EmblemHealth Medicare Advantage REFERENCE GUIDE

2021 Medicare Advantage
HMO/POS/D-SNP Plans
Reference
Guide

B

2021 EmblemHealth Medicare Advantage HMO/POS
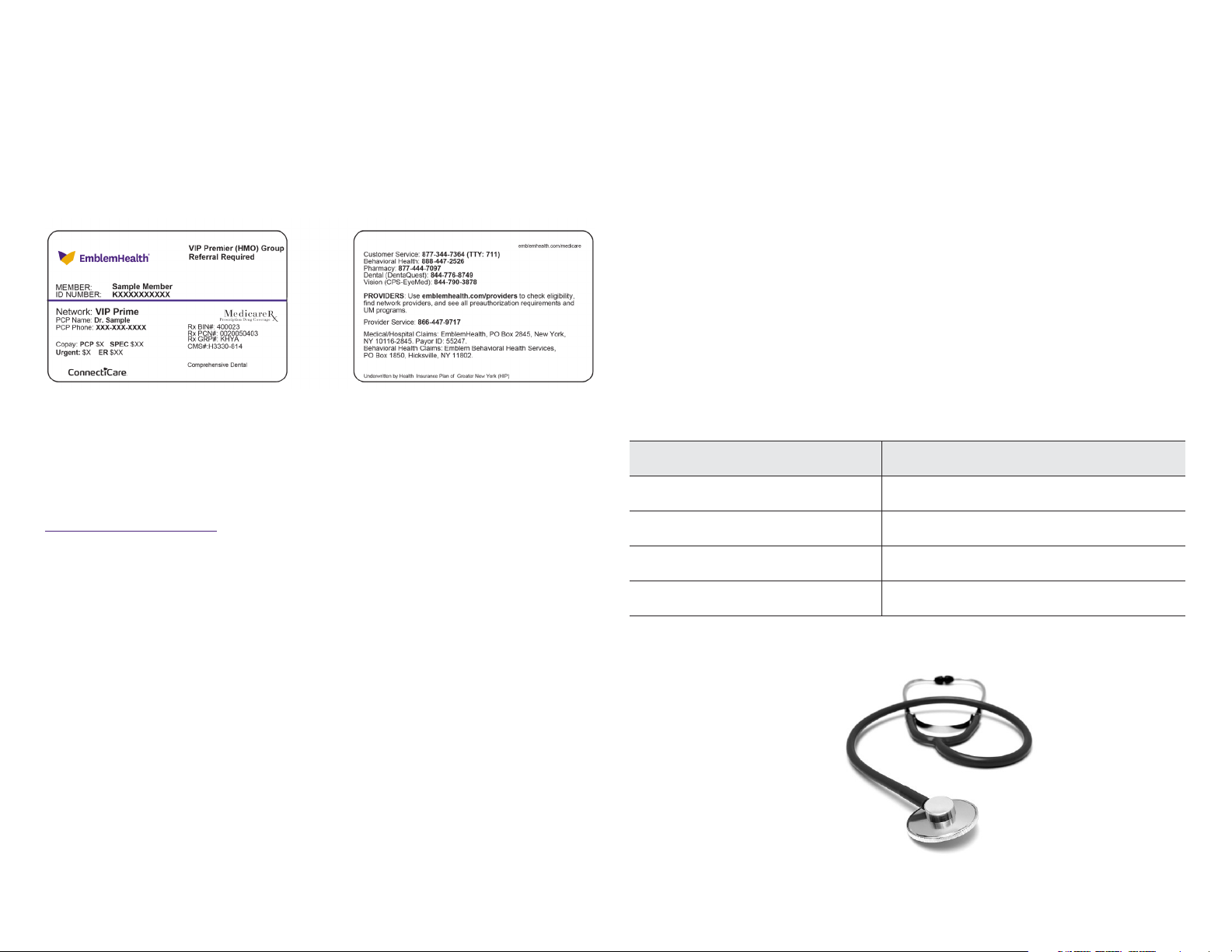
Sample Member ID Card and Plans
No Referral Required
VIP Bold Network
EmblemHealth VIP Dual (HMO D-SNP)
EmblemHealth VIP Dual Select (HMO D-SNP)
EmblemHealth VIP Essential (HMO)
EmblemHealth VIP Go (HMO-POS)
EmblemHealth VIP Gold (HMO)
EmblemHealth VIP Gold Plus (HMO)
EmblemHealth VIP Part B Saver (HMO)
EmblemHealth VIP Passport (HMO)
EmblemHealth VIP Passport NYC (HMO)
EmblemHealth VIP Rx Saver (HMO)
EmblemHealth VIP Solutions (HMO D-SNP)
EmblemHealth VIP Value (HMO)
VIP Reserve Network
EmblemHealth VIP Reserve (HMO)
EmblemHealth VIP Dual Reserve (HMO D-SNP)
Referral Required
VIP Prime Network
EmblemHealth VIP Premier (HMO) Group
EmblemHealth VIP Rx Carve-out (HMO) Group
Click here for a handy, quick reference showing all EmblemHealth plans that do not need a referral.
1

2021 Networks for EmblemHealth Medicare Advantage
HMO/POS Plans
Network and Plan Changes
In 2021, EmblemHealth will be implementing the following changes:
VIP Prime Network to Support Group Plans in 2021
Our VIP Prime Network will continue to be the Medicare network for VIP group plans in
our 24-county Medicare service area. Group plan members require PCPs and referrals
to see specialists.
EmblemHealth Is Offering Two New Medicare Networks with
No Referral Requirements in 2021
EmblemHealth has customized two new Medicare network options for individuals.
All plans will continue to access our vendor partners’ networks and will follow the
same preauthorization rules. Member ID cards will include the name of the new
network and will show “No referral required” on the front of the member ID card.
See sample card on page 3.
VIP Bold is the new network for existing individual plans starting Jan. , . It will
be offered in our 24-county Medicare Advantage service area. Most members will
have access to the ConnectiCare Choice Network. Referrals are no longer required for
members of individual plans.
VIP Reserve is the new network being introduced for our new VIP Reserve individual
plans. The new plans will be available in the Bronx, Manhattan, Queens, and Brooklyn.
Referrals are not required. Because this new network will support our new VIP Dual
Reserve plans, providers in this network will be required to take our annual Special
Needs Plan (SNP) Model of Care training. The new plans being offered with this
network are:
EmblemHealth and ConnectiCare Reciprocity
EmblemHealth’s Medicare Advantage members using VIP Prime and VIP Bold
networks (except Dual SNP members) can use ConnectiCare’s Medicare Choice
Network in Connecticut. Some services are available through delegated networks
and providers only. These include routine vision care and eyewear (EyeMed);
behavioral health (Beacon Health Options); chiropractic, occupational and physical
therapy (Palladian); and dental (DentaQuest).
Similarly, Medicare members using ConnectiCare’s Medicare Choice Network (except
Dual SNP plan members) have access to the VIP Prime Network in New York. Some
services are only available through ConnectiCare’s delegated networks and providers,
such as behavioral health offered through Optum.
ConnectiCare to Offer New Medicare Plans in 2021
• ConnectiCare Choice Dual Basic (HMO D-SNP)
• ConnectiCare Choice Part B Saver (HMO)
See Summary of Companies, Lines of Business, Networks & Benefit Plans for
full details.
Service Area Expansions
The following plans will be sold in additional counties in :
EmblemHealth VIP Solutions: Putnam, Dutchess, Sullivan, Ulster, Albany,
Broome, Columbia, Delaware, Greene, Rensselaer, Saratoga, Schenectady,
Warren, and Washington
• EmblemHealth VIP Reserve (HMO)
• EmblemHealth VIP Dual Reserve (HMO D-SNP)
EmblemHealth VIP Dual Select: Putnam, Dutchess, Sullivan, and Ulster
EmblemHealth VIP Dual: Albany, Broome, Columbia, Delaware, Greene,
Rensselaer, Saratoga, Schenectady, Warren, and Washington
2
Telehealth – A New Benefit
We are happy to offer additional telehealth for PCP, Specialist, individual psychiatry,
mental health, and substance abuse visits starting Jan. . Please see our website for
coding and other telehealth requirements.
New Member IDs for Medicare Dependents
As required by CMS, Medicare Advantage beneficiaries’ dependents will be issued
new, unique member IDs which are not a variation of the subscribers’ IDs. By
Jan. , dependents will all have their own unique member ID cards. Please
check the new ID cards to make note of the new ID numbers and the plan’s referral
requirements, which are also being added to all member ID cards. See the
Member ID Card chapterof the EmblemHealth ProviderManual for sample ID cards.
Health Survey for Medicare and Special Needs
Plan Members
Please encourage your Medicare and Special Needs Plan members to complete the
health risk assessment (HRA) survey over the phone when they get an automated
call from EmblemHealth. This will help our care management team direct them to
appropriate care and support services.
EmblemHealth Member Rewards Program
In 2021, EmblemHealth will continue to offer Medicare Advantage and Special Needs
Plan membersthe EmblemHealth Member Rewards Programto encourage them
to receive primary care and key health screenings. Members will receive a $25 gift
card for each of the following services they receive (earning up to $75 per calendar
year). Please encourage your members to come in for medically appropriate care.
Your claims must be received by December 31 of the calendar year for the incentive
to be paid. Only one reward can be earned for each health service. Timely filing
requirements of 120 days must also be met.
Preventive Services Track Diabetes Track
Annual well-visit Annual well-visit
Breast cancer screening HbA1c test
EmblemHealth Medicare Connect Concierge
Our Medicare members have access to EmblemHealth Medicare Connect
Concierge. This is the one phone number members can call when they need help
solving their health care needs. EmblemHealth Medicare Connect Concierge
can help:
• Make a doctor’s appointment.
• Get referrals for group plan members.
• Coordinate preauthorizations.
• Answer benefit questions.
• Verify mailing address.
• Arrange transportation for members with Medicaid when covered.
To reach Medicare Connect Concierge, please call -- (TTY: ),
8 am to 8 pm, 7 days a week.
Colorectal cancer screening Diabetic eye exam
Flu vaccine Nephropathy screening
3
 Loading...
Loading...