Invacare CG101080, IVCGFMO, CG10180CA User Manual

Invacare®Therapeutic Support Surfaces Catalog
Invacare® Therapeutic Support Surfaces
Patients immobilized and unable to move
can suffer serious destruction of the skin
and soft body tissue in as little as one
hour. This often results in the formation
of a pressure ulcer. A pressure ulcer is
defined as any lesion caused by
unrelieved pressure resulting in
underlying tissue damage.
Complications related to pressure ulcers
cause an estimated 60,000 deaths and
cost over $1.3 billion annually.1However,
most pressure ulcers are treatable and
Invacare
even preventable. Therapeutic Support
Surfaces are a proven way to help
Understanding Pressure Ulcers
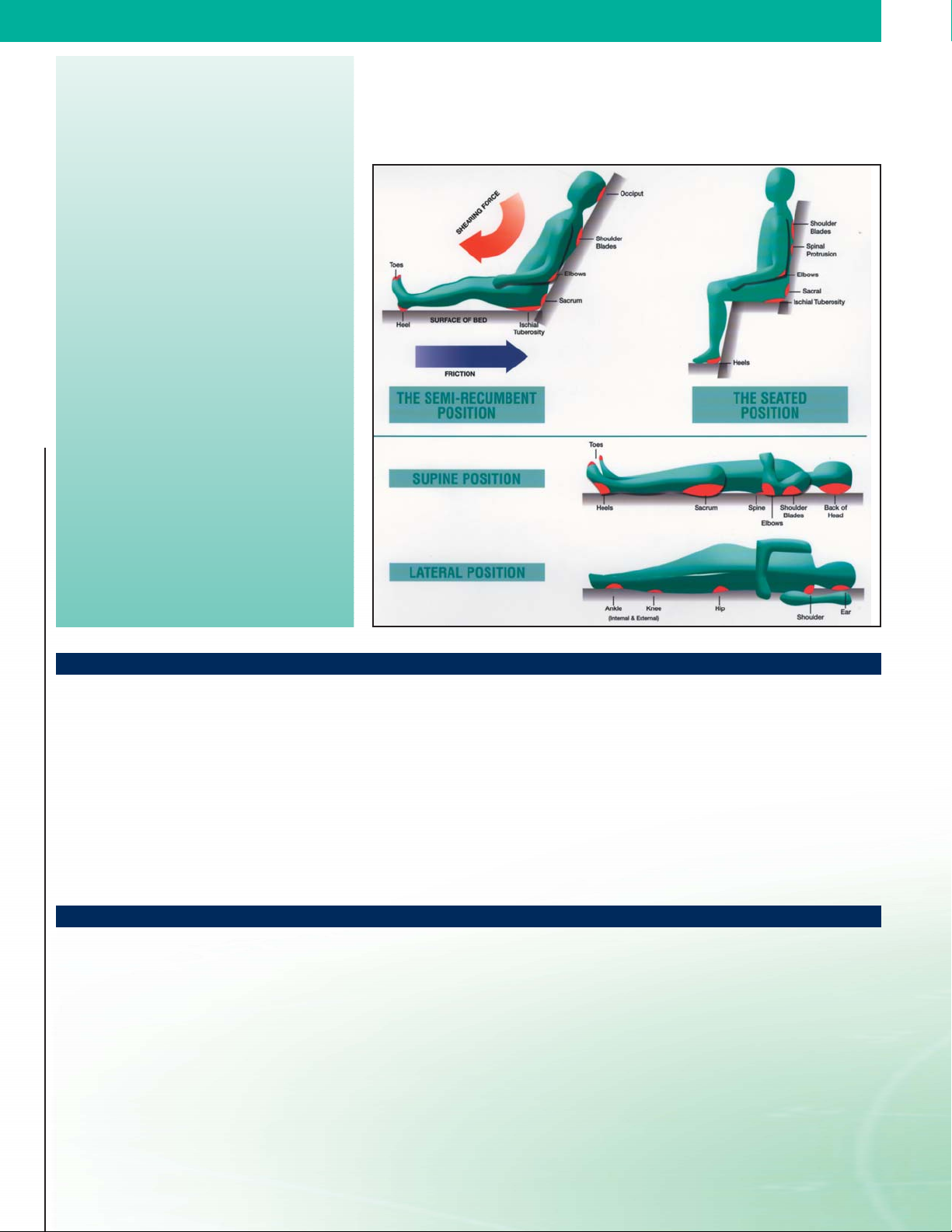
Pressure ulcers are typically located in areas such as heels, elbows, shoulders and
the sacral region and are graded or staged to classify the degree of tissue damage.
The images below identify pressure point areas in different body positions.
®
Therapeutic Support Surfaces
prevent and treat pressure ulcers.
Causes of Pressure Ulcers
Pressure ulcers can be caused by four factors, either individually or in
combination:
• Pressure: Results in compression of soft tissue between a bony
prominence and an external surface, such as a bed. When external
pressure exceeds capillary blood pressure, the blood supply from the
blood vessels to the muscle and skin tissue is impeded, resulting in
tissue breakdown.
• Moisture: Over-hydrates skin, resulting in maceration, which
lowers its resistance to mechanical stresses such as pressure or
friction.
Risk Factors for Pressure Ulcers
Immobility and Inactivity
One of the most important determinants of developing a pressure
ulcer is the ability to move or change positions. Lack of movement can
result in loss of blood flow to the muscles and skin.
Body Shape and Size
Those who are very thin or obese are at a higher risk of developing
pressure ulcers. Very thin people have little cushion between their
skin and bony prominences. Those who are overweight may have
difficulty moving around on their own.
Skin and hygiene
As well as advancing age, some medications or treatments can make
skin thinner and less able to take the wear and tear of everyday life.
2
2
• Shear: Occurs when adjacent surfaces slide across one another,
typically when a patient slides down in bed or chair. The skin
remains stationary against the bed linens while the underlying
tissue shifts. This causes capillaries to stretch and tear, resulting
in reduced blood flow.
• Friction: Caused when the skin is pulled across a coarse surface
such as bed linens, washcloths, or incontinence pads. When friction
is applied to the skin, the outer protective layer is rubbed away. The
soft moist layers of skin are exposed which allow bacteria to enter.
Nutrition
Lack of a balanced diet and sufficient fluids can lead to frail skin.
Infection
An infection can cause an increase in body temperature and
perspiration, resulting in the skin being less supple.
Incontinence
Urine and fecal matter can cause irritation and skin breakdown.
It is important that the skin is cleaned and dried as soon as possible
to minimize maceration.
Circulation
Poor circulation can cause swelling, or edema, in certain areas,
making them less resistant to pressure.
Invacare®Therapeutic Support Surfaces
Therapeutic Support Surfaces
Therapeutic Support Surfaces prevent and treat pressure ulcers by molding to the body
to maximize contact, redistributing weight as uniformly as possible, and reducing
pressure to below capillary closure (32mm/Hg).
have been shown to improve pressure ulcers, there is no compelling evidence that
one support surface consistently performs better than all others, under all circumstances.
The primary concern when choosing a support surface should be the therapeutic benefit
associated with the product.
3
While a variety of support surfaces
Stages of Pressure Ulcers
Pressure ulcers can be graded from Stage
I to Stage IV to classify the degree of
tissue damage. Pressure ulcers do not
necessarily progress from Stage I to
Stage IV or heal from Stage IV to Stage I.
Invacare’s TSS line consists of Group I and Group II surfaces as defined by CMS. Each
Group can further be categorized by the type of surface and whether it is
static.
dynamic or
Group I - Support surfaces designed to prevent pressure ulcers
• Gel Overlay – Uniformly distributes pressure and reduces friction and shear with gel
bladders inside a foam core. Designed to be placed directly on top of an existing
mattress.
• Foam Mattress – Multiple layers of foam for maximum pressure reduction. Designed
to be placed directly on the existing bed frame.
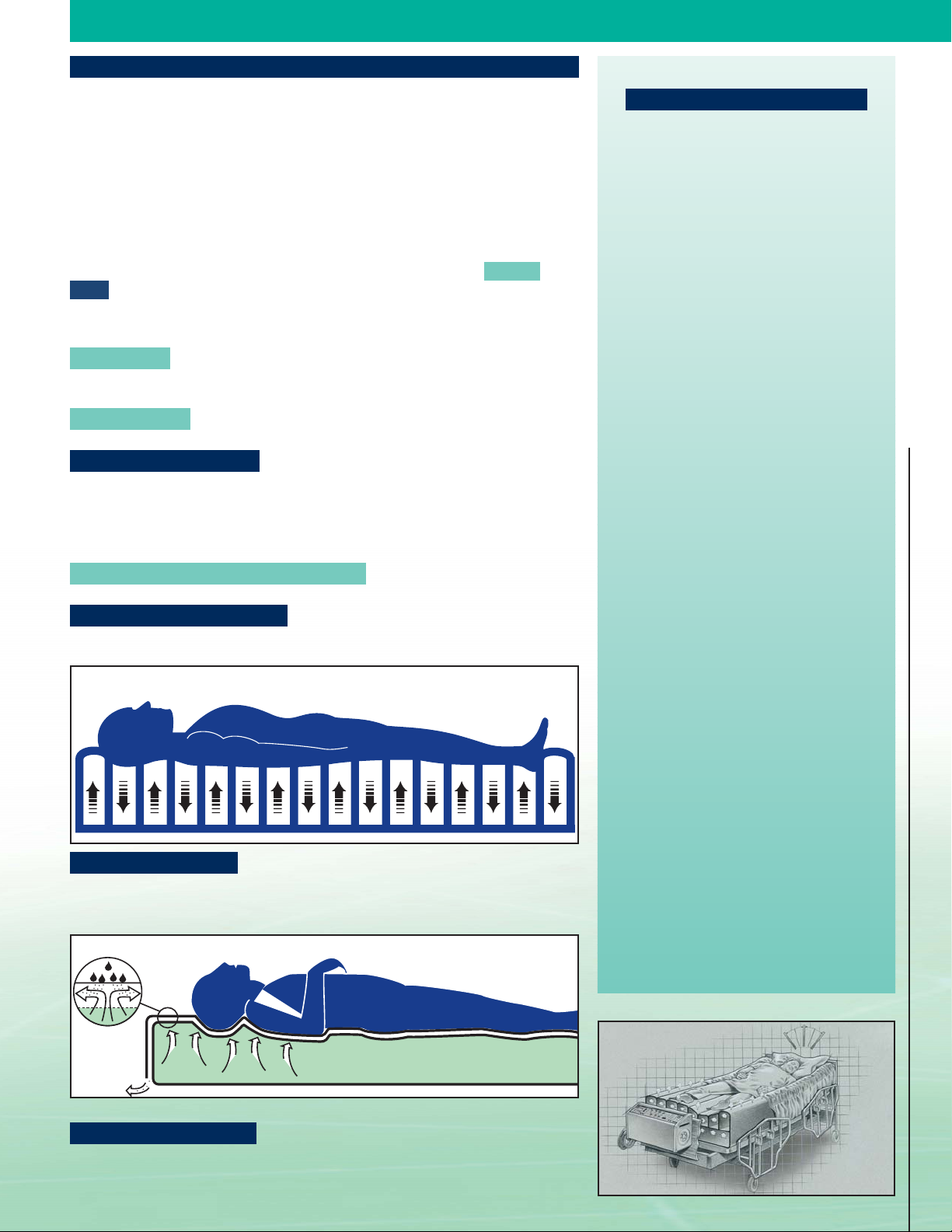
• Alternating Pressure Pad – Alternates inflation and deflation of cells to constantly
change pressure points. Designed to be placed directly on top of an existing mattress.
Group II - Support surfaces designed to prevent and treat pressure ulcers
• Non Powered Pressure Reducing Mattress – Channels air through cells for
maximum patient immersion.
• Alternating Pressure Mattress – Alternates inflation and deflation of cells to
constantly change pressure points and promote circulation.
Alternating Pressure
Stage I: _________________________
Non-blanchable erythema of intact skin,
the heralding lesion of skin ulceration.
In individuals with darker skin,
discoloration of the skin, warmth,
edema, induration, or hardness may
also be indicators.
Stage II: ________________________
Partial thickness skin loss involving
epidermis, dermis, or both.
Stage III: ________________________
Full thickness skin loss involving
damage to or necrosis of subcutaneous
tissue that may extend down to, but not
through, underlying fascia. The ulcer
Invacare
®
Therapeutic Support Surfaces
• Low Air Loss Mattress – Floats the patient on air-filled cells while circulating air
across the skin to reduce moisture and help maintain a constant skin interface
pressure. “True Low Air Loss” utilizes 100-150 liters of air per minute to maintain
normal skin temperature and moisture levels, yet will not dry out therapeutic dressings.
Low Air Loss Pressure
• Lateral Rotation Mattress – Gently rotates the patient from side to side to cyclically
change pressure points. Reduces risk of pulmonary complications, stimulates gastrointestinal tract, improves circulation and provides pressure relief without disturbing
the patient.
presents clinically as a deep crater
with or without undermining adjacent
tissue.
Stage IV: ________________________
Full thickness skin loss with extensive
destruction, tissue necrosis, or damage
to muscle, bone, or supporting structures
(e.g., tendon or joint capsule).
3

Invacare® Therapeutic Support Surfaces
1. Completely immobile
OR
2. Limited mobility or has a pressure ulcer
on the trunk or pelvis, plus one of the following:
-impaired nutritional status
-fecal or urinary incontinence
-altered sensory perception
-compromised circulatory status
1. Multiple stage II pressure ulcers on trunk or pelvis and
-Patient has been on an ulcer treatment program plus
a Group I surface for at least the past month
-Ulcers have worsened or remained the same.
2. Large or multiple Stage III or IV pressure
Invacare
3. Recent myocutaneous flap or skin graft for a
®
Therapeutic Support Surfaces
YES
Require moisture control for
incontinence or perspiration
YES
OR
ulcer(s) on the trunk or pelvis
OR
pressure ulcer on the trunk or pelvis
NO
Standard homecare mattress
NO
Gel overlay, alternating
pressure pad or foam mattress
YES
Low Air Loss
Low Air Loss or Lateral Rotation
This algorithm is a recommended guideline for product selection. It is not a guarantee of product performance.
Patient condition and therapeutic benefit should be the primary drivers of product selection.
NO
Alternating Pressure,
Helpful Hints
• Always follow the directions and advice given by the prescribing
physician.
• Elevate the head of the bed no more than 30˚ whenever possible for
maximum pressure distribution.
• To determine if the patient has bottomed out, place an outstretched
hand, palm up, between the mattress and the patient. The support
surface should have about one-inch of uncompressed surface
between the hand and the patient. If you can feel the patient’s
body, the mattress needs more depth. Either provide a thicker
support surface or add more air to the mattress.
•
Use a static support surface if the patient can assume a variety of
positions without bearing weight on a pressure ulcer.
• Use a dynamic support surface if (1) the patient cannot assume a
variety of positions without bearing weight on a pressure ulcer, or
(2) the patient fully compresses the static support surface.
• Patients should not wear incontinence briefs or pads when using a
therapeutic support surface because they can retain heat and
moisture. Follow existing protocols if available.
• To promote air flow, use flat sheets rather than fitted sheets.
•
When placing a patient on a dynamic surface for the first time,
acclimate them to the therapy by using a static mode for the first
several hours.
4
 Loading...
Loading...