
Infuse™ Bone Graft/LT-Cage™
Lumbar Tapered Fusion Device
Infuse™ Bone Graft/Inter Fix™
Threaded Fusion Device
Infuse™ Bone Graft/Inter Fix™ RP
Threaded Fusion Device – Reduced
Profile
Infuse™ Bone Graft/Perimeter™
Interbody Fusion Device
Infuse™ Bone Graft/Clydesdale™
Spinal System
Infuse™ Bone Graft/Divergence-L™
Anterior/Oblique Lumbar Fusion
System
Infuse™ Bone Graft/Pivox™ Oblique
Lateral Spinal System
0381148E Rev. I
2019-11-04
ENGLISH IMPORTANT MEDICAL INFORMATION
Caution: Federal (USA) law restricts this device to sale by or on the order of a physician with appropriate training.
The following contains important medical information on the use of Infuse™ Bone Graft with a variety of Medtronic interbody
fusion cages. These interbody fusion devices include the LT-Cage™ Lumbar Tapered Fusion Device, the Inter Fix™ Threaded
Fusion Device, the Inter Fix™ RP Threaded Fusion Device, the Perimeter™ Interbody Fusion Device, the Clydesdale™ Spinal
System, the Divergence-L™ Anterior/Oblique Lumbar Fusion System, and the Pivox™ Oblique Lateral Spinal System. Hereafter
in this insert, these cages will be referred to collectively as Medtronic Interbody Fusion Device.
DESCRIPTION
The Infuse™ Bone Graft/Medtronic Interbody Fusion Device consists of two components containing three parts – a spinal fusion
cage, a recombinant human bone morphogenetic protein, and a carrier/scaffold for the bone morphogenetic protein and
resulting bone. The Infuse™ Bone Graft component is inserted into the Medtronic Interbody Fusion Device component to form
the complete Infuse™ Bone Graft/Medtronic Interbody Fusion Device. These components must be used as a system for the
prescribed indication described below. The bone morphogenetic protein solution component must not be used without
the carrier/scaffold component or with a carrier/scaffold component different from the one described in this document.
The Infuse™ Bone Graft component must not be used without the Medtronic Interbody Fusion Device component.
Medtronic Interbody Fusion Device Component
LT-Cage™ Lumbar Tapered Fusion Device
The LT-Cage™ Device consists of a hollow, perforated, machined cylinder with opposing flat sides. There are two holes on
each of the two flat sides. On each of the two rounded aspects, there is a single rounded slot. The implants have a helical screw
thread on the outer surface. One end of the device is closed. The other end is open to be filled with the Infuse™ Bone Graft
component.
The LT-Cage™ implants are made from implant-grade titanium alloy (Ti-6Al-4V) described by such standards as ASTM F136 or
its ISO equivalent.

The LT-Cage™ Lumbar Tapered Fusion Device component is sold separately from the Infuse™ Bone Graft component;
however, these two components must be used together. The package labeling for the LT-Cage™ Lumbar Tapered Fusion
Device contains complete product information for this component.
Inter Fix™ Threaded Fusion Device
The Inter Fix™ Device consists of a hollow, perforated cylinder with parallel sides and an endcap. The endcaps of the Inter
Fix™ cages are sized according to the diameter of the cylinders and are applied to the open end of the cylinders after they are
filled with Infuse™ Bone Graft.
The Inter Fix™ Threaded Fusion Device implants are made from implant-grade titanium alloy (Ti-6Al-4V) described by such
standards as ASTM F136 or its ISO equivalent.
The Inter Fix™ Threaded Fusion Device component is sold separately from the Infuse™ Bone Graft component; however, these
two components must be used together. The package labeling for the Inter Fix™ Threaded Fusion Device contains complete
product information for this component.
Inter Fix™ RP Threaded Fusion Device
The Inter Fix™ RP Device consists of a hollow, perforated cylinder with a single, large, outer-radiused groove along the entire
longitudinal axis that extends into the inside diameter of the device. Both ends of the Inter Fix™ RP implant are closed.
The Inter Fix™ RP Threaded Fusion Device implants are made from implant-grade titanium alloy (Ti-6Al-4V) described by such
standards as ASTM F136 or its ISO equivalent.
The Inter Fix™ RP Threaded Fusion Device component is sold separately from the Infuse™ Bone Graft component; however,
these two components must be used together. The package labeling for the Inter Fix™ RP Threaded Fusion Device contains
complete product information for this component.
Perimeter™ Interbody Fusion Device
The Perimeter™ Interbody Fusion Device consists of PEEK cages of various widths and heights, which can be inserted
between two lumbar or lumbosacral vertebral bodies to give support and correction during lumbar interbody fusion surgeries.
The hollow geometry of the implants allows them to be packed with Infuse™ Bone Graft.
The Perimeter™ Interbody Fusion Device is offered in a variety of sizes, although only certain sizes of the PEEK device are
approved for use with Infuse™ Bone Graft. The device is designed with teeth across both the superior and inferior surfaces to
allow the implant to grip the superior and inferior end plates, thus providing expulsion resistance.
The Perimeter™ Interbody Fusion Device component is sold separately from the Infuse™ Bone Graft component; however,
these two components must be used together. The package labeling for the Perimeter™ Interbody Fusion Device contains
complete product information for this component.
Clydesdale™ Spinal System
The Clydesdale™ Spinal System consists of PEEK cages of various widths and heights, which include tantalum markers. These
devices can be inserted between two lumbar or lumbosacral vertebral bodies to give support and correction during lumbar
interbody fusion surgeries. The hollow geometry of the implants allows them to be packed with Infuse™ Bone Graft.
The Clydesdale™ Spinal System component is sold separately from the Infuse™ Bone Graft component; however, these two
components must be used together. The package labeling for the Clydesdale™ Spinal System contains complete product
information for this component.
Divergence-L™ Anterior/Oblique Lumbar Fusion System
The Divergence-L™Anterior/Oblique Lumbar interbody cages, which are available in various widths, heights, and lordosis, can
be inserted between two lumbar vertebral bodies to give support and correction during lumbar interbody fusion surgeries. The
hollow geometry of the implants allows them to be packed with Infuse™ Bone Graft and must be used with supplemental
fixation. The cages are manufactured from medical grade PEEK and titanium alloy with tantalum markers and are provided
sterile.
Pivox™ Oblique Lateral Spinal System
The Pivox™ Oblique Lateral Spinal System interbody cages are available in various widths, heights, and lordosis, and can be
inserted between two lumbar vertebral bodies to give support and correction during lumbar interbody fusion surgeries. The
hollow geometry of the implants allows them to be packed with Infuse™ Bone Graft and must be used with supplemental
fixation. The cages are manufactured from medical grade PEEK and titanium alloy with tantalum markers and are provided
sterile.
Note: the Inter Fix™ Threaded Fusion Device and the Inter Fix™ RP Threaded Fusion Device may be used together to
treat a spinal level. The LT-Cage™ Lumbar Tapered Fusion Device, the Perimeter™ Interbody Fusion Device, the
Clydesdale™ Spinal System, the Divergence-L™ Anterior/Oblique Lumbar Fusion System, and the Pivox™ Oblique
Lateral Spinal System implants are not to be used in conjunction with either the Inter Fix™ or Inter Fix™ RP implants
to treat a spinal level.
Perimeter™, Clydesdale™, Divergence-L™, and Pivox™ devices must be used with any supplemental fixation system
cleared for use in the lumbar spine.

Infuse™ Bone Graft Component
Infuse™ Bone Graft consists of recombinant human Bone Morphogenetic Protein-2 (rhBMP-2, known as dibotermin alfa) placed
on an absorbable collagen sponge (ACS). The Infuse™ Bone Graft component induces new bone tissue at the site of
implantation. Based on data from non-clinical studies, the bone formation process develops from the outside of the implant
towards the center until the entire Infuse™ Bone Graft component is replaced by trabecular bone.
rhBMP-2 is the active agent in the Infuse™ Bone Graft component. rhBMP-2 is a disulfide-linked dimeric protein molecule with
two major subunit species of 114 and 131 amino acids. Each subunit is glycosylated at one site with high-mannose-type
glycans. rhBMP-2 is produced by a genetically engineered Chinese hamster ovary cell line.
rhBMP-2 and excipients are lyophilized. Upon reconstitution, each milliliter of rhBMP-2 solution contains: 1.5mg of rhBMP-2;
5.0mg sucrose, NF; 25mg glycine, USP; 3.7mg L-glutamic acid, FCC; 0.1mg sodium chloride, USP; 0.1mg polysorbate 80, NF;
and 1.0mL of sterile water. The reconstituted rhBMP-2 solution has a pH of 4.5; is clear, colorless to slightly yellow; and is
essentially free from plainly visible particulate matter. The concentration of rhBMP-2 is 1.5mg/ml.
The ACS is a soft, white, pliable, absorbent implantable matrix for rhBMP-2. ACS is made from bovine Type I collagen obtained
from the deep flexor (Achilles) tendon. The ACS acts as a carrier for the rhBMP-2 and acts as a scaffold for new bone
formation.
The Infuse™ Bone Graft component is prepared at the time of surgery and allowed a prescribed amount of time (no less than
15 minutes) before placement inside of the Medtronic Interbody Fusion Device components. The Instructions for Preparation
contain complete details on preparation of the Infuse™ Bone Graft/Medtronic Interbody Fusion Device.
Various sizes of Infuse™ Bone Graft kits are available based on the internal volume of the Medtronic Interbody Fusion Device
component that is selected. Each kit contains all the components necessary to prepare the Infuse™ Bone Graft component: the
rhBMP-2, which must be reconstituted; sterile water; absorbable collagen sponge(s); syringes with needles; this package insert;
and instructions for preparation. The number of each item may vary depending on the size of the kit.
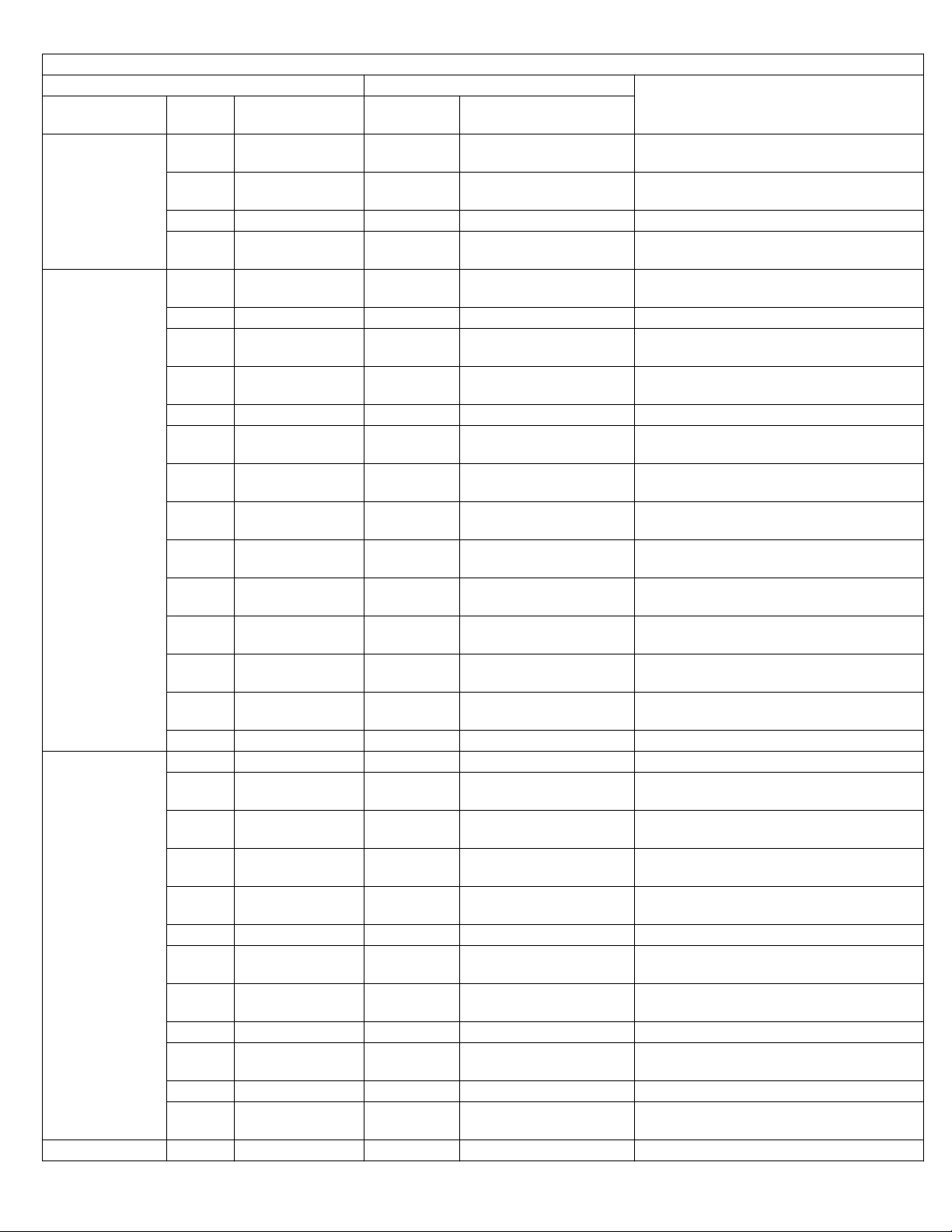
The tables below list the appropriate Infuse™ Bone Graft kit for the corresponding Medtronic Interbody Fusion Device
component size.
Infuse™ Bone Graft/LT-Cage™ Lumbar Tapered Fusion Device Combinations
LT-Cage™ Lumbar Tapered Fusion Device Appropriate Infuse™ Bone Graft Kit
Part #
8941420 14x20 7510200 Small (2.8) 2.8ml
8941423 14x23 7510200 Small (2.8) 2.8ml
8941620 16x20 7510200 Small (2.8) 2.8ml
8941623 16x23 7510400 Medium (5.6) 5.6ml
8941626 16x26 7510400 Medium (5.6) 5.6ml
8941823 18x23 7510400 Medium (5.6) 5.6ml
8941826 18x26 7510600 Large Pre-Cut (8.0) 8.0ml
8941826 18x26 7510800 Large II (8.0) 8.0ml
Size (lead diameter, mm x length,
mm)
Part # Kit name (size in cc)
Reconstituted rhBMP-2/ACS graft
volume
Infuse™ Bone Graft/Inter Fix™ Threaded Fusion Device Combinations (Dual Inter Fix™ Devices)
Inter Fix™ Threaded Fusion Device Appropriate Infuse™ Bone Graft Kit
Part #
890120 12x20 7510200 Small (2.8) 2.8ml
890125 12x25 7510200 Small (2.8) 2.8ml
890140 14x20 7510200 Small (2.8) 2.8ml
890143 14x23 7510200 Small (2.8) 2.8ml
890146 14x26 7510200 Small (2.8) 2.8ml
890149 14x29 7510200 Small (2.8) 2.8ml
890160 16x20 7510200 Small (2.8) 2.8ml
890163 16x23 7510200 Small (2.8) 2.8ml
890166 16x26 7510400 Medium (5.6) 5.6ml
890169 16x29 7510400 Medium (5.6) 5.6ml
890180 18x20 7510400 Medium (5.6) 5.6ml
890183 18x23 7510400 Medium (5.6) 5.6ml
890186 18x26 7510400 Medium (5.6) 5.6ml
890189 18x29 7510400 Medium (5.6) 5.6ml
890200 20x20 7510400 Medium (5.6) 5.6ml
Size (diameter, mm x length,
mm)
Part # Kit name (size in cc)
Reconstituted rhBMP-2/ACS graft
volume

Infuse™ Bone Graft/Inter Fix™ Threaded Fusion Device Combinations (Dual Inter Fix™ Devices)
Inter Fix™ Threaded Fusion Device Appropriate Infuse™ Bone Graft Kit
Part #
Size (diameter, mm x length,
mm)
Part # Kit name (size in cc)
Reconstituted rhBMP-2/ACS graft
volume
890203 20x23 7510400 Medium (5.6) 5.6ml
890206 20x26 7510600 or 7510800 Large (8.0)* 8.0ml
890209 20x29 7510600 or 7510800 Large (8.0)* 8.0ml
890220 22x20 7510600 or 7510800 Large (8.0)* 8.0ml
890223 22x23 7510600 or 7510800 Large (8.0)* 8.0ml
890240 24x20 7510600 or 7510800 Large (8.0)* 8.0ml
* May be either the Large (Pre-Cut) or Large II Kit
Infuse™ Bone Graft/Inter Fix™ and Inter Fix™ RP Threaded Fusion Device Combinations
(Inter Fix™ RP Device with Inter Fix™ Device)
Inter Fix™ and Inter Fix™ RP Threaded Fusion
Devices
Part # of Inter Fix™ De-
†
vices
Size (diameter, mm x
length, mm)
Appropriate Infuse™ Bone Graft Kit
Part # Kit name (size in cc)
Reconstituted
rhBMP-2/ACS graft vol-
890120 12x20 7510200 Small (2.8) 2.8ml
890125 12x25 7510200 Small (2.8) 2.8ml
890140 14x20 7510200 Small (2.8) 2.8ml
890143 14x23 7510200 Small (2.8) 2.8ml
890146 14x26 7510200 Small (2.8) 2.8ml
890149 14x29 7510200 Small (2.8) 2.8ml
890160 16x20 7510200 Small (2.8) 2.8ml
890163 16x23 7510200 Small (2.8) 2.8ml
890166 16x26 7510400 Medium (5.6) 5.6ml
890169 16x29 7510400 Medium (5.6) 5.6ml
890180 18x20 7510400 Medium (5.6) 5.6ml
890183 18x23 7510400 Medium (5.6) 5.6ml
890186 18x26 7510400 Medium (5.6) 5.6ml
890189 18x29 7510400 Medium (5.6) 5.6ml
890200 20x20 7510400 Medium (5.6) 5.6ml
890203 20x23 7510400 Medium (5.6) 5.6ml
890206 20x26 7510600 or 7510800 Large (8.0)* 8.0ml
890209 20x29 7510600 or 7510800 Large (8.0)* 8.0ml
890220 22x20 7510600 or 7510800 Large (8.0)* 8.0ml
890223 22x23 7510600 or 7510800 Large (8.0)* 8.0ml
890226 22x26 7510600 or 7510800 Large (8.0)* 8.0ml
890229 22x29 7510600 or 7510800 Large (8.0)* 8.0ml
890240 24x20 7510600 or 7510800 Large (8.0)* 8.0ml
890243 24x23 7510600 or 7510800 Large (8.0)* 8.0ml
ume
†
The Inter Fix™ Threaded Fusion Device should be used with the corresponding size of the Inter Fix™ RP Threaded Fusion
Device.
* May be either the Large (Pre-Cut) or Large II Kit.
Infuse™ Bone Graft/Inter Fix™ RP Threaded Fusion Device Combinations
(Dual Inter Fix™ RP Devices)
Inter Fix™ RP Threaded Fusion Device Appropriate Infuse™ Bone Graft Kit
Part # Size (diameter, mm x length, mm) Part # Kit size
Reconstituted rhBMP-2/ACS graft vol-
ume
9011221 12x20 7510200 Small (2.8) 2.8ml
9011225 12x25 7510200 Small (2.8) 2.8ml
9011420 14x20 7510200 Small (2.8) 2.8ml
9011423 14x23 7510200 Small (2.8) 2.8ml

Infuse™ Bone Graft/Inter Fix™ RP Threaded Fusion Device Combinations
(Dual Inter Fix™ RP Devices)
Inter Fix™ RP Threaded Fusion Device Appropriate Infuse™ Bone Graft Kit
Part # Size (diameter, mm x length, mm) Part # Kit size
9011426 14x26 7510200 Small (2.8) 2.8ml
9011429 14x29 7510200 Small (2.8) 2.8ml
9011620 16x20 7510200 Small (2.8) 2.8ml
9011623 16x23 7510200 Small (2.8) 2.8ml
9011626 16x26 7510400 Medium (5.6) 5.6ml
9011629 16x29 7510400 Medium (5.6) 5.6ml
9011820 18x20 7510400 Medium (5.6) 5.6ml
9011823 18x23 7510400 Medium (5.6) 5.6ml
9011826 18x26 7510400 Medium (5.6) 5.6ml
9011829 18x29 7510400 Medium (5.6) 5.6ml
9012020 20x20 7510400 Medium (5.6) 5.6ml
9012023 20x23 7510400 Medium (5.6) 5.6ml
9012026 20x26 7510400 Medium (5.6) 5.6ml
9012029 20x29 7510400 Medium (5.6) 5.6ml
9012220 22x20 7510400 Medium (5.6) 5.6ml
9012223 22x23 7510400 Medium (5.6) 5.6ml
9012226 22x26 7510600 or 7510800 Large (8.0)* 8.0ml
9012229 22x29 7510600 or 7510800 Large (8.0)* 8.0ml
9012420 24x20 7510600 or 7510800 Large (8.0)* 8.0ml
9012423 24x23 7510600 or 7510800 Large (8.0)* 8.0ml
Reconstituted rhBMP-2/ACS graft vol-
ume
* May be either the Large (Pre-Cut) or Large II Kit.
SINGLE CAGE USE
The tables below describe how to use the X Small (1.4cc) & XX Small (0.7cc) kits to fill smaller single LT-Cage™, Inter Fix™, or
Inter Fix™ RP devices if the need arises during surgery, due to the loss or contamination of a sponge or sponges. In addition,
information is provided on use of Infuse™ Bone Graft with certain sizes of the Perimeter™, Clydesdale™, Divergence-L™, and
Pivox™ devices, which are implanted at a single device per level.
Infuse™ Bone Graft/LT-Cage™ Lumbar Tapered Fusion Device Combinations
Single LT-Cage™ Device Fill
LT-Cage™ Lumbar Tapered Fusion Device Recommended Infuse™ Bone Graft Kit(s)
Part # Size (lead diameter, mm x length, mm) Part # Kit size
8941420 14x20 7510100 X Small (1.4) 1.4ml
8941423 14x23 7510100 X Small (1.4) 1.4
8941620 16x20
8941623 16x23
Infuse™ Bone Graft/Inter Fix™ Threaded Fusion Device Combinations
Inter Fix™ Threaded Fusion Device Recommended Infuse™ Bone Graft Kit(s)
Part #
890120 12x20 7510050 XX Small (0.7) 0.7
890125 12x25 7510100 X Small (1.4) 1.4
890140 14X20 7510100 X Small (1.4) 1.4
890143 14X23 7510100 X Small (1.4) 1.4
890146 14x26
Size (lead diameter, mm x
length, mm)
7510100+
7510050
7510100+
7510050
Single Inter Fix™ Device Fill
Part # Kit size
7510100+
7510050
X Small (1.4)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
Reconstituted rhBMP-2/ACS graft volume
(cc)
2.1
2.1
Reconstituted rhBMP-2/ACS graft
volume (cc)
2.1

Infuse™ Bone Graft/Inter Fix™ Threaded Fusion Device Combinations
Single Inter Fix™ Device Fill
Inter Fix™ Threaded Fusion Device Recommended Infuse™ Bone Graft Kit(s)
Part #
890149 14X29
890160 16X20
890163 16X23
Part # Size (lead diameter, mm x length, mm) Part # Kit size
9011221 12x20 7510050 XX Small (0.7) 0.7
9011225 12x25 7510100 X Small (1.4) 1.4
9011420 14X20 7510100 X Small (1.4) 1.4
9011423 14X23 7510100 X Small (1.4) 1.4
9011426 14x26
9011429 14X29
9011620 16X20
9011623 16X23
Size (lead diameter, mm x
length, mm)
Infuse™ Bone Graft/Inter Fix™ RP Threaded Fusion Device Combinations
Inter Fix™ Threaded Fusion Device Recommended Infuse™ Bone Graft Kit(s)
Part # Kit size
7510100+
7510050
7510100+
7510050
7510100+
7510050
Single Inter Fix™ RP Device Fill
7510100+
7510050
7510100+
7510050
7510100+
7510050
7510100+
7510050
X Small (1.4)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
Reconstituted rhBMP-2/ACS graft volume
Reconstituted rhBMP-2/ACS graft
volume (cc)
(cc)
2.1
2.1
2.1
2.1
2.1
2.1
2.1
Infuse™ Bone Graft/Perimeter™ Interbody Fusion Device Combinations
Perimeter™ Interbody Fusion Device Appropriate Infuse™ Bone Graft Kit
Footprint, Lordosis Part #
Medium, 8 deg 3492308 8mm 7510100 X Small (1.4) 1.4
3492310 10mm 7510100 X Small (1.4) 1.4
3492312 12mm
3492314 14mm 7510200 Small (2.8) 2.8
3492316 16mm 7510200 Small (2.8) 2.8
3492318 18mm
3492320 20mm
Large, 8 deg 3493308 8mm 7510100 X Small (1.4) 1.4
3493310 10mm
3493312 12mm 7510200 Small (2.8) 2.8
3493314 14mm 7510200 Small (2.8) 2.8
3493316 16mm
3493318 18mm
3493320 20mm
Large, 12 deg 3493412 12mm 7510200 Small (2.8) 2.8
Size
(height)
Part # Kit name (size in cc)
7510100+
7510050
7510200+
7510050
7510200+
7510050
7510100+
7510050
7510200+
7510050
7510200+
7510100
7510200+
7510100
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Reconstituted rhBMP-2/ACS graft volume
2.1
3.5
3.5
2.1
3.5
4.2
4.2

Infuse™ Bone Graft/Perimeter™ Interbody Fusion Device Combinations
Perimeter™ Interbody Fusion Device Appropriate Infuse™ Bone Graft Kit
Footprint, Lordosis Part #
3493414 14mm 7510200 Small (2.8) 2.8
3493416 16mm
3493418 18mm
3493420 20mm
XL, 8 deg
3494310 10mm
3494312 12mm
3494314 14mm 7510400 Medium (5.6) 5.6
3494316 16mm
3494318 18mm
3494320 20mm
Size
(height)
Part # Kit name (size in cc)
7510200+
7510050
7510200+
7510050
7510200+
7510100
7510200+
7510050
7510200+
7510100
7510400+
7510050
7510400+
7510100
7510600+
7510800
Small (2.8)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Medium (5.6)+
XX Small (0.7)
Medium (5.6)+
X Small (1.4)
Large (8.0) or
Large II (8.0)
Reconstituted rhBMP-2/ACS graft volume
3.5
3.5
4.2
3.5
4.2
6.3
7.0
8.0
Infuse™ Bone Graft/Clydesdale™ Spinal System Combinations
Clydesdale™ Spinal System Appropriate Infuse™ Bone Graft Kit
Lordosis, Width Part #
0 deg, 18mm 2969840 8 x 40mm 7510100 X Small (1.4) 1.4
2969845 8 x 45mm
2969850 8 x 50mm 7510200 Small (2.8) 2.8
2969855 8 x 55mm 7510200 Small (2.8) 2.8
2969040 10 x 40mm
2969045 10 x 45mm 7510200 Small (2.8) 2.1
2969050 10 x 50mm
2969055 10 x 55mm
2969240 12 x 40mm 7510200 Small (2.8) 2.8
2969245 12 x 45mm
2969250 12 x 50mm
2969255 12 x 55mm
2969440 14 x 40mm 7510200 Small (2.8) 2.8
2969445 14 x 45mm
2969450 14 x 50mm
2969455 14 x 55mm 7510400 Medium (5.6) 5.6
2969640 16 x 40mm
2969645 16 x 45mm
2969650 16 x 50mm 7510400 Medium (5.6) 5.6
Size
(height X length)
Part # Kit name (size in cc)
7510100+
7510050
7510100+
7510050
7510200+
7510050
7510200+
7510050
7510200+
7510050
7510200+
7510100
7510200+
7510100
7510200+
7510100
7510200+
7510100
7510200+
7510050
7510200+
7510100
X Small (1.4)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Reconstituted rhBMP-2/ACS graft vol-
ume
2.1
2.1
3.5
3.5
3.5
4.2
4.2
4.2
4.2
3.5
4.2

Infuse™ Bone Graft/Clydesdale™ Spinal System Combinations
Clydesdale™ Spinal System Appropriate Infuse™ Bone Graft Kit
Lordosis, Width Part #
2969655 16 x 55mm 7510400 Medium (5.6) 5.6
6 deg, 18mm 2968840 8 x 40mm 7510100 X Small (1.4) 1.4
2968845 8 x 45mm
2968850 8 x 50mm
2968855 8 x 55mm 7510200 Small (2.8) 2.8
2968860 8 x 60mm 7510200 Small (2.8) 2.8
2968040 10 x 40mm
2968045 10 x 45mm
2968050 10 x 50mm 7510200 Small (2.8) 2.8
2968055 10 x 55mm
2968060 10 x 60mm
2968240 12 x 40mm
2968245 12 x 45mm 7510200 Small (2.8) 2.8
2968250 12 x 50mm
2968255 12 x 55mm
2968260 12 x 60mm
2968440 14 x 40mm 7510200 Small (2.8) 2.8
2968445 14 x 45mm
2968450 14 x 50mm
2968455 14 x 55mm
2968460 14 x 60mm 7510400 Medium (5.6) 5.6
2968640 16 x 40mm
2968645 16 x 45mm
2968650 16 x 50mm
2968655 16 x 55mm 7510400 Medium (5.6) 5.6
2968660 16 x 60mm
6 deg, 22mm 2926040 8 x 40mm 7510100 X Small (1.4) 1.4
2926040 10 x 40mm
2926240 12 x 40mm
2926440 14 x 40mm 7510200 Small (2.8) 2.8
2926640 16 x 40mm
2926845 8 x 45mm
Size
(height X length)
Part # Kit name (size in cc)
7510100+
7510050
7510100+
7510050
7510100+
7510050
7510100+
7510050
7510200+
7510050
7510200+
7510050
7510100+
7510050
7510200+
7510050
7510200+
7510100
7510200+
7510100
7510200+
7510050
7510200+
7510100
7510200+
7510100
7510200+
7510050
7510200+
7510100
7510200+
7510100
7510400+
7510050
7510100+
7510050
7510100+
7510050
7510200+
7510050
7510100+
7510050
X Small (1.4)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Medium (5.6)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
Reconstituted rhBMP-2/ACS graft vol-
ume
2.1
2.1
2.1
2.1
3.5
3.5
2.1
3.5
4.2
4.2
3.5
4.2
4.2
3.5
4.2
4.2
6.3
2.1
2.1
3.5
2.1

Infuse™ Bone Graft/Clydesdale™ Spinal System Combinations
Clydesdale™ Spinal System Appropriate Infuse™ Bone Graft Kit
Lordosis, Width Part #
2926045 10 x 45mm
2926245 12 x 45mm 7510200 Small (2.8) 2.8
2926445 14 x 45mm
2926645 16 x 45mm
2926850 8 x 45mm
2926050 10 x 50mm 7510200 Small (2.8) 2.8
2926250 12 x 50mm
2926450 14 x 50mm
2926650 16 x 50mm
2926855 8 x 55mm 7510200 Small (2.8) 2.8
2926055 10 x 55mm
2926255 12 x 55mm
2926455 14 x 55mm
2926655 16 x 55mm 7510400 Medium (5.6) 5.6
2926860 8 x 60mm 7510200 Small (2.8) 2.8
2926060 10 x 60mm
2926260 12 x 60mm
2926460 14 x 60mm 7510400 Medium (5.6) 5.6
2926660 16 x 60mm
12 deg, 22mm 2922040 10 x 40mm 7510100 X Small (1.4) 1.4
2922240 12 x 40mm
2922440 14 x 40mm 7510200 Small (2.8) 2.8
2922640 16 x 40mm
2922045 10 x 45mm
2922245 12 x 45mm 7510200 Small (2.8) 2.8
2922445 14 x 45mm
2922645 16 x 45mm
2922050 10 x 50mm 7510200 Small (2.8) 2.8
2922250 12 x 50mm
2922450 14 x 50mm
2922650 16 x 50mm
2922055 10 x 55mm 7510200 Small (2.8) 2.8
Size
(height X length)
Part # Kit name (size in cc)
7510100+
7510050
7510200+
7510050
7510200+
7510100
7510100+
7510050
7510200+
7510050
7510200+
7510100
7510200+
7510100
7510200+
7510050
7510200+
7510100
7510200+
7510100
7510200+
7510100
7510200+
7510100
7510400+
7510050
7510100+
7510050
7510200+
7510050
7510100+
7510050
7510200+
7510050
7510200+
7510100
7510200+
7510050
7510200+
7510100
7510200+
7510100
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Medium (5.6)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Reconstituted rhBMP-2/ACS graft vol-
ume
2.1
3.5
4.2
2.1
3.5
4.2
4.2
3.5
4.2
4.2
4.2
4.2
6.3
2.1
3.5
2.1
3.5
4.2
3.5
4.2
4.2

Infuse™ Bone Graft/Clydesdale™ Spinal System Combinations
Clydesdale™ Spinal System Appropriate Infuse™ Bone Graft Kit
Lordosis, Width Part #
2922255 12 x 55mm
2922455 14 x 55mm
2922655 16 x 55mm 7510400 Medium (5.6) 5.6
2922060 10 x 60mm
2922260 12 x 60mm
2922460 14 x 60mm
2922660 16 x 60mm 7510400 Medium (5.6) 5.6
Infuse™ Bone Graft/Divergence-L™ Interbody Fusion Device Combinations
Divergence-L™ Interbody Fusion Device Appropriate Infuse™ Bone Graft Kit
Footprint, Lordosis
Small, 6 deg 2151110 10mm 7510100 X Small (1.4) 1.4
Medium, 6 deg 2151210 10mm 7510200 Small (2.8) 2.8
Large, 6 deg 2151310 10mm 7510200 +
Small, 12 deg 2152110 10mm 7510100 X Small (1.4) 1.4
Part # Size
2151112 12mm 7510100+
2151114 14mm 7510200 Small (2.8) 2.8
2151116 16mm 7510200 Small (2.8) 2.8
2151118 18mm 7510200+
2151120 20mm 7510200+
2151212 12mm 7510200+
2151214 14mm 7510200+
2151216 16mm 7510200+
2151218 18mm 7510400 Medium (5.6) 5.6
2151220 20mm 7510400 Medium (5.6) 5.6
2151312 12mm 7510200+
2151314 14mm 7510400 Medium (5.6) 5.6
2151316 16mm 7510400+
2151318 18mm 7510600 or
2151320 20mm 7510600 or
2152112 12mm 7510100 +
2152114 14mm 7510100 +
2152116 16mm 7510200 Small (2.8) 2.8
Size
(height X length)
(height)
Part # Kit name (size in cc)
7510200+
7510050
7510200+
7510100
7510200+
7510050
7510200+
7510100
7510200+
7510100
Part # Kit name (size in cc)
7510050
7510050
7510100
7510050
7510100
7510100
7510050
7510100
7510050
7510800
7510800
7510050
7510050
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Medium (5.6)+
XX Small (0.7)
Large (8.0) or
Large II (8.0)
Large (8.0) or
Large II (8.0)
X Small (1.4)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
Reconstituted rhBMP-2/ACS graft vol-
Reconstituted rhBMP-2/ACS graft vol-
ume
3.5
4.2
3.5
4.2
4.2
ume
2.1
3.5
4.2
3.5
4.2
4.2
3.5
4.2
6.3
8.0
8.0
2.1
2.1

Infuse™ Bone Graft/Divergence-L™ Interbody Fusion Device Combinations
Divergence-L™ Interbody Fusion Device Appropriate Infuse™ Bone Graft Kit
Footprint, Lordosis
Medium, 12 deg 2152210 10mm 7510200 Small (2.8) 2.8
Large, 12 deg 2152312 12mm 7510200+
Small, 18 deg 2153112 12mm 7510100 X Small (1.4) 1.4
Medium, 18 deg 2153214 14mm 7510200 Small (2.8) 2.8
Large, 18 deg 2153316 16mm 7510400 Medium (5.6) 5.6
Small, 24 deg 2154116 16mm 7510100 +
Medium, 24 deg 2154216 16mm 7510200 +
Large, 24 deg 2154318 18mm 7510400 Medium (5.6) 5.6
Part # Size
(height)
2152118 18mm 7510200 +
2152120 20mm 7510200 +
2152212 12mm 7510200 Small (2.8) 2.8
2152214 14mm 7510200 +
2152216 16mm 7510200+
2152218 18mm 7510400 Medium (5.6) 5.6
2152220 20mm 7510400 Medium (5.6) 5.6
2152314 14mm 7510200+
2152316 16mm 7510400 Medium (5.6) 5.6
2152318 18mm 7510400 Medium (5.6)+
2152320 20mm 7510600 or
2153114 14mm 7510100 +
2153116 16mm 7510200 Small (2.8) 2.8
2153118 18mm 7510200 Small (2.8) 2.8
2153120 20mm 7510200 +
2153216 16mm 7510200+
2153218 18mm 7510200+
2153220 20mm 7510400 Medium (5.6) 5.6
2153318 18mm 7510400+
2153320 20mm 7510400 +
2154118 18mm 7510200 Small (2.8) 2.8
2154120 20mm 7510200 +
2154218 18mm 7510200+
2154220 20mm 7510200+
2154320 20mm 7510400+
Part # Kit name (size in cc)
Small (2.8)+
7510050
7510050
7510050
7510100
7510100
7510100
7510800
7510050
7510050
7510100
7510100
7510050
7510100
7510050
7510050
7510050
7510100
7510100
7510050
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
X Small (1.4)
Large (8.0) or
Large II (8.0)
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Medium (5.6)+
XX Small (0.7)
Medium (5.6)+
X Small (1.4)
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Medium (5.6)+
XX Small (0.7)
Reconstituted rhBMP-2/ACS graft vol-
ume
3.5
3.5
3.5
4.2
4.2
4.2
7.0
8.0
2.1
3.5
4.2
4.2
6.3
7.0
2.1
3.5
3.5
4.2
4.2
6.3

Infuse™ Bone Graft/Pivox™ Oblique Lateral Spinal System Combinations
Pivox™ Spinal System Appropriate Infuse™ Bone Graft Kit
Lordosis, Width Part # Size
(height X length)
0 deg, 20mm 2110140 8 x 40mm 7510100 X Small (1.4) 1.4
2110145 8 x 45mm 7510100+
2110150 8 x 50mm 7510100+
2110155 8 x 55mm 7510200 Small (2.8) 2.8
2110160 8 x 60mm 7510200+
2110240 10 x 40mm 7510100 X Small (1.4) 1.4
2110245 10 x 45mm 7510100+
2110250 10 x 50mm 7510200 Small (2.8) 2.8
2110255 10 x 55mm 7510200+
2110260 10 x 60mm 7510200+
2110340 12 x 40mm 7510100+
2110345 12 x 45mm 7510200 Small (2.8) 2.8
2110350 12 x 50mm 7510200+
2110355 12 x 55mm 7510200+
2110360 12 x 60mm 7510400 Medium (5.6) 5.6
2110440 14 x 40mm 7510200 Small (2.8) 2.8
2110445 14 x 45mm 7510200+
2110450 14 x 50mm 7510200+
2110455 14 x 55mm 7510400 Medium (5.6) 5.6
2110460 14 x 60mm 7510400 Medium (5.6) 5.6
2110540 16 x 40mm 7510200 Small (2.8) 2.8
2110545 16 x 45mm 7510200+
2110550 16 x 50mm 7510200+
2110555 16 x 55mm 7510400 Medium (5.6) 5.6
2110560 16 x 60mm 7510400+
6 deg, 20mm 2111140 8 x 40mm 7510100 X Small (1.4) 1.4
2111145 8 x 45mm 7510100 X Small (1.4) 1.4
2111150 8 x 50mm 7510100+
2111155 8 x 55mm 7510200 Small (2.8) 2.8
2111160 8 x 60mm 7510200 Small (2.8) 2.8
2111240 10 x 40mm 7510100 X Small (1.4) 1.4
2111245 10 x 45mm 7510100+
2111250 10 x 50mm 7510200 Small (2.8) 2.8
2111255 10 x 55mm 7510200+
Part # Kit name (size in cc)
X Small (1.4)+
7510050
7510050
7510050
7510050
7510050
7510100
7510050
7510050
7510100
7510050
7510100
7510100
7510100
7510100
7510050
7510050
7510050
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Medium (5.6)+
X Small (1.4)
X Small (1.4)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Reconstituted rhBMP-2/ACS graft vol-
ume
2.1
2.1
3.5
2.1
3.5
4.2
2.1
3.5
4.2
3.5
4.2
4.2
4.2
7.0
2.1
2.1
3.5

Infuse™ Bone Graft/Pivox™ Oblique Lateral Spinal System Combinations
Pivox™ Spinal System Appropriate Infuse™ Bone Graft Kit
Lordosis, Width Part # Size
(height X length)
2111260 10 x 60mm 7510200+
2111340 12 x 40mm 7510100+
2111345 12 x 45mm 7510200 Small (2.8) 2.8
2111350 12 x 50mm 7510200+
2111355 12 x 55mm 7510200+
2111360 12 x 60mm 7510200+
2111440 14 x 40mm 7510100+
2111445 14 x 45mm 7510200+
2111450 14 x 50mm 7510200+
2111455 14 x 55mm 7510200+
2111460 14 x 60mm 7510400 Medium (5.6) 5.6
2111540 16 x 40mm 7510200 Small (2.8) 2.8
2111545 16 x 45mm 7510200+
2111550 16 x 50mm 7510200+
2111555 16 x 55mm 7510400 Medium (5.6) 5.6
2111560 16 x 60mm 7510400+
12 deg, 20mm 2112245 10 x 45mm 7510100+
2112250 10 x 50mm 7510200 Small (2.8) 2.8
2112255 10 x 55mm 7510200 Small (2.8) 2.8
2112260 10 x 60mm 7510200+
2112345 12 x 45mm 7510100+
2112350 12 x 50mm 7510200 Small (2.8) 2.8
2112355 12 x 55mm 7510200+
2112360 12 x 60mm 7510200+
2112445 14 x 45mm 7510200 Small (2.8) 2.8
2112450 14 x 50mm 7510200+
2112455 14 x 55mm 7510200+
2112460 14 x 60mm 7510400 Medium (5.6) 5.6
2112545 16 x 45mm 7510200+
2112550 16 x 50mm 7510200+
2112555 16 x 55mm 7510400 Medium (5.6) 5.6
2112560 16 x 60mm 7510400 Medium (5.6) 5.6
Part # Kit name (size in cc)
7510100
7510050
7510050
7510100
7510100
7510050
7510050
7510100
7510100
7510050
7510100
7510050
7510050
7510050
7510050
7510050
7510100
7510050
7510100
7510050
7510100
Small (2.8)+
X Small (1.4)
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Medium (5.6)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Reconstituted rhBMP-2/ACS graft vol-
ume
4.2
2.1
3.5
4.2
4.2
2.1
3.5
4.2
4.2
3.5
4.2
6.3
2.1
3.5
2.1
3.5
4.2
3.5
4.2
3.5
4.2
Infuse™ Bone Graft/Pivox™ Oblique Lateral Spinal System Combinations
Pivox™ Spinal System Appropriate Infuse™ Bone Graft Kit
Lordosis, Width Part # Size
(height X length)
2112645 18 x 45mm 7510200+
2112650 18 x 50mm 7510200+
2112655 18 x 55mm 7510400 Medium (5.6) 5.6
2112660 18 x 60mm 7510400+
18 deg, 20mm 2113345 12 x 45mm 7510100+
2113350 12 x 50mm 7510200 Small (2.8) 2.8
2113355 12 x 55mm 7510200+
2113360 12 x 60mm 7510200+
2113445 14 x 45mm 7510200 Small (2.8) 2.8
2113450 14 x 50mm 7510200+
2113455 14 x 55mm 7510200+
2113460 14 x 60mm 7510200+
2113545 16 x 45mm 7510200+
2113550 16 x 50mm 7510200+
2113555 16 x 55mm 7510200+
2113645 18 x 45mm 7510200+
2113650 18 x 50mm 7510200+
2113655 18 x 55mm 7510400 Medium (5.6) 5.6
6 deg, 27mm 2131245 10 x 45mm 7510200 Small (2.8) 2.8
2131250 10 x 50mm 7510200+
2131255 10 x 55mm 7510200+
2131345 12 x 45mm 7510200+
2131350 12 x 50mm 7510200+
2131355 12 x 55mm 7510400 Medium (5.6) 5.6
2131445 14 x 45mm 7510200+
2131450 14 x 50mm 7510200+
2131455 14 x 55mm 7510400 Medium (5.6) 5.6
2131545 16 x 45mm 7510200+
2131550 16 x 50mm 7510400 Medium (5.6) 5.6
2131555 16 x 55mm 7510400+
12 deg, 27mm 2132345 12 x 45mm 7510200 Small (2.8) 2.8
Part # Kit name (size in cc)
Small (2.8)+
7510100
7510100
7510100
7510050
7510050
7510100
7510050
7510100
7510100
7510050
7510100
7510100
7510050
7510100
7510050
7510100
7510050
7510100
7510100
7510100
7510100
7510100
X Small (1.4)
Small (2.8)+
X Small (1.4)
Medium (5.6)+
X Small (1.4)
X Small (1.4)+
XX Small (0.7)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Medium (5.6)+
X Small (1.4)
Reconstituted rhBMP-2/ACS graft vol-
ume
4.2
4.2
7.0
2.1
3.5
4.2
3.5
4.2
4.2
3.5
4.2
4.2
3.5
4.2
3.5
4.2
3.5
4.2
4.2
4.2
4.2
7.0

Infuse™ Bone Graft/Pivox™ Oblique Lateral Spinal System Combinations
Pivox™ Spinal System Appropriate Infuse™ Bone Graft Kit
Lordosis, Width Part # Size
(height X length)
2132350 12 x 50mm 7510200+
2132355 12 x 55mm 7510200+
2132445 14 x 45mm 7510200+
2132450 14 x 50mm 7510200+
2132455 14 x 55mm 7510400 Medium (5.6) 5.6
2132545 16 x 45mm 7510200+
2132550 16 x 50mm 7510400 Medium (5.6) 5.6
2132555 16 x 55mm 7510400+
2132645 18 x 45mm 7510200+
2132650 18 x 50mm 7510400+
2132655 18 x 55mm 7510400+
18 deg, 27mm 2133445 14 x 45mm 7510200 Small (2.8) 2.8
2133450 14 x 50mm 7510200+
2133455 14 x 55mm 7510200+
2133545 16 x 45mm 7510200+
2133550 16 x 50mm 7510200+
2133555 16 x 55mm 7510400 Medium (5.6) 5.6
2133645 18 x 45mm 7510200+
2133650 18 x 50mm 7510400 Medium (5.6) 5.6
2133655 18 x 55mm 7510400+
Part # Kit name (size in cc)
Small (2.8)+
7510050
7510100
7510050
7510100
7510100
7510050
7510100
7510050
7510100
7510100
7510100
7510050
7510100
7510100
7510100
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Medium (5.6)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Medium (5.6)+
XX Small (0.7)
Medium (5.6)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Small (2.8)+
XX Small (0.7)
Small (2.8)+
X Small (1.4)
Small (2.8)+
X Small (1.4)
Medium (5.6)+
X Small (1.4)
Reconstituted rhBMP-2/ACS graft vol-
ume
3.5
4.2
3.5
4.2
4.2
6.3
4.2
6.3
7.0
4.2
4.2
3.5
4.2
4.2
7.0
No warranties, express or implied, are made. Implied warranties of merchantability and fitness for a particular purpose or use
are specifically excluded.
INDICATIONS
The Infuse™ Bone Graft/Medtronic Interbody Fusion Device is indicated for spinal fusion procedures in skeletally mature
patients with degenerative disc disease (DDD) at one level from L2-S1. DDD is defined as discogenic back pain with
degeneration of the disc confirmed by patient history and radiographic studies. These DDD patients may also have up to Grade
I spondylolisthesis or Grade 1 retrolisthesis at the involved level. Patients receiving the Infuse™ Bone Graft/Medtronic Interbody
Fusion Device should have had at least six months of nonoperative treatment prior to treatment with the Infuse™ Bone Graft/
Medtronic Interbody Fusion Device.
The following interbody devices and surgical approaches may be used with Infuse™ Bone Graft:
▪ The LT-Cage™ Lumbar Tapered Fusion Device, implanted via an anterior open or an anterior laparoscopic approach at a
single level.
▪ The Inter Fix™ or Inter Fix™ RP Threaded Fusion Device, implanted via an anterior open approach at a single level.
▪ Certain sizes of the Perimeter™ Interbody Fusion Device implanted via a retroperitoneal anterior lumbar interbody fusion
(ALIF) at a single level from L2-S1or an oblique lateral interbody fusion (OLIF) approach at a single level from L5-S1.
▪ Certain sizes of the Clydesdale™ Spinal System, implanted via an OLIF approach at a single level from L
2-L5
.
▪ Certain sizes of the Divergence-L™ Anterior/Oblique Lumbar Fusion System implanted via an ALIF approach at a single
level from L2-S1or an OLIF approach at a single level from L5-S1.

▪ Certain sizes of the Pivox™ Oblique Lateral Spinal System implanted via an OLIF approach at a single-level from L
2-L5
CONTRAINDICATIONS
▪ The Infuse™ Bone Graft/Medtronic Interbody Fusion Device is contraindicated for patients with a known hypersensitivity to
recombinant human Bone Morphogenetic Protein-2, bovine Type I collagen, or to other components of the formulation.
▪ The Infuse™ Bone Graft/Medtronic Interbody Fusion Device should not be used in the vicinity of a resected or extant tumor,
in patients with any active malignancy, or patients undergoing treatment for a malignancy.
▪ Infuse™ Bone Graft/Medtronic Interbody Fusion Device should not be used in patients who are skeletally immature (<18
years of age or no radiographic evidence of epiphyseal closure).
▪ The Infuse™ Bone Graft/Medtronic Interbody Fusion Device should not be used in pregnant women. The potential effects of
rhBMP-2 on the human fetus have not been evaluated.
▪ The Infuse™ Bone Graft/Medtronic Interbody Fusion Device should not be implanted in patients with an active infection at
the operative site or with an allergy to titanium, titanium alloy, or polyetheretherketone.
WARNINGS
▪ In an experimental rabbit study, rhBMP-2 has been shown to elicit antibodies that are capable of crossing the placenta. Re-
duced ossification of the frontal and parietal bones of the skull was noted infrequently (<3%) in fetuses of rabbit dams immunized to rhBMP-2; however, there was no effect noted in limb bud development. There are no adequate and wellcontrolled studies in human pregnant women. Women of child bearing potential should be warned by their surgeon of
potential risk to a fetus and informed of other possible orthopedic treatments.
▪ Women of childbearing potential should be advised that antibody formation to rhBMP-2 or its influence on fetal development
has not been completely assessed. In the clinical trial supporting the safety and effectiveness of the Infuse™ Bone
Graft/LT-Cage™ Lumbar Tapered Fusion Device, 2/277 (0.7%) patients treated with Infuse™ Bone Graft component and
1/127 (0.8%) patients treated with autograft bone developed antibodies to rhBMP-2. The effect of maternal antibodies to
rhBMP-2, as might be present for several months following device implantation, on the unborn fetus is unknown. Additionally, it is unknown whether fetal expression of BMP-2 could re-expose mothers who were previously antibody positive. Theoretically, re-exposure may elicit a more powerful immune response to BMP-2 with possible adverse consequences for the
fetus. However, pregnancy did not lead to an increase in antibodies in the rabbit study. Studies in genetically altered mice
indicate that BMP-2 is critical to fetal development and that a lack of BMP-2 activity may cause neonatal death or birth defects. It is not known if anti-BMP-2 antibodies may affect fetal development or the extent to which these antibodies may
reduce BMP-2 activity.
▪ Infuse™ Bone Graft should not be used immediately prior to or during pregnancy. Women of childbearing potential should
be advised not to become pregnant for one year following treatment with the Infuse™ Bone Graft/Medtronic Interbody Fusion Device.
▪ The safety and effectiveness of the Infuse™ Bone Graft/Medtronic Interbody Fusion Device in nursing mothers has not
been established. It is not known if BMP-2 is excreted in human milk.
.
General
▪ The Infuse™ Bone Graft/Medtronic Interbody Fusion Device should not be used in patients suspected of having a
malignancy at the site of application.
▪ The safety and effectiveness of the use of the Infuse™ Bone Graft component with other spinal implants, implanted at
locations other than the lower lumbar spine, or used in surgical techniques other than anterior open (LT-Cage™, Inter Fix™,
Inter Fix™ RP, Perimeter™, and Divergence-L™ devices), anterior laparoscopic (LT-Cage™ Device), or oblique lateral
(Perimeter™, Clydesdale™, Divergence-L™, and Pivox™ devices) approaches have not been established.
▪ The implantation of the Infuse™ Bone Graft/LT-Cage™ Lumbar Tapered Fusion Device using an anterior laparoscopic
surgical approach is associated with a higher incidence of retrograde ejaculation (10.5%, 6/57 male patients) when
compared to implantation using an anterior open surgical approach (6.4%, 5/78 male patients). Both of these rates are
greater than that for a control group implanted using an open anterior approach who did not receive Infuse™ Bone Graft
(1.5%, 1/68 male patients). In the randomized study of the anterior open surgical approach, retrograde ejaculation occurred
in the Infuse™ Bone Graft group in 17.6% (3/17) of the male patients who underwent the surgery with a transperitoneal
approach, as compared to 3.2% (2/ 61) of the males with a retroperitoneal approach. In the control group, the retrograde
ejaculation rate was 7.6% (1/13) in the males with a transperitoneal approach, as compared to 0% (0/55) in the males with
a retroperitoneal approach. With the two treatment groups pooled, retrograde ejaculation occurred in 13.3% (4/30) of the
males who underwent a transperitoneal approach and in 1.8% (2/116) of the males who underwent a retroperitoneal
approach. This difference is statistically significant (p=0.017, Fisher exact test). Male patients should be informed of this
potential risk prior to considering the use of Infuse™ Bone Graft.
▪ The safety and effectiveness of the use of Infuse™ Bone Graft implanted in the cervical spine has not been established.
This product is only approved for use in the lumbar spine as indicated above.
▪ When anterior cervical spinal fusions were performed using the Infuse™ Bone Graft component, some cases of edema
have been reported within the first postoperative week. In some of these cases, this swelling has been severe enough to
produce airway compromise, sometimes requiring emergency surgery.

▪ In a clinical trial comparing single-level anterior cervical fusion using Infuse™ Bone Graft to a control that did not use
Infuse™ Bone Graft, 16.4% of patients treated with Infuse™ Bone Graft reported dysphagia, compared to 7.3% of
control patients. Most of the dysphagia events occurred within the first four weeks after surgery, and most of these
events were classified as non-serious (e.g. non-life-threatening events not requiring hospitalization). While dysphagia
may occur following anterior cervical procedures, it may occur more frequently or to a greater extent in the presence of
Infuse™ Bone Graft.
▪ When anterior cervical fusions were performed using Infuse™ Bone Graft, the radiographic appearance of anterior
heterotopic ossification (HO) was noted in some patients, most commonly observed anterior and superior to the treated
level. In some of the cases of severe HO, adjacent-level fusion and reduced motion were also noted. HO may occur
more frequently or to a greater extent with the use of Infuse™ Bone Graft.
Bone Formation
▪ Posterior bone formation outside of the disc space was observed in some patients when DDD was treated by a posterior
lumbar interbody fusion procedure. Although it was not clearly associated with key clinical outcome measures (e.g. leg pain)
in most of the cases, bone formation outside of the disc space is not desirable and may potentially lead to nerve
compression, requiring surgical intervention.
▪ Inappropriate use of the product, such as preparing it differently than prescribed, compressing the rhBMP-2/ACS implant
more than necessary, or overfilling the volume intended for new bone formation, may change the concentration of the
rhBMP-2, which may inhibit the ability of the rhBMP-2/ACS to convert to bone and/or cause complications. Such use of the
rhBMP-2/ACS implant may result in radiographic evidence of resorption. These findings may be asymptomatic or
symptomatic. A sheep model developed to test the hypothesis that volume overfilling and/or hyperconcentration of the
rhBMP-2 solution results in radiographic evidence of bone resorption has preliminarily been evaluated and appears to be
supportive of the hypothesized mechanism.
▪ Placement of rhBMP-2/ACS can cause initial resorption of trabecular bone that may be transient.
▪ Device migration has been reported with use of rhBMP-2/ACS in spinal fusion surgery. Device migration has been reported
in the presence and absence of bone resorption.
▪ Nerve compression associated with heterotopic bone formation has been reported in patients undergoing spine surgery with
rhBMP-2/ACS. Surgical intervention may be required to address the symptoms.
Fluid Collection/Edema
▪ The formation of fluid collections (sometimes encapsulated) in some cases resulted in nerve compression and pain, which
may require clinical intervention (aspiration and/or surgical removal) if symptoms persist. Many of these reports have
occurred when rhBMP-2/ACS was used in conjunction with unapproved approaches/devices or in a manner inconsistent
with the instructions for use.
▪ While there is currently anecdotal and literature evidence to suggest that volume overfilling and/or hyperconcentration of the
rhBMP-2 solution may lead to fluid formation and/or edema, animal models for scientifically evaluating these events do not
presently exist.
PRECAUTIONS
Physician note: although the physician is the learned intermediary between the company and the patient, the important
medical information given in this document should be conveyed to the patient.
For US audiences only
General
▪ The safety and effectiveness of repeat applications of the Infuse™ Bone Graft component has not been established.
▪ The Infuse™ Bone Graft/Medtronic Interbody Fusion Device should only be used by surgeons who are experienced in
spinal fusion procedures and have undergone adequate training with this device for anterior laparoscopic, anterior open,
and/or oblique lateral procedures.
▪ Two Medtronic Titanium Threaded Interbody Fusion Device components (i.e. LT-Cage™ Lumbar Tapered Fusion Device,
Inter Fix™ Threaded Fusion Device, or Inter Fix™ RP Threaded Fusion Device) should be implanted side by side at the
surgical level whenever possible. Only one PEEK Perimeter™, Clydesdale™, Divergence-L™, or Pivox™ device may be
implanted at the surgical level.
▪ Unless marked sterile and clearly labeled as such in an unopened sterile package provided by the company, any Medtronic
Interbody Fusion Devices and/or instruments used in surgery must be sterilized by the hospital prior to use according to the
sterilization instructions provided in the product-specific package insert.
▪ When using this device at spinal levels between L
implant placement must be considered.
▪ The formation of exuberant or heterotopic bone growth at the upper lumbar levels (L
certain neurovascular structures (e.g. the aorta and sympathetic nerve chain).
▪ The safety and effectiveness of the device at spinal levels L
established.
and L4, the potential impact of anatomical structures (e.g. the aorta) on
2
- L4) may have a deleterious impact on
2
- L4 or in patients with up to Grade 1 retrolisthesis has not been
2
▪ The Infuse™ Bone Graft/Medtronic Interbody Fusion Device is intended for single use only. Discard unused product and
use a new device for subsequent applications.

▪ Prior to use, inspect the packaging, vials, and stoppers for visible damage. If damage is visible, do not use the product.
Retain the packaging and vials and contact a Medtronic representative.
▪ Do not use after the printed expiration date on the label.
Hepatic and Renal Impairment
▪ The safety and effectiveness of the Infuse™ Bone Graft/Medtronic Interbody Fusion Device in patients with hepatic or renal
impairment has not been established. Pharmacokinetic studies of rhBMP-2 indicate that the renal and hepatic systems are
involved with its clearance.
Geriatrics
▪ Clinical studies of the Infuse™ Bone Graft/LT-Cage™ Lumbar Tapered Fusion Device did not include sufficient numbers of
patients 65 years and older to determine whether they respond differently from younger subjects.
Bone Formation
▪ The safety and effectiveness of the Infuse™ Bone Graft/Medtronic Interbody Fusion Device has not been demonstrated in
patients with metabolic bone diseases.
▪ The potential for heterotopic or undesirable exuberant bone formation exists.
Antibody Formation/Allergic Reactions
▪ The safety and effectiveness of the Infuse™ Bone Graft/Medtronic Interbody Fusion Device has not been demonstrated in
patients with autoimmune disease.
▪ The safety and effectiveness of the Infuse™ Bone Graft/Medtronic Interbody Fusion Device has not been demonstrated in
patients with immunosuppressive disease or suppressed immune systems resulting from radiation therapy, chemotherapy,
steroid therapy, or other treatments.
Immunogenicity
▪ As with all therapeutic proteins, there is a potential for immune responses to be generated to the Infuse™ Bone Graft
component. The immune response to the Infuse™ Bone Graft components was evaluated in 349 investigational patients
and 183 control patients receiving lumbar interbody fusions.
▪ Anti-rhBMP-2 antibodies: 2/349 (0.6%) patients receiving the Infuse™ Bone Graft component developed antibodies vs.
1/183 (0.5%) in the control group.
▪ Anti-bovine Type I collagen antibodies: 18.1% of patients receiving the Infuse™ Bone Graft component developed
antibodies to bovine Type I collagen vs. 14.2% of control patients. No patients in either group developed anti-human
Type I collagen antibodies.
▪ The presence of antibodies to rhBMP-2 was not associated with immune mediated adverse events such as allergic
reactions. The neutralizing capacity of antibodies to rhBMP-2 is not known.
▪ The incidence of antibody detection is highly dependent on the sensitivity and specificity of the assay. Additionally, the
incidence of antibody detection may be influenced by several factors, including sample handling, concomitant medications,
and underlying disease. For these reasons, comparison of the incidence of antibodies to the Infuse™ Bone Graft
component with the incidence of antibodies to other products may be misleading.
ADVERSE EVENTS
The Infuse™ Bone Graft/LT-Cage™ Lumbar Tapered Fusion Device was implanted in 288 investigational patients and
compared to 139 control patients who received the LT-Cage™ Lumbar Tapered Fusion Device filled with iliac crest autograft.
The investigational patients were implanted with the device via either an open anterior surgical approach or a laparoscopic
anterior surgical approach. The control patients were implanted via the open anterior surgical approach only.
Adverse event rates presented are based on the number of patients having at least one occurrence for a particular adverse
event divided by the total number of patients in that treatment group. Because no control subjects were evaluated at the 48- and
72-month time points, the reported events at these time points are only from the investigational subjects.
Surgery Post-op
Complication
Anatomical/
technical diffi-
culty
Back and/or
leg pain
Cancer 0 0 0 0 0 0 0 1 0 0 1 0 1 0
Cardio/vascu-
lar
Death 0 0 0 0 0 0 0 0 0 1 0 0 0 0
Dural injury 0 0 0 0 0 0 0 1 0 0 0 0 0 0
Gastrointesti-
nal
Inv
11 3 0 0 0 0 0 0 0 0 0 0 0 0
0 0 12 4 11 5 12 5 15 4 20 7 8 12
1 0 6 5 5 2 1 3 2 1 4 2 1 1
1 0 40 22 2 0 5 1 7 1 10 3 7 5
Ctrl
(1day-
<4wks)
Inv
Infuse™ Bone Graft/LT-Cage™ Device data combined from all clinical trial experience with the device)
Ctrl
6wks
(≥4wks-
<9wks)
Inv
Ctrl
3mo
(≥9wks-
<5mo)
Inv
ADVERSE EVENTS (AEs)
6mo
(≥5mo-
<9mo)
Inv
Ctrl
Ctrl
12mo
(≥9mo-
<19mo)
Inv
Ctrl
24mo
(≥19mo-
<30mo)
Inv
# of Patients Reporting & Total
AEs (Through 24-mo Report-
ing Window)
Inv #
(% of 288)
Ctrl
Total Events
11(3.8)
11
70(24.3)
78
2(0.7)
2
17(5.9)
20
0(0.0)
0
0(0.0)
0
56(19.4)
72
Total Events
Ctrl #
(% of 139)
3(2.2)
3
33(23.7)
37
1(0.7)
1
12(8.6)
14
1(0.7)
1
1(0.7)
1
27(19.4)
32
48mo
(≥30mo-
<60mo)
Total #
(% of 134)
Total Events
0(0.0)
0
23(17.2)2418(12.9)
4(3.0)
4
7(5.2)
7
2(1.5)
2
0(0.0)
0
14(10.4)
17
(≥60mo-
(% of 140)
Total Events
72mo
84mo)
Total #
0(0.0)
0
21
1(0.7)
1
4(2.9)
4
0(0.0)
0
1(0.7)
1
6(4.3)
8

Surgery Post-op
Complication
Graft site rela-
ted
Implant dis-
placement/
loosening
Infection 0 0 19 9 8 4 5 1 5 1 3 0 0 2
Malpositioned
implant
Neurological 0 0 8 5 7 3 5 2 6 2 13 4 6 8
Non-union* 0 0 0 0 0 0 0 0 1 2 4 0 1 1
Non-union** 0 0 0 1 0 1 2 0 3 4 4 6 1 1
Other 5 6 18 11 9 2 3 4 11 4 15 8 20 8
Other pain 0 0 3 1 2 1 4 2 6 1 10 8 11 3
Respiratory 0 0 3 2 1 0 0 0 1 0 0 1 0 1
Retrograde
ejaculation
Spinal event 0 0 1 2 1 0 6 2 10 4 10 8 9 2
Subsidence 0 0 3 2 2 0 1 0 1 0 0 0 0 0
Trauma 0 0 4 5 5 3 11 7 14 5 28 11 20 8
Urogenital 0 0 24 5 3 0 2 3 6 3 3 1 7 2
Vascular
intra-op
Vertebral frac-
ture
Any adverse
event
Inv
0 0 0 8 0 0 0 0 0 0 0 0 0 0
0 0 1 1 3 0 1 0 0 0 0 0 0 0
5 0 0 0 0 0 0 0 0 0 0 0 0 0
0 0 5 1 4 0 1 0 0 0 2 0 0 0
15 5 0 0 0 0 0 0 0 0 0 0 0 0
0 0 1 0 0 0 0 0 0 0 0 0 0 0
Ctrl
(1day-
<4wks)
Inv
Infuse™ Bone Graft/LT-Cage™ Device data combined from all clinical trial experience with the device)
Ctrl
6wks
(≥4wks-
<9wks)
Inv
Ctrl
3mo
(≥9wks-
<5mo)
Inv
ADVERSE EVENTS (AEs)
6mo
(≥5mo-
<9mo)
Inv
Ctrl
Ctrl
12mo
(≥9mo-
<19mo)
Inv
Ctrl
24mo
(≥19mo-
<30mo)
Inv
# of Patients Reporting & Total
AEs (Through 24-mo Report-
ing Window)
Inv #
(% of 288)
Ctrl
Total Events
0(0.0)
0
5(1.7)
5
36(12.5)
40
5(1.7)
5
39(13.5)
45
6(2.1)
6
10(3.5)
10
62(21.5)
81
31(10.8)
36
5(1.7)
5
11(7.9)1
12
30(10.4)
37
7(2.4)
7
68(23.6)
82
41(14.2)
45
14(4.9)
15
1(0.3)
1
228(79.2) 117(84.2) 84(62.7) 64(45.7)
Ctrl #
(% of 139)
Total Events
8(5.8)
8
1(0.7)
1
16(11.5)
17
0(0.0)
0
23(16.5)
24
3(2.2)
3
13(9.4)
13
37(26.6)
43
13(9.4)
16
4(2.9)
4
1(1.4)2
1
17(12.2)
18
2(1.4)
2
34(24.5)
39
13(9.4)
14
5(3.6)
5
0(0.0)
0
48mo
(≥30mo-
<60mo)
Total #
(% of 134)
Total Events
0(0.0)
0
0(0.0)
0
4(3.0)
4
0(0.0)
0
12(9.0)
12
0(0.0)
0
0(0.0)
0
22(16.4)2917(12.1)
15(11.2)2011(7.9)
1(0.7)
1
0(0.0)
0
9(6.7)
9
0(0.0)
0
21(15.7)2320(14.3)
2(1.5)
2
1(0.7)
1
0(0.0)
0
72mo
(≥60mo-
84mo)
Total #
(% of 140)
Total Events
0(0.0)
0
0(0.0)
0
3(2.1)
3
0(0.0)
0
5(3.6)
5
0(0.0)
0
0(0.0)
0
18
12
1(0.7)
1
0(0.0)
0
8(5.7)
8
0(0.0)
0
22
3(2.1)
3
0(0.0)
0
0(0.0)
0
*Non-union adverse events that have not resulted in second surgery.
**Non-union adverse events that have resulted in a second surgery.
1
Percent of 140 males.
2
Percent of 70 males.
The reported rates of several adverse events were high but similar in both the investigational and control groups. These events
included back and leg pain, neurological events, gastrointestinal events, spinal events, cardiovascular events, and infection.
Some of the reported adverse events required surgical interventions subsequent to the initial surgery. The number of subjects
requiring a second surgical intervention was 10.4% (30/288) in the investigational groups and 13.7% (19/139) in the control
group. The majority of supplemental fixations were due to painful non-union.
Through the 24-month adverse event reporting window, urogenital events occurred with greater frequency in the investigational
groups (14.2%) compared to the control group (9.4%). Retrograde ejaculation rates were greater in the investigational groups
(11 subjects) compared to the control group (1 subject), with the majority of events occurring in the early postoperative period.
The incidence of adverse events that were considered device related, including implant displacement/loosening, implant
malposition, and subsidence, was greater in the investigational groups compared to the control group. The rates of these events
were low, however, and may be partially attributed to a learning curve associated with the laparoscopic surgical approach. The
rate of non-union requiring secondary surgery in the investigational groups was comparable to that of the control group. One
death was reported – a control group subject with cardiovascular disease.
Potential Adverse Events
The following is a list of potential adverse events that may occur with spinal fusion surgery with the Infuse™ Bone Graft/
Medtronic Interbody Fusion Device. Some of these adverse events may have been previously reported in the adverse events
table or have been reported to the manufacturer:
▪ Allergic reaction.
▪ Anaphylactic reaction.
▪ Bone fracture.
▪ Bone resorption, which may be transient.
▪ Bowel or bladder problems.
▪ Cessation of any potential growth of the operated portion of the spine. Loss of spinal mobility or function.
▪ Change in mental status.

▪ Damage to blood vessels and cardiovascular system compromise.
▪ Damage to internal organs and connective tissue.
▪ Death.
▪ Development of respiratory problems.
▪ Disassembly, bending, breakage, loosening, and/or migration of components.
▪ Dural tears.
▪ Elevated erythrocyte sedimentation rate.
▪ Encapsulated fluid collection.
▪ Erythematous tissue.
▪ Fetal development complications.
▪ Foreign body (allergic) reaction.
▪ Gastrointestinal complications.
▪ Hematoma.
▪ Heterotopic and/or exuberant bone formation.
▪ Incisional complications.
▪ Infection.
▪ Inflammation.
▪ Insufflation complications.
▪ Itching.
▪ Localized edema (swelling).
▪ Neurological system compromise.
▪ Non-union (or pseudarthrosis), delayed union, mal-union.
▪ Pain.
▪ Postoperative change in spinal curvature, loss of correction, height, and/or reduction.
▪ Retrograde ejaculation.
▪ Scar formation.
▪ Seroma.
▪ Tissue or nerve damage.
Note: additional surgery may be necessary to correct some of these potential adverse events.
CLINICAL RESULTS
Clinical data to support the safety and effectiveness of the Infuse™ Bone Graft/LT-Cage™ Lumbar Tapered Fusion Device were
collected as part of a prospective, multi-center pivotal study that consisted of randomized and non-randomized arms. The
randomized arm contained two groups, one investigational and one control. The control group was implanted with the LTCage™ Lumbar Tapered Fusion Device filled with iliac crest autograft bone, while the investigational group was implanted with
the Infuse™ Bone Graft/LT-Cage™ Lumbar Tapered Fusion Device. In both cases, the surgical approach was an open anterior
approach. The non-randomized arm contained only an investigational group, where subjects were implanted with the Infuse™
Bone Graft/LT-Cage™ Lumbar Tapered Fusion Device through a laparoscopic anterior approach. The control group from the
randomized arm was used as the control for the non-randomized arm.
Neither the investigators nor the subjects were blinded to the treatment. Subject blinding was not possible due to the second
surgical site resulting from the need to collect the iliac crest grafts. The potential for investigator bias in the clinical outcome
parameters was reduced by having the subjects rate their outcome using objective self-assessments. The radiographic outcome
parameters were performed by independent radiologists who were blinded to treatment. These were the only radiographic
evaluations used for determining radiographic success.
The indication studied was DDD accompanied by back pain with or without leg pain at a single level between L4 and S
confirmed by history and radiographic studies.
1
Clinical and Radiographic Effectiveness Parameters
Patients were evaluated preoperatively (within 6 months of surgery), intraoperatively, and postoperatively at 6 weeks, 3, 6, 12,
and 24 months and biennially thereafter until the last subject enrolled in the study had been seen for their 24-month evaluation.
Complications and adverse events, device-related or not, were evaluated over the course of the clinical trial. At each evaluation
time point, the primary and secondary clinical and radiographic outcome parameters were evaluated. Success was determined
from data collected during the initial 24 months of follow-up. Antibodies to rhBMP-2 and bovine Type I collagen were assessed
preoperatively and at 3 months postoperatively. Antibodies to human Type I collagen were assessed if the antibody response to
bovine Type I collagen was positive.
Primary and secondary clinical and radiographic effectiveness outcome parameters were evaluated for all treated subjects at all
follow-up evaluation time points identified above. The primary clinical parameters assessed were of pain, function, and
neurological status. The secondary clinical outcome parameters assessed were general health status, back and leg pain, donor
site pain (control subjects only), patient satisfaction, and patient global perceived effect of the treatment. The primary
radiographic outcome parameter consisted of evaluations of fusion, while the secondary radiographic assessment was disc
height.
Fusion was evaluated at 6, 12, and 24 months post-op using plain radiographs (AP, lateral, and flexion/extension films) and high
resolution thin-slice CT scans (1mm slices with 1mm index on axial, sagittal, and coronal reconstructions). Fusion was defined

as the presence of bridging bone connecting the inferior and superior vertebral bodies; a lack of motion on flexion/extension (≤
3mm of translation and < 5° of angulation); and no evidence of radiolucencies over more than 50% of either implant. Fusion
success was defined as the presence of all of these parameters plus the lack of a second surgical intervention resulting from a
non-union. All assessments were made from the plain films except for the assessment of bridging bone, which was made using
the CT scans only if bridging bone could not be visualized on the plain film.
Pain and function were measured using the Oswestry Low Back Pain Disability Questionnaire. Success was defined as a 15point improvement in the Oswestry score from the pre-op baseline score.
Neurological status consisted of measurements of four parameters – motor, sensory, reflexes, and straight leg raise (SLR).
Neurological status success was defined as maintenance or improvement of the pre-op baseline score for each parameter.
Overall neurological status success required that each individual parameter be a success for that subject to be counted as a
success.
Patient Demographics and Accountability
A total of 143 open approach investigational and 136 control patients were enrolled in the randomized arm of the study and
received the device. A total of 134 subjects were enrolled in the non-randomized arm of the study and received the device. For
the majority of the demographic parameters, there were no differences in pre-op demographics across the three populations.
Surgical Results and Hospitalization
Surgical and Hospitalization Information
Investigational Open Surgical
Approach
Mean operative time (hrs) 1.6* 2.0 1.9
Mean EBL (ml) 109.8* 153.1 146.1
Hospitalization (days) 3.1 3.3 1.2*
*Statistically different from control
Control Open Surgical Ap-
proach
Investigational Laparoscopic
Surgical Approach
Clinical and Radiographic Effectiveness Evaluation
Individual subject success was defined as success in each of the primary clinical and radiographic outcome parameters.
Success for these parameters included:
1. the presence of radiographic fusion;
2. an improvement of at least 15 points from the baseline Oswestry score;
3. maintenance or improvement in neurological status;
4. the presence of no serious adverse event classified as implant-associated or implant/surgical procedure-associated; and
5. no additional surgical procedure classified as “Failure.”
Study success was expressed as the number of individual subjects categorized as a success divided by the total number of
subjects evaluated. The table below describes the success rates for the individual primary outcome parameters and overall
success. All success rates were based on the data from the 24-month follow-up evaluation, and posterior probabilities of
success were calculated using Bayesian statistical methods.
Posterior Probabilities of Success at 24 Months
Primary Outcome
Variable
Fusion
Oswestry
Neurologic
Overall success
Investigational Open Surgical
Approach
Posterior mean
(95% HPD credible interval)
92.8%
(88.5%, 96.9%)
71.0%
(63.4%, 78.7%)
81.0%
(74.5%, 87.9%)
57.1%
(49.2%, 65.7%)
Control Open Surgical Ap-
proach
Posterior mean
(95% HPD credible interval)
88.1%
(82.6%, 99.3%)
70.9%
(63.1%, 79.1%)
81.7%
(74.9%, 88.7%)
56.7%
(48.3%, 65.0%)
Investigational Laparoscopic
Surgical Approach
Posterior mean
(95% HPD credible interval)
93.0%
(87.9%, 97.5%)
83.0%
(75.6%, 90.5%)
89.0%
(83.1%, 94.8%)
68.0%
(59.3%, 76.5%)
The probability (also called the posterior probability) that the 24-month overall success rate for the investigational groups was
equivalent to the 24-month success rate for the control group was 99.4% for the open surgical approach investigational group
and almost 100% for the laparoscopic surgical approach investigational group.
For a future patient receiving the Infuse™ Bone Graft/LT-Cage™ Lumbar Tapered Fusion Device via the open anterior surgical
approach, the chance (the predictive probability) of overall success at 24 months would be 57.1% for the open surgical
approach. Given the results of the trial, there is a 95% probability that the chance of success ranges from 49.2% to 65.7%. For a
future patient receiving the Infuse™ Bone Graft/LT-Cage™ Lumbar Tapered Fusion Device via the anterior laparoscopic
surgical approach, the chance of overall success at 24 months would be 68.0%. Given the results of the trial, there is a 95%
 Loading...
Loading...