
®
Impella
Circulatory Support System
Controller
With Impella® 2.5
INSTRUCTIONS
FOR USE

IMPORTANT NOTICE: Read this entire manual before using the Impella® Controller and Impella® 2.5 Circulatory Support System
(Impella® 2.5 System). The Impella® 2.5 System is to be used only in accordance with this manual. This manual is only applicable to
Impella® systems using the Impella® Controller.
Information contained in this document is subject to change without notice.
©2009 ABIOMED, Inc. All rights reserved.
The ABIOMED logo and ABIOMED are trademarks of ABIOMED, Inc. and are registered in the U.S.A. and certain foreign countries.
Recovering hearts. Saving lives.
Impella® and RECOVER are trademarks of ABIOMED Europe GmbH, a wholly owned subsidiary of ABIOMED, Inc.,
and are registered in the U.S.A. and certain foreign countries.
is a trademark of ABIOMED, Inc.
IMPELLA® CONTROLLER
®
WITH IMPELLA
2.5
CIRCULATORY SUPPORT SYSTEM
INSTRUCTIONS FOR USE
Rx Only
Abiomed, Inc.
22 Cherry Hill Drive
Danvers, MA 01923
978-777-5410 (voice)
978-777-8411 (fax)
clinical@abiomed.com (email)
Abiomed Europe GmbH
Neuenhofer Weg 3
52074 Aachen, Germany
+49 (241) 8860-0 (voice)
+49 (241) 8860-111 (fax)
europe@abiomed.com (email)
www.abiomed.com
24-Hour Emergency Hotlines:
N. America 1-800-422-8666
Europe +49 (0) 1805 2246633
September 2009
Document No. 0042-9000 Rev. A Draft 3


TABLE OF CONTENTS
INTRODUCTION
Introduction ............................................................................................. I
1 WARNINGS AND CAUTIONS
Warnings ................................................................................................. 1.1
Cautions .................................................................................................. 1.3
2 INDICATIONS, CONTRAINDICATIONS,
AND POTENTIAL ADVERSE EVENTS
Indications ............................................................................................... 2.1
Contraindications ..................................................................................... 2.2
Potential Adverse Events .......................................................................... 2.3
3 THE IMPELL A® 2.5
AND IMPELLA® CONTROLLER
Overview ................................................................................................. 3.1
Impella® 2.5 Catheter .............................................................................. 3.3
Impella® Controller .................................................................................. 3.5
Purge Cassette ......................................................................................... 3.6
Accessories ..............................................................................................3.8
4 USING THE IMPELLA® CONTROLLER
Overview ................................................................................................. 4.1
Impella® Controller Features .................................................................... 4.2
Impella® Controller Home Screen Display .................................................4.4
Impella® Controller Waveform Screen Display .......................................... 4.7
5 USING THE IMPELLA® CONTROLLER
WITH THE IMPELLA® 2.5
Startup ..................................................................................................... 5.1
Case Start ................................................................................................ 5.3
Inserting the Impella® 2.5 Catheter .......................................................... 5.8
Positioning and Starting the Impella® 2.5 Catheter .................................. 5.11
Use of the Repositioning Introducer
and the 13 Fr Peel-Away Introducer .........................................................5.14
Purger Procedures .................................................................................... 5.15
Troubleshooting the Purge System ........................................................... 5.18
Patient Weaning ......................................................................................5.19
How to Change to Backup Controller .......................................................6.15
Emergency Shutdown Procedure .............................................................. 6.15
7 CLEANING, STOR AGE, DISPOSAL,
AND RETURNS
Cleaning .................................................................................................. 7.1
Storing the Impella® Controller ................................................................ 7.1
Disposing of the Pump and Accessories (EU) ............................................ 7.1
Returning an Impella® Pump to Abiomed (US).......................................... 7.1
8 TERMINOLOGY, ABBREVIATIONS,
AND SYMBOLS
Terminology, Abbreviations, and Symbols ................................................ 8.1
9 SYSTEM SPECIFICATIONS
Impella® Controller Mechanical ................................................................ 9.1
Impella® Controller Electrical ................................................................... 9.1
Equipment Design .................................................................................... 9.2
Equipment Classifications ........................................................................ 9.2
Federal Communications Commission (FCC) Notice .................................. 9.3
Electromagnetic Compatibility ................................................................. 9.3
Patient Environment ................................................................................. 9.6
White Connector Cable ............................................................................ 9.8
Pump Parameters ..................................................................................... 9.8
Impella® 2.5 Dimensions ..........................................................................9.9
10 IMPELLA® CONTROLLER ALARMS
Impella® Controller Alarms ....................................................................... 10.1
APPENDICES
Appendix A: Impella® System Limited Service Warranty ..........................A.1
Appendix B: Technical Safety Inspections, Maintenance, and Repair ....... B.1
Appendix C: Abiomed-Approved Guidewires .......................................... C.1
Appendix D: Impella® Controller Menu Structure .................................... D.1
6 PATIENT MANAGEMENT TOPICS
Patient Management Overview ................................................................ 6.1
General Patient Care Considerations ....................................................... 6.1
Transport Within the Hospital .................................................................. 6.1
Right Heart Failure ................................................................................... 6.2
Cardiopulmonary Resuscitation (CPR) ...................................................... 6.2
Defibrillation ............................................................................................ 6.3
ECG Interference ...................................................................................... 6.3
Latex ........................................................................................................ 6.3
Positioning and Placement Devices ..........................................................6.3
Suction .................................................................................................... 6.4
Hemolysis ................................................................................................ 6.4
Understanding and Managing Impella® Position Alarms .......................... 6.6
Repositioning Guide ................................................................................. 6.10
Data Snap Shot Recording ........................................................................ 6.13
Infusion History ........................................................................................ 6.13
Operating the Impella® 2.5 Without Heparin in
the Purge Solution ................................................................................... 6.14
Guidelines for Explant .............................................................................. 6.14


TABLE OF CONTENTS
FIGURES
Figure 3.1 Impella® 2.5 ............................................................................... 3.1
Figure 3.2 Impella® Controller, Impella 2.5, and Accessories ....................... 3.2
Figure 3.3 Impella® 2.5 Catheter ................................................................ 3.3
Figure 3.4 Impella® Controller – Front View ................................................ 3.5
Figure 3.5 Purge Cassette ........................................................................... 3.6
Figure 3.6 White Connector Cable ..............................................................3.8
Figure 3.7 Introducer Kit .............................................................................3.8
Figure 3.8 0.018 in/260 cm Placement Guidewire ....................................... 3.8
Figure 3.9 20% Dextrose in Water .............................................................. 3.9
Figure 3.10 Impella® Controller Cart ........................................................... 3.9
Figure 4.1 Impella® Controller Features – Front and Side Views .................. 4.2
Figure 4.2 Impella® Controller Home Screen Display ...................................4.4
Figure 4.3 Waveform Screen Display (Waveform TBD) ................................. 4.7
Figure 5.1 Impella® Controller Power Switch ...............................................5.1
Figure 5.2 Impella® Controller Startup Screen ............................................. 5.2
Figure 5.3 Inserting Purge Cassette into Impella® Controller ....................... 5.4
Figure 5.4 Default Values for Purge Fluid ....................................................5.5
Figure 5.5 Snapping Plastic Hook to Connector Cable ................................. 5.6
Figure 5.6 Squeezing the White Flush Valve to Prime
the Impella® Catheter Pressure Lumen ..................................... 5.7
Figure 5.7 Inserting the 13 Fr Peel-Away Introducer .................................... 5.8
Figure 5.8 Inserting the 6 Fr Diagnostic Catheter ........................................ 5.9
Figure 5.9 Loading the Catheter on the Guidewire ...................................... 5.10
Figure 5.10 Exiting of the Placement Guidewire from the Catheter .............. 5.10
Figure 5.11 Inserting the Impella® 2.5 Catheter .......................................... 5.10
Figure 5.12 Ventricular Waveform on Placement Signal Screen .................... 5.11
Figure 5.13 Aortic Waveform on Placement Signal Screen ........................... 5.12
Figure 5.14 Selecting Target Flow ............................................................... 5.12
Figure 5.15 Confirming Placement on the Placement Signal Screen ............. 5.13
Figure 5.16 Removing the 13 Fr Peel-Away Introducer ................................ 5.14
Figure 6.1 Correct Catheter Position ........................................................... 6.6
Figure 6.2 Catheter Fully in Ventricle .......................................................... 6.7
Figure 6.3 Impella® Completely in the Aorta or Inlet and Outlet Area
in Ventricle and Pressure Port in Aorta ..................................... 6.8
Figure 6.4 Pump Position Unknown Due to Low Pulsatility
[Waveform TBD; Motor Current y-axis scale to be revised] ....... 6.9
Figure 6.5 Impella® Outlet Area on or near Aortic Valve ............................. 6.10
Figure 6.6 First Repositioning Guide Screen ................................................6.11
Figure 6.7 Second Repositioning Guide Screen ........................................... 6.11
Figure 6.8 Third Repositioning Guide Screen ............................................... 6.12
Figure 6.9 Exit Repositioning Guide Screen ................................................. 6.12
Figure 6.10 Infusion History Screen ............................................................. 6.13
Figure 9.1 Impella® Controller Patient Environment..................................... 9.7
Figure 9.2 Impella® 2.5 Dimensions ............................................................ 9.9
Figure B.1 Inspection Sticker Showing Inspection Required in May 2010 ..... B.1
TABLES
Table 3.1 Impella
Table 3.2 Purge Cassette Components ....................................................3.7
Table 3.3 Impella® 2.5 and Impella® Controller Accessories .................... 3.8
Table 4.1 Impella® Controller Features ....................................................4.3
Table 4.2 Impella® Controller Display Elements .......................................4.4
Table 6.1 Guide for Managing Hemolysis in Various Circumstances ......... 6.5
Table 8.1 Terminology and Abbreviations ................................................ 8.1
Table 8.2 Symbols ................................................................................... 8.1
Table 10.1 Audible Alarm and Notification Indicators................................ 10.1
Table 10.2 Critical (Red) Alarms ................................................................ 10.3
Table 10.3 Warning (Yellow) Alarms.......................................................... 10.5
Table 10.4 Advisor y (White) Notifications ................................................. 10.6
®
2.5 Catheter Components .......................................... 3.3


INTRODUCTION
PURPOSE OF MANUAL
This Instructions for Use manual is designed for healthcare professionals. It contains clinical and
®
technical considerations to guide healthcare professionals in their use of the Impella
®
with the Impella
2.5 Catheter. The Impella® 2.5 and Impella® Controller perform life-sustaining
functions. Use of these components requires a thorough understanding of and adherence to
®
these instructions for use. The Impella
Controller with the Impella® 2.5 may only be used for its
intended purpose.
MANUAL OVERVIEW
®
This manual provides instructions for use of the Impella
Controller with the Impella® 2.5. The
following summarizes the contents of each section:
• Section 1: Warnings and Cautions discusses the warnings and cautions pertaining
®
to the use of the Impella
Controller with the Impella® 2.5.
• Section 2: Indications, Contraindications, and Potential Adverse Events
®
discusses indications for use of the Impella
Controller with the Impella® 2.5 and potential
adverse events.
®
• Section 3: The Impella
2.5 and Impella® Controller provides an overview of the
blood pump and controller and describes the major components and features of each.
®
• Section 4: Using the Impella
®
types on the Impella
Controller.
• Section 5: Using the Impella
Controller describes the controls and various screen
®
Controller with the Impella® 2.5 provides the
procedures for using the controller and blood pump.
Controller
INTRODUCTION
• Section 6: Patient Management Topics provides key information on various topics
®
related to management of patients with the Impella
Controller and Impella® 2.5.
• Section 7: Cleaning, Storage, Disposal, and Returns provides instructions on
cleaning and storing the components, as well as disposing of components and returning
components to Abiomed.
• Section 8: Terminology, Abbreviations, and Symbols provides definitions for key
terms that appear in the manual as well as descriptions of the abbreviations and symbols
®
that appear on Impella
Controller and Impella® 2.5 components and packaging.
• Section 9: System Specifications lists technical information pertaining to the
®
Impella
• Section 10: Impella
Controller and Impella® 2.5.
®
Controller Alarms provides a listing of Impella® Controller
alarms and notifications as well as information on what to do to resolve them.
• Appendices at the end of the manual provide supplemental information about topics
®
including the Impella
and repair; Abiomed-approved guidewires; and the Impella
Impella® Controller with Impella® 2.5
Limited Service Warranty; technical safety inspection, maintenance
®
Controller menu structure.
I


1 WARNINGS AND CAUTIONS
WARNINGS ...................................................................................................1.1
CAUTIONS ....................................................................................................1.2

WARNINGS
1 WARNINGS AND CAUTIONS
The Impella® 2.5 System is intended for use only by personnel trained in accordance
with the Abiomed® Training Program.
Fluoroscopy is required to guide placement of the Impella® 2.5. The small
placement guidewire must be reliably observed at all times.
The sterile components of the Impella® 2.5 System can be used only if the
sterilization indicators show that the contents have been sterilized, the packaging is
not damaged, and the expiration date has not elapsed.
Do NOT resterilize or reuse the Impella® 2.5 Catheter. It is a disposable device and
is intended for single use only.
Retrograde flow will occur across the aortic valve if the Impella® 2.5 is set at a flow
rate of 0 L/min.
To prevent failure of the 13 Fr peel-away introducer, remove the 13 Fr peel-away
introducer prior to transport when activated clotting time (ACT) is less than
150 seconds.
Do NOT use saline in the purge system.
Do NOT use an Impella® 2.5 System if any part of the system is damaged.
To prevent the risk of explosion, do NOT operate the Impella® 2.5 System near
flammable anesthetics.
Warnings
Warnings alert you to
situations that can cause
death or serious injury. The
red symbol
warning messages.
appears before
To prevent malfunction of the locking mechanism of the 13 Fr peel-away introducer,
do NOT hold the hemostatic valve while inserting into the artery.
If at any time during the course of support with the Impella®, the Impella®
Controller alarms “Impella Failure: Sudden Purge Pressure Drop,” follow the
instructions presented in Section 5 of this manual.
Do NOT subject a patient who has been implanted with an Impella® 2.5 to
magnetic resonance imaging (MRI). The strong magnetic energy produced by an
MRI machine may cause the Impella® System components to stop working, and
result in injuries to the patient. An MRI may also damage the electronics of the
Impella® System.
During defibrillation, do NOT touch the pump, cables, or Impella® Controller.
Power the Impella® Controller using its internal battery if the integrity of the
protective earth conductor is questionable.
Impella® Controller with Impella® 2.5
1.1
Medical electrical equipment needs special precautions regarding EMC and needs
to be installed and put into service according to the electromagnetic compatibility
(EMC) information provided in the accompanying documents.
Portable and mobile RF communications equipment can affect medical electrical
equipment.
The equipment or system should not be used adjacent to or stacked with other
equipment. If adjacent or stacked use is necessary, the equipment or system should
be observed to verify normal operation in the configuration in which it will be used.
Use of cables, other than those sold by Abiomed, may result in increased emissions
or decreased immunity of the Impella
®
Controller.
The Impella® Controller uses RFID (radio frequency identification) to identify and
communicate with the purge cassette. Other equipment may interfere with the
Impella® Controller even if that other equipment complies with CISPR emission
requirements.
1.2
1.2
Instructions for Use
CAUTIONS
1 WARNINGS AND CAUTIONS
Handle with care. The Impella® 2.5 Catheter can be damaged during removal from
packaging, preparation, insertion, and removal. Do NOT bend, pull, or place excess
pressure on the catheter or mechanical components at any time.
Do NOT touch the inlet or outlet areas of the catheter and avoid manual
compression of the inlet cannula assembly while placing the device.
Patients with aortic stenosis or other abnormal aortic valve performance may be
compromised by the use of the Impella® 2.5. Patients with aortic valve disease
should be observed for aortic insufficiency.
Use only original accessories and replacement parts supplied by Abiomed.
Do NOT use damaged or contaminated connector cables.
To prevent device failure, do NOT start the Impella® 2.5 Catheter until the
guidewire has been removed.
Do NOT remove the Impella® 2.5 Catheter over the length of the guidewire.
When replacing the purge cassette, the replacement process must be completed
within 4 minutes. The Impella® 2.5 Catheter may be damaged if replacement takes
longer than 4 minutes.
Cautions
Cautions indicate a situation
in which equipment may
malfunction, be damaged, or
cease to operate. The yellow
symbol
caution messages.
appears before
To prevent malfunction of the Impella® Controller, avoid long-term exposure to
direct sunlight and excessive heat (40°C).
To prevent overheating and improper operation, do NOT block the cooling vents of
the Impella® Controller while it is operating.
Do not kink or clamp the Impella® 2.5 Catheter or the 13 Fr peel-away introducer.
The Li-Ion batteries must be charged for 10 hours prior to system operation. After
being unplugged, the Impella® Controller will operate for at least 60 minutes after
the batteries have been fully charged.
Minimize exposure of Impella® 2.5 System components to sources of
electromagnetic interference (EMI). Exposure to sources of EMI, such as cell phones
and two-way radios, may cause operational interference. To clear interference,
either increase the distance between system components and the EMI source or
turn off the EMI source.
Operation of Impella® 2.5 System components may interfere with the operation of
other devices. If interference occurs, increase the distance between the device and
system components.
Impella® Controller with Impella® 2.5
1.3
The use of high-frequency surgical devices may cause temporary interference to the
sensor signals. If continuous interference persists, the following warning message
appears on the display screen: “Sensor Value not Reliable.” Please acknowledge
this message. There is no reason to discontinue use of the pump.
Have a backup Impella® Controller available in the unlikely event of controller
failure.
Do NOT use the bed mount as a handle.
1.4
Instructions for Use

2 INDICATIONS, CONTRAINDICATIONS,
AND POTENTIAL ADVERSE EVENTS
INDICATIONS ................................................................................................2.1
Indications for Use in the United States ............................................................ 2.1
Intended Use in the European Union and Canada ............................................ 2.1
CONTRAINDICATIONS ................................................................................. 2.2
Contraindications in the United States .............................................................2.2
Contraindications in the European Union .........................................................2.2
Contraindications in Canada ............................................................................2.2
POTENTIAL ADVERSE EVENTS ..................................................................... 2.3
Potential Adverse Events (US) ..........................................................................2.3
Possible Complications (EU and Canada) .........................................................2.3
INDICATIONS
INDICATIONS FOR USE IN THE UNITED STATES
®
The Impella
extracorporeal bypass control unit, for periods up to 6 hours. It is also intended to be used to
provide partial circulatory support (for periods up to 6 hours) during procedures not requiring
cardiopulmonary bypass.
The Impella
useful in determining intravascular pressure.
2.5 Circulatory Support System is intended for partial circulatory support using an
®
2.5 Circulatory Support System also provides pressure measurements which are
2
INDICATIONS, CONTRAINDICATIONS, AND POTENTIAL ADVERSE EVENTS
Investigational Device
Exemption (IDE) Clinical
Trials
INTENDED USE IN THE EUROPEAN UNION AND CANADA
®
The Impella
2.5 (intracardiac pump for supporting the left ventricle) is intended for clinical
use in cardiology and in cardiac surgery for up to 5 days for the following indications, as well
as others:
®
• The Impella
2.5 is a circulatory support system for patients with reduced left ventricular
function, eg, post-cardiotomy, low output syndrome, cardiogenic shock after acute
myocardial infarction, or for myocardial protection after acute myocardial infarction
®
• The Impella
2.5 may also be used as a cardiovascular support system during coronary
bypass surgery on the beating heart, particularly in patients with limited preoperative
ejection fraction with a high risk of postoperative low output syndrome
• Support during high risk percutaneous coronary intervention (PCI)
• Post PCI
In addition to the indications
for use outlined in this IFU,
the Impella
Support system is being
evaluated in various FDA
approved clinical trials for
additional indications and
patient populations. Refer
to the study protocols
for additional indications,
contraindications, and
inclusion and exclusion criteria
if the device is being used
under a clinical trial protocol.
®
2.5 Circulatory
Impella® Controller with Impella® 2.5
2.1
CONTRAINDICATIONS
Patients with aortic stenosis or other abnormal aortic valve performance may be
compromised by the use of the Impella® 2.5. Patients with aortic valve disease
should be observed for aortic insufficiency.
CONTRAINDICATIONS IN THE UNITED STATES
• Mechanical aortic valve or heart constrictive device.
• Aortic valve stenosis/calcication (graded as ≥ +2 equivalent to an orice area of 1.5 cm
or less).
• Moderate to severe aortic insufciency (echocardiographic assessment of aortic
insufciency graded as ≥ +2).
®
• Severe peripheral arterial obstructive disease that would preclude Impella
placement.
CONTRAINDICATIONS IN THE EUROPEAN UNION
2.5 device
2
• Mechanical aortic valves, severe aortic valvular stenosis or valvular regurgitation
• Hematological disorder causing fragility of the blood cells or hemolysis
• Hypertrophic obstructive cardiomyopathy (HOCM)
• Aneurysm or necrotomy or severe anomaly of the ascending aorta and/or the aortic arch
• Mural thrombus in the left ventricle
• Ventricular septal defect (VSD) after myocardial infarction
• Anatomic conditions precluding insertion of the pump
• Other illnesses or therapy requirements precluding use of the pump
• Severe peripheral arterial occlusion disease (PAOD) is a relative contraindication
CONTRAINDICATIONS IN CANADA
• Prosthetic aortic valves, severe aortic valvular stenosis or valvular regurgitation
• Hematological disorder causing fragility of the blood cells or hemolysis
• Hypertrophic obstructive cardiomyopathy (HOCM)
• Aneurysm or necrotomy or severe anomaly of the ascending aorta and/or the aortic arch
2.2
• Mural thrombus in the left ventricle
• Ventricular septal defect (VSD) after myocardial infarction
• Anatomic conditions precluding insertion of the pump
• Other illnesses or therapy requirements precluding use of the pump
• Peripheral arterial occlusion disease (PAOD)
Instructions for Use

POTENTIAL ADVERSE EVENTS
POTENTIAL ADVERSE EVENTS (US)
2
INDICATIONS, CONTRAINDICATIONS, AND POTENTIAL ADVERSE EVENTS
• Death
• Aortic insufciency
• Arrhythmia
• Bleeding
• Cardiogenic shock
• Hemolysis
• Insertion site infection
• Perforation
• Respiratory dysfunction
• Thrombocytopenia
• Transient ischemic attack (TIA)
• Ventricular brillation
POSSIBLE COMPLICATIONS (EU AND CANADA)
There are risks of complications with every procedure using a blood pump. These include
among others:
• Cerebral vascular accident (CVA) / Stroke
• Aortic valve injury
• Atrial brillation
• Cardiac tamponade
• Device malfunction
• Hepatic failure
• Myocardial infarction
• Renal failure
• Sepsis
• Thrombotic vascular (non-CNS) complication
• Vascular injury
• Ventricular tachycardia
• Hemolysis
• Bleeding
• Immune reaction
• Embolism, thrombosis
• Vascular injury through to
angionecrotomy
• Positioning problems
• Infection and septicemia
• Dislocation of the pump
• Cardiovalvular injuries due to extreme
movement of the suction cannula in
relation to the cardiac valve or as a result of
attachment by suction of the pump to the
valve system following incorrect positioning
• Endocardiac injuries as a result of
attachment of the pump due to suction
• Pump failure, loss of pump components
following a defect
• Patient dependency on the pump after use
for support
Impella® Controller with Impella® 2.5
2.3


3 THE IMPELLA® 2.5
AND IMPELLA® CONTROLLER
OVERVIEW .................................................................................................... 3.1
IMPELLA
IMPELLA
PURGE CASSETTE .........................................................................................3.6
ACCESSORIES ...............................................................................................3.8
®
2.5 CATHETER ............................................................................ 3.3
®
CONTROLLER ...............................................................................3.5

OVERVIEW
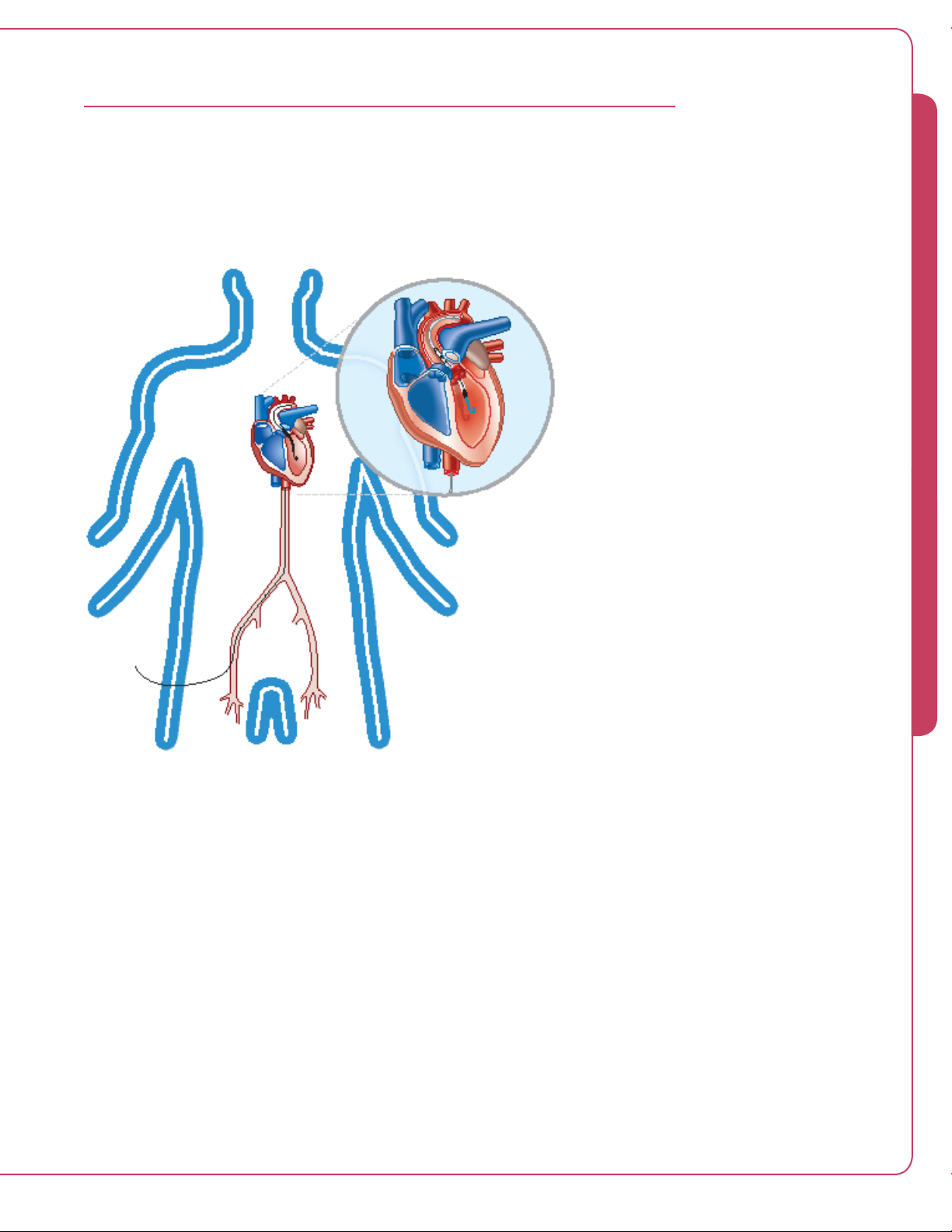
The Impella® 2.5 is an intravascular microaxial blood pump that supports a patient’s circulatory
system. The pump is inserted percutaneously through the femoral artery and into the left
ventricle. (See Figure 3.1.)
3 THE IMPELLA
®
2.5 AND IMPELLA
®
CONTROLLER
Figure 3.1 Impella® 2.5
When properly positioned, the pump delivers blood from the inlet area, which sits inside the
left ventricle, through the cannula, to the outlet opening in the ascending aorta. Physicians and
device operators monitor the correct positioning and functioning of the pump on the display
®
screen of the Impella
This section describes the components of the Impella
Controller.
®
2.5, the Impella® Controller, and the
accessory components.
Impella® Controller with Impella® 2.5
3.1
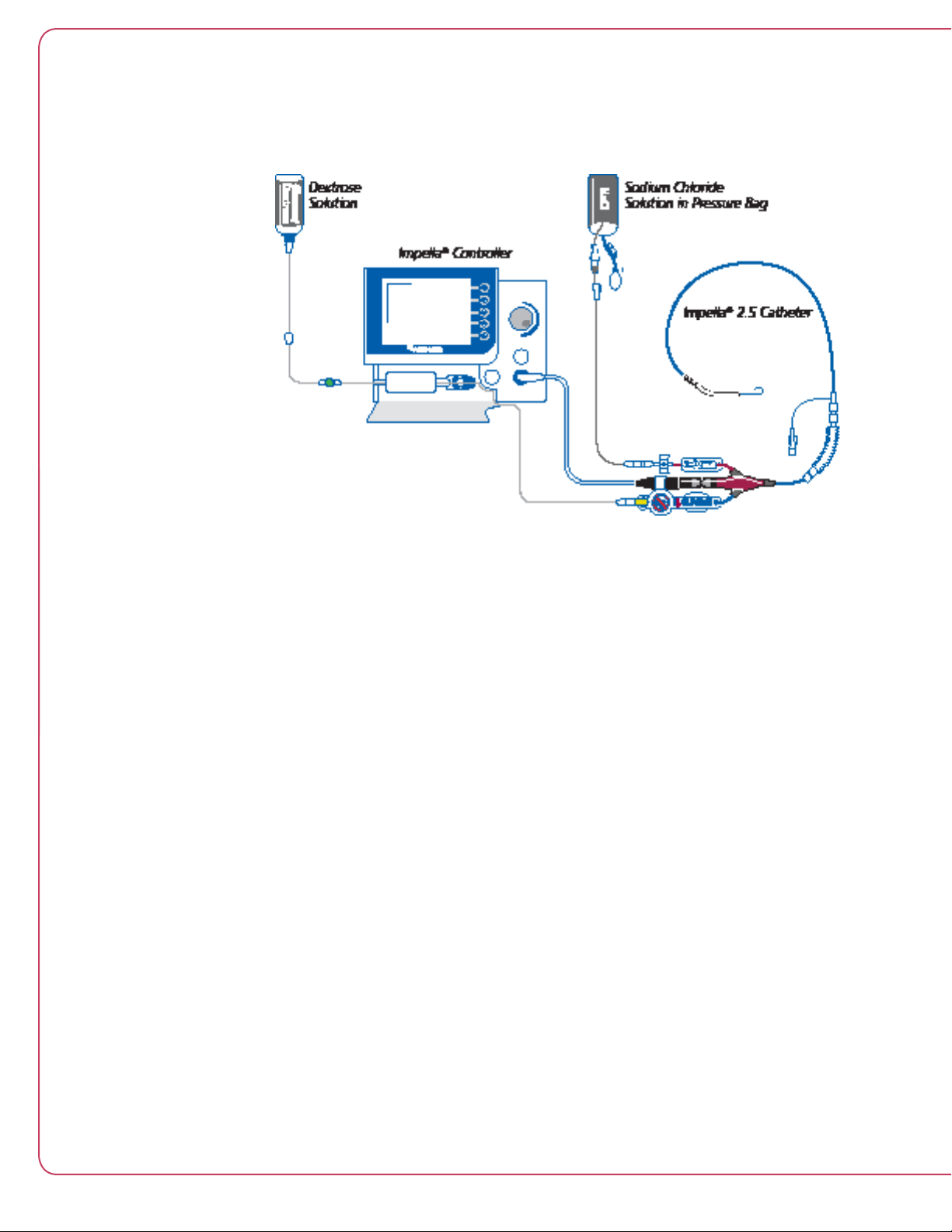
Figure 3.2 illustrates how the Impella® Controller connects to the Impella® 2.5 and accessory
components.
Figure 3.2 Impella® Controller, Impella 2.5, and Accessories
3.2
Instructions for Use
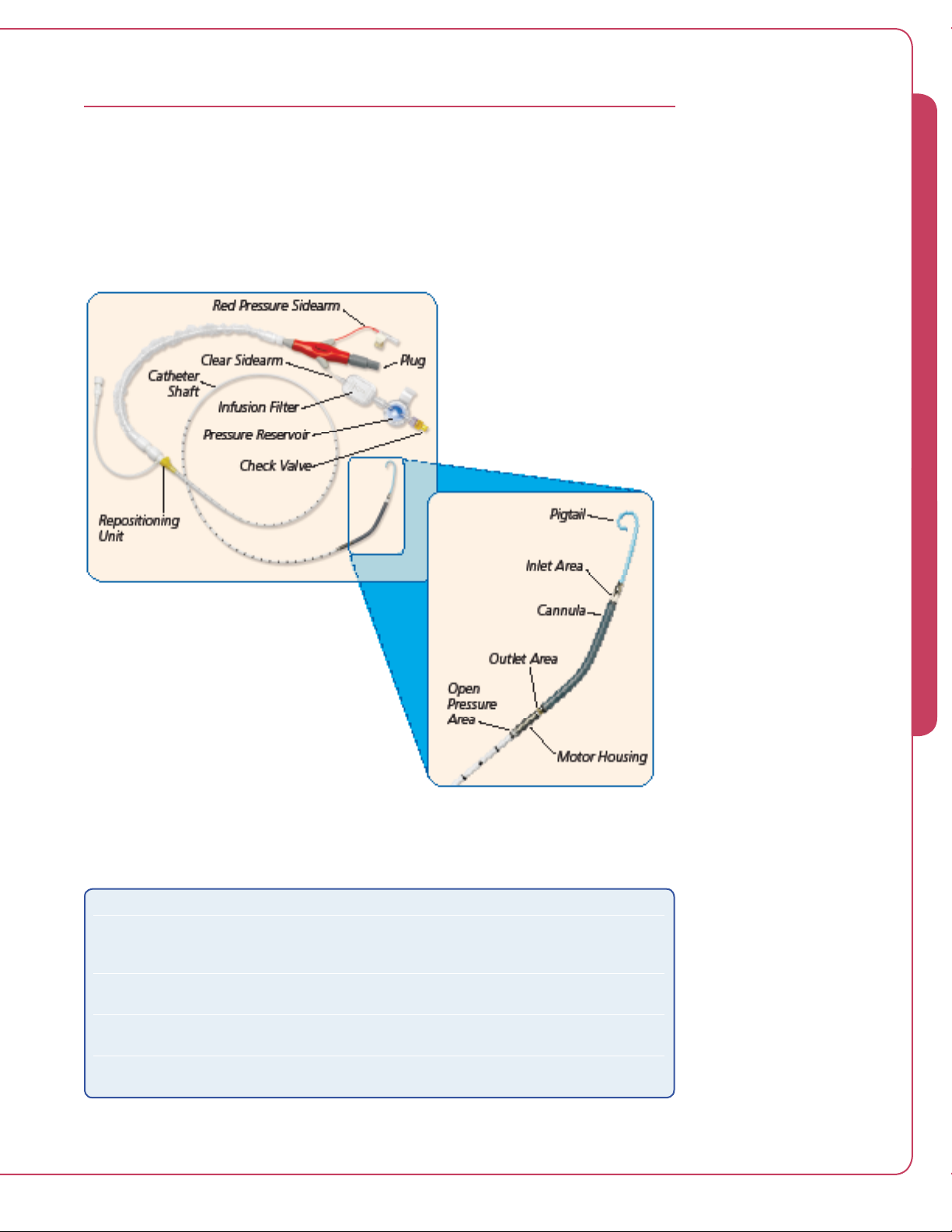
IMPELLA® 2.5 CATHETER
The Impella® 2.5 Catheter is an intravascular microaxial blood pump that delivers up to 2.5
liters of blood per minute from the left ventricle into the aorta. Figure 3.3 illustrates the
®
Impella
check valve on the other end.
2.5 Catheter. Table 3.1 describes each component from the pigtail at one end to the
3 THE IMPELLA
®
2.5 AND IMPELLA
®
CONTROLLER
Figure 3.3 Impella® 2.5 Catheter
®
Table 3.1 Impella
2.5 Catheter Components
Component Description
Pigtail The 6 Fr pigtail is attached to the cannula at the distal end of the inlet
area. It assists with stabilizing the catheter in the correct position in
the left ventricle.
Cannula The 12 Fr cannula has a spiral-shaped reinforced body that is shaped in
a 45-degree angle.
Inlet area The inlet area, where the blood enters the cannula, is located at the
distal tip of the cannula.
Outlet area The proximal end of the cannula is attached to the outlet area where
the blood exits the cannula.
Impella® Controller with Impella® 2.5
3.3
Table 3.1 Impella
®
2.5 Catheter Components (cont’d)
Component Description
Motor housing The motor housing is 12 Fr in diameter and consists of a completely
encapsulated motor.
Open pressure area The open pressure area is an opening located between the motor
housing and the distal end of the catheter shaft.
Catheter shaft A 9 Fr catheter shaft is located between the motor housing and
the plug. The lumen of the catheter shaft contains a purge lumen,
a pressure measurement lumen, and a pump monitoring cable.
The catheter shaft has longitudinal and transversal marks:
• The longitudinal marks along the inner radius of the cannula show
the position of the curved, flexible cannula.
• The transversal marks at 1 cm intervals aid in proper positioning.
Repositioning unit The repositioning unit consists of an introducer and an
anticontamination sleeve with an anchoring ring.
• The introducer (with hemostatic valve) is graduated from 11 Fr to
15 Fr. It is located on the catheter shaft and allows repositioning of
the catheter.
• The anchoring ring of the anticontamination sleeve secures the
catheter sheath to the introducer.
Plug The plug at the proximal end of the catheter connects the catheter to
the Impella® Controller through a connector cable. It has two sidearms:
a red pressure sidearm and a clear sidearm.
Red pressure sidearm The red pressure sidearm is attached to a standard pressure bag and is
used to prime the line of the pressure measurement system.
Clear sidearm The clear sidearm is attached to the purge cassette purge line. It leads
to the infusion filter, the pressure reservoir, and the check valve.
Infusion filter The infusion filter prevents bacterial contamination and prevents air
from entering the catheter.
Pressure reservoir The pressure reservoir includes a flexible rubber diaphragm that
provides additional filling volume by means of an expansion chamber
during purge solution change.
Check valve The yellow check valve ensures that purge fluid does not flow in the
reverse direction when the purge solution is exchanged.
3.4
Instructions for Use

IMPELLA® CONTROLLER
3 THE IMPELLA
The Impella® Controller (see Figure 3.4) provides three vital functions to the operation of the
®
Impella
2.5:
• The controller provides an interface for monitoring and controlling the function of the
Impella 2.5
• The controller provides a uid purge to the Impella 2.5 motor
• The controller provides backup power when the controller is operated away from AC
power
The controller weighs 26 lbs (11.8 kg) and can operate on its internal battery for at least 60
minutes when fully charged.
®
Impella
Controller operation is described in detail in Section 4 of this manual.
Impella® Controller
Battery Power
The controller can operate
on its internal lithium-ion
(Li-Ion) battery for at least 60
minutes when fully charged.
®
2.5 AND IMPELLA
®
CONTROLLER
Figure 3.4 Impella® Controller – Front View
Impella® Controller with Impella® 2.5
3.5
PURGE CASSETTE
Do not use saline in the purge system.
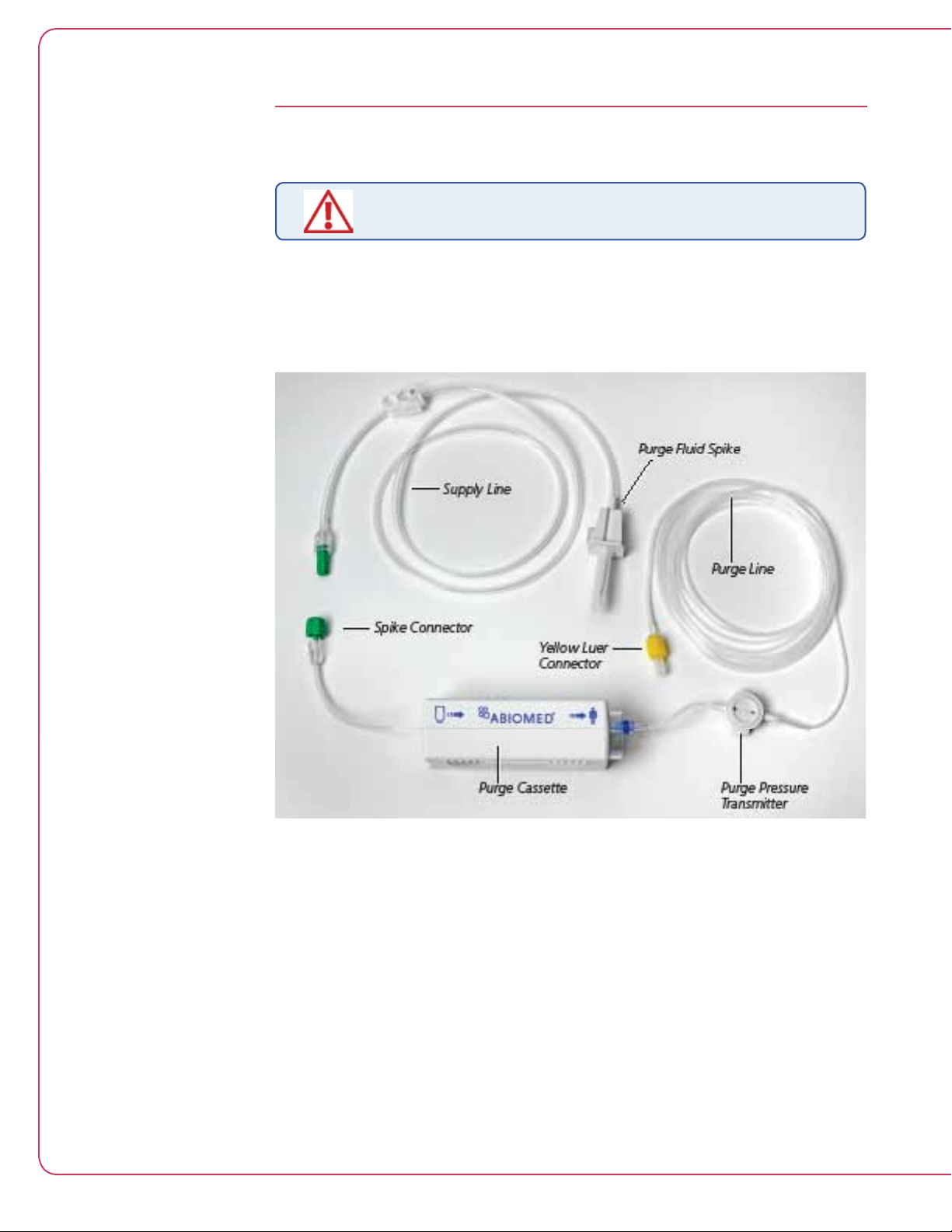
The purge cassette delivers rinsing fluid to the Impella® pump. The purge fluid (typically 20%
dextrose solution plus heparin 50 IU/mL) flows from the purge cassette through the catheter to
the microaxial blood pump to prevent blood from entering the pump motor. Figure 3.5 illustrates
the purge cassette and related components. Table 3.2 describes each component.
3.6
Figure 3.5 Purge Cassette
Instructions for Use

Table 3.2 Purge Cassette Components
Component Description
Purge cassette Contains the components for circulating the purge fluid; maintains the
pressure barrier between the blood and the motor at the proper level
Purge pressure
transmitter
Purge line Carries purge fluid from the purge cassette to the Impella® pump
Yellow luer connector Connects the purge line to the pressure reservoir (yellow luer lock) on
Purge fluid spike One end spikes the purge fluid bag and the other end connects the
Spike connector Connects the purge cassette supply line to the purge fluid spike
Supply line Carries fluid from the purge fluid bag to the purge cassette
Contains a membrane that transmits pressure to the controller based
on the purge pressure in the purge line; a transducer in the controller
measures the pressure so that it can be displayed on the screen
the Impella® pump
bag to the purge cassette supply line
3 THE IMPELLA
®
2.5 AND IMPELLA
®
CONTROLLER
Impella® Controller with Impella® 2.5
3.7

ACCESSORIES
Table 3.3 illustrates and describes the accessories used with the Impella® 2.5 and Impella®
Controller.
Table 3.3 Impella® 2.5 and Impella® Controller Accessories
Component Description
The white connector cable connects the Impella®
2.5 Catheter to the Impella® Controller. The
connector cable is attached to the Impella® pump
in the original packaging.
• The socket at the black end of the cable
connects to the Impella® catheter plug.
• The white plug at the opposite end of the cable
is inserted into the blue pump plug on the front
of the Impella® Controller.
Figure 3.6 White Connector Cable
The introducer kit is used to position the pump.
It contains:
• 13 Fr peel-away introducer with hemostatic valve
• 13 Fr dilator
• 18 G Seldinger needle
• 10 cc syringe
• 0.035 in stiff guidewire
Guidewire Use
It is important to use only
the guidewire supplied with
the system or an Abiomedapproved alternative. Refer
to Appendix C for more
information about Abiomedapproved guidewires.
Figure 3.7 Introducer Kit
The 0.018 in/260 cm placement guidewire is used
for the placement of the catheter. The guidewire
has a radiopaque, shapable tip.
Figure 3.8 0.018 in/260 cm Placement
Guidewire
3.8
Instructions for Use

Component Description
20% dextrose solution with 50 IU/mL of heparin is
used as the purge fluid. The purge cassette infuses
the purge fluid through the catheter.
Figure 3.9 20% Dextrose in Water
The Impella® Controller Cart holds the Impella®
Controller. The cart has wheels for easy transport
of the controller and a storage basket.
3 THE IMPELLA
®
2.5 AND IMPELLA
®
CONTROLLER
Figure 3.10 Impella® Controller Cart
Impella® Controller with Impella® 2.5
3.9


4 USING THE IMPELLA® CONTROLLER
OVERVIEW ....................................................................................................4.1
IMPELLA
IMPELLA
IMPELLA
®
CONTROLLER FEATURES............................................................. 4.2
®
CONTROLLER HOME SCREEN DISPLAY ...................................... 4.4
®
CONTROLLER WAVEFORM SCREEN DISPLAY ..............................4.7
Placement Signal Waveform.............................................................................4.7
Motor Current Waveform ................................................................................. 4.8


OVERVIEW
The Impella® Controller is the primary user control interface for the Impella® 2.5. It controls
®
the pump performance, monitors the Impella
position information regarding the location of the pump across the aortic valve. The controller
can be powered by AC power or can operate on internal battery power for at least 60 minutes
when fully charged.
This section of the manual discusses Impella
2.5 for alarms, and provides real time catheter
®
Controller features and displays.
4 USING THE IMPELLA
®
CONTROLLER
Impella® Controller with Impella® 2.5
4.1

IMPELLA® CONTROLLER FEATURES
Figure 4.1 illustrates the features of the Impella® Controller. These features are described
in Table 4.1.
4.2
Figure 4.1 Impella® Controller Features – Front and Side Views
Instructions for Use

Table 4.1 Impella
®
Controller Features
Feature Description
Display screen Displays user information, including the labels for the soft buttons.
(Display screen elements described in detail later in this section.)
Soft buttons Display, open, navigate, and close menus. The function for each soft button is
defined by labels adjacent to the button on the display screen; function changes
depending on the screen. (Soft button functions are described in Table 4.2)
When the pump is running the default soft button labels are as follows:
• MUTE ALARM
• TARGET FLOW
• DISPLAY
• PURGE SYSTEM
• MENU
Selector knob Rotating push button; turn clockwise and counterclockwise to scroll through
menu items; push to make a selection.
NOTE: In many situations, selector knob function is circular—that is, once
you scroll to the end of the list of selections, the system circles through the
list again as you continue to turn the knob. On some screens, however, the
selector knob function is NOT circular and you must turn the knob in the
reverse direction to get to previous items.
®
Pump plug Connection point on the controller for the Impella
Purge cassette
Spring-loaded door that opens to provide access to the purge cassette
door
Purge cassette Contains the components for circulating purge fluid; maintains the pressure
barrier between the blood and the motor at the proper level. (The purge
cassette and its components are described in Section 3 of this manual.)
Purge pressure
transmitter
Applies pressure to the transducer in the controller so that purge presure can
be measured
Bed mount Metal bracket on the back of the controller; attaches controller to the bed
Purge cassette
door release
RS-232 service
Located on the left side of the controller; press to open the purge cassette
door
Interface for data transfer to an external device
jack
USB connector Connection for downloading data
Ethernet jack Connection for downloading data or software upgrades
®
Equipotential
Used to ground the Impella
Controller according to hospital procedures
ground stud
AC fuses Electrical safety device in the event of current overload
Power cord
For mounting power cord retainer
retainer
mounting holes
Power switch Turns the controller ON or OFF
• ON: Press and hold the power switch key for 3 seconds
®
• OFF: (1) Disconnect the Impella
Catheter from the Impella® Controller.
(2) Press and hold the power switch for 3 seconds.
(3) Press OK to confirm that the controller should be turned off.
NOTE: Holding down the power switch for longer than 30 seconds during
operation will cause the controller to initiate hardware switch-off
AC plug Connection point on the controller for the AC power cord
pump
4 USING THE IMPELLA
®
CONTROLLER
Impella® Controller with Impella® 2.5
4.3

IMPELLA® CONTROLLER HOME SCREEN DISPLAY
The home screen displays operating parameters and information for the entire system.
®
Figure 4.2 illustrates the Impella
described in Table 4.2.
Controller home screen display. Each element of the display is
Figure 4.2 Impella® Controller Home Screen Display
®
Table 4.2 Impella
Controller Display Elements
Display Element Description
Patient identification (ID) Displayed in the upper left corner of the display screen if the
information has been entered. The Patient ID can be up to 31
characters in length.
Pump serial number Displayed in the upper center of the display screen if a blood pump is
connected to the controller.
System date and time The current date and time (24-hour format) are displayed in the upper
right corner of the screen display.
Alarm window The alarm window displays up to 3 alarms simultaneously, in order of
priority from top to bottom.
For each alarm, the alarm window displays:
• Alarm header – displayed in the left column; window is color-
coded red for critical alarms, yellow for warning alarms, white for
advisory notifications, gray for resolved alarms
• Alarm subhead (if applicable) – further describes the alarm
condition
• Detailed text – up to 3 lines of instructions for resolving the alarm
condition are displayed in the right column of the alarm window
next to the alarm header and subhead information
(See Section 10 of this manual for further discussion of Alarms.)
4.4
Instructions for Use

Table 4.2 Impella
®
Controller Display Elements (cont’d)
Display Element Description
Supply line Carries fluid from the purge fluid bag to the purge cassette
Mute Alarm indicator Displayed below the system date and time in the upper right
of the display screen. (See Section 10 of this manual for more
information about the Mute Alarm function.)
• Yellow bell with red X displayed when an alarm is muted.
• Not displayed when an alarm is active but not muted or when
there are no active alarms.
Soft button labels The soft buttons on the Impella® Controller have corresponding
labels adjacent to them on the display screen. These labels change
depending on the type of screen displayed.
MUTE ALARM
• Mutes (silences) active alarms
TARGET FLOW (or NEXT)
• TARGET FLOW – Brings up the target flow icon, which
enables users to set the current flow rate for the Impella 2.5
• NEXT – Advances to the next screen
DISPLAY (or BACK)
• DISPLAY – Brings up the Display menu for viewing
waveforms and navigating to other screen displays
• BACK – Returns to the previous screen
PURGE SYSTEM (or EXIT)
• PURGE SYSTEM – Brings up the Purge System menu for
making changes in purge fluid, purge cassette, or the purge
system, or de-airing the purge system
• EXIT – Exits the current procedure
MENU (or Exit Repositioning Guide)
• MENU – Brings up a menu of options related to controller
settings, alarm history, repositioning, and starting a
procedure
• Exit Repositioning Guide – Exits the repositioning guide
System power area System power information is displayed to the right of the purge
system information on the bottom of the display screen
Battery status
• Bar within battery symbol indicates the overall remaining
capacity of the batteries
• Full green bar for fully charged battery
• Partial green bar for battery that is at least 50% charged
• Partial yellow bar for battery that is between 25% and 50%
charged
• Partial red bar for battery that is less than 25% charged
• Moving gray bar indicates battery is in charging mode
• Numeric percentage of battery power remaining displayed
below the battery icon
AC plug indicator
• Green plug symbol indicates that the controller is running on AC
power
• Gray plug icon with a red X indicates no AC power detected
and the controller is running on battery power
4 USING THE IMPELLA
®
CONTROLLER
Impella® Controller with Impella® 2.5
4.5

Table 4.2 Impella
®
Controller Display Elements (cont’d)
Display Element Description
Purge system area Information about the purge system is displayed to the right of
the flow area at the bottom of the display screen
Purge system marquee
• Strobes from left to right when the purge system is operating
• Slow strobing represents normal purge ow rate
• Fast strobing represents bolus ow rate
Purge rate
• Current purge rate displayed in mL/hr below the purge system
marquee if the purge rate is known
• Not displayed if there is no purge cassette or the procedure has
not yet started
Time remaining in reservoir
• Displays the remaining runtime based on the volume of the
purge fluid bag at the start of the case and the cumulative time
and flow rate of delivery of purge fluid
• Not displayed if there is no purge cassette or the procedure has
not yet started
Flow area Information about Impella® flow is displayed in the lower left
corner of the display screen
Current flow rate
• Mean pump ow displayed in liters per minute (L/min)—
the numbers appear in white if the pump position is correct;
yellow if the pump position is incorrect or unknown
• If the system is unable to calculate ow, a yellow triangular
caution icon is displayed with the message “Flow Calculation
Disabled”
Pump icon
• The circular pump icon rotates when the blood pump is running
Central display area On the home screen, the central display area displays a heart
pictogram and Impella® position indicator message.
Heart pictogram appears in the center of the home screen display
• Provides a visual representation of the current Impella® pump
position
• Overlaid with a translucent yellow “?” when the controller
detects an incorrect pump position or cannot detect pump
position
Impella® position indicator message displayed to the left of the
heart image
• Displays “Impella® Position OK” in green when pump position
is correct
• Displays “Impella® Position Unknown” in yellow when pump
position is unknown
• Displays specic message in yellow when pump position is
incorrect
4.6
Instructions for Use

IMPELLA® CONTROLLER WAVEFORM SCREEN DISPLAY
The waveform screen (see Figure 4.3) displays operating data for the system. The screen displays
up to two waveforms and current pump data in the central display area of the screen.
4 USING THE IMPELLA
®
CONTROLLER
Figure 4.3 Waveform Screen Display (Waveform TBD)
Figure 4.3 shows two time-based waveform signals from different sources.
• Placement signal waveform
• Motor current waveform
PLACEMENT SIGNAL WAVEFORM
The placement signal waveform displays a pressure measurement that corresponds to the
location of the open pressure area of the catheter. The placement signal is used to verify the
position of the microaxial blood pump by evaluating the current pressure waveform as an aortic
or ventricular waveform. The scale for the placement signal waveform is displayed to the left of
the waveform. The default scaling is 0–160 mmHg in 20 mmHg increments, with a minimum
upper limit of 100 mmHg and a maximum upper limit of 240 mmHg for the Impella 2.5.
To the left of the waveform is a display that labels the waveform, provides the units of
measurement, shows the upper and lower range values, and the average value from the samples
received from the last value update. At the bottom of that window is the time scale, which can
be set to 10 seconds, 5 minutes, or 5 hours using the DISPLAY soft button. The default time
scale is 10 seconds.
Impella® Controller with Impella® 2.5
4.7

Motor Current
Motor current is the
measurement of electricity
through the Impella
required to rotate the
®
Impella
microaxial pump.
®
motor
MOTOR CURRENT WAVEFORM
The motor current waveform is a measurement of the electricity through the pump motor. The
scale for the motor current waveform is displayed to the left of the waveform. The default scaling
is 0–1000 mA in 100 mA increments for the Impella 2.5, with a minimum difference between
upper and lower limits of 200 mA and a maximum difference of 1000 mA.
To the left of the waveform is a display that labels the waveform, provides the units of
measurement, shows the upper and lower range values, and the average value from the samples
received from the last value update. The time scale at the bottom of that window can be set
to 10 seconds, 5 minutes, or 5 hours using the DISPLAY soft button. The default time scale
is 10 seconds.
4.8
Instructions for Use

5 USING THE IMPELLA® CONTROLLER
WITH THE IMPELLA® 2.5
STARTUP ....................................................................................................... 5.1
Turning ON the Impella
®
Controller .................................................................. 5.1
The Startup Screen ..........................................................................................5.2
Starting a Case Procedure................................................................................ 5.2
CASE START ..................................................................................................5.3
Overview .........................................................................................................5.3
Initial Setup .....................................................................................................5.3
Prime Purge Tubing .........................................................................................5.4
Enter Purge Fluid Data .....................................................................................5.5
Plug Impella
Prime Impella
®
into Controller ...........................................................................5.6
®
Purge Lumen ...........................................................................5.6
Prime Blood Pressure Lumen ............................................................................5.7
Pre-Insertion Impella
®
Impella
Test Successful ..................................................................................5.7
INSERTING THE IMPELLA
POSITIONING AND STARTING THE IMPELLA
®
Test ..............................................................................5.7
®
2.5 CATHETER ...................................................5.8
®
2.5 CATHETER .................... 5.11
USE OF THE REPOSITIONING INTRODUCER
AND THE 13 Fr PEEL-AWAY INTRODUCER ..................................................5.14
PURGER PROCEDURES ...............................................................................5.15
Purge System Change .................................................................................... 5.15
Purge Fluid Change ....................................................................................... 5.16
Purge Cassette Change ................................................................................. 5.16
De-Air Purge System ...................................................................................... 5.17
TROUBLESHOOTING THE PURGE SYSTEM .................................................. 5.18
Low Purge Pressure .......................................................................................5.18
High Purge Pressure ...................................................................................... 5.18
Purge System Blocked .................................................................................... 5.18
PATIENT WEANING ..................................................................................... 5.19
Rapid Weaning .............................................................................................. 5.19
Slow Weaning ............................................................................................... 5.19
1


STARTUP
Do
NOT
use an Impella® 2.5 System if any part of the system is damaged.
The sterile components of the Impella® 2.5 System can be used only if the
sterilization indicators show that the contents have been sterilized, the packaging is
not damaged, and the expiration date has not elapsed.
Do
NOT
resterilize or reuse the Impella® 2.5 Catheter. It is a disposable device and
is intended for single use only.
To prevent malfunction of the Impella® Controller, avoid long-term exposure to
direct sunlight and excessive heat (40°C).
5 USING THE IMPELLA
®
CONTROLLER WITH THE IMPELLA
To prevent overheating and improper operation, do NOT block the cooling vents of
the Impella
®
Controller while it is operating.
The Li-Ion batteries must be charged for 10 hours prior to system operation. After
being unplugged, the Impella® Controller will operate for at least 60 minutes after
the batteries have been fully charged.
Have a backup Impella® Controller available in the unlikely event of controller
failure.
TURNING ON THE IMPELLA® CONTROLLER
To turn the controller ON:
1. Press and hold the power switch on the right side of the Impella
seconds (see Figure 5.1).
®
Controller for 3
®
2.5
Figure 5.1 Impella® Controller Power Switch
The Impella® Controller automatically performs a system test when turned ON.
A display bar shows the progress of the system test. If the system test passes, the system
displays the startup screen (see Figure 5.2).
Impella® Controller with Impella® 2.5
5.1

If the system test fails, the controller displays a system self check failure message:
SYSTEM SELF CHECK FAILED.
CHANGE CONSOLE IMMEDIATELY.
The controller displays the reason for the system test failure at the bottom of the screen.
THE STARTUP SCREEN
The startup screen (Figure 5.2) appears when you successfully turn ON the Impella® Controller.
Figure 5.2 Impella® Controller Startup Screen
The startup screen displays:
®
• The current status of the Impella
pump (currently no pump connected to the Impella®
Controller in Figure 5.2).
• The current status of the purge cassette (no purge cassette detected in Figure 5.2).
®
• The current version of the software that the Impella
Controller is running.
The startup screen also displays system power information along the bottom of the screen and
two active soft buttons—MUTE ALARM and MENU—along the right side of the screen.
STARTING A CASE PROCEDURE
To start a case procedure:
1. Press the MENU soft button from the startup screen.
2. Scroll the selector knob to “Case Start” on the pop-up menu that appears on the screen.
3. Press the selector knob to select “Case Start”.
After you press the selector knob to select “Case Start” from the menu, the controller displays
®
an 8-screen series that leads you from initial setup through the pre-insertion Impella
test.
5.2
Instructions for Use

CASE START
5 USING THE IMPELLA
Fluoroscopy is required to guide placement of the Impella® 2.5. The small
placement guidewire must be reliably observed at all times.
The sterile components of the Impella® 2.5 System can be used only if the
sterilization indicators show that the contents have been sterilized, the packaging is
not damaged, and the expiration date has not elapsed.
Do
NOT
remove the Impella® 2.5 Catheter over the length of the guidewire.
Handle with care. The Impella® 2.5 Catheter can be damaged during removal from
packaging, preparation, insertion, and removal. Do
NOT
bend, pull, or place excess
pressure on the catheter or mechanical components at any time.
Do
NOT
touch the inlet or outlet areas of the catheter and avoid manual
compression of the inlet cannula assembly while placing the device.
Do not kink or clamp the Impella® 2.5 Catheter or the 13 Fr peel-away introducer.
OVERVIEW
You will need the following materials to complete the setup before starting the case:
• 500 cc bag of D20 with 50 IU of heparin per cc. (Recommended)
Sensitive Medical Device
®
The Impella
is a sensitive medical device
with a microaxial pump with
extremely fine tolerances.
In particular, the inflow and
outflow areas of the distal
and proximal areas of the
pump assembly may be
damaged if subjected to
strong external forces.
2.5 Catheter
®
CONTROLLER WITH THE IMPELLA
®
2.5
• IV ush solution (NaCl) with pressure bag and 96 inches of sterile infusion line.
NOTE: The distal end of the infusion line must remain sterile.
®
The Impella
Controller displays eight screens of instructions to lead you through a case start:
• Initial setup
• Prime purge tubing
• Enter purge uid data
®
• Plug Impella
• Prime Impella
into controller
®
purge lumen
• Prime blood pressure lumen
®
• Pre-insertion Impella
®
• Impella
test successful
test
INITIAL SETUP
1. Open the purge cassette package.
2. Using sterile technique, connect the purge fluid spike to the spike connector on the
end of the purge fluid supply line. Secure the yellow luer connector and pass the purge
®
cassette and supply line to the Impella
Controller operator.
Shaded Steps
All shaded steps require sterile
technique.
Impella® Controller with Impella® 2.5
5.3

Selector Knob Function
3. Open the purge cassette door by pressing the release on the left side of the controller.
®
Insert the purge cassette into the Impella
Controller (as shown in Figure 5.3).
The selector knob function
here is NOT circular (you
CANNOT keep turning
the knob in one direction
to scroll between START
and STOP). Turn the knob
clockwise to scroll to STOP
and counterclockwise to scroll
to START.
• The purge cassette snaps into a molded compartment on the front of the controller.
Follow the diagram on the inside of the purge cassette door for proper placement.
• Slide the purge pressure transmitter into the slot to the right of the purge cassette
until it snaps into place.
• Extend the purge line and close the purge cassette door. There is sufcient room
around the edges of the purge cassette door so that it will not pinch the purge line as
it exits.
Figure 5.3 Inserting Purge Cassette into Impella® Controller
4. Spike the purge fluid bag with the purge fluid spike attached to the end of the supply
line and hang the purge fluid bag.
5. Press the NEXT soft button to advance to the next screen.
PRIME PURGE TUBING
1. Use the selector knob to scroll to START on the screen and press the knob to begin
priming the purge line. The controller will start the priming process at a bolus rate of
250 mL/hr or greater.
®
2. When purge fluid is discharged from the tip of the yellow Impella
connector at the end
of the purge line, scroll to STOP and press the selector knob to stop the flow of purge
fluid.
3. Press NEXT after selecting STOP to proceed to entering purge fluid data.
If you press the BACK button on this screen, the controller will return to step 1 of priming the
purge tubing.
If you do not press STOP within 60 seconds of pressing START, you will get a message that the
purger has stopped. Press BACK if additional purging is required. If the purge fluid has been
discharged from the purge tubing and priming is complete, press NEXT.
5.4
Instructions for Use

ENTER PURGE FLUID DATA
®
The Impella
Controller displays a table of recommended default values for the purge fluid
(see Figure 5.4).
5 USING THE IMPELLA
System Timeout
1. To select the default values displayed on the screen, scroll to OK below the table and
press the selector knob. This will select those values and automatically advance you to
the next screen.
The purger will stop after 60
seconds if the user does not
press STOP. If this happens,
press BACK for additional
priming or NEXT if purge fluid
has been discharged.
®
CONTROLLER WITH THE IMPELLA
®
2.5
Figure 5.4 Default Values for Purge Fluid
2. To change the purge fluid information, scroll to the appropriate item push the selector
knob to select it. Then scroll through the values and push the selector knob to make a
new selection. The controller will use the default values if no other selections are made.
• Purge uid can be set to 100 mL, 250 mL, 500 mL (the default), or 1000 mL.
• Dextrose concentration can be set to 5%, 10%, 20% (the default), 30%, or 40%.
• Heparin concentration can be set to 0, 5, 10, 12.5, 15, 20, 25, or 50 units/mL. (50
units/mL is the default.)
Impella® Controller with Impella® 2.5
5.5

PLUG IMPELLA® INTO CONTROLLER
Important Step
Snapping the plastic hook on
the pressure reservoir to the
connector cable is important
to prevent the tube from
kinking.
Time Delay
Expect a 5 to 10 second
time delay after plugging
in the Impella
before the Impella
automatically advances to the
next screen.
Infusion Bag Pressure
®
pump and
®
Controller
1. Open the Impella® Catheter package using sterile technique and snap the plastic hook
(located on the pressure reservoir of the clear sidearm) to the connector cable as shown
in Figure 5.5.
Figure 5.5 Snapping Plastic Hook to Connector Cable
2. Pass the sterile white connector cable from the Impella® pump off the sterile field. Line
®
up the notch on the Impella
the front of the Impella
3. When the Impella
®
the Impella
flow icon appears on the screen. The controller automatically advances to
®
Controller detects that an operational Impella® pump is plugged in,
connector cable with the notch in the blue pump plug on
®
Controller and plug the cable into the controller.
the next screen.
If the infusion bag is
underinflated, the progress
bar will not be activated.
If the infusion bag is
overinflated, an alarm
will occur.
If a “Sensor Value not
Reliable” alarm appears while
priming the catheter, check
that the pressurized saline
bag is inflated to a pressure
between 300 and 350 mmHg
and not overinflated.
5.6
®
PRIME IMPELLA
PURGE LUMEN
1. Connect the yellow connector on the end of the purge line to the yellow luer connector
®
on the clear sidearm of the Impella
2. Select START to begin priming the Impella
pump.
®
purge lumen. The Impella® Controller will
start at a bolus rate of 250 mL/hour or greater.
®
3. When purge fluid is discharged from the Impella
pump, scroll to and select STOP.
When you press STOP, the bolus stops but purge fluid continues to flow at a low rate.
4. Press NEXT to advance to the next screen.
Instructions for Use

PRIME BLOOD PRESSURE LUMEN
1. Using sterile technique, connect the flush solution tubing to the red luer connector on
®
the red sidearm of the Impella
2. Blood pressure lumen priming starts automatically. Prime the Impella
pressure lumen by squeezing the white flush valve until the Impella
pump.
®
Catheter
®
Controller beeps.
(see Figure 5.6).
When the system detects the target flush solution pressure within the required amount
of time (60 seconds), the system will go to the next step automatically.
5 USING THE IMPELLA
®
CONTROLLER WITH THE IMPELLA
Figure 5.6 Squeezing the White Flush Valve to Prime
the Impella
®
Catheter Pressure Lumen
PRE-INSERTION IMPELLA® TEST
1. Select TEST to start the pre-insertion Impella® test.
The test runs for 2 seconds. When the system detects that the pump is spinning, it
automatically advances to the next step.
If the pre-insertion test fails, the system will instruct you to unplug the Impella
from the controller and disconnect the purge and flush lines from the Impella
®
connectors. You can then press NEXT to set up a new Impella
IMPELLA
®
TEST SUCCESSFUL
pump.
®
®
luer
®
2.5
1. This screen tells you that the Impella® test was successful. Press NEXT to finish Startup.
Impella® Controller with Impella® 2.5
5.7

Use Fluoroscopy for
Placement
INSERTING THE IMPELLA® 2.5 CATHETER
NOTE – Proper surgical procedures and techniques are the responsibility of
the medical professional. The described procedure is furnished for information
purposes only. Each physician must evaluate the appropriateness of the procedure
based on his or her medical training and experience, the type of procedure, and
the type of systems used.
®
Impella
will be compromised if
correct placement cannot
be confirmed. While
other imaging techniques,
such as transesophageal
echocardiography (TEE), can
help confirm the position
of the Impella
placement, TEE does not
allow visualization of the
entire catheter assembly and
is inadequate for reliably
placing the Impella
across the aortic valve.
Maintaining ACT
After insertion of the catheter
(and until explant), ACT
should be maintained at 160
to 180 seconds.
2.5 performance
®
2.5 after
®
2.5
Fluoroscopy is required to guide placement of the Impella® 2.5. The small placement
guidewire must be reliably observed at all times.
To prevent malfunction of the locking mechanism of the 13 Fr peel-away introducer,
do
NOT
hold the hemostatic valve while inserting into the artery.
Do not kink or clamp the Impella® 2.5 Catheter or the 13 Fr peel-away introducer.
Handle with care. The Impella® 2.5 Catheter can be damaged during removal from
packaging, preparation, insertion, and removal. Do
NOT
bend, pull, or place excess
pressure on the catheter or mechanical components at any time.
Do
NOT
touch the inlet or outlet areas of the catheter and avoid manual
compression of the inlet cannula assembly while placing the device.
1. Obtain access to the femoral artery.
2. Insert a 6–8 Fr introducer over the 0.035 guidewire (provided) to pre-dilate the vessel.
3. Remove the 6–8 Fr introducer over the 0.035 guidewire and insert the 13 Fr peel-away
introducer with dilator (see Figure 5.7). While inserting the 13 Fr introducer, hold the
shaft of the introducer to slide it into the artery.
5.8
Figure 5.7 Inserting the 13 Fr Peel-Away Introducer
4. Administer heparin. When the ACT is above 250, remove the 13 Fr dilator.
Instructions for Use

5. Insert a 6 Fr diagnostic catheter with diagnostic guidewire with no side holes (Judkins
Right, Multipurpose, or pigtail recommended, see Figure 5.8) into the 13 Fr introducer
and advance it over a diagnostic guidewire into the left ventricle.
Impella® 2.5 Use in Open
Heart Surgery
5 USING THE IMPELLA
®
CONTROLLER WITH THE IMPELLA
Figure 5.8 Inserting the 6 Fr Diagnostic Catheter
6. Remove the diagnostic guidewire and insert the supplied 0.018 in/260 cm placement
guidewire.
7. Advance the placement guidewire into the left ventricle until the floppy end and 3 to
4 cm of the stiffer part of the guidewire are visible in the left ventricle.
8. Remove the 6 Fr diagnostic catheter.
9. Wet the cannula with sterile water and backload the pigtail section of the catheter onto
the placement guidewire. One or two people can load the catheter on the guidewire.
One-person technique
a. Advance the guidewire into the Impella® Catheter and stabilize the cannula
between the fingers as shown in Figure 5.9. This prevents pinching of the inlet
port. The guidewire must exit the outlet port on the inner radius of the cannula,
as shown by the arrow in Figure 5.9 and in Figure 5.10. The catheter can be
hyperextended as necessary to ensure the guidewire exits on the inner radius of
the cannula.
If the Impella
the OR as part of open heart
surgery, manipulation may be
performed only through the
9 Fr steering catheter. Direct
manipulation of the pump
assembly through the aorta or
ventricle may result in serious
damage to the Impella
device and serious injury to
the patient.
Avoid Damaging Inflow
Area
During placement of the
Impella
care to avoid damage to the
inflow area while holding
the catheter and loading the
placement guidewire.
®
2.5 is used in
®
2.5 device, take
®
2.5
®
2.5
Two-person technique
b. The scrub assistant can help stabilize the catheter by holding the catheter proximal
to the motor. This will allow the implanting physician to visualize the inner radius.
The guidewire must exit the outlet port on the inner radius of the catheter, as
shown by the arrow in Figure 5.9 and in Figure 5.10. The physician can focus on
advancing the guidewire and, if the cannula needs to be hyperextended, the scrub
assistant is available to assist.
Impella® Controller with Impella® 2.5
5.9

Figure 5.9 Loading the Catheter on the Guidewire
Figure 5.10 Exiting of the Placement Guidewire from the Catheter
Do NOT Touch Inlet or
Outlet Areas
While feeding the Impella
through the 13 Fr introducer,
hold the device at the cannula
or motor housing. Do NOT
touch the inlet area or the
outlet area.
®
10. Advance the catheter through the hemostatic valve into the femoral artery
(see Figure 5.11) and along the placement guidewire into the left ventricle using a fixed-
wire technique. Follow the catheter under fluoroscopy as it is advanced into the left
ventricle, being careful not to coil the guidewire in the left ventricle.
Figure 5.11 Inserting the Impella® 2.5 Catheter
5.10
Instructions for Use

To prevent device failure, do not start the Impella® 2.5 Catheter until the guidewire
has been removed.
Do
NOT
remove the Impella® 2.5 Catheter over the length of the guidewire.
11. Remove the placement guidewire.
®
12. Confirm that a ventricular waveform is displayed on the Impella
Controller.
POSITIONING AND STARTING THE IMPELLA® 2.5
CATHETER
Retrograde flow will occur across the aortic valve if the Impella® 2.5 is set at a flow
rate of 0 L/min.
1. Place the catheter plug at the same level as the patient’s heart.
®
2. Confirm that a ventricular waveform is displayed on the Impella
(see Figure 5.12). If a ventricular waveform is not present, gently advance the
catheter forward until a ventricular waveform is present on the placement
signal screen.
Controller
5 USING THE IMPELLA
®
CONTROLLER WITH THE IMPELLA
®
2.5
Figure 5.12 Ventricular Waveform on Placement Signal Screen
Impella® Controller with Impella® 2.5
Importance of Proper
Pump Placement
When the pump is not
correctly placed, the patient
does not profit from the flow
rate shown on the controller
and there is no effective
unloading of the ventricle
(hydraulic short circuit).
5.11

3. Pull the catheter back until an aortic waveform is present on the placement signal
screen (see Figure 5.13).
4. When the aortic waveform is present, pull the catheter back an additional 4 cm.
(The distance between adjacent markings on the catheter is 1 cm.) The pump should
now be centered across the aortic valve.
Figure 5.13 Aortic Waveform on Placement Signal Screen
5. Press the TARGET FLOW soft button to open the flow icon (see Figure 5.14)
5.12
Figure 5.14 Selecting Target Flow
Instructions for Use

6. Turn the selector knob to change the flow rate from 0 L/min to 0.5 L/min.
7. Press the selector knob to select the new flow rate.
8. The flow icon in the lower left corner of the screen begins rotating when the Impella
®
pump begins to operate.
9. Increase the flow rate to 2.5 L/min to confirm correct and stable placement. Placement
should be verified with fluoroscopy and with the placement signal screen (see Figure
5.15).
5 USING THE IMPELLA
Check Positioning at
Maximum Flow
When the flow rate is
increased to maximum flow,
the device has a tendency
to be drawn into the
ventricle. Check positioning
at maximum flow to ensure
proper placement throughout
the performance level setting
range.
®
CONTROLLER WITH THE IMPELLA
Figure 5.15 Confirming Placement on the Placement Signal Screen
10. After correct placement has been achieved, adjust the flow rate to the desired flow.
Flow rates of TBD L/min will default back to TBD L/min after 5 minutes.
11. Reposition the catheter as necessary.
®
2.5
Impella® Controller with Impella® 2.5
5.13

Alternative to Waiting
Until ACT < 150
If you do not want to wait
until ACT is below 150
seconds before removing
the device, you can remove
the device and exchange the
peel-away sheath with a non
peel-away sheath and dilator
over the wire. Then you
can wait until ACT is below
150 seconds and remove
the sheath without risk of
bleeding.
USE OF THE REPOSITIONING INTRODUCER
AND THE 13 Fr PEEL-AWAY INTRODUCER
To prevent failure of the 13 Fr peel-away introducer, remove the 13 Fr peel-away
introducer prior to transport when activated clotting time (ACT) is less than 150
seconds.
1. Flush the sidearm of the repositioning introducer located on the catheter shaft.
2. Carefully flush the sidearm of the 13 Fr introducer and remove the 13 Fr peel-away
introducer completely from the artery over the catheter shaft and apply manual
pressure above the puncture site.
3. Grasp the two “wings” and bend back until the valve assembly comes apart. Continue
to peel the two wings until the introducer is completely separated from the catheter
shaft (see Figure 5.16).
5.14
Figure 5.16 Removing the 13 Fr Peel-Away Introducer
4. Attach a stopcock and flush the repositioning sheath prior to advancing the sheath.
5. Place two deadend caps on the stopcock to prevent further usage. The sideport should
not be used to give medication or draw blood because the blood could potentially clot.
Pressure bags should not be connected to the sideport of the repositioning sheath. If
a pressure bag is connected, the sideport must have an infusion pump or flow limiting
valve in place to control the amount of fluid administered to the patient.
6. Slide the repositioning introducer over the catheter shaft and advance it into the artery
to the yellow eyelet.
7. Secure the yellow section of the repositioning introducer by suturing it to the skin using
the provided eyelet.
Instructions for Use

8. Slide the proximal end of the anticontamination sleeve onto the yellow section of
the repositioning introducer. Lock the anchoring ring in place by turning it clockwise.
Secure the catheter shaft in place by tightening the connected anchoring ring.
9. Carefully extend the anticontamination sleeve to maximum length and secure the end
by tightening the distal anchoring ring.
PURGER PROCEDURES
5 USING THE IMPELLA
®
CONTROLLER WITH THE IMPELLA
When replacing the purge cassette, the replacement process must be completed
within 4 minutes. The Impella® 2.5 Catheter may be damaged if replacement takes
longer than 4 minutes.
There are four procedures for maintaining the Impella® purge system:
• Purge system change (cassette and purge uid)
• Purge uid change
• Purge cassette change
• De-air purge system
Each procedure can be accessed using the PURGE SYSTEM soft button.
This section describes each of those purger procedures.
PURGE SYSTEM CHANGE
These are the steps you will follow to change out the purge cassette and purge fluid.
1. The purge system change out procedure begins with delivery of a bolus to the pressure
reservoir so that the reservoir can maintain purge pressure during the change out. After
the bolus is delivered, the controller automatically proceeds to the next screen.
Replacement Time
If the purge flow is more
than 7 mL/hr or the dextrose
concentration is less than
20%, replacement time
will be less than 4 minutes.
Replacement should always
be performed as quickly as
possible.
®
2.5
2. Disconnect and remove the used purge cassette. If you do not remove the cassette
within 20 seconds, the system will cancel and exit the purge system change procedure.
3. Insert a new purge cassette into the controller. Be sure to slide the purge pressure
transmitter into place and extend the purge line through the gap in the purge cassette
door when you close the door.
4. Turn the selector knob to select START. Press the knob to begin priming the purge line.
5. When purge fluid is discharged from the purge line, scroll to STOP and press the
selector knob.
6. Press NEXT to advance to the next screen and enter purge fluid information.
7A. To select the default purge fluid values displayed on the screen, scroll to and select OK.
This will select those values and automatically advance you to the next screen.
Impella® Controller with Impella® 2.5
5.15

7B. To change the purge fluid information, scroll to the appropriate item and push the
selector knob to select it. Then scroll through the values and push the selector knob to
make a new selection. (Refer to “Entering Purge Fluid Data” in the Startup discussion
at the beginning of this section for a listing of purge fluid, dextrose concentration, and
heparin concentration options.) The controller will use the default values if no other
selections are made.
8. Connect the yellow luer connector on the end of the purge line to the yellow luer
®
connector on the clear sidearm of the Impella
pump.
9. Press NEXT to exit and complete the procedure.
Purge Solution Bottles
If the purge solution is
supplied in bottles, follow the
same procedure as if supplied
in bags.
PURGE FLUID CHANGE
These are the steps you will follow to change only the purge fluid.
1. The purge fluid change procedure begins with delivery of a bolus to the pressure
reservoir so that the reservoir can maintain purge pressure during the change. After the
bolus is delivered, the controller automatically proceeds to the next screen.
2. Replace the purge fluid bag. Press NEXT to advance to the next screen and enter purge
fluid information.
3A. To select the default purge fluid values displayed on the screen, scroll to and select OK.
This will select those values and automatically advance you to the next screen.
3B. To change the purge fluid information, scroll to the appropriate item and push the
selector knob to select it. Then scroll through the values and push the selector knob to
make a new selection. (Refer to “Entering Purge Fluid Data” in the Startup discussion
at the beginning of this section for a listing of purge fluid, dextrose concentration, and
heparin concentration options.) The controller will use the default values if no other
selections are made.
PURGE CASSETTE CHANGE
5.16
These are the steps you will follow to change only the purge cassette.
1. The purge cassette change procedure begins with delivery of a bolus to the pressure
reservoir so that the reservoir can maintains purge pressure during the change. After
the bolus is delivered, the controller automatically proceeds to the next screen.
2. Disconnect and remove the used purge cassette. If you do not remove the cassette
within 20 seconds, the system will cancel and exit the purge cassette change
procedure.
3. Insert a new purge cassette into the controller. Be sure to slide the purge pressure
transmitter into place and extend the purge line through the gap in the purge cassette
door when you close the door.
4. Turn the selector knob to select START. Press the knob to begin priming the purge line.
Instructions for Use

5. When purge fluid is discharged from the purge line, scroll to STOP and press the
selector knob.
6. Press NEXT to advance to the next screen and connect the purge cassette to the
®
Impella
pump.
7. Connect the yellow luer connector on the end of the purge line to the yellow luer
®
connector on the clear sidearm of the Impella
pump.
8. Press NEXT to exit and complete the procedure.
5 USING THE IMPELLA
DE-AIR PURGE SYSTEM
These are the steps you will follow to de-air the purge system. This procedure starts
automatically when the “Air in Purge System” alarm occurs.
1. Make sure that the purge fluid bag is NOT empty or inverted.
®
2. Disconnect the purge line from the yellow luer connector on the Impella
pump.
3. Press START to initiate the de-air function. The system automatically advances to the
next screen.
4. The next screen explains that the de-air procedure is taking place. Wait until the air
is removed from the purge system and the system automatically advances to the next
screen.
5. Confirm that the purge fluid has been discharged from the purge line. If it has not,
press BACK to repeat the air removal process.
6. Connect the yellow luer connector on the end of the purge line to the yellow luer
®
connector on the clear sidearm of the Impella
pump.
7. Press EXIT to complete the de-air procedure.
®
CONTROLLER WITH THE IMPELLA
®
2.5
Impella® Controller with Impella® 2.5
5.17

Purge Pressure
Purge pressure can range
from 300mmHg to
1100 mmHg.
The Impella
algorithm maintains purge
pressure within 50 mmHg of
the target pressure.
®
Controller purge
TROUBLESHOOTING THE PURGE SYSTEM
LOW PURGE PRESSURE
If at any time during the course of support with the Impella®, the Impella®
Controller alarms “Impella Failure: Sudden Purge Pressure Drop,” follow the
instructions below.
1. Inspect the purge system for leaks.
2. If there are no leaks, change to a purge fluid with a higher dextrose concentration. To
do this, open the PURGE SYSTEM menu and select “Purge Fluid Change”. Follow the
instructions on the screen. (Refer to “Purger Procedures” earlier in this section.)
3. If the pressure stabilizes, no other action is required.
If the purge pressure is not stable, proceed to Step 4.
4. If the low purge pressure alarms remain unresolved for more than 5 minutes, this may
be a sign of pump damage. Complete the following steps immediately:
a. Open the flow icon and reduce the flow rate to 0.5 L/min.
®
b. Slowly pull back on the Impella
aorta (approximately 20 cm for an average size patient; 1 cm marks are available
on the catheter).
2.5 Catheter until the pump is in the descending
Unresolved High Purge
Pressure Alarms
High purge pressure alarms
that are not resolved by the
recommendations provided
could be an indication of a
kink in the catheter located
within the artery. In this
case, the motor is no longer
being purged and will
eventually stop. Clinicians
should consider replacing the
®
Impella
pump.
c. Confirm that the pump is still running at a flow rate of 0.5 L/min. Open the flow
icon and reduce the flow rate to 0 L/min.
®
d. Stop the Impella
e. Remove the Impella
pump and turn off the purge system.
®
2.5 Catheter with the use of fluoroscopic imaging. If no
fluoroscopy is available, leave the pump in the descending aorta until imaging is
available for visual assistance with pump integrity during removal.
HIGH PURGE PRESSURE
®
If the purge pressure exceeds 1100 mmHg, the Impella
Controller displays the high purge
pressure alarm message.
1. Inspect the purge system for kinks in the tubing.
2. If pressure remains high, decrease the concentration of dextrose in the purge solution
(eg, dextrose 10%).
PURGE SYSTEM BLOCKED
If a “Purge System Blocked” alarm occurs, the purge fluid flow stops.
1. Check the purge system tubing for kinks or blockages.
5.18
2. Decrease the concentration of dextrose in the purge solution.
3. Replace the purge cassette.
Instructions for Use

PATIENT WEANING
Weaning the patient from the Impella® 2.5 is at the discretion of the physician. (For more
information, refer to “Guidelines for Explant” in Section 6: Patient Management Topics.)
The following weaning protocols are provided as guidance only.
5 USING THE IMPELLA
RAPID WEANING
1. Initiate rapid weaning by decreasing the Impella® flow rate by 0.5 L/min at intervals of
NOT
several minutes. Do
decrease the Impella® flow rate below 0.5 L/min as long as
the pump is in the ventricle.
®
2. When the Impella
0.5 L/min for
3. If the patient’s hemodynamics remain stable, decrease the Impella
flow rate has been reduced by 0.5 L/min, maintain the patient at
at least 10 minutes
before discontinuing circulatory support.
®
flow rate to
0.1 L/min, pull the catheter into the aorta, and stop the pump by reducing the flow rate
to 0 L/min.
4. Explant the catheter.
5. Follow institutional guidelines for percutaneous arterial closure.
®
6. Disconnect the connector cable from the Impella
Controller and turn the controller
OFF.
SLOW WEANING
®
1. Initiate slow weaning by decreasing the Impella
NOT
2 to 3 hours. Do
decrease the Impella® flow rate below 0.5 L/min as long as the
flow rate by 0.5 L/min at intervals of
pump is in the ventricle.
®
2. When the Impella
0.5 L/min for
3. If the patient’s hemodynamics remain stable, decrease the Impella
flow rate has been reduced to 0.5 L/min, maintain the patient at
at least 2 to 3 hours
before discontinuing circulatory support.
®
flow rate to
0.1 L/min, pull the catheter into the aorta, and stop the pump by reducing the flow rate
to 0 L/min.
Remove the Impella® 2.5
With Care
®
CONTROLLER WITH THE IMPELLA
®
2.5
4. Explant the catheter.
5. Follow institutional guidelines for percutaneous arterial closure.
®
6. Disconnect the connector cable from the Impella
Controller and turn the controller
OFF.
Impella® Controller with Impella® 2.5
Removal of the Impella
device must be completed
with care to avoid damage to
the pump assembly.
®
2.5
5.19


6 PATIENT MANAGEMENT TOPICS
PATIENT MANAGEMENT OVERVIEW ............................................................ 6.1
GENERAL PATIENT CARE CONSIDERATIONS ..............................................6.1
TRANSPORT WITHIN THE HOSPITAL ............................................................6.1
RIGHT HEART FAILURE ................................................................................ 6.2
CARDIOPULMONARY RESUSCITATION (CPR) .............................................. 6.2
DEFIBRILLATION .......................................................................................... 6.3
ECG INTERFERENCE ..................................................................................... 6.3
LATEX .......................................................................................................... 6.3
POSITIONING AND PLACEMENT DEVICES .................................................. 6.3
SUCTION ...................................................................................................... 6.4
HEMOLYSIS .................................................................................................. 6.4
UNDERSTANDING AND MANAGING IMPELLA
®
POSITION ALARMS ...........6.6
Correct Position ...............................................................................................6.6
®
Impella
Fully in Ventricle ................................................................................6.7
®
Impella
Completely in the Aorta or Inlet and Outlet Area
in Ventricle and Pressure Port in Aorta .............................................................6.8
Low Native Heart Pulsatility .............................................................................6.9
®
Impella
Outlet Area on or Near Aortic Valve ................................................. 6.10
REPOSITIONING GUIDE ..............................................................................6.10
DATA SNAP SHOT RECORDING ...................................................................6.13
INFUSION HISTORY ....................................................................................6.13
OPERATING THE IMPELLA
®
2.5 WITHOUT HEPARIN IN
THE PURGE SOLUTION................................................................................6.14
GUIDELINES FOR EXPLANT ........................................................................6.14
HOW TO CHANGE TO BACKUP CONTROLLER .............................................6.15
EMERGENCY SHUTDOWN PROCEDURE .....................................................6.15


PATIENT MANAGEMENT OVERVIEW
The information and instructions in this section of the manual are not intended to supersede
established medical procedures concerning patient care. Best practice, as determined by the
medical community, should always be observed. In each case, the clinician must determine
whether the application of information provided is appropriate for the particular clinical setting.
GENERAL PATIENT CARE CONSIDERATIONS
• Do not raise the head of the bed to higher than a 30-degree angle
• Use knee immobilizer as needed to maintain access site straight
• Perform dressing changes per hospital protocol, using aseptic technique
• Assess access site for bleeding and hematoma
®
• Be careful not to pull on the Impella
to another
Catheter when transferring a patient from one bed
6 PATIENT MANAGEMENT TOPICS
• Monitor pedal pulses
TRANSPORT WITHIN THE HOSPITAL
Patients supported with the Impella® 2.5 System may require transport within the hospital for
®
various reasons. Transport can be safe and simple for patients supported with Impella
Considerations for transport within the hospital:
• The Impella
®
Controller and Impella® 2.5 System are designed to operate on battery
power for at least 1 hour.
• Conrm that the battery capacity displayed on the controller is 100%.
• If transport time might be longer than 1 hour, bring an extension cord or conrm
that you will be able to connect the controller to AC power once you arrive at your
destination.
®
• Use care when rolling the Impella
Controller cart, and pay close attention when going
over thresholds and through elevator doors.
®
• Do not stress the Impella
pump cable from the controller to the Impella® red plug.
2.5.
Note: If the Impella
®
Controller is allowed to discharge completely, and the system shuts down
due to low battery, the controller will need to charge for an extended period of time before the
controller will turn back on.
Impella® Controller with Impella® 2.5
6.1

RIGHT HEART FAILURE
The Impella® 2.5 is a left-side support device only. Patients being supported by the Impella® 2.5
should be monitored for signs of right heart failure.
Caregivers should monitor the patient closely for the following potential signs of right heart
failure:
®
• Reduced output from the Impella
• Suction alarms
• Elevated lling pressures (CVP)
• Signs of liver failure
• Elevated pulmonary pressures
If the patient is exhibiting signs of right heart failure, the clinical team should assess the need for
biventricular support.
2.5
CARDIOPULMONARY RESUSCITATION (CPR)
Cardiopulmonary resuscitation (CPR) should be initiated immediately if indicated for any patient
®
being supported by the Impella
If CPR is indicated, the following actions are recommended:
1. Initiate CPR per hospital protocol.
2. Reduce the Impella
3. When cardiac function has been restored:
a. Return the flow rate to previous level.
b. Assess placement signals on the controller.
Note:
• During CPR, placement monitoring and ow calculations will not be accurate.
• If ows do not return to pre-CPR values, verify proper placement of device and sufcient
filling of left ventricle. If placement and filling are not satisfactory, it may be an indication
that the device has been damaged.
2.5.
®
2.5 flow rate to 1 L/min.
6.2
Instructions for Use

DEFIBRILLATION
6 PATIENT MANAGEMENT TOPICS
During defibrillation, do
NOT
touch the pump, cables, or Impella® Controller.
Patients supported by the Impella® 2.5 System can be defibrillated. However, caregivers should
use caution during defibrillation to ensure they do not touch the pump, cables, or controller.
ECG INTERFERENCE
Operating the Impella® Controller may cause interference with electrocardiogram (ECG) signals.
Please check the electrode pads and leads for good fixation and contact. If interference persists,
activate the 50/100 Hz band-elimination filter or the 60/120 Hz band-elimination filter (also
known as notch filter) on your ECG device. The filter frequency will be based on the AC power
frequency for the country in which you are operating the equipment. If your ECG device does
®
not have the appropriate filters, disconnect the Impella
to obtain an undisturbed signal. Please observe the battery status while running the Impella
Controller off AC power.
Controller temporarily from AC power
®
LATEX
The Impella® Controller, Impella® 2.5, and all accessories approved by Abiomed, are
100% latex free.
POSITIONING AND PLACEMENT DEVICES
High quality fluoroscopic imaging is the best method for determining pump position and is
required for pump placement.
Alternative methods for determining pump position include:
• Portable C-Arm uoroscopy
• Transesophageal echocardiography (TEE)
• Chest x-ray
Use Fluoroscopy for
Placement
®
Impella
will be compromised if
correct placement cannot
be confirmed. While
other imaging techniques,
such as transesophageal
echocardiography (TEE), can
help confirm the position
of the Impella
placement, TEE does not
allow visualization of the
entire catheter assembly and
is inadequate for reliably
placing the Impella
across the aortic valve.
2.5 performance
®
2.5 after
®
2.5
Impella® Controller with Impella® 2.5
6.3

Notes on Imaging:
All imaging technology represents the anatomy in two dimensions (2D). It is not possible to
assess the interactions between the device and the intraventricular anatomy that occur in three
dimensions (3D). If a positioning alarm occurs, Abiomed strongly recommends that the device be
repositioned, even if the imaging view shows correct position. Abiomed strongly recommends
®
using fluoroscopy to guide placement and positioning of the Impella
Circulatory Support device.
Alternative imaging techniques, such as transesophageal echocardiography (TEE), can be useful
to confirm the position of the Impella
®
2.5 after placement. However, TEE is inadequate to
reliably perform correct placement across the aortic valve. TEE does not allow visualization of the
entire catheter assembly.
SUCTION
Suction may occur if the blood volume available for the Impella® 2.5 pump is inadequate or
®
restricted. Suction limits the amount of support that the Impella
and results in a decrease in arterial pressure and cardiac output. It can damage blood cells,
leading to hemolysis. It may also be an indicator of right heart failure.
2.5 can provide to the patient
If this alarm occurs, follow the recommended actions in the alarm display by decreasing
the flow rate.
1. Check the pump for correct positioning using imaging. Reposition the device by rotating
or moving it into or out of the ventricle slightly. Either or both of these actions could
help move the inlet of the device away from the interior ventricular wall.
2. Assess patient’s fluid intake and output to confirm adequate volume status.
3. Confirm right ventricular function by assessing CVP or right side function on echo.
If CVP is not an option, check the pulmonary artery diastolic pressure to assess the
patient volume status.
4. Return flow rate to pre-alarm setting.
HEMOLYSIS
When blood is pumped, it is subjected to mechanical forces. Depending on the strength of the
blood cells and the amount of force applied, the cells may be damaged, allowing hemoglobin
to enter the plasma. Pumping forces can be generated by a variety of medical procedures
including heart lung bypass, hemodialysis, or ventricular support device (VAD) support. Patient
conditions—including pump position, pre-existing medical conditions, and small left ventricular
volumes—may also play a role in patient susceptibility to hemolysis.
6.4
Instructions for Use

Patients who develop high levels of hemolysis may show signs of decreased hemoglobin levels,
dark or blood-colored urine, and in some cases, acute renal failure. Plasma-free hemoglobin
(PfHgb) is the best indicator to confirm whether a patient is exposed to an unacceptable level
of hemolysis. Clinically significant hemolysis is defined as two consecutive PfHgb measurements
greater than 40 mg/dL. For surgical patients, the first measurements must be at least 72 hours
post-implant.
Management technique may differ depending on the underlying cause of hemolysis. Table 6.1
provides guidance for various circumstances.
Table 6.1 Guide for Managing Hemolysis in Various Circumstances
Condition Controller Indicators Clinical Indicators Management
Impella® inlet area
in close proximity
to intraventricular
wall
Wrong pump
position
Higher than
needed flow
setting
Inadequate filling
volume
Pre-existing
patient conditions
or other medical
procedures
Note on imaging: All imaging technology represents the anatomy in two dimensions (2D). It is not possible to assess the
interactions between the device and the intraventricular anatomy that occur in three dimensions (3D). Abiomed strongly
recommends that the device be repositioned, even if the imaging view shows correct position.
• Suction alarms
• Lower than expected ows
• Position alarms
• Suction alarms
• Lower than expected ows
• There may be no controller
indicators
• Suction alarms
• Position alarms
• Suction alarms
• Lower than expected ows
N/A • Patient past medical history
Imaging (see note) • Reposition the device by rotating or moving the
Imaging (see note) • Reposition the device by rotating or moving the
• Normal hemodynamics
• Native recovery
• Low CVP
• Low PCWP
• Low AOP
• High PA pressures
• Right heart failure
• High urine output
• Increased bleeding or chest
tube drainage
• Current procedures or
treatments
device into or out of the ventricle slightly. Either or
both of these actions could help move the inlet of
the device away from the intraventricular wall.
• If repositioning will be delayed, reduce the ow
rate if tolerated by patient hemodynamics. Return
to the target flow rate after repositioning.
• Reassess position after ow rate has returned to
desired target value.
device into or out of the ventricle slightly. Either or
both of these actions could help move the inlet of
the device away from the intraventricular wall.
• If repositioning will be delayed, reduce the ow
rate if tolerated by patient hemodynamics. Return
to the target flow rate after repositioning.
• Reassess position after ow rate has returned to
desired target value.
1. Reduce flow rate until patient pressure starts to
drop.
2. Slowly increase flow rate.
• Reduce the ow rate if tolerated by patient
hemodynamics.
• Correct I and O balance.
• Consider giving volume; additional volume will
expand the end systolic ventricular volume.
• Reduce PA pressure.
• Improve right heart function.
6 PATIENT MANAGEMENT TOPICS
Impella® Controller with Impella® 2.5
6.5

UNDERSTANDING AND MANAGING IMPELLA® POSITION
ALARMS
The Impella® Controller continuously monitors the catheter based on the placement signal and
the motor current.
• Placement Signal:
• Motor Current:
Is the signal characteristic of aortic or ventricular pressure?
Is the signal “pulsatile” or “attened”?
If the system alarms with one of the positioning alarms described below, fluoroscopic imaging is
the best method for conrming position. You can also use TEE or a standard chest X-ray.
If the Impella
®
is either partly (just the pigtail) or completely in the ventricle, reposition the device
under imaging guidance. If guidance is not available, use the repositioning guide to reestablish
proper placement. (The repositioning guide is discussed later in this section.)
®
If the Impella
is completely out of the ventricle, do not attempt to reposition the device across
the valve without a guidewire.
The following pages describe possible placement conditions and the associated signal
characteristics and alarm messages as well as actions to take for each.
CORRECT POSITION
If the Impella® 2.5 Catheter is in the correct position, the waveform screen will appear as shown
in Figure 6.1.
6.6
Figure 6.1 Correct Catheter Position
Instructions for Use

IMPELLA® FULLY IN VENTRICLE
®
If the Impella
2.5 Catheter is fully in the ventricle, the following alarm will appear:
Pump Position Wrong
In this situation, the waveform screen will appear as shown in Figure 6.2.
Repositioning Guide
The repositioning guide can
also be used for correcting
®
Impella
positioning.
6 PATIENT MANAGEMENT TOPICS
Figure 6.2 Catheter Fully in Ventricle
Actions to take:
1. Under fluoroscopic guidance, if available, reduce the flow rate to 0.5 L/min and
®
carefully pull back the Impella
Catheter until the aortic waveform signal is showing.
2. When you see the aortic waveform signal, pull the catheter back an additional 4 cm.
Impella® Controller with Impella® 2.5
6.7

IMPELLA® COMPLETELY IN THE AORTA or INLET AND OUTLET AREA
IN VENTRICLE AND PRESSURE PORT IN AORTA
®
If the Impella
2.5 Catheter is completely in the aorta or if the inlet and outlet areas are in the
ventricle and the pressure port is in the aorta, the following alarm will appear:
Pump Position Wrong
In this situation, the waveform screen will appear as shown in Figure 6.3.
Figure 6.3 Impella® Completely in the Aorta or Inlet and Outlet Area
in Ventricle and Pressure Port in Aorta
Actions to take:
1. Under fluoroscopic guidance, determine the pump position.
2. Reduce flow rate to 0.5 L/min and reposition the pump as necessary.
3. If fluoroscopic imaging is not available, reposition the pump according to the
repositioning guide.
4. If step 3 does not provide correct positioning, check the pump position by imaging
methods (fluoroscopy, TEE, or chest x-ray).
6.8
Instructions for Use

LOW NATIVE HEART PULSATILITY
®
In a situation of low native heart pulsatility, the Impella
Controller may not be able to
determine the pump position. You may see the following alarm:
Pump position unknown due to low pulsatility.
In this situation, the waveform screen will appear as shown in Figure 6.4.
6 PATIENT MANAGEMENT TOPICS
Figure 6.4 Pump Position Unknown Due to Low Pulsatility
[Waveform TBD; Motor Current y-axis scale to be revised]
Actions to take:
1. Assess cardiac function.
Impella® Controller with Impella® 2.5
6.9

IMPELLA® OUTLET AREA ON OR NEAR AORTIC VALVE
®
If the Impella
2.5 Catheter outlet area is on or near the aortic valve, the pump may be too deep
in the ventricle. The following alarm will appear:
Impella Outflow Blocked
In this situation, the waveform screen will appear as shown in Figure 6.5.
Figure 6.5 Impella® Outlet Area on or near Aortic Valve
Actions to take:
1. Assess and adjust pump position under fluoroscopic guidance, if available.
2. If fluoroscopic guidance is not available, reduce the flow rate to 0.5 L/min and gently
pull the catheter back 2 cm and see if the condition resolves.
REPOSITIONING GUIDE
Abiomed strongly recommends using fluoroscopy to guide placement and positioning of the
®
Impella
available, you can use the repositioning guide to correct the position of the Impella
across the aortic valve. The repositioning guide provides information about the current position
of the Impella
Circulatory Support device. However, if fluoroscopy or other imaging guidance is not
®
pump
®
pump and the actions required to reposition the pump.
6.10
Instructions for Use

To use the repositioning guide:
1. Press MENU and scroll to “Start Repositioning Guide.” Press the selector knob to
initiation the repositioning guide algorithm.
Figure 6.6 shows the first screen of the repositioning guide. Follow the instructions in
the white instructional display area under the headline “Repositioning Guide Active”.
6 PATIENT MANAGEMENT TOPICS
Figure 6.6 First Repositioning Guide Screen
2. Press OK to confirm reduction in flow rate. The system will reduce flow rate to 1 L/min.
®
3. Push the Impella
pump forward until the placement signal shows ventricular pressure
(see Figure 6.7).
Figure 6.7 Second Repositioning Guide Screen
Impella® Controller with Impella® 2.5
6.11

4. Pull the Impella® pump back until the placement signal shows aortic pressure
(see figure 6.8).
Figure 6.8 Third Repositioning Guide Screen
5. Pull the Impella® pump back 4 marks on the catheter. Each mark equals 1 centimeter.
6. Exit the Repositioning Guide using the Exit Repositioning Guide soft button (see
Figure 6.9). When you exit, the controller returns to the original flow rate level.
6.12
Figure 6.9 Exit Repositioning Guide Screen
Instructions for Use

DATA SNAP SHOT RECORDING
The Impella® Controller can save real-time operating data for later analysis using the Data Snap
Shot feature. Data Snap Shot is automatically turned on during certain alarm conditions to
capture data for analysis. The user can also manually turn on the feature at any time to capture
data for later analysis.
To manually access the Data Snap Shot feature:
1. Press MENU and scroll to “Data Snap Shot”. Press the selector knob.
2. The controller records data for a predefined period of 10 minutes. To stop recording
data before the 10-minute time-out, select “Stop Data Snapshot” from the MENU.
INFUSION HISTORY
The Impella® Controller has an Infusion History screen that displays the amount of heparin and
dextrose infused each hour. The calculations begin when the case start procedure is completed
and flow rate is greater than 0. The system stores at least 8 hours of data. Figure 6.10 shows a
sample Infusion History screen.
6 PATIENT MANAGEMENT TOPICS
Saving Snap Shot Data
If you select “Start Data Snap
Shot” while the controller is
already saving snap shot data,
the controller will start saving
data to a different snap shot
file. Note: Old data will be
overwritten by new data if the
snap shot data memory is full.
Figure 6.10 Infusion History Screen
As you can see, the current time period is displayed at the top of the list. This entry provides the
heparin and dextrose infusion rates from the top of the current hour to the current time.
Impella® Controller with Impella® 2.5
6.13

OPERATING THE IMPELLA® 2.5 WITHOUT HEPARIN IN
THE PURGE SOLUTION
The Impella® 2.5 is designed to be operated with a purge solution that contains heparin.
Operation of the system without heparin in the purge solution has not been tested. In the
event that a patient is intolerant to heparin, due to heparin-induced thrombocytopenia (HIT) or
bleeding, physicians should use their clinical judgment in assessing the risks versus benefits of
®
operating the Impella
System without heparin.
If it is in the best interest of the patient to operate the system without heparin, the dextrose
solution is still required, and physicians should consider an alternative anticoagulant delivered
systemically.
Do not add any alternative anticoagulant (such as a direct thrombin inhibitor) to the purge
solution. The Impella
®
2.5 has not been tested with any alternative anticoagulants present
in the purge solution.
GUIDELINES FOR EXPLANT
Patients being supported with the Impella® 2.5 System should be evaluated for explant on a
regular basis.
To evaluate patients for explant, reduce the Impella
®
2.5 flow rate and look for the following
signs of native heart recovery:
• AO and CVP pressure remain stable
• Native ejections are visible on the patient pressure monitor
• Native ejections increase after volume loading challenge
• Echocardiography reveals pronounced aortic valve opening
If physicians see these signs of native heart recovery and the patient has demonstrated stable,
ongoing recovery—including stable organ (eg, liver, kidney, lung) function—the patient should
be considered for explant.
®
If the patient does not meet the criteria for explant, the patient should remain on Impella
2.5
support, or be transitioned to a longer term device.
6.14
Instructions for Use

HOW TO CHANGE TO BACKUP CONTROLLER
A backup Impella® Controller should be available at all times when a patient is on support. In
®
the event that the controller fails, follow the steps below to transition the Impella
backup controller.
1. Confirm that the backup controller is powered ON and ready.
2. Transfer the purge cassette and purge solution from the primary controller to the
backup controller.
®
3. Remove the white Impella
connector cable from the primary controller and plug it into
the pump plug on the front of the backup controller.
®
4. Once the Impella
pump is connected to the backup controller, the “Quick Start”
message will appear on the screen asking the user to confirm re-starting the Impella
2.5 at the previously set flow rate.
®
5. Press OK within 10 seconds to confirm restarting the Impella
2.5 at the previously set
flow rate.
pump to the
6 PATIENT MANAGEMENT TOPICS
®
EMERGENCY SHUTDOWN PROCEDURE
1. Press and hold the black power button for 30 seconds.
2. An “Emergency Shutdown Imminent” alarm will sound at 15 seconds.
3. The controller will shut down after 30 seconds.
®
NOTE: The Impella
4. Restart the controller.
pump will continue running at the last setting.
Impella® Controller with Impella® 2.5
6.15


7 CLEANING, STORAGE, DISPOSAL,
AND RETURNS
CLEANING .................................................................................................... 7.1
Cleaning the Impella
STORING THE IMPELLA
DISPOSING OF THE PUMP AND ACCESSORIES (EU) ..................................... 7.1
RETURNING AN IMPELLA
®
Controller and Connector Cable .................................... 7.1
®
CONTROLLER ........................................................ 7.1
®
PUMP TO ABIOMED (US) ................................... 7.1


CLEANING
CLEANING THE IMPELLA® CONTROLLER AND CONNECTOR CABLE
7 CLEANING, STORAGE, DISPOSAL, AND RETURNS
• Clean the Impella
®
Controller keypad and display with 70% isopropyl alcohol, or soap and
water.
®
• Clean the Impella
Controller housing with mild detergent.
• Do not allow any uids to enter the connector sockets.
• Clean the connector cable with 70% isopropyl alcohol.
STORING THE IMPELLA® CONTROLLER
The Li-Ion batteries must be charged for 10 hours prior to system operation. After
being unplugged, the Impella® Controller will operate for at least 60 minutes after
the batteries have been fully charged.
• Place the Impella® Controller on a horizontal surface to prevent falling.
• Connect the AC power cord to an AC outlet.
• The battery may be destroyed if the Impella® Controller is stored with a depleted battery.
Storing the Controller
®
To keep the Impella
Controller battery charged,
the controller should be
plugged into an AC outlet and
switched to the ON position
when it is stored.
DISPOSING OF THE PUMP AND ACCESSORIES (EU)
The Impella® pump and connector cable are disposable items that must be disposed of in
accordance with hospital regulations for blood contaminated materials.
The Impella
®
Controller is marked according to Directive 2002/96/EEC. Devices sold within the
EEC can be returned to Abiomed Europe GmbH for correct disposal.
RETURNING AN IMPELLA® PUMP TO ABIOMED (US)
To return an Impella® pump to Abiomed, contact your local Clinical Consultant for an Abiomedapproved return kit (part number 0046-4000).* The kit includes instructions for returning the
pump to Abiomed.
* Only available in the United States
Impella® Controller with Impella® 2.5
7.1

7.2
Instructions for Use

8 TERMINOLOGY, ABBREVIATIONS,
AND SYMBOLS
TERMINOLOGY, ABBREVIATIONS, AND SYMBOLS ......................................8.1


TERMINOLOGY, ABBREVIATIONS, AND SYMBOLS
Table 8.1 Terminology and Abbreviations
Hz Hertz
Pump identification number
Pump housing Enclosure of the Impella
Pump
Purge pressure Pressure present in the Impella® 2.5 and in the infusion line
Purge system Impella® purge cassette used for rinsing the Impella® 2.5
Retrograde flow
V Volt
VA Volt ampere (Watt)
Table 8.2 Symbols
Identification number of the pump; stated on the package
label and on the display screen
®
Central delivery unit of the Impella® 2.5, consisting of the
motor, motor housing, pump housing, cannula with inlet and
outlet, and pigtail at the tip
Reverse flow through the intracardiac pump when the pump
is at a standstill (eg, regurgitation)
8 TERMINOLOGY, ABBREVIATIONS, AND SYMBOLS
2009-02
Caution; comply with documents (eg, Instructions for Use)
Defibrillator-proof type CF equipment
Keep dry
Storage temperature (eg, 0°C to 30°C)
Declares conformity with directive 93/42/EEC for medical
devices
Date of manufacture (eg, February 2009)
Protect from sunlight!
Symbol for lot designation; the manufacturer’s lot
designation must be stated after the LOT symbol
Impella® Controller with Impella® 2.5
8.1

Table 8.2 Symbols (cont’d)
REF 123456 Abiomed part number (eg, part number 123456)
SN 123456 Manufacturer’s serial number (eg, serial number 123456)
Non Sterile! The product is not sterile
2010-06
Use-by date (eg, use before June 2010)
Do not reuse
Sterilized using ethylene oxide
Electric scrap; must be disposed of separately. Must not be
disposed of as domestic waste.
Protective Earth
Protection Class II equipment
8.2
Instructions for Use

9 SYSTEM SPECIFICATIONS
IMPELLA® CONTROLLER MECHANICAL ........................................................9.1
IMPELLA
®
CONTROLLER ELECTRICAL ..........................................................9.1
EQUIPMENT DESIGN ....................................................................................9.2
EQUIPMENT CLASSIFICATIONS ....................................................................9.2
FEDERAL COMMUNICATIONS COMMISSION (FCC) NOTICE ........................9.3
ELECTROMAGNETIC COMPATIBILITY ...........................................................9.3
PATIENT ENVIRONMENT ..............................................................................9.6
WHITE CONNECTOR CABLE ..........................................................................9.8
PUMP PARAMETERS .....................................................................................9.8
IMPELLA
®
2.5 DIMENSIONS .........................................................................9.9


IMPELLA® CONTROLLER MECHANICAL
Parameter Specification
Temperature Operating: 10°C to 40°C (50°F to 104°F)
Storage: –15°C to 50°C (5°F to 122°F)
Relative Humidity Operating: 95%
Storage: 95%
Atmospheric Pressure Operating: 8000 ft (750 hPa) to –1000 ft (1050 hPa)
Storage: 18,000 ft (500 hPa) to –1000 ft (1050 hPa)
Dimensions Height: 351 mm
Width: 443 mm
Depth: 236 mm
Dimensions –
Packaged
Weight Maximum: 11.8 kg (26.1 lbs)
Weight – Packaged Maximum: 13.6 kg (30 lbs)
Maintenance and
repair interval
Height: 508 mm
Width: 559 mm
Depth: 406 mm
12 months
(Work must be performed by technicians authorized by Abiomed)
9 SYSTEM SPECIFICATIONS
IMPELLA® CONTROLLER ELECTRICAL
AC operation 100-230 VAC (nominal); 47-63 Hz; 1.1A
Internal battery operation 14.4 VDC (nominal); lithium ion
Characteristic values
Max. power consumption under load
Device fuse
Running time without AC power with fully
charged batteries
Electrical system Installation in accordance with pertinent
120 VA
2x2 A slow-blow
At least 60 minutes (charging duration of at least
10 hours)
regulations is required for use in medical facilities
(eg, VDE 0100, VDE 0107, or ICE stipulations).
Observe country-specific regulations and national
deviations.
Impella® Controller with Impella® 2.5
9.1

EQUIPMENT DESIGN
The Impella® Controller conforms to the applicable requirements of the following standards:
• UL 60601-1 (2003), 1st Edition
Medical Electrical Equipment, Part 1: General
Requirements for Safety
• CAN/CSA C22.2 No 601.1-M90 (1990; Reafrmed 2005), 2nd Edition
Medical Electrical
Equipment, Part 1: General Requirements for Safety
• EN 60601-1 (1990), 2nd Edition
Medical Electrical Equipment, Part 1: General
Requirements for Safety + A1(93) + A2(95) + A1.3(96)
• IEC 60601-1 (1988), 2nd Edition
Medical Electrical Equipment, Part 1: General
Requirements for Safety + A1(91) + A2(95)
• IEC 60601-1-2 (2001),
Medical Electrical Equipment, Part 1-2: General Requirements for
Safety – Collateral Standard: Electromagnetic Compatibility – Requirements and Tests
• IEC 60601-1-4 (2000), Edition 1.1 Consolidated Edition
Medical Electrical Equipment,
Part 1-4: General Requirements for Safety – Collateral Standard: Programmable Electrical
Medical Systems
• IEC 60601-1-1, (2000/12/01), 2nd Edition
Medical Electrical Equipment, Part 1-1: General
Requirements for Safety – Collateral Standard: Safety Requirements for Medical Electrical
Systems
• IEC 60601-1-8, (2003/08/01), Edition 1
Medical Electrical Equipment, Part 1-8: General
Requirements for Safety – Collateral Standard: General Requirements, Tests and Guidance
for Alarm Systems in Medical Electrical Equipment and Medical Electrical Systems
• IEC 60601-1-6, (2004/06/01), Edition 1
Medical Electrical Equipment, Part 1-6: General
Requirements for Safety – Collateral Standard: Usability
EQUIPMENT CLASSIFICATIONS
Type of protection against electric
shock
Degree of protection against electric
shock for Impella® Controller
Mode of operation Continuous.
Degree of protection against explosion
hazard
Degree of protection against harmful
ingress of water
IEC 60601-1: Class I degree of protection: CF
defibrillation-proof and internally powered. Relies not
only on basic insulation against shock but also includes
additional protection. Accomplished by providing means
for connecting the equipment to the protective earth
conductor of the fixed wiring of the installation in a way
that prevents
if basic insulation
Class I Equipment.
Not suitable for use in the presence of a flammable
anesthetic mixture with air or with oxygen or nitrous
oxide. Also not suitable for use in an oxygen-enriched
atmosphere.
IEC 60529: IPX1 protected against dripping water.
accessible metal parts
fails
.
from becoming live
9.2
Instructions for Use

FEDERAL COMMUNICATIONS COMMISSION (FCC) NOTICE
This device complies with Part 15 of the FCC Rules. Operation is subject to the following two
conditions:
1. This device may not cause harmful interference.
2. This device must accept any interference received, including interference that may cause
undesired operation.
Changes or modifications not expressly approved by Abiomed, Inc. could void the user’s
authority to operate this device.
ELECTROMAGNETIC COMPATIBILITY
Medical electrical equipment needs special precautions regarding EMC and needs
to be installed and put into service according to the electromagnetic compatibility
(EMC) information provided in the accompanying documents.
9 SYSTEM SPECIFICATIONS
Portable and mobile RF communications equipment can affect medical electrical
equipment.
The equipment or system should not be used adjacent to or stacked with other
equipment. If adjacent or stacked use is necessary, the equipment or system should
be observed to verify normal operation in the configuration in which it will be used.
Use of cables, other than those sold by Abiomed, may result in increased emissions
or decreased immunity of the Impella
The Impella® Controller uses RFID (radio frequency identification) to identify and
communicate with the purge cassette. Other equipment may interfere with the
Impella® Controller even if that other equipment complies with CISPR emission
requirements.
®
Controller.
NOTE: The EMC tables and other guidelines that are included in this manual provide
information to the customer or user that is essential in determining the suitability of the
equipment or system for the electromagnetic environment of use, and in managing the
electromagnetic environment of use permit the equipment or system to perform to its intended
use without disturbing other equipment and systems or non-medical electrical equipment.
Impella® Controller with Impella® 2.5
9.3

TABLE 201
Guidance and Manufacturer’s Declaration – Emissions, All Equipment and Systems
The Impella® Controller is intended for use in the electromagnetic environment specified below.
The customer or user of the Impella® Controller should ensure that it is used in such an environment.
Emissions Test Compliance Electromagnetic Enforcement – Guidance
RF Emissions
CISPR 11
Harmonics
IEC 61000-3-2
Flicker
IEC 61000-3-3
Group 1
Class A
Class A The Impella® Controller is suitable for use in all
Complies
The Impella® Controller uses RF energy only for its
internal function. Therefore, its RF emissions are very
low and are not likely to cause any interference in
nearby electronic equipment.
establishments, other than domestic and those directly
connected to the public low-voltage power supply
network that supplies buildings used for domestic
purposes.
TABLE 202
Guidance and Manufacturer’s Declaration – Immunity
The Impella® Controller is intended for use in the electromagnetic environment specified below. The
customer or user of the Impella® Controller should ensure that it is used in such an environment.
Electromagnetic
Environment –
Guidance
Floors should be wood,
concrete, or ceramic tile. If
floors are synthetic, the relative
humidity should be at least
30%.
Mains power quality should be
that of a typical commercial or
hospital environment.
Mains power quality should be
that of a typical commercial or
hospital environment.
Mains power quality should be
that of a typical commercial
or hospital environment.
If the user of the Impella®
Controller requires continued
operation during power
mains interruptions, it is
recommended that the
Impella® Controller be powered
from an uninterruptible power
supply or battery.
fields should be that of a
typical location in a typical
commercial or hospital
environment.
Immunity Test
Electrostatic
Discharge (ESD) IEC
61000-4-2
Electrical Fast
Transient/burst
IEC 61000-4-4
Surge
IEC 61000-4-5
Voltage dips, short
interruptions and
voltage variations
on power supply
input lines
IEC 61000-4-11
Power Frequency
50/60Hz Magnetic
Field
IEC 61000-4-8
IEC 60601
Test Level
±8 kV contact
±15 kV air
±2 kV Mains
±1 kV for input/
output lines
±1 kV Differential
±2 kV Common
> 95% dip for 0.5
cycle
60% dip for 5 cycles
30% dip for 25
cycles
> 95% dip for 5
seconds
3 A/m 3 A/m Power frequency magnetic
Compliance
Level
±8 kV contact
±15 kV air
±2 kV Mains
±1 kV for input/
output lines
±1 kV Differential
±2 kV Common
> 95% dip for 0.5
cycle
60% dip for 5 cycles
30% dip for 25
cycles
> 95% dip for 5
seconds
9.4
Instructions for Use

TABLE 203
PED )1/5.3(=
PED )1/5.3(=
PED )1/7(=
Guidance and Manufacturer’s Declaration – Emissions,
Equipment and Systems that are Life-Supporting
The Impella® Controller is intended for use in the electromagnetic environment specified
below. The customer or user of the Impella® Controller should ensure that it is used in such an
environment.
Electromagnetic
Environment –
Guidance
Portable and mobile RF
communications equipment
should be separated from
the Impella® Controller by no
less than the recommended
separation distances
calculated/listed below:
Immunity Test
Conducted RF
IEC 61000-4-6
Radiated RF
IEC 60601
Test Level
10 Vrms
150 kHz to 80 MHz
10 V/m
Compliance
Level
V1 = 10 Vrms
150 kHz to 80 MHz
E1 = 10 V/m
9 SYSTEM SPECIFICATIONS
IEC 61000-4-3
80 MHz to 2.5 GHz
80 MHz to 2.5 GHz
80 to 800 MHz
800 MHz to 2.5 GHz
Where P is the maximum
power rating in watts and
D is the recommended
separation distance in
meters.
Field strengths from fixed
transmitters, as determined
by an electromagnetic site
survey, should be less than
the compliance levels (V1
and E1).
Interference may occur in
the vicinity of equipment
containing a transmitter.
Impella® Controller with Impella® 2.5
9.5

PATIENT
Pd 3333.2
Pd 3333.2
Pd 3333.2
ENVIRONMENT
Recommended Separation Distances Between Portable and Mobile
RF Communications Equipment and the Impella
TABLE 205
®
Controller,
Equipment and Systems that are Life-Supporting
The Impella® Controller is intended for use in the electromagnetic environment in which radiated
The Impella® Controller and the
disturbances are controlled. The customer or user of the Impella® Controller can help prevent
components of the Impella
electromagnetic interference by maintaining a minimum distance between portable and mobile RF
Controller System are approved
communications equipment and the Impella® Controller as recommended below, according to the
for use within the patient
maximum output power of the communications equipment.
environment defined in IEC
Maximum
60601-1-1 and in the figure
Output Power
below.
(Watts)
®
Recommended Separation Distances
for the Impella® Controller (m)
150 KHz to 80 MHz
80 to 800 MHz
800 MHz to 2.5 GHz
Figure 9.1 Impella®
Controller Patient
Environment
0.01 0.11667 0.11667 0.23333
0.1 0.36894 0.36894 0.73785
1 1.1667 1.1667 2.3333
10 3.6894 3.6894 7.3785
100 11.667 11.667 23.333
=
=
RFID Transmitter / Receiver Specifications
Frequency 13.56 MHz
Receiver bandwidth TBD
Effective radiated power TBD
Modulation TBD
=
9.6
Instructions for Use
 Loading...
Loading...