-dependent, use a Medtronic programmer or Medtronic device manager to program an asynchronous
pacing mode (AOO, VOO, or DOO).
Note: A Medtronic Model 9466 patient magnet will not initiate asynchronous pacing in a Medtronic ICD.
When you have finished the medical procedure or therapy, use a Medtronic programmer or Medtronic device
manager to restore device parameters.
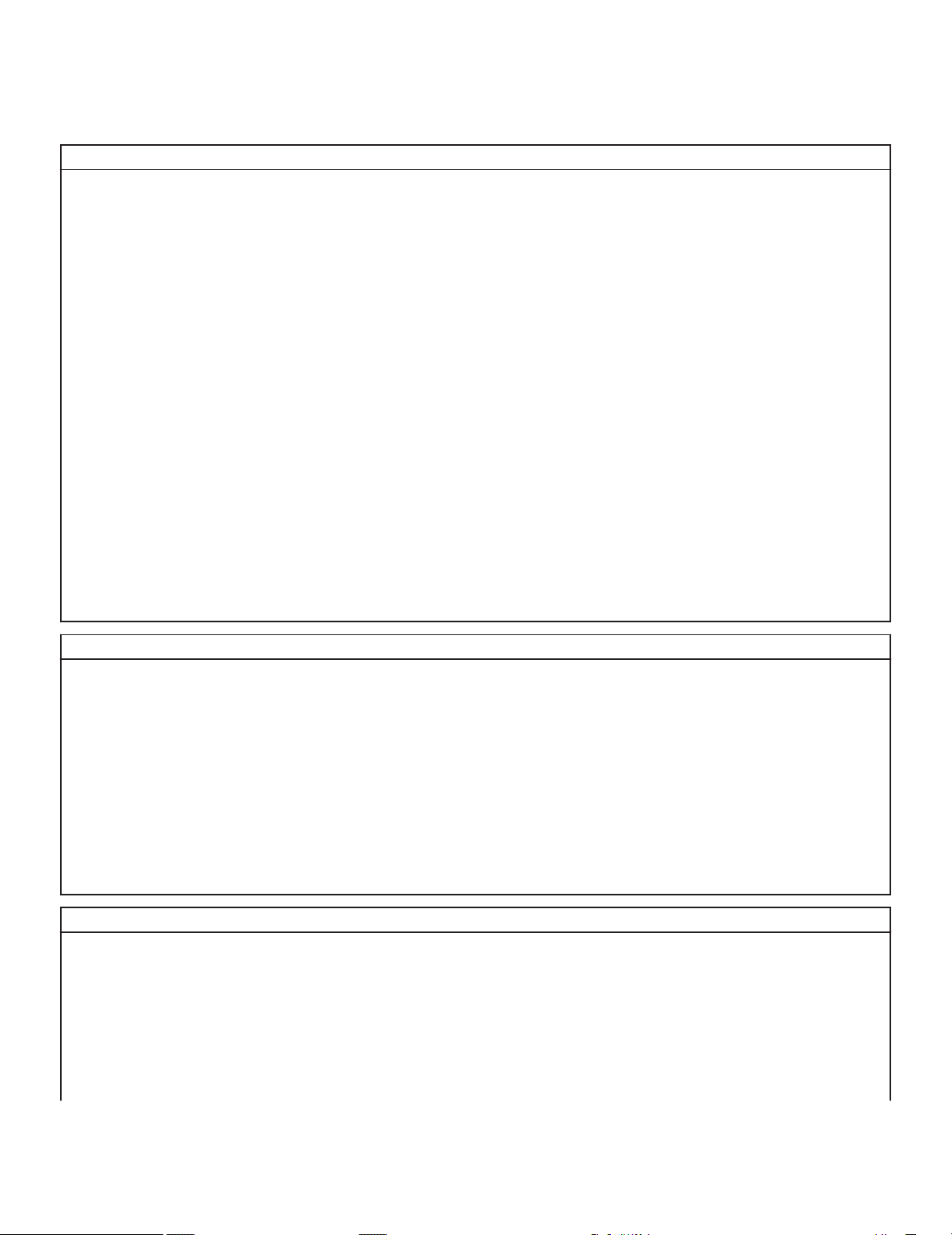
6.5 Medtronic Model 9466 patient magnet
Table 3.
Shape ring
Size
Model 9466 patient magnet specifications
Diameter 75 mm (3 in)
Thickness 16 mm (5/8 in)
21
Page 22

Table 3. Model 9466 patient magnet specifications (continued)
Materials ferrous alloys, coated with epoxy
Minimum field strength 90 gauss, at 40 mm (1.5 in) from magnet surface
Figure 1. Model 9466 patient magnet
Patient magnet storage and handling – Observe the following precautions when storing and handling the
Medtronic Model 9466 patient magnet:
• The patient magnet can damage some electronic devices if it is stored too close to those devices.
• Keep the patient magnet at least 15 cm (6 in) from electronic devices and recordings: VCRs, televisions, and
videotapes; bank cards and credit cards, cordless telephones and mobile telephones, computers, diskettes,
calculators, and similar devices.
• Keep the patient magnet at least 5 cm (2 in) from wristwatches and clocks.
• If soiled, the patient magnet can be wiped clean with a soft cloth or a sponge, or it can be washed with a
non-abrasive cleanser. The patient magnet is not damaged by being submerged in water.
7 Warnings, precautions, and guidance for EMI for patients with an implanted pacemaker or ICD
This chapter provides guidance for you to share with your patients to help them remain safe in or near environments
and devices that can generate EMI.
7.1 Items with no distance restriction from an implanted pacemaker or ICD
The following table represents items that, when used as intended and in good working condition, have no distance
restriction from an implanted pacemaker or ICD.
Table 4.
Bed, adjustable Garage door opener, remote control Medical alert necklace or pendant
Battery charger for household bat-
teries
Blender / food processor Guitar, electric Radio, AM/FM
Bluetooth technology Hair shaver / trimmer, battery pow-
Can opener Hair straightener Remote control, infrared, for
CD/DVD/DVR player or recorder,
without speakers
Examples of household items with no distance restriction for EMI
GPS (global positioning system) Microwave oven
a
ered
Heart rate monitor, chest band Residential power line
Refrigerator
CD/DVD player, television, and so
on.
22
Page 23

Table 4. Examples of household items with no distance restriction for EMI (continued)
Clothes iron Heating pad Satellite dish, receiving
Curling iron Home security system, infrared or
Sauna, electric
ultrasonic
Digital music player (for example,
Hot tub
iPod)
Dishwasher House arrest anklet
Electric blanket or electric mattress
Ionized bracelet Swimming pool
b
d
Smart scale with WiFi or Bluetooth
connectivity
Stove, kitchen
c
e
b
pad
Electronic weight scale Kiln, 115-120 V AC or 220-240 V AC Television
f
Flashlight Massage bed / chair / pad Toaster
a
Compare to hair shaver / trimmer in Table 9, page 25.
b
Hot tub and swimming pool must be properly grounded.
c
Smart scales that measure body composition (BMI) using an electrical current are not recommended.
d
Compare to house arrest bracelet. See Table 7, page 24.
e
60 cm (24 in) distance restriction from induction cooktops.
f
Maintain a 15 cm (6 in) distance from television speakers.
Table 5. Examples of professional and vocational items with no distance restriction for EMI
Anti-theft detection pedestals / electronic article sur-
Calipers, battery powered Laser level, battery oper-
ated
Pager, receiver only
veillance equipment for
retail loss prevention
Automobiles, electric
Automobiles, hybrid
Barcode scanner Hooded hair dryer, salonePhotocopier / copy
a
Safe when walking between the pedestals at normal walking speed. Do not linger near the detection equipment.
b
30 cm (12 in) distance from electric automobile battery charger.
c
A polygraph test introduces direct current into the body. This direct current poses a low risk of affecting a
a
b
d
Diesel engines Office calculator Polygraph / lie detector
c
test
Facsimile (fax) machine Office printer Soldering iron
f
Stud finder, battery oper-
machine
ated
pacemaker or ICD.
d
Compare to hybrid automobiles in Section 7.3.1, Vehicles with engines fueled by gasoline or petrol, page 26.
e
Compare to hair dryer, handheld in Table 7, page 24.
f
Compare to soldering gun; see Table 12, page 26.
Table 6.
Examples of recreational items with no distance restriction for EMI
Casino slot machine Motorcycle vest, heated Tanning booth, electrostatic
Electric golf cart
a
Maintain a 15 cm (6 in) distance from battery during charging.
a
Tanning bed
7.2 Items with a 15 cm (6 in) distance restriction from an implanted pacemaker or ICD
The following table represents items that, when used as intended and in good working condition, have a 15 cm
(6 in) distance restriction from an implanted pacemaker or ICD.
23
Page 24

Table 7. Examples of household items with 15 cm (6 in) distance restriction from an implanted pacemaker or ICD
Air filter, ionized Magnet, small Static electricity generator, “plasma
a
ball”
Amateur radio, ham radio, and
Magnetic back brace or belt Stereo speakers, from magnet
marine radio, < 3 W, from antenna
Canine shock collar for electric pet
containment fence, including
Magnetic cover for tablet computer Television audio headset, from
transmitter near television
remote control and base with
antenna
Clasp, magnetic Magnetic chair pad Tools, battery powered
Electric guitar speakers Magnetic therapy products Tools, small electric, from motor
Electric kitchen appliances, hand-
held
Exercise bicycle, wheel magnet Model cars, airplanes, video drones
Massager, handheld Toothbrush, electric, from charging
base
Toy train, electric, from transformer
— remote controlled, from controller
and rails
antenna
Hair dryer, handheld
b
Refrigerator door, from magnetic
Treadmill, from electric motor
closure strip
Home security system, microwave,
from transmitter
House arrest bracelet
c
Sewing machine or serger, from
motor
Smart meter (used by utility compa-
Ultrasonic or radio frequency pest
control device
Vacuum cleaner, from motor
nies)
a
Do not touch this item.
b
Compare to hooded hair dryer, salon in Table 5, page 23.
c
Compare to house arrest anklet; see Table 4, page 22.
Table 8. Examples of household wireless electronic devices with 15 cm (6 in) distance restriction from an implanted pacemaker or ICD
Activity band or wearable fitness
monitor, if device contains magnets
Earbuds, wireless (from magnet) Remote control, radiofrequency
(RF), for CD/DVD player, television,
and so on
Cellular adaptor for laptop computer eReader Remote keyless entry and remote
car starter key fob
Computer keyboard, wireless Gaming console and controllers Radiofrequency (RF) wireless
charger
Computer: personal, laptop, or tab-
Headphones, from magnets Smart watch
let
Cordless telephone, < 3 W, from
antenna and base station
a
CD/DVD/DVR player and recorder
with speakers
a
See also cordless telephone, 3 to 15 W, in Table 11, page 25
Network router Wi-Fi or cellular modem, from trans-
mitter/receiver
Qi inductive mobile telephone
charger
Caution: Do not carry a wireless device in a pocket or in a shoulder bag near a pacemaker or an ICD.
24
Page 25

Table 9. Examples of professional and vocational items with 15 cm (6 in) distance restriction from an implanted pacemaker or ICD
Badge (name tag) with magnetic
OnStar Technology, from antenna Tools, handheld battery powered
clasp
Badge (security) with externally
Pager, 2-way, ≤ 3 W, from antenna Tools, handheld electric, from motor
activated electronic circuit
Citizens band (CB) radio, ≤ 3 W,
from antenna
Cordless microphone, from trans-
mitter
Extractor wand, for automobile
mechanics
Hair shaver / trimmer, corded
a
Compare to hair shaver / trimmer, battery powered in Table 4.
a
Personal scooter / electric grocery
Security badge wall scanner
cart, from battery, during charging
Piconet wireless computer connec-
Tattoo machine
tor, from antenna
Portable radio (walkie-talkie), ≤ 3 W,
Telephone headset, cordless
from antenna
— —
Mobile telephones
Keep mobile telephones, cellular telephones, or smartphones at least 15 cm (6 in) from an implanted pacemaker
or ICD.
Keep magnetic accessories for mobile telephones at least 15 cm (6 in) from an implanted pacemaker or ICD.
Accessories with magnets can include wireless earbuds, plug-in earbuds, or cases with magnetic clasps.
Table 10. Sample of recreational items with 15 cm (6 in) distance restriction from an implanted pacemaker or ICD
Bingo wand Golf cart, electric, from battery dur-
Marine radio, < 3 W, from antenna
ing charging
Disney MagicBand reader
a
Laser tag, from magnet or transmitter in some vests
a
No distance restriction for Disney MagicBand.
7.3 Items with a 30 cm (12 in) distance restriction from an implanted pacemaker or ICD
The following table represents items that, when used as intended and in good working condition, have a 30 cm
(12 in) distance restriction from an implanted pacemaker or ICD.
Table 11. Examples of household items with 30 cm (12 in) distance restriction from an implanted pacemaker or ICD
Amateur radio, cordless telephonea,
ham radio, or 2-way portable radio, 3
to 15 W, from antenna and base station
Automobile battery charger for gasoline engines
a
Compare to cordless telephone, < 3 W, in Table 8, page 24.
Automobile battery charger / charging station for electric automobiles
Electrical transformer / transformer
box, residential
25
Lawn and garden tools powered by
gasoline / petrol, from ignition sys-
tem (for example, backpack leaf
blowers, snow blowers, chainsaws)
Page 26

Table 12. Examples of professional and vocational items with 30 cm (12 in) distance restriction from an implanted pacemaker or ICD
Cattle prod / stock prod, from electrodes
Degausser / demagnetizer Pagers, 2-way, 3 to 15 W, from
Marine radio, 3 to 15 W, from
antenna
antenna
Transmitters, portable 3 to 15 W,
from antenna
UPS (uninterruptible power source –
commercial power failure back-up
system) up to 200 A
Generators, electric, portable
Soldering gun
a
AC/DC, up to 20 kW
a
Compare to soldering iron, see Table 5, page 23.
7.3.1 Vehicles with engines fueled by gasoline or petrol
Observe the following precautions when using vehicles fueled with gasoline / petrol:
• Do not repair or perform maintenance work on an engine while it is running or when its ignition switch is on.
Repair or perform maintenance work on an engine when both the engine and its ignition switch are off.
• Maintain a 30 cm (12 in) distance between the implanted cardiac device and an engine that is running or that
has its ignition switch turned on.
Note: Diesel engines are safe for patients with an implanted pacemaker or ICD.
Table 13. Examples of vehicles with gasoline / petrol engines with a 30 cm (12 in) distance restriction from an
implanted pacemaker or ICD
All-terrain vehicle (ATV) Equipment / vehicles used for agri-
Motorcycle
culture or construction
Automobile / hybrid automobile
a
Forklift – also fueled by propane or
Snowmobile or snow machine
natural gas
Boat motor Jet ski Truck / lorry
a
Automobile / hybrid automobile have no distance restriction for drivers or passengers.
7.4 Items with a 60 cm (24 in) distance restriction from an implanted pacemaker or ICD
The following table represents items that, when used as intended and in good working condition, have a 60 cm
(24 in) distance restriction from an implanted pacemaker or ICD.
Table 14. Examples of items with a 60 cm (24 in) distance restriction from an implanted pacemaker or ICD
Household items
Amateur radio, ham radio, or walkie-talkie, 15 to
30 W, from antenna
Jumper cables, during use Residential satellite dish, 2-way
Professional and vocational items
Anti-theft tag deactivator GPS survey equipment
Bench-mounted / free-standing tools with motors
≤ 400 horsepower
Forklift, battery powered, from motor Welding equipment with less than 160 A (see Section 7.4.1,
Recreational items
Beach comber / metal detector, from detector
head
Stove, induction cooktop
Radio transmitters, vehicle-mounted, 15 to 30 W – from
antenna
Welding safety precautions, page 27)
Marine radio, single side band, 20–25 W, from antenna
26
Page 27

7.4.1 Welding safety precautions
Patients must observe the follow precautions with welding equipment at currents less than 160 A. (It is not
recommended that patients work with welding equipment at currents greater than 160 A.)
• Work in a dry area with dry gloves and shoes.
• Maintain a 60 cm (24 in) distance between the welding arc and the implanted device.
• Keep the welding cables close together and as far as possible from the implanted device. Place the welding
unit approximately 150 cm (5 ft) from the work area.
• Connect the ground clamp to the metal as close to the point of welding as possible. Arrange the work area so
that if the handle and rod are dropped, they will not contact the metal being welded.
• Wait several seconds between attempts when having difficulty starting a weld.
• Work in an area that offers firm footing and room for movement.
• Work with an informed person who understands these precautions.
• The patient must immediately stop welding and step away from the area if the patient becomes light-headed
or dizzy, or if an implanted ICD delivers a shock.
Note: Aprons or vests will not effectively shield a pacemaker or an ICD from EMI generated by welding equipment.
7.5 Items with low potential for EMI at extended distances from an implanted pacemaker or ICD
The following table lists communications items that have low potential for EMI when used as intended and in good
working condition. These items are safe for patients when their antennae are at, or greater than, the listed distance
from an implanted pacemaker or ICD.
Note: These distances assume free space and an unobstructed line-of-sight.
Table 15. Items with low potential for EMI at extended distances from an implanted pacemaker or ICD
Communications
1 m (3 ft) 2-way portable radio, from antenna – 30 to 50 W.
2 m (6 ft) 2-way portable radio, from antenna – 50 to 125 W.
3 m (9 ft) Amateur radio, ham radio, marine radio, or 2-way portable radio, from antenna – 125 to
250 W.
Cellular tower – ≤ 250 W.
Commercial broadcast towers – 125 to 250 W.
For transmitters with power levels > 250 W, avoid restricted areas that contain the
antenna.
4 m (12 ft) Amateur or ham radio, from antenna – 250 to 500 W.
6 m (20 ft) Amateur or ham radio, from antenna – 500 to 1000 W.
9 m (30 ft) Amateur or ham radio, from antenna – 1000 to 2000 W.
7.6 Items and environments with special considerations for EMI for patients with implanted pacemakers and ICDs
The information in this section discusses electrical equipment and environments that generate EMI that can affect
an implanted pacemaker or ICD. Share this information with patients who work with this equipment or in these
environments, or who can encounter these sources of EMI. Contact Medtronic Technical Services for additional
guidance regarding these environments.
Industrial equipment – The following industrial equipment and environments include high-voltage current,
magnetic fields, or other EMI sources that can affect device operation. Patients may need to avoid using or working
near the following categories of industrial equipment. Medtronic recommends that the employers of patients with
pacemakers or ICDs consult with clinicians before their employees return to work in these environments.
27
Page 28

• Electric furnaces used in the manufacturing of steel
• Induction heating equipment and induction furnaces, such as kilns
• Industrial magnets such as those used in surface grinding and electromagnetic cranes
• Dielectric heaters to heat plastic and dry glue in furniture manufacturing
• Electric arc and resistance welding equipment operating at greater than 160 A (see Section 7.4, Items with a
60 cm (24 in) distance restriction from an implanted pacemaker or ICD, page 26 for guidance with welding
equipment operating at less than 160 A)
• Broadcasting antennas for AM, FM, shortwave radio, and TV stations
• Microwave transmitters
• Power plants, power generators, and transmission power lines
Note: Lower-voltage distribution power lines for homes and businesses are unlikely to affect implanted
cardiac devices.
Anti-theft and security systems
Anti-theft systems – Anti-theft systems are unlikely to affect an implanted pacemaker or ICD. However, as a
precaution, do not linger near or lean against these systems. Walk past or through them at a normal pace. If you
experience symptoms, move away from the equipment. After you move away from the equipment, the device
resumes its previous state of operation.
Security systems – Metal detectors (walk-through archways and handheld wands) and full-body imaging
scanners (millimeter wave scanners, three-dimensional imaging scanners, or backscatter full body scanners)
are unlikely to affect an implanted pacemaker or ICD. These detectors and scanners are common in airports,
courthouses, and other high-security facilities.
When you encounter security systems, observe the following guidelines:
• Always carry your cardiac device ID card. If your cardiac device sets off a metal detector or a security system,
your card is helpful for security staff.
• To minimize the risk of temporary interference with your implanted pacemaker or ICD while going through the
security screening process, do not touch metal surfaces around any screening equipment.
• Do not stop or linger in a walk-through archway; simply walk through the archway at a normal pace.
• If a handheld wand is used, ask the security operator not to hold it over or wave it back and forth over your
implanted pacemaker or ICD.
• If you have concerns about security screening methods, show your cardiac device ID card to the security
operator, request alternative screening, and then follow the security operator’s instructions.
Shock from an electrical outlet (110 V / 220 V)
A momentary shock from an electrical outlet can inhibit pacing in a pacemaker or an ICD. A momentary shock
can reset some parameters to their nominal values. Any parameter changes that occur can be reprogrammed
during an office visit. There is a low risk of permanent damage to a pacemaker or an ICD from a momentary shock
from an electrical outlet.
A prolonged shock greater than 8 s can inhibit pacing in a pacemaker or an ICD, or it can cause delivery of a shock
in an ICD. A prolonged external shock greater than 2 s can cause reversion in a pacemaker. There is a low risk
of permanent damage to a pacemaker, ICD, or leads from a prolonged shock from an electrical outlet.
7.7 Non-EMI environments with special consideration for patients with implanted pacemakers and ICDs
This section includes important information to share with patients about home or work environments that can affect
an implanted pacemaker or ICD. Contact Medtronic Technical Services for additional guidance regarding these
environments.
28
Page 29

Air travel
Air travel in a pressurized cabin is safe for patients with an implanted pacemaker or ICD.
High altitude environments and activities
Medtronic implantable pacemakers and ICDs can withstand air pressure levels equivalent to an altitude limit of
6,000 m (20,000 ft). The following activities are safe for patients with an implanted pacemaker or ICD:
• Hiking, trekking, skiing or vehicle travel up to the altitude limit.
• Camping or extended stays up to the altitude limit.
Rifles, shotguns
Patients should consult their physician for advice and limitations for the use of rifles and shotguns. A rifle or
shotgun should be used on the shoulder that is opposite from the implant location.
Scuba diving, recreational diving
Medtronic implantable pacemakers and ICDs are rated for pressure levels up to 4.0 ATA (atmospheres absolute).
4.0 ATA is approximate to a seawater depth of 30 m (100 ft).
29
Page 30

Page 31

Page 32

Medtronic, Inc.
*M987654A001*
710 Medtronic Parkway
Minneapolis, MN 55432
USA
www.medtronic.com
+1 763 514 4000
Medtronic B.V.
Earl Bakkenstraat 10
6422 PJ Heerlen
The Netherlands
+31 45 566 8000
Canada
Medtronic Canada ULC
99 Hereford Street
Brampton, Ontario L6Y 0R3
Canada
1 800 268 5346
Technical manuals
www.medtronic.com/manuals
© 2021 Medtronic
M987654A001 B
2021-12-01
 Loading...
Loading...