Page 1

C-series
C60 DR
C20 SR
C-series VSF04 1.3 (Vitatron CareLink)
C60A1
C20A1
Reference Manual
Caution: Federal Law (USA) restricts this device to sale by or on the
order of a physician.
Page 2

Page 3

C-series Reference Manual
Contents
Part I General information . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
1 Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
1.1 About this manual . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
1.2 Programming instructions . . . . . . . . . . . . . . . . . . . . . . . . . . 8
2 The pacemaker . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9
2.1 Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9
2.2 Vitatron C60 DR (Model C60A1) . . . . . . . . . . . . . . . . . . . . . 9
2.3 Vitatron C20 SR (Model C20A1) . . . . . . . . . . . . . . . . . . . . . 9
2.4 Connector configuration . . . . . . . . . . . . . . . . . . . . . . . . . . 10
3 The patient . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11
3.1 Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11
3.2 Indications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11
3.3 Contraindications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11
3.4 Potential adverse events . . . . . . . . . . . . . . . . . . . . . . . . . . 12
3.5 Pacing code . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12
3.6 Mode selection decision tree . . . . . . . . . . . . . . . . . . . . . . . 13
3.7 Mode descriptions, indications and contraindications by
mode . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14
4 The programmer . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21
4.1 Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21
4.2 Getting started . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21
4.3 Adjusting the programmer settings . . . . . . . . . . . . . . . . . . 24
4.4 Pacemaker follow-up . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 29
4.5 Emergency programming . . . . . . . . . . . . . . . . . . . . . . . . . 42
4.6 Viewing and adjusting the ECG . . . . . . . . . . . . . . . . . . . . . 43
3
Page 4

C-series Reference Manual
Part II Follow-up and diagnostics . . . . . . . . . . . . . . . . . . . . . . 55
5 Follow-up . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 55
5.1 Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 55
5.2 Post-implant configuration . . . . . . . . . . . . . . . . . . . . . . . . . 55
5.3 Record an ECG . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 56
5.4 Program patient information . . . . . . . . . . . . . . . . . . . . . . . 56
5.5 Checks and programming . . . . . . . . . . . . . . . . . . . . . . . . . 57
5.6 Optimizing the pacemaker . . . . . . . . . . . . . . . . . . . . . . . . . 59
5.7 The ECG/EGM . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 60
5.8 Follow-up frequency and longevity . . . . . . . . . . . . . . . . . . 60
6 Optimizing pacing and sensing . . . . . . . . . . . . . . . . . . . . . . . 67
6.1 Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 67
6.2 Optimizing pacing . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 67
6.3 Optimizing sensing . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 72
6.4 VA interval measurement . . . . . . . . . . . . . . . . . . . . . . . . . 79
6.5 Temporary test . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 83
6.6 Lead measurement . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 85
7 Diagnostics . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 89
7.1 Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 89
7.2 Therapy Advisor . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 89
7.3 Data collection and storage periods . . . . . . . . . . . . . . . . . 90
7.4 Displaying diagnostic data . . . . . . . . . . . . . . . . . . . . . . . . . 92
7.5 Assessing atrial rhythm . . . . . . . . . . . . . . . . . . . . . . . . . . . 97
7.6 Assessing ventricular rhythm . . . . . . . . . . . . . . . . . . . . . . 100
7.7 Assessing AV synchrony . . . . . . . . . . . . . . . . . . . . . . . . . 104
7.8 Assessing rate response . . . . . . . . . . . . . . . . . . . . . . . . . 105
7.9 Assessing sensing . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 106
Part III Pacing therapies . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 113
8 An introduction to Vitatron pacing therapies . . . . . . . . . . . 113
8.1 Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 113
8.2 Basic pacing therapies . . . . . . . . . . . . . . . . . . . . . . . . . . 114
8.3 Pacemaker timing . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 114
4
Page 5

C-series Reference Manual
8.4 Lower rate pacing . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 115
8.5 Maximum rates . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 117
8.6 Refractory period . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 118
8.7 Blanking . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 120
8.8 Ventricular safety pacing (VSP) . . . . . . . . . . . . . . . . . . . . 123
8.9 Atrial hysteresis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 124
8.10 Interference management . . . . . . . . . . . . . . . . . . . . . . . . 127
9 Rate stability . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 129
9.1 Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 129
9.2 Atrial rhythm classification . . . . . . . . . . . . . . . . . . . . . . . . 129
9.3 Atrial tracking behavior . . . . . . . . . . . . . . . . . . . . . . . . . . 131
9.4 Bradyarrhythmia . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 132
9.5 Atrial tachyarrhythmia . . . . . . . . . . . . . . . . . . . . . . . . . . . 134
10 AV synchrony . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 139
10.1 Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 139
10.2 Paced and sensed AV delay . . . . . . . . . . . . . . . . . . . . . . 140
10.3 Adaptive AV delay . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 141
10.4 AV delay hysteresis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 143
10.5 Atrial synchronization pace (ASP) interval . . . . . . . . . . . 145
10.6 Retrograde conduction and PVC management . . . . . . . . 146
11 Rate response . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 153
11.1 Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 153
11.2 Activity sensor . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 153
11.3 Slope . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 154
11.4 Daily learning . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 155
11.5 Fast learning . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 157
11.6 Activity acceleration and deceleration . . . . . . . . . . . . . . . 158
Appendices . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 161
A Safety features . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 161
A.1 Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 161
A.2 Pacemaker restore . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 162
5
Page 6

C-series Reference Manual
B Precautions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 165
B.1 Effects of extreme conditions . . . . . . . . . . . . . . . . . . . . . 165
B.2 Area restrictions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 165
B.3 Environmental and medical therapy hazards . . . . . . . . . 165
C Product specifications Vitatron C60 DR, ............................. 171
C.1 Programming parameters . . . . . . . . . . . . . . . . . . . . . . . . 171
C.2 Technical parameters . . . . . . . . . . . . . . . . . . . . . . . . . . . 175
D Product specifications Vitatron C20 SR .............................. 177
D.1 Programming parameters . . . . . . . . . . . . . . . . . . . . . . . . 177
D.2 Technical parameters . . . . . . . . . . . . . . . . . . . . . . . . . . . 180
Abbreviations . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 183
Index . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 185
6
Page 7

C-series Reference Manual
Part I
General information
1 Introduction
1.1 About this manual
This Reference Manual contains an extensive description of the Vitatron C-series of
pacemakers (Vitatron C60 DR and Vitatron C20 SR).
For ease of use, the manual is divided into three parts.
In Part I, general information is given about the Vitatron pacing system. It begins with an
introduction to the manual (see Chapter 1), and a description of each pacemaker (see
Chapter 2). This is followed by a description of each available pacing mode, together
with the relevant indications and contraindications (see Chapter 3). How to carry
out common programming procedures and program the programmer preferences are
described in Chapter 4.
In Part II, follow-up and diagnostic features are discussed. Basic follow-up procedures
are described in Chapter 5. This is followed by a more detailed description of how to
optimize pacing and sensing characteristics (see Chapter 6). Advice on how to make
optimal use of the diagnostic features included in the pacemakers is given in Chapter 7.
In Part III, there is an extensive description of the pacing therapies. The basic pacing
therapies, including timing characteristics are described in Chapter 8. This is followed by
advice on maintaining rate stability (see Chapter 9), the importance of maintaining and
restoring AV synchrony (see Chapter 10) and rate response (see Chapter 11).
The appendices provide technical information. Safety features are described in
Appendix A and precautions are listed in Appendix B. In Appendix C and Appendix D
the programmable parameters of each individual pacemaker and their most important
specifications are listed.
7
Page 8

C-series Reference Manual Section 1.2
1.2 Programming instructions
The gray block at the beginning of some sections contains instructions for programming
the parameter. For example:
Parameters
⇒ Lower Rate…
⇒ Night Lower Rate
Range: 40 - (5) - 130 min
Availability: All modes, except OOO
The first line contains the name of the icon in the control panel (see Section 4.4). You
can press the value boxes named on the following lines to program the parameter.
The “Range” usually shows the lowest and highest values that you can program. The
number in brackets shows the programming steps within this range. In some cases you
can choose an option, for example “On” or “Off”.
The “Availability” line lists any restrictions on the use of the parameter, for example, in
which modes it is available.
–1
8
Page 9

C-series Reference Manual
2 The pacemaker
2.1 Introduction
The Vitatron C-series consists of a dual chamber pacemaker model (Vitatron C60 DR)
and a single chamber pacemaker model (Vitatron C20 SR). These pacemakers provide
an extensive range of therapies for the treatment of bradycardia.
Each pacemaker has a high quality ECG (EGM) and diagnostic tools which quickly
provide information about the effectiveness of pacemaker therapy and simplify follow-up
sessions.
Therapy Advisor automatically scans pacemaker data at the start of a follow-up session
(battery status, diagnostic data and programmed parameters). It immediately reports any
important events and gives suggestions for programming the pacemaker.
2.2 Vitatron C60 DR (Model C60A1)
The Vitatron C60 DR is a dual chamber rate responsive pacemaker (activity sensing
using an accelerometer) for permanent atrial and ventricular pacing. It has the following
features:
Beat-to-Beat mode switching enables the pacemaker to detect atrial arrhythmias
•
and respond immediately to them
Therapy Advisor, which provides clear and concise advice on pacemaker settings
•
and therapies
2.3 Vitatron C20 SR (Model C20A1)
The Vitatron C20 SR is a single chamber rate responsive pacemaker (activity sensing
using an accelerometer) for permanent atrial or ventricular pacing. It has the following
features:
9
Page 10

C-series Reference Manual Section 2.3
Therapy Advisor, which provides clear and concise advice on pacemaker settings
•
and therapies
2.4 Connector configuration
Vitatron digital pacemakers all have IS-1 connectors. Access to the connector screws
is from above for single chamber pacemakers and from the engraved side for dual
chamber pacemakers (see Figure 2-1).
Figure 2-1. Connector configuration
1 Dual chamber connection
2 Single chamber connection
10
Page 11

C-series Reference Manual
3 The patient
3.1 Introduction
Cardiac pacing is an accepted method of controlling heart rate in patients with
symptomatic bradyarrhythmias. Vitatron pacemakers are therefore intended for use in
patients for whom permanent cardiac pacing is indicated for the treatment of disorders in
impulse formation or conduction.
This chapter describes specific indications and contraindications, together with a
description of each of the available pacing modes.
3.2 Indications
Dual chamber pacing is indicated if AV synchrony needs to be restored to optimize cardiac
output (for example, in patients with symptomatic second or third degree AV block).
Dual chamber rate responsive pacing modes are of specific benefit to patients with
chronotropic incompetence of the sinus node.
Rate responsive modes can help patients who have a requirement for an increase in
pacing rate, in response to physical activity.
Single chamber ventricular pacing can help patients with permanent atrial
tachyarrhythmias, including atrial fibrillation and flutter.
Single chamber atrial pacing can help patients with symptomatic bradyarrhythmias and
normal AV conduction.
3.3 Contraindications
There are no known contraindications to the use of pacemakers as a means to control
the heart rate. The patient’s individual medical condition dictates which particular pacing
system and mode of operation is chosen by the physician.
Rate responsive modes may be contraindicated if they are expected to aggravate clinical
symptoms (angina pectoris for example) or congestive heart failure caused by fast heart
rates.
Pacemakers are contraindicated in the following situations:
dual chamber
•
11
Page 12

C-series Reference Manual Section 3.3
– permanent supraventricular tachyarrhythmias, including atrial fibrillation and
flutter
– expected aggravation of clinical symptoms (for example, angina pectoris) or
congestive heart failure caused by fast heart rates
– inadequate intracavitary atrial complexes
single chamber AAI(R)
•
– AV conduction disturbances
– inadequate intracavitary atrial complexes
single chamber VVI(R)
•
– known pacemaker syndrome
– a need for AV synchrony
– expected aggravation of clinical symptoms (for example angina pectoris) or
congestive heart failure caused by fast heart rates
3.4 Potential adverse events
Adverse events associated with pacemaker systems include: cardiac perforation, cardiac
tamponade, death, erosion through the skin, hematoma/seroma, infection, improper
operation caused by theft-prevention systems, myopotential sensing, nerve stimulation,
muscle stimulation, pacemaker syndrome, rejection phenomena (local tissue reaction,
fibrotic tissue formation, pacemaker migration), threshold elevation, and transvenous
lead-related thrombosis.
3.5 Pacing code
Pacemaker modes are described using the NBG code. The five-letter NBG1code,
named after The North American Society of Pacing and Electrophysiology (NASPE)
and the British Pacing and Electrophysiology Group (BPEG), describes the operation
of implantable pulse generators. The NBG code, which supersedes the ICHD Code, is
described in Table 3-1.
12
Page 13

C-series Reference Manual Section 3.5
Permanent Atrial
Fibrillation/Flutter?
Sinus Node Dysfunction
VVIR
AV Block AV Block
Paroxysmal Atrial
Fibrillation/Flutter?
DDDR + MS DDD(R) AAI(R)
Y N
Paroxysmal Atrial
Fibrillation/Flutter?
DDDR + MS DDD/VDD
Y N
Y N
Y
AV Block
Y N
Y
Y
Table 3-1. The Revised NASPE/BPEG Generic Code for Antibradycardia Pacing
Position: I II III IV V
Category: Chamber(s)
Manufacturers’
designation
Paced
O = None
A = Atrium
V = Ventricle
D = Dual
(A + V)
S = Single
(A or V)
Chamber(s)
Sensed
O = None
A = Atrium
V = Ventricle
D = Dual
(A + V)
S = Single
(A or V)
Response to
Sensing
O = None
T = Triggered
I = Inhibited
D = Dual
(T + I)
Rate
Modulation
O = None
R = Rate
modulation
Multisite
Pacing
O = None
A = Atrium
V = Ventricle
D = Dual
(A + V)
only:
Note: The programmer displays A or V (not S) for chambers paced and sensed.
3.6 Mode selection decision tree
The following basic decision tree is an aid in selecting the best pacing mode for a
particular patient.
Figure 3-1. Basic decision tree (from den Dulk, K et al. Selection of the optimal pacing mode. The
Netherlands Journal of Cardiology 1992; 5:214-225)
1
Bernstein A.D, et al., The Revised NASPE/BPEG Pulse Generator Code, Pace, 25, No 2, Feb 2002.
13
Page 14

C-series Reference Manual Section 3.7
3.7 Mode descriptions, indications and contraindications by mode
3.7.1 DDDR mode
The pacemaker senses and paces in both the atrium and the ventricle. Sensed atrial
events inhibit the atrial channel and start an AV delay. Sensed atrial events conducted to
the ventricles before the end of the AV delay inhibit the ventricular channel. Sensed atrial
events not conducted before the end of the AV delay trigger the release of a ventricular
stimulus (tracking of the atrial rate).
Paced atrial events also start an AV delay. Paced atrial events conducted to the ventricles
before the end of the AV delay inhibit the ventricular channel. Paced atrial events not
conducted before the end of the AV delay trigger the release of a ventricular stimulus.
In the absence of sinus rhythm and spontaneous AV conduction, both chambers are
paced at the sensor rate, the Flywheel rate, or the lower rate (whichever is highest).
In the presence of atrial tachyarrhythmias, Beat-to-Beat mode switching is initiated (the
ventricular rate is stabilized by rate responsive ventricular pacing). The atrial rate is
monitored on a beat to beat basis and AV synchronous pacing is restored as soon as
possible.
Indications:
chronotropic incompetence due to atrial bradyarrhythmia or AV block
•
sick sinus syndrome, including brady-tachy syndrome
•
paroxysmal atrial arrhythmias in patients who require restoration of AV synchrony
•
Contraindications:
permanent atrial tachyarrhythmias, including atrial fibrillation and flutter
•
expected aggravation of clinical symptoms (for example angina pectoris) or
•
congestive heart failure caused by fast heart rates
3.7.2 DDD mode
The pacemaker senses and paces in both the atrium and the ventricle. Sensed atrial
events inhibit the atrial channel and start an AV delay. Sensed atrial events conducted to
the ventricles before the end of the AV delay inhibit the ventricular channel. Sensed atrial
events not conducted before the end of the AV delay trigger the release of a ventricular
stimulus (tracking of the atrial rate).
14
Page 15

C-series Reference Manual Section 3.7
Paced atrial events also start an AV delay. Paced atrial events conducted to the ventricles
before the end of the AV delay inhibit the ventricular channel. Paced atrial events not
conducted before the end of the AV delay trigger the release of a ventricular stimulus.
In the absence of sinus rhythm and spontaneous AV conduction both chambers are
paced either at the Flywheel rate or the lower rate (whichever is highest).
In the presence of atrial tachyarrhythmias, Beat-to-Beat mode switching is initiated. The
atrial rate is monitored on a beat to beat basis and AV synchronous pacing is restored as
soon as possible.
Indications:
intermittent or complete AV block with normal sinus rhythm
•
sick sinus syndrome, including brady-tachy syndrome
•
paroxysmal atrial arrhythmias in patients who require restoration of AV synchrony
•
Contraindications:
permanent atrial arrhythmias, including atrial fibrillation and flutter
•
expected aggravation of clinical symptoms (for example angina pectoris) or
•
congestive heart failure caused by fast heart rates
3.7.3 DDIR mode
The pacemaker senses and paces in both the atrium and the ventricle. Atrial inhibition
does not trigger an AV delay. In the absence of spontaneous conduction to the ventricle
the pacemaker actively resynchronizes the atrium with the ventricle using an atrial
synchronization pace (ASP). The pacing rate is dictated by the sensor rate.
Indications:
atrial bradyarrhythmia in patients with paroxysmal atrial tachyarrhythmias, with or
•
without normal AV conduction
brady-tachy syndrome
•
Contraindications
complete AV block with normal sinus rhythm (allows retrograde P-wave sensing or
•
continuous atrial synchronization pacing)
3.7.4 DDI mode
The pacemaker senses and paces in both the atrium and the ventricle. Atrial inhibition
does not trigger an AV delay. In the absence of spontaneous conduction to the ventricle
15
Page 16

C-series Reference Manual Section 3.7
the pacemaker actively resynchronizes the atrium with the ventricle using an atrial
synchronization pace (ASP). The pacing rate is dictated by the programmed lower rate.
Indications:
atrial bradyarrhythmia in patients with paroxysmal atrial tachyarrhythmias, with or
•
without normal AV conduction
brady-tachy syndrome
•
Contraindications
complete AV block with normal sinus rhythm (allows retrograde P-wave sensing or
•
continuous atrial synchronization pacing)
3.7.5 DOO mode
The pacemaker provides asynchronous, AV sequential pacing at the programmed lower
rate.
Indications:
intended primarily as a temporary mode to reduce the likelihood of triggering or
•
inhibition during electrosurgery or electromagnetic interference
Contraindications:
intrinsic cardiac activity at a rate sufficient to cause competitive pacing
•
3.7.6 VDDR mode
The pacemaker senses in both the atrium and the ventricle but can only pace the
ventricle. It tracks spontaneous sinus rhythm and is inhibited by ventricular sensing.
In the absence of sinus rhythm, or in the presence of atrial tachyarrhythmias, rate
responsive ventricular pacing is initiated.
Indications:
intermittent or complete AV block with normal sinus rhythm, with or without
•
paroxysmal atrial tachyarrhythmia
Contraindications:
likelihood of loss of AV synchrony (atrial bradyarrhythmia) and associated
•
complications (retrograde conduction, anticipated or known pacemaker syndrome)
permanent atrial tachyarrhythmias, including atrial fibrillation and flutter
•
expected aggravation of clinical symptoms (for example angina pectoris) or
•
congestive heart failure caused by fast heart rates
16
Page 17

C-series Reference Manual Section 3.7
inadequate intracavitary atrial complexes
•
3.7.7 VDD mode
The pacemaker senses in both the atrium and the ventricle but can only pace the
ventricle. It tracks spontaneous sinus rhythm and is inhibited by ventricular sensing. In
the absence of sinus rhythm, or in the presence of atrial tachyarrhythmias, ventricular
(VVI) pacing at the programmed lower rate is initiated.
Indications:
intermittent or complete AV block with normal sinus rhythm, with or without
•
paroxysmal atrial tachyarrhythmia
Contraindications:
likelihood of loss of AV synchrony (atrial bradyarrhythmia) and associated
•
complications (retrograde conduction, anticipated or known pacemaker syndrome)
permanent atrial tachyarrhythmias, including atrial fibrillation and flutter
•
inadequate intracavitary atrial complexes
•
3.7.8 VVIR mode
The pacemaker senses and paces in the ventricle and is inhibited by sensed ventricular
events. In the absence of spontaneous ventricular rhythm, rate responsive ventricular
pacing is initiated.
Indications:
permanent atrial fibrillation and flutter with symptomatic ventricular bradyarrhythmia
•
Contraindications:
expected aggravation of clinical symptoms (for example angina pectoris) or
•
congestive heart failure caused by fast heart rates
anticipated or known pacemaker syndrome
•
a need for the restoration of AV synchrony
•
3.7.9 VVI mode
The pacemaker senses and paces in the ventricle and is inhibited by sensed ventricular
events. In the absence of spontaneous ventricular rhythm, ventricular pacing at the
programmed lower pacing rate is initiated.
Indications:
17
Page 18

C-series Reference Manual Section 3.7
permanent atrial fibrillation and flutter with symptomatic ventricular bradyarrhythmia
•
Contraindications:
anticipated or known pacemaker syndrome
•
a need for the restoration of AV synchrony
•
3.7.10 VVT mode
The pacemaker paces and senses in the ventricle. Operation is identical to the VVI mode
except that events sensed during the ventricular escape interval trigger an immediate
pacing pulse.
Indications:
intended as a temporary diagnostic mode, used to verify sensing and evaluate
•
arrhythmias. This mode may also be useful in preventing inappropriate inhibition in
the presence of electromagnetic interference.
Contraindications:
anticipated or known pacemaker syndrome
•
a need for the restoration of AV synchrony
•
3.7.11 VOO mode
The pacemaker paces in the ventricle at the programmed lower rate (asynchronous
ventricular pacing). It is not inhibited by sensed ventricular events.
Indications:
intended primarily as a temporary mode to reduce the likelihood of triggering or
•
inhibition during electrosurgery or electromagnetic interference
Contraindications:
intrinsic cardiac activity at a rate sufficient to cause competitive pacing
•
3.7.12 AAIR mode
The pacemaker senses and paces in the atrium and is inhibited by sensed atrial events.
In the absence of spontaneous rhythm, rate responsive atrial pacing is initiated.
Indications:
atrial bradyarrhythmia with normal AV conduction
•
Contraindications:
18
Page 19

C-series Reference Manual Section 3.7
AV conduction disturbances
•
atrial fibrillation and flutter
•
expected aggravation of clinical symptoms (for example angina pectoris) or
•
congestive heart failure caused by fast heart rates
inadequate intracavitary atrial complexes
•
3.7.13 AAI mode
The pacemaker senses and paces in the atrium and is inhibited by sensed atrial events.
In the absence of spontaneous atrial rhythm, atrial pacing at the programmed rate is
initiated.
Indications:
atrial bradyarrhythmia with normal AV conduction
•
Contraindications:
AV conduction disturbances
•
atrial fibrillation and flutter
•
inadequate intracavitary atrial complexes
•
3.7.14 AAT mode
The pacemaker paces and senses in the atrium. Operation is identical to the AAI mode
except that events sensed during the atrial escape interval trigger an immediate pacing
pulse.
Indications:
intended as a temporary diagnostic mode, used to verify sensing and evaluate
•
arrhythmias. This mode may also be useful in preventing inappropriate inhibition in
the presence of electromagnetic interference.
Contraindications:
inadequate intracavitary atrial complexes
•
3.7.15 AOO mode
The pacemaker paces in the atrium at the programmed lower rate (asynchronous atrial
pacing). It is not inhibited by sensed atrial events.
Indications:
19
Page 20

C-series Reference Manual Section 3.7
intended primarily as a temporary mode to reduce the likelihood of triggering or
•
inhibition during electrosurgery or electromagnetic interference
Contraindications:
intrinsic cardiac activity at a rate sufficient to cause competitive pacing
•
AV conduction disturbances
•
3.7.16 OOO mode
In the OOO mode pacing is switched off.
Indications:
used for diagnostic purposes, such as the analysis of underlying rhythm
•
Contraindications:
patients with no underlying rhythm
•
20
Page 21

C-series Reference Manual
4 The programmer
4.1 Introduction
Vitatron C-series pacemakers can be programmed with a Vitatron CareLink programmer
with Vitatron C-series software. This manual only describes the software for the Vitatron
C-series. For specific programmer information, please refer to the programmer manual
which is provided with the programmer.
This chapter, which describes how to perform various tasks using the programmer, is
divided into five sections:
getting started (see Section 4.2)
•
adjusting the programmer settings (see Section 4.3)
•
starting a follow-up session, programming the pacemaker and general use of the
•
programmer (see Section 4.4)
emergency programming (see Section 4.5)
•
viewing and adjusting the ECG (see Section 4.6)
•
Notes:
Programmers other than the Vitatron CareLink are not compatible.
•
When using a second programmer during the same follow-up session, the first
•
session must be ended before the second begins.
The screens in this chapter show examples based on dual chamber pacemakers,
•
and are subject to minor changes. The screens for single chamber pacemakers
have a simpler layout because many features are not applicable to all models.
Warning: Pacemaker programming should be done only after careful study of
the Pacemaker Manual and after determination of the appropriate parameter
settings. Improper use of the programmer could result in erroneous or inadvertent
programming and improper operation of the telemetry and measurement functions.
4.2 Getting started
After switching the programmer on the Vitatron desktop appears.
21
Page 22
C-series Reference Manual Section 4.2
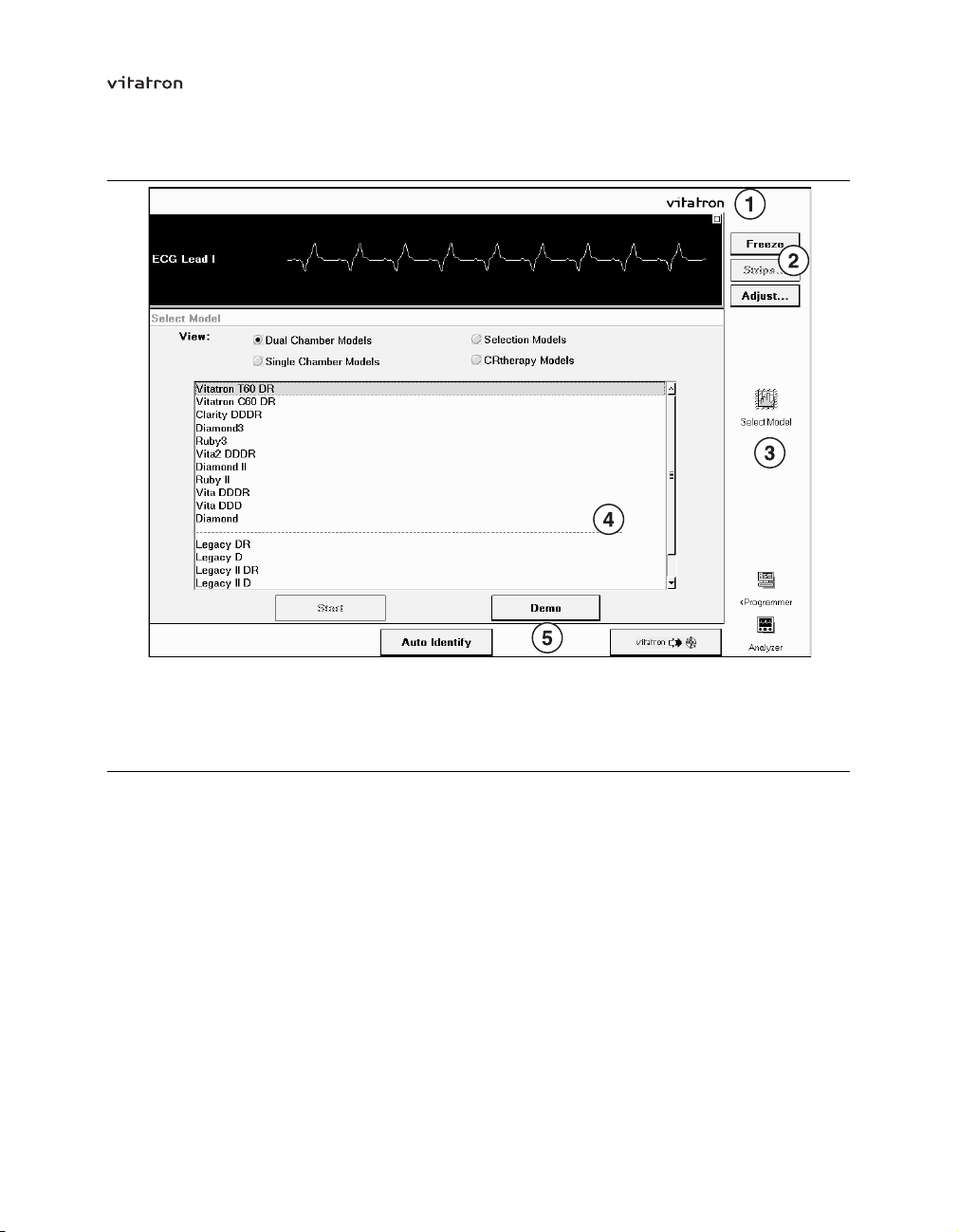
Figure 4-1. The Vitatron desktop
1 Top line
2 ECG window and controls
3 Control panel
4 Main window
5 Button line
The main parts of the desktop are described briefly in this section. The task bar, which
appears above the top line, is described in the programmer manual.
4.2.1 Top line
The desktop always shows the Vitatron logo on the top line. After a programming session
is initiated, the applicable pacemaker model number is also shown. The top line is not
shown in the illustrations used in this chapter.
4.2.2 ECG window and ECG controls
While the desktop is active, the programmer continuously displays the default surface
Electrocardiogram (ECG, lead I, II or III) in the ECG window.
22
Page 23

C-series Reference Manual Section 4.2
The ECG controls on the right allow you to freeze the ECG, adjust the various ECG
settings and ECG markers or recall previously stored ECGs. For a detailed explanation
of these features see Section 4.6.
For instructions on connecting the ECG cable and leads, refer to the relevant programmer
manual.
4.2.3 Control panel
This panel, on the right of the desktop, contains (in addition to the ECG controls) the
following icons:
“Select Model” is used to launch a simulated programming session (demo) - see
•
Section 4.2.4.
“Programmer” gives access to programmer settings - see Section 4.3.
•
“Analyzer”. If the Medtronic lead analysis software and hardware are installed on the
•
programmer, the Vitatron desktop will contain the “Analyzer” icon. Clicking the icon
starts the analyzer program. After ending the analyzer program the programmer
restarts the Vitatron software. For more information about the analyzer please refer
to the documentation provided with it.
4.2.4 Main window
At start-up the main window always contains the Select Model window, which is used
for demonstration purposes. Select a model and press [Demo] to launch a simulated
programming session for the pacemaker in question. A pacemaker follow-up session is
usually started by pressing [Auto Identify]. The [Start] button can only be used to launch
applications that are not started with auto identify.
4.2.5 Button line
The bottom line normally contains two buttons:
[Auto Identify]. Pressing this button starts automatic recognition and interrogation
•
of the pacemaker.
Vitatron to Medtronic switch, which is used to go from Vitatron to Medtronic
•
applications and vice versa.
23
Page 24

C-series Reference Manual Section 4.3
4.3 Adjusting the programmer settings
Prior to launching pacemaker applications you are given the opportunity to change the
main programmer settings. Selecting “Programmer” reveals the following list of options:
Programmer preferences
•
Time and date
•
Software
•
Memory contents files
•
Reload session data
•
4.3.1 Setting programmer preferences
This window allows you to set one or more of the following programmer preferences.
Figure 4-2. Programmer Preferences window
Language – To change the language, press the value box and select the desired
language from the list. The change takes immediate effect.
24
Page 25

C-series Reference Manual Section 4.3
Audio – To mark certain events (for example, programming confirmed, start/end
emergency, end test, error) audible signals are used. The audio option allows you to
switch the sound on or off. To do this press the “Audio” value box and select the desired
option (Off, Low, Medium or High).
If the sound is switched off, only emergency beeps will still be audible. The last three
options are equivalent to “On” and do not provide different volume levels.
Therapy Advisor – This allows you to switch the Therapy Advisor on or off.
Printer – This option is used to select the printer, which is either the built-in (thermal)
strip printer (the default setting) or a full-size external printer. If the full-size printer is
selected, you can select the printer type from a drop-down list of all supported printers. A
number of other print options are also listed:
Number of copies
•
The default number of copies to be printed is set using this option.
Pop-up print options dialog when any print button is selected
•
If this option is activated, every time you click a [Print] button in any window, the
Print - Options window is opened, in which you can overrule the preference settings
for a particular print job.
Auto print initial interrogation report
•
If this option is switched on (the default setting) the results of the initial pacemaker
interrogation are printed as soon as they are available.
You can also adjust the printer preferences during a follow-up session by selecting the
“Session” icon (see Section 4.4.6).
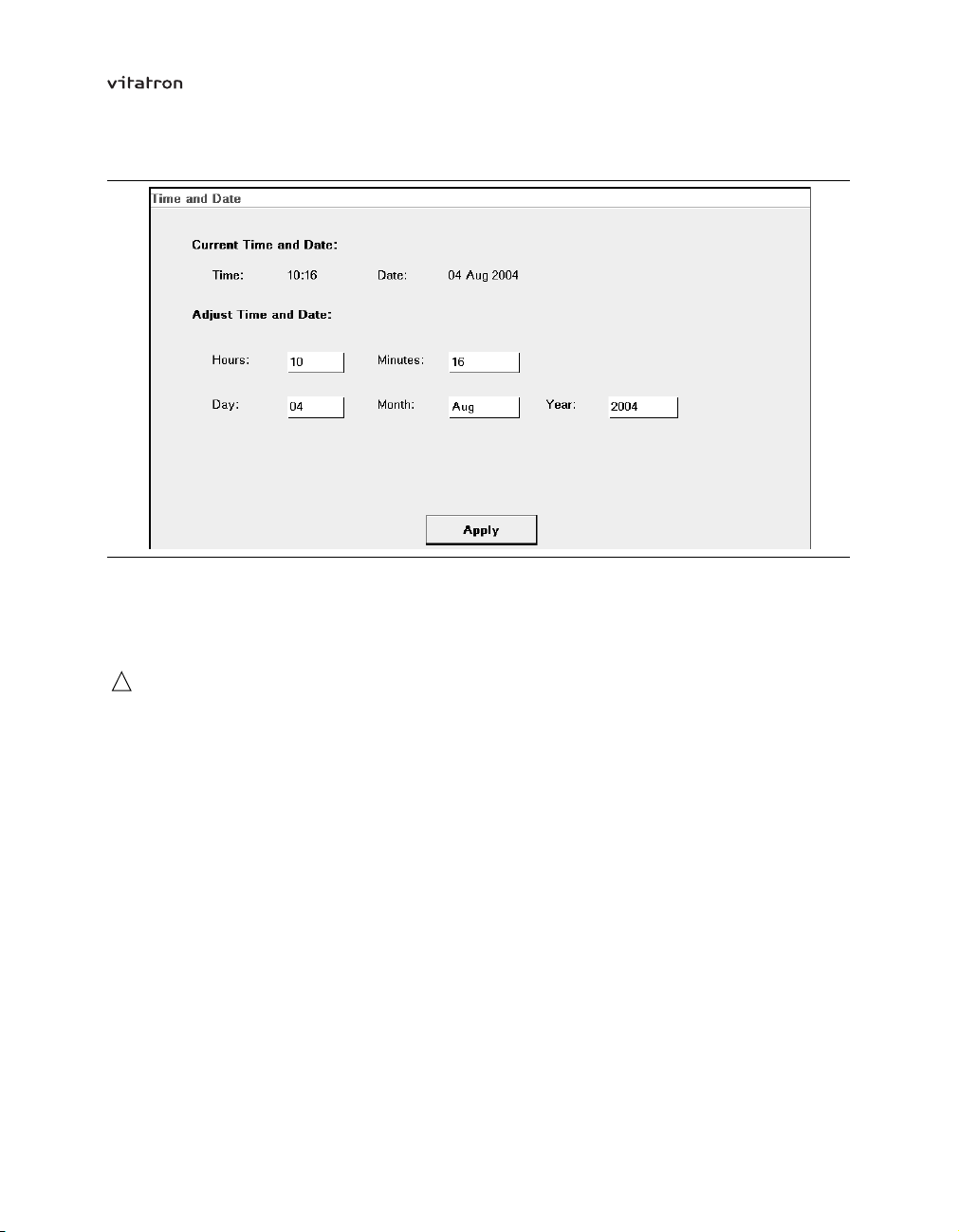
4.3.2 Adjusting time and date
This option allows you to adjust the current time and date in the programmer.
25
Page 26
C-series Reference Manual Section 4.3
Figure 4-3. Time and Date window
To change the programmer time or date, press the relevant value box and select the time
or date. Press [Apply] to apply the changes. Press another icon to leave the window
without making any changes.
Caution: The programmer clock is battery-powered so if the battery is depleted the
date and time will be incorrect and should not be used to set the pacemaker time. A
warning to this effect will be given by the programmer.
4.3.3 Checking software release numbers
The Software window shows the version numbers and service release numbers of the
currently installed Vitatron software.
4.3.4 Managing memory contents files
The Memory Contents Files window lets you copy pacemaker memory files (memory
dumps) from the programmer hard disk to diskette. This can be useful in the case
of programming difficulties, if the pacemaker behavior cannot be interpreted, or if a
pacemaker malfunction is suspected. In such cases, the programmer often generates a
memory contents file. Availability of this file enables Vitatron specialists to evaluate the
pacemaker status and assist during follow-up.
26
Page 27

C-series Reference Manual Section 4.3
Figure 4-4. Memory Contents Files window
All stored pacemaker memory contents files are listed. Each file name starts with an
eight-digit number followed by a year code; if more than one file is listed the one with
the highest number is the newest for that particular year.
To copy a selected file from the programmer to a disk, press [Copy to Diskette].
Use [Delete] to remove a selected file from the programmer.
Cautions:
Make sure only virus-free diskettes are used!
•
Remove the diskette from the disk drive before you turn the programmer off. Do
•
not switch the programmer on if a diskette is in the disk drive.
4.3.5 Reloading session data
Using this feature you can reload session data that has previously been saved to diskette
(see Section 4.4.9). This enables you to perform the following actions:
Analyze (and compare) data from previous follow-ups.
•
Run demo follow-up sessions using different patient profiles.
•
If you choose the reload session data option you are asked to insert the relevant diskette
into the programmer disk drive. The programmer subsequently displays a list of all
session export files stored on the diskette.
27
Page 28

C-series Reference Manual Section 4.3
Figure 4-5. Reload Session Data window
Select the desired file and then press [Reload Data]. This loads the patient data and
allows you to analyze the follow-up data or conduct a demo follow-up session.
Figure 4-6. Example of a Reloaded Data Parameters Therapy window
Reloaded sessions can be identified by the text “Reloaded Data” in the top line and by
the fact that during a reloaded session ECG recordings are shown as a flat line. The
reloaded sessions only contain the data that was read out during initial interrogation of
the pacemaker. The results of any subsequent programming actions or measurements
carried out during the follow-up session are not displayed, although they are stored on
the diskette and can be accessed using commercially available software.
28
Page 29

C-series Reference Manual Section 4.3
During a reloaded session you can simulate a follow-up session and analyze the data.
You can also “reprogram” pacing parameters; any changes may be reflected in the
information presented on the programmer or in reports during the reloaded session.
When you press [End] and return to the Vitatron desktop, all changes will be discarded.
You cannot change the contents of the file on the diskette.
4.4 Pacemaker follow-up
To start automatic pacemaker recognition press [Auto Identify] and position the
programming head. This starts initial interrogation of the pacemaker. Press [Stop] to
return to the Select Model window.
When interrogation is complete (indicated by a progress bar), the Status window shows
the most important pacemaker settings, as well as lead and battery information and
Therapy Advisor messages. The top left-hand corner of the ECG window also shows the
current heart rate (paced or sensed) and the corresponding interval in milliseconds. This
information is derived from the ECG markers.
Figure 4-7. Status window
29
Page 30
C-series Reference Manual Section 4.4
The control panel icons are used to access stored information and to perform
programming and test functions. These icons are described in the rest of this section.
During a follow-up session, the bottom line normally contains two buttons:
The [Emergency] button is always active during a follow-up session. When pressed
•
it programs the pacemaker to emergency settings (see Section 4.5).
The [End Session] button allows you to close the follow-up session (see
•
Section 4.4.7). There is also an option to save pacemaker data to diskette before
closing the session.
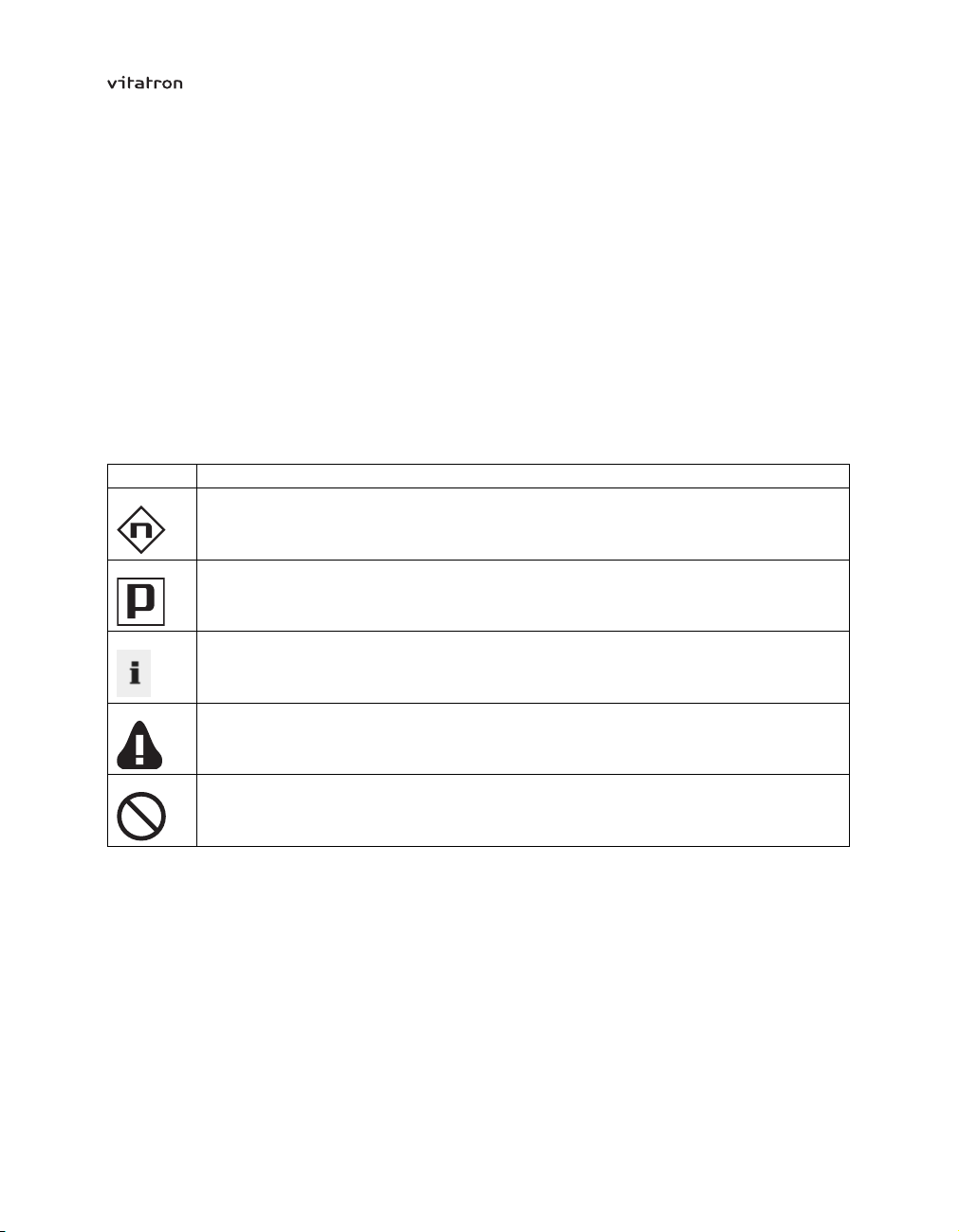
A number of symbols may appear on the screen during interrogation and programming of
the pacemaker. These are listed in Table 4-1.
Table 4-1. Programmer symbols
Symbol
Description
Indicates the nominal (delivery) value of the parameter concerned.
Indicates the currently programmed value of the parameter concerned.
Indicates that more information is available. This information will appear if the icon is
pressed.
Warns of a possible undesirable interaction with other parameters.
Warns that certain parameters are not programmable, or that certain values are not
allowed because of a conflict with other parameters.
It is always advisable, after initial interrogation of the pacemaker, to print a copy of the
pacemaker status for later reference. If the “Auto Print Initial Interrogation Report”
preference is on (see Section 4.3.1) this is done automatically. If not, just press the
[Print] button.
30
Page 31

C-series Reference Manual Section 4.4
Notes:
You cannot program parameters in this window. Select the “Params” icon to change
•
parameter values.
If the programmer is unable to identify the pacemaker the following message is
•
displayed: “Position programming head”.
In the unlikely event that more than one pacemaker is in close proximity to the
•
programming head, the programmer will warn you that more than one pacemaker
has been detected. The pacemakers are then listed and you are asked to select the
one to be interrogated.
4.4.1 Viewing pacemaker data and diagnostics
Selecting the “Data” icon calls up the following list of options:
Status – shows the most important programmed parameter values, lead data, battery
information and patient information, as they were at the start of the session.
Rhythm Overview – gives an overview of pacemaker diagnostics (rhythm characteristics)
and access to more detailed diagnostic information (Holters and histograms).
Battery Status – provides a remaining longevity estimate and measured battery data.
Diagnostic Set-up – allows you to retain data collected since the last follow-up (which is
otherwise automatically cleared one hour after the programming session ends).
For a detailed description of these features refer to Chapter 5 and Chapter 7.
4.4.2 Programming therapy parameters
Select the “Params” icon to see the Parameters Therapy window.
31
Page 32

C-series Reference Manual Section 4.4
Figure 4-8. Parameters Therapy window
To program a parameter, for example, atrial amplitude, press the parameter value box
on the right of the parameter name. A value selection window appears. The currently
programmed value, for example, 2.50 V, is highlighted and followed by a boxed [P] (see
Figure 4-9).
Figure 4-9. Selecting amplitude programming
32
Page 33

C-series Reference Manual Section 4.4
Select a new value, for example, 4.00 V. The value selection window closes. The new
value is boxed to indicate that it is pending and has not yet been programmed (see
Figure 4-10).
Figure 4-10. The chosen value is pending
To program the new value, press [Program] on the bottom right. The box around the
pending value disappears.
Press [Undo Pending] to cancel the pending parameters.
If you open a value selection window and then decide not to select a new value, you can
close the window either by pressing [Close] or by pressing outside the window.
Some parameter names (for example, Mode Switching…) are followed by three dots,
which indicate the presence of a list of related programmable parameters.
If one or more parameters are pending and you try to open another window, a warning
appears asking you to either program or cancel the pending values.
Batch programming – It is also possible to program several parameters in one batch.
To do this select a new value for each parameter you wish to program. All pending
parameter values are then boxed. Individual parameters can subsequently be changed
before final programming.
33
Page 34

C-series Reference Manual Section 4.4
Figure 4-11. Batch programming
Now press [Program]. The values are unboxed, indicating that the corresponding
parameters have been reprogrammed. Press [Undo Pending] to cancel all pending
parameters.
Note: If power to the programmer is unexpectedly lost, removing the programming head
from the pacemaker cancels any temporary features and restores the pacemaker to its
permanently programmed state. Loss of power during permanent programming of a
parameter cancels the programming action. After the programmer is switched back on
and the appropriate application is started, the programming action must be repeated.
If power is lost before permanent programming of batched parameters can be completed,
all reprogramming is cancelled. All parameters then keep the values they had before the
batch programming was started. After restarting the programmer the batch programming
must be repeated.
If power is lost during a follow-up session, the start of session values in the programmer
memory are lost. When the programmer is restarted, the pacemaker is reinterrogated,
giving new start of session values.
Parameter pertinency – Only the parameter values applicable to a selected feature or
mode, for example, atrial amplitude in the AAI mode, are shown. This is called parameter
pertinency.
34
Page 35

C-series Reference Manual Section 4.4
For example, if the pacemaker is in the DDD mode and the atrial amplitude is prepared
for reprogramming from 3.75 V to 2.50 V, the new value is boxed to indicate that it is
pending. If the mode is then changed to VVI, the boxed atrial value of 2.50 V disappears.
However, pressing [Program] results in permanent programming of both the VVI mode
and the atrial amplitude. Following any subsequent reprogramming to an atrial or dual
chamber mode the atrial amplitude will be 2.50 V.
Caution: If you select a pending value for any parameter and then select a new
mode, to which the parameter concerned is not pertinent, the pending value
disappears. However, it is still pending and will be permanently programmed if you
press [Program]. To prevent this, press [Undo Pending].
Nominal programming – Nominal programming is used to change all parameters to
nominal (delivery) values (refer to the product specification in the appendices) or the
settings at the start of the follow-up session.
For nominal programming, press [Revert…] on the bottom left of the Parameters Therapy
window.
Figure 4-12. Revert to Nominal Parameters window
Now choose between “Nominals” and “Settings at Start of Session” and press
[Copy to Params]. The programmer returns to the Parameters Therapy window and all
relevant parameters are boxed showing their new values.
Press [Program] to change all relevant parameters to nominal settings or to the settings
at the start of the session. Press [Undo Pending] to cancel all pending parameters.
To cancel individual pending parameters select the relevant value box and press
[Undo Pending]. In both cases the pending values are then unboxed.
4.4.3 Performing tests
Selecting the “Tests” icon displays the following list of measurements:
35
Page 36

C-series Reference Manual Section 4.4
Threshold Test
•
Sensing Test
•
VA Interval Measurement
•
Fast Learn
•
Temporary Test
•
Lead Measurement
•
For a detailed description of these tests refer to Chapter 6 and to Chapter 11.
4.4.4 Printing reports
Selecting the “Reports” icon takes you to the Reports window (see Figure 4-13), where
you can print reports or define sets of reports for later use.
Figure 4-13. Reports window
The Reports window provides a list of all available reports (left) and all selected reports
(right). The available reports include all the reports that have been generated during
the current session.
To add one or more reports to the list of selected reports, select the name in the available
reports list and press [--->]. To remove a report from the selected reports list, select
its name and press [<---].
36
Page 37

C-series Reference Manual Section 4.4
Press [Print] to print the selected reports on the built-in or external printer.
You can save the set of selected reports for use in future follow-up sessions by
pressing [Save Set…]. Select “New Report”. Give the new report set a name in the
Name/Description value box, and press [Save/Replace] (see Figure 4-14).
Figure 4-14. Save Reports Preference window
Use [Save Session…] to save all session data to diskette (see Section 4.4.9).
4.4.5 Entering patient information
To enter patient data and pacing system information into the pacemaker, select the
“Patient” icon.
37
Page 38

C-series Reference Manual Section 4.4
Figure 4-15. Patient Information window
Patient identification – To enter the patient’s name and ID number, press the
corresponding value box. You can now enter the patient’s name and ID number (both will
accept a maximum of 20 characters) using the on-screen keyboard.
When using the on-screen keyboard press the appropriate characters to select them.
Use the backspace key [<-] to delete the last entered character (you can also delete
characters by selecting them with a sliding movement of the touch pen and then pressing
the backspace key).
Confirm the patient’s name or code by pressing [Enter] or press [Cancel] to leave the
window without programming a name or code. A confirmed name or code is boxed in
the value box, indicating that it is pending.
To enter the patient’s date of birth, press the appropriate value boxes for day, month
and year and then select the correct dates.
Indications for implant – A number of boxes are provided to enter the following
information:
(pacemaker) dependency (yes or no)
•
symptoms
•
indications (atrial or other)
•
indications (AV or ventricular)
•
38
Page 39

C-series Reference Manual Section 4.4
etiology
•
In the value boxes select the indication appropriate for the patient or select “Unspecified”.
Pacemaker time – Here you can alter the pacemaker time (24-hour clock) by pressing
the appropriate value boxes (hours and minutes) and selecting the correct values.
Be aware that changing the pacemaker time clears all diagnostic data stored in the
pacemaker memory. Diagnostic data collected before the change can still be displayed
during the current follow-up session.
Notes – This space is provided so that any additional notes may be added (with a
maximum of 80 characters).
Devices implanted – The programmer automatically displays the pacemaker model
number, serial number and implant date. The implant date can be changed by the user.
Leads – Press this value box to open a secondary window where you can enter the lead
manufacturer, model name, serial number and implant date for each lead.
Physician information – The physician’s name and phone number can be entered here.
Saving patient information – Press [Program] to enter data into the pacemaker. Press
[Undo Pending] to cancel entering patient or pacing system data.
4.4.6 Selecting printer preferences
To change the printer preferences during a follow-up session, select the “Session” icon.
You can select the printer, which is either the built-in (thermal) strip printer (the default
setting) or a full-size external printer. Selecting the full-size printer opens a drop-down list
of all supported printer types (see Figure 4-16). Preferences changed during a follow-up
session become the default settings.
39
Page 40

C-series Reference Manual Section 4.4
Figure 4-16. Printer Preferences window
If you check “Pop-up print options dialog when any print button is selected” you will have
the option to print a full report or current page report every time you press [Print]. The
current page prints only the information in the window that is currently displayed.
For a description of the other printer preference options, see Section 4.3.1.
4.4.7 Ending a follow-up session
To end a programming session just press [End Session…].
Figure 4-17. End/Save Session window with example warning
If applicable a warning is given that programming has not been completed or that a print
job is still in process. A [Save Data…] option allows you to save pacemaker information
40
Page 41

C-series Reference Manual Section 4.4
to a diskette (see Section 4.4.9). This makes it possible to do an “off-line” analysis of the
data by reloading the data at a later stage (see Section 4.3.5).
Confirm that you wish to end the session by pressing [End Now]. To continue with the
current programming session press [Cancel].
Applying the programming head to another pacemaker without switching the programmer
off or without pressing [End Session…] automatically opens the End Session window. If
the session is then ended you return to the Vitatron desktop, and all information stored in
the programmer memory is cleared.
4.4.8 Printing pacemaker data
The [Print] button can be used to print the currently displayed data on the built-in strip
printer or an external printer.
After printing data on the (thermal) strip printer Vitatron recommends that you make
photocopies of printed data (the quality of printing on thermal paper diminishes with time).
4.4.9 Saving pacemaker (session) data to disk
Session data files allow you to save follow-up data to a DOS-formatted diskette. The
saved file contains all data that has been interrogated during the follow-up session. This
includes device data at initial interrogation and all valid parameter data at the moment
the session data file was saved. With a session data file, it is possible to do an “off-line”
analysis of the data by reloading the data at a later stage (see Section 4.3.5).
The session data file also includes the contents of the pacemaker memory as read at
initial interrogation. This information can be useful for Vitatron specialists, in situations
where analysis of the pacemaker function is required.
To save session data, press [End Session…]. Press [Save Data], insert a diskette into
the programmer diskette drive and then press [Start]. The programmer automatically
generates a file name using the current date and time.
You can also save session data by selecting the “Reports” icon. Press [Save Session…],
insert a diskette into the programmer diskette drive and then press [Start]
41
Page 42

C-series Reference Manual Section 4.4
Figure 4-18. Save Session Data to Diskette window
Cautions:
Make sure only virus-free diskettes are used!
•
Remove the diskette from the disk drive before you turn the programmer off. Do
•
not switch the programmer on if a diskette is in the disk drive.
Keep the programming head and any other (electro)magnetic devices away from
•
diskettes; this may erase data stored on the diskettes.
Do not modify the session data file in other applications because the file will
•
become unreadable to Vitatron applications. Vitatron is not responsible for the
inappropriate use of data saved to diskette.
4.5 Emergency programming
If an error occurs, or if you make a mistake during programming, first try to correct it using
normal programming procedures. If this fails press [Emergency] on the programmer to
force the pacemaker to function with the emergency settings listed in Table 4-2. All
other pacing therapy parameters will be programmed to nominal (delivery) settings (refer
to the product specification in the appendices). The programmer will stop all current
activities and restart the follow-up session by interrogating the pacemaker again (see
Section 4.4). Diagnostic data collection stops; diagnostic information is not lost, but
remains in the programmer memory.
As soon as the emergency settings have been programmed, the Status window appears
and all functions are available. You should then reprogram the pacemaker to settings
appropriate for the patient.
42
Page 43

C-series Reference Manual Section 4.5
Note: When programming emergency settings could cause battery depletion, the
programmer first programs the emergency settings, then gives a warning that higher
power consumption may reduce the time remaining before pacemaker replacement
is required. Vitatron recommends that you decrease the output settings. Refer to
Section 5.8 if the output settings are not decreased.
Table 4-2. Emergency settings
a
Mode
Lower rate 60 min
Pulse duration
Pulse amplitude 7.5 V 5.0bV
Sensitivity 2.0 mV 0.7 mV
Refractory period
Polarity (pacing and sensing) unipolar unipolar
a
Mode is VVI, except for single chamber pacemakers programmed to AXX mode.
b
Keeps value if greater than 5 V.
VVI AAI
–1
1.0 ms 1.0 ms
400 ms 400 ms
60 min
–1
Warning: For patients with a co-implanted implantable cardiac defibrillator (ICD),
emergency programming can lead to undesirable interaction with the ICD due to
unipolar pacing.
Cautions:
Emergency programming initiated from Vitatron C-series software only works
•
with Vitatron C-series pacemakers.
Other Vitatron software applications cannot be used for emergency programming
•
of Vitatron C-series pacemakers.
4.6 Viewing and adjusting the ECG
4.6.1 Expanding the ECG window to full size
The ECG window automatically opens in the minimized format when the programmer is
switched on. To view all the available signals, you can expand the ECG window to its full
size using the square button in the upper-right corner of the ECG window. To return to
the partial-view window, press the square button again.
Multiple recordings are displayed during tests (for example, threshold measurement,
sensing tests). The signals are the previously displayed surface ECG combined with
event markers and the intracardiac electrogram (EGM) of the chamber being tested.
43
Page 44

C-series Reference Manual Section 4.6
Figure 4-19. Multiple recordings (during tests)
4.6.2 Displayed recordings
The programmer can display recordings from up to seven sources. The ECG leads (I,
II, and III) are always available and are detected via skin electrodes. The programmer
must be connected to these electrodes with the ECG cable.
Filtered atrial and ventricular EGMs (AEGM and VEGM) are also displayed and can be
switched on and off as desired. (See Section 4.6.3.)
Figure 4-20. Displayed recordings
The seven recordings in Figure 4-20 are shown separately to simplify this explanation.
The Marker Annotation and Marker Intervals can be superimposed on an ECG to facilitate
interpretation. For information on how to arrange the recordings see Section 4.6.4.
44
Page 45

C-series Reference Manual Section 4.6
Marker annotation – Marker annotations depict pacemaker operation by showing events
as they occur. These annotations are intended to simplify ECG interpretation. Typically,
the Marker Annotation channel is superimposed on an ECG recording. Atrial events are
shown above the baseline and ventricular events below it.
The following marker annotations are used:
Atrial events
•
– AP Atrial pace
– AS Atrial sense
– BS Atrial sense in blanking period
– PC Premature atrial contraction
– RC Retrograde atrial sense
– RS Atrial sense in refractory period
– SP Atrial synchronization pace
– TS Atrial tachy sense
– +P Triggered atrial pace
Ventricular events
•
– RS Ventricular sense in refractory period
– VE Premature ventricular contraction
– VP Ventricular pace
– VS Ventricular sense
– XP Ventricular safety pace
– +P Triggered ventricular pace
Note: Parameter programming or pacemaker interrogation may momentarily interrupt the
transmission of the EGM or marker annotations. This can result in missing markers on
the recording.
Marker intervals – The programmer automatically measures the intervals between pace
and sense markers and displays them (in milliseconds) as a separate recording. For dual
chamber modes the AV intervals and the VV intervals are displayed. For single chamber
modes the AA or VV intervals are displayed, depending on the chamber being paced.
45
Page 46

C-series Reference Manual Section 4.6
4.6.3 Adjusting and configuring the display
The Adjust window contains controls that allow you to tailor the ECG display to your
specific needs. To change the ECG settings press [Adjust…] in the top part of the
control panel.
Figure 4-21. Adjusting ECG settings
The following changes can be made:
adjust presentation of the recordings (size, source and color)
•
change sweep speed
•
select EGMs
•
adjust artifact detection level
•
show artifacts (pacing spikes)
•
enable ECG signal filter
•
show blanked atrial senses
•
clean up the ECG window
•
normalize the ECG window
•
Signal size – To adjust the size (or amplitude) of a signal select “Size” in the Adjust
window and alternately press and release the increase or decrease button to change
the size of the signal you want to adjust.
46
Page 47

C-series Reference Manual Section 4.6
Figure 4-22. Adjusting signal size
To return to the default setting, press [Normalize]. This resets the size of all recordings to
the default setting and equalizes the spacing between the recordings.
ECG source – To change the order in which the recordings appear in the window, select
“Source” in the Presentation list. The source of the ECG is then superimposed on the
signal on a white background (see Figure 4-23).
Figure 4-23. Adjusting the source
Note that ECGs may be superimposed on one another (for example, when using marker
intervals or marker annotation). If this is the case the name of the source that is on top
appears. To display an underlying source and move it to the top, select the source name
on the left of the screen. The name changes to show the recording beneath it.
If you want to change the position of a superimposed signal, it must first be put on top so
that its name appears on the left of the screen (see Figure 4-24).
47
Page 48

C-series Reference Manual Section 4.6
Figure 4-24. Changing the source
Now select the source for the ECG you want to change. A list appears displaying source
options. From this list select the desired source. Selecting a new source causes the
source of the recording presently displayed to change positions with the source you
selected.
Color coding – This changes the color of one or more of the recorded signals. To
change the color first select “Color” in the Adjust window.
Select the color field for the recording you want to change and from the list of options,
select the desired color.
Figure 4-25. Selecting the desired color
Sweep speed – By selecting “Sweep speed” from the Adjust window, you can set the
ECG sweep speed to 12.5, 25, 50, or 100 mm/s. The initial default setting is 25 mm/s, but
any change is saved and used as the default at the next follow-up session.
48
Page 49

C-series Reference Manual Section 4.6
Figure 4-26. Selecting sweep speed
EGM selection – This feature lets you activate the atrial and ventricular EGMs, which
are displayed in the ECG window. The following options are available:
Off – no recording is displayed
•
AEGM - the filtered atrial EGM detected by the atrial lead
•
VEGM - the filtered ventricular EGM detected by the ventricular lead
•
Since the EGMs depend on information received from the pacemaker, they are not
displayed unless the programming head is positioned over the pacemaker. This feature is
not available if the pacemaker is recommended for replacement.
Artifact level – If “Show artifacts” is switched on, pacing spikes are shown in the ECG
window. The sensitivity to sensed pacing pulses can then be adjusted by changing the
artifact level. To prevent interference signals being interpreted as pacing pulses or to
prevent certain pacing pulses from being sensed you should select the appropriate
artifact level. The artifact level can range from 1 (very sensitive) to 5 (very insensitive).
The required artifact level may vary due to the amount of electromagnetic interference
(EMI) present at the follow-up site.
Artifact lead – This option determines which ECG lead is used to detect pacing pulses.
During programming and interrogation of the pacemaker, communication signals may
appear as artifacts on the ECG.
Show artifacts – Press the “Show Artifacts” check box to enable or disable pacing
artifact enhancement. A check mark indicates that it is enabled. The two ECGs in
Figure 4-27 show how an ECG appears with and without this feature enabled.
49
Page 50

C-series Reference Manual Section 4.6
Figure 4-27. Artifact enhancement enabled (upper panel) and disabled (lower panel)
ECG filter – Press the “ECG Filter” check box to switch the ECG filter on or off. A check
mark indicates that the filter is switched on. In the presence of interference the filter may
improve the quality of both the displayed and printed ECG. The filter affects the ECG
detection bandwidth as follows:
Filter Off: bandwidth = 0.05 to 100 Hz
•
Filter On: bandwidth = 0.5 to 40 Hz
•
Show blanked senses – If this option is switched off (the check box is not checked)
blanked sensed atrial events are suppressed in the ECG recording. This allows you to
avoid an overload of markers in the ECG recording during periods of high (sensed) atrial
rates. The option is switched on at the start of each new follow-up session.
Cleanup – Press this button to equalize the spacing between the recordings.
Normalize – Press this button to equalize the spacing between the recordings and to
adjust the size of each to the default setting.
Close – Press [Close] to leave the Adjust window.
4.6.4 Arranging the ECGs
In addition to arranging the ECGs by selecting the source, you can use the touch pen to
“drag” an ECG to the desired position. The example below shows how to move the Marker
Annotation recording from its position over Lead II to a position over the ventricular ECG.
Moving an ECG using the touch pen – First decide which ECG you want to reposition.
If its name (Marker Annotation in this case) is not displayed, tap the name of the
superimposed recording to display the hidden name.
50
Page 51

C-series Reference Manual Section 4.6
Figure 4-28. Select the ECG to be moved
Press and hold the touch pen against the name of the ECG you want to move.
Without lifting the touch pen, drag the box now appearing around the recording name
to the desired location.
Figure 4-29. Move the ECG to its new location
When you have the box positioned where you want the ECG to appear, lift the touch
pen. If you are positioning one ECG over another, it will snap into position. To equalize
the spacing between the recordings in the new arrangement, press [Cleanup] in the
Adjust window.
Freezing and analyzing an ECG – This option lets you freeze the last 15 seconds of all
ECGs displayed in the expanded window. Pressing [Freeze] in the ECG control panel
opens the frozen ECG viewing window.
51
Page 52

C-series Reference Manual Section 4.6
Figure 4-30. Freezing an ECG
Controls below the viewing window include the caliper controls and the following buttons:
Press [Adjust…] to open a window of ECG adjustment controls.
•
Press [Strips…] to view (and open) a list of saved recordings.
•
Press [Save] to save the recording presently displayed.
•
Press [Delete] to delete a saved recording. This button is active only if you are
•
viewing a saved recording.
Press [Print…] to print the recording presently displayed.
•
Press [Close] to close the frozen viewing window. If you have not saved the
•
recording, a pop-up window will remind you to save or delete it.
Using the on-screen calipers – The control buttons control the frozen ECG viewing
window by letting you move each of the two vertical cursors appearing in the window to
any desired position. The cursors thus act as calipers allowing you to measure the time
interval between events. The caliper measurement is displayed in milliseconds in the
upper-left corner of the window.
52
Page 53

C-series Reference Manual Section 4.6
Figure 4-31. Using the calipers
Using the caliper positioning buttons – Alternately press and release the appropriate
button to effect small movements, or press and hold the button to effect larger movements.
Viewing other portions of the frozen ECG – Use the vertical scroll bar to scroll the
display up or down to view other ECGs. Tap the scroll up arrow or scroll down arrow to
scroll the ECGs up or down in small increments.
The vertical scroll bar shows the relative position of the window with respect to the total
height of the strip. Touch and drag the box to scroll the strip up or down.
Use the horizontal scroll bar, which operates like the vertical scroll bar, to move the
display to the right or left to see other portions of the15-second strip.
Adjusting the frozen ECGs – Pressing [Adjust…] opens the Adjust window, which
provides some of the same controls available for the ECG window (see Section 4.6.3).
Saving a frozen ECG recording – Provided you have launched a programming session,
you can save the frozen ECG by pressing [Save]. You may then recall the saved
recording for later viewing or printing.
Printing the frozen strip – Press [Print] to print the frozen ECG recording you are
viewing (at 12.5, 25, 50, 100 or 200 mm/s).
53
Page 54

C-series Reference Manual Section 4.6
Recalling and viewing ECGs – Prior to ending the follow-up session, you can recall
and view any ECG collected and saved during the session. Such recordings may be
those saved during a test (for example, the threshold test) or an ECG saved following
use of the Freeze option.
Viewing a previously collected ECG – Press the [Strips…] button in the ECG control
panel or the [Strips…] button in the lower-left corner of the Frozen ECG window. From
the Other Strips window now displayed, select the “Collected by programmer” option.
From the list of recordings in the selection field, select the one you want to view. It may
be necessary to use the scroll bar on the right of the field if there are more than five
recordings available.
Press [Open].
Printing the ECG – To print the ECG using the built-in printer, press the appropriate
printer control button on the left of the programmer. All three ECG recordings are then
printed at 12.5, 25 or 50 mm/s.
The print speed, which is shown when printing starts, can be changed with immediate
effect. This is shown on the printout by a dashed vertical line, followed by the new print
speed.
ECG markers are shown if they are switched on (see Section 4.6.2).
To stop printing, press the appropriate print speed control button.
54
Page 55

C-series Reference Manual
Part II
Follow-up and diagnostics
5 Follow-up
5.1 Introduction
The intention of this chapter is to offer post-implant and follow-up advice to the medical
personnel working with Vitatron pacemakers.
Follow-ups at regular intervals are required to check on the medical condition of the
patient and to confirm that the programmed parameter values are still appropriate.
Additionally, both the operation of the pacemaker and the condition of the battery require
regular monitoring.
The sections in this chapter are arranged as follows:
post-implant configuration (see Section 5.2)
•
record an ECG (see Section 5.3)
•
program patient information (see Section 5.4)
•
checks and programming (see Section 5.5)
•
optimizing the pacemaker (see Section 5.6)
•
the ECG/EGM (ElectroCardioGram/Intracardiac ElectroGraM) (see Section 5.7)
•
follow-up frequency and longevity (see Section 5.8)
•
5.2 Post-implant configuration
During implant, the pacemaker configuration procedure starts automatically once the
pacemaker detects that a lead is connected. Note that even if the pacemaker is a dual
55
Page 56

C-series Reference Manual Section 5.2
chamber device, the procedure begins as soon as the first lead is connected. A minimum
period of two hours is then required for the pacemaker to complete configuration.
If in the first two hours after implant, lead replacement or repositioning is necessary, then
the two-hour configuration period starts again. Vitatron advises you not to program the
pacemaker before implant as this could delay configuration. The pacemaker gives the
required pacing therapy at the delivery settings during the configuration period.
Once configuration is completed, the pacemaker program determines that implant is
complete and automatically programs the implant date. Programming the implant date
activates the diagnostic features and the pacemaker starts to collect diagnostic data. If
the implant date is set manually, the collection of diagnostic data starts one hour later.
Refer to Chapter 7 for a full description of the diagnostic features.
The first time a programming head is placed over the pacemaker after implant, the
programmer synchronizes the implant date in the pacemaker with the programmer date.
Note: Vitatron recommends that you check the pacemaker has set the implant date and
thus has switched on the collection of diagnostic data. If required, you have the option to
manually adjust the implant date (see Section 4.4.5). A time difference may appear in
diagnostic data collected before and after the date change.
5.3 Record an ECG
First, connect the patient to an ECG, either the built-in ECG or an external ECG monitor.
Then record and print out a copy of the ECG. During any programming session, either
post-implant or scheduled follow-up session, keep the ECG active to allow all cardiac
events to be continuously monitored.
As the post-implant ECG provides an important baseline record of the patient, Vitatron
recommends that you place a printout of the ECG in the patient’s file. This ensures
that a record is available for reference during the service life of the pacemaker. For the
same reason Vitatron recommends keeping a printout of the ECG recordings made at
each scheduled follow-up session.
Note: If using an external ECG, as there is no connection with the programmer, it is not
possible to download information such as calibration signals, EGM and ECG markers.
This information is only displayed on the built-in ECG.
5.4 Program patient information
Select the “Patient” icon and then enter the patient and pacing system data in the Patient
Information window. For specific information on programming the data in this window,
56
Page 57

C-series Reference Manual Section 5.4
see Section 4.4.5. This information, stored in the pacemaker, will throughout the service
life of the pacemaker allow you to perform the following tasks:
identify both the patient and the pacemaker system
•
retrieve information about diagnostic and implant information
•
retrieve information on the physician, implant center and the implant that is essential
•
for gathering further information
write comments, remarks and observations on a “notepad” and thus record
•
additional patient information or reminder notes for the next follow-up session. This
can prove especially useful when the patient files are not available.
5.5 Checks and programming
Vitatron suggests the following checks and programming after implant to ensure that the
pacemaker program meets the patient’s requirements.
During routine follow-up sessions, use this section to ensure that any patient changes
are recognized and met. If any help is required with programming, or for specific
programming instructions, refer to Chapter 4.
5.5.1 Interrogate the pacemaker
With the programmer head positioned over the pacemaker, use the Status-Initial
Interrogation window on the programmer to assess the pacemaker status. Print out a
copy of the initial interrogation report. If applicable, print out the diagnostics, including
the Holter and the histogram data. Place all the printouts in the patient’s file so that a
record is available for analysis if required.
If the “Auto print initial interrogation report” option is checked in the Programmer
Preferences window, the results of the initial pacemaker interrogation are printed
automatically (see Section 4.3.1).
Note: As soon as the programmer head is correctly positioned the pacemaker switches
to its magnet pacing rate. This rate continues until either the interrogate button on
the programmer head or the [Auto Identify] button is pressed, and communication is
established. Then the magnet rate is switched off. In patients who experience discomfort
while the magnet rate is active, it is advisable to press the interrogate button before
positioning the programmer head. This limits the length of time during which the magnet
rate is active.
57
Page 58

C-series Reference Manual Section 5.5
5.5.2 Confirm lead function
Check the lead impedance displayed in the Initial Interrogation window. Compare the
values displayed on the screen with the values obtained at the last follow-up session.
5.5.3 Pulse amplitude and pulse duration threshold tests
Use the pulse amplitude and pulse duration threshold tests to determine the minimum
pulse amplitude and pulse duration, at which it is possible to obtain effective capture. If
required, see Section 6.2 for more detailed information on performing these tests. Adapt
the output values if necessary.
5.5.4 Rate response
The delivery setting is the non rate responsive mode.
If the patient requires rate responsive pacing, program the mode setting to the
appropriate rate responsive mode.
5.5.5 Mode switching
The delivery setting is “Fixed”.
There are two options available, “Fixed” and “Auto” (automatic). Unless the patient’s
medical condition dictates differently, Vitatron advises you to use the following settings.
In DDDR mode, ageing patients: program mode switching to “Auto” with mode
•
switching sensitivity set to “Standard”.
In DDDR mode, young patients: program mode switching to “Auto” with mode
•
switching sensitivity set to “Moderate”.
In VDDR mode, all patients: program mode switching to “Fixed” or “Auto”, with mode
•
switching sensitivity set to “Moderate”.
See Section 9.5 for further information on mode switching and mode switching sensitivity.
5.5.6 Lower rate
The delivery setting is 60 min–1.
Use the patient’s medical condition to determine whether to keep the delivery setting, or
to use a more appropriate setting.
See Section 8.4 for further information on the lower rate parameter.
58
Page 59

C-series Reference Manual Section 5.5
5.5.7 Maximum tracking rate
The delivery setting is 140 min–1.
Use the patient’s age and medical condition to determine whether to keep the delivery
setting, or to use a more appropriate setting. For further information, see Section 8.5.
5.6 Optimizing the pacemaker
Vitatron recommends that you perform the following pacemaker optimizing procedures,
both during the post-implant stage and at the subsequent follow-up sessions. These
procedures help to deliver the optimal pacemaker therapy to the patient and ensure a
long pacemaker lifetime.
5.6.1 Optimizing pacing
Having determined the thresholds, check that the pulse amplitude and pulse duration
are appropriate for the patient. When programming the pulse amplitude, as a generally
accepted standard Vitatron recommends that you program a safety margin of twice the
pulse amplitude threshold. When programming the pulse duration, Vitatron recommends
that you program a safety margin of three times the pulse duration threshold. Check that
the pacing polarity settings are appropriate. See Section 6.2 for detailed programming
instructions on optimizing pacing.
5.6.2 Optimizing sensing
First, check that the sensitivity is still at an appropriate setting for the patient. Then check
that the sensing polarity setting is correct. Following on from these checks, carry out
the P-wave and R-wave amplitude tests.
See Section 6.3 for detailed programming instructions on optimizing sensing.
5.6.3 Diagnostics
If there are any significant changes, or if the patient has reported any problems, the
pacemaker diagnostic procedures can help to quickly locate the cause of the problem.
Refer to Chapter 7 for detailed information on using the pacemaker diagnostics.
59
Page 60

C-series Reference Manual Section 5.6
5.6.4 Updating the patient’s file
When the required optimizing and diagnostic procedures are completed, Vitatron
suggests printing out all the data and saving it in the patient’s file. In addition, save the
information to disk (see Section 4.4.9) and place the disk in the patient’s file.
5.7 The ECG/EGM
At the beginning of each follow-up session, Vitatron recommends that you connect the
patient to either the built-in ECG, or an external ECG monitor. If you use the built-in ECG
it is possible to integrate the ECG information with other information from the pacemaker.
See Chapter 4 for a more detailed description.
Note: If using an external ECG, as there is no connection with the programmer,
downloading information such as calibration signals, EGM, and ECG markers, is not
possible. Only the built-in ECG displays this information.
EGM – This feature lets you obtain, display and view graphs of intracardiac signals on
the programmer screen. From the EGM information, you can determine the properties
of intracardiac signals such as amplitudes, intervals and rhythms. It is also possible to
use the information to determine if electromagnetic interference (EMI), far-field and
retrograde signals are affecting the intracardiac signals.
Note: The EGM display is only available when the programming head is in position
over the pacemaker.
5.8 Follow-up frequency and longevity
The follow-up frequency depends on the patient’s condition and the age of the pacemaker.
Use the following pacemaker information to determine the optimal follow-up frequency.
5.8.1 Pacemaker battery lifetime indicators
Data
⇒ Battery Status
The programmer calculates and displays pacemaker lifetime estimates on screen. Use
the Battery Status window to assess the remaining battery lifetime (see Figure 5-1).
There is also additional information on the battery, as well as other pacemaker information
that can affect the service life of the pacemaker under various conditions. From this
information it is possible to make an estimate of the time to the next follow-up session.
60
Page 61

C-series Reference Manual Section 5.8
Figure 5-1. Battery Status window
The programmer calculates the estimated time until the recommended replacement time
(RRT) of the pacemaker. This estimation is based on the programmed settings and the
pacemaker recorded data. Although a small percentage of pacemakers may reach RRT
sooner than the remaining longevity estimate, the main purpose of the feature is as an
aid in estimating the appropriate follow-up session interval.
Battery status and remaining longevity are dependent on the present settings of the
pacemaker. If any of the following remaining longevity critical parameters are pertinent
and if any or all of them are altered, the battery status can change:
mode
•
lower rate
•
pacing polarity (atrial or ventricular)
•
pulse amplitude (atrial or ventricular)
•
pulse duration (atrial or ventricular)
•
tachy fallback rate
•
61
Page 62

C-series Reference Manual Section 5.8
Notes:
Current consumption and remaining longevity are strongly influenced by changes
•
in mode, pacing rate and therapies. Remaining longevity is therefore not always
accurately predictable, as it is highly dependent on the patient/therapy interaction.
At high output settings it is possible that remaining longevity and remaining capacity
•
cannot be estimated accurately. In this case dashes (---) appear in the relevant fields.
When the pacemaker battery is maturing, changing a pacemaker setting to a value
•
that uses more current could result in the battery status changing, for example,
from ’Good’ to ’Ageing’ . Before accepting the change, note that there is then the
possibility of the pacemaker reaching ’Replace PM’ in less then six months at this
stage in the battery’s lifetime.
As a further aid to estimating the pacemaker lifetime, the calculated lifetime figures for
each model are shown.
62
Page 63

C-series Reference Manual Section 5.8
Table 5-1. Calculated lifetime (after 18 months shelf life)
Model Mode 2.5 V 5.0 V
500 Ù 300 Ù 500 Ù
100% pacing 100% pacing 100% pacing
70 min–1, 0.5 ms 70 min–1, 0.5 ms 70 min–1, 0.5 ms
Vitatron C60 DR DDDR
Vitatron C20 SR VVIR
6.4 years 5.6 years 3.4 years
9.6 years 8.9 years 6.2 years
Note: During periods in which the pacemaker senses high frequency atrial rhythms,
especially AF, there will be an increase in power consumption. This will result in a
reduction in battery lifetime. As an example, battery life could be reduced by 15% if the
pacemaker were to sense an AF rhythm of 300 min–1through 25% of the pacemaker
lifetime.
Table 5-2. Calculated lifetime (after 4 months shelf life)
Model Mode 2.5 V, 500 Ù
Vitatron C60 DR DDDR
Vitatron C20 SR VVIR
100% pacing 50% pacing 100%
–1
70 min
0.5 ms
7.2 years 8.1 years 8.3 years 9.1 years 9.7 years
10.5 years 11.4 years 11.6 years 12.4 years 13.0 years
60 min
0.4 ms
–1
70 min
0.5 ms
–1
60 min
0.4 ms
–1
inhibited
70 min
0.5 ms
–1
5.8.2 Follow-up intervals
Vitatron recommends that you schedule a follow-up session at least once a year, even
though the pacemaker memory can store more than a year’s diagnostics.
You can determine the recommended follow-up interval using information provided by the
programmer, or using a magnet, to monitor the battery.
Using the programmer – The follow-up intervals suggested in Table 5-3 are based on
the battery status and estimated longevity. The medical condition of the patient dictates
when to schedule the next follow-up session within the suggested follow-up interval.
Table 5-3. Follow-up intervals - using programmer
Battery status Remaining longevity
“Good” more than one year Dependent on the patient’s condition, up
“Good” more than six months Dependent on the patient’s condition, up to
a
Suggested follow-up interval
to one year.
six months.
63
Page 64

C-series Reference Manual Section 5.8
Table 5-3. Follow-up intervals - using programmer (continued)
Battery status Remaining longevity
a
Suggested follow-up interval
“Ageing” less than six months Dependent on the patient’s condition, up
to three months.
b
“Replace PM”
a
At high output settings remaining longevity cannot be estimated accurately and is shown as “---”. In this
case, the follow-up interval should be less than 3 months.
b
The pacemaker has sufficient battery capacity to operate at reduced output settings for at least 90 days
after the battery status changes to “Replace PM” (see Section 5.8.3).
none
Schedule replacement of the pacemaker.
Using a magnet – Placing a magnet over the pacemaker switches the pacemaker to
fixed rate pacing magnet mode. Removing the magnet causes the pacemaker to revert to
the programmed settings. From the fixed pacing rates shown in Table 5-4 it is possible to
determine battery status without using the programmer.
Warning: In magnet mode the pacemaker operates in an asynchronous pacing
mode. If the intrinsic rate is higher than the magnet rate, this may induce ventricular
tachycardia or ventricular fibrillation.
Table 5-4. Follow-up intervals - using magnet
Magnet pacing
rate
100 min
–1
(600 ms)
–1
95 min
(630 ms)
–1
86 min
(700 ms)
–1
90 min
(670 ms)
a
At high output settings the follow-up interval should be less than three months.
b
The pacemaker has sufficient battery capacity to operate at reduced output settings for at least 90 days
after the battery status changes to “Replace PM” (see Section 5.8.3).
Battery status and pacemaker
restore Suggested follow-up interval
a
“Good” Dependent on the patient’s condition, up
to six months.
“Ageing” Dependent on the patient’s condition, up
to three months.
“Replace PM”
b
Schedule replacement of the pacemaker.
“Partial restore” Refer to Appendix A for information on
how to proceed once a “partial restore”
has occurred.
5.8.3 Pacemaker replacement
During the initial interrogation, if the pacemaker determines that the battery status
appears to be “Ageing” or “Replace PM”, then a warning opens over the Status window.
If available, the time when the status changed from good or ageing is also indicated
(see Figure 5-2).
64
Page 65

C-series Reference Manual Section 5.8
Figure 5-2. Battery warning
When the battery status indicates “Replace PM”, and the programmer determines
that recovery is possible, then the [Recover Status] button is displayed. Pressing
[Recover Status] resets the “Replace PM” indication to either “Ageing” or “Good”,
dependent on the current pacemaker settings.
Check the time when the status changed. The longer the time since the battery
status changed to “Replace PM”, the more urgent it is to replace the pacemaker. The
pacemaker settings and the battery impedance determine the battery status “Replace
PM”. At that moment when the pacemaker determines that the battery status reached
“Replace PM”, 99.9% of the pacemakers have sufficient battery capacity to operate at
“Replace PM” settings for at least 90 days before the pacemaker no longer functions
within specifications.
Note: The period can be less than 90 days if either the settings or the output load of the
pacemaker are greater than normal assumptions.
Pacemaker replacement characteristics – When the pacemaker determines that the
battery status has changed to “Replace PM”, several changes take place automatically to
prolong the battery life (see Table 5-5). Also note that the escape interval lengthens by
100 ms.
Table 5-5. Pacemaker replacement characteristics
Parameter name before “Replace PM” “Replace PM” (RRT)
Mode DDD(R)
VDD(R)
VVI(R)
DDI(R)
AAI(R)
DOO
Flywheel mode As programmed Off
EGM range As programmed Off
PVC synchronous Astim As programmed Off
VVI
VVI
VVI
VVI
AAI
VOO
65
Page 66

C-series Reference Manual Section 5.8
Table 5-5. Pacemaker replacement characteristics (continued)
Parameter name before “Replace PM” “Replace PM” (RRT)
Post-PVC response As programmed Off
Rate response As programmed Off
Tachy fallback rate As programmed Off
Diagnostic data collection Available Suspended
Diagnostics programming Available Not available
Therapy Advisor Available Not available
EGM Available Not available
66
Page 67

C-series Reference Manual
6 Optimizing pacing and sensing
6.1 Introduction
This chapter describes how to program pulse amplitude, pulse duration, sensitivity and
pacing/sensing polarity. It also describes the following procedures, which are useful in
optimizing pacing and sensing:
Pulse amplitude and pulse duration threshold tests, which can be used to optimize
•
pacing conditions. Instructions on how to program the (atrial and ventricular) pulse
amplitude, pulse duration and pacing polarity are given (see Section 6.2).
P-wave and R-wave amplitude tests, which can be used to optimize the sensing
•
conditions. Instructions on how to program the (atrial and ventricular) sensitivity and
sensing polarity are given (see Section 6.3).
VA interval measurement, manual and automatic, which is helpful in diagnosing
•
retrograde conduction and far-field R-wave (FFRW) sensing (see Section 6.4).
Temporary test, which is helpful for temporarily reprogramming pacemaker
•
parameters, for diagnostic purposes and for investigation of FFRW sensing (see
Section 6.5).
Lead measurement, which is used to check the stability of the atrial and ventricular
•
leads (see Section 6.6).
Notes:
The Fast Learn test is described in Section 11.5.
•
During the tests and measurements (except the lead measurement) post-PVC
•
response, tachy fallback rate and Flywheel are temporarily disabled.
When measuring pacing and sensing parameters with pacing system analyzers it
•
should be realized that considerable differences may be observed when the results
are compared with the results of the tests described in this chapter, because the
measuring methods employed by such systems may differ.
6.2 Optimizing pacing
The stimulation threshold is the minimum amount of energy needed to consistently
capture the heart outside the refractory period. Capture occurs when a pacing pulse
is intense enough (pulse amplitude) or long enough (pulse duration) to trigger a
depolarization wave in the myocardium. The stimulation threshold varies from patient
to patient.
67
Page 68

C-series Reference Manual Section 6.2
Measuring the stimulation threshold provides an effective method of assessing the safety
margin between the measured threshold and the programmed pulse amplitude or pulse
duration. An optimally programmed pulse amplitude and pulse duration results in safe
pacing conditions and contributes to the prolongation of the service life of the pacemaker.
6.2.1 Pulse amplitude
Parameters
⇒ Amplitude Atrial
Range: 0.5 - (0.25) - 4.0 - (0.5) - 8.0 V
Availability: DDD(R), DDI(R), DOO, AAI(R), AAT and AOO modes
Parameters
⇒ Amplitude Ventricular
Range: 0.5 - (0.25) - 4.0 - (0.5) - 8.0 V
Availability: DDD(R), DDI(R), DOO, VDD(R), VVI(R), VVT and VOO modes
The pulse amplitude is the intensity or strength of a pacing pulse. Vitatron recommends
programming a safety margin of twice the pulse amplitude threshold (see Section 6.2.3).
6.2.2 Pulse duration
Parameters
⇒ Pulse Duration Atrial
Range: 0.1 - (0.05) - 1.0 ms
Availability: DDD(R), DDI(R), DOO, AAI(R), AAT and AOO modes
Parameters
⇒ Pulse Duration Ventricular
Range: 0.1 - (0.05) - 1.0 ms
Availability: DDD(R), DDI(R), DOO, VDD(R), VVI(R), VVT and VOO modes
Pulse duration is the duration (width) of a pacing pulse. Vitatron recommends
programming a safety margin of three times the pulse duration threshold (see
Section 6.2.3).
68
Page 69

C-series Reference Manual Section 6.2
6.2.3 Pulse amplitude and pulse duration threshold tests
Tests
⇒ Threshold Test
Availability: All modes, except OOO
Measurement of stimulation thresholds makes it possible to determine the minimum pulse
amplitude and duration at which effective capture is obtained. The measurement can be
performed in both the atrium and the ventricle, depending on the programmed mode.
Changes in threshold measurement over time may indicate an unstable lead position,
ischemia, or the effects of (changes in) drug therapy.
Figure 6-1. Threshold Test window with ECG
Setting up the threshold test – To prepare for the test take the following steps:
1. Position the programming head on the pacemaker.
2. Use the “Test Type” drop-down list to select the appropriate threshold test
(Atrial/Ventricular Amplitude or Atrial/Ventricular Pulse Duration).
69
Page 70

C-series Reference Manual Section 6.2
3. Adjust the test values of pulse amplitude and pulse duration in the “Test Value”
column. The selected test value is used as the start value for the threshold test.
4. Adjust the mode and rate in the “Test Value” column. The test modes available
depend on the permanently programmed mode. The test rate can be temporarily
programmed between 80 min
–1
and 120 min–1. The higher rates are useful in
patients with high spontaneous rates, while the lower rates may be more comfortable
for patients with, for example, angina pectoris.
5. Adjust the maximum paced or sensed AV delay in the “Test Value” column. The
standard setting is 200 ms if the test chamber is the atrium and 100 ms if the test
chamber is the ventricle.
6. If required, reprogram the permanent pacing polarity prior to starting or repeating
the measurement.
Performing the threshold test – The following steps describe the general procedure:
1. Press the touch pen on [Press and Hold] and keep it pressed there to perform the
measurement. The pacemaker paces at a decreasing pulse amplitude or pulse
duration until the step-down cycle ends automatically (below 0.25 V or 0.1 ms)
or is stopped manually.
2. Watch the EGM or the ECG carefully. The marker annotations (on the programmer
screen) are useful to identify the atrial or ventricular paced events. As soon as
the EGM or ECG shows loss of capture, release [Press and Hold] or remove the
programming head to stop the measurement.
3. If the measurement is stopped manually, the threshold value is one step-down
value higher than the last active test value. The threshold value is displayed on the
right-hand side of the screen.
4. If the measurement is not stopped manually and the programmer has reached the
end of the step-down cycle, the message “Test ended automatically” is displayed.
The threshold value is 0.1 ms (pulse duration) or 0.25 V (pulse amplitude).
5. If more than six senses occur during 10 consecutive cycles, the measurement is
stopped automatically and a message is displayed. Press [Close] to return to the
Threshold Test window. Increase the test rate or shorten the AV delay in the “Test
Value” column to decrease the number of senses.
6. Press [Print] to print the threshold test report.
7. Press [Test Strip…] to view the ECG strip collected during the last successful
threshold test of the specified type and in the specified chamber.
70
Page 71

C-series Reference Manual Section 6.2
Notes:
The observation of atrial capture can be improved by optimizing the quality of the
•
ECG (see Section 4.6.3).
If the “Permanent” column contains boxed parameters, measuring pacing thresholds
•
is not possible. Press [Program] or [Undo Pending] first, then start the measurement.
During the test, the programming head must be continuously applied to the
•
pacemaker. The measurement is stopped if the programming head is removed.
If the measurement is stopped or completed, the pacemaker returns to its
•
permanently programmed settings.
Measured pulse amplitude and pulse duration thresholds are stored in the
•
programmer memory. They can be printed later by selecting the “Threshold Test”
report in the Reports window.
Reprogramming pulse amplitude and pulse duration – In the “Permanent” column of
the Threshold window, the pacemaker can be programmed to a new (atrial or ventricular)
pulse amplitude or duration based on the outcome of the threshold test. The displayed
test result is the minimum pulse amplitude or pulse duration that can be programmed. As
a generally accepted standard Vitatron recommends programming a safety margin of
three times the pulse duration threshold or twice the pulse amplitude threshold.
6.2.4 Pacing polarity
Parameters
⇒ Sense/Pace Polarity Atrial
Range: Uni, Bi
Availability: DDD(R), DDI(R), DOO, AAI(R), AAT and AOO modes
Parameters
⇒ Sense/Pace Polarity Ventricular
Range: Uni, Bi
Availability: DDD(R), DDI(R), DOO, VDD(R), VVI(R), VVT and VOO modes
If the atrial or ventricular pace polarity is programmed from unipolar to bipolar, the
programmer initiates an automatic polarity check to confirm that a bipolar lead is
connected. If the bipolar lead impedance exceeds 2000 Ù or is less than 200 Ù, the
programmer screen displays a warning that no bipolar lead is detected. Press [OK]
to confirm or [Cancel] to cancel the programming step. If the programming step is
confirmed, press [Program] to program the pending polarity setting.
71
Page 72

C-series Reference Manual Section 6.2
Vitatron recommends programming the pacing polarity to bipolar if bipolar leads are
implanted and muscle or nerve stimulation is observed during unipolar pacing.
Warning: Do not reprogram pacemakers co-implanted with an ICD device to
unipolar pacing.
6.3 Optimizing sensing
The objective is to reliably sense all relevant cardiac signals (P-waves and R-waves)
while rejecting those that originate outside the chamber in which the lead is positioned,
such as myopotentials or far-field R-waves. Programming the appropriate sensitivity or
sensing polarity increases the reliability of sensing.
6.3.1 Sensitivity
Parameters
⇒ Sensitivity Atrial
Range: 0.25 (Bi), 0.3 (Bi), 0.4 (Bi), 0.5 - (0.1) - 1.0 - (0.5) - 7.5 mV
Availability: DDD(R), DDI(R), VDD(R), AAI(R) and AAT modes
Parameters
⇒ Sensitivity Ventricular
Range: 1.0 - (0.5) - 10.0 mV
Availability: DDD(R), DDI(R), VDD(R), VVI(R) and VVT modes
Sensitivity is the programmable threshold of the pacemaker to sense a signal registered
in the atrial or ventricular channel. Programming the sensitivity to a higher setting
decreases the number of sensed P- and R-waves with lower amplitudes.
Vitatron recommends using a sensing safety margin of at least 100%. This means, for
example, programming the atrial sensitivity to a setting less than 0.5 mV if the measured
P-wave amplitude is 1.0 mV (see Section 6.3.3) or programming the ventricular
sensitivity to a setting less than 3.0 mV if the measured R-wave amplitude is 6.0 mV
(see Section 6.3.4).
72
Page 73

C-series Reference Manual Section 6.3
6.3.2 Sensing polarity
Parameters
⇒ Sense/Pace Polarity Atrial
Range: Uni, Bi
Availability: DDD(R), DDI(R), VDD(R), AAI(R) and AAT modes
Parameters
⇒ Sense/Pace Polarity Ventricular
Range: Uni, Bi
Availability: DDD(R), DDI(R), VDD(R), VVI(R) and VVT modes
If the atrial or ventricular sense polarity is programmed from unipolar to bipolar, the
programmer initiates an automatic polarity check to confirm that a bipolar lead is
connected. If the bipolar lead impedance exceeds 2000 Ù or is less than 200 Ù, the
programmer screen displays a warning that no bipolar lead is detected. Press [OK]
to confirm or [Cancel] to cancel the programming step. If the programming step is
confirmed, press [Program] to program the pending polarity setting.
Vitatron recommends programming sensing polarity to bipolar if bipolar leads are
implanted and oversensing is observed during unipolar sensing.
6.3.3 P-wave sensing
Tests
⇒ Sensing Test
⇒ P-Wave Amplitude
Availability: All modes (except single chamber (V) pacemaker)
The P-wave histogram and the P-wave amplitude measurement provide help when
assessing the P-wave sensing safety margin and when programming atrial sensitivity.
First examine the P-wave histogram and look for signs of atrial undersensing, as
described in Section 7.9.1. If atrial undersensing is suspected, measure the P-wave
amplitude.
The P-wave amplitude can be measured even if the permanently programmed pacing
mode does not support atrial sensing.
73
Page 74

C-series Reference Manual Section 6.3
Figure 6-2. Sensing Test window: P-wave Amplitude
Setting up the P-wave amplitude test – To prepare for the test take the following steps:
1. Position the programming head on the pacemaker.
2. Use the “Test Type” drop-down list to select the P-wave amplitude test.
3. Adjust the test value of atrial sensitivity in the “Test Value” column.
4. Adjust the mode or atrial sense polarity in the “Test Value” column. The test modes
available depend on the permanently programmed mode.
5. Select a test rate between 30 min
–1
and 120 min–1in the “Test Value” column.
Performing the P-wave amplitude test – The following steps describe the general
procedure:
1. Press [Start] to start the measurement. The programmer monitors atrial events
and displays the measured amplitude. When the user stops the measurement
the programmer processes the results collected during the last 15 seconds of the
measurement. The test rate is the only parameter that can be changed during
the test.
2. Watch the EGM or the ECG carefully. The marker annotations (on the programmer
screen) are used to identify sensed atrial events. If no spontaneous atrial events are
sensed, try to decrease the test rate or stop the test and increase the atrial sensitivity.
3. Press [Stop] or remove the programming head to stop the measurement.
4. Press [Test Strip…] to view the ECG recorded during the last measurement.
74
Page 75

C-series Reference Manual Section 6.3
5. If the measurement was successful, the last measured P-wave amplitude and the
minimum P-wave amplitude are displayed on the right-hand side of the Sensing
window.
6. Press [Details…] to view the detailed results of the test. They are presented either
in a graph (see Figure 6-3) or in a table. Select the preferred representation by
pressing the “Graph” or “Table” radio button. Press the “Blanked Senses” check box
to mark the atrial senses that would normally be blanked (see Section 8.7 for advice
on adjusting the atrial blanking periods).
7. Press [Print] to print the sensing test report.
8. Press [Close] to leave the Results window.
Figure 6-3. P-wave Amplitude Test - Results (graph)
Notes:
If the “Permanent” column contains boxed parameters, measuring the P-wave
•
amplitude is not possible. Press [Program] or [Undo Pending] first, then start the
measurement.
During the test the programming head must be continuously applied to the
•
pacemaker. The measurement is interrupted if the programming head is removed.
If the measurement is stopped or interrupted, the pacemaker returns to its
•
permanently programmed settings.
During the P-wave amplitude measurement the magnet mode, Flywheel and rate
•
response are temporarily disabled.
75
Page 76

C-series Reference Manual Section 6.3
Reprogramming atrial sensitivity – In the “Permanent” column, you can reprogram
the atrial sensitivity based on the outcome of the test. Before reprogramming the atrial
sensitivity, check the outcome of the test against the P-wave amplitude distribution in
the P-wave histogram (see Section 7.9.1).
Vitatron recommends using a sensing safety margin of at least 100%, which means
programming the atrial sensitivity to a setting less than 50% of the measured P-wave
amplitude. This means, for example, programming the atrial sensitivity to a setting less
than 0.5 mV if the measured P-wave amplitude is 1.0 mV.
If a high atrial sensitivity is required, the sensing polarity should be programmed to
bipolar. Unipolar sensing in combination with high atrial sensitivities may result in
myopotential or FFRW sensing and cause inappropriate mode switching. Myopotential
sensing can be investigated while exercising the pectoral muscles. Check the marker
channel for sensed atrial events not due to sensed P-waves. The latter could apply to
far-field R-wave senses as well. FFRW sensing can be avoided by programming an
appropriate atrial blanking or by reducing the atrial sensitivity. However, reducing the
atrial sensitivity requires the amplitudes of the far-field R-waves to be much smaller than
those of true atrial signals to avoid atrial undersensing. The P-wave histogram reveals
the amplitude distribution of sensed and blanked atrial events. FFRW sensing can be
confirmed by the VA interval histogram, VA interval measurement or temporary test.
In case of spontaneous AV conduction, check for reliable atrial sensing by reducing the
lower rate and programming a short AV delay.
6.3.4 R-wave sensing
Tests
⇒ Sensing Test
⇒ R-wave Amplitude
Availability: All modes (except single chamber (A) pacemaker)
This measurement provides help when assessing the R-wave sensing safety margin and
when programming ventricular sensitivity.
The R-wave amplitude can be measured even if the permanently programmed pacing
mode does not support ventricular sensing.
76
Page 77

C-series Reference Manual Section 6.3
Figure 6-4. Sensing Test window: R-wave Amplitude
Setting up the R-wave amplitude test – To prepare for the test take the following steps:
1. Position the programming head on the pacemaker.
2. Use the “Test Type” drop-down list to select the R-wave amplitude test.
3. Adjust the test value of ventricular sensitivity in the “Test Value” column.
4. Adjust the mode and ventricular sense polarity in the “Test Value” column. The
test modes available depend on the permanently programmed mode. Temporarily
programming the pacemaker to the VVI mode may be useful for patients with a
high degree AV block.
5. In the “Test Value” column, adjust both the (lower) rate and the maximum paced
AV delay to an appropriate value to prevent ventricular pacing. The test rate is
programmable from 30 min
–1
to 120 min–1.
Performing the R-wave amplitude test – The following steps describe the general
procedure:
1. Press [Start] to start the measurement. The programmer monitors ventricular events
until the user stops the measurement. The programmer then processes the results
of the 10 last measured R-wave amplitudes. The test rate and the maximum paced
AV delay are the only parameters that can be changed during the test.
2. Watch the EGM or the ECG carefully. The marker annotations (on the programmer
screen) are used to identify sensed ventricular events. If no ventricular events are
sensed, try to lengthen the maximum paced AV delay or to decrease the test rate.
Alternatively, stop the test and increase the ventricular sensitivity.
3. Press [Stop] or remove the programming head to stop the measurement.
77
Page 78

C-series Reference Manual Section 6.3
4. If no ventricular events are sensed during the measurement, the programmer
screen displays a message.
5. If the measurement was successful, the last measured R-wave amplitude and the
minimum R-wave amplitude are displayed on the right-hand side of the Sensing
window.
6. Press [Test Strip…] to view the ECG recorded during the last measurement.
7. Press [Print] to print the sensing test report.
Notes:
If the “Permanent” column contains boxed parameters, measuring the R-wave
•
amplitude is not possible. Press [Program] or [Undo Pending] first, then start the
measurement.
During the test the programming head must be continuously applied to the
•
pacemaker. The measurement is interrupted if the programming head is removed.
If the measurement is stopped or interrupted, the pacemaker returns to its
•
permanently programmed settings.
During the R-wave amplitude measurement the magnet mode, Flywheel and rate
•
response are temporarily disabled.
Reprogramming ventricular sensitivity – In the “Permanent” column, you can
reprogram the ventricular sensitivity based on the outcome of the test. Vitatron
recommends using a sensing safety margin of at least 100%, which means programming
the ventricular sensitivity to a setting less than 50% of the measured R-wave amplitude.
This means, for example, programming the ventricular sensitivity to a setting less than
3.0 mV if the measured R-wave amplitude is 6.0 mV.
Diagnostic information in the Rhythm Overview window can be helpful when assessing
ventricular sensing. Ventricular undersensing could be suspected if the percentage
ventricle paced counter is higher than expected.
Ventricular oversensing should be suspected if the VSPs counter is high (crosstalk)
or if the PVCs counter is higher than expected (myopotential sensing). Programming
the ventricular sensing polarity to bipolar or selecting a less sensitive ventricular
sensitivity setting (which means programming a higher ventricular sensitivity value) is
then recommended. Use the ECG to check that the PVCs counter is not increased by
atrial undersensing (see Section 7.9.1).
78
Page 79

C-series Reference Manual Section 6.4
6.4 VA interval measurement
Tests
⇒ VA Interval Measurement
Availability: DDD(R), DDI(R), VDD(R) modes
Dual chamber pacemakers feature a VA interval measurement, manual and automatic,
which is helpful in diagnosing retrograde conduction and FFRW sensing. During this test
the interval between the paced ventricular event and the sensed atrial event is measured
at one (manual test) or three (automatic test) ventricular pacing rates. The manual test
should be repeated at different rates to avoid a false positive diagnosis of retrograde
conduction if the sinus rhythm is the same as the ventricular pacing rate.
Warning: During the VA interval measurement the mode is changed to a ventricular
pacing mode. Consequently, there is no response to atrial arrhythmias.
6.4.1 Manual VA interval measurement
Figure 6-5. VA Interval Measurement window (manual test)
Setting up the manual VA interval measurement – To prepare for the measurement
take the following steps:
1. Position the programming head on the pacemaker.
2. Use the “Test Type” drop-down list to select the manual test.
3. Select the test rate in the “Test Value” column. The test rate can be any value from
40 min–1to 130 min–1.
79
Page 80

C-series Reference Manual Section 6.4
4. Adjust the atrial sensitivity, atrial sense polarity and atrial blanking in the “Test Value”
column.
Performing the manual VA interval measurement – The following steps describe
the general procedure:
1. Press [Start] to start the measurement. The programmer measures the VA interval
until the measurement is stopped.
2. Watch the EGM or ECG carefully on the programmer display. The marker
annotations are useful to identify the atrial and ventricular events. The measured
VA intervals are shown as marker intervals in the ECG window. If the pacemaker is
inhibited by spontaneous ventricular activity, stop the measurement and increase
the test rate. The test rate can be changed during the measurement if the VA
interval has already been measured at the new rate.
3. Press [Stop] or remove the programming head to stop the measurement.
4. Press [Test Strip…] to view the ECG recorded during the last measurement.
5. Press [Details…] to view the results of the measurement. They are presented
either in a graph (see Figure 6-7) or in a table. Select the preferred representation
by pressing the “Graph” or “Table” radio button. For the manual test, the last six
measurement rates are displayed.
6. Press [Print] to print the VA interval measurement report.
7. Press [Close] to leave the Results window.
Notes:
If the “Permanent” column contains boxed parameters, measuring the VA intervals is
•
not possible. Press [Program] or [Undo Pending] first, then start the measurement.
During the test the programming head must be continuously applied to the
•
pacemaker. The measurement is interrupted if the programming head is removed.
When the measurement is stopped or interrupted, the pacemaker returns to its
•
permanently programmed settings.
The VA interval is measured in the VVI mode. During the measurement Flywheel
•
and rate response are temporarily disabled.
Measured VA intervals are stored in the programmer memory. They can be printed
•
later by selecting the “VA Interval Measurement” report in the Reports window.
80
Page 81

C-series Reference Manual Section 6.4
6.4.2 Automatic VA interval measurement
Figure 6-6. VA Interval Measurement window (automatic test)
Setting up the automatic VA interval measurement – To prepare for the measurement
take the following steps:
1. Position the programming head on the pacemaker.
2. Use the “Test Type” drop-down list to select the automatic test.
3. Select the maximum test rate in the “Test Value” column. The maximum test rate
can be any value from 40 min
–1
above the programmed lower rate up to 130 min–1.
4. Adjust the atrial sensitivity, atrial sense polarity and atrial blanking in the “Test Value”
column.
Performing the automatic VA interval measurement – The following steps describe
the general procedure:
1. Press [Start] to start the measurement. The programmer automatically starts to
measure the VA interval at a rate 20 min–1above the programmed lower rate. The
start rate is increased by 10 min–1if there are more than three sensed ventricular
events in the first ten pacing cycles. The check for sensed ventricular events and the
increase of the start rate is repeated until fewer than four sensed ventricular events
occur in the first ten pacing cycles. The current rate is then used as the start rate. If
the start rate exceeds the selected maximum test rate, the test is stopped and a
warning is displayed on the programmer screen.
2. The pacemaker automatically repeats the test at a rate 10 min–1above the start rate
and at a rate 20 min–1above the start rate.
81
Page 82

C-series Reference Manual Section 6.4
3. If the test rate of the third measurement exceeds the selected maximum test rate, the
measurement is stopped and a message is displayed on the programmer screen.
4. The measurement ends automatically after the third measurement. The pacemaker
returns to its permanently programmed settings.
5. Press [Test Strip…] to view the ECG recorded during the last measurement.
6. Press [Details…] to view the results of the measurement. They are presented either
in a graph (see Figure 6-7) or in a table. Select the preferred representation by
pressing the “Graph” or “Table” radio button.
7. Press [Print] to print the VA interval measurement report.
8. Press [Close] to leave the Results window.
Figure 6-7. VA Interval Measurement - Results (graph)
Notes:
If the “Permanent” column contains boxed parameters, measuring the VA intervals is
•
not possible. Press [Program] or [Undo Pending] first, then start the measurement.
During the test the programming head must be continuously applied to the
•
pacemaker. The measurement is interrupted if the programming head is removed.
When the measurement is completed or interrupted, the pacemaker returns to
•
its permanently programmed settings.
The VA interval is measured in the VVI mode. During the measurement Flywheel
•
and rate response are temporarily disabled.
Measured VA intervals are stored in the programmer memory. They can be printed
•
later by selecting the “VA Interval Measurement” report in the Reports window.
82
Page 83

C-series Reference Manual Section 6.4
6.4.3 Programming advice to prevent FFRW sensing and retrograde conduction
Programming advice to prevent FFRW sensing – When the measured VA interval is
shorter than 200 ms FFRW sensing should be suspected. Check the EGM or ECG for
retrograde conduction between 150 and 200 ms. Try to eliminate FFRW sensing by
changing the sensing polarity to bipolar, changing the atrial sensitivity to a less sensitive
(higher) setting or lengthening the atrial blanking period.
Programming advice to prevent retrograde conduction – If the VA interval is stable
between 150 and 450 ms, at different ventricular pacing rates, retrograde conduction
should be suspected. To prevent retrograde conduction and avoid inducing pacemaker
mediated tachycardias (PMTs), Vitatron recommends programming mode switching
to “Auto”, PVC synchronous atrial stimulation to “On” or programming a short atrial
synchronization pace (ASP) interval.
Note: Although the VA interval measurement may reveal retrograde conduction in the
test mode (VVI), a permanently programmed AV synchronous mode might prevent the
occurrence of retrograde conduction (see Section 10.6).
6.5 Temporary test
Tests
⇒ Temporary test
Availability: All modes
Temporary test offers the possibility to temporarily reprogram a number of basic pacing
parameters for diagnostic purposes or for testing the effects of reprogramming on pacing.
The permanently programmed settings are restored automatically when the temporary
test ends or when the programming head is removed.
83
Page 84

C-series Reference Manual Section 6.5
Figure 6-8. Temporary Test window (dual chamber pacemaker)
Figure 6-9. Temporary Test window (single chamber pacemaker)
Setting up the temporary test – To prepare for the test take the following steps:
1. Position the programming head on the pacemaker.
2. Adjust the test values for mode, rate, maximum paced AV delay, atrial blanking (on
VP and VS), amplitude (atrial and ventricular), pulse duration (atrial and ventricular)
and sensitivity (atrial and ventricular) in the Temporary Test window.
3. Select the appropriate test mode using the following guidelines:
Use the OOO mode to check the patient’s intrinsic rhythm.
•
Use the AAI mode to check AV conduction at various rates.
•
84
Page 85

C-series Reference Manual Section 6.5
Use the VVI mode to test for pacemaker syndrome (retrograde conduction).
•
Use the triggered modes (AAT and VVT) to check sensing characteristics.
•
4. Increase or decrease the test rate to respectively suppress or search for intrinsic
rhythm
5. Adjust pulse amplitude or pulse duration to investigate crosstalk at high output
settings (in combination with a low sensitivity setting in the other channel).
6. Adjust the temporary sensitivity values to check for myopotentials (in combination,
for example, with a triggered mode) or for crosstalk (in combination with high output
settings in the other channel).
7. In dual chamber pacemakers, temporarily change the atrial blanking period to check
for the occurrence of far-field R-waves (in combination with low atrial sensitivity
settings).
8. In dual chamber pacemakers, temporarily change the maximum paced or sensed AV
delay to search for intrinsic AV conduction, to optimize AV delay or to prevent fusion.
Performing the temporary test – The following steps describe the general procedure:
1. Press [Start] to start the test.
2. Watch the ECG carefully on the programmer display. During the test all parameters,
except mode, can be changed.
3. Press [Stop] or remove the programming head to stop the test. The pacemaker
returns to its permanently programmed settings.
4. Press [Test Strip…] to view the ECG recorded during the last temporary test.
Note: During the test the programming head must be continuously applied to the
pacemaker. The measurement is interrupted if the programming head is removed.
6.6 Lead measurement
Tests
⇒ Lead Measurement
Availability: All modes, except OOO
The lead measurement is used to measure the exact output voltage, mean output
current, pulse energy and lead impedance for the atrial or ventricular lead, as shown in
Figure 6-10. In a single chamber mode, only the active chamber is displayed.
85
Page 86

C-series Reference Manual Section 6.6
The lead measurement is performed automatically every 10 minutes and the most recent
information is read out during initial interrogation of the pacemaker. The results are
stored for later review or printing. If required, the lead measurement can be repeated in
the Lead Measurement window.
Figure 6-10. Lead Measurement window (dual chamber pacemaker)
Performing the lead measurement – The following steps describe the general
procedure:
1. Position the programming head on the pacemaker.
2. Press [Measure] to start the measurement. The measurement ends automatically.
3. If the measurement was successful, the programmer displays the measured lead
impedance, pulse amplitude, pulse energy and average pulse current for the atrial or
ventricular lead. Press [Print] to print the battery status/lead measurement report.
4. If the measurement was not successful, the programmer displays a message
indicating why the lead measurement failed.
86
Page 87

C-series Reference Manual Section 6.6
Notes:
During the test the programming head must be continuously applied to the
•
pacemaker. The measurement is ended if the programming head is removed.
If the pacing or sensing polarity is bipolar, both the unipolar and bipolar lead
•
impedance are measured.
Lead impedance measurement results may be disturbed by electrocardiogram
•
monitoring equipment.
Interpretation of the lead measurement results – The lead measurement provides
information about the safety margin between the measured stimulation threshold and
the actual output voltage. It also gives information about the actual power consumption
of the pacemaker. The trend in lead impedance is an indication for the stability of the
lead. A significant decrease in impedance may indicate an insulation problem or a short
circuit, while a significant increase may indicate a lead fracture, loose setscrew or a
possible electrode dislocation.
87
Page 88

C-series Reference Manual
88
Page 89

C-series Reference Manual
7 Diagnostics
7.1 Introduction
The diagnostic information available in the pacemaker helps the physician to monitor the
patient and to check how the pacemaker is responding. Diagnostics can also reveal
whether pacemaker parameters need adjusting in order to offer the patient optimum
pacing therapy.
This chapter explains how the diagnostics help the user to recognize unexpected patterns
or events. The Therapy Advisor (see Section 7.2) highlights information on important
events and displays suggestions for programming the pacemaker. Rhythm Overview
(see Section 7.4.1) gives an overview of atrial and ventricular rhythm. More detailed
diagnostic information on the distribution of events in graphs, Holters and histograms can
be used to evaluate the effectiveness of pacemaker or drug therapy.
The first part of the chapter provides general information about the following features:
Therapy Advisor (see Section 7.2)
•
data collection and storage (see Section 7.3)
•
how to display the data (see Section 7.4)
•
The second part of the chapter guides you through the diagnostic options available for
assessing the following events:
atrial rhythm (see Section 7.5)
•
ventricular rhythm (see Section 7.6)
•
AV synchrony (see Section 7.7)
•
rate response (see Section 7.8)
•
the pacemaker’s sensing, including P-wave sensing, FFRW sensing and retrograde
•
conduction (see Section 7.9)
7.2 Therapy Advisor
The Therapy Advisor analyzes technical, diagnostic and programming data taken from
the pacemaker memory (battery status, histograms, Holters, counters and programmed
parameters) and alerts you to important events or areas of concern. It also gives
suggestions for programming the pacemaker to offer optimal therapy.
Therapy advice is available in DDD(R), VDD(R), VVI(R) and AAI(R) modes, when data
has been collected for at least one week.
89
Page 90

C-series Reference Manual Section 7.2
Therapy Advisor messages appear in the Status window immediately after initial
interrogation of the pacemaker. The information is based on the contents of pacemaker
memory at initial pacemaker interrogation, and is not updated during the follow-up
session. The Therapy Advisor can be switched on or off in the Programmer Preferences
window (see Section 4.3.1).
Press one of the Therapy Advisor messages to open a window with more diagnostic
information and programming advice for optimizing therapy. Consider whether these
suggestions provide the optimal therapy for the patient or whether specific circumstances
apply which justify a different therapy or setting.
A message in the Therapy Advisor window stating that there is nothing significant to
report means that the pacemaker has not detected anything unusual in the pacemaker
diagnostics.
The Therapy Advisor first checks lead and sensing conditions. If it detects a problem with
lead impedance, P-wave sensing or FFRW sensing, no therapy advice is given. Therapy
advice is not available if the pacemaker has been reset and full restore was not possible,
after emergency programming or when the pacemaker is indicated for replacement.
Notes:
The Therapy Advisor has no knowledge of either the initial indication for pacing or
•
the patient’s medical condition. These are therefore not taken into account when
formulating advice.
Warning: “Therapy Advisor” should not replace the physician’s expert judgement.
7.3 Data collection and storage periods
The pacemaker records each occurrence of specific cardiac events, such as atrial senses
(AS), ventricular paces (VP), or premature ventricular contractions (PVCs). It also collects
data on episodes of certain cardiac behavior, such as a period of atrial tachyarrhythmia.
The pacemaker collects most diagnostic data between follow-up sessions. These
session-to-session diagnostics are intended for assessing the status of the patient since
the last follow-up session. One hour after the end of a session, diagnostic data from the
previous period, including Therapy Advisor information, is cleared from the pacemaker
memory and data collection starts again. There is an option to keep diagnostic data from
the previous follow-up period (see Section 7.3.1).
The pacemaker records the incidence of certain cardiac events and episodes in counters.
The data collected in the main counters is presented in the Rhythm Overview window
(see Section 7.4.1). Some counters display the incidence of events as a percentage of
the collection period. Other counters show how often an event or episode occurred, for
90
Page 91

C-series Reference Manual Section 7.3
example the number of PVCs per day. This represents the average occurrence over
a certain period. The chosen period (minute, hour, day, week, month or year) is the
shortest unit of time during which at least one relevant event or episode occurred. The
atrial and ventricular event counters are listed in Section 7.5.1 and Section 7.6.1.
Holters accumulate data in the pacemaker over a limited collection period. The 24-hour
Holter (see Section 7.4.4) collects data continuously over a 24-hour period. When you
call up this Holter during a follow-up session the programmer displays the data recorded
in the last 24 hours. Data collection continues during the follow-up session. Data older
than 24 hours is cleared automatically. The 30-minute Holter (see Section 7.4.5) is
intended for testing during the follow-up session. You may start collection during a
follow-up session, for example, to show the rate pattern during an exercise stress test.
Notes:
Session-to-session and 24-hour diagnostic data is cleared from the pacemaker if
•
the user reprograms a pacing therapy parameter or resets the pacemaker time.
Diagnostic data collected before the change can still be displayed during the current
follow-up session.
Collection of diagnostic data stops after a partial restore, emergency programming,
•
or when the battery status is “Replace PM”. Any data collected up to that time
remains in the pacemaker’s memory and can still be displayed on the programmer.
After a full restore (see Appendix A), all collected data is cleared and data collection
•
restarts.
7.3.1 Keeping diagnostic data
Data
⇒ Diagnostic Setup
⇒ Keep
The pacemaker normally deletes the session-to-session diagnostics one hour after the
end of a follow-up session. Press [Keep] to save this data. The pacemaker continues
to add diagnostic data to the saved data until the start of the next follow-up session.
Session-to-session diagnostics and the Therapy Advisor are based on all the saved data.
This option is not available if you have permanently reprogrammed a pacing therapy
parameter, or reset the pacemaker time, during the current follow-up session.
91
Page 92

C-series Reference Manual Section 7.4
7.4 Displaying diagnostic data
Therapy advice appears in the Status window after initial pacemaker interrogation.
Press the “Data” icon and select “Rhythm Overview” to access more detailed diagnostics
(see Section 7.4.1).
Four types of diagnostics are available in the pacemaker:
Rhythm Overview gives a quick impression of the patient’s cardiac rhythm in the
•
period since the last follow-up session (see Section 7.4.1).
Diurnal Rhythm Distribution graphs show how the cardiac events and episodes
•
were distributed during each hour of the day in the period since the last follow-up
session (see Section 7.4.2).
Histograms show the distribution of cardiac events and episodes in the period since
•
the last follow-up (see Section 7.5.3 and Section 7.6.3).
Holters are used to reveal trends in rate and rhythm over a limited period (see
•
Section 7.4.4 and Section 7.4.5).
When viewing the diagnostics, press [Close] to close any diagnostic data window and
return to the Rhythm Overview window. Press [Print] for a printed copy of any diagnostic
data window.
In the diagnostic data windows, the “Additional Information” column lists the pacemaker
mode and the settings of relevant pacemaker parameters during the data collection
period.
In diagnostic data graphs, the color green represents physiological rhythm. Yellow
indicates pacing. Red and orange alert you to unexpected or pathological patterns and
events.
In histogram windows, data can be presented in graphical format, or with the exact
values in table format.
Two formats are available for presenting Diurnal Rhythm Distribution and Holter data:
rate profile and rhythm details. Choose the desired type of graph by pressing the
appropriate radio button.
Rate profile – A rate profile diagram shows the atrial and ventricular rates in each time
period, averaged over the collection period. The atrial and ventricular rates will be
identical during AV synchronous operation.
The information is presented in the form of a line diagram, with the rates given in beats
per minute ( min–1). Horizontal lines represent the lower rates (day and night), maximum
pacing rate and maximum tracking rate. The maximum tracking rate is only shown when
92
Page 93

C-series Reference Manual Section 7.4
it falls within the range of recorded rates. A white bar along the x-axis indicates the
daytime hours programmed in the pacemaker.
Rhythm details – Rhythm details graphs present the contents of counters for each
time interval, averaged over the collection period. A split window allows comparison
of two graphs. A white bar along the x-axis indicates the daytime hours programmed
in the pacemaker.
Use the drop-down lists to choose any two rhythm details graphs to display in the top
and bottom graph. Comparison of the two graphs is helpful when analyzing the causes
of cardiac events or pacemaker behavior at certain times. See Section 7.5.2 and
Section 7.6.2 for a list of the available graphs.
7.4.1 Rhythm Overview
Data
⇒ Rhythm Overview
The rhythm overview gives a quick impression of the patient’s cardiac rhythm in the
period since the previous follow-up session (see Figure 7-1). Various counters inform
the user about atrial and ventricular events and episodes, as well as selected episodes
recorded during the collection period. Unexpectedly high or low values in these counters
may indicate that you should look into more detailed diagnostic data to find the cause.
Figure 7-1. The Rhythm Overview window
93
Page 94

C-series Reference Manual Section 7.4
Select one of the graphs to display the distribution of cardiac events in Holters and
histograms.
7.4.2 Diurnal Rhythm Distribution
Data
⇒ Rhythm Overview
⇒ Diurnal Rhythm Distribution
The diurnal rhythm distribution diagnostics show the distribution of certain events over
the day. For each hour of the day, the pacemaker keeps a count of the relevant events
during the whole collection period.
Diurnal rhythm distribution data can help you to correlate cardiac events with patient
activities or the patient’s reaction to drug intake at certain times of the day. This
information is helpful when optimizing the pacemaker settings or drug therapy. You may
also use this information to relieve a patient of symptoms that occur at a particular time
of day. The diurnal rhythm distribution graphs provide baseline information on average
rates and patterns over the collection period. This can be useful, in combination with the
24-hour Holter (see Section 7.4.4), to identify recent changes in rate and rhythm when
a patient presents with new symptoms.
Figure 7-2. Diurnal Rhythm Distribution window: Rhythm Details example
94
Page 95

C-series Reference Manual Section 7.4
Two presentation formats are available, rate profile and rhythm details. The rate profile
diagram shows the atrial and ventricular rates during each hour of the day, averaged over
the collection period. Rhythm details graphs present the contents of counters during
each hour of the day, averaged over the collection period. The available rhythm details
graphs are listed in Section 7.5.2 and Section 7.6.2.
Note: Diurnal rhythm distribution diagnostics are only available if data has been collected
in the pacemaker for at least 24 hours.
7.4.3 Histograms
Data
⇒ Rhythm Overview
⇒ select a histogram
A histogram shows the distribution of events that have occurred since the last follow-up
session. The following histograms are available in diagnostics:
Atrial rate histogram (see Section 7.5.3)
•
Ventricular rate histogram (see Section 7.6.3)
•
P-wave histogram (see Section 7.9.1)
•
VA interval histogram (see Section 7.9.2)
•
Data can be presented in graphical format, or with the exact values in table format.
7.4.4 24-hour Holter
Data
⇒ Rhythm Overview
⇒ 24-Hour Holter
The 24-hour Holter shows information about the rate and rhythm over the day and night
immediately preceding the follow-up session. This may help you to identify unexpected
patterns at the time when the patient reported symptoms (see Figure 7-3).
95
Page 96

C-series Reference Manual Section 7.4
Figure 7-3. The 24-hour Holter window: Rhythm Details example
The 24-hour Holter presents the data collected in counters for each five minutes over the
previous 24 hours. Two graphical formats are available: rate profile and rhythm details.
The rate profile diagram shows the atrial and ventricular rates, averaged over each
five-minute period during the previous 24 hours. The rhythm details graphs present
the contents of counters for each five-minute period over the previous 24 hours. The
rhythm details graphs available for the 24-hour Holter are listed in Section 7.5.2 and
Section 7.6.2.
7.4.5 30-minute Holter
Data
⇒ Rhythm Overview
⇒ 30-Minute Holter
The 30-minute Holter collects data during a follow-up session. It is useful, for example, to
record the rate pattern and the results of the activity sensor during an exercise stress test.
When you select the 30-minute Holter, any data remaining from a previous recording is
displayed. A note states the date on which the data was collected.
To start recording a 30-minute Holter, press [Start] in the Rate Profile window. Any
previously recorded 30-minute Holter data is cleared. Recording stops automatically
96
Page 97

C-series Reference Manual Section 7.4
after 30 minutes. It is not possible to stop the recording manually. At any time during
the 30-minute data collection period, you can see a snapshot of the data collected so
far by closing and reopening the window.
You can restart the 30-minute Holter while it is running by pressing [Start] again.
Two graphical formats are available: rate profile and rhythm details. The rate profile
diagram shows the patient’s atrial and ventricular rates averaged for each 10-second
period over the 30 minutes (see Figure 7-4). Rhythm details graphs present the contents
of counters for each 10-second period over the 30 minutes. The rhythm details graphs
available for the 30-minute Holter are listed in Section 7.5.2 and Section 7.6.2.
Figure 7-4. The 30-minute Holter window: Rate Profile example
Note: The parameter settings are those that were applicable when you started the
30-minute Holter. Changes made to these parameters during recording will not be shown.
7.5 Assessing atrial rhythm
7.5.1 Atrial rhythm overview
Atrial rhythm information enables you to evaluate sinus node function, arrhythmias and
rate response. The Rhythm Overview window summarizes atrial rhythm information.
97
Page 98

C-series Reference Manual Section 7.5
The first three atrial counters in the Rhythm Overview window record all atrial events in
the collection period, and thus add up to 100%. The other counters give information
about the incidence of atrial events and episodes.
Atrium Paced – The percentage of time that the atrium was paced during the collection
period. Information about the incidence of atrial pacing is helpful when programming
the lower rate and night lower rate. A high percentage of atrial pacing may indicate a
need for rate responsive pacing.
Physiologic A senses – The percentage of atrial sensed events that the pacemaker
classified as physiological.
Pathologic A senses – The percentage of atrial sensed events that the pacemaker
classified as bradyarrhythmia or atrial tachyarrhythmia. To investigate the underlying
causes of a high percentage of pathological senses, look at the atrial rate histogram.
PACs – The total number of premature atrial contractions (PACs) recorded by the
pacemaker in the atrial collection period, and the average number of PACs per unit of
time. For more information, refer to the diurnal rhythm distribution graphs or the 24–hour
Holter.
Atrial Tachy Episodes – The number of episodes during which the pacemaker classified
the rhythm as atrial tachyarrhythmia in the collection period, and the average number of
these episodes per unit of time. For more information, look at the atrial rate histogram,
diurnal rhythm distribution graphs or the 24–hour Holter.
Retrograde Conduction Episodes – The total number of episodes of retrograde
conduction detected by the pacemaker in the collection period, and the average number
of episodes per unit of time.
7.5.2 Atrial rhythm details graphs
You can select the following atrial rhythm details graphs in the “Rhythm Details”
drop-down lists of Diurnal Rhythm Distribution or Holters.
Rate Profile – The average atrial and ventricular rates during the collection period. The
rates are given in beats per minute ( min–1), in the form of a line diagram.
Atrial Rhythm – The percentage of time that the pacemaker sensed and paced in the
atrium during the collection period. Atrial sensed events are divided into physiological,
bradyarrhythmia and tachyarrhythmia senses.
98
Page 99

C-series Reference Manual Section 7.5
Atrial Tachy Episodes – The percentage of time or number of episodes during which
the pacemaker detected an atrial tachyarrhythmia during the collection period.
PACs – The percentage of time or number of times that the pacemaker sensed a
premature atrial contraction (PAC) during the collection period.
Note: For Atrial Tachy Episodes and PACs, the diurnal rhythm distribution graphs show
the percentage of time when a certain event or episode occurred; Holter graphs show the
number of events or episodes per unit of time.
7.5.3 Atrial rate histogram
Data
⇒ Rhythm Overview
⇒ Atrial Rate Histogram
Availability: DDD(R), DDI(R), DOO, VDD(R), AAI(R), AAT, AOO modes
The atrial rate histogram shows the rate distribution of all atrial events recorded since
the previous follow-up session. It also shows the proportion of various types of rhythm
as a function of the atrial rate. This can be helpful when assessing the patient’s sinus
node function, arrhythmias and pacemaker-driven rates.
The atrial rate histogram helps you to identify whether the sinus node is functioning
normally. It also provides information about tachyarrhythmias and bradyarrhythmias,
and whether the pacemaker is providing an adequate substitute for normal sinus node
function. Information about bradyarrhythmias is especially important for patients with the
pacemaker programmed in the VDD mode.
This information can be useful when making adjustments in the pacemaker settings for
lower rates, maximum rates and sensors. The histogram can show four types of data.
Brady – The percentage of time that the pacemaker classified atrial senses as atrial
bradyarrhythmia.
Paced – The percentage of time that the pacemaker paced the atrium.
Sinus – The percentage of time that the pacemaker classified atrial senses as
physiological atrial senses.
Tachy – The percentage of time that the pacemaker classified atrial senses as
tachyarrhythmia.
99
Page 100

C-series Reference Manual Section 7.5
The histogram presents data in 21 rate classes, each representing a rate of 10 min
In graph format, the atrial rate histogram shows the occurrence of different rate types
for each rate class (see Figure 7-5). In table format, the atrial rate histogram shows the
rate class and recorded percentages of each rate type.
Figure 7-5. Atrial Rate Histogram window: Graph example
–1
.
7.6 Assessing ventricular rhythm
The following diagnostics can be helpful for evaluating the patient’s AV node function,
mode switching, and rate response in VVIR mode.
Rhythm Overview windows summarize ventricular rhythm information (see
•
Section 7.6.1).
Diurnal Rhythm Distribution and Holters allow you to investigate rhythm details
•
(see Section 7.6.2).
The ventricular rate histogram shows the distribution of ventricular events during the
•
collection period (see Section 7.6.3).
100
 Loading...
Loading...