BIOTRONIK SE and KG PNP Users Manual
Edora 8 ProMRI
Pacemaker | Bradyarrhythmia Therapy |
Cardiac Resynchronization Therapy
Technical Manual
417803
Revision: B (2016-03-23)
®
© BIOTRONIK SE & Co. KG
All rights reserved.
Specification subject to modification, revision and improvement.
® All product names in use may be trademarks or registered trademarks held
by BIOTRONIK or the respective owner.
0123 2016
Index 417803Technical ManualEdora 8
BIOTRONIK SE & Co. KG
Woermannkehre 1
12359 Berlin · Germany
Tel +49 (0) 30 68905-0
Fax +49 (0) 30 6852804
sales@biotronik.com
www.biotronik.com
2
Table of Contents
Table of Contents
Table of Contents
Product Description . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3
Intended Medical Use. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3
Indications. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
Contraindications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
System Overview. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
Diagnostic and Therapy Functions . . . . . . . . . . . . . . . . . . . . . . 9
General Safety Instructions. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11
Operating Conditions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11
Possible Complications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12
Possible Risks. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13
Implantation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15
Implantation Procedure . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15
Precautionary Measures while Programming . . . . . . . . . . . . 18
Magnet Response . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21
Follow-up . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 22
Patient Information. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 23
Replacement Indications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 24
Explantation and Device Replacement . . . . . . . . . . . . . . . . . . 26
Parameters . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 27
Timing . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 27
Pacing and Sensing . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 30
Rate Adaptation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 32
MRI Program. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 33
Preset Programs . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 34
Tolerances of Parameter Values. . . . . . . . . . . . . . . . . . . . . . . 36
Technical Data . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 37
Mechanical Characteristics . . . . . . . . . . . . . . . . . . . . . . . . . . . 37
Electrical Characteristics . . . . . . . . . . . . . . . . . . . . . . . . . . . . 38
Battery Data . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 40
Legend for the Label . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 42

3
Product Description
Intended Medical Use
1 Product Description
Product Description1417803Technical ManualEdora 8
Intended Medical Use
Intended use
Diagnosis and therapy forms
Required expertise
Edora is a family of implantable pacemakers that can be implanted for all
bradycardia arrhythmia indications. The primary objective of the therapy consists of
improving patients' symptoms that can be clinically manifested. The implantation of
the pacemaker is a symptomatic therapy with the following objective:
• Compensation of bradycardia by atrial, ventricular, or AV sequential pacing
• Additional triple-chamber features: Resynchronization of ventricular chamber
contraction via biventricular pacing
The cardiac rhythm is automatically monitored and bradycardia arrhythmias are
treated. All major therapeutic approaches from the field of cardiology and
electrophysiology are unified in this pacemaker family. BIOTRONIK
Home Monitoring
time.
In addition to having basic medical knowledge, the user must be thoroughly familiar
with the operation of a device system.
• Only qualified medical specialists having the special knowledge required for the
proper use of implanted devices are permitted to use them.
• If users do not possess this knowledge, they must be trained accordingly.
®
enables physicians to perform therapy management at any

Indications
4
Product Description
Indications
Guidelines of cardiological
societies
Device types
Pacing modes
Generally approved differential diagnostic methods, indications, and
recommendations for pacemaker therapy apply to BIOTRONIK devices.
The guidelines provided by cardiology associations offer decisive information:
• We recommend observing the indications published by the German Cardiac
Society (Deutsche Gesellschaft für Kardiologie, Herz- und Kreislaufforschung)
and the ESC (European Society of Cardiology).
• This also applies to the guidelines published by the Heart Rhythm Society (HRS),
the American College of Cardiology (ACC), the American Heart Association
(AHA), and other national cardiology associations.
For the following symptoms/expectations, the following device types are indicated:
Symptom/expectation SR DR HF
Disorientation due to bradycardia x x x
Presyncope x x x
Benefit from resynchronization of the right and left
ventricles
Syncope xxx
For the following symptomatic, the following pacing modes are indicated:
Symptom/expectation Pacing mode
Sick sinus syndrome Dual-chamber pacing
Chronic, symptomatic second and third-degree AV block Dual-chamber pacing
Adams-Stokes syndrome Dual-chamber pacing
Symptomatic bilateral bundle branch block when
tachyarrhythmia and other causes have been ruled out
• Chronotropic incompetence
• Benefit from increased pacing rate with physical
activity
Sinus node dysfunction in the presence of normal AV and
intraventricular conduction
Bradycardia in conjunction with the following:
• Normal sinus rhythms with only rare episodes of
AV block or sinus arrest
• Chronic atrial fibrillation
• Severe physical disability
Dual-chamber pacing
R mode or CLS
Atrial pacing
Ventricular pacing
x
MR conditional
ProMRI® labeled MRI conditional pacemakers are safe for use in the MRI
environment when used in conjunction with a complete MRI conditional pacing
system and according to the instructions given in the ProMRI® manual.

Contraindications
5
Product Description
Contraindications
Guidelines
Pacing modes and parameters
No contraindications are known for the implantation of multifunctional singlechamber, dual-chamber, or triple-chamber pacemakers, provided differential
diagnostics precedes implantation according to the appropriate guidelines and no
modes or parameter combinations are configured that pose a risk to the patient.
The compatibility and effectiveness of parameter combinations must be checked
and, as the case may be, adapted after programming.
Set of facts Contraindicated pacing mode
Additionally implanted ICD Unipolar pacing
Set of facts Inappropriate pacing mode
Chronic atrial tachycardia, chronic atrial
fibrillation or flutter
Poor tolerance of pacing rates above the
basic rate, e.g., angina pectoris
AV conduction disorder Atrial single-chamber pacing
Failing AV conduction
Set of facts Adapt parameters
Slow retrograde conduction after
ventricular pacing: Risk of pacemakermediated tachycardia
Poor tolerance of pacing rates above the
basic rate, e.g., angina pectoris
Atrial-controlled modes (DDD, VDD, AAI)
• Extend atrial refractory period (ARP)
and/or:
• Shorten AV delay
• Rarely:
Program to DDI, DVI or VVI
• Lower atrial upper rate
• Lower maximum sensor rate
• Deploy atrial overdrive pacing

System Overview
6
Product Description
System Overview
Device family
Device
Lead connections
This device family consists of single-chamber, dual-chamber and triple-chamber
devices with or without Home Monitoring. Not all device types are available in every
country.
The following device variants are available:
Device type Variant with
Home Monitoring
Single-chamber Edora 8 SR-T Edora 8 SR
Dual-chamber Edora 8 DR-T Edora 8 DR
Triple-chamber Edora 8 HF-T, Edora 8 HF-T QP —
The device's housing is made of biocompatible titanium, welded from the outside
and therefore hermetically sealed. The ellipsoid shape facilitates ingrowth into the
pectoral muscle area. The housing serves as an antipole in the case of unipolar lead
configuration.
BIOTRONIK provides pacemakers with headers for different standardized lead
connections:
•IS-1
•IS-1/IS4
Note: Suitable leads must comply with the norms:
• A device's IS-1 connector port must only be used for connecting leads with an
IS-1 connector that conform to ISO 5841-3.
• A device's IS4 connector port must only be used for connecting leads with an
IS4 connector that conform to ISO 27186.
Variant without
Home Monitoring
Note: The device and leads have to match.
• Only quadripolar leads must be connected to the IS4 connector on device
type HF QP with IS4.
Note: Use only adapters approved by BIOTRONIK for leads with different connections.
• If you have any questions concerning the compatibility of other manufacturers'
leads, please contact BIOTRONIK.
IS-1
The device labeling provides information pertaining to the connection assignment:
SR DR HF
Connector
port
A/RA IS-1 Unipolar, bipolar Atrium DR, HF
V/RV IS-1 Unipolar, bipolar Right ventricle SR, DR, HF
LV IS-1 Unipolar, bipolar Left ventricle HF
Lead
connector
Configuration Implantation site Device type
7
Product Description
System Overview
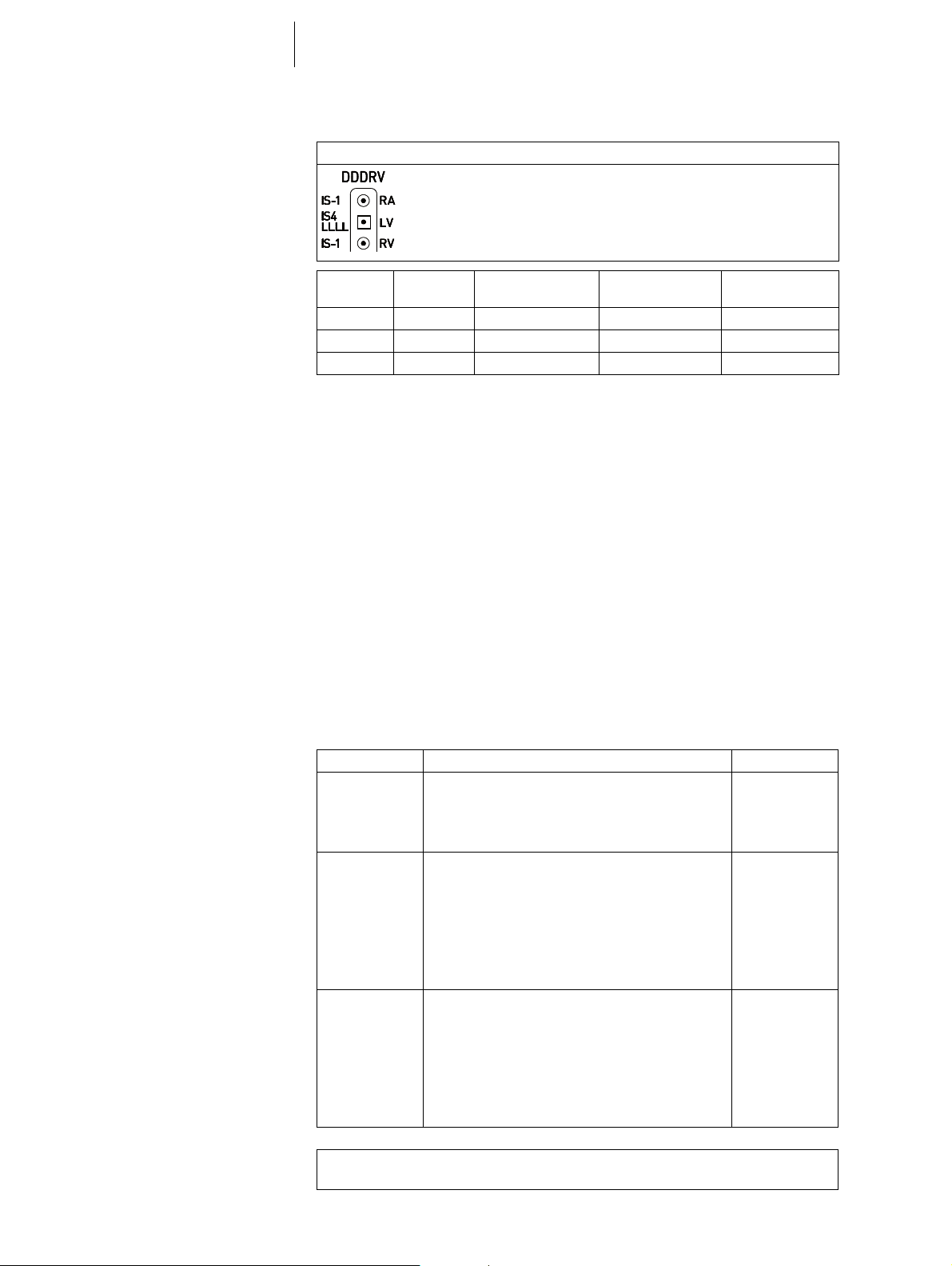
IS-1/IS4
Leads
Telemetry
The device labeling provides information pertaining to the connection assignment:
HF QP
Connector
port
Lead
connector
Configuration Implantation site Device type
RA IS-1 Unipolar, bipolar Atrium HF QP
RV IS-1 Unipolar, bipolar Right ventricle HF QP
LV IS4 Unipolar, bipolar Left ventricle HF QP
BIOTRONIK leads are sheathed in biocompatible silicone. They can be flexibly
maneuvered, are stable long-term, and are equipped for active or passive fixation.
They are implanted using a lead introducer set. Some leads are coated with
polyurethane which is known to increase the gliding properties for the lead. Leads
with steroids reduce inflammatory processes. The fractal design of the leads allows
for low pacing thresholds, high pacing impedance, and a low risk of oversensing.
BIOTRONIK provides adapters to connect already implanted leads to new devices.
Telemetric communication between the device and the programmer can be carried
out following initialization either by applying the programming head (PGH) to the
device or by using wireless wandless telemetry in the programmer.
Programmer
Modes
Using the programmer, the pacing thresholds can be determined and all tests can
be performed during implantation and in-office follow-up. In addition to this, the
programmer is used to set mode and parameter combinations, as well as for
interrogation and saving of data from the device. Leadless ECG, IEGM, markers and
functions are displayed simultaneously on the color display.
The mode setting depends on the individual diagnosis:
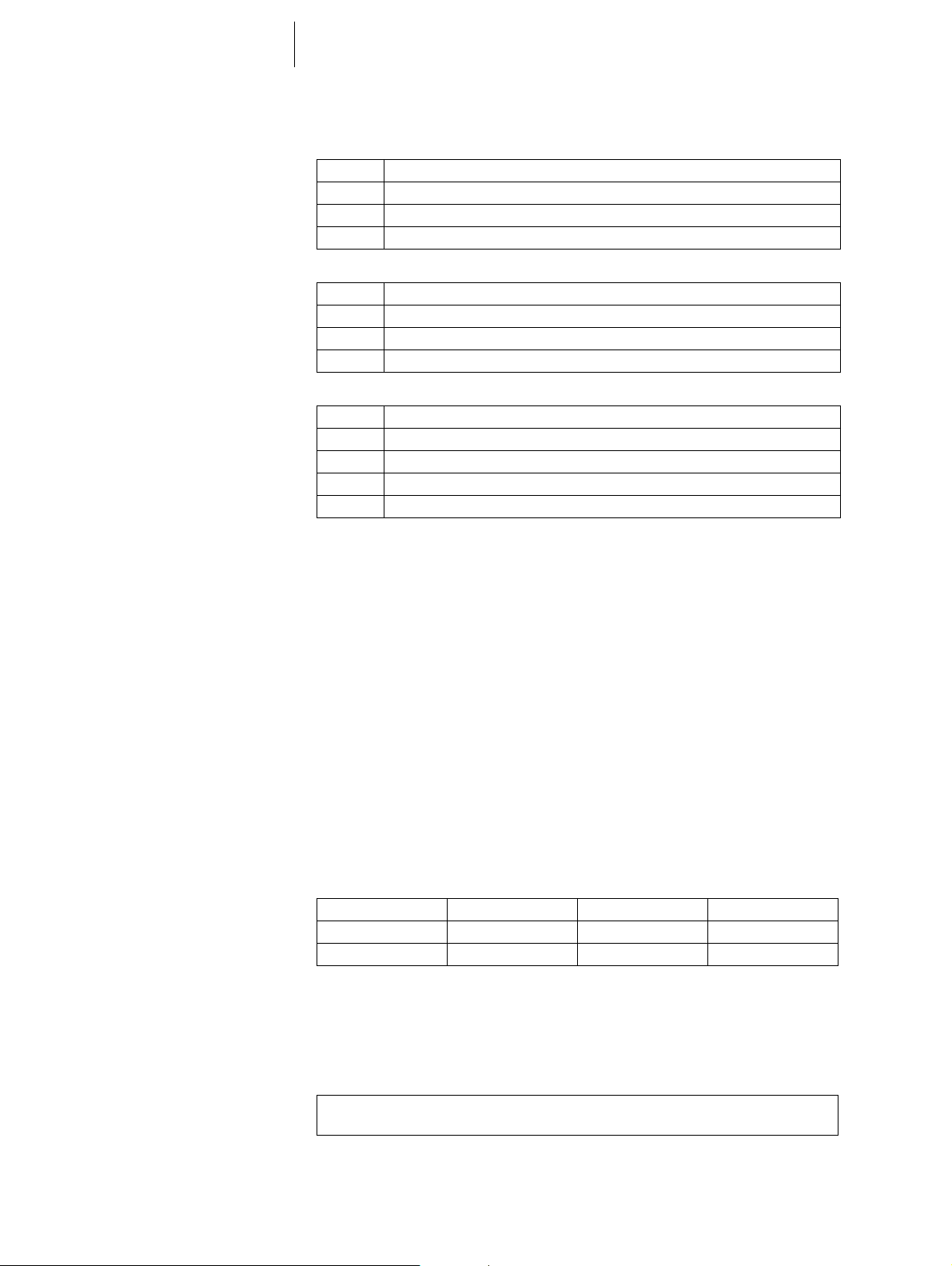
Device type Modes Standard
SR • VVI-CLS
VVIR
• VVIR, V00R, AAIR, A00R
• VVI, VVT, V00, AAI, AAT, A00
•OFF
DR • VVI-CLS; DDD-CLS
DDDR
• DDD-ADI, DDDR-ADIR
• DDDR, DDIR, DVIR, D00R, VDDR, VDIR
• VVIR, V00R, AAIR, A00R
• DDD, DDT, DDI, DVI, D00, VDD, VDI
• VVI, VVT, V00, AAI, AAT, A00
•OFF
HF (QP) • VVI-CLS, DDD-CLS
DDDR
• DDD-ADI, DDDR-ADIR
• DDDR, DDIR, DVIR, D00R, VDDR, VDIR
• VVIR, V00R, AAIR, A00R
• DDD, DDT, DDI, DVI, D00, VDD, VDI
• VVI, VVT, V00, AAI, AAT, A00
•OFF
Note: Home Monitoring is possible in all modes.
The OFF mode only functions temporary, i.e. during a test.
8
Product Description
System Overview
NBG codes
BIOTRONIK Home Monitoring®In addition to effective pacing therapy, BIOTRONIK provides a complete therapy
AAIR or VVIR is the NBG code for the antibradycardia mode of the single-chamber
device:
A/V Pacing in the atrium or ventricle
A/V Sensing in the atrium or ventricle
I Pulse inhibition in the atrium and ventricle
R Rate adaptation
DDDR is the NBG code for the antibradycardia mode of the dual-chamber device:
D Pacing in the atrium and ventricle
D Sensing in the atrium and ventricle
D Pulse inhibition and pulse triggering
R Rate adaptation
DDDRV is the NBG code for the antibradycardia mode of the triple-chamber device:
D Pacing in the atrium and ventricle
D Sensing in the atrium and ventricle
D Pulse inhibition and pulse triggering
R Rate adaptation
V Multisite pacing in both ventricles
management system:
• With Home Monitoring, diagnostic and therapeutic information and technical
data are automatically sent to a stationary or mobile transmitter via an antenna
in the device header. The data are encrypted and sent from the transmitter to
the BIOTRONIK Service Center via the cellular phone network.
• The received data are deciphered and evaluated. Each physician can set the
criteria for evaluation to be used for each patient and can configure the time of
notification via e-mail, SMS or fax.
• A clear overview of the results of this analysis is displayed for the attending
physicians on the protected internet pl
(HMSC).
• Data transmission from the device is performed with a daily device message.
• Device messages, which indicate special events in the patient's heart or in the
device, are forwarded with the following message.
• A test message can be initiated at any time using the programmer to
immediately check the Home Monitoring function.
atform Home Monitoring Service Center
Order numbers for Edora
Package contents
The devices can be obtained as follows:
Edora 8 SR 407164 Edora 8 DR-T 407145
Edora 8 SR-T 407157 Edora 8 HF-T 407138
Edora 8 DR 407152 Edora 8 HF-T QP 407137
The storage package includes the following:
• Sterile packaging with device
• Serial number label
• Patient ID card
• Warranty booklet
Note: The technical manual pertaining to the device is either included in hard copy
form in the storage package or in digital form on the internet.
The sterile packaging includes the following:
•Device
• Screwdriver

9
Product Description
Diagnostic and Therapy Functions
Diagnostic and Therapy Functions
General overview
Diagnostics functions
Antibradycardia pacing
All the systems have extensive features that allow quick diagnosis and delivery of
safe therapy for bradycardia conditions.
• Automatic functions make it easy and fast to implant, configure, and check the
pacemaker.
• Auto-initialization after implantation: The device recognizes the implanted leads
autonomously and sets the polarity. The automatic functions of the software are
activated after 10
• Data from the last interrogations and follow-ups are recorded as well as
arrhythmia episodes; they are stored together with other data to assess the
state of both the patient and the device at any time.
• Continuous automatic below-threshold impedance measurements are
performed in the device independent of the pacing pulse in order to check the
lead for proper functioning.
• Once a telemetry connection has been established during a test procedure in an
in-office follow-up, the IEGM is displayed with markers.
• Sensing: The amplitudes of the P and R waves are measured in the implanted
device fully automatically and permanently to record varying amplitudes. The
sensitivity for the atrium and ventricle is adapted automatically on an ongoing
basis. The measurement data are averaged and the trend can be displayed.
• Pacing thresholds: Pacing thresholds are automatically identified in the device,
in single and dual-chamber devices the right ventricular, in triple-chamber
devices the right and left ventricular pacing thresholds. Capture control adjusts
the pulse amplitudes in such a way that every change of the pacing threshold
results in the patient being paced at an optimal amplitude.
• Timing: Pacing in the atrium is checked particularly carefully in dual and triplechamber devices by an automatic adaptation of the atrial refractory period in
order to avoid pacemaker-mediated tachycardia (Auto PVARP function:
the postventricular atrial refractory period is adapted automatically).
• Additional, special form of rate adaptation: An increased cardiac output
requirement is detected using physiological impedance measurement.
The measuring principle is based on contractile changes (ionotropy) of the
myocardium (CLS function: Closed Loop Stimulation). Rate adaptation is
automatically initialized and optimized in CLS mode.
• Ventricular pacing suppression with devices from the 8 series: Unnecessary
ventricular pacing is avoided by promoting intrinsic conduction (Vp suppression
function). The device can adapt itself to conduction changes. In the case of
intrinsic conduction, the device switches from a DDD(R) to an ADI(R) mode.
• In the course of the follow-up, an automatic test of the AV delay is performed to
improve the heart performance. AV delays are calculated; the optimum values
can be applied.
min.

10
Product Description
Diagnostic and Therapy Functions
Resynchronisation therapy
Programs
ProMRI devices recognize
magnetic resonance imaging
devices
Triple-chamber devices have functions to configure different VV delays in order to
resynchronize the ventricles.
• Capture Control is also available for the left ventricle with automated tracking of
the pacing threshold or automatic threshold monitoring (ATM) for trend
analysis.
• To ensure that no additional surgery is necessary in case of a left-sided increase
of pacing threshold or undesired phrenic nerve stimulation, different pacing
polarities can be set for the left ventricular lead with a triple-chamber device.
Up to 13
• With the QP device type, the LV vector test provides a fast measurement of the
pacing threshold, the phrenic nerve pacing threshold and the pacing
impedance. The relative influence on the service time is also displayed. The
measurement results are evaluated automatically so that the optimal pacing
polarity can be set.
The short RV-LV conduction test supports also the selection.
• An additional diagnostic function with biventricular pacing: Variability of the
heart rate, patient activity, and thoracic impedance are monitored on a continual
basis.
There are two types of therapy programs:
• Default parameters are offered for the most common indications
(ProgramConsult function).
• Individual settings can be saved in 3 individual therapy programs.
The static magnetic field of magnetic resonance imaging devices is reliably
recognized with the aid of a sensor. This sensor can be activated for a maximum of
14 days using the MRI AutoDetect function during an interrogation.
If the patient comes near a magnetic resonance imaging device within the time set,
the implanted device recognizes the static magnetic field and automatically
activates the preset MRI program. Reprogramming to the permanent program
occurs also automatically after leaving the imaging device.
vectors can be used with the HF QP device type.
Home Monitoring functions
The device automatically sends information to the transmitter once a day. In
addition to this, test messages can be initiated using the programmer. Important
medical information includes, among others, the following:
• Ongoing atrial and ventricular arrhythmia
• Parameters relevant to leads in the atrium and ventricle: thresholds, sensing
amplitudes, impedances
• Current statistics on bradycardia therapy
• Individually adjustable timing interval for device messages which provide
additional information pertaining to the device messages
• IEGM online HD® with up to 3 high definition channels
• Transmission of these IEGM recordings with device messages

11
!
!
General Safety Instructions
Operating Conditions
2 General Safety Instructions
General Safety Instructions2417803Technical ManualEdora 8
CAUTION
Safety information
Cardiac electrotherapy is subject to special operating conditions and possible
complications and risks.
• Please take all precautionary measures carefully into account.
Operating Conditions
Technical manuals
Care during shipping and
storage
Temperature
The following technical manuals provide information about usage of the device
systems:
— Technical manual for the device
— Technical manual for the HMSC
— Technical manuals for leads
— Technical manuals for the programmer and its accessories
— Technical manuals for the user interface
— Technical manuals for cables, adapters and accessories
• Technical manuals are either included in hard copy form in the storage package
or in digital form on the internet:
manuals.biotronik.com
• Follow all relevant technical manuals.
• Keep technical manuals for later use.
• Devices are not to be stored close to magnets or sources of electromagnetic
interference.
• Note the effects of the storage period; see Battery Data.
Extremely low and high temperatures affect the service time of the battery in the
device.
• Permitted for shipping and storage:
–10°C to +45°C
Sterile delivery
Sterile packaging
Single use only
The device and the screwdriver have been gas-sterilized. Sterility is guaranteed only
if the blister and quality control seal have not been damaged.
The device and screwdriver are each packaged in 2 separately sealed blisters. The
inner blister is also sterile on the outside so that it can be transferred in a sterile
state during implantation.
The device and screwdriver are intended for single use only.
• Do not use the device if the package is damaged.
• The device must not be resterilized and reused.

12
Possible Complications
General Safety Instructions
Possible Complications
General information on
medical complications
Skeletal myopotentials
Nerve and muscle stimulation
Possible technical failures
Complications for patients and device systems generally recognized among
practitioners also apply to BIOTRONIK devices.
• Normal complications may include fluid accumulation within the device pocket,
infections, or tissue reactions. Primary sources of complication information
include current scientific and technological knowledge.
• It is not possible to guarantee the efficacy of antiarrythmia therapy, even if the
programs have proven successful during tests or subsequent
electrophysiological examinations. In rare cases the set parameters can
become ineffective. In particular it is inevitable that tachyarrhythmias may be
induced.
Bipolar sensing and control of sensitivity are adapted by the device to the rate range
of intrinsic events so that skeletal myopotentials are usually not sensed. Skeletal
myopotentials can nonetheless be classified as intrinsic events especially with a
unipolar configuration and/or very high sensitivity and, depending on the
interference, may cause inhibition or antiarrhythmia therapy.
A device system consisting of a unipolar lead and an uncoated device may result in
undesirable pacing of the diaphragm in the case of an initial or permanent high
setting of the pulse amplitude.
Technical failure of a device system cannot be entirely ruled out. Possible causes
may include the following:
• Lead dislodgement
• Lead fracture
• Insulation defects
• Device component failures
• Battery depletion
Electromagnetic interference
(EMI)
Device behavior in case of EMI
Static magnetic fields
Any device can be sensitive to interference, for example, when external signals are
sensed as intrinsic rhythm.
• BIOTRONIK devices have been designed so that their susceptibility to EMI is
minimal.
• Due to the intensity and variety of EMI, there is no guarantee for safety. It is
generally assumed that EMI produces only minor symptoms in patients - if any.
• Depending on the pacing mode and the type of interference, sources of
interference may lead to pulse inhibition or triggering, an increase in the
sensor-dependent pacing rate or asynchronous pacing.
• Under unfavorable conditions, for example during diagnostic or therapeutic
procedures, interference sources may induce such a high level of energy into
the pacing system that the cardiac tissue surrounding the lead tip is damaged.
In the case of electromagnetic interference or undesired myopotentials, the device
paces asynchronously for the duration of the time that the interference rate is
exceeded.
The pacemaker switches to magnet response from a field strength > 1.0 mT.
Possible Risks
13
General Safety Instructions
Possible Risks
Procedures to avoid
Potentially risky therapeutic
and diagnostic procedures
External defibrillation
The following procedures must be avoided as they may cause harm to the patient or
damage the device and, as a result, put the system functionality at risk:
• Therapeutic ultrasound
• Transcutaneous electrical nerve stimulation
• Hyperbaric oxygen therapy
• Applied pressures higher than normal pressure
If electrical current from an external source is conducted through the body for
diagnostic or therapeutic purposes, then the device can be subjected to
interference and the patient placed at risk.
Arrhythmia or ventricular fibrillation can be induced during diathermic procedures
such as electrocautery, HF ablation or HF surgery. For example, damaging
pressure levels may arise during lithotripsy. Influences on the device are not always
immediately clear.
If potentially risky procedures cannot be avoided, the following should be observed
at all times:
• Electrically insulate patients.
• Switch the pacemaker function to asynchronous modes if needed.
• Do not introduce energy near the device system.
• Check the peripheral pulse of the patient.
• Monitor the patient during and after every intervention.
The device is protected against the energy that is normally induced by external
defibrillation. Nevertheless, any implanted device may be damaged by external
defibrillation. Specifically, the current induced in the implanted leads may result in
necrotic tissue formation close to the electrode/tissue interface. As a result,
sensing properties and pacing thresholds may change.
• Place adhesive electrodes anterior-posterior or perpendicular to the axis
formed by the device to the heart at least 10 cm away from the device and from
implanted leads.
Radiation therapy
The use of radiation therapy must be avoided due to possible damage to the device
and the resulting impaired functional safety. If this type of therapy is to be used
anyway, prior risk/benefit analysis is absolutely necessary. The complexity of
influencing factors such as different sources of radiation, a variety of devices and
therapy conditions makes it impossible to issue directives that guarantee radiation
therapy without an impact on the device. The EN 45502 standard pertaining to active
implantable medical devices requires the following measures during the
administration of therapeutic ionizing radiation:
• Adhere to instructions for potentially risky therapeutic and diagnostic
procedures.
• Shield device against radiation.
• After applying radiation, double-check the device system to make sure it is
functioning properly.
Note: Please contact BIOTRONIK with questions on the risk/benefit analysis.
 Loading...
Loading...