Page 1

Page 2

Table of Contents
Introduction 3
Background 4
What are X rays? 4
How are X rays Generated? 4
Primary and Scatter Radiation 5
Interactions with Matter 5
Biological Eects of Radiation 6
Linear No-Threshold Risk Model 7
Basic X-ray Safety 7
Safety Rules to Minimize Radiation Dose 7
Worker Radiation Dose Limits 8
Medical Procedure Doses 8
MaxRay Safety 9
Backscatter Shield 9
Geometry of the Backscatter Zone 9
Dosimetry 11
Accidental Exposure Prevention 11
Exposure Time 13
Safe Storage 14
Cocoon Training Manual
Table of Contents
//
2
Page 3

Introduction
There are many beneficial uses of ionizing radiation; however, of equal importance we note that there
are potential risks associated with its use. Radiation safety training is an important part of any radiation safety program. Receiving appropriate training ensures users are following proper safety practices to maximize the benefits of ionizing radiation while minimizing potential risks and maintaining
a safe work environment.
In this training manual, we discuss basic X-ray safety in addition to specific safety information about
operating the MaxRay Cocoon. The Cocoon is a small, lightweight, handheld X-ray system meant for
dental radiology that is certified by the FDA and is completely safe when used as intended. All operators must read, and become familiar with, the User’s Manual associated with the Cocoon system.
The MaxRay Cocoon mobile X-ray system.
This handheld unit is to be operated only by authorized personnel. DO NOT operate the Cocoon in
any manner other than that specified herein, and in the User’s Manual. And, DO NOT allow anyone
other than trained and certified personnel to operate the Cocoon unit.
Cocoon Training Manual
Introduction
//
3
Page 4
Background
What are X rays?
X rays are a form of ionizing radiation and are a part of the electromagnetic spectrum. X rays are the
same as the light from the sun, except that their energy is much higher. As X rays travel through and
interact with various materials, human tissue for instance, they transfer energy to the atoms of that
material. This process of energy transfer can result in atomic ionization. X rays can penetrate certain
materials, but they can be blocked or shielded with high-density materials.
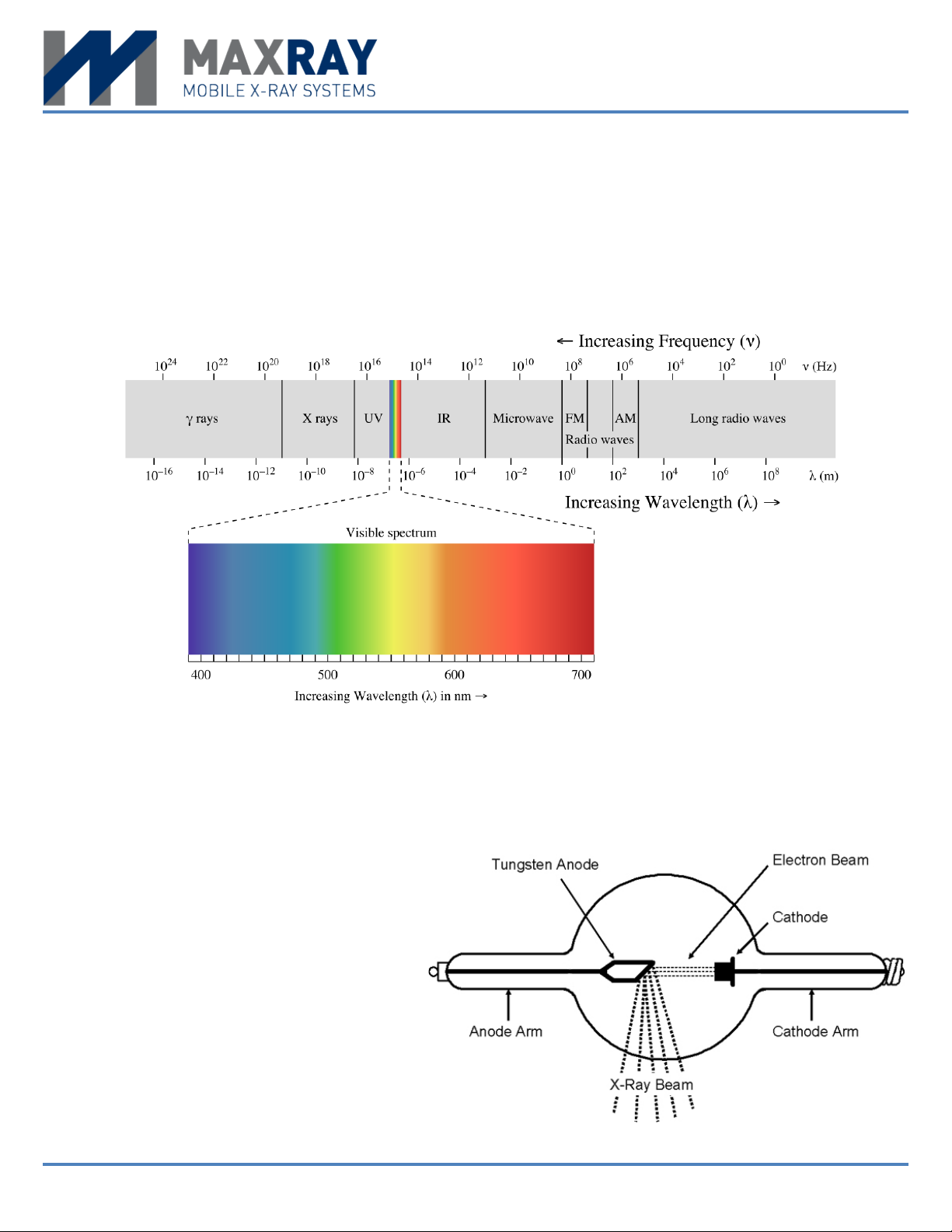
The electromagnetic spectrum.
When living systems are exposed to ionizing radiation there is a risk for biological damage to occur.
Exposure to X rays in the workplace, however, is highly regulated and current safety standards are
very eective at keeping risks to a minimum.
How are X rays Generated?
X rays are produced in a type of vacuum
tube specifically designed for that function. As power is applied to the tube, X
rays are emitted in a prescribe fashion
from a shielded housing.
Diagram of an X-ray tube.
Cocoon Training Manual
Background
//
4
Page 5

Generally, the three parameters that are usually adjusted by the X-ray technician (tube potential
(kVp), tube current (mA), and time (sec)) establish the characteristics of the X-ray beam emanating
from the tube. The tube potential determines the energy range of X rays and the tube current establishes the rate at which X rays are emitted. In the tube, X rays are produced by two means, Bremsstrahlung radiation and characteristic radiation. The two are described below.
Bremsstrahlung Radiation
This is the main type of radiation produced and occurs as the high energy electrons experience a
sudden slowing down, or “breaking”, at the anode target. A spectrum of photon energies is produced.
Bremsstrahlung is also known as “breaking radiation”.
Characteristic Radiation
This type of radiation is produced when an electron interacts with an inner shell electron of a target
atom of the anode. As the inner shell electron is displaced, an electron from an outer shell drops to
fill the vacancy. It is this process that releases characteristic X rays.
All X-ray tubes have some form of filtration, whether it be inherent to the design or added afterward
to adjust the usefulness of the X-ray beam. The X-ray housing will have additional shielding to minimize “leakage radiation” that can cause unwanted exposure to the technician.
Primary and Scatter Radiation
Once X rays leave the tube housing, they are categorized as primary or secondary radiation. Secondary radiation is further characterized into scatter radiation and leakage radiation.
Primary radiation
This type of radiation describes the useful beam of radiation that is produced in the tube and exits the
filtration window as designed. This is the radiation which is fundamental in producing the radiograph.
Continued exposure to the primary beam can result in a significant hazard.
Scatter radiation
This refers to the radiation that is scattered after the primary beam interacts with the patient. The patient is therefore the major source of scatter radiation. Even though the primary beam is much more
intense than scatter radiation, it is this scatter that is of primary concern when protecting the safety
of the worker.
As stated above, leakage radiation refers to radiation from the X-ray tube that penetrates the device
housing. Leakage is usually quite small relative to the primary beam and scatter.
Interactions with Matter
The interaction of X rays with matter is a random process. As tissue is exposed, the X rays may interact with the atoms of the material through which they pass. A small percentage of the X rays will pass
through matter without interacting.
Cocoon Training Manual
Background
//
5
Page 6

Those X rays that interact will do so by one of two methods, photoelectric absorption or Compton
scatter.
Photoelectric absorption
In photoelectric absorption, the incident X-ray energy is completely absorbed in the interaction medium (e.g., tissue) and the X ray is removed from the beam and does not have the ability to scatter.
Compton scatter
With Compton scatter, the incident X ray scatters in the interaction medium and only a partial amount
of original energy is absorbed. The remaining energy goes to the scattered X ray. This scattered energy is therefore available to be absorbed else where, for example, in the technician.
During the process of photoelectric absorption or Compton scatter, energy is transferred to the
interaction medium. We quantify the eect of this energy absorption using a parameter called “absorbed dose”, i.e., the amount of energy absorbed for a given mass of absorbing medium. Someone’s
risk from radiation exposure is directly proportional to the dose they receive. The regulatory agencies set limits on absorbed dose for workers and the general public to ensure that radiation risk is
kept as low as practical.
Biological Eects of Radiation
While X rays are an important part of the diagnostic process, it is important to be aware that there is
potential for biological damage to occur when exposed to ionizing radiation. Eorts should be made
to evaluate the benefit and potential risk in order to avoid unnecessary radiation exposure. The benefits of medical/dental evaluation using X-ray technology are obvious, but the biological eects of
ionizing radiation must be weighed against the benefits. These eects are commonly grouped into
two categories:
Non-stochastic Eects (deterministic eects)
Non-stochastic eects related to those that are non-random and are directly related to the radiation
dose received. For these eects to occur, a threshold dose must be met. Once the threshold has been
exceeded, the severity of biological damage (e.g., skin burns, hair loss, reddening of the skin, cataracts) increases with the dose received. These eects are seen only after exposure to large doses of
radiation (> 1,000 mSv), much larger than doses received when undergoing dental imaging.
Stochastic Eects (probabilistic eects)
Stochastic eects are randomly occurring and the severity of biological damage (e.g., cancer, birth
defects) is independent of the dose received. Since it is based on probability, the chance of occurrence increases with radiation exposure. Stochastic eects are of typical concerned when speaking of
exposure to diagnostic X rays; radiation dose is very small; therefore, the only real potential outcome
is the random chance of cancer.
Cocoon Training Manual
Background
//
6
Page 7

Linear No-Threshold Risk Model
Because the random chance of cancer is so small, science must use a small set of existing data to
predict cancer probability. Currently, the prediction is based on what’s called a “linear, no-threshold
model” and is intended to convey that cancer risk is thought to be proportional (linear) to dose, with
zero dose resulting in zero risk (no-threshold). This model is conservative and follows the philosophy
that it is better that risk be overestimated rather than underestimated.
Basic X-ray Safety
Safety Rules to Minimize Radiation Dose
ALARA. ALARA (As Low As Reasonably Achievable) is a safety principle that ensures radiation expo-
sure levels are kept as low as practical, far below the exposure limits set by the regulatory agencies.
It is a regulatory requirement and it is mandated that all radiation safety programs follow the ALARA
principle.
In order to maintain ALARA, it is important to remember and practice the radiation protection triad
of time, distance, and shielding:
• Time: minimize exposure time;
• Distance: maximize distance (between you and the source); and,
• Shielding: use appropriate radiation shielding.
The most eective shielding for X rays is lead. Patients should be shielded to protect their thyroid
and reproductive organs, and the X-ray technician should wear a leaded apron. Some of the handheld
X-ray systems come equipped with a leaded-plastic backscatter shield which is very eective. With
this shield, leaded aprons may not be required by your regulator, but it’s always a safe bet to wear
the apron anyway.
Cocoon Training Manual
Basic X-ray Safety
//
7
Page 8

Pregnancy. Because the fetus is undergoing rapid cell reproduction, it is important to reduce radiation exposure during pregnancy. As the X-ray operator, if you are, or become, pregnant, you should
notify your employer immediately. It is your responsibility to declare your pregnancy. For the safety
of your patients, you should question the patient regarding the possibility of them being pregnant.
If the patient is, or may be, pregnant, they should be advised by your radiation safety ocer prior to
exposure.
Medical Procedure Doses
Dental imaging procedures contribute to a
much lower patient dose than other imaging
studies. The table to the right presents typical patient doses associated with various
medical imaging procedures.
X-ray (single exposure)
Hand/Foot
Dental
Chest
Abdomen
Pelvis
Mammogram (2 views)
Procedure Dose (mSv)
0.005
0.015
0.10
0.60
0.70
0.72
CT(multiple exposures)
Head
Chest
Full Body
**Data source: NRC
2
7
10
Worker Radiation Dose Limits
Occupational dose limits are set by regulatory agencies to limit cancer risk as well as the other potential biological eects of radiation. Annual occupational dose limits, as established in U.S. federal law
(10 CFR 20) are provided below, however some locally established dose limits may be more protective. Check with your local regulator for dose limits that apply specifically to you.
Type of Limit
Lens of the eye
Skin
Hands and feet
Embryo/fetus
**from 10CFR20.1202 and 10CFR2 0.1208
Cocoon Training Manual
Occupational Dose Limit
50 mSv
150 mSv
500 mSv
500 mSv
5 mSv (over the length of pregnancy)
Basic X-ray Safety
//
8
Page 9

MaxRay Safety
Backscatter Shield
The Cocoon has a circular, lead infused plastic disc
(0.35 mm lead-equivalent) surrounding the X-ray
beam emission port. The purpose of this “backscatter shield” is to absorb radiation scattered from the
patient’s jaw so that it doesn’t reach the operator.
The backscatter shield should never be removed,
as this shield is very eective at reducing radiation
scatter in the direction of the operator. As seen by
the figure, the shield, in relation to the patient’s head,
provides a safety zone in which the operator should
remain during exposures.
(Editor’s Note: The photograph was taken in a studio. In
the clinical setting, the patient and technician would be
wearing leaded protection.)
The backscatter shield provides a safety zone to
the left of the green line.
Geometry of the Backscatter Zone
When producing an X-ray image, the operator should
stand directly behind the unit, holding it in the manner shown. In order to maximize the backscatter
protection area, the emission port should be perpendicular to the area being radiographed, i.e., the
backscatter shield should be parallel to the operator.
Cocoon Training Manual
Proper parallel orientation.
MaxRay Safety
//
9
Page 10

If the backscatter shield is not parallel to the operator, the backscatter zone angel changes, limiting
the zone coverage. When taking a dicult image,
the operator should first attempt to move the patient’s head, while maintaining proper alignment.
This allows for the operator to stay within the backscatter zone and maintain operator safety. Keeping
the backscatter shield parallel to the body is very
important. If the operator holds the Cocoon in the
manner shown, the shield is not protecting their vital organs and radiation exposure is received unduly.
Additionally, the emission port should be held close
to the patient to maximize the backscatter protection zone. As the cone and shield move farther from
the cheek, the angle defining the backscatter protection zone decreases.
Improper usage.
Cocoon Training Manual
Increased distance reduces protection area.
MaxRay Safety
//
10
Page 11

Dosimetry
The Cocoon has been shown to be a very safe handheld X-ray system when used as intended. The
occupational dose from leakage radiation at 1 cm from the case is less than 0.05 mSv to the fingers
for an entire work year. And, as long as the operator remains within the safety zone (provided by the
backscatter shield), their dose to the whole body is less than 0.20 mSv. These dose estimates assume
that the operator makes 7,200 dental X-rays each year; the unit is very safe. For reference, the regulatory dose limits are 500 mSv to the fingers and 50 mSv to the whole body.
Accidental Exposure Prevention
Accidental exposures are easy to prevent if the operator remains aware of the direction in which the
emission port is pointing and the on/o status of the Cocoon. As a general rule, whether on or o,
the operator should NEVER point the Cocoon emission port at anyone, except the area of the patient
about to be radiographed. Exposure occurs only when the activation button is pressed. The operator should remain vigilant and keep their finger o the activation button until ready for the intended
exposure.
As the operator, it is important to be aware of your surroundings in order to maintain ALARA. Always
ensure that you are within the backscatter protection zone, and that all unnecessary persons are out
of the room prior to initiating an exposure.
When taking an image, the current status of the unit on the LCD display window will change from
READY to EXPOSURE, accompanied by voice prompting. The operator will hear a steady tone during
the exposure; this sound will end when the selected time has passed. As a safety feature, the exposure will stop when the activation button is released, even if the selected time cycle is not complete.
Cocoon Training Manual
MaxRay Safety
//
11
Page 12

NEVER attempt to operate the Cocoon handheld X-ray system if any covers, shielding material, collimators, etc. have been removed. As the operator, NEVER place any part of your body in the primary
beam.
An additional safety feature is provided in the handle of the Cocoon. A trigger lock is available and
can be engaged by the operator. With the trigger in the outer position (left picture), the lock is depressed from the left side. This will lock the trigger in the “o” position (right picture), not allowing
engagement of the X-ray emission electronics.
Pressing the trigger lock from the right side of the unit will unlock the trigger and allow for normal
operation.
Cocoon Training Manual
MaxRay Safety
//
12
Page 13

Exposure Time
There is only one variable of exposure on the Cocoon unit that can be changed for a given radiograph … exposure time. The Cocoon has exposure factors of mA and kV that are fixed and cannot be
changed by the operator. The exposure time is changed based on patient age (adult or child), image
receptor (film or digital), and the location of teeth being imaged. The operator makes selections of
age, receptor, and position on the Cocoon, and in turn the Cocoon provides a suggested range of exposure time in increments of 0.05 seconds. For example, a selection of adult, digital (sensor), molar
results in suggested time option of 0.40 seconds (see chart below). See the User’s Manual for more
details on selecting the exposure time.
There is a direct correlation between exposure time and dose. If exposure time is increased, patient
dose increases. There is certainly a trade-o between image quality and patient dose. It is important
to practice ALARA by keeping dose as low as possible while maintaining adequate image quality for
diagnosis. Exposure to the operator and the patient should be limited and having to repeat images
should be avoided.
Cocoon Training Manual
MaxRay Safety
//
13
Page 14

Safe Storage
Because the handheld X-ray system is portable, certain safety precautions must be implemented to
ensure worker and patient safety. For a safe work environment, when not in use, the Cocoon should
be stored in a locked cabinet so that the device is accessible only to authorized personnel.
Cocoon Training Manual
MaxRay Safety
//
14
 Loading...
Loading...