
• Do not place the NIB P cuff over a wound, as this can cause further injury.
• Do not place the NIBP cuff on the same or adjacent arm to a mastectomy, or where the
lymph nodes we r e r emoved, or if a shunt is on that arm. This can lea d to bruising,
inaccurate readings, or negatively impact the drainage of fluids because of temporary
interference to blood flow.
! CAUTION
• Only use recommended MRI NIBP cuffs and tubing identified in section 9.2.
• In AUTO Mode, th e monitor displays results of the last measurement until another
measurement starts. If a patient's condition changes during the time interval between
measurements, the monitor will not detect it.
• Excessive patient motion may cause inaccurate measurements. Minimize motion to
improve blood pressure measurements.
• Avoid crimping or undue bending, twisting, or entanglement of the NIBP hose.
6.4.1.1. Limitations
The following factors may affect the accuracy of measurement:
• Heart rate extremes of less than 40 bpm or greater than 240 bpm
• A regular arterial pressure pulse is hard to detect
• Cardiac arrhythmias
• Physical movement (patient or imposed)
• Rapid blood pressure changes
• Severe shock or hypothermia that reduces blood flow to the peripheries
• Obesity, wh ere a thick layer of fat surrounding a limb dampens the oscillations coming
from the artery
• Edematous extremity
6.4.2. Understanding the Display
1. Measurement Unit (mmHg or kPa)
2. Current Mean Pressure upper and lower alarm lim its
3. NIBP cuff pr essure when inflat ing
4. Time until nex t NI BP Measurement (m inutes : seconds or manual)
5. Current Systolic Pressure upper and lower alarm li mits
6. Most recent NIBP reading
7. Current Diastoli c P re ss ure upper and lower alarm limits
6-25

6.4.3. NIBP Patient Application
When positioning the patient, routine NIBP measurements (including for the condition
hypertension) require the patient to remain silent, still and relaxed, with legs uncrossed and
arms supported. Note that during MRI procedures, patients are typically lying down with their
legs uncrossed and arms supported as needed for the MRI scan. A five minute waiting period
is recommended before starting readings. Ensure that the cuff is at the level of the right atrium
of the heart.
1. Verify that the patient type is corr ec t . Change it if necessary.
2. Ensure tubing is connected to the 3880 monitor
3. Select a correct sized cuff and then apply it as follows:
a. Determine the patient’s limb circumference.
b. Select an appropriate cuff by referring to the limb circumference marked on the
cuff. The width of the cuff should be 40% (50% for neonates) of the limb
circumference, or 2/3 of the uppe r arm’s length. The i nflatable part of the cuff
should be long enough to encircle at least 50% to 80% of the limb.
c. Apply the cuff to an upper arm or leg of the patient and make sure the marking
on the cuff matches the artery location. Do not wrap the cuff too tightly around
the limb. It may cause discoloration, and ischemia of the extremities. Make sure
that the cuff edge falls within the marked range. If it does not, use a larger or
smaller cuff that will fit better.
4. Connect the cuff to the air tubing and make sure that the bladder inside the cover is not
folded and twisted
5. Press the START/STOP button to initiate a blood pressure reading. Hold TART/STOP
button down for three seconds to initiate a STAT burst of three successive NIBP
readings.
NOTE
• Automatic NIBP readings will n ot cy cle when the monit or is i n St andby
6.4.3.1. Setup Checklist
• The hose is correct.
• The connector is fi r mly pushed inside the cuff tube.
• The NIBP hose is pr operly connected to the module and will not detach if pulled.
• The NIBP cuff is correct for the patient’s limb size.
6-26
• There are no hol es or cracks in the cuff bladder or cuff tube.
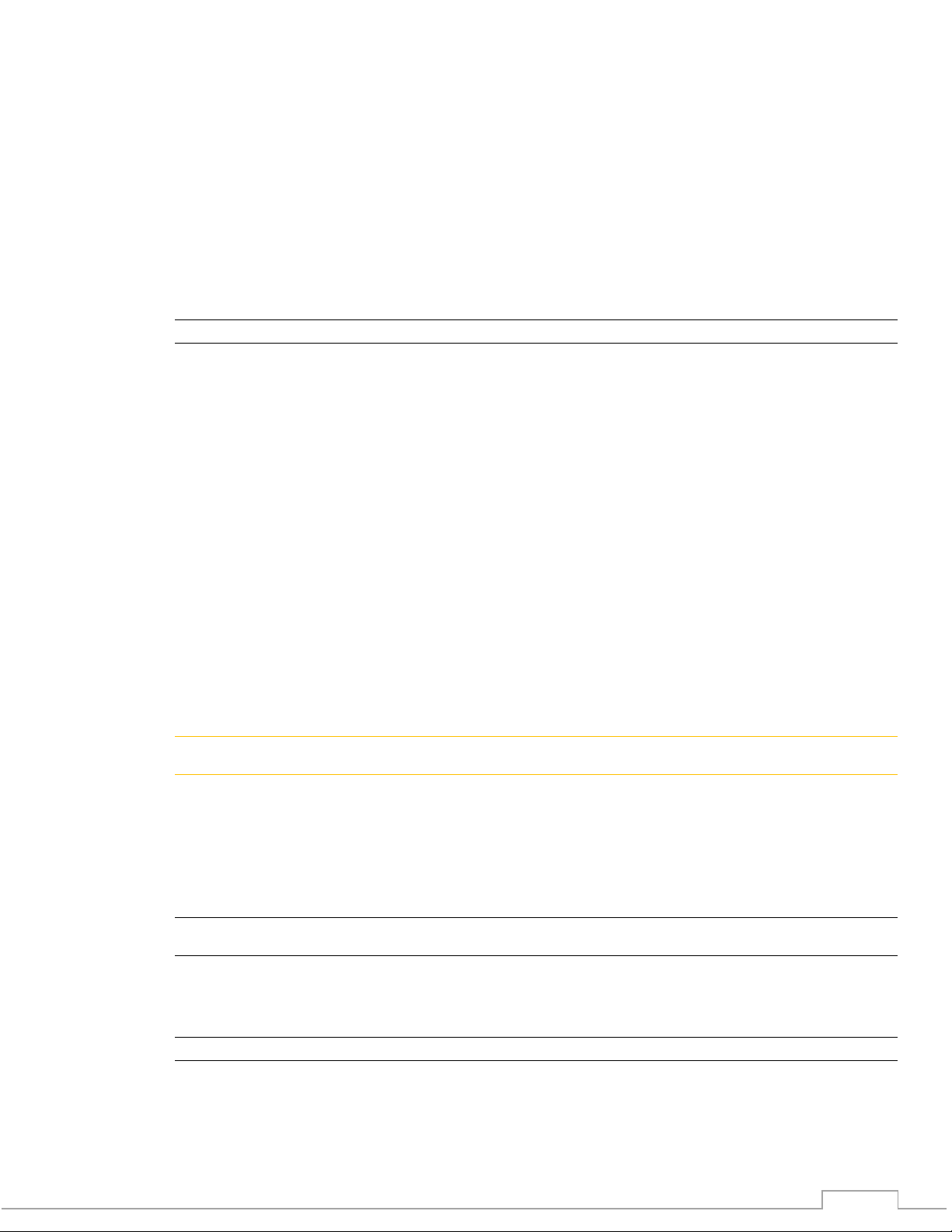
Range
Low
High
Range
Adult
systolic
Off, 30-270
90
160
30-270, Off
diastolic
Off, 10-245
50
90
10-245, Off
mean
Off, 20-255
60
110
20-255, Off
Pediatric /Infant
systolic
Off, 30-270
70
120
30-270, Off
diastolic
Off, 10-245
40
70
10-245, Off
mean
Off, 20-255
50
90
20-255, Off
Neonatal
systolic
Off, 30-130
40
90
30-130, Off
diastolic
Off, 10-100
20
60
10-100, Off
mean
Off, 20-120
25
70
20-120, Off
• All residua l air is squeezed out of the cuff before wrapping it around the arm.
• The symbol indicating the center of the bladder is over the artery.
• The cuff is not loose.
• The cuff is at hear t level.
• The cuff tubes or NIBP tube are not kinked or squeezed together.
• Non-invasive blood pressure is selected to be displayed through Monitor Setup patient
parameters menu.
6.4.4. Changing Frequently Use d NIBP Settings
6.4.4.1. Manual NIBP Mode
To adjust the NIBP mode between manual and automatic follow these steps:
1. Touch the NIBP vital sign numerical box to bring up the NIBP menu
2. For manual mode set the “Auto Cycle Time” to OFF
3. Touch Back button to close the menu
6.4.4.2. Automatic NIBP Int e rval Mode
To adjust the NIBP intervals for the Automatic settings follow these steps.
1. Touch the NIBP vital sign numerical box to bring up the NIBP menu
2. Select “Auto Cycle Time” to show drop down: OFF, 3 min, 5 min, 8 min, 10 min, 15 min,
30 min
3. Make your sel ection
4. Touch Back button to close the menu
6.4.5. NIBP Alarm Limits
Low Limit
Default
Default
High Limit
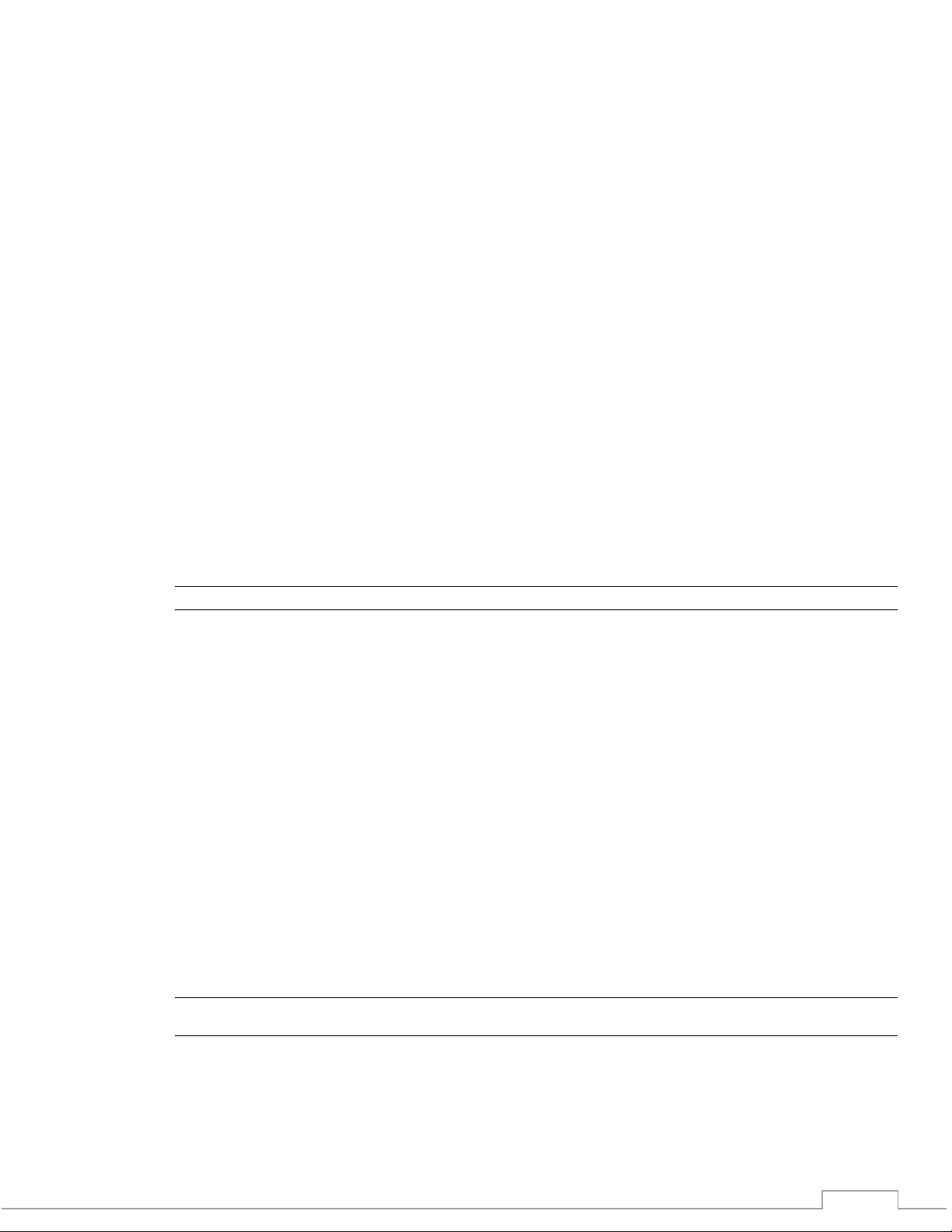
6-27

Message
Trigger Condition
NIBP Inop
Hardware or software failure detected
NIBP Over Press
Pressure exceeds 300 mmHg for Adult / Ped or 150 mmHg for Neonatal patients
15 mmHg remains in the line for Adult / Ped or 5mmHg for Neo for greater than 90 seconds
NIBP Time Out
Pressure remains the same for more than 30 seconds or if measurement exceeds 180 seconds
NIBP Leak
Air leak is detected
Wrong Cuff
Displayed if the NIBP system detects an incorrect cuff size for the selected patient mode
NIBP Occlusion
Occlusion is detected
NIBP Cal Error
Calibration error detected
NIBP Delayed
NIBP reading start has been delayed to allow blood flow to resume
6.4.6. NIBP Messages
-or-
6.5. Temperature Monitoring
6.5.1. Temperature Overv i e w
The 3880 system f eatures a unique and in novative temper ature measureme nt system
supporting surface temperature readings.
6.5.1.1. Temperature Sensor
The fiber-optic temperature sensor is used for the measurement of patient body temperature
using axillary sensing tip placement.
! WARNING
• Frequent medical attention to the sensor axilla site for possible pressure tissue necrosis
should be given during longer term monitoring sessions (4 hours or more), especially on
tender skin of neonatal patients.
! CAUTION
• The fiber-optic temperature sensors are constructed of fiber-optic glass and must
always be handled with care to prevent damage. Improper handling can result in
inaccurate readings.
6.5.1.2. Limitations
The following factors may influence the accuracy of measurement:
• Sensors access to ambient tem perature or drafts
• Do not bend the fiber optic sensor in a radius of less than 15 mm
• Do not expose to temperature above 50
• Do not pull or apply tension to the fiber-optic cable
• Do not alter or modify the accessories
○
C
6.5.2. Underst an d ing the Display
6-28

1. Measurement Unit
2. Curren t Vital Sigh
3. Alarm Limits
4. OVR/UND for Temp extended range <30.0 °C or >44.0 °C(<86.0°F or >111.2°F ),
accuracy ± 0.4 °C
6.5.3. Temperature Patie nt Application
6.5.3.1. Surface T e m p erature A pp l ication
Perform the following procedure to apply the fiber-optic temperature sensor to a patient:
1. Carefully uncoil the sensor, avoid knotting or kinking the fiber optic cable
2. Inspect sensor for damage, including tears or deformations
3. Thoroughly clean and dry the axilla or groin application site
4. Position the sensor tip at the application site
5. Secure sensor with some medical tape
6. Cover application site to block air drafts
! WARNING
• Avoid the use of any metalized foil temperature probe covers, or hydrogel backed probe
covers, as excessive RF heating could occur resulting in inaccurate temperature
measurements and/or burns.
NOTE
• There is a temperature difference between surface temperature and patient body (core)
temperature.
• When monitoring temperature during MRI procedures, the radio frequency (RF) energy
may normally increase the patient’s body temperature.
6.5.3.2. Setup Checklist
• Temperat ur e c able is properly in s er ted into the 3880 system
• Temperat ur e sensor is applied and positioned correctly
• Temperat ur e sensor is not damaged in any way
6.5.4. Changin g the Temperat ur e Settings
6.5.4.1. Units
The temperature format can be in Celsius or Fahrenheit. To adjust the units follow these steps:
1. Touch the Temperature vital sign box
2. Select “Unit”
3. Make your sel ection
4. Touch Back button to close menu
6-29

6.5.5. Temperature Alarm Limits, Celsius
Range
Default Low
High
Range
Adult Temp
Off, 25-40
36
39
25-40, Off
Pediatric Temp
Off, 25-40
36
39
25-40, Off
Neonatal Temp
Off, 25-40
36
39
25-40, Off
Message
Trigger Condition
Temp Inop
Hardware or software failure detected
Temp Probe Fail
Broken sensor detected or a sensor is not attached properly
OVR / UND
Indicating Temp extended range < 30.0 °C or > 44 C°(<86.0°F or
accuracy ± 0.4 °C
Low Limit
Default
High Limit
6.5.6. Temperature Messaging
>111.2°F )
6.5.7. Connecting the Sensor
The fiber optic temperature sensor utilizes a keyed twist locking connector to securely mate to the
temper a ture c o nne c tion port on the right s ide of the 3 8 8 0 M onitor unit. Ro tate the sensor
co nne c tion while ge ntly pushing i nto the ma ting co nnec tion on the monitor. O nc e the ke y wa y
h a s s lid e in t o th e m a t in g s lo t , t u r n t h e o u t e r s h e ll ≈3 0 ° t o lo c k in t o p la c e .
6.5.8. Temperature refer en ce measurement
A baseline temperature meas urement sho uld be made once the fi ber o ptic temperat ure s ensor is
appl ied and befo re s t arting the MR i mage scan , which s ho uld be used as a reference for t he
temperature measured duri ng t he scan.
6-30

7. Using the Recorder
The optional 3885-B Base Station recorder provides hard copies of up to two waveforms and
trend information.
NOTE
• The 3880 MRI Patient monitor does not have an internal recorder. Printing can only be
done if the system is communicating with the optional 3885-B Base Station. The Base
station unit houses and drives the strip chart recorder in response to Record or Print
requests from the 3880 Monitor or 3885-T Remote Tablet hard ( Record) and soft (Print)
keys.
7.1. Loading Paper
To load paper into the recorder review section 2.2.9 for details.
7.2. Recorder Setup Menu
7.2.1. Trace 1
The optional recorder can print one or two waveforms of ECG, SpO2, CO2 waveforms. When
Trace 1 and 2 are selected to print, Trace 1 will appear on the top of the paper. To adjust which
waveform yo u want to print when the Print button is pressed follow these steps:
1. Press the SETTINGS button
2. Select “Recorder Setup”
3. Select “Trace 1”
4. Select desired waveform to print
5. Touch Back button to close the menu
7.2.2. Trace 2
The optional recorder can print one or two waveforms of ECG, SpO2, CO2 waveforms. When
trace 1 and 2 are selected to print, T r ace 2 will appear on the bottom of the paper. To adjust
which wavefor m you want to print when the Print button is pressed follow the se steps:
1. Press the SETTINGS button
2. Select “Recorder Setup”
3. Select “Trace 2”
4. Select desired waveform to print or select OFF to print a single waveform
5. Touch Back button to close the menu
NOTE : Each vital sign parameter must be set ‘ON’ to allow recording of its trace. Also,
with ECG, two leads must be on displa y (d isplay Trace A and B) and set for recording,
to record ECG Trace 2.
7.2.3. Waveform Trace delay
Trace delay allows users to set a time delay before the waveform data is sent to the recorder.
This can account for the time delay between when a user decides to print and when they
actually depress the button. The delay options are 0, 4, 8 and 16 seconds.
To adjust the trace delay foll ow these steps:
1. Press the SETTINGS button
2. Select “Recorder Setup”
7-31

3. Select “Trace Delay”
4. Select des ired delay
5. Touch Back button to close the menu
7.2.4. Auto Strip
Auto strip allows the automatic report feature of the recorder to be switched ON and OFF. The
auto strip will automatica ll y print when a clinic al alarm is detected.
To enable the Aut o St rip follow thes e st eps:
1. Press the SETTINGS button
2. Select “Recorder Setup”
3. Toggle “Auto Strip” ON and OFF
4. Touch Back button to close the menu
7.2.5. Run Time
Recorder Run Time allows users to adjust the length of time the recorder prints when activated.
The options ar e 8, 1 2, 16, 20 and 30 seconds.
To adjust the waveform Record Run Time follow these steps:
1. Press the SETTINGS button
2. Select” Recorder Setup”
3. Select “Run Time“
4. Select desired time
5. Touch Back button to close the menu
7.2.6. Recorder Sweep Speed
The Sweep Speed sw itches the recorder speed between 25 and 50 mm/second.
To adjust recorder Sweep Speed follow these steps:
1. Press the SETTINGS button
2. Select “Recorder Setup”
3. Select “Speed”
4. Select des ired speed
5. Touch Back button to close the menu
7.2.7. To manually start a strip chart recording
Press the front panel “Record” hard key at either the 3880 Monitor or 3885-T Remote Tablet.
7.2.8. Rec order O utput
The strip chart recorder output will be the waveform Trace or Traces selected in the Record
Setup along with the selected delay and run time, with the text printout of all active vital signs
values. The vital signs, such as HR, SpO2, Blood Pressure, GAS measurements, and
Temperature print on the paper in a table at conclusion of the strip run time.
7.3. Printing
7-32

The term “Printing” is used herein to refer to using the strip chart recorder as a printer of text
and numeric information, such as the Tabular Trend table. Strip “Recording” is a specialized
print out of waveform data as described in 7.2.7 and 7.2.8 above. See section 5.5 for instruction
to print Trends.
7-33

8. Pre-Use Operator Verification, Troubleshooting and User
Maintenance
8.1. Overview
Check the following items prior to monitoring to ensure completion of all essential preparations.
Items that are broken, missing, plainly worn, distorted, or contaminated must be replaced
immediately. The 3880 system must not be repaired other than in accordance with written
instructions provided by IRadimed. The device shall not be altered without written approval of
IRadimed. The user has the sole responsibility for any malfu nc ti on which results fro m imp r oper
use, faulty maintenance, improper repair, damage or alteration by anyone other than IRadimed
authorized personnel.
! WARNING
• For proper equipment performance, maintenance and service procedures should be
performed at the recommended intervals as described in the monitor’s service manual.
NOTE
• The IRadimed software design controls include performance of a risk analysis using
methods consistent with ISO 14971 Medical devices - Application of risk management to
medical dev i ces. The 3880 system employs watchdog timers, self-monitoring activities
(memory, c om m unication and sensor checks and so on), and power-on self-diagnostics
(for example, memory checksums).
8.1.1. Battery Life Expectancy
Life expectancy of a battery depends on how frequent and how long it is used. For properly
maintain ed and stored batter i es , the life expectancy is about 2 or 3 years res pectively. For more
aggressi v e and non-traditional use mo dels, the life expectancy maybe less.
recommend s re placing batteries every 2 to 3 years or wh en signs of wear or operation are
noticeably different.
To get the most out of your batteries observe the following guidelines:
• The batter y performance test must be performed ever y year, before monitor repairs, or
whenever the battery is suspected as being the source of the problems.
• Take out the battery before the monitor is shipped or will not be used for more than 3
months.
• The shelf-life of a Lithium Polymer battery is about 6 months when the battery is stored
with the battery power being 50% of the total power.
IRadimed
8-1

8.1.2. Checking a Battery
The user replaceable battery packs utilized in the 3880 patient monitor can be checked outside
of the monitor. Thi s feature allows facilities with multiple batteries to proac t ively select a battery
that has a desired charge level prior to inserting it into the system. To che c k a batteries charg e
follows these steps :
1. Locate the button on the rear corner of the battery (1)
2. Depress the button and the LED indicators will momentarily show the charge status. (2)
8.2. Performance Checks
8.2.1. Daily in between tasks
• Check that s ystem components and ac cessories do not have any visual defects such as
cracks or loo se parts.
• Check that the system components as described in the Care and Cleaning 8.4 part of
this section were cleaned properly after the previous use.
• All supplies and accessories are not passed their expired date.
• Check that batteries are properly inserted and charged.
• Ensure all system components are wir elessly communicated
• Wipe the monitor, PODs and accessory surfaces
• Change all airway patient accessories.
• Ensure that you are using correct accessory sizes for each patient and that they are
properly connected.
• Check that all accessories, cables and monitor parts are clean and working properly.
• Check that you have selected desired parameters to be displayed in digit and waveform
fields.
• Check that the trends of the previous patient are erased.
• Monitor patient type mode and alarm limits are suitable fo r the patient.
• Check the compatibility of the 3880 monitor, sen sors and cables before use
8.2.2. Regular Inspection and Verification
Wireless Communication
• Place the PODs and 3880 Monitor inside the MRI room suite with the door shut. Place
the 3885-T Remote Ta ble t in the control room i n it s desired locat io n and check that the
communication performance is acceptab le.
ECG
• Check that the message 'Leads Off' disa ppears and the waveforms are displayed when
the lead wires are connected to the patient.
Pulse Oximetry
• Check that the R ed Light is visible in t he s ensor
• Check that the SpO
the sensor is connected to the patient
CO
(CO2 only or 3886 Multi-Gas system)
2
value is display ed and the message “P ro be O f f” disappears when
2
8-2

• Occlude the sampling line and check that the message “Occlusion” appears within 30
seconds
NIBP
• Check that the pressure values are displayed for all cuff sizes
Temperature
• Check that the temperature value is displayed when the cable is connected
Recorder
• Check that the strip chart recorder is functional
Alarms
• Turn the monitoring system on and check that the Red, Amber and blue Tri-Color TriColor Alarm D om e Light are lit momentarily
• Check that the speaker gives and audible tones at the desired level
• Use a conventional patient simulator and / or test gasses to verify alarm functionality.
When a problem with the alarm system is suspected, always refer the monitor to a
qualified service personnel.
Battery
• The battery pack should be inspected anytime the battery pack is removed. Look for
signs of physical damage, shock and swelling. Che c k that the battery pack is holding
sufficient operating capacity.
• Check that the battery is communicating with the monitor by observing the battery icon
on the display.
! CAUTION
• Any failure of the inspection of the battery pack will require discontinuance of use and
replacement will be needed.
• If any cells swollen greater than 8 mm thi ck or cause the plas tic case to bulge
discontinue use and contact your support personnel for proper disposal.
8.2.3. Every Twelve Months
Preventative Maintenance Check
• Calibration check of temperature, NIBP and CO
NOTE
• The annual check a c co rd i n g to detailed instruction s of the Service Manual requires
trained service personnel and appropriate testing tools and equipment.
• Verify all calibration / test gas mixture containers are empty before disposal.
• Use only MRI compliant calibration / test gas mixture containers suitable for use in the
MRI enviro nm ent for verification of gas reading s inside of zone IV.
8.3. Service Setup Menu
8.3.1. Software Version
To check the current revision of software in the 3880 system, P OD s and Tablet follow these
steps:
1. Press the SETTINGS Button
2. Select “Service Mode”
3. Enter password
4. Select “Device Information”
5. Check software version
6. Touch Back button to close the menu
/ Multi-Gas Agents Unit
2
8-3
8.4. Care and Cleaning
8.4.1. Introduction
For safe and reliable function and operation of the monitor, regular care has to be carried out in
accordance with manufactures guidelines. Use only manufactures approved substances and
methods to clean and disinfect y our equipment. The warranty does not cover damage caused
by unappro v ed substances or methods.
IRadimed makes no claims regarding the efficacy of the listed chemicals or methods as a
means for controlling infection.
NOTE
• If the monitoring system does not function as it should and troubleshooting cannot solve
the problem, contact your service representative.
• Detailed cleaning instructions provided with any accessory should be followed.
8.4.2. General Guidelines
Keep your equipment and accessories free of dust, dirt and contaminants. To avoid damage to
the 3880 monitor follow these rules:
• Always dilute liquid cleaning agents according the manufacturer’s instructions or use
lowest possible concentration.
• Do not immerse part of the 3880 monitor into liquid.
• Do not pour or use pressurized spray liq uid onto the 3880 monitor or accessories.
• Do not allow liquid to enter the case.
• Never use abrasive materials, solvent or corrosive cleaners.
• Clean the 3880 monitor in a well-ventilated area before and after each patient use.
• Allow components to dry completely prior to use.
• A soft bristled brush may be used to clean narrow areas.
• Do not use hard or pointed objects to clean any part of the monitor.
! WARNING
• Be sure to shut down the system and disconnect all power cables from the outlets
before cleaning the 3880 monitor.
• Do not use unspecified cleaners, materials or methods as they may damage the device,
labels or cause failures.
• Do not use conductive solutions or materials to clean the system.
• Do not reuse sensors intended for single patient use.
! CAUTION
• If liquid is sp illed on the 3880 monitor or accessories and may have entered the system
immediately contact your service personnel.
• Do not use solvent based cleaning agents as damage to the plastic parts could occur.
NOTE
• Before cleaning any equipment, consult your hospital’s regulations for cleaning
• Refer to any superseding instr uc tions accompan y i ng any accessori es or options.
8-4
8.4.3. Cleaning & Disinfecting
The 3880 system should be cleaned on a regular basis. If there is heavy pollution and/or lots of
dust and sand at/in your facility, the 3880 monito r should be cleaned more frequently.
Recommended cleaning agents are:
• Mild Soap (diluted)
• Ammonia (diluted )
• Isopropanol (70% )
• Chloramine (5%)
• Glutaraldehyde (2%)
• Ethyl Alcohol Based (60-95%)
• Chlorine/Bleach Based (4-6%)
• Iodine Based (0.5-5%)
• Phenols (0.2-3%)
• Quaternary Ammonium Compounds (2%)
• Hydrogen Peroxide (<3%)
To clean the 3880 monitor, follow these rules:
1. Shut down the pati ent monitor and disconnect it from power .
2. Clean the displays using a soft, clean clo th da m pened with glass clea ne r .
3. Clean the exterior surface of the 3880 monitor using a soft cloth dampened with an
approved cleaner .
4. Wipe the cleaning solution off the 3880 monitor with a dry cloth.
NOTE
• Disinfection may cause damage to the 3880 monitor and is therefore not recommended
unless otherwise indicat ed in your hospital’s policy. Cleaning the 3880 monitor prior to
disinfecting is recommended.
8.4.4. Sterilizing
Sterilization may cause damage to the 3880 monitor and is therefore not recommended. The
decision to sterilize components must be made per your institution’s requirements with an
awareness of the effects on the integrity of the cables and potential hazards that it may cause.
8.4.5. Cleaning the Recorder Printhead
After the recorder has been used for a long time, deposits of paper debris may collect on the
printhead compromising the print quality and shortening the lifetime of the roller. Follow this
procedure to clean the printhead:
1. Open the Recorder door
2. Gently wipe around the printhead using cotton swa ps dampened with alcohol.
3. After the alcohol has complete dried, reload the paper and close the door.
! CAUTION
• Do not use anythin g t ha t may destroy the thermal print head.
• Do not add unnecessary force to the thermal print head.
8-5

8.5. User Maintenance
Problem
Possible Cause
Solution
1
3880 will not turn on.
Power dial is not in the
1) Turn 3880 ON by
position.
No AC power/battery
1) Plug AC Adapter
charged battery.
8.5.1. Overview
Before every use, a thorough inspection sho uld be performed.
Follow these guidelines when inspecting the 3880 monitor:
• Make sure that the environment and power supply meet the requirements.
• Inspect th e 3880 system and its accessories fo r mechanical dama ge .
• Inspect all power cords for damage, and make sure that their insulation is in good
condition.
• Make sure that only specified accessories are applied.
• Inspect if the alarm system functions correctl y .
• Make sure that the recorder functions correctly and the recorder paper meets the
requirements.
• Make sure that the patient monitor is in good working condition, and batteries have
sufficient charge.
In case of any damage or abnormity, do not use the patient monitor. Contact the hospital’s
biomedical engineers or your authorized
8.5.2. Updating Software
As revisio ns of the software become available, the 3880 can be updated, see service manual
for detail procedure.
IRadimed service personne l imm ediately.
8.6. Troubleshooting Probl ems With No Ons cr e en Mes sag e
The following section is for troubleshooting the 3880 system when there is no corresponding
message displayed on the screen. If a message is displayed on the screen please review Exhibit B of
the operators manual. Please contact IRadimed Technical support at (407) 677-8022 if you need
assistance troubleshooting or are unable to resolve any issues.
8.6.1. Troubleshooting Power Related Problems
correct position
depleted.
rotating the power
dial to the ON
power cord into a
working AC outlet
immediately.
2) Plug AC Adapter
into the circular
power receptacle on
the rear of the
device.
3) Optional Swap low
battery with a fully
8-6

Problem
Possible Cause
Solution
Blown Fuse(s).
1) Replace the fuse in
the power supply
type and procedure.
AC power source has
1) Switch AC power
requirements.
Screen Damaged.
If an audible alarm is
technical support.
2
3885-T will not turn on.
Power ON [ I] key not
1) Turn 3885-T ON by
pressed.
Battery depleted.
1) Plug AC Adapter
charged battery.
box (P/N 1120).
Refer to the service
manual for proper fuse
incorrect voltage.
pressed.
cord to a power
receptacle with
sufficient voltage.
Refer to the service
manual for voltage
heard and the alarm
dome light changes
when the power ON
button is pressed.
1) Investigate the LCD
display screen for
failure.
2) Contact IRadimed
firmly pressing the
ON button firmly.
Listen and feel for
the tactile feedback
to confirm the button
has been properly
power cord into an
AC outlet
immediately.
2) Plug AC Adapter
into the circular
power receptacle on
the rear of the
device.
3) Optional: Swap low
battery with a fully
8-7

Problem
Possible Cause
Solution
3
3885-B will not turn on.
Power ON key not
pressed.
1) Toggle the power
pressed.
Blown Fuse(s).
1) Replace the fuse in
type and procedure.
No AC power
1) Plug AC Adapter
immediately.
AC power source has
1) Switch AC power
requirements.
4
3886 will not turn on.
Power ON key not
1) Toggle the power
pressed.
Blown Fuse(s).
1) Replace the fuse in
type and procedure.
No AC power
1) Plug AC Adapter
immediately.
switch to the ON
position.
Listen and feel for
the tactile feedback
to confirm the button
has been properly
the rear of the 3885T
Refer to the service
manual for proper fuse
power cord into a
working AC outlet
incorrect voltage.
pressed.
cord to a power
receptacle with
sufficient voltage.
Refer to the service
manual for voltage
switch to the ON
position.
Listen and feel for
the tactile feedback
to confirm the button
has been properly
the rear of the 3885T
Refer to the service
manual for proper fuse
power cord into a
working AC outlet
8-8

Problem
Possible Cause
Solution
AC power source has
incorrect voltage.
1) Switch AC power
requirements.
5
ePOD or oPOD will not
Power ON key not
1) Toggle the power
pressed.
Insufficient battery life
1) Plug 3880 system
Technical Support
6
3880 will not operate
Battery not properly
1) Plug AC Adapter
pack before use.
cord to a power
receptacle with
sufficient voltage.
Refer to the service
manual for voltage
turn on
on battery.
pressed.
charged.
switch to the ON
position.
Listen and feel for
the tactile feedback
to confirm the button
has been properly
into AC power.
2) Ensure the POD is
correctly docked and
seated into a
charging bay on the
3880 monitor.
3) Allow to charge a
minimum of 4 hours.
4) Contact IRadimed
power cord into an
AC outlet
immediately.
2) Plug AC Adapter
into the circular
power receptacle on
the rear of the
device.
3) Wait until battery is
fully charged.
4) Press the button on
the exterior of the
battery pack. If no
LED’s illuminate
replace the battery
8-9

Problem
Possible Cause
Solution
Aged battery won't hold
charge.
1) Plug AC Adapter
pack before use.
Battery is in sleep
When the battery test
3880 back in use.
7
Short battery run time.
Battery not charged
1) Plug AC Adapter
off.
power cord into an
AC outlet
immediately.
2) Plug AC Adapter
into the circular
power receptacle on
the rear of the
device.
3) Wait until battery is
fully charged.
4) Press the button on
the exterior of the
battery pack. If no
LED’s illuminate
replace the battery
mode.
long enough.
button is pressed and
no lights illuminate.
1) Insert the dead
battery into a 3880
or 3885-B that is
already turned on
and connected to
AC power.
2) If battery doesn’t
wake up after 1 hour
of charge dispose of
it according to
policy.
3) Replace the battery
prior to putting the
power cord into an
AC outlet
immediately.
2) Plug AC Adapter
into the circular
power receptacle on
the rear of the
device.
3) Check battery by
pressing the test
button on the battery
(1133 battery only).
Note: The batteries will
charge at a faster rate
when the 3880 is turned
8-10

Problem
Possible Cause
Solution
Aged battery will not
hold charge.
1) Plug AC Adapter
technical support.
8
Battery is hard to
Swollen Battery Cells.
Return the device to
removal.
Problem
Possible Cause
Solution
1
No Audible alarm tone
Alarm volume set too low
1) Press the Settings
environment.
Faulty alarm speaker.
1) Contact IRadimed
Technical Support.
2
Continuous alarm tone
Faulty hardware.
1) Note any onscreen
technical support.
power cord into an
AC outlet
immediately.
2) Plug AC Adapter
into the circular
power receptacle on
the rear of the
device.
3) For 1133 batteries
only. After a few
hours of charge
check battery by
pressing the test
button on the
battery.
4) If problem persists
dispose of the
battery according to
policy.
5) Replace battery or
POD with a new
one.
6) If problem persists,
contact IRadimed
remove.
8.6.2. Troubleshooting Alarm Related Problems
heard.
after alarm silence is
pushed.
for the use environment.
IRadimed for battery
Button.
2) Select Alarms
Function
3) Adjust alarm volume
for the intended use
messages.
2) Contact IRadimed
8-11

Problem
Possible Cause
Solution
3
The unit is in Alarm mode
with lights flashing but
The 2 minute Alarm
1) Press the
re-engage.
Audible volume set too
1) Press the Settings
environment.
Problem
Possible Cause
Solution
1
Buttons will not function.
Key not pressed firmly.
1) Repeat key press
been properly pressed.
Faulty key panel.
If the above 2 solutions
Service.
2
Programmed settings are
3880 turned off for
1) Train appropriate
settings.
Volatile memory may not
1) Replace CR2032
Technical Service.
3
Clock is not correct.
Clock not properly
after receipt.
1) Adjust clock time as
Internal coin cell battery
1) Replace CR2032
Technical Service.
Summer/Winter time
1) Adjust clock as
manual.
no audible alarms can be
heard.
Silence button is
activated.
ALARMSILENCE
button to re-engage
alarm volume.
2) Or wait for two
minutes.
After two minutes, alarm
tones will automatically
low to be heard.
2) Select Alarms
3) Adjust alarm volume
8.6.3. Troubles hooting Operation Related Probl em s
Listen for audible and feel
for the tactile feedback to
confirm the button has
are acceptable contact
IRadimed Technical
Button.
Function
for the intended use
more firmly.
restored to default on
power up.
longer than 30 seconds
between uses.
store due to internal Coin
cell battery problem.
adjusted to local time
has become depleted.
change.
personnel that
turning off the 3880
for more than 30
seconds resets
coin cell battery.
2) Contact IRadimed
described in manual.
coin cell battery.
2) Contact IRadimed
described in service
8-12

Problem
Possible Cause
Solution
4 3885-T Remote will not
3880 is not turned ON.
1) Ensure the 3880 is
operational.
3880 is not within
1) Verify 3880 and
needed.
Software incompatibility.
1) Ensure the software
equal.
Incorrect Channel.
1) Ensure that both the
3885-B.
Multiple system
1) Ensure that each
simultaneously).
Loose or damaged
1) Ensure that the
are attached tightly.
Local radio interference
1) Ensure other
system components.
1) Try using a different
communicate on.
communicate to a
selected 3880 or drops
out.
wireless range.
turned on and is
3885-T within 90 ft
(30 m) of 3885-B
and that no other
devices are blocking
the wireless signal.
2) Reposition 3880 to
establish
communication as
revisions for the
3880 and 3885-T are
3885-T, 3885-B and
3880 are operating
on the same
wireless network
channel.
2) Record wireless
network from the
3880.
3) Select matching
wireless channel on
3885-T
4) Select matching
wireless channel on
components on the same
wireless network
channel.
antenna.
prevents communication.
3880 in your facility
are on separate,
unique channels (or
not used
antennas on the
3885-B are in good
working order and
wireless equipment
is greater than 3 feet
away from the 3880
wireless network
channel for the 3880
system to
8-13

Problem
Possible Cause
Solution
MRI Room Attenuation.
1) Ensure the high gain
antenna is attached
Technical Service.
5
ePOD or oPOD will not
3880 is not turned ON.
1) Ensure the 3880 is
operational.
3880 is not within
1) Verify PODS are
needed
Incorrect Channel.
1) Ensure that the
3882 oPOD.
Multiple system
1) Ensure that each
simultaneously).
6
Printer will not print
Wireless communication
1) Ensure wireless
with a recorder
to the correct
receptacle on the
3885-B
2) Position the high
gain antenna so it
has a direct line of
sight to the 3880.
3) Try a different
wireless channel
4) Contact IRadimed
communicate with a
3880
wireless range.
turned on and is
within 9 ft (3 m) of
3880 and that no
other devices, walls
or doors are blocking
the wireless signal.
2) Reposition 3880 to
have a line of sight
to the PODS as
ePOD, oPOD and
3880 are operating
on the same wireless
network channel.
2) Record wireless
network from the
3880.
3) Select matching
wireless channel on
3881 ePOD
4) Select matching
wireless channel on
components on the same
wireless network
channel.
to the 3885-B
3881 and 3882 in
your facility are on
separate, unique
channels that match
a corresponding
3880 (or not used
connection is
established to a
3885-B equipped
8-14

Problem
Possible Cause
Solution
Printer out of paper or
paper jam
1) Review section 7 of
manual
Problem
Possible Cause
Solution
1
Artifact on MR images.
Loose connection to cord
Tighten AC cord connection
Faulty Hardware.
1) Switch to battery
technica l service.
Problem
Possible Cause
Solution
1
ECG Vital Signs are not
1) Ensure the ePOD is
applications training.
8.6.4. Troubleshooting MRI Related Problems
the operators
when running on AC
power.
to Monitor and power
supply.
power.
2) Disconnect the power
cable from the 3880
monitor.
3) Disconnect AC power
cord from the AC
outlet in the MRI r oom.
4) Inspect components
damage.
5) Remove all power
cables from the room.
6) If artifact disappears
then replace faulty
hardware.
7) If artifact is still present
repeat steps for the
3886.
8) If artifact still appears
contact IRadimed
8.6.5. Troubleshooting Vital Sign Related Problems
performing as expected
2) Ensure the ECG
3) Inspect all ECG
4) Review section 6.1
5) Contact your local
on the same
wireless network
channel as the 3880.
parameter is
enabled.
components for
damage and replace
as necessary.
of the operators
manual
representative to
schedule
8-15

Problem
Possible Cause
Solution
Incompatible lead view
for the MRI scan and/or
Change the ECG lead view
sequence.
Poor skin preparation
Re-prep the patient
section 6.
Poor electrode
Reposition/replace
found in section 6.
Poor electrode quality
Replace the electrode with
electrode.
Weak radio link
Verify radio channel
improved reception.
QRS amplitude is less
Change the lead view and
the electrodes.
Faulty ECG ePOD
Replace ECG module, or
service representative.
Incorrect ECG Mode
Select the appropriate
manual.
Patient motion
Ensure that the patient is
not shivering or moving.
ECG lead not properly
Ensure each ECG leadwire
the ePOD.
Damaged ECG lead
Replace ECG lead with an
lead.
electrode placement
to select the best
performing view for the
according the application
procedure found in
placement
than 10 mm/mv
selected
electrodes according to
the application procedure
an IRadimed approved
setting and signal level.
Reposition antenna for
/ or reprep and reposition
refer to qualified technical
ECG filter mode for the
application. Refer to
section 6 of the operators
inserted into the ePOD
is inserted completely into
IRadimed approved ECG
8-16

Problem
Possible Cause
Solution
All other issues
1) Ensure the ePOD is
on the same
applications training.
2
SpO2 not functioning
SpO2 sensor is not
attached to the patient.
Ensure SpO2 sensor is
securely attached.
Poor SpO2 sensor
Reposition/replace SpO2
section 6.
Weak radio link
Verify radio channel
improved reception.
Faulty SpO2 oPOD
Replace SpO2 oPOD, or
service representative.
SPO2 readings are
Sensor positioning
Check the P.I. value and
section 6.
Ensure the SpO2 cable is
SpO2 applicator / grip.
Averaging time
Try adjusting the SpO2
averaging time.
Patients specific anatomy
Skin pigment and certain
readings.
Check that there is no nail
impeding the readings.
Cool temperature is
Check the P.I. value and
touch.
wireless network
channel as the 3880.
2) Ensure the ECG
parameter is
enabled.
3) Inspect all ECG
components for
damage and replace
as necessary.
4) Review section 6.1
of the operators
manual
5) Contact your local
representative to
schedule
unstable or poor
placement
sensor according to
setting and signal level.
Reposition antenna for
refer to qualified technical
try repositioning the
sensor correctly on the
patient according to
correctly inserted into the
anatomy ailments can
cause inconsistent SpO2
affecting patients
perfusion
polish on the patients digit
ensure the patient is not
shivering and that their
digits are warm to the
8-17

Problem
Possible Cause
Solution
interference from NIBP
cuff or arterial catheter.
Move the SpO2 sensor to
functions.
Excessive ambient light
Limit the amount of
as needed.
Excessive patient motion
Ensure that the patient is
not shivering or moving.
Circulation is reduced
Position the sensor at a
the patients digit.
Finger was removed from
Check that the
according to section 6.
SpO2 Vital Signs are not
All other issues
1) Ensure the SpO2
applications training.
3
CO2 not functioning
Sampling line hose is not
connected
Attach sampling line hose.
Leaking sampling line
Re-check fittings to ensure
sampling line hose.
Sampling line filter is wet
Verify proper drying
line hose filter.
Monitor has an internal
leak
Refer to qualified technical
service representative.
Values are too low or
unstable
Monitor has an internal
failure
Refer to qualified technical
service representative.
an application site and
limb that is not being
utilized for other medical
ambient light entering the
sensors. Cover with a cloth
performing as expected
because of excess
pressure
the sensor
different site and ensure it
is not applied to tightly to
appropriate sized sensor is
being used and reapply
parameter is
enabled.
2) Inspect all SpO2
components for
damage and replace
as necessary.
3) Review section 6.2
of the operators
manual.
4) Contact your local
representative to
schedule
hose
or clogged
they are tight. Replace
tubing is in position. Recheck filter to ensure it is
clear. Replace sampling
8-18

Problem
Possible Cause
Solution
EtCO2 Vital Signs are not
performing as expected
All other issues
1) Ensure the EtCO2
applications training.
4
NIBP values seem
Compromised hose or
Check that tubing is not
compressed or loose.
Ensure the patient is not
shivering or moving.
Ensure the correct sized
applied correctly.
Replace Hose or cuff if a
leak is suspected.
Monitor has an internal
leak
Refer to qualified technical
service representative.
Patients Arm Position
Ensure that the patients
arm is at heart level.
Cuff comes off patient
Inappropriate sized cuff
Determine correct cuff
according to section 6.
Cuff applied inside out
Reapply cuff according to
section 6.
NIBP not functioning
NIBP hose or cuff is
disconnected
Ensure NIBP hose is
securely connected.
Monitor has an internal
failure
Refer to qualified technical
service representative.
NIBP Vital Signs are not
All other issues
1) Ensure the NIBP
applications training.
parameter is
enabled.
2) Inspect all EtCO2
components for
damage and leaks
and replace as
necessary.
3) Review section 6.3
of the operators
manual.
4) Contact your local
representative to
schedule
unstable
limb
cuff
stretched, bent,
cuff is being used and
size and apply to patient
performing as expected
parameter is
enabled.
2) Inspect all NIBP
components for
damage and leaks
and replace as
necessary.
3) Review section 6.4
of the operators
manual.
4) Contact your local
representative to
schedule
8-19

Problem
Possible Cause
Solution
5
Temperature error or
intermittent function
Temperature sensor is
the patient.
Re-attach Temperature
Poor Temperature sensor
placement
Reposition/replace
Temperature sensor.
Faulty Temperature
Replace Temperature
representative.
Temperature Vital Signs
All other issues
1) Ensure the
applications training.
6
Respiration and Gases
1) Ensure the 3886 is
applications training.
not securely attached to
sensor.
are not performing as
expected
from 3886 are not
performing as expected
sensor
sensor, or refer to
qualified technical service
Temperature
parameter is
enabled.
2) Inspect all
Temperature cable
for damage or
kinking and replace
as necessary.
3) Review section 6.4
of the operators
manual.
4) Contact your local
representative to
schedule
turned ON
2) Ensure the Gas
parameter is
enabled on the
3880.
3) Inspect all EtCO2
components for
damage and leaks
and replace as
necessary.
4) Review section 6.3.8
of the operators
manual.
5) Contact your local
representative to
schedule
8-20

8.7. Repair
8.7.1. Overview
All repairs on c omponents under war ranty must be performed by authorized IRadimed service
personnel. If the 3880 system fails to function properly or requires maintenance, contact your
IRadimed representative.
! CAUTION
• Decontaminate all equipment prior to performing any repair or before sending to
IRadimed.
• No repair should ever be attempted by anyone not having a thorough knowledge of the
3880 system.
• Only replace damaged components with parts manufactured and authorized by
IRadimed.
NOTE
• Unauthorized repairs will void the w arranty.
• The user of this product shall have sole responsibility for any m alfunction which r esults
from improper use, faulty maintenance, improper repair, damage, or alterations by
anyone other than authorized
IRadimed service personnel.
8.7.2. Changing Fuses
1. Remove the power cord if used.
2. Remove the fuse holder by pulling the holder out with screwdriver.
3. If a fuse is blown, replace it with the IRadimed HE14 fuse which is the correct type an d
rating.
8.7.3. Removing a Paper Jam
If the recorder works incor rectly or produces unusual sounds, check if there is a paper jam. If a
jam is detected follow these steps to remove it:
1. Open the Recorder Door
2. Remove the paper and tear off any damaged paper
3. Reload the paper and close the recorder door.
8-21

8.8. Warranty
IRadimed Corporation warrants the major components of the 3880 system (e.g. 3880, 3885-T
Remote Tablet and 3885-B Base Station) to be free from defects in materials and workmanship
for a period of twelve (12) months from t he date of original de livery to the buyer or to buyer's
order, prov i ded that same is properly operated under conditions of normal use, and that periodic
maintenance and service is per formed. A ninety (90 ) day warranty applies to limited-life parts
and accessories (e.g.1 133 MRI Compatible Bat tery Pack, gating cable, SpO
, ECG, NIBP, CO2,
2
Temperature patient accessories). A thirty (30) day warranty applies to all parts and
accessories not listed above .
This warranty will become null and void if p r od uct has been repaired ot her than by IRadimed
Corporation, or its authorized representative, or if the product has been subject to misuse,
accident, negligence, or abuse.
IRadimed Corporation's sole obligation under this warranty is limited to repairing a product
which has been reported to IRadimed Corporation's Technical Servic e Center during norm al
business hours and shipped transportation prepaid. IRadimed Corporation is not liable for any
damages including, but not limited to, incidental damages, consequential damages or special
damages.
This warranty is in lieu of any other warranties, guar antees or conditions, includi ng
merchantability or fitness for a particular purpose. The remedies under this warranty are
exclusive and IRadimed Corporation neither assumes nor authorizes anyon e t o as sume for it
any other obligation in connection with the sale or repair of its products.
A purchased Maintenance Extension agreement provides for an additional 1, 2, or 3 years of
authorized repair for major products. The maintenance extension period will begin at the end of
the standard warranty period, and continue until the end of the maintenance extension period
purchased. The extended maintenance does not apply to equipment which has been subject to
abuse or neglect.
Maintenance Extensions purchased after the standard warranty has expired shall require a
physical inspec tion by IRadimed Corporation prior to purchase of any Maintenance Extension.
An additional service fee may also be required to bring the out of warranty product(s) within
specifications before any maintenance extension can be activated. (Cost of such inspection and
possible repair to the product will be communicated to customer at that time). We reserve the
right to refuse the sale of Maintenance Extension to any Product.
IRadimed Corporation warrants any such product subject to a Maintenance Extension
agreement shall, other than its expendable parts, provided that same is properly operated under
conditions of normal use, and th at periodic maint enance and servic e is performed; be repaired
by IRadimed and restored to full operational specification as where applicable at the time of
original manufacture. Any Ma intenance Ext ension will become null and void if product has been
repaired other than by IRad imed Corporatio n, or its authorized representative, or if the product
has been subject to misuse, accident, negligence or abuse.
Should a unit perform outside of IRadimed specifications and cannot be corrected by on site
technicians with instruction and support from IRadimed and unit must be returned to IRadimed
for repair, a loaner unit, if available, may be provided.
IRADIME D CORPORAT ION PRODUCT S CONTAIN PRO PRIETARY COPY WRITTEN
MATERIAL; ALL RIGHTS ARE RESERVED BY IRADIMED CORPORATION
8-22

9. Accessories
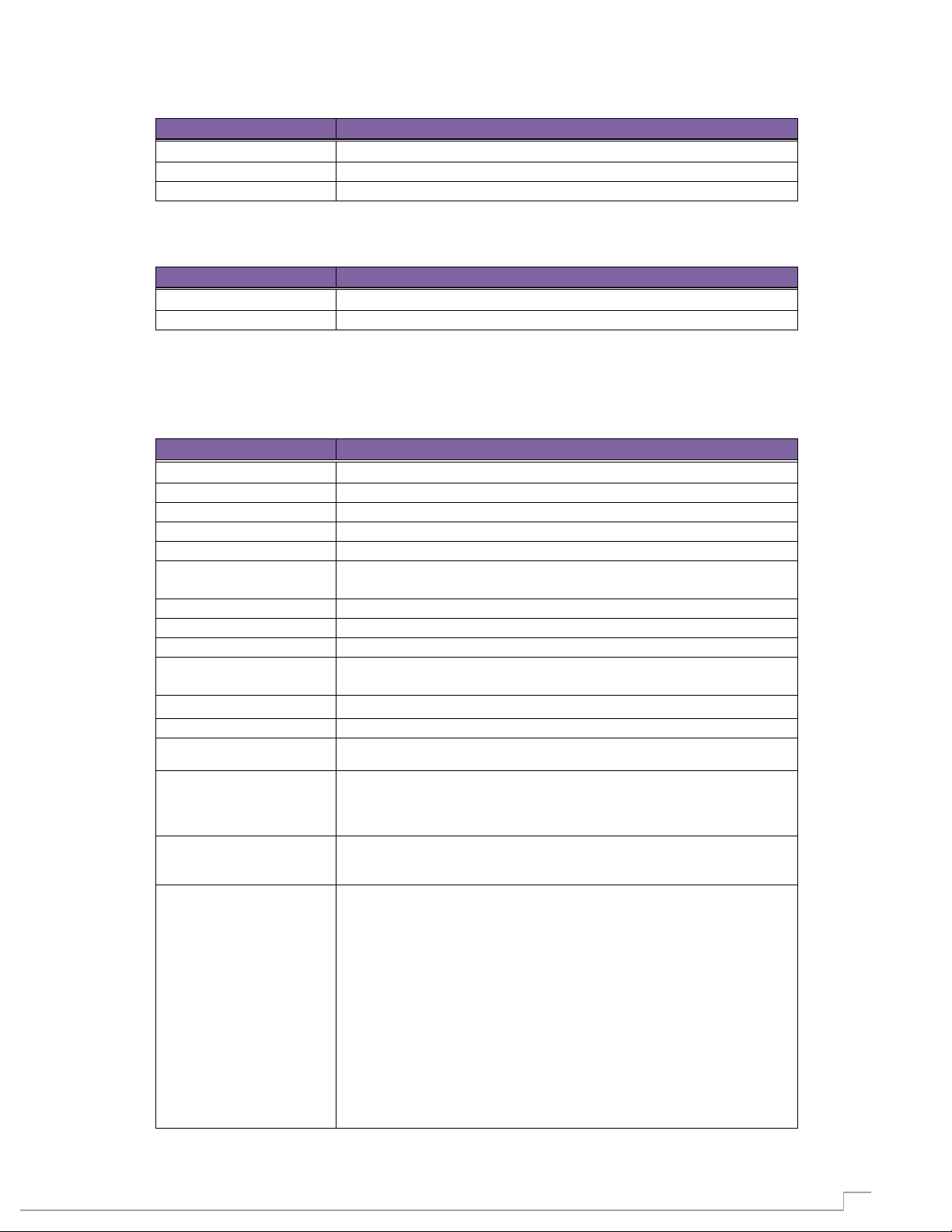
Part Number
Description
Image
Use Type
1171
Reusable Sensor Grip Kit (Pack of 3)
1821
Fiber Optic oPOD SpO2 Cable
3882
8 Channel Wireless oPOD
technology. For use with the IRadimed 3880.
Part Number
Description
Image
Use Type
1832LA
Large Adult Reusable Cuff (34-44cm)
patient use.
1832A
Adult Reusable Cuff (27-35cm)
patient use.
1832SA
Small Adult Reusable Cuff (20.5-28.5cm)
patient use.
The packaging of the accessories is color coded to help identify which access ories are most
likely appropriate for your par ticular pati ent.
• Gray – All patient sizes
• Neonatal (Birth to one month of age) – Purple
• Infant (One month to two years of age) – Orange
• Child (Two to Twelve years of age) – Green
• Adult (Above twelv e years of age) – Blue
NOTE
• All materials that come in contact with patients and users comply with ISO 10993-1.
To order replacement parts contact your IRadimed representative or call 1-866-677-8022
9.1. SpO
9.2. NIBP
2
Reusable Sensors Grip come in 3 sizes (Grips only)
Fiber optic SpO2 cable for use with IRadimed oPODs.
Wireless MRI SpO2 module featuring Masimo
Multiple Use
Multiple Use
Multiple Use
Reusable Non-Invasive blood pressure cuff are
constructed of an extremely soft, easy to clean material
to provide a long usable life and support multiple
Multiple Use
Reusable Non-Invasive blood pressure cuff are
constructed of an extremely soft, easy to clean material
to provide a long usable life and support multiple
Reusable Non-Invasive blood pressure cuff are
constructed of an extremely soft, easy to clean material
to provide a long usable life and support multiple
Multiple Use
Multiple Use
9-1

Part Number
Description
Image
Use Type
1832P
Pediatric Reusable Cuff (14-21.5cm)
patient use.
1832I
Infant Reusable Cuff (9-15cm)
patient use.
1833N4-10
Neonatal Size 4 Cuff (7-13cm) (Box of 10)
1833N3-10
Neonatal Size 3 Cuff (6-11cm) (Box of 10)
1833N2-10
Neonatal Size 2 Cuff (4-8cm) (Box of 10)
1833N1-10
Neonatal Size 1 Cuff (3-6cm) (Box of 10)
1831
NIBP Swift Connect NIBP Hose
Part Number
Description
Image
Use Type
1813-3
ECG Skin Prep Gel (Box of 3)
skin for MRI ECG electrodes.
1811
9” Five Lead ePOD MRI Leadwire (AAMI)
AAMI color coding. For Use with IRadimed ePOD only.
1811E
9” Five Lead ePOD MRI Leadwire (IEC)
IEC color coding. For Use with IRadimed ePOD only.
3881
8 Channel Wireless ePOD
Reusable Non-Invasive blood pressure cuff are
constructed of an extremely soft, easy to clean material
to provide a long usable life and support multiple
Reusable Non-Invasive blood pressure cuff are
constructed of an extremely soft, easy to clean material
to provide a long usable life and support multiple
Single Use Non-Invasive blood pressure cuffs are
constructed of soft fabric material that conform to the
tiniest of patients.
Single Use Non-Invasive blood pressure cuffs are
constructed of soft fabric material that conform to the
tiniest of patients.
Single Use Non-Invasive blood pressure cuffs are
constructed of soft fabric material that conform to the
tiniest of patients.
Multiple Use
Multiple Use
Single Use
Single Use
Single Use
9.3. ECG
Single Use Non-Invasive blood pressure cuffs are
constructed of soft fabric material that conform to the
tiniest of patients.
Single lumen non-invasive blood pressure hose
featuring simple connections
Package of 3 tubes of skin prep gel to prepare patients
ECG leadwire for 3 and 5 lead ECG applications with
ECG leadwire for 3 and 5 lead ECG applications with
Single Use
Multiple Use
Multiple Use
Multiple Use
Multiple Use
Wireless MRI ECG module for use with the IRadimed
3880
Multiple Use
9-2

Part Number
Description
Image
Use Type
1842A-25
Adult Nasal Cannula (Pack of 25)
1842P-25
Pediatric Nasal Cannula (Pack of 25)
1842I-25
Infant Nasal Cannula (Pack of 25)
1841-25
Coextruded Sample Line (Pack of 25)
Part Number
Description
Image
Use Type
1849-25
Nomoline Agent Sample Line (2m) (Pack of 25)
Module only
1846-25
Scavenge Hose (Pack of 25)
1848
Verification Check Gas
Part Number
Description
Image
Use Type
1851
Optical Temperature Sensor
9.4. CO2/Respiration Mo nitoring
Single use standard nasal cannula
Single use standard nasal cannula
Single use standard nasal cannula
Sample line for use with capnography and anesthetic
agent gas monitoring. For use with P/N 1849.
9.5. Multi-Gas (Agents) Monitoring
For use with IRadimed’s 3886 Wireless Multigas
Single Use
Single Use
Single Use
Single Use
Single Use
For use with IRadimed’s 3886 Wireless Multigas
Module only
For use with IRadimed’s 3886 Wireless Multigas
Module only
9.6. Temperature
Multiple use Fiber Optic temperature sensor
Single Use
Multiple Use
Multiple Use
9-3

Part Number
Description
Image
Use Type
1881
Universal Gating Interface
Systems equipped with cardiac gating leads
Part Number
Description
Image
Use Type
1133
3880 Battery
Non-Magnetic battery used with the 3880
1188
3885T Battery
Non-Magnetic battery used with the 3885T
1122
DC Power Cable, 10 feet (3m)
with the 1120 power supply
1120
Power Supply / Charger
Replacement power cable us ed with the 1122 cable
1128
North America AC Power Cord, 10 feet (3m)
1121
North America AC Power Cord, 3 feet (1m)
with the 1120 power supply
Part
Number
Description
Image
Use Type
1882-3
3885B Recorder Paper (Pack of 3)
9.7. Gating
Non-Magnetic gating interface cable for use with MRI
9.8. Power Supply
Replacement power cable used to interface the 3880
Replacement power cable us ed with 3885 and 3886
Multiple Use
Multiple Use
Multiple Use
Multiple Use
Multiple Use
Multiple Use
Replacement power cable used to interface the 3880
9.9. Recorder
3 Rolls of printer paper for the 3885B recorder
Multiple Use
Multiple Use
9-4

10-1
10. Exhibits
Technical Parameters
Technical Detail
Type:
Color TFT resistive touchscreen
Screen Size:
25.7 cm (10.1 inches) diagonal
Pixels:
800 by 480
Backlight:
LED
Screen Update Rate
2 Hz
Waveform Display Mode:
Moving Waveform
Waveform Display Width:
~145 mm
Waveform Display Height:
ECG Single Waveform:
~48mm max
ECG Dual Waveform:
~20mm max
All other Waveforms:
~25mm max
A. Specifications
10.1. Overview
Standard S ystem Components
• 3880 MRI Patient Monitor
• Wireless ECG POD
• Wireless SpO
• Non- Invasive Blood Pressure
• Accessories
Optional System Components
• 3885-T Remote Tablet ‘ Extended Range’ Control Room Display
• 3885-B Base Station with recorder
• CO
• Temperat ur e v i tal sign
• 3886 Multi-Gas Anesthetic Agent , 3886 Unit
Clinical Parameters
• Dual Channel, 5 Lead ECG
• Pulse Oximetry
• Perfusion Index
• Non – Invasive Blood Pressure
• Sidestream Capnography, Et CO
• Respirat ion Rate
• Fiber Optic Temperature
• Dual Anesthetic Agents
• Inspired N
• Inspired O
• MAC
POD
2
and Respiration vital signs
2
0
2
2
and CO2
2
10.1.1. Technical Specifications
10.1.1.1. Display

10-2
Technical Parameters
Technical Detail
Power:
Rotary On, Off
Feature Hard Keys:
Trends, Print, NIBP Start/Stop and Alarm Silence
Setup Hard Keys:
Setup and Standby
Soft Keys:
Touchscreen
Technical Parameters
Technical Detail
Power:
Push Button On, Off
Feature Hard Keys:
Trends, Print, NIBP Start/Stop and Alarm Silence
Setup Hard Keys:
Setup and Standby
Soft Keys:
Touchscreen
Technical Parameters
Technical Detail
Power:
Push Button On, Off
Hard Keys:
Channel Selection
Technical Parameters
Technical Detail
Power:
Toggle
Channel Select:
Button
Technical Parameters
Technical Detail
Types:
Tabular
Trend Memory:
50 readings
Tabular Intervals:
3, 5, 8, 10, 15, 30, Auto NIBP
Data Types:
HR, SpO2, NIBP, EtCO2, Resp, Temp, MAC, O2
Technical Parameters
Technical Detail
Indication:
Audible & Visual
Levels:
High, Medium, Low and Information Messages
Volume:
User Adjustable, 50 to 85 dba, or OFF
Silence:
Permanent or 2 minutes timed hold
10.1.1.2. User Interface
10.1.1.2.1. Monitor
10.1.1.2.2. Tablet
10.1.1.2.3. PODS
10.1.1.2.4. Base Station
10.1.1.3. Application Features
10.1.1.3.1 Trend Reports
10.1.1.3.2 Alarms

10-3
Technical Parameters
Technical Detail
IEC:
60601-1, 60601-1-2, 60601-1-8, 60601-2-27, 60601-2-49, 80601-2-30,
80601-2-55, 80601-2-56, 80601-2-61
Med Device Directive:
93/42/EEC, 2007/47/EEC
Defibrillator Protection:
Up to 5 KV
Defibrillator Recovery
Time:
During a defibrillation procedure, the ECG waveform will saturate then
recover in less than 5 seconds
Technical Parameters
Technical Detail
3880 Monitor:
23 cm (8.8 inches)
3885-T Remote Tablet:
19.6 cm (7.7 inches)
3885-B Base Station:
18.8 cm (7.4 inches)
3881/3882 Wireless
9.5 cm (3.8 inches)
3886 Multi-Gas Unit
8 cm (3.13 inches)
Technical Parameters
Technical Detail
3880 Monitor:
29 cm (11.4 inches)
3885-T Remote Tablet:
26.7 cm (10.5 inches)
3885-B Base Station:
38 cm (15 inches)
3881/3882 Wireless
PODS:
2.0 cm (0.8 inches)
3886 Multi-Gas Unit
14.7 cm (5.8 inches)
Technical Parameters
Technical Detail
3880 Monitor:
12.7 cm (5 inches)
3885-T Remote Tablet:
4.5 cm (1.8 inches)
3885-B Base Station:
12 cm (4.8 inches)
3881/3882 Wireless
PODS:
5.7 cm (2.3 inches)
3886 Multi-Gas Unit
10.2 cm (4.1 inches)
Technical Parameters
Technical Detail
3880 Monitor:
4 kg (8.9 lbs)
3885-T Remote Tablet:
1.6 kg (3.6 lbs)
3885-B Base Station:
2.1 kg (4.6 lbs)
3881/3882 Wireless
PODS:
73 g (0.16 lbs) (without sensors/leads)
3886 Multi-Gas Unit
1.04 kg (2.3 lbs)
PODS:
10.1.1.4. Safety Standards
10.1.1.5. Physical Specifications
10.1.1.5.1. Height
10.1.1.5.2.
Width
10.1.1.5.3. Depth
10.1.1.5.4. Weight

10-4
10.1.1.6. Electrical Specifications
Technical Parameters
Technical Detail
Power
Requirements
Voltage Range:
(All 3880 system components)
85 - 264 VAC
Frequency Range:
50 - 60 Hz
Max Consumption:
3885-B Base Station
< 65 VA during charging, 388 5 -B
3886 Multi-Gas Unit
< 10 VA
Battery Capacity
3880 Monitor:
14.8 V at 6 Ah Lithium Polymer
3885-T Remote Tablet:
7.4 V at 6 Ah Lithium Polymer
3881/3882 W ireless PODS:
3.7 V at 1200 mAh Lithium Polymer
Battery Operation
Time
3880 Monitor:
>8 hours with NIBP readings every 5 minutes
3885-T Remote Tablet:
>10 hours
3881/3882 Wireless PODS:
>12 hours
Battery Charge Time
3880 Monitor:
< 5 hours to 90% capacity
3885-T Remote Tablet:
< 5 hours to 90% capacity
3881/3882 Wireless PODS:
< 3 hours to 90% capacity
Power On
Boot Time:
< 4 seconds
Technical Parameters
Technical Detail
Operating
All 3880 system components
Temperature Range:
+10○ to + 40○ C (+50○ to + 104○ F)
Humidity Range:
5% to 85% RH, non-condensing
Altitude Range:
0 – 5000 meters, Pressure: 1010hPa – 540hPa
Storage
All 3880 system components
Temperature Range:
-20○ to + 50○ C (-4○ to + 122○ F)
Humidity Range:
5% to 95% RH, non-condensing
Altitude Range:
0 – 5000 meters, Pressure 1010hPa – 540hPa
Technical Parameters
Technical Detail
3880 Monitor
MR Environment Safety:
MRI Conditional
Magnetic Field Limit:
30,000 Gauss
MRI System:
0.5 to 3.0 Tesla MRI Systems
3881/3882 Wireless PODS
MR Environment Safety:
MRI Conditional
SAR:
≤4 W/kg whole body average SAR
Magnetic Field Limit:
30,000 Gauss
MRI System:
0.5 to 3.0 Tesla MRI Systems
3885-T Remote Tablet
MR Environment Safety:
MRI Conditional
Magnetic Field Limit:
15,000 Gauss
3885-B Base Station
MR Environment Safety:
MRI Unsafe
Accessories
MR Environment Safety:
MRI Safe as listed in Section 9.1-9.7
3886 Multi-Gas Unit
Magnetic Field Limit:
MR conditional 600 gauss
3880 Monitor
< 40 VA during charging
10.1.1.7. Environmental Specifications
10.1.1.8. MRI Conditions
10-5
10.1.1.9. Recorder
Technical Parameters
Technical Detail
Technique:
Thermal line recorder at 3885-B Base Station
Data Type:
Single or Dual Waveform; Tabular
Paper Speed:
12.5 or 25mm/sec continuous
Technical Parameters
Technical Detail
Technique:
Cardiac or Peripheral
Digital Pulses:
3.3 p-p signal with a pulse duration of 10ms ± 3ms
Technical Parameters
Technical Detail
Lead Set Configuration:
3 and 5 lead
Lead Color:
AAMI/AHA and IEC
Lead Configurations:
I, II, III, V, AVF, AVR, AVL
Lead Fail:
Passive, sensing signal imbalance
Input Impedance:
> 2.5MΩ (according to IEC 60601‐2‐27, 50.102.3)
Electrode Contact
≤ 20K ohms @ 10 Hz
Heart Rate:
30 - 250 bpm
Heart Rate Accuracy:
± 1% or ± 5 BPM, whichever is greater
Heart Rate Resolution:
1 beat per minute (BPM)
Heart Rate T-Wave
1.3 mV with a 1mV QRS amplitude
Cardiotach Sensitivity:
200 μV minimum
Cardiotach Bandwidth:
0.5 - 40 Hz
Heart Rate (HR)
Averaging Method:
Five point Mean filter
Heart Rate Meter
Irregular Rhythm:
A1: Ventricular bigeminy: 40 BPM
A4: Bidirectional systoles 90 – 110 BPM
Response Time of Heart
in Heart Rate:
HR change from 80 to 120 BPM: 5 sec
Time to Alarm for
B1 ‐ Vent Tachycardia
Gain 2.0 (9.7, 12.6, 8.9, 11.8, 8.3) Average: 4.01 seconds
10.1.1.10. Gating
10.1.1.11. Vital Signs
10.1.1.11.1. ECG
Impedance:
Rejection:
Accuracy and Response
to
Rate Meter to Change
Tachycardia:
A2: Slow alternating ventricular bigeminy: 30 BPM
A3: Rapid alternating ventricular bigeminy: 59 BPM
HR change from 80 to 40 BPM: 9 sec
1 mVpp, 206 BPM:
Gain 0.5 (12.03, 11.04, 14.1, 11.8, 11.4) Average: 6.25 sec (The
monitoring system may temporarily exit the alarm condition
during the arrhythmia waveform duration.)
Gain 1.0 (11.9, 11.6, 9.2, 9.6, 10.9) Average: 2.59 seconds
Gain 2.0 (8.8, 9.1, 10.3, 9.4, 12.1) Average: 3.93 seconds
B2 ‐ Vent Tachycardia
2 mVpp, 195 BPM:
Gain 0.5 (9.0, 10.4, 12.3, 8.1, 10.4) Average: 3.99 seconds
Gain 1.0 (8.4, 7.7, 12.5, 7.7, 8.3) Average: 1.82 seconds

10-6
10.1.1.11.2. SpO2
Technical Parameters
Technical Detail
Technique:
Masimo SET®
Saturation Range:
1% - 100%
Saturation Accuracy:
± 2.1% at 70% - 99% (full scale)
< 70% oxygen saturation is unspecified
Saturation Resolution:
1%
Pulse Rate Range:
30 - 240 ppm
Pulse Rate Accuracy:
± 3 ppm
Pulse Rate Resolution:
1 pulse per minute (PPM)
Wavelength Range:
660 nm / 905 nm Note: Wavelength range can be especially useful to
clinicians
Emitted Light Energy
< 1.2mW maximum average at 905nm
Calibration Range:
70 - 100%
Minimum sensor Bend
Radius
4 cm (1.6 inches)
SpO2 averaging time:
6 seconds
Technical Parameters
Technical Detail
Technique:
Oscillometric
Modes:
Manual, Automatic and STAT
Measurement Time:
< 60 seconds typical; standard adult cuff
Systolic Measureable
Adult/Pediatric: 40 - 270 mmHg (5.3 - 36 kPa)
Diastolic Measureable
Adult/Pediatric: 25 - 245 mmHg (3.3 - 32 kPa)
Mean Measureable
Adult/Pediatric: 30 - 255 mmHg (4 - 34 kPa)
Pressure Accuracy:
Max. Std. Deviation: <8 mmHg (1.1 kPa)
Pressure Resolution:
1 mmHg (0.1 kPa)
Pulse Rate Range:
30-240 ppm
Pulse Rate Accuracy:
± 1% or ± 5 BPM, whichever is greater
Max Cuff Inflation
Adult/Pediatric: 270 mmHg
Pressure Transducer
0 - 300 mmHg (0 - 40 kPa)
Transducer Accuracy:
The greater of ± 2 mmHg or 2% of the reading
Overpressure Protection:
Adult: 300 mmHg (40 kPa) < 2 seconds
Initial Pressure:
Adult: 165 mmHg (22 kPa)
STAT Mode:
3 consecutive NIBP Readings
Minimum Time Between
Auto: 30 seconds (non STAT)
10.1.1.11.3. NIBP
Pressure Range:
Pressure Range:
Pressure Range:
Pressure:
Range:
Neonatal: 30 - 130 mmHg (4 - 17 kPa)
Neonatal: 10 - 100 mmHg (1.3 - 13 kPa)
Neonatal: 15 - 120 mmHg (2 - 16 kPa)
Max. Mean Error: within ± 5mmHg (±0.7 kPa)
Neonatal: 140 mmHg
Pediatric: 300 mmHg (40 kPa) < 2 seconds
Neonatal: 150 mmHg (20 kPa) < 2 seconds
Pediatric: 165 mmHg (22 kPa)
Neonatal: 100 mmHg (13.3 kPa)
All initial pressures ± 15 mmHg (2 kPa)
Readings:
Manual: 5 seconds

10-7
10.1.1.11.4. CO2 Only, Internal System
Technical Parameters
Technical Detail
Technique:
Sidestream, Non-dispersive infrared absorption technique
Range:
0-15% CO2, or partial pressures at STP: 0-115 mmHg, or 0 - 16 kPa,
Accuracy:
± 0.43 Vol% +8%, or ± 3.75 mmHg +8%, or ±0.5kPa +8%
Resolution:
1 mmHg, 0.1%, 0.1 kPa
Warmup Ti me:
< 10 seconds (concentrations reported and full accuracy)
Response Time:
< 5 seconds for sample, 150mS waveform response
Flow Rate:
80 ± 20 ml/min
Calibration:
Automatic
Technical Parameters
Technical Detail
Source:
Capnogram
Range:
3 - 120 breaths per minute
Accuracy:
1 bpm
Resolution:
1 bpm
Technical Parameters
Technical Detail
Technique:
Sidestream, Non-dispersive infrared (NDIR) absorption
technique
Warmup Ti me:
< 20 seconds (concentrations reported and full accuracy)
Response Time:
≤ 5 seconds
Flow Rate:
50 ± 10 ml/min
Calibration:
Automatic
Drift of Measurement
None
Accuracy degradation wi th rate
Above 80 RPM, end-tidal agent measurements will
to the respiration rate as follows: ET=80Et(nom)/RR
CO2 and Respiration
Ranges and accuracy same as 10.1.1.11.4 and 5 above
N2O Range:
0 - 100 vol%
N2O Accuracy:
± 2 vol% + 2%
N2O Resolution:
1%
Primary Agent ID
0.15 vol%
Secondary Agent ID
0.20 vol% + 10% of total agent concentration
Multiple Agent (>2) Detect
0.20 vol % +/- 10% of total agents concentration
Sev Range:
0 - 10 vol%, accuracy ±0.15vol% +5%
ISO, HAL, ENF Range:
0 - 8%, accuracy ±0.15vol% +5%
Des Range:
0 - 22%, accuracy ±0.15vol% +5%
Sev, ISO, HAL, ENF, DES Accuracy:
± 0.15 vol% + 5%
Sev, ISO, HAL, ENF, DES Resolution:
0.1%
Interfering Gas Effects
Tested according to IEC 80601-2-55
Nitrous Oxide
No effect at 60%
Halothane
No effect at 4%
Enflurane
No effect at 8%
Isoflurane
No effect at 8%
Sevoflurane
No effect at 8%
Xenon
-10 % of reading @ 80 vol%
Helium
-6 % of reading @ 50 vol%
10.1.1.11.5. Respiration
10.1.1.11.6. Multi-Gas, Agents, P/N 3886
typically decrease below the nominal value in proportion

10-8
Desflurane
+12 % of reading @ 15 vol%
Ethanol
No effect at 0.3 vol%
Isopropanol
No effect at 0.5 vol%
Acetone / Metabolic Ketones
No effect at 1 vol%
Methane
No effect at 3 vol%
Carbon Monoxide
No effect at 1 vol%
Nitrogen Monoxide
No effect at 0.02 vol%
Oxygen
No effect at 100 vol%
10.1.1.11.7. O2 (Part of 3886)
Resolution
1%
Range
0 to 100 %
Accuracy 0 to 59%
+/- 3%
Accuracy 60 to 100%
+/- 5%
Technical Parameters
Technical Detail
Technique:
Direct Fiber-Optic
Range:
30 - 44○ C (86 – 111.2○ F)
Accuracy:
± 0.3○ C (±0.54○ F)
Extended Range:
10○ C to 50○ C (50○ F to 122○ F)
Extended Range
Accuracy:
±0.4○ C (±0.72○ F)
Resolution:
0.1○
Response Time:
< 20 seconds
Application Type:
Axillary or skin surface
Message
Trigger Condition
Priority
Apnea
Respiration detection system ( CO2 / Multi-Gas) reports Apnea
High
Agent Unit Connecting
Indicates 3880 attempting to make connection with 3886 Multi-gas Unit
N/A
Check Print Door
Printer door is not fully closed
N/A
CO2 Occlusion
Gas sampling line is occluded
Med
CO2 Overscale
Co2 measurement exceeds range of the display scale
Low
CO2 Zeroing
Performing a Zero reference in gas system
N/A
COMM LOSS
Wireless communication loss with 3885-B for more than 4 seconds
Low
Crit Mon Batt
≤ 5% of battery capacity in 3880 monitor
Med
Crit Tab Batt
≤ 5% of battery capacity in 3885-T Remote Tablet
Med
Data Delay
Display update error or delay possible
High
ECG Batt Crit
Battery level in ECG transmitter POD at extreme low level
Med
ECG Inop
Hardware or software failure detected
Med
ECG Lead Fail
Lead wire has no electrical connection to the patient or ECG level overscale
Low
EtCO2 Cal Error
Calibration error detected
Med
10.1.1.11.8. Temperature
B. Messages, Alerts, Alarm Priority

10-9
Gas System Inop
Hardware or software failure detected in a gas measurement system
Med
Gas System Warmup
CO2/Multi-Gas unit warming up
N/A
LAN Conn Error
LAN connection errors preventing communication
Low
Low ECG Batt
≤ 15% of battery capacity left in ePOD
Low
Low Mon Batt
≤ 15% of battery capacity left in 3880 monitor
Low
Low SpO2 Batt
≤ 15% of battery capacity left in oPOD
Low
Low Sig IQ
SpO2 unit reports Signal IQ Low
Low
Low Tab Batt
≤ 15% of battery capacity left in 3885-T Remote Tablet
Low
Low Perfusion
Low perfusion detected by SpO2
Low
Mag Field High
Agent bench magnetic field limitations surpassed
Med
Multi Agent MAC
The MAC value consists of more than one agent
Med
Mixed Agents
More than two agents may be present
Med
NIBP Cal Error
Calibration error detected
Med
NIBP Delayed
NIBP reading start held for blood flow
N/A
NIBP Inop
Hardware or software failure detected
Med
NIBP Leak
Air leak is detected
Low
NIBP Occlusion
Occlusion is detected
Med
NIBP Over Press
Pressure exceeds 300 mmHg for Adult / Ped or 150 mmHg for Neonatal
patients
greater than 90 seconds
Low
NIBP Time Out
Pressure remains the same for more than 30 seconds or if
measurement exceeds 180 seconds
Low
No Sample Line
CO2 sampling line disconnected, 3886 Only
Low
Out of Paper
Recorder paper has run out at Base
Low
POST Fail
Power on self-test failure
Med
Recorder Inop
Hardware or software failure detected in Base recorder
Low
Recorder Off Line
Print head is too hot or communication loss to the recorder/Base
Low
Radio Inop
Radio failure detected with comm to 3885 Base/Tablet
Med
SEE MESSAGES!
Critical message area full
High
Sp02 Batt Crit
Battery level in SpO2 transmitter POD at extreme low level
High
SpO2 Noisy
SpO2 unit reports noisy signals from sensor
Low
SpO2 Hi Light
SpO2 unit reports high ambient light at sensor
Low
SpO2 Bad Probe
SpO2 sensor damaged or not compatible
Low
SpO2 Inop
Hardware or software failure detected
Med
SpO2 No Probe
SpO2 sensor is disconnected from the oPOD
N/A
SpO2 Probe Off
SpO2 sensor is not properly attached to the patient
Med
SpO2 Searching
Searching for patient pulse
N/A
SW Mismatch
Software version difference between 3880 components
Low
Temp Inop
Hardware or software failure detected
Med
Temp Probe Fail
Broken sensor detected or a sensor is not attached properly
Low
Wrong Cuff
NIBP system detects an incorrect cuff size for the selected patient mode
Low
-or15 mmHg remains in the line for Adult / Ped or 5mmHg for Neo for
All vital signs with alarm limits use high priority indication for violations.
Priority is indicated with visual and audible indications:
Low – Blue, Medium – Yellow, High – Red. See section 4.1.4

10-10
Watch Dog Fail Safe timeout indicated by continuous audio alarm tone and flashing red alarm dome.
C. Repair
All repairs on products under warranty must be performed by Iradimed Corporation personnel, or
an authorized Iradimed Corporation Service and Repair Center.
Unauthorized repairs will void the warranty.
If a device fails to function properly or requires maintenance, contact Iradimed
Technical Service at 1-407-677-8022 within the U.S., +001-407-677U.S.(during normal business hours EST), or by E-mail at
Corporation Technical Service will advise you
to return the device to Iradimed
a.
Obtain a Return Authorization Number. This will ensure proper routing and
Corporation for repair, please do the following:
of the corrective action required. If you are advised
techsupport@iradimed.com. Iradimed
8022 from outside the
facilitate timely repair of your monitoring device.
b.
Clean monit o ring device prior to shipment. Do not ship contaminated product
to IRadimed Corporation for repair.
c.
Package the monitoring device with adequate protection. If available, use the
original carton and packing materials in which the monitoring device was
d.
e.
shipped
Include a brief description of the problem as well as the name, address and phone
number of the person to be contacted for additional
Include a purchase order with the monitoring devic e being returned if it is out of
from Iradimed Corporation.
information.
warranty; Iradimed Corporation Technical Services can advise you of your
monitoring devic e’s warranty status if need be. Repairs will be made at
Iradimed Corporation’s current list price for the replacement part(s) plus a
reasonable labor charge.
f.
Ship the monitoring device transportation prepaid, to the location specified by your
Iradimed Corporation Service Representative with the Return Authorization
Number written on the outside of the shipping carton.
Repairs will be made,
normally, within two (2) weeks and the monitoring device will
prepaid.
To ensure full reliability, it is recommended that all repairs be made by an Iradimed
Authorized Service and Repair center. For repair at your facility, a
competent individual
experienced in the repair of monitoring device can repair the monitoring device only IF
authorized by Iradimed Corporation Technical Service prior to the repair.
CAUTION: No repair should ever be attempted by anyone not having a
knowledge of the repair of Iradimed Corporation monitoring device. Only replace
parts with components manufactured or sold by Iradimed Corporation.
Corporation Technical Service and Repair Center for service
and technical assistance.
Corporation
be returned to you
Corporation
it is
complete
damaged
Contact the Iradimed

10-11
D. Masimo SETTM Technology
D.1. Masimo SET Principles of Operation
The Masimo SET ® MS pu lse oximeter is based on three princi ples:
1. Oxyhemoglobin and deoxyhemoglobin differ in their absorption of red and infrared light
(spectrophotometry).
2. The volume of arterial blood in tissue and the light absorbed by the blood changes during
the pulse (plethysmography).
3. Arterio-venous shunti ng is highly variable and that fluctuating absorban ce by venous blood
is a major compo nent of noise during the pulse.
The Masimo SET® MS pulse oximeter as well as traditional pulse oximetry determines SpO
passing red a nd infrared light i nto a capillary bed an d m easuring changes in light absorpt ion
during the pulsatile cycle. Red and infrared light-emitting diodes (LEDs) in oximetry sensors
serve as the light sources, a photodiode serves as the photodetector.
Traditio nal pulse oximetry assumes that all pulsations in the light absorbance sig nal are caused
by oscillations in the arterial blood volume. This assumes that the blood flow in the region of the
sensor passes entirely through the capillary bed rather than through any arterio-venous shunts.
The traditional pulse oximeter calculates the ratio of pulsatile absorbance (AC) to the mean
absorbance (DC) at each of two wave l engths, 660 nm and 905 nm:
• S(660) = AC(660)/DC(660)
• S(905) = AC(905)/DC(905)
The oximeter then calculates the ratio of these two arterial pulse-added absorbance signals:
• R = S(660)/S(905)
This value of R is used to find the saturation SpO
software. The values in the look-up table are based upon human blood studies against a
laboratory co-oximeter on healthy adult vol unteers in induced hy poxia studies.
The Masimo SET ® MS bo ard pulse oximeter assumes that arterio-venous shuntin g is highly
variable and that fluctuating absorbance by venous blood is the major component of noise
during the pulse. MS board decomposes S(660) and S(905) into an arterial signal plus a noise
component and calculates the ratio of the arterial signals without the noise:
• S(660) = S1 + N1
• S(905) = S2 + N2
• R = S1/S2
Again, R is the ratio of two arterial pulse-added absorbance signals and its value is used t o find
the saturation SpO
in the empirically derived equation are based upon human blood studies against a laboratory
co-oximeter on healthy adult volunteers in induced hypoxia studies.
The above equations are combined and a noise reference (N’) is determined:
• N’ = S(660) - S(905) x R
If there is no noise N’ = 0: then S(660) = S(905) x R which is the same relationship for the
traditional pulse oximet er .
The equation for the noise reference is based on the value of R, the value being sought to
determine the SpO
correspond to SpO
R-values. The S(660) and S(905) signa ls are processed with each possible N’ noise reference
in an empirically derived equation into the oximeter’s software. The values
2
. The MS board software sweeps through possible values of R that
2
values between 1% and 100% and gener at es an N’ value for each of th ese
2
in a look-up table built into the oximeter’s
2
by
2

10-12
through an adaptive correlation canceler (A CC) which yields an output power for each possible
MEASURED A
VALUES
Range
A
90-100 %
1.30 %
80-90 %
1.78 %
70-80 %
2.80 %
Range
A
70-100 %
± 2.1 %
Overall Claimed Accuracy Value
value of R (i.e., each possible SpO
from 1% to 100%). The result is a Discrete Saturation
2
Transform (DST™) plot of relative outpu t power versus possibleSpO2 value as sho wn i n th e
following figure w he r e R corresponds to SpO
= 97%:
2
RMS
RMS
RMS
SpO2 Performance information of measured A(rms) accuracy shown in tabular form by range.
Graphic plots below of sampled points from blood study w it h Iradimed 1170 FO Se ns or :

10-13

10-14
E. Internal CO2 Only, and Masimo Multi-Gas Systems Detail Operation
Term
Explanation
AA
Anesthetic Agent
BTPS
Body Temperature and Pressure Saturated
delay time
The delay time is defined as the time required for
result
in
10% of
the
final value
Et cone.
End-tidal (expired) concentration
Fi cone.
Inspired gas concentration
harmful
Substances introduced in the patient circuit to an
the patient
ICU
Intensive Care Unit
LEG!
Light Emitting Gas Inlet. Status indicator
integrat ed in the gas sample inlet port
MAC value
1 MAC (Minimum Alveolar Concentration) is the
response to a noxious or surgical stimulus
MOD
Medical Device Directive
MRI
Magnetic Resonance Imaging
The 3880 MRI Patient monitoring system has two options for gas measurement. There being a
‘built in’ CO2/Respi ra ti on only option and an externally packaged Multi-Gas option with full
automatic anesthetic agent identification as well as ‘fast’ parametric O2, known as P/N 3886.
The ‘built in’ CO2 only option is housed within the 3880 monitor unit and operable to the full
magnetic limits of the 3880 monitor unit, 30,000 Gauss. Using the Parameter Setup menu, the
user can select CO2 only which will activate this internal CO2 unit and display CO2 waveform,
Et and Fi CO2 as well as respiration this in te r nal unit measures.
Likewise, from the Parameters Setup menu the operator can select Agents which turns off the
internal CO2 only unit and causes the 3880 monitor unit to co m m unicate with the exter nal 3886
Multi-Gas unit. The 3880 now displays CO2 waveform, Et and Fi CO2, respiration, anesthetic
agents, N2O, and 02 from the 3886 unit. The core of the 3886 is the Masimo/Phasein ISA
sidestream OR+ Multi-Gas system which includ es the Servomex Pm1116 Fast Oxygen
transducer. These devices have a long history o f su cc essful deployment in various non-MRI
monitors. The 3886 unit, provides magnetic and RF shielding allowing use in MR with magnetic
fields up to 600 Gauss, as such the 3886 is to be mounted on the MR gas machine or other
fixed position below 600 Gauss.
Terms and definitions
Specific terms and definitions used in this manual and explained below:
substances
a step function change at the
amount that may cause harm to substances
alveolar concentration (end-tidal) of the agent at
which 50% of individuals fail to move in
sampling site
to

10-15
OR
Operating Room
rise time
Time required to achieve a rise from 1O % to
90 % of final value when a step function
sampling site
sampling
A sampling line configuration consists of a
spontaneous breathing patient
STP
Standard Temperature and Pressure:
Total
Time from a step function change in gas level
time
USS
Universal Serial Bus
zeroing
Ambient gas reference measurement used to
calibration point for the oxygen
measurements
change in concentration occurs at the
line config
system
response
time
Nomoline Family sampling line connected to
either a patient breathing circuit or
101.3 ± 4 kPa atmospheric and gas pressure
22 ± 5 °C ambient temperature
at the sampling site to the ach ievement of
90% of the final gas reading of the gas
monitor.
Total s y s tem response time= Delay time+ Ris e
establish zero concentration levels
N
and Anesthetic Agents, as well as a
O
2
for CO
,
2
E.1.1. Warnings an d Cautions
To avoid water conden s ati on inside the ISA module an d the c onnecting tubings,
ensure that the surrounding temperatur e of the IS A mo du le a nd th e co nnecting tubings
does not fall below the am bi en t t em perature of the Nomoline sa m pl in g line.
E.1.2.
ISA OR+
The 3886 Multi-Gas Unit contains the Masimo ISA OR+ which is a low-flow sidestream
multigas analyzer designed to monitor respiratory
mixtures containing any two of the five anesthetic agents
Sevoflurane and Desflurane in the OR and the ICU. Its low sampling flow and low agent
identification threshold makes the ISA AX+ a perfect choice for adult and pediatric
applications, as well as for the m onitoring of infant patients with low tidal volum es and high
respiratory rates .
ISA OR+ sidestream analyzer offers the addition of oxygen
means of an integrated paramagnetic O
In the following information regarding the 3886 Multi-Gas Unit, the Masimo term “OR+” is
used interchangeably.
3886 Multi-Gas Unit
sensor.
2
concentrations of CO
Halothane, Enflurane, lsoflurane ,
measurement capabilities by
N
,
2
O and gas
2

10-16
E.2.
Theory and design, 3886 Multi-Gas System
E.2.1.
The measurement of CO
gases
Gas measurements and identification
N
O and anesthetic agents is based on the fact that different
,
2
2
absorb infrared light at specific wavelengths. The analysis of respiratory gases by
the ISA gas analyzers are therefore performed by continuously measuring the infrared
light absorption in the gas flow through an infrared spectrometer. Oxygen, on the other
hand, does not absorb infrared light to the same extent as other breathing gases and is
therefore measured using alternative methods.
The gas analysis
The heart of the ISA gas analyzer is the multi-channel spectrometer which uses a
proprietary broadband infrared radiation source to transmit light through the gas sample.
Before reaching the gas sample, the light path is intersected by narrowband optical filters
that only allow light corresponding to selected wavelength peaks of the measured gases
to pass. At the other end of the light path, a sensor detects the portion of the light that is
not absorbed by the gas. The amplitude of the detector output is an inverse function of
the gas concentration.
Thus, at a concentration of zero, the amplitude is at its maximum.
If the gas sample is a mix ture of several components that absorb light at t he s a me
wavelength, such as a mixture of two anesthetic agents, the absorbed radiation will be
the sum of the absorption of the agents. To determine the concentration of each of the
individual gases, several filters have to be used. The ISA gas analyzers therefore uses
the SIGMA spectrometer, which contains up to nine different narrowband filters to
O and a mixture of any two of the five
facilitate simultaneous measurement of CO
anesthetic agents.
N
,
2
2
JS
Figure 4-1. Gas absorption spectra.
The selection of the optical filters within the spectrometer is crucial to the characteristics
and performance of the gas analyzers. The ISA spectrometer uses the strong absorption
peaks at
and 4.5 µm for CO
10 µm long
wave infrared range (LWIR) for the anesthetic agent calculations. The LWIR
and N
2
O measurements and five wavelengths in the 8 to
2
contains strong absorption peaks for the anesthetic agents and negligible interference
from other common respiratory gases, such as alcohol and acetone, which could degrade

10-17
measurement accuracy.
In addition to the measurement filters, two optical filters appropriately located within the 4
to 10 µm range are used as references.
E.2.2. Oxygen measuremen t , Paramagnetic
Oxygen does not absorb infrared light to the same extent as other breathing gases and is
therefore measured using alternative methods. The ISA OR+ analyzer is fitted with a
paramagnetic oxygen sensor.
Paramagnetic oxygen analysis
Paramagnetic oxygen analysis is based on measurements of the attractive force exerted
by a strong magnetic field applied to the oxygen molecules in a gas mixture. The
paramagnetic analyzer distinguishes oxygen from other gases as a function of their
magnetic susceptibility. Due to its paramagnetic nature, oxygen is attracted into the
magnetic field, while most other gases are not. On a scale, where oxygen is assigned the
value 100, most other gases have a magnetic susceptibility of close to zero.
The Servomex sensors
The oxygen sensor included in the 3886 Multi-Gas system as part of the ISA OR+ gas
analyzer is the Pm1116 paramagnetic oxygen sensor from Servomex. In these sensors, a
symmetrical non- uniform magnetic field is created. If oxygen is present, it will be attracted
into the strongest part of this field. Two nitrogen-filled glass spheres are mounted on a
rotating suspension within the magnetic field. Centrally on this suspension, a mirror is
mounted. A light beam projected on the_mirror is reflected onto a pair of photocells.
Oxygen attracted into the magnetic field will push the glass spheres from the strongest
part of the magnetic field, causing the suspension to rotate.
When this rotation is detected by the photocells, a signal is generated and passe d t o a
feedback system. The feedback system will pass a current around a wire mounted on the
suspension, causing a restoring torque that keeps the suspension in its original position.
The current flowin g ar o und th e wire is measured. This curr e nt i s dire c t l y prop or t ional to
the oxygen concentration.
Figure 4-2. Oxygen measurement with Servomex paramagnetic oxygen sensors.
The most important benefits of the paramagnetic oxygen sensor are:
•
Fast rise time
•
High stability and accuracy
•
No chemicals to replace or renew
•
Low maintenance requirement

10-18
E.2.3. Sampling
A sidestream gas analyzer continuously removes a gas sample flow from the respiratory
circuit, for example a nasal cannula, a respiratory mask or the Y-piece of an intubated
patient. The gas sample is fed through a sampling line to the gas analyzer. The sampled
gas is usually warm and humid, and cools down in contact with the wall of the sampling
line. Water therefore condenses in form of droplets on the inner wall of the sampling line.
These droplets could potentially occlude the sampling line and interfere with the gas
measurement.
The Nomoline Family
To overcome the shortfalls of current gas sampling solutions, the Nomoline Family
sampling lines have been developed for the ISA sidestream gas analyzers.
Unlike traditional solutions that remove water vapor and collect water in a container, the
Nomoline Family sampling lines incorporates a unique water separation
(NO MO
isture)
section, which removes condensed water. The NOMO section also has a bacteria filter
which protects the gas analyzer from water intrusion and cross contamination.
Figure 4-3 . The NOMO section.
The Nomoline Family sampling lines are specially designed for 50 sml/min low sample
flow applications. The Nomoline Family sample lines have a very low dead space that
,
results in an
possible even at
ultra-fast rise time, making measurements of CO
high respiratory rates. ISA sidestream gas analyzers are therefore
suitable for adult, pediatric and infant patients.
N2O and anesthetic agents
2
The Nomoline Family sampling lines are available in a wide variety of versions for both
intubated and spontaneously breathing patients and in both disposable and ReSposable
configurations - intubated patients can for instance be monitored using the disposable
Nomoline Airway adapter Set or a combination of the multiple patient use Nomoline
Adapter and a disposable Nomoline Extension / T-adapter.
The Nomoline Airway Adapter Set with integrated airway adapter can be used with
intubated patients.
The Nomoline with a male Luer Lock type connector is compatible with any normal
configuration that uses a female Luer Lock connector. When connecting to a T-adapter,

10-19
be sure to use a Masimo T-adapter that samples the gas from the center of the T-adapter
(see below). See section
for ordering details.
12
Flow control
During normal operation, a sidestream gas analyzer is continuously fed with a small
sample gas flow. To pull the gas through the sampling line and maintain a steady flo w, a
high-precision flow control system is required. In !SA sidestream gas analyzers, the flow
control system consists of an integrated micro pump, a zero valve and a flow controller.
The pump is fitted with a low-power brushless motor incorporating three miniature ball
bearings to ensure trouble free operation without the need for regular maintenance. Its
balanced shaft design and integrated pneumatic fil ter virtually eliminates pressure and flow
variations.
System response
In any sidestream gas analyzer, there are three major time parameters characterizing the
system:
•
•
•
Total system response time
Delay time
Rise time
When designing a sidestream gas monitoring system, the physical characterist ics of
several components have to be considered. Parameters such as sampling line volume,
tubing material and the physical design of the sampling interfaces play decisive roles in
determining the responsiveness of the system.
Generally, the total system response time equals the delay time plus the rise time.
The rise time is defined as the time required for a step function change at the sampling
site to bring about a rise from 10% to 90% of the final gas concentration value. The total
numbers of gas fittings together with the physical design of the fittings are examples that
effects the rise time. Fast rise times are important when monitoring infants with high
breathing rates.
The delay time is defined as the time required for a step function change at the sampling
site to result in 10% of the final value. Parameters affecting the delay time are the sample
flow rate, tubing length and tubing inner diameter. In mainstream gas monitoring, where
no tubing exist, the delay time is virtually zero, whereas a sidestream system has a
sample delay time of a few seconds.
Leak test
1.
Connect a Nomoline Adapter and a Nomoline Extension sampling line or equivalent to
the ISA gas analyzer, with the analyzer connected to Masimo Gas Master.
2.
Tightly block the gas inlet of the Nomoline sampling line.
Check the field "Atm press - cuvette press [kPa]" in Masimo Gas Master - the
pressure value will start to rapidly increase, until the internal pump stops.
When the internal pump stops and while keeping the inlet blocked, quickly block the
exhaust port tightl y. When blocked, the "Atm press - cuvette press [kPa]" in Masimo
Gas Master shall be >6 kPa.
3.
Stop the pump by sending parameter "Stop pump" under "Installation & maintenance"

10-20
in Masimo Gas Master.
in the Gas span check.
4.
Wait about 1O seconds until the "Atm press - cuvette press [kPa]"value as shown by the
Masimo Gas Master is stable. Note the value.
5.
Wait additional 10 seconds.
6.
Check that the "Atm press - cuvette press [ kPa]"value has not changed more than 3 kPa in
10 seconds.
7.
If the "Atm press - cuvette press [kPa}" value changes more than 3kPa in 10 seconds,
check tubing and fittings for leakage. If the problem persists, return the analyzer to Masimo
Sweden (see section 9).
Note:
In step 5, if the "Atm press - cuvette press [kPa]" is less than 6 kPa, repeat
steps 1 to 3 blocking the exhaust port quicker.
Gas span calibration
Only perform the gas span calibration if the gas span check fails repeatedly.
Before performing the gas span calibration, ensure that the SETO2 and SETN2O values are
set (if applicable for your gas analyzer model) correctly to match the corresponding calibration
gas.
Span calibration can be performed using gases within the ranges:
4.0% ≤ CO
45% ≤ O
2
30% ≤ N2O ≤ 100% - for ISA Multigas only
≤
2.0%
DES ≤ 12.0% - for ISA Multigas only
11.0%
2 ≤
≤ 100% - for ISA Multigas with Servomex only
The accuracy of the individual components of the calibration gas mixture shall each have
an accuracy of at least +/-0.03 vol% or +/-(0.02 vol% +0.1% of reading), whichever is
greater.
Note
: DES shall be used for span calibration of all 5 agents (HAL, ENF, ISO, SEV, DES).
Note: Gas span calibration should be performed only for the gas components that failed
1.
Warm up the ISA gas analyzer for at least 1 min
2.
Send "Pre span calibration zeroing" and make sure that the surrounding gas is normal air
(21%
3.
For each gas that failed the Gas span check, perform step 4 to 7. Always
perform the span
Example:
4.
Supply the calibration gas and wait for at least 30 seconds.
5.
Send the corr esponding span cal ibration command.
6.
Wait until the gas span calibration is no longer in progress. The calibrationgas can be
turned off when "span calibration is in progress" no longer is set, but the
calibration
paramagnetic
O
2
and 0%
CO
2),
calibration with the gases in order
Span calibration of O
and CO
2
O
, N2O , DES and
2
only, start with O
2
CO
then CO
2
O
continues for about 40 s with a special zeroing during which the Servomex
O
sensor is sensitive to mechanical movements.
2
2
2
span
2
.

10-21
7.
Notes:
If the calibration process fails, the flag SPAN_ERR is set, and will stay
active until the next successful calibration is passed.
Verify the gas readings
As long as no sampling line is connected, an ISA gas analyzer stays in a low-power,
sleep mode. Once the sampling line is connected, the ISA gas analyzer switches to
measuring mode and starts delivering gas data.
E.2.4.
Zeroing ·
The infrared gas analyzer needs to establish a zero reference level for the CO
,
N
0
and
2
2
anesthetic agent gas measurement. This zero calibration is here referred to as
"Zeroing".
ISA sidestream gas analyzers perform Zeroing automatically by switching the gas
sampling from the respiratory circuit to ambient air. The automatic Zeroing takes less
than 3 seconds for ISA CO2 gas analyzers and less than 10 seconds for ISA multigas
analyzers. If the ISA sidestream gas analyzer is fitted with an oxygen sensor, the
automatic Zeroing will also include room air calibration of the oxygen sensor. Since a
successful Zeroing requires the presence of ambient
that the ISA is placed in a well-ventilated place.
During Zeroing, if JSA's
level
will
be different from the gas level at the sampling site
ISA OR+ Multigas
exhaust
gas is
returned to the patient circuit, the returned gas
analyzers normally perform Z eroing directly at startup (with or
air (21% O
and 0% CO
2
ensure
) ,
2
without Nomoline attached), when a steady operating temperature is achieved and
every
thereafter
is changed from sleep mode to measurement mode.
8 h from start up. A Zeroing is also performed when the operating mode
Additional automatic Zeroing can however be performed if the system consider it
necessary.
E.2.5.
Flow reference zeroing
Addition to the Zeroing the ISA sidestream gas analyzer also perform an automatic flow
reference zeroing
1
h from startup and thereafter
zeroing the ISA sidestream gas analyzers switch from gas sampling from the respiratory
circuit to ambient air while the pump is switched off. Hence no flow will be drawn from the
reference inlet. During the automatic flow reference zeroing , which takes less than 8
seconds , the LEGI will be blinking with a green light.
every
96h. During a flow reference

10-22
N2O concentration
in gas mix
Effect on gas reading
Displayed value if true
concentration is 5.0 vol% CO2
0 vol%
0 % relative
5.0 vol%
30 vol%
5.17 % relative
5.3 vol%
60 vol%
10.34 % relative
5.5 vol%
82 vol%
14.14 % relative
5.7 vol%
E.2.6.
Gas data considerations
Gas measurement units
Effects of humidity
N2O , O
The partial pressure and the volume percentage of CO
depend
on the amount of water vapor in the measured gas. The
,
2
calibrated to show 20.8 vol% at actual ambient temperature and humidit y level, instead of
O
showing actual
room air with 0.7
partial pressure. 20.8 vol%
vol% H
concentration (at 1013 hPa this equals for example 25°C and
20
23% RH). The measurement of CO
by the IA-be nch) will
always show the actual partial pressure at the current humidity level.
2,
N
corresponds to the actual
2
O, and anesthetic agents (e.g. all gases measured
2
In the alveoli of the patient, the breathing gas is saturated with water vapor at body
temperature (BTPS). When the breathing gas flows through the sampling line, the gas
temperature will adapt to ambient before reaching the gas analyzer. As the NOMO
section removes all condensed water, no water will reach the ISA gas analyzer. The
relative humidity of the sampled gas will be about 95%.
If
values at BTPS are required, the following equation can be used:
CO
2
and anesthetic agents
2
O
2 measurement will be
O
concentration in
2
where :
EtCO2
Pamb = Ambient pressure sent from ISA [kPa]
= EtC
value sent from ISA [vol %]
O
2
3.8 = Typical partial pressure of water vapor condensed between patient circuit and ISA [kPa)
EtC02(BTPS)
Spectral broadening
The presence of oxygen and nitrous oxide can cause some interference in the CO
measurement. This is known as spectral broadening.
= EtCO
gas concentration at BTPS [vol%]
2
2
Nitrous oxide, N
O:
2
ISA sidestream analyzers automatically compensates for spectral broadening caused by
nitrous oxide.
Below is the typical ef fect if using the default value (0 vol% N20) when measuring on gas
mixtures with different N20 concentrations:

10-23
Oxygen, O2:
Effect on gas
21 vol%
0 % relative
5.0 vol%
50 vol%
-2.76 % relative
4.9 vol%
70 vol%
-4.67 % relative
4.8 vol%
95 vol%
-7.05 % relative
4.7 vol%
ISA OR+ sidestream units automatically compensates for spectral
broadening caused by oxygen
Below is the typical effect if using the default value (21 vol%
mixtures with different O
concentrations:
2
0
)
when measuring on gas
2
O
concentration in
2
gas mix
reading
Displayed value if true
concentration is 5.0 vol% CO
2
E.3. Specifications
E.3.1. Intended use
The ISA OR+ product is intended to be connected to other medical backboard devices for
monitoring of breath rate and the following breathing gases:
ISA OR+: CO
2, O2, N2
ISA OR+ is intended to be connected to a patient breathing circuit for monitoring of inspired
/expired gases during anesthesia, recovery and respiratory care. The intended environment
is the operating suite, intensive care unit and patient room. ISA CO2 is also intended to be
used in road ambulances. The intended patient population is adult, pediatric and infant
patients.
Nomoline sampling cannulas are intended to be used as accessories to the ISA gas
analyzers. They are connected to the nostrils or to the nostrils and mouth on spontaneously
breathing
with CO
patients for sampling of CO
2
sampling. The intended patient population is adult, pediatric and infant patients.
O ,Halothane, lsoflurane, Enflurane, Sevoflurane and Desflurane
•
Some models are also used to deliver O2 in parallel
2

10-24
Sensor head
2 to 9 channel NDIR type gas analyzer measuring at 4 to 10 µm. Dat a
acquisition rate 10 kHz(sample rate 20 Hz/channel)
Compensations
ISA OR+:
Automatic compensation for pressure and temperature.
Manual compensation for broadening effects on CO2
Calibration
No span calibration is required for the IR bench. An automatic Zeroing is
performed typically 1 to 3 times per day.
Warm-u p time
ISA OR+:
identification enabled and full accuracy)
Rise time1
HAL < 400 ms
Primary agent threshold
(ISA OR+)
0.15 vol% When an agent is identified, concentrations will be reported even
below 0.15 vol% as long as apnea is not detected
Secondary agent threshold
(ISA OR+)
0.2 vol% + 10% of total agent concentration
Agent identification time
(ISA OR+)
< 20 seconds (typically < 10 seconds)
Total system response time
ISA OR+ < 4 seconds
(with 2 m Nomoline Airway Adapter Set sampling line)
Gas
Range 1
Accuracy
N2O
0 to 100 vol%
±(2 vol% + 2% of reading)
O2
0 to 100 vol%
±(1 vol%+ 2% of reading)
E.3.2. Gas Analyzer
<20 seconds (Concentrations reported, automatic agent
At 50 sml/min sample flow
ISA OR+
CO2 ≤ 300 ms
N
O, O2, ENF, ISO, SEV, DES < 400 ms
2
1
Measured according to EN ISO 80601-2-55
E.3.3.
Accuracy - standard conditions
The following accu r acy specifications are valid for dry sin gle gases at 22 ± 5 'C and 1013 ± 40 hPa:
CO2 0 to 15 vol%
HAL, ENF, ISO
SEV
DES
0 to 8 vol%
0 to 10 vol%
0 to 22 vol%
±(0.2 vol%+ 2% of reading)
±(0.15 vol% + 5% of reading)
±(0.15 vol% + 5% of reading)
±(0.15 vol% + 5% of reading)

10-25
E.3.4.
Gas
Accuracy
CO2
±(0.5 kPA + 8% of reading)
N2O
±(2 kPA + 5% of reading)
Agents2
±(0.2 kPA + 10% of reading)
O2
±(2 kPA + 2% of reading)
Gas
Gas level
CO2
Agents
N2O of
CO2 only option
3886
ISA OR+
N2O
4)
60 Vol%
- 2)
- 1)
- 1)
- 1)
HAL
4)
4 Vol%
- 6)
- 1)
- 1)
- 1)
ENF, ISO, SEV
4)
5 Vol%
- 6)
- 1)
- 1)
- 1)
DES
4)
15 Vol%
- 6)
- 1)
- 1)
- 1)
Xe (Xenon)
4)
80 Vol%
-10% of reading 3)
- 1)
- 1)
He (Helium)
4)
50 Vol%
-6% of reading 3)
- 1)
- 1)
Metered dose inhaler
propellants
Not for use with metered dose inhaler propellants
C2H5OH (Ethanol)
4)
0.3 Vol%
- 1)
- 1)
- 1)
- 1)
C3H7OH (Isopropanol)
4)
0.5 Vol%
- 1)
- 1)
- 1)
- 1)
CH3COCH3 (Acetone)
4)
1 Vol%
- 1)
- 1)
- 1)
- 1)
CH4 (Methane)
4)
3 Vol%
- 1)
- 1)
- 1)
- 1)
CO (Carbon monoxide)
5)
1 Vol%
- 1)
- 1)
- 1)
- 1)
O2
5)
100 Vol%
- 2)
- 2)
- 1)
- 1)
Accuracy - all conditions
The following accuracy specifications are valid for all specified environmental conditions
except for interference specified in section E3.5 (effects from water vapor partial pressure on
gas readings) and section E3.6 (interfering gas effects).
±(3.75 mmHg + 8% of reading)
±(15 mmHg + 5% of reading)
±(1.5 mmHg + 10% of reading)
1
All gas concentrations are reported in units of volume percent and may be translated into mmHg or kPa by using the
reported atmospheric pressure.
2 The accuracy specification is not valid if more than two agents are present in the gas mixture. If more than two agents
are present, an alarm will be set.
E.3.5.
Effects from water vapor partial pressure on gas readings
When the breathing gas through the sampling lin e, the gas temperature will adapt to the
ambient temperature before reaching the gas analyzer. The mea s ur e m ent of a ll ga s e s wi ll
always show the actu al par t ia l pr e s sur e a t the c ur rent humidity level in t he ga s s am p le. As the
NOMO section remo ve s al l co nd en s ed wa t er, no water will reach the ISA gas analyzer.
However reading will typically be 6% lower than corresponding partial pressure after removal of
all water.
E.3.6.
4)
Interfering gas effects
of 3886
3886

10-26
Note 1: Negligible interference, effect included in the specification “Accuracy, all conditions” above.
Note 2: Negligible interference with N
O / O2 concentrations correctly set, effect included in the
2
specification “Accuracy, all conditions” above.
Note 3: Interference at indicated gas level. For example, 50 vol% Helium typically decreases the CO
readings by 6%. This means that if measuring on a mixture containing 5.0 vol% CO
vol% Helium, the actual measured CO
vol% CO
.
2
concentration will typically be (1-0.06) * 5.0 vol% = 4. 7
2
Note 4: According to the EN ISO 80601-2-55:2011 standard.
Note 5: In addition to the EN ISO 80601-2-55:2011 standard.
Note 6: CO2 Only internal option is contra-indicated for use with anesthetic agents, no interfering gas
testing or specification per EN ISO 80601-2-55 standard.
and 50
2
2

10-27
Symbol
Used for
Symbol
Used For
MR Safe: Completely safe
MR field.
MR Conditional: Use in
operator safety
F. Symbol Conventions and meanings
or
Manufacturer
Manufacturer/ Date of
Manufacture
Use by date; do not use
after the year (YYYY),
month (MM)
Consult Instructions for Use
Non sterile
the MR environment is
restricted to certain
conditions of use to
ensure patient and
or
or
CE Mark
Do Not Reuse
Federal Communications
Commission radio
certification
Authorized EU Representative
for use with no potential
for interaction with the
MR Unsafe: Must not be
used in an MRI
environment
Fragile
Atmospheric Pressure Limits
Humidity Limits, noncondensing
Temperature Limits
QR Code, Unique Device
Identifier
Instructions for Use must be
consulted
Prescription Only
Quantity in Package
Part Number
Serial Number
Lot Number
Defibrillator-proof type
CF equipment (IEC 60601-
1) protection against

10-28
Shock
Radio Source
Protected against harmful
Not for General Waste
–
Gas Inlet
Power On
Battery, negative contact
+
Direct Current
Universal Serial Bus (USB) IPX1
Alarm sound system is
capable of audio sound
triggered by alarms/alerts
Gas Outlet
Power Off
Battery, positive contact
Alternating Current
effects of dripping water per
IEC 60529
Audio Alarms Off; ALARM
conditions can visually
indicate, if ALARM not OFF
Audible Alarms Paused
(includes 120 second
countdown timer adjacent to
symbol)
Alarm condition is occurring
All Alarms Off: Indefinitely
pauses all alarms and
terminates automatic NIBP
measurements
Connected to AC mains
3880 Patient Monitor battery
life
Wireless Signal Strength
3885-T Remote Tablet battery
life
3881 ECG ePOD battery life
No Battery, or Battery unable
3881 SpO2 oPOD battery life
Heartbeat Detected
to communicate remaining
life
Fuse
Settings button: Access
monitor setup menus
Trend button: Trend Screen
access and adjustment

10-29
NIBP START/STOP button:
readings.
RECORD button: Starts strip
chart recorder for hard copy
printout at recorder in the
optional 3885-B Base Station
Initiates a NIBP measurement
when one is not in progress,
or stops an NIBP in progress.
Holding START/STOP button
for 3 seconds initiates STAT

10-30
G. Manufactures Technical Declaration
Guidance and manufacturer’s declaration—electromagnetic emissions
The 3880 System is intended for use in the electromagnetic environment specified below.
Emissions Test
Compliance
Electromagnetic environment - guidance
RF emissions
Group 1
The 3880 System must emit electromagnetic
Nearby electronic equipment may be affected.
RF emissions
CISPR 11
Class B
The 3880 System is suitable for use in all
Harmonic
61000-3-2
Not applicable
Voltage
61000-3-3
Not applicable
EMC Information Tables as required by EN 60601-1-2:2007 Clause 5
In accordan ce with EN 60601-1-2:2007 Medical Electrical Equipment – Part 1-2: General
requirements for safety – Collateral standard: Electromagnetic Compatibility – Requirements and
tests
1. “Medical Electrical Equipment needs special precautions regarding EMC and needs
to be installed and p ut into servi ce according to the EMC information provided in the
Accompanying Documents” (the following tables).
2. “Portable and Mobile RF Communications Equipment can affect Medical
Electrical Equipment”.
3. “The equipment or system should not be used adjacent to or stacked with other
equipment and that if adjacent or stacked use is necessary, the equipment or system
should be obse rved to verify normal operation in the configuration in which it is used”.
The following tabl es (as required in EN 60601-1-2:2007) provide information regarding the
Electromagnetic Compatibility (EMC) of this product and its accessories.
Table 201—Guidance and manufacturer’s declaration— electromagnetic emissions—for all EQUIPMENT and SYSTEMS
The customer or the user of the 3880 System should assure that it is used in such an
CISPR 11
emissions IEC
fluctuations/flicker
emissions IEC
energy in order to perform its intended function
(remote communications within an specific band for
WLAN; i.e. 2.431 to 2.474 GHz).
establishments other than domestic and those
directly connected to the public low-voltage power
supply network that supplies buildings used for
domestic purposes.

10-31
3880 System
Guidance and manufacturer’s declaration—e lectromagnetic immunity
The 3880 System is intended for use in the electromagnetic environment customer or the user of the 3880 System should
assure that i t is used in such an
Immunity test
IEC 60601 test
level
Compliance level
Electromagnetic environment - guidance
Electrostatic discharge
(ESD)
IEC
±6 kV contact
±8 kV air
±6 kV contact
±8 kV air
Floors should be wood, concrete, or ceramic
tile. If floors are covered with synthetic material,
the relative humidity should be at least 30 %.
Electrical fast
transient/burst
IEC 61000
±2 kV for power
supply li nes
input/output lines
±2 kV for power supply
lines
lines
Mains powe r quality shoul d be that of a typical
commerci al or hospital environment.
Surge
IEC 61000
±1 kV differential
mode
±2 kV
mode
±1 kV differential mode
±2 kV common mode
Mains powe r quality shoul d be that of a typical
commerci al or hospital environment.
Voltage dips, short
<5 % UT (>95 %
<5 % UT (>95 % dip in
Mains powe r quality shoul d be that of a typical
interruptions, and volta ge
variations on power supply
input lines
IEC 61000
dip in UT) for 0.5
cycle
40 % UT (60 %
dip in UT) for 5
cycles
70 % UT (30 %
UT) for 0.5 cycle
40 % UT (60 % dip in
UT) for 5 cycles
70 % UT (30 % dip in
commercial or hospital environment. If the user
of the 3880 System requires continued
operation during power mains interruptions, it is
recommended that the 3880 System be
powered from an uninterru ptible power supply or
a
dip in UT) for 25
cycles
<5
UT) for 25 cycles
<5 % UT(>95 % dip in
dip in UT) for 5
sec
UT) for 5 sec
Power frequency (50/60
Hz) magnetic field
IEC 61000
3 A/m
3 A/m
Power frequency magnetic fields should be at
levels characteristic of a typical location in a
typical c om mercial or hospital environment.
NOTE—UT is the a.c. mains voltage prior to application of the test level.
Table 202—Guidance and manufacturer’s declaration— electromagnetic immunity—for all EQUIPMENT and SYSTEMS
environment.
61000-4-2
-4-4
-4-5
-4-11
-4-8
±1 kV for
common
% UT(>95 %
±1 kV for input/output
battery.

10-32
Table 203—Guidance and manufacturer’s declaration— electromagnetic immunity—for LIFE-SUPPORTING EQUIPMENT and SYSTEMS
Guidance and manufacturer’s declaration —electromagnetic immunity
The 3880 System is intended for use in the electromagnetic environment customer or the user of the 3880 System
Immunity test
IEC 60601 test
level
Compliance level
Electromagnetic environment - guidance
Portable and mobile RF communicat i ons equipment should be
used no closer to any part of the 3880 System, including
cables , than the rec om mended separation di stance calculated
from the equation applicable to the frequency of the transmitter.
Recommended separation distance
150 kHz to 80 MHz
outside ISM bands
150 kHz to 80 MHz
outside ISM bands
a
where P is the maximum output power rating of the transmitter in
watts (W) according to the transmit ter manufacturer and d is the
recommended separation distan ce in me ters (m).b
Field strengths from fixed RF transmitters, as determined by an
electromagnetic site survey,
c
should be less than the compliance
level in each frequency range.d
Interference may occur in the vicinit y of equip men t mar ked wi th
the following symbol:
IEC 60417, No. 417-IEC5140, "Source of Non-Ionizing Radiation"
Symbol
and people.
a
The ISM (industrial, scientific, and medical) bands between 150 kHz and 80 MHz are 6.765 MHz to 6.795 MHz; 13.553 MHz to 13.567 MHz;
Conducted RF 3 Vrms
IEC 61000-4-6
10 Vrms
Radiated RF 10 Vrms
80 MHz to 2.5 GHz
IEC 61000-4-3
should assure that it is used in such an environment.
a
3 V d = 1.17 ¥ P
10 V
10 V/m
d = 1.20 ¥ P
d = 1.20 ¥ P
d = 2.33 ¥ P
80 MHz to 800 MHz
800 MHz to 2.5 GHz
NOTE 1—At 80 MHz and 800 MHz, the higher frequency range applies.
NOTE 2—These guidelines may not apply in all situations. Electromagnetic propagation is affected by absorption and reflection from structures, objects,
26.957 MHz to 27.283 MHz; and 40.66 MHz to 40.70 MHz
b
The compliance levels in the ISM frequency bands between 150 kHz and 80 MHz and in the frequency range 80 MHz to 2.5 GHz are intended to
decrease the likelihood that mobile/portable communications equipment could cause interference if it is inadvertently brought into patient areas. For this
reason, an additional factor of 10/3 is used in calculating the recommended separation distance for transmitters in these frequency ranges.
c
Field strengths from fixed transmitters, such as base stations for radio (cellular/cordless) telephones and land mobile radios, amateur radio, AM and
FM radio broadcast, and TV broadcast cannot be predicted theoretically with accuracy. To assess the electromagnetic environment due to fixed RF
transmitters, an electromagnetic site survey should be considered. If the measured field strength in the location in which the 3880 System is used
exceeds the applicable RF compliance level above, the 3880 System should be observed to verify normal operation. If abnormal performance is
observed, additional measures may be necessary, such as re-orienting or relocating the 3880 System.
d
Over the frequency range 150 kHz to 80 MHz, field strengths should be less than [V 1] V/m

10-33
3880 System
Recommended separation distances between portable and mobile RF communications equipment and the
The 3880 System is intended for use in an electromagnetic environment in which radiated RF disturbances are
controlled. The customer or the user of the 3880 System can help prev
maintaining a minimum distance between portable and mobile RF communications equipment (transmitters) and
the 3880 System as recommended below, according to the maximum output power of the communications
equipment.
Rated
Separation distance according to frequency of transmitter
m
150 kHz to 80 MHz
150 kHz to 80 MHz in
80 MHz to 800 MHz
800 MHz to 2.5 GHz
0.01
0.12
0.12
0.12
0.23
1
1.17
1.2
1.17
2.33
10
3.8
3.8
3.8
7.67
For transmitters rated at a maximum output power not listed above, the recommended separation distance d in meters (m) can be determined
bands
communications
Table 205—Recommended separation distances between portable and mobile RF communications equipment and the EQUIPMENT or SYSTEM—
for LIFE-SUPPORTING EQUIPMENT and SYSTEMS
3880 System
ent electromagnetic interference by
maximum
output power
of transmitter
W
0.1 0.38 0.38 0.38 0.77
100 11.67 12 11.67 23.33
outside ISM bands
d = 1.17 √ P
ISM bands
d = 1.2 √ P
d = 1.2 √ P
d = 2.33 √ P
using the equation applicable to the frequency of the transmitter, where P is the maximum output power rating of the transmitter in watts (W)
according to the transmitter manufacturer.
NOTE 1—At 80 MHz and 800 MHz, the separation distance for the higher frequency range applies.
NOTE 2—The ISM (industrial, scientific, and medical) bands between 150 kHz and 80 MHz are 6.765 MHz to 6.795 MHz; 13.553 MHz to
13.567 MHz; 26.957 MHz to 27.283 MHz; and 40.66 MHz to 40.70 MHz.
NOTE 3—An additional factor of 10/3 is used in calculating the recommended separation distance for transmitters in the ISM frequency
between 150 kHz and 80 MHz and in the frequency range 80 MHz to 2.5 GHz to decrease the likelihood that mobile/portable
equipment could cause interference if it is inadvertently brought into patient areas.
NOTE 4—These guidelines may not apply in all situations. Electromagnetic propagation is affected by absorption and reflection from
structures, objects, and people.
Recommended separation distances between the 3880 System components and local radio frequency devices, such as WiFi AP devices, for wireless
coexistence: Maintain a 2 meter ( 6’) separation.

10-34
This page is intentionally left blank.

10-35

10-36

10-37
 Loading...
Loading...