Page 1
PRESTIGE™ CERVICAL DISC
Implant package contents (superior and inferior disc
components, bone screws, lock screws) provided sterile.
Instrument set contents provided non-sterile.
2017-02-15
0381252E Rev. C
IMPORTANT INFORMATION ON THE PRESTIGE™ CERVICAL DISC
DESCRIPTION
The PRESTIGE™ Cervical Disc is a two-piece articulating metal-on-metal device that is inserted into the intervertebral disc
space at a single cervical level using an anterior approach. The device is manufactured from wrought type 316 stainless steel
(ASTM F-138) and consists of two metal plates which function via a ball and trough mechanism. The superior component of the
implant contains the ball portion of the mechanism, and the inferior component incorporates the trough portion. The flat portion
of each component, which contacts the vertebral endplate, is roughened through a grit blasting process.
Each component is affixed to the vertebral body by two bone screws through an anterior flange. The bone screws are held in
place by a lock screw mechanism. In the implanted disc, the bone screws are divergent in the cephalic/caudal direction and
convergent in the medial/lateral direction.
The device assembly was designed to allow the following motions ex-vivo: a minimum of 10° motion off the neutral position in
flexion/extension and lateral bending, unconstrained axial rotation, and 2 mm of anterior/posterior translation.
The available components are shown in the table below.
Table 1: PRESTIGE™ Cervical Disc Device Configurations
Catalog Number Component Description
6961260 6 mm x 12 mm Disc Assembly
6961460 6 mm x 14 mm Disc Assembly
6961660 6 mm x 16 mm Disc Assembly
6961270 7 mm x 12 mm Disc Assembly
6961470 7 mm x 14 mm Disc Assembly
6961670 7 mm x 16 mm Disc Assembly
6961870 7 mm x 18 mm Disc Assembly
6961480 8 mm x 14 mm Disc Assembly
6961680 8 mm x 16 mm Disc Assembly
6961880 8 mm x 18 mm Disc Assembly
6960013/6961340* Self-Tap Bone Screw 4.0 mm x 13 mm
6960015/6961540* Self-Tap Bone Screw 4.0 mm x 15 mm
6960113/6961345* Self-Tap Bone Screw 4.5 mm x 13 mm
6960115/6961545* Self-Tap Bone Screw 4.5 mm x 15 mm
6960120/6961120* Lock Screw
* Catalog number for screws in implant box / catalog number for separately packaged extra screws, if needed.
Implied warranties of merchantability and fitness for a particular purpose or use are specifically excluded. See the MDT Catalog
or price list for further information about warranties and limitations of liability.
Page 2

INDICATIONS
The PRESTIGE™ Cervical Disc is indicated in skeletally mature patients for reconstruction of the disc at one level from C3-C7
following single-level discectomy for intractable radiculopathy (arm pain and/or a neurological deficit) with or without neck pain,
or myelopathy due to a single-level abnormality localized to the disc space and at least one of the following conditions confirmed
by radiographic imaging (CT, MRI, X- rays): herniated nucleus pulposus and/or osteophyte formation. The PRESTIGE™ device
is implanted via an open anterior approach. Patients should have failed at least 6 weeks of conservative treatment prior to
implantation of the PRESTIGE™ Cervical Disc.
CONTRAINDICATIONS
The PRESTIGE™ Cervical Disc should not be implanted in patients with an active infection or with an allergy to stainless steel.
WARNINGS
The PRESTIGE™ Cervical Disc should only be used by surgeons who are experienced in the surgical procedure and have
undergone adequate training with this device. A lack of adequate experience and/or training may lead to a higher incidence of
adverse events, such as neurological complications.
Due to the proximity of vascular and neurological structures to the implantation site, there are risks of serious or fatal
hemorrhage and risks of neurological damage with the use of this device. Serious or fatal hemorrhage may also occur if the
great vessels are eroded or punctured during implantation and are subsequently damaged due to breakage of implants,
migration of implants, or if pulsatile erosion of the vessels occurs because of close apposition of the implants.
PRECAUTIONS
The safety and effectiveness of this device has not been established in patients with the following conditions:
▪ More than one cervical level with DDD;
▪ Not skeletally mature;
▪ Clinically significant cervical instability;
▪ Prior fusion at adjacent cervical level;
▪ Severe facet joint pathology of involved vertebral bodies;
▪ Prior surgery at treated level;
▪ Osteopenia, osteomalacia, or osteoporosis as defined by bone mineral density T-score of -3.5, or -2.5 with vertebral crush
fracture;
▪ Spinal metastases;
▪ Chronic or acute renal failure or history of renal disease;
▪ Taking medications known to potentially interfere with bone/soft tissue healing (e.g. steroids);
▪ Pregnant; and
▪ Severe insulin dependent diabetes.
In addition, safety and effectiveness of the device has not been established in patients who have not undergone at least six
weeks of conservative treatment or had signs of progression or spinal cord/nerve root compression with continued nonoperative care.
Implanted metal alloys release metallic ions into the body (especially those devices with metal-on-metal articulating surfaces).
The long term effect of these ions on the body is not known.
Wear rates higher than those predicted based on bench testing have been observed during in vivo wear analyses of several
explanted PRESTIGE™ Cervical Disc devices. In addition, there has been evidence of metallosis accompanied by a chronic
macrophage-dominated inflammatory response in subjects who have had the device removed. While there has been no direct
causal association between the wear-related findings and implant loosening/osteolysis, device failure or overall clinical
outcomes, high wear and associated metallosis and chronic inflammation are potential precursors of longer-term failure.
PRE-OPERATIVE
Patient selection is extremely important. In selecting patients for a total disc replacement, the following factors can be of
extreme importance to the success of the procedure: the patient’s occupation or activity level; a condition of senility, mental
illness, alcoholism or drug abuse; and certain degenerative diseases (e.g., degenerative scoliosis or ankylosing spondylitis) that
may be so advanced at the time of implantation that the expected useful life of the device is substantially decreased.
Correct selection of the appropriate implant size is extremely important to assure the placement and function of the disc. See
the surgical technique manual for step-by-step instructions.
INTRA-OPERATIVE
Use aseptic technique when removing the PRESTIGE™ Cervical Disc Replacement components from the innermost packaging.
Use care when handling a PRESTIGE™ component to ensure that it does not come in contact with objects that could damage
the implant. Exercise care to ensure that implantation instruments do not contact the highly polished articulating surfaces of the
endplates. Damaged implants are no longer functionally reliable.
To prevent unnecessary damage to the bearing surfaces, ensure that tissue debris is not trapped within the assembly.
PRESTIGE™ Cervical Disc Replacement components should not be used with components or instruments of spinal systems
from other manufacturers. See the surgical technique manual for step-by-step instructions.
Surgical implants must never be re-used or re-implanted. Even though the device appears undamaged, it may have small
defects and internal stress patterns that may lead to early breakage.
Page 3

POST-OPERATIVE
Patients in the clinical study were instructed to use non-steroidal anti-inflammatory drugs (NSAIDs) for two weeks
postoperatively. It has been reported in the literature that short-term postoperative use of NSAIDs may reduce the instance of
heterotopic ossification.
Patients should be instructed in postoperative care procedures and should be advised of the importance of adhering to these
procedures for successful treatment with the device, including the avoidance of heavy lifting, repetitive bending, and high-impact
exercise or athletic activity for 60 days postoperative.
POTENTIAL ADVERSE EVENTS
Risks associated with the use of the PRESTIGE™ Cervical Disc include: 1) those commonly associated with any surgery; 2)
those specifically associated with cervical spinal surgery using an anterior approach; and 3) those associated with a spinal
implant, as well as those pertaining to the PRESTIGE™ Cervical Disc. However, the causality of these adverse events is not
exclusive to these categories. There is also the risk that this surgical procedure will not be effective, and may not relieve or may
cause worsening of preoperative symptoms. Some of these effects may have been previously reported in the adverse events
table.
1. Risks associated with any surgical procedure are those such as abscess; cellulitis; wound dehiscence; wound necrosis;
edema; hematoma; heart and vascular complications; hypertension; thrombosis; ischemia; embolism; thromboembolism;
hemorrhage; thrombophlebitis; adverse reactions to anesthesia; pulmonary complications; organ, nerve or muscular
damage; seizure, convulsion, or changes to mental status; and complications of pregnancy including miscarriage and fetal
birth defects.
2. Risks associated with anterior interbody surgery of the cervical spine include dysphagia; dysphasia; dysphonia; hoarseness;
vocal cord paralysis; laryngeal palsy; sore throat; recurring aspirations; nerve deficits or damage; tracheal, esophageal, and
pharyngeal perforation; airway obstruction; external chylorrhea; warmth or tingling in the extremities; deficit or damage to
the spinal cord, nerve roots, or nerves possibly resulting in paralysis or pain; dural tears or leaking; cerebrospinal fistula;
discitis, arachnoiditis, and/or other types of inflammation; loss of disc height; loss of proper curvature, correction, height or
reduction of the spine; vertebral slipping; scarring, herniation or degeneration of adjacent discs; surrounding soft tissue
damage, spinal stenosis; spondylolysis; otitis media; fistula; vascular damage and/or rupture; and headache.
3. Risks associated with implants in the spine, including the PRESTIGE™ device, are early or late loosening of the
components; disassembly; bending or breakage of any or all of the components; implant migration; malpositioning of
implant; loss of purchase; sizing issues with components; anatomical or technical difficulties; implant fracture; bone fracture;
skin penetration, irritation, pain, bursitis resulting from pressure on the skin from component parts in patients with
inadequate tissue coverage over the implant; foreign body reaction to the implants including possible tumor formation,
autoimmune disease, metallosis, and/or scarring; possible tissue reaction; bone resorption; bone formation that may reduce
spinal motion or result in a fusion, either at the treated level or at adjacent levels; development of new radiculopathy;
myelopathy or pain; cessation of bone growth of the operated portion of the spine; tissue or nerve damage caused by
improper positioning and placement of implants or instruments; loss of neurological function; decreased strength of
extremities; decreased reflexes; appearance of cord or nerve root injury; loss of bowel and/or bladder control or other types
of urological system compromise; gastrointestinal and/or reproductive system compromise; and interference with
radiographic imaging because of the presence of the implant.
4. Wound, local, and/or systemic infections.
5. Surgical instrument bending or breakage, as well as the possibility of a fragment of a broken instrument remaining in the
patient.
6. Inability to resume activities of normal daily living, including loss of consortium.
7. Death.
NOTE: For the specific adverse events that occurred in the clinical study of the PRESTIGE™ Cervical Disc, please see
Safety Results in the CLINICAL STUDIES section below. Additional surgery may be necessary to correct some of the
adverse effects.
CLINICAL STUDIES
A multi-center, prospective, randomized, non-inferiority clinical trial of the PRESTIGE™ Cervical Disc was conducted in the
United States comparing the anterior spinal use of the PRESTIGE™ device to fusion using allograft and plating stabilization, the
control, in the treatment of patients with symptomatic degenerative disc disease for an Investigational Device Exemption (IDE)
(G010188). A total of 541 patients were enrolled in the clinical trial: 276 patients in the investigational PRESTIGE™ device
treatment group and 265 patients in the control arm. Fifty-nine additional continued access patients also received the
investigational treatment. Twenty-five of the continued access patients were simultaneously enrolled into a Metal Ion cohort, and
had blood collected for metal ion analysis at each follow-up time point.
A Post-Approval Study required as a condition of PMA approval was also conducted to follow the original IDE subject cohort
through 84 months postoperatively.
Page 4

SUMMARY OF THE IDE AND POST-APPROVAL STUDY (PAS) METHODS
Study Objectives
IDE Study
The primary objective of the IDE study was to demonstrate that the overall success rate for the investigational PRESTIGE™
Cervical Disc treatment is statistically non-inferior to, the overall success rate of the control treatment at 24 months following
surgery as determined by a prespecified non-inferiority margin of 0.10. If statistical non-inferiority was established, the
investigational treatment is considered to be safe and effective and the study was considered a success.
Other secondary objectives were to compare the success rates of individual effectiveness endpoints and neurological status at
24 months following surgery.
PAS Study
The primary objective of the post-approval study was to demonstrate that the overall success rate for the investigational
PRESTIGE™ Cervical Disc treatment is statistically non-inferior to the overall success rate of the control treatment at 84 months
following surgery, as determined by a pre-specified non-inferiority margin of 0.10. If statistical non-inferiority was established,
the investigational treatment is considered to be safe and effective and the study was considered a success.
Other secondary objectives were to compare the success rates of individual effectiveness endpoints and neurological status at
84 months following surgery.
Study Designs
IDE Study
The IDE study was a multi-center, prospective, randomized, controlled clinical trial comparing the investigational PRESTIGE™
Cervical Disc treatment to the control treatment. Data were collected at pre-operative, discharge, 6 weeks, 3 months, 6 months,
12 months (1 year) and at 24 months (2 years).
PAS Study
The post-approval study was a prospective study to continue follow-up on the subjects who participated in the IDE study. Data
were collected at 36 months (3 years), 60 months (5 years), and 84 months (7 years) postoperative to determine the long-term
safety and effectiveness of the device.
Inclusion and Exclusion Criteria
Patient eligibility criteria were defined in the original IDE clinical study protocol. No exclusion of any patient was planned for the
post-approval study. As defined in the IDE study protocol, prospective patients were diagnosed with symptomatic cervical
degenerative disc disease according to the following inclusion/exclusion criteria. Patients were geographically stable and were
able to attend follow-up examinations at the investigational site. In addition, all patients agreed to undergo the necessary
preoperative and postoperative evaluations specified in the Clinical Investigational Plan (CIP).
Inclusion Criteria:
All patients participating in this study were required to meet all of the following inclusion criteria:
1. Cervical degenerative disc disease defined as: intractable radiculopathy and/or myelopathy with at least one of the following
characteristics and producing symptomatic nerve root and/or spinal cord compression as documented by patient history
{e.g., pain [neck and/or arm pain], functional deficit and/or neurological deficit, and radiographic studies (e.g., CT, MRI, xrays, etc.)}:
a) herniated disc
b) osteophyte formation
2. One cervical level requiring surgical treatment;
3. C3-C4 disc to C6-C7 disc level of involvement;
4. Unresponsive to non-operative treatment for approximately six weeks or has the presence of progressive symptoms or
signs of nerve root/spinal cord compression in the face of continued non-operative management;
5. No previous surgical intervention at the involved level or any subsequent, planned/staged surgical procedure at the involved
or adjacent level(s);
6. At least 18 years of age at the time of surgery;
7. Preoperative Neck Disability Index score ≥ 30;
8. Preoperative neck pain score of > 20 (based on the Preoperative Neck and Arm Pain Questionnaire);
9. Not pregnant at the time of surgery;
10. Willing to comply with the study plan and sign the Patient Informed Consent Form.
Exclusion Criteria:
A patient meeting any of the following criteria was to be excluded from the study:
1. Cervical spinal condition other than symptomatic cervical disc disease requiring surgical treatment at the involved level;
2. Documented or diagnosed cervical instability defined by dynamic (flexion/extension) radiographs showing:
a) Sagittal plane translation > 3.5 mm or;
b) Sagittal plane angulation > 20°;
Page 5

3. More than one cervical level requiring surgical treatment;
4. Fused level adjacent to the level to be treated;
5. Severe pathology of the facet joints of the involved vertebral bodies;
6. Previous surgical intervention at the involved level;
7. Previously diagnosed with osteopenia or osteomalacia;
8. Any of the following that may be associated with a diagnosis of osteoporosis (if any of the below risk factors were present, a
DEXA Scan was required to determine eligibility, with a measured BMD of -3.5, or 2.5 with vertebral crush fracture,
considered a criteria for exclusion):
a) Postmenopausal non-black female over 60 years of age who weighs less than 140 pounds.
b) Postmenopausal female that has sustained a non-traumatic hip, spine, or wrist fracture.
c) Male over the age of 70.
d) Male over the age of 60 that has sustained a non-traumatic hip or spine fracture.
9. Presence of spinal metastases;
10. Overt or active bacterial infection, either local or systemic;
11. Severe insulin dependent diabetes;
12. Chronic or acute renal failure or prior history of renal disease;
13. Fever (temperature > 101° F oral) at the time of surgery;
14. Documented allergy or intolerance to stainless steel, titanium, or a titanium alloy;
15. Mental incompetence. (If questionable, psychiatric consult was obtained);
16. Incarceration;
17. Pregnancy;
18. Alcohol and/or drug abuse, as defined by currently undergoing treatment for alcohol and/or drug abuse;
19. Use of drugs (e.g., steroids or methotrexate) which may interfere with bone metabolism within two weeks prior to the
planned date of spinal surgery (excluding routine perioperative anti-inflammatory drugs;
20. History of an endocrine or metabolic disorder known to affect osteogenesis (e.g., Paget’s Disease, renal osteodystrophy,
Ehlers-Danlos Syndrome, or osteogenesis imperfecta);
21. Condition that requires postoperative medications that interfere with the stability of the implant or fusion, such as steroids.
(Excluding low dose aspirin for prophylactic anticoagulation and routine perioperative anti-inflammatory drugs);
22. Treatment with an Investigational therapy within 28 days prior to implantation surgery, or plans for such treatment earlier
than 16 weeks following the study treatment.
Study Population
The studies included 541 enrolled IDE, continued access and metal ion study subjects who were at least 18 years old at the
time of the surgery and met the study inclusion and exclusion criteria.
Post-Operative Care
The recommended post-operative care included avoidance of heavy lifting, repetitive bending, and high-impact exercise or
athletic activity for 60 days postoperatively. Avoidance of prolonged NSAID use (beyond 2 weeks postop) was also specified in
the postoperative regimen, although the use of NSAIDs was recommended for the first two weeks postoperatively. The use of
electrical bone growth stimulators was prohibited during the 24-month follow-up period. Patients who smoked were also
encouraged to discontinue smoking.
IDE and PAS Follow-up Schedules
For the IDE study, patients were evaluated preoperatively (within 6 months of surgery), intraoperatively, and postoperatively at 6
weeks, 3, 6, 12, and 24 months. For the PAS study, patients were evaluated at 36, 60, and 84 months. At each evaluation time
point, the primary and secondary clinical and radiographic outcome parameters were evaluated as shown in Table 2. For the
IDE, success was determined from data collected during the initial 24 months of follow-up. For the post-approval study, success
was determined from the data collected up to 84 months.
Page 6
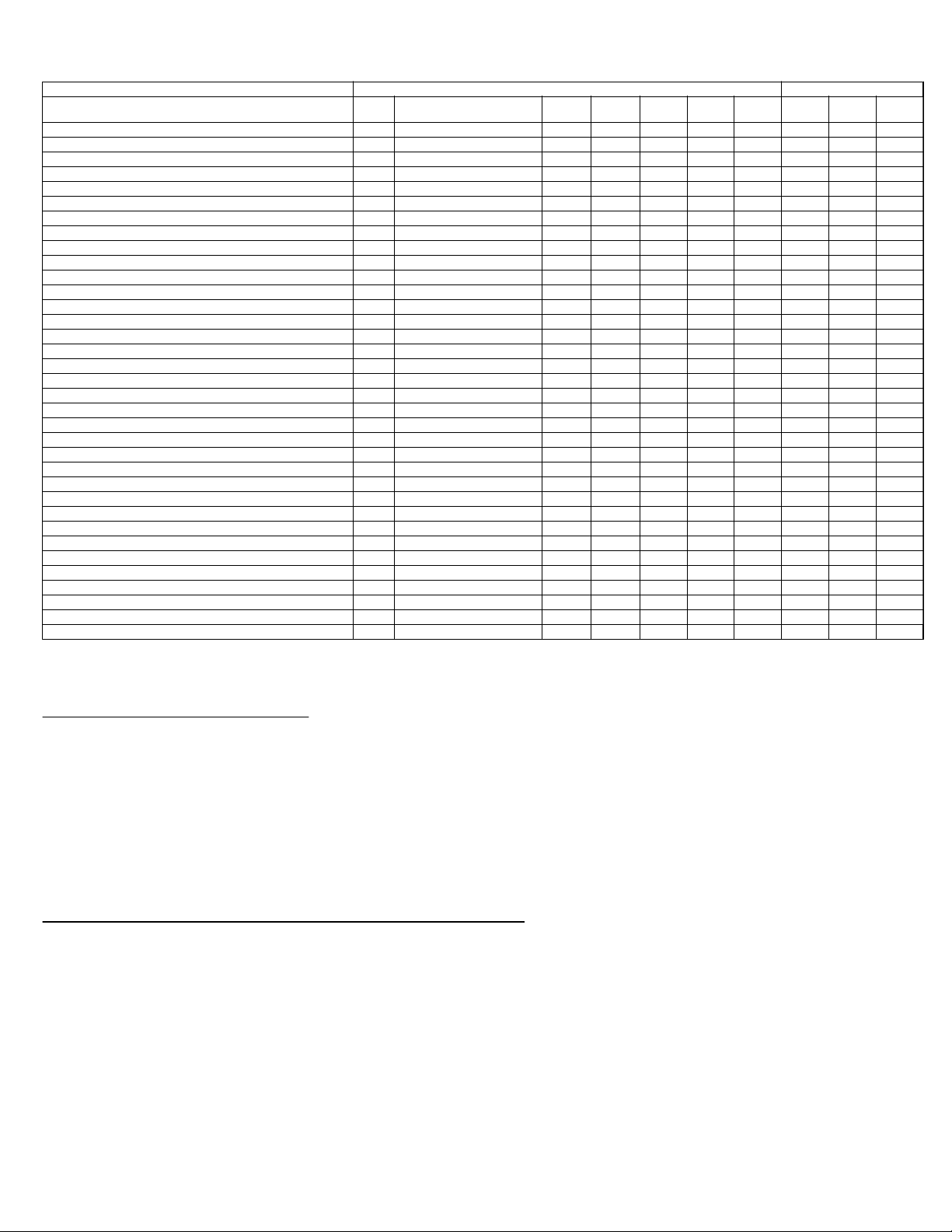
Table 2: Schedule of Study Assessments
Evaluation Pre-op Surgery/ Hospital Discharge 6 wks
Preoperative Information
Obtain Screening Form X
Confirm Patient Eligibility X
Obtain Informed Consent X
Open Randomization Envelope X
Case Report Forms
Patient Enrollment X
Patient Qualification X
Preoperative Data X
Prior History Questionnaire X
Neurological Status X X X X X X X X X
Preoperative Gait Assessment and Foraminal Compression Test X
Preoperative Patient Survey X
Preoperative Neck Disability Index X
Preoperative Neck and Arm Pain Questionnaire X
Health Status Questionnaire (SF-36) X X X X X
Radiologic Data X X X X X X X X X X
Surgery Data X
Hospital Discharge X
Postoperative Data X X XXX
Postoperative Patient Survey X X XXXXXX
Neck Disability Index X X XXXXXX
Postoperative Neck and Arm Pain Questionnaire X X X X X X X X
Postoperative Gait Assessment and Foraminal Compression Test X X X X X X X X
Adverse Event Form (if any) X X X X X X X X X
Patient Accountability (if needed) X X X X X X X X
Outstanding (Unresolved) Adverse Event (if any) X X X X X X X X X
Imaging
Radiographs and Scans
Anterior/Posterior X-ray X X X X X X X X X X
Lateral X-ray X X X XXXXXXX
Right/Left Lateral Bend X-rays X X X X X X X X X
Flexion/Extension X-rays X X X X X X X X X
CT and/or MRI X
DEXA Scan X
IDE Study Post-approval Study
(± 2wks)
3 Mo
(± 2wks)
6 Mo
(± 1 Mo)
12 Mo
(± 2 Mo)
24 Mo
(± 2 Mo)
36 Mo
(± 3 Mo)
60 Mo
(± 3 Mo)
84 Mo
(± 3 Mo)
Data Source
New data collection
IDE and PAS Study Endpoints
The primary endpoint for both the IDE and post-approval studies was a composite variable termed “overall success” which
included key safety and effectiveness considerations. The effectiveness component of the overall success variable was
comprised of both Neck Disability Index (NDI) and disc height success as measured by Functional Spinal Unit (FSU) height.
The safety components of the overall success variable were neurological status success, absence of a serious implant- or
implant/surgical procedure-associated adverse event or a second surgery that is classified as a “failure”. The combined
effectiveness and safety component determined whether a patient was an overall success. An alternate overall success
determination was also evaluated without disc height success. Overall success was determined at the 24-month time point for
the IDE and the 84-month time point for the post-approval study.
Secondary endpoints for both the IDE and post-approval studies included neck pain, arm pain, general health status, patient
satisfaction, patient global perceived effect, and gait assessments.
Strengths and Limitations of the Clinical Study Design
The following are important study design strengths of the IDE study as well as the post-approval study:
▪ The PAS provided extended term profile of safety and effectiveness as well as functional data established on a multicenter,
randomized, controlled clinical trial.
▪ The consistency of data gathering approaches and endpoints was maintained through both the IDE and the PAS studies.
▪ The strength and reliability of the final IDE and PAS conclusions were confirmed by several sensitivity analyses.
▪ The study design minimized potential biases by integrating a wide variety of assessments including subjective data,
physician-judged and core laboratory-assessed evaluations.
The following potential study design limitations should also be considered when interpreting the results of the IDE study as well
as the post-approval study:
▪ Although overall success (without FSU) data was available for 89% of all subjects at 24 months, due to the long-term nature
of the IDE and the post-approval studies, progressive lower follow-up rates at each subsequent follow-up visit through 84
months were anticipated, which may affect interpretation of long-term study results.
▪ Several of the primary and secondary study endpoints are subjective (e.g., NDI, pain scores, SF-36), and this subjectivity
may present biases.
Page 7

▪ Both the investigator and the patient were blinded to the randomized treatment throughout the screening and informed
consent process; however, the patient and surgeon were not blinded following the assignment of treatment group by the
sponsor. Like other clinical studies appraising artificial cervical disc devices, it was unfeasible to mask subjects to their
treatment assignment. This was well-adjusted by integrating result measures judged by both the surgeon and core
laboratories.
▪ The capability to evaluate device performance for individual segments of the subject population is limited. This limitation is
mainly because the study was not designed to assess performance among subgroups. Any subgroup analyses should be
evaluated with caution.
SUMMARY OF THE IDE AND POST-APPROVAL STUDY RESULTS
Subject Accountability
The subject accountability data for the patients enrolled IDE and post-approval studies covering 34 sites are summarized in
Table 3.
Table 3: Subject Accountability
IDE Study Post Approval Study
6 Mo
(± 1 Mo)
(86.2%)
(66.2%)
224
172
(± 2 Mo)
263
(95.6%)
204
(74.2%)
12 Mo
223
(87.1%)
172
(67.2%)
(± 2 Mo)
251
(91.3%)
189
(68.7%)
24 Mo
220
(86.6%)
169
(66.5%)
(± 3 Mo)
198
(72.0%)
150
(54.5%)
36 Mo
160
(63.2%)
124
(49.0%)
(± 3 Mo)
220
(81.8%)
167
(62.1%)
60 Mo
188
(76.1%)
138
(55.9%)
(± 3 Mo)
212
(78.8%)
168
(62.5%)
84 Mo
Variable Inv Ctrl Inv Ctrl Inv Ctrl Inv Ctrl Inv Ctrl Inv Ctrl Inv Ctrl
Total Enrolled Patients 276 265 276 265 276 265 276 265 276 265 276 265 276 265
Cumulative Withdrawn(s) After Surgery 0214171919513514
Cumulative Deaths 01010202032525
Theoretical Follow-up
Patients Evaluated Early
Patients Not Yet Over due
Expected
Evaluable for Overall Success without FSU (% of Total Expected) 254
Evaluable for Overall Success with FSU (% of Total Expected) 197
1
2
3
4
276 262 275 260 275 256 275 254 275 253 269 247 269 246
276 262 275 260 275 256 275 254 275 253 269 247 269 246
(92.0%)
(71.4%)
3 Mo
(± 2wks)
00000000000000
00000000000000
239
181
256
(93.1%)
196
(71.3%)
(91.2%)
(69.1%)
182
(74.0%)
135
(54.9%)
______________________________________________________________
1
Theoretical=Enrolled- Cumulative Deaths - Cumulative Withdrawn After Surgery
2
Patients that completed follow-up visits early in the visit window.
3
Number of patients who did not have evaluation on or before 08 Oct 2012 but were within the window.
4
Expected = Theoretical + Patients Evaluated Early for visit - Not Yet Overdue
Subject Demographics and Baseline Parameters
Table 4 summarizes the study patient demographics and baseline characteristics for the PRESTIGE™ Investigational and
control groups. The demographics of the study population are consistent with the demographics reported for prior cervical
artificial disc studies conducted in the U.S. The investigational and control treatment groups were very similar with regards to
the demographics and baseline parameters, and there were no statistical differences (p<0.05) for any of the variables in Table 4
with the exception of alcohol use
Table 4: Study Patient Demographics and Baseline Characteristics
Variables Inv
(N=276)
Age (years) 43.3 ± 7.6 43.9 ± 8.8 0.435
Height (inches) 67.4 ± 3.9 67.5 ± 4.2 0.767
Weight (lbs.) 181.7 ± 39.7 184.7 ± 41.5 0.389
Sex (% male) 128/276 (46.4%) 122/265 (46.0%) 1.000
Race
Caucasian
Black
Asian
Hispanic
Other
260/276 (94.2%)
6/276 (2.2%)
1/276 (0.4%)
7/276 (2.5%)
2/276 (0.7%)
Marital Status
Single
Married
Divorced
Separated
Widowed
44/276 (15.9%)
188/276 (68.1%)
36/276 (13.0%)
5/276 (1.8%)
3/276 (1.1%)
Ctrl
(N=265)
243/265 (91.7%)
13/265 (4.9%)
2/265 (0.8%)
6/265 (2.3%)
1/265 (0.4%)
32/265 (12.0%)
204/265 (77.0%)
24/265 (9.1%)
3/265 (1.1%)
2/265 (0.8%)
p-value
0.448
0.240
Page 8
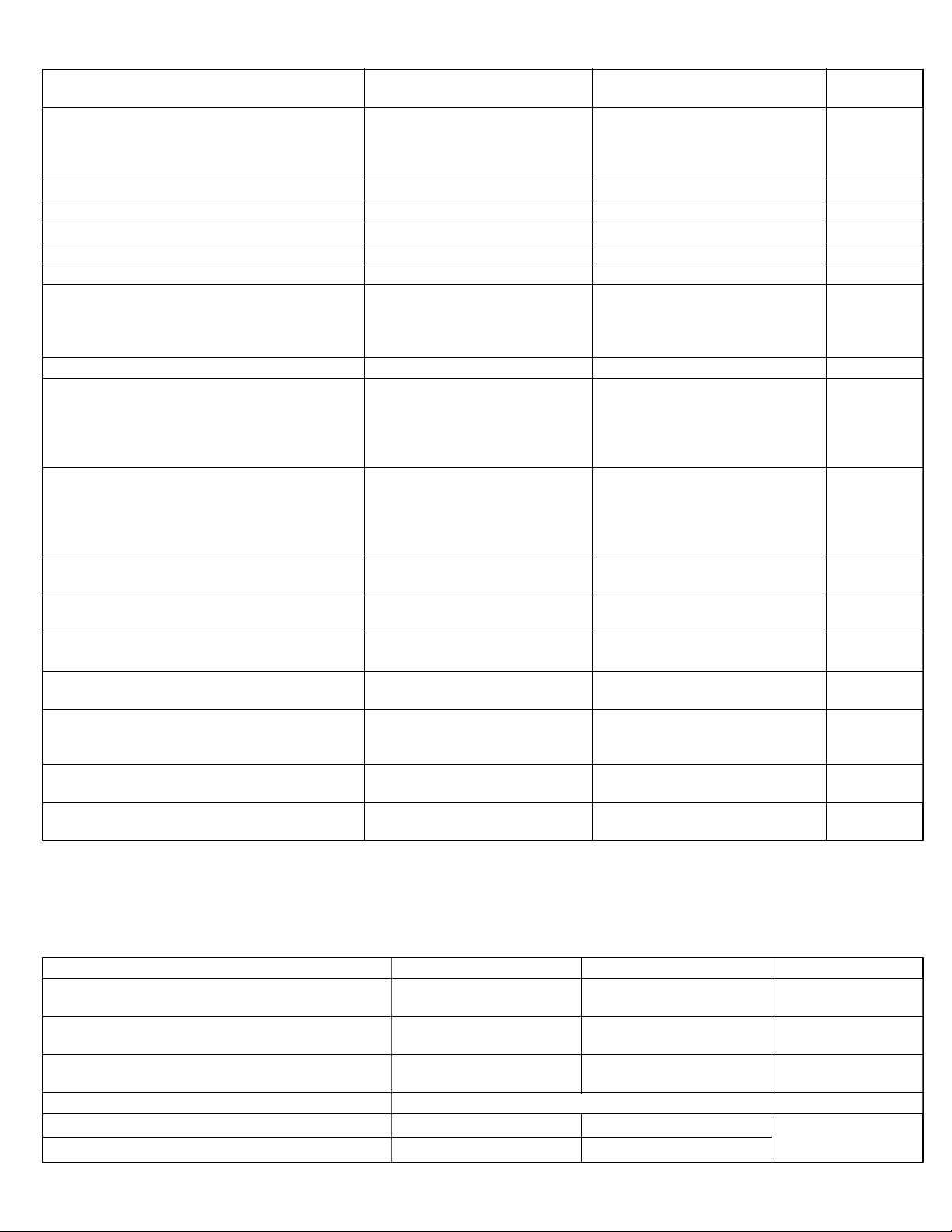
Table 4: Study Patient Demographics and Baseline Characteristics (continued)
Variables Inv
(N=276)
Education Level
< High School
High School
h School
> Hig
10/276 (3.6%)
73/276 (26.4%)
193/276 (69.9%)
Worker’s Compensation 32/276 (11.6%) 35/265 (13.2%) 0.603
Unresolved Spinal Litigation 30/276 (10.9%) 32/265 (12.1%) 0.687
Tobacco Used 95/276 (34.4%) 92/265 (34.7%) 1.000
Alcohol Used 120/276 (43.5%) 141/265 (53.2%) 0.025
Preoperative Work Status 182/276 (65.9%) 166/265 (62.6%) 0.473
Duration of Symptom
< 6 Weeks
6 Weeks to 6 Months
> 6
Months
21/276 (7.6%)
81/276 (29.3%)
174/276 (63.0%)
Previous Neck Surgery 1/276 (0.4%) 2/265 (0.8%) 0.617
Preoperative Medication use
Non-Narcotics
Weak Narcotics
Strong Narcotics
Muscle Relaxants
197/274 (71.9%)
130/275 (47.3%)
57/273 (20.9%)
119/274 (43.4%)
Preoperative Pain Status
Neither Arm or Neck Pain
Arm Pain Only
Neck Pain Only
Arm and Neck Pain
1/276 (0.4%)
1/276 (0.4%)
33/276 (12.0%)
241/276 (87.3%)
Baseline ROM Angulation 7.55 ± 4.25
Range: 0.43 - 24.85
Baseline ROM Translation 0.26 ± 0.26:
Range: 0.00 - 1.96
NDI 55.7 ± 14.8
Range: 6.0 – 94.0
SF-36 PCS 31.9 ± 7.0
Range: 15.3 – 51.7
SF-36 MCS 42.4 ± 12.1
Range: 16.3 – 65.3
Neck Pain Score 68.2 ± 22.7
Range: 2.0 – 100.0
Arm Pain Score 59.1 ± 29.4
Range: 0.0 – 100.0
Ctrl
(N=265)
14/265 (5.3%)
77/265 (29.2%)
173/265 (65.5%)
15/265 (5.7%)
89/265 (33.6%)
161/265 (60.8)
187/263 (71.1%)
127/263 (48.3%)
58/264 (22.0%)
114/264 (43.2%)
0/265 (0.0%)
0/265 (0.0%)
26/265 (9.8%)
238/265 (90.2%)
7.87 ± 4.32
Range: 0.74 – 21.34
0.26 ± 0.25
Range:0.00 – 1.64
56.4 ± 15.9
Range: 26.0 – 100.0
32.0 ± 7.5
Range: 7.9 – 56.0
42.7 ± 12.4
12.4
Range: 14.1 – 70.8
69.3 ± 21.5
Range: 20.0 – 100.0
62.4 ± 28.5
Rang
e: 0.0 – 100.0
p-value
0.458
0.435
0.849
0.863
0.833
1.000
0.491
0.446
0.989
0.632
0.760
0.795
0.553
0.191
Surgical and Hospitalization Information
Table 5 summarizes the information related to the surgical procedures and postoperative hospitalizations of subjects. The most
common treated surgical levels were C5-C6 and C6-C7. Table 6 summarizes device implanted by size and level. The mean
operative time; mean estimated blood loss volume; and the hospitalization times were similar in both groups.
Table 5: Surgical Results
Inv Ctrl p
Op
erative Time (hrs)
Mean ± SD 1.6 ± 0.6 1.4 ± 0.5 <0.001
EBL (ml)
Mean ± SD 60.1 ± 63.0 57.5 ± 68.1 0.635
Hospitalization (days)
Mean ± SD 1.1 ± 0.6 1.0 ± 0.5 0.041
Spinal level treated
C
(%) 7 (2.5) 10 (3.8)
3-4
C
(%) 14 (5.1) 15 (5.7)
4-5
- Value
0.041
Page 9

Table 5: Surgical Results (continued)
Inv Ctrl p
C
(%) 142 (51.4) 149 (56.2)
5-6
C
(%) 113 (40.9) 91 (34.3)
6-7
- Value
Table 6: All PRESTIGE™ Devices Implanted by Size and Level
Treated Level
C3-C4 C4-C5 C5-C6 C6-C7 Total by Implant Size
Implant Size combinations
(Upper/Lower)
Upper: 6mm x 12mm
Lower: 6mm x 12mm
Upper: 7mm x 12mm
Lower: 7mm x 12mm
Upper: 7mm x 12mm
Lower: 7mm x 14mm
Upper: 7mm x 14mm
Lower: 7mm x 14mm
Upper: 8mm x 12mm
Lower: 8mm x 12mm
Upper: 8mm x 14mm
Lower: 8mm x 14mm
4 8 89 52 153/276 (55.4%)
0 3 23 16 42/276 (15.2%)
0 0 0 1 1/276 (0.4%)
2 2 20 30 54/276 (19.6%)
0 1 6 4 11/276 (4.0%)
1 0 4 10 15/276 (5.4%)
Total by Treated Level 7/276 (2.5%) 14/276 (5.1%) 142/276 (51.4%) 113/276 (40.9%) 276/276 (100.0%)
Safety Results
The safety of the PRESTIGE™ was assessed by monitoring intraoperative and postoperative complications. Radiographs were
examined for evidence of device migration or breakage. Observations of subsidence were reported by investigators as adverse
events. All radiographic endpoints were evaluated independently by a core laboratory.
Adverse Events
The adverse effects, as shown in Table 7 below, were reported from the 276 PRESTIGE™ device patients and 265 control
patients enrolled in the multi-center clinical study. Adverse event rates presented are based on the number of patients having at
least one occurrence for a particular adverse event divided by the total number of patients in that treatment group. Statistical
comparison of the adverse events was conducted using time to event analysis respectively for the cumulative event rate for any
adverse events up to 24-months visit and up to 84-months visit as shown in Table 8. The overall cumulative AE rate for events
up to 24-months visit (89.2% in the investigational group versus 90.2% in the control group, p-value form log-rank test = 0.692)
and up to 84-months visit (97.7% in the investigational group versus 94.5% in the control group, p-value form log-rank test =
0.958) are comparable between the two treatment groups. Additionally, Table 9 and 10, respectively summarize the adverse
events that are classified as device or device/surgical procedure related and the adverse events that are serious.
Page 10

Table 7: Adverse Events for US IDE5 and Post-Approval Studies
IDE PAS
6 Mo (≥5
Control
Mo-<9
Mo)
Invest
12 Mo (≥9
Control
Mo-<19
Mo)
Invest
Control
24 Mo
(≥19 Mo-
<30 Mo)
Invest
# of Patients
Reporting &
Total adverse events
Inv #
Patients
(% of
276) Total
# Events
Control
Complication
Surgery Post-
Invest
6
Control
operative
(1 day-<4
Wks)
Invest
Control
6 Wks
(≥4
Wks-<9
Wks)
Invest
Control
3 Mo (≥9
Wks-<5
Mo)
Invest
(≤ 24 Mo)
Patients
265) Total
# Events
Ctrl #
(% of
36 Mo
(≥30 Mo-
<42 Mo)
Invest
Control
48 Mo
(≥42 Mo-
<54 Mo)
Invest
Control
60 Mo
(≥54 Mo-
<66 Mo)
Invest
Control
72 Mo
(≥66 Mo-
<78 Mo)
Invest
Control
84 Mo
(≥78
Mo-<90
Mo)
Invest
Control
# of Patients
Reporting &
Total adverse events
(≤ 84 Mo)
Inv #
Patients
(% of
276) Total
# Events
Ctrl #
Patients
(% of
265) Total
# Events
Anatomical/Tec
hnical Difficulty
Cancer 00 0 100000030215 (1.8)52 (0.8)2211001610012 (4.3)145 (1.9)
Cardiovascular 00 2 2003 2 12112106 18 (6.5)2713 (4.9)14833556945439 (14.1)5731 (11.7)
Carpal Tunnel
Syndrome
Death 00 0 0000 1 000 1 0 1 0 (0.0)03 (1.1)300220000002 (0.7)25 (1.9)
Dysphagia/
Dysphonia
Gastrointestinal 0 3 4 4 0 1 4 2 5 2 15 12 7 9 30 (10.9)3530 (11.3)339566166937556 (20.3)8251 (19.2)
Implant
Displacement/
Loosening
Infection 2 0 7 3 1 5 6 1 4 2 11 8 6 9 32 (11.6)3724 (9.1)281171061121075762 (22.5)8441 (15.5)
Neck and/or
Arm Pain
Neurological 4 1 9 10 10 5 13 11 15 5 23 19 10 21 68 (24.6)8460 (2
Non-Union 00 0 0020 2 030 2 0 0 0 (0.0)09 (3.4)900000000000 (0.0)09 (3.4)
Non-Union Pending
7
Other
Other Pain
Respiratory 1 0 1 2001 0 122 2 4 3 10 (3.6)108 (3.0)9136222441222 (8.0)2419 (7.2)
Spinal Event 0 1 3 416614366 9 81423 (8.3)2750 (18.9)54311518612956645 (16.3)5682 (30.9)
Subsidence 00 0 00000100000 1 (0.4)10 (0.0)000000000203 (1.1)30 (0.0)
Trauma 0 0 6 3 6 6 14 14 15 10 22 11 26 18 72 (26.1)8950 (18.9)6220 17 14 22 19 16 19 18 11 9 107 (38.8)
Urogenital 0 0 0 0013 2 237 2101 20 (7.2)228 (3.0)98 5 16 2 4 7 3 5 5 2 44 (15.9)5823 (8.7)
Vascular Intra-Op21 211000000010 5 (1.8)62 (0.8)210010000006 (2.2)73 (1.1)
Any Adverse
Events
10 000000000000 1 (0.4)10 (0.0)000000000001 (0.4)10 (0.0)
00 10113100937418 (6.5)217 (2.6)9020131102124 (8.7)2712 (4.5)
561511131210110024 (8.7)2422 (8.3)23201224101029 (10.5)3126 (9.8)
00 010110000211 2 (0.7)25 (1.9)511002100106 (2.2)67 (2.6)
5 1 26 17 30 12 28 39 49 29 34 42 33 28 145 (52.5)
00 000001060707 0 (0.0)021 (7.9)2100000000010 (0.0)022 (8.3)
3 6 19 17 10 8 13 13 19 6 35 27 33 48 81 (29.3)
8
2 3 5 4 9 4 13 16 20 14 31 19 37 24 82 (29.7)
25 22 100 80 70 55 109 121 136 90 210 169 195 195 235 (85.1)
121 (45.7)
205
85 (32.1)
132
64 (24.2)8436 22 47 25 26 22 28 11 19 11 137 (49.6)
117
219 (82.6)
845
16 21 23 14 27 15 7 4 6 11 178 (64.5)
168
2.6)7212 8 5 12 14 13 6 4 11 11 99 (35.9)
34 21 34 19 43 38 13 31 17 10 137 (49.6)
125
164 127 173 137 180 146 125 97 99 80 259 (93.8)
732
284
132
273
273
172
1586
0
5
36
14
5
29
58
7
57
148 (55.8)
233
87 (32.8)
120
9
22
127 (47.9)
244
107 (40.4)
175
22
106
0
93 (35.1)
144
30
3
232 (87.5)
1319
______________________________________________________________
5
Based on 24-month cohort at time of interim analysis as pre-specified in IDE protocol.
6
Control=Single level anterior interbody fusion procedure with allograft and plate stabilization.
7
Other consists of various events that do not fit into another category, such as allergic reaction, depression, or insomnia.
8
Other Pain consists of non-neck and/or arm pain events such as headache, lower back pain, or leg pain.
Page 11

Table 8: Statistical Comparison of Adverse Events Rates using Time to Event Analysis
Treatments Number of Patients Cumulative Rate (%) P-Values
Inv
Anatomical/Technical Difficulty 1 0 0.4 0.0 0.327 0.327 1 0 0.4 0.0 0.327 0.327
Cancer 5 2 2.6 1.2 0.325 0.353 12 5 5.2 2.4 0.148 0.174
Cardiovascular 18 13 7.5 7.8 0.521 0.491 39 31 17.8 15.5 0.601 0.609
Carpal Tunnel Syndrome 18 7 8.9 3.7 0.049 0.050 24 12 10.6 6.0 0.076 0.072
Death 0 3 0.0 1.7 0.068 0.068 2 5 0.9 2.2 0.197 0.165
Dysphagia/
Dysphonia
Gastrointestinal 30 30 12.6 15.9 0.707 0.769 56 51 24.7 24.9 0.915 0.976
Implant Displacement/
Loosening
Infection 32 24 13.7 12.7 0.419 0.363 62 41 27.0 20.5 0.091 0.093
Neck and/or Arm Pain 145 121 58.3 53.6 0.156 0.094 178 148 70.2 64.8 0.094 0.070
Neurological 68 60 27.9 29.9 0.731 0.615 99 87 42.5 41.5 0.790 0.631
Non-Union 0 9 0.0 3.6 0.002 0.002 0 9 0.0 3.6 0.002 0.002
Non-Union - Pending 0 21 0.0 11.6 <0.001 <0.001 0 22 0.0 10.0 <0.001 <0.001
7
Other
8
Other Pain
Respiratory 10 8 5.2 4.5 0.788 0.795 22 19 9.7 10.1 0.897 0.841
Spinal Event 23 50 10.4 24.7 <0.001 <0.001 45 82 20.9 38.9 <0.001 <0.001
Subsidence 1 0 0.4 0.0 0.341 0.341 3 0 2.3 0.0 0.087 0.145
Trauma 72 50 32.4 25.0 0.102 0.118 107 93 44.9 44.9 0.688 0.445
Urogenital 20 8 10.4 3.7 0.045 0.053 44 23 20.1 12.2 0.024 0.018
Vascular Intra-Op 5 2 1.8 0.8 0.280 0.281 6 3 2.2 1.3 0.360 0.330
Any Adverse Events 235 219 89.2 90.2 0.692 0.708 259 232 97.7 94.5 0.958 0.722
(N=276)
24 22 8.7 8.4 0.916 0.929 29 26 11.5 10.5 0.868 0.935
2 5 1.1 2.5 0.200 0.190 6 7 3.1 3.1 0.623 0.449
81 85 34.3 42.9 0.359 0.475 137 127 57.2 57.1 0.637 0.639
82 64 37.4 31.0 0.305 0.373 137 107 58.7 50.1 0.081 0.134
Ctrl
(N=265)
Up to 24 Months Visit Up to 84 Months Visit
Inv
(N=276)
Ctrl
(N=265)
(Inv Vs Ctrl)
Log- Rank Wilcoxon Inv
Number of Patients Cumulative Rate (%) P-Values
(N=276)
Ctrl
(N=265)
Inv
(N=276)
Ctrl
(N=265)
(Inv Vs Ctrl)
Log- Rank Wilcoxon
Table 9: Adverse Events Classified as Device-Related or Device/Surgical Procedure-Related in US IDE5 and PostApproval Studies
Surgery Post-
Complication
Invest
Dysphagia/
Dysphonia
Implant
Displacement/
Loosening
Neck and/or
Arm Pain
Neurological 0 0 0 0 1010002000 4 (1.4)40 (0.0)00000000000 4 (1.4)40 (0.0)
Non-Union 0 0 0 0 0102030100 0 (0.0)07 (2.6)70000000000 0 (0.0)07 (2.6)
Non-UnionPending
Spinal Event 0 0 0 0 1000000000 1 (0.4)10 (0.0)00011201220 7 (2.5)73 (1.1)
Subsidence 0 0 0 0 0000100000 1 (0.4)10 (0.0)00000000000 1 (0.4)10 (0.0)
Trauma 0 0 0 0 00000010 00 1 (0.4)10 (0.0)00000000000 1 (0.4)10 (0.0)
Any Adverse
Events
0 0 1 0 00000000 00 1 (0.4)10 (0.0)00000000000 1 (0.4)10 (0.0)
0 0 0 1 01100002 11 2 (0.7)25 (1.9)51100210010 6 (2.2)67 (2.6)
0 0 0 0 10001000 00 2 (0.7)20 (0.0)00000000000 2 (0.7)20 (0.0)
0 0 0 0 00010605 04 0 (0.0)016 (6.0)160000000001 0 (0.0)017 (6.4)
0 0 1 1 32232938 15 11 (4.0)1227 (10.2)281111411231 20 (7.2)2232 (12.1)
6
Control
operative (1
day-<4 Wks)
Invest
Control
6 Wks
(≥4 Wks-
<9 Wks)
Invest
Control
IDE PAS
3 Mo (≥9
Wks-<5
Invest
Mo)
(≥5 Mo-
<9 Mo)
Control
6 Mo
Invest
12 Mo
(≥9 Mo-
<19 Mo)
Control
Invest
24 Mo
Mo-<30
Control
# of Patients Reporting
(≥19
Total adverse events
Mo)
Patients
(% of 276)
Total #
Events
Invest
Control
Inv #
&
(≤ 24 Mo)
(% of 265)
Ctrl #
Patients
Total #
Events
36 Mo
(≥30
Mo-<42
Mo)
Invest
48 Mo
Mo-<54
Control
(≥42
Mo)
Invest
60 Mo
Mo-<66
Control
(≥54
Mo)
Invest
72 Mo
Mo-<78
Control
(≥66
Mo)
Invest
84 Mo
Mo-<90
Control
# of Patients Reporting
(≥78
Total adverse events
Mo)
Patients
(% of 276)
Total #
Events
Invest
Control
Inv #
&
(≤ 84 Mo)
(% of 265)
Ctrl #
Patients
Total #
Events
0
7
0
0
7
17
3
0
0
34
Page 12

Table 10: Adverse Events Classified as Serious Adverse Events in US IDE5 and Post-Approval Studies
IDE PAS
6 Mo (≥5
Mo-<9
Mo)
12 Mo (≥9
Mo-<19
Mo)
24 Mo
(≥19 Mo-
<30 Mo)
# of Patients
Reporting &
Total adverse events
(≤ 24 Mo)
Ctrl #
(% of
276)
Total #
Events
192
Patients
(% of
Total #
Events
102 (38.5)
Patients
Wks)
6 Wks (≥4
Wks-<9
Surgery Post-
Complication Inv
Cancer 00 0 10000002021 4 (1.4)42 (0.8)2211001610012 (4.3)135 (1.9)
Cardiovascular001 0 002001805113 (4.7)162 (0.8)2512332503024 (8.7)348 (3.0)
Carpal Tunnel
Syndrome
Death 00 0 00001000101 0 (0.0)03 (1.1)30022000000 2 (0.7)25 (1.9)
Dysphagia/
Dysphonia
Gastrointestinal001 2 011111855514 (5.1)1614 (5.3)153252102531331 (11.2)4025 (9.4)
Implant
Displacement/
Loosening
Infection 100 1 0101101315 4 (1.4)410 (3.8)11323241332216 (5.8)1918 (16.8)
Neck and/or
Arm Pain
Neurological 10 1 2 1012006100 9 (3.3)105 (1.9)5010510102213 (4.7)1413 (4.9)
Non-Union 00 0 0 0202030100 0 (0.0)08 (3.0)80000000000 0 (0.0)08 (3.0)
Non-Union Pending
7
Other
Other Pain
Respiratory 10 0 00000001110 3 (1.1)31 (0.4)11031002100 9 (3.3)93 (1.1)
Spinal Event 000 2 133624452510 (3.6)1224 (9.1)25051600130010 (3.6)1435 (13.2)
Trauma 002 1 104622638320 (7.2)2313 (4.9)158566107896245 (16.3)6135 (13.2)
Urogenital 000 0 0010101151 8 (2.9)82 (0.8)26510004212124 (8.7)2812 (4.5)
Vascular Intra-Op20 0 100000000002 (0.07)21 (0.4)11000000000 3 (1.1)31 (0.4)
Any Adverse
Events
00 1 0111000505110 (3.6)132 (0.8)2010130001114 (5.1)175 (1.9)
10 0 00000001000 2 (0.7)20 (0.0)00001100000 3 (1.1)31 (0.4)
00 0 00000000000 0 (0.0)00 (0.0)00000000010 1 (0.4)10 (0.0)
00 5 0733632463222 (8.0)2516 (6.0)19432110001028 (10.1)3320 (
00 0 00000000100 0 (0.0)01 (0.4)10000000000 0 (0.0)01 (0.4)
00 1 40144531047623 (8.3)2721 (7.9)2287781093104346 (16.7)5944 (16.6)
8
00 1 31022431059524 (8.7)2718 (6.8)2713 5 10 10 7 7 13 3 2 0 54 (19.6)7240 (15.1)
6 0 13 17 12 12 22 31 19 19 67 37 53 36 106 (38.4)
operative
(1 day-<4
6
Inv Ctrl Inv Ctrl Inv Ctrl Inv Ctrl Inv Ctrl Inv Ctrl Inv #
Ctrl
Wks)
3 Mo (≥9
Wks-<5
Mo)
36 Mo
(≥30 Mo<42 Mo)
InvCtrlInvCtrlInvCtrlInvCtrlInvCtrl Inv #
265)
54 38 52 48 50 33 49 34 25 14 160 (58.0)
152
48 Mo
(≥42 Mo-
<54 Mo)
60 Mo
(≥54 Mo-
<66 Mo)
72 Mo
(≥66 Mo-
<78 Mo)
84 Mo
(≥78 Mo<90 Mo)
# of Patients
Reporting &
Total adverse events
(≤ 84 Mo)
Ctrl #
(% of
276)
Total #
422
Patients
(% of
265)
Total #
Events
5
8
5
5
1
27
0
21
23
13
8
1
59
43
3
39
44
13
1
149 (56.2)
319
Patients
Events
7.5)
Table 11 provides summary data on the number of adverse events in each treatment group by treatment level, including posthoc statistical analysis and comparison between the PRESTIGE™ investigational group and control group through the 24month visit and 84-month visit for each level. The 95% confidence interval (CI) was derived using the normal approximation to
the binomial distributions with standard error derived using Farrington and Manning Method.
Table 11: Summary of Total Adverse Events by Level Treated through 24 and 84 Months
Adverse Events Up to 24 Months Adverse Events# Up to 84 Months
Observed Event Rate Point Estimate and
Inv
(N=276)
Ctrl
(N=265)
95% Confidence
Limit*
(P(I) - P(C))
Any Adverse
Event
Observed Event Rate Point Estimate and
Inv
(N=276)
Ctrl
(N=265)
95% Confidence
Limit*
(P(I) - P(C))
C3-C4 7/7 (100.0%) 9/10 (90.0%) 0.100 [-0.127, 0.327] 7/7 (100.0%) 9/10 (90.0%) 0.100 [-0.127, 0.327]
C4-C5 13/14 (92.9%) 12/15 (80.0%) 0.129 [-0.123, 0.380] 14/14 (100.0%) 12/15 (80.0%) 0.200 [-0.022, 0.422]
C5-C6 127/142
(89.4%)
124/149
(83.2%)
0.062 [-0.017, 0.141] 139/142
(97.9%)
131/149
(87.9%)
0.100 [ 0.040, 0.159]
C6-C7 88/113 (77.9%) 74/91 (81.3%) -0.034 [-0.146, 0.077] 99/113 (87.6%) 80/91 (87.9%) -0.003 [-0.094, 0.088]
#Including all adverse events that happened during the IDE study and the PAS study.
*Confidence Limits for the proportion difference are derived by using the Farrington-Manning method.
Table 12 lists the brief definition of each category of adverse events.
Page 13

Table 12: Adverse Event Categories
Adverse Event Category Definition
Anatomical/Technical Difficulty Intraoperative (or perioperative) difficulty due to the patient’s physical structure
or due to a technical problem during the study surgery.
Cancer A malignancy or malignant tumor/neoplasm
Cardiovascular (i.e. MI, Stroke) Any condition of the heart and heart related vessels with exception of injury
sustained during study surgery.
Carpal Tunnel Syndrome Condition in which there is soreness, tenderness, and weakness of the muscles
of the thumb caused by pressure on the medial nerve at the point at which it
goes through the carpal tunnel of the wrist.
Death Termination of life due to any cause.
Dysphagia/Dysphonia Difficulty in swallowing or speaking; including hoarseness or voice disorders.
Gastrointestinal Condition pertaining to the entire alimentary system including the mouth,
esophagus, stomach, small intestine, large intestine, rectum, and anus.
Conditions involving the liver, gall bladder, bile duct, and pancreas are also
included in this category.
Implant Displacement/Loosening Incomplete or partial dislocation of the implant, wear around the implant,
loosening of the implant surface, or breakage of any implant or implant
component.
Spinal Event Event involving diagnoses at one or more spine levels; usually confirmed via
radiologic findings.
Infection An infection regardless of pathogen, which may or may not be confirmed by
culture or laboratory test.
Neck and/or Arm Pain Pain involving the neck, arm, or neck and arm, such events may include
discomfort and spams in these regions, but does not include neurological
symptoms.
Neurological Event that involves a feeling or awareness of condition within the body resulting
from stimulation of sensory receptors or involves stimulation of the motor
neurons that induce movements, as nerves or muscles.
Non-Union Failure of the vertebral bodies to fuse at the treated level and more than likely
required surgical intervention. This applies to the control group only.
Non-Union Outcome Pending Delay in the vertebral bodies to fuse at the treated level or fusion outcome
unknown. More than likely did not require surgical intervention. This applies to
the control group only.
Other Event not associated with any other categories (e.g., weight loss, tinnitus,
substance abuse, insomnia).
Other Pain Pain (including stiffness, strain, tightness) in an area that is not of the cervical
spine region.
Respiratory Ailments or symptoms associated with respiration or the respiratory system.
Subsidence Sinking or settling of the artificial disc into the vertebral body.
Trauma Physical injury caused by a physical force or traumatic event (or damage
inflicted on the body as the direct result or indirect result of an external force
(e.g. motor vehicle accident, fall, etc.).
Urogenital Event related to or affecting the organs or functions of excretion and
reproduction. Note: Urinary tract infections are captured under Infection.
Vascular Injury Intra-OP Injury to a vascular structure that is sustained during the course of the operative
procedure; initial study surgery only.
Subsequent Surgical Interventions
Table 13 summarizes the secondary surgical interventions in the PRESTIGE™ and control treatment groups that occurred up to
the 24-month visit and up to 84-month visit. Revisions, removals, and supplemental fixations were considered second surgery
failures in the clinical study. Table 13 also presents the statistical comparison of secondary surgeries between the PRESTIGE™
and control treatment groups. The rate of patients who had any secondary surgery at the target level were significantly less in
the investigational group up to 24-month visit and up to 84-month visit. Similar trend was observed in the following categories:
revisions and elective removal.
Page 14

Table 13: Secondary Surgical Procedures
Secondary Surgeries Up to 24 Months Secondary Surgeries Up to 84 Months
Treatment
Revisions 0 4 0.038 0.038 0 5 0.019 0.020
Removal 6 8 0.446 0.407 8 8 0.808 0.604
Removal - Elective 0 4 0.032 0.032 0 13 <0.001 <0.001
Supplemental Fixations 0 3 0.065 0.065 0 5 0.017 0.017
Re-operations 4 2 0.483 0.485 4 4 0.894 0.843
Total Patients Who Had Any Second Surgery at the Treated Level 9 19 0.025 0.022 11 29 <0.001 <0.001
Number of patients
Inv
(N=276)
Ctrl
(N=265)
P-Value
(Inv vs Ctrl)
Log-Rank Wilcoxon
Number of patients
Inv
(N=276)
(N=265)
Ctrl
P-Value
(Inv vs Ctrl)
Log-Rank Wilcoxon
Table 14: Secondary Surgical Interventions at the Index Level – Procedure Details
Days To
Index
Level
Surgery
Time To
Index Level
Surgery
Group Cause/Adverse Event Action
Investigational Right shoulder pain / C5
radiculopathy
C4-C5 decompressive
foraminotomy
Investigational Neck pain with headaches C6-C7 explant of PRESTIGE™
Secondary
Surgical
Intervention
Category
Re-Operation 57 6 Weeks
Removal 261 6 Months
Cervical Disc followed by ACDF
Investigational Left arm pain and
Cervical foraminotomy Re-Operation 289 12 Months
paresthesia into forearm and
hand; left cervical
radiculopathy
Investigational Neck / shoulder arm pain /
decreased sensation in little
finger
Investigational Radiating arm pain C5-C6 posterior foraminotomy,
C6-C7 explant of PRESTIGE™
Cervical Disc followed by C5-C7
ACDF
Removal 303 12 Months
Re-Operation 336 12 Months
discectomy, and nerve root
exploration
Investigational C8 radiculopathy C6-C7 explant of PRESTIGE™
Removal 438 12 Months
Cervical Disc followed by ACDF
Investigational Motor Vehicle Accident C5-C6 posterior cervical
Re-Operation 455 12 Months
laminectomy
Investigational Radiating arm pain C5-C6 explant of PRESTIGE™
Removal 508 12 Months
Cervical Disc followed by removal
of osteophytes and C5-C6
segmental fixation
Investigational C6 nerve root blunting and
facet disease secondary to
baseball injury
Investigational Left side radiculopathy C5-C6 explant of PRESTIGE™
C5-C6 explant of PRESTIGE™
Cervical Disc Followed by C5-C7
ACDF
Removal 786 24 Months
Removal 833 24 Months
Cervical Disc
Investigational Numbness and tingling, left
arm; C4-C5, C6-C7 annular
tears
Investigational Broken screws inferior to the
artificial disc in the C6
vertebral body
C5-C6 explant of PRESTIGE™
Cervical Disc followed by C4-C7
ACDF
C5-C6 explant of PRESTIGE™
Cervical Disc followed by anterior
and posterior fusion
Removal 1095 36 Months
Removal 2564 84 Months
Control Residual foraminal stenosis Left foraminotomy Revision 2 1 day - <4
weeks
Control Deltoid weakness, left C5 posterior foraminotomy Re-Operation 43 6 Weeks
Control Esophageal abscess C5-C6 removal of cervical plate
Removal 63 3 Months
and allograft, debridement of
esophageal abscess, and
esophageal fistula repair
Control HNP At C5-C6 C6-C7 removal of cervical plate
Revision 88 3 Months
followed by C5-C7 ACDF with two
level plate
Page 15

Table 14: Secondary Surgical Interventions at the Index Level – Procedure Details (continued)
Days To
Index
Level
Surgery
Time To
Index Level
Surgery
Group Cause/Adverse Event Action
Control C7 pain and numbness C5-C7 fusion with allograft and
Secondary
Surgical
Intervention
Category
Revision 98 3 Months
anterior plate
Control Adjacent level disc herniation C5-C7 discectomy and fusion Revision 140 3 Months
Control Fusion has not yet fused Bone Growth Stimulator Supplemental
183 6 Months
Fixation - External
Bone Growth
Stimulator
Control Patient with continued neck
and arm pain
Bone Growth Stimulator Supplemental
Fixation - External
185 6 Months
Bone Growth
Stimulator
Control Pseudoarthrosis Bone Growth Stimulator Supplemental
207 6 Months
Fixation - External
Bone Growth
Stimulator
Control Neck pain, headaches and
dizziness
C5-C6 removal of cervical plate
and allograft followed by graft,
Removal 241 6 Months
BMP, and plate
Control Posterior cervical region/
trapezius pain/spasm;
bilateral arm pain
Control C7 pain and numbness Bone Growth Stimulator Supplemental
C5-C6 removal of cervical plate
and allograft; ACDF with iliac crest
and stem cells
Removal 272 6 Months
278 12 Months
Fixation - External
Bone Growth
Stimulator
Control Patient with continued neck
and arm pain
C5-C6 removal of cervical plate
and allograft followed by C5-C6
Removal 284 12 Months
cervical fusion with graft, BMP and
plate
Control Pseudoarthrosis C5-C6 removal of cervical plate
Removal 293 12 Months
and allograft followed by cervical
fusion with autograft and plate
Control C7 pain and numbness C5-C6 removal of cervical plate
Removal 326 12 Months
followed by C5-C7 revision
arthrodesis with graft and plate
Control Pseudoarthrosis External Bone Growth Stimulator Supplemental
352 12 Months
Fixation - External
Bone Growth
Stimulator
Control Neck and shoulder pain Bone Growth Stimulator Supplemental
372 12 Months
Fixation - External
Bone Growth
Stimulator
Control Neck pain with right posterior
scapular pain
Control Neck and shoulder pain C6-C7 removal of cervical plate
C6-C7 removal of cervical plate to
facilitate a C5-C6 ACDF
Removal -
385 12 Months
Elective
Removal 399 12 Months
and allograft followed by C4-C7
anterior cervical fusion with graft,
BMP, and plate
Control Degenerative changes C6-
C7; C5-C6 lucency;
remodeling at C5-C6
C5-C6 removal of cervical plate
(elective) followed by C6-C7
cervical discectomy and fusion
Removal -
Elective
407 12 Months
anteriorly; facet inflammatory
changes C5-C6; foraminal
bony encroachments at C6C7 and C5-C6
Page 16

Table 14: Secondary Surgical Interventions at the Index Level – Procedure Details (continued)
Secondary
Group Cause/Adverse Event Action
Surgical
Intervention
Category
Control Chronic C6-C7
radiculopathy, C4-C5 mild
C5-C6 posterior cervical fusion
with screws and rods
Supplemental
Fixation
spondylosis, foraminal
narrowing and left arm pain
Control Involuntary thumb/torso
movements
Control Neck pain, glenohumeral
joint, cervical spondylosis
C4, C5, C6, C7, and T1 cervical
laminectomy
C5-C6 removal of anterior cervical
plate; exploration of C5-C6 fusion;
Re-Operation 506 12 Months
Removal -
Elective
C6-C7 ACDF with C5-C7
instrumentation
Control C7 pain and numbness C5-C7 posterior fusion with plating Supplemental
Fixation
Control Pseudoarthrosis C5-C6 posterior lateral cervical
fusion
Control C6-C7 incomplete fusion;
neck pain with headaches
C6-C7 removal of cervical plate
followed by C5-C6 ACDF
Control Lucency C5-C6 removal of cervical plate
Supplemental
Fixation
Removal -
Elective
Removal 840 24 Months
followed by C5-C6 anterior cervical
discectomy with allograft and plate
Control C6-C7 incomplete fusion;
neck pain with headaches
C5-C6, C6-C7 right foraminotomies
with C6-C7 nerve root
Revision 1050 36 Months
decompression
Control Neck and shoulder pain C6-C7 posterior fusion with BMP
and posterior instrumentation
Control Neck pain radiating to right
shoulder/arm due to motor
C5-C6 removal of cervical plate
followed by C6-C7 ACDF with plate
Supplemental
Fixation
Removal -
Elective
vehicle accident, small right
posterior osteophytes with
cord edema at C6-C7, right
HNP with moderate spinal
stenosis
Control C6-C7 pseudoarthrosis;
resorption of graft
Control C6-C7 pseudoarthrosis;
resorption of graft
C6-C7 posterior fusion with BMP Supplemental
Fixation
Bone Growth Stimulator Supplemental
Fixation - External
Bone Growth
Stimulator
Control C6-C7 herniation, foramen
impingement, osteophyte
compression
C5-C6 removal of cervical plate,
C6-C7 anterior discectomy and
osteophytectomy with anterior
Removal -
Elective
interbody fusion and plating
Control Neck and left arm pain C5-C6 removal of cervical plate,
C6-C7 foraminotomy with
Removal -
Elective
arthrodesis instrumentation
Control C3-C4 severe spondylitic
changes with bilateral
C5-C6 removal of cervical plate;
C3-C4 and C4-C5 ACDF
Removal -
Elective
spurring, left paracentral disc
osteophytes complex,
bilateral foraminal
encroachment, and C4-C5
severe spondylitic changes
Control C4, C5, and C6 foraminal
stenosis; C5-C6 herniation
C6-C7 removal of cervical plate
followed by C5-C6 discectomy with
Removal -
Elective
anterior plating
Control Degenerative changes at C5-
C6 with possible small disc
C5-C7 removal of cervical plate
followed by C5-C6 ACDF with
Removal -
Elective
cervical plate
Days To
Index
Level
Surgery
Time To
Index Level
Surgery
474 12 Months
513 12 Months
525 12 Months
613 24 Months
756 24 Months
1094 36 Months
1211 36 Months
1259 36 Months
1391 48 Months
1512 48 Months
1560 48 Months
1665 60 Months
1679 60 Months
1729 60 Months
Page 17

Table 14: Secondary Surgical Interventions at the Index Level – Procedure Details (continued)
Days To
Index
Level
Surgery
1806 60 Months
2242 72 Months
2425 84 Months
Time To
Index Level
Surgery
Group Cause/Adverse Event Action
protrusion, osteophytes at
C5-C6
Control Shallow protrusion and
hypertrophy at C3-C4, mild
stenosis and protrusion at
C5-C6, adjacent segment
degeneration at C5-C6
Control C6-C7 spondylosis; C6-C7
disc bulge; C4 spondylosis
Control Osteophytosis and
arthropathy C5
Control Right C6 radiculopathy and
foraminal narrowing at C6-C7
Control Epidural abscess C5-C6 laminectomy with
Revision of cervical fusion Removal -
C5-C6 removal of cervical plate
with placement of artificial cervical
disc
C6-C7 removal of cervical plate
and local bone followed by C5-C6
ACDF
C5-C6 anterolateral foraminotomy,
right
evacuation of epidural abscess
Secondary
Surgical
Intervention
Category
Elective
Removal -
Elective
Removal -
Elective
Re-Operation 2486 84 Months
Re-Operation 2514 84 Months
Explant Analysis Findings
The histology analysis of the peri-prosthetic tissue demonstrated metallosis, metallic debris, and corrosion products with an
attendant mild to moderate chronic inflammatory host response. However, none of the tissue samples from any of the
accessions showed histologic evidence of muscle attachment destruction, nerve damage, bone resorption, osteolysis, eryptosis,
pseudo-tumors, or lymphocytic masses.
Metal Ion Analysis
Implanted metal alloys release metallic ions into the body (especially those devices with metal-on-metal articulating surfaces). In
a prospective, longitudinal study of 25 subjects examining serum chromium (Cr) and nickel (Ni) concentrations in subjects
implanted with PRESTIGE™ Cervical Disc, the median Cr and Ni concentrations observed at pre-op were 0.07 ng/mL Cr and
0.09 ng/mL Ni and at 84 months were 0.20 ng/mL and 0.19 ng/mL, respectively. The maximum concentrations observed in
these patients was <2.0 ng/ml for chromium and <1.1 ng/ml for nickel. A review of adverse events for subjects implanted with
the PRESTIGE™ Cervical Disc did not reveal any signs or symptoms suggestive of systemic metal toxicity.
Neurological Status
Table 15 below shows the distributions of patients in the two treatment groups whose postoperative neurological condition was
either maintained or improved for the three functions assessed (i.e., motor function, sensory function, and reflexes). The overall
neurological success rates were high for both groups. The overall neurological success rates at all postoperative time periods
are greater than or equal to 88.2% for investigational group and greater than or equal to 79.7% in the control group, which are
the neurological success rates that were observed at 84 months postoperatively. Similar results were observed at all postoperative time points. Non-inferiority of the investigational group was achieved for overall neurological success at all time-points
including 24-month visit and 84-month. Superiority of the investigation group was achieved for overall neurological success in
six of the eight established time points (3, 12, 24, 36, 60 and 84 months, with the exception of six weeks and six months).
Table 15: Summary of Success Rates of Neurological Status
p-
value
ime Point Variable Inv
T
(N= 276)
6 weeks Motor 264 (96.7%) 242 (95.3%) <0.001 0.201
Sensory 257 (94.1%) 239 (94.1%) <0.001 0.491
Reflexes 265 (97.4%) 240 (94.5%) <0.001 0.043
Overall 245 (90.1%) 222 (87.4%) <0.001 0.166
3 Months Motor 249 (97.3%) 232 (96.3%) <0.001 0.264
Sensory 240 (93.8%) 223 (92.5%) <0.001 0.295
Reflexes 250 (98.0%) 229 (95.0%) <0.001 0.032
Overall 235 (91.8%) 210 (87.1%) <0.001 0.045
6 Months Motor 251 (97.7%) 222 (97.4%) <0.001 0.417
Sensory 245 (95.3%) 215 (94.3%) <0.001 0.304
Reflexes 250 (97.3%) 221 (96.9%) <0.001 0.410
Ctrl
(N= 265)
Non-inferiority
(d=0.1)
Superiority
Page 18

Table 15: Summary of Success Rates of Neurological Status (continued)
p-
value
ime Point Variable Inv
T
(N= 276)
Overall 238 (92.6%) 205 (89.9%) <0.001 0.146
12 Months Motor 262 (99.2%) 216 (95.6%) <0.001 0.004
Sensory 249 (94.3%) 203 (89.8%) <0.001 0.032
Reflexes 259 (98.1%) 215 (95.1%) <0.001 0.032
Overall 245 (92.8%) 194 (85.8%) <0.001 0.006
24 Months Motor 244 (97.2%) 209 (95.0%) <0.001 0.106
Sensory 237 (94.4%) 195 (88.6%) <0.001 0.012
Reflexes 246 (98.0%) 209 (95.0%) <0.001 0.036
Overall 230 (91.6%) 184 (83.6%) <0.001 0.004
36 Months Motor 194 (98.5%) 151 (93.8%) <0.001 0.009
Sensory 189 (95.9%) 139 (86.3%) <0.001 <0.001
Reflexes 190 (96.4%) 153 (95.0%) <0.001 0.253
Overall 182 (92.4%) 134 (83.2%) <0.001 0.004
60 Months Motor 217 (99.1%) 185 (97.9%) <0.001 0.157
Sensory 210 (95.9%) 171 (90.5%) <0.001 0.014
Reflexes 210 (95.9%) 175 (92.6%) <0.001 0.075
Overall 202 (92.2%) 162 (85.7%) <0.001 0.017
84 Months Motor 205 (97.2%) 174 (95.6%) <0.001 0.204
Sensory 195 (92.4%) 158 (86.8%) <0.001 0.033
Reflexes 201 (95.3%) 163 (89.6%) <0.001 0.016
Overall 186 (88.2%) 145 (79.7%) <0.001 0.011
Ctrl
(N= 265)
Non-inferiority
(d=0.1)
Superiority
Effectiveness Results
Primary Effectiveness Analysis
The primary endpoint was determined at 24 months (for the IDE) and 84 months (for the PAS) as a composite of the following
parameters: pain and functional disability, neurological status, adverse events, secondary surgical interventions, and a
radiographic spinal unit height determination. This was termed overall success.
Individual subject success (i.e. overall success) was defined as attainment of all of the following:
1. An improvement of at least 15 points from the baseline Neck Disability Index (NDI) score;
2. Maintenance or improvement in neurological status;
3. No serious adverse event classified as implant-associated or implant/surgical procedure-associated;
4. No additional surgical procedure classified as “Failure”; and
5. Functional spinal unit (FSU) height maintenance. FSU height was considered maintained if it did not decrease more than 2
mm after 6 weeks following surgery.
Because of difficulty in evaluating FSU, due to anatomical interference with the radiographic image, an alternative overall
success determination was made based on the above criteria without the addition of functional spinal unit (FSU) height
maintenance.
Overall Success Summary
Table 16 below presents the observed success rates for each group and the p-values of the non-inferiority and superiority of the
investigational group over the control group for individual outcome parameters and overall success at 24-month visit and 84month visit. The p-value values were calculated using the z-test of the normal approximation to the binomial distributions with
the standard error derived using Farrington and Manning Method. Non-inferiority of the PRESTIGE™ group to the control group
was demonstrated for all endpoints listed in Table 16 at both 24 and 84 months. Statistical superiority of the PRESTIGE™
group to the control group was also demonstrated for overall success (both with and without the FSU height component) and
the neurological variable at both 24 and 84 months. The NDI and FSU components were not found to be statistically superior in
the PRESTIGE™ group at the 24 month or 84 month time points.
Page 19

Table 16: Statistical Comparison of Overall Success and Its Components
24 Months 84 Months
Inv Ctrl P-Value Inv Ctrl P-Value
Primary
Outcome
Variable
Observed
Rate
(95%
Confidence
Interval)
NDI Success 82.2%
(76.9%,
86.7%)
Neurological
Success
91.6%
(87.5%,
94.8%)
FSU Height
Success
97.4%
(94.0%,
99.1%)
Overall
Success
(without FSU)
Overall
Success
(with FSU)
77.7%
(72.0%,
82.7%)
77.8%
(71.2%,
83.5%)
Observed
Rate
(95%
Confidence
Interval)
80.8%
(75.0%,
85.8%)
83.6%
(78.1%,
88.3%)
95.1%
(90.6%,
97.9%)
67.7%
(61.1%,
73.9%)
63.9%
(56.2%,
71.1%)
Observed
Non-
Inferiority
Superiority
Rate
(95%
Confidence
Interval)
< 0.001 0.349 84.8%
(79.3%,
89.4%)
< 0.001 0.004 88.2%
(83.0%,
92.2%)
< 0.001 0.131 95.8%
(91.5%,
98.3%)
< 0.001 0.008 75.0%
(68.6%,
80.7%)
< 0.001 0.002 72.6%
(65.2%,
79
.2%)
Observed
Rate
(95%
Confidence
Interval)
80.1%
(73.5%,
85.7%)
79.7%
(73.1%,
85.3%)
96.9%
(92.1%,
99.1%)
63.7%
(56.3%,
70.7%)
60.0%
(51.2%,
68.3%)
The number of patients with primary outcome variable data at 24 and 84 months are listed in Table 17.
Non-
Inferiority
Superiority
< 0.001 0.109
< 0.001 0.011
< 0.001 0.683
< 0.001 0.008
< 0.001 0.010
Table 17: Patient Data Available for Overall Success and Its Components
24 Months 84 Months
Primary Outcome Variable
Inv Ctrl Inv Ctrl
NDI 253 219 211 181
Neurological 251 220 211 162
FSU Height 190 164 166 127
Overall Success (without FSU)* 251 220 212 182
Overall Success (with FSU)* 189 169 168 135
*If a patient failed based on either a second surgery or serious, possibly implant- or implant/surgical procedure-associated adverse event, the patient was
counted as an Overall Success failure and included in the analysis, regardless of whether or not they had the FSU measurement, NDI score, or neurological
outcome.
A time course of overall success for both treatment groups is shown in Table 18.
Table 18: Time Course of Observed Success Rates
Variables Cohort 3 Mo 6 Mo 12 Mo 24 Mo 36 Mo 60 Mo 84 Mo
NDI Inv (N=276) 219/253
Ctrl (N=265) 174/235
Neurological Inv (N=276) 235/256
Ctrl (N=265) 210/241
FSU Height Inv (N=276) 200/200
Ctrl (N=265) 182/182
Overall Success
(without FSU)*
Overall Success
(with FSU)*
Inv (N=276) 207/254
Ctrl (N=265) 154/239
Inv (N=276) 163/197
Ctrl (N=265) 113/181
(86.6%)
(74.0%)
(91.8%)
(87.1%)
(100.0%)
(100.0%)
(81.5%)
(64.4%)
(82.7%)
(62.4%)
IDE PAS
210/257
(81.7%)
173/224
(77.2%)
238/257
(92.6%)
205/228
(89.9%)
199/200
(99.5%)
174/175
(99.4%)
197/256
(77.0%)
159/224
(71.0%)
150/196
(76.5%)
119/172
(69.2%)
217/263
(82.5%)
176/222
(79.3%)
245/264
(92.8%)
194/226
(85.8%)
202/205
(98.5%)
164/172
(95.3%)
204/263
(77.6%)
151/223
(67.7%)
157/204
(77.0%)
110/172
(64.0%)
208/253
(82.2%)
177/219
(80.8%)
230/251
(91.6%)
184/220
(83.6%)
185/190
(97.4%)
156/164
(95.1%)
195/251
(77.7%)
149/220
(67.7%)
147/189
(77.8%)
108/169
(63.9%)
163/197
(82.7%)
127/159
(79.9%)
182/197
(92.4%)
134/161
(83.2%)
143/148
(96.6%)
118/120
(98.3%)
154/198
(77.8%)
105/160
(65.6%)
114/150
(76.0%)
81/124
(65.3%)
187/219
(85.4%)
156/187
(83.4%)
202/219
(92.2%)
162/189
(85.7%)
153/165
(92.7%)
128/134
(95.5%)
172/220
(78.2%)
135/188
(71.8%)
119/167
(71.3%)
90/138
(65.2%)
179/211
(84.8%)
145/181
(80.1%)
186/211
(88.2%)
145/182
(79.7%)
159/166
(95.8%)
123/127
(96.9%)
159/212
(75.0%)
116/182
(63.7%)
122/168
(72.6%)
81/135
(60.0%)
Table 19 provides overall success for both treatment groups stratified by the treated level including post-hoc statistical analysis
and comparisons between the groups for each level.
Page 20

Table 19: Overall Success by Treated Level
24 Months 84 Months
Observed Rate
(95% Confidence
Interval)
50.0%
(15.7%, 84.3%)
80.0%
(28.4%, 99.5%)
54.5%
(23.4%, 83.3%)
50.0%
(18.7%, 81.3%)
68.8%
(59.9%, 76.8%)
63.7%
(54.1%, 72.6%)
69.7%
(58.1%, 79.8%)
65.9%
(49.4%, 79.9%)
Non-Inferiority Superiority Observed Rate
0.355 0.500 75.0%
0.636 0.755 33.3%
0.003 0.013 75.0%
0.007 0.029 75.0%
0.008 0.250 69.7%
<0.001 0.046 69.7%
<0.001 0.014 81.6%
<0.001 0.015 79.6%
(95% Confidence
Interval)
(19.4%, 99.4%)
(0.8%, 90.6%)
(42.8%, 94.5%)
(42.8%, 94.5%)
(60.2%, 78.2%)
(59.6%, 78.5%)
(71.9%, 89.1%)
(66.5%, 89.4%)
Observed Rate
(95% Confidence
(8.5%, 75.5%)
(11.8%, 88.2%)
(26.2%, 87.8%)
(9.9%, 81.6%)
(50.0%, 69.4%)
(44.7%, 66.3%)
(61.6%, 85.0%)
(58.8%, 89.3%)
Interval)
37.5%
50.0%
60.0%
42.9%
60.0%
55.7%
74.6%
76.5%
Non-Inferiority Superiority
0.059 0.110
0.576 0.682
0.104 0.226
0.031 0.081
0.001 0.068
<0.001 0.024
0.006 0.154
0.067 0.363
Levels Treated Primary Outcome
C3-C4 Overall Success
C4-C5 Overall Success
C5-C6 Overall Success
C6-C7 Overall Success
Variable
(without FSU)
Overall Success
(with FSU)
(without FSU)
Overall Success
(with FSU)
(without FSU)
Overall Success
(with FSU)
(without FSU)
Overall Success
(with FSU)
Inv Ctrl P-Value Inv Ctrl P-Value
Observed Rate
(95% Confidence
Interval)
50.0%
(11.8%, 88.2%)
60.0%
(14.7%, 94.7%)
92.9%
(66.1%, 99.8%)
85.7%
(57.2%, 98.2%)
72.7%
(64.1%, 80.2%)
74.1%
(65.0%, 81.9%)
83.5%
(74.9%, 90.1%)
84.5%
(72.6%, 92.7%)
Sensitivity Analyses
To assess the impact of lost to follow-up at 84-month visits, which includes the slightly unbalanced distribution of some baseline
variables and the overall success status at 24 months among the subjects with 84-month follow-up versus those without,
several sensitivity analyses were conducted. To assess the impact of slightly unbalanced distribution of some baseline
variables, propensity score analyses were conducted to adjust for any confounding effect of the demographic and prognostic
variables, regardless whether they were significantly different between the subjects who completed PAS versus those who did
not. Overall 32 variables, including the gender, worker’s comp and unresolved spinal litigation which show some imbalance
among the subjects with 84-month follow-up versus those without, were used to construct the propensity score for the two
treatment groups. The result shows that by the adjusting propensity score, most conclusions are consistent with the initial
results without adjustment. Table 20 shows the result of the overall success without FSU at 24 months and 84 months with the
propensity score adjustment and without adjustment, the conclusion of non-inferiority and superiority for overall success without
FSU are consistent using these two different methods. The same conclusion holds for the overall success with FSU and the
component of the primary endpoint as well.
Table 20: Overall Success without FSU at 24 Months and 84 Months with/without Propensity Score Adjustment
Observed Rate P-Value
Investigational Control Non-Inferiority Superiority
Overall success at 24 Months
(without FSU)
Overall success at 84 Months
(without FSU)
Without Propensity Score Adjustment 77.7% 67.7% <0.001 0.008
With Propensity Score Adjustment 77.7% 67.7% <0.001 0.004
Without Propensity Score Adjustment 75.0% 63.7% <0.001 0.008
With Propensity Score Adjustment 75.0% 63.7% <0.001 0.017
In addition, to assess the slightly unbalanced distribution of the overall success status at 24 months among the subjects with 84month follow-up versus those without, several sensitivity analyses, including “Missing = Failure”, “Missing = Success”, “Last
Observation Carried Forward (LOCF)” were performed to evaluate the impact of the missing data in the analysis of primary
endpoints. Table 21, using the overall success without FSU at 84 months as an example, shows that the conclusion remains
robust regardless of type of sensitivity analysis.
Table 21: Overall Success without FSU at 84 Months under Various Scenarios
Observed Overall Success
(without FSU)
Missing =
Failure
Missing =
Success
Overall Success
(without FSU)
Overall Success
(without FSU)
LOCF Overall Success
(without FSU)
Investigational Group
(N=276)
159/212
(75.0%)
159/276
(57.6%)
223/276
(80.8%)
201/284
(73.4%)
Control Group
(N=265)
116/182
(63.7%)
116/265
(43.8%)
164/265
(61.9%)
168/254
(66.1%)
P-value
(Non-inferiority)
< 0.001 0.008
< 0.001 < 0.001
< 0.001 0.055
< 0.001 0.035
P-value
(Superiority)
In addition, the tipping point analyses were conducted to further support the above conclusion. Again, using overall success
without FSU at 84-month as an example, the analyses shows that in order to reach the tipping point for the non-inferiority
conclusion, there must be at least 45 more control successes than investigational successes, which is dramatically biased in
favor of the control group. Additionally, in order to reach the superiority conclusion, there must be at least 18 more control
Page 21

successes than investigational success group, which is also biased in favor of the control group. Similar conclusion holds for
overall success with FSU at 84 months as well.
These analyses confirm that the overall study conclusion remains robust despite the slight unbalanced distribution of some
baseline variables and the overall success status at 24 months among the subjects with 84-month follow-up versus those
without.
Secondary Effectiveness Analysis
The secondary endpoints assessed were Neck Pain, Arm Pain, SF-36 Health Survey and, Gait Assessment while other
measurement include Foraminal Compression, Work Status, Patient Satisfaction, Radiographic, Global Perceived Effect, and
Doctor’s Perception. Table 22 describes the results of the secondary effectiveness endpoints and other measurements at 24
and 84 months.
Table 22: Secondary Endpoints and Other Measurements
IDE PAS
24-Month Observed Success Rate 84 -Month Observed Success Rate
Variable
Neck pain
Success
Failure
Arm pain
Success
Failure
SF-36 PCS
Success
Failure
SF-36 MCS
Success
Failure
Patient Perceived Effect
Success
Failure
Patient Satisfaction
Success
Failure
Doctor Perception
Success
Failure
Gait
Success
Failure
Work Status
Median days until return to work
Inv
(N=276)
241/253 (95.3%)
12/253 (4.7%)
231/253 (91.3%)
22/253 (8.7%)
210/248 (84.7%)
38/248 (15.3%)
169/248 (68.1%)
79/248 (31.9%)
236/252 (93.7%)
16/252 (6.3%)
222/252 (88.1%)
30/252 (11.9%)
233/251 (92.8%)
18/251 (7.2%)
247/251 (98.4%)
4/251 (1.6%)
45 Days 61 Days n/a
Ctrl
(N=265)
213/219 (97.3%)
6/219 (2.7%)
208/219 (95.0%)
11/219 (5.0%)
186/216 (86.1%)
30/216 (13.9%)
150/216 (69.4%)
66/216 (30.6%)
199/219 (90.9%)
20/219 (9.1%)
192/219 (87.7%)
27/219 (12.3%)
194/220 (88.2%)
26/220 (11.8%)
219/220 (99.5%)
1/220 (0.5%)
Inv
(N=276)
201/210 (95.7%)
9/210 (4.3%)
192/210 (91.4%)
18/210 (8.6%)
173/208 (83.2%)
35/208 (16.8%)
151/208 (72.6%)
57/208 (27.4%)
197/210 (93.8%)
13/210 (6.2%)
195/211 (92.4%)
16/211 (7.6%)
193/211 (91.5%)
18/211 (8.5%)
206/211 (97.6%)
5/211 (2.4%)
Ctrl
(N=265)
172/180 (95.6%)
8/180 (4.4%)
167/180 (92.8%)
13/180 (7.2%)
141/178 (79.2%)
37/178 (20.8%)
125/178 (70.2%)
53/178 (29.8%)
164/181 (90.6%)
17/181 (9.4%)
155/181 (85.6%)
26/181 (14.4%)
151/182 (83.0%)
31/182 (17.0%)
179/182 (98.4%)
3/181 (1.6%)
Radiographic Assessments
For patients receiving the PRESTIGE™ device, the mean angular motion values at 24 and 84 months postoperative,
respectively, were 7.73° (n=238) and 6.75° (n=206) as compared to a preoperative value of 7.55° (n=216). The range of motion
values measured from flexion/extension radiographs at 24 months and at 84 months for the PRESTIGE™ device patients are
presented in the histogram below.
Range of Motion
Overall, 206 subjects had range of motion data collected at 84 months, with 58 (28.2%) having a range of motion (ROM) ≤ 4°
and 148 (71.8%) have range of motion > 4°. The NDI, neck pain, arm pain, neurological, secondary surgery, serious associated
adverse events success status, ROM summary tables compared clinical endpoints between the investigational subjects with a
range of motion > 4° to those with a range of motion ≤ 4°. All of the data show that there is no significant difference between
these two subgroups at any time-point.
Additionally, Medtronic conducted a correlation analysis for the range of motion with NDI, neck pain and arm pain as continuous
variables. This analysis did not appear to show any correlation between range of motion and any of these variables at any time
point.
The following two figures show the ROM at 24-month and 84-month visits.
Page 22

Figure 1: Histogram of PRESTIGE™ Cervical Disc Angular Range of Motion at 24 Months
Number of Patients by ROM at 24 Months in Investigational Group
Number of Patients
Note: Parenthesis '(' or ')' indicates exclusive, and square bracket '[' or ']' indicates inclusive. For example, (1° -2°] means >1° and <=2°.
0=0°, 1=(0°-1°], 2=(1°-2°], 3=(2°-3°], 4=(3°-4°], 5=(4°-5°], 6=(5°-6°], 7=(6°-7°], 8=(7°-8°], 9= (8°-9°], 10=(9°-10°], 11=(10°-11°], 12=(11°-12°],
13=(12°-13°], 14=(13°-14°], 15=(14°-15°], 16=(15°-16°], 17=(16°-17°], 18=(17°-18°], 19=(18°-19°], 20=(19°-20°], 21=(20°-21°], 22=(21°-22°].
ROM
Figure 2: Histogram of PRESTIGE™ Cervical Disc Angular Range of Motion at 84 Months
Number of Patients by ROM at 84 Months in Investigational Group
Number of Patients
Note: Parenthesis '(' or ')' indicates exclusive, and square bracket '[' or ']' indicates inclusive. For example, (1° -2°] means >1° and <=2°.
0=0°, 1=(0°-1°], 2=(1°-2°], 3=(2°-3°], 4=(3°-4°], 5=(4°-5°], 6=(5°-6°], 7=(6°-7°], 8=(7°-8°], 9= (8°-9°], 10=(9°-10°], 11=(10°-11°], 12=(11°-12°],
13=(12°-13°], 14=(13°-14°], 15=(14°-15°], 16=(15°-16°], 17=(16°-17°], 18=(17°-18°], 19=(18°-19°], 20=(19°-20°], 21=(20°-21°], 22=(21°-22°].
ROM
Bridging Bone
Heterotopic ossification (HO) was not collected as a part of the IDE and post-approval study protocols. However, bridging bone
(an extreme scenario of HO) was assessed for the investigational subjects during the IDE and post-approval studies. Bridging
bone was defined as evidence of a continuous bony connection from the superior vertebral body to the inferior vertebral body
laterally, anteriorly, and/or posteriorly. The radiographic results are shown in Table 23. Two investigational patients were found
to have bridging bone at the 24-month time point while twenty investigational patients were found to have bridging bone at the
84-month time point.
Additional subgroup analyses at 84 months (20 investigational Patients with bridging bone versus 181 investigational patients
without bridging bone) were also conducted in order to determine whether bridging bone was correlated with clinical outcomes.
The analysis assessed the following clinical outcomes: NDI, Neck/Arm pain, and overall success. Data demonstrated that
patients with bridging bone had similar clinical outcomes when compared to patients without bridging bone at all time-points. In
conclusion, the study data suggests that bridging bone was not correlated with unwanted safety or effectiveness consequences
and was not linked to specific patient or surgical variables.
Table 23: Time Course of Bridging Bone
6 Weeks
3 Months
6 Months
12 Months
24 Months
Bridging Bone PRESTIGE Subjects
(N=276)
No 267 (100.0%)
Yes 0 (0.0%)
No 253 (100.0%)
Yes 0 (0.0%)
No 254 (99.6%)
Yes 1 (0.4%)
No 255 (98.5%)
Yes 4 (1.5%)
No 248 (99.2%)
Page 23

Table 23: Time Course of Bridging Bone (continued)
Bridging Bone PRESTIGE Subjects
(N=276)
Yes 2 (0.8%)
36 Months
60 Months
84 Months
No 183 (96.3%)
Yes 7 (3.7%)
No 196 (93.8%)
Yes 13 (6.2%)
No 181 (90.0%)
Yes 20 (10.0%)
Radiolucency
A post-hoc analysis of radiographic observations was conducted to assess for radiolucency. A total of 17 unique investigational
patients were found to have an observation of radiolucency and/or device loosening.
At 84 months post-operative, nine of the 17 identified radiolucency cases were considered mild, five moderate and only three
patients were scored as having severe radiolucency. Fourteen of these 17 patients were considered an overall success. Only
one case with observed radiolucency (and one of three severe radiolucency cases) was associated with a device removal.
However, this removal was associated with a traumatic event and inferior bone screw fracture. Histology findings for this patient
were similar to other explanted subjects (without observed radiolucency) with no acute inflammation, osteolysis, pseudotumor or
lymphatic masses observed. Therefore, trauma and device breakage (screw fracture) may be associated with this device
loosening, severe radiolucency adjacent to the device, and device removal.
Adjacent Segment Disease
Several biomechanical studies have shown increased pressure in the disc spaces adjacent to an anterior cervical fusion and
increased range of motion (ROM) in the adjacent discs. Disc disease and degeneration in general, however, are difficult to
measure and characterize. Therefore, the examination and comparison of additional surgeries at adjacent levels were of
primary interest for this post-approval study as mentioned in the protocol, because of their clinical significance.
Cumulatively up to the end of the post-approval study at the 84-month follow-up, 11 investigational patients (4.6%, life-table
estimate) underwent additional surgeries as shown in Table 24 and Table 25. During the same time frame, 24 control patients
(11.9%, life-table estimate) underwent additional surgeries at any level other than the index procedure. The difference was
statistically significant (p = 0.008; log-rank test). Figure 3 illustrates the time-to-event comparison between Investigational and
Control Groups for additional surgeries involved with other cervical levels over the study period.
Table 24: Subjects with Adjacent Level Surgical Treatment
Treatment
Any Adjacent Surgery Occurred in Cervical Region
Number of Patients
Inv Ctrl Inv Ctrl Log-Rank Wilcoxon
Up to 24 Months 4 11 1.5 4.6
Up to 84 Months 11 24 4.6 11.9
Cumulative Rate
(%)
P-value
(Inv vs Ctrl)
0.008 0.008
Additional non-surgical interventions or procedures were also compared between the treatment groups. The rate of any
intervention appeared to be lower in the Investigational Group (1.4% versus 5.3%) as compared to the Control Group and the
frequencies of facet injection, ESI, steroid injection, trigger point injection were all numerically lower in the investigational group.
Collectively, these data reflect long-term therapeutic advantage in favor of the investigational group.
Figure 3: Comparison of Time to Additional Surgery Involved with Adjacent Levels between Investigational and Control Groups
Treatment
Group
% Patients Who Had Secondary Surgeries Involved with Adjacent Levels
PRESTIGE® ST Control
Logrank=0.008
Months from Index Surgery to Second ary Surgery
Page 24

Table 25: Secondary Surgical Interventions at the Adjacent Level – Procedure Details
Group Patient ID
Investigational 1916 C6-C7
Investigational 1002 C6-C7 Herniated disc C5-C6 C5-C7 ACDF Other 368 12 Months
Investigational 1209 C5-C6 Motor Vehicle Accident C6-C7 microdiscectomy and fusion Other 510 12 Months
Investigational 3141 C5-C6
Investigational 307 C5-C6 Facet pain, cervical C4-C5 ACDF with PEEK and BMP Other 917 36 Months
Investigational 2802 C5-C6 Left side radiculopathy C3-C4 anterior, C6-C7 posterior instrumentation Other 1077 36 Months
Investigational 2858 C5-C6
Investigational 2802 C5-C6 Left side radiculopathy Removal of wires from surgery in May 2006 Other 1116 36 Months
Investigational 3144 C5-C6 C6-C7 disc disease and migraine headaches C6-C7 anterior cervical discectomy Other 1371 48 Months
Investigational 2855 C5-C6
Investigational 2802 C5-C6 Left side radiculopathy C3-C7 posterior fusion Other 1575 48 Months
Investigational 2807 C6-C7
Investigational 615 C4-C5
Investigational 3144 C5-C6 Suspected failed fusion at C6-C7 C6-C7 exploration and re-fusion Other 2150 72 Months
Investigational 2807 C6-C7 Numbness in fingers with neck and shoulder C5-C6 posterior cervical fusion Other 2215 72 Months
Investigational 615 C4-C5
Investigational 615 C4-C5
Investigational 615 C4-C5
Control 3310 C6-C7 HNP at C5-C6 C5-C7 ACDF with two level cervical plate Revision 88 3 Months
Control 2507 C5-C6 C7 pain and numbness C5-C7 fusion with allograft and anterior plate Revision 98 3 Months
Control 1713 C5-C6 Adjacent level disc herniation C5-C7 discectomy and fusion Revision 140 3 Months
Control 2507 C5-C6 C7 pain and numbness
Control 215 C6-C7 Neck pain with right posterior scapular pain C5-C6 ACDF Removal - Elective 385 12 Months
Control 2716 C6-C7 Neck and shoulder pain
Control 3117 C5-C6
Control 2915 C6-C7 C3-4 foraminal stenosis, C5-6 herniated disc Posterior cervical foraminotomy Other 482 12 Months
Control 608 C6-C7 Involuntary thumb/ torso movements C4, C5, C6, C7, and T1 cervical laminectomy Re-Operation 506 12 Months
Control 1112 C5-C6
Control 2507 C5-C6 C7 pain and numbness C5-C7 posterior fusion with plating
Control 226 C5-C6 Adjacent segment disease at C6-7 C6-C7 ACDF Other 550 12 Months
Control 235 C6-C7
Control 2507 C5-C6
Control 908 C5-C6 HNP C6-C7 C6-C7 ACDF Other 959 36 Months
Control 235 C6-C7
Control 1820 C6-C7 Headaches C3-C4 ACDF Other 1183 36 Months
Control 1914 C5-C6
Control 231 C5-C6
Control 1208 C5-C6 Neck and left arm pain
Control 528 C5-C6
Control 2918 C6-C7
Control 803 C6-C7
Control 219 C5-C6 Right-sided neck pain and shoulder pain
Control 539 C4-C5
Control 219 C5-C6 Right-sided neck pain and shoulder pain C3, C4, C5 right medial branch radiofrequency Other 1901 60 Months
Control 2507 C5-C6
Index Surgery
Level
Cause/Adverse Event Action
Neck / shoulder arm pain / decreased sensation
C6 nerve root blunting and facet disease
Numbness and tingling, left arm; C4-C5 / C6-C7
Cervical strain, C6-C7 subluxation, C4-C5/C6-C7
Pain in right arm, numbness in fingers with neck
Disc bulging and end plate spurring at C4-C5
Disc bulging and end plate spurring at C4-C5
Disc bulging and end plate spurring at C4-C5
Disc bulging and end plate spurring at C4-C5
Degenerative changes C6-C7; C5-C6 lucency;
remodeling at C5-C6 anteriorly; facet
inflammatory changes C5-C6; foraminal bony
encroachments at C6-C7 and C5-C6
Neck pain, glenohumeral joint, cervical
Incomplete fusion at C6-7; neck pain with
C3-C4 disc degeneration, C3-C4 bulging, C3-C4
Incomplete fusion at C6-7; neck pain with
Neck pain radiating to right shoulder/arm due to
motor vehicle accident, small right posterior
osteophytes with cord edema at C6-C7, right
HNP with moderate spinal stenosis
C6-C7 herniation, foramen impi ngement,
Severe spondylitic changes C3-C4 with bilateral
spurring, left paracentral disc osteophytes
complex, bilateral foraminal encroachment, and
severe spondylitic changes at C4-C5
Foraminal stenosis C4, C5 and C6; herniation at
Degenerative changes at C5-C6 with possible
small disc protrusion, osteophytes at C5-C6
Shallow protrusion and hypertrophy at C3-C4,
mild stenosis and protrusion at C5-C6, adjacent
C3-C4 disc degeneration, C3-C4 bulging, C3-C4
in little finger
secondary to baseball injury
annular tears
hypermobility
and shoulder
and C6-C7
and C6-C7
and C6-C7
and C6-C7
spondylosis
headaches
pseudoarthrosis
headaches
osteophyte compression
C5-C6
segment degeneration at C5-C6
pseudoarthrosis
C5-C7 ACDF Removal 303 12 Months
C5-C7 ACDF Removal 786 24 Months
C5-C6 explant of PRESTIGE™ cervical disc followed
C4-C5, C6-7 anterior cervical microdiscectomy and
C3-C6 radiofrequency of the median branch of the
C3-C5 radiofrequency of the median branch of the
C5-C7 radiofrequency of the median branch of the
C5-C7 radiofrequency of the medial branch of the
C5-C6 removal plate followed by C5-C7 revision
arthrodesis with autograft and cervical plate
C6-C7 removal of cervical plate and allograft followed
by C4-C7 anterior cervical fusion with BMP and plate
C5-C6 removal of cervical plate (elective) followed by
C5-C6 removal of anterior cervical plate; exploration
of C5-C6 fusion; C6-C7 ACDF using PEEK and BMP
C6-C7 removal of cervical plate followed by C5-C6
C5-C7 removal of plating, C4-C5 ACDF Other 846 24 Months
C5-C6, C6-C7 right foraminotomies with C6-C7 nerve
C5-C6 removal of cervical plate followed by C6-C7
C5-C6 removal of cervical plate, C6-C7 anterior
discectomy and osteophytectomy with anterior
C5-C6 removal of cervical plate, C6-C7 foraminotomy
C5-C6 removal of cervical plate; C3-C4 and C4-C5
C6-C7 removal of cervical plate followed by C5-C6
C5-C7 removal of cervical plate followed by C5-C6
C3, C4, C5 radiofrequency ablation of right sided
C4-C6 removal of anterior cervical plate followed by
by C4-C7 ACDF
placement of an artifical disc
C5-C6 discectomy and fusion Other 1694 60 Months
dorsal rami/cervical-right
dorsal rami/cervical-left
dorsal rami/cervical-right
dorsal rami/cervical-left
C6-C7 cervical discectomy and fusion
with instrumentation from C5 TO C7
ACDF
root decompression
ACDF with plate
interbody fusion and plating
with arthrodesis instrumentation
ACDF
discectomy with anterior plating
ACDF with Cervical plate
medial branch nerves
Revision of cervical fusion Removal - Elective 1806 60 Months
C3-C4 ACDF
Secondary
Surgical
Intervention
Category
Removal 1095 36 Months
Other 1546 48 Months
Other 1944 60 Months
Other 2260 72 Months
Other 2406 84 Months
Other 2446 84 Months
Removal 326 12 Months
Removal 399 12 Months
Removal - Elective 407 12 Months
Removal - Elective 513 12 Months
Supplemental
Fixation
Removal - Elective 756 24 Months
Revision 1050 36 Months
Removal - Elective 1211 36 Months
Removal - Elective 1512 48 Months
Removal - Elective 1560 48 Months
Removal - Elective 1665 60 Months
Removal - Elective 1679 60 Months
Removal - Elective 1729 60 Months
Other 1768 60 Months
Other 1959 60 Months
Days to
Adjacent
Level
Surgery
Time to Adjacent
Level Surgery
525 12 Months
Page 25

Table 25: Secondary Surgical Interventions at the Adjacent Level – Procedure Details (continued)
Group Patient ID
Control 1720 C5-C6
Control 219 C5-C6 Right-sided neck pain and shoulder pain C3, C4, C5 right medial branch radiofrequency Other 2062 72 Months
Control 2507 C5-C6
Control 2809 C5-C6
Control 219 C5-C6
Control 215 C6-C7
Control 2918 C6-C7
Control 1612 C6-C7 Osteophytosis and Arthropathy C5
Control 2918 C6-C7 Pre-vertebral abscess
Index Surgery
Level
Cause/Adverse Event Action
Chronic C6-C7 radiculopathy, C4-C5 mild
spondylosis and foraminal narrowing, neck and
C3-C4 disc degeneration, C3-C4 bulging, C3-C4
C6-C7 spondylosis; C6-C7 disc bulge; C4
Right-sided neck pain and shoulder painRight-
sided neck pain and shoulder pain
Foraminal narrowing C3-C4 and canal narrowing
Foraminal stenosis C4, C5 and C6; herniation at
chest pain
pseudoarthrosis
spondylosis
C4-C5
C5-C6
C5-C6 hardware removal and C6-C7 ACDF Other 1988 60 Months
C3-C4 anterior cervical discectomy, redo with internal
C5-C6 removal of cervical plate with placement of
C4 right hemilaminectomy; C4-C5 medial facetectomy
C6-C7 removal of cervical plate followed by C5-C6
C4-C5 drainage of possible abscess and removal of
fixation and iliac bone graft
artificial cervical disc
C3, C4, C5 right medial branch radiofrequency Other 2293 72 Months
and foraminotomy
C4-C5 anterior cervical discectomy with fusion Other 2423 84 Months
ACDF with interbody cage, plate, and local bone
plating
Secondary
Surgical
Intervention
Category
Other 2183 72 Months
Removal - Elective 2242 72 Months
Other 2401 84 Months
Removal - Elective 2425 84 Months
Other 2436 84 Months
Days to
Adjacent
Level
Surgery
Time to Adjacent
Level Surgery
Fusion Outcome Data
Ten patients were found to have had a device removal followed by fusion surgery at the target level. Of these patients, postfusion imaging data was available for only six of the patients. In those six patients, various degrees of bridging bone were
observed. The radiographic observations suggested that only one out of the six patients was judged as likely not fused, two out
of the six patients was judged as likely undetermined and three out of the six patients were judged as likely fused.
Conclusions Drawn from the Study Data
In summary, the overall success rate for the Investigational Group at 24 and 84 months was found to be not only statistically
non-inferior to the Control Group rate, but also superior, regardless of which definition of overall success was used. Therefore,
the primary clinical study objective was met, thus indicating that the PRESTIGE™ Cervical Disc System is as safe and effective
in the long term as the current standard of care for treating symptomatic cervical degenerative disc disease.
PACKAGING
Packages for each of the components should be intact upon receipt. If a loaner or consignment system is used, all sets should
be carefully checked for completeness and all components including instruments should be carefully checked to ensure that
there is no damage prior to use. Damaged packages or products should not be used, and should be returned to MEDTRONIC.
CLEANING AND DECONTAMINATION
Unless just removed from an unopened MEDTRONIC package, all instruments and implants must be disassembled (if
applicable) and cleaned using neutral cleaners before sterilization and introduction into a sterile surgical field or (if applicable)
return of the product to MEDTRONIC. Cleaning and disinfecting of instruments can be performed with aldehyde-free solvents at
higher temperatures. Cleaning and decontamination must include the use of neutral cleaners followed by a deionized water
rinse.
Note: certain cleaning solutions such as those containing formalin, glutaraldehyde, bleach and/or other alkaline cleaners may
damage some devices, particularly instruments; these solutions should
not be used. Also, many instruments require
disassembly before cleaning.
All products should be treated with care. Improper use or handling may lead to damage and/or possible improper functioning of
the device.
STERILIZATION
The contents of the implant package for the PRESTIGE™ Cervical Disc, including the superior and inferior disc components,
bone screws, and lock screws, are provided sterile via gamma irradiation. The contents of instrument sets are provided nonsterile.
Unless marked sterile and clearly labeled as such in an unopened sterile package provided by the company, all implants and
instruments used in surgery
Only sterile products should be placed in the operative field. Unless specified elsewhere, these products are recommended to
be steam sterilized by the hospital using one of the sets of process parameters below:
mustbe sterilized by the hospital prior to use. Remove all packaging materials prior to sterilization.
Table 26: Sterilization Parameters
METHOD CYCLE TEMPERATURE EXPOSURE TIME
Steam Pre-Vacuum 270°F (132°C) 4 Minutes
Steam Gravity 250°F (121°C) 60 Minutes
Steam* Pre-Vacuum* 273°F (134°C)* 20 Minutes*
Steam* Gravity* 273°F (134°C)* 20 Minutes*
Page 26

NOTE: Because of the many variables involved in sterilization, each medical facility should calibrate and verify the sterilization
process (e.g. temperatures, times) used for their equipment.
*For outside the United States, some non-U.S. Health Care Authorities recommend sterilization according to these parameters
so as to minimize the potential risk of transmission of Creutzfeldt-Jakob disease, especially of surgical instruments that could
come into contact with the central nervous system.
Remove all packaging material prior to sterilization. Only sterile implants and instruments should be used in surgery. No implant
should be re-used once it comes into contact with human tissue or body fluid. Always immediately clean and re-sterilize
instruments that have been used in surgery. This process must be performed before handling or (if applicable) returning to
MEDTRONIC.
CONFORMANCE TO STANDARDS
The PRESTIGE™ Cervical Disc is manufactured from type 316 stainless steel per ASTM F138.
PRODUCT COMPLAINTS
Any Health Care Professional (e.g., customer or user of this system of products), who has any complaints or who has
experienced any dissatisfaction in the product quality, identity, durability, reliability, safety, effectiveness and/or performance,
should notify the distributor or MEDTRONIC. Further, if any of the implanted spinal system component(s) ever “malfunctions,”
(i.e., does not meet any of its performance specifications or otherwise does not perform as intended), or is suspected of doing
so, the distributor should be notified immediately. If any MEDTRONIC product ever “malfunctions” and may have caused or
contributed to the death or serious injury of a patient, the distributor should be notified immediately by telephone, fax or written
correspondence. When filing a complaint, please provide the component(s) name and number, lot number(s), your name and
address, the nature of the complaint and notification of whether a written report from the distributor is requested. Complaints
may also be reported directly to Medwatch at http://
www.fda.gov/medwatch.
FURTHER INFORMATION
Recommended directions for use of this system (surgical operative techniques) are available at no charge upon request. If
further information is needed or required, please contact MEDTRONIC.
DEVICE RETRIEVALS
Should it be necessary to remove a PRESTIGE™ Cervical Disc device, please call MEDTRONIC prior to the scheduled surgery
for product/tissue retrieval information.
FOR US AUDIENCES ONLY
CAUTION: FEDERAL LAW (USA) RESTRICTS THESE DEVICES TO SALE BY OR ON THE ORDER OF A PHYSICIAN.
©2017 MEDTRONIC SOFAMOR DANEK. All rights reserved.
Page 27

Medtronic Sofamor Danek USA, Inc.
1800 Pyramid Place
Memphis, TN 38132
Telephone: 800 933 2635 (USA)
901 396 3133 (Outside USA)
Fax: 901 396 0356
DESCRIPTION OF DEVICE MARKINGS
Batch code
Catalogue number
CAUTION: Federal law (USA) restricts these devices to
sale by or on the order of a physician.
Consult instructions for use
Do not re-use
For US audiences only
The device complies with European Directive MDD
93/42/EEC
Medtronic B.V.
Earl Bakkenstraat 10
6422 PJ Heerlen
The Netherlands
Tel: + 31 45 566 80 00
Authorized representative in the European Community
Do not use if package is damaged
Manufacturer
Sterilized using irradiation
Use-by date
 Loading...
Loading...