BIOTRONIK SE and KG TACHBORAX Users Manual
Inlexa 1
VR-T, DR-T, HF-T
ICD-Familie | Tachyarrhythmietherapie |
Kardiale Resynchronisationstherapie
Gebrauchsanweisung
420651
Revision: A (2015-12-09)
© BIOTRONIK SE & Co. KG
Alle Rechte vorbehalten.
Technische Änderungen vorbehalten.
® Alle verwendeten Produktnamen können Marken oder eingetragene Marken von
BIOTRONIK oder dem jeweiligen Eigentümer sein.
Index 420651GebrauchsanweisungInlexa 1 VR-T, DR-T, HF-T,
BIOTRONIK SE & Co. KG
Woermannkehre 1
12359 Berlin · Germany
Tel +49 (0) 30 68905-0
Fax +49 (0) 30 6852804
sales@biotronik.com
www.biotronik.com
1
1 Product Description
Product Description1403736Technical Manual
Intended Medical Use
Intended use Inlexa 1 is part of a family of implantable cardioverter-defibrillators (ICDs). The
primary objective of the therapy is to prevent sudden cardiac death. Furthermore,
the device is capable of treating bradycardia arrhythmias and cardiac resynchronization therapy with multisite ventricular pacing.
The implantation of an ICD is a symptomatic therapy with the following objectives:
• Termination of spontaneous ventricular fibrillation (VF) through shock delivery
• Termination of spontaneous ventricular tachycardia (VT) through antitachycardia pacing (ATP); in case of ineffective ATP or hemodynamically not tolerated
VT, with shock delivery
• Cardiac resynchronization through multisite ventricular pacing (triple-chamber
devices)
• Compensation of bradycardia through ventricular (single-chamber devices) or
AV sequential pacing (dual- and triple-chamber devices)
Diagnosis and
therapy forms
Required expertise In addition to having basic medical knowledge, the user must be thoroughly familiar
Indications Inlexa 1 can treat life-threatening ventricular arrhythmias with antitachycardia
Single-chamber and
dual-chamber
The device monitors the heart rhythm and automatically detects and terminates
cardiac arrest resulting from ventricular tachyarrhythmia. All major therapeutic
approaches from the field of cardiology and electrophysiology are included.
BIOTRONIK Home Monitoring
ment at any time.
with the operation and the operation conditions of a device system.
• Only qualified medical specialists having this required special knowledge are
permitted to use implantable devices.
• If users do not possess this knowledge, they must be trained accordingly.
pacing and defibrillation.
Generally approved differential diagnostics methods, indications, and recommendations for ICD therapy apply to BIOTRONIK devices. See the current guidelines of
cardiology associations for guidance.
We recommend observing the indications published by the German Cardiac Society
(Deutsche Gesellschaft für Kardiologie, Herz- und Kreislaufforschung) and the ESC
(European Society of Cardiology). This also applies to the guidelines published by
the Heart Rhythm Society (HRS), the American College of Cardiology (ACC), the
American Heart Association (AHA), and other national cardiology associations.
Single-chamber and dual-chamber ICDs are indicated for patients with the
following risk:
• Sudden cardiac death caused by ventricular arrhythmias
®
enables physicians to perform therapy manage-
Triple-chamber Triple-chamber ICDs are indicated for patients with the following risks:
• Sudden cardiac death caused by ventricular arrhythmias
• Congestive heart failure with ventricular asynchrony

Contraindications Known contraindications:
DF-1
RV
SVC
DF-1 IS-1
RA
IS-1
RV
System Overview
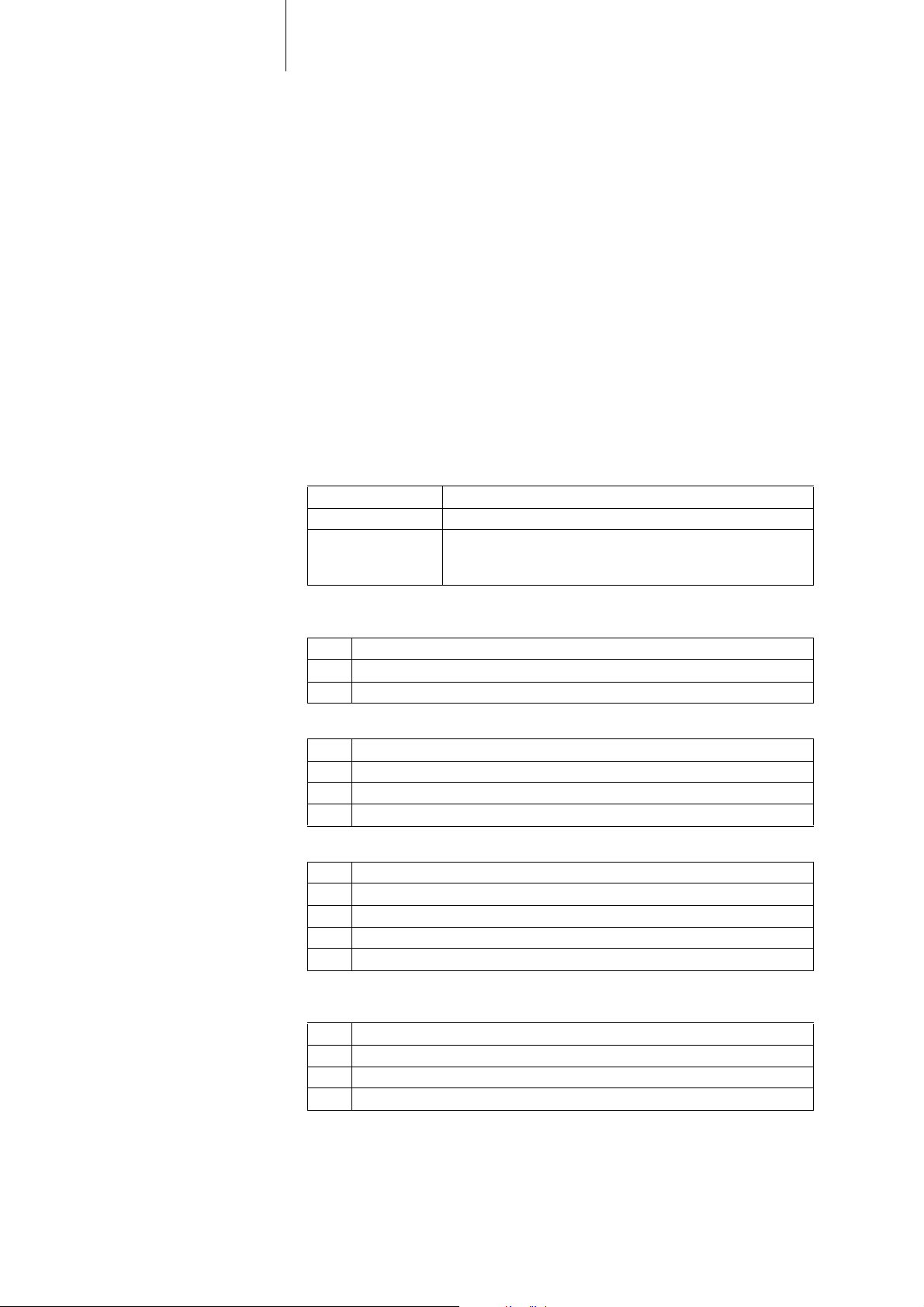
Device family The complete Inlexa 1device family consists of sev eral dev ice types with a DF-1/IS-1
2
• Tachyarrhythmia caused by temporary or reversible irritation, e.g. poisoning,
electrolyte imbalance, hypoxia, sepsis or acute myocardial infarction
• Such frequent VT or VF that the therapies would cause an unacceptably rapid
depletion of the device batteries
• VT with few or without clinically relevant symptoms
• VT or VF treatable by surgery
• Concomitant diseases that would substantially limit a positive prognosis
• Accelerated intrinsic rhythm
connection.
•Single-chamber: VR-T
•Dual-chamber: DR-T
• Triple-chamber: HF-T
Note: Not all device types are available in every country.
Device The device's housing is made of biocompatible titanium, welded from outside and
thus hermetically sealed. The ellipsoid shape facilitates implantation in the pectoral
muscle area.
The connections for bipolar pacing and sensing (and unipolar connections for the
triple-chamber device) as well as for shock delivery are found in the device header.
The housing serves as a potential antipole during shock delivery or in the case of
unipolar lead configuration.
DF-1/IS-1 The labeling on each device provides information pertaining to the connector port
assignment in the header.
VR DR HF
DF-1
SVC
DF-1
RV
Connector
port
IS-1
RV
Lead
connector
DF-1
SVC
DF-1
RV
Configuration Implantation site Device type
IS-1
LV
IS-1
RA
IS-1
RV
RA IS-1 Bipolar Atrium DR, HF
(R)V IS-1 Bipolar (Right) ventricle VR, DR, HF
RV DF-1 Shock coil Right ventricle VR, DR, HF
SVC DF-1 Shock coil Superior vena
VR, DR, HF
cava
LV IS-1 Unipolar, bipolar Left ventricle HF
Leads
BIOTRONIK leads are sheathed with biocompatible silicone. They can be flexibly
maneuvered, are stable long-term, and are equipped for active or passive fixation.
They are implanted using a lead introducer set. Some leads are coated with polyurethane which is known to increase the sliding properties for the lead. Leads with
steroids reduce inflammatory processes. The fractal design of the electrodes
provides for low pacing thresholds. BIOTRONIK provides adapters to connect
already implanted leads to new devices.
3
Telemetry Telemetric communication between the device and the programmer can be carried
out following initialization either by applying the programming head (PGH) to the
device or by using wireless radio frequency (RF) telemetry in the programmer.
BIOTRONIK calls this function SafeSync
Programmer Implantation and follow-up are performed with BIOTRONIK's portable
programmer: Programmer software PSW version N.N. and higher
There is a programmer with integrated RF telemetry and one with a separate
SafeSync Module.
Leadless ECG, IEGM, markers and functions are displayed simultaneously on the
color display.
Using the programmer, the pacing thresholds can be determined and all tests can
be performed during in-office follow-up. If necessary, the current software is transferred to the device during implantation.
In addition to this, the programmer is used to set mode and parameter combinations, as well as for interrogation and saving of data from the device.
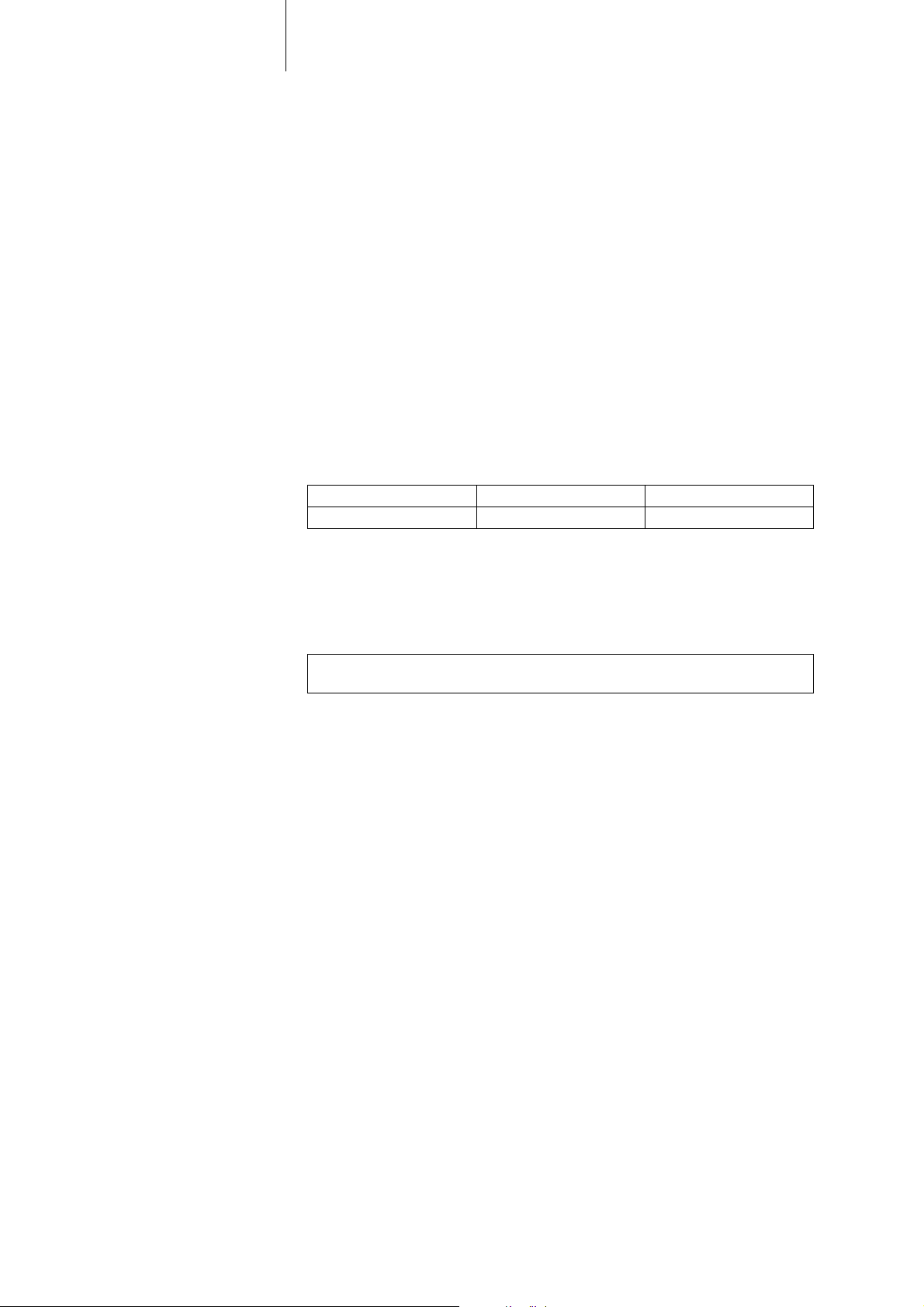
Modes The mode setting depends on the individual diagnosis:
Device type Modes
VR VVI; VVIR; VOO; OFF
DR, HF DDD; DDDR; DDDR-ADIR; DDD-ADI; DDI; DDIR;
VDD; VDDR; VDI; VDIR
VVI; VVIR; AAI; AAIR; VOO; DOO; OFF
®
.
NBD and NBG codes VVE is the NBD code for the antitachycardia mode of the single-cha
chamber, and triple-chamber devices:
V Shock in the ventricle
V Antitachycardia pacing (ATP) in the ventricle
E Detection via IEGM analysis
DDDR is the NBG code for the antibradycardia mode of the dual-chamber devices:
D Pacing in the atrium and ventricle
D Sensing in the atrium and ventricle
D Pulse inhibition and pulse triggering
R Rate adaptation
DDDRV is the NBG code for the antibradycardia mode of the triple-chamber devices:
D Pacing in the atrium and ventricle
D Sensing in the atrium and ventricle
D Pulse inhibition and pulse triggering
R Rate adaptation
V Multisite pacing in both ventricles
VVIR is the NBG code for the antibradycardia pacing modes of the single-chamber
device:
V Ventricular pacing
V Sensing in the ventricle
I Pulse inhibition in the ventricle
R Rate adaptation
mber, dual-
4
BIOTRONIK
Home Monitoring
Inlexa 1order numbers Not all device types are available in every country:
Package contents
®
In addition to effective pacing therapy, BIOTRONIK provides a complete therapy
management system:
• With Home Monitoring, diagnostic and therapeutic information as well as
technical data are automatically sent to a stationary or mobile transmitter via an
antenna in the device header. The data are encrypted and sent from the transmitter to the BIOTRONIK Service Center via the cellular phone network.
• The received data are deciphered and evaluated. Each physician can set the
criteria for evaluation to be used for each patient and can configure the time of
notification via e-mail, SMS or fax.
• A clear overview of the results of this analysis is displayed for the attending
physicians on the protected Internet platform Home Monitoring Service Center
(HMSC).
• Data transmission from the device is performed with a daily device message.
• Device messages which indicate special events in the heart or in the device are
forwarded immediately.
• A test message can be initiated at any time using the programmer to immediately check the Home Monitoring function.
VR-T DR-T HF-T
405797 405796 40579
The storage package includes the following:
• Sterile packaging with device
• Serial number label
• Patient ID card
• Warranty booklet
Note: The technical manual pertaining to the device is either included in hard copy
form in the storage package or in digital form on the internet.
The sterile container includes the following:
• Device, blind plugs (if applicable)
• Screwdriver

5
Therapeutic and Diagnostic Functions
Diagnostic functions • Data from implantation and the most recent interrogations and follow-ups are
recorded as well as arrhythmia episodes; they are stored together with other
data to assess both the patients' and the device's state at any time.
• To check the lead for proper functioning, an automatic impedance measurement using subthreshold pacing pulses is performed in the device.
• Leadless ECG function: For all device types, far-field derivation can be
measured without external leads between the right ventricular shock coil and
housing, which, depending on the implantation site, corresponds to ECG
derivation II or III (Einthoven).
• Once a telemetry connection has been established during a test procedure in an
in-office follow-up, the leadless ECG and the IEGM are displayed with markers.
Antitachycardia pacing • The ICD can treat ventricular tachycardia with antitachycardia pacing (ATP); ATP
can also be delivered in the VF zone (ATP One Shot) when the stability criterion
indicating that this will be effective before shock delivery (monomorphic
rapid VTs) is met.
• Depending on the device type, the device program contains not only the ICD
functions but also all pacemaker functions for 1, 2 or 3 chambers. The heart
rhythm is continuously monitored; each arrhythmia is classified according to
the heart rate and the adjustable detection criteria. Depending on the preset
values, antibradycardia as well as antitachycardia therapy is inhibited or
delivered.
Cardioversion, defibrillation • The ICD can treat ventricular tachyarrhythmia with cardioversion and/or defi-
brillation. Shock polarity and energy can be programmed individually. Shock
energies between 2.0 and 40 J are possible depending on the device family.
Before delivery of the shock, the ICD can be set to only deliver a shock when
ongoing tachyarrhythmia is confirmed; during this time period the device can
identify spontaneous conversion of the tachyarrhythmia and cancel the charging
process if necessary.
• The shock paths can be set between the different shock coils (SVC/RV) and/or
the housing.
Antibradycardia pacing
and CRT
• Innovative rate hystereses, automatic sensor functions, and a night program
promote the patient's intrinsic rhythm, avoid overdrive pacing, and facilitate
adaptation of the device to the individual needs of the patient.
• Thresholds: atrial as well as ventricular pacing thresholds are automatically
determined in the device, automatic threshold monitoring (ATM) for trend
analysis.
• Setting an upper tracking rate for the atrium prevents unspecific atrial pacing,
thus reducing the risk of pacemaker-mediated tachycardia.
• Positive AV hysteresis functions support intrinsic conduction and thus the
natural contraction sequence. Negative AV hysteresis functions support the
cardiac resynchronization therapy by maintaining pacing in stress situations.
• For resynchronization of the ventricles, triple-chamber implants have functions
for multisite pacing with possible VV delays in either direction.
• To ensure that no additional surgery is necessary in case of a left-sided increase
of pacing threshold or undesired phrenic nerve stimulation, different pacing
polarities can be set for the left ventricular lead with a triple-chamber device.
Storing programs There are different therapy programs:
• Parameter settings effective for the most common indications in pre-configured
programs (Program Consult).
• For special indications, individual parameter settings can be stored in up to
three therapy programs.

6
Home Monitoring functions • The device automatically sends information to the transmitter once a day. It also
sends messages related to events, which are immediately forwarded to the
Service Center. In addition to this, test messages can be initiated using the
programmer.
• Appointments for Home Monitoring-supported follow-ups can be scheduled via
the HMSC.
• Important medical information in the device messages include the following:
— Atrial and ventricular arrhythmias
— Parameters relevant to leads in the atrium and ventricle: pacing thresholds,
sensing amplitudes, impedances
— Current statistics
—IEGM online HD
®
with up to 3 high definition channels
7
2 General Safety Instructions
General Safety Instructions2403736Technical Manual
Operating Conditions
Technical manuals The following technical manuals provide information about usage of the device
systems:
— Technical manual for the device
— Technical manual for the HMSC
— Technical manual for the electrodes
— Technical manuals for the programmer and its accessories
— Technical manuals for the user interface
— Technical manuals for cables, adapters and accessories
• Technical manuals are either included in hard copy form in the storage package
or in digital form on the internet: manuals.biotronik.com
• Follow all relevant technical manuals.
• Reserve technical manuals for later use.
Care during shipping
and storage
Delivery in shipment mode The device is delivered in shipment mode to protect the battery; capacitor reforming
Temperature Extremely low and high temperatures affect the service time of the battery in the
Sterile delivery The device and the screwdriver have been gas-sterilized. Sterility is guaranteed only
Sterile packaging The device and screwdriver are packaged in two separately sealed blisters. The
Single use only The device and screwdriver are intended for single use only.
• Devices must not be stored or transported close to magnets or sources of electromagnetic interference.
• Note the effects of the storage duration; see Battery Data.
required during storage could result in controlled extended charge times of the
shock capacitors.
• The shipment mode is displayed on the programmer after the initial interrogation (it is deactivated during implantation by the first valid (in-range) measurement of the pacing impedance).
device.
• Temperatures of +5°C to +45°C are permitted for transport, storage, and use.
if the blister and quality control seal have not been damaged.
inner blister is also sterile on the outside so that it can be transferred in a sterile
state during implantation.
• Do not use the device if the package is damaged.
• The device must not be resterilized and reused.

8
Possible Complications
General information on
medical complications
Skeletal myopotentials Bipolar sensing and control of sensitivity are adapted by the device to the rate range
Possible technical failures Technical failure of a device system cannot be entirely ruled out. Possible causes
Complications for patients and device systems generally recognized among practitioners also apply to BIOTRONIK devices.
• Normal complications may include fluid accumulation within the device pocket,
infections, or tissue reactions. Primary sources of complication information
include current scientific and technological knowledge.
• It is impossible to guarantee the efficacy of antitachycardia therapy, even if the
programs have proven successful during tests or subsequent electrophysiological examinations. In rare cases the set parameters may become ineffective.
It is possible for therapies to induce or accelerate tachycardia and cause
sustained ventricular flutter or fibrillation.
of intrinsic events so that skeletal myopotentials are usually not recorded. Skeletal
myopotentials can nonetheless be classified as intrinsic events especially at very
high sensing sensitivity and, depending on the interference, may cause inhibition or
antiarrhythmia therapy.
In the case of undesired myopotentials, the device switches to asynchronous pacing
if the interference rate is exceeded.
can include the following:
• Lead dislodgement, lead fracture
• Insulation defects
• Device component failures
• Battery depletion
• Interrupted telemetry
Electromagnetic
interference (EMI)
Device behavior in
case of EMI
Static magnetic fields The magnetic sensor in the device detects magnetic fields starting at a magnetic
Any device can be sensitive to interference if external signals are sensed as intrinsic
rhythm or if measurements prevent rate adaptation.
• BIOTRONIK devices have been designed so that their susceptibility to EMI is
minimal.
• Due to the intensity and variety of EMI, there is no guarantee for safety. It is
generally assumed that EMI produces only minor symptoms, if any, in patients.
• Depending on the pacing mode and the type of interference, sources of interference may lead to pulse inhibition or triggering, an increase in the sensordependent pacing rate or asynchronous pacing.
• Under unfavorable conditions, for example during therapeutic or diagnostic
procedures, interference sources may induce such a high level of energy into
the pacing system that the cardiac tissue surrounding the lead tip is damaged.
In case of electromagnetic interference, the device switches to asynchronous
pacing for as long as the interference rate is exceeded.
flux density of approximately 1.5 mT. Magnetic fields below 1 mT do not affect the
sensor.

Possible Risks
Procedures to avoid The following procedures must be avoided, as they may cause harm to the patient
9
or damage the device and, as a result, put the system functionality at risk:
• Transcutaneous electrical nerve stimulation
• Hyperbaric oxygen therapy
• Applied pressures higher than normal pressure
Risky therapeutic and
diagnostic procedures
External defibrillation The device is protected against the energy that is normally induced by external defi-
If electrical current from an external source is conducted through the body for diagnostic or therapeutic purposes, then the device can be subjected to interference,
which can place the patient at risk.
Arrhythmia or ventricular fibrillation can be induced during diathermic procedures
such as electrocautery, HF ablation or HF surgery. For example, damaging
pressure levels may arise during lithotripsy. For example, excessive warming of
body tissue near the device system may occur during therapeutic ultrasound. Influences on the device are not always immediately clear.
If risky procedures cannot be avoided, the following should be observed at all times:
• Electrically insulate the patient.
• Switch off the ICD's detection function. The pacemaker function can remain
active. The device may need to be switched to asynchronous modes for this.
• Do not introduce energy near the device system.
• Additionally check the peripheral pulse of the patient.
• Monitor the patient during and after every intervention.
brillation. Nevertheless, any implanted device may be damaged by external defibrillation. Specifically, the current induced in the implanted leads may result in necrotic
tissue formation close to the electrode/tissue interface. As a result, sensing properties and pacing thresholds may change.
• Place adhesive electrodes anterior-posterior or perpendicular to the axis
formed by the device to the heart at least 10 cm away from the device and from
implanted leads.
Radiation therapy The use of radiation therapy must be avoided due to possible damage to the device
and the resulting impaired functional safety. If this type of therapy is to be used
anyway, prior risk/benefit analysis is absolutely necessary. The complexity of influencing factors such as different sources of radiation, a variety of devices and
therapy conditions makes it impossible to issue directives that guarantee radiation
therapy without an impact on the device. The EN 45502 standard pertaining to active
implantable medical devices requires the following measures during the administration of therapeutic ionizing radiation:
• Adhere to instructions for risky therapy and diagnosis procedures.
• Shield device against radiation.
• After applying radiation, double-check the device system to make sure it is functioning properly.
Note: Please contact BIOTRONIK with questions during the risk/benefit analysis.
Magnetic resonance
imaging
Magnetic resonance imaging must be avoided due to the associated high frequency
fields and magnetic flux density: Damage or destruction of the device system by
strong magnetic interaction and damage to the patient by excessive warming of the
body tissue in the area surrounding the device system.
10
!
!
3 Implantation
Implantation3403736Technical Manual
Implantation Procedure
Having parts ready The following parts that correspond to the requirements of the EC Directive 90/385/
EEC are required:
• BIOTRONIK device with blind plug and screwdriver
• BIOTRONIK leads and lead introducer set
— Single-chamber device: one bipolar ICD lead with 1 or 2 shock coils for the
ventricle
— Dual-chamber device: one bipolar lead for the atrium and one bipolar ICD
lead for the ventricle with 1 or 2 shock coils
— Triple-chamber device: an additional unipolar or bipolar LV lead
• The lead connections DF-1 and IS-1 are permitted. Use only adapters approved
by BIOTRONIK for leads with different lead connections or leads from other
manufacturers.
• BIOTRONIK programmer (with integrated SafeSync RF telemetry or with
separate SafeSync Module) and approved cables
• External multi-channel ECG device
• Keep spare parts for all sterile components.
Keeping an external
defibrillator ready
Unpacking the device
Checking parts Damage to any of the parts can result in complications or technical failures.
To be able to respond to unforeseeable emergencies or possible technical failures
of the device:
• Keep an external defibrillator and paddles or patch electrodes ready.
WARNING
Inadequate therapy due to defective device
If an unpacked device is dropped on a hard surface during handling, electronic
parts could be damaged.
• Use a replacement device.
• Return the damaged device to BIOTRONIK.
• Peel the sealing paper off of the outer blister at the marked position in the
direction indicated by the arrow. The inner blister must not come into contact
with persons who have not sterilized their hands or gloves, nor with non-sterile
instruments!
• Take hold of the inner blister by the gripping tab and take it out of the outer
blister.
• Peel the sealing paper off of the sterile inner blister at the marked position in
the direction indicated by the arrow.
• Check for damage before and after unpacking all parts.
• Replace damaged parts.
• Upon delivery, the tachyarrhythmia therapy function in the ICD is deactivated.
The ICD must only be implanted in this state.
• Leads must not be shortened.
 Loading...
Loading...